User login
Combo can improve survival in certain AML patients
In a phase 3 trial, adding the quinolone derivative vosaroxin (Qinprezo) to treatment with cytarabine did not improve overall survival in patients with relapsed or refractory acute myeloid leukemia (AML).
However, the combination did confer a survival benefit when transplant patients were excluded from the analysis and in patients age 60 and older.
Results of this trial were recently announced by Sunesis Pharmaceuticals, the company developing vosaroxin.
The results are set to be presented in more detail at an upcoming scientific conference.
The trial, known as VALOR, enrolled 711 AML patients who had relapsed or become refractory to treatment for the first time. The patients were randomized to receive cytarabine plus vosaroxin or cytarabine plus placebo. They were stratified for age, geography, and disease status.
The trial did not meet its primary endpoint of demonstrating a significant improvement in overall survival. The median overall survival was 7.5 months in the vosaroxin-cytarabine arm and 6.1 months in the placebo-cytarabine arm (hazard ratio [HR]=0.865, P=0.06).
However, there was a significant benefit in complete response rate with vosaroxin over placebo—30.1% and 16.3%, respectively (P=0.0000148).
Because transplant could confound the primary analysis, the researchers planned a predefined analysis of overall survival censoring for stem cell transplant.
In this analysis, patients receiving the vosaroxin combination had a median overall survival of 6.7 months, compared to 5.3 months for placebo and cytarabine (HR=0.809, P=0.02).
Results according to age
For age, the researchers stratified patients into those age 60 years and older and those younger than 60 years at enrollment.
For the younger patients (n=260), the median overall survival was 9.1 months in the vosaroxin-cytarabine arm and 7.9 months in the placebo-cytarabine arm (HR=1.079, not significant).
The complete response rates were 26.9% and 20.8%, respectively (P=0.24). The rate of stem cell transplant was 45.8% in this age group.
For patients aged 60 years and older (n=451), the median overall survival was 7.1 months in the vosaroxin-cytarabine arm and 5.0 months in the placebo-cytarabine arm (HR=0.755, P=0.006).
The complete response rates were 31.9% and 13.8%, respectively (P=0.0000048). The rate of stem cell transplant was 20.2% for this age group.
Adverse events and mortality
In the intent-to-treat population, grade 3 or higher non-hematologic adverse events that were more common in the vosaroxin arm were gastrointestinal and infection-related toxicities. This is consistent with events observed in previous company trials.
The rate of serious adverse events was 55.5% in the vosaroxin-cytarabine arm and 35.7% in the placebo-cytarabine arm.
All-cause mortality rates were similar between the arms. Thirty-day mortality rates were 7.9% in the vosaroxin-cytarabine arm and 6.6% in the placebo-cytarabine arm. And 60-day mortality rates were 19.7% and 19.4%, respectively.
Regulatory plans
Based on the results of the trial, Sunesis plans to submit a marketing authorization application for vosaroxin to the European Medicines Agency. The company also plans to meet with the US Food and Drug Administration (FDA) to determine the appropriate regulatory path forward.
The FDA and the European Commission have already granted orphan designation to vosaroxin for the treatment of AML. The drug has been granted fast track designation by the FDA as well, for the potential treatment of relapsed or refractory AML in combination with cytarabine. ![]()
In a phase 3 trial, adding the quinolone derivative vosaroxin (Qinprezo) to treatment with cytarabine did not improve overall survival in patients with relapsed or refractory acute myeloid leukemia (AML).
However, the combination did confer a survival benefit when transplant patients were excluded from the analysis and in patients age 60 and older.
Results of this trial were recently announced by Sunesis Pharmaceuticals, the company developing vosaroxin.
The results are set to be presented in more detail at an upcoming scientific conference.
The trial, known as VALOR, enrolled 711 AML patients who had relapsed or become refractory to treatment for the first time. The patients were randomized to receive cytarabine plus vosaroxin or cytarabine plus placebo. They were stratified for age, geography, and disease status.
The trial did not meet its primary endpoint of demonstrating a significant improvement in overall survival. The median overall survival was 7.5 months in the vosaroxin-cytarabine arm and 6.1 months in the placebo-cytarabine arm (hazard ratio [HR]=0.865, P=0.06).
However, there was a significant benefit in complete response rate with vosaroxin over placebo—30.1% and 16.3%, respectively (P=0.0000148).
Because transplant could confound the primary analysis, the researchers planned a predefined analysis of overall survival censoring for stem cell transplant.
In this analysis, patients receiving the vosaroxin combination had a median overall survival of 6.7 months, compared to 5.3 months for placebo and cytarabine (HR=0.809, P=0.02).
Results according to age
For age, the researchers stratified patients into those age 60 years and older and those younger than 60 years at enrollment.
For the younger patients (n=260), the median overall survival was 9.1 months in the vosaroxin-cytarabine arm and 7.9 months in the placebo-cytarabine arm (HR=1.079, not significant).
The complete response rates were 26.9% and 20.8%, respectively (P=0.24). The rate of stem cell transplant was 45.8% in this age group.
For patients aged 60 years and older (n=451), the median overall survival was 7.1 months in the vosaroxin-cytarabine arm and 5.0 months in the placebo-cytarabine arm (HR=0.755, P=0.006).
The complete response rates were 31.9% and 13.8%, respectively (P=0.0000048). The rate of stem cell transplant was 20.2% for this age group.
Adverse events and mortality
In the intent-to-treat population, grade 3 or higher non-hematologic adverse events that were more common in the vosaroxin arm were gastrointestinal and infection-related toxicities. This is consistent with events observed in previous company trials.
The rate of serious adverse events was 55.5% in the vosaroxin-cytarabine arm and 35.7% in the placebo-cytarabine arm.
All-cause mortality rates were similar between the arms. Thirty-day mortality rates were 7.9% in the vosaroxin-cytarabine arm and 6.6% in the placebo-cytarabine arm. And 60-day mortality rates were 19.7% and 19.4%, respectively.
Regulatory plans
Based on the results of the trial, Sunesis plans to submit a marketing authorization application for vosaroxin to the European Medicines Agency. The company also plans to meet with the US Food and Drug Administration (FDA) to determine the appropriate regulatory path forward.
The FDA and the European Commission have already granted orphan designation to vosaroxin for the treatment of AML. The drug has been granted fast track designation by the FDA as well, for the potential treatment of relapsed or refractory AML in combination with cytarabine. ![]()
In a phase 3 trial, adding the quinolone derivative vosaroxin (Qinprezo) to treatment with cytarabine did not improve overall survival in patients with relapsed or refractory acute myeloid leukemia (AML).
However, the combination did confer a survival benefit when transplant patients were excluded from the analysis and in patients age 60 and older.
Results of this trial were recently announced by Sunesis Pharmaceuticals, the company developing vosaroxin.
The results are set to be presented in more detail at an upcoming scientific conference.
The trial, known as VALOR, enrolled 711 AML patients who had relapsed or become refractory to treatment for the first time. The patients were randomized to receive cytarabine plus vosaroxin or cytarabine plus placebo. They were stratified for age, geography, and disease status.
The trial did not meet its primary endpoint of demonstrating a significant improvement in overall survival. The median overall survival was 7.5 months in the vosaroxin-cytarabine arm and 6.1 months in the placebo-cytarabine arm (hazard ratio [HR]=0.865, P=0.06).
However, there was a significant benefit in complete response rate with vosaroxin over placebo—30.1% and 16.3%, respectively (P=0.0000148).
Because transplant could confound the primary analysis, the researchers planned a predefined analysis of overall survival censoring for stem cell transplant.
In this analysis, patients receiving the vosaroxin combination had a median overall survival of 6.7 months, compared to 5.3 months for placebo and cytarabine (HR=0.809, P=0.02).
Results according to age
For age, the researchers stratified patients into those age 60 years and older and those younger than 60 years at enrollment.
For the younger patients (n=260), the median overall survival was 9.1 months in the vosaroxin-cytarabine arm and 7.9 months in the placebo-cytarabine arm (HR=1.079, not significant).
The complete response rates were 26.9% and 20.8%, respectively (P=0.24). The rate of stem cell transplant was 45.8% in this age group.
For patients aged 60 years and older (n=451), the median overall survival was 7.1 months in the vosaroxin-cytarabine arm and 5.0 months in the placebo-cytarabine arm (HR=0.755, P=0.006).
The complete response rates were 31.9% and 13.8%, respectively (P=0.0000048). The rate of stem cell transplant was 20.2% for this age group.
Adverse events and mortality
In the intent-to-treat population, grade 3 or higher non-hematologic adverse events that were more common in the vosaroxin arm were gastrointestinal and infection-related toxicities. This is consistent with events observed in previous company trials.
The rate of serious adverse events was 55.5% in the vosaroxin-cytarabine arm and 35.7% in the placebo-cytarabine arm.
All-cause mortality rates were similar between the arms. Thirty-day mortality rates were 7.9% in the vosaroxin-cytarabine arm and 6.6% in the placebo-cytarabine arm. And 60-day mortality rates were 19.7% and 19.4%, respectively.
Regulatory plans
Based on the results of the trial, Sunesis plans to submit a marketing authorization application for vosaroxin to the European Medicines Agency. The company also plans to meet with the US Food and Drug Administration (FDA) to determine the appropriate regulatory path forward.
The FDA and the European Commission have already granted orphan designation to vosaroxin for the treatment of AML. The drug has been granted fast track designation by the FDA as well, for the potential treatment of relapsed or refractory AML in combination with cytarabine. ![]()
NICE rejects obinutuzumab for CLL

