User login
VIDEO: Abnormal endocrinology labs? Look beyond ‘usual suspects’
PHILADELPHIA – Psychiatric medications can affect prolactin levels, while antibodies can affect thyroid-stimulating hormone levels. Hirsutism may be the result of polycystic ovary syndrome – but it may also be caused by congenital adrenal hyperplasia.
And if that’s not confounding enough, physicians should add to the medical factors that can influence lab reports what Dr. Ellen L. Connor says is the importance of "knowing the typical ranges of the assays you are using, and what the ranges considered normal are at the [laboratory] you’re working with."
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Connor of the department of pediatric endocrinology at the University of Wisconsin, Madison, reviews what can change prolactin levels, how to get the most clinical utility out of thyroid tests, what is the gold standard for testosterone testing in women, how best to test and interpret vitamin D levels, and what adrenal malfunctions are possible in young women. She also stresses the value of working with knowledgeable lab personnel.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – Psychiatric medications can affect prolactin levels, while antibodies can affect thyroid-stimulating hormone levels. Hirsutism may be the result of polycystic ovary syndrome – but it may also be caused by congenital adrenal hyperplasia.
And if that’s not confounding enough, physicians should add to the medical factors that can influence lab reports what Dr. Ellen L. Connor says is the importance of "knowing the typical ranges of the assays you are using, and what the ranges considered normal are at the [laboratory] you’re working with."
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Connor of the department of pediatric endocrinology at the University of Wisconsin, Madison, reviews what can change prolactin levels, how to get the most clinical utility out of thyroid tests, what is the gold standard for testosterone testing in women, how best to test and interpret vitamin D levels, and what adrenal malfunctions are possible in young women. She also stresses the value of working with knowledgeable lab personnel.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – Psychiatric medications can affect prolactin levels, while antibodies can affect thyroid-stimulating hormone levels. Hirsutism may be the result of polycystic ovary syndrome – but it may also be caused by congenital adrenal hyperplasia.
And if that’s not confounding enough, physicians should add to the medical factors that can influence lab reports what Dr. Ellen L. Connor says is the importance of "knowing the typical ranges of the assays you are using, and what the ranges considered normal are at the [laboratory] you’re working with."
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Connor of the department of pediatric endocrinology at the University of Wisconsin, Madison, reviews what can change prolactin levels, how to get the most clinical utility out of thyroid tests, what is the gold standard for testosterone testing in women, how best to test and interpret vitamin D levels, and what adrenal malfunctions are possible in young women. She also stresses the value of working with knowledgeable lab personnel.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM NASPAG 2014
AUDIO: Polycystic ovary syndrome seen as ‘multiple diseases’
PHILADELPHIA – "My personal opinion is that polycystic ovary syndrome is probably multiple diseases."
That’s according to Dr. Selma Witchel, an associate professor of pediatric endocrinology at the Children’s Hospital of Pittsburgh, University of Pittsburgh Medical Center, who discussed diagnosis and management of PCOS in an interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology.
The best approach to treating young women with PCOS depends on a number of factors, Dr. Witchel notes. She also explains the most appropriate off-label use of metformin, as well as when using it can pose risks to the patient. Dr. Witchel also discusses novel therapies, including the potential promise of acupuncture and the off-label use of statins, and how to help pediatric patients transition to adult care.
On Twitter @whitneymcknight.com
PHILADELPHIA – "My personal opinion is that polycystic ovary syndrome is probably multiple diseases."
That’s according to Dr. Selma Witchel, an associate professor of pediatric endocrinology at the Children’s Hospital of Pittsburgh, University of Pittsburgh Medical Center, who discussed diagnosis and management of PCOS in an interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology.
The best approach to treating young women with PCOS depends on a number of factors, Dr. Witchel notes. She also explains the most appropriate off-label use of metformin, as well as when using it can pose risks to the patient. Dr. Witchel also discusses novel therapies, including the potential promise of acupuncture and the off-label use of statins, and how to help pediatric patients transition to adult care.
On Twitter @whitneymcknight.com
PHILADELPHIA – "My personal opinion is that polycystic ovary syndrome is probably multiple diseases."
That’s according to Dr. Selma Witchel, an associate professor of pediatric endocrinology at the Children’s Hospital of Pittsburgh, University of Pittsburgh Medical Center, who discussed diagnosis and management of PCOS in an interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology.
The best approach to treating young women with PCOS depends on a number of factors, Dr. Witchel notes. She also explains the most appropriate off-label use of metformin, as well as when using it can pose risks to the patient. Dr. Witchel also discusses novel therapies, including the potential promise of acupuncture and the off-label use of statins, and how to help pediatric patients transition to adult care.
On Twitter @whitneymcknight.com
EXPERT ANALYSIS FROM THE NASPAG ANNUAL MEETING
Hepatitis B screening recommended for high-risk patients
Physicians should screen all asymptomatic but high-risk adolescents and adults for hepatitis B virus infection, according to an updated recommendation by the U.S. Preventive Services Task Force that was published online May 27 in Annals of Internal Medicine.
Since the last USPSTF recommendation on HBV screening in 2004, which focused on the general population and didn’t advocate screening of this subset of patients, research has documented that antiviral treatment improves both intermediate outcomes such as virologic and histologic responses and long-term outcomes such as prevention of hepatocellular carcinoma, cirrhosis, and end-stage liver disease.
Given this effectiveness, along with the 98% sensitivity and specificity of HBV screening tests, the group has now issued a level B recommendation that high-risk patients be screened, said Dr. Michael L. LeFevre, chair of the USPSTF and professor of family and community medicine at the University of Missouri, Columbia, and his associates.
High-risk patients include the following:
• People born in regions where the prevalence of HBV infection is 2% or greater, such as sub-Saharan Africa, central and southeast Asia, China, the Pacific Islands, and parts of Latin America. People born in these areas account for 47%-95% of the chronic HBV infection in the United States.
• American-born children of parents from these regions, who may not have been vaccinated in infancy.
• HIV-positive persons.
• IV-drug users.
• Household contacts of people with HBV infection.
• Men who have sex with men.
The updated USPSTF recommendations are in line with those of the Centers for Disease Control and Prevention, the American Association for the Study of Liver Diseases, the Institute of Medicine, and the American Academy of Family Physicians. The CDC additionally recommends HBV screening for blood, organ, or tissue donors; people with occupational or other exposure to infectious blood or body fluids; and patients receiving hemodialysis, cytotoxic therapy, or immunosuppressive therapy.
The USPSTF still does not recommend HBV screening for the general population. The prevalence of the infection is low in the U.S. general population, and most members of the general population who are infected with HBV do not develop the chronic form of the infection and do not develop complications like hepatocellular carcinoma or cirrhosis. The potential harms of general screening, then, probably exceed the potential benefits, Dr. LeFevre and his associates noted (Ann Intern. Med. 2014 May 27 [doi:10.7326/M14-1018]).
The USPSTF has separate recommendations regarding hepatitis B in pregnant women. These, along with the updated recommendations for high-risk patients, are available at www.uspreventiveservicestaskforce.org.
The USPSTF is a voluntary group funded by the Agency for Healthcare Research and Quality but otherwise independent of the federal government. Dr. LeFevre and his associates reported no potential financial conflicts of interest.
These "long overdue" recommendations are "a dramatic and welcome upgrade from the 2004 USPSTF guidelines, which issued a grade D recommendation against screening asymptomatic persons for HBV infection," said Dr. Ruma Rajbhandari and Dr. Raymond T. Chung.
"Many would argue that the USPSTF should have endorsed screening for HBV infection in high-risk populations a decade ago," they wrote. The group lagged far behind the American Association for the Study of Liver Diseases’ recommendations in 2001 and the CDC’s recommendations in 2005. "We may have thus missed an opportunity to screen many high-risk persons in the United States," Dr. Rajbhandari and Dr. Chung said.
The USPSTF update "would be more useful if they provided a clearer definition of the high-risk patient. ... We worry that busy generalist clinicians do not have the time to estimate their patients’ risks for HBV infection." Physicians may find it more helpful to look up the CDC’s table listing all the factors that render a patient high risk, they added.
Dr. Rajbhandari and Dr. Chung are with the liver center and gastrointestinal division at Massachusetts General Hospital, Boston. They reported no relevant conflicts of interest. These remarks were taken from their editorial accompanying Dr. Lefevre’s report (Ann. Intern. Med. 2014 May 27 [doi:10.7326/M14-1153]).
