User login
Depression and substance abuse
VIDEO: Intestinal remodeling contributes to HbA1c drop after Roux-en-Y gastric bypass
CHICAGO – Of medical and surgical tactics to tackle long-term weight loss, , and gene expression in the Roux limb may hold the key to the surgery’s efficacy, according to an ongoing study.
“We know that Roux-en-Y gastric bypass surgery is highly effective as not only a weight-loss therapy, but more and more we’re appreciating its role as a diabetes therapy as well,” said Margaret Stefater, MD, PhD, speaking in an interview at the annual meeting of the Endocrine Society.
The study, she said, was designed to learn more about the intestine’s contribution to the salubrious effect that Roux-en-Y surgery has on diabetes.
“We used microarray in order to characterize gene expression in the intestine” to gain a broad understanding of the processes that are altered after surgery, said Dr. Stefater, a pediatric endocrinology fellow at Boston Children’s Hospital. More specifically, though, the study looked at an individual’s changes in gene expression over time and correlated those changes with that patient’s clinical picture.
The data reported by Dr. Stefater and shared in a press conference, represent part of an ongoing longitudinal prospective study of 32 patients.
“The study aims to characterize gene expression for the first postoperative year,” and findings from the first 6 postoperative months of 19 patients were shared at the meeting, said Dr. Stefater. “This is the first look at our cohort.”
So far, she and her colleagues have compared gene expression using microarray at 1 month and 6 months post-surgery, comparing change across time and change from baseline data.
From hundreds of candidate genes, Dr. Stefater and her colleagues have developed a smaller gene list that, even in the first postoperative month, is predictive of changes in hemoglobin A1c levels over time. “Remarkably, the changes in a select list of genes out to 1 month is actually able to predict hemoglobin A1c levels out to 1 year,” she said. “This speaks to the fact that biological reprogramming in the intestine is somehow related to glycemic response in patients.
“We hope that by understanding these processes, we can home in on those processes that are most likely to be mechanistically responsible for these changes, and then to reverse-engineer this surgery to identify processes or targets which may be good places to start when we think about creating better, or nonsurgical, therapies for people who have obesity and diabetes,” said Dr. Stefater.
Dr. Stefater reported no relevant financial disclosures.
SOURCE: Stefater MA et al. ENDO 2018, Abstract OR 12-6.
CHICAGO – Of medical and surgical tactics to tackle long-term weight loss, , and gene expression in the Roux limb may hold the key to the surgery’s efficacy, according to an ongoing study.
“We know that Roux-en-Y gastric bypass surgery is highly effective as not only a weight-loss therapy, but more and more we’re appreciating its role as a diabetes therapy as well,” said Margaret Stefater, MD, PhD, speaking in an interview at the annual meeting of the Endocrine Society.
The study, she said, was designed to learn more about the intestine’s contribution to the salubrious effect that Roux-en-Y surgery has on diabetes.
“We used microarray in order to characterize gene expression in the intestine” to gain a broad understanding of the processes that are altered after surgery, said Dr. Stefater, a pediatric endocrinology fellow at Boston Children’s Hospital. More specifically, though, the study looked at an individual’s changes in gene expression over time and correlated those changes with that patient’s clinical picture.
The data reported by Dr. Stefater and shared in a press conference, represent part of an ongoing longitudinal prospective study of 32 patients.
“The study aims to characterize gene expression for the first postoperative year,” and findings from the first 6 postoperative months of 19 patients were shared at the meeting, said Dr. Stefater. “This is the first look at our cohort.”
So far, she and her colleagues have compared gene expression using microarray at 1 month and 6 months post-surgery, comparing change across time and change from baseline data.
From hundreds of candidate genes, Dr. Stefater and her colleagues have developed a smaller gene list that, even in the first postoperative month, is predictive of changes in hemoglobin A1c levels over time. “Remarkably, the changes in a select list of genes out to 1 month is actually able to predict hemoglobin A1c levels out to 1 year,” she said. “This speaks to the fact that biological reprogramming in the intestine is somehow related to glycemic response in patients.
