User login
Mesh erosion less likely in prior vaginal prolapse repair
CHICAGO – The presence of scar tissue may protect against synthetic mesh erosion following vaginal prolapse repair, according to findings from a retrospective case-control study.
The findings provide further support for the existing American College of Obstetricians and Gynecologists recommendation that vaginal mesh repair should be reserved for women with recurrent prolapse, and may be helpful for preoperative counseling in these patients, according to Dr. Nicholas Kongoasa of Saint Peter’s University Hospital, New Brunswick, N.J.
"Women are four times less likely to have mesh erosion if they have previously undergone prolapse repair, and that mesh should be reserved for those who fail primary repair," Dr. Kongoasa said in an interview.
Dr. Kongoasa was unable to make his presentation at the scheduled session at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Patients in the study included all those who underwent mesh-augmented pelvic floor repair between June 1, 2008, and Dec. 31, 2011. All surgeries were performed by a single surgeon using polypropylene mesh. Of 810 mesh-augmented pelvic floor repair surgeries, 688 involved no prior vaginal prolapse surgery and 142 were in patients with a prior vaginal prolapse repair.
The two groups did not differ with respect to mean operating time, intraoperative complications, postoperative complications, hospital stay, or prolapse recurrence. Also, they were similar in terms of demographics and pelvic organ prolapse quantification staging with the exception of prior hysterectomy in the prior surgery group.
During follow-ups of 1-4.5 years, mesh erosion occurred in 10.6% of those with no prior vaginal prolapse surgery, and in 2.8% of those with prior vaginal prolapse surgery (odds ratio, 4.1).
Among those with mesh erosion, no differences were seen between those with and without prior surgery with respect to time to diagnosis or location and size of erosion.
"The large number of cases and the high odds ratio warrant that this subject be further investigated by future prospective studies," he said.
The study was limited by its retrospective nature and the fact that some patients who experienced complications may have sought care elsewhere.
As for why previous surgery may protect against mesh erosion, "my personal theory is that there is generally less blood supply to the previously operated area, and this may lead to less inflammation and reaction to the foreign body," he said.
Dr. Kongoasa reported having no disclosures.
CHICAGO – The presence of scar tissue may protect against synthetic mesh erosion following vaginal prolapse repair, according to findings from a retrospective case-control study.
The findings provide further support for the existing American College of Obstetricians and Gynecologists recommendation that vaginal mesh repair should be reserved for women with recurrent prolapse, and may be helpful for preoperative counseling in these patients, according to Dr. Nicholas Kongoasa of Saint Peter’s University Hospital, New Brunswick, N.J.
"Women are four times less likely to have mesh erosion if they have previously undergone prolapse repair, and that mesh should be reserved for those who fail primary repair," Dr. Kongoasa said in an interview.
Dr. Kongoasa was unable to make his presentation at the scheduled session at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Patients in the study included all those who underwent mesh-augmented pelvic floor repair between June 1, 2008, and Dec. 31, 2011. All surgeries were performed by a single surgeon using polypropylene mesh. Of 810 mesh-augmented pelvic floor repair surgeries, 688 involved no prior vaginal prolapse surgery and 142 were in patients with a prior vaginal prolapse repair.
The two groups did not differ with respect to mean operating time, intraoperative complications, postoperative complications, hospital stay, or prolapse recurrence. Also, they were similar in terms of demographics and pelvic organ prolapse quantification staging with the exception of prior hysterectomy in the prior surgery group.
During follow-ups of 1-4.5 years, mesh erosion occurred in 10.6% of those with no prior vaginal prolapse surgery, and in 2.8% of those with prior vaginal prolapse surgery (odds ratio, 4.1).
Among those with mesh erosion, no differences were seen between those with and without prior surgery with respect to time to diagnosis or location and size of erosion.
"The large number of cases and the high odds ratio warrant that this subject be further investigated by future prospective studies," he said.
The study was limited by its retrospective nature and the fact that some patients who experienced complications may have sought care elsewhere.
As for why previous surgery may protect against mesh erosion, "my personal theory is that there is generally less blood supply to the previously operated area, and this may lead to less inflammation and reaction to the foreign body," he said.
Dr. Kongoasa reported having no disclosures.
CHICAGO – The presence of scar tissue may protect against synthetic mesh erosion following vaginal prolapse repair, according to findings from a retrospective case-control study.
The findings provide further support for the existing American College of Obstetricians and Gynecologists recommendation that vaginal mesh repair should be reserved for women with recurrent prolapse, and may be helpful for preoperative counseling in these patients, according to Dr. Nicholas Kongoasa of Saint Peter’s University Hospital, New Brunswick, N.J.
"Women are four times less likely to have mesh erosion if they have previously undergone prolapse repair, and that mesh should be reserved for those who fail primary repair," Dr. Kongoasa said in an interview.
Dr. Kongoasa was unable to make his presentation at the scheduled session at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Patients in the study included all those who underwent mesh-augmented pelvic floor repair between June 1, 2008, and Dec. 31, 2011. All surgeries were performed by a single surgeon using polypropylene mesh. Of 810 mesh-augmented pelvic floor repair surgeries, 688 involved no prior vaginal prolapse surgery and 142 were in patients with a prior vaginal prolapse repair.
The two groups did not differ with respect to mean operating time, intraoperative complications, postoperative complications, hospital stay, or prolapse recurrence. Also, they were similar in terms of demographics and pelvic organ prolapse quantification staging with the exception of prior hysterectomy in the prior surgery group.
During follow-ups of 1-4.5 years, mesh erosion occurred in 10.6% of those with no prior vaginal prolapse surgery, and in 2.8% of those with prior vaginal prolapse surgery (odds ratio, 4.1).
Among those with mesh erosion, no differences were seen between those with and without prior surgery with respect to time to diagnosis or location and size of erosion.
"The large number of cases and the high odds ratio warrant that this subject be further investigated by future prospective studies," he said.
The study was limited by its retrospective nature and the fact that some patients who experienced complications may have sought care elsewhere.
As for why previous surgery may protect against mesh erosion, "my personal theory is that there is generally less blood supply to the previously operated area, and this may lead to less inflammation and reaction to the foreign body," he said.
Dr. Kongoasa reported having no disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Vaginal mesh repair should be reserved for women with recurrent prolapse.
Major finding: Mesh erosion occurred in 10.6% of those without and 2.8% of those with prior vaginal prolapse surgery (OR, 4.10).
Data source: A retrospective case-control study involving 810 repairs.
Disclosures: Dr. Kongoasa reported having no disclosures.
Johnson & Johnson halts power morcellator sales, for now
Ethicon, a Johnson & Johnson company, has temporarily halted sales of its laparoscopic power morcellators for the treatment of uterine fibroids, following concerns that the devices could spread cancerous tissue in women with unsuspected uterine sarcoma.
The company is suspending global sales, distribution, and promotion of its three morcellation devices until the role of morcellation for patients with symptomatic fibroid disease is redefined by the Food and Drug Administration (FDA) and the medical communities.
The suspended products include the Gynecare Morcellex Tissue Morcellator, the Morcellex Sigma Tissue Morcellator System, and the Gynecare X-tract Tissue Morcellator.
"Ethicon morcellation devices have always included cautions in their instructions for use about the potential spread of malignant (or suspected malignant) tissue," the company said in a statement. "However, interpretation of the available epidemiological evidence is complex, and it is difficult to diagnose certain malignancies in advance of surgery."
On April 17, the FDA issued a safety communication to patients and physicians warning that if laparoscopic power morcellation is performed in women with unsuspected uterine sarcoma, there is a risk that the procedure could spread the cancerous tissue within the abdomen and pelvis, significantly worsening the patient’s chances of long-term survival.
"For this reason, and because there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids."
The FDA recommended that physicians not use laparoscopic uterine power morcellation in women with known or suspected uterine cancer and that they carefully consider all the available treatment options for women with symptomatic uterine fibroids.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Ethicon, a Johnson & Johnson company, has temporarily halted sales of its laparoscopic power morcellators for the treatment of uterine fibroids, following concerns that the devices could spread cancerous tissue in women with unsuspected uterine sarcoma.
The company is suspending global sales, distribution, and promotion of its three morcellation devices until the role of morcellation for patients with symptomatic fibroid disease is redefined by the Food and Drug Administration (FDA) and the medical communities.
The suspended products include the Gynecare Morcellex Tissue Morcellator, the Morcellex Sigma Tissue Morcellator System, and the Gynecare X-tract Tissue Morcellator.
"Ethicon morcellation devices have always included cautions in their instructions for use about the potential spread of malignant (or suspected malignant) tissue," the company said in a statement. "However, interpretation of the available epidemiological evidence is complex, and it is difficult to diagnose certain malignancies in advance of surgery."
On April 17, the FDA issued a safety communication to patients and physicians warning that if laparoscopic power morcellation is performed in women with unsuspected uterine sarcoma, there is a risk that the procedure could spread the cancerous tissue within the abdomen and pelvis, significantly worsening the patient’s chances of long-term survival.
"For this reason, and because there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids."
The FDA recommended that physicians not use laparoscopic uterine power morcellation in women with known or suspected uterine cancer and that they carefully consider all the available treatment options for women with symptomatic uterine fibroids.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Ethicon, a Johnson & Johnson company, has temporarily halted sales of its laparoscopic power morcellators for the treatment of uterine fibroids, following concerns that the devices could spread cancerous tissue in women with unsuspected uterine sarcoma.
The company is suspending global sales, distribution, and promotion of its three morcellation devices until the role of morcellation for patients with symptomatic fibroid disease is redefined by the Food and Drug Administration (FDA) and the medical communities.
The suspended products include the Gynecare Morcellex Tissue Morcellator, the Morcellex Sigma Tissue Morcellator System, and the Gynecare X-tract Tissue Morcellator.
"Ethicon morcellation devices have always included cautions in their instructions for use about the potential spread of malignant (or suspected malignant) tissue," the company said in a statement. "However, interpretation of the available epidemiological evidence is complex, and it is difficult to diagnose certain malignancies in advance of surgery."
On April 17, the FDA issued a safety communication to patients and physicians warning that if laparoscopic power morcellation is performed in women with unsuspected uterine sarcoma, there is a risk that the procedure could spread the cancerous tissue within the abdomen and pelvis, significantly worsening the patient’s chances of long-term survival.
"For this reason, and because there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids."
The FDA recommended that physicians not use laparoscopic uterine power morcellation in women with known or suspected uterine cancer and that they carefully consider all the available treatment options for women with symptomatic uterine fibroids.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
VIDEO: HPV testing predicted to displace most Pap smears
CHICAGO – Dr. Laurie J. McKenzie, who is a member of the ACOG Committee on the Scientific Program and the medical faculties of the University of Texas and Baylor College of Medicine, Houston, interviews Dr. Michael M. Frumovitz of the University of Texas MD Anderson Cancer Center, Houston, the presenter of the John I. Brewer Memorial Lecture on cervical cancer screening.