Credit: Linda Bartlett
In a new draft guidance, the UK’s National Institute for Health and Care Excellence (NICE) has said it cannot recommend obinutuzumab (Gazyvaro) to treat chronic lymphocytic leukemia (CLL).
NICE CEO Sir Andrew Dillon said that although data suggest obinutuzumab is effective, there were too many “uncertainties” in the information submitted by Roche, the company developing the drug.
So NICE cannot be sure obinutuzumab would be an effective use of the National Health Service’s resources.
This is despite the fact that Roche offered to discount the drug’s list price of £26,496 per treatment course.
NICE is accepting comments on the draft guidance until 5 pm on October 23.
Obinutuzumab is a glycoengineered, humanized, monoclonal antibody that selectively binds to the extracellular domain of the CD20 antigen on B cells. The drug induces antibody-dependent cellular cytotoxicity and caspase-independent apoptosis.
The European Commission approved obinutuzumab in July for use in combination with chlorambucil to treat patients with previously untreated CLL who have comorbidities that make them ineligible to receive fludarabine-based therapy.
Obinutuzumab was approved for this indication in the US in November 2013.
Obinutuzumab is marketed as Gazyvaro in the European Union and Switzerland but as Gazyva in the US and the rest of the world. ![]()

Credit: Linda Bartlett
In a new draft guidance, the UK’s National Institute for Health and Care Excellence (NICE) has said it cannot recommend obinutuzumab (Gazyvaro) to treat chronic lymphocytic leukemia (CLL).
NICE CEO Sir Andrew Dillon said that although data suggest obinutuzumab is effective, there were too many “uncertainties” in the information submitted by Roche, the company developing the drug.
So NICE cannot be sure obinutuzumab would be an effective use of the National Health Service’s resources.
This is despite the fact that Roche offered to discount the drug’s list price of £26,496 per treatment course.
NICE is accepting comments on the draft guidance until 5 pm on October 23.
Obinutuzumab is a glycoengineered, humanized, monoclonal antibody that selectively binds to the extracellular domain of the CD20 antigen on B cells. The drug induces antibody-dependent cellular cytotoxicity and caspase-independent apoptosis.
The European Commission approved obinutuzumab in July for use in combination with chlorambucil to treat patients with previously untreated CLL who have comorbidities that make them ineligible to receive fludarabine-based therapy.
Obinutuzumab was approved for this indication in the US in November 2013.
Obinutuzumab is marketed as Gazyvaro in the European Union and Switzerland but as Gazyva in the US and the rest of the world. ![]()

Credit: Linda Bartlett
In a new draft guidance, the UK’s National Institute for Health and Care Excellence (NICE) has said it cannot recommend obinutuzumab (Gazyvaro) to treat chronic lymphocytic leukemia (CLL).
NICE CEO Sir Andrew Dillon said that although data suggest obinutuzumab is effective, there were too many “uncertainties” in the information submitted by Roche, the company developing the drug.
So NICE cannot be sure obinutuzumab would be an effective use of the National Health Service’s resources.
This is despite the fact that Roche offered to discount the drug’s list price of £26,496 per treatment course.
NICE is accepting comments on the draft guidance until 5 pm on October 23.
Obinutuzumab is a glycoengineered, humanized, monoclonal antibody that selectively binds to the extracellular domain of the CD20 antigen on B cells. The drug induces antibody-dependent cellular cytotoxicity and caspase-independent apoptosis.
The European Commission approved obinutuzumab in July for use in combination with chlorambucil to treat patients with previously untreated CLL who have comorbidities that make them ineligible to receive fludarabine-based therapy.
Obinutuzumab was approved for this indication in the US in November 2013.
Obinutuzumab is marketed as Gazyvaro in the European Union and Switzerland but as Gazyva in the US and the rest of the world. ![]()
Product appears safe, effective in rel/ref ALL

Credit: Bill Branson
Eryaspase, a product consisting of L-asparaginase encapsulated in red blood cells, may be safer and more effective than native E coli L-asparaginase, results of a phase 2/3 study suggest.
In patients with relapsed or refractory acute lymphoblastic leukemia (ALL), eryaspase given in combination with chemotherapy produced a higher complete response rate and fewer allergic reactions than native E coli L-asparaginase in combination with chemotherapy.
Eryaspase was also well-tolerated in patients who had previously experienced allergic reactions to L-asparaginase.
ERYTECH Pharma, the company developing eryaspase, recently announced these results from the GRASPIVOTALL trial.
The study included 80 children and adults with relapsed or refractory ALL, who were randomized to 1 of 3 treatment arms.
In the first 2 arms, researchers compared eryaspase to native E coli L-asparaginase, both in combination with standard chemotherapy (COOPRALL), in patients without prior allergies to L-asparaginase. In the third arm, the team evaluated eryaspase for patients who have experienced allergic reactions related to asparaginase in their first-line treatment.
The primary endpoint of the study consisted of 2 objectives: (a) superior safety, expressed as a significant reduction of the incidence of allergic reactions with eryaspase compared to native L-asparaginase, and (b) noninferior duration of asparaginase activity above the threshold of 100 IU/L during the induction phase in the nonallergic patients. Both endpoints needed to be met for the study to be considered positive.
The main secondary efficacy endpoints included complete response, minimal residual disease, event-free survival, and overall survival.
At 1 year of follow-up, both primary endpoints were met. There was a significant reduction of allergic reactions in the eryaspase arm compared to the native L-asparaginase arm—0% (0/26) and 42.9% (12/28), respectively (P<0.001).
And there was a significant increase in the duration of circulating asparaginase activity in the eryaspase arm compared to the native L-asparaginase arm. Asparaginase levels were maintained above 100 IU/L for an average of 20.5 days with up to 2 injections during the first month of treatment with eryaspase, compared to 9.2 days in the native L-asparaginase arm, with up to 8 injections of L-asparaginase (P<0.001).
In addition, the complete response rate was higher with eryaspase. At the end of the induction phase, 71.4% of patients (n=15) in the eryaspase arm had a complete response, compared to 42.3% of patients (n=11) in the native L-asparaginase arm.
Finally, the study showed that eryaspase is well-tolerated by patients with previous allergies to L-asparaginase. Two of the 26 patients with prior allergies to L-asparaginase experienced mild allergic reactions to eryaspase.
“The results of this study are an important step forward for the treatment of ALL patients that are at risk to receive L-asparaginase, which remains an important unmet medical need,” said Yves Betrand, MD, of the Institute for Pediatric Hematology and Oncology in Lyon, France.
“The virtual absence of allergic reactions, also in patients with prior allergies to L-asparaginase, is very encouraging.”
The analysis of additional secondary and exploratory endpoints for this study is ongoing. ERYTECH said results will be available later this year and are set to be presented at an upcoming scientific conference.
Based on the results of this and earlier studies of eryaspase, ERYTECH intends to submit its application for European Marketing Authorization in the first half of 2015.
The company also plans to accelerate the product’s development in ALL in the US and to launch phase 2 clinical trials in additional oncology indications with high unmet medical need. A phase 2b study of eryaspase in acute myeloid leukemia is already underway, with more than half of the patients enrolled. ![]()

