User login
Combo could treat AML, other cancers

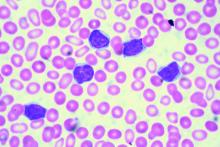
A novel combination has shown promise for treating acute myeloid leukemia (AML) and other cancers, according to preclinical research published in Cancer Cell.
Researchers found that combining a DNMT inhibitor and a PARP inhibitor greatly increases the drugs’ anti-tumor activity, and the combination could be effective in malignancies that are not responsive to PARP inhibitors or DNMT inhibitors alone.
Experiments showed that, when combined, the 2 types of inhibitors cause interactions that significantly disrupt cancer cells’ ability to survive DNA damage.
“Our preclinical data suggest that combining low doses of these inhibitors will enhance the clinical effects of both drugs as a potential treatment for patients with AML,” said study author Feyruz V. Rassool, PhD, of the University of Maryland School of Medicine in Baltimore.
“Moreover, our initial data suggest that subtypes of AML with a poor prognosis are likely to be sensitive to this new therapeutic approach.”
Dr Rassool and her colleagues assessed the activity of a DNMT inhibitor—decitabine or 5-azacytidine—in combination with a PARP inhibitor—veliparib or talazoparib—against AML and breast cancer.
In both AML and breast cancer cells, combination treatment increased cytotoxicity and decreased clonogenicity, compared to treatment with either type of inhibitor alone.
The combination of 5-azacytidine and talazoparib produced “very robust responses” in 2 mouse models of AML (MV411 and MOLM14), according to the researchers.
“[It was] somewhat of a surprise that leukemia cells were this sensitive to the combination treatment,” said study author Stephen B. Baylin, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medical Institutions in Baltimore.
“And if further research confirms our findings, it looks like it also could be useful for breast cancer and ovarian cancers for which PARP inhibitors have not been useful as yet.”
How the inhibitors work together
Dr Baylin noted that PARP helps repair naturally occurring breaks in strands of DNA, and some cancers rely more frequently on PARP than others.
“[PARP inhibitors] work according to how intensely and durably the PARP enzyme is trapped at certain DNA damage sites,” he explained. “If you can ramp up the duration and intensity of this trapping, you could potentially increase the efficacy of the drug[s].”
“We figured that if we pair 5-azacytidine and a PARP inhibitor like talazoparib, we may be able to increase PARP trapping at DNA damage sites.”
That’s because 5-azacytidine blocks proteins that attach gene-regulating methyl groups to DNA and traps those proteins on DNA. The proteins blocked by 5-azacytidine also interact with PARP enzymes at DNA damage sites.
In fact, the researchers did find that combining 5-azacytidine and talazoparib increased the time that PARP was trapped at sites of DNA damage in cancer cells. The time was extended from 30 minutes to 3-6 hours after treatment.
Next steps
Based on the results of this research, a clinical trial is planned to test whether low doses of decitabine and talazoparib can be safely combined and whether this therapy will be effective in AML patients.
The researchers are especially interested in testing the combination in patients who cannot receive intensive chemotherapy, whose leukemia is resistant to treatment, or who have relapsed after treatment.
“This is really a new paradigm mechanism that is being translated into a clinical trial,” Dr Rassool said. “It’s not just putting 2 drugs together.”
“We have shown in the laboratory that the proteins that these inhibitors target actually interact, so the effects of these inhibitors are enhanced through this interaction. Therein lies the novelty of this new approach.” ![]()

A novel combination has shown promise for treating acute myeloid leukemia (AML) and other cancers, according to preclinical research published in Cancer Cell.
Researchers found that combining a DNMT inhibitor and a PARP inhibitor greatly increases the drugs’ anti-tumor activity, and the combination could be effective in malignancies that are not responsive to PARP inhibitors or DNMT inhibitors alone.
Experiments showed that, when combined, the 2 types of inhibitors cause interactions that significantly disrupt cancer cells’ ability to survive DNA damage.
“Our preclinical data suggest that combining low doses of these inhibitors will enhance the clinical effects of both drugs as a potential treatment for patients with AML,” said study author Feyruz V. Rassool, PhD, of the University of Maryland School of Medicine in Baltimore.
“Moreover, our initial data suggest that subtypes of AML with a poor prognosis are likely to be sensitive to this new therapeutic approach.”
Dr Rassool and her colleagues assessed the activity of a DNMT inhibitor—decitabine or 5-azacytidine—in combination with a PARP inhibitor—veliparib or talazoparib—against AML and breast cancer.
In both AML and breast cancer cells, combination treatment increased cytotoxicity and decreased clonogenicity, compared to treatment with either type of inhibitor alone.
The combination of 5-azacytidine and talazoparib produced “very robust responses” in 2 mouse models of AML (MV411 and MOLM14), according to the researchers.
“[It was] somewhat of a surprise that leukemia cells were this sensitive to the combination treatment,” said study author Stephen B. Baylin, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medical Institutions in Baltimore.
“And if further research confirms our findings, it looks like it also could be useful for breast cancer and ovarian cancers for which PARP inhibitors have not been useful as yet.”
How the inhibitors work together
Dr Baylin noted that PARP helps repair naturally occurring breaks in strands of DNA, and some cancers rely more frequently on PARP than others.
“[PARP inhibitors] work according to how intensely and durably the PARP enzyme is trapped at certain DNA damage sites,” he explained. “If you can ramp up the duration and intensity of this trapping, you could potentially increase the efficacy of the drug[s].”
“We figured that if we pair 5-azacytidine and a PARP inhibitor like talazoparib, we may be able to increase PARP trapping at DNA damage sites.”
That’s because 5-azacytidine blocks proteins that attach gene-regulating methyl groups to DNA and traps those proteins on DNA. The proteins blocked by 5-azacytidine also interact with PARP enzymes at DNA damage sites.
In fact, the researchers did find that combining 5-azacytidine and talazoparib increased the time that PARP was trapped at sites of DNA damage in cancer cells. The time was extended from 30 minutes to 3-6 hours after treatment.
Next steps
Based on the results of this research, a clinical trial is planned to test whether low doses of decitabine and talazoparib can be safely combined and whether this therapy will be effective in AML patients.
The researchers are especially interested in testing the combination in patients who cannot receive intensive chemotherapy, whose leukemia is resistant to treatment, or who have relapsed after treatment.
“This is really a new paradigm mechanism that is being translated into a clinical trial,” Dr Rassool said. “It’s not just putting 2 drugs together.”
“We have shown in the laboratory that the proteins that these inhibitors target actually interact, so the effects of these inhibitors are enhanced through this interaction. Therein lies the novelty of this new approach.” ![]()

