User login
Adding Immunoglobulin to HBV Vaccine No Help
Major Finding: The addition of hepatitis B immunoglobulin to hepatitis B prophylaxis with the recombinant HBV vaccine does not confer additional protection to newborns of chronically infected mothers.
Data Source: A randomized controlled trial of 222 infants born to mothers who tested positive for hepatitis B surface antigen.
Disclosures: Dr. Sarin and Dr. Pande reported having no relevant financial disclosures.
BOSTON – The recombinant hepatitis B vaccine confers as much protection when given alone as it does when given together with hepatitis B immunoglobulin to newborns of chronically infected mothers, but neither regimen is optimally effective, a study has shown.
The randomized controlled trial assessed the hepatitis B virus (HBV) status of 222 infants born to mothers who tested positive for hepatitis B surface antigen (HBsAg). The rate of protection observed in infants who received only the vaccine was statistically similar to that of infants who received the vaccine plus hepatitis B immune globulin (HBIG).
A total of 39% of the vaccine-only group and 41% of the combination group remained infection free at a minimum of 18 weeks after birth, Dr. Shiv K. Sarin reported at the meeting noting that nearly half of the babies in both groups developed occult HBV infections.
The current standard of care for preventing HBV infection in babies born to mothers who are HBsAg positive is the recombinant hepatitis B virus vaccine plus HBIG; however, previous studies have suggested the possibility that the vaccine alone may be as effective as the combination therapy, said Dr. Sarin of the Institute of Liver and Biliary Sciences in New Delhi.
To test this hypothesis, Dr. Sarin, along with lead investigator Dr. Chandana Pande, a research associate at G.B. Pant Hospital in New Delhi, and colleagues randomized the newborns of 222 women who screened positive for HBsAg during their prenatal care to receive the 0.5-mL recombinant HBV vaccine at birth, 6 weeks, 10 weeks, and 14 weeks, either alone (116 infants) or with 0.5 mL intramuscular HBIG (106 infants). Mothers on antiviral therapy and those with coinfections were excluded from the investigation, he said.
All of the babies were assessed at a minimum of 18 weeks for HBsAg, HBV-DNA, and antibodies to HBsAg (anti-HBs). The study's primary end point was freedom from overt or occult HBV infection with adequate immune response, defined as anti-HBs titers of at least 10 IU/mL, Dr. Sarin said in a poster presentation.
Babies with overt HBV infection were those whose blood specimens tested positive for HBsAg by enzyme-linked immunosorbent assay, whereas babies with occult infection were negative for HBsAg but positive for HBV-DNA by polymerase chain reaction testing, he said. Babies with no infection but whose anti-HBs titers were less than 10 IU/mL were categorized as having a poor immune response.
At 18 weeks after birth, there were no significant differences between the combination therapy group and monotherapy group with respect to the number of babies meeting the study's primary end point, Dr. Sarin reported. Specifically, 43 babies in the combination group and 45 in the vaccine-only group remained free of overt or occult HBV infection with adequate immune response.
Of the babies not meeting the primary end point, 9 had overt HBV infection, including 2 in the combination group and 7 in the vaccine-only group, and 106 developed occult HBV infection, including 52 in the combination group and 54 in the vaccine-only group, Dr. Sarin said. Neither of these differences attained statistical significance, nor did the between-group difference in the number of infants demonstrating a poor immune response, he said.
Major Finding: The addition of hepatitis B immunoglobulin to hepatitis B prophylaxis with the recombinant HBV vaccine does not confer additional protection to newborns of chronically infected mothers.
Data Source: A randomized controlled trial of 222 infants born to mothers who tested positive for hepatitis B surface antigen.
Disclosures: Dr. Sarin and Dr. Pande reported having no relevant financial disclosures.
BOSTON – The recombinant hepatitis B vaccine confers as much protection when given alone as it does when given together with hepatitis B immunoglobulin to newborns of chronically infected mothers, but neither regimen is optimally effective, a study has shown.
The randomized controlled trial assessed the hepatitis B virus (HBV) status of 222 infants born to mothers who tested positive for hepatitis B surface antigen (HBsAg). The rate of protection observed in infants who received only the vaccine was statistically similar to that of infants who received the vaccine plus hepatitis B immune globulin (HBIG).
A total of 39% of the vaccine-only group and 41% of the combination group remained infection free at a minimum of 18 weeks after birth, Dr. Shiv K. Sarin reported at the meeting noting that nearly half of the babies in both groups developed occult HBV infections.
The current standard of care for preventing HBV infection in babies born to mothers who are HBsAg positive is the recombinant hepatitis B virus vaccine plus HBIG; however, previous studies have suggested the possibility that the vaccine alone may be as effective as the combination therapy, said Dr. Sarin of the Institute of Liver and Biliary Sciences in New Delhi.
To test this hypothesis, Dr. Sarin, along with lead investigator Dr. Chandana Pande, a research associate at G.B. Pant Hospital in New Delhi, and colleagues randomized the newborns of 222 women who screened positive for HBsAg during their prenatal care to receive the 0.5-mL recombinant HBV vaccine at birth, 6 weeks, 10 weeks, and 14 weeks, either alone (116 infants) or with 0.5 mL intramuscular HBIG (106 infants). Mothers on antiviral therapy and those with coinfections were excluded from the investigation, he said.
All of the babies were assessed at a minimum of 18 weeks for HBsAg, HBV-DNA, and antibodies to HBsAg (anti-HBs). The study's primary end point was freedom from overt or occult HBV infection with adequate immune response, defined as anti-HBs titers of at least 10 IU/mL, Dr. Sarin said in a poster presentation.
Babies with overt HBV infection were those whose blood specimens tested positive for HBsAg by enzyme-linked immunosorbent assay, whereas babies with occult infection were negative for HBsAg but positive for HBV-DNA by polymerase chain reaction testing, he said. Babies with no infection but whose anti-HBs titers were less than 10 IU/mL were categorized as having a poor immune response.
At 18 weeks after birth, there were no significant differences between the combination therapy group and monotherapy group with respect to the number of babies meeting the study's primary end point, Dr. Sarin reported. Specifically, 43 babies in the combination group and 45 in the vaccine-only group remained free of overt or occult HBV infection with adequate immune response.
Of the babies not meeting the primary end point, 9 had overt HBV infection, including 2 in the combination group and 7 in the vaccine-only group, and 106 developed occult HBV infection, including 52 in the combination group and 54 in the vaccine-only group, Dr. Sarin said. Neither of these differences attained statistical significance, nor did the between-group difference in the number of infants demonstrating a poor immune response, he said.
Major Finding: The addition of hepatitis B immunoglobulin to hepatitis B prophylaxis with the recombinant HBV vaccine does not confer additional protection to newborns of chronically infected mothers.
Data Source: A randomized controlled trial of 222 infants born to mothers who tested positive for hepatitis B surface antigen.
Disclosures: Dr. Sarin and Dr. Pande reported having no relevant financial disclosures.
BOSTON – The recombinant hepatitis B vaccine confers as much protection when given alone as it does when given together with hepatitis B immunoglobulin to newborns of chronically infected mothers, but neither regimen is optimally effective, a study has shown.
The randomized controlled trial assessed the hepatitis B virus (HBV) status of 222 infants born to mothers who tested positive for hepatitis B surface antigen (HBsAg). The rate of protection observed in infants who received only the vaccine was statistically similar to that of infants who received the vaccine plus hepatitis B immune globulin (HBIG).
A total of 39% of the vaccine-only group and 41% of the combination group remained infection free at a minimum of 18 weeks after birth, Dr. Shiv K. Sarin reported at the meeting noting that nearly half of the babies in both groups developed occult HBV infections.
The current standard of care for preventing HBV infection in babies born to mothers who are HBsAg positive is the recombinant hepatitis B virus vaccine plus HBIG; however, previous studies have suggested the possibility that the vaccine alone may be as effective as the combination therapy, said Dr. Sarin of the Institute of Liver and Biliary Sciences in New Delhi.
To test this hypothesis, Dr. Sarin, along with lead investigator Dr. Chandana Pande, a research associate at G.B. Pant Hospital in New Delhi, and colleagues randomized the newborns of 222 women who screened positive for HBsAg during their prenatal care to receive the 0.5-mL recombinant HBV vaccine at birth, 6 weeks, 10 weeks, and 14 weeks, either alone (116 infants) or with 0.5 mL intramuscular HBIG (106 infants). Mothers on antiviral therapy and those with coinfections were excluded from the investigation, he said.
All of the babies were assessed at a minimum of 18 weeks for HBsAg, HBV-DNA, and antibodies to HBsAg (anti-HBs). The study's primary end point was freedom from overt or occult HBV infection with adequate immune response, defined as anti-HBs titers of at least 10 IU/mL, Dr. Sarin said in a poster presentation.
Babies with overt HBV infection were those whose blood specimens tested positive for HBsAg by enzyme-linked immunosorbent assay, whereas babies with occult infection were negative for HBsAg but positive for HBV-DNA by polymerase chain reaction testing, he said. Babies with no infection but whose anti-HBs titers were less than 10 IU/mL were categorized as having a poor immune response.
At 18 weeks after birth, there were no significant differences between the combination therapy group and monotherapy group with respect to the number of babies meeting the study's primary end point, Dr. Sarin reported. Specifically, 43 babies in the combination group and 45 in the vaccine-only group remained free of overt or occult HBV infection with adequate immune response.
Of the babies not meeting the primary end point, 9 had overt HBV infection, including 2 in the combination group and 7 in the vaccine-only group, and 106 developed occult HBV infection, including 52 in the combination group and 54 in the vaccine-only group, Dr. Sarin said. Neither of these differences attained statistical significance, nor did the between-group difference in the number of infants demonstrating a poor immune response, he said.
From the Annual Meeting of the American Association for the Study of Liver Diseases
Birth Rate for U.S. Teens Falls to Lowest Level
The birth rate for U.S. teens aged 15-19 years fell to the lowest level since recording began in 1940, according to new data for 2009.
The 2009 teen birth rate was 39.1 births per 1,000 teens, down 6% from the 2008 rate of 41.5 births per 1,000, according to the report by the CDC National Center for Health Statistics. The 2009 rate was 37% lower than in 1991, the peak year for teen births. The CDC's annual report is based on virtually 100% of vital records collected in the 50 U.S. states, the District of Columbia, and U.S. territories. The report is available at www.cdc.gov/nchs
Overall fertility also fell in 2009 to 66.7 births per 1,000 women aged 15-44 years, compared with 68.6 per 1,000 women in 2008. The CDC's preliminary estimate of births in 2009 was 4,131,019, 3% less than 2008. Early data through June 2010 suggest that the decline in fertility has continued, according to the report.
Fertility rates increased in only one age group: women aged 40-44 years. In that group, the 2009 rate was 10.1 births per 1,000 women, up 3% from the 2008 figure and the highest rate since 1967.
The rate of preterm births declined for the third straight year, to 12.2% of all births in 2009. The rate of cesarean deliveries rose to a record high of 32.9% in 2009, up from 32.3% in 2008.
The low birth weight rate remained unchanged at about 8.2% between 2008 and 2009.
The CDC also reported the total fertility rate (TFR) – an estimate of the number of births that a hypothetical group of 1,000 women would have over their lifetimes, based on the age-specific rates of a particular year. The TFR for 2009 was 2,007.5, down 4% from the rate in 2008. This is the largest decline in TFR since 1973. The 2008 and 2009 rates were both below the replacement rate of 2,100 births per 1,000 women. The U.S. TFR was below replacement for every year between 1972 and 2005 and above replacement in 2006 and 2007.
The birth rate for U.S. teens aged 15-19 years fell to the lowest level since recording began in 1940, according to new data for 2009.
The 2009 teen birth rate was 39.1 births per 1,000 teens, down 6% from the 2008 rate of 41.5 births per 1,000, according to the report by the CDC National Center for Health Statistics. The 2009 rate was 37% lower than in 1991, the peak year for teen births. The CDC's annual report is based on virtually 100% of vital records collected in the 50 U.S. states, the District of Columbia, and U.S. territories. The report is available at www.cdc.gov/nchs
Overall fertility also fell in 2009 to 66.7 births per 1,000 women aged 15-44 years, compared with 68.6 per 1,000 women in 2008. The CDC's preliminary estimate of births in 2009 was 4,131,019, 3% less than 2008. Early data through June 2010 suggest that the decline in fertility has continued, according to the report.
Fertility rates increased in only one age group: women aged 40-44 years. In that group, the 2009 rate was 10.1 births per 1,000 women, up 3% from the 2008 figure and the highest rate since 1967.
The rate of preterm births declined for the third straight year, to 12.2% of all births in 2009. The rate of cesarean deliveries rose to a record high of 32.9% in 2009, up from 32.3% in 2008.
The low birth weight rate remained unchanged at about 8.2% between 2008 and 2009.
The CDC also reported the total fertility rate (TFR) – an estimate of the number of births that a hypothetical group of 1,000 women would have over their lifetimes, based on the age-specific rates of a particular year. The TFR for 2009 was 2,007.5, down 4% from the rate in 2008. This is the largest decline in TFR since 1973. The 2008 and 2009 rates were both below the replacement rate of 2,100 births per 1,000 women. The U.S. TFR was below replacement for every year between 1972 and 2005 and above replacement in 2006 and 2007.
The birth rate for U.S. teens aged 15-19 years fell to the lowest level since recording began in 1940, according to new data for 2009.
The 2009 teen birth rate was 39.1 births per 1,000 teens, down 6% from the 2008 rate of 41.5 births per 1,000, according to the report by the CDC National Center for Health Statistics. The 2009 rate was 37% lower than in 1991, the peak year for teen births. The CDC's annual report is based on virtually 100% of vital records collected in the 50 U.S. states, the District of Columbia, and U.S. territories. The report is available at www.cdc.gov/nchs
Overall fertility also fell in 2009 to 66.7 births per 1,000 women aged 15-44 years, compared with 68.6 per 1,000 women in 2008. The CDC's preliminary estimate of births in 2009 was 4,131,019, 3% less than 2008. Early data through June 2010 suggest that the decline in fertility has continued, according to the report.
Fertility rates increased in only one age group: women aged 40-44 years. In that group, the 2009 rate was 10.1 births per 1,000 women, up 3% from the 2008 figure and the highest rate since 1967.
The rate of preterm births declined for the third straight year, to 12.2% of all births in 2009. The rate of cesarean deliveries rose to a record high of 32.9% in 2009, up from 32.3% in 2008.
The low birth weight rate remained unchanged at about 8.2% between 2008 and 2009.
The CDC also reported the total fertility rate (TFR) – an estimate of the number of births that a hypothetical group of 1,000 women would have over their lifetimes, based on the age-specific rates of a particular year. The TFR for 2009 was 2,007.5, down 4% from the rate in 2008. This is the largest decline in TFR since 1973. The 2008 and 2009 rates were both below the replacement rate of 2,100 births per 1,000 women. The U.S. TFR was below replacement for every year between 1972 and 2005 and above replacement in 2006 and 2007.
From the Centers For Disease Control and Prevention
If Possible, Delay Delivery Until 39 Weeks
Neonates who are delivered at 36-38 weeks' gestation after fetal lung maturity is confirmed have nearly double the risk of adverse outcomes, compared with neonates delivered at 39 or 40 weeks, a large retrospective cohort study has shown.
The mean birth weight in 459 neonates with confirmed lung maturity who were delivered at 36-38 weeks' gestation was 3,017 g, compared with 3,362 g in 13,339 neonates delivered at 39-40 weeks. The risk of a composite outcome including death, adverse respiratory outcomes, hypoglycemia, treated hyperbilirubinemia, generalized seizures, necrotizing enterocolitis, hypoxic ischemic encephalopathy, periventricular leukomalacia, and suspected or proven sepsis was 6.1% in those in the 36- to 38-week group, compared with 2.5% in the 39- to 40-week group, Dr. Elizabeth Bates of the University of Alabama at Birmingham and her colleagues reported.
Early delivery remained a significant risk factor for the composite outcome after investigators adjusted for maternal age, ethnicity, parity, neonatal sex, intended mode of delivery, and any medical complication – including diabetes and hypertension. Early delivery was also a significant risk factor for several individual outcomes, including respiratory distress syndrome (adjusted odds ratio, 7.6); treated hyperbilirubinemia (AOR, 11.2); and hypoglycemia (AOR, 5.8), the investigators found (Obstet. Gynecol. 2010; 116:1288-95).
The incidence of the primary composite outcome generally decreased with increasing gestational age, they noted (9.2% incidence at 36 weeks, 3.2% at 37 weeks, 5.2% at 38 weeks, and 2.5% at 39-40 weeks).
Patients included in the study were women with a singleton pregnancy receiving prenatal care and giving birth at a single center from January 1999 to December 2008. Among those who were delivered at 36-38 weeks following documentation of fetal lung maturity, 42.5% had completed 36 weeks, 40.7% had completed 37 weeks, and only 16.8% had completed 38 weeks. Of those who were delivered at 38-40 weeks, 56.2% had completed 39 weeks, and 43.8% had completed 40 weeks. The mean gestational age was 37.1 weeks in those delivered at 36-38 weeks and was 39.8 weeks in those who delivered at 38-40 weeks.
The study findings are concerning, because fetal lung maturity is known to reduce the risk of respiratory morbidity, and confirmation of fetal lung maturity is “a recognized exception to longstanding recommendations against elective delivery before 39 weeks' gestation,” Dr. Bates and her associates noted.
Also, despite existing recommendations to the contrary, one-third of elective cesarean deliveries in one large study were performed before 39 weeks, they said.
Taken together, the findings in the current study “are consistent with relative immaturity at 36-38 weeks (regardless of lung maturity), compared with 39-40 weeks, and lower threshold for admission to the NICU and for invasive sepsis work-ups (suspected sepsis),” the investigators wrote.
They added that the findings should be considered in light of the study's limitations – including the retrospective study design and the related possibility of confounding, and the fact that the study does not fully address the risk of stillbirth associated with either delivery strategy studied. Nonetheless, they concluded that the findings suggest that “in the absence of ongoing concern about fetal death or maternal well-being if the pregnancy continued, delivery should be delayed until 39 weeks.”
The findings also suggest that purely elective fetal lung maturity testing and early delivery should be avoided, Dr. Bates and her associates noted.
One of the study authors, Dr. Alan T. N. Tita, was a Women's Reproductive Health Research Advanced Scholar at the University of Alabama at Birmingham at the time of the study and received funding from the National Institute of Child Health and Human Development. No relevant financial disclosures were reported by the other authors.
View on The News
Reconsider What Constitutes Term Birth
“This paper further advances our understanding of the optimal conditions for delivering a baby free of major health complications. Specifically, it confirms findings from a number of previous studies suggesting that babies born before 39 weeks' gestation have a significantly increased risk of complications, including respiratory distress syndrome, even if their lungs appear to be fully mature via biomarker testing,” Dr. E. Albert Reece said in an interview.
More importantly, he said, the study suggests that current definitions of what constitute a term birth may need to be reconsidered.
“Indeed, currently babies born between 37 and 42 completed weeks of pregnancy are considered full term, whereas babies born before 37 weeks of pregnancy are completed are considered preterm. However, if the results of this study are to be believed, they suggest that babies born before 39 weeks of gestation might be considered preterm as well.”
This may mean that the definition for term needs to be revised upward to 39-42 weeks, he added.
“It also means that physicians should try to do everything possible to keep from delivering women until they've reached 39 weeks of gestation, unless there are valid reasons for delivery to protect the health of the mother,” he said.
Vitals
DR. REECE is the John Z. and Akiko K. Bowers Distinguished Professor and dean of the University of Maryland School of Medicine, Baltimore. He is also professor in the departments of obstetrics and gynecology, medicine, and biochemistry and molecular biology. Dr. Reece said he had no relevant financial disclosures.
Neonates who are delivered at 36-38 weeks' gestation after fetal lung maturity is confirmed have nearly double the risk of adverse outcomes, compared with neonates delivered at 39 or 40 weeks, a large retrospective cohort study has shown.
The mean birth weight in 459 neonates with confirmed lung maturity who were delivered at 36-38 weeks' gestation was 3,017 g, compared with 3,362 g in 13,339 neonates delivered at 39-40 weeks. The risk of a composite outcome including death, adverse respiratory outcomes, hypoglycemia, treated hyperbilirubinemia, generalized seizures, necrotizing enterocolitis, hypoxic ischemic encephalopathy, periventricular leukomalacia, and suspected or proven sepsis was 6.1% in those in the 36- to 38-week group, compared with 2.5% in the 39- to 40-week group, Dr. Elizabeth Bates of the University of Alabama at Birmingham and her colleagues reported.
Early delivery remained a significant risk factor for the composite outcome after investigators adjusted for maternal age, ethnicity, parity, neonatal sex, intended mode of delivery, and any medical complication – including diabetes and hypertension. Early delivery was also a significant risk factor for several individual outcomes, including respiratory distress syndrome (adjusted odds ratio, 7.6); treated hyperbilirubinemia (AOR, 11.2); and hypoglycemia (AOR, 5.8), the investigators found (Obstet. Gynecol. 2010; 116:1288-95).
The incidence of the primary composite outcome generally decreased with increasing gestational age, they noted (9.2% incidence at 36 weeks, 3.2% at 37 weeks, 5.2% at 38 weeks, and 2.5% at 39-40 weeks).
Patients included in the study were women with a singleton pregnancy receiving prenatal care and giving birth at a single center from January 1999 to December 2008. Among those who were delivered at 36-38 weeks following documentation of fetal lung maturity, 42.5% had completed 36 weeks, 40.7% had completed 37 weeks, and only 16.8% had completed 38 weeks. Of those who were delivered at 38-40 weeks, 56.2% had completed 39 weeks, and 43.8% had completed 40 weeks. The mean gestational age was 37.1 weeks in those delivered at 36-38 weeks and was 39.8 weeks in those who delivered at 38-40 weeks.
The study findings are concerning, because fetal lung maturity is known to reduce the risk of respiratory morbidity, and confirmation of fetal lung maturity is “a recognized exception to longstanding recommendations against elective delivery before 39 weeks' gestation,” Dr. Bates and her associates noted.
Also, despite existing recommendations to the contrary, one-third of elective cesarean deliveries in one large study were performed before 39 weeks, they said.
Taken together, the findings in the current study “are consistent with relative immaturity at 36-38 weeks (regardless of lung maturity), compared with 39-40 weeks, and lower threshold for admission to the NICU and for invasive sepsis work-ups (suspected sepsis),” the investigators wrote.
They added that the findings should be considered in light of the study's limitations – including the retrospective study design and the related possibility of confounding, and the fact that the study does not fully address the risk of stillbirth associated with either delivery strategy studied. Nonetheless, they concluded that the findings suggest that “in the absence of ongoing concern about fetal death or maternal well-being if the pregnancy continued, delivery should be delayed until 39 weeks.”
The findings also suggest that purely elective fetal lung maturity testing and early delivery should be avoided, Dr. Bates and her associates noted.
One of the study authors, Dr. Alan T. N. Tita, was a Women's Reproductive Health Research Advanced Scholar at the University of Alabama at Birmingham at the time of the study and received funding from the National Institute of Child Health and Human Development. No relevant financial disclosures were reported by the other authors.
View on The News
Reconsider What Constitutes Term Birth
“This paper further advances our understanding of the optimal conditions for delivering a baby free of major health complications. Specifically, it confirms findings from a number of previous studies suggesting that babies born before 39 weeks' gestation have a significantly increased risk of complications, including respiratory distress syndrome, even if their lungs appear to be fully mature via biomarker testing,” Dr. E. Albert Reece said in an interview.
More importantly, he said, the study suggests that current definitions of what constitute a term birth may need to be reconsidered.
“Indeed, currently babies born between 37 and 42 completed weeks of pregnancy are considered full term, whereas babies born before 37 weeks of pregnancy are completed are considered preterm. However, if the results of this study are to be believed, they suggest that babies born before 39 weeks of gestation might be considered preterm as well.”
This may mean that the definition for term needs to be revised upward to 39-42 weeks, he added.
“It also means that physicians should try to do everything possible to keep from delivering women until they've reached 39 weeks of gestation, unless there are valid reasons for delivery to protect the health of the mother,” he said.
Vitals
DR. REECE is the John Z. and Akiko K. Bowers Distinguished Professor and dean of the University of Maryland School of Medicine, Baltimore. He is also professor in the departments of obstetrics and gynecology, medicine, and biochemistry and molecular biology. Dr. Reece said he had no relevant financial disclosures.
Neonates who are delivered at 36-38 weeks' gestation after fetal lung maturity is confirmed have nearly double the risk of adverse outcomes, compared with neonates delivered at 39 or 40 weeks, a large retrospective cohort study has shown.
The mean birth weight in 459 neonates with confirmed lung maturity who were delivered at 36-38 weeks' gestation was 3,017 g, compared with 3,362 g in 13,339 neonates delivered at 39-40 weeks. The risk of a composite outcome including death, adverse respiratory outcomes, hypoglycemia, treated hyperbilirubinemia, generalized seizures, necrotizing enterocolitis, hypoxic ischemic encephalopathy, periventricular leukomalacia, and suspected or proven sepsis was 6.1% in those in the 36- to 38-week group, compared with 2.5% in the 39- to 40-week group, Dr. Elizabeth Bates of the University of Alabama at Birmingham and her colleagues reported.
Early delivery remained a significant risk factor for the composite outcome after investigators adjusted for maternal age, ethnicity, parity, neonatal sex, intended mode of delivery, and any medical complication – including diabetes and hypertension. Early delivery was also a significant risk factor for several individual outcomes, including respiratory distress syndrome (adjusted odds ratio, 7.6); treated hyperbilirubinemia (AOR, 11.2); and hypoglycemia (AOR, 5.8), the investigators found (Obstet. Gynecol. 2010; 116:1288-95).
The incidence of the primary composite outcome generally decreased with increasing gestational age, they noted (9.2% incidence at 36 weeks, 3.2% at 37 weeks, 5.2% at 38 weeks, and 2.5% at 39-40 weeks).
Patients included in the study were women with a singleton pregnancy receiving prenatal care and giving birth at a single center from January 1999 to December 2008. Among those who were delivered at 36-38 weeks following documentation of fetal lung maturity, 42.5% had completed 36 weeks, 40.7% had completed 37 weeks, and only 16.8% had completed 38 weeks. Of those who were delivered at 38-40 weeks, 56.2% had completed 39 weeks, and 43.8% had completed 40 weeks. The mean gestational age was 37.1 weeks in those delivered at 36-38 weeks and was 39.8 weeks in those who delivered at 38-40 weeks.
The study findings are concerning, because fetal lung maturity is known to reduce the risk of respiratory morbidity, and confirmation of fetal lung maturity is “a recognized exception to longstanding recommendations against elective delivery before 39 weeks' gestation,” Dr. Bates and her associates noted.
Also, despite existing recommendations to the contrary, one-third of elective cesarean deliveries in one large study were performed before 39 weeks, they said.
Taken together, the findings in the current study “are consistent with relative immaturity at 36-38 weeks (regardless of lung maturity), compared with 39-40 weeks, and lower threshold for admission to the NICU and for invasive sepsis work-ups (suspected sepsis),” the investigators wrote.
They added that the findings should be considered in light of the study's limitations – including the retrospective study design and the related possibility of confounding, and the fact that the study does not fully address the risk of stillbirth associated with either delivery strategy studied. Nonetheless, they concluded that the findings suggest that “in the absence of ongoing concern about fetal death or maternal well-being if the pregnancy continued, delivery should be delayed until 39 weeks.”
The findings also suggest that purely elective fetal lung maturity testing and early delivery should be avoided, Dr. Bates and her associates noted.
One of the study authors, Dr. Alan T. N. Tita, was a Women's Reproductive Health Research Advanced Scholar at the University of Alabama at Birmingham at the time of the study and received funding from the National Institute of Child Health and Human Development. No relevant financial disclosures were reported by the other authors.
View on The News
Reconsider What Constitutes Term Birth
“This paper further advances our understanding of the optimal conditions for delivering a baby free of major health complications. Specifically, it confirms findings from a number of previous studies suggesting that babies born before 39 weeks' gestation have a significantly increased risk of complications, including respiratory distress syndrome, even if their lungs appear to be fully mature via biomarker testing,” Dr. E. Albert Reece said in an interview.
More importantly, he said, the study suggests that current definitions of what constitute a term birth may need to be reconsidered.
“Indeed, currently babies born between 37 and 42 completed weeks of pregnancy are considered full term, whereas babies born before 37 weeks of pregnancy are completed are considered preterm. However, if the results of this study are to be believed, they suggest that babies born before 39 weeks of gestation might be considered preterm as well.”
This may mean that the definition for term needs to be revised upward to 39-42 weeks, he added.