Credit: Bill Branson
Eryaspase, a product consisting of L-asparaginase encapsulated in red blood cells, may be safer and more effective than native E coli L-asparaginase, results of a phase 2/3 study suggest.
In patients with relapsed or refractory acute lymphoblastic leukemia (ALL), eryaspase given in combination with chemotherapy produced a higher complete response rate and fewer allergic reactions than native E coli L-asparaginase in combination with chemotherapy.
Eryaspase was also well-tolerated in patients who had previously experienced allergic reactions to L-asparaginase.
ERYTECH Pharma, the company developing eryaspase, recently announced these results from the GRASPIVOTALL trial.
The study included 80 children and adults with relapsed or refractory ALL, who were randomized to 1 of 3 treatment arms.
In the first 2 arms, researchers compared eryaspase to native E coli L-asparaginase, both in combination with standard chemotherapy (COOPRALL), in patients without prior allergies to L-asparaginase. In the third arm, the team evaluated eryaspase for patients who have experienced allergic reactions related to asparaginase in their first-line treatment.
The primary endpoint of the study consisted of 2 objectives: (a) superior safety, expressed as a significant reduction of the incidence of allergic reactions with eryaspase compared to native L-asparaginase, and (b) noninferior duration of asparaginase activity above the threshold of 100 IU/L during the induction phase in the nonallergic patients. Both endpoints needed to be met for the study to be considered positive.
The main secondary efficacy endpoints included complete response, minimal residual disease, event-free survival, and overall survival.
At 1 year of follow-up, both primary endpoints were met. There was a significant reduction of allergic reactions in the eryaspase arm compared to the native L-asparaginase arm—0% (0/26) and 42.9% (12/28), respectively (P<0.001).
And there was a significant increase in the duration of circulating asparaginase activity in the eryaspase arm compared to the native L-asparaginase arm. Asparaginase levels were maintained above 100 IU/L for an average of 20.5 days with up to 2 injections during the first month of treatment with eryaspase, compared to 9.2 days in the native L-asparaginase arm, with up to 8 injections of L-asparaginase (P<0.001).
In addition, the complete response rate was higher with eryaspase. At the end of the induction phase, 71.4% of patients (n=15) in the eryaspase arm had a complete response, compared to 42.3% of patients (n=11) in the native L-asparaginase arm.
Finally, the study showed that eryaspase is well-tolerated by patients with previous allergies to L-asparaginase. Two of the 26 patients with prior allergies to L-asparaginase experienced mild allergic reactions to eryaspase.
“The results of this study are an important step forward for the treatment of ALL patients that are at risk to receive L-asparaginase, which remains an important unmet medical need,” said Yves Betrand, MD, of the Institute for Pediatric Hematology and Oncology in Lyon, France.
“The virtual absence of allergic reactions, also in patients with prior allergies to L-asparaginase, is very encouraging.”
The analysis of additional secondary and exploratory endpoints for this study is ongoing. ERYTECH said results will be available later this year and are set to be presented at an upcoming scientific conference.
Based on the results of this and earlier studies of eryaspase, ERYTECH intends to submit its application for European Marketing Authorization in the first half of 2015.
The company also plans to accelerate the product’s development in ALL in the US and to launch phase 2 clinical trials in additional oncology indications with high unmet medical need. A phase 2b study of eryaspase in acute myeloid leukemia is already underway, with more than half of the patients enrolled. ![]()

Credit: Bill Branson
Eryaspase, a product consisting of L-asparaginase encapsulated in red blood cells, may be safer and more effective than native E coli L-asparaginase, results of a phase 2/3 study suggest.
In patients with relapsed or refractory acute lymphoblastic leukemia (ALL), eryaspase given in combination with chemotherapy produced a higher complete response rate and fewer allergic reactions than native E coli L-asparaginase in combination with chemotherapy.
Eryaspase was also well-tolerated in patients who had previously experienced allergic reactions to L-asparaginase.
ERYTECH Pharma, the company developing eryaspase, recently announced these results from the GRASPIVOTALL trial.
The study included 80 children and adults with relapsed or refractory ALL, who were randomized to 1 of 3 treatment arms.
In the first 2 arms, researchers compared eryaspase to native E coli L-asparaginase, both in combination with standard chemotherapy (COOPRALL), in patients without prior allergies to L-asparaginase. In the third arm, the team evaluated eryaspase for patients who have experienced allergic reactions related to asparaginase in their first-line treatment.
The primary endpoint of the study consisted of 2 objectives: (a) superior safety, expressed as a significant reduction of the incidence of allergic reactions with eryaspase compared to native L-asparaginase, and (b) noninferior duration of asparaginase activity above the threshold of 100 IU/L during the induction phase in the nonallergic patients. Both endpoints needed to be met for the study to be considered positive.
The main secondary efficacy endpoints included complete response, minimal residual disease, event-free survival, and overall survival.
At 1 year of follow-up, both primary endpoints were met. There was a significant reduction of allergic reactions in the eryaspase arm compared to the native L-asparaginase arm—0% (0/26) and 42.9% (12/28), respectively (P<0.001).
And there was a significant increase in the duration of circulating asparaginase activity in the eryaspase arm compared to the native L-asparaginase arm. Asparaginase levels were maintained above 100 IU/L for an average of 20.5 days with up to 2 injections during the first month of treatment with eryaspase, compared to 9.2 days in the native L-asparaginase arm, with up to 8 injections of L-asparaginase (P<0.001).
In addition, the complete response rate was higher with eryaspase. At the end of the induction phase, 71.4% of patients (n=15) in the eryaspase arm had a complete response, compared to 42.3% of patients (n=11) in the native L-asparaginase arm.
Finally, the study showed that eryaspase is well-tolerated by patients with previous allergies to L-asparaginase. Two of the 26 patients with prior allergies to L-asparaginase experienced mild allergic reactions to eryaspase.
“The results of this study are an important step forward for the treatment of ALL patients that are at risk to receive L-asparaginase, which remains an important unmet medical need,” said Yves Betrand, MD, of the Institute for Pediatric Hematology and Oncology in Lyon, France.
“The virtual absence of allergic reactions, also in patients with prior allergies to L-asparaginase, is very encouraging.”
The analysis of additional secondary and exploratory endpoints for this study is ongoing. ERYTECH said results will be available later this year and are set to be presented at an upcoming scientific conference.
Based on the results of this and earlier studies of eryaspase, ERYTECH intends to submit its application for European Marketing Authorization in the first half of 2015.
The company also plans to accelerate the product’s development in ALL in the US and to launch phase 2 clinical trials in additional oncology indications with high unmet medical need. A phase 2b study of eryaspase in acute myeloid leukemia is already underway, with more than half of the patients enrolled. ![]()
Targeting drug resistance earlier

Credit: PNAS
PHILADELPHIA—A combination treatment strategy that takes tumor evolution into account could help us avoid drug resistance in hematologic malignancies, researchers say.
Preclinical experiments suggest we can prevent resistance by starting secondary treatment prior to relapse.
For example, a patient receiving dasatinib for acute lymphoblastic leukemia (ALL) could benefit from receiving crizotinib or foretinib during the early stages of clonal evolution.
The researchers described this strategy in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“Our goal is to identify vulnerabilities in cancer across stages of tumor evolution while it is developing resistance to initial treatment, to help guide the design of drug combination strategies,” said Douglas Lauffenburger, PhD, of the Koch Institute for Integrative Cancer Research at MIT in Boston.
“There may be many stages in a tumor evolution while under treatment that may make them vulnerable to already existing therapies. Rather than waiting for the tumor to become resistant to the first treatment and then thinking about a second-line drug to use, we can capitalize on opportunities that exploit vulnerabilities at different early stages, as the tumor is evolving to become resistant to the first drug.”
Dr Lauffenburger and his colleagues used a combination of computational and experimental approaches to identify drugs likely to be effective against a murine ALL cell line as the cells evolve.
To develop drug combinations based on the characteristics of evolving tumors, the researchers used escalating doses of imatinib, dasatinib, nilotinib, foretinib, and crizotinib on ALL cells.
As some cells exhibited resistance to a particular drug, the team treated the resistant cells with other drugs to check for cross-resistance. They found that resistant cells surviving at low multiples of the original drug dose actually demonstrated sensitization to certain other drugs, with the sensitization abrogated at higher doses.
Specifically, cell populations that were resistant to dasatinib at 1x and 2x IC90 became even more sensitive to crizotinib and foretinib. However, the sensitivity was lost at IC90 4x and above.
“Instead of only looking for the most resistant population of ALL cells at the end of this selection process, we monitored for drug sensitivity of the cells at each stage of the dose escalation,” Dr Lauffenburger explained.
“This led us to discover the vulnerabilities of a tumor at different stages of clonal evolution, a phenomenon we would have missed if we only analyzed for drug sensitivity at the last stage of this process, which is equivalent to when a patient has relapsed.” ![]()