A novel combination has shown promise for treating acute myeloid leukemia (AML) and other cancers, according to preclinical research published in Cancer Cell.
Researchers found that combining a DNMT inhibitor and a PARP inhibitor greatly increases the drugs’ anti-tumor activity, and the combination could be effective in malignancies that are not responsive to PARP inhibitors or DNMT inhibitors alone.
Experiments showed that, when combined, the 2 types of inhibitors cause interactions that significantly disrupt cancer cells’ ability to survive DNA damage.
“Our preclinical data suggest that combining low doses of these inhibitors will enhance the clinical effects of both drugs as a potential treatment for patients with AML,” said study author Feyruz V. Rassool, PhD, of the University of Maryland School of Medicine in Baltimore.
“Moreover, our initial data suggest that subtypes of AML with a poor prognosis are likely to be sensitive to this new therapeutic approach.”
Dr Rassool and her colleagues assessed the activity of a DNMT inhibitor—decitabine or 5-azacytidine—in combination with a PARP inhibitor—veliparib or talazoparib—against AML and breast cancer.
In both AML and breast cancer cells, combination treatment increased cytotoxicity and decreased clonogenicity, compared to treatment with either type of inhibitor alone.
The combination of 5-azacytidine and talazoparib produced “very robust responses” in 2 mouse models of AML (MV411 and MOLM14), according to the researchers.
“[It was] somewhat of a surprise that leukemia cells were this sensitive to the combination treatment,” said study author Stephen B. Baylin, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medical Institutions in Baltimore.
“And if further research confirms our findings, it looks like it also could be useful for breast cancer and ovarian cancers for which PARP inhibitors have not been useful as yet.”
How the inhibitors work together
Dr Baylin noted that PARP helps repair naturally occurring breaks in strands of DNA, and some cancers rely more frequently on PARP than others.
“[PARP inhibitors] work according to how intensely and durably the PARP enzyme is trapped at certain DNA damage sites,” he explained. “If you can ramp up the duration and intensity of this trapping, you could potentially increase the efficacy of the drug[s].”
“We figured that if we pair 5-azacytidine and a PARP inhibitor like talazoparib, we may be able to increase PARP trapping at DNA damage sites.”
That’s because 5-azacytidine blocks proteins that attach gene-regulating methyl groups to DNA and traps those proteins on DNA. The proteins blocked by 5-azacytidine also interact with PARP enzymes at DNA damage sites.
In fact, the researchers did find that combining 5-azacytidine and talazoparib increased the time that PARP was trapped at sites of DNA damage in cancer cells. The time was extended from 30 minutes to 3-6 hours after treatment.
Next steps
Based on the results of this research, a clinical trial is planned to test whether low doses of decitabine and talazoparib can be safely combined and whether this therapy will be effective in AML patients.
The researchers are especially interested in testing the combination in patients who cannot receive intensive chemotherapy, whose leukemia is resistant to treatment, or who have relapsed after treatment.
“This is really a new paradigm mechanism that is being translated into a clinical trial,” Dr Rassool said. “It’s not just putting 2 drugs together.”
“We have shown in the laboratory that the proteins that these inhibitors target actually interact, so the effects of these inhibitors are enhanced through this interaction. Therein lies the novelty of this new approach.” ![]()
STIM1 long-term follow-up confirms imatinib discontinuation safety
Imatinib discontinuation is safe in patients with chronic myeloid leukemia (CML) who have sustained deep molecular response with no late molecular recurrence, according to long-term follow-up of the French Stop Imatinib Study (STIM1).
Over a median follow-up of 77 months after treatment discontinuation in 100 patients with CML who had undetectable minimal residual disease (UMRD) for at least 2 years, 61 lost UMRD after a median of 2.5 months, and 1 died with UMRD at 10 months, Gabriel Etienne, MD, of Institut Bergonie, Bordeaux, France, and colleagues reported online in the Journal of Clinical Oncology.
Of the 61 patients who lost UMRD, 57 restarted treatment and 55 achieved a second UMRD at a median of 4.3 months. The median time to second UMRD in patients with molecular recurrence with or without loss of major molecular response at the time of relapse was 4.2 months and 5 months, respectively. At a median of 73 months, none of the patients with molecular recurrence experienced CML progression. The rate of molecular recurrence-free survival overall was 43% at 6 months, 40% at 18 months, and 38% at 60 months, the investigators reported (2016 Oct. 3. doi: 10.1200/JCO.2016.68.2914).
These final long-term results of the STIM1 trial confirm the safety of imatinib discontinuation in CML patients with deep molecular response, and “make treatment-free remission legitimate as a criterion of treatment evaluation in the future,” the investigators concluded, noting that the possibility of improved results in patients treated with second-generation tyrosine kinase inhibitors as first- or second-line therapy is currently being evaluated in ongoing discontinuation trials.
Imatinib discontinuation is safe in patients with chronic myeloid leukemia (CML) who have sustained deep molecular response with no late molecular recurrence, according to long-term follow-up of the French Stop Imatinib Study (STIM1).
Over a median follow-up of 77 months after treatment discontinuation in 100 patients with CML who had undetectable minimal residual disease (UMRD) for at least 2 years, 61 lost UMRD after a median of 2.5 months, and 1 died with UMRD at 10 months, Gabriel Etienne, MD, of Institut Bergonie, Bordeaux, France, and colleagues reported online in the Journal of Clinical Oncology.
Of the 61 patients who lost UMRD, 57 restarted treatment and 55 achieved a second UMRD at a median of 4.3 months. The median time to second UMRD in patients with molecular recurrence with or without loss of major molecular response at the time of relapse was 4.2 months and 5 months, respectively. At a median of 73 months, none of the patients with molecular recurrence experienced CML progression. The rate of molecular recurrence-free survival overall was 43% at 6 months, 40% at 18 months, and 38% at 60 months, the investigators reported (2016 Oct. 3. doi: 10.1200/JCO.2016.68.2914).
These final long-term results of the STIM1 trial confirm the safety of imatinib discontinuation in CML patients with deep molecular response, and “make treatment-free remission legitimate as a criterion of treatment evaluation in the future,” the investigators concluded, noting that the possibility of improved results in patients treated with second-generation tyrosine kinase inhibitors as first- or second-line therapy is currently being evaluated in ongoing discontinuation trials.
Imatinib discontinuation is safe in patients with chronic myeloid leukemia (CML) who have sustained deep molecular response with no late molecular recurrence, according to long-term follow-up of the French Stop Imatinib Study (STIM1).
Over a median follow-up of 77 months after treatment discontinuation in 100 patients with CML who had undetectable minimal residual disease (UMRD) for at least 2 years, 61 lost UMRD after a median of 2.5 months, and 1 died with UMRD at 10 months, Gabriel Etienne, MD, of Institut Bergonie, Bordeaux, France, and colleagues reported online in the Journal of Clinical Oncology.
Of the 61 patients who lost UMRD, 57 restarted treatment and 55 achieved a second UMRD at a median of 4.3 months. The median time to second UMRD in patients with molecular recurrence with or without loss of major molecular response at the time of relapse was 4.2 months and 5 months, respectively. At a median of 73 months, none of the patients with molecular recurrence experienced CML progression. The rate of molecular recurrence-free survival overall was 43% at 6 months, 40% at 18 months, and 38% at 60 months, the investigators reported (2016 Oct. 3. doi: 10.1200/JCO.2016.68.2914).
These final long-term results of the STIM1 trial confirm the safety of imatinib discontinuation in CML patients with deep molecular response, and “make treatment-free remission legitimate as a criterion of treatment evaluation in the future,” the investigators concluded, noting that the possibility of improved results in patients treated with second-generation tyrosine kinase inhibitors as first- or second-line therapy is currently being evaluated in ongoing discontinuation trials.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: The rate of molecular recurrence-free survival overall was 43% at 24 months, 40% at 18 months, and 38% at 60 months.
Data source: Long-term follow-up of 100 patients from the STIM1 trial.
Disclosures: STIM1 was supported by grants from the French Ministry of Health Programme Hospitalier de Recherche and by the Institut National du Cancer. Dr. Etienne reported financial relationships with Novartis, Bristol-Myers Squibb, and ARIAD Pharmaceuticals. Coauthors reported relationships with several pharmaceutical companies.
Minimal residual disease status predicts 10-year survival in CLL
Patients who have chronic lymphocytic leukemia and achieve minimal residual disease negativity have a high probability of long-term progression-free and overall survival, irrespective of the type of therapy they receive, reported Marwan Kwok, MD, of Queen Elizabeth Hospital Birmingham (England) and colleagues.
Minimal residual disease (MRD) negativity, defined as less than 1 chronic lymphocytic leukemic (CLL) cell detectable per 10,000 leukocytes, has been shown to independently predict clinical outcome in the front line setting, but the long-term prognostic value of MRD status in other therapeutic settings remains unclear. “Our results demonstrate the long-term benefit of achieving MRD negativity regardless of the therapeutic setting and treatment modality, and support its use as a prognostic marker for long-term PFS (progression-free survival) and as a potential therapeutic goal in CLL,” the authors wrote (Blood. 2016 Oct 3. doi: 10.1182/blood-2016-05-714162).
The researchers retrospectively analyzed, with up to 18 years of follow-up, all 133 CLL patients at St. James’s University Hospital in Leeds, England, who achieved at least a partial response with various therapies between 1996 and 2007 and who received a bone marrow MRD assessment at the end of treatment, according to the international harmonized approach.
MRD negativity correlated with progression-free and overall survival, and the association was independent of the type and line of treatment, as well as adverse cytogenetic findings, the investigators said.
For those who achieved MRD negativity in front-line treatment, the 10-year progression-free survival was 65%; survival in patients who did not achieve MRD negativity was 10%. Overall survival at 10 years was 70% for those who achieved MRD negativity and 30% for MRD-positive patients.
The authors had no relevant financial disclosures.
Patients who have chronic lymphocytic leukemia and achieve minimal residual disease negativity have a high probability of long-term progression-free and overall survival, irrespective of the type of therapy they receive, reported Marwan Kwok, MD, of Queen Elizabeth Hospital Birmingham (England) and colleagues.
Minimal residual disease (MRD) negativity, defined as less than 1 chronic lymphocytic leukemic (CLL) cell detectable per 10,000 leukocytes, has been shown to independently predict clinical outcome in the front line setting, but the long-term prognostic value of MRD status in other therapeutic settings remains unclear. “Our results demonstrate the long-term benefit of achieving MRD negativity regardless of the therapeutic setting and treatment modality, and support its use as a prognostic marker for long-term PFS (progression-free survival) and as a potential therapeutic goal in CLL,” the authors wrote (Blood. 2016 Oct 3. doi: 10.1182/blood-2016-05-714162).
The researchers retrospectively analyzed, with up to 18 years of follow-up, all 133 CLL patients at St. James’s University Hospital in Leeds, England, who achieved at least a partial response with various therapies between 1996 and 2007 and who received a bone marrow MRD assessment at the end of treatment, according to the international harmonized approach.
MRD negativity correlated with progression-free and overall survival, and the association was independent of the type and line of treatment, as well as adverse cytogenetic findings, the investigators said.
For those who achieved MRD negativity in front-line treatment, the 10-year progression-free survival was 65%; survival in patients who did not achieve MRD negativity was 10%. Overall survival at 10 years was 70% for those who achieved MRD negativity and 30% for MRD-positive patients.
The authors had no relevant financial disclosures.
Patients who have chronic lymphocytic leukemia and achieve minimal residual disease negativity have a high probability of long-term progression-free and overall survival, irrespective of the type of therapy they receive, reported Marwan Kwok, MD, of Queen Elizabeth Hospital Birmingham (England) and colleagues.
Minimal residual disease (MRD) negativity, defined as less than 1 chronic lymphocytic leukemic (CLL) cell detectable per 10,000 leukocytes, has been shown to independently predict clinical outcome in the front line setting, but the long-term prognostic value of MRD status in other therapeutic settings remains unclear. “Our results demonstrate the long-term benefit of achieving MRD negativity regardless of the therapeutic setting and treatment modality, and support its use as a prognostic marker for long-term PFS (progression-free survival) and as a potential therapeutic goal in CLL,” the authors wrote (Blood. 2016 Oct 3. doi: 10.1182/blood-2016-05-714162).
The researchers retrospectively analyzed, with up to 18 years of follow-up, all 133 CLL patients at St. James’s University Hospital in Leeds, England, who achieved at least a partial response with various therapies between 1996 and 2007 and who received a bone marrow MRD assessment at the end of treatment, according to the international harmonized approach.
MRD negativity correlated with progression-free and overall survival, and the association was independent of the type and line of treatment, as well as adverse cytogenetic findings, the investigators said.
For those who achieved MRD negativity in front-line treatment, the 10-year progression-free survival was 65%; survival in patients who did not achieve MRD negativity was 10%. Overall survival at 10 years was 70% for those who achieved MRD negativity and 30% for MRD-positive patients.
The authors had no relevant financial disclosures.
FROM BLOOD
Key clinical point:
Major finding: Overall survival at 10 years was 70% for those who achieved MRD negativity and 30% for those who did not.
Data source: Retrospective, single-center study of 133 patients with chronic lymphocytic leukemia.
Disclosures: The authors had no relevant financial disclosures.
CD49d trumps novel recurrent mutations for predicting overall survival in CLL
CD49d was a strong predictor of overall survival in a cohort of 778 unselected patients with chronic lymphocytic leukemia, reported Michele Dal Bo, MD, of Centro di Riferimento Oncologico, in Aviano, Italy, and colleagues.
High CD49d expression was an independent predictor of poor overall survival in a multivariate Cox analysis (hazard ratio = 1.88, P less than .0001) and in each category of a risk stratification model. Among other biological prognosticators, CD49d was among the top predictors of overall survival (variable importance = 0.0410) along with immunoglobulin heavy chain variable (IGHV) gene mutational status and TP53 abnormalities. “In this context, TP53 disruption and NOTCH1 mutations retained prognostic relevance, in keeping with their roles in CLL cell immuno-chemoresistance,” the authors wrote.
CD49d was a strong predictor of overall survival in a cohort of 778 unselected patients with chronic lymphocytic leukemia, reported Michele Dal Bo, MD, of Centro di Riferimento Oncologico, in Aviano, Italy, and colleagues.
High CD49d expression was an independent predictor of poor overall survival in a multivariate Cox analysis (hazard ratio = 1.88, P less than .0001) and in each category of a risk stratification model. Among other biological prognosticators, CD49d was among the top predictors of overall survival (variable importance = 0.0410) along with immunoglobulin heavy chain variable (IGHV) gene mutational status and TP53 abnormalities. “In this context, TP53 disruption and NOTCH1 mutations retained prognostic relevance, in keeping with their roles in CLL cell immuno-chemoresistance,” the authors wrote.
CD49d was a strong predictor of overall survival in a cohort of 778 unselected patients with chronic lymphocytic leukemia, reported Michele Dal Bo, MD, of Centro di Riferimento Oncologico, in Aviano, Italy, and colleagues.
High CD49d expression was an independent predictor of poor overall survival in a multivariate Cox analysis (hazard ratio = 1.88, P less than .0001) and in each category of a risk stratification model. Among other biological prognosticators, CD49d was among the top predictors of overall survival (variable importance = 0.0410) along with immunoglobulin heavy chain variable (IGHV) gene mutational status and TP53 abnormalities. “In this context, TP53 disruption and NOTCH1 mutations retained prognostic relevance, in keeping with their roles in CLL cell immuno-chemoresistance,” the authors wrote.
Device could aid treatment decisions in ALL, other cancers

