User login
Impact and Recovery of VHA Epilepsy Care Services During the COVID-19 Pandemic
The COVID-19 pandemic affected diverse workplaces globally, leading to temporary and permanent changes across the health care landscape. Included among the impacted areas of care were epilepsy and electroencephalogram (EEG) clinicians and services. Surveys among epilepsy specialists and neurophysiologists conducted at the onset of the pandemic to evaluate working conditions include analyses from the American Epilepsy Society (AES), the National Association of Epilepsy Centers (NAEC), the International League Against Epilepsy, and an Italian national survey.1-4 These investigations revealed reductions in epilepsy monitoring unit (EMU) admissions (23% decline), epilepsy surgery (6% decline), inpatient EEG (22% of respondents reported decline), and patients having difficulty accessing epilepsy professionals (28% of respondents reported decline) or obtaining medications (20% of respondents reported decline).1-3
While such research provided evidence for changes to epilepsy care in 2020, there are limited data on subsequent adaptations during the pandemic. These studies did not incorporate data on the spread of COVID-19 or administrative workload numbers to analyze service delivery beyond self reports. This study aimed to address this gap in the literature by highlighting results from longitudinal national surveys conducted at the Epilepsy Centers of Excellence (ECoE), a specialty care service within the Veterans Health Administration (VHA), which annually serves > 9 million veterans.5 The ECoE represents epileptologists and neurophysiologists across the United States at the 17 primary facilities that were established at the time of this survey (2 ECoEs have been added since survey completion) in 4 geographical regions and for which other regional facilities refer patients for diagnostic services or specialty care.6
National surveys were conducted among the ECoE directors regarding adaptations made from May 2020 to June 2022 to provide a comprehensive account of limitations they experienced and how adjustments have been made to improve patient care. Survey responses were compared to administrative workload numbers and COVID-19 spread data from the Centers for Disease Control and Prevention (CDC) to provide a comprehensive analysis of performance during the pandemic.
METHODS
Data were collected as part of a quality improvement initiative by the VHA ECoE; institutional review board approval was not required. An 18-item survey covering 5 broad domains was sent to ECoE directors 4 separate times to accumulate data from 4 time periods: May to June 2020 (T1); December 2020 to February 2021 (T2); July to August 2021 (T3); and June to July 2022 (T4). These periods correspond to the following phases of the pandemic: T1, onset of pandemic; T2, vaccine availability; T3, Delta variant predominant; T4, Omicron variant predominant.
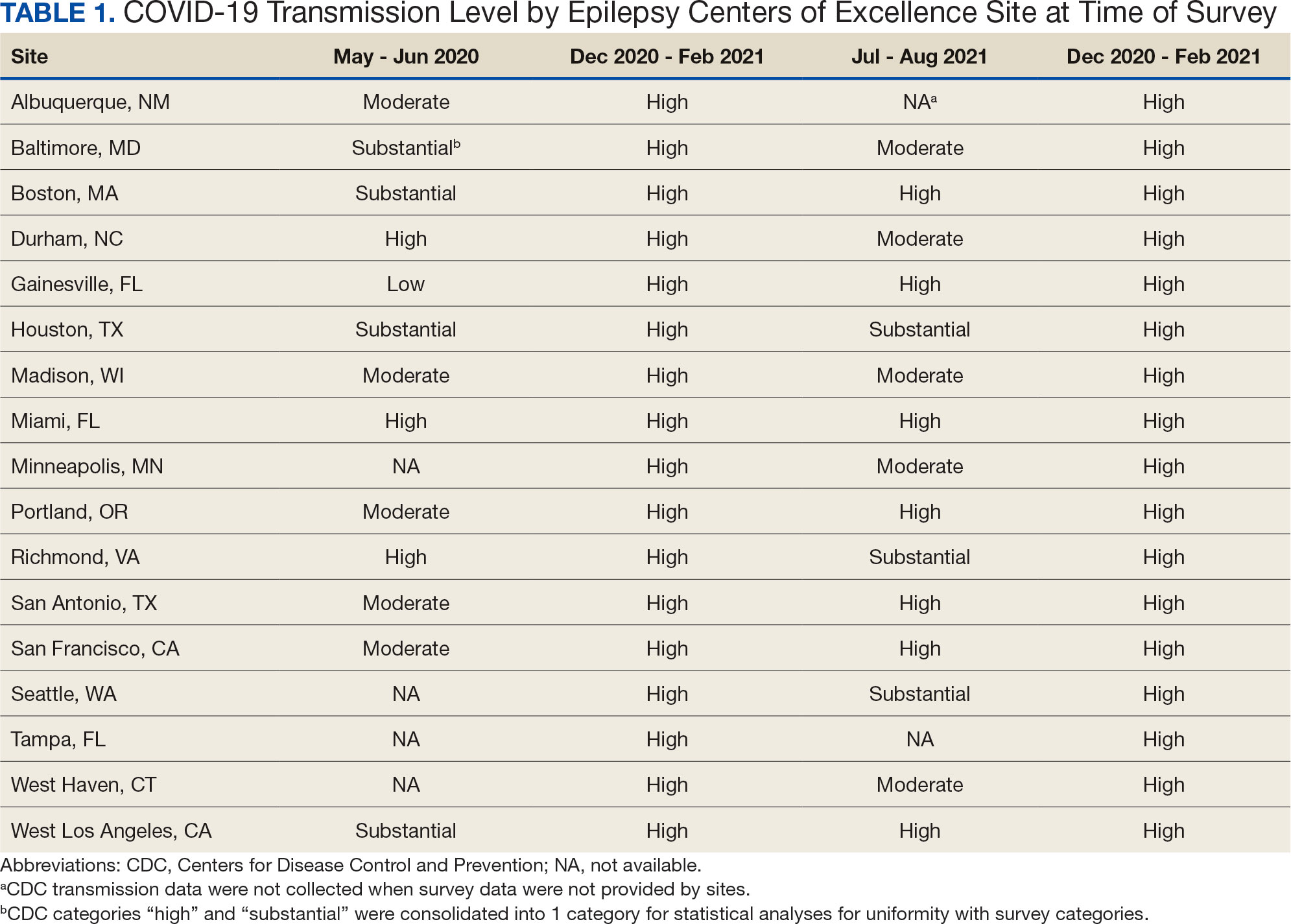
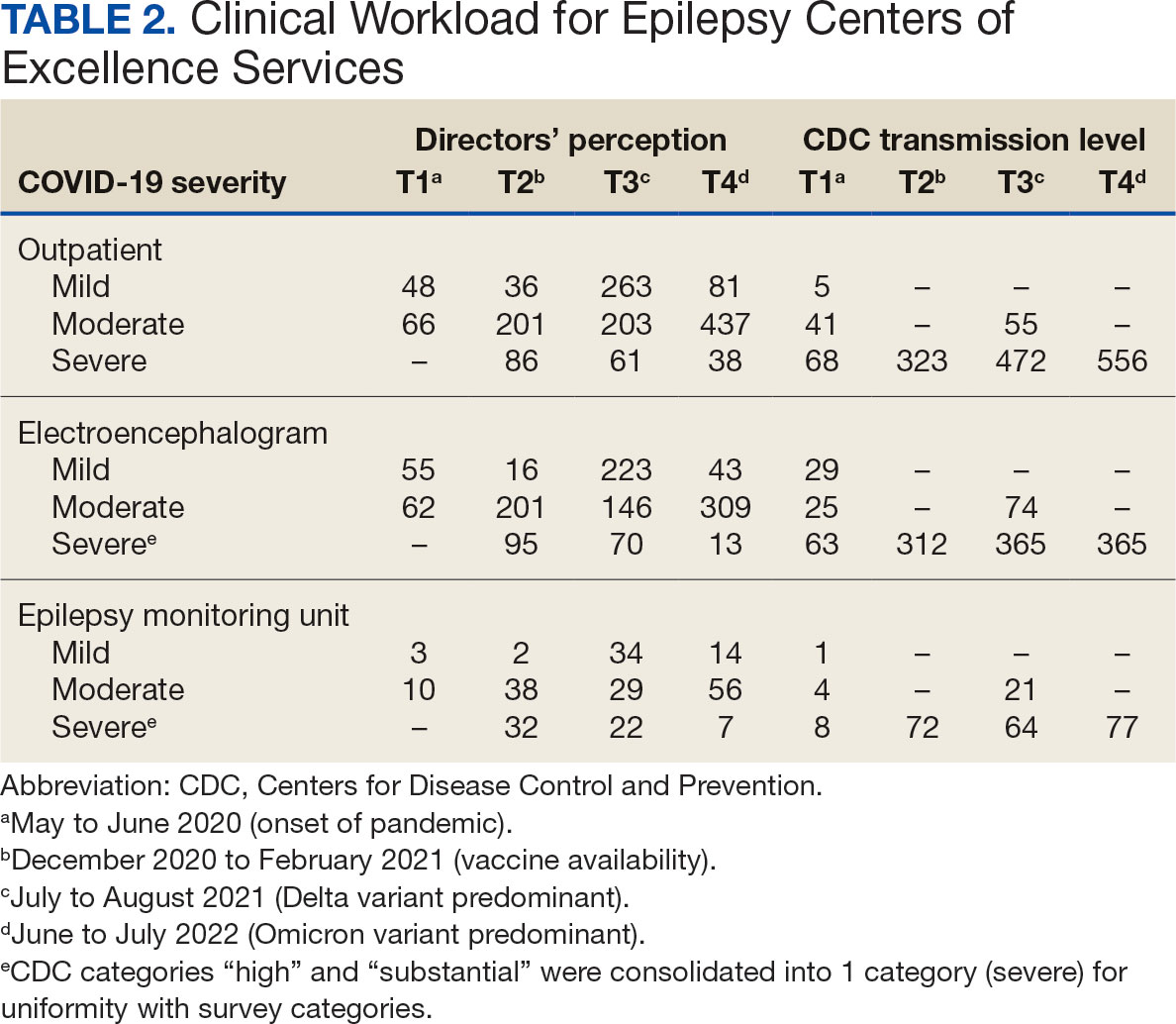
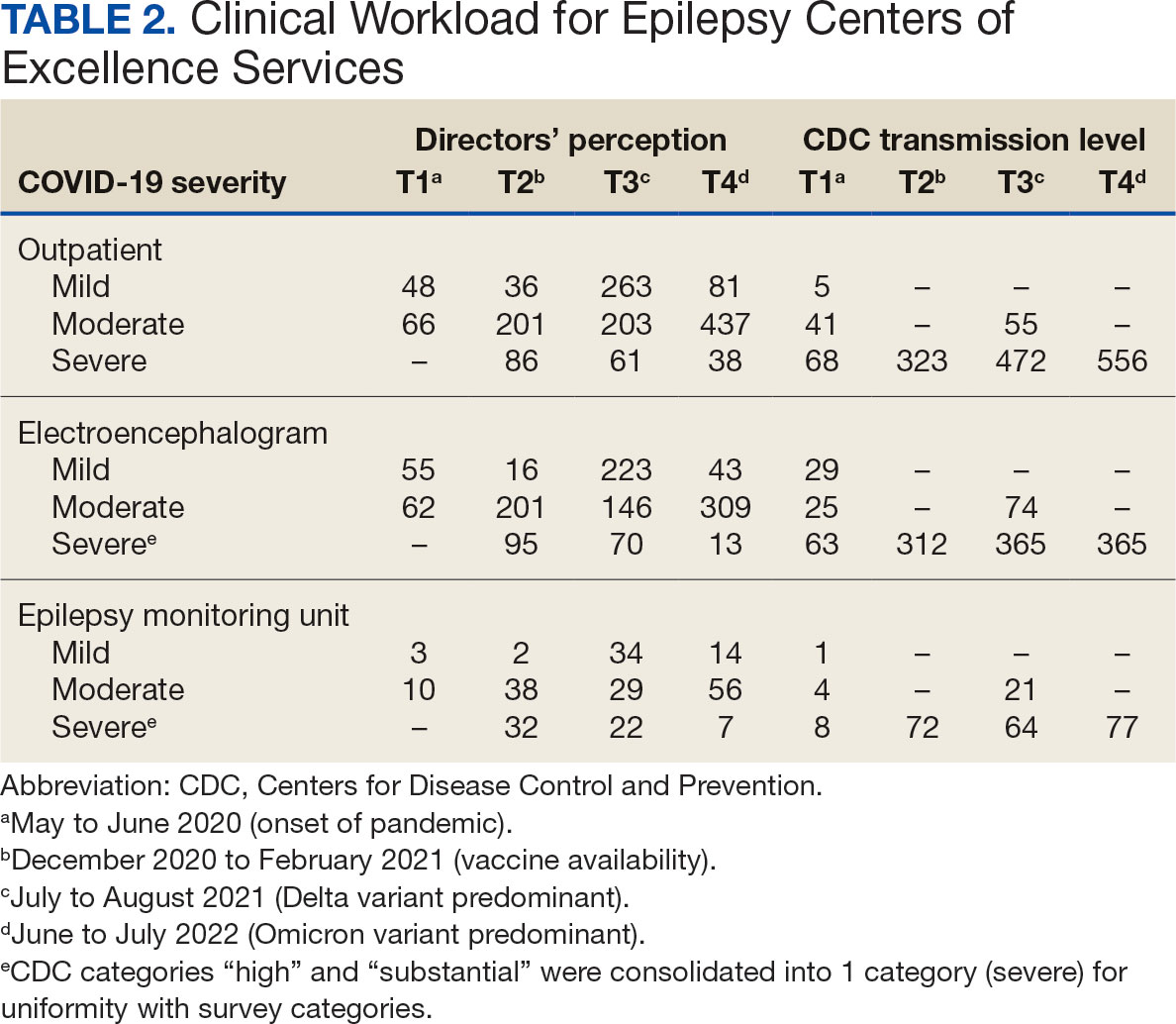
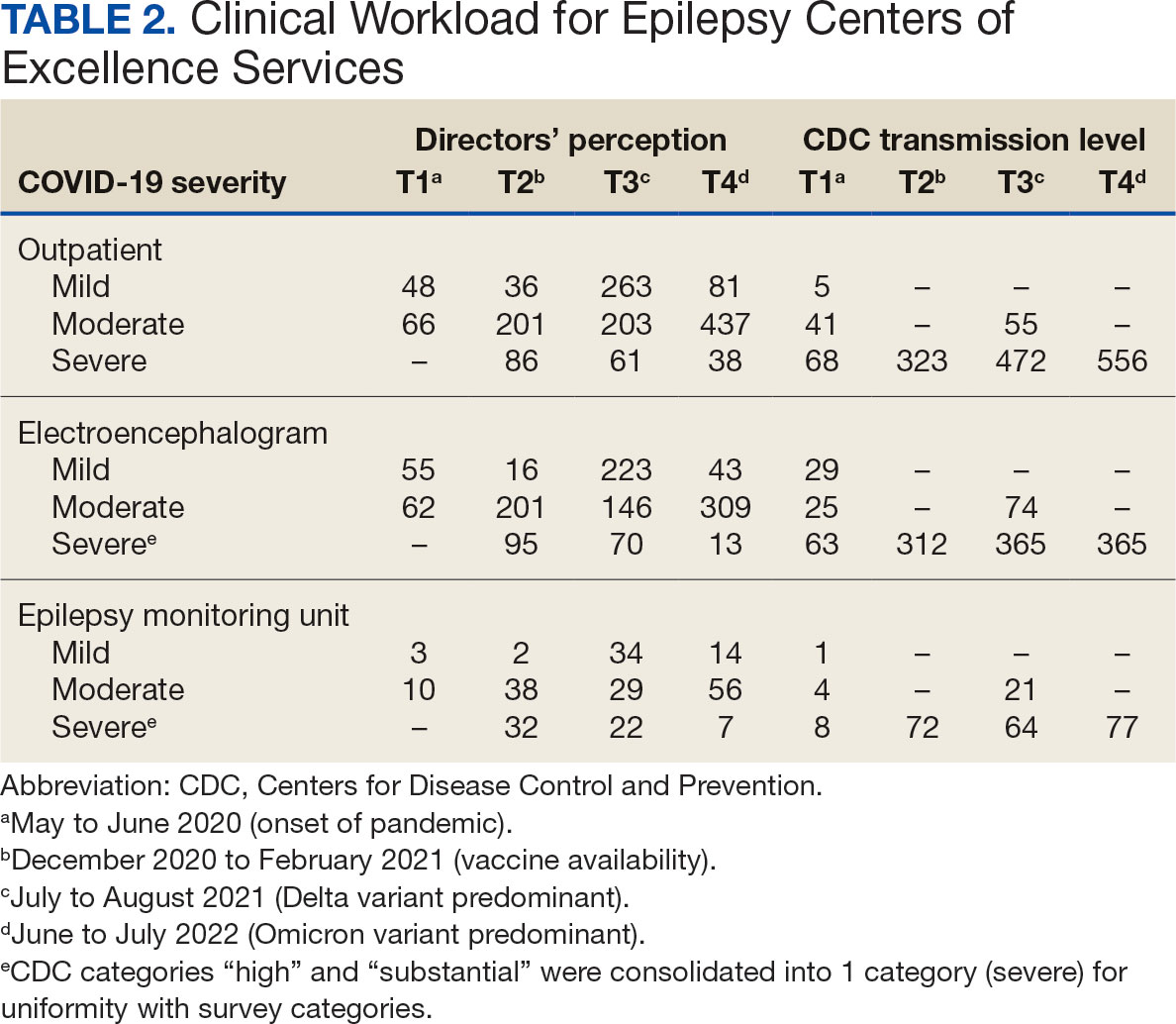
Data on the spread of COVID-19 were collected from the CDC archived dataset, US COVID-19 County Level of Community Transmission Historical Changes (Table 1).7 Administrative workload (patient counts) for EEG, EMU, and outpatient clinics were extracted from VHA administrative databases for the participating sites for the months prior to each survey: T1, April 2020; T2, November 2020; T3, June 2021; and T4, May 2022 (Table 2).
