User login
Median DOR, PFS not yet reached for ibrutinib in CLL

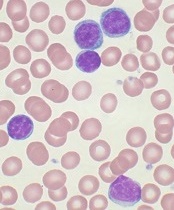
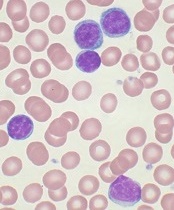
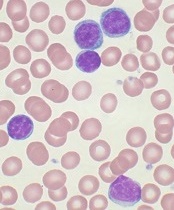
Photo courtesy of
Janssen Biotech, Inc.
NEW YORK—Long-term follow-up of single-agent ibrutinib at the approved dose of 420 mg daily confirms that the Bruton’s tyrosine kinase inhibitor produces rapid and durable responses in patients with chronic lymphocytic leukemia (CLL), according to an update presented at Lymphoma & Myeloma 2015.
At up to 44 months of follow-up, the median duration of response (DOR) and progression-free survival (PFS) have not yet been reached.
At 30 months, the PFS rate was 96% for treatment-naïve patients and 76% for relapsed or refractory patients. Patients with del 17p had a median PFS of 32.4 months.
“Virtually all the patients do respond to treatment,” said Steven Coutre, MD, of Stanford University School of Medicine in California.
“Only a handful of patients achieve less than CR [complete response] or PR [partial response],” he said during his presentation at the meeting.
Phase 1/2b and extension studies
Ninety-four patients enrolled in the phase 1/2b (PCYC-1102) and extension (PCYC-1103) studies received 420 mg of ibrutinib once daily.
“We initially enrolled patients with relapsed/refractory CLL,” Dr Coutre clarified. “Then, because of the significant efficacy and safety that was observed, we added a second cohort of treatment-naïve patients age 65 and older.”
The treatment-naïve (TN) cohort consisted of 27 CLL patients. The relapsed or refractory (R/R) cohort consisted of 67 patients with CLL or small lymphocytic lymphoma, including patients with high-risk disease, which was defined as disease progression less than 24 months after the start of a chemoimmunotherapy regimen or refractory to the most recent regimen.
The median time on study was 32 months (range, 0–44).
In the TN cohort, the median age was 71, 78% were ECOG performance status 0, and most had advanced disease as indicated by Rai stage.
In the R/R cohort, the median age was 66, 40% were ECOG performance status 0, 57% were ECOG performance status 1, and 52% had bulky nodes greater than 5 cm.
“We had a significant representation of high-risk cytogenetic abnormalities,” Dr Coutre noted.
In the R/R group, 34% of patients had del 17p, and 33% had del 11q. In the TN cohort, 7% of patients had del 17p, and none had del 11q.
“There were also a significant number of cytopenias,” Dr Coutre said, “as one might expect in a heavily pretreated patient population.”
The number of prior therapies was also “quite significant,” he said, with 55% having a median of 4 or more therapies (range, 1–12).
“It really stretches the imagination to figure out what those 12 different regimens were,” he commented.
All R/R patients had prior chemotherapy, 94% a nucleoside analog, 90% an alkylator (including bendamustine), 99% anti-CD20-based therapy, 97% anti-CD20-based chemoimmunotherapy, 24% alemtuzumab, and 6% idelalisib.
The median time on treatment was 30.4 months (range, 1.3–44.2) for TN patients and 21.9 months (range, 0.3–44.6) for R/R patients. The majority of patients in both groups remain on ibrutinib—81% of the TN patients and 60% of R/R patients.
Safety
“Only 1 patient in the treatment-naïve cohort has progressed,” Dr Coutre noted. “That was a patient with deletion 17p [who progressed in about 8 months].”
The primary reasons for discontinuing therapy were progressive disease (1 TN, 11 R/R), adverse events (AEs; 3 TN, 9 R/R), consent withdrawal (1 TN, 2 R/R), investigators’ decision (0 TN, 4 R/R), and other reasons (0 TN, 1 R/R).
“Discontinuations due to AEs occurred predominantly early,” Dr Coutre observed. “So of the 12 patients [who discontinued due to AEs], 7 discontinued in the first year, 3 in the second year, and only 2 beyond year 3.”
Grade 3 or higher AEs occurred in 55 R/R patients (82%) and 17 TN patients (63%). Infection occurred in 48% of R/R patients and 11% of TN patients. Dr Coutre pointed out that most of these AEs were not related to ibrutinib.
Grade 3 or higher ibrutinib-related AEs occurred in 6 TN patients (22%) and 25 R/R patients (37%). One TN patient and 8 R/R patients experienced grade 3 or higher serious ibrutinib-related AEs.
One TN patient and 7 R/R patients required a dose reduction due to an AE. However, the dose reductions occurred predominantly during the first year, Dr Coutre noted.
Regarding time to onset of grade 3 or higher AEs, Dr Coutre said most of the events occurred early and decreased with time. Pneumonia and atrial fibrillation followed this pattern, as did neutropenia and thrombocytopenia. Hypertension was the exception, occurring during all years.
Nonhematologic AEs of grade 3 or higher that occurred in at least 5% of patients were pneumonia, hypertension, diarrhea, hyponatremia, and atrial fibrillation in TN patients, and sepsis, cellulitis, dehydration, and fatigue in R/R patients.
Hematologic AEs of grade 3 or higher in each cohort included neutropenia, thrombocytopenia, and anemia.
“The drug doesn’t seem to be myelosuppressive,” Dr Coutre noted. “We don’t have prolonged cytopenias as patients stay on treatment.”
One TN patient and 7 R/R patients died during the study.
Response and survival
The response rate (as assessed by the investigators) was 85% for TN patients. Twenty-six percent of patients achieved a complete response, 52% a partial response (PR), and 7% a PR with lymphocytosis.
The response rate for R/R patients was 94%. Nine percent achieved a complete response, 82% a PR, and 3% a PR with lymphocytosis.
The median time to the best response was 7.4 months for both cohorts.
The median DOR has not been reached in either cohort, but the 30-month DOR was 95.2% for TN patients and 79.1% for R/R patients.
The 30-month PFS was 95.8% for TN patients and 75.9% for R/R patients.
At 30 months, the PFS rate was 59.6% for patients with del 17p and 82.4% for patients with del 11q. The median PFS for patients with del 17p was 32.4 months, and it was not reached for patients with del 11q. For patients with neither of these abnormalities, the median PFS has not been reached.
“Overall survival was equally impressive,” Dr Coutre said.
The median overall survival has not been reached for any group, and 30-month overall survival is 81.3% for del 17p patients, 88.2% for patients with del 11q, and 90.3% for patients with neither abnormality.
“[I]brutinib induces rapid and durable responses that continue to improve over time . . . ,” Dr Coutre said.
He added that the drug is well-tolerated, “allowing us to continue patients on treatment, which, I think, is particularly important for these types of drugs because we clearly see that patients have significant clinical benefit, despite the fact that they still often have easily detectable disease, particularly in the bone marrow.”
“So one of the challenges is going to be [to determine] how to use these drugs on a long-term basis and [see if we can] use them in a more time-limited fashion.”
Ibrutinib is approved by the US Food and Drug Administration for 4 indications: patients with CLL who have received at least 1 prior therapy, CLL patients with del 17p, patients with mantle cell lymphoma, and patients with Waldenström’s macroglobulinemia.
Ibrutinib is distributed and marketed as Imbruvica by Pharmacyclics and also marketed by Janssen Biotech, Inc. ![]()

Photo courtesy of
Janssen Biotech, Inc.
NEW YORK—Long-term follow-up of single-agent ibrutinib at the approved dose of 420 mg daily confirms that the Bruton’s tyrosine kinase inhibitor produces rapid and durable responses in patients with chronic lymphocytic leukemia (CLL), according to an update presented at Lymphoma & Myeloma 2015.
At up to 44 months of follow-up, the median duration of response (DOR) and progression-free survival (PFS) have not yet been reached.
At 30 months, the PFS rate was 96% for treatment-naïve patients and 76% for relapsed or refractory patients. Patients with del 17p had a median PFS of 32.4 months.
“Virtually all the patients do respond to treatment,” said Steven Coutre, MD, of Stanford University School of Medicine in California.
“Only a handful of patients achieve less than CR [complete response] or PR [partial response],” he said during his presentation at the meeting.
Phase 1/2b and extension studies
Ninety-four patients enrolled in the phase 1/2b (PCYC-1102) and extension (PCYC-1103) studies received 420 mg of ibrutinib once daily.
“We initially enrolled patients with relapsed/refractory CLL,” Dr Coutre clarified. “Then, because of the significant efficacy and safety that was observed, we added a second cohort of treatment-naïve patients age 65 and older.”
The treatment-naïve (TN) cohort consisted of 27 CLL patients. The relapsed or refractory (R/R) cohort consisted of 67 patients with CLL or small lymphocytic lymphoma, including patients with high-risk disease, which was defined as disease progression less than 24 months after the start of a chemoimmunotherapy regimen or refractory to the most recent regimen.
The median time on study was 32 months (range, 0–44).
In the TN cohort, the median age was 71, 78% were ECOG performance status 0, and most had advanced disease as indicated by Rai stage.
In the R/R cohort, the median age was 66, 40% were ECOG performance status 0, 57% were ECOG performance status 1, and 52% had bulky nodes greater than 5 cm.
“We had a significant representation of high-risk cytogenetic abnormalities,” Dr Coutre noted.
In the R/R group, 34% of patients had del 17p, and 33% had del 11q. In the TN cohort, 7% of patients had del 17p, and none had del 11q.
“There were also a significant number of cytopenias,” Dr Coutre said, “as one might expect in a heavily pretreated patient population.”
The number of prior therapies was also “quite significant,” he said, with 55% having a median of 4 or more therapies (range, 1–12).
“It really stretches the imagination to figure out what those 12 different regimens were,” he commented.
All R/R patients had prior chemotherapy, 94% a nucleoside analog, 90% an alkylator (including bendamustine), 99% anti-CD20-based therapy, 97% anti-CD20-based chemoimmunotherapy, 24% alemtuzumab, and 6% idelalisib.
The median time on treatment was 30.4 months (range, 1.3–44.2) for TN patients and 21.9 months (range, 0.3–44.6) for R/R patients. The majority of patients in both groups remain on ibrutinib—81% of the TN patients and 60% of R/R patients.
Safety
“Only 1 patient in the treatment-naïve cohort has progressed,” Dr Coutre noted. “That was a patient with deletion 17p [who progressed in about 8 months].”
The primary reasons for discontinuing therapy were progressive disease (1 TN, 11 R/R), adverse events (AEs; 3 TN, 9 R/R), consent withdrawal (1 TN, 2 R/R), investigators’ decision (0 TN, 4 R/R), and other reasons (0 TN, 1 R/R).
“Discontinuations due to AEs occurred predominantly early,” Dr Coutre observed. “So of the 12 patients [who discontinued due to AEs], 7 discontinued in the first year, 3 in the second year, and only 2 beyond year 3.”
Grade 3 or higher AEs occurred in 55 R/R patients (82%) and 17 TN patients (63%). Infection occurred in 48% of R/R patients and 11% of TN patients. Dr Coutre pointed out that most of these AEs were not related to ibrutinib.
Grade 3 or higher ibrutinib-related AEs occurred in 6 TN patients (22%) and 25 R/R patients (37%). One TN patient and 8 R/R patients experienced grade 3 or higher serious ibrutinib-related AEs.
One TN patient and 7 R/R patients required a dose reduction due to an AE. However, the dose reductions occurred predominantly during the first year, Dr Coutre noted.
Regarding time to onset of grade 3 or higher AEs, Dr Coutre said most of the events occurred early and decreased with time. Pneumonia and atrial fibrillation followed this pattern, as did neutropenia and thrombocytopenia. Hypertension was the exception, occurring during all years.
Nonhematologic AEs of grade 3 or higher that occurred in at least 5% of patients were pneumonia, hypertension, diarrhea, hyponatremia, and atrial fibrillation in TN patients, and sepsis, cellulitis, dehydration, and fatigue in R/R patients.
Hematologic AEs of grade 3 or higher in each cohort included neutropenia, thrombocytopenia, and anemia.
“The drug doesn’t seem to be myelosuppressive,” Dr Coutre noted. “We don’t have prolonged cytopenias as patients stay on treatment.”
One TN patient and 7 R/R patients died during the study.
Response and survival
The response rate (as assessed by the investigators) was 85% for TN patients. Twenty-six percent of patients achieved a complete response, 52% a partial response (PR), and 7% a PR with lymphocytosis.
The response rate for R/R patients was 94%. Nine percent achieved a complete response, 82% a PR, and 3% a PR with lymphocytosis.
The median time to the best response was 7.4 months for both cohorts.
The median DOR has not been reached in either cohort, but the 30-month DOR was 95.2% for TN patients and 79.1% for R/R patients.
The 30-month PFS was 95.8% for TN patients and 75.9% for R/R patients.
At 30 months, the PFS rate was 59.6% for patients with del 17p and 82.4% for patients with del 11q. The median PFS for patients with del 17p was 32.4 months, and it was not reached for patients with del 11q. For patients with neither of these abnormalities, the median PFS has not been reached.
“Overall survival was equally impressive,” Dr Coutre said.
The median overall survival has not been reached for any group, and 30-month overall survival is 81.3% for del 17p patients, 88.2% for patients with del 11q, and 90.3% for patients with neither abnormality.
“[I]brutinib induces rapid and durable responses that continue to improve over time . . . ,” Dr Coutre said.
He added that the drug is well-tolerated, “allowing us to continue patients on treatment, which, I think, is particularly important for these types of drugs because we clearly see that patients have significant clinical benefit, despite the fact that they still often have easily detectable disease, particularly in the bone marrow.”
“So one of the challenges is going to be [to determine] how to use these drugs on a long-term basis and [see if we can] use them in a more time-limited fashion.”
Ibrutinib is approved by the US Food and Drug Administration for 4 indications: patients with CLL who have received at least 1 prior therapy, CLL patients with del 17p, patients with mantle cell lymphoma, and patients with Waldenström’s macroglobulinemia.
Ibrutinib is distributed and marketed as Imbruvica by Pharmacyclics and also marketed by Janssen Biotech, Inc. ![]()