These "long overdue" recommendations are "a dramatic and welcome upgrade from the 2004 USPSTF guidelines, which issued a grade D recommendation against screening asymptomatic persons for HBV infection," said Dr. Ruma Rajbhandari and Dr. Raymond T. Chung.
"Many would argue that the USPSTF should have endorsed screening for HBV infection in high-risk populations a decade ago," they wrote. The group lagged far behind the American Association for the Study of Liver Diseases’ recommendations in 2001 and the CDC’s recommendations in 2005. "We may have thus missed an opportunity to screen many high-risk persons in the United States," Dr. Rajbhandari and Dr. Chung said.
The USPSTF update "would be more useful if they provided a clearer definition of the high-risk patient. ... We worry that busy generalist clinicians do not have the time to estimate their patients’ risks for HBV infection." Physicians may find it more helpful to look up the CDC’s table listing all the factors that render a patient high risk, they added.
Dr. Rajbhandari and Dr. Chung are with the liver center and gastrointestinal division at Massachusetts General Hospital, Boston. They reported no relevant conflicts of interest. These remarks were taken from their editorial accompanying Dr. Lefevre’s report (Ann. Intern. Med. 2014 May 27 [doi:10.7326/M14-1153]).
These "long overdue" recommendations are "a dramatic and welcome upgrade from the 2004 USPSTF guidelines, which issued a grade D recommendation against screening asymptomatic persons for HBV infection," said Dr. Ruma Rajbhandari and Dr. Raymond T. Chung.
"Many would argue that the USPSTF should have endorsed screening for HBV infection in high-risk populations a decade ago," they wrote. The group lagged far behind the American Association for the Study of Liver Diseases’ recommendations in 2001 and the CDC’s recommendations in 2005. "We may have thus missed an opportunity to screen many high-risk persons in the United States," Dr. Rajbhandari and Dr. Chung said.
The USPSTF update "would be more useful if they provided a clearer definition of the high-risk patient. ... We worry that busy generalist clinicians do not have the time to estimate their patients’ risks for HBV infection." Physicians may find it more helpful to look up the CDC’s table listing all the factors that render a patient high risk, they added.
Dr. Rajbhandari and Dr. Chung are with the liver center and gastrointestinal division at Massachusetts General Hospital, Boston. They reported no relevant conflicts of interest. These remarks were taken from their editorial accompanying Dr. Lefevre’s report (Ann. Intern. Med. 2014 May 27 [doi:10.7326/M14-1153]).
Physicians should screen all asymptomatic but high-risk adolescents and adults for hepatitis B virus infection, according to an updated recommendation by the U.S. Preventive Services Task Force that was published online May 27 in Annals of Internal Medicine.
Since the last USPSTF recommendation on HBV screening in 2004, which focused on the general population and didn’t advocate screening of this subset of patients, research has documented that antiviral treatment improves both intermediate outcomes such as virologic and histologic responses and long-term outcomes such as prevention of hepatocellular carcinoma, cirrhosis, and end-stage liver disease.
Given this effectiveness, along with the 98% sensitivity and specificity of HBV screening tests, the group has now issued a level B recommendation that high-risk patients be screened, said Dr. Michael L. LeFevre, chair of the USPSTF and professor of family and community medicine at the University of Missouri, Columbia, and his associates.
High-risk patients include the following:
• People born in regions where the prevalence of HBV infection is 2% or greater, such as sub-Saharan Africa, central and southeast Asia, China, the Pacific Islands, and parts of Latin America. People born in these areas account for 47%-95% of the chronic HBV infection in the United States.
• American-born children of parents from these regions, who may not have been vaccinated in infancy.
• HIV-positive persons.
• IV-drug users.
• Household contacts of people with HBV infection.
• Men who have sex with men.
The updated USPSTF recommendations are in line with those of the Centers for Disease Control and Prevention, the American Association for the Study of Liver Diseases, the Institute of Medicine, and the American Academy of Family Physicians. The CDC additionally recommends HBV screening for blood, organ, or tissue donors; people with occupational or other exposure to infectious blood or body fluids; and patients receiving hemodialysis, cytotoxic therapy, or immunosuppressive therapy.
The USPSTF still does not recommend HBV screening for the general population. The prevalence of the infection is low in the U.S. general population, and most members of the general population who are infected with HBV do not develop the chronic form of the infection and do not develop complications like hepatocellular carcinoma or cirrhosis. The potential harms of general screening, then, probably exceed the potential benefits, Dr. LeFevre and his associates noted (Ann Intern. Med. 2014 May 27 [doi:10.7326/M14-1018]).
The USPSTF has separate recommendations regarding hepatitis B in pregnant women. These, along with the updated recommendations for high-risk patients, are available at www.uspreventiveservicestaskforce.org.
The USPSTF is a voluntary group funded by the Agency for Healthcare Research and Quality but otherwise independent of the federal government. Dr. LeFevre and his associates reported no potential financial conflicts of interest.
Physicians should screen all asymptomatic but high-risk adolescents and adults for hepatitis B virus infection, according to an updated recommendation by the U.S. Preventive Services Task Force that was published online May 27 in Annals of Internal Medicine.
Since the last USPSTF recommendation on HBV screening in 2004, which focused on the general population and didn’t advocate screening of this subset of patients, research has documented that antiviral treatment improves both intermediate outcomes such as virologic and histologic responses and long-term outcomes such as prevention of hepatocellular carcinoma, cirrhosis, and end-stage liver disease.
Given this effectiveness, along with the 98% sensitivity and specificity of HBV screening tests, the group has now issued a level B recommendation that high-risk patients be screened, said Dr. Michael L. LeFevre, chair of the USPSTF and professor of family and community medicine at the University of Missouri, Columbia, and his associates.
High-risk patients include the following:
• People born in regions where the prevalence of HBV infection is 2% or greater, such as sub-Saharan Africa, central and southeast Asia, China, the Pacific Islands, and parts of Latin America. People born in these areas account for 47%-95% of the chronic HBV infection in the United States.
• American-born children of parents from these regions, who may not have been vaccinated in infancy.
• HIV-positive persons.
• IV-drug users.
• Household contacts of people with HBV infection.
• Men who have sex with men.
The updated USPSTF recommendations are in line with those of the Centers for Disease Control and Prevention, the American Association for the Study of Liver Diseases, the Institute of Medicine, and the American Academy of Family Physicians. The CDC additionally recommends HBV screening for blood, organ, or tissue donors; people with occupational or other exposure to infectious blood or body fluids; and patients receiving hemodialysis, cytotoxic therapy, or immunosuppressive therapy.
The USPSTF still does not recommend HBV screening for the general population. The prevalence of the infection is low in the U.S. general population, and most members of the general population who are infected with HBV do not develop the chronic form of the infection and do not develop complications like hepatocellular carcinoma or cirrhosis. The potential harms of general screening, then, probably exceed the potential benefits, Dr. LeFevre and his associates noted (Ann Intern. Med. 2014 May 27 [doi:10.7326/M14-1018]).
The USPSTF has separate recommendations regarding hepatitis B in pregnant women. These, along with the updated recommendations for high-risk patients, are available at www.uspreventiveservicestaskforce.org.
The USPSTF is a voluntary group funded by the Agency for Healthcare Research and Quality but otherwise independent of the federal government. Dr. LeFevre and his associates reported no potential financial conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: HBV screening is appropriate in all at-risk populations.
Major finding: Physicians should screen all adolescents and adults at high risk for HBV infection, including those born in regions where the virus is endemic, American-born children of such parents, household contacts of people with HBV, people with HIV, IV-drug users, and men who have sex with men.
Data source: A comprehensive review of the literature since 2004 regarding the benefits and harms of screening high-risk patients for HBV infection, and a compilation of recommendations for screening high-risk patients.
Disclosures: The USPSTF is a voluntary group funded by the Agency for Healthcare Research and Quality but otherwise independent of the federal government. Dr. LeFevre and his associates reported no potential financial conflicts of interest.
Transvaginal ultrasonography of ovarian cyst
Longer laparoscopic and robotic hysterectomy time ups perioperative risk
CHICAGO – Longer operative time is independently associated with perioperative morbidity after laparoscopic and robotic hysterectomy, according to a review of cases from the American College of Surgeons National Surgical Quality Improvement Program.