Survey Structure and Content
The survey was developed by the ECoE and was not validated prior to its use due to the time-sensitive nature of gathering information during the pandemic. The first survey (T1) was an emailed spreadsheet with open-ended questions to gauge availability of services (ie, outpatient clinic, EEG, EMU), assess whether safety precautions were being introduced, and understand whether national or local guidelines were thought to be helpful. Responses from this and subsequent surveys were standardized into yes/no and multiple choice formats. Subsequent surveys were administered online using a Research Electronic Data Capture tool.8,9
Availability of outpatient epilepsy services across the 4 time periods were categorized as unlimited (in-person with no restrictions), limited (in-person with restrictions), planned (not currently performed but scheduled for the near future), and unavailable (no in-person services offered) (eAppendices 1-6, available in article PDF).
Statistical Analyses
Analyses were performed to compare survey responses to workload and CDC data on COVID-19 community spread. The following associations were examined: (1) CDC COVID-19 spread vs respondents’ perception of spread; (2) respondents’ perception of spread vs availability of services; (3) CDC COVID-19 spread vs availability of services; (4) respondents’ perception of spread vs workload; and (5) CDC COVID-19 spread vs workload. Availability of services was dichotomized for analyses, with limited or fully available services classified as available. As services were mostly open at T3 regardless of the spread of the virus, and the CDC COVID-19 spread classification for all sites was severe or high at T2 and T4, corresponding associations were not tested at these time points. For associations 1 through 3, Fisher exact tests were used; for associations 4 and 5, Mann-Whitney U tests (where the COVID-19 spread fell into 2 categories) and Kruskal-Wallis tests (for 3 categories of COVID-19 spread) were performed. All tests were 2-tailed and performed at 0.05 error rate. Bonferroni corrections were applied to adjust P values for multiple hypotheses tests.
RESULTS
From the 17 sites invited, responses at each time point were obtained from 13 (T1),17 (T2), 15 (T3), and 16 (T4) centers. There was no significant association between self-reported COVID-19 spread and CDC classification of COVID spread. There were no associations between COVID-19 community spread (respondent reported or CDC severity level) and outpatient clinic availability (self-reported or workload captured). At T3, a positive association was found between the CDC spread level and workload (P = .008), but this was not significant after Bonferroni correction (P = .06).
EEG availability surpassed EMU availability at all time points, although EMU services made some recovery at T3 and T4. No associations were found between COVID-19 community spread (self-reported or CDC severity level) and outpatient EEG or EMU availability (self-reported or workload captured). At T3, there was a positive association between EEG workload and CDC COVID-19 severity level (P = .04), but this was not significant after Bonferroni correction (P = .30).
For outpatient EEG, staff and patient mask use were universally implemented by T2, while the use of full personal protective equipment (PPE) occurred at a subset of sites (T2, 6/17 [35%]; T3, 3/15 [20%]; T4: 4/16 [25%]). COVID-19 testing was rarely implemented prior to outpatient EEG (T1, 0 sites; T2, 1 site; T3, 1 site; T4, 0 sites). Within the EMU, safety precautions including COVID-19 testing, patient mask usage, staff mask usage, and aerosolization demonstrated a sustained majority usage across the 4 surveys.
National and Local Guidelines
The open-ended survey at T1 asked site directors, “Should there be national recommendations on how EEGs and related procedures should be done during the pandemic or should this be left to local conditions?” Responses were mixed, with 5 respondents desiring a national standard, 4 respondents favoring a local response, and 4 respondents believing a national standard should be in place but with modifications based on local outbreak levels and needs.
Surveys performed at T2 through T4 asked, “Which of the following do you feel was/will be helpful in adapting to COVID-19–related changes?” Overall, there was substantial agreement that guidelines were helpful. Most sites anticipated permanent changes in enhanced safety precautions and telehealth.
DISCUSSION
This longitudinal study across 4 time points describes how epilepsy services within the VHA and ECoE adapted to the COVID-19 pandemic. The first survey, conducted 2 months after COVID-19 was declared a pandemic, allowed a comparison with other concurrent US national surveys.1,2,10 The subsequent surveys describe longitudinal adaptations to balance patient and staff safety with service availability and is a unique feature of the current report. Results demonstrate flexibility and adaptability by the ECoEs surveyed, which surprisingly did not show significant associations between CDC COVID-19 spread data and administrative workload data.
Trends in Availability of Services
The most significant impact of COVID-19 restrictions was during T1. There were no significant relationships between service availability/workload and objective CDC COVID-19 spread levels or subjective self-reported COVID-19 spread. Respondents’ perceptions of local COVID-19 spread showed no association with CDC COVID-19 spread data. It appears that subjective perception of spread may be unreliable and factors other than actual or perceived COVID-19 spread were likely driving patterns for service availability.
In-person outpatient visits were most impacted at T1, similar to other civilian surveys, with only 1 site reporting in-person outpatient visits without limitations.1,2 These numbers significantly changed by T2, with all sites offering either limited or unlimited in-person visits. While the surveys did not evaluate factors leading to this rapid recovery, it may be related to the availability of COVID-19 vaccinations within the VHA during this time.11 The US Department of Veterans Affairs was the first federal agency to mandate employee vaccination.12 By the most recent time point (T4), all responding sites offered outpatient visits. Outpatient EEGs followed a similar trend, with T1 being the most restrictive and full, unrestricted outpatient EEGs available by T3.
Fiscal year (FY) trends from ECoE annual reports suggest that encounters slowly recovered over the course of the pandemic. In FY 2019 there were 13,143 outpatient encounters and 6394 EEGs, which dropped to 8097 outpatient encounters and 4432 EEGs in FY 2020 before rising to 8489 outpatient encounters and 5604 EEGs in FY 2021 and 9772 outpatient encounters and 5062 EEGs in FY 2022. Thus, while clinicians described availability of services, patients may have remained hesitant or were otherwise unable to fulfill in-person appointments. The increased availability of home EEG (145 encounter days in 2021 and 436 encounter days in 2022) may be filling this gap.
In contrast to outpatient clinics and EEG, EMU availability showed relatively slower reimplementation. In the last survey, about 30% of sites were still not offering EMU or had limited services. Early trends regarding reduced staffing and patient reluctance for elective admission cited in other surveys may have also affected EMU availability within the VHA.2,13 Consistent with trends in availability, ECoE annual report data suggest EMU patient participation was about one-half of prepandemic rates: 3069 encounters in FY 2019 dropped to 1614 encounters in 2020. By 2021, rates were about two-thirds of prepandemic rates with 2058 encounters in 2021 and 2101 encounters in 2022.
Early survey results (T1) from this study echo trends from other surveys. In the AES survey (April to June 2020), about a quarter of respondents (22%) reported doing fewer EEG studies than usual. The Italian national survey (April 2020) revealed reduced presurgical evaluations (81%), ambulatory EEG (78%), standard EEG (5%) and long-term EEG (32%).4 In the NAEC survey (end of 2020)—which roughly corresponded to T2—outpatient EEGs were still < 75% of pre-COVID levels in one-half of the centers.
National and Local Guidelines
Both national and local guidelines were perceived as useful by most respondents, with national guidelines being more beneficial. This aligns with the NAEC survey, where there was a perceived need for detailed recommendations for PPE and COVID-19 testing of patients, visitors, and staff. Based on national and local guidelines, ECoE implemented safety procedures, as reflected in responses. Staff masking procedures appeared to be the most widely adopted for all services, while the use of full PPE waned as the pandemic progressed. COVID-19 testing was rarely used for routine outpatient visits but common in EMU admissions. This is similar to a survey conducted by the American Academy of Neurology which found full PPE implementation intermittently in outpatient settings and more frequently in inpatient settings.14
Telehealth Attitudes
While most sites anticipated permanent implementation of safety precautions and telehealth, the latter was consistently reported as more likely to be sustained. The VHA had a large and well-developed system of telehealth services that considerably predated the pandemic.15,16 Through this established infrastructure, remote services were quickly increased across the VHA.17-19 This telehealth structure was supplemented by the ability of VHA clinicians to practice across state lines, following a 2018 federal rule.20 The AES survey noted the VHA ECoE's longstanding experience with telehealth as a model for telemedicine use in providing direct patient care, remote EEG analysis, and clinician-to-clinician consultation.1
Trends in the number of telehealth patients seen, observed through patterns in ECoE annual reports are consistent with positive views toward this method of service provision. Specifically, these annual reports capture trends in Video Telehealth Clinic (local station), Video Telehealth Clinic (different station), Home Video Telehealth, Telephone Clinic, and eConsults. Though video telehealth at in-person stations had a precipitous drop in 2020 that continued to wane in subsequent years (898 encounters in 2019; 455 encounters in 2020; 90 encounters in 2021; 88 encounters in 2022), use of home video telehealth rose over time (143 encounters in 2019; 1003 encounters in 2020; 3206 encounters in 2021; 3315 encounters in 2022). Use of telephone services rose drastically in 2020 but has since become a less frequently used service method (2636 in 2019; 5923 in 2020; 5319 in 2021; 3704 in 2022).
Limitations
While the survey encouraged a high response rate, this limited its scope and interpretability. While the availability of services was evaluated, the underlying reasons were not queried. Follow-up questions about barriers to reopening may have allowed for a better understanding of why some services, such as EMU, continued to operate suboptimally later in the pandemic. Similarly, asking about unique strategies or barriers for telehealth would have allowed for a better understanding of its current and future use. We hypothesize that staffing changes during the pandemic may have influenced the availability of services, but changes to staffing were not assessed via the survey and were not readily available via other sources (eg, ECoE annual reports) at the time of publication. An additional limitation is the lack of comparable surveys in the literature for time points T2 to T4, as most analogous surveys were performed early in 2020.
Conclusions
This longitudinal study performed at 4 time points during the COVID-19 pandemic is the first to offer a comprehensive picture of changes to epilepsy and EEG services over time, given that other similar surveys lacked follow-up. Results reveal a significant limitation of services at VHA ECoE shortly after the onset of the pandemic, with return to near-complete operational status 2 years later. While safety precautions and telehealth are predicted to continue, telehealth is perceived as a more permanent change in services.
Albert DVF, Das RR, Acharya JN, et al. The impact of COVID-19 on epilepsy care: a survey of the American Epilepsy Society membership. Epilepsy Curr. 2020;20(5):316-324. doi:10.1177/1535759720956994
Ahrens SM, Ostendorf AP, Lado FA, et al. Impact of the COVID-19 pandemic on epilepsy center practice in the United States. Neurology. 2022;98(19):e1893-e1901. doi:10.1212/WNL.0000000000200285
Cross JH, Kwon CS, Asadi-Pooya AA, et al. Epilepsy care during the COVID-19 pandemic. Epilepsia. 2021;62(10):2322-2332. doi:10.1111/epi.17045
Assenza G, Lanzone J, Ricci L, et al. Electroencephalography at the time of Covid-19 pandemic in Italy. Neurol Sci. 2020;41(8):1999-2004. doi:10.1007/s10072-020-04546-8
US Department of Veterans Affairs. National Center for Veterans Analysis and Statistics. Veteran population. Updated September 7, 2022. Accessed October 25, 2024. https://www.va.gov/vetdata/veteran_population.asp
US Department of Veterans Affairs, Veterans Health Administration. Epilepsy Centers of Excellence (ECoE). Annual report fiscal year 2019. Accessed October 25, 2024. https://www.epilepsy.va.gov/docs/FY19AnnualReport-VHAEpilepsyCentersofExcellence.pdf
Centers for Disease Control and Prevention. United States COVID-19 county level of community transmission historical changes – ARCHIVED. Updated February 20, 2024. Accessed October 25, 2024. https://data.cdc.gov/Public-Health-Surveillance/United-States-COVID-19-County-Level-of-Community-T/nra9-vzzn
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
World Health Organization. Rolling updates on coronavirus disease (COVID-19). Updated July 31, 2020. Accessed October 25, 2024. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
US Department of Veterans Affairs. VA announces initial plans for COVID-19 vaccine distribution. News release. December 10, 2020. Accessed October 25, 2024. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5580
Steinhauer J. V.A. Issues Vaccine Mandate for Health Care Workers, a First for a Federal Agency. The New York Times. August 16, 2021. Accessed October 25, 2024. https://www.nytimes.com/2021/07/26/us/politics/veterans-affairs-coronavirus-covid-19.html
Zafar SF, Khozein RJ, LaRoche SM, Westover MB, Gilmore EJ. Impact of the COVID-19 pandemic on continuous EEG utilization. J Clin Neurophysiol. 2022;39(7):567-574. doi:10.1097/WNP.0000000000000802
Qureshi AI, Rheaume C, Huang W, et al. COVID-19 exposure during neurology practice. Neurologist. 2021;26(6):225-230. doi:10.1097/NRL.0000000000000346
Darkins A, Cruise C, Armstrong M, Peters J, Finn M. Enhancing access of combat-wounded veterans to specialist rehabilitation services: the VA Polytrauma Telehealth Network. Arch Phys Med Rehabil. 2008;89(1):182-187. doi:10.1016/j.apmr.2007.07.027
Darkins A, Ryan P, Kobb R, et al. Care coordination/home telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health. 2008;14(10):1118-1126. doi:10.1089/tmj.2008.0021
Gentry MT, Puspitasari AJ, McKean AJ, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E Health. 2021;27(12):1385-1392. doi:10.1089/tmj.2020.0575
Connolly SL, Stolzmann KL, Heyworth L, et al. Patient and provider predictors of telemental health use prior to and during the COVID-19 pandemic within the Department of Veterans Affairs. Am Psychol. 2022;77(2):249-261. doi:10.1037/amp0000895
Shelton CJ, Kim A, Hassan AM, Bhat A, Barnello J, Castro CA. System-wide implementation of telehealth to support military veterans and their families in response to COVID-19: a paradigm shift. J Mil Veteran Fam Health. 2020;6(S2):50-57. doi:10.3138/jmvfh-CO19-0003
VA expands telehealth by allowing health care providers to treat patients across state lines. News release. US Dept of Veterans Affairs. May 11, 2018. Accessed October 25, 2024. https://news.va.gov/press-room/va-expands-telehealth-by-allowing-health-care-providers-to-treat-patients-across-state-lines/
The COVID-19 pandemic affected diverse workplaces globally, leading to temporary and permanent changes across the health care landscape. Included among the impacted areas of care were epilepsy and electroencephalogram (EEG) clinicians and services. Surveys among epilepsy specialists and neurophysiologists conducted at the onset of the pandemic to evaluate working conditions include analyses from the American Epilepsy Society (AES), the National Association of Epilepsy Centers (NAEC), the International League Against Epilepsy, and an Italian national survey.1-4 These investigations revealed reductions in epilepsy monitoring unit (EMU) admissions (23% decline), epilepsy surgery (6% decline), inpatient EEG (22% of respondents reported decline), and patients having difficulty accessing epilepsy professionals (28% of respondents reported decline) or obtaining medications (20% of respondents reported decline).1-3
While such research provided evidence for changes to epilepsy care in 2020, there are limited data on subsequent adaptations during the pandemic. These studies did not incorporate data on the spread of COVID-19 or administrative workload numbers to analyze service delivery beyond self reports. This study aimed to address this gap in the literature by highlighting results from longitudinal national surveys conducted at the Epilepsy Centers of Excellence (ECoE), a specialty care service within the Veterans Health Administration (VHA), which annually serves > 9 million veterans.5 The ECoE represents epileptologists and neurophysiologists across the United States at the 17 primary facilities that were established at the time of this survey (2 ECoEs have been added since survey completion) in 4 geographical regions and for which other regional facilities refer patients for diagnostic services or specialty care.6
National surveys were conducted among the ECoE directors regarding adaptations made from May 2020 to June 2022 to provide a comprehensive account of limitations they experienced and how adjustments have been made to improve patient care. Survey responses were compared to administrative workload numbers and COVID-19 spread data from the Centers for Disease Control and Prevention (CDC) to provide a comprehensive analysis of performance during the pandemic.
METHODS
Data were collected as part of a quality improvement initiative by the VHA ECoE; institutional review board approval was not required. An 18-item survey covering 5 broad domains was sent to ECoE directors 4 separate times to accumulate data from 4 time periods: May to June 2020 (T1); December 2020 to February 2021 (T2); July to August 2021 (T3); and June to July 2022 (T4). These periods correspond to the following phases of the pandemic: T1, onset of pandemic; T2, vaccine availability; T3, Delta variant predominant; T4, Omicron variant predominant.