Credit: PNAS
PHILADELPHIA—A combination treatment strategy that takes tumor evolution into account could help us avoid drug resistance in hematologic malignancies, researchers say.
Preclinical experiments suggest we can prevent resistance by starting secondary treatment prior to relapse.
For example, a patient receiving dasatinib for acute lymphoblastic leukemia (ALL) could benefit from receiving crizotinib or foretinib during the early stages of clonal evolution.
The researchers described this strategy in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“Our goal is to identify vulnerabilities in cancer across stages of tumor evolution while it is developing resistance to initial treatment, to help guide the design of drug combination strategies,” said Douglas Lauffenburger, PhD, of the Koch Institute for Integrative Cancer Research at MIT in Boston.
“There may be many stages in a tumor evolution while under treatment that may make them vulnerable to already existing therapies. Rather than waiting for the tumor to become resistant to the first treatment and then thinking about a second-line drug to use, we can capitalize on opportunities that exploit vulnerabilities at different early stages, as the tumor is evolving to become resistant to the first drug.”
Dr Lauffenburger and his colleagues used a combination of computational and experimental approaches to identify drugs likely to be effective against a murine ALL cell line as the cells evolve.
To develop drug combinations based on the characteristics of evolving tumors, the researchers used escalating doses of imatinib, dasatinib, nilotinib, foretinib, and crizotinib on ALL cells.
As some cells exhibited resistance to a particular drug, the team treated the resistant cells with other drugs to check for cross-resistance. They found that resistant cells surviving at low multiples of the original drug dose actually demonstrated sensitization to certain other drugs, with the sensitization abrogated at higher doses.
Specifically, cell populations that were resistant to dasatinib at 1x and 2x IC90 became even more sensitive to crizotinib and foretinib. However, the sensitivity was lost at IC90 4x and above.
“Instead of only looking for the most resistant population of ALL cells at the end of this selection process, we monitored for drug sensitivity of the cells at each stage of the dose escalation,” Dr Lauffenburger explained.
“This led us to discover the vulnerabilities of a tumor at different stages of clonal evolution, a phenomenon we would have missed if we only analyzed for drug sensitivity at the last stage of this process, which is equivalent to when a patient has relapsed.” ![]()

Credit: PNAS
PHILADELPHIA—A combination treatment strategy that takes tumor evolution into account could help us avoid drug resistance in hematologic malignancies, researchers say.
Preclinical experiments suggest we can prevent resistance by starting secondary treatment prior to relapse.
For example, a patient receiving dasatinib for acute lymphoblastic leukemia (ALL) could benefit from receiving crizotinib or foretinib during the early stages of clonal evolution.
The researchers described this strategy in a poster at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“Our goal is to identify vulnerabilities in cancer across stages of tumor evolution while it is developing resistance to initial treatment, to help guide the design of drug combination strategies,” said Douglas Lauffenburger, PhD, of the Koch Institute for Integrative Cancer Research at MIT in Boston.
“There may be many stages in a tumor evolution while under treatment that may make them vulnerable to already existing therapies. Rather than waiting for the tumor to become resistant to the first treatment and then thinking about a second-line drug to use, we can capitalize on opportunities that exploit vulnerabilities at different early stages, as the tumor is evolving to become resistant to the first drug.”
Dr Lauffenburger and his colleagues used a combination of computational and experimental approaches to identify drugs likely to be effective against a murine ALL cell line as the cells evolve.
To develop drug combinations based on the characteristics of evolving tumors, the researchers used escalating doses of imatinib, dasatinib, nilotinib, foretinib, and crizotinib on ALL cells.
As some cells exhibited resistance to a particular drug, the team treated the resistant cells with other drugs to check for cross-resistance. They found that resistant cells surviving at low multiples of the original drug dose actually demonstrated sensitization to certain other drugs, with the sensitization abrogated at higher doses.
Specifically, cell populations that were resistant to dasatinib at 1x and 2x IC90 became even more sensitive to crizotinib and foretinib. However, the sensitivity was lost at IC90 4x and above.
“Instead of only looking for the most resistant population of ALL cells at the end of this selection process, we monitored for drug sensitivity of the cells at each stage of the dose escalation,” Dr Lauffenburger explained.
“This led us to discover the vulnerabilities of a tumor at different stages of clonal evolution, a phenomenon we would have missed if we only analyzed for drug sensitivity at the last stage of this process, which is equivalent to when a patient has relapsed.” ![]()
Drug can prevent chemo-induced nausea, vomiting

Credit: Rhoda Baer
MADRID—A small molecule called rolapitant can prevent nausea and vomiting in patients receiving cisplatin-based chemotherapy, results of a phase 3 trial suggest.
When given prior to chemotherapy, rolapitant induced a complete response in about 70% of patients.
These patients had no emesis after chemotherapy and did not require any rescue medication.
“This agent makes a significant difference in the way people tolerate their chemotherapy,” said Martin Chasen, MD, of Ottawa Hospital Cancer Centre in Canada.
“Patients experienced no loss in quality of life, and, in fact, many saw meaningful improvements. One of the patients in the rolapitant cohort reported that he had just finished 18 holes of golf one week after receiving chemotherapy. This is in sharp contrast to many patients on current standard anti-emetics that are too ill to get out of bed within a week after each cycle of cisplatin.”
Dr Chasen and his colleagues reported these results at the ESMO 2014 Congress (abstract LBA47_PR).
The team had set out to evaluate rolapitant, a novel antagonist of the NK-1 receptor, for the prevention of severe nausea and vomiting often experienced by patients receiving cisplatin-based chemotherapy, which may cause dose reductions and treatment discontinuation.
The trial included 532 patients who were randomized 1:1 to receive rolapitant plus granisetron/dexamethasone or placebo plus granisetron/dexamethasone prior to chemotherapy.
The primary endpoint was complete response (defined as the patient having no emesis and not requiring any rescue medication) in the delayed phase (>24-120 hours) post-chemotherapy. Key secondary endpoints included complete response during the acute phase (0-24 hours) and overall (0-120 hours).
The trial met its primary endpoint, with 72.7% of patients receiving rolapitant achieving a complete response in the delayed phase, compared to 58.4% of those receiving placebo (P<0.001).
Rolapitant also improved the complete response rate compared to placebo in the acute phase—83.7% and 73.7%, respectively (P=0.005).
Overall, the complete response rates were 70.1% and 56.5%, respectively (P=0.001).
Patients receiving rolapitant tended to report that chemotherapy had less of an impact on their daily quality of life, although the difference between the treatment arms was not significant—72.8% vs 67.8% (P=0.231).
“Rolapitant demonstrated a significant effect in both the acute and delayed phases,” Dr Chasen noted. “Our primary endpoint was achieved in the delayed phase—an incredible result.”
“We know that the NK-1 receptor in the brain must be blocked to control nausea and vomiting. Rolapitant is an exceptionally long-term receptor blocker that binds to the receptor and remains in place for up to 120 hours, therefore not allowing the chemotherapy to induce nausea and vomiting.”
Dr Chasen added that rolapitant may prove effective in patients receiving less emetogenic cancer treatments as well. ![]()