The overall complication rate in the 9,064 laparoscopic and robotic hysterectomies recorded in the database (ACS NSQIP) increased significantly and in tandem with increasing operative time, Dr. Tatiana L. Catanzarite reported in a blue ribbon poster at the annual meeting of the American Congress of Obstetricians and Gynecologists.
For example, the overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes, according to Dr. Catanzarite of Northwestern University, Chicago.
Operative time of 240 minutes or longer was associated with increased overall complications, medical complications, surgical complications, reoperation, transfusion, urinary tract infection, and deep vein thrombosis/pulmonary embolism on both bivariate and multivariable regression analysis. Factors associated with operative time of 240 minutes or longer included age over 50 years, obesity, nonsmoking status, hypertension, history of stroke or transient ischemic attack, and American Anesthesiologists Society (ASA) class greater than 3, she noted.
Patients included in the database, which contains prospectively collected data for more than 240 variables from more than 460 participating institutions, underwent total or subtotal laparoscopic hysterectomy between 2006 and 2011. Patients with concomitant procedures, emergency surgery, gynecologic cancer, ASA class 5, or operative time less than 20 minutes were excluded from the analysis.
Similar findings have been reported for general surgery, but studies in gynecology have been conflicting, Dr. Catanzarite noted.
"Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency," she wrote.
Dr. Catanzarite reported having no relevant financial disclosures.
CHICAGO – Longer operative time is independently associated with perioperative morbidity after laparoscopic and robotic hysterectomy, according to a review of cases from the American College of Surgeons National Surgical Quality Improvement Program.
The overall complication rate in the 9,064 laparoscopic and robotic hysterectomies recorded in the database (ACS NSQIP) increased significantly and in tandem with increasing operative time, Dr. Tatiana L. Catanzarite reported in a blue ribbon poster at the annual meeting of the American Congress of Obstetricians and Gynecologists.
For example, the overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes, according to Dr. Catanzarite of Northwestern University, Chicago.
Operative time of 240 minutes or longer was associated with increased overall complications, medical complications, surgical complications, reoperation, transfusion, urinary tract infection, and deep vein thrombosis/pulmonary embolism on both bivariate and multivariable regression analysis. Factors associated with operative time of 240 minutes or longer included age over 50 years, obesity, nonsmoking status, hypertension, history of stroke or transient ischemic attack, and American Anesthesiologists Society (ASA) class greater than 3, she noted.
Patients included in the database, which contains prospectively collected data for more than 240 variables from more than 460 participating institutions, underwent total or subtotal laparoscopic hysterectomy between 2006 and 2011. Patients with concomitant procedures, emergency surgery, gynecologic cancer, ASA class 5, or operative time less than 20 minutes were excluded from the analysis.
Similar findings have been reported for general surgery, but studies in gynecology have been conflicting, Dr. Catanzarite noted.
"Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency," she wrote.
Dr. Catanzarite reported having no relevant financial disclosures.
CHICAGO – Longer operative time is independently associated with perioperative morbidity after laparoscopic and robotic hysterectomy, according to a review of cases from the American College of Surgeons National Surgical Quality Improvement Program.
The overall complication rate in the 9,064 laparoscopic and robotic hysterectomies recorded in the database (ACS NSQIP) increased significantly and in tandem with increasing operative time, Dr. Tatiana L. Catanzarite reported in a blue ribbon poster at the annual meeting of the American Congress of Obstetricians and Gynecologists.
For example, the overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes, according to Dr. Catanzarite of Northwestern University, Chicago.
Operative time of 240 minutes or longer was associated with increased overall complications, medical complications, surgical complications, reoperation, transfusion, urinary tract infection, and deep vein thrombosis/pulmonary embolism on both bivariate and multivariable regression analysis. Factors associated with operative time of 240 minutes or longer included age over 50 years, obesity, nonsmoking status, hypertension, history of stroke or transient ischemic attack, and American Anesthesiologists Society (ASA) class greater than 3, she noted.
Patients included in the database, which contains prospectively collected data for more than 240 variables from more than 460 participating institutions, underwent total or subtotal laparoscopic hysterectomy between 2006 and 2011. Patients with concomitant procedures, emergency surgery, gynecologic cancer, ASA class 5, or operative time less than 20 minutes were excluded from the analysis.
Similar findings have been reported for general surgery, but studies in gynecology have been conflicting, Dr. Catanzarite noted.
"Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency," she wrote.
Dr. Catanzarite reported having no relevant financial disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Future research should aim to identify risk factors for excessive operative time in order to select appropriate candidates for minimally invasive approaches and maximize surgical efficiency.
Major finding: The overall complication rate was 2.79% for operative time of 20-59 minutes and 18.75% for operative time greater than 360 minutes.
Data source: A retrospective study of more than 9,000 cases.
Disclosures: Dr. Catanzarite reported having no relevant financial disclosures.
Perioperative complications of hysterectomy vary by route
SCOTTSDALE, ARIZ. – Rates of perioperative complications among women undergoing hysterectomy for benign indications vary according to the route, an ancillary analysis of a retrospective cohort study found.
Analyses were based on 1,440 women who underwent hysterectomy at four teaching hospitals, with procedures about evenly split between the eras before and after introduction of robotic surgery, lead author Dr. Salma Rahimi of Mount Sinai Hospital, New York, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
In the prerobot era, the rate of intraoperative complications – injury of the ureter, bladder, or bowel, or transfusion – was lowest at 3.7% for laparoscopic hysterectomy, about half that for abdominal procedures, and roughly the same as that for vaginal ones. The rate of postoperative complications – infection requiring antibiotics, transfusion, small bowel obstruction, or ileus – was 1.8% with laparoscopic hysterectomy, roughly a third of that seen with the other approaches.
In the postrobot era, the rate of intraoperative complications was 2.8% with vaginal hysterectomy, the lowest value for any approach, including the robotic one. The rate of postoperative complications was 3.0% for robotic hysterectomy, about a quarter of that for abdominal procedures and roughly on a par with that for vaginal and laparoscopic ones.
"Our data demonstrate that a vaginal hysterectomy is associated with fewer intraoperative complications in both the pre- and postrobot period," Dr. Rahimi commented. However, "vaginal hysterectomy was associated with more postoperative infections in the prerobot period."
"The highest complications were noted in the abdominal group, mostly due to transfusions, infections, small bowel obstructions, and ileus," she added.
Introducing the study, she noted that the American College of Obstetricians and Gynecologists recommends vaginal hysterectomy as a first choice over other routes given its relatively better outcomes and lower rates of complications (Obstet. Gynecol. 2009;114:1156-8). "Despite this, most are performed by laparotomy, and there is an increasing trend toward the use of minimally invasive abdominal approaches. Only about 20% are performed by the vaginal approach," she said.
The investigators studied women undergoing hysterectomy identified through the Fellows’ Pelvic Research Network. All of the operations were performed at hospitals with an obstetrics and gynecology residency and had a fellow belonging to the network. Women were excluded if their hysterectomy was performed by a gynecologic oncologist, was for a suspected malignancy, or was done emergently (including cesarean hysterectomies).
Analyses were based on 732 women in the prerobot era (the year before introduction of robotics at each hospital) and 708 in the postrobot era (2011). Characteristics of the women from the two eras were essentially the same, Dr. Rahimi reported at the meeting, jointly sponsored by the American College of Surgeons.
In the prerobot era, the rate of intraoperative complications was 3.9% for vaginal hysterectomy, compared with 7.4% for abdominal hysterectomy (P less than .05) and 3.7% for laparoscopic hysterectomy (P not significant).
The rate of postoperative complications was 8.3% for vaginal hysterectomy, compared with 7.4% for abdominal hysterectomy (P not significant) and 1.8% for laparoscopic hysterectomy (P = .001). These differences were mainly driven by higher rates of infection with the vaginal and abdominal approaches, and a higher rate of small bowel obstruction and ileus with the abdominal approach.
In the postrobot era, the rate of intraoperative complications was 2.8% for vaginal hysterectomy, compared with 10.8% for abdominal hysterectomy (P = .003), 4.6% for laparoscopic hysterectomy (P not significant), and 3.0% for robotic hysterectomy (P not significant). The differences were mainly due to a higher rate of transfusion with the abdominal approach.