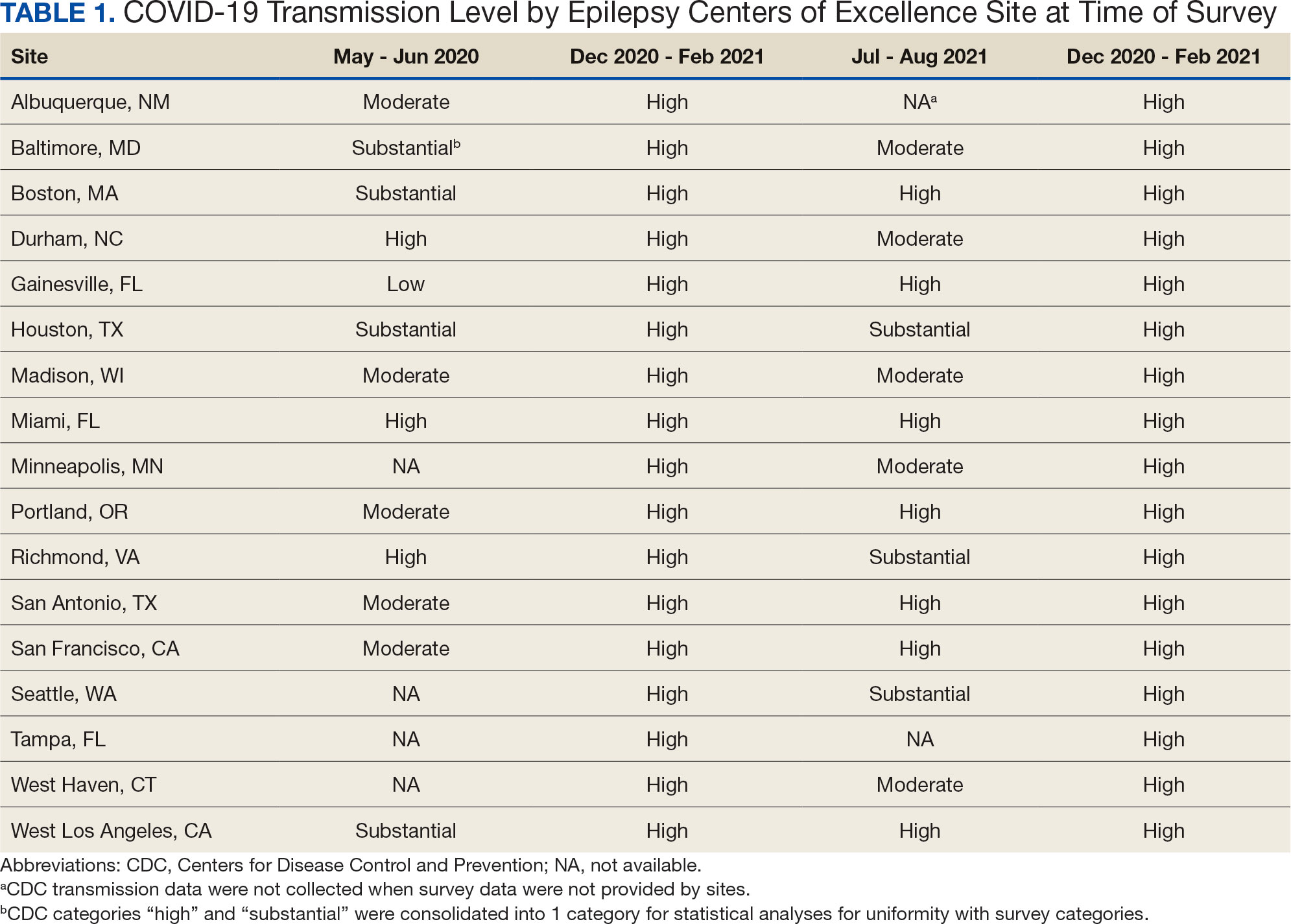
Data on the spread of COVID-19 were collected from the CDC archived dataset, US COVID-19 County Level of Community Transmission Historical Changes (Table 1).7 Administrative workload (patient counts) for EEG, EMU, and outpatient clinics were extracted from VHA administrative databases for the participating sites for the months prior to each survey: T1, April 2020; T2, November 2020; T3, June 2021; and T4, May 2022 (Table 2).
Survey Structure and Content
The survey was developed by the ECoE and was not validated prior to its use due to the time-sensitive nature of gathering information during the pandemic. The first survey (T1) was an emailed spreadsheet with open-ended questions to gauge availability of services (ie, outpatient clinic, EEG, EMU), assess whether safety precautions were being introduced, and understand whether national or local guidelines were thought to be helpful. Responses from this and subsequent surveys were standardized into yes/no and multiple choice formats. Subsequent surveys were administered online using a Research Electronic Data Capture tool.8,9
Availability of outpatient epilepsy services across the 4 time periods were categorized as unlimited (in-person with no restrictions), limited (in-person with restrictions), planned (not currently performed but scheduled for the near future), and unavailable (no in-person services offered) (eAppendices 1-6, available in article PDF).
Statistical Analyses
Analyses were performed to compare survey responses to workload and CDC data on COVID-19 community spread. The following associations were examined: (1) CDC COVID-19 spread vs respondents’ perception of spread; (2) respondents’ perception of spread vs availability of services; (3) CDC COVID-19 spread vs availability of services; (4) respondents’ perception of spread vs workload; and (5) CDC COVID-19 spread vs workload. Availability of services was dichotomized for analyses, with limited or fully available services classified as available. As services were mostly open at T3 regardless of the spread of the virus, and the CDC COVID-19 spread classification for all sites was severe or high at T2 and T4, corresponding associations were not tested at these time points. For associations 1 through 3, Fisher exact tests were used; for associations 4 and 5, Mann-Whitney U tests (where the COVID-19 spread fell into 2 categories) and Kruskal-Wallis tests (for 3 categories of COVID-19 spread) were performed. All tests were 2-tailed and performed at 0.05 error rate. Bonferroni corrections were applied to adjust P values for multiple hypotheses tests.
RESULTS
From the 17 sites invited, responses at each time point were obtained from 13 (T1),17 (T2), 15 (T3), and 16 (T4) centers. There was no significant association between self-reported COVID-19 spread and CDC classification of COVID spread. There were no associations between COVID-19 community spread (respondent reported or CDC severity level) and outpatient clinic availability (self-reported or workload captured). At T3, a positive association was found between the CDC spread level and workload (P = .008), but this was not significant after Bonferroni correction (P = .06).
EEG availability surpassed EMU availability at all time points, although EMU services made some recovery at T3 and T4. No associations were found between COVID-19 community spread (self-reported or CDC severity level) and outpatient EEG or EMU availability (self-reported or workload captured). At T3, there was a positive association between EEG workload and CDC COVID-19 severity level (P = .04), but this was not significant after Bonferroni correction (P = .30).
For outpatient EEG, staff and patient mask use were universally implemented by T2, while the use of full personal protective equipment (PPE) occurred at a subset of sites (T2, 6/17 [35%]; T3, 3/15 [20%]; T4: 4/16 [25%]). COVID-19 testing was rarely implemented prior to outpatient EEG (T1, 0 sites; T2, 1 site; T3, 1 site; T4, 0 sites). Within the EMU, safety precautions including COVID-19 testing, patient mask usage, staff mask usage, and aerosolization demonstrated a sustained majority usage across the 4 surveys.
National and Local Guidelines
The open-ended survey at T1 asked site directors, “Should there be national recommendations on how EEGs and related procedures should be done during the pandemic or should this be left to local conditions?” Responses were mixed, with 5 respondents desiring a national standard, 4 respondents favoring a local response, and 4 respondents believing a national standard should be in place but with modifications based on local outbreak levels and needs.
Surveys performed at T2 through T4 asked, “Which of the following do you feel was/will be helpful in adapting to COVID-19–related changes?” Overall, there was substantial agreement that guidelines were helpful. Most sites anticipated permanent changes in enhanced safety precautions and telehealth.
DISCUSSION
This longitudinal study across 4 time points describes how epilepsy services within the VHA and ECoE adapted to the COVID-19 pandemic. The first survey, conducted 2 months after COVID-19 was declared a pandemic, allowed a comparison with other concurrent US national surveys.1,2,10 The subsequent surveys describe longitudinal adaptations to balance patient and staff safety with service availability and is a unique feature of the current report. Results demonstrate flexibility and adaptability by the ECoEs surveyed, which surprisingly did not show significant associations between CDC COVID-19 spread data and administrative workload data.
Trends in Availability of Services
The most significant impact of COVID-19 restrictions was during T1. There were no significant relationships between service availability/workload and objective CDC COVID-19 spread levels or subjective self-reported COVID-19 spread. Respondents’ perceptions of local COVID-19 spread showed no association with CDC COVID-19 spread data. It appears that subjective perception of spread may be unreliable and factors other than actual or perceived COVID-19 spread were likely driving patterns for service availability.
In-person outpatient visits were most impacted at T1, similar to other civilian surveys, with only 1 site reporting in-person outpatient visits without limitations.1,2 These numbers significantly changed by T2, with all sites offering either limited or unlimited in-person visits. While the surveys did not evaluate factors leading to this rapid recovery, it may be related to the availability of COVID-19 vaccinations within the VHA during this time.11 The US Department of Veterans Affairs was the first federal agency to mandate employee vaccination.12 By the most recent time point (T4), all responding sites offered outpatient visits. Outpatient EEGs followed a similar trend, with T1 being the most restrictive and full, unrestricted outpatient EEGs available by T3.
Fiscal year (FY) trends from ECoE annual reports suggest that encounters slowly recovered over the course of the pandemic. In FY 2019 there were 13,143 outpatient encounters and 6394 EEGs, which dropped to 8097 outpatient encounters and 4432 EEGs in FY 2020 before rising to 8489 outpatient encounters and 5604 EEGs in FY 2021 and 9772 outpatient encounters and 5062 EEGs in FY 2022. Thus, while clinicians described availability of services, patients may have remained hesitant or were otherwise unable to fulfill in-person appointments. The increased availability of home EEG (145 encounter days in 2021 and 436 encounter days in 2022) may be filling this gap.
In contrast to outpatient clinics and EEG, EMU availability showed relatively slower reimplementation. In the last survey, about 30% of sites were still not offering EMU or had limited services. Early trends regarding reduced staffing and patient reluctance for elective admission cited in other surveys may have also affected EMU availability within the VHA.2,13 Consistent with trends in availability, ECoE annual report data suggest EMU patient participation was about one-half of prepandemic rates: 3069 encounters in FY 2019 dropped to 1614 encounters in 2020. By 2021, rates were about two-thirds of prepandemic rates with 2058 encounters in 2021 and 2101 encounters in 2022.
Early survey results (T1) from this study echo trends from other surveys. In the AES survey (April to June 2020), about a quarter of respondents (22%) reported doing fewer EEG studies than usual. The Italian national survey (April 2020) revealed reduced presurgical evaluations (81%), ambulatory EEG (78%), standard EEG (5%) and long-term EEG (32%).4 In the NAEC survey (end of 2020)—which roughly corresponded to T2—outpatient EEGs were still < 75% of pre-COVID levels in one-half of the centers.
National and Local Guidelines
Both national and local guidelines were perceived as useful by most respondents, with national guidelines being more beneficial. This aligns with the NAEC survey, where there was a perceived need for detailed recommendations for PPE and COVID-19 testing of patients, visitors, and staff. Based on national and local guidelines, ECoE implemented safety procedures, as reflected in responses. Staff masking procedures appeared to be the most widely adopted for all services, while the use of full PPE waned as the pandemic progressed. COVID-19 testing was rarely used for routine outpatient visits but common in EMU admissions. This is similar to a survey conducted by the American Academy of Neurology which found full PPE implementation intermittently in outpatient settings and more frequently in inpatient settings.14
Telehealth Attitudes
While most sites anticipated permanent implementation of safety precautions and telehealth, the latter was consistently reported as more likely to be sustained. The VHA had a large and well-developed system of telehealth services that considerably predated the pandemic.15,16 Through this established infrastructure, remote services were quickly increased across the VHA.17-19 This telehealth structure was supplemented by the ability of VHA clinicians to practice across state lines, following a 2018 federal rule.20 The AES survey noted the VHA ECoE's longstanding experience with telehealth as a model for telemedicine use in providing direct patient care, remote EEG analysis, and clinician-to-clinician consultation.1
Trends in the number of telehealth patients seen, observed through patterns in ECoE annual reports are consistent with positive views toward this method of service provision. Specifically, these annual reports capture trends in Video Telehealth Clinic (local station), Video Telehealth Clinic (different station), Home Video Telehealth, Telephone Clinic, and eConsults. Though video telehealth at in-person stations had a precipitous drop in 2020 that continued to wane in subsequent years (898 encounters in 2019; 455 encounters in 2020; 90 encounters in 2021; 88 encounters in 2022), use of home video telehealth rose over time (143 encounters in 2019; 1003 encounters in 2020; 3206 encounters in 2021; 3315 encounters in 2022). Use of telephone services rose drastically in 2020 but has since become a less frequently used service method (2636 in 2019; 5923 in 2020; 5319 in 2021; 3704 in 2022).
Limitations
While the survey encouraged a high response rate, this limited its scope and interpretability. While the availability of services was evaluated, the underlying reasons were not queried. Follow-up questions about barriers to reopening may have allowed for a better understanding of why some services, such as EMU, continued to operate suboptimally later in the pandemic. Similarly, asking about unique strategies or barriers for telehealth would have allowed for a better understanding of its current and future use. We hypothesize that staffing changes during the pandemic may have influenced the availability of services, but changes to staffing were not assessed via the survey and were not readily available via other sources (eg, ECoE annual reports) at the time of publication. An additional limitation is the lack of comparable surveys in the literature for time points T2 to T4, as most analogous surveys were performed early in 2020.
Conclusions
This longitudinal study performed at 4 time points during the COVID-19 pandemic is the first to offer a comprehensive picture of changes to epilepsy and EEG services over time, given that other similar surveys lacked follow-up. Results reveal a significant limitation of services at VHA ECoE shortly after the onset of the pandemic, with return to near-complete operational status 2 years later. While safety precautions and telehealth are predicted to continue, telehealth is perceived as a more permanent change in services.
The COVID-19 pandemic affected diverse workplaces globally, leading to temporary and permanent changes across the health care landscape. Included among the impacted areas of care were epilepsy and electroencephalogram (EEG) clinicians and services. Surveys among epilepsy specialists and neurophysiologists conducted at the onset of the pandemic to evaluate working conditions include analyses from the American Epilepsy Society (AES), the National Association of Epilepsy Centers (NAEC), the International League Against Epilepsy, and an Italian national survey.1-4 These investigations revealed reductions in epilepsy monitoring unit (EMU) admissions (23% decline), epilepsy surgery (6% decline), inpatient EEG (22% of respondents reported decline), and patients having difficulty accessing epilepsy professionals (28% of respondents reported decline) or obtaining medications (20% of respondents reported decline).1-3
While such research provided evidence for changes to epilepsy care in 2020, there are limited data on subsequent adaptations during the pandemic. These studies did not incorporate data on the spread of COVID-19 or administrative workload numbers to analyze service delivery beyond self reports. This study aimed to address this gap in the literature by highlighting results from longitudinal national surveys conducted at the Epilepsy Centers of Excellence (ECoE), a specialty care service within the Veterans Health Administration (VHA), which annually serves > 9 million veterans.5 The ECoE represents epileptologists and neurophysiologists across the United States at the 17 primary facilities that were established at the time of this survey (2 ECoEs have been added since survey completion) in 4 geographical regions and for which other regional facilities refer patients for diagnostic services or specialty care.6
National surveys were conducted among the ECoE directors regarding adaptations made from May 2020 to June 2022 to provide a comprehensive account of limitations they experienced and how adjustments have been made to improve patient care. Survey responses were compared to administrative workload numbers and COVID-19 spread data from the Centers for Disease Control and Prevention (CDC) to provide a comprehensive analysis of performance during the pandemic.
METHODS
Data were collected as part of a quality improvement initiative by the VHA ECoE; institutional review board approval was not required. An 18-item survey covering 5 broad domains was sent to ECoE directors 4 separate times to accumulate data from 4 time periods: May to June 2020 (T1); December 2020 to February 2021 (T2); July to August 2021 (T3); and June to July 2022 (T4). These periods correspond to the following phases of the pandemic: T1, onset of pandemic; T2, vaccine availability; T3, Delta variant predominant; T4, Omicron variant predominant.
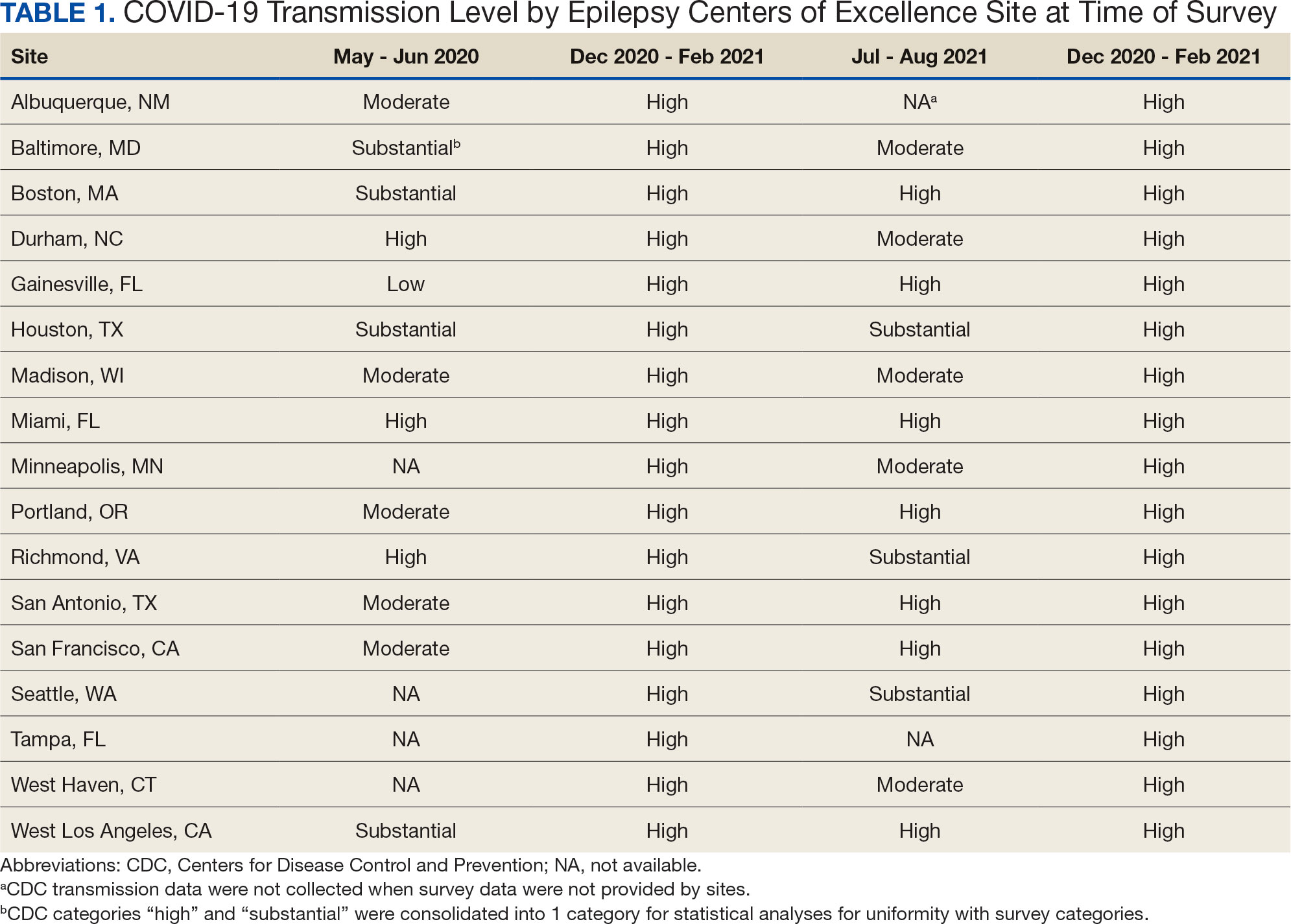
Data on the spread of COVID-19 were collected from the CDC archived dataset, US COVID-19 County Level of Community Transmission Historical Changes (Table 1).7 Administrative workload (patient counts) for EEG, EMU, and outpatient clinics were extracted from VHA administrative databases for the participating sites for the months prior to each survey: T1, April 2020; T2, November 2020; T3, June 2021; and T4, May 2022 (Table 2).