“We hope that by understanding these processes, we can home in on those processes that are most likely to be mechanistically responsible for these changes, and then to reverse-engineer this surgery to identify processes or targets which may be good places to start when we think about creating better, or nonsurgical, therapies for people who have obesity and diabetes,” said Dr. Stefater.
Dr. Stefater reported no relevant financial disclosures.
SOURCE: Stefater MA et al. ENDO 2018, Abstract OR 12-6.
CHICAGO – Of medical and surgical tactics to tackle long-term weight loss, , and gene expression in the Roux limb may hold the key to the surgery’s efficacy, according to an ongoing study.
“We know that Roux-en-Y gastric bypass surgery is highly effective as not only a weight-loss therapy, but more and more we’re appreciating its role as a diabetes therapy as well,” said Margaret Stefater, MD, PhD, speaking in an interview at the annual meeting of the Endocrine Society.
The study, she said, was designed to learn more about the intestine’s contribution to the salubrious effect that Roux-en-Y surgery has on diabetes.
“We used microarray in order to characterize gene expression in the intestine” to gain a broad understanding of the processes that are altered after surgery, said Dr. Stefater, a pediatric endocrinology fellow at Boston Children’s Hospital. More specifically, though, the study looked at an individual’s changes in gene expression over time and correlated those changes with that patient’s clinical picture.
The data reported by Dr. Stefater and shared in a press conference, represent part of an ongoing longitudinal prospective study of 32 patients.
“The study aims to characterize gene expression for the first postoperative year,” and findings from the first 6 postoperative months of 19 patients were shared at the meeting, said Dr. Stefater. “This is the first look at our cohort.”
So far, she and her colleagues have compared gene expression using microarray at 1 month and 6 months post-surgery, comparing change across time and change from baseline data.
From hundreds of candidate genes, Dr. Stefater and her colleagues have developed a smaller gene list that, even in the first postoperative month, is predictive of changes in hemoglobin A1c levels over time. “Remarkably, the changes in a select list of genes out to 1 month is actually able to predict hemoglobin A1c levels out to 1 year,” she said. “This speaks to the fact that biological reprogramming in the intestine is somehow related to glycemic response in patients.
“We hope that by understanding these processes, we can home in on those processes that are most likely to be mechanistically responsible for these changes, and then to reverse-engineer this surgery to identify processes or targets which may be good places to start when we think about creating better, or nonsurgical, therapies for people who have obesity and diabetes,” said Dr. Stefater.
Dr. Stefater reported no relevant financial disclosures.
SOURCE: Stefater MA et al. ENDO 2018, Abstract OR 12-6.
REPORTING FROM ENDO 2018
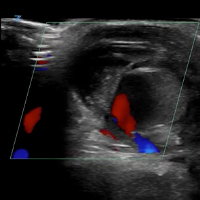
VIDEO: Ultrasound with Doppler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
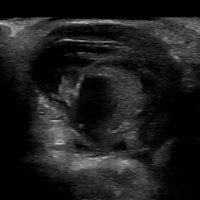
VIDEO: Initial Bedside Ultrasound of Pulsatile Hand Mass



Cenk Ayata, MD, & Messoud Ashina, MD



Bridget Mueller, MD, PhD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Paul Rizzoli, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Christopher Gottschalk, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Nanotechnology is making a mark in gastroenterology
BOSTON – Nanotechnology, though small in scale, is making a big difference in gastroenterology. Nanoparticles can deliver therapeutic compounds or enable other diagnostic tools, said Vadim Backman, PhD, the Walter Dill Scott Professor of Biomedical Engineering at Northwestern University, Chicago, in a video interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. Nanotechnology can treat disease by reprogramming gene expression or gene regulation. Nanoparticle formulations are FDA approved now for treatment of esophageal, colon, and pancreatic cancers, said Dr. Backman in a video interview, but the ability of nanotechnology to reprogram biological processes at the genetic level has researchers looking at treating inflammatory diseases and regenerating tissues.