The rate of postoperative complications was 5.1% for vaginal hysterectomy, compared with 13.9% for abdominal hysterectomy (P = .008), 3.6% for laparoscopic hysterectomy (P not significant), and 3.0% for robotic hysterectomy (P not significant). The differences again were mainly due to a higher rate of transfusion when surgery was done abdominally.
Dr. Rahimi disclosed no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – Rates of perioperative complications among women undergoing hysterectomy for benign indications vary according to the route, an ancillary analysis of a retrospective cohort study found.
Analyses were based on 1,440 women who underwent hysterectomy at four teaching hospitals, with procedures about evenly split between the eras before and after introduction of robotic surgery, lead author Dr. Salma Rahimi of Mount Sinai Hospital, New York, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
In the prerobot era, the rate of intraoperative complications – injury of the ureter, bladder, or bowel, or transfusion – was lowest at 3.7% for laparoscopic hysterectomy, about half that for abdominal procedures, and roughly the same as that for vaginal ones. The rate of postoperative complications – infection requiring antibiotics, transfusion, small bowel obstruction, or ileus – was 1.8% with laparoscopic hysterectomy, roughly a third of that seen with the other approaches.
In the postrobot era, the rate of intraoperative complications was 2.8% with vaginal hysterectomy, the lowest value for any approach, including the robotic one. The rate of postoperative complications was 3.0% for robotic hysterectomy, about a quarter of that for abdominal procedures and roughly on a par with that for vaginal and laparoscopic ones.
"Our data demonstrate that a vaginal hysterectomy is associated with fewer intraoperative complications in both the pre- and postrobot period," Dr. Rahimi commented. However, "vaginal hysterectomy was associated with more postoperative infections in the prerobot period."
"The highest complications were noted in the abdominal group, mostly due to transfusions, infections, small bowel obstructions, and ileus," she added.
Introducing the study, she noted that the American College of Obstetricians and Gynecologists recommends vaginal hysterectomy as a first choice over other routes given its relatively better outcomes and lower rates of complications (Obstet. Gynecol. 2009;114:1156-8). "Despite this, most are performed by laparotomy, and there is an increasing trend toward the use of minimally invasive abdominal approaches. Only about 20% are performed by the vaginal approach," she said.
The investigators studied women undergoing hysterectomy identified through the Fellows’ Pelvic Research Network. All of the operations were performed at hospitals with an obstetrics and gynecology residency and had a fellow belonging to the network. Women were excluded if their hysterectomy was performed by a gynecologic oncologist, was for a suspected malignancy, or was done emergently (including cesarean hysterectomies).
Analyses were based on 732 women in the prerobot era (the year before introduction of robotics at each hospital) and 708 in the postrobot era (2011). Characteristics of the women from the two eras were essentially the same, Dr. Rahimi reported at the meeting, jointly sponsored by the American College of Surgeons.
In the prerobot era, the rate of intraoperative complications was 3.9% for vaginal hysterectomy, compared with 7.4% for abdominal hysterectomy (P less than .05) and 3.7% for laparoscopic hysterectomy (P not significant).
The rate of postoperative complications was 8.3% for vaginal hysterectomy, compared with 7.4% for abdominal hysterectomy (P not significant) and 1.8% for laparoscopic hysterectomy (P = .001). These differences were mainly driven by higher rates of infection with the vaginal and abdominal approaches, and a higher rate of small bowel obstruction and ileus with the abdominal approach.
In the postrobot era, the rate of intraoperative complications was 2.8% for vaginal hysterectomy, compared with 10.8% for abdominal hysterectomy (P = .003), 4.6% for laparoscopic hysterectomy (P not significant), and 3.0% for robotic hysterectomy (P not significant). The differences were mainly due to a higher rate of transfusion with the abdominal approach.
The rate of postoperative complications was 5.1% for vaginal hysterectomy, compared with 13.9% for abdominal hysterectomy (P = .008), 3.6% for laparoscopic hysterectomy (P not significant), and 3.0% for robotic hysterectomy (P not significant). The differences again were mainly due to a higher rate of transfusion when surgery was done abdominally.
Dr. Rahimi disclosed no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – Rates of perioperative complications among women undergoing hysterectomy for benign indications vary according to the route, an ancillary analysis of a retrospective cohort study found.
Analyses were based on 1,440 women who underwent hysterectomy at four teaching hospitals, with procedures about evenly split between the eras before and after introduction of robotic surgery, lead author Dr. Salma Rahimi of Mount Sinai Hospital, New York, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
In the prerobot era, the rate of intraoperative complications – injury of the ureter, bladder, or bowel, or transfusion – was lowest at 3.7% for laparoscopic hysterectomy, about half that for abdominal procedures, and roughly the same as that for vaginal ones. The rate of postoperative complications – infection requiring antibiotics, transfusion, small bowel obstruction, or ileus – was 1.8% with laparoscopic hysterectomy, roughly a third of that seen with the other approaches.
In the postrobot era, the rate of intraoperative complications was 2.8% with vaginal hysterectomy, the lowest value for any approach, including the robotic one. The rate of postoperative complications was 3.0% for robotic hysterectomy, about a quarter of that for abdominal procedures and roughly on a par with that for vaginal and laparoscopic ones.
"Our data demonstrate that a vaginal hysterectomy is associated with fewer intraoperative complications in both the pre- and postrobot period," Dr. Rahimi commented. However, "vaginal hysterectomy was associated with more postoperative infections in the prerobot period."
"The highest complications were noted in the abdominal group, mostly due to transfusions, infections, small bowel obstructions, and ileus," she added.
Introducing the study, she noted that the American College of Obstetricians and Gynecologists recommends vaginal hysterectomy as a first choice over other routes given its relatively better outcomes and lower rates of complications (Obstet. Gynecol. 2009;114:1156-8). "Despite this, most are performed by laparotomy, and there is an increasing trend toward the use of minimally invasive abdominal approaches. Only about 20% are performed by the vaginal approach," she said.
The investigators studied women undergoing hysterectomy identified through the Fellows’ Pelvic Research Network. All of the operations were performed at hospitals with an obstetrics and gynecology residency and had a fellow belonging to the network. Women were excluded if their hysterectomy was performed by a gynecologic oncologist, was for a suspected malignancy, or was done emergently (including cesarean hysterectomies).
Analyses were based on 732 women in the prerobot era (the year before introduction of robotics at each hospital) and 708 in the postrobot era (2011). Characteristics of the women from the two eras were essentially the same, Dr. Rahimi reported at the meeting, jointly sponsored by the American College of Surgeons.
In the prerobot era, the rate of intraoperative complications was 3.9% for vaginal hysterectomy, compared with 7.4% for abdominal hysterectomy (P less than .05) and 3.7% for laparoscopic hysterectomy (P not significant).
The rate of postoperative complications was 8.3% for vaginal hysterectomy, compared with 7.4% for abdominal hysterectomy (P not significant) and 1.8% for laparoscopic hysterectomy (P = .001). These differences were mainly driven by higher rates of infection with the vaginal and abdominal approaches, and a higher rate of small bowel obstruction and ileus with the abdominal approach.
In the postrobot era, the rate of intraoperative complications was 2.8% for vaginal hysterectomy, compared with 10.8% for abdominal hysterectomy (P = .003), 4.6% for laparoscopic hysterectomy (P not significant), and 3.0% for robotic hysterectomy (P not significant). The differences were mainly due to a higher rate of transfusion with the abdominal approach.
The rate of postoperative complications was 5.1% for vaginal hysterectomy, compared with 13.9% for abdominal hysterectomy (P = .008), 3.6% for laparoscopic hysterectomy (P not significant), and 3.0% for robotic hysterectomy (P not significant). The differences again were mainly due to a higher rate of transfusion when surgery was done abdominally.
Dr. Rahimi disclosed no relevant conflicts of interest.
AT SGS 2014
Key clinical point: Intraoperative complications tend to be low with vaginal, laparoscopic, and robotic hysterectomies.
Major finding: In the postrobot era, the rate of intraoperative complications was 2.8% for vaginal procedures, 10.8% for abdominal ones, 4.6% for laparoscopic ones, and 3.0% for robotic ones.
Data source: An ancillary analysis of a retrospective cohort study of 1,440 cases of hysterectomy done for benign indications
Disclosures: Dr. Rahimi disclosed no relevant conflicts of interest.