During a video interview at the annual meeting of the American Congress of Obstetricians and Gynecologists, they discuss reductions in cervical dysplasia that have already been seen with HPV vaccination in Australia and note the barriers to HPV vaccination in the United States. Dr. Frumovitz predicts that HPV testing will ultimately replace Pap smears for primary screening in most cases and discusses the potential for high-resolution microendoscopy to change how cervical lesions are diagnosed and treated.
CHICAGO – Dr. Laurie J. McKenzie, who is a member of the ACOG Committee on the Scientific Program and the medical faculties of the University of Texas and Baylor College of Medicine, Houston, interviews Dr. Michael M. Frumovitz of the University of Texas MD Anderson Cancer Center, Houston, the presenter of the John I. Brewer Memorial Lecture on cervical cancer screening.
During a video interview at the annual meeting of the American Congress of Obstetricians and Gynecologists, they discuss reductions in cervical dysplasia that have already been seen with HPV vaccination in Australia and note the barriers to HPV vaccination in the United States. Dr. Frumovitz predicts that HPV testing will ultimately replace Pap smears for primary screening in most cases and discusses the potential for high-resolution microendoscopy to change how cervical lesions are diagnosed and treated.
CHICAGO – Dr. Laurie J. McKenzie, who is a member of the ACOG Committee on the Scientific Program and the medical faculties of the University of Texas and Baylor College of Medicine, Houston, interviews Dr. Michael M. Frumovitz of the University of Texas MD Anderson Cancer Center, Houston, the presenter of the John I. Brewer Memorial Lecture on cervical cancer screening.
During a video interview at the annual meeting of the American Congress of Obstetricians and Gynecologists, they discuss reductions in cervical dysplasia that have already been seen with HPV vaccination in Australia and note the barriers to HPV vaccination in the United States. Dr. Frumovitz predicts that HPV testing will ultimately replace Pap smears for primary screening in most cases and discusses the potential for high-resolution microendoscopy to change how cervical lesions are diagnosed and treated.
EXPERT ANALYSIS AT THE ACOG ANNUAL CLINICAL MEETING
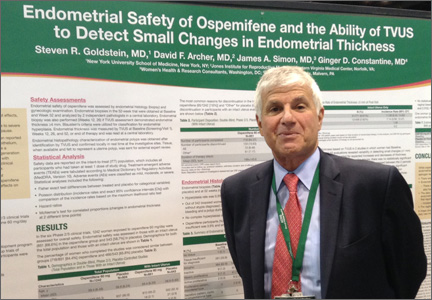
Ospemifene found to have minimal effects on the endometrium at 52 weeks
Ospemifene was FDA-approved in 2013 to treat moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy (VVA) due to menopause. This nonestrogenenic drug has tissue selective agonist/antagonist effects—a selective estrogen-receptor modulator (SERM). Tamoxifen, a first-generation SERM, increases the risk of endometrial cancer. However, the second-generation SERM raloxifene is not associated with this increased risk. In preclinical studies and clinical trials, ospemifene has been shown to exert positive effects on the vaginal epithelium and minimal effects on the endometrium.
Steven R. Goldstein, MD, from New York University School of Medicine, and colleagues set out to determine the endometrial safety of ospemifene in six Phase 2/3 clinical trials of postemenopausal women with up to 52 weeks of exposure to ospemifene 60 mg/day versus placebo.
Endometrial safety of the study drug was assessed in a total of 1,349 women with an intact uterus (851 in the ospemifene group vs 543 in the placebo group).
Results
Endometrial biopsies obtained at 52 weeks revealed a rate of endometrial hyperplasia of 0.3%.
Of 342 biopsied women, “there was a single case of a woman with simple hyperplasia,” says Dr. Goldstein. “She was 52 years old, had become menopausal at age 49 and had been taking hormone therapy for about 2 years before entering the trial. After 4 months of ospemifene, she had an episode of bleeding and was diagnosed with proliferative endometrium. The study drug was stopped with a plan to follow up in 3 months; 89 days later she had another episode of bleeding and was diagnosed with simple hyperplasia. She was treated with a single course of progestogen, the hyperplasia resolved, and then she was noted to have a benign polyp.”
No complex hyperplasias or carcinomas were found.
Ospemifene participants with histologic findings other than inactive, atrophic, or insufficient was 3.5% at 52 weeks, and this finding was similar to baseline endometrial biopsy results for placebo (4.0%).
The incidence of active and disordered type endometrial proliferation was less than 1% of participants treated with ospemifene. The vaginal bleeding incidence was similar in the treatment and placebo groups.
“This data tells me that this drug is clearly acting like its cousin raloxifene in the uterus, with virtually no active proliferation and no true hyperplasia. The FDA guidance for any of these products is less than 1% hyperplasia in 1 year, and there was a single case out of 342 biopsies, says Dr. Goldstein.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Reference
Goldstein SR, Archer DF, Simon JS, Constantine GD. Endometrial safety of ospemifene and the ability of transvaginal ultrasound to detect small changes in endometrial thickness. Poster presented at the American Congress of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting. Chicago, IL; April 28, 2014.
Ospemifene was FDA-approved in 2013 to treat moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy (VVA) due to menopause. This nonestrogenenic drug has tissue selective agonist/antagonist effects—a selective estrogen-receptor modulator (SERM). Tamoxifen, a first-generation SERM, increases the risk of endometrial cancer. However, the second-generation SERM raloxifene is not associated with this increased risk. In preclinical studies and clinical trials, ospemifene has been shown to exert positive effects on the vaginal epithelium and minimal effects on the endometrium.
Steven R. Goldstein, MD, from New York University School of Medicine, and colleagues set out to determine the endometrial safety of ospemifene in six Phase 2/3 clinical trials of postemenopausal women with up to 52 weeks of exposure to ospemifene 60 mg/day versus placebo.
Endometrial safety of the study drug was assessed in a total of 1,349 women with an intact uterus (851 in the ospemifene group vs 543 in the placebo group).
Results
Endometrial biopsies obtained at 52 weeks revealed a rate of endometrial hyperplasia of 0.3%.
Of 342 biopsied women, “there was a single case of a woman with simple hyperplasia,” says Dr. Goldstein. “She was 52 years old, had become menopausal at age 49 and had been taking hormone therapy for about 2 years before entering the trial. After 4 months of ospemifene, she had an episode of bleeding and was diagnosed with proliferative endometrium. The study drug was stopped with a plan to follow up in 3 months; 89 days later she had another episode of bleeding and was diagnosed with simple hyperplasia. She was treated with a single course of progestogen, the hyperplasia resolved, and then she was noted to have a benign polyp.”
No complex hyperplasias or carcinomas were found.
Ospemifene participants with histologic findings other than inactive, atrophic, or insufficient was 3.5% at 52 weeks, and this finding was similar to baseline endometrial biopsy results for placebo (4.0%).
The incidence of active and disordered type endometrial proliferation was less than 1% of participants treated with ospemifene. The vaginal bleeding incidence was similar in the treatment and placebo groups.
“This data tells me that this drug is clearly acting like its cousin raloxifene in the uterus, with virtually no active proliferation and no true hyperplasia. The FDA guidance for any of these products is less than 1% hyperplasia in 1 year, and there was a single case out of 342 biopsies, says Dr. Goldstein.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Ospemifene was FDA-approved in 2013 to treat moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy (VVA) due to menopause. This nonestrogenenic drug has tissue selective agonist/antagonist effects—a selective estrogen-receptor modulator (SERM). Tamoxifen, a first-generation SERM, increases the risk of endometrial cancer. However, the second-generation SERM raloxifene is not associated with this increased risk. In preclinical studies and clinical trials, ospemifene has been shown to exert positive effects on the vaginal epithelium and minimal effects on the endometrium.
Steven R. Goldstein, MD, from New York University School of Medicine, and colleagues set out to determine the endometrial safety of ospemifene in six Phase 2/3 clinical trials of postemenopausal women with up to 52 weeks of exposure to ospemifene 60 mg/day versus placebo.
Endometrial safety of the study drug was assessed in a total of 1,349 women with an intact uterus (851 in the ospemifene group vs 543 in the placebo group).
Results
Endometrial biopsies obtained at 52 weeks revealed a rate of endometrial hyperplasia of 0.3%.
Of 342 biopsied women, “there was a single case of a woman with simple hyperplasia,” says Dr. Goldstein. “She was 52 years old, had become menopausal at age 49 and had been taking hormone therapy for about 2 years before entering the trial. After 4 months of ospemifene, she had an episode of bleeding and was diagnosed with proliferative endometrium. The study drug was stopped with a plan to follow up in 3 months; 89 days later she had another episode of bleeding and was diagnosed with simple hyperplasia. She was treated with a single course of progestogen, the hyperplasia resolved, and then she was noted to have a benign polyp.”
No complex hyperplasias or carcinomas were found.
Ospemifene participants with histologic findings other than inactive, atrophic, or insufficient was 3.5% at 52 weeks, and this finding was similar to baseline endometrial biopsy results for placebo (4.0%).
The incidence of active and disordered type endometrial proliferation was less than 1% of participants treated with ospemifene. The vaginal bleeding incidence was similar in the treatment and placebo groups.
“This data tells me that this drug is clearly acting like its cousin raloxifene in the uterus, with virtually no active proliferation and no true hyperplasia. The FDA guidance for any of these products is less than 1% hyperplasia in 1 year, and there was a single case out of 342 biopsies, says Dr. Goldstein.
MORE NEWS and HIGHLIGHTS from ACOG's 2014 ANNUAL CLINICAL MEETING
Survey: Most average-risk pregnant women preferred NIPT to invasive testing
Adding infertility assessment and treatment to your practice
Delivery notes after shoulder dystocia often lack critical elements
Reference
Goldstein SR, Archer DF, Simon JS, Constantine GD. Endometrial safety of ospemifene and the ability of transvaginal ultrasound to detect small changes in endometrial thickness. Poster presented at the American Congress of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting. Chicago, IL; April 28, 2014.
Reference
Goldstein SR, Archer DF, Simon JS, Constantine GD. Endometrial safety of ospemifene and the ability of transvaginal ultrasound to detect small changes in endometrial thickness. Poster presented at the American Congress of Obstetricians and Gynecologists (ACOG) Annual Clinical Meeting. Chicago, IL; April 28, 2014.
VIDEO: Dr. Rosanne Kho: Selecting patients for minimally invasive vaginal surgery.
CHICAGO – Dr. Rosanne M. Kho discussed patient selection for vaginal approaches in an interview with Dr. Daniel M. Breitkopf of the Mayo Clinic in Rochester, Minn., at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Dr. Kho of the Mayo Clinic in Phoenix noted that there are only a few contraindications to the vaginal approach and emphasized the importance of incorporating lessons from robotic and minimally invasive surgery into vaginal hysterectomy. Dr. Kho warned of an impending health care crisis as a result of inadequate training in vaginal approaches.