BOSTON – Nanotechnology, though small in scale, is making a big difference in gastroenterology. Nanoparticles can deliver therapeutic compounds or enable other diagnostic tools, said Vadim Backman, PhD, the Walter Dill Scott Professor of Biomedical Engineering at Northwestern University, Chicago, in a video interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. Nanotechnology can treat disease by reprogramming gene expression or gene regulation. Nanoparticle formulations are FDA approved now for treatment of esophageal, colon, and pancreatic cancers, said Dr. Backman in a video interview, but the ability of nanotechnology to reprogram biological processes at the genetic level has researchers looking at treating inflammatory diseases and regenerating tissues.
BOSTON – Nanotechnology, though small in scale, is making a big difference in gastroenterology. Nanoparticles can deliver therapeutic compounds or enable other diagnostic tools, said Vadim Backman, PhD, the Walter Dill Scott Professor of Biomedical Engineering at Northwestern University, Chicago, in a video interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. Nanotechnology can treat disease by reprogramming gene expression or gene regulation. Nanoparticle formulations are FDA approved now for treatment of esophageal, colon, and pancreatic cancers, said Dr. Backman in a video interview, but the ability of nanotechnology to reprogram biological processes at the genetic level has researchers looking at treating inflammatory diseases and regenerating tissues.
FROM THE 2018 AGA TECH SUMMIT
VIDEO: Digital innovation, consumer point of view can solve clinical problems
BOSTON – Carla E. Small, MBA, senior director of innovation at Boston Children’s Hospital, addressed digital health care in a video interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. It is really just providing health care to patients in a digital world, she said, adding that she prefers the term “tech-enabled health care.” One up-and-coming example of this is the use of Alexa-type voice devices to do work and solve small clinical problems. Her program did a nationwide survey of pediatricians and found that half were interested in using voice technology. Artificial intelligence is another area of technology that Boston Children’s is using – in particular, they have created algorithms that help pediatricians analyze brain scans of young children, because so few pediatricians are trained in this area. The innovation program also has taken the digital world to pediatric patients in a program called Health Voyager in which children can take a virtual journey through their own diseased intestinal system.
BOSTON – Carla E. Small, MBA, senior director of innovation at Boston Children’s Hospital, addressed digital health care in a video interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. It is really just providing health care to patients in a digital world, she said, adding that she prefers the term “tech-enabled health care.” One up-and-coming example of this is the use of Alexa-type voice devices to do work and solve small clinical problems. Her program did a nationwide survey of pediatricians and found that half were interested in using voice technology. Artificial intelligence is another area of technology that Boston Children’s is using – in particular, they have created algorithms that help pediatricians analyze brain scans of young children, because so few pediatricians are trained in this area. The innovation program also has taken the digital world to pediatric patients in a program called Health Voyager in which children can take a virtual journey through their own diseased intestinal system.
BOSTON – Carla E. Small, MBA, senior director of innovation at Boston Children’s Hospital, addressed digital health care in a video interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. It is really just providing health care to patients in a digital world, she said, adding that she prefers the term “tech-enabled health care.” One up-and-coming example of this is the use of Alexa-type voice devices to do work and solve small clinical problems. Her program did a nationwide survey of pediatricians and found that half were interested in using voice technology. Artificial intelligence is another area of technology that Boston Children’s is using – in particular, they have created algorithms that help pediatricians analyze brain scans of young children, because so few pediatricians are trained in this area. The innovation program also has taken the digital world to pediatric patients in a program called Health Voyager in which children can take a virtual journey through their own diseased intestinal system.
FROM THE 20I8 AGA TECH SUMMIT