Buccal acyclovir delays recurrence of herpes labialis
ALBUQUERQUE – A single buccal application of acyclovir delayed recurrence of herpes labialis by an average of 100 days, compared with placebo, according to the results of a randomized, double-blind, phase III study.
The 50-mg buccal mucoadhesive tablet also reduced recurrence of herpes labialis by 9.4% during the 9-month follow-up period, Dr. Christopher Downing said at the annual meeting of the Society for Investigative Dermatology.
The tablet is designed to be applied to the gum above the canine incisor at the time of prodromal symptoms, said Dr. Downing of the Center for Clinical Studies in Webster, Texas. Patients hold the tablet in place for 30 seconds, and acyclovir is then absorbed into the labial mucosa for the next 6-8 hours, Dr. Downing said, adding that salivary and mucosal concentrations remain at high levels for at least 24 hours.
"We know that the replication of HSV-1 is highest before and during the first hours of prodromal symptoms," Dr. Downing added. "Therefore, rapid and high concentrations of antiviral drug are needed."
The researchers enrolled 775 immunocompetent patients who had experienced at least four recurrent episodes of herpes labialis in the past 12 months. Patients had to be able to identify their prodromal symptoms to be enrolled in the study. A total of 378 patients were randomized to receive the acyclovir buccal tablet, while 397 were randomized to placebo. In all, 537 patients were evaluated during the entire 9-month follow-up period, and 59 patients had missing data.
A total of 330 patients had recurrence of a primary vesicular lesion, but a significantly fewer 149 (64.2%) in the treatment group vs. 181 (73.6%) in the control group (P = 0.027). In a subanalysis of 415 patients who applied the tablet within the first hour after noticing prodromal symptoms, lesions recurred in 63.2% of the treatment group and in 71.6% of the placebo group, said Dr. Downing.
The time to the next recurrence in the treatment group was 304 days (standard deviation, 19.4 days), compared with 199 days for the placebo group (SD, 9.3 days; P = 0.042).
The tablet "may modify the clinical course of labial herpes," the investigators noted. "By having a high salivary concentration and a high mucosal concentration of acyclovir during the time of highest replication, we’re seeing a difference in time to recurrence," said Dr. Downing. "We’re not sure exactly what the mechanism of action is."
Senior author Dr. Pierre Attali is with BioAlliance Pharma in Paris, which manufactures acyclovir Lauriad, a mucoadhesive buccal tablet.
ALBUQUERQUE – A single buccal application of acyclovir delayed recurrence of herpes labialis by an average of 100 days, compared with placebo, according to the results of a randomized, double-blind, phase III study.
The 50-mg buccal mucoadhesive tablet also reduced recurrence of herpes labialis by 9.4% during the 9-month follow-up period, Dr. Christopher Downing said at the annual meeting of the Society for Investigative Dermatology.
The tablet is designed to be applied to the gum above the canine incisor at the time of prodromal symptoms, said Dr. Downing of the Center for Clinical Studies in Webster, Texas. Patients hold the tablet in place for 30 seconds, and acyclovir is then absorbed into the labial mucosa for the next 6-8 hours, Dr. Downing said, adding that salivary and mucosal concentrations remain at high levels for at least 24 hours.
"We know that the replication of HSV-1 is highest before and during the first hours of prodromal symptoms," Dr. Downing added. "Therefore, rapid and high concentrations of antiviral drug are needed."
The researchers enrolled 775 immunocompetent patients who had experienced at least four recurrent episodes of herpes labialis in the past 12 months. Patients had to be able to identify their prodromal symptoms to be enrolled in the study. A total of 378 patients were randomized to receive the acyclovir buccal tablet, while 397 were randomized to placebo. In all, 537 patients were evaluated during the entire 9-month follow-up period, and 59 patients had missing data.
A total of 330 patients had recurrence of a primary vesicular lesion, but a significantly fewer 149 (64.2%) in the treatment group vs. 181 (73.6%) in the control group (P = 0.027). In a subanalysis of 415 patients who applied the tablet within the first hour after noticing prodromal symptoms, lesions recurred in 63.2% of the treatment group and in 71.6% of the placebo group, said Dr. Downing.
The time to the next recurrence in the treatment group was 304 days (standard deviation, 19.4 days), compared with 199 days for the placebo group (SD, 9.3 days; P = 0.042).
The tablet "may modify the clinical course of labial herpes," the investigators noted. "By having a high salivary concentration and a high mucosal concentration of acyclovir during the time of highest replication, we’re seeing a difference in time to recurrence," said Dr. Downing. "We’re not sure exactly what the mechanism of action is."
Senior author Dr. Pierre Attali is with BioAlliance Pharma in Paris, which manufactures acyclovir Lauriad, a mucoadhesive buccal tablet.
ALBUQUERQUE – A single buccal application of acyclovir delayed recurrence of herpes labialis by an average of 100 days, compared with placebo, according to the results of a randomized, double-blind, phase III study.
The 50-mg buccal mucoadhesive tablet also reduced recurrence of herpes labialis by 9.4% during the 9-month follow-up period, Dr. Christopher Downing said at the annual meeting of the Society for Investigative Dermatology.
The tablet is designed to be applied to the gum above the canine incisor at the time of prodromal symptoms, said Dr. Downing of the Center for Clinical Studies in Webster, Texas. Patients hold the tablet in place for 30 seconds, and acyclovir is then absorbed into the labial mucosa for the next 6-8 hours, Dr. Downing said, adding that salivary and mucosal concentrations remain at high levels for at least 24 hours.
"We know that the replication of HSV-1 is highest before and during the first hours of prodromal symptoms," Dr. Downing added. "Therefore, rapid and high concentrations of antiviral drug are needed."
The researchers enrolled 775 immunocompetent patients who had experienced at least four recurrent episodes of herpes labialis in the past 12 months. Patients had to be able to identify their prodromal symptoms to be enrolled in the study. A total of 378 patients were randomized to receive the acyclovir buccal tablet, while 397 were randomized to placebo. In all, 537 patients were evaluated during the entire 9-month follow-up period, and 59 patients had missing data.
A total of 330 patients had recurrence of a primary vesicular lesion, but a significantly fewer 149 (64.2%) in the treatment group vs. 181 (73.6%) in the control group (P = 0.027). In a subanalysis of 415 patients who applied the tablet within the first hour after noticing prodromal symptoms, lesions recurred in 63.2% of the treatment group and in 71.6% of the placebo group, said Dr. Downing.
The time to the next recurrence in the treatment group was 304 days (standard deviation, 19.4 days), compared with 199 days for the placebo group (SD, 9.3 days; P = 0.042).
The tablet "may modify the clinical course of labial herpes," the investigators noted. "By having a high salivary concentration and a high mucosal concentration of acyclovir during the time of highest replication, we’re seeing a difference in time to recurrence," said Dr. Downing. "We’re not sure exactly what the mechanism of action is."
Senior author Dr. Pierre Attali is with BioAlliance Pharma in Paris, which manufactures acyclovir Lauriad, a mucoadhesive buccal tablet.
AT THE 2014 SID ANNUAL MEETING
Symptoms differ for anterior and posterior prolapse
SCOTTSDALE, ARIZ. – Obstetric risk factors for stage II anterior and posterior pelvic organ prolapse are essentially the same, but symptoms differ, according to a cohort study reported at the annual meeting of the Society of Gynecologic Surgeons.
Investigators led by Dr. MaryAnn Wilbur of the department of obstetrics and gynecology at Johns Hopkins University, Baltimore, analyzed data from women who were 5-10 years out from a first delivery, comparing 85 women with posterior prolapse (with or without concomitant anterior prolapse), 334 women with isolated anterior prolapse, and 1,078 women with no prolapse.
The results showed that having had a vaginal delivery was a risk factor for both posterior and anterior prolapse. But the women with posterior prolapse were significantly more likely to report a loss of gas from the rectum, having to push on the vagina to complete a bowel movement, having a sensation of bulge, and having asked a physician for help because of their symptoms.
"Not surprisingly, prolapse was associated with vaginal delivery, but when we compare anterior versus posterior prolapse, there were no differences in terms of obstetric risk factors, at least that we could perceive in this study," Dr. Wilbur commented. "But the symptomatology was different between those two groups," although the reasons for this difference were not readily apparent.