Credit: Rhoda Baer
MADRID—A small molecule called rolapitant can prevent nausea and vomiting in patients receiving cisplatin-based chemotherapy, results of a phase 3 trial suggest.
When given prior to chemotherapy, rolapitant induced a complete response in about 70% of patients.
These patients had no emesis after chemotherapy and did not require any rescue medication.
“This agent makes a significant difference in the way people tolerate their chemotherapy,” said Martin Chasen, MD, of Ottawa Hospital Cancer Centre in Canada.
“Patients experienced no loss in quality of life, and, in fact, many saw meaningful improvements. One of the patients in the rolapitant cohort reported that he had just finished 18 holes of golf one week after receiving chemotherapy. This is in sharp contrast to many patients on current standard anti-emetics that are too ill to get out of bed within a week after each cycle of cisplatin.”
Dr Chasen and his colleagues reported these results at the ESMO 2014 Congress (abstract LBA47_PR).
The team had set out to evaluate rolapitant, a novel antagonist of the NK-1 receptor, for the prevention of severe nausea and vomiting often experienced by patients receiving cisplatin-based chemotherapy, which may cause dose reductions and treatment discontinuation.
The trial included 532 patients who were randomized 1:1 to receive rolapitant plus granisetron/dexamethasone or placebo plus granisetron/dexamethasone prior to chemotherapy.
The primary endpoint was complete response (defined as the patient having no emesis and not requiring any rescue medication) in the delayed phase (>24-120 hours) post-chemotherapy. Key secondary endpoints included complete response during the acute phase (0-24 hours) and overall (0-120 hours).
The trial met its primary endpoint, with 72.7% of patients receiving rolapitant achieving a complete response in the delayed phase, compared to 58.4% of those receiving placebo (P<0.001).
Rolapitant also improved the complete response rate compared to placebo in the acute phase—83.7% and 73.7%, respectively (P=0.005).
Overall, the complete response rates were 70.1% and 56.5%, respectively (P=0.001).
Patients receiving rolapitant tended to report that chemotherapy had less of an impact on their daily quality of life, although the difference between the treatment arms was not significant—72.8% vs 67.8% (P=0.231).
“Rolapitant demonstrated a significant effect in both the acute and delayed phases,” Dr Chasen noted. “Our primary endpoint was achieved in the delayed phase—an incredible result.”
“We know that the NK-1 receptor in the brain must be blocked to control nausea and vomiting. Rolapitant is an exceptionally long-term receptor blocker that binds to the receptor and remains in place for up to 120 hours, therefore not allowing the chemotherapy to induce nausea and vomiting.”
Dr Chasen added that rolapitant may prove effective in patients receiving less emetogenic cancer treatments as well. ![]()

Credit: Rhoda Baer
MADRID—A small molecule called rolapitant can prevent nausea and vomiting in patients receiving cisplatin-based chemotherapy, results of a phase 3 trial suggest.
When given prior to chemotherapy, rolapitant induced a complete response in about 70% of patients.
These patients had no emesis after chemotherapy and did not require any rescue medication.
“This agent makes a significant difference in the way people tolerate their chemotherapy,” said Martin Chasen, MD, of Ottawa Hospital Cancer Centre in Canada.
“Patients experienced no loss in quality of life, and, in fact, many saw meaningful improvements. One of the patients in the rolapitant cohort reported that he had just finished 18 holes of golf one week after receiving chemotherapy. This is in sharp contrast to many patients on current standard anti-emetics that are too ill to get out of bed within a week after each cycle of cisplatin.”
Dr Chasen and his colleagues reported these results at the ESMO 2014 Congress (abstract LBA47_PR).
The team had set out to evaluate rolapitant, a novel antagonist of the NK-1 receptor, for the prevention of severe nausea and vomiting often experienced by patients receiving cisplatin-based chemotherapy, which may cause dose reductions and treatment discontinuation.
The trial included 532 patients who were randomized 1:1 to receive rolapitant plus granisetron/dexamethasone or placebo plus granisetron/dexamethasone prior to chemotherapy.
The primary endpoint was complete response (defined as the patient having no emesis and not requiring any rescue medication) in the delayed phase (>24-120 hours) post-chemotherapy. Key secondary endpoints included complete response during the acute phase (0-24 hours) and overall (0-120 hours).
The trial met its primary endpoint, with 72.7% of patients receiving rolapitant achieving a complete response in the delayed phase, compared to 58.4% of those receiving placebo (P<0.001).
Rolapitant also improved the complete response rate compared to placebo in the acute phase—83.7% and 73.7%, respectively (P=0.005).
Overall, the complete response rates were 70.1% and 56.5%, respectively (P=0.001).
Patients receiving rolapitant tended to report that chemotherapy had less of an impact on their daily quality of life, although the difference between the treatment arms was not significant—72.8% vs 67.8% (P=0.231).
“Rolapitant demonstrated a significant effect in both the acute and delayed phases,” Dr Chasen noted. “Our primary endpoint was achieved in the delayed phase—an incredible result.”
“We know that the NK-1 receptor in the brain must be blocked to control nausea and vomiting. Rolapitant is an exceptionally long-term receptor blocker that binds to the receptor and remains in place for up to 120 hours, therefore not allowing the chemotherapy to induce nausea and vomiting.”
Dr Chasen added that rolapitant may prove effective in patients receiving less emetogenic cancer treatments as well. ![]()
Hypercalcemia may be indicator for hematologic cancers

Credit: Graham Colm
Hypercalcemia could be an early indication of cancer, according to a study published in the British Journal of Cancer.
The connection between hypercalcemia and cancer is well known, but this study shows the condition can predate cancer diagnosis in primary care.
The association between hypercalcemia and cancers was particularly strong in men. And myeloma and other hematologic malignancies were among the most common cancers associated with hypercalcemia.
“All previous studies on hypercalcemia and cancer had been carried out with patients who had already been diagnosed with cancer; hypercalcemia was seen as a late effect of the cancer,” said study author Fergus Hamilton, of the University of Bristol in the UK.
“We wanted to look at the issue from a different perspective and find out if high calcium levels in blood could be used as an early indicator of cancer and, therefore, in the diagnosis of cancer.”
So the researchers analyzed the electronic records of 54,267 patients with elevated calcium levels and found that hypercalcemia was strongly associated with cancer, especially in males.
The positive predictive values for cancer in men were 11.5% for calcium levels between 2.60 and 2.79 mmol l-1, 27.9% for 2.8-2.99 mmol l-1, and 50% for >3.0 mmol l-1. In women, the corresponding values were 4.1%, 8.7%, and 16.7%, respectively.
In men, the most common cancers associated with hypercalcemia were lung (34%), prostate (21%), colorectal (8%), myeloma (8%), and other hematologic cancers (8%). There were 12 other cancer types recorded as well (19%).
In women, the most common cancers were myeloma (24%), breast (18%), other hematologic cancers (10%), lung (8%), and metastatic cancer with unknown primary (8%). There were 16 other cancers recorded among women (32%).
The researchers found no difference in calcium levels among the different cancers.
“We were surprised by the gender difference,” Dr Hamilton said. “There are a number of possible explanations for this, but we think it might be because women are much more likely to have hyperparathyroidism, another cause of hypercalcemia. Men rarely get this condition, so their hypercalcemia is more likely to be due to cancer.” ![]()

Credit: Graham Colm
Hypercalcemia could be an early indication of cancer, according to a study published in the British Journal of Cancer.
The connection between hypercalcemia and cancer is well known, but this study shows the condition can predate cancer diagnosis in primary care.
The association between hypercalcemia and cancers was particularly strong in men. And myeloma and other hematologic malignancies were among the most common cancers associated with hypercalcemia.
“All previous studies on hypercalcemia and cancer had been carried out with patients who had already been diagnosed with cancer; hypercalcemia was seen as a late effect of the cancer,” said study author Fergus Hamilton, of the University of Bristol in the UK.
“We wanted to look at the issue from a different perspective and find out if high calcium levels in blood could be used as an early indicator of cancer and, therefore, in the diagnosis of cancer.”
So the researchers analyzed the electronic records of 54,267 patients with elevated calcium levels and found that hypercalcemia was strongly associated with cancer, especially in males.
The positive predictive values for cancer in men were 11.5% for calcium levels between 2.60 and 2.79 mmol l-1, 27.9% for 2.8-2.99 mmol l-1, and 50% for >3.0 mmol l-1. In women, the corresponding values were 4.1%, 8.7%, and 16.7%, respectively.
In men, the most common cancers associated with hypercalcemia were lung (34%), prostate (21%), colorectal (8%), myeloma (8%), and other hematologic cancers (8%). There were 12 other cancer types recorded as well (19%).
In women, the most common cancers were myeloma (24%), breast (18%), other hematologic cancers (10%), lung (8%), and metastatic cancer with unknown primary (8%). There were 16 other cancers recorded among women (32%).
The researchers found no difference in calcium levels among the different cancers.
“We were surprised by the gender difference,” Dr Hamilton said. “There are a number of possible explanations for this, but we think it might be because women are much more likely to have hyperparathyroidism, another cause of hypercalcemia. Men rarely get this condition, so their hypercalcemia is more likely to be due to cancer.” ![]()