Photo courtesy of
Janssen Biotech, Inc.
NEW YORK—Long-term follow-up of single-agent ibrutinib at the approved dose of 420 mg daily confirms that the Bruton’s tyrosine kinase inhibitor produces rapid and durable responses in patients with chronic lymphocytic leukemia (CLL), according to an update presented at Lymphoma & Myeloma 2015.
At up to 44 months of follow-up, the median duration of response (DOR) and progression-free survival (PFS) have not yet been reached.
At 30 months, the PFS rate was 96% for treatment-naïve patients and 76% for relapsed or refractory patients. Patients with del 17p had a median PFS of 32.4 months.
“Virtually all the patients do respond to treatment,” said Steven Coutre, MD, of Stanford University School of Medicine in California.
“Only a handful of patients achieve less than CR [complete response] or PR [partial response],” he said during his presentation at the meeting.
Phase 1/2b and extension studies
Ninety-four patients enrolled in the phase 1/2b (PCYC-1102) and extension (PCYC-1103) studies received 420 mg of ibrutinib once daily.
“We initially enrolled patients with relapsed/refractory CLL,” Dr Coutre clarified. “Then, because of the significant efficacy and safety that was observed, we added a second cohort of treatment-naïve patients age 65 and older.”
The treatment-naïve (TN) cohort consisted of 27 CLL patients. The relapsed or refractory (R/R) cohort consisted of 67 patients with CLL or small lymphocytic lymphoma, including patients with high-risk disease, which was defined as disease progression less than 24 months after the start of a chemoimmunotherapy regimen or refractory to the most recent regimen.
The median time on study was 32 months (range, 0–44).
In the TN cohort, the median age was 71, 78% were ECOG performance status 0, and most had advanced disease as indicated by Rai stage.
In the R/R cohort, the median age was 66, 40% were ECOG performance status 0, 57% were ECOG performance status 1, and 52% had bulky nodes greater than 5 cm.
“We had a significant representation of high-risk cytogenetic abnormalities,” Dr Coutre noted.
In the R/R group, 34% of patients had del 17p, and 33% had del 11q. In the TN cohort, 7% of patients had del 17p, and none had del 11q.
“There were also a significant number of cytopenias,” Dr Coutre said, “as one might expect in a heavily pretreated patient population.”
The number of prior therapies was also “quite significant,” he said, with 55% having a median of 4 or more therapies (range, 1–12).
“It really stretches the imagination to figure out what those 12 different regimens were,” he commented.
All R/R patients had prior chemotherapy, 94% a nucleoside analog, 90% an alkylator (including bendamustine), 99% anti-CD20-based therapy, 97% anti-CD20-based chemoimmunotherapy, 24% alemtuzumab, and 6% idelalisib.
The median time on treatment was 30.4 months (range, 1.3–44.2) for TN patients and 21.9 months (range, 0.3–44.6) for R/R patients. The majority of patients in both groups remain on ibrutinib—81% of the TN patients and 60% of R/R patients.
Safety
“Only 1 patient in the treatment-naïve cohort has progressed,” Dr Coutre noted. “That was a patient with deletion 17p [who progressed in about 8 months].”
The primary reasons for discontinuing therapy were progressive disease (1 TN, 11 R/R), adverse events (AEs; 3 TN, 9 R/R), consent withdrawal (1 TN, 2 R/R), investigators’ decision (0 TN, 4 R/R), and other reasons (0 TN, 1 R/R).
“Discontinuations due to AEs occurred predominantly early,” Dr Coutre observed. “So of the 12 patients [who discontinued due to AEs], 7 discontinued in the first year, 3 in the second year, and only 2 beyond year 3.”
Grade 3 or higher AEs occurred in 55 R/R patients (82%) and 17 TN patients (63%). Infection occurred in 48% of R/R patients and 11% of TN patients. Dr Coutre pointed out that most of these AEs were not related to ibrutinib.
Grade 3 or higher ibrutinib-related AEs occurred in 6 TN patients (22%) and 25 R/R patients (37%). One TN patient and 8 R/R patients experienced grade 3 or higher serious ibrutinib-related AEs.
One TN patient and 7 R/R patients required a dose reduction due to an AE. However, the dose reductions occurred predominantly during the first year, Dr Coutre noted.
Regarding time to onset of grade 3 or higher AEs, Dr Coutre said most of the events occurred early and decreased with time. Pneumonia and atrial fibrillation followed this pattern, as did neutropenia and thrombocytopenia. Hypertension was the exception, occurring during all years.
Nonhematologic AEs of grade 3 or higher that occurred in at least 5% of patients were pneumonia, hypertension, diarrhea, hyponatremia, and atrial fibrillation in TN patients, and sepsis, cellulitis, dehydration, and fatigue in R/R patients.
Hematologic AEs of grade 3 or higher in each cohort included neutropenia, thrombocytopenia, and anemia.
“The drug doesn’t seem to be myelosuppressive,” Dr Coutre noted. “We don’t have prolonged cytopenias as patients stay on treatment.”
One TN patient and 7 R/R patients died during the study.
Response and survival
The response rate (as assessed by the investigators) was 85% for TN patients. Twenty-six percent of patients achieved a complete response, 52% a partial response (PR), and 7% a PR with lymphocytosis.
The response rate for R/R patients was 94%. Nine percent achieved a complete response, 82% a PR, and 3% a PR with lymphocytosis.
The median time to the best response was 7.4 months for both cohorts.
The median DOR has not been reached in either cohort, but the 30-month DOR was 95.2% for TN patients and 79.1% for R/R patients.
The 30-month PFS was 95.8% for TN patients and 75.9% for R/R patients.
At 30 months, the PFS rate was 59.6% for patients with del 17p and 82.4% for patients with del 11q. The median PFS for patients with del 17p was 32.4 months, and it was not reached for patients with del 11q. For patients with neither of these abnormalities, the median PFS has not been reached.
“Overall survival was equally impressive,” Dr Coutre said.
The median overall survival has not been reached for any group, and 30-month overall survival is 81.3% for del 17p patients, 88.2% for patients with del 11q, and 90.3% for patients with neither abnormality.
“[I]brutinib induces rapid and durable responses that continue to improve over time . . . ,” Dr Coutre said.
He added that the drug is well-tolerated, “allowing us to continue patients on treatment, which, I think, is particularly important for these types of drugs because we clearly see that patients have significant clinical benefit, despite the fact that they still often have easily detectable disease, particularly in the bone marrow.”
“So one of the challenges is going to be [to determine] how to use these drugs on a long-term basis and [see if we can] use them in a more time-limited fashion.”
Ibrutinib is approved by the US Food and Drug Administration for 4 indications: patients with CLL who have received at least 1 prior therapy, CLL patients with del 17p, patients with mantle cell lymphoma, and patients with Waldenström’s macroglobulinemia.
Ibrutinib is distributed and marketed as Imbruvica by Pharmacyclics and also marketed by Janssen Biotech, Inc. ![]()
Alternative splicing enables resistance to CTL019

Photo from Penn Medicine
New research has provided an explanation for resistance to CTL019, a CD19 chimeric antigen receptor (CAR) T-cell therapy.
Investigators analyzed samples from children with B-cell acute lymphoblastic leukemia (B-ALL) and found evidence to suggest that CTL019 resistance can be caused by CD19 splicing alterations.
These alterations prompt the loss of certain parts of the CD19 protein that are recognized by the CAR T cells.
The team described this work in Cancer Discovery.
They noted that 10% to 20% of B-ALL patients treated with CD19-directed immunotherapy may experience relapse.
“Some of them can be successfully retreated, but, in others, a more pernicious kind of leukemia may emerge, which no longer responds to CTL019,” said study author Andrei Thomas-Tikhonenko, PhD, of the University of Pennsylvania in Philadelphia.
“In some cases, resistance is accompanied by the disappearance of the target CD19 protein from the cell surface . . . . Our goal was to figure out how the CD19 protein manages to vanish and whether it is gone for good or whether it could, under certain circumstances, be coaxed back.”
“Our initial finding from this study was that, in most cases, the CD19 genetic code was not irretrievably lost. We also discovered that the CD19 protein was still being made, but as a shorter version, which escapes detection by the immune system.”
To understand the mechanism of CTL019 resistance, Dr Thomas-Tikhonenko and his colleagues studied multiple tumor samples from 4 children with B-ALL. The samples were collected before the patients were treated with CTL019 and/or after they developed resistance to the therapy.
The investigators found that, in some cases, 1 copy of the gene coding for CD19 (located on chromosome 16) was deleted, and the other copy was damaged as a result of mutations in coding areas of the CD19 gene, most frequently in exon 2.
However, the team also discovered alternatively spliced CD19 messenger RNA species in which exons 2, 5, and 6 were frequently skipped, making mutations in exon 2 largely irrelevant.
Subsequent investigation revealed that deletion of exons 5 and 6 resulted in premature termination of CD19.
Deletion of exon 2 resulted in the production of a modified version of CD19, which was more stable than its standard version. The shortened protein was functional and could perform many of the tasks that CD19 is known to handle, but it cannot be targeted by CTL019.
The importance of exon skipping in CTL019 resistance cannot be overstated, Dr Thomas-Tikhonenko said.
“Without exons 5 and 6, the CD19 protein has no way of being retained on the cell surface,” he explained. “The case of missing exon 2 is more complex. Although the resultant protein can make it to the cell surface, albeit not very efficiently, it can no longer be recognized by CTL019.”
He and his colleagues believe this research can inform future use of CTL019 and immunotherapy in general.
“[A]lternative splicing could be a potent, built-in mechanism of resistance, and it might be better to target proteins that, unlike CD19, are not prone to exon skipping,” Dr Thomas-Tikhonenko said.
“[In addition,] it might be important to preselect patients for CTL019 and similar therapies and make sure that the alternatively spliced CD19 variants are not already present in their leukemias. If they are, resistance could develop very quickly.”
Designing new immunotherapeutics that can recognize the shortened version of CD19 is another approach to overcoming CTL019 resistance, he added.
He and his colleagues noted that this study was limited by the relatively small number of samples analyzed, which might have prevented the investigators from identifying additional mechanisms of resistance. ![]()