The investigators analyzed data collected at enrollment, 5-10 years after a first delivery, from women in the Mothers’ Outcomes After Delivery cohort. Most had had their delivery at Greater Baltimore Medical Center, a large community hospital.
The women’s obstetric history was reviewed, they underwent examination including the pelvic organ prolapse quantification (POP-Q) system assessment, and they completed validated measures of symptoms, including the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) and the Colorectal-Anal Impact Questionnaire (CRAIQ).
The investigators categorized the women as having posterior prolapse (with a point A posterior value on the POP-Q greater than or equal to –1) with or without anterior prolapse, isolated anterior prolapse (with a point A anterior value greater than or equal to –1), or no prolapse.
It was not possible to study isolated posterior prolapse because only 20 women had posterior prolapse without concomitant anterior prolapse, Dr. Wilbur explained at the meeting, which was jointly sponsored by the American College of Surgeons.
Compared with the no-prolapse group, both the posterior and anterior prolapse groups were more likely to have completed the first stage of labor (85% and 76% vs. 53%) and to have had a vaginal delivery (79% and 70% vs. 40%), she reported.
The two prolapse groups were similar with respect to these and a variety of other obstetric factors, such as having a prolonged second stage of labor, having an infant weighing at least 4,000 g, having an operative delivery, having an episiotomy, and experiencing perineal tears.
But relative to their counterparts with anterior prolapse, women with posterior prolapse were more likely to report a loss of gas from the rectum (odds ratio, 1.79), having to push on the vagina to complete a bowel movement (1.72), having a sensation of bulge (2.58), and having asked a physician for help because of prolapse symptoms (3.24).
Women with anterior prolapse were similar to women with no prolapse on most of these measures. The exception was that women without prolapse were, not surprisingly, less likely to have asked a physician for help (odds ratio, 0.27).
"We are following these women over time. So those 1,497 women came in for the first visit, but as of today we have 3,840 person-visits, and in the final manuscript, we did do generalized estimating equations where we followed those trends over time," Dr. Wilbur commented. "They are actually very similar to the enrollment data."
The study’s main shortcoming is its potential lack of generalizability, she said. "Greater Baltimore Medical Center does deliver women who are mostly white and relatively affluent in comparison to the general American population."
Dr. Wilbur disclosed no relevant conflicts of interest
SCOTTSDALE, ARIZ. – Obstetric risk factors for stage II anterior and posterior pelvic organ prolapse are essentially the same, but symptoms differ, according to a cohort study reported at the annual meeting of the Society of Gynecologic Surgeons.
Investigators led by Dr. MaryAnn Wilbur of the department of obstetrics and gynecology at Johns Hopkins University, Baltimore, analyzed data from women who were 5-10 years out from a first delivery, comparing 85 women with posterior prolapse (with or without concomitant anterior prolapse), 334 women with isolated anterior prolapse, and 1,078 women with no prolapse.
The results showed that having had a vaginal delivery was a risk factor for both posterior and anterior prolapse. But the women with posterior prolapse were significantly more likely to report a loss of gas from the rectum, having to push on the vagina to complete a bowel movement, having a sensation of bulge, and having asked a physician for help because of their symptoms.
"Not surprisingly, prolapse was associated with vaginal delivery, but when we compare anterior versus posterior prolapse, there were no differences in terms of obstetric risk factors, at least that we could perceive in this study," Dr. Wilbur commented. "But the symptomatology was different between those two groups," although the reasons for this difference were not readily apparent.
The investigators analyzed data collected at enrollment, 5-10 years after a first delivery, from women in the Mothers’ Outcomes After Delivery cohort. Most had had their delivery at Greater Baltimore Medical Center, a large community hospital.
The women’s obstetric history was reviewed, they underwent examination including the pelvic organ prolapse quantification (POP-Q) system assessment, and they completed validated measures of symptoms, including the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) and the Colorectal-Anal Impact Questionnaire (CRAIQ).
The investigators categorized the women as having posterior prolapse (with a point A posterior value on the POP-Q greater than or equal to –1) with or without anterior prolapse, isolated anterior prolapse (with a point A anterior value greater than or equal to –1), or no prolapse.
It was not possible to study isolated posterior prolapse because only 20 women had posterior prolapse without concomitant anterior prolapse, Dr. Wilbur explained at the meeting, which was jointly sponsored by the American College of Surgeons.
Compared with the no-prolapse group, both the posterior and anterior prolapse groups were more likely to have completed the first stage of labor (85% and 76% vs. 53%) and to have had a vaginal delivery (79% and 70% vs. 40%), she reported.
The two prolapse groups were similar with respect to these and a variety of other obstetric factors, such as having a prolonged second stage of labor, having an infant weighing at least 4,000 g, having an operative delivery, having an episiotomy, and experiencing perineal tears.
But relative to their counterparts with anterior prolapse, women with posterior prolapse were more likely to report a loss of gas from the rectum (odds ratio, 1.79), having to push on the vagina to complete a bowel movement (1.72), having a sensation of bulge (2.58), and having asked a physician for help because of prolapse symptoms (3.24).
Women with anterior prolapse were similar to women with no prolapse on most of these measures. The exception was that women without prolapse were, not surprisingly, less likely to have asked a physician for help (odds ratio, 0.27).
"We are following these women over time. So those 1,497 women came in for the first visit, but as of today we have 3,840 person-visits, and in the final manuscript, we did do generalized estimating equations where we followed those trends over time," Dr. Wilbur commented. "They are actually very similar to the enrollment data."
The study’s main shortcoming is its potential lack of generalizability, she said. "Greater Baltimore Medical Center does deliver women who are mostly white and relatively affluent in comparison to the general American population."
Dr. Wilbur disclosed no relevant conflicts of interest
SCOTTSDALE, ARIZ. – Obstetric risk factors for stage II anterior and posterior pelvic organ prolapse are essentially the same, but symptoms differ, according to a cohort study reported at the annual meeting of the Society of Gynecologic Surgeons.
Investigators led by Dr. MaryAnn Wilbur of the department of obstetrics and gynecology at Johns Hopkins University, Baltimore, analyzed data from women who were 5-10 years out from a first delivery, comparing 85 women with posterior prolapse (with or without concomitant anterior prolapse), 334 women with isolated anterior prolapse, and 1,078 women with no prolapse.
The results showed that having had a vaginal delivery was a risk factor for both posterior and anterior prolapse. But the women with posterior prolapse were significantly more likely to report a loss of gas from the rectum, having to push on the vagina to complete a bowel movement, having a sensation of bulge, and having asked a physician for help because of their symptoms.
"Not surprisingly, prolapse was associated with vaginal delivery, but when we compare anterior versus posterior prolapse, there were no differences in terms of obstetric risk factors, at least that we could perceive in this study," Dr. Wilbur commented. "But the symptomatology was different between those two groups," although the reasons for this difference were not readily apparent.
The investigators analyzed data collected at enrollment, 5-10 years after a first delivery, from women in the Mothers’ Outcomes After Delivery cohort. Most had had their delivery at Greater Baltimore Medical Center, a large community hospital.
The women’s obstetric history was reviewed, they underwent examination including the pelvic organ prolapse quantification (POP-Q) system assessment, and they completed validated measures of symptoms, including the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) and the Colorectal-Anal Impact Questionnaire (CRAIQ).
The investigators categorized the women as having posterior prolapse (with a point A posterior value on the POP-Q greater than or equal to –1) with or without anterior prolapse, isolated anterior prolapse (with a point A anterior value greater than or equal to –1), or no prolapse.
It was not possible to study isolated posterior prolapse because only 20 women had posterior prolapse without concomitant anterior prolapse, Dr. Wilbur explained at the meeting, which was jointly sponsored by the American College of Surgeons.
Compared with the no-prolapse group, both the posterior and anterior prolapse groups were more likely to have completed the first stage of labor (85% and 76% vs. 53%) and to have had a vaginal delivery (79% and 70% vs. 40%), she reported.
The two prolapse groups were similar with respect to these and a variety of other obstetric factors, such as having a prolonged second stage of labor, having an infant weighing at least 4,000 g, having an operative delivery, having an episiotomy, and experiencing perineal tears.