Survey Structure and Content
The survey was developed by the ECoE and was not validated prior to its use due to the time-sensitive nature of gathering information during the pandemic. The first survey (T1) was an emailed spreadsheet with open-ended questions to gauge availability of services (ie, outpatient clinic, EEG, EMU), assess whether safety precautions were being introduced, and understand whether national or local guidelines were thought to be helpful. Responses from this and subsequent surveys were standardized into yes/no and multiple choice formats. Subsequent surveys were administered online using a Research Electronic Data Capture tool.8,9
Availability of outpatient epilepsy services across the 4 time periods were categorized as unlimited (in-person with no restrictions), limited (in-person with restrictions), planned (not currently performed but scheduled for the near future), and unavailable (no in-person services offered) (eAppendices 1-6, available in article PDF).
Statistical Analyses
Analyses were performed to compare survey responses to workload and CDC data on COVID-19 community spread. The following associations were examined: (1) CDC COVID-19 spread vs respondents’ perception of spread; (2) respondents’ perception of spread vs availability of services; (3) CDC COVID-19 spread vs availability of services; (4) respondents’ perception of spread vs workload; and (5) CDC COVID-19 spread vs workload. Availability of services was dichotomized for analyses, with limited or fully available services classified as available. As services were mostly open at T3 regardless of the spread of the virus, and the CDC COVID-19 spread classification for all sites was severe or high at T2 and T4, corresponding associations were not tested at these time points. For associations 1 through 3, Fisher exact tests were used; for associations 4 and 5, Mann-Whitney U tests (where the COVID-19 spread fell into 2 categories) and Kruskal-Wallis tests (for 3 categories of COVID-19 spread) were performed. All tests were 2-tailed and performed at 0.05 error rate. Bonferroni corrections were applied to adjust P values for multiple hypotheses tests.
RESULTS
From the 17 sites invited, responses at each time point were obtained from 13 (T1),17 (T2), 15 (T3), and 16 (T4) centers. There was no significant association between self-reported COVID-19 spread and CDC classification of COVID spread. There were no associations between COVID-19 community spread (respondent reported or CDC severity level) and outpatient clinic availability (self-reported or workload captured). At T3, a positive association was found between the CDC spread level and workload (P = .008), but this was not significant after Bonferroni correction (P = .06).
EEG availability surpassed EMU availability at all time points, although EMU services made some recovery at T3 and T4. No associations were found between COVID-19 community spread (self-reported or CDC severity level) and outpatient EEG or EMU availability (self-reported or workload captured). At T3, there was a positive association between EEG workload and CDC COVID-19 severity level (P = .04), but this was not significant after Bonferroni correction (P = .30).
For outpatient EEG, staff and patient mask use were universally implemented by T2, while the use of full personal protective equipment (PPE) occurred at a subset of sites (T2, 6/17 [35%]; T3, 3/15 [20%]; T4: 4/16 [25%]). COVID-19 testing was rarely implemented prior to outpatient EEG (T1, 0 sites; T2, 1 site; T3, 1 site; T4, 0 sites). Within the EMU, safety precautions including COVID-19 testing, patient mask usage, staff mask usage, and aerosolization demonstrated a sustained majority usage across the 4 surveys.
National and Local Guidelines
The open-ended survey at T1 asked site directors, “Should there be national recommendations on how EEGs and related procedures should be done during the pandemic or should this be left to local conditions?” Responses were mixed, with 5 respondents desiring a national standard, 4 respondents favoring a local response, and 4 respondents believing a national standard should be in place but with modifications based on local outbreak levels and needs.
Surveys performed at T2 through T4 asked, “Which of the following do you feel was/will be helpful in adapting to COVID-19–related changes?” Overall, there was substantial agreement that guidelines were helpful. Most sites anticipated permanent changes in enhanced safety precautions and telehealth.
DISCUSSION
This longitudinal study across 4 time points describes how epilepsy services within the VHA and ECoE adapted to the COVID-19 pandemic. The first survey, conducted 2 months after COVID-19 was declared a pandemic, allowed a comparison with other concurrent US national surveys.1,2,10 The subsequent surveys describe longitudinal adaptations to balance patient and staff safety with service availability and is a unique feature of the current report. Results demonstrate flexibility and adaptability by the ECoEs surveyed, which surprisingly did not show significant associations between CDC COVID-19 spread data and administrative workload data.
Trends in Availability of Services
The most significant impact of COVID-19 restrictions was during T1. There were no significant relationships between service availability/workload and objective CDC COVID-19 spread levels or subjective self-reported COVID-19 spread. Respondents’ perceptions of local COVID-19 spread showed no association with CDC COVID-19 spread data. It appears that subjective perception of spread may be unreliable and factors other than actual or perceived COVID-19 spread were likely driving patterns for service availability.
In-person outpatient visits were most impacted at T1, similar to other civilian surveys, with only 1 site reporting in-person outpatient visits without limitations.1,2 These numbers significantly changed by T2, with all sites offering either limited or unlimited in-person visits. While the surveys did not evaluate factors leading to this rapid recovery, it may be related to the availability of COVID-19 vaccinations within the VHA during this time.11 The US Department of Veterans Affairs was the first federal agency to mandate employee vaccination.12 By the most recent time point (T4), all responding sites offered outpatient visits. Outpatient EEGs followed a similar trend, with T1 being the most restrictive and full, unrestricted outpatient EEGs available by T3.
Fiscal year (FY) trends from ECoE annual reports suggest that encounters slowly recovered over the course of the pandemic. In FY 2019 there were 13,143 outpatient encounters and 6394 EEGs, which dropped to 8097 outpatient encounters and 4432 EEGs in FY 2020 before rising to 8489 outpatient encounters and 5604 EEGs in FY 2021 and 9772 outpatient encounters and 5062 EEGs in FY 2022. Thus, while clinicians described availability of services, patients may have remained hesitant or were otherwise unable to fulfill in-person appointments. The increased availability of home EEG (145 encounter days in 2021 and 436 encounter days in 2022) may be filling this gap.
In contrast to outpatient clinics and EEG, EMU availability showed relatively slower reimplementation. In the last survey, about 30% of sites were still not offering EMU or had limited services. Early trends regarding reduced staffing and patient reluctance for elective admission cited in other surveys may have also affected EMU availability within the VHA.2,13 Consistent with trends in availability, ECoE annual report data suggest EMU patient participation was about one-half of prepandemic rates: 3069 encounters in FY 2019 dropped to 1614 encounters in 2020. By 2021, rates were about two-thirds of prepandemic rates with 2058 encounters in 2021 and 2101 encounters in 2022.
Early survey results (T1) from this study echo trends from other surveys. In the AES survey (April to June 2020), about a quarter of respondents (22%) reported doing fewer EEG studies than usual. The Italian national survey (April 2020) revealed reduced presurgical evaluations (81%), ambulatory EEG (78%), standard EEG (5%) and long-term EEG (32%).4 In the NAEC survey (end of 2020)—which roughly corresponded to T2—outpatient EEGs were still < 75% of pre-COVID levels in one-half of the centers.
National and Local Guidelines
Both national and local guidelines were perceived as useful by most respondents, with national guidelines being more beneficial. This aligns with the NAEC survey, where there was a perceived need for detailed recommendations for PPE and COVID-19 testing of patients, visitors, and staff. Based on national and local guidelines, ECoE implemented safety procedures, as reflected in responses. Staff masking procedures appeared to be the most widely adopted for all services, while the use of full PPE waned as the pandemic progressed. COVID-19 testing was rarely used for routine outpatient visits but common in EMU admissions. This is similar to a survey conducted by the American Academy of Neurology which found full PPE implementation intermittently in outpatient settings and more frequently in inpatient settings.14
Telehealth Attitudes
While most sites anticipated permanent implementation of safety precautions and telehealth, the latter was consistently reported as more likely to be sustained. The VHA had a large and well-developed system of telehealth services that considerably predated the pandemic.15,16 Through this established infrastructure, remote services were quickly increased across the VHA.17-19 This telehealth structure was supplemented by the ability of VHA clinicians to practice across state lines, following a 2018 federal rule.20 The AES survey noted the VHA ECoE's longstanding experience with telehealth as a model for telemedicine use in providing direct patient care, remote EEG analysis, and clinician-to-clinician consultation.1
Trends in the number of telehealth patients seen, observed through patterns in ECoE annual reports are consistent with positive views toward this method of service provision. Specifically, these annual reports capture trends in Video Telehealth Clinic (local station), Video Telehealth Clinic (different station), Home Video Telehealth, Telephone Clinic, and eConsults. Though video telehealth at in-person stations had a precipitous drop in 2020 that continued to wane in subsequent years (898 encounters in 2019; 455 encounters in 2020; 90 encounters in 2021; 88 encounters in 2022), use of home video telehealth rose over time (143 encounters in 2019; 1003 encounters in 2020; 3206 encounters in 2021; 3315 encounters in 2022). Use of telephone services rose drastically in 2020 but has since become a less frequently used service method (2636 in 2019; 5923 in 2020; 5319 in 2021; 3704 in 2022).
Limitations
While the survey encouraged a high response rate, this limited its scope and interpretability. While the availability of services was evaluated, the underlying reasons were not queried. Follow-up questions about barriers to reopening may have allowed for a better understanding of why some services, such as EMU, continued to operate suboptimally later in the pandemic. Similarly, asking about unique strategies or barriers for telehealth would have allowed for a better understanding of its current and future use. We hypothesize that staffing changes during the pandemic may have influenced the availability of services, but changes to staffing were not assessed via the survey and were not readily available via other sources (eg, ECoE annual reports) at the time of publication. An additional limitation is the lack of comparable surveys in the literature for time points T2 to T4, as most analogous surveys were performed early in 2020.
Conclusions
This longitudinal study performed at 4 time points during the COVID-19 pandemic is the first to offer a comprehensive picture of changes to epilepsy and EEG services over time, given that other similar surveys lacked follow-up. Results reveal a significant limitation of services at VHA ECoE shortly after the onset of the pandemic, with return to near-complete operational status 2 years later. While safety precautions and telehealth are predicted to continue, telehealth is perceived as a more permanent change in services.
Albert DVF, Das RR, Acharya JN, et al. The impact of COVID-19 on epilepsy care: a survey of the American Epilepsy Society membership. Epilepsy Curr. 2020;20(5):316-324. doi:10.1177/1535759720956994
Ahrens SM, Ostendorf AP, Lado FA, et al. Impact of the COVID-19 pandemic on epilepsy center practice in the United States. Neurology. 2022;98(19):e1893-e1901. doi:10.1212/WNL.0000000000200285
Cross JH, Kwon CS, Asadi-Pooya AA, et al. Epilepsy care during the COVID-19 pandemic. Epilepsia. 2021;62(10):2322-2332. doi:10.1111/epi.17045
Assenza G, Lanzone J, Ricci L, et al. Electroencephalography at the time of Covid-19 pandemic in Italy. Neurol Sci. 2020;41(8):1999-2004. doi:10.1007/s10072-020-04546-8
US Department of Veterans Affairs. National Center for Veterans Analysis and Statistics. Veteran population. Updated September 7, 2022. Accessed October 25, 2024. https://www.va.gov/vetdata/veteran_population.asp
US Department of Veterans Affairs, Veterans Health Administration. Epilepsy Centers of Excellence (ECoE). Annual report fiscal year 2019. Accessed October 25, 2024. https://www.epilepsy.va.gov/docs/FY19AnnualReport-VHAEpilepsyCentersofExcellence.pdf
Centers for Disease Control and Prevention. United States COVID-19 county level of community transmission historical changes – ARCHIVED. Updated February 20, 2024. Accessed October 25, 2024. https://data.cdc.gov/Public-Health-Surveillance/United-States-COVID-19-County-Level-of-Community-T/nra9-vzzn
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
World Health Organization. Rolling updates on coronavirus disease (COVID-19). Updated July 31, 2020. Accessed October 25, 2024. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
US Department of Veterans Affairs. VA announces initial plans for COVID-19 vaccine distribution. News release. December 10, 2020. Accessed October 25, 2024. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5580
Steinhauer J. V.A. Issues Vaccine Mandate for Health Care Workers, a First for a Federal Agency. The New York Times. August 16, 2021. Accessed October 25, 2024. https://www.nytimes.com/2021/07/26/us/politics/veterans-affairs-coronavirus-covid-19.html
Zafar SF, Khozein RJ, LaRoche SM, Westover MB, Gilmore EJ. Impact of the COVID-19 pandemic on continuous EEG utilization. J Clin Neurophysiol. 2022;39(7):567-574. doi:10.1097/WNP.0000000000000802
Qureshi AI, Rheaume C, Huang W, et al. COVID-19 exposure during neurology practice. Neurologist. 2021;26(6):225-230. doi:10.1097/NRL.0000000000000346
Darkins A, Cruise C, Armstrong M, Peters J, Finn M. Enhancing access of combat-wounded veterans to specialist rehabilitation services: the VA Polytrauma Telehealth Network. Arch Phys Med Rehabil. 2008;89(1):182-187. doi:10.1016/j.apmr.2007.07.027
Darkins A, Ryan P, Kobb R, et al. Care coordination/home telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health. 2008;14(10):1118-1126. doi:10.1089/tmj.2008.0021
Gentry MT, Puspitasari AJ, McKean AJ, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E Health. 2021;27(12):1385-1392. doi:10.1089/tmj.2020.0575
Connolly SL, Stolzmann KL, Heyworth L, et al. Patient and provider predictors of telemental health use prior to and during the COVID-19 pandemic within the Department of Veterans Affairs. Am Psychol. 2022;77(2):249-261. doi:10.1037/amp0000895
Shelton CJ, Kim A, Hassan AM, Bhat A, Barnello J, Castro CA. System-wide implementation of telehealth to support military veterans and their families in response to COVID-19: a paradigm shift. J Mil Veteran Fam Health. 2020;6(S2):50-57. doi:10.3138/jmvfh-CO19-0003
VA expands telehealth by allowing health care providers to treat patients across state lines. News release. US Dept of Veterans Affairs. May 11, 2018. Accessed October 25, 2024. https://news.va.gov/press-room/va-expands-telehealth-by-allowing-health-care-providers-to-treat-patients-across-state-lines/
Albert DVF, Das RR, Acharya JN, et al. The impact of COVID-19 on epilepsy care: a survey of the American Epilepsy Society membership. Epilepsy Curr. 2020;20(5):316-324. doi:10.1177/1535759720956994
Ahrens SM, Ostendorf AP, Lado FA, et al. Impact of the COVID-19 pandemic on epilepsy center practice in the United States. Neurology. 2022;98(19):e1893-e1901. doi:10.1212/WNL.0000000000200285
Cross JH, Kwon CS, Asadi-Pooya AA, et al. Epilepsy care during the COVID-19 pandemic. Epilepsia. 2021;62(10):2322-2332. doi:10.1111/epi.17045
Assenza G, Lanzone J, Ricci L, et al. Electroencephalography at the time of Covid-19 pandemic in Italy. Neurol Sci. 2020;41(8):1999-2004. doi:10.1007/s10072-020-04546-8
US Department of Veterans Affairs. National Center for Veterans Analysis and Statistics. Veteran population. Updated September 7, 2022. Accessed October 25, 2024. https://www.va.gov/vetdata/veteran_population.asp
US Department of Veterans Affairs, Veterans Health Administration. Epilepsy Centers of Excellence (ECoE). Annual report fiscal year 2019. Accessed October 25, 2024. https://www.epilepsy.va.gov/docs/FY19AnnualReport-VHAEpilepsyCentersofExcellence.pdf
Centers for Disease Control and Prevention. United States COVID-19 county level of community transmission historical changes – ARCHIVED. Updated February 20, 2024. Accessed October 25, 2024. https://data.cdc.gov/Public-Health-Surveillance/United-States-COVID-19-County-Level-of-Community-T/nra9-vzzn
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
World Health Organization. Rolling updates on coronavirus disease (COVID-19). Updated July 31, 2020. Accessed October 25, 2024. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
US Department of Veterans Affairs. VA announces initial plans for COVID-19 vaccine distribution. News release. December 10, 2020. Accessed October 25, 2024. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5580
Steinhauer J. V.A. Issues Vaccine Mandate for Health Care Workers, a First for a Federal Agency. The New York Times. August 16, 2021. Accessed October 25, 2024. https://www.nytimes.com/2021/07/26/us/politics/veterans-affairs-coronavirus-covid-19.html
Zafar SF, Khozein RJ, LaRoche SM, Westover MB, Gilmore EJ. Impact of the COVID-19 pandemic on continuous EEG utilization. J Clin Neurophysiol. 2022;39(7):567-574. doi:10.1097/WNP.0000000000000802
Qureshi AI, Rheaume C, Huang W, et al. COVID-19 exposure during neurology practice. Neurologist. 2021;26(6):225-230. doi:10.1097/NRL.0000000000000346
Darkins A, Cruise C, Armstrong M, Peters J, Finn M. Enhancing access of combat-wounded veterans to specialist rehabilitation services: the VA Polytrauma Telehealth Network. Arch Phys Med Rehabil. 2008;89(1):182-187. doi:10.1016/j.apmr.2007.07.027
Darkins A, Ryan P, Kobb R, et al. Care coordination/home telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health. 2008;14(10):1118-1126. doi:10.1089/tmj.2008.0021
Gentry MT, Puspitasari AJ, McKean AJ, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E Health. 2021;27(12):1385-1392. doi:10.1089/tmj.2020.0575
Connolly SL, Stolzmann KL, Heyworth L, et al. Patient and provider predictors of telemental health use prior to and during the COVID-19 pandemic within the Department of Veterans Affairs. Am Psychol. 2022;77(2):249-261. doi:10.1037/amp0000895
Shelton CJ, Kim A, Hassan AM, Bhat A, Barnello J, Castro CA. System-wide implementation of telehealth to support military veterans and their families in response to COVID-19: a paradigm shift. J Mil Veteran Fam Health. 2020;6(S2):50-57. doi:10.3138/jmvfh-CO19-0003
VA expands telehealth by allowing health care providers to treat patients across state lines. News release. US Dept of Veterans Affairs. May 11, 2018. Accessed October 25, 2024. https://news.va.gov/press-room/va-expands-telehealth-by-allowing-health-care-providers-to-treat-patients-across-state-lines/
Self-Management in Epilepsy Care: Untapped Opportunities (FULL)
Epilepsy is a chronic neurologic condition defined by recurrent seizures not provoked by an environmental or a reversible trigger. About 1% of the US population has an epilepsy diagnosis, and an even higher percentage of the world’s population has seizures.1 For the many US soldiers who sustain blast-and concussion-related injuries, posttraumatic epilepsy is a potential risk.2 Although the risk of epilepsy remains unknown, the Veterans Health Administration (VHA) prioritizes diagnosis and management of the condition. Fortunately, antiepileptic therapies are effective for most patients. About 65% of patients can be free of seizures with use of a single daily medication.3 Although the other 35% often experience refractory seizures, advanced medication regimens, surgical approaches, and innovative devices can effect improvement in some cases.