A new device might help physicians choose the optimal treatment for cancer patients, according to research published in Nature Biotechnology.
The device was designed to predict responses to treatment by measuring individual cell growth after drug exposure.
Researchers found they could predict whether a particular drug would kill leukemia or glioblastoma cells, based on how the drug affected the cells’ mass.
“We’ve developed a functional assay that can measure drug response of individual cells while maintaining viability for downstream analysis such as sequencing,” said study author Scott Manalis, PhD, of the Massachusetts Institute of Technology in Cambridge.
He and his colleagues were inspired to develop their assay, in part, by a test that has been used for decades to choose antibiotics to treat bacterial infections. The antibiotic susceptibility test involves simply taking bacteria from a patient, exposing them to a range of antibiotics, and observing whether the bacteria grow or die.
To translate that approach to cancer, the researchers needed a way to rapidly measure cell responses to drugs, and to do it with a limited number of cells.
For the past several years, Dr Manalis’s lab has been developing a device known as a suspended microchannel resonator (SMR).
According to the researchers, the SMR can measure cell masses 10 to 100 times more accurately than any other technique. This allows for the precise calculation of growth rates of single cells over short periods of time.
For this study, Dr Manalis and his colleagues used the SMR to determine whether drug susceptibility could be predicted by measuring cancer cell growth rates following drug exposure.
The team analyzed cells from patients with different subtypes of glioblastoma and B-cell acute lymphocytic leukemia (ALL) that have previously been shown to be either sensitive or resistant to specific therapies—MDM2 inhibitors for glioblastoma and BCR-ABL inhibitors for ALL.
After exposing the cancer cells to the drugs, the researchers waited about 15 hours, then measured the cell’s growth rates. Each cell was measured several times over a period of 15 to 20 minutes, providing enough data for the team to calculate the mass accumulation rate.
They found that cells known to be susceptible to a given therapy changed the way they accumulate mass, whereas resistant cells continued to grow as if unaffected.
“We’re able to show that cells we know are sensitive to therapy respond by dramatically reducing their growth rate relative to cells that are resistant,” said study author Mark Stevens, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And because the cells are still alive, we have the opportunity to study the same cells following our measurement.”
The researchers said a major advantage of this technique is that it can be done with very small numbers of cells. In the experiments with ALL cells, the team showed they could get accurate results with a droplet of blood containing about 1000 ALL cells.
Another advantage is the speed at which small changes in cell mass can be measured, said Anthony Letai, MD, PhD, of the Dana-Farber Cancer Institute.
“This system is well suited to making rapid measurements,” said Dr Letai, who was not involved in this study. “I look forward to seeing them apply this to many more cancers and many more drugs.”
The researchers are now using their technique to test cells’ susceptibility to drugs, then isolate the cells and sequence the RNA found in them, revealing which genes are turned on.
“Now that we have a way to identify cells that are not responding to a given therapy, we are excited about isolating these cells and analyzing them to understand mechanisms of resistance,” Dr Manalis said.
In another recent paper published in Nature Biotechnology, the researchers described a higher throughput version of the SMR device that can do in 1 day the same number of measurements that took several months with the device used in this study.
This is an important step toward making the approach suitable for clinical samples, Dr Manalis said. ![]()

A new device might help physicians choose the optimal treatment for cancer patients, according to research published in Nature Biotechnology.
The device was designed to predict responses to treatment by measuring individual cell growth after drug exposure.
Researchers found they could predict whether a particular drug would kill leukemia or glioblastoma cells, based on how the drug affected the cells’ mass.
“We’ve developed a functional assay that can measure drug response of individual cells while maintaining viability for downstream analysis such as sequencing,” said study author Scott Manalis, PhD, of the Massachusetts Institute of Technology in Cambridge.
He and his colleagues were inspired to develop their assay, in part, by a test that has been used for decades to choose antibiotics to treat bacterial infections. The antibiotic susceptibility test involves simply taking bacteria from a patient, exposing them to a range of antibiotics, and observing whether the bacteria grow or die.
To translate that approach to cancer, the researchers needed a way to rapidly measure cell responses to drugs, and to do it with a limited number of cells.
For the past several years, Dr Manalis’s lab has been developing a device known as a suspended microchannel resonator (SMR).
According to the researchers, the SMR can measure cell masses 10 to 100 times more accurately than any other technique. This allows for the precise calculation of growth rates of single cells over short periods of time.
For this study, Dr Manalis and his colleagues used the SMR to determine whether drug susceptibility could be predicted by measuring cancer cell growth rates following drug exposure.
The team analyzed cells from patients with different subtypes of glioblastoma and B-cell acute lymphocytic leukemia (ALL) that have previously been shown to be either sensitive or resistant to specific therapies—MDM2 inhibitors for glioblastoma and BCR-ABL inhibitors for ALL.
After exposing the cancer cells to the drugs, the researchers waited about 15 hours, then measured the cell’s growth rates. Each cell was measured several times over a period of 15 to 20 minutes, providing enough data for the team to calculate the mass accumulation rate.
They found that cells known to be susceptible to a given therapy changed the way they accumulate mass, whereas resistant cells continued to grow as if unaffected.
“We’re able to show that cells we know are sensitive to therapy respond by dramatically reducing their growth rate relative to cells that are resistant,” said study author Mark Stevens, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And because the cells are still alive, we have the opportunity to study the same cells following our measurement.”
The researchers said a major advantage of this technique is that it can be done with very small numbers of cells. In the experiments with ALL cells, the team showed they could get accurate results with a droplet of blood containing about 1000 ALL cells.
Another advantage is the speed at which small changes in cell mass can be measured, said Anthony Letai, MD, PhD, of the Dana-Farber Cancer Institute.
“This system is well suited to making rapid measurements,” said Dr Letai, who was not involved in this study. “I look forward to seeing them apply this to many more cancers and many more drugs.”
The researchers are now using their technique to test cells’ susceptibility to drugs, then isolate the cells and sequence the RNA found in them, revealing which genes are turned on.
“Now that we have a way to identify cells that are not responding to a given therapy, we are excited about isolating these cells and analyzing them to understand mechanisms of resistance,” Dr Manalis said.
In another recent paper published in Nature Biotechnology, the researchers described a higher throughput version of the SMR device that can do in 1 day the same number of measurements that took several months with the device used in this study.
This is an important step toward making the approach suitable for clinical samples, Dr Manalis said. ![]()