Credit: Graham Colm
Hypercalcemia could be an early indication of cancer, according to a study published in the British Journal of Cancer.
The connection between hypercalcemia and cancer is well known, but this study shows the condition can predate cancer diagnosis in primary care.
The association between hypercalcemia and cancers was particularly strong in men. And myeloma and other hematologic malignancies were among the most common cancers associated with hypercalcemia.
“All previous studies on hypercalcemia and cancer had been carried out with patients who had already been diagnosed with cancer; hypercalcemia was seen as a late effect of the cancer,” said study author Fergus Hamilton, of the University of Bristol in the UK.
“We wanted to look at the issue from a different perspective and find out if high calcium levels in blood could be used as an early indicator of cancer and, therefore, in the diagnosis of cancer.”
So the researchers analyzed the electronic records of 54,267 patients with elevated calcium levels and found that hypercalcemia was strongly associated with cancer, especially in males.
The positive predictive values for cancer in men were 11.5% for calcium levels between 2.60 and 2.79 mmol l-1, 27.9% for 2.8-2.99 mmol l-1, and 50% for >3.0 mmol l-1. In women, the corresponding values were 4.1%, 8.7%, and 16.7%, respectively.
In men, the most common cancers associated with hypercalcemia were lung (34%), prostate (21%), colorectal (8%), myeloma (8%), and other hematologic cancers (8%). There were 12 other cancer types recorded as well (19%).
In women, the most common cancers were myeloma (24%), breast (18%), other hematologic cancers (10%), lung (8%), and metastatic cancer with unknown primary (8%). There were 16 other cancers recorded among women (32%).
The researchers found no difference in calcium levels among the different cancers.
“We were surprised by the gender difference,” Dr Hamilton said. “There are a number of possible explanations for this, but we think it might be because women are much more likely to have hyperparathyroidism, another cause of hypercalcemia. Men rarely get this condition, so their hypercalcemia is more likely to be due to cancer.” ![]()
Preventing cancer-related infection