Increasingly, patients are urged to practice epilepsy self-management. The idea of self-managing epilepsy, which has existed for decades, is supported primarily by a theory of robust patient education intended to increase disease knowledge and improve decision making. Multiple formal self-management programs have been developed and academically tested for patients with epilepsy. In a 2013 report, the Institute of Medicine emphasized the importance of research on the effects of behavioral self-management interventions on health outcomes and quality of life for people with epilepsy. The report recommended improving and expanding educational opportunities for patients.4 Nevertheless, self-management programs have not found widespread traction in mainstream clinical use.
This article provides a review of chronic disease self-management with a focus on its application and study in epilepsy. The authors discuss self-management, including underlying theory, definitions, and various tools. The principal formal epilepsy programs that have been studied and published are highlighted and summarized. This review also includes a discussion of the potential barriers to successful implementation of these epilepsy programs along with emerging solutions and tools for addressing these barriers.
Self-Management Theory
Disease self-management originated in social cognitive theory, which addresses the cognitive, emotional, and behavioral aspects of behavior change and is relevant to managing chronic illness.5,6 Self-management of chronic illness is defined as the daily actions that people take to keep their illness under control, to minimize its impact on physical health status and functioning, and to cope with psychosocial sequelae.7 These actions include making informed decisions about care, performing activities intended to manage the condition, and applying the necessary skills to maintain adequate psychosocial functioning.7
Related to self-management is self-efficacy, people’s confidence in their ability to engage in these actions.7 Evidence-based self-management and self-efficacy strategies are recognized as central in managing a variety of chronic diseases by improving the medical, emotional, and social role that management demands of chronic conditions.8
Self-management and self-efficacy have been explored in patients with epilepsy for decades, with various approaches being developed, implemented, and tested. Findings of several historical studies discussed in this review indicate that patients with epilepsy and high levels of self-efficacy are more successful in performing self-care tasks.9 This growing body of evidence led to the establishment of the Managing Epilepsy Well network in 2007.10 The Centers for Disease Control and Prevention created the network to expand epilepsy self-management research. Since 2007, more research has been focused on the potential for online and mobile health approaches in supporting epilepsy self-management and on intervention studies evaluating e-tools.
Elements of Epilepsy Self-Management
The first element of an epilepsy-specific self-management program is formal education on the diagnosis, treatment, and psychosocial impact of epilepsy and on strategies for coping with it. This element usually includes tools for evaluating and understanding epilepsy, with the goal of empowering patients to become actively engaged in managing and coping with their epilepsy diagnosis. Medication adherence is key in the optimal management of epilepsy. This point is evident in the development of a validated metric for self-efficacy: the Epilepsy Self-Efficacy Scale (ESES).11 Of the 33 items on the ESES, 14 are devoted to aspects of medication management. Other crucial behavioral elements for epilepsy self-management relate to lifestyle issues, such as safety, diet, exercise, sleep, and stress management.
Various self-management programs have incorporated tracking systems for these lifestyle elements as well as epilepsy-specific measures, such as seizure frequency, duration, and type. In addition, social support is an important factor in chronic illness self-management. Results of several studies support the hypothesis that higher levels of social support, particularly disease- and regimen-specific support, are related to better self-management behaviors.12 An increasing number of formal epilepsy self-management programs include peer support platforms and peer navigator features in their suite of services.
Patient Education and Self-Management Programs
Over the past several decades, multiple research groups have developed, implemented, and tested formal self-management platforms for patients with epilepsy. Designs and results of prominent studies are summarized in the Table.
More recent programs also included a focus on peer-to-peer support and patient-driven content within the educational curriculum.16,17 In 2015, Hixson and colleagues used an entirely patient-driven online platform.18 Unlike the programs described thus far, this platform made educational modules available and did not require that patients complete them. Peer-to-peer support and self-tracking tools were prominently featured, and patients used them. In addition, this intervention focused exclusively on a group of US veterans with epilepsy.
Tools for Improving Self-Management
Self-management programs for patients with epilepsy historically have involved formalized programs conducted face-to-face with other patients, with professional moderators, and perhaps with caregivers. These programs depended entirely on in-person educational sessions and in-person support groups and were found to be very effective in improving self-management skills, though they were labor-intensive and logistically challenging for both practitioners and patients.
Since the advent of the Internet and mobile connectivity, many programs have incorporated the same elements in more accessible form. Educational content appears in live webinars and asynchronous video educational modules; the latter are attractive because patients and caregivers can access them independently at any time. Also readily available are tools for day-to-day self-management of medical conditions. These tools include mobile and online diaries for tracking seizure metrics and medication adherence reminder systems. Last, a variety of online and mobile disease-specific social networking platforms allow patients to connect directly to others without having to travel long distances to meet in-person. Although these digital solutions may not provide the exact experience offered by an in-person support group, the promise of superior accessibility creates an advantage in terms of accessibility and flexibility.
Self-Management in the Literature
In a recent review of care delivery and self-managementstrategies for adults with epilepsy, Bradley and colleagues analyzed 18 different studies of 16 separate interventions and concluded that 2 interventions, the specialist epilepsy nurse and self-management education, had some evidence of benefit. Four studies, detailed next, had the highest quality design, based on a focus on epilepsy self-management specifically, a prospective hypothesis-driven approach, and rigorous methodology.19
In 1990, Helgeson and colleagues evaluated Sepulveda Epilepsy Education, a 2-day in-person program designed to provide medical education and psychosocial therapy to patients with an epilepsy diagnosis.13 The program was based on the theory that having a better understanding of their epilepsy helps people cope with the condition. Medical, social, and emotional topics are covered. Medical topics include epilepsy and how it may change over time, as well as diagnosis, treatment, and first aid; social and emotional topics include coping with the psychological aspects of epilepsy, family, social aspects, and employment. In this small study (38 patients total), compared with the control group (18 patients), the treatment group (20 patients) demonstrated a significant reduction in the level of fear of death and brain damage caused by seizures, a significant decrease in hazardous medical self-management practices, and a significant decrease in misconceptions about epilepsy. The treatment group also increased their medication adherence, as determined by serum drug levels. In addition, statistically nonsignificant trends were shown by the treatment group toward improved emotional, interpersonal, and vocational functioning; improved adjustment to seizures; and improved overall psychosocial functioning.
In 2002, May and Pfäfflin evaluated the efficacy of the Modular Service Package Epilepsy (MOSES) educational program.14 This program was specifically developed to improve patient knowledge about epilepsy and its consequences and diagnostic and therapeutic measures, and to improve patient understanding of psychosocial and occupational problems. It was the first comprehensive program used in German-speaking countries. It had 9 modules: coping with epilepsy, epidemiology, basic knowledge, diagnostics, therapy, self-control, prognosis, psychosocial aspects, and network. To complete the program, patients work through about fourteen 1-hour lessons. The controlled, randomized study by May and Pfäfflin involved 242 patients (113 treatment, 129 control) aged 16 to 80 years. Patients in the treatment (MOSES) group demonstrated significant improvements in 2 of the 9 modules (knowledge, coping with epilepsy), had improved self-reported seizure outcomes, were more satisfied with therapy, experienced better tolerability of antiepileptic drugs with fewer adverse effects (AEs), and were highly satisfied with the program. The researchers concluded that educational programs, such as MOSES, should become a standard service for specialized epilepsy care.
Developed over many years, WebEase is an online epilepsy self-management program that supports education on medication, stress, and sleep management. In 2011, DiIorio and colleagues reported on a WebEase trial in which 194 patients were randomly assigned to either a treatment group (n = 96) or a wait-list control group (n = 96), and 2 were lost to follow up.11 After accounting for study criteria and study drop out, 70 participants completed the treatment arm, and 78 completed the control arm. The study measured the impact of the platform on multiple outcome metrics, including 3 behavioral areas of focus. At follow-up, self-reported levels of medication adherence were higher for patients in the treatment group than for those in the control group. Analyses also compared patients who completed WebEase modules with those who did not. Patients who completed at least some WebEase modules reported higher levels of self-efficacy, and a trend toward significance was found for medication adherence, perceived stress, self-management, and knowledge. The authors concluded that online tools that support epilepsy self-management could be effective.11
In 2015, Fraser and colleagues reported the results of the Program for Active Consumer Engagement in Self-Management in Epilepsy (PACES in Epilepsy), a consumer-generated self-management program.16 In the trial, 83 adults with chronic epilepsy were initially assigned either to an in-person intervention or to treatment as usual. After study drop outs, 38 patients remained in the intervention arm, with 40 in the control arm. In the intervention, 6 to 8 adults met for a 75-minute group session 1 evening per week for 8 weeks; these sessions were co-led by a psychologist and a trained peer with epilepsy. Topics included medical, psychosocial, cognitive, and self-management aspects of epilepsy, in addition to community integration and optimization of epilepsy-related communication. Outcomes were measured with various instruments, including the ESES, the Quality of Life in Epilepsy-31 (QOLIE-31), the Epilepsy Self-Management Scale (ESMS), the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7. Each test was administered at baseline and after intervention. Outcomes were assessed immediately after program completion (8 weeks) and at follow-up 6 months later.
Findings suggested a substantial positive impact on epilepsy self-management capacities at program completion. In addition, benefit was sustained, particularly for epilepsy information management, over the 6 months after program completion. On the QOLIE-31 at 6 months, management of medication AEs also remained significantly improved, and fatigue management was improved at the P < .05 level. The researchers concluded that the PACES in Epilepsy program might have a more sustained impact on management of disability than on mood. They also noted that the effect was greater immediately after program completion than at 6 months. Patients gave the PACES program high satisfaction ratings.
Although these programs take slightly different approaches to epilepsy self-management, they have a similar focus: directed patient education. Furthermore, most of these programs are conducted in person, usually in a support group setting. In the WebEase trial, patients seem to have completed the online modules in a study setting, and a peer support component was not included. Overall, all programs successfully demonstrated various benefits for trial patients. These outcomes suggest that despite their subtle differences in approach, formal self-management programs are benefiting patients.
None of these platforms was designed for or specifically tested veterans with epilepsy. Although veterans theoretically would benefit from the same tools used by nonveterans, Iraq and Afghanistan veterans with epilepsy are more likely than are those without epilepsy to have mental and physical comorbidities and significantly higher mortality.2 Therefore, veterans potentially could benefit more from evidence-based chronic disease self-management programs designed to reduce physical and psychiatric comorbidities. Furthermore, programs that incorporate peer-to-peer support and direct links to VA care teams and mental health providers could be valuable.18
One research effort that directly addressed these issues is the Policy for Optimized Epilepsy Management (POEM) study, conducted by Hixson and colleagues in 2015.18 This study, not included in the review by Bradley and colleagues, used a purely online- and mobile-based social networking platform to promote self-management practices.19 Unlike the other programs described here, POEM did not require that patients view or attend formal educational seminars, though these seminars were available through the online platform for patient self-directed viewing. In addition, the intervention heavily promoted peer-to-peer engagement and disease tracking as means of increasing self-knowledge and activation. This study was unlike the other platforms in another way: It specifically focused on veterans with epilepsy, based on the idea that many veterans had a shared experience that would optimize a peer support approach.
The POEM investigators did not use a controlled design but found a significant benefit for both ESES and ESMS metrics on within-subject comparisons. Similar to the PACES in Epilepsy study, the POEM study found the highest benefit on the information management subscale of the ESMS.16 Practically speaking, this means patients were better able to use and manage digital and mobile information resources for controlling epilepsy. The POEM study results further reinforced the idea that epilepsy self-management programs are beneficial and expanded on earlier research to emphasize the value of peer support networks and digital interventions that can be used by patients at their convenience. These features provide greater access to more patients and maintain the crucial elements of peer-to-peer learning and counseling.
Implementation Barriers
Confirming the effectiveness of self-management programs is only the beginning of formal implementation and adoption. The real-world success of patient self-management programs has been documented for a few chronic diseases, including epilepsy. However, there is little research or commentary on lessons learned or on the challenges encountered with wide implementation of these programs.
Initial Setup and Sponsorship
To promote wider adoption, researchers should include commentary on initial setup, ongoing patient acceptance, and continual provider support. Many of the initial challenges in self-management programs involve a changing paradigm in the delivery and economics of health care. The transition to a more consumer-oriented health model with an emphasis on outcomes and patient-reported variables likely will support self-management strategies but is only slowly evolving. Many health care providers, hospitals, and payers may not be familiar with or have proper incentivizes to explore self-management tools even when proven effective.
More specifically, these epilepsy self-management programs are treatment adjuncts well suited to military and veteran health care systems. Self-management closely aligns with the overall VHA mission, vision, and values, including formal Department of Veteran Affairs (VA) goals and the MyVA priorities that collectively embrace improvement in access, a veteran-centric approach, and quality for improvement of the entire VA experience. Self-management platforms in the VA are recognized as empowering veterans and are thought to indirectly improve access to health care.20,21
The barriers of sponsorship and financial support likely will persist in the private health care sector but are less likely to significantly affect the VHA. Self-management programs have been researched and implemented for many health conditions across the VHA. For example, the VA Talent Management System course Patient Self-Management: Skill Building (TMS 6467) offers education and training to all clinical practitioners and managers involved in patient education and self-management activities for a variety of chronic medical conditions. Regarding epilepsy self-management more specifically, a patient brochure on the practice is distributed by the VHA Epilepsy Centers of Excellence (ECoEs) and an associated consortium.22 Last, a national provider educational lecture series has a corresponding patient and caregiver lecture set that emphasizes education and self-management behaviors.
Labor, Time, and Resource Needs
The most time-intensive aspect of designing self-management programs is developing the tool that allows clinicians and patients to work together. From a program perspective, the tool must be available and helpful not only to patients and specialists, but also to primary care providers. Tertiary-care centers usually accept the responsibility for program initiation, including patient recruitment, logistics coordination, and health care professional staffing. For epilepsy, the small pool of relevant specialists and centers limits the number of self-management education sessions that can be hosted and increases the need for complex travel and scheduling tasks. However, ECoE communication lines provide a basic infrastructure for collaboration and for development of tools that can be helpful to all clinicians treating veterans with epilepsy.23
Given the issues with coordinating the logistics of in-person programs at brick-and-mortar sites, this type of program may not be the best option for some patients and facilities. Alternative approaches, such as telehealth and asynchronous digital platforms, could expand access and increase convenience. Even though remotely administered programs may not be as powerful for some patients, the promise of scalable access supports consideration of these approaches.
Patient and Caregiver Logistics
Veterans with epilepsy may also have comorbid traumatic brain injury (TBI) and posttraumatic stress disorder, which can complicate self-managed care. In addition, many veterans live in rural areas and have limited travel options. All these factors challenge the success of epilepsy self-management programs. However, the network of ECoEs and associated consortium facilities can step up to deliver self-management tools and information.
The infrastructure of the VHA patient aligned care team (PACT) also contributes to the integration of self-management training. The PACT model takes a personalized, comprehensive, coordinated approach to promote team-based, veteran-centric care and actively partners with other VHA offices to incorporate alternative care services, including peer support and self-management platforms. The combination represents fertile ground for implementation and promotion of self-management tools in the VHA epilepsy population.
Health Care Economics
Given the uncertainties of the US health care economy, it is not surprising that many experts advocate a fundamental redesign of the health care team relationship and information infrastructure.24 This realignment includes partnering directly with patients and their families to encourage more reliance on self-management practices. Unfortunately, this approach does not lend itself to the well-entrenched business model on which most community medical practices are based. Health system leadership often must be convinced there are potential cost savings or a return on investment for new programs. As there is no consistent, comprehensive reimbursement policy for programs focused on self-management, health care systems must be creative and innovative when appraising the financial consequences of such programs.
Epilepsy remains a huge burden. In 2000, the annual total cost of epilepsy treatment in the US was $362 million for new patients and $2 billion for existing cases.25 Within the VHA, the occurrence of posttraumatic epilepsy among the increasing number of veterans with TBI contributes to the burden, and posttraumatic epilepsy and psychogenic nonepileptic seizures complicate treatment approaches. The incidence of comorbidities, including anxiety and depression, has been as high as 50%.23 Epilepsy health care programs are evaluating ways to validate their ability to minimize cost, improve access, and maintain quality of service. Integration of self-management should be included in these efforts.