But relative to their counterparts with anterior prolapse, women with posterior prolapse were more likely to report a loss of gas from the rectum (odds ratio, 1.79), having to push on the vagina to complete a bowel movement (1.72), having a sensation of bulge (2.58), and having asked a physician for help because of prolapse symptoms (3.24).
Women with anterior prolapse were similar to women with no prolapse on most of these measures. The exception was that women without prolapse were, not surprisingly, less likely to have asked a physician for help (odds ratio, 0.27).
"We are following these women over time. So those 1,497 women came in for the first visit, but as of today we have 3,840 person-visits, and in the final manuscript, we did do generalized estimating equations where we followed those trends over time," Dr. Wilbur commented. "They are actually very similar to the enrollment data."
The study’s main shortcoming is its potential lack of generalizability, she said. "Greater Baltimore Medical Center does deliver women who are mostly white and relatively affluent in comparison to the general American population."
Dr. Wilbur disclosed no relevant conflicts of interest
AT SGS 2014
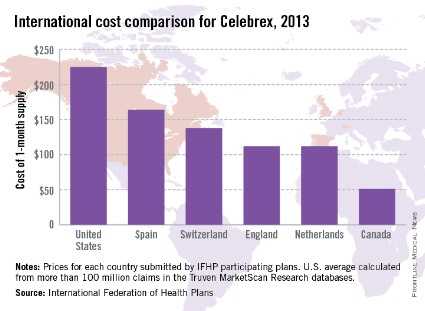
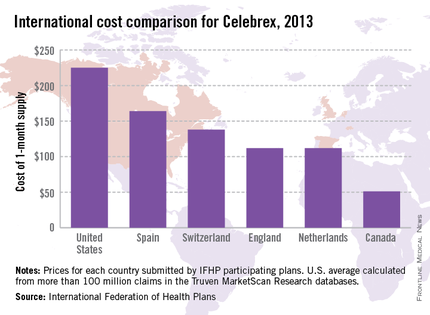
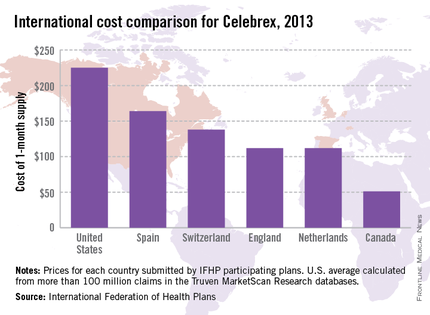
Celebrex cost high in United States, low in Canada
North America is home to the most expensive and least expensive Celebrex, according to the International Federation of Health Plans’ 2013 Comparative Price Report.
The average price for a 1-month supply of Celebrex (celecoxib) was $225 in the United States last year, compared with $51 in Canada, the IFHP reported. The other countries in the survey were the Netherlands ($112), England ($112), Switzerland ($138), and Spain ($164).
Celebrex is approved in the United States for the treatment of osteoarthritis, rheumatoid arthritis, juvenile rheumatoid arthritis in patients 2 years and older, ankylosing spondylitis, acute pain, and primary dysmenorrhea.
The IFHP comprises more than 100 member companies in 25 countries. For the survey, the price for each country was submitted by participating member plans. Some prices are drawn from the public sector, some from the private, and some from both. U.S. averages were calculated from more than 100 million claims in the Truven MarketScan Research databases.
North America is home to the most expensive and least expensive Celebrex, according to the International Federation of Health Plans’ 2013 Comparative Price Report.
The average price for a 1-month supply of Celebrex (celecoxib) was $225 in the United States last year, compared with $51 in Canada, the IFHP reported. The other countries in the survey were the Netherlands ($112), England ($112), Switzerland ($138), and Spain ($164).
Celebrex is approved in the United States for the treatment of osteoarthritis, rheumatoid arthritis, juvenile rheumatoid arthritis in patients 2 years and older, ankylosing spondylitis, acute pain, and primary dysmenorrhea.
The IFHP comprises more than 100 member companies in 25 countries. For the survey, the price for each country was submitted by participating member plans. Some prices are drawn from the public sector, some from the private, and some from both. U.S. averages were calculated from more than 100 million claims in the Truven MarketScan Research databases.
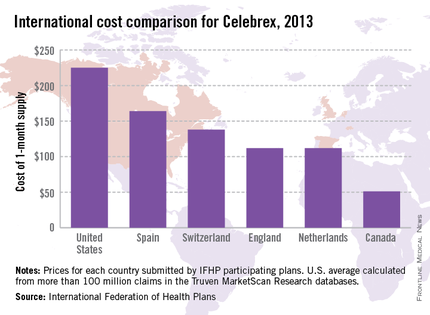
North America is home to the most expensive and least expensive Celebrex, according to the International Federation of Health Plans’ 2013 Comparative Price Report.
The average price for a 1-month supply of Celebrex (celecoxib) was $225 in the United States last year, compared with $51 in Canada, the IFHP reported. The other countries in the survey were the Netherlands ($112), England ($112), Switzerland ($138), and Spain ($164).
Celebrex is approved in the United States for the treatment of osteoarthritis, rheumatoid arthritis, juvenile rheumatoid arthritis in patients 2 years and older, ankylosing spondylitis, acute pain, and primary dysmenorrhea.
The IFHP comprises more than 100 member companies in 25 countries. For the survey, the price for each country was submitted by participating member plans. Some prices are drawn from the public sector, some from the private, and some from both. U.S. averages were calculated from more than 100 million claims in the Truven MarketScan Research databases.
Women’s Health Initiative study netted $37 billion in savings
The massive Women’s Health Initiative estrogen plus progestin clinical trial netted more than $37 billion in savings in the 10 years after it was published, largely by curtailing postmenopausal women’s use of combined hormone therapy, which in turn prevented 126,000 cases of breast cancer and 76,000 cardiovascular events, according to a report published online May 5 in Annals of Internal Medicine.
"The net health yield for women in the United States was approximately 145,000 more quality-of-life-years than would have occurred in the absence of the trial," said Joshua A. Roth, Ph.D., of the public health sciences division, Fred Hutchinson Cancer Research Center and Group Health Research Institute, Seattle, and his associates.
So even though the 2002 trial was one of the most expensive publicly funded studies ever – costing the National Institutes of Health an estimated $260 million in 2012 U.S. dollars – it yielded clinical and economic returns of approximately $140 for every dollar invested in it, they noted.
"Our findings suggest that large public research investments can yield considerable clinical and economic value when targeted to address research questions with great clinical relevance and public health effect," the investigators wrote.
One of the primary debates regarding public funding of research concerns its overall "returns" to society. To estimate the returns of the WHI-EP trial, Dr. Roth and his colleagues developed several mathematical models so they could simulate the 10-year health outcomes of American women aged 50-79 years if the study had never taken place – that is, if it had never been reported that combined hormone therapy (HT) raised the risks of cardiovascular disease, venous thromboembolism, and breast cancer (albeit reducing the risks of fracture and colon cancer).
Publication of those results led to an immediate 50% decrease in the use of combined HT and a continuing decline of 5%-10% per year thereafter, the researchers said.
They compared disease incidence, survival rates, and direct medical expenditures between a "WHI scenario" and a "no WHI scenario" to calculate the net economic and clinical returns of the trial through the year 2012.
Approximately 39.1 million women were eligible for combined HT during the study period. An estimated 5.2 million used combined HT in the WHI scenario, but 9.5 million would have used it if there had never been a WHI, given the usage trends during the years preceding the trial.
Relative to the no-WHI scenario, there were 126,000 fewer cases of breast cancer, 76,000 fewer cases of cardiovascular disease (CVD), and 80,000 fewer cases of venous thromboembolism in the WHI scenario. On the other side of the scale, there also were 263,000 more osteoporotic fractures and 15,000 more cases of colorectal cancer.
"Compared with the no-WHI scenario, the WHI scenario resulted in $35.2 billion in direct medical expenditure savings. Most of the savings came from fewer combined HT users and associated office visits ($26.2 billion), decreased breast cancer incidence ($4.5 billion), and decreased CVD incidence ($2.2 billion), offsetting increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion)," Dr. Roth and his associates said (Ann. Intern. Med. 2014;160:594-602).
The WHI scenario, compared with the no-WHI scenario, yielded 145,000 QALYs (quality-adjusted life-years), mainly because of the improved quality of life of women who avoided breast cancer and CVD. This greatly offset the reductions in QALYs that would have been due to increased fractures in the no-WHI scenario.