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()
Speaker offers alternatives for sustainable TKI use in CML
NEW YORK—If any oncology drugs warrant a high price, BCR-ABL tyrosine kinase inhibitors (TKIs) could make a strong case, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
TKIs have revolutionized the therapeutic landscape in chronic myeloid leukemia (CML), said Neil P. Shah, MD, PhD, of the UCSF
Helen Diller Family Comprehensive Cancer Center in San Francisco.
Five-year overall survival is 93% in CML patients treated with imatinib. And 80,000 people are estimated to be living with CML in 2014, a number that is expected to double by 2035.
Yet the increase in life expectancy places a burden on the healthcare system, Dr Shah said, particularly since the price of BCR-ABL TKIs has risen dramatically.
A year of imatinib therapy circa 2001 cost approximately $30,000, and by 2013, approximately $92,000. Second-generation (2G) TKIs cost even more, at about $115,000 annually, and the third-generation TKI ponatinib costs about $138,000 annually.
Confounding the financial picture will be the advent of generic imatinib, which will be available in the US in early 2016.
Generic imatinib will, presumably, be less expensive than the brand-name drug. However, it is not clear whether it will be as effective or what impact it will have on the 2G and 3G TKIs.
With all that in mind, Dr Shah provided some options for maximizing therapeutic outcomes in a fiscally responsible manner.
He based his potential solutions on evidence-based premises. First, imatinib is a highly active therapy for many chronic-phase CML patients. The 8-year update of the IRIS study shows that 53% of patients sustain complete cytogenetic remission (CCyR) with imatinib.
Second, patients who are likely to do well on TKI therapy can be identified early based on their BCR-ABL PCR levels after 3 months of therapy.
This important 3-month milestone has been incorporated into the NCCN guidelines. Patients who achieve BCR-ABL/ABL levels of 10% or less have a significantly better overall survival than those who have levels greater than 10%.
Third, the ENESTnd and DASISION studies demonstrated that nilotinib and dasatinib elicit achievement of important treatment milestones (PCR<10% at 3 months and CCyR after 12 months) in a significantly higher proportion of patients than imatinib. But to date, neither agent has produced a significant improvement in overall survival.
And fourth, while nilotinib and dasatinib have an undisputable clinical benefit over imatinib in terms of transformation to accelerated phase/blast crisis (AP/BC), these agents cost between $23,000 and $31,000 more than imatinib for an annual course of treatment.
Dr Shah calculated that to achieve approximately 10 fewer AP/BC transformations over 5 years, approximately 300 patients would need to be treated at an additional cost of $37.5 million. This equates to $3.75 million in additional costs for 1 transformation event spared over 5 years.
“We do have to keep in mind transformation events are not cheap,” he said. “So when these happen, patients need to be hospitalized for chemotherapy, typically, or they have to go to allogeneic stem cell transplantation.”
So Dr Shah proffered 3 potential approaches for fiscally sustainable TKI use.
The first approach would be to initiate imatinib in most, if not all, chronic-phase CML patients. If they achieve BCR-ABL levels <10% at 3 months or partial CyR after 12 months, then continue imatinib. If not, switch to a 2G TKI.
Dr Shah noted that 40% to 60% of patients will have a deep, durable response to imatinib.
The second approach would be to initiate 2G TKIs in newly diagnosed patients. And when they achieve CCyR or major molecular response (MMR), enroll them in a clinical trial.
These trials could investigate a switch to imatinib, use of a lower dose of the 2G TKI, a switch to interferon-alfa, the addition of a CYP3A4 inhibitor (such as grapefruit) and a lower dose, or another investigational option.
And the third approach would be to initiate imatinib or an approved 2G TKI in newly diagnosed patients. When they achieve targeted molecular remission, enroll them in a treatment-discontinuation trial.
Dr Shah pointed out that in the STIM study, 61% of patients remained in complete molecular remission 60 months after discontinuing imatinib, and 40% experienced treatment-free survival.
Taking into account the cost of imatinib and the number of months without treatment, STIM investigators estimated the savings to be €4,587,500, or approximately $6 to $7 million.
Patients who relapsed 6 to 9 months after discontinuing imatinib tended to respond well to a rechallenge with imatinib. But Dr Shah cautioned that, at present, discontinuation should only be performed in the context of a clinical trial. ![]()
NEW YORK—If any oncology drugs warrant a high price, BCR-ABL tyrosine kinase inhibitors (TKIs) could make a strong case, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
TKIs have revolutionized the therapeutic landscape in chronic myeloid leukemia (CML), said Neil P. Shah, MD, PhD, of the UCSF
Helen Diller Family Comprehensive Cancer Center in San Francisco.
Five-year overall survival is 93% in CML patients treated with imatinib. And 80,000 people are estimated to be living with CML in 2014, a number that is expected to double by 2035.
Yet the increase in life expectancy places a burden on the healthcare system, Dr Shah said, particularly since the price of BCR-ABL TKIs has risen dramatically.
A year of imatinib therapy circa 2001 cost approximately $30,000, and by 2013, approximately $92,000. Second-generation (2G) TKIs cost even more, at about $115,000 annually, and the third-generation TKI ponatinib costs about $138,000 annually.
Confounding the financial picture will be the advent of generic imatinib, which will be available in the US in early 2016.
Generic imatinib will, presumably, be less expensive than the brand-name drug. However, it is not clear whether it will be as effective or what impact it will have on the 2G and 3G TKIs.
With all that in mind, Dr Shah provided some options for maximizing therapeutic outcomes in a fiscally responsible manner.
He based his potential solutions on evidence-based premises. First, imatinib is a highly active therapy for many chronic-phase CML patients. The 8-year update of the IRIS study shows that 53% of patients sustain complete cytogenetic remission (CCyR) with imatinib.
Second, patients who are likely to do well on TKI therapy can be identified early based on their BCR-ABL PCR levels after 3 months of therapy.
This important 3-month milestone has been incorporated into the NCCN guidelines. Patients who achieve BCR-ABL/ABL levels of 10% or less have a significantly better overall survival than those who have levels greater than 10%.
Third, the ENESTnd and DASISION studies demonstrated that nilotinib and dasatinib elicit achievement of important treatment milestones (PCR<10% at 3 months and CCyR after 12 months) in a significantly higher proportion of patients than imatinib. But to date, neither agent has produced a significant improvement in overall survival.
And fourth, while nilotinib and dasatinib have an undisputable clinical benefit over imatinib in terms of transformation to accelerated phase/blast crisis (AP/BC), these agents cost between $23,000 and $31,000 more than imatinib for an annual course of treatment.
Dr Shah calculated that to achieve approximately 10 fewer AP/BC transformations over 5 years, approximately 300 patients would need to be treated at an additional cost of $37.5 million. This equates to $3.75 million in additional costs for 1 transformation event spared over 5 years.
“We do have to keep in mind transformation events are not cheap,” he said. “So when these happen, patients need to be hospitalized for chemotherapy, typically, or they have to go to allogeneic stem cell transplantation.”
So Dr Shah proffered 3 potential approaches for fiscally sustainable TKI use.
The first approach would be to initiate imatinib in most, if not all, chronic-phase CML patients. If they achieve BCR-ABL levels <10% at 3 months or partial CyR after 12 months, then continue imatinib. If not, switch to a 2G TKI.
Dr Shah noted that 40% to 60% of patients will have a deep, durable response to imatinib.
The second approach would be to initiate 2G TKIs in newly diagnosed patients. And when they achieve CCyR or major molecular response (MMR), enroll them in a clinical trial.
These trials could investigate a switch to imatinib, use of a lower dose of the 2G TKI, a switch to interferon-alfa, the addition of a CYP3A4 inhibitor (such as grapefruit) and a lower dose, or another investigational option.
And the third approach would be to initiate imatinib or an approved 2G TKI in newly diagnosed patients. When they achieve targeted molecular remission, enroll them in a treatment-discontinuation trial.
Dr Shah pointed out that in the STIM study, 61% of patients remained in complete molecular remission 60 months after discontinuing imatinib, and 40% experienced treatment-free survival.
Taking into account the cost of imatinib and the number of months without treatment, STIM investigators estimated the savings to be €4,587,500, or approximately $6 to $7 million.
Patients who relapsed 6 to 9 months after discontinuing imatinib tended to respond well to a rechallenge with imatinib. But Dr Shah cautioned that, at present, discontinuation should only be performed in the context of a clinical trial. ![]()
NEW YORK—If any oncology drugs warrant a high price, BCR-ABL tyrosine kinase inhibitors (TKIs) could make a strong case, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
TKIs have revolutionized the therapeutic landscape in chronic myeloid leukemia (CML), said Neil P. Shah, MD, PhD, of the UCSF
Helen Diller Family Comprehensive Cancer Center in San Francisco.
Five-year overall survival is 93% in CML patients treated with imatinib. And 80,000 people are estimated to be living with CML in 2014, a number that is expected to double by 2035.
Yet the increase in life expectancy places a burden on the healthcare system, Dr Shah said, particularly since the price of BCR-ABL TKIs has risen dramatically.
A year of imatinib therapy circa 2001 cost approximately $30,000, and by 2013, approximately $92,000. Second-generation (2G) TKIs cost even more, at about $115,000 annually, and the third-generation TKI ponatinib costs about $138,000 annually.
Confounding the financial picture will be the advent of generic imatinib, which will be available in the US in early 2016.
Generic imatinib will, presumably, be less expensive than the brand-name drug. However, it is not clear whether it will be as effective or what impact it will have on the 2G and 3G TKIs.
With all that in mind, Dr Shah provided some options for maximizing therapeutic outcomes in a fiscally responsible manner.
He based his potential solutions on evidence-based premises. First, imatinib is a highly active therapy for many chronic-phase CML patients. The 8-year update of the IRIS study shows that 53% of patients sustain complete cytogenetic remission (CCyR) with imatinib.
Second, patients who are likely to do well on TKI therapy can be identified early based on their BCR-ABL PCR levels after 3 months of therapy.
This important 3-month milestone has been incorporated into the NCCN guidelines. Patients who achieve BCR-ABL/ABL levels of 10% or less have a significantly better overall survival than those who have levels greater than 10%.
Third, the ENESTnd and DASISION studies demonstrated that nilotinib and dasatinib elicit achievement of important treatment milestones (PCR<10% at 3 months and CCyR after 12 months) in a significantly higher proportion of patients than imatinib. But to date, neither agent has produced a significant improvement in overall survival.
And fourth, while nilotinib and dasatinib have an undisputable clinical benefit over imatinib in terms of transformation to accelerated phase/blast crisis (AP/BC), these agents cost between $23,000 and $31,000 more than imatinib for an annual course of treatment.
Dr Shah calculated that to achieve approximately 10 fewer AP/BC transformations over 5 years, approximately 300 patients would need to be treated at an additional cost of $37.5 million. This equates to $3.75 million in additional costs for 1 transformation event spared over 5 years.
“We do have to keep in mind transformation events are not cheap,” he said. “So when these happen, patients need to be hospitalized for chemotherapy, typically, or they have to go to allogeneic stem cell transplantation.”
So Dr Shah proffered 3 potential approaches for fiscally sustainable TKI use.
The first approach would be to initiate imatinib in most, if not all, chronic-phase CML patients. If they achieve BCR-ABL levels <10% at 3 months or partial CyR after 12 months, then continue imatinib. If not, switch to a 2G TKI.
Dr Shah noted that 40% to 60% of patients will have a deep, durable response to imatinib.
The second approach would be to initiate 2G TKIs in newly diagnosed patients. And when they achieve CCyR or major molecular response (MMR), enroll them in a clinical trial.
These trials could investigate a switch to imatinib, use of a lower dose of the 2G TKI, a switch to interferon-alfa, the addition of a CYP3A4 inhibitor (such as grapefruit) and a lower dose, or another investigational option.
And the third approach would be to initiate imatinib or an approved 2G TKI in newly diagnosed patients. When they achieve targeted molecular remission, enroll them in a treatment-discontinuation trial.
Dr Shah pointed out that in the STIM study, 61% of patients remained in complete molecular remission 60 months after discontinuing imatinib, and 40% experienced treatment-free survival.
Taking into account the cost of imatinib and the number of months without treatment, STIM investigators estimated the savings to be €4,587,500, or approximately $6 to $7 million.
Patients who relapsed 6 to 9 months after discontinuing imatinib tended to respond well to a rechallenge with imatinib. But Dr Shah cautioned that, at present, discontinuation should only be performed in the context of a clinical trial.
Method can detect drivers of AML
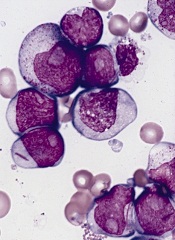
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.”
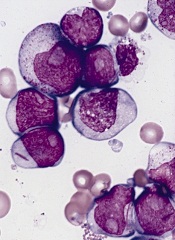
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.”
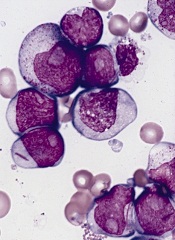
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.”
Murine studies support use of TKIs in ALL subtype