The VHA represents a unique health care environment for testing and implementing self-management programs. Although the VHA is not immune to the traditional business models of medicine, it is less dependent on them, and it disproportionately cares for patients for long spans of time. From the health care team perspective, data indicate that ECoE physicians represent a high percentage of VHA epilepsy specialists but directly see only about 20% of veterans with an epilepsy or seizure-associated diagnosis. Therefore, future collaboration and connectivity of consortium sites can have a broader impact on self-management—highlighting the fact that concerted, scaled self-management programs have an important role in the VHA health care delivery system and should be promoted.26
Final Insights and Opportunities
Despite the barriers to adoption, formal epilepsy self-management programs are making gains in maturity and academic credibility. As the health care economy gradually shifts to more outcomes-based models, these offerings likely will become more valued, particularly by health care organizations focused on cost sharing, by large self-insuring employers, or organizations like the VHA where patients maintain a long-term relationship. Nevertheless, for the more resource-intensive, in-person self-management programs, adoption may remain constrained. Digital and mobile platforms should serve as more accessible entry points, with lower costs and more rapid scaling potential. Even though these online platforms may not have the same impact as intensive face-to-face programs, their scalability and constant accessibility should make them attractive, and the relatively modest cost of implementing self-guided programs should reduce barriers to adoption.
Integrated health care systems, such as the VHA and various European health systems, can serve as models for self-management implementation. Incorporating a live clinical implementation into parallel research efforts can continue to produce vital academic information on the real-world impact of these solutions, and this evidence in turn can be used to support policies that foster widespread adoption. More specifically, the ECoE model represents a clear opportunity to promote widespread implementation of self-management. The ECoEs are already publishing self-management materials that health care teams can use in patient counseling,and several self-care studies are being conducted within the network.22 In this model, compared with private sector health systems, ECoEs are well positioned to advance the use of formal self-management strategies.
The proposed epilepsy self-management model for ECoEs would be based on an iterative program that incorporates best practices from each of the research studies discussed earlier. With the publication of new research, successful self-management tools would be incorporated into the programs. From a curriculum perspective, educational platforms on medication adherence, seizure safety, and information/data management should be included. Evidence is increasing that peer support and use of licensed peer navigators should be incorporated as well. Last, flexible and asynchronous digital methods should be added to self-management platforms to maximize patient access. These features build on the growing body of evidence to maximize the likelihood of a successful and sustainable self-management strategy for patients with epilepsy.
Click here to read the digital edition.
1. Fiest KM, Sauro KM, Wiebe S, et al. Prevalence and incidence in epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88(3):296-303.
2. Pugh MJ, Van Cott AC, Amuan M, et al. Epilepsy among Iraq and Afghanistan war veterans—United States, 2002-2015. MMWR. 2016;65(44):1224-1227.
3. Kwan P, Brodie MJ. Effectiveness of first antiepileptic drug. Epilepsia. 2001;42(10):1255-1260.
4. Hesdorffer DC, Beck V, Begley CE, et al. Research implications of the Institute of Medicine report, Epilepsy Across the Spectrum: Promoting Health and Understanding. Epilepsia. 2013;54(2):207-216.
5. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
6. Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977.
7. Clark, NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-management of chronic disease by older adults. J Aging Health. 1991;3(1):3-27.
8. Ory MG, Ahn SM, Jiang L, et al. Successes of a national study of the Chronic Disease Self-Management Program: meeting the triple aim of health care reform. Med Care. 2013;51(11):992-998.
9. DiIorio C, Shafer PO, Letz R, Henry TR, Schomer DL, Yeager K; Project EASE Study Group. Behavioral, social and affective factors associated with self-efficacy for self-management among people with epilepsy. Epilepsy Behav. 2006;9(1):158-163.
10. Shegog R, Bamps YA, Patel A, et al. Managing Epilepsy Well: emerging e-tools for epilepsy self-management. Epilepsy Behav. 2013;29(1):133-140.
11. DiIorio C, Bamps Y, Walker ER, Escoffery C. Results of a research study evaluating WebEase, an online epilepsy self-management program. Epilepsy Behav. 2011;22(3):469-474.
12. Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003;30(2):170-195.
13. Helgeson DC, Mittan R, Tan SY, Chayasirisobhon S. Sepulveda Epilepsy Education: the efficacy of a psychoeducational treatment programme in treating medical and psychosocial aspects of epilepsy. Epilepsia. 1990;31(1):75-82.
14. May TW, Pfäfflin M. The efficacy of an educational treatment program for patients with epilepsy (MOSES): results of a controlled, randomized study. Modular Service Package Epilepsy. Epilepsia. 2002;43(5):539-549.
15. Aliasgharpour M, Dehgahn Nayeri N, Yadegary MA, Haghani H. Effects of an educational program on self-management in patients with epilepsy. Seizure. 2013;22(1):48-52.
16. Fraser RT, Johnson EK, Lashley S, et al. PACES in Epilepsy: results of a self-management randomized controlled trial. Epilepsia. 2015;56(8):1264-1274.
17. Laybourne AH, Morgan M, Watkins SH, Lawton R, Ridsdale L, Goldstein LH. Self-management for people with poorly controlled epilepsy: participants’ views of the UK self-management in epilepsy (SMILE) program. Epilepsy Behav. 2015;52(pt A):159-164.
18. Hixson JD, Barnes D, Parko K, et al. Patients optimizing epilepsy management via an online community: the POEM study. Neurology. 2015;85(2):129-136.
19. Bradley PM, Lindsay B, Fleeman N. Care delivery and self-management strategies for adults with epilepsy. Cochrane Database Syst Rev. 2016;2:CD006244.
20. Allicock M, Haynes-Maslow L, Carr C, et al. Training veterans to provide peer support in a weight-management program: MOVE! Prev Chronic Dis. 2013;10:E185.
21. Damush TM, Jackson GL, Powers BJ, et al. Implementing evidence-based patient self-management programs in the Veterans Health Administration: perspectives on delivery system design considerations. J Gen Intern Med. 2010;25(suppl 1):68-71.
22. Caraveo N, Chen S, Evrard C, Ozuna J; Epilepsy Centers of Excellence Nursing Workgroup. Self-management in epilepsy: a guide for healthcare professionals. https://www.epilepsy.va.gov/Library/Self-Management%20In%20Epilepsy.pdf. Published Winter 2015. Accessed February 26, 2018.
23. Rehman R, Kelly PR, Husain AM, Tran TT. Characteristics of veterans diagnosed with seizures within the Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762.
24. Merry MD. Healthcare’s need for revolutionary change. Quality Prog. 2003;36(9):31-35.
25. Halpern M, Rentz A, Murray M. Cost of illness of epilepsy in the US: comparison of patient-based and population-based estimates. Neuroepidemiology. 2000;19(2):87-99.
26. Kelly P, Chinta R. Do centers of excellence excel in patient outcomes?: Evidence from U.S. Veterans Health Administration Centers for Epilepsy. Int J Manage Excellence. 2015;4(3):529-538.
Epilepsy is a chronic neurologic condition defined by recurrent seizures not provoked by an environmental or a reversible trigger. About 1% of the US population has an epilepsy diagnosis, and an even higher percentage of the world’s population has seizures.1 For the many US soldiers who sustain blast-and concussion-related injuries, posttraumatic epilepsy is a potential risk.2 Although the risk of epilepsy remains unknown, the Veterans Health Administration (VHA) prioritizes diagnosis and management of the condition. Fortunately, antiepileptic therapies are effective for most patients. About 65% of patients can be free of seizures with use of a single daily medication.3 Although the other 35% often experience refractory seizures, advanced medication regimens, surgical approaches, and innovative devices can effect improvement in some cases.
Increasingly, patients are urged to practice epilepsy self-management. The idea of self-managing epilepsy, which has existed for decades, is supported primarily by a theory of robust patient education intended to increase disease knowledge and improve decision making. Multiple formal self-management programs have been developed and academically tested for patients with epilepsy. In a 2013 report, the Institute of Medicine emphasized the importance of research on the effects of behavioral self-management interventions on health outcomes and quality of life for people with epilepsy. The report recommended improving and expanding educational opportunities for patients.4 Nevertheless, self-management programs have not found widespread traction in mainstream clinical use.
This article provides a review of chronic disease self-management with a focus on its application and study in epilepsy. The authors discuss self-management, including underlying theory, definitions, and various tools. The principal formal epilepsy programs that have been studied and published are highlighted and summarized. This review also includes a discussion of the potential barriers to successful implementation of these epilepsy programs along with emerging solutions and tools for addressing these barriers.
Self-Management Theory
Disease self-management originated in social cognitive theory, which addresses the cognitive, emotional, and behavioral aspects of behavior change and is relevant to managing chronic illness.5,6 Self-management of chronic illness is defined as the daily actions that people take to keep their illness under control, to minimize its impact on physical health status and functioning, and to cope with psychosocial sequelae.7 These actions include making informed decisions about care, performing activities intended to manage the condition, and applying the necessary skills to maintain adequate psychosocial functioning.7
Related to self-management is self-efficacy, people’s confidence in their ability to engage in these actions.7 Evidence-based self-management and self-efficacy strategies are recognized as central in managing a variety of chronic diseases by improving the medical, emotional, and social role that management demands of chronic conditions.8
Self-management and self-efficacy have been explored in patients with epilepsy for decades, with various approaches being developed, implemented, and tested. Findings of several historical studies discussed in this review indicate that patients with epilepsy and high levels of self-efficacy are more successful in performing self-care tasks.9 This growing body of evidence led to the establishment of the Managing Epilepsy Well network in 2007.10 The Centers for Disease Control and Prevention created the network to expand epilepsy self-management research. Since 2007, more research has been focused on the potential for online and mobile health approaches in supporting epilepsy self-management and on intervention studies evaluating e-tools.
Elements of Epilepsy Self-Management
The first element of an epilepsy-specific self-management program is formal education on the diagnosis, treatment, and psychosocial impact of epilepsy and on strategies for coping with it. This element usually includes tools for evaluating and understanding epilepsy, with the goal of empowering patients to become actively engaged in managing and coping with their epilepsy diagnosis. Medication adherence is key in the optimal management of epilepsy. This point is evident in the development of a validated metric for self-efficacy: the Epilepsy Self-Efficacy Scale (ESES).11 Of the 33 items on the ESES, 14 are devoted to aspects of medication management. Other crucial behavioral elements for epilepsy self-management relate to lifestyle issues, such as safety, diet, exercise, sleep, and stress management.
Various self-management programs have incorporated tracking systems for these lifestyle elements as well as epilepsy-specific measures, such as seizure frequency, duration, and type. In addition, social support is an important factor in chronic illness self-management. Results of several studies support the hypothesis that higher levels of social support, particularly disease- and regimen-specific support, are related to better self-management behaviors.12 An increasing number of formal epilepsy self-management programs include peer support platforms and peer navigator features in their suite of services.
Patient Education and Self-Management Programs
Over the past several decades, multiple research groups have developed, implemented, and tested formal self-management platforms for patients with epilepsy. Designs and results of prominent studies are summarized in the Table.
More recent programs also included a focus on peer-to-peer support and patient-driven content within the educational curriculum.16,17 In 2015, Hixson and colleagues used an entirely patient-driven online platform.18 Unlike the programs described thus far, this platform made educational modules available and did not require that patients complete them. Peer-to-peer support and self-tracking tools were prominently featured, and patients used them. In addition, this intervention focused exclusively on a group of US veterans with epilepsy.
Tools for Improving Self-Management
Self-management programs for patients with epilepsy historically have involved formalized programs conducted face-to-face with other patients, with professional moderators, and perhaps with caregivers. These programs depended entirely on in-person educational sessions and in-person support groups and were found to be very effective in improving self-management skills, though they were labor-intensive and logistically challenging for both practitioners and patients.
Since the advent of the Internet and mobile connectivity, many programs have incorporated the same elements in more accessible form. Educational content appears in live webinars and asynchronous video educational modules; the latter are attractive because patients and caregivers can access them independently at any time. Also readily available are tools for day-to-day self-management of medical conditions. These tools include mobile and online diaries for tracking seizure metrics and medication adherence reminder systems. Last, a variety of online and mobile disease-specific social networking platforms allow patients to connect directly to others without having to travel long distances to meet in-person. Although these digital solutions may not provide the exact experience offered by an in-person support group, the promise of superior accessibility creates an advantage in terms of accessibility and flexibility.
Self-Management in the Literature
In a recent review of care delivery and self-managementstrategies for adults with epilepsy, Bradley and colleagues analyzed 18 different studies of 16 separate interventions and concluded that 2 interventions, the specialist epilepsy nurse and self-management education, had some evidence of benefit. Four studies, detailed next, had the highest quality design, based on a focus on epilepsy self-management specifically, a prospective hypothesis-driven approach, and rigorous methodology.19
In 1990, Helgeson and colleagues evaluated Sepulveda Epilepsy Education, a 2-day in-person program designed to provide medical education and psychosocial therapy to patients with an epilepsy diagnosis.13 The program was based on the theory that having a better understanding of their epilepsy helps people cope with the condition. Medical, social, and emotional topics are covered. Medical topics include epilepsy and how it may change over time, as well as diagnosis, treatment, and first aid; social and emotional topics include coping with the psychological aspects of epilepsy, family, social aspects, and employment. In this small study (38 patients total), compared with the control group (18 patients), the treatment group (20 patients) demonstrated a significant reduction in the level of fear of death and brain damage caused by seizures, a significant decrease in hazardous medical self-management practices, and a significant decrease in misconceptions about epilepsy. The treatment group also increased their medication adherence, as determined by serum drug levels. In addition, statistically nonsignificant trends were shown by the treatment group toward improved emotional, interpersonal, and vocational functioning; improved adjustment to seizures; and improved overall psychosocial functioning.
In 2002, May and Pfäfflin evaluated the efficacy of the Modular Service Package Epilepsy (MOSES) educational program.14 This program was specifically developed to improve patient knowledge about epilepsy and its consequences and diagnostic and therapeutic measures, and to improve patient understanding of psychosocial and occupational problems. It was the first comprehensive program used in German-speaking countries. It had 9 modules: coping with epilepsy, epidemiology, basic knowledge, diagnostics, therapy, self-control, prognosis, psychosocial aspects, and network. To complete the program, patients work through about fourteen 1-hour lessons. The controlled, randomized study by May and Pfäfflin involved 242 patients (113 treatment, 129 control) aged 16 to 80 years. Patients in the treatment (MOSES) group demonstrated significant improvements in 2 of the 9 modules (knowledge, coping with epilepsy), had improved self-reported seizure outcomes, were more satisfied with therapy, experienced better tolerability of antiepileptic drugs with fewer adverse effects (AEs), and were highly satisfied with the program. The researchers concluded that educational programs, such as MOSES, should become a standard service for specialized epilepsy care.
Developed over many years, WebEase is an online epilepsy self-management program that supports education on medication, stress, and sleep management. In 2011, DiIorio and colleagues reported on a WebEase trial in which 194 patients were randomly assigned to either a treatment group (n = 96) or a wait-list control group (n = 96), and 2 were lost to follow up.11 After accounting for study criteria and study drop out, 70 participants completed the treatment arm, and 78 completed the control arm. The study measured the impact of the platform on multiple outcome metrics, including 3 behavioral areas of focus. At follow-up, self-reported levels of medication adherence were higher for patients in the treatment group than for those in the control group. Analyses also compared patients who completed WebEase modules with those who did not. Patients who completed at least some WebEase modules reported higher levels of self-efficacy, and a trend toward significance was found for medication adherence, perceived stress, self-management, and knowledge. The authors concluded that online tools that support epilepsy self-management could be effective.11
In 2015, Fraser and colleagues reported the results of the Program for Active Consumer Engagement in Self-Management in Epilepsy (PACES in Epilepsy), a consumer-generated self-management program.16 In the trial, 83 adults with chronic epilepsy were initially assigned either to an in-person intervention or to treatment as usual. After study drop outs, 38 patients remained in the intervention arm, with 40 in the control arm. In the intervention, 6 to 8 adults met for a 75-minute group session 1 evening per week for 8 weeks; these sessions were co-led by a psychologist and a trained peer with epilepsy. Topics included medical, psychosocial, cognitive, and self-management aspects of epilepsy, in addition to community integration and optimization of epilepsy-related communication. Outcomes were measured with various instruments, including the ESES, the Quality of Life in Epilepsy-31 (QOLIE-31), the Epilepsy Self-Management Scale (ESMS), the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7. Each test was administered at baseline and after intervention. Outcomes were assessed immediately after program completion (8 weeks) and at follow-up 6 months later.
Findings suggested a substantial positive impact on epilepsy self-management capacities at program completion. In addition, benefit was sustained, particularly for epilepsy information management, over the 6 months after program completion. On the QOLIE-31 at 6 months, management of medication AEs also remained significantly improved, and fatigue management was improved at the P < .05 level. The researchers concluded that the PACES in Epilepsy program might have a more sustained impact on management of disability than on mood. They also noted that the effect was greater immediately after program completion than at 6 months. Patients gave the PACES program high satisfaction ratings.
Although these programs take slightly different approaches to epilepsy self-management, they have a similar focus: directed patient education. Furthermore, most of these programs are conducted in person, usually in a support group setting. In the WebEase trial, patients seem to have completed the online modules in a study setting, and a peer support component was not included. Overall, all programs successfully demonstrated various benefits for trial patients. These outcomes suggest that despite their subtle differences in approach, formal self-management programs are benefiting patients.
None of these platforms was designed for or specifically tested veterans with epilepsy. Although veterans theoretically would benefit from the same tools used by nonveterans, Iraq and Afghanistan veterans with epilepsy are more likely than are those without epilepsy to have mental and physical comorbidities and significantly higher mortality.2 Therefore, veterans potentially could benefit more from evidence-based chronic disease self-management programs designed to reduce physical and psychiatric comorbidities. Furthermore, programs that incorporate peer-to-peer support and direct links to VA care teams and mental health providers could be valuable.18
One research effort that directly addressed these issues is the Policy for Optimized Epilepsy Management (POEM) study, conducted by Hixson and colleagues in 2015.18 This study, not included in the review by Bradley and colleagues, used a purely online- and mobile-based social networking platform to promote self-management practices.19 Unlike the other programs described here, POEM did not require that patients view or attend formal educational seminars, though these seminars were available through the online platform for patient self-directed viewing. In addition, the intervention heavily promoted peer-to-peer engagement and disease tracking as means of increasing self-knowledge and activation. This study was unlike the other platforms in another way: It specifically focused on veterans with epilepsy, based on the idea that many veterans had a shared experience that would optimize a peer support approach.