“It also means that physicians should try to do everything possible to keep from delivering women until they've reached 39 weeks of gestation, unless there are valid reasons for delivery to protect the health of the mother,” he said.
Vitals
DR. REECE is the John Z. and Akiko K. Bowers Distinguished Professor and dean of the University of Maryland School of Medicine, Baltimore. He is also professor in the departments of obstetrics and gynecology, medicine, and biochemistry and molecular biology. Dr. Reece said he had no relevant financial disclosures.
From Obstetrics & Gynecology
UPDATE ON OBSTETRICS
- How to manage a short cervix to lower the risk of preterm delivery
Joseph R. Wax, MD (May 2010) - When is VBAC appropriate?
Aviva Lee-Parritz, MD (July 2010) - What can be safer than having a baby in the USA? (Commentary)
Louis L. Weinstein, MD (May 2010)
From an evolutionary standpoint, not much has changed in pregnancy and childbirth. From a clinical perspective, however, flux is a constant. Three issues, in particular, have seen notable development over the past year:
- optimal timing of elective delivery
- screening for thrombophilias in women who experience recurrent pregnancy loss, fetal growth restriction, preeclampsia, or placental abruption
- use of magnesium sulfate for fetal neuroprotection.
Of course, in the specialties of obstetrics and perinatal medicine, research continues in a variety of other subject areas, as well. Simulation training, diagnosis and management of gestational diabetes, and rescue steroid treatment are three examples. Other issues being explored include the use of progesterone to prevent prematurity, the use of ultrasonography to measure cervical length, and the safety of vaginal birth after cesarean delivery. The three areas highlighted here are not the only ones “ready for prime time,” but they are areas of considerable interest and debate.
We have a tradition in obstetrics of not embracing change too quickly. We learned this lesson through our experience with diethylstilbestrol (DES) and thalidomide, and we must continue to use caution whenever new technologies or management approaches are proposed.
30 weeks is the rule, provided delivery is truly elective
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
When it comes to elective delivery, no one would argue against the wisdom of continuing pregnancy until at least 39 weeks’ gestation in the absence of complications. But what data form the basis of this wisdom, and when might it be prudent to consider earlier delivery?
In a widely publicized study, Tita and colleagues concluded that elective repeat cesarean delivery before 39 weeks of gestation (i.e., 37 through 38-6/7 weeks) is associated with a higher rate of neonatal respiratory distress and other adverse neonatal outcomes than is delivery at 39 to 40 weeks. Note, however, that the primary outcome of this study was a composite. Therefore, the findings should be interpreted with some caution.
In their report, Tita and coworkers acknowledged that the transient and predominantly minor complications associated with delivery before 39 weeks must be weighed against the risk of fetal death inherent in delaying delivery through 38 full weeks—and an accompanying editorial made the same point.1 Stillbirth occurs at a rate of 1 case for every 1,000 births in the 37- to 39-week gestational age range—a rate that may be higher than the risks associated with delivery. Even so, the risk of stillbirth at 37 to 39 weeks is very small, and that risk is unlikely to be lowered through routine antenatal fetal testing. We should also remember that the risks of neonatal respiratory distress, transient tachypnea, admission to the neonatal intensive care unit (NICU), and even cerebral palsy2 may be increased with delivery at 37 to 38 weeks, or at 42 weeks or later, compared with delivery at 40 weeks.
All truly elective deliveries should occur at or after 39 weeks of gestation. However, when indicated, earlier delivery is acceptable—even essential—if we are to minimize maternal and neonatal morbidity and mortality in high-risk circumstances, such as hypertensive disorders of pregnancy, placenta previa, fetal growth restriction, and other conditions.
Investigations are under way to determine whether there is a role for routine betamethasone administration (regardless of indication or gestational age) in the absence of labor before 39 weeks. Until those data come in, we should continue to follow current practice guidelines for antenatal maternal administration of betamethasone—namely, a single course given between 24 and 34 weeks in women who have an elevated risk of preterm delivery.
Population-based screening for thrombophilias is not recommended
Silver RM, Zhao Y, Spong CY, et al, for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (NICHD MFMU) Network. Prothrombin gene G20210A mutation and obstetric complications. Obstet Gynecol. 2010;115(1):14–20.
Said JM, Higgins JR, Moses EK, et al. Inherited thrombophilia polymorphisms and pregnancy outcomes in nulliparous women. Obstet Gynecol. 2010;115(1):5–13.
Since the mid-1990s, screening for thrombophilias has been recommended in the evaluation of a variety of adverse reproductive outcomes, including, but not limited to:
- recurrent pregnancy loss
- unexplained stillbirth
- placental abruption
- preeclampsia
- fetal growth restriction.
When a thrombophilia is detected in these settings, the practitioner faces a dilemma—namely, what to do when the mother is otherwise healthy and asymptomatic. All too often the finding of a thrombophilia leads to the initiation of some anticoagulation regimen, ranging from low-dose aspirin all the way to therapeutic anticoagulation with heparin.
Over the past year, several studies and expert opinions have been published that recast the role of thrombophilia screening in obstetric practice.
Writing for the Maternal-Fetal Medicine Units (MFMU) Network, Silver and colleagues concluded that the prothrombin (PT) gene mutation G20210A was not associated with pregnancy loss, preeclampsia, fetal growth restriction, or placental abruption in a low-risk, prospective cohort.
Said and coworkers reached a similar conclusion. In a blinded, prospective cohort study, they screened for the following mutations in 2,034 healthy nulliparous women before 22 weeks’ gestation:
- factor V Leiden mutation
- PT gene G20210A mutation
- methylenetetrahydrofolate reductase enzyme (MTHFR) C677T
- MTHFR A1298C
- thrombomodulin polymorphism.
The majority of asymptomatic women who carried an inherited thrombophilia polymorphism had a successful pregnancy outcome. In fact, homozygosity of the MTHFR A1298C mutation was found to be protective.
Population-based screening for thrombophilias is not recommended. In fact, some authors have advised against screening for thrombophilias even in the setting of a thrombotic event, suggesting it has limited utility.3
The main reason to screen for a thrombophilia at this time is to explore idiopathic thrombosis or a strong family history of the same. There is no need to screen for thrombophilias when the patient has a history of pregnancy loss, placental abruption, preeclampsia, and fetal growth restriction.
If you give magnesium sulfate for fetal neuroprotection, adhere to a protocol
ACOG Committee Opinion No. 455: Magnesium sulfate before anticipated preterm birth for neuroprotection. Obstet Gynecol. 2010;115(3):669–671.
Magnesium sulfate has a long and glorious history in obstetrics, having been used to prevent eclampsia, to treat preterm uterine contractions, and now, potentially, to reduce the incidence of central nervous system damage among prematurely delivered infants.
Cerebral palsy (CP) is most commonly associated with prematurity and intrauterine fetal infection. Only in the past two decades has there been a shift away from assigning the cause of most cases of CP to intrapartum events. Nevertheless, CP remains an important concern among patients and providers, and research continues to find ways to prevent CP or minimize its effects.
Numerous large trials have explored the use of magnesium sulfate to prevent CP in preterm infants. Although their findings have not been as definitive as researchers had hoped, some data do suggest that magnesium sulfate has a protective effect.
The American Congress of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) urge caution in regard to the use of magnesium sulfate for fetal neuroprotection. The SMFM points out that the reported benefits of magnesium sulfate in this setting have been derived largely from secondary analyses. The SMFM recommends that, if magnesium is used at all, it should be administered according to one of the published protocols (three are cited in the ACOG opinion).
The SMFM goes on to warn against choosing magnesium sulfate as a tocolytic solely because of its possible neuroprotective effects.
In a Committee Opinion published last year, ACOG was a bit more definite. “The Committee on Obstetric Practice and the Society for Maternal-Fetal Medicine recognize that none of the individual studies found a benefit with regard to their primary outcome,” the opinion states. “However, the available evidence suggests that magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, concurrent tocolysis, and monitoring in concordance with one of the larger trials.”
Recent editorials have cautioned against using magnesium sulfate for fetal neuroprotection until more data become available,4 or have left it up to the individual practitioners (or institution) to decide whether it is advisable.5
The use of magnesium sulfate for fetal neuroprotection when preterm delivery seems likely requires additional research. For now, this practice should be governed strictly by protocol. And it should not be viewed as “standard of care” by our legal colleagues.
When administering magnesium sulfate, avoid giving a cumulative total in excess of 50 g, as this amount may increase the risk of pediatric death.6
We want to hear from you! Tell us what you think.
1. Greene MF. Making small risks even smaller. N Engl J Med. 2009;360(2):183-184.
2. Moster D, Wilcox AJ, Vollset SE, Markestad T, Lie RT. Cerebral palsy among term and postterm births. JAMA. 2010;304(9):976-982.
3. Scifres CM, Macones GA. The utility of thrombophilia testing in pregnant women with thrombosis; fact or fiction? Am J Obstet Gynecol. 2008;199(4):344.e1–7.-
4. Stanley FJ, Crowther C. Antenatal magnesium sulfate for neuroprotection before preterm birth? N Engl J Med. 2008;359(9):962-964.
5. Macones GA. MgSO4 for CP prevention: too good to be true? Am J Obstet Gynecol. 2009;200(6):589.-
6. Mittendorf R, Covert R, Boman J, et al. Is tocolytic magnesium sulfate associated with increased total paediatric mortality? Lancet. 1997;350(9090):1517-1518.
- How to manage a short cervix to lower the risk of preterm delivery
Joseph R. Wax, MD (May 2010) - When is VBAC appropriate?
Aviva Lee-Parritz, MD (July 2010) - What can be safer than having a baby in the USA? (Commentary)
Louis L. Weinstein, MD (May 2010)
From an evolutionary standpoint, not much has changed in pregnancy and childbirth. From a clinical perspective, however, flux is a constant. Three issues, in particular, have seen notable development over the past year:
- optimal timing of elective delivery
- screening for thrombophilias in women who experience recurrent pregnancy loss, fetal growth restriction, preeclampsia, or placental abruption
- use of magnesium sulfate for fetal neuroprotection.
Of course, in the specialties of obstetrics and perinatal medicine, research continues in a variety of other subject areas, as well. Simulation training, diagnosis and management of gestational diabetes, and rescue steroid treatment are three examples. Other issues being explored include the use of progesterone to prevent prematurity, the use of ultrasonography to measure cervical length, and the safety of vaginal birth after cesarean delivery. The three areas highlighted here are not the only ones “ready for prime time,” but they are areas of considerable interest and debate.
We have a tradition in obstetrics of not embracing change too quickly. We learned this lesson through our experience with diethylstilbestrol (DES) and thalidomide, and we must continue to use caution whenever new technologies or management approaches are proposed.
30 weeks is the rule, provided delivery is truly elective
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
When it comes to elective delivery, no one would argue against the wisdom of continuing pregnancy until at least 39 weeks’ gestation in the absence of complications. But what data form the basis of this wisdom, and when might it be prudent to consider earlier delivery?
In a widely publicized study, Tita and colleagues concluded that elective repeat cesarean delivery before 39 weeks of gestation (i.e., 37 through 38-6/7 weeks) is associated with a higher rate of neonatal respiratory distress and other adverse neonatal outcomes than is delivery at 39 to 40 weeks. Note, however, that the primary outcome of this study was a composite. Therefore, the findings should be interpreted with some caution.
In their report, Tita and coworkers acknowledged that the transient and predominantly minor complications associated with delivery before 39 weeks must be weighed against the risk of fetal death inherent in delaying delivery through 38 full weeks—and an accompanying editorial made the same point.1 Stillbirth occurs at a rate of 1 case for every 1,000 births in the 37- to 39-week gestational age range—a rate that may be higher than the risks associated with delivery. Even so, the risk of stillbirth at 37 to 39 weeks is very small, and that risk is unlikely to be lowered through routine antenatal fetal testing. We should also remember that the risks of neonatal respiratory distress, transient tachypnea, admission to the neonatal intensive care unit (NICU), and even cerebral palsy2 may be increased with delivery at 37 to 38 weeks, or at 42 weeks or later, compared with delivery at 40 weeks.
All truly elective deliveries should occur at or after 39 weeks of gestation. However, when indicated, earlier delivery is acceptable—even essential—if we are to minimize maternal and neonatal morbidity and mortality in high-risk circumstances, such as hypertensive disorders of pregnancy, placenta previa, fetal growth restriction, and other conditions.
Investigations are under way to determine whether there is a role for routine betamethasone administration (regardless of indication or gestational age) in the absence of labor before 39 weeks. Until those data come in, we should continue to follow current practice guidelines for antenatal maternal administration of betamethasone—namely, a single course given between 24 and 34 weeks in women who have an elevated risk of preterm delivery.
Population-based screening for thrombophilias is not recommended
Silver RM, Zhao Y, Spong CY, et al, for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (NICHD MFMU) Network. Prothrombin gene G20210A mutation and obstetric complications. Obstet Gynecol. 2010;115(1):14–20.
Said JM, Higgins JR, Moses EK, et al. Inherited thrombophilia polymorphisms and pregnancy outcomes in nulliparous women. Obstet Gynecol. 2010;115(1):5–13.
Since the mid-1990s, screening for thrombophilias has been recommended in the evaluation of a variety of adverse reproductive outcomes, including, but not limited to:
- recurrent pregnancy loss
- unexplained stillbirth
- placental abruption
- preeclampsia
- fetal growth restriction.
When a thrombophilia is detected in these settings, the practitioner faces a dilemma—namely, what to do when the mother is otherwise healthy and asymptomatic. All too often the finding of a thrombophilia leads to the initiation of some anticoagulation regimen, ranging from low-dose aspirin all the way to therapeutic anticoagulation with heparin.
Over the past year, several studies and expert opinions have been published that recast the role of thrombophilia screening in obstetric practice.
Writing for the Maternal-Fetal Medicine Units (MFMU) Network, Silver and colleagues concluded that the prothrombin (PT) gene mutation G20210A was not associated with pregnancy loss, preeclampsia, fetal growth restriction, or placental abruption in a low-risk, prospective cohort.
Said and coworkers reached a similar conclusion. In a blinded, prospective cohort study, they screened for the following mutations in 2,034 healthy nulliparous women before 22 weeks’ gestation:
- factor V Leiden mutation
- PT gene G20210A mutation
- methylenetetrahydrofolate reductase enzyme (MTHFR) C677T
- MTHFR A1298C
- thrombomodulin polymorphism.
The majority of asymptomatic women who carried an inherited thrombophilia polymorphism had a successful pregnancy outcome. In fact, homozygosity of the MTHFR A1298C mutation was found to be protective.
Population-based screening for thrombophilias is not recommended. In fact, some authors have advised against screening for thrombophilias even in the setting of a thrombotic event, suggesting it has limited utility.3
The main reason to screen for a thrombophilia at this time is to explore idiopathic thrombosis or a strong family history of the same. There is no need to screen for thrombophilias when the patient has a history of pregnancy loss, placental abruption, preeclampsia, and fetal growth restriction.
If you give magnesium sulfate for fetal neuroprotection, adhere to a protocol
ACOG Committee Opinion No. 455: Magnesium sulfate before anticipated preterm birth for neuroprotection. Obstet Gynecol. 2010;115(3):669–671.
Magnesium sulfate has a long and glorious history in obstetrics, having been used to prevent eclampsia, to treat preterm uterine contractions, and now, potentially, to reduce the incidence of central nervous system damage among prematurely delivered infants.
Cerebral palsy (CP) is most commonly associated with prematurity and intrauterine fetal infection. Only in the past two decades has there been a shift away from assigning the cause of most cases of CP to intrapartum events. Nevertheless, CP remains an important concern among patients and providers, and research continues to find ways to prevent CP or minimize its effects.
Numerous large trials have explored the use of magnesium sulfate to prevent CP in preterm infants. Although their findings have not been as definitive as researchers had hoped, some data do suggest that magnesium sulfate has a protective effect.
The American Congress of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) urge caution in regard to the use of magnesium sulfate for fetal neuroprotection. The SMFM points out that the reported benefits of magnesium sulfate in this setting have been derived largely from secondary analyses. The SMFM recommends that, if magnesium is used at all, it should be administered according to one of the published protocols (three are cited in the ACOG opinion).
The SMFM goes on to warn against choosing magnesium sulfate as a tocolytic solely because of its possible neuroprotective effects.
In a Committee Opinion published last year, ACOG was a bit more definite. “The Committee on Obstetric Practice and the Society for Maternal-Fetal Medicine recognize that none of the individual studies found a benefit with regard to their primary outcome,” the opinion states. “However, the available evidence suggests that magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, concurrent tocolysis, and monitoring in concordance with one of the larger trials.”
Recent editorials have cautioned against using magnesium sulfate for fetal neuroprotection until more data become available,4 or have left it up to the individual practitioners (or institution) to decide whether it is advisable.5
The use of magnesium sulfate for fetal neuroprotection when preterm delivery seems likely requires additional research. For now, this practice should be governed strictly by protocol. And it should not be viewed as “standard of care” by our legal colleagues.
When administering magnesium sulfate, avoid giving a cumulative total in excess of 50 g, as this amount may increase the risk of pediatric death.6
We want to hear from you! Tell us what you think.
- How to manage a short cervix to lower the risk of preterm delivery
Joseph R. Wax, MD (May 2010) - When is VBAC appropriate?
Aviva Lee-Parritz, MD (July 2010) - What can be safer than having a baby in the USA? (Commentary)
Louis L. Weinstein, MD (May 2010)
From an evolutionary standpoint, not much has changed in pregnancy and childbirth. From a clinical perspective, however, flux is a constant. Three issues, in particular, have seen notable development over the past year:
- optimal timing of elective delivery
- screening for thrombophilias in women who experience recurrent pregnancy loss, fetal growth restriction, preeclampsia, or placental abruption
- use of magnesium sulfate for fetal neuroprotection.
Of course, in the specialties of obstetrics and perinatal medicine, research continues in a variety of other subject areas, as well. Simulation training, diagnosis and management of gestational diabetes, and rescue steroid treatment are three examples. Other issues being explored include the use of progesterone to prevent prematurity, the use of ultrasonography to measure cervical length, and the safety of vaginal birth after cesarean delivery. The three areas highlighted here are not the only ones “ready for prime time,” but they are areas of considerable interest and debate.
We have a tradition in obstetrics of not embracing change too quickly. We learned this lesson through our experience with diethylstilbestrol (DES) and thalidomide, and we must continue to use caution whenever new technologies or management approaches are proposed.
30 weeks is the rule, provided delivery is truly elective
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
When it comes to elective delivery, no one would argue against the wisdom of continuing pregnancy until at least 39 weeks’ gestation in the absence of complications. But what data form the basis of this wisdom, and when might it be prudent to consider earlier delivery?
In a widely publicized study, Tita and colleagues concluded that elective repeat cesarean delivery before 39 weeks of gestation (i.e., 37 through 38-6/7 weeks) is associated with a higher rate of neonatal respiratory distress and other adverse neonatal outcomes than is delivery at 39 to 40 weeks. Note, however, that the primary outcome of this study was a composite. Therefore, the findings should be interpreted with some caution.
In their report, Tita and coworkers acknowledged that the transient and predominantly minor complications associated with delivery before 39 weeks must be weighed against the risk of fetal death inherent in delaying delivery through 38 full weeks—and an accompanying editorial made the same point.1 Stillbirth occurs at a rate of 1 case for every 1,000 births in the 37- to 39-week gestational age range—a rate that may be higher than the risks associated with delivery. Even so, the risk of stillbirth at 37 to 39 weeks is very small, and that risk is unlikely to be lowered through routine antenatal fetal testing. We should also remember that the risks of neonatal respiratory distress, transient tachypnea, admission to the neonatal intensive care unit (NICU), and even cerebral palsy2 may be increased with delivery at 37 to 38 weeks, or at 42 weeks or later, compared with delivery at 40 weeks.
All truly elective deliveries should occur at or after 39 weeks of gestation. However, when indicated, earlier delivery is acceptable—even essential—if we are to minimize maternal and neonatal morbidity and mortality in high-risk circumstances, such as hypertensive disorders of pregnancy, placenta previa, fetal growth restriction, and other conditions.
Investigations are under way to determine whether there is a role for routine betamethasone administration (regardless of indication or gestational age) in the absence of labor before 39 weeks. Until those data come in, we should continue to follow current practice guidelines for antenatal maternal administration of betamethasone—namely, a single course given between 24 and 34 weeks in women who have an elevated risk of preterm delivery.
Population-based screening for thrombophilias is not recommended
Silver RM, Zhao Y, Spong CY, et al, for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (NICHD MFMU) Network. Prothrombin gene G20210A mutation and obstetric complications. Obstet Gynecol. 2010;115(1):14–20.
Said JM, Higgins JR, Moses EK, et al. Inherited thrombophilia polymorphisms and pregnancy outcomes in nulliparous women. Obstet Gynecol. 2010;115(1):5–13.
Since the mid-1990s, screening for thrombophilias has been recommended in the evaluation of a variety of adverse reproductive outcomes, including, but not limited to:
- recurrent pregnancy loss
- unexplained stillbirth
- placental abruption
- preeclampsia
- fetal growth restriction.
When a thrombophilia is detected in these settings, the practitioner faces a dilemma—namely, what to do when the mother is otherwise healthy and asymptomatic. All too often the finding of a thrombophilia leads to the initiation of some anticoagulation regimen, ranging from low-dose aspirin all the way to therapeutic anticoagulation with heparin.
Over the past year, several studies and expert opinions have been published that recast the role of thrombophilia screening in obstetric practice.
Writing for the Maternal-Fetal Medicine Units (MFMU) Network, Silver and colleagues concluded that the prothrombin (PT) gene mutation G20210A was not associated with pregnancy loss, preeclampsia, fetal growth restriction, or placental abruption in a low-risk, prospective cohort.
Said and coworkers reached a similar conclusion. In a blinded, prospective cohort study, they screened for the following mutations in 2,034 healthy nulliparous women before 22 weeks’ gestation:
- factor V Leiden mutation
- PT gene G20210A mutation
- methylenetetrahydrofolate reductase enzyme (MTHFR) C677T
- MTHFR A1298C
- thrombomodulin polymorphism.
The majority of asymptomatic women who carried an inherited thrombophilia polymorphism had a successful pregnancy outcome. In fact, homozygosity of the MTHFR A1298C mutation was found to be protective.
Population-based screening for thrombophilias is not recommended. In fact, some authors have advised against screening for thrombophilias even in the setting of a thrombotic event, suggesting it has limited utility.3
The main reason to screen for a thrombophilia at this time is to explore idiopathic thrombosis or a strong family history of the same. There is no need to screen for thrombophilias when the patient has a history of pregnancy loss, placental abruption, preeclampsia, and fetal growth restriction.
If you give magnesium sulfate for fetal neuroprotection, adhere to a protocol
ACOG Committee Opinion No. 455: Magnesium sulfate before anticipated preterm birth for neuroprotection. Obstet Gynecol. 2010;115(3):669–671.
Magnesium sulfate has a long and glorious history in obstetrics, having been used to prevent eclampsia, to treat preterm uterine contractions, and now, potentially, to reduce the incidence of central nervous system damage among prematurely delivered infants.
Cerebral palsy (CP) is most commonly associated with prematurity and intrauterine fetal infection. Only in the past two decades has there been a shift away from assigning the cause of most cases of CP to intrapartum events. Nevertheless, CP remains an important concern among patients and providers, and research continues to find ways to prevent CP or minimize its effects.
Numerous large trials have explored the use of magnesium sulfate to prevent CP in preterm infants. Although their findings have not been as definitive as researchers had hoped, some data do suggest that magnesium sulfate has a protective effect.
The American Congress of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) urge caution in regard to the use of magnesium sulfate for fetal neuroprotection. The SMFM points out that the reported benefits of magnesium sulfate in this setting have been derived largely from secondary analyses. The SMFM recommends that, if magnesium is used at all, it should be administered according to one of the published protocols (three are cited in the ACOG opinion).
The SMFM goes on to warn against choosing magnesium sulfate as a tocolytic solely because of its possible neuroprotective effects.
In a Committee Opinion published last year, ACOG was a bit more definite. “The Committee on Obstetric Practice and the Society for Maternal-Fetal Medicine recognize that none of the individual studies found a benefit with regard to their primary outcome,” the opinion states. “However, the available evidence suggests that magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, concurrent tocolysis, and monitoring in concordance with one of the larger trials.”
Recent editorials have cautioned against using magnesium sulfate for fetal neuroprotection until more data become available,4 or have left it up to the individual practitioners (or institution) to decide whether it is advisable.5
The use of magnesium sulfate for fetal neuroprotection when preterm delivery seems likely requires additional research. For now, this practice should be governed strictly by protocol. And it should not be viewed as “standard of care” by our legal colleagues.
When administering magnesium sulfate, avoid giving a cumulative total in excess of 50 g, as this amount may increase the risk of pediatric death.6
We want to hear from you! Tell us what you think.
1. Greene MF. Making small risks even smaller. N Engl J Med. 2009;360(2):183-184.
2. Moster D, Wilcox AJ, Vollset SE, Markestad T, Lie RT. Cerebral palsy among term and postterm births. JAMA. 2010;304(9):976-982.
3. Scifres CM, Macones GA. The utility of thrombophilia testing in pregnant women with thrombosis; fact or fiction? Am J Obstet Gynecol. 2008;199(4):344.e1–7.-
4. Stanley FJ, Crowther C. Antenatal magnesium sulfate for neuroprotection before preterm birth? N Engl J Med. 2008;359(9):962-964.
5. Macones GA. MgSO4 for CP prevention: too good to be true? Am J Obstet Gynecol. 2009;200(6):589.-
6. Mittendorf R, Covert R, Boman J, et al. Is tocolytic magnesium sulfate associated with increased total paediatric mortality? Lancet. 1997;350(9090):1517-1518.
1. Greene MF. Making small risks even smaller. N Engl J Med. 2009;360(2):183-184.
2. Moster D, Wilcox AJ, Vollset SE, Markestad T, Lie RT. Cerebral palsy among term and postterm births. JAMA. 2010;304(9):976-982.
3. Scifres CM, Macones GA. The utility of thrombophilia testing in pregnant women with thrombosis; fact or fiction? Am J Obstet Gynecol. 2008;199(4):344.e1–7.-
4. Stanley FJ, Crowther C. Antenatal magnesium sulfate for neuroprotection before preterm birth? N Engl J Med. 2008;359(9):962-964.
5. Macones GA. MgSO4 for CP prevention: too good to be true? Am J Obstet Gynecol. 2009;200(6):589.-
6. Mittendorf R, Covert R, Boman J, et al. Is tocolytic magnesium sulfate associated with increased total paediatric mortality? Lancet. 1997;350(9090):1517-1518.
More strategies to avoid malpractice hazards on labor and delivery
Sound strategies to avoid malpractice hazards on labor and delivery
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD
CASE 1: Pregestational diabetes, large baby, birth injury
A 31-year-old gravida 1 is admitted to labor and delivery. She is at 39-5/7 weeks’ gestation, dated by last menstrual period and early sonogram. The woman is a pregestational diabetic and uses insulin to control her blood glucose level.
Three weeks before admission, ultrasonography (US) revealed an estimated fetal weight of 3,650 g—at the 71st percentile for gestational age.
After an unremarkable course of labor, delivery is complicated by severe shoulder dystocia. The newborn has a birth weight of 4,985 g and sustains an Erb’s palsy-type injury. The mother develops a rectovaginal fistula after a fourth-degree tear.
In the first part of this article, we discussed how an allegation of malpractice can arise because of an unexpected event or outcome for a mother in your care, or her baby, apart from any specific clinical action you undertook. We offered an example: Counseling that you provide about options for prenatal care that falls short of full understanding by the patient.
In this article, we enter the realm of the hands-on practice of medicine and discuss causation: namely, the actions of a physician, in the course of managing labor and delivering a baby, that put that physician at risk of a charge of malpractice because the medical care 1) is inconsistent with current medical practice and thus 2) harmed mother or newborn.
Let’s return to the opening case above and discuss key considerations for the physician. Three more cases follow that, with analysis and recommendations.
Considerations in CASE 1
- A woman who has pregestational diabetes should receive ongoing counseling about the risks of fetal anomalies, macrosomia, and problems in the neonatal period. Be certain that she understands that these risks can be ameliorated, but not eliminated, with careful blood glucose control.
- The fetus of a diabetic gravida develops a relative decrease in the ratio of head circumference-to-abdominal circumference that predisposes it to shoulder dystocia. Cesarean delivery can decrease, but not eliminate, the risk of traumatic birth injury in a diabetic mother. (Of course, cesarean delivery will, on its own, substantially increase the risk of maternal morbidity—including at any subsequent cesarean delivery.)
What do they mean? terms and concepts intended to bolster your work and protect you
It’s not easy to define what constitutes “best care” in a given clinical circumstance. Generalizations are useful, but they may possess an inherent weakness: “Best practices,” “evidence-based care,” “standardization of care,” and “uniformity of care” usually apply more usefully to populations than individuals.
Such concepts derive from broader applications in economics, politics, and science. They are useful to define a reasonable spectrum of anticipated practices, and they certainly have an expanding role in the care of patients and in medical education (TABLE). Clinical guidelines serve as strategies that may be very helpful to the clinician. All of us understand and implement appropriate care in the great majority of clinical scenarios, but none of us are, or can be, expert in all situations. Referencing and using guidelines can fill a need for a functional starting point when expertise is lacking or falls short.
Best practices result from evidence-directed decision-making. This concept logically yields a desirable uniformity of practice. Although we all believe that our experience is our best teacher, we may best serve patients if we sample knowledge and wisdom from controlled clinical trials and from the experiences of others. What is accepted local practice must also be considered important when you devise a plan of care.1,2
A selected glossary of clinical care guidelines
| Term | What does it mean? |
|---|---|
| “Best practice” | A process or activity that is believed to be more effective at delivering a particular outcome than any other when applied to a particular condition or circumstance. The idea? With proper processes, checks, and testing, a desired outcome can be delivered with fewer problems and unforeseen complications than otherwise possible.5 |
| “Evidence-based care” | The best available process or activity arising from both 1) individual expertise and 2) best external evidence derived from systematic research.6 |
| “Standard of care” | A clinical practice to maximize success and minimize risk, applied to professional decision-making.7 |
| “Uniformity of practice” | Use of systematic, literature-based research findings to develop an approach that is efficacious and safe; that maximizes benefit; and that minimizes risk.8 |
Consider the management of breech presentation that is recognized at the 36th week antepartum visit: Discussion with the patient should include 1) reference to concerns with congenital anomalies and genetic syndromes, 2) in-utero growth and development, and 3) the delivery process. The management algorithm may include external cephalic version, elective cesarean delivery before onset of labor, or cesarean delivery after onset of labor. Each approach has advocates—based on expert opinion clinical trials.
Management options may vary from institution to institution, however, because of limited availability of certain services—such as the expertise required for a trial of external cephalic version, the availability of on-site cesarean delivery capabilities, and patient and clinician preferences.
Uniformity of care, based on best practices, can therefore simplify the care process and decrease the risk that may be associated with individual experience-based management. Adhering to a uniform practice augments the clinician’s knowledge and allows for enhanced nursing and therapeutic efficiency.
The greatest benefit of using an evidence-based, widely accepted approach, however, is the potential to diminish poor practice and consequent malpractice exposure for both clinicians and the hospital.
Note: Although your adherence to clinical guidelines, best practices, and uniformity of care ought to be consistent with established standards of care, don’t automatically consider any deviation a lapse or failing because it’s understood and accepted that some local variability exists in practice.
Prelude to birth: triage and admission Triage. Most women in labor arrive at the hospital or birthing center to an area set aside for labor and delivery triage. There, 1) recording of the chief complaint and vital signs and 2) completion of a brief history and physical generate a call to the clinician.
The record produced in triage should be scrutinized carefully for accuracy. Clarify, in as timely a manner as possible, any errors in:
- timing (possibly because of different clocks set to different times)
- the precise capture of the chief complaint
- reporting difficulty or ease in reaching the responsible clinician.
Whether these records are electronic or paper, an addendum marked with the time is always acceptable. Never attempt to correct a record! Always utilize a late entry or addendum.
Admission. After the patient is admitted, she generally undergoes an admission protocol, specific to the hospital, regarding her situation. This includes:
- the history
- special requests
- any previously agreed-on plan of care
- any problems that have developed since her last prenatal visit.
This protocol is generally completed by a nurse, resident, nurse practitioner, or physician assistant.
Hospitals generally request input from the attending physician on the specifics of the admission, based on those hospital protocols. There may be some room to individualize the admission process to labor and delivery.
4 pillars of care during labor
In general, labor is defined as progressive dilation of the cervix. Several parameters serve as guidelines regarding adequate progress through the various stages of labor.
Fetal monitoring. Continuous evaluation of the fetus during labor is a routine part of intrapartum care. Recording and observing the FHR tracing is an accepted—and expected—practice. Documentation of the FHR in the medical record is specifically required, and should include both the physician’s and nursing notes.
Anesthesia care. The patient’s preference and the availability of options allows for several accepted practices regarding anesthesia and analgesia during L & D. Does she want epidural anesthesia during labor, for example? Intravenous narcotics? Her choice is an important facet of your provision of care.
However, such choice requires the patient to give consent and to understand the risk-benefit equation. Documentation by nursing of the patient’s consent and understanding should be complete, including discussion and administration. Anesthesia staff should be clear, complete, and legible in making a record.
Neonatal care. If logistics permit, a member of the pediatrics service should be routinely available to see the newborn at delivery. The patient should view the pediatrician and obstetrician as partners working as a team for the benefit of the mother and her family. This can enhance the patient’s understanding and confidence about the well being of her baby.
Documentation. Although deficient documentation does not, itself, lead to a finding of malpractice, appropriate documentation plays an important role in demonstrating that clinical practices have addressed issues about both allegation and causation of potential adverse outcomes.
We cannot overemphasize that nursing documentation should complement and be consistent with notes made by the physician. That said, nursing notes are not a substitute for the physician’s notes. Practices that integrate the written comments of nursing and physician into a single set of progress notes facilitate this complementary interaction.
3 more clinical scenarios
CASE 2: Admitted at term with contractions
The initial exam determines that this 21-year-old gravida 1 is 2/80/-1. Re-examination in 3 hours finds her at 3-4/80/0.
She requests pain relief and states that she wants epidural anesthesia.
Evaluation 2 hours later suggests secondary arrest of dilation. Oxytocin is begun.
Soon after, late decelerations are observed on the FHR monitor.
Use of exogenous oxytocin in L & D is a double-edged sword: The drug can enhance the safety and efficacy of labor and delivery for mother and fetus, but using it in an unregulated manner (in terms of its indication and administration) can subject both to increased risk.
In fact, it is fair to say that the most widespread and potentially dangerous intervention during labor is the administration of oxytocin. Many expert opinions, guidelines, and strategies have been put forward about intrapartum use of oxytocin. These include consideration of:
- indications
- dosage (including the maximum)
- interval
- fetal response
- ultimately, the availability of a physician during administration to manage any problem that arises.
Considerations in CASE 2
- Always clearly indicate the reason for using oxytocin: Is this an induction? Or an augmentation? Was there evidence of fetal well-being, or non-reassurance, before oxytocin was administered? Certainly, there are circumstances in which either fetal status or non-progression of labor (or both) are an indication for oxytocin. A clear, concise, and properly timed progress note is always appropriate under these circumstances.
- Discuss treatment with the patient. Does she understand why this therapy is being recommended? Does she agree to its use? And does she understand what the alternatives are?
- Verify that nursing has accurately charted this process. Ensure that the nursing staff’s notes are complete and are consistent with yours.
- Simplify the entire process: Use premixed solution and protocol-driven orders. Know what the standards and protocols are in your department. Minimizing patient-to-patient variability should lessen the risk of error.
- Always be available in L & D for the first 30 minutes that oxytocin is being administered. If a problem with excessive uterine activity is going to occur, it is most likely to do so upon initial administration.
- Monitor the FHR continuously. At the first suggestion of a change in fetal status, discontinue oxytocin. Perform a pelvic exam to reassess the situation. Understand and apply appropriate inutero resuscitative measures (IV fluids, O2, change in maternal position). Depending on circumstances, you can consider a restart of oxytocin after the FHR returns to its pre-oxytocin pattern.
- Monitor uterine response to oxytocin. If the membranes are ruptured and if it is clinically feasible, an intrauterine pressure transducer will allow you to more objectively assess the uterine response to oxytocin and make decisions on that basis. Determine beforehand whether the patient is agreeable to this intervention.
- When oxytocin is used for augmentation, reassess labor within 4 hours of achieving a satisfactory pattern. If minimal progress is not made, assess the clinical situation to determine why oxytocin, at an adequate response level, has failed to return labor to a normal active phase slope. Are there minor degrees of malposition? Is there an element of cephalopelvic disproportion? Recall that progress in labor is dependent on multiple factors.
- Chart the process concurrently. Specify options for delivery before delivery.
CASE 3: Spontaneous delivery arrests after delivery of the head
The patient is a multipara with three prior normal vaginal deliveries. Her diabetic screen is negative. At admission, the estimated fetal weight was 3,628 g—in the same range as her other deliveries. A nuchal cord is absent.
After the patient assumes the McRobert’s position, delivery is accomplished with suprapubic pressure. Weakness is noted in the newborn’s right upper extremity. Birth weight is 3,515 g.
Maneuvers to manage shoulder dystocia should be part of all clinicians’ skill set. The sequence of those maneuvers, and their timing, are subject to some variation. Efficacy seems to be related most to recognizing and performing each maneuver properly.
Guidelines for managing shoulder dystocia should include reference to 1) the initial evaluation of the patient on admission to labor and delivery and 2) the delivery itself.3
Considerations in CASE 3
- Before you admit them to L & D, counsel patients who have diabetes, morbid obesity (body mass index >40), or birth trauma in a prior delivery, or who have had a prior large infant (>9 lb birth weight), about the risk of shoulder dystocia. Present possible alternatives, and draw the patient into the conversation.
- Consider delivering all women at term in the McRobert’s position, prophylactically.
- Always check for a nuchal cord after delivery of the head. If you find one, reduce it if possible. Take a few seconds and carefully assess the situation before you cut the umbilical cord.
- Lateral traction on the fetus’ head has the potential to cause tension on the brachial plexus, or make it worse. Gentle rotation of the head (<90 degrees) can move the shoulders into a more favorable location for delivery. Don’t rush—call for assistance! Continuously explain to the patient what you are doing; reassure her about the process.
- Use suprapubic pressure wisely. The anterior shoulder may be dislodged by direct downward force; suprapubic force in a lateral direction may also dislodge the shoulder. Apply force from above the patient’s pelvis. Your assistant will have the best mechanical advantage by standing on a stool.
- Is an episiotomy or episioproctotomy advantageous? In attempting to reach either the anterior or posterior shoulder vaginally, individualized assessment is called for.
- When the posterior shoulder cannot be satisfactorily engaged and moved, try doing so with the anterior shoulder. Insert your hand between the symphysis and the fetal head and place downward pressure on the head to dislodge it and complete the delivery.
- If it becomes necessary to attempt delivery by direct traction on the posterior hand or arm, try to avoid extension. Maintain flexion and move the upper extremity across the fetal chest before you attempt extension.
- Repeat these maneuvers a second time before you attempt cephalic replacement or other maneuvers. Remember to move with deliberate speed to lessen the risk of making the injury worse. Have pediatric support present. Continue speaking with and reassuring the patient.
- Under anesthesia in the operating room, perform a hysterotomy incision. With an assistant working through the vagina, combine the forces available to complete the delivery.
- After delivery is complete, take time to write a note. (Speak with the patient and her family first, however.) Read the notes written by nursing. If they are not available when you write your note, mention that. Add a second note later, when nursing notes become available.
CASE 4: Meconium-stained fluid
A 35-year-old multigravida is 6 to 7 cm dilated. Her membranes have just spontaneously ruptured; you note copious meconium-stained fluid. The FHR demonstrates recurrent variable decelerations; baseline fetal heart rate remains normal.
The description and implications of various FHR patterns are important when documenting the fetal metabolic state during the birth process. Current guidelines have attempted to simplify, standardize, and clarify the interpretation of the FHR tracing.4
Considerations in CASE 4
- Explain the situation to the patient. Perform a pelvic examination. If possible, wait for nursing assistance to ensure accurate documentation.
- Reassure the patient; help her move to a lateral position. Observe the FHR monitor for a response.
- Administer supplemental O2. Increase IV fluids to facilitate utero-placental perfusion.
- If useful or necessary, consider attaching a fetal scalp electrode to better delineate fetal status.
- When the FHR returns to baseline state (before spontaneous rupture of membranes), perform vibro-acoustic stimulation as a test to support fetal well-being.
- Engage the patient and her family in a discussion about the sequence of events. Depending on the acuity of the situation, allow her to voice her concerns and reiterate what has occurred, and what will occur.
- Outline a plan of management to the patient—verbally and in the record—with clear reference to events that have occurred. Then, stick to that plan!
- Carefully review corresponding nursing notes. Always write your own assessment of events and actions.
Summing up: three “keepers”
First, the cornerstones of your effort to reduce malpractice risk are 1) thoughtful and informed discussion with the patient and 2) clear, concise documentation.
Second, don’t expect to be able to eliminate unnecessary or inappropriate allegations of medical malpractice; the best you can do is limit them.
Third, and most important, remember: The knowledgeable clinician you strive to be will make appropriate judgments in a timely fashion and will take appropriate actions to provide good medical care.
We want to hear from you! Tell us what you think.
1. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
2. Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199(2):105.e1-e7.
3. Crofts JF, Fox F, Ellis D. Observations from 450 shoulder dystocia simulations: lessons for skills training. Obstet Gynecol. 2008;112(4):906-912.
4. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring. Obstet Gynecol. 2008;112(3):661-666.
5. Best practice. Web site. 2010. http://www.businessdictionary.com/definition/best-practice.html. Accessed December 17, 2010.
6. Sackett DL, Rosenberg WC, Gray JA, Haynes BR, Richardson WS. Evidence based medicine: what it is and what it isn’t 1996;312(7023):71-72.
7. Hayes EJ, Weinstein L. Improving patient safety and uniformity of care by a standardized regimen for the use of oxytocin. Am J Obstet Gynecol. 2008;198(6):622.e1-7.
8. Proctor SJ, Taylor PR. A practical guide to continuous population-based data collection (PACE): a process facilitating uniformity of care and research into practice. 2000;93(2):67-73.
9. Cohen W, Friedman EA. Management of Labor. Baltimore, MD: University Park Press; 1983.
Sound strategies to avoid malpractice hazards on labor and delivery
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD
CASE 1: Pregestational diabetes, large baby, birth injury
A 31-year-old gravida 1 is admitted to labor and delivery. She is at 39-5/7 weeks’ gestation, dated by last menstrual period and early sonogram. The woman is a pregestational diabetic and uses insulin to control her blood glucose level.
Three weeks before admission, ultrasonography (US) revealed an estimated fetal weight of 3,650 g—at the 71st percentile for gestational age.
After an unremarkable course of labor, delivery is complicated by severe shoulder dystocia. The newborn has a birth weight of 4,985 g and sustains an Erb’s palsy-type injury. The mother develops a rectovaginal fistula after a fourth-degree tear.
In the first part of this article, we discussed how an allegation of malpractice can arise because of an unexpected event or outcome for a mother in your care, or her baby, apart from any specific clinical action you undertook. We offered an example: Counseling that you provide about options for prenatal care that falls short of full understanding by the patient.
In this article, we enter the realm of the hands-on practice of medicine and discuss causation: namely, the actions of a physician, in the course of managing labor and delivering a baby, that put that physician at risk of a charge of malpractice because the medical care 1) is inconsistent with current medical practice and thus 2) harmed mother or newborn.
Let’s return to the opening case above and discuss key considerations for the physician. Three more cases follow that, with analysis and recommendations.
Considerations in CASE 1
- A woman who has pregestational diabetes should receive ongoing counseling about the risks of fetal anomalies, macrosomia, and problems in the neonatal period. Be certain that she understands that these risks can be ameliorated, but not eliminated, with careful blood glucose control.
- The fetus of a diabetic gravida develops a relative decrease in the ratio of head circumference-to-abdominal circumference that predisposes it to shoulder dystocia. Cesarean delivery can decrease, but not eliminate, the risk of traumatic birth injury in a diabetic mother. (Of course, cesarean delivery will, on its own, substantially increase the risk of maternal morbidity—including at any subsequent cesarean delivery.)
What do they mean? terms and concepts intended to bolster your work and protect you
It’s not easy to define what constitutes “best care” in a given clinical circumstance. Generalizations are useful, but they may possess an inherent weakness: “Best practices,” “evidence-based care,” “standardization of care,” and “uniformity of care” usually apply more usefully to populations than individuals.
Such concepts derive from broader applications in economics, politics, and science. They are useful to define a reasonable spectrum of anticipated practices, and they certainly have an expanding role in the care of patients and in medical education (TABLE). Clinical guidelines serve as strategies that may be very helpful to the clinician. All of us understand and implement appropriate care in the great majority of clinical scenarios, but none of us are, or can be, expert in all situations. Referencing and using guidelines can fill a need for a functional starting point when expertise is lacking or falls short.
Best practices result from evidence-directed decision-making. This concept logically yields a desirable uniformity of practice. Although we all believe that our experience is our best teacher, we may best serve patients if we sample knowledge and wisdom from controlled clinical trials and from the experiences of others. What is accepted local practice must also be considered important when you devise a plan of care.1,2
A selected glossary of clinical care guidelines
| Term | What does it mean? |
|---|---|
| “Best practice” | A process or activity that is believed to be more effective at delivering a particular outcome than any other when applied to a particular condition or circumstance. The idea? With proper processes, checks, and testing, a desired outcome can be delivered with fewer problems and unforeseen complications than otherwise possible.5 |
| “Evidence-based care” | The best available process or activity arising from both 1) individual expertise and 2) best external evidence derived from systematic research.6 |
| “Standard of care” | A clinical practice to maximize success and minimize risk, applied to professional decision-making.7 |
| “Uniformity of practice” | Use of systematic, literature-based research findings to develop an approach that is efficacious and safe; that maximizes benefit; and that minimizes risk.8 |
Consider the management of breech presentation that is recognized at the 36th week antepartum visit: Discussion with the patient should include 1) reference to concerns with congenital anomalies and genetic syndromes, 2) in-utero growth and development, and 3) the delivery process. The management algorithm may include external cephalic version, elective cesarean delivery before onset of labor, or cesarean delivery after onset of labor. Each approach has advocates—based on expert opinion clinical trials.
Management options may vary from institution to institution, however, because of limited availability of certain services—such as the expertise required for a trial of external cephalic version, the availability of on-site cesarean delivery capabilities, and patient and clinician preferences.
Uniformity of care, based on best practices, can therefore simplify the care process and decrease the risk that may be associated with individual experience-based management. Adhering to a uniform practice augments the clinician’s knowledge and allows for enhanced nursing and therapeutic efficiency.
The greatest benefit of using an evidence-based, widely accepted approach, however, is the potential to diminish poor practice and consequent malpractice exposure for both clinicians and the hospital.
Note: Although your adherence to clinical guidelines, best practices, and uniformity of care ought to be consistent with established standards of care, don’t automatically consider any deviation a lapse or failing because it’s understood and accepted that some local variability exists in practice.
Prelude to birth: triage and admission Triage. Most women in labor arrive at the hospital or birthing center to an area set aside for labor and delivery triage. There, 1) recording of the chief complaint and vital signs and 2) completion of a brief history and physical generate a call to the clinician.
The record produced in triage should be scrutinized carefully for accuracy. Clarify, in as timely a manner as possible, any errors in:
- timing (possibly because of different clocks set to different times)
- the precise capture of the chief complaint
- reporting difficulty or ease in reaching the responsible clinician.
Whether these records are electronic or paper, an addendum marked with the time is always acceptable. Never attempt to correct a record! Always utilize a late entry or addendum.
Admission. After the patient is admitted, she generally undergoes an admission protocol, specific to the hospital, regarding her situation. This includes:
- the history
- special requests
- any previously agreed-on plan of care
- any problems that have developed since her last prenatal visit.
This protocol is generally completed by a nurse, resident, nurse practitioner, or physician assistant.
Hospitals generally request input from the attending physician on the specifics of the admission, based on those hospital protocols. There may be some room to individualize the admission process to labor and delivery.
4 pillars of care during labor
In general, labor is defined as progressive dilation of the cervix. Several parameters serve as guidelines regarding adequate progress through the various stages of labor.
Fetal monitoring. Continuous evaluation of the fetus during labor is a routine part of intrapartum care. Recording and observing the FHR tracing is an accepted—and expected—practice. Documentation of the FHR in the medical record is specifically required, and should include both the physician’s and nursing notes.
Anesthesia care. The patient’s preference and the availability of options allows for several accepted practices regarding anesthesia and analgesia during L & D. Does she want epidural anesthesia during labor, for example? Intravenous narcotics? Her choice is an important facet of your provision of care.
However, such choice requires the patient to give consent and to understand the risk-benefit equation. Documentation by nursing of the patient’s consent and understanding should be complete, including discussion and administration. Anesthesia staff should be clear, complete, and legible in making a record.
Neonatal care. If logistics permit, a member of the pediatrics service should be routinely available to see the newborn at delivery. The patient should view the pediatrician and obstetrician as partners working as a team for the benefit of the mother and her family. This can enhance the patient’s understanding and confidence about the well being of her baby.
Documentation. Although deficient documentation does not, itself, lead to a finding of malpractice, appropriate documentation plays an important role in demonstrating that clinical practices have addressed issues about both allegation and causation of potential adverse outcomes.
We cannot overemphasize that nursing documentation should complement and be consistent with notes made by the physician. That said, nursing notes are not a substitute for the physician’s notes. Practices that integrate the written comments of nursing and physician into a single set of progress notes facilitate this complementary interaction.
3 more clinical scenarios
CASE 2: Admitted at term with contractions
The initial exam determines that this 21-year-old gravida 1 is 2/80/-1. Re-examination in 3 hours finds her at 3-4/80/0.
She requests pain relief and states that she wants epidural anesthesia.
Evaluation 2 hours later suggests secondary arrest of dilation. Oxytocin is begun.
Soon after, late decelerations are observed on the FHR monitor.
Use of exogenous oxytocin in L & D is a double-edged sword: The drug can enhance the safety and efficacy of labor and delivery for mother and fetus, but using it in an unregulated manner (in terms of its indication and administration) can subject both to increased risk.
In fact, it is fair to say that the most widespread and potentially dangerous intervention during labor is the administration of oxytocin. Many expert opinions, guidelines, and strategies have been put forward about intrapartum use of oxytocin. These include consideration of:
- indications
- dosage (including the maximum)
- interval
- fetal response
- ultimately, the availability of a physician during administration to manage any problem that arises.
Considerations in CASE 2
- Always clearly indicate the reason for using oxytocin: Is this an induction? Or an augmentation? Was there evidence of fetal well-being, or non-reassurance, before oxytocin was administered? Certainly, there are circumstances in which either fetal status or non-progression of labor (or both) are an indication for oxytocin. A clear, concise, and properly timed progress note is always appropriate under these circumstances.
- Discuss treatment with the patient. Does she understand why this therapy is being recommended? Does she agree to its use? And does she understand what the alternatives are?
- Verify that nursing has accurately charted this process. Ensure that the nursing staff’s notes are complete and are consistent with yours.
- Simplify the entire process: Use premixed solution and protocol-driven orders. Know what the standards and protocols are in your department. Minimizing patient-to-patient variability should lessen the risk of error.
- Always be available in L & D for the first 30 minutes that oxytocin is being administered. If a problem with excessive uterine activity is going to occur, it is most likely to do so upon initial administration.
- Monitor the FHR continuously. At the first suggestion of a change in fetal status, discontinue oxytocin. Perform a pelvic exam to reassess the situation. Understand and apply appropriate inutero resuscitative measures (IV fluids, O2, change in maternal position). Depending on circumstances, you can consider a restart of oxytocin after the FHR returns to its pre-oxytocin pattern.
- Monitor uterine response to oxytocin. If the membranes are ruptured and if it is clinically feasible, an intrauterine pressure transducer will allow you to more objectively assess the uterine response to oxytocin and make decisions on that basis. Determine beforehand whether the patient is agreeable to this intervention.
- When oxytocin is used for augmentation, reassess labor within 4 hours of achieving a satisfactory pattern. If minimal progress is not made, assess the clinical situation to determine why oxytocin, at an adequate response level, has failed to return labor to a normal active phase slope. Are there minor degrees of malposition? Is there an element of cephalopelvic disproportion? Recall that progress in labor is dependent on multiple factors.
- Chart the process concurrently. Specify options for delivery before delivery.
CASE 3: Spontaneous delivery arrests after delivery of the head
The patient is a multipara with three prior normal vaginal deliveries. Her diabetic screen is negative. At admission, the estimated fetal weight was 3,628 g—in the same range as her other deliveries. A nuchal cord is absent.
After the patient assumes the McRobert’s position, delivery is accomplished with suprapubic pressure. Weakness is noted in the newborn’s right upper extremity. Birth weight is 3,515 g.
Maneuvers to manage shoulder dystocia should be part of all clinicians’ skill set. The sequence of those maneuvers, and their timing, are subject to some variation. Efficacy seems to be related most to recognizing and performing each maneuver properly.
Guidelines for managing shoulder dystocia should include reference to 1) the initial evaluation of the patient on admission to labor and delivery and 2) the delivery itself.3
Considerations in CASE 3
- Before you admit them to L & D, counsel patients who have diabetes, morbid obesity (body mass index >40), or birth trauma in a prior delivery, or who have had a prior large infant (>9 lb birth weight), about the risk of shoulder dystocia. Present possible alternatives, and draw the patient into the conversation.
- Consider delivering all women at term in the McRobert’s position, prophylactically.
- Always check for a nuchal cord after delivery of the head. If you find one, reduce it if possible. Take a few seconds and carefully assess the situation before you cut the umbilical cord.
- Lateral traction on the fetus’ head has the potential to cause tension on the brachial plexus, or make it worse. Gentle rotation of the head (<90 degrees) can move the shoulders into a more favorable location for delivery. Don’t rush—call for assistance! Continuously explain to the patient what you are doing; reassure her about the process.
- Use suprapubic pressure wisely. The anterior shoulder may be dislodged by direct downward force; suprapubic force in a lateral direction may also dislodge the shoulder. Apply force from above the patient’s pelvis. Your assistant will have the best mechanical advantage by standing on a stool.
- Is an episiotomy or episioproctotomy advantageous? In attempting to reach either the anterior or posterior shoulder vaginally, individualized assessment is called for.
- When the posterior shoulder cannot be satisfactorily engaged and moved, try doing so with the anterior shoulder. Insert your hand between the symphysis and the fetal head and place downward pressure on the head to dislodge it and complete the delivery.
- If it becomes necessary to attempt delivery by direct traction on the posterior hand or arm, try to avoid extension. Maintain flexion and move the upper extremity across the fetal chest before you attempt extension.
- Repeat these maneuvers a second time before you attempt cephalic replacement or other maneuvers. Remember to move with deliberate speed to lessen the risk of making the injury worse. Have pediatric support present. Continue speaking with and reassuring the patient.
- Under anesthesia in the operating room, perform a hysterotomy incision. With an assistant working through the vagina, combine the forces available to complete the delivery.
- After delivery is complete, take time to write a note. (Speak with the patient and her family first, however.) Read the notes written by nursing. If they are not available when you write your note, mention that. Add a second note later, when nursing notes become available.
CASE 4: Meconium-stained fluid
A 35-year-old multigravida is 6 to 7 cm dilated. Her membranes have just spontaneously ruptured; you note copious meconium-stained fluid. The FHR demonstrates recurrent variable decelerations; baseline fetal heart rate remains normal.
The description and implications of various FHR patterns are important when documenting the fetal metabolic state during the birth process. Current guidelines have attempted to simplify, standardize, and clarify the interpretation of the FHR tracing.4
Considerations in CASE 4
- Explain the situation to the patient. Perform a pelvic examination. If possible, wait for nursing assistance to ensure accurate documentation.
- Reassure the patient; help her move to a lateral position. Observe the FHR monitor for a response.
- Administer supplemental O2. Increase IV fluids to facilitate utero-placental perfusion.
- If useful or necessary, consider attaching a fetal scalp electrode to better delineate fetal status.
- When the FHR returns to baseline state (before spontaneous rupture of membranes), perform vibro-acoustic stimulation as a test to support fetal well-being.
- Engage the patient and her family in a discussion about the sequence of events. Depending on the acuity of the situation, allow her to voice her concerns and reiterate what has occurred, and what will occur.
- Outline a plan of management to the patient—verbally and in the record—with clear reference to events that have occurred. Then, stick to that plan!
- Carefully review corresponding nursing notes. Always write your own assessment of events and actions.
Summing up: three “keepers”
First, the cornerstones of your effort to reduce malpractice risk are 1) thoughtful and informed discussion with the patient and 2) clear, concise documentation.
Second, don’t expect to be able to eliminate unnecessary or inappropriate allegations of medical malpractice; the best you can do is limit them.
Third, and most important, remember: The knowledgeable clinician you strive to be will make appropriate judgments in a timely fashion and will take appropriate actions to provide good medical care.
We want to hear from you! Tell us what you think.
Sound strategies to avoid malpractice hazards on labor and delivery
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD
CASE 1: Pregestational diabetes, large baby, birth injury
A 31-year-old gravida 1 is admitted to labor and delivery. She is at 39-5/7 weeks’ gestation, dated by last menstrual period and early sonogram. The woman is a pregestational diabetic and uses insulin to control her blood glucose level.
Three weeks before admission, ultrasonography (US) revealed an estimated fetal weight of 3,650 g—at the 71st percentile for gestational age.
After an unremarkable course of labor, delivery is complicated by severe shoulder dystocia. The newborn has a birth weight of 4,985 g and sustains an Erb’s palsy-type injury. The mother develops a rectovaginal fistula after a fourth-degree tear.
In the first part of this article, we discussed how an allegation of malpractice can arise because of an unexpected event or outcome for a mother in your care, or her baby, apart from any specific clinical action you undertook. We offered an example: Counseling that you provide about options for prenatal care that falls short of full understanding by the patient.
In this article, we enter the realm of the hands-on practice of medicine and discuss causation: namely, the actions of a physician, in the course of managing labor and delivering a baby, that put that physician at risk of a charge of malpractice because the medical care 1) is inconsistent with current medical practice and thus 2) harmed mother or newborn.
Let’s return to the opening case above and discuss key considerations for the physician. Three more cases follow that, with analysis and recommendations.
Considerations in CASE 1
- A woman who has pregestational diabetes should receive ongoing counseling about the risks of fetal anomalies, macrosomia, and problems in the neonatal period. Be certain that she understands that these risks can be ameliorated, but not eliminated, with careful blood glucose control.
- The fetus of a diabetic gravida develops a relative decrease in the ratio of head circumference-to-abdominal circumference that predisposes it to shoulder dystocia. Cesarean delivery can decrease, but not eliminate, the risk of traumatic birth injury in a diabetic mother. (Of course, cesarean delivery will, on its own, substantially increase the risk of maternal morbidity—including at any subsequent cesarean delivery.)
What do they mean? terms and concepts intended to bolster your work and protect you
It’s not easy to define what constitutes “best care” in a given clinical circumstance. Generalizations are useful, but they may possess an inherent weakness: “Best practices,” “evidence-based care,” “standardization of care,” and “uniformity of care” usually apply more usefully to populations than individuals.
Such concepts derive from broader applications in economics, politics, and science. They are useful to define a reasonable spectrum of anticipated practices, and they certainly have an expanding role in the care of patients and in medical education (TABLE). Clinical guidelines serve as strategies that may be very helpful to the clinician. All of us understand and implement appropriate care in the great majority of clinical scenarios, but none of us are, or can be, expert in all situations. Referencing and using guidelines can fill a need for a functional starting point when expertise is lacking or falls short.
Best practices result from evidence-directed decision-making. This concept logically yields a desirable uniformity of practice. Although we all believe that our experience is our best teacher, we may best serve patients if we sample knowledge and wisdom from controlled clinical trials and from the experiences of others. What is accepted local practice must also be considered important when you devise a plan of care.1,2
A selected glossary of clinical care guidelines
| Term | What does it mean? |
|---|---|
| “Best practice” | A process or activity that is believed to be more effective at delivering a particular outcome than any other when applied to a particular condition or circumstance. The idea? With proper processes, checks, and testing, a desired outcome can be delivered with fewer problems and unforeseen complications than otherwise possible.5 |
| “Evidence-based care” | The best available process or activity arising from both 1) individual expertise and 2) best external evidence derived from systematic research.6 |
| “Standard of care” | A clinical practice to maximize success and minimize risk, applied to professional decision-making.7 |
| “Uniformity of practice” | Use of systematic, literature-based research findings to develop an approach that is efficacious and safe; that maximizes benefit; and that minimizes risk.8 |
Consider the management of breech presentation that is recognized at the 36th week antepartum visit: Discussion with the patient should include 1) reference to concerns with congenital anomalies and genetic syndromes, 2) in-utero growth and development, and 3) the delivery process. The management algorithm may include external cephalic version, elective cesarean delivery before onset of labor, or cesarean delivery after onset of labor. Each approach has advocates—based on expert opinion clinical trials.
Management options may vary from institution to institution, however, because of limited availability of certain services—such as the expertise required for a trial of external cephalic version, the availability of on-site cesarean delivery capabilities, and patient and clinician preferences.
Uniformity of care, based on best practices, can therefore simplify the care process and decrease the risk that may be associated with individual experience-based management. Adhering to a uniform practice augments the clinician’s knowledge and allows for enhanced nursing and therapeutic efficiency.
The greatest benefit of using an evidence-based, widely accepted approach, however, is the potential to diminish poor practice and consequent malpractice exposure for both clinicians and the hospital.
Note: Although your adherence to clinical guidelines, best practices, and uniformity of care ought to be consistent with established standards of care, don’t automatically consider any deviation a lapse or failing because it’s understood and accepted that some local variability exists in practice.
Prelude to birth: triage and admission Triage. Most women in labor arrive at the hospital or birthing center to an area set aside for labor and delivery triage. There, 1) recording of the chief complaint and vital signs and 2) completion of a brief history and physical generate a call to the clinician.
The record produced in triage should be scrutinized carefully for accuracy. Clarify, in as timely a manner as possible, any errors in:
- timing (possibly because of different clocks set to different times)
- the precise capture of the chief complaint
- reporting difficulty or ease in reaching the responsible clinician.
Whether these records are electronic or paper, an addendum marked with the time is always acceptable. Never attempt to correct a record! Always utilize a late entry or addendum.
Admission. After the patient is admitted, she generally undergoes an admission protocol, specific to the hospital, regarding her situation. This includes:
- the history
- special requests
- any previously agreed-on plan of care
- any problems that have developed since her last prenatal visit.
This protocol is generally completed by a nurse, resident, nurse practitioner, or physician assistant.
Hospitals generally request input from the attending physician on the specifics of the admission, based on those hospital protocols. There may be some room to individualize the admission process to labor and delivery.
4 pillars of care during labor
In general, labor is defined as progressive dilation of the cervix. Several parameters serve as guidelines regarding adequate progress through the various stages of labor.
Fetal monitoring. Continuous evaluation of the fetus during labor is a routine part of intrapartum care. Recording and observing the FHR tracing is an accepted—and expected—practice. Documentation of the FHR in the medical record is specifically required, and should include both the physician’s and nursing notes.
Anesthesia care. The patient’s preference and the availability of options allows for several accepted practices regarding anesthesia and analgesia during L & D. Does she want epidural anesthesia during labor, for example? Intravenous narcotics? Her choice is an important facet of your provision of care.
However, such choice requires the patient to give consent and to understand the risk-benefit equation. Documentation by nursing of the patient’s consent and understanding should be complete, including discussion and administration. Anesthesia staff should be clear, complete, and legible in making a record.
Neonatal care. If logistics permit, a member of the pediatrics service should be routinely available to see the newborn at delivery. The patient should view the pediatrician and obstetrician as partners working as a team for the benefit of the mother and her family. This can enhance the patient’s understanding and confidence about the well being of her baby.
Documentation. Although deficient documentation does not, itself, lead to a finding of malpractice, appropriate documentation plays an important role in demonstrating that clinical practices have addressed issues about both allegation and causation of potential adverse outcomes.
We cannot overemphasize that nursing documentation should complement and be consistent with notes made by the physician. That said, nursing notes are not a substitute for the physician’s notes. Practices that integrate the written comments of nursing and physician into a single set of progress notes facilitate this complementary interaction.
3 more clinical scenarios
CASE 2: Admitted at term with contractions
The initial exam determines that this 21-year-old gravida 1 is 2/80/-1. Re-examination in 3 hours finds her at 3-4/80/0.
She requests pain relief and states that she wants epidural anesthesia.
Evaluation 2 hours later suggests secondary arrest of dilation. Oxytocin is begun.
Soon after, late decelerations are observed on the FHR monitor.
Use of exogenous oxytocin in L & D is a double-edged sword: The drug can enhance the safety and efficacy of labor and delivery for mother and fetus, but using it in an unregulated manner (in terms of its indication and administration) can subject both to increased risk.
In fact, it is fair to say that the most widespread and potentially dangerous intervention during labor is the administration of oxytocin. Many expert opinions, guidelines, and strategies have been put forward about intrapartum use of oxytocin. These include consideration of:
- indications
- dosage (including the maximum)
- interval
- fetal response
- ultimately, the availability of a physician during administration to manage any problem that arises.
Considerations in CASE 2
- Always clearly indicate the reason for using oxytocin: Is this an induction? Or an augmentation? Was there evidence of fetal well-being, or non-reassurance, before oxytocin was administered? Certainly, there are circumstances in which either fetal status or non-progression of labor (or both) are an indication for oxytocin. A clear, concise, and properly timed progress note is always appropriate under these circumstances.
- Discuss treatment with the patient. Does she understand why this therapy is being recommended? Does she agree to its use? And does she understand what the alternatives are?
- Verify that nursing has accurately charted this process. Ensure that the nursing staff’s notes are complete and are consistent with yours.
- Simplify the entire process: Use premixed solution and protocol-driven orders. Know what the standards and protocols are in your department. Minimizing patient-to-patient variability should lessen the risk of error.
- Always be available in L & D for the first 30 minutes that oxytocin is being administered. If a problem with excessive uterine activity is going to occur, it is most likely to do so upon initial administration.
- Monitor the FHR continuously. At the first suggestion of a change in fetal status, discontinue oxytocin. Perform a pelvic exam to reassess the situation. Understand and apply appropriate inutero resuscitative measures (IV fluids, O2, change in maternal position). Depending on circumstances, you can consider a restart of oxytocin after the FHR returns to its pre-oxytocin pattern.
- Monitor uterine response to oxytocin. If the membranes are ruptured and if it is clinically feasible, an intrauterine pressure transducer will allow you to more objectively assess the uterine response to oxytocin and make decisions on that basis. Determine beforehand whether the patient is agreeable to this intervention.
- When oxytocin is used for augmentation, reassess labor within 4 hours of achieving a satisfactory pattern. If minimal progress is not made, assess the clinical situation to determine why oxytocin, at an adequate response level, has failed to return labor to a normal active phase slope. Are there minor degrees of malposition? Is there an element of cephalopelvic disproportion? Recall that progress in labor is dependent on multiple factors.
- Chart the process concurrently. Specify options for delivery before delivery.
CASE 3: Spontaneous delivery arrests after delivery of the head
The patient is a multipara with three prior normal vaginal deliveries. Her diabetic screen is negative. At admission, the estimated fetal weight was 3,628 g—in the same range as her other deliveries. A nuchal cord is absent.
After the patient assumes the McRobert’s position, delivery is accomplished with suprapubic pressure. Weakness is noted in the newborn’s right upper extremity. Birth weight is 3,515 g.
Maneuvers to manage shoulder dystocia should be part of all clinicians’ skill set. The sequence of those maneuvers, and their timing, are subject to some variation. Efficacy seems to be related most to recognizing and performing each maneuver properly.
Guidelines for managing shoulder dystocia should include reference to 1) the initial evaluation of the patient on admission to labor and delivery and 2) the delivery itself.3
Considerations in CASE 3
- Before you admit them to L & D, counsel patients who have diabetes, morbid obesity (body mass index >40), or birth trauma in a prior delivery, or who have had a prior large infant (>9 lb birth weight), about the risk of shoulder dystocia. Present possible alternatives, and draw the patient into the conversation.
- Consider delivering all women at term in the McRobert’s position, prophylactically.
- Always check for a nuchal cord after delivery of the head. If you find one, reduce it if possible. Take a few seconds and carefully assess the situation before you cut the umbilical cord.
- Lateral traction on the fetus’ head has the potential to cause tension on the brachial plexus, or make it worse. Gentle rotation of the head (<90 degrees) can move the shoulders into a more favorable location for delivery. Don’t rush—call for assistance! Continuously explain to the patient what you are doing; reassure her about the process.
- Use suprapubic pressure wisely. The anterior shoulder may be dislodged by direct downward force; suprapubic force in a lateral direction may also dislodge the shoulder. Apply force from above the patient’s pelvis. Your assistant will have the best mechanical advantage by standing on a stool.
- Is an episiotomy or episioproctotomy advantageous? In attempting to reach either the anterior or posterior shoulder vaginally, individualized assessment is called for.
- When the posterior shoulder cannot be satisfactorily engaged and moved, try doing so with the anterior shoulder. Insert your hand between the symphysis and the fetal head and place downward pressure on the head to dislodge it and complete the delivery.
- If it becomes necessary to attempt delivery by direct traction on the posterior hand or arm, try to avoid extension. Maintain flexion and move the upper extremity across the fetal chest before you attempt extension.
- Repeat these maneuvers a second time before you attempt cephalic replacement or other maneuvers. Remember to move with deliberate speed to lessen the risk of making the injury worse. Have pediatric support present. Continue speaking with and reassuring the patient.
- Under anesthesia in the operating room, perform a hysterotomy incision. With an assistant working through the vagina, combine the forces available to complete the delivery.
- After delivery is complete, take time to write a note. (Speak with the patient and her family first, however.) Read the notes written by nursing. If they are not available when you write your note, mention that. Add a second note later, when nursing notes become available.
CASE 4: Meconium-stained fluid
A 35-year-old multigravida is 6 to 7 cm dilated. Her membranes have just spontaneously ruptured; you note copious meconium-stained fluid. The FHR demonstrates recurrent variable decelerations; baseline fetal heart rate remains normal.
The description and implications of various FHR patterns are important when documenting the fetal metabolic state during the birth process. Current guidelines have attempted to simplify, standardize, and clarify the interpretation of the FHR tracing.4
Considerations in CASE 4
- Explain the situation to the patient. Perform a pelvic examination. If possible, wait for nursing assistance to ensure accurate documentation.
- Reassure the patient; help her move to a lateral position. Observe the FHR monitor for a response.
- Administer supplemental O2. Increase IV fluids to facilitate utero-placental perfusion.
- If useful or necessary, consider attaching a fetal scalp electrode to better delineate fetal status.
- When the FHR returns to baseline state (before spontaneous rupture of membranes), perform vibro-acoustic stimulation as a test to support fetal well-being.
- Engage the patient and her family in a discussion about the sequence of events. Depending on the acuity of the situation, allow her to voice her concerns and reiterate what has occurred, and what will occur.
- Outline a plan of management to the patient—verbally and in the record—with clear reference to events that have occurred. Then, stick to that plan!
- Carefully review corresponding nursing notes. Always write your own assessment of events and actions.
Summing up: three “keepers”
First, the cornerstones of your effort to reduce malpractice risk are 1) thoughtful and informed discussion with the patient and 2) clear, concise documentation.
Second, don’t expect to be able to eliminate unnecessary or inappropriate allegations of medical malpractice; the best you can do is limit them.
Third, and most important, remember: The knowledgeable clinician you strive to be will make appropriate judgments in a timely fashion and will take appropriate actions to provide good medical care.
We want to hear from you! Tell us what you think.
1. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
2. Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199(2):105.e1-e7.
3. Crofts JF, Fox F, Ellis D. Observations from 450 shoulder dystocia simulations: lessons for skills training. Obstet Gynecol. 2008;112(4):906-912.
4. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring. Obstet Gynecol. 2008;112(3):661-666.
5. Best practice. Web site. 2010. http://www.businessdictionary.com/definition/best-practice.html. Accessed December 17, 2010.
6. Sackett DL, Rosenberg WC, Gray JA, Haynes BR, Richardson WS. Evidence based medicine: what it is and what it isn’t 1996;312(7023):71-72.
7. Hayes EJ, Weinstein L. Improving patient safety and uniformity of care by a standardized regimen for the use of oxytocin. Am J Obstet Gynecol. 2008;198(6):622.e1-7.
8. Proctor SJ, Taylor PR. A practical guide to continuous population-based data collection (PACE): a process facilitating uniformity of care and research into practice. 2000;93(2):67-73.
9. Cohen W, Friedman EA. Management of Labor. Baltimore, MD: University Park Press; 1983.
1. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
2. Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199(2):105.e1-e7.
3. Crofts JF, Fox F, Ellis D. Observations from 450 shoulder dystocia simulations: lessons for skills training. Obstet Gynecol. 2008;112(4):906-912.
4. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring. Obstet Gynecol. 2008;112(3):661-666.
5. Best practice. Web site. 2010. http://www.businessdictionary.com/definition/best-practice.html. Accessed December 17, 2010.
6. Sackett DL, Rosenberg WC, Gray JA, Haynes BR, Richardson WS. Evidence based medicine: what it is and what it isn’t 1996;312(7023):71-72.
7. Hayes EJ, Weinstein L. Improving patient safety and uniformity of care by a standardized regimen for the use of oxytocin. Am J Obstet Gynecol. 2008;198(6):622.e1-7.
8. Proctor SJ, Taylor PR. A practical guide to continuous population-based data collection (PACE): a process facilitating uniformity of care and research into practice. 2000;93(2):67-73.
9. Cohen W, Friedman EA. Management of Labor. Baltimore, MD: University Park Press; 1983.
Postpartum hemorrhage: 11 critical questions, answered by an expert
We know the potentially tragic outcome of postpartum hemorrhage (PPH): Worldwide, more than 140,000 women die every year as a result of PPH—one death every 4 minutes! Lest you dismiss PPH as a concern largely for developing countries, where it accounts for 25% of maternal deaths, consider this: In our highly developed nation, it accounts for nearly 8% of maternal deaths—a troubling statistic, to say the least.
The significant maternal death rate associated with PPH, and questions about how to reduce it, prompted the editors of OBG Management to talk with Haywood L. Brown, MD. Dr. Brown is Roy T. Parker Professor and chair of obstetrics and gynecology at Duke University Medical Center in Durham, NC. He is also a nationally recognized specialist in maternal-fetal medicine. In this interview, he discusses the full spectrum of management of PPH, from proactive assessment of a woman’s risk to determination of the cause to the tactic of last resort, emergent hysterectomy.
Uterine atony is the leading cause of postpartum hemorrhage. When medical management fails to stanch the bleeding, bilateral uterine artery ligation is one surgical option.
1. What is PPH?
OBG Management: Dr. Brown, let’s start with a simple but important aspect of PPH—how do you define it?
Dr. Brown: Obstetric hemorrhage is excessive bleeding that occurs during the intrapartum or postpartum period—specifically, estimated blood loss of 500 mL or more after vaginal delivery or 1,000 mL or more after cesarean delivery.
PPH is characterized as early or late, depending on whether the bleeding occurs within 24 hours of delivery (early, or primary) or between 24 hours and 6 to 12 weeks postpartum (late, or secondary). Primary PPH occurs in 4% to 6% of pregnancies.
Another way to define PPH: a decline of 10% or more in the baseline hematocrit level.
OBG Management: How do you measure blood loss?
Dr. Brown: The estimation of blood loss after delivery is an inexact science and typically yields an underestimation. Most clinicians rely on visual inspection to estimate the amount of blood collected in the drapes after vaginal delivery and in the suction bottles after cesarean delivery. Some facilities weigh lap pads or drapes to get a more accurate assessment of blood loss. In a routine delivery, no specific calorimetric measuring devices are used to estimate blood loss.
At my institution, we make an attempt to estimate blood loss at every delivery—vaginal or cesarean—and record the estimate. By doing this routinely, the clinician improves in accuracy and becomes more adept at identifying excessive bleeding.
OBG Management: Is blood loss the only variable that arouses concern about possible hemorrhage?
Dr. Brown: Because pregnant women experience an increase in blood volume and physiologic cardiovascular changes, the usual sign of significant bleeding can sometimes be masked. Therefore, any changes in maternal vital signs, such as a drop in blood pressure, tachycardia, or sensorial changes, may suggest that more blood has been lost than has been estimated.
Hypotension, dizziness, tachycardia or palpitations, and decreasing urine output will typically occur when more than 10% of maternal blood volume has been lost. In this situation, the patient should be given additional fluids, and a second intravenous line should be started using large-bore, 14-gauge access. In addition, the patient’s hemoglobin and hematocrit levels should be measured. All these actions constitute a first-line strategy to prevent shock and potential irreversible renal failure and cardiovascular collapse.
Low: 500 to 1,000 mL
This level of hemorrhage should be anticipated and can usually be managed with uterine massage and administration of a uterotonic agent, such as oxytocin. Intravenous fluids and careful monitoring of maternal vital signs are also warranted.
Active management of the third stage of labor has been shown to reduce the risk of significant postpartum hemorrhage (PPH). Active management includes:
- administration of a uterotonic agent immediately after delivery of the infant
- early cord clamping and cutting
- gentle cord traction with uterine counter-traction when the uterus is well contracted
- uterine massage.2
If these methods are unsuccessful in correcting the atony, uterotonics such as a prostaglandin (rectally administered misoprostol [800 mg] or intramuscular carboprost tromethamine [Hemabate; 250 μg/mL]) will usually succeed.
Medium: 1,000 to 1,500 mL
Blood loss of this volume is usually accompanied by cardiovascular signs, such as a fall in blood pressure, diaphoresis, and tachycardia. Women with this level of hemorrhage exhibit mild signs of shock.
It is important to correct maternal hypotension with fluids, restabilize vital signs, and resolve the bleeding expeditiously. If uterotonics and massage fail to stanch the bleeding, consider placing a balloon (e.g., Bakri balloon). Once the balloon is placed and inflated, it can be left for as long as 24 hours or until the uterus regains its tone.
Be sure to check hemoglobin and hematocrit levels and transfuse the patient, if necessary, especially if vital signs have not stabilized.
High: 1,500 to 2,000 mL, or greater
This is a medical emergency that must be managed aggressively to prevent morbidity and death. Blood loss of this volume will usually bring significant cardiovascular changes, such as hypotension, tachycardia, restlessness, pallor, oliguria, and cardiovascular collapse from hemorrhagic shock. this degree of blood loss means that the patient has lost 25% to 35% of her blood volume and will need blood-product replacement to prevent coagulation and the cascade of hemorrhage.
If conservative measures are unsuccessful, timely surgical intervention with B-Lynch suture, uterine vessel ligation, or hysterectomy is lifesaving.—HAYWOOD L. BROWN, MD
2. What causes PPH?
OBG Management: Why does PPH occur?
Dr. Brown: The leading cause is uterine atony, a failure of the uterus to contract and undergo resolution following delivery of an infant. Approximately 80% of cases of early PPH are related to uterine atony.
There are other causes of PPH:
- lacerations of the genital tract (perineum, vagina, cervix, or uterus)
- retained fragments of placental tissue
- uterine rupture
- blood clotting abnormalities
- uterine inversion.
3. Is it possible to prepare for PPH?
OBG Management: What is the starting point for management of PPH?
Dr. Brown: Prevention of, and preparation for, hemorrhage begin well before delivery. During the prenatal period, for example, it is important to assess the woman’s level of risk for PPH. Among the variables that increase her risk:
- any situation that leads to overstretching of the uterus, including multiple gestation, whether delivery is vaginal or cesarean
- a history of PPH.
It is important that women with these characteristics maintain adequate hemoglobin and hematocrit levels by taking vitamin and iron supplements in the antepartum period.
In addition, women who have abnormal placental implantation, such as placenta previa, are at risk for bleeding during the antepartum period and during cesarean delivery. They should maintain a hematocrit in the mid-30s because of expected blood loss during delivery.
OBG Management: What preparatory steps should be taken at the time of hospital admission if a woman has an elevated risk of bleeding?
Dr. Brown: When the patient is hospitalized in anticipation of delivery—whether vaginal or cesarean—the team should assess her hemoglobin and hematocrit levels and type and screen for possible transfusion. The patient should also be apprised of her risk and the potential for transfusion.
Last, the anesthesia team should be alerted to her risk factors for postpartum bleeding.
4. What intrapartum variables signal an increased risk of PPH?
OBG Management: During labor and delivery, what variables signal an elevated risk of bleeding?
Dr. Brown: Risk factors for hemorrhage become more apparent during this period. They include prolonged or rapid labor, prolonged use of oxytocin, operative delivery, infections such as chorioamnionitis, and vaginal birth after cesarean delivery (VBAC).
Bleeding with VBAC merits special attention because it could signal uterine rupture. Women who have a low transverse uterine scar and who undergo VBAC have a risk of uterine scar separation during labor of 0.5% to 1%.
OBG Management: What about retained placenta or a placenta that requires manual removal?
Dr. Brown: These intrapartum variables are not as easy to anticipate. They may suggest a condition such as placenta accreta, especially if the patient is undergoing VBAC.
Uterine inversion can also lead to hemorrhage and is a medical emergency.
OBG Management: What steps should be taken at the time of labor to ensure a safe outcome?
Dr. Brown: A type and screen should be available for all women on labor and delivery, and the team should anticipate the need to cross-match for blood if there is a high potential for transfusion. For example, a woman known to have anemia (hematocrit <30%) should have a cross-match performed so that blood can be prepared for transfusion.
In addition, women who are undergoing planned delivery for placental implantation disorders should have blood in the operating room ready for transfusion when cesarean is performed. These women are at great risk of hemorrhage and peripartum hysterectomy.
5. What first-line strategies do you recommend?
OBG Management: Do you recommend oxytocin administration and fundal massage for every patient after delivery of the infant?
Dr. Brown: Yes. These strategies lessen the risk of uterine atony and excessive bleeding after vaginal delivery. At the time of cesarean delivery, expression of the placenta and uterine massage, along with oxytocin administration, reduce the risk of excessive blood loss.
If bleeding continues even after the uterus begins to contract, look for other causes of the bleeding, such as uterine laceration or retained placental fragments.
OBG Management: What uterotonic agents do you use besides oxytocin, and when?
Dr. Brown: Oxytocin is the first-line agent for control of hemorrhage. I give a dosage of 10 to 40 U/L of normal saline or lactated Ringer solution, infused continuously. Alternatively, 10 U can be given intramuscularly (IM). Second-line drugs and their dosages are listed in the TABLE.
Uterotonic agents and how to administer them
| Drug | Dosage and route | Considerations |
|---|---|---|
| FIRST-LINE | ||
| Oxytocin | 10–40 U/L of saline or lactated ringer solution, infused continuously, Or 10 U IM | The preferred drug—often the only one needed |
| SECOND-LINE | ||
| Misoprostol (Cytotec, Prostaglandin e1) | 800–1,000 μg can be given rectally | Often, the second-line drug that is given just after oxytocin because it is easy to administer |
| Methylergonovine (Methergine) | 0.2 mg IM every 2–4 hr | Contraindicated in hypertension |
| Carboprost tromethamine (Hemabate) | 0.25 mg IM every 15–90 minutes (maximum of 8 doses) | Avoid in patients who have asthma. Contra-indicated in hepatic, renal, and cardiac disease |
| Dinoprostone (Prostin e2) | 20 mg suppository can be given vaginally or rectally every 2 hours | Avoid in hypotension |
6. How do you assess the patient once PPH is identified?
OBG Management: How do you assess the patient after hemorrhage begins?
Dr. Brown: We recheck the hemoglobin and hematocrit levels and monitor vital signs for hypotension and tachycardia. We also begin fluid resuscitation and type and cross-match blood and blood products.
A delayed response to hemorrhage raises the risk of maternal morbidity and death.
We notify the anesthesia team when it seems likely that a surgical approach to the hemorrhage will be needed. And we notify interventional radiology if the bleeding may respond to uterine artery embolization.
7. Why is it important to replace blood products?
OBG Management: You’ve been known to say, “The more blood a patient loses, the more blood she loses.” What do you mean by that?
Dr. Brown: Excessive bleeding leads to a loss of critical clotting factors that are made in the liver. Once the clotting factors are depleted, the woman is at risk of coagulopathy or disseminated intravascular coagulation. This depletion potentiates the cycle of hemorrhage. When that occurs, the hemorrhage can be controlled only with transfusion of red blood cells (RBCs) and replacement of clotting factors with fresh frozen plasma, platelets, and cryoprecipitate, along with prompt correction of the process that is causing the bleeding.
OBG Management: What blood products do you administer to a patient with hemorrhage, and when?
Dr. Brown: The first line of defense for blood loss requiring transfusion is packed RBCs. Each unit of packed cells increases the hematocrit by 3% and hemoglobin by 1 g/dL, assuming bleeding is under control. After that, consider:
- Platelets. Depending on the severity of the hemorrhage and the level of platelets once the coagulation status is checked, platelets can be given. A 50-mL unit can raise the platelet count 5,000–10,000/mm3. Platelets should be considered if the count is below 50,000/mm3.
- Fresh frozen plasma should be given to replace clotting factors. Fresh frozen plasma contains fibrinogen, antithrombin III, factor V, and factor VIII. Each unit of fresh frozen plasma increases the fibrinogen level by 10 mg/dL.
- Cryoprecipitate contains fibrinogen, factors VIII and XIII, and von Willebrand factor. Each unit of cryoprecipitate increases fibrinogen by 10 mg/dL.
- Factor VII can be given if the hemorrhage is still active, but it should only be given after fresh frozen plasma and cryo-precipitate have been given to replace clotting factors. Factor VII is ineffective without clotting factor replacement prior to its administration. This medication is associated with a high risk of thromboembolism. It is also expensive.
- Synthetic fibrinogen (RiaSTAP) is available for use in the United States, but it has FDA approval only for the treatment of acute bleeding in patients who have congenital fibrinogen deficiency. It may have potential for use during PPH when essential clotting factors have been depleted.
A woman who is obese has additional risk factors for hemorrhage. Obesity itself is associated with prolonged labor and large-for-gestational-age infants, which, in turn, lead to poor contractility of the uterus and the potential for early postpartum hemorrhage.
Begin by ensuring that the obese or morbidly obese woman has appropriate intravenous access at the time of labor and receives early regional anesthesia (epidural). also alert anesthesia to the risk and assess baseline hemoglobin and hematocrit levels, including a type and screen.
An obese woman undergoing cesarean delivery has a heightened risk of uterine laceration, difficult extraction of the fetus, and uterine atony, especially if prolonged labor preceded the cesarean. Second-stage arrest and prolonged pushing before the cesarean may make extraction of the infant difficult and lead to poor uterine contractility once the placenta is removed.
All obese women, as well as other women at risk of postpartum uterine atony, should have oxytocin infused before the placenta is removed, especially at the time of cesarean delivery. Expressing the placenta at the time of cesarean delivery—as opposed to manual removal—is associated with lower blood loss and allows the uterus to begin contracting before the placenta is removed.—HAYWOOD L. BROWN, MD
8. When do you use the intrauterine balloon?
OBG Management: When is the intrauterine balloon a management option?
Dr. Brown: The balloon offers a way to actively manage hemorrhage and has been associated with decreasing morbidity and a reduced need for surgical intervention, including hysterectomy. It works through a tamponade effect. Once the balloon is inflated with 300 to 500 mL of saline, it compresses the uterine cavity until the uterus develops predelivery tone. It can be left in place as long as 24 hours, need be.
Several balloons are available for use, with the Bakri balloon being the prototype. The balloon may cut off uterine blood flow as a mechanism of action.
Before the advent of manufactured balloons, uterine tamponade was attempted using packing with gauze and a large-bore Foley catheter.
9. How do you proceed when surgery is necessary?
OBG Management: What surgical techniques—aside from hysterectomy—may be useful in stanching hemorrhage?
Dr. Brown: The first-line surgical approach after vaginal delivery is uterine exploration to evacuate uterine clots and check for retained placental fragments. This act alone may impart improved uterine contractility. If retained placental fragments are suspected, a gentle curettage of the uterine cavity, using a large curette, is appropriate.
When it is obvious that atony is the cause of the hemorrhage, and medical management has failed, these surgical steps are appropriate:
- Uterine artery ligation, using the “O’Leary” technique, can be performed bilaterally. The utero-ovarian vessels can also be ligated (but not cut!)
- B-Lynch suture as a technique to compress the uterus. This strategy uses outside, draping, absorbable suture to collapse the uterine cavity. It can be quite successful when combined with the use of uterotonics. One study reported more than 1,000 B-Lynch procedures, with only seven failures.1 Hemostatic multiple-square compression is a surgical technique that works according to a similar principle
- Hypogastric artery ligation can be performed by an experienced surgeon but is rarely employed in severe hemorrhage owing to the risk of complications and lengthy procedure time.
OBG Management: When does hysterectomy become an option?
Dr. Brown: Hysterectomy is the last defense against morbidity and maternal death from hemorrhage due to atony.
Clearly, when hysterectomy is performed, sooner is better than later, especially if uterine artery ligation and B-Lynch suture do not appear to be controlling the hemorrhage and the patient is hemodynamically unstable.
If the patient is a young woman with low parity, the uterus should be preserved, if at all possible, unless the hemorrhage cannot be controlled and the woman’s life is jeopardized.
When a uterine rupture has occurred, usually after a VBAC attempt, it may be prudent to proceed to hysterectomy, especially if the uterus appears to be difficult to repair.
10. When do you call for help?
OBG Management: When do you call in extra help?
Dr. Brown: As soon as hemorrhage occurs, the team should be assembled. It is critical that anesthesia be notified immediately, in the event that the patient requires surgical management. The blood bank should be notified that blood and blood products are likely to be required.
We designate a nursing leader to monitor the patient and another to keep the staff and unit on alert for potential surgical intervention. If uterine rupture or an invasive placental abnormality is suspected, we assemble the surgical team, including any potential consultant surgeon. We also notify the best available surgeons so that they can be ready to perform the necessary techniques. In addition, we notify the OR and surgical intensive care unit, in case they are needed.
OBG Management: How can obstetricians and obstetric units practice the response to OB hemorrhage so that, when a hemorrhage occurs, they are at the top of their game?
Dr. Brown: Obstetric units prepare by performing drills and simulations. These drills are now considered part of most units’ quality and safety programs.
Because obstetric hemorrhage can occur on any unit at any time, the team must be prepared to respond around the clock promptly and effectively to reduce the risk of morbidity and death.
After emergent surgical management of obstetric hemorrhage, the team should be assembled again to discuss what occurred and how they performed or could have performed more effectively as a team.
OBG Management: Should all obstetricians who perform repeat cesarean delivery be able to perform a cesarean hysterectomy in the event that uncontrollable hemorrhage is encountered?
Dr. Brown: It is an absolute must that any clinician who allows VBAC be capable of performing peripartum cesarean hysterectomy and know the indications for hysterectomy, as we have discussed. In fact, any obstetrician who performs cesarean delivery should be capable of performing a cesarean hysterectomy.
11. What do you recommend for practice?
OBG Management: How would you summarize the main points of management of postpartum hemorrhage?
Dr. Brown: I would suggest that the first step is organizing the team (obstetricians, nurses, anesthesiologist), followed by:
- resuscitation of the mother with oxygen and fluids through large-bore intravenous access sites
- notification of the blood bank (with typing and cross-matching) of the possible need for 4 to 6 U of blood for trans-fusion
- liberal assessment of laboratory values, especially coagulation status (International Normalized Ratio [INR], prothrombin time, and partial thromboplastin time) and blood counts (hemoglobin and hematocrit). Values may be lower if there has been significant blood loss and aggressive fluid resuscitation. Blood products such as fresh frozen plasma and cryoprecipitate are indicated, in addition to packed RBCs, if the patient has or is developing a coagulopathy. Also give platelets if the count is low. Once it becomes apparent that surgical intervention will be necessary, begin transfusion and replace clotting factors before beginning the procedure
- monitoring of vital signs and urine output throughout resuscitation and medical and surgical intervention
- elimination of the cause of bleeding as soon as possible by whatever means necessary to prevent maternal death, beginning with conservative medical management and, if necessary, followed by surgical intervention.
Tell us about a challenging case of postpartum hemorrhage and how you managed it.
Go to Send Us Your Letters. Please include your name, city, and state. We’ll publish intriguing “pearls” in an upcoming issue.
1. Allam MS, B-Lynch C. The B-Lynch and other uterine compression techniques. Int J Gynaecol Obstet. 2005;89(3):236-241.
2. Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev. 2000;(3):CD000007.-
- Activated factor VII proves to be a lifesaver in postpartum hemorrhage
Robert L. Barbieri, MD (February 2007) - Postpartum hemorrhage: Solutions to 2 intractable cases
Michael L. Stitely, MD, and Robert B. Gherman, MD (April 2007) - Give a uterotonic routinely during the third stage of labor
Robert L. Barbieri, MD (May 2007) - Consider retroperitoneal packing for postpartum hemorrhage
Maj. William R. Fulton, DO (July 2008) - You should add the Bakri balloon to your treatments for OB bleeds
Robert L. Barbieri, MD (February 2009) - Planning reduces the risk of maternal death. This tool helps.
Robert L. Barbieri, MD (August 2009) - What you can do to optimize blood conservation in ObGyn practice
Eric J. Bieber, MD, Linda Scott, RN, Corinna Muller, DO, Nancy Nuss, RN, and Edie L. Derian, MD (February 2010)
We know the potentially tragic outcome of postpartum hemorrhage (PPH): Worldwide, more than 140,000 women die every year as a result of PPH—one death every 4 minutes! Lest you dismiss PPH as a concern largely for developing countries, where it accounts for 25% of maternal deaths, consider this: In our highly developed nation, it accounts for nearly 8% of maternal deaths—a troubling statistic, to say the least.
The significant maternal death rate associated with PPH, and questions about how to reduce it, prompted the editors of OBG Management to talk with Haywood L. Brown, MD. Dr. Brown is Roy T. Parker Professor and chair of obstetrics and gynecology at Duke University Medical Center in Durham, NC. He is also a nationally recognized specialist in maternal-fetal medicine. In this interview, he discusses the full spectrum of management of PPH, from proactive assessment of a woman’s risk to determination of the cause to the tactic of last resort, emergent hysterectomy.
Uterine atony is the leading cause of postpartum hemorrhage. When medical management fails to stanch the bleeding, bilateral uterine artery ligation is one surgical option.
1. What is PPH?
OBG Management: Dr. Brown, let’s start with a simple but important aspect of PPH—how do you define it?
Dr. Brown: Obstetric hemorrhage is excessive bleeding that occurs during the intrapartum or postpartum period—specifically, estimated blood loss of 500 mL or more after vaginal delivery or 1,000 mL or more after cesarean delivery.
PPH is characterized as early or late, depending on whether the bleeding occurs within 24 hours of delivery (early, or primary) or between 24 hours and 6 to 12 weeks postpartum (late, or secondary). Primary PPH occurs in 4% to 6% of pregnancies.
Another way to define PPH: a decline of 10% or more in the baseline hematocrit level.
OBG Management: How do you measure blood loss?
Dr. Brown: The estimation of blood loss after delivery is an inexact science and typically yields an underestimation. Most clinicians rely on visual inspection to estimate the amount of blood collected in the drapes after vaginal delivery and in the suction bottles after cesarean delivery. Some facilities weigh lap pads or drapes to get a more accurate assessment of blood loss. In a routine delivery, no specific calorimetric measuring devices are used to estimate blood loss.
At my institution, we make an attempt to estimate blood loss at every delivery—vaginal or cesarean—and record the estimate. By doing this routinely, the clinician improves in accuracy and becomes more adept at identifying excessive bleeding.
OBG Management: Is blood loss the only variable that arouses concern about possible hemorrhage?
Dr. Brown: Because pregnant women experience an increase in blood volume and physiologic cardiovascular changes, the usual sign of significant bleeding can sometimes be masked. Therefore, any changes in maternal vital signs, such as a drop in blood pressure, tachycardia, or sensorial changes, may suggest that more blood has been lost than has been estimated.
Hypotension, dizziness, tachycardia or palpitations, and decreasing urine output will typically occur when more than 10% of maternal blood volume has been lost. In this situation, the patient should be given additional fluids, and a second intravenous line should be started using large-bore, 14-gauge access. In addition, the patient’s hemoglobin and hematocrit levels should be measured. All these actions constitute a first-line strategy to prevent shock and potential irreversible renal failure and cardiovascular collapse.
Low: 500 to 1,000 mL
This level of hemorrhage should be anticipated and can usually be managed with uterine massage and administration of a uterotonic agent, such as oxytocin. Intravenous fluids and careful monitoring of maternal vital signs are also warranted.
Active management of the third stage of labor has been shown to reduce the risk of significant postpartum hemorrhage (PPH). Active management includes:
- administration of a uterotonic agent immediately after delivery of the infant
- early cord clamping and cutting
- gentle cord traction with uterine counter-traction when the uterus is well contracted
- uterine massage.2
If these methods are unsuccessful in correcting the atony, uterotonics such as a prostaglandin (rectally administered misoprostol [800 mg] or intramuscular carboprost tromethamine [Hemabate; 250 μg/mL]) will usually succeed.
Medium: 1,000 to 1,500 mL
Blood loss of this volume is usually accompanied by cardiovascular signs, such as a fall in blood pressure, diaphoresis, and tachycardia. Women with this level of hemorrhage exhibit mild signs of shock.
It is important to correct maternal hypotension with fluids, restabilize vital signs, and resolve the bleeding expeditiously. If uterotonics and massage fail to stanch the bleeding, consider placing a balloon (e.g., Bakri balloon). Once the balloon is placed and inflated, it can be left for as long as 24 hours or until the uterus regains its tone.
Be sure to check hemoglobin and hematocrit levels and transfuse the patient, if necessary, especially if vital signs have not stabilized.
High: 1,500 to 2,000 mL, or greater
This is a medical emergency that must be managed aggressively to prevent morbidity and death. Blood loss of this volume will usually bring significant cardiovascular changes, such as hypotension, tachycardia, restlessness, pallor, oliguria, and cardiovascular collapse from hemorrhagic shock. this degree of blood loss means that the patient has lost 25% to 35% of her blood volume and will need blood-product replacement to prevent coagulation and the cascade of hemorrhage.
If conservative measures are unsuccessful, timely surgical intervention with B-Lynch suture, uterine vessel ligation, or hysterectomy is lifesaving.—HAYWOOD L. BROWN, MD
2. What causes PPH?
OBG Management: Why does PPH occur?
Dr. Brown: The leading cause is uterine atony, a failure of the uterus to contract and undergo resolution following delivery of an infant. Approximately 80% of cases of early PPH are related to uterine atony.
There are other causes of PPH:
- lacerations of the genital tract (perineum, vagina, cervix, or uterus)
- retained fragments of placental tissue
- uterine rupture
- blood clotting abnormalities
- uterine inversion.
3. Is it possible to prepare for PPH?
OBG Management: What is the starting point for management of PPH?
Dr. Brown: Prevention of, and preparation for, hemorrhage begin well before delivery. During the prenatal period, for example, it is important to assess the woman’s level of risk for PPH. Among the variables that increase her risk:
- any situation that leads to overstretching of the uterus, including multiple gestation, whether delivery is vaginal or cesarean
- a history of PPH.
It is important that women with these characteristics maintain adequate hemoglobin and hematocrit levels by taking vitamin and iron supplements in the antepartum period.
In addition, women who have abnormal placental implantation, such as placenta previa, are at risk for bleeding during the antepartum period and during cesarean delivery. They should maintain a hematocrit in the mid-30s because of expected blood loss during delivery.
OBG Management: What preparatory steps should be taken at the time of hospital admission if a woman has an elevated risk of bleeding?
Dr. Brown: When the patient is hospitalized in anticipation of delivery—whether vaginal or cesarean—the team should assess her hemoglobin and hematocrit levels and type and screen for possible transfusion. The patient should also be apprised of her risk and the potential for transfusion.
Last, the anesthesia team should be alerted to her risk factors for postpartum bleeding.
4. What intrapartum variables signal an increased risk of PPH?
OBG Management: During labor and delivery, what variables signal an elevated risk of bleeding?
Dr. Brown: Risk factors for hemorrhage become more apparent during this period. They include prolonged or rapid labor, prolonged use of oxytocin, operative delivery, infections such as chorioamnionitis, and vaginal birth after cesarean delivery (VBAC).
Bleeding with VBAC merits special attention because it could signal uterine rupture. Women who have a low transverse uterine scar and who undergo VBAC have a risk of uterine scar separation during labor of 0.5% to 1%.
OBG Management: What about retained placenta or a placenta that requires manual removal?
Dr. Brown: These intrapartum variables are not as easy to anticipate. They may suggest a condition such as placenta accreta, especially if the patient is undergoing VBAC.
Uterine inversion can also lead to hemorrhage and is a medical emergency.
OBG Management: What steps should be taken at the time of labor to ensure a safe outcome?
Dr. Brown: A type and screen should be available for all women on labor and delivery, and the team should anticipate the need to cross-match for blood if there is a high potential for transfusion. For example, a woman known to have anemia (hematocrit <30%) should have a cross-match performed so that blood can be prepared for transfusion.
In addition, women who are undergoing planned delivery for placental implantation disorders should have blood in the operating room ready for transfusion when cesarean is performed. These women are at great risk of hemorrhage and peripartum hysterectomy.
5. What first-line strategies do you recommend?
OBG Management: Do you recommend oxytocin administration and fundal massage for every patient after delivery of the infant?
Dr. Brown: Yes. These strategies lessen the risk of uterine atony and excessive bleeding after vaginal delivery. At the time of cesarean delivery, expression of the placenta and uterine massage, along with oxytocin administration, reduce the risk of excessive blood loss.
If bleeding continues even after the uterus begins to contract, look for other causes of the bleeding, such as uterine laceration or retained placental fragments.
OBG Management: What uterotonic agents do you use besides oxytocin, and when?
Dr. Brown: Oxytocin is the first-line agent for control of hemorrhage. I give a dosage of 10 to 40 U/L of normal saline or lactated Ringer solution, infused continuously. Alternatively, 10 U can be given intramuscularly (IM). Second-line drugs and their dosages are listed in the TABLE.
Uterotonic agents and how to administer them
| Drug | Dosage and route | Considerations |
|---|---|---|
| FIRST-LINE | ||
| Oxytocin | 10–40 U/L of saline or lactated ringer solution, infused continuously, Or 10 U IM | The preferred drug—often the only one needed |
| SECOND-LINE | ||
| Misoprostol (Cytotec, Prostaglandin e1) | 800–1,000 μg can be given rectally | Often, the second-line drug that is given just after oxytocin because it is easy to administer |
| Methylergonovine (Methergine) | 0.2 mg IM every 2–4 hr | Contraindicated in hypertension |
| Carboprost tromethamine (Hemabate) | 0.25 mg IM every 15–90 minutes (maximum of 8 doses) | Avoid in patients who have asthma. Contra-indicated in hepatic, renal, and cardiac disease |
| Dinoprostone (Prostin e2) | 20 mg suppository can be given vaginally or rectally every 2 hours | Avoid in hypotension |
6. How do you assess the patient once PPH is identified?
OBG Management: How do you assess the patient after hemorrhage begins?
Dr. Brown: We recheck the hemoglobin and hematocrit levels and monitor vital signs for hypotension and tachycardia. We also begin fluid resuscitation and type and cross-match blood and blood products.
A delayed response to hemorrhage raises the risk of maternal morbidity and death.
We notify the anesthesia team when it seems likely that a surgical approach to the hemorrhage will be needed. And we notify interventional radiology if the bleeding may respond to uterine artery embolization.
7. Why is it important to replace blood products?
OBG Management: You’ve been known to say, “The more blood a patient loses, the more blood she loses.” What do you mean by that?
Dr. Brown: Excessive bleeding leads to a loss of critical clotting factors that are made in the liver. Once the clotting factors are depleted, the woman is at risk of coagulopathy or disseminated intravascular coagulation. This depletion potentiates the cycle of hemorrhage. When that occurs, the hemorrhage can be controlled only with transfusion of red blood cells (RBCs) and replacement of clotting factors with fresh frozen plasma, platelets, and cryoprecipitate, along with prompt correction of the process that is causing the bleeding.
OBG Management: What blood products do you administer to a patient with hemorrhage, and when?
Dr. Brown: The first line of defense for blood loss requiring transfusion is packed RBCs. Each unit of packed cells increases the hematocrit by 3% and hemoglobin by 1 g/dL, assuming bleeding is under control. After that, consider:
- Platelets. Depending on the severity of the hemorrhage and the level of platelets once the coagulation status is checked, platelets can be given. A 50-mL unit can raise the platelet count 5,000–10,000/mm3. Platelets should be considered if the count is below 50,000/mm3.
- Fresh frozen plasma should be given to replace clotting factors. Fresh frozen plasma contains fibrinogen, antithrombin III, factor V, and factor VIII. Each unit of fresh frozen plasma increases the fibrinogen level by 10 mg/dL.
- Cryoprecipitate contains fibrinogen, factors VIII and XIII, and von Willebrand factor. Each unit of cryoprecipitate increases fibrinogen by 10 mg/dL.
- Factor VII can be given if the hemorrhage is still active, but it should only be given after fresh frozen plasma and cryo-precipitate have been given to replace clotting factors. Factor VII is ineffective without clotting factor replacement prior to its administration. This medication is associated with a high risk of thromboembolism. It is also expensive.
- Synthetic fibrinogen (RiaSTAP) is available for use in the United States, but it has FDA approval only for the treatment of acute bleeding in patients who have congenital fibrinogen deficiency. It may have potential for use during PPH when essential clotting factors have been depleted.
A woman who is obese has additional risk factors for hemorrhage. Obesity itself is associated with prolonged labor and large-for-gestational-age infants, which, in turn, lead to poor contractility of the uterus and the potential for early postpartum hemorrhage.
Begin by ensuring that the obese or morbidly obese woman has appropriate intravenous access at the time of labor and receives early regional anesthesia (epidural). also alert anesthesia to the risk and assess baseline hemoglobin and hematocrit levels, including a type and screen.
An obese woman undergoing cesarean delivery has a heightened risk of uterine laceration, difficult extraction of the fetus, and uterine atony, especially if prolonged labor preceded the cesarean. Second-stage arrest and prolonged pushing before the cesarean may make extraction of the infant difficult and lead to poor uterine contractility once the placenta is removed.
All obese women, as well as other women at risk of postpartum uterine atony, should have oxytocin infused before the placenta is removed, especially at the time of cesarean delivery. Expressing the placenta at the time of cesarean delivery—as opposed to manual removal—is associated with lower blood loss and allows the uterus to begin contracting before the placenta is removed.—HAYWOOD L. BROWN, MD
8. When do you use the intrauterine balloon?
OBG Management: When is the intrauterine balloon a management option?
Dr. Brown: The balloon offers a way to actively manage hemorrhage and has been associated with decreasing morbidity and a reduced need for surgical intervention, including hysterectomy. It works through a tamponade effect. Once the balloon is inflated with 300 to 500 mL of saline, it compresses the uterine cavity until the uterus develops predelivery tone. It can be left in place as long as 24 hours, need be.
Several balloons are available for use, with the Bakri balloon being the prototype. The balloon may cut off uterine blood flow as a mechanism of action.
Before the advent of manufactured balloons, uterine tamponade was attempted using packing with gauze and a large-bore Foley catheter.
9. How do you proceed when surgery is necessary?
OBG Management: What surgical techniques—aside from hysterectomy—may be useful in stanching hemorrhage?
Dr. Brown: The first-line surgical approach after vaginal delivery is uterine exploration to evacuate uterine clots and check for retained placental fragments. This act alone may impart improved uterine contractility. If retained placental fragments are suspected, a gentle curettage of the uterine cavity, using a large curette, is appropriate.
When it is obvious that atony is the cause of the hemorrhage, and medical management has failed, these surgical steps are appropriate:
- Uterine artery ligation, using the “O’Leary” technique, can be performed bilaterally. The utero-ovarian vessels can also be ligated (but not cut!)
- B-Lynch suture as a technique to compress the uterus. This strategy uses outside, draping, absorbable suture to collapse the uterine cavity. It can be quite successful when combined with the use of uterotonics. One study reported more than 1,000 B-Lynch procedures, with only seven failures.1 Hemostatic multiple-square compression is a surgical technique that works according to a similar principle
- Hypogastric artery ligation can be performed by an experienced surgeon but is rarely employed in severe hemorrhage owing to the risk of complications and lengthy procedure time.
OBG Management: When does hysterectomy become an option?
Dr. Brown: Hysterectomy is the last defense against morbidity and maternal death from hemorrhage due to atony.
Clearly, when hysterectomy is performed, sooner is better than later, especially if uterine artery ligation and B-Lynch suture do not appear to be controlling the hemorrhage and the patient is hemodynamically unstable.
If the patient is a young woman with low parity, the uterus should be preserved, if at all possible, unless the hemorrhage cannot be controlled and the woman’s life is jeopardized.
When a uterine rupture has occurred, usually after a VBAC attempt, it may be prudent to proceed to hysterectomy, especially if the uterus appears to be difficult to repair.
10. When do you call for help?
OBG Management: When do you call in extra help?
Dr. Brown: As soon as hemorrhage occurs, the team should be assembled. It is critical that anesthesia be notified immediately, in the event that the patient requires surgical management. The blood bank should be notified that blood and blood products are likely to be required.
We designate a nursing leader to monitor the patient and another to keep the staff and unit on alert for potential surgical intervention. If uterine rupture or an invasive placental abnormality is suspected, we assemble the surgical team, including any potential consultant surgeon. We also notify the best available surgeons so that they can be ready to perform the necessary techniques. In addition, we notify the OR and surgical intensive care unit, in case they are needed.
OBG Management: How can obstetricians and obstetric units practice the response to OB hemorrhage so that, when a hemorrhage occurs, they are at the top of their game?
Dr. Brown: Obstetric units prepare by performing drills and simulations. These drills are now considered part of most units’ quality and safety programs.
Because obstetric hemorrhage can occur on any unit at any time, the team must be prepared to respond around the clock promptly and effectively to reduce the risk of morbidity and death.
After emergent surgical management of obstetric hemorrhage, the team should be assembled again to discuss what occurred and how they performed or could have performed more effectively as a team.
OBG Management: Should all obstetricians who perform repeat cesarean delivery be able to perform a cesarean hysterectomy in the event that uncontrollable hemorrhage is encountered?
Dr. Brown: It is an absolute must that any clinician who allows VBAC be capable of performing peripartum cesarean hysterectomy and know the indications for hysterectomy, as we have discussed. In fact, any obstetrician who performs cesarean delivery should be capable of performing a cesarean hysterectomy.
11. What do you recommend for practice?
OBG Management: How would you summarize the main points of management of postpartum hemorrhage?
Dr. Brown: I would suggest that the first step is organizing the team (obstetricians, nurses, anesthesiologist), followed by:
- resuscitation of the mother with oxygen and fluids through large-bore intravenous access sites
- notification of the blood bank (with typing and cross-matching) of the possible need for 4 to 6 U of blood for trans-fusion
- liberal assessment of laboratory values, especially coagulation status (International Normalized Ratio [INR], prothrombin time, and partial thromboplastin time) and blood counts (hemoglobin and hematocrit). Values may be lower if there has been significant blood loss and aggressive fluid resuscitation. Blood products such as fresh frozen plasma and cryoprecipitate are indicated, in addition to packed RBCs, if the patient has or is developing a coagulopathy. Also give platelets if the count is low. Once it becomes apparent that surgical intervention will be necessary, begin transfusion and replace clotting factors before beginning the procedure
- monitoring of vital signs and urine output throughout resuscitation and medical and surgical intervention
- elimination of the cause of bleeding as soon as possible by whatever means necessary to prevent maternal death, beginning with conservative medical management and, if necessary, followed by surgical intervention.
Tell us about a challenging case of postpartum hemorrhage and how you managed it.
Go to Send Us Your Letters. Please include your name, city, and state. We’ll publish intriguing “pearls” in an upcoming issue.
We know the potentially tragic outcome of postpartum hemorrhage (PPH): Worldwide, more than 140,000 women die every year as a result of PPH—one death every 4 minutes! Lest you dismiss PPH as a concern largely for developing countries, where it accounts for 25% of maternal deaths, consider this: In our highly developed nation, it accounts for nearly 8% of maternal deaths—a troubling statistic, to say the least.
The significant maternal death rate associated with PPH, and questions about how to reduce it, prompted the editors of OBG Management to talk with Haywood L. Brown, MD. Dr. Brown is Roy T. Parker Professor and chair of obstetrics and gynecology at Duke University Medical Center in Durham, NC. He is also a nationally recognized specialist in maternal-fetal medicine. In this interview, he discusses the full spectrum of management of PPH, from proactive assessment of a woman’s risk to determination of the cause to the tactic of last resort, emergent hysterectomy.
Uterine atony is the leading cause of postpartum hemorrhage. When medical management fails to stanch the bleeding, bilateral uterine artery ligation is one surgical option.
1. What is PPH?
OBG Management: Dr. Brown, let’s start with a simple but important aspect of PPH—how do you define it?
Dr. Brown: Obstetric hemorrhage is excessive bleeding that occurs during the intrapartum or postpartum period—specifically, estimated blood loss of 500 mL or more after vaginal delivery or 1,000 mL or more after cesarean delivery.
PPH is characterized as early or late, depending on whether the bleeding occurs within 24 hours of delivery (early, or primary) or between 24 hours and 6 to 12 weeks postpartum (late, or secondary). Primary PPH occurs in 4% to 6% of pregnancies.
Another way to define PPH: a decline of 10% or more in the baseline hematocrit level.
OBG Management: How do you measure blood loss?
Dr. Brown: The estimation of blood loss after delivery is an inexact science and typically yields an underestimation. Most clinicians rely on visual inspection to estimate the amount of blood collected in the drapes after vaginal delivery and in the suction bottles after cesarean delivery. Some facilities weigh lap pads or drapes to get a more accurate assessment of blood loss. In a routine delivery, no specific calorimetric measuring devices are used to estimate blood loss.
At my institution, we make an attempt to estimate blood loss at every delivery—vaginal or cesarean—and record the estimate. By doing this routinely, the clinician improves in accuracy and becomes more adept at identifying excessive bleeding.
OBG Management: Is blood loss the only variable that arouses concern about possible hemorrhage?
Dr. Brown: Because pregnant women experience an increase in blood volume and physiologic cardiovascular changes, the usual sign of significant bleeding can sometimes be masked. Therefore, any changes in maternal vital signs, such as a drop in blood pressure, tachycardia, or sensorial changes, may suggest that more blood has been lost than has been estimated.
Hypotension, dizziness, tachycardia or palpitations, and decreasing urine output will typically occur when more than 10% of maternal blood volume has been lost. In this situation, the patient should be given additional fluids, and a second intravenous line should be started using large-bore, 14-gauge access. In addition, the patient’s hemoglobin and hematocrit levels should be measured. All these actions constitute a first-line strategy to prevent shock and potential irreversible renal failure and cardiovascular collapse.
Low: 500 to 1,000 mL
This level of hemorrhage should be anticipated and can usually be managed with uterine massage and administration of a uterotonic agent, such as oxytocin. Intravenous fluids and careful monitoring of maternal vital signs are also warranted.
Active management of the third stage of labor has been shown to reduce the risk of significant postpartum hemorrhage (PPH). Active management includes:
- administration of a uterotonic agent immediately after delivery of the infant
- early cord clamping and cutting
- gentle cord traction with uterine counter-traction when the uterus is well contracted
- uterine massage.2
If these methods are unsuccessful in correcting the atony, uterotonics such as a prostaglandin (rectally administered misoprostol [800 mg] or intramuscular carboprost tromethamine [Hemabate; 250 μg/mL]) will usually succeed.
Medium: 1,000 to 1,500 mL
Blood loss of this volume is usually accompanied by cardiovascular signs, such as a fall in blood pressure, diaphoresis, and tachycardia. Women with this level of hemorrhage exhibit mild signs of shock.
It is important to correct maternal hypotension with fluids, restabilize vital signs, and resolve the bleeding expeditiously. If uterotonics and massage fail to stanch the bleeding, consider placing a balloon (e.g., Bakri balloon). Once the balloon is placed and inflated, it can be left for as long as 24 hours or until the uterus regains its tone.
Be sure to check hemoglobin and hematocrit levels and transfuse the patient, if necessary, especially if vital signs have not stabilized.
High: 1,500 to 2,000 mL, or greater
This is a medical emergency that must be managed aggressively to prevent morbidity and death. Blood loss of this volume will usually bring significant cardiovascular changes, such as hypotension, tachycardia, restlessness, pallor, oliguria, and cardiovascular collapse from hemorrhagic shock. this degree of blood loss means that the patient has lost 25% to 35% of her blood volume and will need blood-product replacement to prevent coagulation and the cascade of hemorrhage.
If conservative measures are unsuccessful, timely surgical intervention with B-Lynch suture, uterine vessel ligation, or hysterectomy is lifesaving.—HAYWOOD L. BROWN, MD
2. What causes PPH?
OBG Management: Why does PPH occur?
Dr. Brown: The leading cause is uterine atony, a failure of the uterus to contract and undergo resolution following delivery of an infant. Approximately 80% of cases of early PPH are related to uterine atony.
There are other causes of PPH:
- lacerations of the genital tract (perineum, vagina, cervix, or uterus)
- retained fragments of placental tissue
- uterine rupture
- blood clotting abnormalities
- uterine inversion.
3. Is it possible to prepare for PPH?
OBG Management: What is the starting point for management of PPH?
Dr. Brown: Prevention of, and preparation for, hemorrhage begin well before delivery. During the prenatal period, for example, it is important to assess the woman’s level of risk for PPH. Among the variables that increase her risk:
- any situation that leads to overstretching of the uterus, including multiple gestation, whether delivery is vaginal or cesarean
- a history of PPH.
It is important that women with these characteristics maintain adequate hemoglobin and hematocrit levels by taking vitamin and iron supplements in the antepartum period.
In addition, women who have abnormal placental implantation, such as placenta previa, are at risk for bleeding during the antepartum period and during cesarean delivery. They should maintain a hematocrit in the mid-30s because of expected blood loss during delivery.
OBG Management: What preparatory steps should be taken at the time of hospital admission if a woman has an elevated risk of bleeding?
Dr. Brown: When the patient is hospitalized in anticipation of delivery—whether vaginal or cesarean—the team should assess her hemoglobin and hematocrit levels and type and screen for possible transfusion. The patient should also be apprised of her risk and the potential for transfusion.
Last, the anesthesia team should be alerted to her risk factors for postpartum bleeding.
4. What intrapartum variables signal an increased risk of PPH?
OBG Management: During labor and delivery, what variables signal an elevated risk of bleeding?
Dr. Brown: Risk factors for hemorrhage become more apparent during this period. They include prolonged or rapid labor, prolonged use of oxytocin, operative delivery, infections such as chorioamnionitis, and vaginal birth after cesarean delivery (VBAC).
Bleeding with VBAC merits special attention because it could signal uterine rupture. Women who have a low transverse uterine scar and who undergo VBAC have a risk of uterine scar separation during labor of 0.5% to 1%.
OBG Management: What about retained placenta or a placenta that requires manual removal?
Dr. Brown: These intrapartum variables are not as easy to anticipate. They may suggest a condition such as placenta accreta, especially if the patient is undergoing VBAC.
Uterine inversion can also lead to hemorrhage and is a medical emergency.
OBG Management: What steps should be taken at the time of labor to ensure a safe outcome?
Dr. Brown: A type and screen should be available for all women on labor and delivery, and the team should anticipate the need to cross-match for blood if there is a high potential for transfusion. For example, a woman known to have anemia (hematocrit <30%) should have a cross-match performed so that blood can be prepared for transfusion.
In addition, women who are undergoing planned delivery for placental implantation disorders should have blood in the operating room ready for transfusion when cesarean is performed. These women are at great risk of hemorrhage and peripartum hysterectomy.
5. What first-line strategies do you recommend?
OBG Management: Do you recommend oxytocin administration and fundal massage for every patient after delivery of the infant?
Dr. Brown: Yes. These strategies lessen the risk of uterine atony and excessive bleeding after vaginal delivery. At the time of cesarean delivery, expression of the placenta and uterine massage, along with oxytocin administration, reduce the risk of excessive blood loss.
If bleeding continues even after the uterus begins to contract, look for other causes of the bleeding, such as uterine laceration or retained placental fragments.
OBG Management: What uterotonic agents do you use besides oxytocin, and when?
Dr. Brown: Oxytocin is the first-line agent for control of hemorrhage. I give a dosage of 10 to 40 U/L of normal saline or lactated Ringer solution, infused continuously. Alternatively, 10 U can be given intramuscularly (IM). Second-line drugs and their dosages are listed in the TABLE.
Uterotonic agents and how to administer them
| Drug | Dosage and route | Considerations |
|---|---|---|
| FIRST-LINE | ||
| Oxytocin | 10–40 U/L of saline or lactated ringer solution, infused continuously, Or 10 U IM | The preferred drug—often the only one needed |
| SECOND-LINE | ||
| Misoprostol (Cytotec, Prostaglandin e1) | 800–1,000 μg can be given rectally | Often, the second-line drug that is given just after oxytocin because it is easy to administer |
| Methylergonovine (Methergine) | 0.2 mg IM every 2–4 hr | Contraindicated in hypertension |
| Carboprost tromethamine (Hemabate) | 0.25 mg IM every 15–90 minutes (maximum of 8 doses) | Avoid in patients who have asthma. Contra-indicated in hepatic, renal, and cardiac disease |
| Dinoprostone (Prostin e2) | 20 mg suppository can be given vaginally or rectally every 2 hours | Avoid in hypotension |
6. How do you assess the patient once PPH is identified?
OBG Management: How do you assess the patient after hemorrhage begins?
Dr. Brown: We recheck the hemoglobin and hematocrit levels and monitor vital signs for hypotension and tachycardia. We also begin fluid resuscitation and type and cross-match blood and blood products.
A delayed response to hemorrhage raises the risk of maternal morbidity and death.
We notify the anesthesia team when it seems likely that a surgical approach to the hemorrhage will be needed. And we notify interventional radiology if the bleeding may respond to uterine artery embolization.
7. Why is it important to replace blood products?
OBG Management: You’ve been known to say, “The more blood a patient loses, the more blood she loses.” What do you mean by that?
Dr. Brown: Excessive bleeding leads to a loss of critical clotting factors that are made in the liver. Once the clotting factors are depleted, the woman is at risk of coagulopathy or disseminated intravascular coagulation. This depletion potentiates the cycle of hemorrhage. When that occurs, the hemorrhage can be controlled only with transfusion of red blood cells (RBCs) and replacement of clotting factors with fresh frozen plasma, platelets, and cryoprecipitate, along with prompt correction of the process that is causing the bleeding.
OBG Management: What blood products do you administer to a patient with hemorrhage, and when?
Dr. Brown: The first line of defense for blood loss requiring transfusion is packed RBCs. Each unit of packed cells increases the hematocrit by 3% and hemoglobin by 1 g/dL, assuming bleeding is under control. After that, consider:
- Platelets. Depending on the severity of the hemorrhage and the level of platelets once the coagulation status is checked, platelets can be given. A 50-mL unit can raise the platelet count 5,000–10,000/mm3. Platelets should be considered if the count is below 50,000/mm3.
- Fresh frozen plasma should be given to replace clotting factors. Fresh frozen plasma contains fibrinogen, antithrombin III, factor V, and factor VIII. Each unit of fresh frozen plasma increases the fibrinogen level by 10 mg/dL.
- Cryoprecipitate contains fibrinogen, factors VIII and XIII, and von Willebrand factor. Each unit of cryoprecipitate increases fibrinogen by 10 mg/dL.
- Factor VII can be given if the hemorrhage is still active, but it should only be given after fresh frozen plasma and cryo-precipitate have been given to replace clotting factors. Factor VII is ineffective without clotting factor replacement prior to its administration. This medication is associated with a high risk of thromboembolism. It is also expensive.
- Synthetic fibrinogen (RiaSTAP) is available for use in the United States, but it has FDA approval only for the treatment of acute bleeding in patients who have congenital fibrinogen deficiency. It may have potential for use during PPH when essential clotting factors have been depleted.
A woman who is obese has additional risk factors for hemorrhage. Obesity itself is associated with prolonged labor and large-for-gestational-age infants, which, in turn, lead to poor contractility of the uterus and the potential for early postpartum hemorrhage.
Begin by ensuring that the obese or morbidly obese woman has appropriate intravenous access at the time of labor and receives early regional anesthesia (epidural). also alert anesthesia to the risk and assess baseline hemoglobin and hematocrit levels, including a type and screen.
An obese woman undergoing cesarean delivery has a heightened risk of uterine laceration, difficult extraction of the fetus, and uterine atony, especially if prolonged labor preceded the cesarean. Second-stage arrest and prolonged pushing before the cesarean may make extraction of the infant difficult and lead to poor uterine contractility once the placenta is removed.
All obese women, as well as other women at risk of postpartum uterine atony, should have oxytocin infused before the placenta is removed, especially at the time of cesarean delivery. Expressing the placenta at the time of cesarean delivery—as opposed to manual removal—is associated with lower blood loss and allows the uterus to begin contracting before the placenta is removed.—HAYWOOD L. BROWN, MD
8. When do you use the intrauterine balloon?
OBG Management: When is the intrauterine balloon a management option?
Dr. Brown: The balloon offers a way to actively manage hemorrhage and has been associated with decreasing morbidity and a reduced need for surgical intervention, including hysterectomy. It works through a tamponade effect. Once the balloon is inflated with 300 to 500 mL of saline, it compresses the uterine cavity until the uterus develops predelivery tone. It can be left in place as long as 24 hours, need be.
Several balloons are available for use, with the Bakri balloon being the prototype. The balloon may cut off uterine blood flow as a mechanism of action.
Before the advent of manufactured balloons, uterine tamponade was attempted using packing with gauze and a large-bore Foley catheter.
9. How do you proceed when surgery is necessary?
OBG Management: What surgical techniques—aside from hysterectomy—may be useful in stanching hemorrhage?
Dr. Brown: The first-line surgical approach after vaginal delivery is uterine exploration to evacuate uterine clots and check for retained placental fragments. This act alone may impart improved uterine contractility. If retained placental fragments are suspected, a gentle curettage of the uterine cavity, using a large curette, is appropriate.
When it is obvious that atony is the cause of the hemorrhage, and medical management has failed, these surgical steps are appropriate:
- Uterine artery ligation, using the “O’Leary” technique, can be performed bilaterally. The utero-ovarian vessels can also be ligated (but not cut!)
- B-Lynch suture as a technique to compress the uterus. This strategy uses outside, draping, absorbable suture to collapse the uterine cavity. It can be quite successful when combined with the use of uterotonics. One study reported more than 1,000 B-Lynch procedures, with only seven failures.1 Hemostatic multiple-square compression is a surgical technique that works according to a similar principle
- Hypogastric artery ligation can be performed by an experienced surgeon but is rarely employed in severe hemorrhage owing to the risk of complications and lengthy procedure time.
OBG Management: When does hysterectomy become an option?
Dr. Brown: Hysterectomy is the last defense against morbidity and maternal death from hemorrhage due to atony.
Clearly, when hysterectomy is performed, sooner is better than later, especially if uterine artery ligation and B-Lynch suture do not appear to be controlling the hemorrhage and the patient is hemodynamically unstable.
If the patient is a young woman with low parity, the uterus should be preserved, if at all possible, unless the hemorrhage cannot be controlled and the woman’s life is jeopardized.
When a uterine rupture has occurred, usually after a VBAC attempt, it may be prudent to proceed to hysterectomy, especially if the uterus appears to be difficult to repair.
10. When do you call for help?
OBG Management: When do you call in extra help?
Dr. Brown: As soon as hemorrhage occurs, the team should be assembled. It is critical that anesthesia be notified immediately, in the event that the patient requires surgical management. The blood bank should be notified that blood and blood products are likely to be required.
We designate a nursing leader to monitor the patient and another to keep the staff and unit on alert for potential surgical intervention. If uterine rupture or an invasive placental abnormality is suspected, we assemble the surgical team, including any potential consultant surgeon. We also notify the best available surgeons so that they can be ready to perform the necessary techniques. In addition, we notify the OR and surgical intensive care unit, in case they are needed.
OBG Management: How can obstetricians and obstetric units practice the response to OB hemorrhage so that, when a hemorrhage occurs, they are at the top of their game?
Dr. Brown: Obstetric units prepare by performing drills and simulations. These drills are now considered part of most units’ quality and safety programs.
Because obstetric hemorrhage can occur on any unit at any time, the team must be prepared to respond around the clock promptly and effectively to reduce the risk of morbidity and death.
After emergent surgical management of obstetric hemorrhage, the team should be assembled again to discuss what occurred and how they performed or could have performed more effectively as a team.
OBG Management: Should all obstetricians who perform repeat cesarean delivery be able to perform a cesarean hysterectomy in the event that uncontrollable hemorrhage is encountered?
Dr. Brown: It is an absolute must that any clinician who allows VBAC be capable of performing peripartum cesarean hysterectomy and know the indications for hysterectomy, as we have discussed. In fact, any obstetrician who performs cesarean delivery should be capable of performing a cesarean hysterectomy.
11. What do you recommend for practice?
OBG Management: How would you summarize the main points of management of postpartum hemorrhage?
Dr. Brown: I would suggest that the first step is organizing the team (obstetricians, nurses, anesthesiologist), followed by:
- resuscitation of the mother with oxygen and fluids through large-bore intravenous access sites
- notification of the blood bank (with typing and cross-matching) of the possible need for 4 to 6 U of blood for trans-fusion
- liberal assessment of laboratory values, especially coagulation status (International Normalized Ratio [INR], prothrombin time, and partial thromboplastin time) and blood counts (hemoglobin and hematocrit). Values may be lower if there has been significant blood loss and aggressive fluid resuscitation. Blood products such as fresh frozen plasma and cryoprecipitate are indicated, in addition to packed RBCs, if the patient has or is developing a coagulopathy. Also give platelets if the count is low. Once it becomes apparent that surgical intervention will be necessary, begin transfusion and replace clotting factors before beginning the procedure
- monitoring of vital signs and urine output throughout resuscitation and medical and surgical intervention
- elimination of the cause of bleeding as soon as possible by whatever means necessary to prevent maternal death, beginning with conservative medical management and, if necessary, followed by surgical intervention.
Tell us about a challenging case of postpartum hemorrhage and how you managed it.
Go to Send Us Your Letters. Please include your name, city, and state. We’ll publish intriguing “pearls” in an upcoming issue.
1. Allam MS, B-Lynch C. The B-Lynch and other uterine compression techniques. Int J Gynaecol Obstet. 2005;89(3):236-241.
2. Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev. 2000;(3):CD000007.-
- Activated factor VII proves to be a lifesaver in postpartum hemorrhage
Robert L. Barbieri, MD (February 2007) - Postpartum hemorrhage: Solutions to 2 intractable cases
Michael L. Stitely, MD, and Robert B. Gherman, MD (April 2007) - Give a uterotonic routinely during the third stage of labor
Robert L. Barbieri, MD (May 2007) - Consider retroperitoneal packing for postpartum hemorrhage
Maj. William R. Fulton, DO (July 2008) - You should add the Bakri balloon to your treatments for OB bleeds
Robert L. Barbieri, MD (February 2009) - Planning reduces the risk of maternal death. This tool helps.
Robert L. Barbieri, MD (August 2009) - What you can do to optimize blood conservation in ObGyn practice
Eric J. Bieber, MD, Linda Scott, RN, Corinna Muller, DO, Nancy Nuss, RN, and Edie L. Derian, MD (February 2010)
1. Allam MS, B-Lynch C. The B-Lynch and other uterine compression techniques. Int J Gynaecol Obstet. 2005;89(3):236-241.
2. Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev. 2000;(3):CD000007.-
- Activated factor VII proves to be a lifesaver in postpartum hemorrhage
Robert L. Barbieri, MD (February 2007) - Postpartum hemorrhage: Solutions to 2 intractable cases
Michael L. Stitely, MD, and Robert B. Gherman, MD (April 2007) - Give a uterotonic routinely during the third stage of labor
Robert L. Barbieri, MD (May 2007) - Consider retroperitoneal packing for postpartum hemorrhage
Maj. William R. Fulton, DO (July 2008) - You should add the Bakri balloon to your treatments for OB bleeds
Robert L. Barbieri, MD (February 2009) - Planning reduces the risk of maternal death. This tool helps.
Robert L. Barbieri, MD (August 2009) - What you can do to optimize blood conservation in ObGyn practice
Eric J. Bieber, MD, Linda Scott, RN, Corinna Muller, DO, Nancy Nuss, RN, and Edie L. Derian, MD (February 2010)
Cease the practice of early elective delivery, says March of Dimes
“39 weeks is the rule, provided delivery is truly elective”
“If you give magnesium sulfate for fetal neuroprotection, adhere to a protocol”
(Update on Obstetrics; January 2011)
John T. Repke, MD, and Jaimey M. Pauli, MD
“More strategies to avoid malpractice hazards on labor and delivery”
(Second of two parts; Focus on Professional Liability; January 2011)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD
Obstetricians and other providers of intrapartum care can improve birth outcomes significantly by eliminating the practice of elective delivery before 39 full weeks of gestation. That’s a key recommendation in a report issued by the March of Dimes at the end of 2010.1
In tandem with the report and accompanying formal recommendations for clinical care, the March of Dimes is expanding a quality improvement program to reduce unnecessary inductions and cesarean deliveries, noted Scott D. Berns, MD, MPH, at a presentation by the organization in New York on December 15. Dr. Berns is senior vice president for Chapter Programs of the March of Dimes and editor of the report, Toward Improving the Outcome of Pregnancy III (TIOP III). He is also clinical professor of pediatrics at the Warren Alpert Medical School at Brown University.
“It’s about babies being born at the right time for the right reasons,” Dr. Berns said.
Medical inductions are too common
A key focus of TIOP III is the need to curtail the practice of elective “term” delivery at 37 and 38 weeks of gestation. As the report notes, although “there are many valid medical and obstetric indications for delivery before 39 weeks of gestation, medical justification for a significant proportion of early deliveries is questionable.”1
Of particular concern is the use of medical induction of labor at 37 to 39 weeks without a legitimate indication—a practice that has increased dramatically over the past decade and that raises the rate of cesarean delivery, said Mark R. Chassin, MD, MPP, MPH, who spoke at the New York release of the report. Dr. Chassin is President of the Joint Commission.
Morbidity rises with early delivery
Early term delivery is widespread. As many as 30% of all births in the United States are performed electively (“without identifiable medical or obstetric indication”) before 39 weeks’ gestation, said Dr. Berns. This statistic includes elective induction of labor and elective primary and repeat cesarean delivery, he added.
The morbidity associated with these early births is significant:
- The rate of admission to a newborn intensive care unit (NICU) doubles in infants born electively at 38 to 39 weeks of gestation, compared with those delivered at or beyond 39 weeks
- “Infants born before 39 completed weeks of gestation also have a higher incidence of respiratory distress syndrome and infant death than those delivered later”1
- There is evidence that neonatal morbidity increases even after fetal lung maturity is confirmed when elective delivery takes place before 39 weeks.1
ACOG has also warned against early elective delivery.2
The March of Dimes Foundation offers a toolkit on its Web site for clinicians to use to reduce the rate of elective delivery before 39 full weeks of gestation. It’s available at http://www.marchofdimes.com/professionals/less-than-39-weeks-toolkit.aspx.
Other intrapartum actions can boost outcomes
Other recommendations for improving intrapartum care and pregnancy outcomes included in TIOP III:
- Introduce facility-based protocols and develop effective leadership to eliminate elective deliveries before 39 weeks’ gestation
- Use standardized, low-dose oxytocin protocols for induction and augmentation of labor. (According to TIOP III: “Oxtyocin is the drug most commonly associated with preventable adverse events during childbirth and is also the drug most frequently implicated in professional liability claims.”1
- Uniformly implement unambiguous protocols for monitoring oxytocin infusion
- Avoid “inappropriate” cesarean delivery and de-emphasize the cesarean delivery rate as a primary quality indicator
- Adopt protocols for administration of magnesium sulfate for fetal neuroprotection in preterm infants
- Enhance and support a team approach to obstetric emergencies, and promote clinician understanding of intermediate and abnormal fetal heart rate patterns
- Use available checklists to document maneuvers—including those avoided—in the management of shoulder dystocia
- Develop a “robust quality improvement program” for intrapartum care processes.1
“39 weeks is the rule, provided delivery is truly elective”
“If you give magnesium sulfate for fetal neuroprotection, adhere to a protocol”
(Update on Obstetrics; January 2011)
John T. Repke, MD, and Jaimey M. Pauli, MD
“More strategies to avoid malpractice hazards on labor and delivery”
(Second of two parts; Focus on Professional Liability; January 2011)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD
Obstetricians and other providers of intrapartum care can improve birth outcomes significantly by eliminating the practice of elective delivery before 39 full weeks of gestation. That’s a key recommendation in a report issued by the March of Dimes at the end of 2010.1
In tandem with the report and accompanying formal recommendations for clinical care, the March of Dimes is expanding a quality improvement program to reduce unnecessary inductions and cesarean deliveries, noted Scott D. Berns, MD, MPH, at a presentation by the organization in New York on December 15. Dr. Berns is senior vice president for Chapter Programs of the March of Dimes and editor of the report, Toward Improving the Outcome of Pregnancy III (TIOP III). He is also clinical professor of pediatrics at the Warren Alpert Medical School at Brown University.
“It’s about babies being born at the right time for the right reasons,” Dr. Berns said.
Medical inductions are too common
A key focus of TIOP III is the need to curtail the practice of elective “term” delivery at 37 and 38 weeks of gestation. As the report notes, although “there are many valid medical and obstetric indications for delivery before 39 weeks of gestation, medical justification for a significant proportion of early deliveries is questionable.”1
Of particular concern is the use of medical induction of labor at 37 to 39 weeks without a legitimate indication—a practice that has increased dramatically over the past decade and that raises the rate of cesarean delivery, said Mark R. Chassin, MD, MPP, MPH, who spoke at the New York release of the report. Dr. Chassin is President of the Joint Commission.
Morbidity rises with early delivery
Early term delivery is widespread. As many as 30% of all births in the United States are performed electively (“without identifiable medical or obstetric indication”) before 39 weeks’ gestation, said Dr. Berns. This statistic includes elective induction of labor and elective primary and repeat cesarean delivery, he added.
The morbidity associated with these early births is significant:
- The rate of admission to a newborn intensive care unit (NICU) doubles in infants born electively at 38 to 39 weeks of gestation, compared with those delivered at or beyond 39 weeks
- “Infants born before 39 completed weeks of gestation also have a higher incidence of respiratory distress syndrome and infant death than those delivered later”1
- There is evidence that neonatal morbidity increases even after fetal lung maturity is confirmed when elective delivery takes place before 39 weeks.1
ACOG has also warned against early elective delivery.2
The March of Dimes Foundation offers a toolkit on its Web site for clinicians to use to reduce the rate of elective delivery before 39 full weeks of gestation. It’s available at http://www.marchofdimes.com/professionals/less-than-39-weeks-toolkit.aspx.
Other intrapartum actions can boost outcomes
Other recommendations for improving intrapartum care and pregnancy outcomes included in TIOP III:
- Introduce facility-based protocols and develop effective leadership to eliminate elective deliveries before 39 weeks’ gestation
- Use standardized, low-dose oxytocin protocols for induction and augmentation of labor. (According to TIOP III: “Oxtyocin is the drug most commonly associated with preventable adverse events during childbirth and is also the drug most frequently implicated in professional liability claims.”1
- Uniformly implement unambiguous protocols for monitoring oxytocin infusion
- Avoid “inappropriate” cesarean delivery and de-emphasize the cesarean delivery rate as a primary quality indicator
- Adopt protocols for administration of magnesium sulfate for fetal neuroprotection in preterm infants
- Enhance and support a team approach to obstetric emergencies, and promote clinician understanding of intermediate and abnormal fetal heart rate patterns
- Use available checklists to document maneuvers—including those avoided—in the management of shoulder dystocia
- Develop a “robust quality improvement program” for intrapartum care processes.1
“39 weeks is the rule, provided delivery is truly elective”
“If you give magnesium sulfate for fetal neuroprotection, adhere to a protocol”
(Update on Obstetrics; January 2011)
John T. Repke, MD, and Jaimey M. Pauli, MD
“More strategies to avoid malpractice hazards on labor and delivery”
(Second of two parts; Focus on Professional Liability; January 2011)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD
Obstetricians and other providers of intrapartum care can improve birth outcomes significantly by eliminating the practice of elective delivery before 39 full weeks of gestation. That’s a key recommendation in a report issued by the March of Dimes at the end of 2010.1
In tandem with the report and accompanying formal recommendations for clinical care, the March of Dimes is expanding a quality improvement program to reduce unnecessary inductions and cesarean deliveries, noted Scott D. Berns, MD, MPH, at a presentation by the organization in New York on December 15. Dr. Berns is senior vice president for Chapter Programs of the March of Dimes and editor of the report, Toward Improving the Outcome of Pregnancy III (TIOP III). He is also clinical professor of pediatrics at the Warren Alpert Medical School at Brown University.
“It’s about babies being born at the right time for the right reasons,” Dr. Berns said.
Medical inductions are too common
A key focus of TIOP III is the need to curtail the practice of elective “term” delivery at 37 and 38 weeks of gestation. As the report notes, although “there are many valid medical and obstetric indications for delivery before 39 weeks of gestation, medical justification for a significant proportion of early deliveries is questionable.”1
Of particular concern is the use of medical induction of labor at 37 to 39 weeks without a legitimate indication—a practice that has increased dramatically over the past decade and that raises the rate of cesarean delivery, said Mark R. Chassin, MD, MPP, MPH, who spoke at the New York release of the report. Dr. Chassin is President of the Joint Commission.
Morbidity rises with early delivery
Early term delivery is widespread. As many as 30% of all births in the United States are performed electively (“without identifiable medical or obstetric indication”) before 39 weeks’ gestation, said Dr. Berns. This statistic includes elective induction of labor and elective primary and repeat cesarean delivery, he added.
The morbidity associated with these early births is significant:
- The rate of admission to a newborn intensive care unit (NICU) doubles in infants born electively at 38 to 39 weeks of gestation, compared with those delivered at or beyond 39 weeks
- “Infants born before 39 completed weeks of gestation also have a higher incidence of respiratory distress syndrome and infant death than those delivered later”1
- There is evidence that neonatal morbidity increases even after fetal lung maturity is confirmed when elective delivery takes place before 39 weeks.1
ACOG has also warned against early elective delivery.2
The March of Dimes Foundation offers a toolkit on its Web site for clinicians to use to reduce the rate of elective delivery before 39 full weeks of gestation. It’s available at http://www.marchofdimes.com/professionals/less-than-39-weeks-toolkit.aspx.
Other intrapartum actions can boost outcomes
Other recommendations for improving intrapartum care and pregnancy outcomes included in TIOP III:
- Introduce facility-based protocols and develop effective leadership to eliminate elective deliveries before 39 weeks’ gestation
- Use standardized, low-dose oxytocin protocols for induction and augmentation of labor. (According to TIOP III: “Oxtyocin is the drug most commonly associated with preventable adverse events during childbirth and is also the drug most frequently implicated in professional liability claims.”1
- Uniformly implement unambiguous protocols for monitoring oxytocin infusion
- Avoid “inappropriate” cesarean delivery and de-emphasize the cesarean delivery rate as a primary quality indicator
- Adopt protocols for administration of magnesium sulfate for fetal neuroprotection in preterm infants
- Enhance and support a team approach to obstetric emergencies, and promote clinician understanding of intermediate and abnormal fetal heart rate patterns
- Use available checklists to document maneuvers—including those avoided—in the management of shoulder dystocia
- Develop a “robust quality improvement program” for intrapartum care processes.1
Data Watch: Diabetes-Related Hospital Stays in Pregnancy on the Rise
Source Elsevier Global Medical News
Source Elsevier Global Medical News
Source Elsevier Global Medical News
Fish Oil Didn't Help Postpartum Depression
The use of DHA-rich fish oil supplements during pregnancy did not reduce the rate of postpartum depression in mothers or improve neurodevelopment in their children, according to a report.
“Current recommendations suggest that pregnant women increase their dietary DHA [docosahexaenoic acid] to improve their health outcomes as well as those of their children,” and the industry “successfully markets prenatal supplements with DHA to optimize brain function of mother and infant,” noted Maria Makrides, Ph.D., of Women's and Children's Hospital at Flinders Medical Centre in Adelaide, Australia, and her associates.
However, intervention trials with open-label designs, small sample sizes, high attrition rates, or poor statistical power have produced inconclusive results. Dr. Makrides and her colleagues performed the DOMINO (DHA to Optimize Mother Infant Outcome) trial to assess the efficacy and safety of DHA supplements.
In the double-blind trial, 2,320 women with singleton pregnancies who were attending five Australian perinatal centers were randomly assigned to take three fish oil capsules (1,197 women) or placebo capsules containing vegetable oil (1,202 women) daily. The fish oil capsules contained 800 mg/day of DHA and 100 mg/day of eicosapentaenoic acid. The study subjects were enrolled before they reached 21 weeks' gestation and took the supplements until delivery (JAMA 2010;304:1675-83).
The primary maternal outcome was a high level of depressive symptoms during the first 6 months post partum, as assessed by a score of more than 12 on the self-administered Edinburgh Postnatal Depression Scale. The incidence of that outcome was not significantly different between women who took fish oil capsules (9.7%) and the control subjects (11.2%).
In addition, the percentage of women who received a medical diagnosis of depression during the study did not differ significantly between the two groups.
The primary childhood outcome was neurodevelopment at age 18 months, as assessed by scores on the Cognitive and Language Composite Scales of the BSID-III (Bayley Scales of Infant and Toddler Development, third edition). Neither the mean cognitive scores nor the mean language scores differed significantly between children of mothers who took fish oil supplements and children of the control mothers. Similarly, scores on measures of motor development, social-emotional behavior, and adaptive behavior were not significantly different.
The women who took fish oil supplements had a lower rate of very preterm birth (1.1%) compared with the control group (2.3%). However, that was offset by their higher rate of postterm births requiring obstetric intervention (17.6% vs. 13.7%).
Adverse effects, including rates of hemorrhage and antenatal hospitalization, did not differ between the two study groups. The only adverse event that occurred more often in the DHA group than in the controls was eructation.
The Australian National Health and Medical Research Council funded the DOMINO study. Dr. Makrides reported serving on scientific advisory boards for Nestle, Fonterrra, and Nutricia.
DHA-rich fish oil supplements during pregnancy did not reduce the rate of postpartum depression or improve neurodevelopment in children.
Source ©Clayton Hansen/iStockphoto
View on the News
A Noteworthy Finding
One noteworthy finding of the DOMINO trial is that women who took fish oil supplements had a significantly lower risk of very preterm birth (defined as delivery before 34 weeks' gestation) than did women in the control group, said Dr. Emily Oken and Dr. Mandy B. Belfort.
The rate of very preterm birth was 1.1% with DHA-rich supplements (13 such births), compared with 2.3% with placebo (27 such births). The downstream benefits of that difference included lower rates of low birth weight, fewer admissions to the neonatal intensive care unit, and a nonsignificant 30% reduction in infant mortality.“
“Although the absolute numbers of these outcomes were small, the relative benefits were large,” they noted.
“For now, pregnant women should take care to get the recommended intake of 200 mg/day of DHA, either by including low-mercury, high-DHA fish in their diets or by taking a daily n-3 PUFA (polyunsaturated fatty acid) supplement. The benefit of higher intakes remains unclear,” Dr. Oken and Dr. Belfort concluded.
DR.OKEN is at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston. DR. BELFORT is at Children's Hospital Boston. Neither Dr. Oken nor Dr. Belfort reported any financial disclosures. The comments were taken from their editorial accompanying the report (JAMA 2010;304:1717-8).
The use of DHA-rich fish oil supplements during pregnancy did not reduce the rate of postpartum depression in mothers or improve neurodevelopment in their children, according to a report.
“Current recommendations suggest that pregnant women increase their dietary DHA [docosahexaenoic acid] to improve their health outcomes as well as those of their children,” and the industry “successfully markets prenatal supplements with DHA to optimize brain function of mother and infant,” noted Maria Makrides, Ph.D., of Women's and Children's Hospital at Flinders Medical Centre in Adelaide, Australia, and her associates.
However, intervention trials with open-label designs, small sample sizes, high attrition rates, or poor statistical power have produced inconclusive results. Dr. Makrides and her colleagues performed the DOMINO (DHA to Optimize Mother Infant Outcome) trial to assess the efficacy and safety of DHA supplements.
In the double-blind trial, 2,320 women with singleton pregnancies who were attending five Australian perinatal centers were randomly assigned to take three fish oil capsules (1,197 women) or placebo capsules containing vegetable oil (1,202 women) daily. The fish oil capsules contained 800 mg/day of DHA and 100 mg/day of eicosapentaenoic acid. The study subjects were enrolled before they reached 21 weeks' gestation and took the supplements until delivery (JAMA 2010;304:1675-83).
The primary maternal outcome was a high level of depressive symptoms during the first 6 months post partum, as assessed by a score of more than 12 on the self-administered Edinburgh Postnatal Depression Scale. The incidence of that outcome was not significantly different between women who took fish oil capsules (9.7%) and the control subjects (11.2%).
In addition, the percentage of women who received a medical diagnosis of depression during the study did not differ significantly between the two groups.
The primary childhood outcome was neurodevelopment at age 18 months, as assessed by scores on the Cognitive and Language Composite Scales of the BSID-III (Bayley Scales of Infant and Toddler Development, third edition). Neither the mean cognitive scores nor the mean language scores differed significantly between children of mothers who took fish oil supplements and children of the control mothers. Similarly, scores on measures of motor development, social-emotional behavior, and adaptive behavior were not significantly different.
The women who took fish oil supplements had a lower rate of very preterm birth (1.1%) compared with the control group (2.3%). However, that was offset by their higher rate of postterm births requiring obstetric intervention (17.6% vs. 13.7%).
Adverse effects, including rates of hemorrhage and antenatal hospitalization, did not differ between the two study groups. The only adverse event that occurred more often in the DHA group than in the controls was eructation.
The Australian National Health and Medical Research Council funded the DOMINO study. Dr. Makrides reported serving on scientific advisory boards for Nestle, Fonterrra, and Nutricia.
DHA-rich fish oil supplements during pregnancy did not reduce the rate of postpartum depression or improve neurodevelopment in children.
Source ©Clayton Hansen/iStockphoto
View on the News
A Noteworthy Finding
One noteworthy finding of the DOMINO trial is that women who took fish oil supplements had a significantly lower risk of very preterm birth (defined as delivery before 34 weeks' gestation) than did women in the control group, said Dr. Emily Oken and Dr. Mandy B. Belfort.
The rate of very preterm birth was 1.1% with DHA-rich supplements (13 such births), compared with 2.3% with placebo (27 such births). The downstream benefits of that difference included lower rates of low birth weight, fewer admissions to the neonatal intensive care unit, and a nonsignificant 30% reduction in infant mortality.“
“Although the absolute numbers of these outcomes were small, the relative benefits were large,” they noted.
“For now, pregnant women should take care to get the recommended intake of 200 mg/day of DHA, either by including low-mercury, high-DHA fish in their diets or by taking a daily n-3 PUFA (polyunsaturated fatty acid) supplement. The benefit of higher intakes remains unclear,” Dr. Oken and Dr. Belfort concluded.
DR.OKEN is at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston. DR. BELFORT is at Children's Hospital Boston. Neither Dr. Oken nor Dr. Belfort reported any financial disclosures. The comments were taken from their editorial accompanying the report (JAMA 2010;304:1717-8).
The use of DHA-rich fish oil supplements during pregnancy did not reduce the rate of postpartum depression in mothers or improve neurodevelopment in their children, according to a report.
“Current recommendations suggest that pregnant women increase their dietary DHA [docosahexaenoic acid] to improve their health outcomes as well as those of their children,” and the industry “successfully markets prenatal supplements with DHA to optimize brain function of mother and infant,” noted Maria Makrides, Ph.D., of Women's and Children's Hospital at Flinders Medical Centre in Adelaide, Australia, and her associates.
However, intervention trials with open-label designs, small sample sizes, high attrition rates, or poor statistical power have produced inconclusive results. Dr. Makrides and her colleagues performed the DOMINO (DHA to Optimize Mother Infant Outcome) trial to assess the efficacy and safety of DHA supplements.
In the double-blind trial, 2,320 women with singleton pregnancies who were attending five Australian perinatal centers were randomly assigned to take three fish oil capsules (1,197 women) or placebo capsules containing vegetable oil (1,202 women) daily. The fish oil capsules contained 800 mg/day of DHA and 100 mg/day of eicosapentaenoic acid. The study subjects were enrolled before they reached 21 weeks' gestation and took the supplements until delivery (JAMA 2010;304:1675-83).
The primary maternal outcome was a high level of depressive symptoms during the first 6 months post partum, as assessed by a score of more than 12 on the self-administered Edinburgh Postnatal Depression Scale. The incidence of that outcome was not significantly different between women who took fish oil capsules (9.7%) and the control subjects (11.2%).
In addition, the percentage of women who received a medical diagnosis of depression during the study did not differ significantly between the two groups.
The primary childhood outcome was neurodevelopment at age 18 months, as assessed by scores on the Cognitive and Language Composite Scales of the BSID-III (Bayley Scales of Infant and Toddler Development, third edition). Neither the mean cognitive scores nor the mean language scores differed significantly between children of mothers who took fish oil supplements and children of the control mothers. Similarly, scores on measures of motor development, social-emotional behavior, and adaptive behavior were not significantly different.
The women who took fish oil supplements had a lower rate of very preterm birth (1.1%) compared with the control group (2.3%). However, that was offset by their higher rate of postterm births requiring obstetric intervention (17.6% vs. 13.7%).
Adverse effects, including rates of hemorrhage and antenatal hospitalization, did not differ between the two study groups. The only adverse event that occurred more often in the DHA group than in the controls was eructation.
The Australian National Health and Medical Research Council funded the DOMINO study. Dr. Makrides reported serving on scientific advisory boards for Nestle, Fonterrra, and Nutricia.
DHA-rich fish oil supplements during pregnancy did not reduce the rate of postpartum depression or improve neurodevelopment in children.
Source ©Clayton Hansen/iStockphoto
View on the News
A Noteworthy Finding
One noteworthy finding of the DOMINO trial is that women who took fish oil supplements had a significantly lower risk of very preterm birth (defined as delivery before 34 weeks' gestation) than did women in the control group, said Dr. Emily Oken and Dr. Mandy B. Belfort.
The rate of very preterm birth was 1.1% with DHA-rich supplements (13 such births), compared with 2.3% with placebo (27 such births). The downstream benefits of that difference included lower rates of low birth weight, fewer admissions to the neonatal intensive care unit, and a nonsignificant 30% reduction in infant mortality.“
“Although the absolute numbers of these outcomes were small, the relative benefits were large,” they noted.
“For now, pregnant women should take care to get the recommended intake of 200 mg/day of DHA, either by including low-mercury, high-DHA fish in their diets or by taking a daily n-3 PUFA (polyunsaturated fatty acid) supplement. The benefit of higher intakes remains unclear,” Dr. Oken and Dr. Belfort concluded.
DR.OKEN is at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston. DR. BELFORT is at Children's Hospital Boston. Neither Dr. Oken nor Dr. Belfort reported any financial disclosures. The comments were taken from their editorial accompanying the report (JAMA 2010;304:1717-8).
From JAMA
Sound strategies to avoid malpractice hazards on labor and delivery
CASE: Is TOLAC feasible?
Your patient is a 33-year-old gravida 3, para 2002, with a previous cesarean delivery who was admitted to labor and delivery with premature ruptured membranes at term. She is not contracting. Fetal status is reassuring.
Her obstetric history is of one normal, spontaneous delivery followed by one cesarean delivery, both occurring at term.
She wants to know if she can safely undergo a trial of labor, or if she must have a repeat cesarean delivery. How should you counsel her?
At the start of any discussion about how to reduce your risk of being sued for malpractice because of your work as an obstetrician, in particular during labor and delivery, two distinct, underlying avenues of concern need to be addressed. Before moving on to discuss strategy, then, let’s consider what they are and how they arise: Allegation (perception). You are at risk of an allegation of malpractice (or of a perception of malpractice) because of an unexpected event or outcome for mother or baby. Allegation and perception can arise apart from any specific clinical action you undertook, or did not undertake. An example? Counseling about options for care that falls short of full understanding by the patient.
Allegation and perception are the subjects of this first installment of our two-part article on strategies for avoiding claims of malpractice in L & D that begin with the first prenatal visit.
Causation. Your actions—what you do in the course of providing prenatal care and delivering a baby—put you at risk of a charge of malpractice when you have provided medical care that 1) is inconsistent with current medical practice and thus 2) harmed the mother or newborn.
For a medical malpractice case to go forward, it must meet a well-defined paradigm that teases apart components of causation, beginning with your duty to the patient (TABLE 1).
TABLE 1 Signposts in the medical malpractice paradigm
| When the clinical issue at hand is … | … Then the legal term is … |
|---|---|
| A health-care professional’s obligation to provide care | “Duty” |
| A deviation in the care that was provided | “Standard of care” |
| An allegation that a breach in the standard of care resulted in injury | “Proximate cause” |
| An assertion or finding that an injury is “compensable” | “Damages” |
| Source: Yale New Haven Medical Center, 1997.5 | |
Allegation of malpractice arises from a range of sources, as we’ll discuss, but it is causation that reflects the actual, hands-on practice of medicine. We’ll examine strategies for avoiding charges of causation in the second part of this article.
(For now, we’ll just note that a recent excellent review of intrapartum interventions and their basis in evidence1 offers a model for evaluating a number of widely utilized practices in obstetrics. The goal, of course, is to minimize bad outcomes that follow from causation. Regrettably, that evidence-based approach is a limited one, because of a paucity of adequately controlled studies about OB practice.)
CASE: Continued
You consider your patient’s comment that she would like to avoid a repeat cesarean delivery, and advise her that she may safely attempt vaginal birth.
When spontaneous labor does not occur in 6 hours, oxytocin is administered. She dilates to 9 cm and begins to push spontaneously.
The fetal heart rate then drops to 70/min; fetal station, which had been +2, is now -1. A Stat cesarean delivery is performed. Uterine rupture with partial fetal expulsion is found. Apgar scores are 1, 3, and 5 at 1, 5, and 10 minutes.
Your patient requires a hysterectomy to control bleeding.
Some broad considerations for the physician arising from this CASE
- The counseling that you provide to a patient should be nondirective; it should include your opinion, however, about the best option available to her. Insert yourself into this hypothetical case, for discussion’s sake: Did you provide that important opinion to her?
- You must make certain that she clearly understands the risks and benefits of a procedure or other action, and the available alternatives. Did you undertake a check of her comprehension, given the anxiety and confusion of the moment?
- When an adverse outcome ensues—however unlikely it was to occur—it is necessary for you to review the circumstances with the patient as soon as clinically possible. Did you “debrief” and counsel her before and after the hysterectomy?
No more “perfect outcomes”: Our role changed, so did our risk
From the moment an OB patient enters triage, until her arrival home with her infant, this crucial period of her life is colored by concern, curiosity, myth, and fear.
Every woman anticipates the birth of a healthy infant. In an earlier era, the patient and her family relied on the sage advice of their physician to ensure this outcome. To an extent, physicians themselves reinforced this reliance, embracing the notion that they were, in fact, able to provide such a perfect outcome.
With advances that have been made in reproductive medicine, pregnancy has become more readily available to women with increasingly advanced disease; this has made labor and delivery more challenging to them and to their physicians. Realistically, our role as physicians is now better expressed as providing advice to help a woman achieve the best possible outcome, recognizing her individual clinical circumstances, instead of ensuring a perfect outcome.
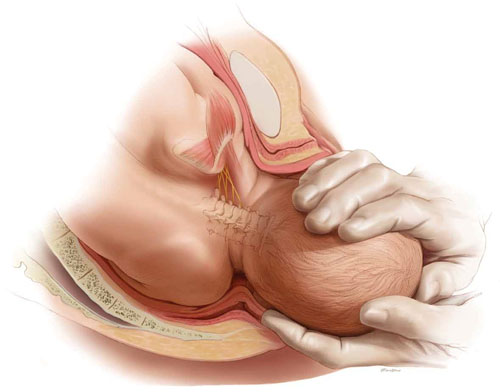
Every woman anticipates the birth of a healthy baby. But the role of the OB is better expressed as helping her achieve the best possible outcome, not a perfect outcome. ABOVE: Shoulder dystocia is one of the most treacherous and frightening—and litigated—complications of childbirth, yet it is, for the most part, unpredictable and unpreventable in the course of even routine delivery.
Key concept #1
COMMUNICATION
Communication is central to patients’ comprehension about the care that you provide to them. But to enter a genuine dialogue with a patient under your care, and with her family, can challenge your communication skills.
First, you need written and verbal skills. Second, you need to know how to read visual cues.
Third, the messages that you deliver to the patient are influenced by:
- your style of communication
- your cultural background
- the setting in which you’re providing care (office, hospital).
Where are such skills developed? For one, biopsychosocial models that are employed in medical student education and resident training aid the physician in developing appropriate communication skills.
But training alone cannot overcome the fact that communication is a double-sided activity: Patients bring many of their own variables to a dialogue. How patients understand and interact with you—and with other providers and the health-care system—is not, therefore, directly or strictly within your sphere of influence.
Yet your sensitivity to a patient’s issues can go a long way toward ameliorating her misconceptions and prejudices. Here are several suggestions, developed by others, to optimize patients’ understanding of their care2,3:
- Apply what’s known as flip default. Assume the patient does not understand the information that you’re providing. Ask her to repeat your instructions back to you (as is done with a verbal order in the hospital).
- Manage face-to-face time effectively. Don’t attempt to teach a patient everything about her care at once. Focus on the critical aspects of her case and on providing understanding; use a strategy of sequential learning.
- Reduce the “overwhelm” factor. Periodically, stop and ask the patient if she has questions. Don’t wait until the end of the appointment to do this.
- Eliminate jargon. When you notify a patient about the results of testing, for example, clarify what the results say about her health and mean for her care. Do so in plain language.
- Recognize her preconceptions. Discuss any psychosocial issues head on with the patient. Use an interpreter or a social worker, or counselors from other fields, as appropriate.
Remember: All health-care personnel need to understand the importance of making the patient comfortable in the often foreign, and sometimes sterile, milieu of the medical office and hospital.
Key concept #2
TRUST
Trust between patient and clinician is, we believe, the most basic necessity for ameliorating allegations of malpractice—secondary only, perhaps, to your knowledge of medicine.
Trust can be enhanced by interactions that demonstrate to both parties the advisability of working together to resolve a problem. Any aspect of the physician-patient interaction that is potentially adversarial does not serve the interests of either.
We encourage you to construct a communication bridge, so to speak, with your patient. Begin by:
- introducing yourself to her and explaining your role in her care
- making appropriate eye contact with her
- maintaining a positive attitude
- dressing appropriately
- making her feel that she is your No. 1 priority.
There is more.
Recognize the duality of respect
- Ask the patient how she wishes to be addressed
- Ask about her belief system
- Explain the specifics of her care without arrogance.
Engender trust
- Be honest with her
- Be on her side
- Take time with her
- Allow her the right that she has to select from the options or to refuse treatment
- Disclose to the patient your status as a student or resident, if that is your rank.
Recognize the benefits of partnership
Forging a partnership with the patient:
- improves the accuracy of information
- eases ongoing communication
- facilitates informed consent
- provides an opportunity for you to educate her.
TABLE 2 When building trust, both patient and physician
are charged with responsibilities
| In regard to … | The patient’s responsibility is to … | The physician’s responsibility is to … |
|---|---|---|
| Gathering an honest and complete medical history | Know and report | Question completely |
| Being adherent to prescribed care | Follow through | Make reasonable demands |
| Making decisions about care | Ask questions and actively participate in choices Make realistic requests | Be knowledgeable about available alternatives Individualize options |
Key concept #3
SHARED RESPONSIBILITY
Patient and physician both have responsibilities that are important to achieving an optimal outcome; so does the hospital (TABLE 2 and TABLE 3). Both patient and physician should practice full disclosure throughout the course of care; this will benefit both of you.4 Here are a few select examples.
TABLE 3 Relative degrees of responsibility for a good outcome
vary across interested parties, but none are exempt
| Area of emphasis | Hospital’s responsibility | Physician’s responsibility | Patient’s responsibility |
|---|---|---|---|
| Creating a positive environment for care | 3+ | 2+ | 1+ |
| Providing clear communication | 3+ | 3+ | 3+ |
| Obtaining informed consent | 3+ | 3+ | 3+ |
| Making reasonable requests | 1+ | 1+ | 3+ |
| Compliance | 3+ | 3+ | 3+ |
| Key to the relative scale: 1+: at the least, minimally responsible; 2+: at the least, somewhat responsible; 3+, responsible to the greatest degree. | |||
The importance of the intake form
At the outset of OB care, in most practices, the patient provides the initial detailed medical history by completing a form in the waiting room. In reviewing and completing this survey with her during the appointment, pay particular attention to those questions for which the response has been left blank.
Patients need to understand that key recommendations about their care, and a proper analysis of their concerns, are based on the information that they provide on this survey. In our practices, we find that patients answer most of these early questions without difficulty—even inquiries of a personal nature, such as the number of prior pregnancies, or drug, alcohol, and smoking habits—as long as they understand why it’s in their best interests for you to have this information. If they leave a question blank and you do not follow up verbally, you may have lost invaluable information that can affect the outcome of her pregnancy.
What should you do when, occasionally, a patient refuses to answer one of your questions? We recommend that you record her refusal on the form itself, where the note remains part of the record.
Keep in mind that all necessary and useful information about a patient may not be available, or may not be appropriate to consider, at the initial prenatal visit. In that case, you have an ongoing opportunity—at subsequent visits during the pregnancy—to develop her full medical profile and algorithm.
The necessity of adherence
It almost goes without saying: To provide the care that our patients need, we sometimes require the unpleasant of them—to undergo evaluations, or testing, or to take medications that may be inconvenient or costly.
After you explain the specific course of care to a patient—whether you’re ordering a test or writing a prescription—your follow-up must include notation in the record of adherence. The fact is that both of you share responsibility for having her understand the importance of adherence to your instructions and the consequences of limited adherence or nonadherence.
Recall one of the lessons from the case that introduced this article: For the patient to make an informed decision about her care, the clinician must have thorough knowledge of 1) the risks and benefits of whatever intervention is being proposed in the particular clinical scenario and 2) the available alternatives. It is key that you communicate your risk-benefit assessment accurately to the patient.
Follow-up
Sometimes, new medical problems arise during subsequent prenatal visits. Follow-up appointments also provide an opportunity for you to expand your attention to problems identified earlier. Regardless of what the patient reported about her history and current health at the initial prenatal visit, listen for her to bring new issues to light for resolution later in the pregnancy that will have an impact on L & D. Again, it goes without saying but needs to be said: The OB clinician needs to have whatever skills are necessary to 1) fully evaluate the progress of a pregnancy and 2) make recommendations for care in light of changes in the status of mother and fetus along the way.
TABLE 4 Examples of the cardinal rule of “Be specific”
when you document care
| Instead of noting … | … Use alternative wording |
|---|---|
| “Mild vaginal bleeding” | “Vaginal bleeding requiring two pads an hour” |
| “Gentle traction” | “The shoulders were rotated before assisting the patient’s expulsive efforts” |
| “Patient refuses…” [or “declines…”] | “Patient voiced the nature of the problem and the alternatives that i have explained to her” |
| “Expedited cesarean section” | “The time from decision to incision was 35 minutes” |
Basic principles of documentation
The medical record is the best witness to interactions between a physician and a patient. In the record, we’re required to write a “5-C” description of events—namely, one that is:
- correct
- comprehensive
- conscientious
- clear
- contemporaneous.
Avoid medical jargon in the record. Be careful not to use vague terminology or descriptions, such as “mild vaginal bleeding,” “gentle traction,” or “patient refuses and accepts the consequences.” Specificity is the key to accuracy with respect to documentation (TABLE 4).
Editor’s note: Part 2 of this article will appear in the January 2011 issue of OBG Management. The authors’ analysis of L & D malpractice claims moves to a discussion of causation—by way of 4 troubling cases.
You’ll find a rich, useful archive of expert analysis of your professional liability and malpractice risk, at www.obgmanagement.com
• 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
• After a patient’s unexpected death, First Aid for the emotionally wounded
Ronald A. Chez, MD, and Wayne Fortin, MS (April 2010)
• Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates, Senior Editor, with Lewis Laska, JD, PhD (October 2009)
• Can a change in practice patterns reduce the number of OB malpractice claims?
Jason K. Baxter, MD, MSCP, and Louis Weinstein, MD (April 2009)
• Strategies for breaking bad news to patients
Barry Bub, MD (September 2008)
• Stuff of nightmares: Criminal prosecution for malpractice
Gary Steinman, MD, PhD (August 2008)
• Deposition Dos and Don’ts: How to answer 8 tricky questions
James L. Knoll, IV, MD, and Phillip J. Resnick, MD (May 2008)
• Playing high-stakes poker: Do you fight—or settle—that malpractice lawsuit?
Jeffrey Segal, MD (April 2008)
We want to hear from you! Tell us what you think.
1. Berghella V, Baxter JK, Chauhan SP. Evidence-based labor and delivery management. Am J Obstet Gynecol. 2008;199(5):445-454.
2. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980-986.
3. Huvane K. Health literacy: reading is just the beginning. Focus on multicultural healthcare. 2007;3(4):16-19.
4. Giordano K. Legal Principles. In: O’Grady JP, Gimovsky ML, Bayer-Zwirello L, Giordano K, eds. Operative Obstetrics. 2nd ed. New York: Cambridge University Press; 2008.
5. The Four Elements of Medical Malpractice Yale New Haven Medical Center: Issues in Risk Management. 1997.
CASE: Is TOLAC feasible?
Your patient is a 33-year-old gravida 3, para 2002, with a previous cesarean delivery who was admitted to labor and delivery with premature ruptured membranes at term. She is not contracting. Fetal status is reassuring.
Her obstetric history is of one normal, spontaneous delivery followed by one cesarean delivery, both occurring at term.
She wants to know if she can safely undergo a trial of labor, or if she must have a repeat cesarean delivery. How should you counsel her?
At the start of any discussion about how to reduce your risk of being sued for malpractice because of your work as an obstetrician, in particular during labor and delivery, two distinct, underlying avenues of concern need to be addressed. Before moving on to discuss strategy, then, let’s consider what they are and how they arise: Allegation (perception). You are at risk of an allegation of malpractice (or of a perception of malpractice) because of an unexpected event or outcome for mother or baby. Allegation and perception can arise apart from any specific clinical action you undertook, or did not undertake. An example? Counseling about options for care that falls short of full understanding by the patient.
Allegation and perception are the subjects of this first installment of our two-part article on strategies for avoiding claims of malpractice in L & D that begin with the first prenatal visit.
Causation. Your actions—what you do in the course of providing prenatal care and delivering a baby—put you at risk of a charge of malpractice when you have provided medical care that 1) is inconsistent with current medical practice and thus 2) harmed the mother or newborn.
For a medical malpractice case to go forward, it must meet a well-defined paradigm that teases apart components of causation, beginning with your duty to the patient (TABLE 1).
TABLE 1 Signposts in the medical malpractice paradigm
| When the clinical issue at hand is … | … Then the legal term is … |
|---|---|
| A health-care professional’s obligation to provide care | “Duty” |
| A deviation in the care that was provided | “Standard of care” |
| An allegation that a breach in the standard of care resulted in injury | “Proximate cause” |
| An assertion or finding that an injury is “compensable” | “Damages” |
| Source: Yale New Haven Medical Center, 1997.5 | |
Allegation of malpractice arises from a range of sources, as we’ll discuss, but it is causation that reflects the actual, hands-on practice of medicine. We’ll examine strategies for avoiding charges of causation in the second part of this article.
(For now, we’ll just note that a recent excellent review of intrapartum interventions and their basis in evidence1 offers a model for evaluating a number of widely utilized practices in obstetrics. The goal, of course, is to minimize bad outcomes that follow from causation. Regrettably, that evidence-based approach is a limited one, because of a paucity of adequately controlled studies about OB practice.)
CASE: Continued
You consider your patient’s comment that she would like to avoid a repeat cesarean delivery, and advise her that she may safely attempt vaginal birth.
When spontaneous labor does not occur in 6 hours, oxytocin is administered. She dilates to 9 cm and begins to push spontaneously.
The fetal heart rate then drops to 70/min; fetal station, which had been +2, is now -1. A Stat cesarean delivery is performed. Uterine rupture with partial fetal expulsion is found. Apgar scores are 1, 3, and 5 at 1, 5, and 10 minutes.
Your patient requires a hysterectomy to control bleeding.
Some broad considerations for the physician arising from this CASE
- The counseling that you provide to a patient should be nondirective; it should include your opinion, however, about the best option available to her. Insert yourself into this hypothetical case, for discussion’s sake: Did you provide that important opinion to her?
- You must make certain that she clearly understands the risks and benefits of a procedure or other action, and the available alternatives. Did you undertake a check of her comprehension, given the anxiety and confusion of the moment?
- When an adverse outcome ensues—however unlikely it was to occur—it is necessary for you to review the circumstances with the patient as soon as clinically possible. Did you “debrief” and counsel her before and after the hysterectomy?
No more “perfect outcomes”: Our role changed, so did our risk
From the moment an OB patient enters triage, until her arrival home with her infant, this crucial period of her life is colored by concern, curiosity, myth, and fear.
Every woman anticipates the birth of a healthy infant. In an earlier era, the patient and her family relied on the sage advice of their physician to ensure this outcome. To an extent, physicians themselves reinforced this reliance, embracing the notion that they were, in fact, able to provide such a perfect outcome.
With advances that have been made in reproductive medicine, pregnancy has become more readily available to women with increasingly advanced disease; this has made labor and delivery more challenging to them and to their physicians. Realistically, our role as physicians is now better expressed as providing advice to help a woman achieve the best possible outcome, recognizing her individual clinical circumstances, instead of ensuring a perfect outcome.
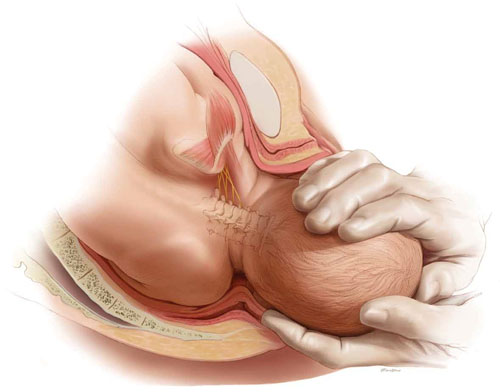
Every woman anticipates the birth of a healthy baby. But the role of the OB is better expressed as helping her achieve the best possible outcome, not a perfect outcome. ABOVE: Shoulder dystocia is one of the most treacherous and frightening—and litigated—complications of childbirth, yet it is, for the most part, unpredictable and unpreventable in the course of even routine delivery.
Key concept #1
COMMUNICATION
Communication is central to patients’ comprehension about the care that you provide to them. But to enter a genuine dialogue with a patient under your care, and with her family, can challenge your communication skills.
First, you need written and verbal skills. Second, you need to know how to read visual cues.
Third, the messages that you deliver to the patient are influenced by:
- your style of communication
- your cultural background
- the setting in which you’re providing care (office, hospital).
Where are such skills developed? For one, biopsychosocial models that are employed in medical student education and resident training aid the physician in developing appropriate communication skills.
But training alone cannot overcome the fact that communication is a double-sided activity: Patients bring many of their own variables to a dialogue. How patients understand and interact with you—and with other providers and the health-care system—is not, therefore, directly or strictly within your sphere of influence.
Yet your sensitivity to a patient’s issues can go a long way toward ameliorating her misconceptions and prejudices. Here are several suggestions, developed by others, to optimize patients’ understanding of their care2,3:
- Apply what’s known as flip default. Assume the patient does not understand the information that you’re providing. Ask her to repeat your instructions back to you (as is done with a verbal order in the hospital).
- Manage face-to-face time effectively. Don’t attempt to teach a patient everything about her care at once. Focus on the critical aspects of her case and on providing understanding; use a strategy of sequential learning.
- Reduce the “overwhelm” factor. Periodically, stop and ask the patient if she has questions. Don’t wait until the end of the appointment to do this.
- Eliminate jargon. When you notify a patient about the results of testing, for example, clarify what the results say about her health and mean for her care. Do so in plain language.
- Recognize her preconceptions. Discuss any psychosocial issues head on with the patient. Use an interpreter or a social worker, or counselors from other fields, as appropriate.
Remember: All health-care personnel need to understand the importance of making the patient comfortable in the often foreign, and sometimes sterile, milieu of the medical office and hospital.
Key concept #2
TRUST
Trust between patient and clinician is, we believe, the most basic necessity for ameliorating allegations of malpractice—secondary only, perhaps, to your knowledge of medicine.
Trust can be enhanced by interactions that demonstrate to both parties the advisability of working together to resolve a problem. Any aspect of the physician-patient interaction that is potentially adversarial does not serve the interests of either.
We encourage you to construct a communication bridge, so to speak, with your patient. Begin by:
- introducing yourself to her and explaining your role in her care
- making appropriate eye contact with her
- maintaining a positive attitude
- dressing appropriately
- making her feel that she is your No. 1 priority.
There is more.
Recognize the duality of respect
- Ask the patient how she wishes to be addressed
- Ask about her belief system
- Explain the specifics of her care without arrogance.
Engender trust
- Be honest with her
- Be on her side
- Take time with her
- Allow her the right that she has to select from the options or to refuse treatment
- Disclose to the patient your status as a student or resident, if that is your rank.
Recognize the benefits of partnership
Forging a partnership with the patient:
- improves the accuracy of information
- eases ongoing communication
- facilitates informed consent
- provides an opportunity for you to educate her.
TABLE 2 When building trust, both patient and physician
are charged with responsibilities
| In regard to … | The patient’s responsibility is to … | The physician’s responsibility is to … |
|---|---|---|
| Gathering an honest and complete medical history | Know and report | Question completely |
| Being adherent to prescribed care | Follow through | Make reasonable demands |
| Making decisions about care | Ask questions and actively participate in choices Make realistic requests | Be knowledgeable about available alternatives Individualize options |
Key concept #3
SHARED RESPONSIBILITY
Patient and physician both have responsibilities that are important to achieving an optimal outcome; so does the hospital (TABLE 2 and TABLE 3). Both patient and physician should practice full disclosure throughout the course of care; this will benefit both of you.4 Here are a few select examples.
TABLE 3 Relative degrees of responsibility for a good outcome
vary across interested parties, but none are exempt
| Area of emphasis | Hospital’s responsibility | Physician’s responsibility | Patient’s responsibility |
|---|---|---|---|
| Creating a positive environment for care | 3+ | 2+ | 1+ |
| Providing clear communication | 3+ | 3+ | 3+ |
| Obtaining informed consent | 3+ | 3+ | 3+ |
| Making reasonable requests | 1+ | 1+ | 3+ |
| Compliance | 3+ | 3+ | 3+ |
| Key to the relative scale: 1+: at the least, minimally responsible; 2+: at the least, somewhat responsible; 3+, responsible to the greatest degree. | |||
The importance of the intake form
At the outset of OB care, in most practices, the patient provides the initial detailed medical history by completing a form in the waiting room. In reviewing and completing this survey with her during the appointment, pay particular attention to those questions for which the response has been left blank.
Patients need to understand that key recommendations about their care, and a proper analysis of their concerns, are based on the information that they provide on this survey. In our practices, we find that patients answer most of these early questions without difficulty—even inquiries of a personal nature, such as the number of prior pregnancies, or drug, alcohol, and smoking habits—as long as they understand why it’s in their best interests for you to have this information. If they leave a question blank and you do not follow up verbally, you may have lost invaluable information that can affect the outcome of her pregnancy.
What should you do when, occasionally, a patient refuses to answer one of your questions? We recommend that you record her refusal on the form itself, where the note remains part of the record.
Keep in mind that all necessary and useful information about a patient may not be available, or may not be appropriate to consider, at the initial prenatal visit. In that case, you have an ongoing opportunity—at subsequent visits during the pregnancy—to develop her full medical profile and algorithm.
The necessity of adherence
It almost goes without saying: To provide the care that our patients need, we sometimes require the unpleasant of them—to undergo evaluations, or testing, or to take medications that may be inconvenient or costly.
After you explain the specific course of care to a patient—whether you’re ordering a test or writing a prescription—your follow-up must include notation in the record of adherence. The fact is that both of you share responsibility for having her understand the importance of adherence to your instructions and the consequences of limited adherence or nonadherence.
Recall one of the lessons from the case that introduced this article: For the patient to make an informed decision about her care, the clinician must have thorough knowledge of 1) the risks and benefits of whatever intervention is being proposed in the particular clinical scenario and 2) the available alternatives. It is key that you communicate your risk-benefit assessment accurately to the patient.
Follow-up
Sometimes, new medical problems arise during subsequent prenatal visits. Follow-up appointments also provide an opportunity for you to expand your attention to problems identified earlier. Regardless of what the patient reported about her history and current health at the initial prenatal visit, listen for her to bring new issues to light for resolution later in the pregnancy that will have an impact on L & D. Again, it goes without saying but needs to be said: The OB clinician needs to have whatever skills are necessary to 1) fully evaluate the progress of a pregnancy and 2) make recommendations for care in light of changes in the status of mother and fetus along the way.
TABLE 4 Examples of the cardinal rule of “Be specific”
when you document care
| Instead of noting … | … Use alternative wording |
|---|---|
| “Mild vaginal bleeding” | “Vaginal bleeding requiring two pads an hour” |
| “Gentle traction” | “The shoulders were rotated before assisting the patient’s expulsive efforts” |
| “Patient refuses…” [or “declines…”] | “Patient voiced the nature of the problem and the alternatives that i have explained to her” |
| “Expedited cesarean section” | “The time from decision to incision was 35 minutes” |
Basic principles of documentation
The medical record is the best witness to interactions between a physician and a patient. In the record, we’re required to write a “5-C” description of events—namely, one that is:
- correct
- comprehensive
- conscientious
- clear
- contemporaneous.
Avoid medical jargon in the record. Be careful not to use vague terminology or descriptions, such as “mild vaginal bleeding,” “gentle traction,” or “patient refuses and accepts the consequences.” Specificity is the key to accuracy with respect to documentation (TABLE 4).
Editor’s note: Part 2 of this article will appear in the January 2011 issue of OBG Management. The authors’ analysis of L & D malpractice claims moves to a discussion of causation—by way of 4 troubling cases.
You’ll find a rich, useful archive of expert analysis of your professional liability and malpractice risk, at www.obgmanagement.com
• 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
• After a patient’s unexpected death, First Aid for the emotionally wounded
Ronald A. Chez, MD, and Wayne Fortin, MS (April 2010)
• Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates, Senior Editor, with Lewis Laska, JD, PhD (October 2009)
• Can a change in practice patterns reduce the number of OB malpractice claims?
Jason K. Baxter, MD, MSCP, and Louis Weinstein, MD (April 2009)
• Strategies for breaking bad news to patients
Barry Bub, MD (September 2008)
• Stuff of nightmares: Criminal prosecution for malpractice
Gary Steinman, MD, PhD (August 2008)
• Deposition Dos and Don’ts: How to answer 8 tricky questions
James L. Knoll, IV, MD, and Phillip J. Resnick, MD (May 2008)
• Playing high-stakes poker: Do you fight—or settle—that malpractice lawsuit?
Jeffrey Segal, MD (April 2008)
We want to hear from you! Tell us what you think.
CASE: Is TOLAC feasible?
Your patient is a 33-year-old gravida 3, para 2002, with a previous cesarean delivery who was admitted to labor and delivery with premature ruptured membranes at term. She is not contracting. Fetal status is reassuring.
Her obstetric history is of one normal, spontaneous delivery followed by one cesarean delivery, both occurring at term.
She wants to know if she can safely undergo a trial of labor, or if she must have a repeat cesarean delivery. How should you counsel her?
At the start of any discussion about how to reduce your risk of being sued for malpractice because of your work as an obstetrician, in particular during labor and delivery, two distinct, underlying avenues of concern need to be addressed. Before moving on to discuss strategy, then, let’s consider what they are and how they arise: Allegation (perception). You are at risk of an allegation of malpractice (or of a perception of malpractice) because of an unexpected event or outcome for mother or baby. Allegation and perception can arise apart from any specific clinical action you undertook, or did not undertake. An example? Counseling about options for care that falls short of full understanding by the patient.
Allegation and perception are the subjects of this first installment of our two-part article on strategies for avoiding claims of malpractice in L & D that begin with the first prenatal visit.
Causation. Your actions—what you do in the course of providing prenatal care and delivering a baby—put you at risk of a charge of malpractice when you have provided medical care that 1) is inconsistent with current medical practice and thus 2) harmed the mother or newborn.
For a medical malpractice case to go forward, it must meet a well-defined paradigm that teases apart components of causation, beginning with your duty to the patient (TABLE 1).
TABLE 1 Signposts in the medical malpractice paradigm
| When the clinical issue at hand is … | … Then the legal term is … |
|---|---|
| A health-care professional’s obligation to provide care | “Duty” |
| A deviation in the care that was provided | “Standard of care” |
| An allegation that a breach in the standard of care resulted in injury | “Proximate cause” |
| An assertion or finding that an injury is “compensable” | “Damages” |
| Source: Yale New Haven Medical Center, 1997.5 | |
Allegation of malpractice arises from a range of sources, as we’ll discuss, but it is causation that reflects the actual, hands-on practice of medicine. We’ll examine strategies for avoiding charges of causation in the second part of this article.
(For now, we’ll just note that a recent excellent review of intrapartum interventions and their basis in evidence1 offers a model for evaluating a number of widely utilized practices in obstetrics. The goal, of course, is to minimize bad outcomes that follow from causation. Regrettably, that evidence-based approach is a limited one, because of a paucity of adequately controlled studies about OB practice.)
CASE: Continued
You consider your patient’s comment that she would like to avoid a repeat cesarean delivery, and advise her that she may safely attempt vaginal birth.
When spontaneous labor does not occur in 6 hours, oxytocin is administered. She dilates to 9 cm and begins to push spontaneously.
The fetal heart rate then drops to 70/min; fetal station, which had been +2, is now -1. A Stat cesarean delivery is performed. Uterine rupture with partial fetal expulsion is found. Apgar scores are 1, 3, and 5 at 1, 5, and 10 minutes.
Your patient requires a hysterectomy to control bleeding.
Some broad considerations for the physician arising from this CASE
- The counseling that you provide to a patient should be nondirective; it should include your opinion, however, about the best option available to her. Insert yourself into this hypothetical case, for discussion’s sake: Did you provide that important opinion to her?
- You must make certain that she clearly understands the risks and benefits of a procedure or other action, and the available alternatives. Did you undertake a check of her comprehension, given the anxiety and confusion of the moment?
- When an adverse outcome ensues—however unlikely it was to occur—it is necessary for you to review the circumstances with the patient as soon as clinically possible. Did you “debrief” and counsel her before and after the hysterectomy?
No more “perfect outcomes”: Our role changed, so did our risk
From the moment an OB patient enters triage, until her arrival home with her infant, this crucial period of her life is colored by concern, curiosity, myth, and fear.
Every woman anticipates the birth of a healthy infant. In an earlier era, the patient and her family relied on the sage advice of their physician to ensure this outcome. To an extent, physicians themselves reinforced this reliance, embracing the notion that they were, in fact, able to provide such a perfect outcome.
With advances that have been made in reproductive medicine, pregnancy has become more readily available to women with increasingly advanced disease; this has made labor and delivery more challenging to them and to their physicians. Realistically, our role as physicians is now better expressed as providing advice to help a woman achieve the best possible outcome, recognizing her individual clinical circumstances, instead of ensuring a perfect outcome.
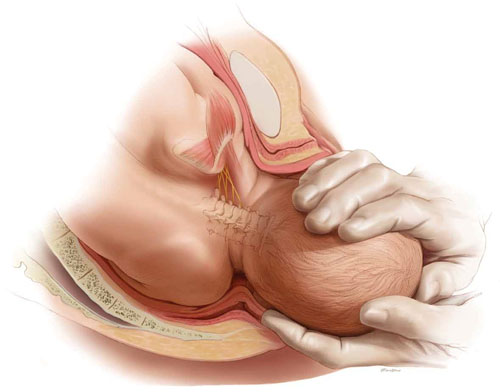
Every woman anticipates the birth of a healthy baby. But the role of the OB is better expressed as helping her achieve the best possible outcome, not a perfect outcome. ABOVE: Shoulder dystocia is one of the most treacherous and frightening—and litigated—complications of childbirth, yet it is, for the most part, unpredictable and unpreventable in the course of even routine delivery.
Key concept #1
COMMUNICATION
Communication is central to patients’ comprehension about the care that you provide to them. But to enter a genuine dialogue with a patient under your care, and with her family, can challenge your communication skills.
First, you need written and verbal skills. Second, you need to know how to read visual cues.
Third, the messages that you deliver to the patient are influenced by:
- your style of communication
- your cultural background
- the setting in which you’re providing care (office, hospital).
Where are such skills developed? For one, biopsychosocial models that are employed in medical student education and resident training aid the physician in developing appropriate communication skills.
But training alone cannot overcome the fact that communication is a double-sided activity: Patients bring many of their own variables to a dialogue. How patients understand and interact with you—and with other providers and the health-care system—is not, therefore, directly or strictly within your sphere of influence.
Yet your sensitivity to a patient’s issues can go a long way toward ameliorating her misconceptions and prejudices. Here are several suggestions, developed by others, to optimize patients’ understanding of their care2,3:
- Apply what’s known as flip default. Assume the patient does not understand the information that you’re providing. Ask her to repeat your instructions back to you (as is done with a verbal order in the hospital).
- Manage face-to-face time effectively. Don’t attempt to teach a patient everything about her care at once. Focus on the critical aspects of her case and on providing understanding; use a strategy of sequential learning.
- Reduce the “overwhelm” factor. Periodically, stop and ask the patient if she has questions. Don’t wait until the end of the appointment to do this.
- Eliminate jargon. When you notify a patient about the results of testing, for example, clarify what the results say about her health and mean for her care. Do so in plain language.
- Recognize her preconceptions. Discuss any psychosocial issues head on with the patient. Use an interpreter or a social worker, or counselors from other fields, as appropriate.
Remember: All health-care personnel need to understand the importance of making the patient comfortable in the often foreign, and sometimes sterile, milieu of the medical office and hospital.
Key concept #2
TRUST
Trust between patient and clinician is, we believe, the most basic necessity for ameliorating allegations of malpractice—secondary only, perhaps, to your knowledge of medicine.
Trust can be enhanced by interactions that demonstrate to both parties the advisability of working together to resolve a problem. Any aspect of the physician-patient interaction that is potentially adversarial does not serve the interests of either.
We encourage you to construct a communication bridge, so to speak, with your patient. Begin by:
- introducing yourself to her and explaining your role in her care
- making appropriate eye contact with her
- maintaining a positive attitude
- dressing appropriately
- making her feel that she is your No. 1 priority.
There is more.
Recognize the duality of respect
- Ask the patient how she wishes to be addressed
- Ask about her belief system
- Explain the specifics of her care without arrogance.
Engender trust
- Be honest with her
- Be on her side
- Take time with her
- Allow her the right that she has to select from the options or to refuse treatment
- Disclose to the patient your status as a student or resident, if that is your rank.
Recognize the benefits of partnership
Forging a partnership with the patient:
- improves the accuracy of information
- eases ongoing communication
- facilitates informed consent
- provides an opportunity for you to educate her.
TABLE 2 When building trust, both patient and physician
are charged with responsibilities
| In regard to … | The patient’s responsibility is to … | The physician’s responsibility is to … |
|---|---|---|
| Gathering an honest and complete medical history | Know and report | Question completely |
| Being adherent to prescribed care | Follow through | Make reasonable demands |
| Making decisions about care | Ask questions and actively participate in choices Make realistic requests | Be knowledgeable about available alternatives Individualize options |
Key concept #3
SHARED RESPONSIBILITY
Patient and physician both have responsibilities that are important to achieving an optimal outcome; so does the hospital (TABLE 2 and TABLE 3). Both patient and physician should practice full disclosure throughout the course of care; this will benefit both of you.4 Here are a few select examples.
TABLE 3 Relative degrees of responsibility for a good outcome
vary across interested parties, but none are exempt
| Area of emphasis | Hospital’s responsibility | Physician’s responsibility | Patient’s responsibility |
|---|---|---|---|
| Creating a positive environment for care | 3+ | 2+ | 1+ |
| Providing clear communication | 3+ | 3+ | 3+ |
| Obtaining informed consent | 3+ | 3+ | 3+ |
| Making reasonable requests | 1+ | 1+ | 3+ |
| Compliance | 3+ | 3+ | 3+ |
| Key to the relative scale: 1+: at the least, minimally responsible; 2+: at the least, somewhat responsible; 3+, responsible to the greatest degree. | |||
The importance of the intake form
At the outset of OB care, in most practices, the patient provides the initial detailed medical history by completing a form in the waiting room. In reviewing and completing this survey with her during the appointment, pay particular attention to those questions for which the response has been left blank.
Patients need to understand that key recommendations about their care, and a proper analysis of their concerns, are based on the information that they provide on this survey. In our practices, we find that patients answer most of these early questions without difficulty—even inquiries of a personal nature, such as the number of prior pregnancies, or drug, alcohol, and smoking habits—as long as they understand why it’s in their best interests for you to have this information. If they leave a question blank and you do not follow up verbally, you may have lost invaluable information that can affect the outcome of her pregnancy.
What should you do when, occasionally, a patient refuses to answer one of your questions? We recommend that you record her refusal on the form itself, where the note remains part of the record.
Keep in mind that all necessary and useful information about a patient may not be available, or may not be appropriate to consider, at the initial prenatal visit. In that case, you have an ongoing opportunity—at subsequent visits during the pregnancy—to develop her full medical profile and algorithm.
The necessity of adherence
It almost goes without saying: To provide the care that our patients need, we sometimes require the unpleasant of them—to undergo evaluations, or testing, or to take medications that may be inconvenient or costly.
After you explain the specific course of care to a patient—whether you’re ordering a test or writing a prescription—your follow-up must include notation in the record of adherence. The fact is that both of you share responsibility for having her understand the importance of adherence to your instructions and the consequences of limited adherence or nonadherence.
Recall one of the lessons from the case that introduced this article: For the patient to make an informed decision about her care, the clinician must have thorough knowledge of 1) the risks and benefits of whatever intervention is being proposed in the particular clinical scenario and 2) the available alternatives. It is key that you communicate your risk-benefit assessment accurately to the patient.
Follow-up
Sometimes, new medical problems arise during subsequent prenatal visits. Follow-up appointments also provide an opportunity for you to expand your attention to problems identified earlier. Regardless of what the patient reported about her history and current health at the initial prenatal visit, listen for her to bring new issues to light for resolution later in the pregnancy that will have an impact on L & D. Again, it goes without saying but needs to be said: The OB clinician needs to have whatever skills are necessary to 1) fully evaluate the progress of a pregnancy and 2) make recommendations for care in light of changes in the status of mother and fetus along the way.
TABLE 4 Examples of the cardinal rule of “Be specific”
when you document care
| Instead of noting … | … Use alternative wording |
|---|---|
| “Mild vaginal bleeding” | “Vaginal bleeding requiring two pads an hour” |
| “Gentle traction” | “The shoulders were rotated before assisting the patient’s expulsive efforts” |
| “Patient refuses…” [or “declines…”] | “Patient voiced the nature of the problem and the alternatives that i have explained to her” |
| “Expedited cesarean section” | “The time from decision to incision was 35 minutes” |
Basic principles of documentation
The medical record is the best witness to interactions between a physician and a patient. In the record, we’re required to write a “5-C” description of events—namely, one that is:
- correct
- comprehensive
- conscientious
- clear
- contemporaneous.
Avoid medical jargon in the record. Be careful not to use vague terminology or descriptions, such as “mild vaginal bleeding,” “gentle traction,” or “patient refuses and accepts the consequences.” Specificity is the key to accuracy with respect to documentation (TABLE 4).
Editor’s note: Part 2 of this article will appear in the January 2011 issue of OBG Management. The authors’ analysis of L & D malpractice claims moves to a discussion of causation—by way of 4 troubling cases.
You’ll find a rich, useful archive of expert analysis of your professional liability and malpractice risk, at www.obgmanagement.com
• 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
• After a patient’s unexpected death, First Aid for the emotionally wounded
Ronald A. Chez, MD, and Wayne Fortin, MS (April 2010)
• Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates, Senior Editor, with Lewis Laska, JD, PhD (October 2009)
• Can a change in practice patterns reduce the number of OB malpractice claims?
Jason K. Baxter, MD, MSCP, and Louis Weinstein, MD (April 2009)
• Strategies for breaking bad news to patients
Barry Bub, MD (September 2008)
• Stuff of nightmares: Criminal prosecution for malpractice
Gary Steinman, MD, PhD (August 2008)
• Deposition Dos and Don’ts: How to answer 8 tricky questions
James L. Knoll, IV, MD, and Phillip J. Resnick, MD (May 2008)
• Playing high-stakes poker: Do you fight—or settle—that malpractice lawsuit?
Jeffrey Segal, MD (April 2008)
We want to hear from you! Tell us what you think.
1. Berghella V, Baxter JK, Chauhan SP. Evidence-based labor and delivery management. Am J Obstet Gynecol. 2008;199(5):445-454.
2. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980-986.
3. Huvane K. Health literacy: reading is just the beginning. Focus on multicultural healthcare. 2007;3(4):16-19.
4. Giordano K. Legal Principles. In: O’Grady JP, Gimovsky ML, Bayer-Zwirello L, Giordano K, eds. Operative Obstetrics. 2nd ed. New York: Cambridge University Press; 2008.
5. The Four Elements of Medical Malpractice Yale New Haven Medical Center: Issues in Risk Management. 1997.
1. Berghella V, Baxter JK, Chauhan SP. Evidence-based labor and delivery management. Am J Obstet Gynecol. 2008;199(5):445-454.
2. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980-986.
3. Huvane K. Health literacy: reading is just the beginning. Focus on multicultural healthcare. 2007;3(4):16-19.
4. Giordano K. Legal Principles. In: O’Grady JP, Gimovsky ML, Bayer-Zwirello L, Giordano K, eds. Operative Obstetrics. 2nd ed. New York: Cambridge University Press; 2008.
5. The Four Elements of Medical Malpractice Yale New Haven Medical Center: Issues in Risk Management. 1997.