PHILADELPHIA—Experiments in mice reinforce the idea that tyrosine kinase inhibitors (TKIs) can treat patients with Ph-like acute lymphoblastic leukemia (ALL).
Investigators recently identified genomic alterations in Ph-like ALL that suggest these patients might respond to TKIs, and tests in a small number of patients supported this theory.
Now, preclinical results show that kinase fusions in Ph-like ALL activate signaling pathways differently, and this affects sensitivity to TKIs.
Kathryn Roberts, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues presented these results at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We recently described a subtype of B-cell acute lymphoblastic leukemia with very poor outcome that is characterized by genetic alterations involving tyrosine kinases, termed Ph-like ALL,” Dr Roberts said. “We wanted to examine whether these alterations contribute to the development of Ph-like ALL and determine if they could be targeted with tyrosine kinase inhibitors.”
“We showed, for the first time, that the kinase alterations we tested contribute to the development of Ph-like ALL, and that Ph-like ALL can be treated effectively with tyrosine kinase inhibitors in animal models. These findings provide a strong rationale for treating Ph-like ALL patients with targeted therapies to improve their survival.”
Dr Roberts and her colleagues first introduced kinase alterations—RCSD1-ABL2, SSBP2-CSF1R, or PAX5-JAK2—in IL-7-dependent, Arf-/- mouse pre-B cells expressing IK6.
They found that each fusion conferred cytokine-independent growth in vitro. And mice that received transplants of pre-B cells expressing RCSD1-ABL2 or SSBP2-CSF1R developed ALL with a pre-B immunophenotype.
The investigators then assessed the activation of kinase signaling pathways and TKI sensitivity in Arf-/- pre-B cells and human leukemic cells harvested from xenografted mice expressing ETV6-ABL1, RANBP2-ABL1, PAG1-ABL2, RCSD1-ABL2, SSBP2-CSF1R, IGH-EPOR, ATF7IP-JAK2, and PAX5-JAK2.
In both cell types, signaling pathway activation and TKI sensitivity differed according to the kinase fusion.
Cells expressing ABL1-class kinase fusions (ABL1, ABL2, CSF1R, and PDGFRB) exhibited pSTAT5 activation that was inhibited by imatinib or dasatinib. But in cells expressing ATF7IP-JAK2, PAX5-JAK2, or IGH-EPOR, pSTAT5 activation was only inhibited by ruxolitinib.
Finally, the investigators tested dasatinib in xenograft models of ETV6-ABL1, RCSD1-ABL2, PAG1-ABL2, or SSBP2-CSF1R ALL.
They found that treated mice had significantly lower leukemic burdens and splenic weights than control mice. And STAT5 phosphorylation was attenuated in cells from treated mice.
“Our studies show that different FDA-approved TKIs such as imatinib, dasatinib, ruxolitinib, or crizotinib could potentially be used to treat Ph-like ALL patients, depending on the type of kinase alterations their tumors bear,” Dr Roberts said.
“We were able to gain a better understanding of the genetics underlying Ph-like ALL, and our studies could help identify patients who will not respond optimally to current therapy. By knowing the exact genetic alteration upfront, we may be able to implement different therapeutic strategies to improve the survival rate of future patients with ALL.”

PHILADELPHIA—Experiments in mice reinforce the idea that tyrosine kinase inhibitors (TKIs) can treat patients with Ph-like acute lymphoblastic leukemia (ALL).
Investigators recently identified genomic alterations in Ph-like ALL that suggest these patients might respond to TKIs, and tests in a small number of patients supported this theory.
Now, preclinical results show that kinase fusions in Ph-like ALL activate signaling pathways differently, and this affects sensitivity to TKIs.
Kathryn Roberts, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues presented these results at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We recently described a subtype of B-cell acute lymphoblastic leukemia with very poor outcome that is characterized by genetic alterations involving tyrosine kinases, termed Ph-like ALL,” Dr Roberts said. “We wanted to examine whether these alterations contribute to the development of Ph-like ALL and determine if they could be targeted with tyrosine kinase inhibitors.”
“We showed, for the first time, that the kinase alterations we tested contribute to the development of Ph-like ALL, and that Ph-like ALL can be treated effectively with tyrosine kinase inhibitors in animal models. These findings provide a strong rationale for treating Ph-like ALL patients with targeted therapies to improve their survival.”
Dr Roberts and her colleagues first introduced kinase alterations—RCSD1-ABL2, SSBP2-CSF1R, or PAX5-JAK2—in IL-7-dependent, Arf-/- mouse pre-B cells expressing IK6.
They found that each fusion conferred cytokine-independent growth in vitro. And mice that received transplants of pre-B cells expressing RCSD1-ABL2 or SSBP2-CSF1R developed ALL with a pre-B immunophenotype.
The investigators then assessed the activation of kinase signaling pathways and TKI sensitivity in Arf-/- pre-B cells and human leukemic cells harvested from xenografted mice expressing ETV6-ABL1, RANBP2-ABL1, PAG1-ABL2, RCSD1-ABL2, SSBP2-CSF1R, IGH-EPOR, ATF7IP-JAK2, and PAX5-JAK2.
In both cell types, signaling pathway activation and TKI sensitivity differed according to the kinase fusion.
Cells expressing ABL1-class kinase fusions (ABL1, ABL2, CSF1R, and PDGFRB) exhibited pSTAT5 activation that was inhibited by imatinib or dasatinib. But in cells expressing ATF7IP-JAK2, PAX5-JAK2, or IGH-EPOR, pSTAT5 activation was only inhibited by ruxolitinib.
Finally, the investigators tested dasatinib in xenograft models of ETV6-ABL1, RCSD1-ABL2, PAG1-ABL2, or SSBP2-CSF1R ALL.
They found that treated mice had significantly lower leukemic burdens and splenic weights than control mice. And STAT5 phosphorylation was attenuated in cells from treated mice.
“Our studies show that different FDA-approved TKIs such as imatinib, dasatinib, ruxolitinib, or crizotinib could potentially be used to treat Ph-like ALL patients, depending on the type of kinase alterations their tumors bear,” Dr Roberts said.
“We were able to gain a better understanding of the genetics underlying Ph-like ALL, and our studies could help identify patients who will not respond optimally to current therapy. By knowing the exact genetic alteration upfront, we may be able to implement different therapeutic strategies to improve the survival rate of future patients with ALL.”

PHILADELPHIA—Experiments in mice reinforce the idea that tyrosine kinase inhibitors (TKIs) can treat patients with Ph-like acute lymphoblastic leukemia (ALL).
Investigators recently identified genomic alterations in Ph-like ALL that suggest these patients might respond to TKIs, and tests in a small number of patients supported this theory.
Now, preclinical results show that kinase fusions in Ph-like ALL activate signaling pathways differently, and this affects sensitivity to TKIs.
Kathryn Roberts, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues presented these results at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
“We recently described a subtype of B-cell acute lymphoblastic leukemia with very poor outcome that is characterized by genetic alterations involving tyrosine kinases, termed Ph-like ALL,” Dr Roberts said. “We wanted to examine whether these alterations contribute to the development of Ph-like ALL and determine if they could be targeted with tyrosine kinase inhibitors.”
“We showed, for the first time, that the kinase alterations we tested contribute to the development of Ph-like ALL, and that Ph-like ALL can be treated effectively with tyrosine kinase inhibitors in animal models. These findings provide a strong rationale for treating Ph-like ALL patients with targeted therapies to improve their survival.”
Dr Roberts and her colleagues first introduced kinase alterations—RCSD1-ABL2, SSBP2-CSF1R, or PAX5-JAK2—in IL-7-dependent, Arf-/- mouse pre-B cells expressing IK6.
They found that each fusion conferred cytokine-independent growth in vitro. And mice that received transplants of pre-B cells expressing RCSD1-ABL2 or SSBP2-CSF1R developed ALL with a pre-B immunophenotype.
The investigators then assessed the activation of kinase signaling pathways and TKI sensitivity in Arf-/- pre-B cells and human leukemic cells harvested from xenografted mice expressing ETV6-ABL1, RANBP2-ABL1, PAG1-ABL2, RCSD1-ABL2, SSBP2-CSF1R, IGH-EPOR, ATF7IP-JAK2, and PAX5-JAK2.
In both cell types, signaling pathway activation and TKI sensitivity differed according to the kinase fusion.
Cells expressing ABL1-class kinase fusions (ABL1, ABL2, CSF1R, and PDGFRB) exhibited pSTAT5 activation that was inhibited by imatinib or dasatinib. But in cells expressing ATF7IP-JAK2, PAX5-JAK2, or IGH-EPOR, pSTAT5 activation was only inhibited by ruxolitinib.
Finally, the investigators tested dasatinib in xenograft models of ETV6-ABL1, RCSD1-ABL2, PAG1-ABL2, or SSBP2-CSF1R ALL.
They found that treated mice had significantly lower leukemic burdens and splenic weights than control mice. And STAT5 phosphorylation was attenuated in cells from treated mice.
“Our studies show that different FDA-approved TKIs such as imatinib, dasatinib, ruxolitinib, or crizotinib could potentially be used to treat Ph-like ALL patients, depending on the type of kinase alterations their tumors bear,” Dr Roberts said.
“We were able to gain a better understanding of the genetics underlying Ph-like ALL, and our studies could help identify patients who will not respond optimally to current therapy. By knowing the exact genetic alteration upfront, we may be able to implement different therapeutic strategies to improve the survival rate of future patients with ALL.”