Photo from Penn Medicine
New research has provided an explanation for resistance to CTL019, a CD19 chimeric antigen receptor (CAR) T-cell therapy.
Investigators analyzed samples from children with B-cell acute lymphoblastic leukemia (B-ALL) and found evidence to suggest that CTL019 resistance can be caused by CD19 splicing alterations.
These alterations prompt the loss of certain parts of the CD19 protein that are recognized by the CAR T cells.
The team described this work in Cancer Discovery.
They noted that 10% to 20% of B-ALL patients treated with CD19-directed immunotherapy may experience relapse.
“Some of them can be successfully retreated, but, in others, a more pernicious kind of leukemia may emerge, which no longer responds to CTL019,” said study author Andrei Thomas-Tikhonenko, PhD, of the University of Pennsylvania in Philadelphia.
“In some cases, resistance is accompanied by the disappearance of the target CD19 protein from the cell surface . . . . Our goal was to figure out how the CD19 protein manages to vanish and whether it is gone for good or whether it could, under certain circumstances, be coaxed back.”
“Our initial finding from this study was that, in most cases, the CD19 genetic code was not irretrievably lost. We also discovered that the CD19 protein was still being made, but as a shorter version, which escapes detection by the immune system.”
To understand the mechanism of CTL019 resistance, Dr Thomas-Tikhonenko and his colleagues studied multiple tumor samples from 4 children with B-ALL. The samples were collected before the patients were treated with CTL019 and/or after they developed resistance to the therapy.
The investigators found that, in some cases, 1 copy of the gene coding for CD19 (located on chromosome 16) was deleted, and the other copy was damaged as a result of mutations in coding areas of the CD19 gene, most frequently in exon 2.
However, the team also discovered alternatively spliced CD19 messenger RNA species in which exons 2, 5, and 6 were frequently skipped, making mutations in exon 2 largely irrelevant.
Subsequent investigation revealed that deletion of exons 5 and 6 resulted in premature termination of CD19.
Deletion of exon 2 resulted in the production of a modified version of CD19, which was more stable than its standard version. The shortened protein was functional and could perform many of the tasks that CD19 is known to handle, but it cannot be targeted by CTL019.
The importance of exon skipping in CTL019 resistance cannot be overstated, Dr Thomas-Tikhonenko said.
“Without exons 5 and 6, the CD19 protein has no way of being retained on the cell surface,” he explained. “The case of missing exon 2 is more complex. Although the resultant protein can make it to the cell surface, albeit not very efficiently, it can no longer be recognized by CTL019.”
He and his colleagues believe this research can inform future use of CTL019 and immunotherapy in general.
“[A]lternative splicing could be a potent, built-in mechanism of resistance, and it might be better to target proteins that, unlike CD19, are not prone to exon skipping,” Dr Thomas-Tikhonenko said.
“[In addition,] it might be important to preselect patients for CTL019 and similar therapies and make sure that the alternatively spliced CD19 variants are not already present in their leukemias. If they are, resistance could develop very quickly.”
Designing new immunotherapeutics that can recognize the shortened version of CD19 is another approach to overcoming CTL019 resistance, he added.
He and his colleagues noted that this study was limited by the relatively small number of samples analyzed, which might have prevented the investigators from identifying additional mechanisms of resistance. ![]()

Photo from Penn Medicine
New research has provided an explanation for resistance to CTL019, a CD19 chimeric antigen receptor (CAR) T-cell therapy.
Investigators analyzed samples from children with B-cell acute lymphoblastic leukemia (B-ALL) and found evidence to suggest that CTL019 resistance can be caused by CD19 splicing alterations.
These alterations prompt the loss of certain parts of the CD19 protein that are recognized by the CAR T cells.
The team described this work in Cancer Discovery.
They noted that 10% to 20% of B-ALL patients treated with CD19-directed immunotherapy may experience relapse.
“Some of them can be successfully retreated, but, in others, a more pernicious kind of leukemia may emerge, which no longer responds to CTL019,” said study author Andrei Thomas-Tikhonenko, PhD, of the University of Pennsylvania in Philadelphia.
“In some cases, resistance is accompanied by the disappearance of the target CD19 protein from the cell surface . . . . Our goal was to figure out how the CD19 protein manages to vanish and whether it is gone for good or whether it could, under certain circumstances, be coaxed back.”
“Our initial finding from this study was that, in most cases, the CD19 genetic code was not irretrievably lost. We also discovered that the CD19 protein was still being made, but as a shorter version, which escapes detection by the immune system.”
To understand the mechanism of CTL019 resistance, Dr Thomas-Tikhonenko and his colleagues studied multiple tumor samples from 4 children with B-ALL. The samples were collected before the patients were treated with CTL019 and/or after they developed resistance to the therapy.
The investigators found that, in some cases, 1 copy of the gene coding for CD19 (located on chromosome 16) was deleted, and the other copy was damaged as a result of mutations in coding areas of the CD19 gene, most frequently in exon 2.
However, the team also discovered alternatively spliced CD19 messenger RNA species in which exons 2, 5, and 6 were frequently skipped, making mutations in exon 2 largely irrelevant.
Subsequent investigation revealed that deletion of exons 5 and 6 resulted in premature termination of CD19.
Deletion of exon 2 resulted in the production of a modified version of CD19, which was more stable than its standard version. The shortened protein was functional and could perform many of the tasks that CD19 is known to handle, but it cannot be targeted by CTL019.
The importance of exon skipping in CTL019 resistance cannot be overstated, Dr Thomas-Tikhonenko said.
“Without exons 5 and 6, the CD19 protein has no way of being retained on the cell surface,” he explained. “The case of missing exon 2 is more complex. Although the resultant protein can make it to the cell surface, albeit not very efficiently, it can no longer be recognized by CTL019.”
He and his colleagues believe this research can inform future use of CTL019 and immunotherapy in general.
“[A]lternative splicing could be a potent, built-in mechanism of resistance, and it might be better to target proteins that, unlike CD19, are not prone to exon skipping,” Dr Thomas-Tikhonenko said.
“[In addition,] it might be important to preselect patients for CTL019 and similar therapies and make sure that the alternatively spliced CD19 variants are not already present in their leukemias. If they are, resistance could develop very quickly.”
Designing new immunotherapeutics that can recognize the shortened version of CD19 is another approach to overcoming CTL019 resistance, he added.
He and his colleagues noted that this study was limited by the relatively small number of samples analyzed, which might have prevented the investigators from identifying additional mechanisms of resistance. ![]()
Germline genetic variation linked to pediatric ALL

Photo courtesy of
St. Jude/Seth Dixon
Germline variations in the ETV6 gene are associated with an increased risk of developing pediatric acute lymphoblastic leukemia (ALL), according to research published in The Lancet Oncology.
Researchers said the magnitude of the risk must still be determined, as well as how the variants identified may promote ALL.
The evidence suggests that ETV6 variation alone is not sufficient to cause ALL but may play a significant role in inherited predisposition to childhood ALL.
The researchers discovered the association between the ETV6 variants and childhood ALL by sequencing the whole exome of a family in which the mother and 2 of the 3 children have a history of pediatric ALL.
All were treated at St. Jude Children’s Research Hospital in Memphis, Tennessee, and are now cancer-free.
The researchers identified a novel non-sense ETV6 variant (p.Arg359X) in this mother and her 3 children, including a daughter who has not been diagnosed with cancer. The father does not have the variant.
This variant is predicted to result in the production of a shortened ETV6 protein that cannot fulfill its normal function of binding to DNA and regulating the expression of other genes.
The researchers screened an additional 4405 children with ALL and found 31 ETV6 exonic variants—21 missense, 5 frameshift, 4 non-sense, and 1 splice site—that are potentially related to leukemia risk in 35 patients, or almost 1% of the patients screened.
The variants identified were unique to ALL patients or extremely rare in the general population, the researchers said.
Patients with the variants tended to be older when diagnosed with ALL (10.2 years vs 4.7 years; P=0.017) and were more likely to have hyperdiploid leukemia. Sixty-four percent of ALL cases with germline ETV6 variants were hyperdiploid, compared to 27% of ALL cases without the variants (P=0.0050).
The variants were not associated with a particular ethnicity or with the outcome of ALL therapy.
The researchers also noted that almost half of the ETV6 variants identified (n=15) clustered in the erythroblast transformation specific domain.
“That suggests the loss or alteration of this DNA-binding function of ETV6 may be critical to cancer promotion,” said study author Jun J. Yang, PhD, of St. Jude.
“This is the latest example of the important role that genetic variation and inheritance plays in ALL risk. That has clear clinical implications and will help us understand the biology driving this cancer.”
These findings build on previous work that revealed an association between inherited ETV6 variations and thrombocytopenia in families with a susceptibility to hematologic malignancies. The researchers said this new study further solidifies the association between ETV6 and pediatric ALL. ![]()

Photo courtesy of
St. Jude/Seth Dixon
Germline variations in the ETV6 gene are associated with an increased risk of developing pediatric acute lymphoblastic leukemia (ALL), according to research published in The Lancet Oncology.
Researchers said the magnitude of the risk must still be determined, as well as how the variants identified may promote ALL.
The evidence suggests that ETV6 variation alone is not sufficient to cause ALL but may play a significant role in inherited predisposition to childhood ALL.
The researchers discovered the association between the ETV6 variants and childhood ALL by sequencing the whole exome of a family in which the mother and 2 of the 3 children have a history of pediatric ALL.
All were treated at St. Jude Children’s Research Hospital in Memphis, Tennessee, and are now cancer-free.
The researchers identified a novel non-sense ETV6 variant (p.Arg359X) in this mother and her 3 children, including a daughter who has not been diagnosed with cancer. The father does not have the variant.
This variant is predicted to result in the production of a shortened ETV6 protein that cannot fulfill its normal function of binding to DNA and regulating the expression of other genes.
The researchers screened an additional 4405 children with ALL and found 31 ETV6 exonic variants—21 missense, 5 frameshift, 4 non-sense, and 1 splice site—that are potentially related to leukemia risk in 35 patients, or almost 1% of the patients screened.
The variants identified were unique to ALL patients or extremely rare in the general population, the researchers said.
Patients with the variants tended to be older when diagnosed with ALL (10.2 years vs 4.7 years; P=0.017) and were more likely to have hyperdiploid leukemia. Sixty-four percent of ALL cases with germline ETV6 variants were hyperdiploid, compared to 27% of ALL cases without the variants (P=0.0050).
The variants were not associated with a particular ethnicity or with the outcome of ALL therapy.
The researchers also noted that almost half of the ETV6 variants identified (n=15) clustered in the erythroblast transformation specific domain.
“That suggests the loss or alteration of this DNA-binding function of ETV6 may be critical to cancer promotion,” said study author Jun J. Yang, PhD, of St. Jude.
“This is the latest example of the important role that genetic variation and inheritance plays in ALL risk. That has clear clinical implications and will help us understand the biology driving this cancer.”
These findings build on previous work that revealed an association between inherited ETV6 variations and thrombocytopenia in families with a susceptibility to hematologic malignancies. The researchers said this new study further solidifies the association between ETV6 and pediatric ALL. ![]()

Photo courtesy of
St. Jude/Seth Dixon
Germline variations in the ETV6 gene are associated with an increased risk of developing pediatric acute lymphoblastic leukemia (ALL), according to research published in The Lancet Oncology.
Researchers said the magnitude of the risk must still be determined, as well as how the variants identified may promote ALL.
The evidence suggests that ETV6 variation alone is not sufficient to cause ALL but may play a significant role in inherited predisposition to childhood ALL.
The researchers discovered the association between the ETV6 variants and childhood ALL by sequencing the whole exome of a family in which the mother and 2 of the 3 children have a history of pediatric ALL.
All were treated at St. Jude Children’s Research Hospital in Memphis, Tennessee, and are now cancer-free.
The researchers identified a novel non-sense ETV6 variant (p.Arg359X) in this mother and her 3 children, including a daughter who has not been diagnosed with cancer. The father does not have the variant.
This variant is predicted to result in the production of a shortened ETV6 protein that cannot fulfill its normal function of binding to DNA and regulating the expression of other genes.
The researchers screened an additional 4405 children with ALL and found 31 ETV6 exonic variants—21 missense, 5 frameshift, 4 non-sense, and 1 splice site—that are potentially related to leukemia risk in 35 patients, or almost 1% of the patients screened.
The variants identified were unique to ALL patients or extremely rare in the general population, the researchers said.
Patients with the variants tended to be older when diagnosed with ALL (10.2 years vs 4.7 years; P=0.017) and were more likely to have hyperdiploid leukemia. Sixty-four percent of ALL cases with germline ETV6 variants were hyperdiploid, compared to 27% of ALL cases without the variants (P=0.0050).
The variants were not associated with a particular ethnicity or with the outcome of ALL therapy.
The researchers also noted that almost half of the ETV6 variants identified (n=15) clustered in the erythroblast transformation specific domain.
“That suggests the loss or alteration of this DNA-binding function of ETV6 may be critical to cancer promotion,” said study author Jun J. Yang, PhD, of St. Jude.
“This is the latest example of the important role that genetic variation and inheritance plays in ALL risk. That has clear clinical implications and will help us understand the biology driving this cancer.”
These findings build on previous work that revealed an association between inherited ETV6 variations and thrombocytopenia in families with a susceptibility to hematologic malignancies. The researchers said this new study further solidifies the association between ETV6 and pediatric ALL. ![]()
Cancer care in Latin America