A new device might help physicians choose the optimal treatment for cancer patients, according to research published in Nature Biotechnology.
The device was designed to predict responses to treatment by measuring individual cell growth after drug exposure.
Researchers found they could predict whether a particular drug would kill leukemia or glioblastoma cells, based on how the drug affected the cells’ mass.
“We’ve developed a functional assay that can measure drug response of individual cells while maintaining viability for downstream analysis such as sequencing,” said study author Scott Manalis, PhD, of the Massachusetts Institute of Technology in Cambridge.
He and his colleagues were inspired to develop their assay, in part, by a test that has been used for decades to choose antibiotics to treat bacterial infections. The antibiotic susceptibility test involves simply taking bacteria from a patient, exposing them to a range of antibiotics, and observing whether the bacteria grow or die.
To translate that approach to cancer, the researchers needed a way to rapidly measure cell responses to drugs, and to do it with a limited number of cells.
For the past several years, Dr Manalis’s lab has been developing a device known as a suspended microchannel resonator (SMR).
According to the researchers, the SMR can measure cell masses 10 to 100 times more accurately than any other technique. This allows for the precise calculation of growth rates of single cells over short periods of time.
For this study, Dr Manalis and his colleagues used the SMR to determine whether drug susceptibility could be predicted by measuring cancer cell growth rates following drug exposure.
The team analyzed cells from patients with different subtypes of glioblastoma and B-cell acute lymphocytic leukemia (ALL) that have previously been shown to be either sensitive or resistant to specific therapies—MDM2 inhibitors for glioblastoma and BCR-ABL inhibitors for ALL.
After exposing the cancer cells to the drugs, the researchers waited about 15 hours, then measured the cell’s growth rates. Each cell was measured several times over a period of 15 to 20 minutes, providing enough data for the team to calculate the mass accumulation rate.
They found that cells known to be susceptible to a given therapy changed the way they accumulate mass, whereas resistant cells continued to grow as if unaffected.
“We’re able to show that cells we know are sensitive to therapy respond by dramatically reducing their growth rate relative to cells that are resistant,” said study author Mark Stevens, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And because the cells are still alive, we have the opportunity to study the same cells following our measurement.”
The researchers said a major advantage of this technique is that it can be done with very small numbers of cells. In the experiments with ALL cells, the team showed they could get accurate results with a droplet of blood containing about 1000 ALL cells.
Another advantage is the speed at which small changes in cell mass can be measured, said Anthony Letai, MD, PhD, of the Dana-Farber Cancer Institute.
“This system is well suited to making rapid measurements,” said Dr Letai, who was not involved in this study. “I look forward to seeing them apply this to many more cancers and many more drugs.”
The researchers are now using their technique to test cells’ susceptibility to drugs, then isolate the cells and sequence the RNA found in them, revealing which genes are turned on.
“Now that we have a way to identify cells that are not responding to a given therapy, we are excited about isolating these cells and analyzing them to understand mechanisms of resistance,” Dr Manalis said.
In another recent paper published in Nature Biotechnology, the researchers described a higher throughput version of the SMR device that can do in 1 day the same number of measurements that took several months with the device used in this study.
This is an important step toward making the approach suitable for clinical samples, Dr Manalis said. ![]()
Cost may hinder timely TKI initiation for CML
Nearly a third of Medicare beneficiaries with chronic myeloid leukemia (CML) did not initiate tyrosine kinase inhibitor therapy within 6 months of diagnosis, according to a review of SEER-Medicare data.
The findings suggest that out-of-pocket costs might be a barrier to timely initiation of tyrosine kinase inhibitor (TKI) therapy in CML patients, Aaron N. Winn of the University of North Carolina at Chapel Hill and his colleagues reported online ahead of print in the Journal of Clinical Oncology.
Of 393 individuals diagnosed with CML between 2007 and 2011, only 68% initiated TKI therapy within 180 days (median, 75 days), and 61% of those patients were adherent. Earlier treatment initiation was associated with receipt of cost-sharing subsidies (hazard ratio, 1.35), more-recent diagnosis (HR, 1.14), and living in a big metropolitan area (HR, 1.80) or metropolitan area vs. an urban area (HR, 1.84), while later treatment initiation was associated with higher levels of comorbidity (HR, 0.81) and age older than 80 years vs. age younger than 70 years (HR, 0.53)
Multivariate analysis showed that therapy initiation within 180 days was significantly more likely among those with more-recent diagnosis (relative risk, 1.06) and those living in a large metropolitan area vs. an urban area (RR, 1.57), and was significantly less likely among those older than age 80 years vs. those younger than age 70 years (RR, 0.71). Adherence within 180 days of therapy initiation was higher for those diagnosed in more-recent years (RR, 1.07) and lower for patients aged 80 years or older vs. 66-69 years (RR, 0.74), the investigators found (J Clin Oncol. 2016 Oct 3. doi: 10/1200/JCO.2016.67.4184).
“Our findings highlight important gaps in TKI use among Medicare beneficiaries with CML and suggest that high cost sharing may result in delays in initiation of these life-saving medications,” they concluded.
This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
Nearly a third of Medicare beneficiaries with chronic myeloid leukemia (CML) did not initiate tyrosine kinase inhibitor therapy within 6 months of diagnosis, according to a review of SEER-Medicare data.
The findings suggest that out-of-pocket costs might be a barrier to timely initiation of tyrosine kinase inhibitor (TKI) therapy in CML patients, Aaron N. Winn of the University of North Carolina at Chapel Hill and his colleagues reported online ahead of print in the Journal of Clinical Oncology.
Of 393 individuals diagnosed with CML between 2007 and 2011, only 68% initiated TKI therapy within 180 days (median, 75 days), and 61% of those patients were adherent. Earlier treatment initiation was associated with receipt of cost-sharing subsidies (hazard ratio, 1.35), more-recent diagnosis (HR, 1.14), and living in a big metropolitan area (HR, 1.80) or metropolitan area vs. an urban area (HR, 1.84), while later treatment initiation was associated with higher levels of comorbidity (HR, 0.81) and age older than 80 years vs. age younger than 70 years (HR, 0.53)
Multivariate analysis showed that therapy initiation within 180 days was significantly more likely among those with more-recent diagnosis (relative risk, 1.06) and those living in a large metropolitan area vs. an urban area (RR, 1.57), and was significantly less likely among those older than age 80 years vs. those younger than age 70 years (RR, 0.71). Adherence within 180 days of therapy initiation was higher for those diagnosed in more-recent years (RR, 1.07) and lower for patients aged 80 years or older vs. 66-69 years (RR, 0.74), the investigators found (J Clin Oncol. 2016 Oct 3. doi: 10/1200/JCO.2016.67.4184).
“Our findings highlight important gaps in TKI use among Medicare beneficiaries with CML and suggest that high cost sharing may result in delays in initiation of these life-saving medications,” they concluded.
This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
Nearly a third of Medicare beneficiaries with chronic myeloid leukemia (CML) did not initiate tyrosine kinase inhibitor therapy within 6 months of diagnosis, according to a review of SEER-Medicare data.
The findings suggest that out-of-pocket costs might be a barrier to timely initiation of tyrosine kinase inhibitor (TKI) therapy in CML patients, Aaron N. Winn of the University of North Carolina at Chapel Hill and his colleagues reported online ahead of print in the Journal of Clinical Oncology.
Of 393 individuals diagnosed with CML between 2007 and 2011, only 68% initiated TKI therapy within 180 days (median, 75 days), and 61% of those patients were adherent. Earlier treatment initiation was associated with receipt of cost-sharing subsidies (hazard ratio, 1.35), more-recent diagnosis (HR, 1.14), and living in a big metropolitan area (HR, 1.80) or metropolitan area vs. an urban area (HR, 1.84), while later treatment initiation was associated with higher levels of comorbidity (HR, 0.81) and age older than 80 years vs. age younger than 70 years (HR, 0.53)
Multivariate analysis showed that therapy initiation within 180 days was significantly more likely among those with more-recent diagnosis (relative risk, 1.06) and those living in a large metropolitan area vs. an urban area (RR, 1.57), and was significantly less likely among those older than age 80 years vs. those younger than age 70 years (RR, 0.71). Adherence within 180 days of therapy initiation was higher for those diagnosed in more-recent years (RR, 1.07) and lower for patients aged 80 years or older vs. 66-69 years (RR, 0.74), the investigators found (J Clin Oncol. 2016 Oct 3. doi: 10/1200/JCO.2016.67.4184).
“Our findings highlight important gaps in TKI use among Medicare beneficiaries with CML and suggest that high cost sharing may result in delays in initiation of these life-saving medications,” they concluded.
This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: TKI initiation within 180 days was significantly less likely among those older than age 80 years vs. those under age 70 years (relative risk, 0.71).
Data source: A review of SEER-Medicare data for 393 patients.
Disclosures: This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
Immunotherapy produces CRs in kids with rel/ref ALL
The bispecific T-cell engager (BiTE®) antibody blinatumomab can produce complete responses (CRs) in pediatric patients with relapsed/refractory B-cell precursor acute lymphoblastic leukemia (ALL), according to a phase 1/2 study published in the Journal of Clinical Oncology.
Of the patients who received the recommended dosage of blinatumomab, 39% achieved a CR within the first 2 treatment cycles.
And 52% of these patients achieved a complete minimal residual disease (MRD) response.
“This study showed that [blinatumomab] can induce deep molecular remissions in children with highly refractory, multiply relapsed ALL,” said study author Lia Gore, MD, of University of Colorado Anschutz Medical Campus in Aurora, Colorado.
However, most of these remissions did not last. Although a few of the complete responders were still alive and in CR at the study’s 2-year follow-up, more than half had relapsed, and two-thirds had died.
This trial, known as Study ‘205, was supported by Amgen.
Study ‘205 included 93 pediatric patients with relapsed or refractory B-cell precursor ALL. Patients received blinatumomab as a continuous intravenous infusion—49 patients in the phase 1 portion of the trial and 44 in phase 2. The patients were followed for 2 years.
Toxicities and recommended dose
There were 4 dose-limiting toxicities during the phase 1 portion of the trial, and 2 of these events were fatal. One patient treated at 15 μg/m2/day developed grade 4 cytokine release syndrome (CRS), which was deemed related to grade 4 gastrointestinal hemorrhage.
Two patients treated at 30 μg/m2/day had grade 4 CRS. One case was attributed to grade 5 cardiac failure, and the other was treated successfully with tocilizumab.
One patient treated at 15 μg/m2/day had grade 5 respiratory failure with cardiac arrest after hypotonia and muscle weakness after 7 days of infusion with blinatumomab. This patient experienced febrile neutropenia and pneumonia shortly before the start of the infusion.
Based on these toxicities, the maximum-tolerated dose of blinatumomab was 15 μg/m2/day, but a step-wise dosage was recommended to reduce the risk of CRS.
So the recommended dose was 5 μg/m2/day on days 1-7 and 15 μg/m2/day on days 8-28 for cycle 1, and 15 μg/m2/day on days 1-28 for subsequent cycles.
Dose adjustment was possible in case of adverse events. Patients who responded to blinatumomab but later relapsed had the option to be retreated with blinatumomab.
Treatment at recommended dose
Seventy patients received at least 1 infusion of blinatumomab at the recommended dose. The median number of treatment cycles was 1 (range, 1 to 5).
The patients’ median age was 8 years (range, 7 months to 17 years). Forty patients (57%) had undergone allogeneic transplant prior to receiving blinatumomab, and 39 (56%) had refractory disease. Four patients had less than the 25% bone marrow blasts required for protocol entry but had more than 5% blasts.
Adverse events
The most common adverse events among the patients who received the recommended dose of blinatumomab were pyrexia (80%), anemia (41%), nausea (33%), and headache (30%).
The most frequent grade 3 or higher events were anemia (36%), thrombocytopenia (21%), febrile neutropenia (17%), hypokalemia (17%), and neutropenia (17%).
Eight patients developed CRS. Three had grade 3 and 1 had grade 4 CRS. Two of these patients had treatment interruptions, and 2 discontinued treatment permanently. All 4 patients achieved a CR.
Ten patients (14%) had treatment interruptions due to adverse events, and 4 (6%) discontinued treatment permanently because of adverse events.
Six patients had fatal adverse events. Three died after they went on to allogeneic transplant—1 of multiorgan failure, 1 of sepsis, and 1 of respiratory failure. The 3 other deaths were due to fungal infection, multiorgan failure, and thrombocytopenia.
Response and follow-up
Among the 70 patients who received the recommended dose of blinatumomab, 27 (39%) achieved a CR within the first 2 cycles. Fourteen of these patients (52%) achieved complete MRD response.
CRs were achieved across subgroups, and complete MRD response rates were similar across subgroups.
Thirteen of the 27 patients (48%) who achieved a CR went on to receive an allogeneic transplant.
At the end of the 2-year follow-up, 4 of the 27 complete responders were still in remission.
Two of the patients had relapsed but were still alive, 3 had withdrawn consent (1 in CR and 2 after relapse), 3 had died in CR after transplant, and 15 had relapsed and died.
Of the 43 patients who did not achieve a CR within the first 2 treatment cycles, 8 were still alive at the end of the 2-year follow-up. ![]()
The bispecific T-cell engager (BiTE®) antibody blinatumomab can produce complete responses (CRs) in pediatric patients with relapsed/refractory B-cell precursor acute lymphoblastic leukemia (ALL), according to a phase 1/2 study published in the Journal of Clinical Oncology.
Of the patients who received the recommended dosage of blinatumomab, 39% achieved a CR within the first 2 treatment cycles.
And 52% of these patients achieved a complete minimal residual disease (MRD) response.
“This study showed that [blinatumomab] can induce deep molecular remissions in children with highly refractory, multiply relapsed ALL,” said study author Lia Gore, MD, of University of Colorado Anschutz Medical Campus in Aurora, Colorado.
However, most of these remissions did not last. Although a few of the complete responders were still alive and in CR at the study’s 2-year follow-up, more than half had relapsed, and two-thirds had died.
This trial, known as Study ‘205, was supported by Amgen.
Study ‘205 included 93 pediatric patients with relapsed or refractory B-cell precursor ALL. Patients received blinatumomab as a continuous intravenous infusion—49 patients in the phase 1 portion of the trial and 44 in phase 2. The patients were followed for 2 years.
Toxicities and recommended dose
There were 4 dose-limiting toxicities during the phase 1 portion of the trial, and 2 of these events were fatal. One patient treated at 15 μg/m2/day developed grade 4 cytokine release syndrome (CRS), which was deemed related to grade 4 gastrointestinal hemorrhage.
Two patients treated at 30 μg/m2/day had grade 4 CRS. One case was attributed to grade 5 cardiac failure, and the other was treated successfully with tocilizumab.
One patient treated at 15 μg/m2/day had grade 5 respiratory failure with cardiac arrest after hypotonia and muscle weakness after 7 days of infusion with blinatumomab. This patient experienced febrile neutropenia and pneumonia shortly before the start of the infusion.
Based on these toxicities, the maximum-tolerated dose of blinatumomab was 15 μg/m2/day, but a step-wise dosage was recommended to reduce the risk of CRS.
So the recommended dose was 5 μg/m2/day on days 1-7 and 15 μg/m2/day on days 8-28 for cycle 1, and 15 μg/m2/day on days 1-28 for subsequent cycles.
Dose adjustment was possible in case of adverse events. Patients who responded to blinatumomab but later relapsed had the option to be retreated with blinatumomab.
Treatment at recommended dose
Seventy patients received at least 1 infusion of blinatumomab at the recommended dose. The median number of treatment cycles was 1 (range, 1 to 5).
The patients’ median age was 8 years (range, 7 months to 17 years). Forty patients (57%) had undergone allogeneic transplant prior to receiving blinatumomab, and 39 (56%) had refractory disease. Four patients had less than the 25% bone marrow blasts required for protocol entry but had more than 5% blasts.
Adverse events
The most common adverse events among the patients who received the recommended dose of blinatumomab were pyrexia (80%), anemia (41%), nausea (33%), and headache (30%).
The most frequent grade 3 or higher events were anemia (36%), thrombocytopenia (21%), febrile neutropenia (17%), hypokalemia (17%), and neutropenia (17%).
Eight patients developed CRS. Three had grade 3 and 1 had grade 4 CRS. Two of these patients had treatment interruptions, and 2 discontinued treatment permanently. All 4 patients achieved a CR.
Ten patients (14%) had treatment interruptions due to adverse events, and 4 (6%) discontinued treatment permanently because of adverse events.
Six patients had fatal adverse events. Three died after they went on to allogeneic transplant—1 of multiorgan failure, 1 of sepsis, and 1 of respiratory failure. The 3 other deaths were due to fungal infection, multiorgan failure, and thrombocytopenia.
Response and follow-up
Among the 70 patients who received the recommended dose of blinatumomab, 27 (39%) achieved a CR within the first 2 cycles. Fourteen of these patients (52%) achieved complete MRD response.
CRs were achieved across subgroups, and complete MRD response rates were similar across subgroups.
Thirteen of the 27 patients (48%) who achieved a CR went on to receive an allogeneic transplant.
At the end of the 2-year follow-up, 4 of the 27 complete responders were still in remission.
Two of the patients had relapsed but were still alive, 3 had withdrawn consent (1 in CR and 2 after relapse), 3 had died in CR after transplant, and 15 had relapsed and died.
Of the 43 patients who did not achieve a CR within the first 2 treatment cycles, 8 were still alive at the end of the 2-year follow-up. ![]()
The bispecific T-cell engager (BiTE®) antibody blinatumomab can produce complete responses (CRs) in pediatric patients with relapsed/refractory B-cell precursor acute lymphoblastic leukemia (ALL), according to a phase 1/2 study published in the Journal of Clinical Oncology.
Of the patients who received the recommended dosage of blinatumomab, 39% achieved a CR within the first 2 treatment cycles.
And 52% of these patients achieved a complete minimal residual disease (MRD) response.
“This study showed that [blinatumomab] can induce deep molecular remissions in children with highly refractory, multiply relapsed ALL,” said study author Lia Gore, MD, of University of Colorado Anschutz Medical Campus in Aurora, Colorado.
However, most of these remissions did not last. Although a few of the complete responders were still alive and in CR at the study’s 2-year follow-up, more than half had relapsed, and two-thirds had died.
This trial, known as Study ‘205, was supported by Amgen.
Study ‘205 included 93 pediatric patients with relapsed or refractory B-cell precursor ALL. Patients received blinatumomab as a continuous intravenous infusion—49 patients in the phase 1 portion of the trial and 44 in phase 2. The patients were followed for 2 years.
Toxicities and recommended dose
There were 4 dose-limiting toxicities during the phase 1 portion of the trial, and 2 of these events were fatal. One patient treated at 15 μg/m2/day developed grade 4 cytokine release syndrome (CRS), which was deemed related to grade 4 gastrointestinal hemorrhage.
Two patients treated at 30 μg/m2/day had grade 4 CRS. One case was attributed to grade 5 cardiac failure, and the other was treated successfully with tocilizumab.
One patient treated at 15 μg/m2/day had grade 5 respiratory failure with cardiac arrest after hypotonia and muscle weakness after 7 days of infusion with blinatumomab. This patient experienced febrile neutropenia and pneumonia shortly before the start of the infusion.
Based on these toxicities, the maximum-tolerated dose of blinatumomab was 15 μg/m2/day, but a step-wise dosage was recommended to reduce the risk of CRS.
So the recommended dose was 5 μg/m2/day on days 1-7 and 15 μg/m2/day on days 8-28 for cycle 1, and 15 μg/m2/day on days 1-28 for subsequent cycles.
Dose adjustment was possible in case of adverse events. Patients who responded to blinatumomab but later relapsed had the option to be retreated with blinatumomab.
Treatment at recommended dose
Seventy patients received at least 1 infusion of blinatumomab at the recommended dose. The median number of treatment cycles was 1 (range, 1 to 5).
The patients’ median age was 8 years (range, 7 months to 17 years). Forty patients (57%) had undergone allogeneic transplant prior to receiving blinatumomab, and 39 (56%) had refractory disease. Four patients had less than the 25% bone marrow blasts required for protocol entry but had more than 5% blasts.
Adverse events
The most common adverse events among the patients who received the recommended dose of blinatumomab were pyrexia (80%), anemia (41%), nausea (33%), and headache (30%).
The most frequent grade 3 or higher events were anemia (36%), thrombocytopenia (21%), febrile neutropenia (17%), hypokalemia (17%), and neutropenia (17%).
Eight patients developed CRS. Three had grade 3 and 1 had grade 4 CRS. Two of these patients had treatment interruptions, and 2 discontinued treatment permanently. All 4 patients achieved a CR.
Ten patients (14%) had treatment interruptions due to adverse events, and 4 (6%) discontinued treatment permanently because of adverse events.
Six patients had fatal adverse events. Three died after they went on to allogeneic transplant—1 of multiorgan failure, 1 of sepsis, and 1 of respiratory failure. The 3 other deaths were due to fungal infection, multiorgan failure, and thrombocytopenia.
Response and follow-up
Among the 70 patients who received the recommended dose of blinatumomab, 27 (39%) achieved a CR within the first 2 cycles. Fourteen of these patients (52%) achieved complete MRD response.
CRs were achieved across subgroups, and complete MRD response rates were similar across subgroups.
Thirteen of the 27 patients (48%) who achieved a CR went on to receive an allogeneic transplant.
At the end of the 2-year follow-up, 4 of the 27 complete responders were still in remission.
Two of the patients had relapsed but were still alive, 3 had withdrawn consent (1 in CR and 2 after relapse), 3 had died in CR after transplant, and 15 had relapsed and died.
Of the 43 patients who did not achieve a CR within the first 2 treatment cycles, 8 were still alive at the end of the 2-year follow-up. ![]()
‘Practice-changing’ treatments emerging in AML