On Twitter @maryjodales
CHICAGO – Dr. Rosanne M. Kho discussed patient selection for vaginal approaches in an interview with Dr. Daniel M. Breitkopf of the Mayo Clinic in Rochester, Minn., at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Dr. Kho of the Mayo Clinic in Phoenix noted that there are only a few contraindications to the vaginal approach and emphasized the importance of incorporating lessons from robotic and minimally invasive surgery into vaginal hysterectomy. Dr. Kho warned of an impending health care crisis as a result of inadequate training in vaginal approaches.
On Twitter @maryjodales
CHICAGO – Dr. Rosanne M. Kho discussed patient selection for vaginal approaches in an interview with Dr. Daniel M. Breitkopf of the Mayo Clinic in Rochester, Minn., at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Dr. Kho of the Mayo Clinic in Phoenix noted that there are only a few contraindications to the vaginal approach and emphasized the importance of incorporating lessons from robotic and minimally invasive surgery into vaginal hysterectomy. Dr. Kho warned of an impending health care crisis as a result of inadequate training in vaginal approaches.
On Twitter @maryjodales
EXPERT ANALYSIS AT THE ACOG ANNUAL CLINICAL MEETING
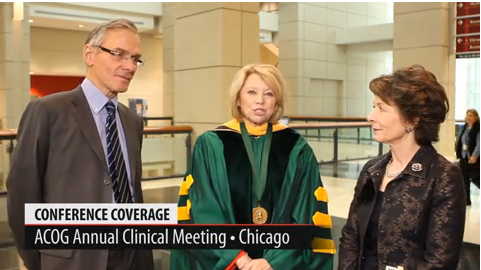
ACOG President Dr. Jeanne A. Conry interviews Dr. Leslie Regan and Dr. Mark Hanson
CHICAGO – "Every Woman, Every Time," Dr. Jeanne A. Conry’s presidential theme, was front and center at the President’s Program at the annual meeting the American Congress of Obstetricians and Gynecologists. In this exclusive video interview, Dr. Conry spoke with Dr. Lesley Regan about her presentation on basic rights to health care and Dr. Mark Hanson about the role of obstetrician-gynecologists in preventive health initiatives to reduce noncommunicable diseases. Prof. Regan leads global women’s health efforts for the Royal College of Obstetricians & Gynaecologists in London and chairs the Committee for Sexual and Reproductive Rights for the International Federation of Gynecology and Obstetrics.
Prof. Hanson, director of the academic unit of human development and health at the University of Southhampton in the United Kingdom, has focused his work on new ways to reduce disease processes and improve health by championing preventive interventions during preconception, throughout pregnancy, and in infancy and childhood.
The program also included Dr. Tyrone Hayes, professor of biology at the University of California, Berkeley, whose research findings on the impact of environmental chemicals on health demonstrate why industry must bear the burden of proof for safety before products are introduced.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – "Every Woman, Every Time," Dr. Jeanne A. Conry’s presidential theme, was front and center at the President’s Program at the annual meeting the American Congress of Obstetricians and Gynecologists. In this exclusive video interview, Dr. Conry spoke with Dr. Lesley Regan about her presentation on basic rights to health care and Dr. Mark Hanson about the role of obstetrician-gynecologists in preventive health initiatives to reduce noncommunicable diseases. Prof. Regan leads global women’s health efforts for the Royal College of Obstetricians & Gynaecologists in London and chairs the Committee for Sexual and Reproductive Rights for the International Federation of Gynecology and Obstetrics.
Prof. Hanson, director of the academic unit of human development and health at the University of Southhampton in the United Kingdom, has focused his work on new ways to reduce disease processes and improve health by championing preventive interventions during preconception, throughout pregnancy, and in infancy and childhood.
The program also included Dr. Tyrone Hayes, professor of biology at the University of California, Berkeley, whose research findings on the impact of environmental chemicals on health demonstrate why industry must bear the burden of proof for safety before products are introduced.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – "Every Woman, Every Time," Dr. Jeanne A. Conry’s presidential theme, was front and center at the President’s Program at the annual meeting the American Congress of Obstetricians and Gynecologists. In this exclusive video interview, Dr. Conry spoke with Dr. Lesley Regan about her presentation on basic rights to health care and Dr. Mark Hanson about the role of obstetrician-gynecologists in preventive health initiatives to reduce noncommunicable diseases. Prof. Regan leads global women’s health efforts for the Royal College of Obstetricians & Gynaecologists in London and chairs the Committee for Sexual and Reproductive Rights for the International Federation of Gynecology and Obstetrics.
Prof. Hanson, director of the academic unit of human development and health at the University of Southhampton in the United Kingdom, has focused his work on new ways to reduce disease processes and improve health by championing preventive interventions during preconception, throughout pregnancy, and in infancy and childhood.
The program also included Dr. Tyrone Hayes, professor of biology at the University of California, Berkeley, whose research findings on the impact of environmental chemicals on health demonstrate why industry must bear the burden of proof for safety before products are introduced.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2014 ACOG ANNUAL CLINICAL MEETING
Topical lidocaine reduces menopausal dyspareunia
Applying topical liquid lidocaine to the vulvar vestibule prior to penetration allows for comfortable intercourse in breast cancer survivors with severe menopausal dyspareunia, according to findings from a randomized, controlled study involving 46 women.
During a double-blind phase of the study, patients randomized to apply 4% aqueous lidocaine had less intercourse pain than those who applied saline (median pain scores of 1.0 and 5.3 out of 10, respectively), according to Dr. Martha F. Goetsch of Oregon Health and Science University, Portland, who will report the finding at the annual meeting of the American Congress of Obstetricians and Gynecologists.
During an open-label phase of the study in which all patients were allowed to apply lidocaine, 37 of 41 (90%) reported comfortable penetration, and sexual distress scores decreased from a median of 30.5 to a median of 14. Additionally, 17 of 20 women (85%) who were abstaining from intercourse because of the discomfort had resumed penetrative intimacy, said Dr. Goetsch, whose abstract was awarded first prize among oral presentations by ACOG.
Patients included in the study were estrogen-deficient breast cancer survivors with severe penetrative dyspareunia not associated with pelvic muscle or organ pain. All had severe vulvovaginal atrophy. During the 1-month blinded phase of the study, the women applied either the lidocaine or the saline to the vulvar vestibule for 3 minutes prior to penetration. Effects of twice-weekly tampon insertion or intercourse were documented in a diary. No partners complained of numbness resulting from the lidocaine.
The findings are notable, because breast cancer survivors number in the millions in the United States alone.
"They often suffer from severe dyspareunia and are urged to refrain from using estrogen, which is the therapy most effective for dyspareunia in menopause," Dr. Goetsch said in an interview.
Furthermore, prior research has focused primarily on vaginal atrophy as the cause of dyspareunia in postmenopausal women.
"This study showed that pain could be prevented even though atrophy was unchanged," she said, noting that this suggests that perhaps atrophy is the wrong therapeutic focus.
"Success came with therapy to the vestibule, not the vagina," she said.
Dr. Goetsch reported having no disclosures.
Applying topical liquid lidocaine to the vulvar vestibule prior to penetration allows for comfortable intercourse in breast cancer survivors with severe menopausal dyspareunia, according to findings from a randomized, controlled study involving 46 women.
During a double-blind phase of the study, patients randomized to apply 4% aqueous lidocaine had less intercourse pain than those who applied saline (median pain scores of 1.0 and 5.3 out of 10, respectively), according to Dr. Martha F. Goetsch of Oregon Health and Science University, Portland, who will report the finding at the annual meeting of the American Congress of Obstetricians and Gynecologists.
During an open-label phase of the study in which all patients were allowed to apply lidocaine, 37 of 41 (90%) reported comfortable penetration, and sexual distress scores decreased from a median of 30.5 to a median of 14. Additionally, 17 of 20 women (85%) who were abstaining from intercourse because of the discomfort had resumed penetrative intimacy, said Dr. Goetsch, whose abstract was awarded first prize among oral presentations by ACOG.
Patients included in the study were estrogen-deficient breast cancer survivors with severe penetrative dyspareunia not associated with pelvic muscle or organ pain. All had severe vulvovaginal atrophy. During the 1-month blinded phase of the study, the women applied either the lidocaine or the saline to the vulvar vestibule for 3 minutes prior to penetration. Effects of twice-weekly tampon insertion or intercourse were documented in a diary. No partners complained of numbness resulting from the lidocaine.
The findings are notable, because breast cancer survivors number in the millions in the United States alone.
"They often suffer from severe dyspareunia and are urged to refrain from using estrogen, which is the therapy most effective for dyspareunia in menopause," Dr. Goetsch said in an interview.
Furthermore, prior research has focused primarily on vaginal atrophy as the cause of dyspareunia in postmenopausal women.
"This study showed that pain could be prevented even though atrophy was unchanged," she said, noting that this suggests that perhaps atrophy is the wrong therapeutic focus.
"Success came with therapy to the vestibule, not the vagina," she said.
Dr. Goetsch reported having no disclosures.
Applying topical liquid lidocaine to the vulvar vestibule prior to penetration allows for comfortable intercourse in breast cancer survivors with severe menopausal dyspareunia, according to findings from a randomized, controlled study involving 46 women.
During a double-blind phase of the study, patients randomized to apply 4% aqueous lidocaine had less intercourse pain than those who applied saline (median pain scores of 1.0 and 5.3 out of 10, respectively), according to Dr. Martha F. Goetsch of Oregon Health and Science University, Portland, who will report the finding at the annual meeting of the American Congress of Obstetricians and Gynecologists.
During an open-label phase of the study in which all patients were allowed to apply lidocaine, 37 of 41 (90%) reported comfortable penetration, and sexual distress scores decreased from a median of 30.5 to a median of 14. Additionally, 17 of 20 women (85%) who were abstaining from intercourse because of the discomfort had resumed penetrative intimacy, said Dr. Goetsch, whose abstract was awarded first prize among oral presentations by ACOG.
Patients included in the study were estrogen-deficient breast cancer survivors with severe penetrative dyspareunia not associated with pelvic muscle or organ pain. All had severe vulvovaginal atrophy. During the 1-month blinded phase of the study, the women applied either the lidocaine or the saline to the vulvar vestibule for 3 minutes prior to penetration. Effects of twice-weekly tampon insertion or intercourse were documented in a diary. No partners complained of numbness resulting from the lidocaine.
The findings are notable, because breast cancer survivors number in the millions in the United States alone.
"They often suffer from severe dyspareunia and are urged to refrain from using estrogen, which is the therapy most effective for dyspareunia in menopause," Dr. Goetsch said in an interview.