patient and her father
Photo by Rhoda Baer
Despite progress made in cancer care in Latin America in the last 2 years, substantial barriers remain to ensure optimal clinical management, according to a report commissioned by The Lancet Oncology.
The report, an update from a report published in 2013, details a number of improvements in cancer care in Latin America, either specifically related to cancer or to general healthcare initiatives that will also benefit cancer patients.
However, the updated report also suggests that major changes are needed in many areas to increase the standard of cancer care in Latin America.
Progress made
According to the report, progress has been made in the following areas.
The proportion of people in Latin America affiliated with any kind of health insurance program grew from 46% to 60% between 2008 and 2013.
For 2014, the World Health Organization (WHO) reported an 8% increase in the number of countries (60% of the whole region) with a National Cancer Plan. The following countries have newly adopted plans: Suriname, Ecuador, Dominican Republic, Trinidad and Tobago, Puerto Rico, Peru, El Salvador, and Colombia.
In addition, Latin America—most notably, Brazil and Argentina—has begun to address the shortage of cancer specialists.
Brazil has shown an increase of 77% in oncologists since 2011 (from 1457 to 2577). Concurrently, the number of hematologists has also increased by 40% (from 1420 in 2011 to 1985 in 2015), and that of radiotherapists by 12% (from 444 in 2011 to 497 in 2015). These rises are in the context of an 11% increase in cancer cases in Brazil (from 518,000 new cases in 2012 to 576,000 in 2014).
Many countries across Latin America have signed on to the Global Action Plan for the Prevention and Control of Non-Communicable Diseases 2013-2020, endorsed by the WHO, which aims to achieve a 25% reduction in premature mortality from non-communicable diseases (including cancer) by 2025.
The Colombian Ministry of Health and Social Protection has expanded its social insurance program to cover all types of cancer.
Since January 2014, the administration of chemotherapy and radiation treatments is free of charge in Uruguay.
The Atlas of Palliative Care was published in Latin America, which revealed a growth of more than 400% in the number of palliative services since 2006.
Room for improvement
The report indicates that the following issues are still problems in Latin America.
Compared with high-income countries, Latin America in 2015 remains behind in terms of public expenditure on health and cancer care.
Argentina and Mexico spend around 6% of their gross national product on healthcare, compared to 9% for the UK, 11% for Germany, and 17% for the US, which reflects a gap between Latin American and other countries not only proportionately but also in terms of absolute dollars. Only Brazil, at 9%, is close to the proportion spent in high-income countries.
In Latin America, only Brazil, Cuba, Costa Rica, and Uruguay are considered to have integration of social security and public insurance, and only Brazil, Cuba, and Costa Rica can be judged to have universal healthcare.
Many countries still have no specific training in palliative care (including Bolivia, El Salvador, Honduras, and Nicaragua).
Additionally, data from 2002 showed that Latin America accounted for less than 1% of the world’s opioid drug consumption for pain relief. Consumption of strong opioids still lags behind developed countries today, with no Latin American country exceeding 15 mg/capita per year.
Under-implementation of new technologies has not improved substantially since the previous Lancet Oncology Commission in 2013. There are a few exceptions, however, such as PET scanning technology improvements in Uruguay.
Pharmaceutical trials for expensive new anticancer therapies are largely unhelpful to most patients in Latin America. Patients participating in trials of expensive new anticancer therapies sometimes cannot complete treatment once their trial ends, and the trials often do not lead to approval in these regions.
There are often geographical disparities where most cancer specialists are located in major hospitals in big cities, requiring patients from rural and remote areas to travel far distances to these hospitals for cancer care.
In addition, waiting times in these centers can be unacceptably long, with reports from Mexico and Brazil describing median waiting times of 7 months or more for patients with breast cancer from symptomatic presentation to initial treatment.
Better cancer registries are desperately needed in all Latin American countries to more accurately quantify the cancer burden in the region and the resources required to combat it, according to the report. ![]()

patient and her father
Photo by Rhoda Baer
Despite progress made in cancer care in Latin America in the last 2 years, substantial barriers remain to ensure optimal clinical management, according to a report commissioned by The Lancet Oncology.
The report, an update from a report published in 2013, details a number of improvements in cancer care in Latin America, either specifically related to cancer or to general healthcare initiatives that will also benefit cancer patients.
However, the updated report also suggests that major changes are needed in many areas to increase the standard of cancer care in Latin America.
Progress made
According to the report, progress has been made in the following areas.
The proportion of people in Latin America affiliated with any kind of health insurance program grew from 46% to 60% between 2008 and 2013.
For 2014, the World Health Organization (WHO) reported an 8% increase in the number of countries (60% of the whole region) with a National Cancer Plan. The following countries have newly adopted plans: Suriname, Ecuador, Dominican Republic, Trinidad and Tobago, Puerto Rico, Peru, El Salvador, and Colombia.
In addition, Latin America—most notably, Brazil and Argentina—has begun to address the shortage of cancer specialists.
Brazil has shown an increase of 77% in oncologists since 2011 (from 1457 to 2577). Concurrently, the number of hematologists has also increased by 40% (from 1420 in 2011 to 1985 in 2015), and that of radiotherapists by 12% (from 444 in 2011 to 497 in 2015). These rises are in the context of an 11% increase in cancer cases in Brazil (from 518,000 new cases in 2012 to 576,000 in 2014).
Many countries across Latin America have signed on to the Global Action Plan for the Prevention and Control of Non-Communicable Diseases 2013-2020, endorsed by the WHO, which aims to achieve a 25% reduction in premature mortality from non-communicable diseases (including cancer) by 2025.
The Colombian Ministry of Health and Social Protection has expanded its social insurance program to cover all types of cancer.
Since January 2014, the administration of chemotherapy and radiation treatments is free of charge in Uruguay.
The Atlas of Palliative Care was published in Latin America, which revealed a growth of more than 400% in the number of palliative services since 2006.
Room for improvement
The report indicates that the following issues are still problems in Latin America.
Compared with high-income countries, Latin America in 2015 remains behind in terms of public expenditure on health and cancer care.
Argentina and Mexico spend around 6% of their gross national product on healthcare, compared to 9% for the UK, 11% for Germany, and 17% for the US, which reflects a gap between Latin American and other countries not only proportionately but also in terms of absolute dollars. Only Brazil, at 9%, is close to the proportion spent in high-income countries.
In Latin America, only Brazil, Cuba, Costa Rica, and Uruguay are considered to have integration of social security and public insurance, and only Brazil, Cuba, and Costa Rica can be judged to have universal healthcare.
Many countries still have no specific training in palliative care (including Bolivia, El Salvador, Honduras, and Nicaragua).
Additionally, data from 2002 showed that Latin America accounted for less than 1% of the world’s opioid drug consumption for pain relief. Consumption of strong opioids still lags behind developed countries today, with no Latin American country exceeding 15 mg/capita per year.
Under-implementation of new technologies has not improved substantially since the previous Lancet Oncology Commission in 2013. There are a few exceptions, however, such as PET scanning technology improvements in Uruguay.
Pharmaceutical trials for expensive new anticancer therapies are largely unhelpful to most patients in Latin America. Patients participating in trials of expensive new anticancer therapies sometimes cannot complete treatment once their trial ends, and the trials often do not lead to approval in these regions.
There are often geographical disparities where most cancer specialists are located in major hospitals in big cities, requiring patients from rural and remote areas to travel far distances to these hospitals for cancer care.
In addition, waiting times in these centers can be unacceptably long, with reports from Mexico and Brazil describing median waiting times of 7 months or more for patients with breast cancer from symptomatic presentation to initial treatment.
Better cancer registries are desperately needed in all Latin American countries to more accurately quantify the cancer burden in the region and the resources required to combat it, according to the report. ![]()