NEW YORK—We are “finally” making progress in the treatment of acute myeloid leukemia (AML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
Jessica K. Altman, MD, said a number of developments have resulted in improved AML treatment, including a better understanding of biology and prognostic assessment, continued advances in transplant, and updating standard treatments and incorporating novel agents in both relapsed/refractory and newly diagnosed patients.
“There are a couple of practice-changing treatments in acute myeloid leukemia, 2 of which happened over the last decade: daunorubicin intensification and the use of FLT3 inhibitors,” said Dr Altman, an associate professor at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Dr Altman went on to explain that novel therapies for AML can be divided into 2 basic categories. There are agents that don’t depend on mutation status (like daunorubicin) and those that are mutation-specific (like FLT3 inhibitors).
Therapies not dependent on mutational complexity
The therapies that are not dependent on mutational complexity include anti-CD33 antibodies, BCL‐2 inhibitors, a dose-intensified anthracycline regimen, and different formulations of 7+3, including CPX‐351.
Escalated daunorubicin
Randomized trials of escalated daunorubicin (90 vs 45 mg/m2) have demonstrated benefit in complete responses (CRs) and overall survival (OS) in intermediate-risk patients and patients with core-binding factor mutation. They have demonstrated benefit in OS in FLT3 ITD+ patients.
In patients up to 65 years of age, 60–90 mg/m2 of daunorubicin is now standard.
“It’s still not clear to me—and I don’t know if it ever will be—if 90 is equivalent to 60,” Dr Altman said.
CPX-351
CPX-351 is a liposomal formulation of cytarabine and daunorubicin. In a randomized, phase 3 study of older adults with secondary AML, the median OS was 9.56 months for patients treated with CPX-351 and 5.95 months for patients on the 7+3 regimen (P=0.005).
The median event-free survival was significantly better with CPX-351 (P=0.021), as was the rate of CR + CR with incomplete blood count recovery (CRi). The rate of CR + CRi was 47.7% with CPX-351 and 33.3% for 7+3 (P=0.016).
A similar number of patients went on to transplant in each arm. Grade 3-5 adverse events were similar in frequency and severity in both arms—92% with CPX-351 vs 91% with 7+3.
SGN-CD33A
CD33 is not a new target in myeloid leukemia, Dr Altman pointed out. Gemtuzumab ozogamicin has been studied, approved by the US Food and Drug Administration, and then withdrawn.
However, an increasing number of studies with gemtuzumab are underway, she said, and the agent may once again have a place in the AML armamentarium.
The newest CD33 construct is SGN-CD33A, a stable dipeptide linker that enables uniform drug loading of a pyrrolobenzodiazepine dimer that crosslinks DNA and leads to cell death.
“Single-agent data was quite promising,” Dr Altman noted, with a CR + CRi rate of 41% in previously treated patients and 58% in 12 treatment-naïve patients.
These results prompted a combination study of SGN-CD33A with hypomethylating agents.
“Results were higher than expected with a hypomethylating agent,” Dr Altman pointed out.
The CR + CRi + CR with incomplete platelet recovery was 58%. And the median relapse-free survival was 7.7 months.
A phase 3 randomized trial of SGN-CD33A is planned.
Venetoclax
BCL-2 inhibitors are the fourth type of agent not dependent on mutation complexity. Venetoclax (ABT‐199) is a small‐molecule BCL-2 inhibitor that leads to the initiation of apoptosis.
In a phase 1b trial of venetoclax in combination with a hypomethylating agent, the overall CR rate was 35%, and the CRi rate was 35%.
“Again, higher than what would be expected with a hypomethylating agent alone,” Dr Altman said.
In a phase 1b/2 trial of venetoclax in combination with low‐dose cytarabine, the CR + CRi rate was 54%. Patients responded even if they had prior exposure to hypomethylating agents.
Mutation-specific novel agents
The FLT3 inhibitor midostaurin and the IDH inhibitors AG-120 and AG-221 are among the most exciting mutation-specific agents and the ones most progressed, according to Dr Altman.
FLT3-ITD is mutated in about 30% of AML patients and carries an unfavorable prognosis, and the IDH mutation occurs in about 10% and confers a favorable prognosis.
Midostaurin
A phase 3, randomized, double-blind study of daunorubicin/cytarabine induction and high-dose cytarabine consolidation with midostaurin (PKC412) or placebo had a 59% CR rate by day 60 in the midostaurin arm, compared with 53% in the placebo arm.
“The CR rate was slightly higher in the midostaurin arm,” Dr Altman said, “but what’s the most remarkable about this study is the difference in overall survival.”
The median OS in the midostaurin arm was 74.7 months, compared with 25.6 months in the placebo arm (P=0.0074).
“The major take-home message from this clinical trial,” Dr Altman said, “is that midostaurin improved the overall survival when added to standard therapy and represents a new standard of care.”
AG-120 and AG-221
Two IDH inhibitors that have substantial data available are the IDH1 inhibitor AG-120 and the IDH2 inhibitor AG-221.
As of October 2015, 78 patients had been treated with AG-120 in a phase 1 trial, yielding an overall response rate of 35% and a CR rate of 15%.
As of September 2015, 209 patients had been treated with AG-221 in a phase 1/2 trial, and 66 are still on study. The overall response rate was 37% in 159 adults with relapsed/refractory AML, with a median duration of response of 6.9 months. The CR rate was 18%.
Investigators have initiated a phase 3 study of AG-221 compared to conventional care regimens. ![]()