Furthermore, prior research has focused primarily on vaginal atrophy as the cause of dyspareunia in postmenopausal women.
"This study showed that pain could be prevented even though atrophy was unchanged," she said, noting that this suggests that perhaps atrophy is the wrong therapeutic focus.
"Success came with therapy to the vestibule, not the vagina," she said.
Dr. Goetsch reported having no disclosures.
FROM THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Consider lidocaine as an option for women with severe menopausal dyspareunia for whom estrogen therapy is not recommended.
Major finding: 37 of 41 patients (90%) reported comfortable penetration during intercourse.
Data source: A randomized, controlled, double-blind study of 46 women.
Disclosures: Dr. Goetsch reported having no disclosures.
P4 Medicine: A new approach to health and disease
TAMPA – Paradigm changes drive radical changes in science, according to Dr. Leroy Hood, a renowned scientist and inventor who joined forces with Ohio State University to create the P4 Medicine Institute to "drive innovative approaches to disease prevention and maintenance of health and wellness by applying systems biology to medicine and care delivery."
P4 medicine (Predictive, Preventive, Personalized, Participatory) "is really the convergence of three megatrends in medicine: systems medicine on one hand, big data and its analytics on the other hand, and patient-activated social networks," Dr. Hood, president of the Institute for Systems Biology, Seattle, said at the annual meeting of the Society of Gynecologic Oncology.
As an invited presidential lecturer at the meeting, Dr. Hood described the two central features of systems medicine and how they will facilitate P4 medicine. The first feature is the idea that in the next 5-10 years, individuals will have a "virtual cloud of billions of data points."
"Biological networks exist at the level of genes, the level of proteins, the level of cells, the level of organs, and obviously at the level of the individual through social networks. What is really critical is that in disease, that ‘network of networks’ becomes disease-perturbed and it alters the nature of the information it can handle. If you can capture that altered information, you gain fundamental new insights into biological mechanisms and you can design new strategies both for diagnosis and for therapy," Dr. Hood said.
What is lacking in American medicine, however, is the second feature of systems medicine: an understanding of the dynamics of how these disease-perturbed networks change with time throughout the course of the disease.
P4 medicine differs from evidence-based medicine in that it is proactive rather than reactive; it is focused on the individual and, increasingly, on wellness; it is "all about creating, for each patient, this global data cloud that gives us deep insights into the individual" and that produces predictive and actionable models of wellness and disease; and, most fundamentally, it "argues that the current clinical trial system is totally broken," Dr. Hood said.
"The idea that for a cancer diagnosis, you take 30,000 patients, give them a placebo drug, extract from the patients and put in curves their responses, and from those curves you make generalizations about how to treat the population and how well the drug has done, is wrong in every way. Each individual is different genetically and environmentally," he explained, noting that P4 medicine analyzes "the unique individual and then aggregates those into groups in accordance with what environmental opportunities you’d like to explore."
Acceptance of this new health care concept will depend upon patient-activated social networks, he said.
"I think that’s the only way we can change the incredibly conservative nature of both physicians and the health care system itself," he added.
P4 medicine is mainly about two things – quantifying wellness and demystifying disease, he said.
In contemporary health care, with regard to these two fundamental concepts, three major things have been missing: metrics for wellness, the ability to do longitudinal studies of disease, and the ability to do studies at the point of initiation. A study now underway based on the concept of P4 medicine will allow for all three.
It is a Framingham-like longitudinal study that aims to enroll 100,000 individuals who will be followed for 20-30 years. Participants will quickly be divided into two groups, including those who remain well or improve in health, and those who transition from wellness to disease.
Very soon, the study population will be large enough to see all major diseases, including cancer.
"But the really important point is that we’ll have multiple data points all the way across this longitudinal study so we can go back to the earliest origins of the divergence of wellness to disease for a particular patient, and we can look at mechanisms and new approaches to diagnostics, and hopefully change that disease trajectory very early on to a wellness trajectory," he said.
The first phase of the study, which launched in March, will enroll 1,000 individuals within a year, working up to 10,000 and ultimately to 100,000.
The plan is to collect numerous measurements, including "physical trait kinds of measurements," clinical chemistries, and special measurements of the gut microbiome and organ-specific blood protein fingerprints to monitor wellness-to-disease transitions in the brain, heart, and liver.
"And all of these data will be integrated together by analytics to create these models for each individual that are all focused on identifying and prioritizing a series of actionable traits.
In the short-term, Dr. Hood predicts that the longitudinal study will allow for creation of models for each individual to optimize wellness and minimize disease. In the intermediate term, the data from the well people will be mined for metrics of wellness. Long term, the study will generate a database that elucidates factors associated with the transition from wellness to disease, allowing alteration of the trajectory of disease for many patients.
"My own view is that in a 10- to 15-year period, the wellness industry will be independent from the health care industry, and its total market cap will far exceed that of the health care industry. What is exciting to think is that now, today, we’re just beginning to create the companies that will be the Googles and the Microsofts of the wellness industry. It really is a unique and exciting kind of opportunity," he said.
There’s no way to predict how long it will take for P4 medicine to be fully realized.
"But we are in a unique position now, for the first time, to begin looking at the dynamics of not one human disease, but many different human diseases," he said.
TAMPA – Paradigm changes drive radical changes in science, according to Dr. Leroy Hood, a renowned scientist and inventor who joined forces with Ohio State University to create the P4 Medicine Institute to "drive innovative approaches to disease prevention and maintenance of health and wellness by applying systems biology to medicine and care delivery."
P4 medicine (Predictive, Preventive, Personalized, Participatory) "is really the convergence of three megatrends in medicine: systems medicine on one hand, big data and its analytics on the other hand, and patient-activated social networks," Dr. Hood, president of the Institute for Systems Biology, Seattle, said at the annual meeting of the Society of Gynecologic Oncology.
As an invited presidential lecturer at the meeting, Dr. Hood described the two central features of systems medicine and how they will facilitate P4 medicine. The first feature is the idea that in the next 5-10 years, individuals will have a "virtual cloud of billions of data points."
"Biological networks exist at the level of genes, the level of proteins, the level of cells, the level of organs, and obviously at the level of the individual through social networks. What is really critical is that in disease, that ‘network of networks’ becomes disease-perturbed and it alters the nature of the information it can handle. If you can capture that altered information, you gain fundamental new insights into biological mechanisms and you can design new strategies both for diagnosis and for therapy," Dr. Hood said.
What is lacking in American medicine, however, is the second feature of systems medicine: an understanding of the dynamics of how these disease-perturbed networks change with time throughout the course of the disease.
P4 medicine differs from evidence-based medicine in that it is proactive rather than reactive; it is focused on the individual and, increasingly, on wellness; it is "all about creating, for each patient, this global data cloud that gives us deep insights into the individual" and that produces predictive and actionable models of wellness and disease; and, most fundamentally, it "argues that the current clinical trial system is totally broken," Dr. Hood said.
"The idea that for a cancer diagnosis, you take 30,000 patients, give them a placebo drug, extract from the patients and put in curves their responses, and from those curves you make generalizations about how to treat the population and how well the drug has done, is wrong in every way. Each individual is different genetically and environmentally," he explained, noting that P4 medicine analyzes "the unique individual and then aggregates those into groups in accordance with what environmental opportunities you’d like to explore."
Acceptance of this new health care concept will depend upon patient-activated social networks, he said.
"I think that’s the only way we can change the incredibly conservative nature of both physicians and the health care system itself," he added.
P4 medicine is mainly about two things – quantifying wellness and demystifying disease, he said.
In contemporary health care, with regard to these two fundamental concepts, three major things have been missing: metrics for wellness, the ability to do longitudinal studies of disease, and the ability to do studies at the point of initiation. A study now underway based on the concept of P4 medicine will allow for all three.
It is a Framingham-like longitudinal study that aims to enroll 100,000 individuals who will be followed for 20-30 years. Participants will quickly be divided into two groups, including those who remain well or improve in health, and those who transition from wellness to disease.
Very soon, the study population will be large enough to see all major diseases, including cancer.
"But the really important point is that we’ll have multiple data points all the way across this longitudinal study so we can go back to the earliest origins of the divergence of wellness to disease for a particular patient, and we can look at mechanisms and new approaches to diagnostics, and hopefully change that disease trajectory very early on to a wellness trajectory," he said.
The first phase of the study, which launched in March, will enroll 1,000 individuals within a year, working up to 10,000 and ultimately to 100,000.
The plan is to collect numerous measurements, including "physical trait kinds of measurements," clinical chemistries, and special measurements of the gut microbiome and organ-specific blood protein fingerprints to monitor wellness-to-disease transitions in the brain, heart, and liver.
"And all of these data will be integrated together by analytics to create these models for each individual that are all focused on identifying and prioritizing a series of actionable traits.
In the short-term, Dr. Hood predicts that the longitudinal study will allow for creation of models for each individual to optimize wellness and minimize disease. In the intermediate term, the data from the well people will be mined for metrics of wellness. Long term, the study will generate a database that elucidates factors associated with the transition from wellness to disease, allowing alteration of the trajectory of disease for many patients.
"My own view is that in a 10- to 15-year period, the wellness industry will be independent from the health care industry, and its total market cap will far exceed that of the health care industry. What is exciting to think is that now, today, we’re just beginning to create the companies that will be the Googles and the Microsofts of the wellness industry. It really is a unique and exciting kind of opportunity," he said.
There’s no way to predict how long it will take for P4 medicine to be fully realized.
"But we are in a unique position now, for the first time, to begin looking at the dynamics of not one human disease, but many different human diseases," he said.
TAMPA – Paradigm changes drive radical changes in science, according to Dr. Leroy Hood, a renowned scientist and inventor who joined forces with Ohio State University to create the P4 Medicine Institute to "drive innovative approaches to disease prevention and maintenance of health and wellness by applying systems biology to medicine and care delivery."
P4 medicine (Predictive, Preventive, Personalized, Participatory) "is really the convergence of three megatrends in medicine: systems medicine on one hand, big data and its analytics on the other hand, and patient-activated social networks," Dr. Hood, president of the Institute for Systems Biology, Seattle, said at the annual meeting of the Society of Gynecologic Oncology.
As an invited presidential lecturer at the meeting, Dr. Hood described the two central features of systems medicine and how they will facilitate P4 medicine. The first feature is the idea that in the next 5-10 years, individuals will have a "virtual cloud of billions of data points."
"Biological networks exist at the level of genes, the level of proteins, the level of cells, the level of organs, and obviously at the level of the individual through social networks. What is really critical is that in disease, that ‘network of networks’ becomes disease-perturbed and it alters the nature of the information it can handle. If you can capture that altered information, you gain fundamental new insights into biological mechanisms and you can design new strategies both for diagnosis and for therapy," Dr. Hood said.
What is lacking in American medicine, however, is the second feature of systems medicine: an understanding of the dynamics of how these disease-perturbed networks change with time throughout the course of the disease.