patient and her father
Photo by Rhoda Baer
Despite progress made in cancer care in Latin America in the last 2 years, substantial barriers remain to ensure optimal clinical management, according to a report commissioned by The Lancet Oncology.
The report, an update from a report published in 2013, details a number of improvements in cancer care in Latin America, either specifically related to cancer or to general healthcare initiatives that will also benefit cancer patients.
However, the updated report also suggests that major changes are needed in many areas to increase the standard of cancer care in Latin America.
Progress made
According to the report, progress has been made in the following areas.
The proportion of people in Latin America affiliated with any kind of health insurance program grew from 46% to 60% between 2008 and 2013.
For 2014, the World Health Organization (WHO) reported an 8% increase in the number of countries (60% of the whole region) with a National Cancer Plan. The following countries have newly adopted plans: Suriname, Ecuador, Dominican Republic, Trinidad and Tobago, Puerto Rico, Peru, El Salvador, and Colombia.
In addition, Latin America—most notably, Brazil and Argentina—has begun to address the shortage of cancer specialists.
Brazil has shown an increase of 77% in oncologists since 2011 (from 1457 to 2577). Concurrently, the number of hematologists has also increased by 40% (from 1420 in 2011 to 1985 in 2015), and that of radiotherapists by 12% (from 444 in 2011 to 497 in 2015). These rises are in the context of an 11% increase in cancer cases in Brazil (from 518,000 new cases in 2012 to 576,000 in 2014).
Many countries across Latin America have signed on to the Global Action Plan for the Prevention and Control of Non-Communicable Diseases 2013-2020, endorsed by the WHO, which aims to achieve a 25% reduction in premature mortality from non-communicable diseases (including cancer) by 2025.
The Colombian Ministry of Health and Social Protection has expanded its social insurance program to cover all types of cancer.
Since January 2014, the administration of chemotherapy and radiation treatments is free of charge in Uruguay.
The Atlas of Palliative Care was published in Latin America, which revealed a growth of more than 400% in the number of palliative services since 2006.
Room for improvement
The report indicates that the following issues are still problems in Latin America.
Compared with high-income countries, Latin America in 2015 remains behind in terms of public expenditure on health and cancer care.
Argentina and Mexico spend around 6% of their gross national product on healthcare, compared to 9% for the UK, 11% for Germany, and 17% for the US, which reflects a gap between Latin American and other countries not only proportionately but also in terms of absolute dollars. Only Brazil, at 9%, is close to the proportion spent in high-income countries.
In Latin America, only Brazil, Cuba, Costa Rica, and Uruguay are considered to have integration of social security and public insurance, and only Brazil, Cuba, and Costa Rica can be judged to have universal healthcare.
Many countries still have no specific training in palliative care (including Bolivia, El Salvador, Honduras, and Nicaragua).
Additionally, data from 2002 showed that Latin America accounted for less than 1% of the world’s opioid drug consumption for pain relief. Consumption of strong opioids still lags behind developed countries today, with no Latin American country exceeding 15 mg/capita per year.
Under-implementation of new technologies has not improved substantially since the previous Lancet Oncology Commission in 2013. There are a few exceptions, however, such as PET scanning technology improvements in Uruguay.
Pharmaceutical trials for expensive new anticancer therapies are largely unhelpful to most patients in Latin America. Patients participating in trials of expensive new anticancer therapies sometimes cannot complete treatment once their trial ends, and the trials often do not lead to approval in these regions.
There are often geographical disparities where most cancer specialists are located in major hospitals in big cities, requiring patients from rural and remote areas to travel far distances to these hospitals for cancer care.
In addition, waiting times in these centers can be unacceptably long, with reports from Mexico and Brazil describing median waiting times of 7 months or more for patients with breast cancer from symptomatic presentation to initial treatment.
Better cancer registries are desperately needed in all Latin American countries to more accurately quantify the cancer burden in the region and the resources required to combat it, according to the report. ![]()
The search continues for additional targets in CLL
showing CLL
Image by Mary Ann Thompson
NEW YORK—Despite enormous advances in therapies for chronic lymphocytic leukemia (CLL) that target the B-cell receptor (BCR) signaling pathway, there is still room for improvement, according to investigators at the Mayo Clinic.
Bruton’s tyrosine kinase (BTK) and phosphoinositide-3 kinase delta (PI3Kδ) inhibitors are major players in mediating BCR signaling, yet both have off-target effects.
“These agents are not curative, and resistance develops,” explained Neil Kay, MD, of the Mayo Clinic in Rochester, Minnesota.
He described the Axl receptor tyrosine kinase and its inhibitor, TP-0903, at Lymphoma & Myeloma 2015, and discussed how it may be another promising target for CLL therapy.
Pros and cons of current therapies
Ibrutinib, a potent, irreversible, covalent inhibitor of BTK, inhibits interleukin 2 kinase, an essential enzyme in Th2 T cells.
“The potential benefit of this,” Dr Kay said, “is it shifts the balance between Th1 and Th2 T cells and potentially enhances antitumor immune responses.”
However, ibrutinib may cause off-target effects, including defects of platelet function, atrial fibrillation probably related to the inhibition of cardiac PI3K-AKT signaling, and decreased efficacy of anti-CD20 antibodies as mediated by natural killer cells.
In addition, long-term exposure to ibrutinib can induce signal mutations associated with resistance.
Idelalisib, a reversible inhibitor of the delta isoform of PI3K, modulates malignant B-cell signaling and inhibits the chemokines CCL3 and 4. It does not inhibit antibody-dependent cell-mediated cytotoxicity mediated by anti-CD20 antibodies, and it may stimulate antitumor responses.
However, idelalisib may also increase the incidence of diarrhea and colitis and can cause transaminitis and pneumonitis.
Axl receptor tyrosine kinase
So Dr Kay and fellow researchers explored whether CLL B cells express other active receptor tyrosine kinases (RTKs), and if so, what their functional implication is in CLL B-cell survival.
And what they detected is active Axl RTK and basic fibroblast growth factor receptor 3 (FGFR3) RTK in CLL B cells. The human Axl gene, a member of the TAM family of RTKs, is located on chromosome 19q13.2 and encodes a protein weighing 100–140 kD.
When Axl is activated, it initiates various signaling pathways, including cell survival, proliferation, apoptosis inhibition, migration, cell adhesion, and cytokine production. It does this through interactions with a number of signaling molecules, including PI3K and phospholipase C γ2 (PLCγ2), among others.
Most important, Axl is overexpressed in a number of human malignancies, including acute myeloid leukemia, and is associated with poor survivorship.
The research team immunoprecipitated Axl RTK from CLL B-cell lysates and examined them for co-localization by Western blot for the proteins PI3K, c-Src, Syk, PLCγ2, ZAP-70, and Lyn.
“What we think currently is that Axl provides a docking site for these key signaling molecules,” Dr Kay said.
The team found that, by inhibiting Axl with TP-0903, they were able to induce robust apoptosis in CLL B cells, including those from high-risk 17p– and 11q– CLL. They also observed that Axl inhibition resulted in significant reduction of the anti-apoptotic proteins Bcl-2, XIAP, and Mcl-1 and upregulation of the pro-apoptotic protein BIM in CLL B cells.
They then tested the BTK inhibitors ibrutinib and TP-4216 with and without the Axl inhibitor TP-0903 and found that concurrent administration of TP-0903 with the reversible BTK inhibitor TP-4216 had additive effects on apoptosis. This was not the case when it was added to ibrutinib.
“There was much more dramatic upregulation with the reversible BTK inhibitor,” Dr Kay emphasized.
He said Axl inhibition is a therapeutic opportunity in that these inhibitors are orally bioavailable and would be candidates for clinical testing. These inhibitors may minimize drug resistance and prevent the emergence of Richter’s transformation, he added.
The researchers received TP-0903 from Tolero Pharmaceuticals. ![]()
showing CLL
Image by Mary Ann Thompson
NEW YORK—Despite enormous advances in therapies for chronic lymphocytic leukemia (CLL) that target the B-cell receptor (BCR) signaling pathway, there is still room for improvement, according to investigators at the Mayo Clinic.
Bruton’s tyrosine kinase (BTK) and phosphoinositide-3 kinase delta (PI3Kδ) inhibitors are major players in mediating BCR signaling, yet both have off-target effects.
“These agents are not curative, and resistance develops,” explained Neil Kay, MD, of the Mayo Clinic in Rochester, Minnesota.
He described the Axl receptor tyrosine kinase and its inhibitor, TP-0903, at Lymphoma & Myeloma 2015, and discussed how it may be another promising target for CLL therapy.
Pros and cons of current therapies
Ibrutinib, a potent, irreversible, covalent inhibitor of BTK, inhibits interleukin 2 kinase, an essential enzyme in Th2 T cells.
“The potential benefit of this,” Dr Kay said, “is it shifts the balance between Th1 and Th2 T cells and potentially enhances antitumor immune responses.”
However, ibrutinib may cause off-target effects, including defects of platelet function, atrial fibrillation probably related to the inhibition of cardiac PI3K-AKT signaling, and decreased efficacy of anti-CD20 antibodies as mediated by natural killer cells.
In addition, long-term exposure to ibrutinib can induce signal mutations associated with resistance.
Idelalisib, a reversible inhibitor of the delta isoform of PI3K, modulates malignant B-cell signaling and inhibits the chemokines CCL3 and 4. It does not inhibit antibody-dependent cell-mediated cytotoxicity mediated by anti-CD20 antibodies, and it may stimulate antitumor responses.
However, idelalisib may also increase the incidence of diarrhea and colitis and can cause transaminitis and pneumonitis.
Axl receptor tyrosine kinase
So Dr Kay and fellow researchers explored whether CLL B cells express other active receptor tyrosine kinases (RTKs), and if so, what their functional implication is in CLL B-cell survival.
And what they detected is active Axl RTK and basic fibroblast growth factor receptor 3 (FGFR3) RTK in CLL B cells. The human Axl gene, a member of the TAM family of RTKs, is located on chromosome 19q13.2 and encodes a protein weighing 100–140 kD.
When Axl is activated, it initiates various signaling pathways, including cell survival, proliferation, apoptosis inhibition, migration, cell adhesion, and cytokine production. It does this through interactions with a number of signaling molecules, including PI3K and phospholipase C γ2 (PLCγ2), among others.
Most important, Axl is overexpressed in a number of human malignancies, including acute myeloid leukemia, and is associated with poor survivorship.
The research team immunoprecipitated Axl RTK from CLL B-cell lysates and examined them for co-localization by Western blot for the proteins PI3K, c-Src, Syk, PLCγ2, ZAP-70, and Lyn.
“What we think currently is that Axl provides a docking site for these key signaling molecules,” Dr Kay said.
The team found that, by inhibiting Axl with TP-0903, they were able to induce robust apoptosis in CLL B cells, including those from high-risk 17p– and 11q– CLL. They also observed that Axl inhibition resulted in significant reduction of the anti-apoptotic proteins Bcl-2, XIAP, and Mcl-1 and upregulation of the pro-apoptotic protein BIM in CLL B cells.
They then tested the BTK inhibitors ibrutinib and TP-4216 with and without the Axl inhibitor TP-0903 and found that concurrent administration of TP-0903 with the reversible BTK inhibitor TP-4216 had additive effects on apoptosis. This was not the case when it was added to ibrutinib.
“There was much more dramatic upregulation with the reversible BTK inhibitor,” Dr Kay emphasized.
He said Axl inhibition is a therapeutic opportunity in that these inhibitors are orally bioavailable and would be candidates for clinical testing. These inhibitors may minimize drug resistance and prevent the emergence of Richter’s transformation, he added.
The researchers received TP-0903 from Tolero Pharmaceuticals. ![]()
showing CLL
Image by Mary Ann Thompson
NEW YORK—Despite enormous advances in therapies for chronic lymphocytic leukemia (CLL) that target the B-cell receptor (BCR) signaling pathway, there is still room for improvement, according to investigators at the Mayo Clinic.
Bruton’s tyrosine kinase (BTK) and phosphoinositide-3 kinase delta (PI3Kδ) inhibitors are major players in mediating BCR signaling, yet both have off-target effects.
“These agents are not curative, and resistance develops,” explained Neil Kay, MD, of the Mayo Clinic in Rochester, Minnesota.
He described the Axl receptor tyrosine kinase and its inhibitor, TP-0903, at Lymphoma & Myeloma 2015, and discussed how it may be another promising target for CLL therapy.
Pros and cons of current therapies
Ibrutinib, a potent, irreversible, covalent inhibitor of BTK, inhibits interleukin 2 kinase, an essential enzyme in Th2 T cells.
“The potential benefit of this,” Dr Kay said, “is it shifts the balance between Th1 and Th2 T cells and potentially enhances antitumor immune responses.”
However, ibrutinib may cause off-target effects, including defects of platelet function, atrial fibrillation probably related to the inhibition of cardiac PI3K-AKT signaling, and decreased efficacy of anti-CD20 antibodies as mediated by natural killer cells.
In addition, long-term exposure to ibrutinib can induce signal mutations associated with resistance.
Idelalisib, a reversible inhibitor of the delta isoform of PI3K, modulates malignant B-cell signaling and inhibits the chemokines CCL3 and 4. It does not inhibit antibody-dependent cell-mediated cytotoxicity mediated by anti-CD20 antibodies, and it may stimulate antitumor responses.
However, idelalisib may also increase the incidence of diarrhea and colitis and can cause transaminitis and pneumonitis.
Axl receptor tyrosine kinase
So Dr Kay and fellow researchers explored whether CLL B cells express other active receptor tyrosine kinases (RTKs), and if so, what their functional implication is in CLL B-cell survival.
And what they detected is active Axl RTK and basic fibroblast growth factor receptor 3 (FGFR3) RTK in CLL B cells. The human Axl gene, a member of the TAM family of RTKs, is located on chromosome 19q13.2 and encodes a protein weighing 100–140 kD.
When Axl is activated, it initiates various signaling pathways, including cell survival, proliferation, apoptosis inhibition, migration, cell adhesion, and cytokine production. It does this through interactions with a number of signaling molecules, including PI3K and phospholipase C γ2 (PLCγ2), among others.
Most important, Axl is overexpressed in a number of human malignancies, including acute myeloid leukemia, and is associated with poor survivorship.
The research team immunoprecipitated Axl RTK from CLL B-cell lysates and examined them for co-localization by Western blot for the proteins PI3K, c-Src, Syk, PLCγ2, ZAP-70, and Lyn.
“What we think currently is that Axl provides a docking site for these key signaling molecules,” Dr Kay said.
The team found that, by inhibiting Axl with TP-0903, they were able to induce robust apoptosis in CLL B cells, including those from high-risk 17p– and 11q– CLL. They also observed that Axl inhibition resulted in significant reduction of the anti-apoptotic proteins Bcl-2, XIAP, and Mcl-1 and upregulation of the pro-apoptotic protein BIM in CLL B cells.
They then tested the BTK inhibitors ibrutinib and TP-4216 with and without the Axl inhibitor TP-0903 and found that concurrent administration of TP-0903 with the reversible BTK inhibitor TP-4216 had additive effects on apoptosis. This was not the case when it was added to ibrutinib.
“There was much more dramatic upregulation with the reversible BTK inhibitor,” Dr Kay emphasized.
He said Axl inhibition is a therapeutic opportunity in that these inhibitors are orally bioavailable and would be candidates for clinical testing. These inhibitors may minimize drug resistance and prevent the emergence of Richter’s transformation, he added.
The researchers received TP-0903 from Tolero Pharmaceuticals. ![]()
New test could help fight leukemia

Image courtesy of NIAID
Researchers say they have developed a test that can reveal how the immune system would respond to vaccines for leukemia.
To conduct this test, cancer-specific-proteins are spotted onto a microscope slide.
They are then incubated with a patient blood sample to show whether the immune system can recognize the proteins.
The researchers believe this test could inform immunotherapy trial development and eventually direct the treatment of leukemia.
They described the test in PLOS ONE.
The team explained that cellular arrays using peptide-MHC (pMHC) tetramers allow the simultaneous detection of different antigen-specific T-cell populations that are naturally circulating in leukemia patients and healthy individuals.
The researchers developed a pMHC array to detect CD8+ T-cell populations in leukemia patients that recognize epitopes within viral antigens and leukemia antigens.
Experiments showed this test was at least as sensitive as flow cytometry.
The pMHC array successfully identified more than 40 T-cell populations. It identified T cells that recognized various tumor antigen epitopes in patients with acute myeloid leukemia and acute lymphoblastic leukemia.
“This [test] would allow us to know how good a patients’ immune system is and potentially which proteins their immune system will react to, allowing us to prioritize which proteins we use to develop anticancer vaccines,” said study author Barbara Guinn, PhD, of the University of Southampton in the UK.
“In the future, we may be able to monitor patient immune responses as they are treated in clinical trials, helping us to direct the immune system more efficiently against cancer cells.”
Dr Guinn has spent a large part of her career investigating the differences between cancer cells and normal cells in terms of the proteins they make. She has been able to identify a number of proteins that are overexpressed in tumor cells but not healthy cells.
“Some of these proteins act as biomarkers for patient survival,” she said, “and some of them have helped us understand more about how cancer develops in subgroups of patients with leukemia.” ![]()

Image courtesy of NIAID
Researchers say they have developed a test that can reveal how the immune system would respond to vaccines for leukemia.
To conduct this test, cancer-specific-proteins are spotted onto a microscope slide.
They are then incubated with a patient blood sample to show whether the immune system can recognize the proteins.
The researchers believe this test could inform immunotherapy trial development and eventually direct the treatment of leukemia.
They described the test in PLOS ONE.
The team explained that cellular arrays using peptide-MHC (pMHC) tetramers allow the simultaneous detection of different antigen-specific T-cell populations that are naturally circulating in leukemia patients and healthy individuals.
The researchers developed a pMHC array to detect CD8+ T-cell populations in leukemia patients that recognize epitopes within viral antigens and leukemia antigens.
Experiments showed this test was at least as sensitive as flow cytometry.
The pMHC array successfully identified more than 40 T-cell populations. It identified T cells that recognized various tumor antigen epitopes in patients with acute myeloid leukemia and acute lymphoblastic leukemia.
“This [test] would allow us to know how good a patients’ immune system is and potentially which proteins their immune system will react to, allowing us to prioritize which proteins we use to develop anticancer vaccines,” said study author Barbara Guinn, PhD, of the University of Southampton in the UK.
“In the future, we may be able to monitor patient immune responses as they are treated in clinical trials, helping us to direct the immune system more efficiently against cancer cells.”
Dr Guinn has spent a large part of her career investigating the differences between cancer cells and normal cells in terms of the proteins they make. She has been able to identify a number of proteins that are overexpressed in tumor cells but not healthy cells.
“Some of these proteins act as biomarkers for patient survival,” she said, “and some of them have helped us understand more about how cancer develops in subgroups of patients with leukemia.” ![]()