The POEM investigators did not use a controlled design but found a significant benefit for both ESES and ESMS metrics on within-subject comparisons. Similar to the PACES in Epilepsy study, the POEM study found the highest benefit on the information management subscale of the ESMS.16 Practically speaking, this means patients were better able to use and manage digital and mobile information resources for controlling epilepsy. The POEM study results further reinforced the idea that epilepsy self-management programs are beneficial and expanded on earlier research to emphasize the value of peer support networks and digital interventions that can be used by patients at their convenience. These features provide greater access to more patients and maintain the crucial elements of peer-to-peer learning and counseling.
Implementation Barriers
Confirming the effectiveness of self-management programs is only the beginning of formal implementation and adoption. The real-world success of patient self-management programs has been documented for a few chronic diseases, including epilepsy. However, there is little research or commentary on lessons learned or on the challenges encountered with wide implementation of these programs.
Initial Setup and Sponsorship
To promote wider adoption, researchers should include commentary on initial setup, ongoing patient acceptance, and continual provider support. Many of the initial challenges in self-management programs involve a changing paradigm in the delivery and economics of health care. The transition to a more consumer-oriented health model with an emphasis on outcomes and patient-reported variables likely will support self-management strategies but is only slowly evolving. Many health care providers, hospitals, and payers may not be familiar with or have proper incentivizes to explore self-management tools even when proven effective.
More specifically, these epilepsy self-management programs are treatment adjuncts well suited to military and veteran health care systems. Self-management closely aligns with the overall VHA mission, vision, and values, including formal Department of Veteran Affairs (VA) goals and the MyVA priorities that collectively embrace improvement in access, a veteran-centric approach, and quality for improvement of the entire VA experience. Self-management platforms in the VA are recognized as empowering veterans and are thought to indirectly improve access to health care.20,21
The barriers of sponsorship and financial support likely will persist in the private health care sector but are less likely to significantly affect the VHA. Self-management programs have been researched and implemented for many health conditions across the VHA. For example, the VA Talent Management System course Patient Self-Management: Skill Building (TMS 6467) offers education and training to all clinical practitioners and managers involved in patient education and self-management activities for a variety of chronic medical conditions. Regarding epilepsy self-management more specifically, a patient brochure on the practice is distributed by the VHA Epilepsy Centers of Excellence (ECoEs) and an associated consortium.22 Last, a national provider educational lecture series has a corresponding patient and caregiver lecture set that emphasizes education and self-management behaviors.
Labor, Time, and Resource Needs
The most time-intensive aspect of designing self-management programs is developing the tool that allows clinicians and patients to work together. From a program perspective, the tool must be available and helpful not only to patients and specialists, but also to primary care providers. Tertiary-care centers usually accept the responsibility for program initiation, including patient recruitment, logistics coordination, and health care professional staffing. For epilepsy, the small pool of relevant specialists and centers limits the number of self-management education sessions that can be hosted and increases the need for complex travel and scheduling tasks. However, ECoE communication lines provide a basic infrastructure for collaboration and for development of tools that can be helpful to all clinicians treating veterans with epilepsy.23
Given the issues with coordinating the logistics of in-person programs at brick-and-mortar sites, this type of program may not be the best option for some patients and facilities. Alternative approaches, such as telehealth and asynchronous digital platforms, could expand access and increase convenience. Even though remotely administered programs may not be as powerful for some patients, the promise of scalable access supports consideration of these approaches.
Patient and Caregiver Logistics
Veterans with epilepsy may also have comorbid traumatic brain injury (TBI) and posttraumatic stress disorder, which can complicate self-managed care. In addition, many veterans live in rural areas and have limited travel options. All these factors challenge the success of epilepsy self-management programs. However, the network of ECoEs and associated consortium facilities can step up to deliver self-management tools and information.
The infrastructure of the VHA patient aligned care team (PACT) also contributes to the integration of self-management training. The PACT model takes a personalized, comprehensive, coordinated approach to promote team-based, veteran-centric care and actively partners with other VHA offices to incorporate alternative care services, including peer support and self-management platforms. The combination represents fertile ground for implementation and promotion of self-management tools in the VHA epilepsy population.
Health Care Economics
Given the uncertainties of the US health care economy, it is not surprising that many experts advocate a fundamental redesign of the health care team relationship and information infrastructure.24 This realignment includes partnering directly with patients and their families to encourage more reliance on self-management practices. Unfortunately, this approach does not lend itself to the well-entrenched business model on which most community medical practices are based. Health system leadership often must be convinced there are potential cost savings or a return on investment for new programs. As there is no consistent, comprehensive reimbursement policy for programs focused on self-management, health care systems must be creative and innovative when appraising the financial consequences of such programs.
Epilepsy remains a huge burden. In 2000, the annual total cost of epilepsy treatment in the US was $362 million for new patients and $2 billion for existing cases.25 Within the VHA, the occurrence of posttraumatic epilepsy among the increasing number of veterans with TBI contributes to the burden, and posttraumatic epilepsy and psychogenic nonepileptic seizures complicate treatment approaches. The incidence of comorbidities, including anxiety and depression, has been as high as 50%.23 Epilepsy health care programs are evaluating ways to validate their ability to minimize cost, improve access, and maintain quality of service. Integration of self-management should be included in these efforts.
The VHA represents a unique health care environment for testing and implementing self-management programs. Although the VHA is not immune to the traditional business models of medicine, it is less dependent on them, and it disproportionately cares for patients for long spans of time. From the health care team perspective, data indicate that ECoE physicians represent a high percentage of VHA epilepsy specialists but directly see only about 20% of veterans with an epilepsy or seizure-associated diagnosis. Therefore, future collaboration and connectivity of consortium sites can have a broader impact on self-management—highlighting the fact that concerted, scaled self-management programs have an important role in the VHA health care delivery system and should be promoted.26
Final Insights and Opportunities
Despite the barriers to adoption, formal epilepsy self-management programs are making gains in maturity and academic credibility. As the health care economy gradually shifts to more outcomes-based models, these offerings likely will become more valued, particularly by health care organizations focused on cost sharing, by large self-insuring employers, or organizations like the VHA where patients maintain a long-term relationship. Nevertheless, for the more resource-intensive, in-person self-management programs, adoption may remain constrained. Digital and mobile platforms should serve as more accessible entry points, with lower costs and more rapid scaling potential. Even though these online platforms may not have the same impact as intensive face-to-face programs, their scalability and constant accessibility should make them attractive, and the relatively modest cost of implementing self-guided programs should reduce barriers to adoption.
Integrated health care systems, such as the VHA and various European health systems, can serve as models for self-management implementation. Incorporating a live clinical implementation into parallel research efforts can continue to produce vital academic information on the real-world impact of these solutions, and this evidence in turn can be used to support policies that foster widespread adoption. More specifically, the ECoE model represents a clear opportunity to promote widespread implementation of self-management. The ECoEs are already publishing self-management materials that health care teams can use in patient counseling,and several self-care studies are being conducted within the network.22 In this model, compared with private sector health systems, ECoEs are well positioned to advance the use of formal self-management strategies.
The proposed epilepsy self-management model for ECoEs would be based on an iterative program that incorporates best practices from each of the research studies discussed earlier. With the publication of new research, successful self-management tools would be incorporated into the programs. From a curriculum perspective, educational platforms on medication adherence, seizure safety, and information/data management should be included. Evidence is increasing that peer support and use of licensed peer navigators should be incorporated as well. Last, flexible and asynchronous digital methods should be added to self-management platforms to maximize patient access. These features build on the growing body of evidence to maximize the likelihood of a successful and sustainable self-management strategy for patients with epilepsy.
Click here to read the digital edition.
Epilepsy is a chronic neurologic condition defined by recurrent seizures not provoked by an environmental or a reversible trigger. About 1% of the US population has an epilepsy diagnosis, and an even higher percentage of the world’s population has seizures.1 For the many US soldiers who sustain blast-and concussion-related injuries, posttraumatic epilepsy is a potential risk.2 Although the risk of epilepsy remains unknown, the Veterans Health Administration (VHA) prioritizes diagnosis and management of the condition. Fortunately, antiepileptic therapies are effective for most patients. About 65% of patients can be free of seizures with use of a single daily medication.3 Although the other 35% often experience refractory seizures, advanced medication regimens, surgical approaches, and innovative devices can effect improvement in some cases.
Increasingly, patients are urged to practice epilepsy self-management. The idea of self-managing epilepsy, which has existed for decades, is supported primarily by a theory of robust patient education intended to increase disease knowledge and improve decision making. Multiple formal self-management programs have been developed and academically tested for patients with epilepsy. In a 2013 report, the Institute of Medicine emphasized the importance of research on the effects of behavioral self-management interventions on health outcomes and quality of life for people with epilepsy. The report recommended improving and expanding educational opportunities for patients.4 Nevertheless, self-management programs have not found widespread traction in mainstream clinical use.
This article provides a review of chronic disease self-management with a focus on its application and study in epilepsy. The authors discuss self-management, including underlying theory, definitions, and various tools. The principal formal epilepsy programs that have been studied and published are highlighted and summarized. This review also includes a discussion of the potential barriers to successful implementation of these epilepsy programs along with emerging solutions and tools for addressing these barriers.
Self-Management Theory
Disease self-management originated in social cognitive theory, which addresses the cognitive, emotional, and behavioral aspects of behavior change and is relevant to managing chronic illness.5,6 Self-management of chronic illness is defined as the daily actions that people take to keep their illness under control, to minimize its impact on physical health status and functioning, and to cope with psychosocial sequelae.7 These actions include making informed decisions about care, performing activities intended to manage the condition, and applying the necessary skills to maintain adequate psychosocial functioning.7
Related to self-management is self-efficacy, people’s confidence in their ability to engage in these actions.7 Evidence-based self-management and self-efficacy strategies are recognized as central in managing a variety of chronic diseases by improving the medical, emotional, and social role that management demands of chronic conditions.8
Self-management and self-efficacy have been explored in patients with epilepsy for decades, with various approaches being developed, implemented, and tested. Findings of several historical studies discussed in this review indicate that patients with epilepsy and high levels of self-efficacy are more successful in performing self-care tasks.9 This growing body of evidence led to the establishment of the Managing Epilepsy Well network in 2007.10 The Centers for Disease Control and Prevention created the network to expand epilepsy self-management research. Since 2007, more research has been focused on the potential for online and mobile health approaches in supporting epilepsy self-management and on intervention studies evaluating e-tools.
Elements of Epilepsy Self-Management
The first element of an epilepsy-specific self-management program is formal education on the diagnosis, treatment, and psychosocial impact of epilepsy and on strategies for coping with it. This element usually includes tools for evaluating and understanding epilepsy, with the goal of empowering patients to become actively engaged in managing and coping with their epilepsy diagnosis. Medication adherence is key in the optimal management of epilepsy. This point is evident in the development of a validated metric for self-efficacy: the Epilepsy Self-Efficacy Scale (ESES).11 Of the 33 items on the ESES, 14 are devoted to aspects of medication management. Other crucial behavioral elements for epilepsy self-management relate to lifestyle issues, such as safety, diet, exercise, sleep, and stress management.
Various self-management programs have incorporated tracking systems for these lifestyle elements as well as epilepsy-specific measures, such as seizure frequency, duration, and type. In addition, social support is an important factor in chronic illness self-management. Results of several studies support the hypothesis that higher levels of social support, particularly disease- and regimen-specific support, are related to better self-management behaviors.12 An increasing number of formal epilepsy self-management programs include peer support platforms and peer navigator features in their suite of services.
Patient Education and Self-Management Programs
Over the past several decades, multiple research groups have developed, implemented, and tested formal self-management platforms for patients with epilepsy. Designs and results of prominent studies are summarized in the Table.
More recent programs also included a focus on peer-to-peer support and patient-driven content within the educational curriculum.16,17 In 2015, Hixson and colleagues used an entirely patient-driven online platform.18 Unlike the programs described thus far, this platform made educational modules available and did not require that patients complete them. Peer-to-peer support and self-tracking tools were prominently featured, and patients used them. In addition, this intervention focused exclusively on a group of US veterans with epilepsy.
Tools for Improving Self-Management
Self-management programs for patients with epilepsy historically have involved formalized programs conducted face-to-face with other patients, with professional moderators, and perhaps with caregivers. These programs depended entirely on in-person educational sessions and in-person support groups and were found to be very effective in improving self-management skills, though they were labor-intensive and logistically challenging for both practitioners and patients.
Since the advent of the Internet and mobile connectivity, many programs have incorporated the same elements in more accessible form. Educational content appears in live webinars and asynchronous video educational modules; the latter are attractive because patients and caregivers can access them independently at any time. Also readily available are tools for day-to-day self-management of medical conditions. These tools include mobile and online diaries for tracking seizure metrics and medication adherence reminder systems. Last, a variety of online and mobile disease-specific social networking platforms allow patients to connect directly to others without having to travel long distances to meet in-person. Although these digital solutions may not provide the exact experience offered by an in-person support group, the promise of superior accessibility creates an advantage in terms of accessibility and flexibility.
Self-Management in the Literature
In a recent review of care delivery and self-managementstrategies for adults with epilepsy, Bradley and colleagues analyzed 18 different studies of 16 separate interventions and concluded that 2 interventions, the specialist epilepsy nurse and self-management education, had some evidence of benefit. Four studies, detailed next, had the highest quality design, based on a focus on epilepsy self-management specifically, a prospective hypothesis-driven approach, and rigorous methodology.19
In 1990, Helgeson and colleagues evaluated Sepulveda Epilepsy Education, a 2-day in-person program designed to provide medical education and psychosocial therapy to patients with an epilepsy diagnosis.13 The program was based on the theory that having a better understanding of their epilepsy helps people cope with the condition. Medical, social, and emotional topics are covered. Medical topics include epilepsy and how it may change over time, as well as diagnosis, treatment, and first aid; social and emotional topics include coping with the psychological aspects of epilepsy, family, social aspects, and employment. In this small study (38 patients total), compared with the control group (18 patients), the treatment group (20 patients) demonstrated a significant reduction in the level of fear of death and brain damage caused by seizures, a significant decrease in hazardous medical self-management practices, and a significant decrease in misconceptions about epilepsy. The treatment group also increased their medication adherence, as determined by serum drug levels. In addition, statistically nonsignificant trends were shown by the treatment group toward improved emotional, interpersonal, and vocational functioning; improved adjustment to seizures; and improved overall psychosocial functioning.
In 2002, May and Pfäfflin evaluated the efficacy of the Modular Service Package Epilepsy (MOSES) educational program.14 This program was specifically developed to improve patient knowledge about epilepsy and its consequences and diagnostic and therapeutic measures, and to improve patient understanding of psychosocial and occupational problems. It was the first comprehensive program used in German-speaking countries. It had 9 modules: coping with epilepsy, epidemiology, basic knowledge, diagnostics, therapy, self-control, prognosis, psychosocial aspects, and network. To complete the program, patients work through about fourteen 1-hour lessons. The controlled, randomized study by May and Pfäfflin involved 242 patients (113 treatment, 129 control) aged 16 to 80 years. Patients in the treatment (MOSES) group demonstrated significant improvements in 2 of the 9 modules (knowledge, coping with epilepsy), had improved self-reported seizure outcomes, were more satisfied with therapy, experienced better tolerability of antiepileptic drugs with fewer adverse effects (AEs), and were highly satisfied with the program. The researchers concluded that educational programs, such as MOSES, should become a standard service for specialized epilepsy care.
Developed over many years, WebEase is an online epilepsy self-management program that supports education on medication, stress, and sleep management. In 2011, DiIorio and colleagues reported on a WebEase trial in which 194 patients were randomly assigned to either a treatment group (n = 96) or a wait-list control group (n = 96), and 2 were lost to follow up.11 After accounting for study criteria and study drop out, 70 participants completed the treatment arm, and 78 completed the control arm. The study measured the impact of the platform on multiple outcome metrics, including 3 behavioral areas of focus. At follow-up, self-reported levels of medication adherence were higher for patients in the treatment group than for those in the control group. Analyses also compared patients who completed WebEase modules with those who did not. Patients who completed at least some WebEase modules reported higher levels of self-efficacy, and a trend toward significance was found for medication adherence, perceived stress, self-management, and knowledge. The authors concluded that online tools that support epilepsy self-management could be effective.11
In 2015, Fraser and colleagues reported the results of the Program for Active Consumer Engagement in Self-Management in Epilepsy (PACES in Epilepsy), a consumer-generated self-management program.16 In the trial, 83 adults with chronic epilepsy were initially assigned either to an in-person intervention or to treatment as usual. After study drop outs, 38 patients remained in the intervention arm, with 40 in the control arm. In the intervention, 6 to 8 adults met for a 75-minute group session 1 evening per week for 8 weeks; these sessions were co-led by a psychologist and a trained peer with epilepsy. Topics included medical, psychosocial, cognitive, and self-management aspects of epilepsy, in addition to community integration and optimization of epilepsy-related communication. Outcomes were measured with various instruments, including the ESES, the Quality of Life in Epilepsy-31 (QOLIE-31), the Epilepsy Self-Management Scale (ESMS), the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7. Each test was administered at baseline and after intervention. Outcomes were assessed immediately after program completion (8 weeks) and at follow-up 6 months later.
Findings suggested a substantial positive impact on epilepsy self-management capacities at program completion. In addition, benefit was sustained, particularly for epilepsy information management, over the 6 months after program completion. On the QOLIE-31 at 6 months, management of medication AEs also remained significantly improved, and fatigue management was improved at the P < .05 level. The researchers concluded that the PACES in Epilepsy program might have a more sustained impact on management of disability than on mood. They also noted that the effect was greater immediately after program completion than at 6 months. Patients gave the PACES program high satisfaction ratings.