P4 medicine differs from evidence-based medicine in that it is proactive rather than reactive; it is focused on the individual and, increasingly, on wellness; it is "all about creating, for each patient, this global data cloud that gives us deep insights into the individual" and that produces predictive and actionable models of wellness and disease; and, most fundamentally, it "argues that the current clinical trial system is totally broken," Dr. Hood said.
"The idea that for a cancer diagnosis, you take 30,000 patients, give them a placebo drug, extract from the patients and put in curves their responses, and from those curves you make generalizations about how to treat the population and how well the drug has done, is wrong in every way. Each individual is different genetically and environmentally," he explained, noting that P4 medicine analyzes "the unique individual and then aggregates those into groups in accordance with what environmental opportunities you’d like to explore."
Acceptance of this new health care concept will depend upon patient-activated social networks, he said.
"I think that’s the only way we can change the incredibly conservative nature of both physicians and the health care system itself," he added.
P4 medicine is mainly about two things – quantifying wellness and demystifying disease, he said.
In contemporary health care, with regard to these two fundamental concepts, three major things have been missing: metrics for wellness, the ability to do longitudinal studies of disease, and the ability to do studies at the point of initiation. A study now underway based on the concept of P4 medicine will allow for all three.
It is a Framingham-like longitudinal study that aims to enroll 100,000 individuals who will be followed for 20-30 years. Participants will quickly be divided into two groups, including those who remain well or improve in health, and those who transition from wellness to disease.
Very soon, the study population will be large enough to see all major diseases, including cancer.
"But the really important point is that we’ll have multiple data points all the way across this longitudinal study so we can go back to the earliest origins of the divergence of wellness to disease for a particular patient, and we can look at mechanisms and new approaches to diagnostics, and hopefully change that disease trajectory very early on to a wellness trajectory," he said.
The first phase of the study, which launched in March, will enroll 1,000 individuals within a year, working up to 10,000 and ultimately to 100,000.
The plan is to collect numerous measurements, including "physical trait kinds of measurements," clinical chemistries, and special measurements of the gut microbiome and organ-specific blood protein fingerprints to monitor wellness-to-disease transitions in the brain, heart, and liver.
"And all of these data will be integrated together by analytics to create these models for each individual that are all focused on identifying and prioritizing a series of actionable traits.
In the short-term, Dr. Hood predicts that the longitudinal study will allow for creation of models for each individual to optimize wellness and minimize disease. In the intermediate term, the data from the well people will be mined for metrics of wellness. Long term, the study will generate a database that elucidates factors associated with the transition from wellness to disease, allowing alteration of the trajectory of disease for many patients.
"My own view is that in a 10- to 15-year period, the wellness industry will be independent from the health care industry, and its total market cap will far exceed that of the health care industry. What is exciting to think is that now, today, we’re just beginning to create the companies that will be the Googles and the Microsofts of the wellness industry. It really is a unique and exciting kind of opportunity," he said.
There’s no way to predict how long it will take for P4 medicine to be fully realized.
"But we are in a unique position now, for the first time, to begin looking at the dynamics of not one human disease, but many different human diseases," he said.
EXPERT ANALYSIS FROM THE ANNUAL MEETING ON WOMEN’S CANCER
FDA approves cobas HPV test as first-line cervical cancer screen
The Food and Drug Administration on April 24 approved the cobas HPV test as a first-line screening test for primary cervical cancer.
The cobas HPV test uses a sample of cervical cells to detect DNA from 14 high-risk human papillomavirus types. The test, which is approved for women aged 25 years and older, identifies HPV 16 and 18. It can concurrently detect 12 other types of high-risk HPVs, according to the FDA.
The FDA recommended that women who test positive for HPV 16 or HPV 18 using the cobas HPV test have a colposcopy. Those who test positive for one or more of the 12 other high-risk HPV types should have a Pap test to determine the need for a colposcopy.
The cobas HPV test results should be used along with patient screening history and risk factors, and current professional guidelines when making clinical decisions, the FDA advised.
The test, which is manufactured by Roche Molecular Diagnostics, was first approved in 2011 for use in conjunction with or as a follow-up to a Pap test. With the current approval, the cobas test can now be used as the primary cervical cancer screening test.
The approval means women will have more screening options, said Alberto Gutierrez, Ph.D., director of the FDA Office of In Vitro Diagnostics and Radiological Health.
"Roche Diagnostics conducted a well-designed study that provided the FDA with a reasonable assurance of the safety and effectiveness when used as a primary screening tool for cervical cancer," Dr. Gutierrez said in a statement.
Despite some concerns about the potential for confusion and its off-label use, the FDA’s Microbiology Devices Advisory Committee voted unanimously on March 12 to support expanding the approval of the cobas HPV test to include first-line use for primary cervical cancer screening. Some panelists noted that it will be up to professional societies to integrate the new test into their practice guidelines and to educate physicians and patients about its use.
The decision to approve the test was based on the results of the ATHENA trial, a prospective study of 47,208 women in the United States, and 3-year follow-up data. The results indicate that HPV testing alone provides greater protection against CIN3 (cervical intraepithelial neoplasia grade 3) and invasive cervical cancer than does cytology alone, and that primary HPV testing provides a similar level of protection against CIN3 and invasive cervical cancer as does cotesting with HPV testing and cytology, according to Roche.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The Food and Drug Administration on April 24 approved the cobas HPV test as a first-line screening test for primary cervical cancer.
The cobas HPV test uses a sample of cervical cells to detect DNA from 14 high-risk human papillomavirus types. The test, which is approved for women aged 25 years and older, identifies HPV 16 and 18. It can concurrently detect 12 other types of high-risk HPVs, according to the FDA.
The FDA recommended that women who test positive for HPV 16 or HPV 18 using the cobas HPV test have a colposcopy. Those who test positive for one or more of the 12 other high-risk HPV types should have a Pap test to determine the need for a colposcopy.
The cobas HPV test results should be used along with patient screening history and risk factors, and current professional guidelines when making clinical decisions, the FDA advised.
The test, which is manufactured by Roche Molecular Diagnostics, was first approved in 2011 for use in conjunction with or as a follow-up to a Pap test. With the current approval, the cobas test can now be used as the primary cervical cancer screening test.
The approval means women will have more screening options, said Alberto Gutierrez, Ph.D., director of the FDA Office of In Vitro Diagnostics and Radiological Health.
"Roche Diagnostics conducted a well-designed study that provided the FDA with a reasonable assurance of the safety and effectiveness when used as a primary screening tool for cervical cancer," Dr. Gutierrez said in a statement.
Despite some concerns about the potential for confusion and its off-label use, the FDA’s Microbiology Devices Advisory Committee voted unanimously on March 12 to support expanding the approval of the cobas HPV test to include first-line use for primary cervical cancer screening. Some panelists noted that it will be up to professional societies to integrate the new test into their practice guidelines and to educate physicians and patients about its use.
The decision to approve the test was based on the results of the ATHENA trial, a prospective study of 47,208 women in the United States, and 3-year follow-up data. The results indicate that HPV testing alone provides greater protection against CIN3 (cervical intraepithelial neoplasia grade 3) and invasive cervical cancer than does cytology alone, and that primary HPV testing provides a similar level of protection against CIN3 and invasive cervical cancer as does cotesting with HPV testing and cytology, according to Roche.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The Food and Drug Administration on April 24 approved the cobas HPV test as a first-line screening test for primary cervical cancer.
The cobas HPV test uses a sample of cervical cells to detect DNA from 14 high-risk human papillomavirus types. The test, which is approved for women aged 25 years and older, identifies HPV 16 and 18. It can concurrently detect 12 other types of high-risk HPVs, according to the FDA.
The FDA recommended that women who test positive for HPV 16 or HPV 18 using the cobas HPV test have a colposcopy. Those who test positive for one or more of the 12 other high-risk HPV types should have a Pap test to determine the need for a colposcopy.
The cobas HPV test results should be used along with patient screening history and risk factors, and current professional guidelines when making clinical decisions, the FDA advised.
The test, which is manufactured by Roche Molecular Diagnostics, was first approved in 2011 for use in conjunction with or as a follow-up to a Pap test. With the current approval, the cobas test can now be used as the primary cervical cancer screening test.
The approval means women will have more screening options, said Alberto Gutierrez, Ph.D., director of the FDA Office of In Vitro Diagnostics and Radiological Health.
"Roche Diagnostics conducted a well-designed study that provided the FDA with a reasonable assurance of the safety and effectiveness when used as a primary screening tool for cervical cancer," Dr. Gutierrez said in a statement.
Despite some concerns about the potential for confusion and its off-label use, the FDA’s Microbiology Devices Advisory Committee voted unanimously on March 12 to support expanding the approval of the cobas HPV test to include first-line use for primary cervical cancer screening. Some panelists noted that it will be up to professional societies to integrate the new test into their practice guidelines and to educate physicians and patients about its use.
The decision to approve the test was based on the results of the ATHENA trial, a prospective study of 47,208 women in the United States, and 3-year follow-up data. The results indicate that HPV testing alone provides greater protection against CIN3 (cervical intraepithelial neoplasia grade 3) and invasive cervical cancer than does cytology alone, and that primary HPV testing provides a similar level of protection against CIN3 and invasive cervical cancer as does cotesting with HPV testing and cytology, according to Roche.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
2014 Update on cervical disease
Advances in cervical cancer screening continue apace. We are fortunate that these advances are based on a substantial amount of high-quality prospective evidence. Many of these advances are designed to target the women who have clinically relevant disease while minimizing harm and anxiety caused by unnecessary procedures related to cervical screening test abnormalities that have little clinical relevance.
With clinicians being regularly judged on performance and outcomes, adoption of advances and new guidelines should be considered relatively quickly by women’s health providers.
In this article, I focus on two significant advances of the past (and coming) year:
- recent application and unanimous approval by a Food and Drug Administration (FDA) expert panel for the use of the cobas human papillomavirus (HPV) DNA test as a primary cervical cancer screen
- the latest update of guidelines on the management of abnormal cervical screening tests from the American Society for Colposcopy and Cervical Pathology (ASCCP).
cobas HPV TEST IS POISED FOR FDA APPROVAL AS A PRIMARY SCREEN FOR CERVICAL CANCER
Wright TC Jr, Stoler MH, Behrens CM, Apple R, Derion T, Wright TL. The ATHENA human papillomavirus study: design, methods, and baseline results. Am J Obstet Gynecol. 2012;206(1):46.e1–e11.
An FDA expert panel unanimously approved the cobas (Roche Molecular Diagnostics; Pleasanton, California) HPV DNA test on March 12, 2014. The FDA will decide on potential approval within the coming months. Although the FDA sometimes reaches a different decision from one of its advisory committees when it comes to a final vote on a product or device, most often the FDA concurs with the committee’s judgment. Therefore, approval of the cobas HPV test as a primary screen is likely.