Image courtesy of NIAID
Researchers say they have developed a test that can reveal how the immune system would respond to vaccines for leukemia.
To conduct this test, cancer-specific-proteins are spotted onto a microscope slide.
They are then incubated with a patient blood sample to show whether the immune system can recognize the proteins.
The researchers believe this test could inform immunotherapy trial development and eventually direct the treatment of leukemia.
They described the test in PLOS ONE.
The team explained that cellular arrays using peptide-MHC (pMHC) tetramers allow the simultaneous detection of different antigen-specific T-cell populations that are naturally circulating in leukemia patients and healthy individuals.
The researchers developed a pMHC array to detect CD8+ T-cell populations in leukemia patients that recognize epitopes within viral antigens and leukemia antigens.
Experiments showed this test was at least as sensitive as flow cytometry.
The pMHC array successfully identified more than 40 T-cell populations. It identified T cells that recognized various tumor antigen epitopes in patients with acute myeloid leukemia and acute lymphoblastic leukemia.
“This [test] would allow us to know how good a patients’ immune system is and potentially which proteins their immune system will react to, allowing us to prioritize which proteins we use to develop anticancer vaccines,” said study author Barbara Guinn, PhD, of the University of Southampton in the UK.
“In the future, we may be able to monitor patient immune responses as they are treated in clinical trials, helping us to direct the immune system more efficiently against cancer cells.”
Dr Guinn has spent a large part of her career investigating the differences between cancer cells and normal cells in terms of the proteins they make. She has been able to identify a number of proteins that are overexpressed in tumor cells but not healthy cells.
“Some of these proteins act as biomarkers for patient survival,” she said, “and some of them have helped us understand more about how cancer develops in subgroups of patients with leukemia.” ![]()
Team aims to inhibit Notch safely

Photo courtesy of the
University of Michigan
A new study suggests a potential way to block one of the most common cancer-causing genes without causing severe side effects.
The Notch gene plays a role in many cancers, and it’s the most common cancer-causing gene in T-cell acute lymphoblastic leukemia (T-ALL).
About 60% of children and adults with T-ALL harbor a Notch mutation.
Unfortunately, drugs that inhibit Notch can cause serious side effects, such as skin cancers.
Now, investigators have discovered a potential new target to inhibit Notch without the toxic effects.
They found that a protein called Zmiz1 sticks to Notch, prompting the gene to turn on its cancer function. But Zmiz1 does not impact normal, healthy Notch functions.
“Notch controls the genes that cause cancer, but it’s also important for normal health,” said Mark Chiang, MD, PhD, of the University of Michigan in Ann Arbor.
“The challenge is to knock out the cancer function of Notch but preserve its normal function. If you unstick Zmiz1 from Notch, the cancer cells die. And Zmiz1 seems to be selective in turning on the cancer functions of Notch.”
Dr Chiang and his colleagues found that mice lived longer when Zmiz1 was deleted. The mice had normal body weight and no severe side effects from Zmiz1 deletion.
The investigators reported these results in Immunity.
“Our goal is to develop a drug to sit right between Notch and Zmiz1 that could break apart the bond,” Dr Chiang said. “We think this would block the Notch cancer pathway without causing toxic side effects, like we see with current Notch inhibitors.”
He noted that a majority of children with T-ALL are cured, but about 20% will relapse. Those children face a grim prognosis.
“We need to develop therapies against Notch to help kids with relapsed cancer and to cure kids with fewer toxicities or long-term effects,” Dr Chiang said. “Our current treatments may often be curative, but there can be a huge price to pay in late effects.”
To further this research, Dr Chiang and his colleagues plan to use X-ray crystallography to create a 3-dimensional image of Notch and Zmiz1 in an effort to understand how they are sticking together. This could help the team to design a drug to separate the proteins. ![]()

Photo courtesy of the
University of Michigan
A new study suggests a potential way to block one of the most common cancer-causing genes without causing severe side effects.
The Notch gene plays a role in many cancers, and it’s the most common cancer-causing gene in T-cell acute lymphoblastic leukemia (T-ALL).
About 60% of children and adults with T-ALL harbor a Notch mutation.
Unfortunately, drugs that inhibit Notch can cause serious side effects, such as skin cancers.
Now, investigators have discovered a potential new target to inhibit Notch without the toxic effects.
They found that a protein called Zmiz1 sticks to Notch, prompting the gene to turn on its cancer function. But Zmiz1 does not impact normal, healthy Notch functions.
“Notch controls the genes that cause cancer, but it’s also important for normal health,” said Mark Chiang, MD, PhD, of the University of Michigan in Ann Arbor.
“The challenge is to knock out the cancer function of Notch but preserve its normal function. If you unstick Zmiz1 from Notch, the cancer cells die. And Zmiz1 seems to be selective in turning on the cancer functions of Notch.”
Dr Chiang and his colleagues found that mice lived longer when Zmiz1 was deleted. The mice had normal body weight and no severe side effects from Zmiz1 deletion.
The investigators reported these results in Immunity.
“Our goal is to develop a drug to sit right between Notch and Zmiz1 that could break apart the bond,” Dr Chiang said. “We think this would block the Notch cancer pathway without causing toxic side effects, like we see with current Notch inhibitors.”
He noted that a majority of children with T-ALL are cured, but about 20% will relapse. Those children face a grim prognosis.
“We need to develop therapies against Notch to help kids with relapsed cancer and to cure kids with fewer toxicities or long-term effects,” Dr Chiang said. “Our current treatments may often be curative, but there can be a huge price to pay in late effects.”
To further this research, Dr Chiang and his colleagues plan to use X-ray crystallography to create a 3-dimensional image of Notch and Zmiz1 in an effort to understand how they are sticking together. This could help the team to design a drug to separate the proteins. ![]()

Photo courtesy of the
University of Michigan
A new study suggests a potential way to block one of the most common cancer-causing genes without causing severe side effects.
The Notch gene plays a role in many cancers, and it’s the most common cancer-causing gene in T-cell acute lymphoblastic leukemia (T-ALL).
About 60% of children and adults with T-ALL harbor a Notch mutation.
Unfortunately, drugs that inhibit Notch can cause serious side effects, such as skin cancers.
Now, investigators have discovered a potential new target to inhibit Notch without the toxic effects.
They found that a protein called Zmiz1 sticks to Notch, prompting the gene to turn on its cancer function. But Zmiz1 does not impact normal, healthy Notch functions.
“Notch controls the genes that cause cancer, but it’s also important for normal health,” said Mark Chiang, MD, PhD, of the University of Michigan in Ann Arbor.
“The challenge is to knock out the cancer function of Notch but preserve its normal function. If you unstick Zmiz1 from Notch, the cancer cells die. And Zmiz1 seems to be selective in turning on the cancer functions of Notch.”
Dr Chiang and his colleagues found that mice lived longer when Zmiz1 was deleted. The mice had normal body weight and no severe side effects from Zmiz1 deletion.
The investigators reported these results in Immunity.
“Our goal is to develop a drug to sit right between Notch and Zmiz1 that could break apart the bond,” Dr Chiang said. “We think this would block the Notch cancer pathway without causing toxic side effects, like we see with current Notch inhibitors.”
He noted that a majority of children with T-ALL are cured, but about 20% will relapse. Those children face a grim prognosis.
“We need to develop therapies against Notch to help kids with relapsed cancer and to cure kids with fewer toxicities or long-term effects,” Dr Chiang said. “Our current treatments may often be curative, but there can be a huge price to pay in late effects.”
To further this research, Dr Chiang and his colleagues plan to use X-ray crystallography to create a 3-dimensional image of Notch and Zmiz1 in an effort to understand how they are sticking together. This could help the team to design a drug to separate the proteins.
How a cancer diagnosis affects income

receiving treatment
Photo by Rhoda Baer
A new study indicates that when American adults are diagnosed with
cancer, they experience significant decreases in the probability of
working, in the number of hours they work, and correspondingly, in their
incomes.
Additionally, these effects appear to be more pronounced among men than women.
Anna Zajacova, PhD, of the University of Wyoming in Laramie, and her colleagues reported these findings in Cancer.
The researchers analyzed data from the Panel Study of Income Dynamics, a nationally representative, prospective, population-based, observational study with individual and family level economic information. The data spanned the period from 1999 to 2009.
The team used models to estimate the impact of cancer on employment, hours worked, individual income, and total family income.
The results showed that, after a cancer diagnosis, the probability of a patient being employed dropped by almost 10 percentage points, and hours worked declined by up to 200 hours, or about 5 weeks of full-time work, in the first year.
Annual labor market earnings dropped almost 40% within 2 years of diagnosis, and they remained lower than before diagnosis. Total family income declined by 20%, although it recovered within 4 years of cancer diagnosis.
These effects were primarily driven by losses among male cancer survivors. For women diagnosed with cancer, the losses were largely not statistically significant.
“Fifteen million American adults are cancer survivors, and American families need economic support while they are dealing with the rigors of cancer treatment,” Dr Zajacova said.
“Our paper suggests that families where an adult—especially a working-age male—is diagnosed with cancer suffer short-term and long-term declines in their economic well-being. We need to improve workplace and insurance safety nets so families can focus on dealing with the cancer treatment rather than deal with the financial and employment fallout.”

receiving treatment
Photo by Rhoda Baer
A new study indicates that when American adults are diagnosed with
cancer, they experience significant decreases in the probability of
working, in the number of hours they work, and correspondingly, in their
incomes.
Additionally, these effects appear to be more pronounced among men than women.
Anna Zajacova, PhD, of the University of Wyoming in Laramie, and her colleagues reported these findings in Cancer.
The researchers analyzed data from the Panel Study of Income Dynamics, a nationally representative, prospective, population-based, observational study with individual and family level economic information. The data spanned the period from 1999 to 2009.
The team used models to estimate the impact of cancer on employment, hours worked, individual income, and total family income.
The results showed that, after a cancer diagnosis, the probability of a patient being employed dropped by almost 10 percentage points, and hours worked declined by up to 200 hours, or about 5 weeks of full-time work, in the first year.
Annual labor market earnings dropped almost 40% within 2 years of diagnosis, and they remained lower than before diagnosis. Total family income declined by 20%, although it recovered within 4 years of cancer diagnosis.
These effects were primarily driven by losses among male cancer survivors. For women diagnosed with cancer, the losses were largely not statistically significant.
“Fifteen million American adults are cancer survivors, and American families need economic support while they are dealing with the rigors of cancer treatment,” Dr Zajacova said.
“Our paper suggests that families where an adult—especially a working-age male—is diagnosed with cancer suffer short-term and long-term declines in their economic well-being. We need to improve workplace and insurance safety nets so families can focus on dealing with the cancer treatment rather than deal with the financial and employment fallout.”

receiving treatment
Photo by Rhoda Baer
A new study indicates that when American adults are diagnosed with
cancer, they experience significant decreases in the probability of
working, in the number of hours they work, and correspondingly, in their
incomes.
Additionally, these effects appear to be more pronounced among men than women.
Anna Zajacova, PhD, of the University of Wyoming in Laramie, and her colleagues reported these findings in Cancer.
The researchers analyzed data from the Panel Study of Income Dynamics, a nationally representative, prospective, population-based, observational study with individual and family level economic information. The data spanned the period from 1999 to 2009.
The team used models to estimate the impact of cancer on employment, hours worked, individual income, and total family income.
The results showed that, after a cancer diagnosis, the probability of a patient being employed dropped by almost 10 percentage points, and hours worked declined by up to 200 hours, or about 5 weeks of full-time work, in the first year.
Annual labor market earnings dropped almost 40% within 2 years of diagnosis, and they remained lower than before diagnosis. Total family income declined by 20%, although it recovered within 4 years of cancer diagnosis.
These effects were primarily driven by losses among male cancer survivors. For women diagnosed with cancer, the losses were largely not statistically significant.
“Fifteen million American adults are cancer survivors, and American families need economic support while they are dealing with the rigors of cancer treatment,” Dr Zajacova said.
“Our paper suggests that families where an adult—especially a working-age male—is diagnosed with cancer suffer short-term and long-term declines in their economic well-being. We need to improve workplace and insurance safety nets so families can focus on dealing with the cancer treatment rather than deal with the financial and employment fallout.”
Group identifies potential target for AML