The net economic return of the WHI was calculated to be $37.1 billion. Savings from reduced use of combined HT drove the early economic value of the trial, and later value was driven by a combination of combined HT expenditure savings and QALY gains.
"This level of value was robust across plausible uncertainty ranges, and remained greater than $20 billion in all simulations that we evaluated," they wrote.
"Our analysis of the economic return from the WHI-EP trial suggests that, in certain circumstances, public investments in large prospective trials with high clinical and public health relevance could provide a similarly large positive rate of return in the long term," the investigators added.
The massive Women’s Health Initiative estrogen plus progestin clinical trial netted more than $37 billion in savings in the 10 years after it was published, largely by curtailing postmenopausal women’s use of combined hormone therapy, which in turn prevented 126,000 cases of breast cancer and 76,000 cardiovascular events, according to a report published online May 5 in Annals of Internal Medicine.
"The net health yield for women in the United States was approximately 145,000 more quality-of-life-years than would have occurred in the absence of the trial," said Joshua A. Roth, Ph.D., of the public health sciences division, Fred Hutchinson Cancer Research Center and Group Health Research Institute, Seattle, and his associates.
So even though the 2002 trial was one of the most expensive publicly funded studies ever – costing the National Institutes of Health an estimated $260 million in 2012 U.S. dollars – it yielded clinical and economic returns of approximately $140 for every dollar invested in it, they noted.
"Our findings suggest that large public research investments can yield considerable clinical and economic value when targeted to address research questions with great clinical relevance and public health effect," the investigators wrote.
One of the primary debates regarding public funding of research concerns its overall "returns" to society. To estimate the returns of the WHI-EP trial, Dr. Roth and his colleagues developed several mathematical models so they could simulate the 10-year health outcomes of American women aged 50-79 years if the study had never taken place – that is, if it had never been reported that combined hormone therapy (HT) raised the risks of cardiovascular disease, venous thromboembolism, and breast cancer (albeit reducing the risks of fracture and colon cancer).
Publication of those results led to an immediate 50% decrease in the use of combined HT and a continuing decline of 5%-10% per year thereafter, the researchers said.
They compared disease incidence, survival rates, and direct medical expenditures between a "WHI scenario" and a "no WHI scenario" to calculate the net economic and clinical returns of the trial through the year 2012.
Approximately 39.1 million women were eligible for combined HT during the study period. An estimated 5.2 million used combined HT in the WHI scenario, but 9.5 million would have used it if there had never been a WHI, given the usage trends during the years preceding the trial.
Relative to the no-WHI scenario, there were 126,000 fewer cases of breast cancer, 76,000 fewer cases of cardiovascular disease (CVD), and 80,000 fewer cases of venous thromboembolism in the WHI scenario. On the other side of the scale, there also were 263,000 more osteoporotic fractures and 15,000 more cases of colorectal cancer.
"Compared with the no-WHI scenario, the WHI scenario resulted in $35.2 billion in direct medical expenditure savings. Most of the savings came from fewer combined HT users and associated office visits ($26.2 billion), decreased breast cancer incidence ($4.5 billion), and decreased CVD incidence ($2.2 billion), offsetting increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion)," Dr. Roth and his associates said (Ann. Intern. Med. 2014;160:594-602).
The WHI scenario, compared with the no-WHI scenario, yielded 145,000 QALYs (quality-adjusted life-years), mainly because of the improved quality of life of women who avoided breast cancer and CVD. This greatly offset the reductions in QALYs that would have been due to increased fractures in the no-WHI scenario.
The net economic return of the WHI was calculated to be $37.1 billion. Savings from reduced use of combined HT drove the early economic value of the trial, and later value was driven by a combination of combined HT expenditure savings and QALY gains.
"This level of value was robust across plausible uncertainty ranges, and remained greater than $20 billion in all simulations that we evaluated," they wrote.
"Our analysis of the economic return from the WHI-EP trial suggests that, in certain circumstances, public investments in large prospective trials with high clinical and public health relevance could provide a similarly large positive rate of return in the long term," the investigators added.
The massive Women’s Health Initiative estrogen plus progestin clinical trial netted more than $37 billion in savings in the 10 years after it was published, largely by curtailing postmenopausal women’s use of combined hormone therapy, which in turn prevented 126,000 cases of breast cancer and 76,000 cardiovascular events, according to a report published online May 5 in Annals of Internal Medicine.
"The net health yield for women in the United States was approximately 145,000 more quality-of-life-years than would have occurred in the absence of the trial," said Joshua A. Roth, Ph.D., of the public health sciences division, Fred Hutchinson Cancer Research Center and Group Health Research Institute, Seattle, and his associates.
So even though the 2002 trial was one of the most expensive publicly funded studies ever – costing the National Institutes of Health an estimated $260 million in 2012 U.S. dollars – it yielded clinical and economic returns of approximately $140 for every dollar invested in it, they noted.
"Our findings suggest that large public research investments can yield considerable clinical and economic value when targeted to address research questions with great clinical relevance and public health effect," the investigators wrote.
One of the primary debates regarding public funding of research concerns its overall "returns" to society. To estimate the returns of the WHI-EP trial, Dr. Roth and his colleagues developed several mathematical models so they could simulate the 10-year health outcomes of American women aged 50-79 years if the study had never taken place – that is, if it had never been reported that combined hormone therapy (HT) raised the risks of cardiovascular disease, venous thromboembolism, and breast cancer (albeit reducing the risks of fracture and colon cancer).
Publication of those results led to an immediate 50% decrease in the use of combined HT and a continuing decline of 5%-10% per year thereafter, the researchers said.
They compared disease incidence, survival rates, and direct medical expenditures between a "WHI scenario" and a "no WHI scenario" to calculate the net economic and clinical returns of the trial through the year 2012.
Approximately 39.1 million women were eligible for combined HT during the study period. An estimated 5.2 million used combined HT in the WHI scenario, but 9.5 million would have used it if there had never been a WHI, given the usage trends during the years preceding the trial.
Relative to the no-WHI scenario, there were 126,000 fewer cases of breast cancer, 76,000 fewer cases of cardiovascular disease (CVD), and 80,000 fewer cases of venous thromboembolism in the WHI scenario. On the other side of the scale, there also were 263,000 more osteoporotic fractures and 15,000 more cases of colorectal cancer.
"Compared with the no-WHI scenario, the WHI scenario resulted in $35.2 billion in direct medical expenditure savings. Most of the savings came from fewer combined HT users and associated office visits ($26.2 billion), decreased breast cancer incidence ($4.5 billion), and decreased CVD incidence ($2.2 billion), offsetting increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion)," Dr. Roth and his associates said (Ann. Intern. Med. 2014;160:594-602).
The WHI scenario, compared with the no-WHI scenario, yielded 145,000 QALYs (quality-adjusted life-years), mainly because of the improved quality of life of women who avoided breast cancer and CVD. This greatly offset the reductions in QALYs that would have been due to increased fractures in the no-WHI scenario.
The net economic return of the WHI was calculated to be $37.1 billion. Savings from reduced use of combined HT drove the early economic value of the trial, and later value was driven by a combination of combined HT expenditure savings and QALY gains.
"This level of value was robust across plausible uncertainty ranges, and remained greater than $20 billion in all simulations that we evaluated," they wrote.
"Our analysis of the economic return from the WHI-EP trial suggests that, in certain circumstances, public investments in large prospective trials with high clinical and public health relevance could provide a similarly large positive rate of return in the long term," the investigators added.
FROM ANNALS OF INTERNAL MEDICINE
Major Finding: The WHI resulted in $35.2 billion in direct medical expenditure savings, most of which came from fewer combined HT users and associated office visits ($26.2 billion), decreased breast cancer incidence ($4.5 billion), and decreased CVD incidence ($2.2 billion); this offset increases in expenditures for greater fracture incidence ($4.8 billion) and colorectal cancer ($1.0 billion).
Data Source: An analysis of mathematical models that estimated clinical and economic outcomes if the WHI-EP had not been performed in 2002, the risk/benefit profile of combined HT had not been reported, and women had continued to use combined HT through 2012.
Disclosures: This study was supported in part by the National Institute on Aging; the WHI was funded by the National Heart, Lung, and Blood Institute. Dr. Roth and her associates reported no financial conflicts of interest.