NEW YORK—We are “finally” making progress in the treatment of acute myeloid leukemia (AML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
Jessica K. Altman, MD, said a number of developments have resulted in improved AML treatment, including a better understanding of biology and prognostic assessment, continued advances in transplant, and updating standard treatments and incorporating novel agents in both relapsed/refractory and newly diagnosed patients.
“There are a couple of practice-changing treatments in acute myeloid leukemia, 2 of which happened over the last decade: daunorubicin intensification and the use of FLT3 inhibitors,” said Dr Altman, an associate professor at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Dr Altman went on to explain that novel therapies for AML can be divided into 2 basic categories. There are agents that don’t depend on mutation status (like daunorubicin) and those that are mutation-specific (like FLT3 inhibitors).
Therapies not dependent on mutational complexity
The therapies that are not dependent on mutational complexity include anti-CD33 antibodies, BCL‐2 inhibitors, a dose-intensified anthracycline regimen, and different formulations of 7+3, including CPX‐351.
Escalated daunorubicin
Randomized trials of escalated daunorubicin (90 vs 45 mg/m2) have demonstrated benefit in complete responses (CRs) and overall survival (OS) in intermediate-risk patients and patients with core-binding factor mutation. They have demonstrated benefit in OS in FLT3 ITD+ patients.
In patients up to 65 years of age, 60–90 mg/m2 of daunorubicin is now standard.
“It’s still not clear to me—and I don’t know if it ever will be—if 90 is equivalent to 60,” Dr Altman said.
CPX-351
CPX-351 is a liposomal formulation of cytarabine and daunorubicin. In a randomized, phase 3 study of older adults with secondary AML, the median OS was 9.56 months for patients treated with CPX-351 and 5.95 months for patients on the 7+3 regimen (P=0.005).
The median event-free survival was significantly better with CPX-351 (P=0.021), as was the rate of CR + CR with incomplete blood count recovery (CRi). The rate of CR + CRi was 47.7% with CPX-351 and 33.3% for 7+3 (P=0.016).
A similar number of patients went on to transplant in each arm. Grade 3-5 adverse events were similar in frequency and severity in both arms—92% with CPX-351 vs 91% with 7+3.
SGN-CD33A
CD33 is not a new target in myeloid leukemia, Dr Altman pointed out. Gemtuzumab ozogamicin has been studied, approved by the US Food and Drug Administration, and then withdrawn.
However, an increasing number of studies with gemtuzumab are underway, she said, and the agent may once again have a place in the AML armamentarium.
The newest CD33 construct is SGN-CD33A, a stable dipeptide linker that enables uniform drug loading of a pyrrolobenzodiazepine dimer that crosslinks DNA and leads to cell death.
“Single-agent data was quite promising,” Dr Altman noted, with a CR + CRi rate of 41% in previously treated patients and 58% in 12 treatment-naïve patients.
These results prompted a combination study of SGN-CD33A with hypomethylating agents.
“Results were higher than expected with a hypomethylating agent,” Dr Altman pointed out.
The CR + CRi + CR with incomplete platelet recovery was 58%. And the median relapse-free survival was 7.7 months.
A phase 3 randomized trial of SGN-CD33A is planned.
Venetoclax
BCL-2 inhibitors are the fourth type of agent not dependent on mutation complexity. Venetoclax (ABT‐199) is a small‐molecule BCL-2 inhibitor that leads to the initiation of apoptosis.
In a phase 1b trial of venetoclax in combination with a hypomethylating agent, the overall CR rate was 35%, and the CRi rate was 35%.
“Again, higher than what would be expected with a hypomethylating agent alone,” Dr Altman said.
In a phase 1b/2 trial of venetoclax in combination with low‐dose cytarabine, the CR + CRi rate was 54%. Patients responded even if they had prior exposure to hypomethylating agents.
Mutation-specific novel agents
The FLT3 inhibitor midostaurin and the IDH inhibitors AG-120 and AG-221 are among the most exciting mutation-specific agents and the ones most progressed, according to Dr Altman.
FLT3-ITD is mutated in about 30% of AML patients and carries an unfavorable prognosis, and the IDH mutation occurs in about 10% and confers a favorable prognosis.
Midostaurin
A phase 3, randomized, double-blind study of daunorubicin/cytarabine induction and high-dose cytarabine consolidation with midostaurin (PKC412) or placebo had a 59% CR rate by day 60 in the midostaurin arm, compared with 53% in the placebo arm.
“The CR rate was slightly higher in the midostaurin arm,” Dr Altman said, “but what’s the most remarkable about this study is the difference in overall survival.”
The median OS in the midostaurin arm was 74.7 months, compared with 25.6 months in the placebo arm (P=0.0074).
“The major take-home message from this clinical trial,” Dr Altman said, “is that midostaurin improved the overall survival when added to standard therapy and represents a new standard of care.”
AG-120 and AG-221
Two IDH inhibitors that have substantial data available are the IDH1 inhibitor AG-120 and the IDH2 inhibitor AG-221.
As of October 2015, 78 patients had been treated with AG-120 in a phase 1 trial, yielding an overall response rate of 35% and a CR rate of 15%.
As of September 2015, 209 patients had been treated with AG-221 in a phase 1/2 trial, and 66 are still on study. The overall response rate was 37% in 159 adults with relapsed/refractory AML, with a median duration of response of 6.9 months. The CR rate was 18%.
Investigators have initiated a phase 3 study of AG-221 compared to conventional care regimens. ![]()

NEW YORK—We are “finally” making progress in the treatment of acute myeloid leukemia (AML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
Jessica K. Altman, MD, said a number of developments have resulted in improved AML treatment, including a better understanding of biology and prognostic assessment, continued advances in transplant, and updating standard treatments and incorporating novel agents in both relapsed/refractory and newly diagnosed patients.
“There are a couple of practice-changing treatments in acute myeloid leukemia, 2 of which happened over the last decade: daunorubicin intensification and the use of FLT3 inhibitors,” said Dr Altman, an associate professor at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Dr Altman went on to explain that novel therapies for AML can be divided into 2 basic categories. There are agents that don’t depend on mutation status (like daunorubicin) and those that are mutation-specific (like FLT3 inhibitors).
Therapies not dependent on mutational complexity
The therapies that are not dependent on mutational complexity include anti-CD33 antibodies, BCL‐2 inhibitors, a dose-intensified anthracycline regimen, and different formulations of 7+3, including CPX‐351.
Escalated daunorubicin
Randomized trials of escalated daunorubicin (90 vs 45 mg/m2) have demonstrated benefit in complete responses (CRs) and overall survival (OS) in intermediate-risk patients and patients with core-binding factor mutation. They have demonstrated benefit in OS in FLT3 ITD+ patients.
In patients up to 65 years of age, 60–90 mg/m2 of daunorubicin is now standard.
“It’s still not clear to me—and I don’t know if it ever will be—if 90 is equivalent to 60,” Dr Altman said.
CPX-351
CPX-351 is a liposomal formulation of cytarabine and daunorubicin. In a randomized, phase 3 study of older adults with secondary AML, the median OS was 9.56 months for patients treated with CPX-351 and 5.95 months for patients on the 7+3 regimen (P=0.005).
The median event-free survival was significantly better with CPX-351 (P=0.021), as was the rate of CR + CR with incomplete blood count recovery (CRi). The rate of CR + CRi was 47.7% with CPX-351 and 33.3% for 7+3 (P=0.016).
A similar number of patients went on to transplant in each arm. Grade 3-5 adverse events were similar in frequency and severity in both arms—92% with CPX-351 vs 91% with 7+3.
SGN-CD33A
CD33 is not a new target in myeloid leukemia, Dr Altman pointed out. Gemtuzumab ozogamicin has been studied, approved by the US Food and Drug Administration, and then withdrawn.
However, an increasing number of studies with gemtuzumab are underway, she said, and the agent may once again have a place in the AML armamentarium.
The newest CD33 construct is SGN-CD33A, a stable dipeptide linker that enables uniform drug loading of a pyrrolobenzodiazepine dimer that crosslinks DNA and leads to cell death.
“Single-agent data was quite promising,” Dr Altman noted, with a CR + CRi rate of 41% in previously treated patients and 58% in 12 treatment-naïve patients.
These results prompted a combination study of SGN-CD33A with hypomethylating agents.
“Results were higher than expected with a hypomethylating agent,” Dr Altman pointed out.
The CR + CRi + CR with incomplete platelet recovery was 58%. And the median relapse-free survival was 7.7 months.
A phase 3 randomized trial of SGN-CD33A is planned.
Venetoclax
BCL-2 inhibitors are the fourth type of agent not dependent on mutation complexity. Venetoclax (ABT‐199) is a small‐molecule BCL-2 inhibitor that leads to the initiation of apoptosis.
In a phase 1b trial of venetoclax in combination with a hypomethylating agent, the overall CR rate was 35%, and the CRi rate was 35%.
“Again, higher than what would be expected with a hypomethylating agent alone,” Dr Altman said.
In a phase 1b/2 trial of venetoclax in combination with low‐dose cytarabine, the CR + CRi rate was 54%. Patients responded even if they had prior exposure to hypomethylating agents.
Mutation-specific novel agents
The FLT3 inhibitor midostaurin and the IDH inhibitors AG-120 and AG-221 are among the most exciting mutation-specific agents and the ones most progressed, according to Dr Altman.
FLT3-ITD is mutated in about 30% of AML patients and carries an unfavorable prognosis, and the IDH mutation occurs in about 10% and confers a favorable prognosis.
Midostaurin
A phase 3, randomized, double-blind study of daunorubicin/cytarabine induction and high-dose cytarabine consolidation with midostaurin (PKC412) or placebo had a 59% CR rate by day 60 in the midostaurin arm, compared with 53% in the placebo arm.
“The CR rate was slightly higher in the midostaurin arm,” Dr Altman said, “but what’s the most remarkable about this study is the difference in overall survival.”
The median OS in the midostaurin arm was 74.7 months, compared with 25.6 months in the placebo arm (P=0.0074).
“The major take-home message from this clinical trial,” Dr Altman said, “is that midostaurin improved the overall survival when added to standard therapy and represents a new standard of care.”
AG-120 and AG-221
Two IDH inhibitors that have substantial data available are the IDH1 inhibitor AG-120 and the IDH2 inhibitor AG-221.
As of October 2015, 78 patients had been treated with AG-120 in a phase 1 trial, yielding an overall response rate of 35% and a CR rate of 15%.
As of September 2015, 209 patients had been treated with AG-221 in a phase 1/2 trial, and 66 are still on study. The overall response rate was 37% in 159 adults with relapsed/refractory AML, with a median duration of response of 6.9 months. The CR rate was 18%.
Investigators have initiated a phase 3 study of AG-221 compared to conventional care regimens. ![]()
Drug granted conditional approval to treat CLL in Canada