Although these programs take slightly different approaches to epilepsy self-management, they have a similar focus: directed patient education. Furthermore, most of these programs are conducted in person, usually in a support group setting. In the WebEase trial, patients seem to have completed the online modules in a study setting, and a peer support component was not included. Overall, all programs successfully demonstrated various benefits for trial patients. These outcomes suggest that despite their subtle differences in approach, formal self-management programs are benefiting patients.
None of these platforms was designed for or specifically tested veterans with epilepsy. Although veterans theoretically would benefit from the same tools used by nonveterans, Iraq and Afghanistan veterans with epilepsy are more likely than are those without epilepsy to have mental and physical comorbidities and significantly higher mortality.2 Therefore, veterans potentially could benefit more from evidence-based chronic disease self-management programs designed to reduce physical and psychiatric comorbidities. Furthermore, programs that incorporate peer-to-peer support and direct links to VA care teams and mental health providers could be valuable.18
One research effort that directly addressed these issues is the Policy for Optimized Epilepsy Management (POEM) study, conducted by Hixson and colleagues in 2015.18 This study, not included in the review by Bradley and colleagues, used a purely online- and mobile-based social networking platform to promote self-management practices.19 Unlike the other programs described here, POEM did not require that patients view or attend formal educational seminars, though these seminars were available through the online platform for patient self-directed viewing. In addition, the intervention heavily promoted peer-to-peer engagement and disease tracking as means of increasing self-knowledge and activation. This study was unlike the other platforms in another way: It specifically focused on veterans with epilepsy, based on the idea that many veterans had a shared experience that would optimize a peer support approach.
The POEM investigators did not use a controlled design but found a significant benefit for both ESES and ESMS metrics on within-subject comparisons. Similar to the PACES in Epilepsy study, the POEM study found the highest benefit on the information management subscale of the ESMS.16 Practically speaking, this means patients were better able to use and manage digital and mobile information resources for controlling epilepsy. The POEM study results further reinforced the idea that epilepsy self-management programs are beneficial and expanded on earlier research to emphasize the value of peer support networks and digital interventions that can be used by patients at their convenience. These features provide greater access to more patients and maintain the crucial elements of peer-to-peer learning and counseling.
Implementation Barriers
Confirming the effectiveness of self-management programs is only the beginning of formal implementation and adoption. The real-world success of patient self-management programs has been documented for a few chronic diseases, including epilepsy. However, there is little research or commentary on lessons learned or on the challenges encountered with wide implementation of these programs.
Initial Setup and Sponsorship
To promote wider adoption, researchers should include commentary on initial setup, ongoing patient acceptance, and continual provider support. Many of the initial challenges in self-management programs involve a changing paradigm in the delivery and economics of health care. The transition to a more consumer-oriented health model with an emphasis on outcomes and patient-reported variables likely will support self-management strategies but is only slowly evolving. Many health care providers, hospitals, and payers may not be familiar with or have proper incentivizes to explore self-management tools even when proven effective.
More specifically, these epilepsy self-management programs are treatment adjuncts well suited to military and veteran health care systems. Self-management closely aligns with the overall VHA mission, vision, and values, including formal Department of Veteran Affairs (VA) goals and the MyVA priorities that collectively embrace improvement in access, a veteran-centric approach, and quality for improvement of the entire VA experience. Self-management platforms in the VA are recognized as empowering veterans and are thought to indirectly improve access to health care.20,21
The barriers of sponsorship and financial support likely will persist in the private health care sector but are less likely to significantly affect the VHA. Self-management programs have been researched and implemented for many health conditions across the VHA. For example, the VA Talent Management System course Patient Self-Management: Skill Building (TMS 6467) offers education and training to all clinical practitioners and managers involved in patient education and self-management activities for a variety of chronic medical conditions. Regarding epilepsy self-management more specifically, a patient brochure on the practice is distributed by the VHA Epilepsy Centers of Excellence (ECoEs) and an associated consortium.22 Last, a national provider educational lecture series has a corresponding patient and caregiver lecture set that emphasizes education and self-management behaviors.
Labor, Time, and Resource Needs
The most time-intensive aspect of designing self-management programs is developing the tool that allows clinicians and patients to work together. From a program perspective, the tool must be available and helpful not only to patients and specialists, but also to primary care providers. Tertiary-care centers usually accept the responsibility for program initiation, including patient recruitment, logistics coordination, and health care professional staffing. For epilepsy, the small pool of relevant specialists and centers limits the number of self-management education sessions that can be hosted and increases the need for complex travel and scheduling tasks. However, ECoE communication lines provide a basic infrastructure for collaboration and for development of tools that can be helpful to all clinicians treating veterans with epilepsy.23
Given the issues with coordinating the logistics of in-person programs at brick-and-mortar sites, this type of program may not be the best option for some patients and facilities. Alternative approaches, such as telehealth and asynchronous digital platforms, could expand access and increase convenience. Even though remotely administered programs may not be as powerful for some patients, the promise of scalable access supports consideration of these approaches.
Patient and Caregiver Logistics
Veterans with epilepsy may also have comorbid traumatic brain injury (TBI) and posttraumatic stress disorder, which can complicate self-managed care. In addition, many veterans live in rural areas and have limited travel options. All these factors challenge the success of epilepsy self-management programs. However, the network of ECoEs and associated consortium facilities can step up to deliver self-management tools and information.
The infrastructure of the VHA patient aligned care team (PACT) also contributes to the integration of self-management training. The PACT model takes a personalized, comprehensive, coordinated approach to promote team-based, veteran-centric care and actively partners with other VHA offices to incorporate alternative care services, including peer support and self-management platforms. The combination represents fertile ground for implementation and promotion of self-management tools in the VHA epilepsy population.
Health Care Economics
Given the uncertainties of the US health care economy, it is not surprising that many experts advocate a fundamental redesign of the health care team relationship and information infrastructure.24 This realignment includes partnering directly with patients and their families to encourage more reliance on self-management practices. Unfortunately, this approach does not lend itself to the well-entrenched business model on which most community medical practices are based. Health system leadership often must be convinced there are potential cost savings or a return on investment for new programs. As there is no consistent, comprehensive reimbursement policy for programs focused on self-management, health care systems must be creative and innovative when appraising the financial consequences of such programs.
Epilepsy remains a huge burden. In 2000, the annual total cost of epilepsy treatment in the US was $362 million for new patients and $2 billion for existing cases.25 Within the VHA, the occurrence of posttraumatic epilepsy among the increasing number of veterans with TBI contributes to the burden, and posttraumatic epilepsy and psychogenic nonepileptic seizures complicate treatment approaches. The incidence of comorbidities, including anxiety and depression, has been as high as 50%.23 Epilepsy health care programs are evaluating ways to validate their ability to minimize cost, improve access, and maintain quality of service. Integration of self-management should be included in these efforts.
The VHA represents a unique health care environment for testing and implementing self-management programs. Although the VHA is not immune to the traditional business models of medicine, it is less dependent on them, and it disproportionately cares for patients for long spans of time. From the health care team perspective, data indicate that ECoE physicians represent a high percentage of VHA epilepsy specialists but directly see only about 20% of veterans with an epilepsy or seizure-associated diagnosis. Therefore, future collaboration and connectivity of consortium sites can have a broader impact on self-management—highlighting the fact that concerted, scaled self-management programs have an important role in the VHA health care delivery system and should be promoted.26
Final Insights and Opportunities
Despite the barriers to adoption, formal epilepsy self-management programs are making gains in maturity and academic credibility. As the health care economy gradually shifts to more outcomes-based models, these offerings likely will become more valued, particularly by health care organizations focused on cost sharing, by large self-insuring employers, or organizations like the VHA where patients maintain a long-term relationship. Nevertheless, for the more resource-intensive, in-person self-management programs, adoption may remain constrained. Digital and mobile platforms should serve as more accessible entry points, with lower costs and more rapid scaling potential. Even though these online platforms may not have the same impact as intensive face-to-face programs, their scalability and constant accessibility should make them attractive, and the relatively modest cost of implementing self-guided programs should reduce barriers to adoption.
Integrated health care systems, such as the VHA and various European health systems, can serve as models for self-management implementation. Incorporating a live clinical implementation into parallel research efforts can continue to produce vital academic information on the real-world impact of these solutions, and this evidence in turn can be used to support policies that foster widespread adoption. More specifically, the ECoE model represents a clear opportunity to promote widespread implementation of self-management. The ECoEs are already publishing self-management materials that health care teams can use in patient counseling,and several self-care studies are being conducted within the network.22 In this model, compared with private sector health systems, ECoEs are well positioned to advance the use of formal self-management strategies.
The proposed epilepsy self-management model for ECoEs would be based on an iterative program that incorporates best practices from each of the research studies discussed earlier. With the publication of new research, successful self-management tools would be incorporated into the programs. From a curriculum perspective, educational platforms on medication adherence, seizure safety, and information/data management should be included. Evidence is increasing that peer support and use of licensed peer navigators should be incorporated as well. Last, flexible and asynchronous digital methods should be added to self-management platforms to maximize patient access. These features build on the growing body of evidence to maximize the likelihood of a successful and sustainable self-management strategy for patients with epilepsy.
Click here to read the digital edition.
1. Fiest KM, Sauro KM, Wiebe S, et al. Prevalence and incidence in epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88(3):296-303.
2. Pugh MJ, Van Cott AC, Amuan M, et al. Epilepsy among Iraq and Afghanistan war veterans—United States, 2002-2015. MMWR. 2016;65(44):1224-1227.
3. Kwan P, Brodie MJ. Effectiveness of first antiepileptic drug. Epilepsia. 2001;42(10):1255-1260.
4. Hesdorffer DC, Beck V, Begley CE, et al. Research implications of the Institute of Medicine report, Epilepsy Across the Spectrum: Promoting Health and Understanding. Epilepsia. 2013;54(2):207-216.
5. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
6. Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977.
7. Clark, NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-management of chronic disease by older adults. J Aging Health. 1991;3(1):3-27.
8. Ory MG, Ahn SM, Jiang L, et al. Successes of a national study of the Chronic Disease Self-Management Program: meeting the triple aim of health care reform. Med Care. 2013;51(11):992-998.
9. DiIorio C, Shafer PO, Letz R, Henry TR, Schomer DL, Yeager K; Project EASE Study Group. Behavioral, social and affective factors associated with self-efficacy for self-management among people with epilepsy. Epilepsy Behav. 2006;9(1):158-163.
10. Shegog R, Bamps YA, Patel A, et al. Managing Epilepsy Well: emerging e-tools for epilepsy self-management. Epilepsy Behav. 2013;29(1):133-140.
11. DiIorio C, Bamps Y, Walker ER, Escoffery C. Results of a research study evaluating WebEase, an online epilepsy self-management program. Epilepsy Behav. 2011;22(3):469-474.
12. Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003;30(2):170-195.
13. Helgeson DC, Mittan R, Tan SY, Chayasirisobhon S. Sepulveda Epilepsy Education: the efficacy of a psychoeducational treatment programme in treating medical and psychosocial aspects of epilepsy. Epilepsia. 1990;31(1):75-82.
14. May TW, Pfäfflin M. The efficacy of an educational treatment program for patients with epilepsy (MOSES): results of a controlled, randomized study. Modular Service Package Epilepsy. Epilepsia. 2002;43(5):539-549.
15. Aliasgharpour M, Dehgahn Nayeri N, Yadegary MA, Haghani H. Effects of an educational program on self-management in patients with epilepsy. Seizure. 2013;22(1):48-52.
16. Fraser RT, Johnson EK, Lashley S, et al. PACES in Epilepsy: results of a self-management randomized controlled trial. Epilepsia. 2015;56(8):1264-1274.
17. Laybourne AH, Morgan M, Watkins SH, Lawton R, Ridsdale L, Goldstein LH. Self-management for people with poorly controlled epilepsy: participants’ views of the UK self-management in epilepsy (SMILE) program. Epilepsy Behav. 2015;52(pt A):159-164.
18. Hixson JD, Barnes D, Parko K, et al. Patients optimizing epilepsy management via an online community: the POEM study. Neurology. 2015;85(2):129-136.
19. Bradley PM, Lindsay B, Fleeman N. Care delivery and self-management strategies for adults with epilepsy. Cochrane Database Syst Rev. 2016;2:CD006244.
20. Allicock M, Haynes-Maslow L, Carr C, et al. Training veterans to provide peer support in a weight-management program: MOVE! Prev Chronic Dis. 2013;10:E185.
21. Damush TM, Jackson GL, Powers BJ, et al. Implementing evidence-based patient self-management programs in the Veterans Health Administration: perspectives on delivery system design considerations. J Gen Intern Med. 2010;25(suppl 1):68-71.
22. Caraveo N, Chen S, Evrard C, Ozuna J; Epilepsy Centers of Excellence Nursing Workgroup. Self-management in epilepsy: a guide for healthcare professionals. https://www.epilepsy.va.gov/Library/Self-Management%20In%20Epilepsy.pdf. Published Winter 2015. Accessed February 26, 2018.
23. Rehman R, Kelly PR, Husain AM, Tran TT. Characteristics of veterans diagnosed with seizures within the Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762.
24. Merry MD. Healthcare’s need for revolutionary change. Quality Prog. 2003;36(9):31-35.
25. Halpern M, Rentz A, Murray M. Cost of illness of epilepsy in the US: comparison of patient-based and population-based estimates. Neuroepidemiology. 2000;19(2):87-99.
26. Kelly P, Chinta R. Do centers of excellence excel in patient outcomes?: Evidence from U.S. Veterans Health Administration Centers for Epilepsy. Int J Manage Excellence. 2015;4(3):529-538.
1. Fiest KM, Sauro KM, Wiebe S, et al. Prevalence and incidence in epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88(3):296-303.
2. Pugh MJ, Van Cott AC, Amuan M, et al. Epilepsy among Iraq and Afghanistan war veterans—United States, 2002-2015. MMWR. 2016;65(44):1224-1227.
3. Kwan P, Brodie MJ. Effectiveness of first antiepileptic drug. Epilepsia. 2001;42(10):1255-1260.
4. Hesdorffer DC, Beck V, Begley CE, et al. Research implications of the Institute of Medicine report, Epilepsy Across the Spectrum: Promoting Health and Understanding. Epilepsia. 2013;54(2):207-216.
5. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
6. Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977.
7. Clark, NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-management of chronic disease by older adults. J Aging Health. 1991;3(1):3-27.
8. Ory MG, Ahn SM, Jiang L, et al. Successes of a national study of the Chronic Disease Self-Management Program: meeting the triple aim of health care reform. Med Care. 2013;51(11):992-998.
9. DiIorio C, Shafer PO, Letz R, Henry TR, Schomer DL, Yeager K; Project EASE Study Group. Behavioral, social and affective factors associated with self-efficacy for self-management among people with epilepsy. Epilepsy Behav. 2006;9(1):158-163.
10. Shegog R, Bamps YA, Patel A, et al. Managing Epilepsy Well: emerging e-tools for epilepsy self-management. Epilepsy Behav. 2013;29(1):133-140.
11. DiIorio C, Bamps Y, Walker ER, Escoffery C. Results of a research study evaluating WebEase, an online epilepsy self-management program. Epilepsy Behav. 2011;22(3):469-474.
12. Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003;30(2):170-195.
13. Helgeson DC, Mittan R, Tan SY, Chayasirisobhon S. Sepulveda Epilepsy Education: the efficacy of a psychoeducational treatment programme in treating medical and psychosocial aspects of epilepsy. Epilepsia. 1990;31(1):75-82.
14. May TW, Pfäfflin M. The efficacy of an educational treatment program for patients with epilepsy (MOSES): results of a controlled, randomized study. Modular Service Package Epilepsy. Epilepsia. 2002;43(5):539-549.
15. Aliasgharpour M, Dehgahn Nayeri N, Yadegary MA, Haghani H. Effects of an educational program on self-management in patients with epilepsy. Seizure. 2013;22(1):48-52.
16. Fraser RT, Johnson EK, Lashley S, et al. PACES in Epilepsy: results of a self-management randomized controlled trial. Epilepsia. 2015;56(8):1264-1274.
17. Laybourne AH, Morgan M, Watkins SH, Lawton R, Ridsdale L, Goldstein LH. Self-management for people with poorly controlled epilepsy: participants’ views of the UK self-management in epilepsy (SMILE) program. Epilepsy Behav. 2015;52(pt A):159-164.
18. Hixson JD, Barnes D, Parko K, et al. Patients optimizing epilepsy management via an online community: the POEM study. Neurology. 2015;85(2):129-136.
19. Bradley PM, Lindsay B, Fleeman N. Care delivery and self-management strategies for adults with epilepsy. Cochrane Database Syst Rev. 2016;2:CD006244.
20. Allicock M, Haynes-Maslow L, Carr C, et al. Training veterans to provide peer support in a weight-management program: MOVE! Prev Chronic Dis. 2013;10:E185.
21. Damush TM, Jackson GL, Powers BJ, et al. Implementing evidence-based patient self-management programs in the Veterans Health Administration: perspectives on delivery system design considerations. J Gen Intern Med. 2010;25(suppl 1):68-71.
22. Caraveo N, Chen S, Evrard C, Ozuna J; Epilepsy Centers of Excellence Nursing Workgroup. Self-management in epilepsy: a guide for healthcare professionals. https://www.epilepsy.va.gov/Library/Self-Management%20In%20Epilepsy.pdf. Published Winter 2015. Accessed February 26, 2018.
23. Rehman R, Kelly PR, Husain AM, Tran TT. Characteristics of veterans diagnosed with seizures within the Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762.
24. Merry MD. Healthcare’s need for revolutionary change. Quality Prog. 2003;36(9):31-35.
25. Halpern M, Rentz A, Murray M. Cost of illness of epilepsy in the US: comparison of patient-based and population-based estimates. Neuroepidemiology. 2000;19(2):87-99.
26. Kelly P, Chinta R. Do centers of excellence excel in patient outcomes?: Evidence from U.S. Veterans Health Administration Centers for Epilepsy. Int J Manage Excellence. 2015;4(3):529-538.