Related article: FDA Advisory Committee recommends HPV test as primary screening tool for cervical cancer Deborah Reale (News for your Practice, March 2014)
The cobas HPV test yields a pooled result for 12 high-risk HPV types (hrHPV 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68), as well as individual results for types 16 and 18; it also has an internal control for specimen adequacy. HPV 16 and 18 account for roughly 70% of all cases of cervical cancer, and infection with both types are known to place women at high risk for having clinically relevant disease—more so than the other hrHPV types.
COMMITTEE REVIEWED DATA FROM ATHENA IN VOTING FOR APPROVAL
In considering the cobas HPV test, the advisory committee reviewed data from the Addressing the Need for Advanced HPV Diagnostics (ATHENA) trial, a prospective, multicenter, US-based study of 47,208 women aged 21 and older. These women were recruited at the time of undergoing routine screening for cervical cancer; only 2.6% had been vaccinated against HPV. All were screened by liquid-based cytology and an HPV test. Those who had abnormal cytology or a positive test for a high-risk HPV type underwent colposcopy, as did a randomly selected group of women aged 25 or older who tested negative on both tests.
The prevalence of abnormal findings was:
- 7.1% for liquid-based cytology
- 12.6% for pooled high-risk HPV
- 2.8% for HPV 16
- 1.0% for HPV 18.
As expected, cytologic abnormalities and infection with high-risk HPV types declined with increasing age. The adjusted prevalence of cervical intraepithelial neoplasia (CIN) grade 2 or higher in women aged 25 to 34 years was 2.3%; it declined to 1.5% among women older than age 34. Of note, approximately 500,000 US women are given a diagnosis of CIN 2 or CIN 3 each year in the United States.
WHY ATHENA IS IMPORTANT
This US-based trial was designed to assess the medical utility of pooled high-risk HPV DNA in addition to genotyping for HPV 16 and 18 in three populations:
- women aged 21 and older with a cytologic finding of atypical squamous cells of undetermined significance (ASC-US)
- women aged 30 and older with normal cytology
- women aged 25 and older in the overall screening population with any cytologic finding.
Investigators were particularly interested in the use of the HPV test as:
- a triage for women with abnormal cytologic findings
- an adjunct to guide clinical management of women with negative cytology results
- a potential front-line test in the screening of women aged 25 and older.
Related article: Endometrial cancer update: The move toward personalized cancer care Lindsay M. Kuroki, MD, and David G. Mutch, MD (October 2013)
The participants of the ATHENA trial were representative of women undergoing screening for cervical cancer in the United States—both in terms of demographics and in the distribution of cytologic findings. For example, recent US census data indicate that the female population is 79% white, 13% black, and 16% Hispanic or Latino—figures comparable to the breakdown of race/ethnicity in the ATHENA trial.
The trial was conducted in a baseline phase (published in 2012) and a 3-year follow-up phase (not yet published). The 3-year data were reviewed by the FDA advisory committee during its consideration of the cobas HPV test as a primary screen.
DESPITE PROBABLE APPROVAL, INCREMENTAL CHANGE IS LIKELY
Although a move to the HPV test as the primary screen is a definite paradigm shift for what has been cytology-based screening since the initiation of cervical cancer screening, the changeover from primary cytology to primary HPV testing likely will be slow. It will require education of clinicians as well as patients, and a shift in many internal procedures for pathology laboratories.
The ATHENA trial also leaves some intriguing questions unanswered:
- How do we transition women into the new screening strategy? Many women today still undergo cytology screening with reflex HPV testing, as appropriate, and an increasing number of women aged 30 and older undergo cotesting with both cytology and HPV testing. When should they begin screening in a primary HPV testing setting? And what screening intervals will be recommended? If a woman already has been screened with cytology, how should she transition into and at what interval should she begin primary HPV screening?
- How should we manage women’s care after the first round of primary HPV testing? The ATHENA trial so far only has outcomes data after one round of HPV testing. While some data are available from Europe, we do not know what happens after two or three rounds of screening with primary HPV testing in a large US-based cohort. We clearly will be identifying and treating many women with preinvasive disease from screening after one round of testing, at a rate likely higher than with cytology alone—a good thing. We also likely will be reducing the number of unnecessary colposcopies for cytology that are not related to hrHPV.
What this EVIDENCE means for practice
Screening women using the cobas HPV test as a primary screen will require considerable education of providers and patients to explain how this change will affect how a woman will be managed after being screened for cervical cancer. Though much remains to be determined about this new cervical cancer screening paradigm (eg, logistics, timing, use of secondary tests), it should reduce the number of screening tests and colposcopies necessary to detect clinically relevant disease.
UPDATED ASCCP GUIDELINES EMPHASIZE EQUAL MANAGEMENT FOR EQUAL RISK
Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1–S27.
In formulating this latest set of guidelines for the management of abnormal cervical cancer screening tests and cancer precursors, the ASCCP led a conference consisting of scientific stakeholders to perform a comprehensive review of the literature. Also, with study investigators at Kaiser Permanente Northern California (KPNC) and the National Cancer Institute, the guidelines panel also modeled and assessed data on risk after abnormal tests from almost 1.4 million women followed over 8 years in the KPNC Medical Care Plan—this cohort has provided us with “big data.”
The sheer size of the Kaiser Permanente population made it possible for the ASCCP-led panel to validate its previous guidelines or to modify them, where needed. It also made risk-based stratification possible for even rare abnormalities and clinical outcomes.
Although findings from the KPNC population may not be fully generalizable to the US population as a whole, they enhance our understanding of the optimal management of abnormal cervical cancer screening tests and cancer precursors. More widely dispersed study cohorts on a similar scale in the United States are unlikely in the near future.
Related article: Update on cervical disease Mark H. Einstein, MD, MS, and J. Thomas Cox, MD (May 2013)
SEVERAL SIGNIFICANT MODIFICATIONS
Although the ASCCP reaffirmed most elements of its 2006 consensus management guidelines, it did make a number of changes:
- Women who have ASC-US cytology but test HPV-negative now should be followed with cotesting at 3 years rather than 5 years before they return to routine screening.
- Women near age 65 who have a negative finding on ASC-US cytology and HPV testing should not exit screening.
- Women who have ASC-US cytology and test HPV-positive should go to immediate colposcopy, regardless of hrHPV results, including genotyping.
- Women who test positive for HPV 16 or 18 but have negative cytology should undergo immediate colposcopy.
- Women aged 21 to 24 years should be managed as conservatively and minimally invasively as possible, especially when an abnormality is minor.
- Endocervical curettage reported as CIN 1 should be managed as CIN 1, not as a positive endocervical curettage.
- When a cytologic sample is unsatisfactory, sampling usually should be repeated, even when HPV cotesting results are known. However, negative cytology that lacks sufficient endocervical cells or a transformation zone component usually can be managed without frequent follow-up.
Related article: New cervical Ca screening guidelines recommend less frequent assessment Janelle Yates (News for your Practice; April 2012)
EQUAL MANAGEMENT SHOULD BE PERFORMED FOR ABNORMAL TESTS THAT INDICATE EQUAL RISK
The ASCCP-led management panel unanimously agreed to several basic assumptions in formulating the updated guidelines. For example, they concurred that achieving zero risk for cancer is impossible and that attempts to achieve zero risk (which typically means more frequent testing) may cause harm. They also cited the 2011 American Cancer Society/ASCCP/American Society for Clinical Pathology consensus screening document, which stated: “Optimal prevention strategies should identify those HPV-related abnormalities likely to progress to invasive cancers while avoiding destructive treatment of abnormalities not destined to become cancerous.”1
The panel also agreed that CIN 3+ is a “reasonable proxy for cancer risk.” When calculating risk, the KPNC data were modeled for all combinations of cytology and HPV testing, using CIN 3+ for many of the outcomes, and when outcomes were rare, using CIN 2+. The theme of equal management for equal risk was the rationale behind the management approaches detailed in the TABLE. Risks were deemed to be low and return to normal screening was recommended when the risks were similar to the rate of CIN 3+ 3 years after negative cytology or 5 years after negative cotesting. However, immediate colposcopy was recommended when the 5-year risk of CIN 3+ for the combination of cytology and hrHPV testing, when indicated, exceeded 5%. A 6-month to 12-month return (intermediate risk) is indicated with a risk of CIN3+ of 2% to 5%.
An emphasis on avoiding harms
Abnormal findings at the time of cervical cancer screening can lead to a number of harms for the patient, including anxiety and emotional distress, particularly when colposcopy is necessary, as well as time lost from home and work life. For this reason, the guidelines panel emphasized that colposcopy and other interventions should be avoided when the risk of CIN 3+ is low and when the cervical screening abnormalities are likely to resolve without treatment.
However, women who experience postcoital bleeding, unexplained abnormal vaginal bleeding, pelvic pain, abnormal discharge, or a visible lesion should be managed promptly on an individualized basis.
Long-term effects of HPV vaccination are unknown
Among the areas that remain to be addressed are the unknown effects of widespread prophylactic HPV vaccination over the long term. We also lack full understanding of whether and how HPV vaccination will alter the incidence and management of cytologic and histologic abnormalities. Given the low rates of vaccination against HPV in the United States at present, this will need to be re-evaluated in the future.
What this EVIDENCE means for practice
The updated ASCCP guidelines are inherently complex, but their complexity arises from a large body of high-quality prospective data from a large population of women. Equal risk should result in equal management of cervical screening test abnormalities. Practitioners need not feel obligated to memorize the guidelines, owing to the availability of algorithms for specific findings in specific populations at the ASCCP Web site (www.asccp.org/consensus2012). Apps also are available for the iPhone, iPad, and Android.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Reference
- Saslow D, Solomon D, Lawson HW, et al;ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172.
Advances in cervical cancer screening continue apace. We are fortunate that these advances are based on a substantial amount of high-quality prospective evidence. Many of these advances are designed to target the women who have clinically relevant disease while minimizing harm and anxiety caused by unnecessary procedures related to cervical screening test abnormalities that have little clinical relevance.
With clinicians being regularly judged on performance and outcomes, adoption of advances and new guidelines should be considered relatively quickly by women’s health providers.
In this article, I focus on two significant advances of the past (and coming) year:
- recent application and unanimous approval by a Food and Drug Administration (FDA) expert panel for the use of the cobas human papillomavirus (HPV) DNA test as a primary cervical cancer screen
- the latest update of guidelines on the management of abnormal cervical screening tests from the American Society for Colposcopy and Cervical Pathology (ASCCP).
cobas HPV TEST IS POISED FOR FDA APPROVAL AS A PRIMARY SCREEN FOR CERVICAL CANCER
Wright TC Jr, Stoler MH, Behrens CM, Apple R, Derion T, Wright TL. The ATHENA human papillomavirus study: design, methods, and baseline results. Am J Obstet Gynecol. 2012;206(1):46.e1–e11.