of venetoclax (Venclexta)
Photo courtesy of AbbVie
Health Canada has issued a Notice of Compliance with Conditions (NOC/c) for the BCL-2 inhibitor venetoclax (Venclexta™).
This means venetoclax is conditionally approved for use in patients with previously treated chronic lymphocytic leukemia (CLL) who have 17p deletion or no other available treatment options.
An NOC/c is authorization to market a drug with the condition that the sponsor perform additional studies to verify a clinical benefit.
The NOC/c policy is designed to provide access to:
- Drugs that can treat serious, life-threatening, or severely debilitating diseases
- Drugs that can treat conditions for which no drug is currently marketed in Canada
- Drugs that provide a significant increase in efficacy or significant decrease in risk when compared to existing drugs marketed in Canada.
Venetoclax (previously ABT‐199) is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Venetoclax is currently under evaluation in phase 3 trials for the treatment of relapsed, refractory, and previously untreated CLL.
Phase 2 trial
Results from a phase 2 trial of venetoclax in CLL (M13-982, NCT01889186) were published in The Lancet Oncology in June. The trial enrolled 107 patients with relapsed or refractory CLL and 17p deletion.
Patients received venetoclax at 400 mg once daily following a weekly ramp-up schedule for the first 5 weeks. The primary endpoint was overall response rate, as determined by an independent review committee.
At a median follow-up of 12.1 months, 85 patients had responded to treatment, for an overall response rate of 79%.
Eight patients (8%) achieved a complete response or complete response with incomplete count recovery, 3 (3%) had a near-partial response, and 74 (69%) had a partial response. Twenty-two patients (21%) did not respond.
At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival. The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse was 96%. The most frequent grade 3/4 adverse events were neutropenia (40%), infection (20%), anemia (18%), and thrombocytopenia (15%).
The incidence of serious adverse events was 55%. The most common of these events were pyrexia (7%), autoimmune hemolytic anemia (7%), pneumonia (6%), and febrile neutropenia (5%).
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients during the ramp-up period only. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the past, TLS has caused deaths in patients receiving venetoclax. In response, AbbVie stopped dose-escalation in patients receiving the drug and suspended enrollment in phase 1 trials.
However, researchers subsequently found that a modified dosing schedule, prophylaxis, and patient monitoring can reduce the risk of TLS. ![]()

of venetoclax (Venclexta)
Photo courtesy of AbbVie
Health Canada has issued a Notice of Compliance with Conditions (NOC/c) for the BCL-2 inhibitor venetoclax (Venclexta™).
This means venetoclax is conditionally approved for use in patients with previously treated chronic lymphocytic leukemia (CLL) who have 17p deletion or no other available treatment options.
An NOC/c is authorization to market a drug with the condition that the sponsor perform additional studies to verify a clinical benefit.
The NOC/c policy is designed to provide access to:
- Drugs that can treat serious, life-threatening, or severely debilitating diseases
- Drugs that can treat conditions for which no drug is currently marketed in Canada
- Drugs that provide a significant increase in efficacy or significant decrease in risk when compared to existing drugs marketed in Canada.
Venetoclax (previously ABT‐199) is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Venetoclax is currently under evaluation in phase 3 trials for the treatment of relapsed, refractory, and previously untreated CLL.
Phase 2 trial
Results from a phase 2 trial of venetoclax in CLL (M13-982, NCT01889186) were published in The Lancet Oncology in June. The trial enrolled 107 patients with relapsed or refractory CLL and 17p deletion.
Patients received venetoclax at 400 mg once daily following a weekly ramp-up schedule for the first 5 weeks. The primary endpoint was overall response rate, as determined by an independent review committee.
At a median follow-up of 12.1 months, 85 patients had responded to treatment, for an overall response rate of 79%.
Eight patients (8%) achieved a complete response or complete response with incomplete count recovery, 3 (3%) had a near-partial response, and 74 (69%) had a partial response. Twenty-two patients (21%) did not respond.
At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival. The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse was 96%. The most frequent grade 3/4 adverse events were neutropenia (40%), infection (20%), anemia (18%), and thrombocytopenia (15%).
The incidence of serious adverse events was 55%. The most common of these events were pyrexia (7%), autoimmune hemolytic anemia (7%), pneumonia (6%), and febrile neutropenia (5%).
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients during the ramp-up period only. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the past, TLS has caused deaths in patients receiving venetoclax. In response, AbbVie stopped dose-escalation in patients receiving the drug and suspended enrollment in phase 1 trials.
However, researchers subsequently found that a modified dosing schedule, prophylaxis, and patient monitoring can reduce the risk of TLS. ![]()

of venetoclax (Venclexta)
Photo courtesy of AbbVie
Health Canada has issued a Notice of Compliance with Conditions (NOC/c) for the BCL-2 inhibitor venetoclax (Venclexta™).
This means venetoclax is conditionally approved for use in patients with previously treated chronic lymphocytic leukemia (CLL) who have 17p deletion or no other available treatment options.
An NOC/c is authorization to market a drug with the condition that the sponsor perform additional studies to verify a clinical benefit.
The NOC/c policy is designed to provide access to:
- Drugs that can treat serious, life-threatening, or severely debilitating diseases
- Drugs that can treat conditions for which no drug is currently marketed in Canada
- Drugs that provide a significant increase in efficacy or significant decrease in risk when compared to existing drugs marketed in Canada.
Venetoclax (previously ABT‐199) is being developed by AbbVie and Genentech, a member of the Roche Group. The drug is jointly commercialized by the companies in the US and by AbbVie outside of the US.
Venetoclax is currently under evaluation in phase 3 trials for the treatment of relapsed, refractory, and previously untreated CLL.
Phase 2 trial
Results from a phase 2 trial of venetoclax in CLL (M13-982, NCT01889186) were published in The Lancet Oncology in June. The trial enrolled 107 patients with relapsed or refractory CLL and 17p deletion.
Patients received venetoclax at 400 mg once daily following a weekly ramp-up schedule for the first 5 weeks. The primary endpoint was overall response rate, as determined by an independent review committee.
At a median follow-up of 12.1 months, 85 patients had responded to treatment, for an overall response rate of 79%.
Eight patients (8%) achieved a complete response or complete response with incomplete count recovery, 3 (3%) had a near-partial response, and 74 (69%) had a partial response. Twenty-two patients (21%) did not respond.
At the time of analysis, the median duration of response had not been reached. The same was true for progression-free survival and overall survival. The progression-free survival estimate for 12 months was 72%, and the overall survival estimate was 87%.
The incidence of treatment-emergent adverse was 96%. The most frequent grade 3/4 adverse events were neutropenia (40%), infection (20%), anemia (18%), and thrombocytopenia (15%).
The incidence of serious adverse events was 55%. The most common of these events were pyrexia (7%), autoimmune hemolytic anemia (7%), pneumonia (6%), and febrile neutropenia (5%).
Grade 3 laboratory tumor lysis syndrome (TLS) was reported in 5 patients during the ramp-up period only. Three of these patients continued on venetoclax, but 2 patients required a dose interruption of 1 day each.
In the past, TLS has caused deaths in patients receiving venetoclax. In response, AbbVie stopped dose-escalation in patients receiving the drug and suspended enrollment in phase 1 trials.
However, researchers subsequently found that a modified dosing schedule, prophylaxis, and patient monitoring can reduce the risk of TLS. ![]()
Doc offers advice on choosing a frontline TKI

Photo by D. Meyer
NEW YORK—Evaluating treatment goals is essential when choosing which tyrosine kinase inhibitor (TKI) to prescribe for a patient with newly diagnosed chronic myeloid leukemia (CML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
“Deciding what TKI to start people on really depends on what your goals are for that patient,” said the speaker, Jerald Radich, MD, of the Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance in Seattle, Washington.
Because the 3 TKIs approved for frontline treatment of CML—imatinib, dasatinib, and nilotinib—produce “amazingly similar” responses, treatment compliance becomes an important factor in patient outcomes, he noted.
“If you take 90% of your imatinib, your MMR [major molecular response] is 90%,” he said. “Your CMR [complete molecular response] is 40%. So taking drug obviously trumps the decision of what drug to take.”
Dr Radich added that the major goal of treatment is to keep patients out of accelerated-phase blast crisis. Once people progress to blast crisis on a TKI, the median survival is less than 1 year.
“So that’s why you treat people aggressively, that’s why you monitor them molecularly, to prevent that from happening,” he said.
Treatment goals
Aside from preventing patients from progressing to blast crisis, treatment goals vary.
Achieving early molecular response (MR) impacts progression and survival, as does achieving a complete cytogenetic response (CCyR).
A major molecular response (MMR) is considered a “safe haven,” Dr Radich said, because once people achieve it, they almost never progress if they stay on drug.
And with a deep/complete molecular response (CMR), patients may potentially discontinue the drug.
So how your response goals line up determines how you use the agents for your treatment course, Dr Radich said.
In all response categories—patients with CCyR, MMR, MR, CMR—survival is virtually within 95% of survival for the general population.
“This is absolutely astonishing,” Dr Radich said.
He emphasized the importance of molecular testing at 3 months and achieving a BCR-ABL level of less than 10%.
Patients who have more than 10% blasts at 3 months have an 88% chance of achieving MMR at 4 years, while those who still have more than 10% blasts at 6 months have a 3.3% chance of achieving MMR at 4 years.
Toxicity
Side effects common to the 3 frontline TKIs are myelosuppression, transaminase elevation, and change in electrolytes. Dr Radich noted that imatinib doesn’t cause much myelosuppression.
“You can give imatinib on day 28 after allogeneic transplant, and it doesn’t affect the counts, which I think is pretty darn good proof that it doesn’t have any primary hematopoietic toxicity,” he said. “You can’t try that trick with the others.”
Venous and arterial cardiovascular events with TKIs are more recently coming to light.
Cardiovascular events with imatinib are about the same as the general population, Dr Radich said.
“[In] fact, some people think it might be protective,” he noted.
Discontinuation
“When we first started treating people with these drugs, we figured that they would be on them for life . . . ,” Dr Radich said. “[Y]ou’d always have a reservoir of CML cells because you can’t extinguish all the stem cells.”
A mathematical model predicted it would take 30 to 40 years to wipe out all CML cells with a TKI. The cumulative cure rate after 15 years of treatment would be 14%. After 30 years, it would be 31%.
Conducting a discontinuation trial would have been out of the question based on these predictions.
“Fortunately, some of the people who did the next trials hadn’t read that literature,” Dr Radich said.
One discontinuation trial (EURO-SKI) included patients who had been on drug for at least 3 years and had CMR for at least 1 year. About half stayed in PCR negativity, now up to 4 years.
A number of trials are now underway evaluating the possibility of TKI discontinuation, and they are showing that between 40% and 50% of patients can remain off drug for years.
Using generic imatinib
While generic imatinib is good for cost-effective, long-term use, second-generation TKIs are better at preventing accelerated-phase blast crisis, Dr Radich said.
The second generation is also better at producing deep remissions, and discontinuation could bring with it a cost savings.
Dr Radich calculated that it cost about $2.5 million for every patient who achieves treatment-free remission using a TKI, while transplant cost $1.31 million per patient who achieves treatment-free remission.
So generic imatinib is good for low- and intermediate-risk patients, as well as for older, sicker patients.
Second-generation TKIs are appropriate for higher-risk patients until they achieve a CCyR or MMR, then they can switch to generic imatinib.
And second-generation TKIs should be used for younger patients in whom drug discontinuation is important.
Frontline treatment observations
In summary, Dr Radich made the following observations about frontline treatment in CML.
- For overall survival, imatinib is equivalent to second-generation TKIs.
- To achieve a deep MR, a second-generation TKI is better than imatinib.
- Discontinuation is equally successful with all TKIs.
- For lower-risk CML, imatinib is equivalent to second-generation TKIs.
- When it comes to progression and possibly high-risk CML, second-generation TKIs are better than imatinib.
- Second-generation TKIs produce more long-term toxicities than imatinib.
- There is substantial cost savings with generics.