marrow cells generated by AE
Image courtesy of
The Rockefeller University
Preclinical research has revealed a potential therapeutic target for acute myeloid leukemia (AML)—the histone demethylase JMJD1C.
Investigators found that JMJD1C interacts with RUNX1–RUNX1T1 (formerly AML1-ETO and abbreviated here as AE), a transcription factor generated by the t(8;21) translocation in AML.
However, the team also found that JMJD1C is required for proliferation in many AML cell lines, not just those with AE.
Robert G. Roeder, PhD, of The Rockefeller University in New York, New York, and his colleagues detailed these findings in Genes and Development.
The investigators began this study by searching for proteins that interact with AE, and they identified JMJD1C. To investigate the relationship between JMJD1C and AE, the team explored the broader effects of removing JMJD1C.
“We found that numerous genes were downregulated upon loss of JMJD1C, and the set overlaps significantly with the genes that are normally activated by AE,” said study author Mo Chen, PhD, a researcher in Dr Roeder’s lab.
The investigators also found that AML cells are addicted to the presence of JMJD1C, and, without it, they cannot survive. The team observed an increase in apoptosis when JMJD1C was depleted from Kasumi-1 and SKNO-1 cell lines.
With subsequent experiments, the investigators confirmed that JMJD1C interacts with AE and demonstrated that JMJD1C is required for AE to exert its cancer-promoting effects. But they also found that JMJD1C plays an even broader role in AML.
“We were very surprised to find that JMJD1C is required for the proliferation of other acute myeloid leukemia cell lines, which do not have AE,” Dr Chen said.
The team found that depleting JMJD1C compromised the growth of the following cell lines: Kasumi-1 (AML1-ETO; AML M2), MOLM-13 (MLL-AF9, FLT3ITD; AML M5a), THP-1 (MLL-AF9, NRASmut; AML M5), HNT-34 (BCR-ABL1; AML M4), MV4-11 (MLL-AF4; AML M5), CMK (JAK3A527V; AML M7+ Down’s Syndrome), HEL (AML M6), NOMO-1 (MLL-AF9; AML M5a), NB4 (PML-RARα; AML M3), and HL-60 (MYC amplification; AML M2).
The only cell line that was not affected by depletion of JMJD1C was KG-1 (NRASmut; AML).
To build upon this discovery, the investigators looked for transcription factors aside from AE that might be responsible for JMJD1C addiction. The team found at least 2—LYL1 and HEB—that can recruit JMJD1C to target genes in diseased cells that lack AE, fueling leukemia growth.
The investigators said these results suggest JMJD1C may play a general role in promoting the growth of myeloid leukemias.
“We are excited because this type of general phenomena is an ideal target for drug development,” Dr Roeder said. “Our work will facilitate the development of selective inhibitors against JMJD1C, which is a highly promising therapeutic target for multiple types of leukemia.”

marrow cells generated by AE
Image courtesy of
The Rockefeller University
Preclinical research has revealed a potential therapeutic target for acute myeloid leukemia (AML)—the histone demethylase JMJD1C.
Investigators found that JMJD1C interacts with RUNX1–RUNX1T1 (formerly AML1-ETO and abbreviated here as AE), a transcription factor generated by the t(8;21) translocation in AML.
However, the team also found that JMJD1C is required for proliferation in many AML cell lines, not just those with AE.
Robert G. Roeder, PhD, of The Rockefeller University in New York, New York, and his colleagues detailed these findings in Genes and Development.
The investigators began this study by searching for proteins that interact with AE, and they identified JMJD1C. To investigate the relationship between JMJD1C and AE, the team explored the broader effects of removing JMJD1C.
“We found that numerous genes were downregulated upon loss of JMJD1C, and the set overlaps significantly with the genes that are normally activated by AE,” said study author Mo Chen, PhD, a researcher in Dr Roeder’s lab.
The investigators also found that AML cells are addicted to the presence of JMJD1C, and, without it, they cannot survive. The team observed an increase in apoptosis when JMJD1C was depleted from Kasumi-1 and SKNO-1 cell lines.
With subsequent experiments, the investigators confirmed that JMJD1C interacts with AE and demonstrated that JMJD1C is required for AE to exert its cancer-promoting effects. But they also found that JMJD1C plays an even broader role in AML.
“We were very surprised to find that JMJD1C is required for the proliferation of other acute myeloid leukemia cell lines, which do not have AE,” Dr Chen said.
The team found that depleting JMJD1C compromised the growth of the following cell lines: Kasumi-1 (AML1-ETO; AML M2), MOLM-13 (MLL-AF9, FLT3ITD; AML M5a), THP-1 (MLL-AF9, NRASmut; AML M5), HNT-34 (BCR-ABL1; AML M4), MV4-11 (MLL-AF4; AML M5), CMK (JAK3A527V; AML M7+ Down’s Syndrome), HEL (AML M6), NOMO-1 (MLL-AF9; AML M5a), NB4 (PML-RARα; AML M3), and HL-60 (MYC amplification; AML M2).
The only cell line that was not affected by depletion of JMJD1C was KG-1 (NRASmut; AML).
To build upon this discovery, the investigators looked for transcription factors aside from AE that might be responsible for JMJD1C addiction. The team found at least 2—LYL1 and HEB—that can recruit JMJD1C to target genes in diseased cells that lack AE, fueling leukemia growth.
The investigators said these results suggest JMJD1C may play a general role in promoting the growth of myeloid leukemias.
“We are excited because this type of general phenomena is an ideal target for drug development,” Dr Roeder said. “Our work will facilitate the development of selective inhibitors against JMJD1C, which is a highly promising therapeutic target for multiple types of leukemia.”