An FDA expert panel unanimously approved the cobas (Roche Molecular Diagnostics; Pleasanton, California) HPV DNA test on March 12, 2014. The FDA will decide on potential approval within the coming months. Although the FDA sometimes reaches a different decision from one of its advisory committees when it comes to a final vote on a product or device, most often the FDA concurs with the committee’s judgment. Therefore, approval of the cobas HPV test as a primary screen is likely.
Related article: FDA Advisory Committee recommends HPV test as primary screening tool for cervical cancer Deborah Reale (News for your Practice, March 2014)
The cobas HPV test yields a pooled result for 12 high-risk HPV types (hrHPV 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68), as well as individual results for types 16 and 18; it also has an internal control for specimen adequacy. HPV 16 and 18 account for roughly 70% of all cases of cervical cancer, and infection with both types are known to place women at high risk for having clinically relevant disease—more so than the other hrHPV types.
COMMITTEE REVIEWED DATA FROM ATHENA IN VOTING FOR APPROVAL
In considering the cobas HPV test, the advisory committee reviewed data from the Addressing the Need for Advanced HPV Diagnostics (ATHENA) trial, a prospective, multicenter, US-based study of 47,208 women aged 21 and older. These women were recruited at the time of undergoing routine screening for cervical cancer; only 2.6% had been vaccinated against HPV. All were screened by liquid-based cytology and an HPV test. Those who had abnormal cytology or a positive test for a high-risk HPV type underwent colposcopy, as did a randomly selected group of women aged 25 or older who tested negative on both tests.
The prevalence of abnormal findings was:
- 7.1% for liquid-based cytology
- 12.6% for pooled high-risk HPV
- 2.8% for HPV 16
- 1.0% for HPV 18.
As expected, cytologic abnormalities and infection with high-risk HPV types declined with increasing age. The adjusted prevalence of cervical intraepithelial neoplasia (CIN) grade 2 or higher in women aged 25 to 34 years was 2.3%; it declined to 1.5% among women older than age 34. Of note, approximately 500,000 US women are given a diagnosis of CIN 2 or CIN 3 each year in the United States.
WHY ATHENA IS IMPORTANT
This US-based trial was designed to assess the medical utility of pooled high-risk HPV DNA in addition to genotyping for HPV 16 and 18 in three populations:
- women aged 21 and older with a cytologic finding of atypical squamous cells of undetermined significance (ASC-US)
- women aged 30 and older with normal cytology
- women aged 25 and older in the overall screening population with any cytologic finding.
Investigators were particularly interested in the use of the HPV test as:
- a triage for women with abnormal cytologic findings
- an adjunct to guide clinical management of women with negative cytology results
- a potential front-line test in the screening of women aged 25 and older.
Related article: Endometrial cancer update: The move toward personalized cancer care Lindsay M. Kuroki, MD, and David G. Mutch, MD (October 2013)
The participants of the ATHENA trial were representative of women undergoing screening for cervical cancer in the United States—both in terms of demographics and in the distribution of cytologic findings. For example, recent US census data indicate that the female population is 79% white, 13% black, and 16% Hispanic or Latino—figures comparable to the breakdown of race/ethnicity in the ATHENA trial.
The trial was conducted in a baseline phase (published in 2012) and a 3-year follow-up phase (not yet published). The 3-year data were reviewed by the FDA advisory committee during its consideration of the cobas HPV test as a primary screen.
DESPITE PROBABLE APPROVAL, INCREMENTAL CHANGE IS LIKELY
Although a move to the HPV test as the primary screen is a definite paradigm shift for what has been cytology-based screening since the initiation of cervical cancer screening, the changeover from primary cytology to primary HPV testing likely will be slow. It will require education of clinicians as well as patients, and a shift in many internal procedures for pathology laboratories.
The ATHENA trial also leaves some intriguing questions unanswered:
- How do we transition women into the new screening strategy? Many women today still undergo cytology screening with reflex HPV testing, as appropriate, and an increasing number of women aged 30 and older undergo cotesting with both cytology and HPV testing. When should they begin screening in a primary HPV testing setting? And what screening intervals will be recommended? If a woman already has been screened with cytology, how should she transition into and at what interval should she begin primary HPV screening?
- How should we manage women’s care after the first round of primary HPV testing? The ATHENA trial so far only has outcomes data after one round of HPV testing. While some data are available from Europe, we do not know what happens after two or three rounds of screening with primary HPV testing in a large US-based cohort. We clearly will be identifying and treating many women with preinvasive disease from screening after one round of testing, at a rate likely higher than with cytology alone—a good thing. We also likely will be reducing the number of unnecessary colposcopies for cytology that are not related to hrHPV.
What this EVIDENCE means for practice
Screening women using the cobas HPV test as a primary screen will require considerable education of providers and patients to explain how this change will affect how a woman will be managed after being screened for cervical cancer. Though much remains to be determined about this new cervical cancer screening paradigm (eg, logistics, timing, use of secondary tests), it should reduce the number of screening tests and colposcopies necessary to detect clinically relevant disease.
UPDATED ASCCP GUIDELINES EMPHASIZE EQUAL MANAGEMENT FOR EQUAL RISK
Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1–S27.
In formulating this latest set of guidelines for the management of abnormal cervical cancer screening tests and cancer precursors, the ASCCP led a conference consisting of scientific stakeholders to perform a comprehensive review of the literature. Also, with study investigators at Kaiser Permanente Northern California (KPNC) and the National Cancer Institute, the guidelines panel also modeled and assessed data on risk after abnormal tests from almost 1.4 million women followed over 8 years in the KPNC Medical Care Plan—this cohort has provided us with “big data.”
The sheer size of the Kaiser Permanente population made it possible for the ASCCP-led panel to validate its previous guidelines or to modify them, where needed. It also made risk-based stratification possible for even rare abnormalities and clinical outcomes.
Although findings from the KPNC population may not be fully generalizable to the US population as a whole, they enhance our understanding of the optimal management of abnormal cervical cancer screening tests and cancer precursors. More widely dispersed study cohorts on a similar scale in the United States are unlikely in the near future.
Related article: Update on cervical disease Mark H. Einstein, MD, MS, and J. Thomas Cox, MD (May 2013)
SEVERAL SIGNIFICANT MODIFICATIONS
Although the ASCCP reaffirmed most elements of its 2006 consensus management guidelines, it did make a number of changes:
- Women who have ASC-US cytology but test HPV-negative now should be followed with cotesting at 3 years rather than 5 years before they return to routine screening.
- Women near age 65 who have a negative finding on ASC-US cytology and HPV testing should not exit screening.
- Women who have ASC-US cytology and test HPV-positive should go to immediate colposcopy, regardless of hrHPV results, including genotyping.
- Women who test positive for HPV 16 or 18 but have negative cytology should undergo immediate colposcopy.
- Women aged 21 to 24 years should be managed as conservatively and minimally invasively as possible, especially when an abnormality is minor.
- Endocervical curettage reported as CIN 1 should be managed as CIN 1, not as a positive endocervical curettage.
- When a cytologic sample is unsatisfactory, sampling usually should be repeated, even when HPV cotesting results are known. However, negative cytology that lacks sufficient endocervical cells or a transformation zone component usually can be managed without frequent follow-up.
Related article: New cervical Ca screening guidelines recommend less frequent assessment Janelle Yates (News for your Practice; April 2012)
EQUAL MANAGEMENT SHOULD BE PERFORMED FOR ABNORMAL TESTS THAT INDICATE EQUAL RISK
The ASCCP-led management panel unanimously agreed to several basic assumptions in formulating the updated guidelines. For example, they concurred that achieving zero risk for cancer is impossible and that attempts to achieve zero risk (which typically means more frequent testing) may cause harm. They also cited the 2011 American Cancer Society/ASCCP/American Society for Clinical Pathology consensus screening document, which stated: “Optimal prevention strategies should identify those HPV-related abnormalities likely to progress to invasive cancers while avoiding destructive treatment of abnormalities not destined to become cancerous.”1
The panel also agreed that CIN 3+ is a “reasonable proxy for cancer risk.” When calculating risk, the KPNC data were modeled for all combinations of cytology and HPV testing, using CIN 3+ for many of the outcomes, and when outcomes were rare, using CIN 2+. The theme of equal management for equal risk was the rationale behind the management approaches detailed in the TABLE. Risks were deemed to be low and return to normal screening was recommended when the risks were similar to the rate of CIN 3+ 3 years after negative cytology or 5 years after negative cotesting. However, immediate colposcopy was recommended when the 5-year risk of CIN 3+ for the combination of cytology and hrHPV testing, when indicated, exceeded 5%. A 6-month to 12-month return (intermediate risk) is indicated with a risk of CIN3+ of 2% to 5%.
An emphasis on avoiding harms
Abnormal findings at the time of cervical cancer screening can lead to a number of harms for the patient, including anxiety and emotional distress, particularly when colposcopy is necessary, as well as time lost from home and work life. For this reason, the guidelines panel emphasized that colposcopy and other interventions should be avoided when the risk of CIN 3+ is low and when the cervical screening abnormalities are likely to resolve without treatment.
However, women who experience postcoital bleeding, unexplained abnormal vaginal bleeding, pelvic pain, abnormal discharge, or a visible lesion should be managed promptly on an individualized basis.
Long-term effects of HPV vaccination are unknown
Among the areas that remain to be addressed are the unknown effects of widespread prophylactic HPV vaccination over the long term. We also lack full understanding of whether and how HPV vaccination will alter the incidence and management of cytologic and histologic abnormalities. Given the low rates of vaccination against HPV in the United States at present, this will need to be re-evaluated in the future.
What this EVIDENCE means for practice
The updated ASCCP guidelines are inherently complex, but their complexity arises from a large body of high-quality prospective data from a large population of women. Equal risk should result in equal management of cervical screening test abnormalities. Practitioners need not feel obligated to memorize the guidelines, owing to the availability of algorithms for specific findings in specific populations at the ASCCP Web site (www.asccp.org/consensus2012). Apps also are available for the iPhone, iPad, and Android.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Advances in cervical cancer screening continue apace. We are fortunate that these advances are based on a substantial amount of high-quality prospective evidence. Many of these advances are designed to target the women who have clinically relevant disease while minimizing harm and anxiety caused by unnecessary procedures related to cervical screening test abnormalities that have little clinical relevance.
With clinicians being regularly judged on performance and outcomes, adoption of advances and new guidelines should be considered relatively quickly by women’s health providers.
In this article, I focus on two significant advances of the past (and coming) year:
- recent application and unanimous approval by a Food and Drug Administration (FDA) expert panel for the use of the cobas human papillomavirus (HPV) DNA test as a primary cervical cancer screen
- the latest update of guidelines on the management of abnormal cervical screening tests from the American Society for Colposcopy and Cervical Pathology (ASCCP).
cobas HPV TEST IS POISED FOR FDA APPROVAL AS A PRIMARY SCREEN FOR CERVICAL CANCER
Wright TC Jr, Stoler MH, Behrens CM, Apple R, Derion T, Wright TL. The ATHENA human papillomavirus study: design, methods, and baseline results. Am J Obstet Gynecol. 2012;206(1):46.e1–e11.
An FDA expert panel unanimously approved the cobas (Roche Molecular Diagnostics; Pleasanton, California) HPV DNA test on March 12, 2014. The FDA will decide on potential approval within the coming months. Although the FDA sometimes reaches a different decision from one of its advisory committees when it comes to a final vote on a product or device, most often the FDA concurs with the committee’s judgment. Therefore, approval of the cobas HPV test as a primary screen is likely.
Related article: FDA Advisory Committee recommends HPV test as primary screening tool for cervical cancer Deborah Reale (News for your Practice, March 2014)
The cobas HPV test yields a pooled result for 12 high-risk HPV types (hrHPV 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68), as well as individual results for types 16 and 18; it also has an internal control for specimen adequacy. HPV 16 and 18 account for roughly 70% of all cases of cervical cancer, and infection with both types are known to place women at high risk for having clinically relevant disease—more so than the other hrHPV types.
COMMITTEE REVIEWED DATA FROM ATHENA IN VOTING FOR APPROVAL
In considering the cobas HPV test, the advisory committee reviewed data from the Addressing the Need for Advanced HPV Diagnostics (ATHENA) trial, a prospective, multicenter, US-based study of 47,208 women aged 21 and older. These women were recruited at the time of undergoing routine screening for cervical cancer; only 2.6% had been vaccinated against HPV. All were screened by liquid-based cytology and an HPV test. Those who had abnormal cytology or a positive test for a high-risk HPV type underwent colposcopy, as did a randomly selected group of women aged 25 or older who tested negative on both tests.
The prevalence of abnormal findings was:
- 7.1% for liquid-based cytology
- 12.6% for pooled high-risk HPV
- 2.8% for HPV 16
- 1.0% for HPV 18.
As expected, cytologic abnormalities and infection with high-risk HPV types declined with increasing age. The adjusted prevalence of cervical intraepithelial neoplasia (CIN) grade 2 or higher in women aged 25 to 34 years was 2.3%; it declined to 1.5% among women older than age 34. Of note, approximately 500,000 US women are given a diagnosis of CIN 2 or CIN 3 each year in the United States.
WHY ATHENA IS IMPORTANT
This US-based trial was designed to assess the medical utility of pooled high-risk HPV DNA in addition to genotyping for HPV 16 and 18 in three populations:
- women aged 21 and older with a cytologic finding of atypical squamous cells of undetermined significance (ASC-US)
- women aged 30 and older with normal cytology
- women aged 25 and older in the overall screening population with any cytologic finding.
Investigators were particularly interested in the use of the HPV test as:
- a triage for women with abnormal cytologic findings
- an adjunct to guide clinical management of women with negative cytology results
- a potential front-line test in the screening of women aged 25 and older.
Related article: Endometrial cancer update: The move toward personalized cancer care Lindsay M. Kuroki, MD, and David G. Mutch, MD (October 2013)
The participants of the ATHENA trial were representative of women undergoing screening for cervical cancer in the United States—both in terms of demographics and in the distribution of cytologic findings. For example, recent US census data indicate that the female population is 79% white, 13% black, and 16% Hispanic or Latino—figures comparable to the breakdown of race/ethnicity in the ATHENA trial.
The trial was conducted in a baseline phase (published in 2012) and a 3-year follow-up phase (not yet published). The 3-year data were reviewed by the FDA advisory committee during its consideration of the cobas HPV test as a primary screen.
DESPITE PROBABLE APPROVAL, INCREMENTAL CHANGE IS LIKELY
Although a move to the HPV test as the primary screen is a definite paradigm shift for what has been cytology-based screening since the initiation of cervical cancer screening, the changeover from primary cytology to primary HPV testing likely will be slow. It will require education of clinicians as well as patients, and a shift in many internal procedures for pathology laboratories.
The ATHENA trial also leaves some intriguing questions unanswered:
- How do we transition women into the new screening strategy? Many women today still undergo cytology screening with reflex HPV testing, as appropriate, and an increasing number of women aged 30 and older undergo cotesting with both cytology and HPV testing. When should they begin screening in a primary HPV testing setting? And what screening intervals will be recommended? If a woman already has been screened with cytology, how should she transition into and at what interval should she begin primary HPV screening?
- How should we manage women’s care after the first round of primary HPV testing? The ATHENA trial so far only has outcomes data after one round of HPV testing. While some data are available from Europe, we do not know what happens after two or three rounds of screening with primary HPV testing in a large US-based cohort. We clearly will be identifying and treating many women with preinvasive disease from screening after one round of testing, at a rate likely higher than with cytology alone—a good thing. We also likely will be reducing the number of unnecessary colposcopies for cytology that are not related to hrHPV.
What this EVIDENCE means for practice
Screening women using the cobas HPV test as a primary screen will require considerable education of providers and patients to explain how this change will affect how a woman will be managed after being screened for cervical cancer. Though much remains to be determined about this new cervical cancer screening paradigm (eg, logistics, timing, use of secondary tests), it should reduce the number of screening tests and colposcopies necessary to detect clinically relevant disease.
UPDATED ASCCP GUIDELINES EMPHASIZE EQUAL MANAGEMENT FOR EQUAL RISK
Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1–S27.
In formulating this latest set of guidelines for the management of abnormal cervical cancer screening tests and cancer precursors, the ASCCP led a conference consisting of scientific stakeholders to perform a comprehensive review of the literature. Also, with study investigators at Kaiser Permanente Northern California (KPNC) and the National Cancer Institute, the guidelines panel also modeled and assessed data on risk after abnormal tests from almost 1.4 million women followed over 8 years in the KPNC Medical Care Plan—this cohort has provided us with “big data.”
The sheer size of the Kaiser Permanente population made it possible for the ASCCP-led panel to validate its previous guidelines or to modify them, where needed. It also made risk-based stratification possible for even rare abnormalities and clinical outcomes.
Although findings from the KPNC population may not be fully generalizable to the US population as a whole, they enhance our understanding of the optimal management of abnormal cervical cancer screening tests and cancer precursors. More widely dispersed study cohorts on a similar scale in the United States are unlikely in the near future.
Related article: Update on cervical disease Mark H. Einstein, MD, MS, and J. Thomas Cox, MD (May 2013)
SEVERAL SIGNIFICANT MODIFICATIONS
Although the ASCCP reaffirmed most elements of its 2006 consensus management guidelines, it did make a number of changes:
- Women who have ASC-US cytology but test HPV-negative now should be followed with cotesting at 3 years rather than 5 years before they return to routine screening.
- Women near age 65 who have a negative finding on ASC-US cytology and HPV testing should not exit screening.
- Women who have ASC-US cytology and test HPV-positive should go to immediate colposcopy, regardless of hrHPV results, including genotyping.
- Women who test positive for HPV 16 or 18 but have negative cytology should undergo immediate colposcopy.
- Women aged 21 to 24 years should be managed as conservatively and minimally invasively as possible, especially when an abnormality is minor.
- Endocervical curettage reported as CIN 1 should be managed as CIN 1, not as a positive endocervical curettage.
- When a cytologic sample is unsatisfactory, sampling usually should be repeated, even when HPV cotesting results are known. However, negative cytology that lacks sufficient endocervical cells or a transformation zone component usually can be managed without frequent follow-up.
Related article: New cervical Ca screening guidelines recommend less frequent assessment Janelle Yates (News for your Practice; April 2012)
EQUAL MANAGEMENT SHOULD BE PERFORMED FOR ABNORMAL TESTS THAT INDICATE EQUAL RISK
The ASCCP-led management panel unanimously agreed to several basic assumptions in formulating the updated guidelines. For example, they concurred that achieving zero risk for cancer is impossible and that attempts to achieve zero risk (which typically means more frequent testing) may cause harm. They also cited the 2011 American Cancer Society/ASCCP/American Society for Clinical Pathology consensus screening document, which stated: “Optimal prevention strategies should identify those HPV-related abnormalities likely to progress to invasive cancers while avoiding destructive treatment of abnormalities not destined to become cancerous.”1
The panel also agreed that CIN 3+ is a “reasonable proxy for cancer risk.” When calculating risk, the KPNC data were modeled for all combinations of cytology and HPV testing, using CIN 3+ for many of the outcomes, and when outcomes were rare, using CIN 2+. The theme of equal management for equal risk was the rationale behind the management approaches detailed in the TABLE. Risks were deemed to be low and return to normal screening was recommended when the risks were similar to the rate of CIN 3+ 3 years after negative cytology or 5 years after negative cotesting. However, immediate colposcopy was recommended when the 5-year risk of CIN 3+ for the combination of cytology and hrHPV testing, when indicated, exceeded 5%. A 6-month to 12-month return (intermediate risk) is indicated with a risk of CIN3+ of 2% to 5%.
An emphasis on avoiding harms
Abnormal findings at the time of cervical cancer screening can lead to a number of harms for the patient, including anxiety and emotional distress, particularly when colposcopy is necessary, as well as time lost from home and work life. For this reason, the guidelines panel emphasized that colposcopy and other interventions should be avoided when the risk of CIN 3+ is low and when the cervical screening abnormalities are likely to resolve without treatment.
However, women who experience postcoital bleeding, unexplained abnormal vaginal bleeding, pelvic pain, abnormal discharge, or a visible lesion should be managed promptly on an individualized basis.
Long-term effects of HPV vaccination are unknown
Among the areas that remain to be addressed are the unknown effects of widespread prophylactic HPV vaccination over the long term. We also lack full understanding of whether and how HPV vaccination will alter the incidence and management of cytologic and histologic abnormalities. Given the low rates of vaccination against HPV in the United States at present, this will need to be re-evaluated in the future.
What this EVIDENCE means for practice
The updated ASCCP guidelines are inherently complex, but their complexity arises from a large body of high-quality prospective data from a large population of women. Equal risk should result in equal management of cervical screening test abnormalities. Practitioners need not feel obligated to memorize the guidelines, owing to the availability of algorithms for specific findings in specific populations at the ASCCP Web site (www.asccp.org/consensus2012). Apps also are available for the iPhone, iPad, and Android.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
Reference
- Saslow D, Solomon D, Lawson HW, et al;ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172.
Reference
- Saslow D, Solomon D, Lawson HW, et al;ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172.
Dr. Mark Einstein anticipated final FDA approval of the first HPV test for primary cervical cancer screening and, in this UPDATE ON CERVICAL DISEASE, expands on the data behind the approval and how your practice could change