Photo by D. Meyer
NEW YORK—Evaluating treatment goals is essential when choosing which tyrosine kinase inhibitor (TKI) to prescribe for a patient with newly diagnosed chronic myeloid leukemia (CML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
“Deciding what TKI to start people on really depends on what your goals are for that patient,” said the speaker, Jerald Radich, MD, of the Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance in Seattle, Washington.
Because the 3 TKIs approved for frontline treatment of CML—imatinib, dasatinib, and nilotinib—produce “amazingly similar” responses, treatment compliance becomes an important factor in patient outcomes, he noted.
“If you take 90% of your imatinib, your MMR [major molecular response] is 90%,” he said. “Your CMR [complete molecular response] is 40%. So taking drug obviously trumps the decision of what drug to take.”
Dr Radich added that the major goal of treatment is to keep patients out of accelerated-phase blast crisis. Once people progress to blast crisis on a TKI, the median survival is less than 1 year.
“So that’s why you treat people aggressively, that’s why you monitor them molecularly, to prevent that from happening,” he said.
Treatment goals
Aside from preventing patients from progressing to blast crisis, treatment goals vary.
Achieving early molecular response (MR) impacts progression and survival, as does achieving a complete cytogenetic response (CCyR).
A major molecular response (MMR) is considered a “safe haven,” Dr Radich said, because once people achieve it, they almost never progress if they stay on drug.
And with a deep/complete molecular response (CMR), patients may potentially discontinue the drug.
So how your response goals line up determines how you use the agents for your treatment course, Dr Radich said.
In all response categories—patients with CCyR, MMR, MR, CMR—survival is virtually within 95% of survival for the general population.
“This is absolutely astonishing,” Dr Radich said.
He emphasized the importance of molecular testing at 3 months and achieving a BCR-ABL level of less than 10%.
Patients who have more than 10% blasts at 3 months have an 88% chance of achieving MMR at 4 years, while those who still have more than 10% blasts at 6 months have a 3.3% chance of achieving MMR at 4 years.
Toxicity
Side effects common to the 3 frontline TKIs are myelosuppression, transaminase elevation, and change in electrolytes. Dr Radich noted that imatinib doesn’t cause much myelosuppression.
“You can give imatinib on day 28 after allogeneic transplant, and it doesn’t affect the counts, which I think is pretty darn good proof that it doesn’t have any primary hematopoietic toxicity,” he said. “You can’t try that trick with the others.”
Venous and arterial cardiovascular events with TKIs are more recently coming to light.
Cardiovascular events with imatinib are about the same as the general population, Dr Radich said.
“[In] fact, some people think it might be protective,” he noted.
Discontinuation
“When we first started treating people with these drugs, we figured that they would be on them for life . . . ,” Dr Radich said. “[Y]ou’d always have a reservoir of CML cells because you can’t extinguish all the stem cells.”
A mathematical model predicted it would take 30 to 40 years to wipe out all CML cells with a TKI. The cumulative cure rate after 15 years of treatment would be 14%. After 30 years, it would be 31%.
Conducting a discontinuation trial would have been out of the question based on these predictions.
“Fortunately, some of the people who did the next trials hadn’t read that literature,” Dr Radich said.
One discontinuation trial (EURO-SKI) included patients who had been on drug for at least 3 years and had CMR for at least 1 year. About half stayed in PCR negativity, now up to 4 years.
A number of trials are now underway evaluating the possibility of TKI discontinuation, and they are showing that between 40% and 50% of patients can remain off drug for years.
Using generic imatinib
While generic imatinib is good for cost-effective, long-term use, second-generation TKIs are better at preventing accelerated-phase blast crisis, Dr Radich said.
The second generation is also better at producing deep remissions, and discontinuation could bring with it a cost savings.
Dr Radich calculated that it cost about $2.5 million for every patient who achieves treatment-free remission using a TKI, while transplant cost $1.31 million per patient who achieves treatment-free remission.
So generic imatinib is good for low- and intermediate-risk patients, as well as for older, sicker patients.
Second-generation TKIs are appropriate for higher-risk patients until they achieve a CCyR or MMR, then they can switch to generic imatinib.
And second-generation TKIs should be used for younger patients in whom drug discontinuation is important.
Frontline treatment observations
In summary, Dr Radich made the following observations about frontline treatment in CML.
- For overall survival, imatinib is equivalent to second-generation TKIs.
- To achieve a deep MR, a second-generation TKI is better than imatinib.
- Discontinuation is equally successful with all TKIs.
- For lower-risk CML, imatinib is equivalent to second-generation TKIs.
- When it comes to progression and possibly high-risk CML, second-generation TKIs are better than imatinib.
- Second-generation TKIs produce more long-term toxicities than imatinib.
- There is substantial cost savings with generics.


Photo by D. Meyer
NEW YORK—Evaluating treatment goals is essential when choosing which tyrosine kinase inhibitor (TKI) to prescribe for a patient with newly diagnosed chronic myeloid leukemia (CML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
“Deciding what TKI to start people on really depends on what your goals are for that patient,” said the speaker, Jerald Radich, MD, of the Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance in Seattle, Washington.
Because the 3 TKIs approved for frontline treatment of CML—imatinib, dasatinib, and nilotinib—produce “amazingly similar” responses, treatment compliance becomes an important factor in patient outcomes, he noted.
“If you take 90% of your imatinib, your MMR [major molecular response] is 90%,” he said. “Your CMR [complete molecular response] is 40%. So taking drug obviously trumps the decision of what drug to take.”
Dr Radich added that the major goal of treatment is to keep patients out of accelerated-phase blast crisis. Once people progress to blast crisis on a TKI, the median survival is less than 1 year.
“So that’s why you treat people aggressively, that’s why you monitor them molecularly, to prevent that from happening,” he said.
Treatment goals
Aside from preventing patients from progressing to blast crisis, treatment goals vary.
Achieving early molecular response (MR) impacts progression and survival, as does achieving a complete cytogenetic response (CCyR).
A major molecular response (MMR) is considered a “safe haven,” Dr Radich said, because once people achieve it, they almost never progress if they stay on drug.
And with a deep/complete molecular response (CMR), patients may potentially discontinue the drug.
So how your response goals line up determines how you use the agents for your treatment course, Dr Radich said.
In all response categories—patients with CCyR, MMR, MR, CMR—survival is virtually within 95% of survival for the general population.
“This is absolutely astonishing,” Dr Radich said.
He emphasized the importance of molecular testing at 3 months and achieving a BCR-ABL level of less than 10%.
Patients who have more than 10% blasts at 3 months have an 88% chance of achieving MMR at 4 years, while those who still have more than 10% blasts at 6 months have a 3.3% chance of achieving MMR at 4 years.
Toxicity
Side effects common to the 3 frontline TKIs are myelosuppression, transaminase elevation, and change in electrolytes. Dr Radich noted that imatinib doesn’t cause much myelosuppression.
“You can give imatinib on day 28 after allogeneic transplant, and it doesn’t affect the counts, which I think is pretty darn good proof that it doesn’t have any primary hematopoietic toxicity,” he said. “You can’t try that trick with the others.”
Venous and arterial cardiovascular events with TKIs are more recently coming to light.
Cardiovascular events with imatinib are about the same as the general population, Dr Radich said.
“[In] fact, some people think it might be protective,” he noted.
Discontinuation
“When we first started treating people with these drugs, we figured that they would be on them for life . . . ,” Dr Radich said. “[Y]ou’d always have a reservoir of CML cells because you can’t extinguish all the stem cells.”
A mathematical model predicted it would take 30 to 40 years to wipe out all CML cells with a TKI. The cumulative cure rate after 15 years of treatment would be 14%. After 30 years, it would be 31%.
Conducting a discontinuation trial would have been out of the question based on these predictions.
“Fortunately, some of the people who did the next trials hadn’t read that literature,” Dr Radich said.
One discontinuation trial (EURO-SKI) included patients who had been on drug for at least 3 years and had CMR for at least 1 year. About half stayed in PCR negativity, now up to 4 years.
A number of trials are now underway evaluating the possibility of TKI discontinuation, and they are showing that between 40% and 50% of patients can remain off drug for years.
Using generic imatinib
While generic imatinib is good for cost-effective, long-term use, second-generation TKIs are better at preventing accelerated-phase blast crisis, Dr Radich said.
The second generation is also better at producing deep remissions, and discontinuation could bring with it a cost savings.
Dr Radich calculated that it cost about $2.5 million for every patient who achieves treatment-free remission using a TKI, while transplant cost $1.31 million per patient who achieves treatment-free remission.
So generic imatinib is good for low- and intermediate-risk patients, as well as for older, sicker patients.
Second-generation TKIs are appropriate for higher-risk patients until they achieve a CCyR or MMR, then they can switch to generic imatinib.
And second-generation TKIs should be used for younger patients in whom drug discontinuation is important.
Frontline treatment observations
In summary, Dr Radich made the following observations about frontline treatment in CML.
- For overall survival, imatinib is equivalent to second-generation TKIs.
- To achieve a deep MR, a second-generation TKI is better than imatinib.
- Discontinuation is equally successful with all TKIs.
- For lower-risk CML, imatinib is equivalent to second-generation TKIs.
- When it comes to progression and possibly high-risk CML, second-generation TKIs are better than imatinib.
- Second-generation TKIs produce more long-term toxicities than imatinib.
- There is substantial cost savings with generics.