marrow cells generated by AE
Image courtesy of
The Rockefeller University
Preclinical research has revealed a potential therapeutic target for acute myeloid leukemia (AML)—the histone demethylase JMJD1C.
Investigators found that JMJD1C interacts with RUNX1–RUNX1T1 (formerly AML1-ETO and abbreviated here as AE), a transcription factor generated by the t(8;21) translocation in AML.
However, the team also found that JMJD1C is required for proliferation in many AML cell lines, not just those with AE.
Robert G. Roeder, PhD, of The Rockefeller University in New York, New York, and his colleagues detailed these findings in Genes and Development.
The investigators began this study by searching for proteins that interact with AE, and they identified JMJD1C. To investigate the relationship between JMJD1C and AE, the team explored the broader effects of removing JMJD1C.
“We found that numerous genes were downregulated upon loss of JMJD1C, and the set overlaps significantly with the genes that are normally activated by AE,” said study author Mo Chen, PhD, a researcher in Dr Roeder’s lab.
The investigators also found that AML cells are addicted to the presence of JMJD1C, and, without it, they cannot survive. The team observed an increase in apoptosis when JMJD1C was depleted from Kasumi-1 and SKNO-1 cell lines.
With subsequent experiments, the investigators confirmed that JMJD1C interacts with AE and demonstrated that JMJD1C is required for AE to exert its cancer-promoting effects. But they also found that JMJD1C plays an even broader role in AML.
“We were very surprised to find that JMJD1C is required for the proliferation of other acute myeloid leukemia cell lines, which do not have AE,” Dr Chen said.
The team found that depleting JMJD1C compromised the growth of the following cell lines: Kasumi-1 (AML1-ETO; AML M2), MOLM-13 (MLL-AF9, FLT3ITD; AML M5a), THP-1 (MLL-AF9, NRASmut; AML M5), HNT-34 (BCR-ABL1; AML M4), MV4-11 (MLL-AF4; AML M5), CMK (JAK3A527V; AML M7+ Down’s Syndrome), HEL (AML M6), NOMO-1 (MLL-AF9; AML M5a), NB4 (PML-RARα; AML M3), and HL-60 (MYC amplification; AML M2).
The only cell line that was not affected by depletion of JMJD1C was KG-1 (NRASmut; AML).
To build upon this discovery, the investigators looked for transcription factors aside from AE that might be responsible for JMJD1C addiction. The team found at least 2—LYL1 and HEB—that can recruit JMJD1C to target genes in diseased cells that lack AE, fueling leukemia growth.
The investigators said these results suggest JMJD1C may play a general role in promoting the growth of myeloid leukemias.
“We are excited because this type of general phenomena is an ideal target for drug development,” Dr Roeder said. “Our work will facilitate the development of selective inhibitors against JMJD1C, which is a highly promising therapeutic target for multiple types of leukemia.”
NCCN unveils 'Evidence Blocks' to facilitate treatment discussions
SAN FRANCISCO – The National Comprehensive Cancer Network (NCCN) has introduced an easy-to-use visual tool called Evidence Blocks to help physicians and patients compare various treatment options and individualize the selection among them.
“This information can serve as a starting point for shared decision making between the patient and health care team based on individual patients’ value systems,” chief executive officer Dr. Robert W. Carlson said at the NCCN Annual Congress: Hematologic Malignancies, where the tool was unveiled in a session and related press conference.
The first two NCCN guidelines to incorporate the Evidence Blocks – those for multiple myeloma and chronic myelogenous leukemia – were released at the same time. The organization hopes to incorporate them into all of its guidelines by early 2017, he said.
Development of the Evidence Blocks
The NCCN developed the Evidence Blocks to address requests from various stakeholders, according to Dr. Carlson. Guideline users wanted to know more about the rationale behind recommended therapies, asked for inclusion of information on costs, and sought an aid that would allow patients to make decisions based on their individual values.
“The patient perception of value is what should be most important to us,” he commented. “But even among patients, the concept of value differs greatly from patient to patient,” based on factors such as age, comorbidities, treatment goals, and health insurance coverage.
Each Evidence Block graphically displays five measures of information on a recommended therapy: efficacy, safety, quality of the evidence supporting the recommendation, consistency of the evidence supporting the recommendation, and affordability. Each column in the block represents one measure.
Blue shading indicates panelists’ average numeric score for the therapy on that measure rounded to the nearest integer, ranging from 1 (least favorable) to 5 (most favorable). Therefore, the more shading a therapy has, the more favorable its score.
The Evidence Blocks are added to the guidelines and aligned vertically on pages. “This display of the information graphically allows for very efficient scanning of multiple options for therapy. Comparisons across several regimens can be done very quickly and intuitively,” Dr. Carlson noted.
“We believe that the presentation of this type of information allows the health care provider and patient to make their own judgments of the value of specific interventions,” he added.
The affordability measure has generated the most discussion among panelists and stakeholders, according to Dr. Carlson. For this measure, panelists estimated the total cost of care for a therapy, including the costs of drugs, administration, required supportive care, toxicity monitoring, and care associated with management of toxicity. Scores range from very expensive to very inexpensive.
“We don’t use a dollar amount. Rather, it’s sort of what’s the total cost to society, if you will, of the medical intervention part of this,” he explained. “It’s important to understand that these estimates are not necessarily what a patient would pay because many patients have insurance programs that cover all of this cost.… However, we felt it was important to give patients as well as providers an estimate of what the overall magnitude of expense is because there are patients who have huge deductibles, there’s the doughnut hole within Medicare, and there are patients who have no insurance.”
The Evidence Blocks may help address a “conspiracy of silence” between physicians and patients when it comes to discussing treatment costs, whereby neither party wants to bring up this thorny issue, according to Dr. Carlson. “The Evidence Blocks demystify the discussion of cost because the affordability issue is there in front of you. So it gives people permission to talk about cost and affordability.”
It should be relatively easy to teach patients to use the Evidence Blocks. “I think you’ll find your patients will actually be interested in this and that they will not have as much difficulty interpreting this as you think they will, because the patient advocacy groups and the patient advocates that we have spoken with about this, they get this almost instantly,” he said.
Oncologist perspective
There is a critical need for tools such as the Evidence Blocks in making treatment decisions today, according to Dr. George Somlo, professor in the department of medical oncology and therapeutics research at the City of Hope Comprehensive Cancer Center in Duarte, Calif., and also a member of the NCCN multiple myeloma and breast cancer guideline panels.
Treatment options for multiple myeloma, as for many cancers, have exploded in the past few decades, he noted. “How do you go from making sense of having two drugs with a very poor outcome predicted to having literally dozens of agents approved and used in combination, and in essence being at the verge of curing patients with multiple myeloma?”
Dr. Somlo agreed that inclusion of costs in the Evidence Blocks would likely be beneficial as a conversation starter, recalling, “I’ve had patients who did not fill their prescription for a potentially curative medication because they were worried about the $2,500 or $3,500 copay.”
Patient-physician discussion will be important when it comes to using information from the new tool, he said. For example, in the NCCN guideline for multiple myeloma, some of the first-line regimens have identical Evidence Blocks; thus, consideration of factors such as comorbidities will become important.
“This kind of evidence-based scoring system can guide that kind of discussion with the patient and can tailor the individual therapeutic regimens,” he concluded.
Patient perspective
Breast cancer survivor Marta Nichols, who is vice president of investor relations at GoDaddy and a member of the California Breast Cancer Research Council based in San Francisco, welcomed the Evidence Blocks as a tool that will allow patients to make more informed decisions according to what matters most to them.
Only 33 years old at diagnosis, she and her husband had just begun to think about starting a family. “So my primary concern coming into my physician’s office was my fertility and what impact the treatment would have on my fertility. Certainly most physicians are concerned with efficacy – they want to see you survive. My concern was not just surviving, but also thriving and being able to give birth to children down the line,” she explained.
Patients today are overwhelmed not only by their cancer diagnosis, but also by the many treatment options and the new emphasis on shared decision making, Ms. Nichols noted. And that’s where the Evidence Blocks can make a difference.
“When I was diagnosed, it would have been hugely helpful for me to have information laid out in this very clear and systematic way… It would have given us the ability to make a much more informed decision,” she commented.
Multiple myeloma survivor Donald B. Orosco, who is president and chief financial officer of Orosco & Associates and owner of Monterey (Calif.) Speed and Sport, agreed, noting that his priorities when given the diagnosis more than two decades ago at age 47 differed somewhat.
“I adopted the feeling early on that I probably wasn’t going to see a cure for the disease in my lifetime, but I could accept that,” he elaborated. “I just said ‘Really, I’m interested in quality-of-life issues. I’d like to see my kids go into high school or possibly college.’ So I adopted [an approach of] trying to find something for me that would keep me alive and give me a relatively comfortable quality of life, that would allow me to continue to race cars or do whatever I had to do.”
Dr. Carlson, Dr. Somlo, Ms. Nichols, and Mr. Orosco disclosed no relevant conflicts of interest.
SAN FRANCISCO – The National Comprehensive Cancer Network (NCCN) has introduced an easy-to-use visual tool called Evidence Blocks to help physicians and patients compare various treatment options and individualize the selection among them.
“This information can serve as a starting point for shared decision making between the patient and health care team based on individual patients’ value systems,” chief executive officer Dr. Robert W. Carlson said at the NCCN Annual Congress: Hematologic Malignancies, where the tool was unveiled in a session and related press conference.
The first two NCCN guidelines to incorporate the Evidence Blocks – those for multiple myeloma and chronic myelogenous leukemia – were released at the same time. The organization hopes to incorporate them into all of its guidelines by early 2017, he said.
Development of the Evidence Blocks
The NCCN developed the Evidence Blocks to address requests from various stakeholders, according to Dr. Carlson. Guideline users wanted to know more about the rationale behind recommended therapies, asked for inclusion of information on costs, and sought an aid that would allow patients to make decisions based on their individual values.
“The patient perception of value is what should be most important to us,” he commented. “But even among patients, the concept of value differs greatly from patient to patient,” based on factors such as age, comorbidities, treatment goals, and health insurance coverage.
Each Evidence Block graphically displays five measures of information on a recommended therapy: efficacy, safety, quality of the evidence supporting the recommendation, consistency of the evidence supporting the recommendation, and affordability. Each column in the block represents one measure.
Blue shading indicates panelists’ average numeric score for the therapy on that measure rounded to the nearest integer, ranging from 1 (least favorable) to 5 (most favorable). Therefore, the more shading a therapy has, the more favorable its score.
The Evidence Blocks are added to the guidelines and aligned vertically on pages. “This display of the information graphically allows for very efficient scanning of multiple options for therapy. Comparisons across several regimens can be done very quickly and intuitively,” Dr. Carlson noted.
“We believe that the presentation of this type of information allows the health care provider and patient to make their own judgments of the value of specific interventions,” he added.
The affordability measure has generated the most discussion among panelists and stakeholders, according to Dr. Carlson. For this measure, panelists estimated the total cost of care for a therapy, including the costs of drugs, administration, required supportive care, toxicity monitoring, and care associated with management of toxicity. Scores range from very expensive to very inexpensive.
“We don’t use a dollar amount. Rather, it’s sort of what’s the total cost to society, if you will, of the medical intervention part of this,” he explained. “It’s important to understand that these estimates are not necessarily what a patient would pay because many patients have insurance programs that cover all of this cost.… However, we felt it was important to give patients as well as providers an estimate of what the overall magnitude of expense is because there are patients who have huge deductibles, there’s the doughnut hole within Medicare, and there are patients who have no insurance.”
The Evidence Blocks may help address a “conspiracy of silence” between physicians and patients when it comes to discussing treatment costs, whereby neither party wants to bring up this thorny issue, according to Dr. Carlson. “The Evidence Blocks demystify the discussion of cost because the affordability issue is there in front of you. So it gives people permission to talk about cost and affordability.”
It should be relatively easy to teach patients to use the Evidence Blocks. “I think you’ll find your patients will actually be interested in this and that they will not have as much difficulty interpreting this as you think they will, because the patient advocacy groups and the patient advocates that we have spoken with about this, they get this almost instantly,” he said.
Oncologist perspective
There is a critical need for tools such as the Evidence Blocks in making treatment decisions today, according to Dr. George Somlo, professor in the department of medical oncology and therapeutics research at the City of Hope Comprehensive Cancer Center in Duarte, Calif., and also a member of the NCCN multiple myeloma and breast cancer guideline panels.
Treatment options for multiple myeloma, as for many cancers, have exploded in the past few decades, he noted. “How do you go from making sense of having two drugs with a very poor outcome predicted to having literally dozens of agents approved and used in combination, and in essence being at the verge of curing patients with multiple myeloma?”
Dr. Somlo agreed that inclusion of costs in the Evidence Blocks would likely be beneficial as a conversation starter, recalling, “I’ve had patients who did not fill their prescription for a potentially curative medication because they were worried about the $2,500 or $3,500 copay.”
Patient-physician discussion will be important when it comes to using information from the new tool, he said. For example, in the NCCN guideline for multiple myeloma, some of the first-line regimens have identical Evidence Blocks; thus, consideration of factors such as comorbidities will become important.
“This kind of evidence-based scoring system can guide that kind of discussion with the patient and can tailor the individual therapeutic regimens,” he concluded.
Patient perspective
Breast cancer survivor Marta Nichols, who is vice president of investor relations at GoDaddy and a member of the California Breast Cancer Research Council based in San Francisco, welcomed the Evidence Blocks as a tool that will allow patients to make more informed decisions according to what matters most to them.
Only 33 years old at diagnosis, she and her husband had just begun to think about starting a family. “So my primary concern coming into my physician’s office was my fertility and what impact the treatment would have on my fertility. Certainly most physicians are concerned with efficacy – they want to see you survive. My concern was not just surviving, but also thriving and being able to give birth to children down the line,” she explained.
Patients today are overwhelmed not only by their cancer diagnosis, but also by the many treatment options and the new emphasis on shared decision making, Ms. Nichols noted. And that’s where the Evidence Blocks can make a difference.
“When I was diagnosed, it would have been hugely helpful for me to have information laid out in this very clear and systematic way… It would have given us the ability to make a much more informed decision,” she commented.
Multiple myeloma survivor Donald B. Orosco, who is president and chief financial officer of Orosco & Associates and owner of Monterey (Calif.) Speed and Sport, agreed, noting that his priorities when given the diagnosis more than two decades ago at age 47 differed somewhat.
“I adopted the feeling early on that I probably wasn’t going to see a cure for the disease in my lifetime, but I could accept that,” he elaborated. “I just said ‘Really, I’m interested in quality-of-life issues. I’d like to see my kids go into high school or possibly college.’ So I adopted [an approach of] trying to find something for me that would keep me alive and give me a relatively comfortable quality of life, that would allow me to continue to race cars or do whatever I had to do.”
Dr. Carlson, Dr. Somlo, Ms. Nichols, and Mr. Orosco disclosed no relevant conflicts of interest.
SAN FRANCISCO – The National Comprehensive Cancer Network (NCCN) has introduced an easy-to-use visual tool called Evidence Blocks to help physicians and patients compare various treatment options and individualize the selection among them.
“This information can serve as a starting point for shared decision making between the patient and health care team based on individual patients’ value systems,” chief executive officer Dr. Robert W. Carlson said at the NCCN Annual Congress: Hematologic Malignancies, where the tool was unveiled in a session and related press conference.
The first two NCCN guidelines to incorporate the Evidence Blocks – those for multiple myeloma and chronic myelogenous leukemia – were released at the same time. The organization hopes to incorporate them into all of its guidelines by early 2017, he said.
Development of the Evidence Blocks
The NCCN developed the Evidence Blocks to address requests from various stakeholders, according to Dr. Carlson. Guideline users wanted to know more about the rationale behind recommended therapies, asked for inclusion of information on costs, and sought an aid that would allow patients to make decisions based on their individual values.
“The patient perception of value is what should be most important to us,” he commented. “But even among patients, the concept of value differs greatly from patient to patient,” based on factors such as age, comorbidities, treatment goals, and health insurance coverage.
Each Evidence Block graphically displays five measures of information on a recommended therapy: efficacy, safety, quality of the evidence supporting the recommendation, consistency of the evidence supporting the recommendation, and affordability. Each column in the block represents one measure.
Blue shading indicates panelists’ average numeric score for the therapy on that measure rounded to the nearest integer, ranging from 1 (least favorable) to 5 (most favorable). Therefore, the more shading a therapy has, the more favorable its score.
The Evidence Blocks are added to the guidelines and aligned vertically on pages. “This display of the information graphically allows for very efficient scanning of multiple options for therapy. Comparisons across several regimens can be done very quickly and intuitively,” Dr. Carlson noted.
“We believe that the presentation of this type of information allows the health care provider and patient to make their own judgments of the value of specific interventions,” he added.
The affordability measure has generated the most discussion among panelists and stakeholders, according to Dr. Carlson. For this measure, panelists estimated the total cost of care for a therapy, including the costs of drugs, administration, required supportive care, toxicity monitoring, and care associated with management of toxicity. Scores range from very expensive to very inexpensive.
“We don’t use a dollar amount. Rather, it’s sort of what’s the total cost to society, if you will, of the medical intervention part of this,” he explained. “It’s important to understand that these estimates are not necessarily what a patient would pay because many patients have insurance programs that cover all of this cost.… However, we felt it was important to give patients as well as providers an estimate of what the overall magnitude of expense is because there are patients who have huge deductibles, there’s the doughnut hole within Medicare, and there are patients who have no insurance.”
The Evidence Blocks may help address a “conspiracy of silence” between physicians and patients when it comes to discussing treatment costs, whereby neither party wants to bring up this thorny issue, according to Dr. Carlson. “The Evidence Blocks demystify the discussion of cost because the affordability issue is there in front of you. So it gives people permission to talk about cost and affordability.”
It should be relatively easy to teach patients to use the Evidence Blocks. “I think you’ll find your patients will actually be interested in this and that they will not have as much difficulty interpreting this as you think they will, because the patient advocacy groups and the patient advocates that we have spoken with about this, they get this almost instantly,” he said.
Oncologist perspective
There is a critical need for tools such as the Evidence Blocks in making treatment decisions today, according to Dr. George Somlo, professor in the department of medical oncology and therapeutics research at the City of Hope Comprehensive Cancer Center in Duarte, Calif., and also a member of the NCCN multiple myeloma and breast cancer guideline panels.
Treatment options for multiple myeloma, as for many cancers, have exploded in the past few decades, he noted. “How do you go from making sense of having two drugs with a very poor outcome predicted to having literally dozens of agents approved and used in combination, and in essence being at the verge of curing patients with multiple myeloma?”
Dr. Somlo agreed that inclusion of costs in the Evidence Blocks would likely be beneficial as a conversation starter, recalling, “I’ve had patients who did not fill their prescription for a potentially curative medication because they were worried about the $2,500 or $3,500 copay.”
Patient-physician discussion will be important when it comes to using information from the new tool, he said. For example, in the NCCN guideline for multiple myeloma, some of the first-line regimens have identical Evidence Blocks; thus, consideration of factors such as comorbidities will become important.
“This kind of evidence-based scoring system can guide that kind of discussion with the patient and can tailor the individual therapeutic regimens,” he concluded.
Patient perspective
Breast cancer survivor Marta Nichols, who is vice president of investor relations at GoDaddy and a member of the California Breast Cancer Research Council based in San Francisco, welcomed the Evidence Blocks as a tool that will allow patients to make more informed decisions according to what matters most to them.
Only 33 years old at diagnosis, she and her husband had just begun to think about starting a family. “So my primary concern coming into my physician’s office was my fertility and what impact the treatment would have on my fertility. Certainly most physicians are concerned with efficacy – they want to see you survive. My concern was not just surviving, but also thriving and being able to give birth to children down the line,” she explained.
Patients today are overwhelmed not only by their cancer diagnosis, but also by the many treatment options and the new emphasis on shared decision making, Ms. Nichols noted. And that’s where the Evidence Blocks can make a difference.
“When I was diagnosed, it would have been hugely helpful for me to have information laid out in this very clear and systematic way… It would have given us the ability to make a much more informed decision,” she commented.
Multiple myeloma survivor Donald B. Orosco, who is president and chief financial officer of Orosco & Associates and owner of Monterey (Calif.) Speed and Sport, agreed, noting that his priorities when given the diagnosis more than two decades ago at age 47 differed somewhat.
“I adopted the feeling early on that I probably wasn’t going to see a cure for the disease in my lifetime, but I could accept that,” he elaborated. “I just said ‘Really, I’m interested in quality-of-life issues. I’d like to see my kids go into high school or possibly college.’ So I adopted [an approach of] trying to find something for me that would keep me alive and give me a relatively comfortable quality of life, that would allow me to continue to race cars or do whatever I had to do.”
Dr. Carlson, Dr. Somlo, Ms. Nichols, and Mr. Orosco disclosed no relevant conflicts of interest.
AT NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES




