User login
Revision Anterior Cruciate Ligament Reconstruction With Bone–Patellar Tendon–Bone Allograft and Extra-Articular Iliotibial Band Tenodesis
Primary anterior cruciate ligament (ACL) reconstruction has satisfactory outcomes in 75% to 97% of patients.1-3 Despite this high success rate, the number of revision ACL reconstructions has risen4 and is likely underreported.5 Recurrent instability occurs if the reconstructed ligament fails to provide adequate anterior and rotational knee stability. Causes of graft failure include repeat trauma, early return to high-demand activity, poor operative technique (including poor graft placement), failure to address concomitant pathology, and perioperative complications (eg, infection, stiffness).4 In addition, most patients who have revision ACL reconstruction received autograft tissue in the initial surgery, and allograft is thus not uncommon in revision ACL surgery. Allograft tissue has longer incorporation times6 and increased incidence of recurrent postoperative instability when compared with autograft tissue.7 Extra-articular tenodesis may thus be used to provide additional stability to the revision allograft tissue while it incorporates.
In this article, we describe our use of an extra-articular iliotibial band (ITB) tenodesis as an augmentative procedure in patients undergoing revision ACL reconstruction with bone–patellar tendon–bone (BPTB) allograft.
Surgical Technique
After induction of anesthesia and careful positioning, the patient is prepared and draped in the usual sterile fashion. Standard anteromedial, anterolateral, and superolateral outflow portals are established, and diagnostic arthroscopy is performed to inspect the cruciate ligaments, menisci, and articular cartilage (Figure 1). Peripheral meniscal tears should be repaired (Figure 2), and central or inner tears should be débrided to a stable rim. If meniscal repair is performed, sutures should be tied at the end of the case. Unstable articular cartilage defects should also be débrided. An 8- to 12-cm lateral hockey-stick incision is then made from the Gerdy tubercle to the inferior edge of the lateral femoral epicondyle in preparation for the ITB tenodesis (Figure 1). The lateral collateral ligament (LCL), the lateral head of the gastrocnemius, and the ITB are identified. The peroneal nerve should be significantly distal to the working field.
Remnants of the previous ACL graft are débrided, and, if necessary, a modified notchplasty is performed. A position for the new femoral tunnel is located and is confirmed with intraoperative fluoroscopy. This tunnel is established with compaction drill bits and dilated to the appropriate diameter through the anteromedial portal with the knee in 120° of flexion.
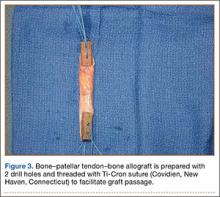
BPTB allograft is prepared first by cutting its central third to the desired diameter (Figure 3). The bone-plug ends are prepared with compaction pliers. Two 2.0-mm drill holes are made in each of the allograft bone plugs, and a No. 5 Ti-Cron suture (Covidien, New Haven, Connecticut) is placed through each of the holes. We typically use 2 sutures on each bone plug.
A tibial tunnel is then established with an ACL drill guide under arthroscopic visualization and intraoperative fluoroscopy for confirmation of correct pin placement. We use Kirschner wires (with parallel pin guides as needed), compaction drills, and dilators to create a well-positioned tunnel of the appropriate diameter. The allograft is then passed through the tibia and femur in retrograde fashion. We secure the femoral side with an AO (Arbeitsgemeinschaft für Osteosynthesefragen) 4.5-mm bicortical screw and washer. Our tibial fixation is secured after the ITB tenodesis. The knee is then cycled a dozen times.
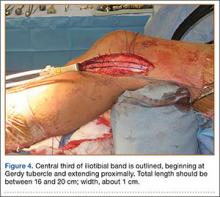
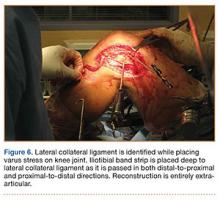
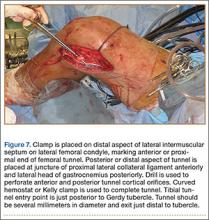
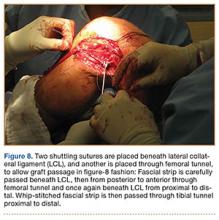
In preparation for the ITB tenodesis, we lengthen our previously made incision by about 4 cm proximally along the posterior aspect of the ITB. The central portion of the ITB is then outlined at the Gerdy tubercle and split with a No. 10 blade. This generally leaves an approximately 12- to 14-mm strip of ITB centrally (Figure 4). This portion should be gently lifted from the underlying tissue attachments distally at the insertion on the Gerdy tubercle. The interval between the LCL and lateral capsule of the knee is identified, and a No. 2 Ti-Cron whip-stitch is thrown through the free end of the ITB graft (Figure 5). The anterior aspect of the femoral tunnel is at the distal aspect of the lateral femoral condyle, and the posterior aspect is at the juncture of the proximal LCL and the lateral head of the gastrocnemius. The cortices of these landmarks should be perforated with a drill, and a curved instrument should be used to create a bone tunnel at this location (Figure 6). The tibial tunnel is just posterior and distal to the Gerdy tubercle and should be created in similar fashion. The graft is then passed underneath the LCL (Figure 7), through the proximal tunnel that has been created on the lateral femoral condyle, and then back down through the LCL and back onto itself after exiting the tibial tunnel (Figure 8). With the knee at 30° of flexion, the ITB graft is tensioned and sutured down to intact ITB fascia just proximal to the tibial tunnel orifice (Figure 9). We check knee range of motion (ROM) and then perform a Lachman test to assess changes in knee stability. The pivot shift examination is omitted to avoid placing excessive stress on the tenodesis. The tibial side of the patellar tendon allograft is then tensioned and secured over an AO 4.5-mm bicortical screw with washer with the knee in full extension. The screw is then tightened at 30° of knee flexion.
The ITB fascia is closed to the lateral femoral epicondyle with a running heavy suture, and all incisions are then irrigated and closed (Figures 10, 11). Standard sterile surgical dressing, Cryo/Cuff (Aircast, Vista, California), and brace are applied with the knee locked at 20°. Patients are generally discharged home the same day and followed up in clinic 1 week after surgery.
Complications
The peroneal nerve must be identified and protected during the open lateral procedure. In addition, the need for the extra lateral incision poses a slightly higher risk for infection compared with the traditional arthroscopic revision ACL procedure. Last, the additional tunnels required for the tenodesis can increase the theoretical potential for distal femur fracture and ACL graft fixation failure on the femoral side.
Postoperative Management
The operative knee is kept in extension in a brace locked at 20° for week 1 after surgery. Isometric quadriceps exercises are started immediately after surgery. Flexion to 90° is allowed starting week 2 after surgery, when the patient begins supervised active/passive flexion and progressive ROM exercises. In most cases, full ROM should be achieved by 6 to 8 weeks after surgery. Patients are progressed in their weight-bearing status by about 25% of their body weight per week, and use of crutches should be discontinued by week 4 after surgery. The brace should be discontinued by week 6 after surgery, when use of stationary bicycle and closed chain exercises begin. The patient may begin jogging when the operative leg regains 80% of contralateral quadriceps strength via Cybex strength testing. Functional drills begin in month 6, but patients should be counseled against returning to sport any earlier than 9 months after surgery.
Discussion
Achieving a successful outcome in revision ACL surgery (vs primary ACL surgery) is a significant challenge. Any of numerous factors can make the revision surgery more challenging, including existing poorly placed tunnels, tunnel expansion, lack of ideal graft choice, loss of secondary stabilizers, and deviations of the weight-bearing axis. Therefore, outcomes of revision surgery tend to be more moderate than outcomes of primary procedures.4,8-12
Revision ACL reconstruction techniques are varied and can involve use of autograft or allograft tissue as well as extra-articular augmentation techniques. Diamantopoulos and colleagues8 reported the outcomes of revision ACL reconstruction using bone–tendon–bone, hamstring, or quadriceps autografts in 107 patients. The majority of patients had improved outcome measures (mean Lysholm score improved from 51.5 to 88.5) and side-to-side laxity measurements. However, only 36.4% returned to preinjury activity level. Similarly, Noyes and Barber-Westin9 reported the outcomes of revision ACL reconstruction using quadriceps tendon–patellar bone autograft in 21 patients. Although there was significant improvement in terms of symptoms and activity level, 4 of the 21 knees were graded abnormal or severely abnormal on the IKDC (International Knee Documentation Committee) ligament rating. In a systematic review, pooled results of revision ACL reconstructions reiterated the above results.10 Eight hundred sixty-three patients from 21 studies were included in the analysis, which found significantly worse subjective outcomes than for primary procedures and a dramatically higher failure rate for the re-reconstructed ACL.
Several authors have directly compared primary cohorts with revision cohorts. Ahn and colleagues11 compared the outcomes of 59 revision ACL reconstructions with those of 117 primary reconstructions at a single institution. Although statistical comparison of stability between primary and revision ACL reconstructions showed no difference, revision reconstructions fared more poorly in terms of quality of life and return to activity compared with primary reconstructions. In a large cohort study of the Danish registry, revisions were found to have worse subjective outcomes than primary reconstructions as well.12 The study also found that the rerupture risk was significantly higher (relative risk, 2.05) when allograft was used.
Given the inferior results of revision surgery, our technique is recommended to augment the stability of reconstructed knees in the setting of revision ACL reconstruction. Adding the extra-articular procedure may augment the revised graft and protect it from excessive stress.13 A cadaver study compared double-bundle ACL reconstruction with single-bundle hamstring reconstruction plus extra-articular lateral tenodesis and found improved internal rotation control at 30° of flexion in the latter.14 Using contralateral 4-strand hamstring autograft in combination with an extra-articular lateral augment can have encouraging outcomes. Ferretti and colleagues15 reported an average Lysholm score of 95 in 12 patients who underwent this revision procedure and good anterior-to-posterior stability in 11 of the 12 patients. Trojani and colleagues16 reported on a cohort of 163 patients who underwent ACL revision surgery over a 10-year period. The authors found that 80% of patients with a lateral extra-articular tenodesis performed to augment their revision reconstruction had a negative pivot shift at long-term follow-up—versus only 63% of patients who underwent isolated revision ACL reconstruction. This finding was statistically significant, but the authors did not find any differences in IKDC scores between groups. These results support the initial biomechanical findings of Engebretsen and colleagues,17 who found that adding a lateral tenodesis decreased the forces on the reconstructed graft by 15%.
Conclusion
This technique allows for protection of the intra-articular allograft ligament reconstruction with improved rotational control that may potentially allow for improved subjective outcomes and protect against graft failure. Given the common pitfalls with stability in revision ACL surgery with allograft, this lateral extra-articular procedure can be an important structural augmentation in this challenging clinical issue in knee surgery.
1. Bach BR Jr. Revision anterior cruciate ligament surgery. Arthroscopy. 2003;19(suppl 1):14-29.
2. Baer GS, Harner CD. Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26(4):661-681.
3. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior cruciate ligament reconstruction autograft choice: bone–tendon–bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986-1995.
4. Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):199-217.
5. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6):622-627.
6. Jackson DW, Grood ES, Goldstein JD, et al. A comparison of patellar tendon autograft and allograft used for anterior cruciate ligament reconstruction in the goat model. Am J Sports Med. 1993;21(2):176-185.
7. Mascarenhas R, Tranovich M, Karpie JC, Irrgang JJ, Fu FH, Harner CD. Patellar tendon anterior cruciate ligament reconstruction in the high-demand patient: evaluation of autograft versus allograft reconstruction. Arthroscopy. 2010;26(9 Suppl):S58-S66.
8. Diamantopoulos AP, Lorbach O, Paessler HH. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36(5):851-860.
9. Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon–patellar bone autograft. Am J Sports Med. 2006;34(4):553-564.
10. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531-536.
11. Ahn JH, Lee YS, Ha HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med. 2008;36(10):1889-1895.
12. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551-1557.
13. Ferretti A, Conteduca F, Monaco E, De Carli A, D’Arrigo C. Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am. 2006;88(11):2373-2379.
14. Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1168-1174.
15. Ferretti A, Monaco E, Caperna L, Palma T, Conteduca F. Revision ACL reconstruction using contralateral hamstrings. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):690-695.
16. Trojani C, Beaufils P, Burdin G, et al. Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1565-1570.
17. Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169-176.
Primary anterior cruciate ligament (ACL) reconstruction has satisfactory outcomes in 75% to 97% of patients.1-3 Despite this high success rate, the number of revision ACL reconstructions has risen4 and is likely underreported.5 Recurrent instability occurs if the reconstructed ligament fails to provide adequate anterior and rotational knee stability. Causes of graft failure include repeat trauma, early return to high-demand activity, poor operative technique (including poor graft placement), failure to address concomitant pathology, and perioperative complications (eg, infection, stiffness).4 In addition, most patients who have revision ACL reconstruction received autograft tissue in the initial surgery, and allograft is thus not uncommon in revision ACL surgery. Allograft tissue has longer incorporation times6 and increased incidence of recurrent postoperative instability when compared with autograft tissue.7 Extra-articular tenodesis may thus be used to provide additional stability to the revision allograft tissue while it incorporates.
In this article, we describe our use of an extra-articular iliotibial band (ITB) tenodesis as an augmentative procedure in patients undergoing revision ACL reconstruction with bone–patellar tendon–bone (BPTB) allograft.
Surgical Technique
After induction of anesthesia and careful positioning, the patient is prepared and draped in the usual sterile fashion. Standard anteromedial, anterolateral, and superolateral outflow portals are established, and diagnostic arthroscopy is performed to inspect the cruciate ligaments, menisci, and articular cartilage (Figure 1). Peripheral meniscal tears should be repaired (Figure 2), and central or inner tears should be débrided to a stable rim. If meniscal repair is performed, sutures should be tied at the end of the case. Unstable articular cartilage defects should also be débrided. An 8- to 12-cm lateral hockey-stick incision is then made from the Gerdy tubercle to the inferior edge of the lateral femoral epicondyle in preparation for the ITB tenodesis (Figure 1). The lateral collateral ligament (LCL), the lateral head of the gastrocnemius, and the ITB are identified. The peroneal nerve should be significantly distal to the working field.
Remnants of the previous ACL graft are débrided, and, if necessary, a modified notchplasty is performed. A position for the new femoral tunnel is located and is confirmed with intraoperative fluoroscopy. This tunnel is established with compaction drill bits and dilated to the appropriate diameter through the anteromedial portal with the knee in 120° of flexion.
BPTB allograft is prepared first by cutting its central third to the desired diameter (Figure 3). The bone-plug ends are prepared with compaction pliers. Two 2.0-mm drill holes are made in each of the allograft bone plugs, and a No. 5 Ti-Cron suture (Covidien, New Haven, Connecticut) is placed through each of the holes. We typically use 2 sutures on each bone plug.
A tibial tunnel is then established with an ACL drill guide under arthroscopic visualization and intraoperative fluoroscopy for confirmation of correct pin placement. We use Kirschner wires (with parallel pin guides as needed), compaction drills, and dilators to create a well-positioned tunnel of the appropriate diameter. The allograft is then passed through the tibia and femur in retrograde fashion. We secure the femoral side with an AO (Arbeitsgemeinschaft für Osteosynthesefragen) 4.5-mm bicortical screw and washer. Our tibial fixation is secured after the ITB tenodesis. The knee is then cycled a dozen times.
In preparation for the ITB tenodesis, we lengthen our previously made incision by about 4 cm proximally along the posterior aspect of the ITB. The central portion of the ITB is then outlined at the Gerdy tubercle and split with a No. 10 blade. This generally leaves an approximately 12- to 14-mm strip of ITB centrally (Figure 4). This portion should be gently lifted from the underlying tissue attachments distally at the insertion on the Gerdy tubercle. The interval between the LCL and lateral capsule of the knee is identified, and a No. 2 Ti-Cron whip-stitch is thrown through the free end of the ITB graft (Figure 5). The anterior aspect of the femoral tunnel is at the distal aspect of the lateral femoral condyle, and the posterior aspect is at the juncture of the proximal LCL and the lateral head of the gastrocnemius. The cortices of these landmarks should be perforated with a drill, and a curved instrument should be used to create a bone tunnel at this location (Figure 6). The tibial tunnel is just posterior and distal to the Gerdy tubercle and should be created in similar fashion. The graft is then passed underneath the LCL (Figure 7), through the proximal tunnel that has been created on the lateral femoral condyle, and then back down through the LCL and back onto itself after exiting the tibial tunnel (Figure 8). With the knee at 30° of flexion, the ITB graft is tensioned and sutured down to intact ITB fascia just proximal to the tibial tunnel orifice (Figure 9). We check knee range of motion (ROM) and then perform a Lachman test to assess changes in knee stability. The pivot shift examination is omitted to avoid placing excessive stress on the tenodesis. The tibial side of the patellar tendon allograft is then tensioned and secured over an AO 4.5-mm bicortical screw with washer with the knee in full extension. The screw is then tightened at 30° of knee flexion.
The ITB fascia is closed to the lateral femoral epicondyle with a running heavy suture, and all incisions are then irrigated and closed (Figures 10, 11). Standard sterile surgical dressing, Cryo/Cuff (Aircast, Vista, California), and brace are applied with the knee locked at 20°. Patients are generally discharged home the same day and followed up in clinic 1 week after surgery.
Complications
The peroneal nerve must be identified and protected during the open lateral procedure. In addition, the need for the extra lateral incision poses a slightly higher risk for infection compared with the traditional arthroscopic revision ACL procedure. Last, the additional tunnels required for the tenodesis can increase the theoretical potential for distal femur fracture and ACL graft fixation failure on the femoral side.
Postoperative Management
The operative knee is kept in extension in a brace locked at 20° for week 1 after surgery. Isometric quadriceps exercises are started immediately after surgery. Flexion to 90° is allowed starting week 2 after surgery, when the patient begins supervised active/passive flexion and progressive ROM exercises. In most cases, full ROM should be achieved by 6 to 8 weeks after surgery. Patients are progressed in their weight-bearing status by about 25% of their body weight per week, and use of crutches should be discontinued by week 4 after surgery. The brace should be discontinued by week 6 after surgery, when use of stationary bicycle and closed chain exercises begin. The patient may begin jogging when the operative leg regains 80% of contralateral quadriceps strength via Cybex strength testing. Functional drills begin in month 6, but patients should be counseled against returning to sport any earlier than 9 months after surgery.
Discussion
Achieving a successful outcome in revision ACL surgery (vs primary ACL surgery) is a significant challenge. Any of numerous factors can make the revision surgery more challenging, including existing poorly placed tunnels, tunnel expansion, lack of ideal graft choice, loss of secondary stabilizers, and deviations of the weight-bearing axis. Therefore, outcomes of revision surgery tend to be more moderate than outcomes of primary procedures.4,8-12
Revision ACL reconstruction techniques are varied and can involve use of autograft or allograft tissue as well as extra-articular augmentation techniques. Diamantopoulos and colleagues8 reported the outcomes of revision ACL reconstruction using bone–tendon–bone, hamstring, or quadriceps autografts in 107 patients. The majority of patients had improved outcome measures (mean Lysholm score improved from 51.5 to 88.5) and side-to-side laxity measurements. However, only 36.4% returned to preinjury activity level. Similarly, Noyes and Barber-Westin9 reported the outcomes of revision ACL reconstruction using quadriceps tendon–patellar bone autograft in 21 patients. Although there was significant improvement in terms of symptoms and activity level, 4 of the 21 knees were graded abnormal or severely abnormal on the IKDC (International Knee Documentation Committee) ligament rating. In a systematic review, pooled results of revision ACL reconstructions reiterated the above results.10 Eight hundred sixty-three patients from 21 studies were included in the analysis, which found significantly worse subjective outcomes than for primary procedures and a dramatically higher failure rate for the re-reconstructed ACL.
Several authors have directly compared primary cohorts with revision cohorts. Ahn and colleagues11 compared the outcomes of 59 revision ACL reconstructions with those of 117 primary reconstructions at a single institution. Although statistical comparison of stability between primary and revision ACL reconstructions showed no difference, revision reconstructions fared more poorly in terms of quality of life and return to activity compared with primary reconstructions. In a large cohort study of the Danish registry, revisions were found to have worse subjective outcomes than primary reconstructions as well.12 The study also found that the rerupture risk was significantly higher (relative risk, 2.05) when allograft was used.
Given the inferior results of revision surgery, our technique is recommended to augment the stability of reconstructed knees in the setting of revision ACL reconstruction. Adding the extra-articular procedure may augment the revised graft and protect it from excessive stress.13 A cadaver study compared double-bundle ACL reconstruction with single-bundle hamstring reconstruction plus extra-articular lateral tenodesis and found improved internal rotation control at 30° of flexion in the latter.14 Using contralateral 4-strand hamstring autograft in combination with an extra-articular lateral augment can have encouraging outcomes. Ferretti and colleagues15 reported an average Lysholm score of 95 in 12 patients who underwent this revision procedure and good anterior-to-posterior stability in 11 of the 12 patients. Trojani and colleagues16 reported on a cohort of 163 patients who underwent ACL revision surgery over a 10-year period. The authors found that 80% of patients with a lateral extra-articular tenodesis performed to augment their revision reconstruction had a negative pivot shift at long-term follow-up—versus only 63% of patients who underwent isolated revision ACL reconstruction. This finding was statistically significant, but the authors did not find any differences in IKDC scores between groups. These results support the initial biomechanical findings of Engebretsen and colleagues,17 who found that adding a lateral tenodesis decreased the forces on the reconstructed graft by 15%.
Conclusion
This technique allows for protection of the intra-articular allograft ligament reconstruction with improved rotational control that may potentially allow for improved subjective outcomes and protect against graft failure. Given the common pitfalls with stability in revision ACL surgery with allograft, this lateral extra-articular procedure can be an important structural augmentation in this challenging clinical issue in knee surgery.
Primary anterior cruciate ligament (ACL) reconstruction has satisfactory outcomes in 75% to 97% of patients.1-3 Despite this high success rate, the number of revision ACL reconstructions has risen4 and is likely underreported.5 Recurrent instability occurs if the reconstructed ligament fails to provide adequate anterior and rotational knee stability. Causes of graft failure include repeat trauma, early return to high-demand activity, poor operative technique (including poor graft placement), failure to address concomitant pathology, and perioperative complications (eg, infection, stiffness).4 In addition, most patients who have revision ACL reconstruction received autograft tissue in the initial surgery, and allograft is thus not uncommon in revision ACL surgery. Allograft tissue has longer incorporation times6 and increased incidence of recurrent postoperative instability when compared with autograft tissue.7 Extra-articular tenodesis may thus be used to provide additional stability to the revision allograft tissue while it incorporates.
In this article, we describe our use of an extra-articular iliotibial band (ITB) tenodesis as an augmentative procedure in patients undergoing revision ACL reconstruction with bone–patellar tendon–bone (BPTB) allograft.
Surgical Technique
After induction of anesthesia and careful positioning, the patient is prepared and draped in the usual sterile fashion. Standard anteromedial, anterolateral, and superolateral outflow portals are established, and diagnostic arthroscopy is performed to inspect the cruciate ligaments, menisci, and articular cartilage (Figure 1). Peripheral meniscal tears should be repaired (Figure 2), and central or inner tears should be débrided to a stable rim. If meniscal repair is performed, sutures should be tied at the end of the case. Unstable articular cartilage defects should also be débrided. An 8- to 12-cm lateral hockey-stick incision is then made from the Gerdy tubercle to the inferior edge of the lateral femoral epicondyle in preparation for the ITB tenodesis (Figure 1). The lateral collateral ligament (LCL), the lateral head of the gastrocnemius, and the ITB are identified. The peroneal nerve should be significantly distal to the working field.
Remnants of the previous ACL graft are débrided, and, if necessary, a modified notchplasty is performed. A position for the new femoral tunnel is located and is confirmed with intraoperative fluoroscopy. This tunnel is established with compaction drill bits and dilated to the appropriate diameter through the anteromedial portal with the knee in 120° of flexion.
BPTB allograft is prepared first by cutting its central third to the desired diameter (Figure 3). The bone-plug ends are prepared with compaction pliers. Two 2.0-mm drill holes are made in each of the allograft bone plugs, and a No. 5 Ti-Cron suture (Covidien, New Haven, Connecticut) is placed through each of the holes. We typically use 2 sutures on each bone plug.
A tibial tunnel is then established with an ACL drill guide under arthroscopic visualization and intraoperative fluoroscopy for confirmation of correct pin placement. We use Kirschner wires (with parallel pin guides as needed), compaction drills, and dilators to create a well-positioned tunnel of the appropriate diameter. The allograft is then passed through the tibia and femur in retrograde fashion. We secure the femoral side with an AO (Arbeitsgemeinschaft für Osteosynthesefragen) 4.5-mm bicortical screw and washer. Our tibial fixation is secured after the ITB tenodesis. The knee is then cycled a dozen times.
In preparation for the ITB tenodesis, we lengthen our previously made incision by about 4 cm proximally along the posterior aspect of the ITB. The central portion of the ITB is then outlined at the Gerdy tubercle and split with a No. 10 blade. This generally leaves an approximately 12- to 14-mm strip of ITB centrally (Figure 4). This portion should be gently lifted from the underlying tissue attachments distally at the insertion on the Gerdy tubercle. The interval between the LCL and lateral capsule of the knee is identified, and a No. 2 Ti-Cron whip-stitch is thrown through the free end of the ITB graft (Figure 5). The anterior aspect of the femoral tunnel is at the distal aspect of the lateral femoral condyle, and the posterior aspect is at the juncture of the proximal LCL and the lateral head of the gastrocnemius. The cortices of these landmarks should be perforated with a drill, and a curved instrument should be used to create a bone tunnel at this location (Figure 6). The tibial tunnel is just posterior and distal to the Gerdy tubercle and should be created in similar fashion. The graft is then passed underneath the LCL (Figure 7), through the proximal tunnel that has been created on the lateral femoral condyle, and then back down through the LCL and back onto itself after exiting the tibial tunnel (Figure 8). With the knee at 30° of flexion, the ITB graft is tensioned and sutured down to intact ITB fascia just proximal to the tibial tunnel orifice (Figure 9). We check knee range of motion (ROM) and then perform a Lachman test to assess changes in knee stability. The pivot shift examination is omitted to avoid placing excessive stress on the tenodesis. The tibial side of the patellar tendon allograft is then tensioned and secured over an AO 4.5-mm bicortical screw with washer with the knee in full extension. The screw is then tightened at 30° of knee flexion.
The ITB fascia is closed to the lateral femoral epicondyle with a running heavy suture, and all incisions are then irrigated and closed (Figures 10, 11). Standard sterile surgical dressing, Cryo/Cuff (Aircast, Vista, California), and brace are applied with the knee locked at 20°. Patients are generally discharged home the same day and followed up in clinic 1 week after surgery.
Complications
The peroneal nerve must be identified and protected during the open lateral procedure. In addition, the need for the extra lateral incision poses a slightly higher risk for infection compared with the traditional arthroscopic revision ACL procedure. Last, the additional tunnels required for the tenodesis can increase the theoretical potential for distal femur fracture and ACL graft fixation failure on the femoral side.
Postoperative Management
The operative knee is kept in extension in a brace locked at 20° for week 1 after surgery. Isometric quadriceps exercises are started immediately after surgery. Flexion to 90° is allowed starting week 2 after surgery, when the patient begins supervised active/passive flexion and progressive ROM exercises. In most cases, full ROM should be achieved by 6 to 8 weeks after surgery. Patients are progressed in their weight-bearing status by about 25% of their body weight per week, and use of crutches should be discontinued by week 4 after surgery. The brace should be discontinued by week 6 after surgery, when use of stationary bicycle and closed chain exercises begin. The patient may begin jogging when the operative leg regains 80% of contralateral quadriceps strength via Cybex strength testing. Functional drills begin in month 6, but patients should be counseled against returning to sport any earlier than 9 months after surgery.
Discussion
Achieving a successful outcome in revision ACL surgery (vs primary ACL surgery) is a significant challenge. Any of numerous factors can make the revision surgery more challenging, including existing poorly placed tunnels, tunnel expansion, lack of ideal graft choice, loss of secondary stabilizers, and deviations of the weight-bearing axis. Therefore, outcomes of revision surgery tend to be more moderate than outcomes of primary procedures.4,8-12
Revision ACL reconstruction techniques are varied and can involve use of autograft or allograft tissue as well as extra-articular augmentation techniques. Diamantopoulos and colleagues8 reported the outcomes of revision ACL reconstruction using bone–tendon–bone, hamstring, or quadriceps autografts in 107 patients. The majority of patients had improved outcome measures (mean Lysholm score improved from 51.5 to 88.5) and side-to-side laxity measurements. However, only 36.4% returned to preinjury activity level. Similarly, Noyes and Barber-Westin9 reported the outcomes of revision ACL reconstruction using quadriceps tendon–patellar bone autograft in 21 patients. Although there was significant improvement in terms of symptoms and activity level, 4 of the 21 knees were graded abnormal or severely abnormal on the IKDC (International Knee Documentation Committee) ligament rating. In a systematic review, pooled results of revision ACL reconstructions reiterated the above results.10 Eight hundred sixty-three patients from 21 studies were included in the analysis, which found significantly worse subjective outcomes than for primary procedures and a dramatically higher failure rate for the re-reconstructed ACL.
Several authors have directly compared primary cohorts with revision cohorts. Ahn and colleagues11 compared the outcomes of 59 revision ACL reconstructions with those of 117 primary reconstructions at a single institution. Although statistical comparison of stability between primary and revision ACL reconstructions showed no difference, revision reconstructions fared more poorly in terms of quality of life and return to activity compared with primary reconstructions. In a large cohort study of the Danish registry, revisions were found to have worse subjective outcomes than primary reconstructions as well.12 The study also found that the rerupture risk was significantly higher (relative risk, 2.05) when allograft was used.
Given the inferior results of revision surgery, our technique is recommended to augment the stability of reconstructed knees in the setting of revision ACL reconstruction. Adding the extra-articular procedure may augment the revised graft and protect it from excessive stress.13 A cadaver study compared double-bundle ACL reconstruction with single-bundle hamstring reconstruction plus extra-articular lateral tenodesis and found improved internal rotation control at 30° of flexion in the latter.14 Using contralateral 4-strand hamstring autograft in combination with an extra-articular lateral augment can have encouraging outcomes. Ferretti and colleagues15 reported an average Lysholm score of 95 in 12 patients who underwent this revision procedure and good anterior-to-posterior stability in 11 of the 12 patients. Trojani and colleagues16 reported on a cohort of 163 patients who underwent ACL revision surgery over a 10-year period. The authors found that 80% of patients with a lateral extra-articular tenodesis performed to augment their revision reconstruction had a negative pivot shift at long-term follow-up—versus only 63% of patients who underwent isolated revision ACL reconstruction. This finding was statistically significant, but the authors did not find any differences in IKDC scores between groups. These results support the initial biomechanical findings of Engebretsen and colleagues,17 who found that adding a lateral tenodesis decreased the forces on the reconstructed graft by 15%.
Conclusion
This technique allows for protection of the intra-articular allograft ligament reconstruction with improved rotational control that may potentially allow for improved subjective outcomes and protect against graft failure. Given the common pitfalls with stability in revision ACL surgery with allograft, this lateral extra-articular procedure can be an important structural augmentation in this challenging clinical issue in knee surgery.
1. Bach BR Jr. Revision anterior cruciate ligament surgery. Arthroscopy. 2003;19(suppl 1):14-29.
2. Baer GS, Harner CD. Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26(4):661-681.
3. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior cruciate ligament reconstruction autograft choice: bone–tendon–bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986-1995.
4. Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):199-217.
5. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6):622-627.
6. Jackson DW, Grood ES, Goldstein JD, et al. A comparison of patellar tendon autograft and allograft used for anterior cruciate ligament reconstruction in the goat model. Am J Sports Med. 1993;21(2):176-185.
7. Mascarenhas R, Tranovich M, Karpie JC, Irrgang JJ, Fu FH, Harner CD. Patellar tendon anterior cruciate ligament reconstruction in the high-demand patient: evaluation of autograft versus allograft reconstruction. Arthroscopy. 2010;26(9 Suppl):S58-S66.
8. Diamantopoulos AP, Lorbach O, Paessler HH. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36(5):851-860.
9. Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon–patellar bone autograft. Am J Sports Med. 2006;34(4):553-564.
10. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531-536.
11. Ahn JH, Lee YS, Ha HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med. 2008;36(10):1889-1895.
12. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551-1557.
13. Ferretti A, Conteduca F, Monaco E, De Carli A, D’Arrigo C. Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am. 2006;88(11):2373-2379.
14. Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1168-1174.
15. Ferretti A, Monaco E, Caperna L, Palma T, Conteduca F. Revision ACL reconstruction using contralateral hamstrings. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):690-695.
16. Trojani C, Beaufils P, Burdin G, et al. Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1565-1570.
17. Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169-176.
1. Bach BR Jr. Revision anterior cruciate ligament surgery. Arthroscopy. 2003;19(suppl 1):14-29.
2. Baer GS, Harner CD. Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26(4):661-681.
3. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior cruciate ligament reconstruction autograft choice: bone–tendon–bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986-1995.
4. Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):199-217.
5. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6):622-627.
6. Jackson DW, Grood ES, Goldstein JD, et al. A comparison of patellar tendon autograft and allograft used for anterior cruciate ligament reconstruction in the goat model. Am J Sports Med. 1993;21(2):176-185.
7. Mascarenhas R, Tranovich M, Karpie JC, Irrgang JJ, Fu FH, Harner CD. Patellar tendon anterior cruciate ligament reconstruction in the high-demand patient: evaluation of autograft versus allograft reconstruction. Arthroscopy. 2010;26(9 Suppl):S58-S66.
8. Diamantopoulos AP, Lorbach O, Paessler HH. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36(5):851-860.
9. Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon–patellar bone autograft. Am J Sports Med. 2006;34(4):553-564.
10. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531-536.
11. Ahn JH, Lee YS, Ha HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med. 2008;36(10):1889-1895.
12. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551-1557.
13. Ferretti A, Conteduca F, Monaco E, De Carli A, D’Arrigo C. Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am. 2006;88(11):2373-2379.
14. Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1168-1174.
15. Ferretti A, Monaco E, Caperna L, Palma T, Conteduca F. Revision ACL reconstruction using contralateral hamstrings. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):690-695.
16. Trojani C, Beaufils P, Burdin G, et al. Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1565-1570.
17. Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169-176.
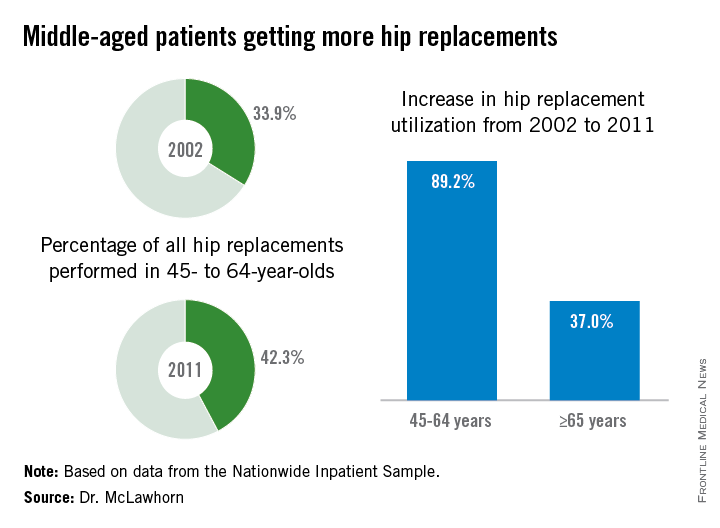
Hip replacements not just for the elderly anymore
Hip replacement is becoming more common among middle-aged Americans at the same time as the number of surgeons who perform the procedure is declining, Dr. Alexander S. McLawhorn said at the annual meeting of the American Academy of Orthopaedic Surgeons in Las Vegas.
In 2011, patients aged 45-64 years underwent 42.3% of the hip replacements performed, compared with 33.9% in 2002. The number of replacements performed rose from approximately 68,000 in 2002 to 128,000 in 2011, an increase of 89.2%, compared with an increase of 37.0% among those aged 65 years and older, according to data from the Nationwide Inpatient Sample.
This “observed growth was best explained by an expansion of the middle-aged population in the United States. This particular age group is projected to continue expanding, and as such the demand for [hip replacement] in this active group of patients will likely continue to rise as well,” Dr. McLawhorn of the Hospital for Special Surgery, New York, said in a written statement.
According to membership data from the AAOS, however, the number of physicians performing hip replacements declined by almost 29% from 2002 to 2011, which will “increase the future revision burden” on those surgeons who are still doing the procedure, the investigators said.
Dr. McLawhorn had no conflicts to report, but one of his associates disclosed relationships with Ethicon, the Knee Society, Medtronic, Mekanika, and Zimmer.
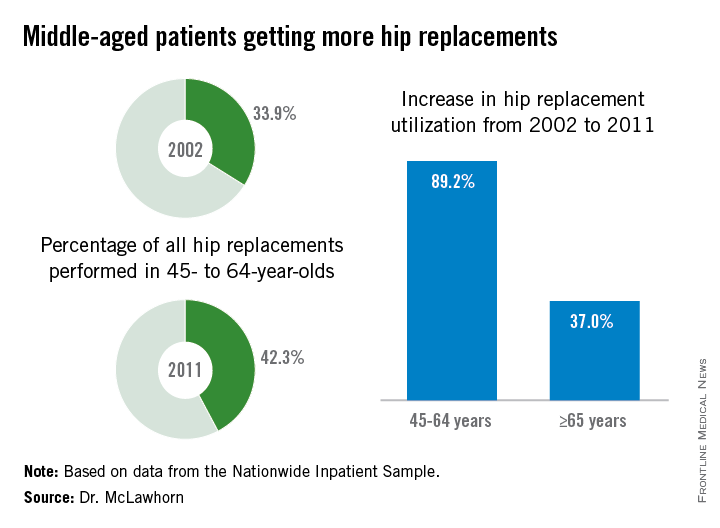
Hip replacement is becoming more common among middle-aged Americans at the same time as the number of surgeons who perform the procedure is declining, Dr. Alexander S. McLawhorn said at the annual meeting of the American Academy of Orthopaedic Surgeons in Las Vegas.
In 2011, patients aged 45-64 years underwent 42.3% of the hip replacements performed, compared with 33.9% in 2002. The number of replacements performed rose from approximately 68,000 in 2002 to 128,000 in 2011, an increase of 89.2%, compared with an increase of 37.0% among those aged 65 years and older, according to data from the Nationwide Inpatient Sample.
This “observed growth was best explained by an expansion of the middle-aged population in the United States. This particular age group is projected to continue expanding, and as such the demand for [hip replacement] in this active group of patients will likely continue to rise as well,” Dr. McLawhorn of the Hospital for Special Surgery, New York, said in a written statement.
According to membership data from the AAOS, however, the number of physicians performing hip replacements declined by almost 29% from 2002 to 2011, which will “increase the future revision burden” on those surgeons who are still doing the procedure, the investigators said.
Dr. McLawhorn had no conflicts to report, but one of his associates disclosed relationships with Ethicon, the Knee Society, Medtronic, Mekanika, and Zimmer.
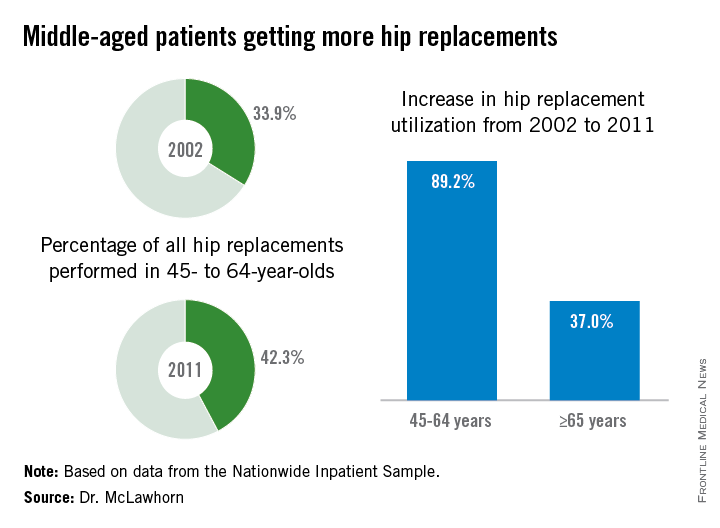
Hip replacement is becoming more common among middle-aged Americans at the same time as the number of surgeons who perform the procedure is declining, Dr. Alexander S. McLawhorn said at the annual meeting of the American Academy of Orthopaedic Surgeons in Las Vegas.
In 2011, patients aged 45-64 years underwent 42.3% of the hip replacements performed, compared with 33.9% in 2002. The number of replacements performed rose from approximately 68,000 in 2002 to 128,000 in 2011, an increase of 89.2%, compared with an increase of 37.0% among those aged 65 years and older, according to data from the Nationwide Inpatient Sample.
This “observed growth was best explained by an expansion of the middle-aged population in the United States. This particular age group is projected to continue expanding, and as such the demand for [hip replacement] in this active group of patients will likely continue to rise as well,” Dr. McLawhorn of the Hospital for Special Surgery, New York, said in a written statement.
According to membership data from the AAOS, however, the number of physicians performing hip replacements declined by almost 29% from 2002 to 2011, which will “increase the future revision burden” on those surgeons who are still doing the procedure, the investigators said.
Dr. McLawhorn had no conflicts to report, but one of his associates disclosed relationships with Ethicon, the Knee Society, Medtronic, Mekanika, and Zimmer.
FROM AAOS 2015
Child Pedestrians More Likely to Be Struck By Motor Vehicles in the Spring Months, While Unsupervised, Near Schools and Bus Stops
LAS VEGAS—Most child pedestrian injuries involving a motor vehicle occurred while children were unsupervised, near schools and bus stops, and in the spring months during the afternoon and evening hours, according to research presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
Pedestrian injuries are among the leading causes of pediatric deaths in the United States. In 2012, 557 child and young adult pedestrians younger than 20 years were killed by motor vehicles in the US and 22,000 were injured, according to the National Highway Traffic Safety Administration. Nearly three-fourths (73%) of pedestrian fatalities occur in urban settings.
In this study, researchers reviewed electronic medical records of 100 child pedestrian emergency department visits at St. Christopher’s Hospital for Children in Philadelphia from January 1 to December 21, 2012, including ambulance dispatch data, patient demographics, procedure(s), diagnoses, and length of stay. First responder narratives provided accident scene descriptions, including the individuals who were present at the time of the accident and the type of intersection or property where the injuries occurred. Google Maps were used to identify the accident site, injury clusters, and specific street locations.
The patients included 79 boys and 21 girls with an average age of 8 years. Sixty-one percent of patients were evaluated in the emergency department only, or were admitted for less than 24 hours, while 39 patients were admitted for 24 hours or more with a mean length of stay of 1.98 days. Eleven patients were admitted to the Intensive Care Unit (ICU) for at least 1 day. Among the other findings:
• At the time of the trauma, 40% of the children were accompanied to the emergency department by a parent or guardian, 34% by friends or peers, 13% by older siblings, and 13% were alone.
• Most injuries occurred around the time of school dismissal and during evening hours: 29% of injuries occurred between 2 PM and 5 PM, and 42% between 5 PM and 9 PM.
• The greatest number of injuries occurred during the month of June (13%) followed by the other spring months.
• Of the 44 cases with enough accident scene information to perform a detailed analysis, 70% (31) of the children were injured mid-block, and 18% (8) at a crosswalk. Nearly 10% (5) were struck on private property, a sidewalk, or in a parking lot.
• Injury clusters were identified near schools and public bus stops used by students for transportation to and from school.
“Accidents most frequently occurred when no parental supervision was present from the time of school dismissal until the early evening hours, and were most often located mid-block,” said orthopedic surgery resident and lead study author Alexa J. Karkenny, MD. “Injuries peaked during the warm months and clustered both near schools and bus stops located near schools.
“Keeping these spatial, temporal, and behavioral predictors of pediatric orthopedic trauma in mind, we can help guide prevention strategies in urban settings,” said Dr. Karkenny. In the emergency department, “knowledge of the high-risk injuries in this subset of patients can help the trauma team to prioritize patient evaluations, which is especially important in complicated cases involving multiple injuries.”
Injury prevention efforts should focus on improved supervision at school dismissal and public transportation safety near school zones, the study authors concluded.
LAS VEGAS—Most child pedestrian injuries involving a motor vehicle occurred while children were unsupervised, near schools and bus stops, and in the spring months during the afternoon and evening hours, according to research presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
Pedestrian injuries are among the leading causes of pediatric deaths in the United States. In 2012, 557 child and young adult pedestrians younger than 20 years were killed by motor vehicles in the US and 22,000 were injured, according to the National Highway Traffic Safety Administration. Nearly three-fourths (73%) of pedestrian fatalities occur in urban settings.
In this study, researchers reviewed electronic medical records of 100 child pedestrian emergency department visits at St. Christopher’s Hospital for Children in Philadelphia from January 1 to December 21, 2012, including ambulance dispatch data, patient demographics, procedure(s), diagnoses, and length of stay. First responder narratives provided accident scene descriptions, including the individuals who were present at the time of the accident and the type of intersection or property where the injuries occurred. Google Maps were used to identify the accident site, injury clusters, and specific street locations.
The patients included 79 boys and 21 girls with an average age of 8 years. Sixty-one percent of patients were evaluated in the emergency department only, or were admitted for less than 24 hours, while 39 patients were admitted for 24 hours or more with a mean length of stay of 1.98 days. Eleven patients were admitted to the Intensive Care Unit (ICU) for at least 1 day. Among the other findings:
• At the time of the trauma, 40% of the children were accompanied to the emergency department by a parent or guardian, 34% by friends or peers, 13% by older siblings, and 13% were alone.
• Most injuries occurred around the time of school dismissal and during evening hours: 29% of injuries occurred between 2 PM and 5 PM, and 42% between 5 PM and 9 PM.
• The greatest number of injuries occurred during the month of June (13%) followed by the other spring months.
• Of the 44 cases with enough accident scene information to perform a detailed analysis, 70% (31) of the children were injured mid-block, and 18% (8) at a crosswalk. Nearly 10% (5) were struck on private property, a sidewalk, or in a parking lot.
• Injury clusters were identified near schools and public bus stops used by students for transportation to and from school.
“Accidents most frequently occurred when no parental supervision was present from the time of school dismissal until the early evening hours, and were most often located mid-block,” said orthopedic surgery resident and lead study author Alexa J. Karkenny, MD. “Injuries peaked during the warm months and clustered both near schools and bus stops located near schools.
“Keeping these spatial, temporal, and behavioral predictors of pediatric orthopedic trauma in mind, we can help guide prevention strategies in urban settings,” said Dr. Karkenny. In the emergency department, “knowledge of the high-risk injuries in this subset of patients can help the trauma team to prioritize patient evaluations, which is especially important in complicated cases involving multiple injuries.”
Injury prevention efforts should focus on improved supervision at school dismissal and public transportation safety near school zones, the study authors concluded.
LAS VEGAS—Most child pedestrian injuries involving a motor vehicle occurred while children were unsupervised, near schools and bus stops, and in the spring months during the afternoon and evening hours, according to research presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
Pedestrian injuries are among the leading causes of pediatric deaths in the United States. In 2012, 557 child and young adult pedestrians younger than 20 years were killed by motor vehicles in the US and 22,000 were injured, according to the National Highway Traffic Safety Administration. Nearly three-fourths (73%) of pedestrian fatalities occur in urban settings.
In this study, researchers reviewed electronic medical records of 100 child pedestrian emergency department visits at St. Christopher’s Hospital for Children in Philadelphia from January 1 to December 21, 2012, including ambulance dispatch data, patient demographics, procedure(s), diagnoses, and length of stay. First responder narratives provided accident scene descriptions, including the individuals who were present at the time of the accident and the type of intersection or property where the injuries occurred. Google Maps were used to identify the accident site, injury clusters, and specific street locations.
The patients included 79 boys and 21 girls with an average age of 8 years. Sixty-one percent of patients were evaluated in the emergency department only, or were admitted for less than 24 hours, while 39 patients were admitted for 24 hours or more with a mean length of stay of 1.98 days. Eleven patients were admitted to the Intensive Care Unit (ICU) for at least 1 day. Among the other findings:
• At the time of the trauma, 40% of the children were accompanied to the emergency department by a parent or guardian, 34% by friends or peers, 13% by older siblings, and 13% were alone.
• Most injuries occurred around the time of school dismissal and during evening hours: 29% of injuries occurred between 2 PM and 5 PM, and 42% between 5 PM and 9 PM.
• The greatest number of injuries occurred during the month of June (13%) followed by the other spring months.
• Of the 44 cases with enough accident scene information to perform a detailed analysis, 70% (31) of the children were injured mid-block, and 18% (8) at a crosswalk. Nearly 10% (5) were struck on private property, a sidewalk, or in a parking lot.
• Injury clusters were identified near schools and public bus stops used by students for transportation to and from school.
“Accidents most frequently occurred when no parental supervision was present from the time of school dismissal until the early evening hours, and were most often located mid-block,” said orthopedic surgery resident and lead study author Alexa J. Karkenny, MD. “Injuries peaked during the warm months and clustered both near schools and bus stops located near schools.
“Keeping these spatial, temporal, and behavioral predictors of pediatric orthopedic trauma in mind, we can help guide prevention strategies in urban settings,” said Dr. Karkenny. In the emergency department, “knowledge of the high-risk injuries in this subset of patients can help the trauma team to prioritize patient evaluations, which is especially important in complicated cases involving multiple injuries.”
Injury prevention efforts should focus on improved supervision at school dismissal and public transportation safety near school zones, the study authors concluded.
More Than One-Third of Division I College Athletes May Have Low Vitamin D Levels
LAS VEGAS—A new study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS) found that more than one-third of elite, Division I college athletes may have low levels of vitamin D, which aids the absorption of calcium. Male, black, and Hispanic athletes are at greatest risk, researchers reported.
“Although multiple studies have demonstrated a high prevalence of vitamin D insufficiency across various populations, there is a paucity of data regarding elite level athletes,” said orthopedic surgeon and lead study author Diego Villacis, MD, Administrative Chief Resident at the University of Southern California. “Recent studies also have demonstrated that vitamin D levels have a direct relationship with muscle power, force, velocity, and optimal bone mass.”
In this study, which appeared in the February 2014 online issue of Sports Health, researchers measured the serum 25-hydroxyvitamin D (serum 25) levels of 223 athletes (121 men and 102 women) between June 2012 and August 2012. The mean serum 25 level for the athletes, enrolled in a broad range of indoor and outdoor sports, was 40.1 ±14.9 ng/mL (≥32 ng/mL is considered normal; 20 to <32 ng/mL, insufficient; and <20 ng/mL, deficient). Overall, 66.4% of participants had sufficient vitamin D levels and 33.6% had insufficient or deficient levels.
Men were 2.8 times more likely to have an abnormal vitamin D level, according to the results, and athletes with darker skin tones also faced a “much higher risk” for insufficient vitamin D. Black athletes were 19.1 times more likely to have abnormal vitamin D levels compared to white athletes, and Hispanics, 6.1 times more likely.
“Our study demonstrated abnormal vitamin D levels in nearly one out of three elite NCAA Division I athletes tested,” said Dr. Villacis. “Although there is much more work to be done, our results open the possibility for improved performance and most importantly decreased risk of injury with correction of vitamin D levels. This may potentially be achieved simply and safely through modification of diet, sunlight exposure, and vitamin D supplementation.”
LAS VEGAS—A new study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS) found that more than one-third of elite, Division I college athletes may have low levels of vitamin D, which aids the absorption of calcium. Male, black, and Hispanic athletes are at greatest risk, researchers reported.
“Although multiple studies have demonstrated a high prevalence of vitamin D insufficiency across various populations, there is a paucity of data regarding elite level athletes,” said orthopedic surgeon and lead study author Diego Villacis, MD, Administrative Chief Resident at the University of Southern California. “Recent studies also have demonstrated that vitamin D levels have a direct relationship with muscle power, force, velocity, and optimal bone mass.”
In this study, which appeared in the February 2014 online issue of Sports Health, researchers measured the serum 25-hydroxyvitamin D (serum 25) levels of 223 athletes (121 men and 102 women) between June 2012 and August 2012. The mean serum 25 level for the athletes, enrolled in a broad range of indoor and outdoor sports, was 40.1 ±14.9 ng/mL (≥32 ng/mL is considered normal; 20 to <32 ng/mL, insufficient; and <20 ng/mL, deficient). Overall, 66.4% of participants had sufficient vitamin D levels and 33.6% had insufficient or deficient levels.
Men were 2.8 times more likely to have an abnormal vitamin D level, according to the results, and athletes with darker skin tones also faced a “much higher risk” for insufficient vitamin D. Black athletes were 19.1 times more likely to have abnormal vitamin D levels compared to white athletes, and Hispanics, 6.1 times more likely.
“Our study demonstrated abnormal vitamin D levels in nearly one out of three elite NCAA Division I athletes tested,” said Dr. Villacis. “Although there is much more work to be done, our results open the possibility for improved performance and most importantly decreased risk of injury with correction of vitamin D levels. This may potentially be achieved simply and safely through modification of diet, sunlight exposure, and vitamin D supplementation.”
LAS VEGAS—A new study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS) found that more than one-third of elite, Division I college athletes may have low levels of vitamin D, which aids the absorption of calcium. Male, black, and Hispanic athletes are at greatest risk, researchers reported.
“Although multiple studies have demonstrated a high prevalence of vitamin D insufficiency across various populations, there is a paucity of data regarding elite level athletes,” said orthopedic surgeon and lead study author Diego Villacis, MD, Administrative Chief Resident at the University of Southern California. “Recent studies also have demonstrated that vitamin D levels have a direct relationship with muscle power, force, velocity, and optimal bone mass.”
In this study, which appeared in the February 2014 online issue of Sports Health, researchers measured the serum 25-hydroxyvitamin D (serum 25) levels of 223 athletes (121 men and 102 women) between June 2012 and August 2012. The mean serum 25 level for the athletes, enrolled in a broad range of indoor and outdoor sports, was 40.1 ±14.9 ng/mL (≥32 ng/mL is considered normal; 20 to <32 ng/mL, insufficient; and <20 ng/mL, deficient). Overall, 66.4% of participants had sufficient vitamin D levels and 33.6% had insufficient or deficient levels.
Men were 2.8 times more likely to have an abnormal vitamin D level, according to the results, and athletes with darker skin tones also faced a “much higher risk” for insufficient vitamin D. Black athletes were 19.1 times more likely to have abnormal vitamin D levels compared to white athletes, and Hispanics, 6.1 times more likely.
“Our study demonstrated abnormal vitamin D levels in nearly one out of three elite NCAA Division I athletes tested,” said Dr. Villacis. “Although there is much more work to be done, our results open the possibility for improved performance and most importantly decreased risk of injury with correction of vitamin D levels. This may potentially be achieved simply and safely through modification of diet, sunlight exposure, and vitamin D supplementation.”
Women Fare Better Than Men Following Total Knee, Hip Replacement
LAS VEGAS—While women may have their first total joint replacement (TJR) at an older age, they are less likely to have complications related to their surgery or require revision surgery, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). The findings contradict the theory that TJR is underutilized in female patients because they have worse outcomes than men.
Researchers reviewed patient databases from an Ontario hospital for first-time primary total hip replacement (THR) and total knee replacement (TKR) patients between 2002 and 2009. There were 37,881 THR surgeries (53.8% female) and 59,564 TKR surgeries (60.5% female). Women who underwent THR were significantly older than males (70 years vs. 65 years); however, there was no difference in age between male and female patients undergoing TKR (median age 68 years for both). A greater proportion of female patients undergoing TJR were defined as frail (6.6% vs. 3.5% for THR; and, 6.7% vs. 4% for TKR).
Following surgery, men were:
• 15% more likely to return to the emergency department within 30 days of hospital discharge following either THR or TKR.
• 60% and 70% more likely to have an acute myocardial infarction within 3 months following THR and TKR, respectively.
• 50% more likely to require a revision arthroplasty within 2 years of TKR.
• 25% more likely to be readmitted to the hospital and 70% more likely to experience an infection or revision surgery within 2 years of TKR, compared to women.
“Despite the fact that women have a higher prevalence of advanced hip and knee arthritis, prior research indicates that North American women with arthritis are less likely to receive joint replacement than men,” said lead study author Bheeshma Ravi, MD, PhD, an orthopedic surgery resident at the University of Toronto. “One possible explanation is that women are less often offered or accept surgery because their risk of serious complications following surgery is greater than that of men.
“In this study, we found that while overall rates of serious complications were low for both groups, they were lower for women than for men for both hip and knee replacement, particularly the latter” said Dr. Ravi. “Thus, the previously documented sex difference utilization of TJR cannot be explained by differential risks of complications following surgery.”
LAS VEGAS—While women may have their first total joint replacement (TJR) at an older age, they are less likely to have complications related to their surgery or require revision surgery, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). The findings contradict the theory that TJR is underutilized in female patients because they have worse outcomes than men.
Researchers reviewed patient databases from an Ontario hospital for first-time primary total hip replacement (THR) and total knee replacement (TKR) patients between 2002 and 2009. There were 37,881 THR surgeries (53.8% female) and 59,564 TKR surgeries (60.5% female). Women who underwent THR were significantly older than males (70 years vs. 65 years); however, there was no difference in age between male and female patients undergoing TKR (median age 68 years for both). A greater proportion of female patients undergoing TJR were defined as frail (6.6% vs. 3.5% for THR; and, 6.7% vs. 4% for TKR).
Following surgery, men were:
• 15% more likely to return to the emergency department within 30 days of hospital discharge following either THR or TKR.
• 60% and 70% more likely to have an acute myocardial infarction within 3 months following THR and TKR, respectively.
• 50% more likely to require a revision arthroplasty within 2 years of TKR.
• 25% more likely to be readmitted to the hospital and 70% more likely to experience an infection or revision surgery within 2 years of TKR, compared to women.
“Despite the fact that women have a higher prevalence of advanced hip and knee arthritis, prior research indicates that North American women with arthritis are less likely to receive joint replacement than men,” said lead study author Bheeshma Ravi, MD, PhD, an orthopedic surgery resident at the University of Toronto. “One possible explanation is that women are less often offered or accept surgery because their risk of serious complications following surgery is greater than that of men.
“In this study, we found that while overall rates of serious complications were low for both groups, they were lower for women than for men for both hip and knee replacement, particularly the latter” said Dr. Ravi. “Thus, the previously documented sex difference utilization of TJR cannot be explained by differential risks of complications following surgery.”
LAS VEGAS—While women may have their first total joint replacement (TJR) at an older age, they are less likely to have complications related to their surgery or require revision surgery, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). The findings contradict the theory that TJR is underutilized in female patients because they have worse outcomes than men.
Researchers reviewed patient databases from an Ontario hospital for first-time primary total hip replacement (THR) and total knee replacement (TKR) patients between 2002 and 2009. There were 37,881 THR surgeries (53.8% female) and 59,564 TKR surgeries (60.5% female). Women who underwent THR were significantly older than males (70 years vs. 65 years); however, there was no difference in age between male and female patients undergoing TKR (median age 68 years for both). A greater proportion of female patients undergoing TJR were defined as frail (6.6% vs. 3.5% for THR; and, 6.7% vs. 4% for TKR).
Following surgery, men were:
• 15% more likely to return to the emergency department within 30 days of hospital discharge following either THR or TKR.
• 60% and 70% more likely to have an acute myocardial infarction within 3 months following THR and TKR, respectively.
• 50% more likely to require a revision arthroplasty within 2 years of TKR.
• 25% more likely to be readmitted to the hospital and 70% more likely to experience an infection or revision surgery within 2 years of TKR, compared to women.
“Despite the fact that women have a higher prevalence of advanced hip and knee arthritis, prior research indicates that North American women with arthritis are less likely to receive joint replacement than men,” said lead study author Bheeshma Ravi, MD, PhD, an orthopedic surgery resident at the University of Toronto. “One possible explanation is that women are less often offered or accept surgery because their risk of serious complications following surgery is greater than that of men.
“In this study, we found that while overall rates of serious complications were low for both groups, they were lower for women than for men for both hip and knee replacement, particularly the latter” said Dr. Ravi. “Thus, the previously documented sex difference utilization of TJR cannot be explained by differential risks of complications following surgery.”
Black, Hispanic Patients More Likely to Be Readmitted to the Hospital Within 30 Days Following Hip or Knee Replacement Surgery
LAS VEGAS—Black and Hispanic patients were 62% and 50%, respectively, more likely to be readmitted to the hospital within 30 days after total joint replacement (TJR) surgery compared to white patients, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). In addition, Medicaid patients were 40% more likely to be readmitted to the hospital than patients with private insurance. Poorer outcomes, due in part to patient comorbidities, may reflect limited access to primary care, insufficient patient-doctor communication, researchers suggest.
Disparities in the provision of health care services have long been documented, including that black patients utilize hip and total knee replacement at rates nearly 40% less than white patients, despite having comparable or higher rates of osteoarthritis.
In this study, researchers analyzed 5 years of data—demographic (including race/ethnicity), clinical, and billing—on nearly 53,000 patients admitted to Connecticut hospitals for TJR from 2008 to 2012. The average patient age was 67 years, and the vast majority of patients were white (87%), covered by Medicare (56.7%), and female (61%).
The overall 30-day readmission rate for patients was 5.2%. The most common reasons for readmission were postoperative infection (8%), infection and inflammatory reaction due to internal joint prosthesis (6%), hematoma complications during a procedure (3%), and dislocation of a prosthetic joint (3%). Among the other study findings:
• Readmission rates were 83.5 per thousand for black patients, 78.9 for Hispanic patients, and 53.3 for white patients.
• Longer length of hospital stay was significantly associated with increased odds of readmission.
• When controlling for comorbidities and type of insurance coverage, the readmission rate for Hispanic patients dropped 44%, and for black patients, 38%. Black patients remained significantly more likely than white patients to be readmitted following surgery, after controlling for comorbidities.
• Patients covered by Medicare were 30% more likely to be readmitted within 30 days following discharge compared to patients covered by private insurance, and Medicaid patients were 40% more likely.
Recent research using national data on Medicare suggests that community-based factors, such as availability of general practitioners in the area, may be as or more important than hospital factors in determining readmission rates, and that patients may have few options other than hospital care for both urgent and non-urgent conditions related to their surgery or other conditions.
“Using an all-payer database, our study shows that black patients who undergo total knee replacement may have poorer outcomes,” said lead study author and orthopedic surgeon Courtland Lewis, MD. “After controlling for two key variables implicated in race and ethnic disparities in hospital readmission—preoperative comorbidities and type of insurance coverage—black patients still have a 35% higher likelihood of all-cause, 30-day readmission compared to white patients.
“Our ongoing research in this area is focused on other factors, such as the patient’s connection to primary care and patient-provider communication, that may explain this troubling finding,” said Dr. Lewis.
LAS VEGAS—Black and Hispanic patients were 62% and 50%, respectively, more likely to be readmitted to the hospital within 30 days after total joint replacement (TJR) surgery compared to white patients, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). In addition, Medicaid patients were 40% more likely to be readmitted to the hospital than patients with private insurance. Poorer outcomes, due in part to patient comorbidities, may reflect limited access to primary care, insufficient patient-doctor communication, researchers suggest.
Disparities in the provision of health care services have long been documented, including that black patients utilize hip and total knee replacement at rates nearly 40% less than white patients, despite having comparable or higher rates of osteoarthritis.
In this study, researchers analyzed 5 years of data—demographic (including race/ethnicity), clinical, and billing—on nearly 53,000 patients admitted to Connecticut hospitals for TJR from 2008 to 2012. The average patient age was 67 years, and the vast majority of patients were white (87%), covered by Medicare (56.7%), and female (61%).
The overall 30-day readmission rate for patients was 5.2%. The most common reasons for readmission were postoperative infection (8%), infection and inflammatory reaction due to internal joint prosthesis (6%), hematoma complications during a procedure (3%), and dislocation of a prosthetic joint (3%). Among the other study findings:
• Readmission rates were 83.5 per thousand for black patients, 78.9 for Hispanic patients, and 53.3 for white patients.
• Longer length of hospital stay was significantly associated with increased odds of readmission.
• When controlling for comorbidities and type of insurance coverage, the readmission rate for Hispanic patients dropped 44%, and for black patients, 38%. Black patients remained significantly more likely than white patients to be readmitted following surgery, after controlling for comorbidities.
• Patients covered by Medicare were 30% more likely to be readmitted within 30 days following discharge compared to patients covered by private insurance, and Medicaid patients were 40% more likely.
Recent research using national data on Medicare suggests that community-based factors, such as availability of general practitioners in the area, may be as or more important than hospital factors in determining readmission rates, and that patients may have few options other than hospital care for both urgent and non-urgent conditions related to their surgery or other conditions.
“Using an all-payer database, our study shows that black patients who undergo total knee replacement may have poorer outcomes,” said lead study author and orthopedic surgeon Courtland Lewis, MD. “After controlling for two key variables implicated in race and ethnic disparities in hospital readmission—preoperative comorbidities and type of insurance coverage—black patients still have a 35% higher likelihood of all-cause, 30-day readmission compared to white patients.
“Our ongoing research in this area is focused on other factors, such as the patient’s connection to primary care and patient-provider communication, that may explain this troubling finding,” said Dr. Lewis.
LAS VEGAS—Black and Hispanic patients were 62% and 50%, respectively, more likely to be readmitted to the hospital within 30 days after total joint replacement (TJR) surgery compared to white patients, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). In addition, Medicaid patients were 40% more likely to be readmitted to the hospital than patients with private insurance. Poorer outcomes, due in part to patient comorbidities, may reflect limited access to primary care, insufficient patient-doctor communication, researchers suggest.
Disparities in the provision of health care services have long been documented, including that black patients utilize hip and total knee replacement at rates nearly 40% less than white patients, despite having comparable or higher rates of osteoarthritis.
In this study, researchers analyzed 5 years of data—demographic (including race/ethnicity), clinical, and billing—on nearly 53,000 patients admitted to Connecticut hospitals for TJR from 2008 to 2012. The average patient age was 67 years, and the vast majority of patients were white (87%), covered by Medicare (56.7%), and female (61%).
The overall 30-day readmission rate for patients was 5.2%. The most common reasons for readmission were postoperative infection (8%), infection and inflammatory reaction due to internal joint prosthesis (6%), hematoma complications during a procedure (3%), and dislocation of a prosthetic joint (3%). Among the other study findings:
• Readmission rates were 83.5 per thousand for black patients, 78.9 for Hispanic patients, and 53.3 for white patients.
• Longer length of hospital stay was significantly associated with increased odds of readmission.
• When controlling for comorbidities and type of insurance coverage, the readmission rate for Hispanic patients dropped 44%, and for black patients, 38%. Black patients remained significantly more likely than white patients to be readmitted following surgery, after controlling for comorbidities.
• Patients covered by Medicare were 30% more likely to be readmitted within 30 days following discharge compared to patients covered by private insurance, and Medicaid patients were 40% more likely.
Recent research using national data on Medicare suggests that community-based factors, such as availability of general practitioners in the area, may be as or more important than hospital factors in determining readmission rates, and that patients may have few options other than hospital care for both urgent and non-urgent conditions related to their surgery or other conditions.
“Using an all-payer database, our study shows that black patients who undergo total knee replacement may have poorer outcomes,” said lead study author and orthopedic surgeon Courtland Lewis, MD. “After controlling for two key variables implicated in race and ethnic disparities in hospital readmission—preoperative comorbidities and type of insurance coverage—black patients still have a 35% higher likelihood of all-cause, 30-day readmission compared to white patients.
“Our ongoing research in this area is focused on other factors, such as the patient’s connection to primary care and patient-provider communication, that may explain this troubling finding,” said Dr. Lewis.
Stem Cells May Significantly Improve Tendon Healing, Reduce Retear Risk in Rotator Cuff Surgery
LAS VEGAS—An injection of a patient’s bone marrow stem cells during rotator cuff surgery significantly improved healing and tendon durability, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
The French study, of which a portion appeared in the September 2014 issue of International Orthopaedics, included 90 patients who underwent rotator cuff surgery. Forty-five of the patients received injections of bone marrow concentrate (BMC) mesenchymal stem cells (MSCs) at the surgical site, and 45 had their rotator cuff repaired or reattached without MSCs. Researchers tried to make the 2 groups as equivalent as possible based on rotator cuff tear size, tendon rupture location, dominate shoulder, gender, and age.
Patient ultrasound images were obtained each month following surgery for 24 months. In addition, magnetic resonance imaging was obtained of patient shoulders at 3 and 6 months following surgery, and at 1 year, 2 years, and 10 years following surgery.
At 6 months, all 45 of the patients who received MSCs had healed rotator cuff tendons, compared to 30 (67%) of the patients who did not receive MSCs. The use of BMC also prevented further ruptures or retears. At 10 years after surgery, intact rotator cuffs were found in 39 (87%) of the MSC patients, but just 20 (44%) of the non-MSC patients.
In addition, “some retears or new tears occurred after 1 year,” said lead study author Philippe Hernigou, MD, an orthopedic surgeon at the University of Paris. “These retears were more frequently associated with the control group patients who were not treated with MSCs.
“While the risk of a retear after arthroscopic repair of the rotator cuff has been well documented, publications with long-term follow-up (more than 3 years) are relatively limited,” said Dr. Hernigou. “Many patients undergoing rotator cuff repair surgery show advanced degeneration of the tendons, which are thinner and atrophic, probably explaining why negative results are so often reported in the literature, with frequent post-operative complications, especially retear. Observations in the MSC treatment group support the potential that MSC treatment has both a short-term and long-term benefit in reducing the rate of tendon retear.”
LAS VEGAS—An injection of a patient’s bone marrow stem cells during rotator cuff surgery significantly improved healing and tendon durability, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
The French study, of which a portion appeared in the September 2014 issue of International Orthopaedics, included 90 patients who underwent rotator cuff surgery. Forty-five of the patients received injections of bone marrow concentrate (BMC) mesenchymal stem cells (MSCs) at the surgical site, and 45 had their rotator cuff repaired or reattached without MSCs. Researchers tried to make the 2 groups as equivalent as possible based on rotator cuff tear size, tendon rupture location, dominate shoulder, gender, and age.
Patient ultrasound images were obtained each month following surgery for 24 months. In addition, magnetic resonance imaging was obtained of patient shoulders at 3 and 6 months following surgery, and at 1 year, 2 years, and 10 years following surgery.
At 6 months, all 45 of the patients who received MSCs had healed rotator cuff tendons, compared to 30 (67%) of the patients who did not receive MSCs. The use of BMC also prevented further ruptures or retears. At 10 years after surgery, intact rotator cuffs were found in 39 (87%) of the MSC patients, but just 20 (44%) of the non-MSC patients.
In addition, “some retears or new tears occurred after 1 year,” said lead study author Philippe Hernigou, MD, an orthopedic surgeon at the University of Paris. “These retears were more frequently associated with the control group patients who were not treated with MSCs.
“While the risk of a retear after arthroscopic repair of the rotator cuff has been well documented, publications with long-term follow-up (more than 3 years) are relatively limited,” said Dr. Hernigou. “Many patients undergoing rotator cuff repair surgery show advanced degeneration of the tendons, which are thinner and atrophic, probably explaining why negative results are so often reported in the literature, with frequent post-operative complications, especially retear. Observations in the MSC treatment group support the potential that MSC treatment has both a short-term and long-term benefit in reducing the rate of tendon retear.”
LAS VEGAS—An injection of a patient’s bone marrow stem cells during rotator cuff surgery significantly improved healing and tendon durability, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
The French study, of which a portion appeared in the September 2014 issue of International Orthopaedics, included 90 patients who underwent rotator cuff surgery. Forty-five of the patients received injections of bone marrow concentrate (BMC) mesenchymal stem cells (MSCs) at the surgical site, and 45 had their rotator cuff repaired or reattached without MSCs. Researchers tried to make the 2 groups as equivalent as possible based on rotator cuff tear size, tendon rupture location, dominate shoulder, gender, and age.
Patient ultrasound images were obtained each month following surgery for 24 months. In addition, magnetic resonance imaging was obtained of patient shoulders at 3 and 6 months following surgery, and at 1 year, 2 years, and 10 years following surgery.
At 6 months, all 45 of the patients who received MSCs had healed rotator cuff tendons, compared to 30 (67%) of the patients who did not receive MSCs. The use of BMC also prevented further ruptures or retears. At 10 years after surgery, intact rotator cuffs were found in 39 (87%) of the MSC patients, but just 20 (44%) of the non-MSC patients.
In addition, “some retears or new tears occurred after 1 year,” said lead study author Philippe Hernigou, MD, an orthopedic surgeon at the University of Paris. “These retears were more frequently associated with the control group patients who were not treated with MSCs.
“While the risk of a retear after arthroscopic repair of the rotator cuff has been well documented, publications with long-term follow-up (more than 3 years) are relatively limited,” said Dr. Hernigou. “Many patients undergoing rotator cuff repair surgery show advanced degeneration of the tendons, which are thinner and atrophic, probably explaining why negative results are so often reported in the literature, with frequent post-operative complications, especially retear. Observations in the MSC treatment group support the potential that MSC treatment has both a short-term and long-term benefit in reducing the rate of tendon retear.”
Hip Replacements in Middle-Age Nearly Double From 2002-2011, Outpacing Growth in Elderly Population
LAS VEGAS—The number of total hip replacements (THRs) nearly doubled among middle-age patients between 2002 and 2011, primarily due to the expansion of the middle-age population in the United States, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Continued growth in utilization of hip replacement surgery in patients ages 45 to 64 years, an increase in revision surgeries for this population as they age, and a nearly 30% decline in the number of surgeons who perform THR could have significant implications for future health care costs, THR demand, and access, researchers said.
The researchers used the Nationwide Inpatient Sample (NIS) to identify primary THRs performed between 2002 and 2011 in patients ages 45 to 64 years, as well as related hospital charges. Population data and projections were obtained from the US Census Bureau and surgeon workforce estimates from the AAOS.
In 2011, 42.3% of THRs were performed in patients ages 45 to 64 years compared to 33.9% in 2002. Utilization of THR in this age group increased 89.2% from 2002 to 2011, from approximately 68,000 THRs in 2002 to 128,000 THRs in 2011. The overall population increased 21.3%. In addition, the authors found that:
• Growth of THR utilization in the 45- to 64-year-old age group grew 2.4 times faster than it did in the Medicare-aged population (age > 65 years).
• A rise in the prevalence of obesity, a known risk factor for hip osteoarthritis, among middle-age Americans was not significantly associated with increased THR utilization.
• Mean hospital charges in the THR 45- to 64-year-old age group declined 5.7% from 2002 to 2011, and declined 2.5% in the Medicare population (age > 65 years).
• Mean physician reimbursement per THR, in 2011 US dollars, declined 26.2% over the same period.
• Concurrently, the number of physicians reporting that they performed THR surgeries declined 28.2%.
“The purpose of this study was to identify potential drivers of THR utilization in the middle-age patient segment,” said lead study author Alexander S. McLawhorn, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery in New York City. “Our multivariable statistical model suggested that the observed growth was best explained by an expansion of the middle-age population in the US. This particular age group is projected to continue expanding, and as such the demand for THR in this active group of patients will likely continue to rise as well. Our results underscore concerns about consumption of premium-priced implants in younger patients and the future revision burden this trend implies in the face of a dwindling number of physicians who specialize in hip arthroplasty surgery.”
LAS VEGAS—The number of total hip replacements (THRs) nearly doubled among middle-age patients between 2002 and 2011, primarily due to the expansion of the middle-age population in the United States, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Continued growth in utilization of hip replacement surgery in patients ages 45 to 64 years, an increase in revision surgeries for this population as they age, and a nearly 30% decline in the number of surgeons who perform THR could have significant implications for future health care costs, THR demand, and access, researchers said.
The researchers used the Nationwide Inpatient Sample (NIS) to identify primary THRs performed between 2002 and 2011 in patients ages 45 to 64 years, as well as related hospital charges. Population data and projections were obtained from the US Census Bureau and surgeon workforce estimates from the AAOS.
In 2011, 42.3% of THRs were performed in patients ages 45 to 64 years compared to 33.9% in 2002. Utilization of THR in this age group increased 89.2% from 2002 to 2011, from approximately 68,000 THRs in 2002 to 128,000 THRs in 2011. The overall population increased 21.3%. In addition, the authors found that:
• Growth of THR utilization in the 45- to 64-year-old age group grew 2.4 times faster than it did in the Medicare-aged population (age > 65 years).
• A rise in the prevalence of obesity, a known risk factor for hip osteoarthritis, among middle-age Americans was not significantly associated with increased THR utilization.
• Mean hospital charges in the THR 45- to 64-year-old age group declined 5.7% from 2002 to 2011, and declined 2.5% in the Medicare population (age > 65 years).
• Mean physician reimbursement per THR, in 2011 US dollars, declined 26.2% over the same period.
• Concurrently, the number of physicians reporting that they performed THR surgeries declined 28.2%.
“The purpose of this study was to identify potential drivers of THR utilization in the middle-age patient segment,” said lead study author Alexander S. McLawhorn, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery in New York City. “Our multivariable statistical model suggested that the observed growth was best explained by an expansion of the middle-age population in the US. This particular age group is projected to continue expanding, and as such the demand for THR in this active group of patients will likely continue to rise as well. Our results underscore concerns about consumption of premium-priced implants in younger patients and the future revision burden this trend implies in the face of a dwindling number of physicians who specialize in hip arthroplasty surgery.”
LAS VEGAS—The number of total hip replacements (THRs) nearly doubled among middle-age patients between 2002 and 2011, primarily due to the expansion of the middle-age population in the United States, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Continued growth in utilization of hip replacement surgery in patients ages 45 to 64 years, an increase in revision surgeries for this population as they age, and a nearly 30% decline in the number of surgeons who perform THR could have significant implications for future health care costs, THR demand, and access, researchers said.
The researchers used the Nationwide Inpatient Sample (NIS) to identify primary THRs performed between 2002 and 2011 in patients ages 45 to 64 years, as well as related hospital charges. Population data and projections were obtained from the US Census Bureau and surgeon workforce estimates from the AAOS.
In 2011, 42.3% of THRs were performed in patients ages 45 to 64 years compared to 33.9% in 2002. Utilization of THR in this age group increased 89.2% from 2002 to 2011, from approximately 68,000 THRs in 2002 to 128,000 THRs in 2011. The overall population increased 21.3%. In addition, the authors found that:
• Growth of THR utilization in the 45- to 64-year-old age group grew 2.4 times faster than it did in the Medicare-aged population (age > 65 years).
• A rise in the prevalence of obesity, a known risk factor for hip osteoarthritis, among middle-age Americans was not significantly associated with increased THR utilization.
• Mean hospital charges in the THR 45- to 64-year-old age group declined 5.7% from 2002 to 2011, and declined 2.5% in the Medicare population (age > 65 years).
• Mean physician reimbursement per THR, in 2011 US dollars, declined 26.2% over the same period.
• Concurrently, the number of physicians reporting that they performed THR surgeries declined 28.2%.
“The purpose of this study was to identify potential drivers of THR utilization in the middle-age patient segment,” said lead study author Alexander S. McLawhorn, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery in New York City. “Our multivariable statistical model suggested that the observed growth was best explained by an expansion of the middle-age population in the US. This particular age group is projected to continue expanding, and as such the demand for THR in this active group of patients will likely continue to rise as well. Our results underscore concerns about consumption of premium-priced implants in younger patients and the future revision burden this trend implies in the face of a dwindling number of physicians who specialize in hip arthroplasty surgery.”
Study Identifies Low Back Pain Risk Factors
LAS VEGAS—Nicotine dependence, obesity, alcohol abuse, and depressive disorders are risk factors for low back pain, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Monitoring and counseling at-risk patients may prevent and minimize pain and improve quality of life, researchers said.
According to the U.S. Centers for Disease Control and Prevention’s (CDC) 2012 National Health Survey, nearly one-third of American adults reported that they had experienced low back pain during the previous 3 months. Determining modifiable risk factors for low back pain could help avoid or diminish the financial and emotional costs of this condition.
Researchers reviewed electronic records of more than 26 million patients from 13 health care systems across the United States, including 1.2 million patients diagnosed with low back pain (approximately 4.54% of the patient records).
The review found that 19.3% of the patients diagnosed with a depressive disorder reported lower back pain, as did 16.75% of patients diagnosed as obese (BMI > 30kg/m²), 16.53% of the patients diagnosed with nicotine dependence, and 14.66% with reported alcohol abuse. Patients with nicotine dependence, obesity, depressive disorders, and alcohol abuse had statistically significant relative risks of 4.489, 6.007, 5.511, and 3.326 for low back pain, respectively, when compared to other patients.
“This study used an electronic health care database to identify modifiable risk factors—obesity, depressive disorders, alcohol and tobacco use—in patients with low back pain,” said lead study author and orthopedic surgeon Scott Shemory, MD. “The findings will allow physicians to better counsel and more closely follow their high-risk patients.”
LAS VEGAS—Nicotine dependence, obesity, alcohol abuse, and depressive disorders are risk factors for low back pain, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Monitoring and counseling at-risk patients may prevent and minimize pain and improve quality of life, researchers said.
According to the U.S. Centers for Disease Control and Prevention’s (CDC) 2012 National Health Survey, nearly one-third of American adults reported that they had experienced low back pain during the previous 3 months. Determining modifiable risk factors for low back pain could help avoid or diminish the financial and emotional costs of this condition.
Researchers reviewed electronic records of more than 26 million patients from 13 health care systems across the United States, including 1.2 million patients diagnosed with low back pain (approximately 4.54% of the patient records).
The review found that 19.3% of the patients diagnosed with a depressive disorder reported lower back pain, as did 16.75% of patients diagnosed as obese (BMI > 30kg/m²), 16.53% of the patients diagnosed with nicotine dependence, and 14.66% with reported alcohol abuse. Patients with nicotine dependence, obesity, depressive disorders, and alcohol abuse had statistically significant relative risks of 4.489, 6.007, 5.511, and 3.326 for low back pain, respectively, when compared to other patients.
“This study used an electronic health care database to identify modifiable risk factors—obesity, depressive disorders, alcohol and tobacco use—in patients with low back pain,” said lead study author and orthopedic surgeon Scott Shemory, MD. “The findings will allow physicians to better counsel and more closely follow their high-risk patients.”
LAS VEGAS—Nicotine dependence, obesity, alcohol abuse, and depressive disorders are risk factors for low back pain, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Monitoring and counseling at-risk patients may prevent and minimize pain and improve quality of life, researchers said.
According to the U.S. Centers for Disease Control and Prevention’s (CDC) 2012 National Health Survey, nearly one-third of American adults reported that they had experienced low back pain during the previous 3 months. Determining modifiable risk factors for low back pain could help avoid or diminish the financial and emotional costs of this condition.
Researchers reviewed electronic records of more than 26 million patients from 13 health care systems across the United States, including 1.2 million patients diagnosed with low back pain (approximately 4.54% of the patient records).
The review found that 19.3% of the patients diagnosed with a depressive disorder reported lower back pain, as did 16.75% of patients diagnosed as obese (BMI > 30kg/m²), 16.53% of the patients diagnosed with nicotine dependence, and 14.66% with reported alcohol abuse. Patients with nicotine dependence, obesity, depressive disorders, and alcohol abuse had statistically significant relative risks of 4.489, 6.007, 5.511, and 3.326 for low back pain, respectively, when compared to other patients.
“This study used an electronic health care database to identify modifiable risk factors—obesity, depressive disorders, alcohol and tobacco use—in patients with low back pain,” said lead study author and orthopedic surgeon Scott Shemory, MD. “The findings will allow physicians to better counsel and more closely follow their high-risk patients.”
A Not-So-Old Football Injury
ANSWER
Imaging shows a ventral dislocation of the lunate. There is also a tiny avulsion fracture on the ulnar aspect of the adjacent triquetrum.
The patient was referred to orthopedics for a perilunate dislocation of the left wrist. He underwent successful closed reduction and was placed in a short arm cast for four weeks.
ANSWER
Imaging shows a ventral dislocation of the lunate. There is also a tiny avulsion fracture on the ulnar aspect of the adjacent triquetrum.
The patient was referred to orthopedics for a perilunate dislocation of the left wrist. He underwent successful closed reduction and was placed in a short arm cast for four weeks.
ANSWER
Imaging shows a ventral dislocation of the lunate. There is also a tiny avulsion fracture on the ulnar aspect of the adjacent triquetrum.
The patient was referred to orthopedics for a perilunate dislocation of the left wrist. He underwent successful closed reduction and was placed in a short arm cast for four weeks.

A 15-year-old boy presents for evaluation of left wrist pain. He says that two days ago, while playing football, he fell onto his outstretched left hand, which twisted upon impact with the ground. Immediately after the fall, he experienced severe pain. Since then, the pain has been constant, although it lessens to a moderate dull ache at rest and sharpens with activity. He denies any numbness or tingling in the affected hand and wrist. There are no other areas of injury from the fall, nor is there significant medical history. Physical exam identifies moderate left wrist swelling with focal tenderness over the volar aspect of the distal radius, extending to the wrist. The patient has limited active and passive flexion and extension of the left hand and wrist, along with reduced grip strength due to pain. There is mild navicular tenderness. Radial pulse is 2+, the hand is warm to the touch, and the skin is intact. Sensation is intact in all of the digits, which also demonstrate brisk capillary refill. Radiographs of the left wrist are obtained. What is your impression?