User login
Epidermodysplasia Verruciformis: Successful Treatment With Squaric Acid Dibutylester
Epidermodysplasia verruciformis (EV) is an uncommon autosomal-recessive inherited disorder characterized by disseminated cutaneous warts in predisposed patients who are highly susceptible to genus â-papillomavirus infections. Squaric acid dibutylester (SADBE) is a contact sensitizer agent that has gained general acceptance over the years for the treatment of a variety of dermatologic diseases, including alopecia areata and cutaneous warts. We report the case of a 40-year-old woman with a balanced chromosomal translocation and lymphocytopenia who presented with the sole clinical finding of refractory multiple flat warts that had been present for 25 years. After failed attempts at therapy with oral isotretinoin, cryotherapy with topical trichloroacetic acid, and topical tretinoin, the lesions were successfully eradicated with topical SADBE with prior sensitization.
Case Report
A 40-year-old woman presented with multiple flat warts on the bilateral arms and legs of 25 years’ duration (Figure 1) that had been unsuccessfully treated by an outside physician with imiquimod cream 5% and tazarotene gel 0.1%. Her medical history was remarkable for recurrent upper respiratory tract infections, urinary tract infections, yeast infections, and otitis media. She also reported a history of 6 spontaneous miscarriages that had been attributed to a balanced chromosomal translocation between chromosomes 12 and 14.
  |
Laboratory evaluation revealed leukopenia, lymphopenia, and hypogammaglobulinemia, with a white blood cell count of 3600/μL (reference range, 4500–11,000/mL), a lymphocyte count of 12.1% (20%–45%), absolute CD4 count of 77 cells/μL (490–1740 cells/μL), absolute CD8 count of 56 cells/mL (180–1170 cells/μL), and serum IgM level of 17 mg/dL (48–271 mg/dL). Human immunodeficiency virus (HIV) titers were negative.
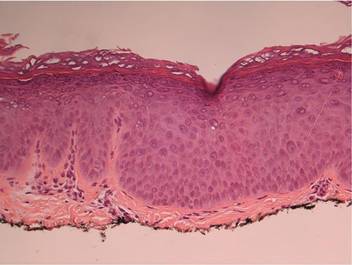
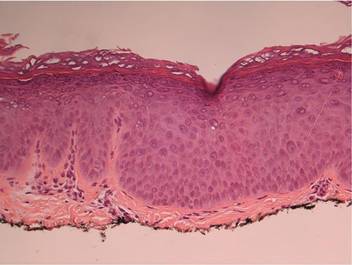
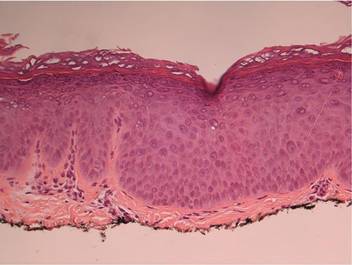
On physical examination numerous pink, flat-topped papules were noted on the forehead and bilateral arms and legs. Histologic analysis of a tangential plane biopsy of a lesion on the right leg revealed hyperkeratosis of the stratum corneum and epidermal hyperplasia (Figure 2). The epidermis also showed focal papillomatosis with areas of hypergranulosis and viropathic changes; these findings were consistent with a diagnosis of verruca plana. Human papillomavirus (HPV) DNA typing by polymerase chain reaction from the verrucous lesions showed HPV type 20, which has been associated with EV. Based on the patient’s clinical findings and HPV subtype, she was diagnosed with atypical EV.
Subsequent treatment with liquid nitrogen, tretinoin cream 0.1%, and topical trichloroacetic acid 50% failed. She received oral isotretinoin at a dosage of 80 mg daily for 9 months, but the lesions persisted and she developed alopecia and ankle stiffness; therefore, the isotretinoin was discontinued. Candida antigen testing revealed that the patient was anergic, and SADBE sensitization was subsequently initiated. Squaric acid dibutylester was utilized as a sensitizing agent, and it was formulated as 2% and 0.2% solutions in acetone, supplied in 20-mL tinted glass bottles.
Squaric acid dibutylester solution 2% under occlusion was applied to a test area on the right forearm. Three days later, results indicated prominent erythema and inflammation at the application site. Two weeks later, a chronic dermatitic response was noted at the test site (Figure 3). Squaric acid dibutylester 0.2% was then applied to an affected area on the right shin and was kept under occlusion for 48 hours. One month later, no notable changes in the lesions were observed, and no further treatments were performed. Three months later, the patient returned for evaluation and it was noted that the flat warts on the right shin that had been treated with SADBE 0.2% 4 months prior had resolved (Figure 4). Subsequently, it was noted that all of the lesions had regressed, even those that had not been treated with SADBE.
Comment
Epidermodysplasia verruciformis is a rare genodermatosis caused by a group of phylogenetically related viruses1 belonging to the β-papillomavirus genus.2,3 It is characterized by a combination of pityriasis versicolor–like lesions, reddish verrucalike plaques, and seborrheic keratosis–like plaques,1,4 preferentially on sun-exposed areas.5 The lesions undergo malignant transformation in 30% to 60% of patients,3,6 especially into squamous cell carcinomas.7 The most frequent HPV types found in EV skin lesions are 5, 8, 9, 12, 14, 15, 17, and 19 to 25; types 5 and 8 are found in 90% of cutaneous squamous cell carcinomas in EV patients.2 Human papillomavirus type 20, the type identified in our patient, has been isolated from warts in EV patients,1,2 though it is not the most common type. It has been shown that more than one HPV type could be present concurrently in the same EV patient,1 which necessitates close follow-up for skin cancer evaluation in all EV patients, as oncogenic strains may be present in some lesions.
  |
Epidermodysplasia verruciformis has no particular predisposition for race or geographic location.1,7 It usually is inherited in an autosomal-recessive fashion1,4,7 and has been linked to mutations in 2 EV genes located on chromosome 17: EVER1/TCM6 and EVER2/TCM8.8 However, approximately 25% of EV cases are not associated with these gene mutations,5,9 as demonstrated in our patient. Autosomal-dominant or X-linked mutations also have been reported.10 In our case, a chromosomal abnormality in the form of a balanced chromosomal translocation was present, which is unique. A connection between EV and balanced chromosomal translocation cannot be excluded and warrants further investigation.
Epidermodysplasia verruciformis has been associated with decreased cell-mediated immunity.1,7 However, nonimmunologic factors likely contribute considering the rarity of EV-like eruptions in immunodeficiency disorders11 as well as its frequent coinfection with HPV type 312 and its association with EVER1/TCM6 and EVER2/TCM8.8 Epidermodysplasia verruciformis–like lesions have been reported in several immunosuppressed states, including HIV infection,13 combined variable immunodeficiency syndrome,14 IgM deficiency,15 and CD4+ T-cell lymphocytopenia.11 Our patient’s findings fit the latter diagnostic criteria, as she had a chronically low CD4 count of 77 cells/μL, negative HIV titers, and absence of alternative explanation to the lymphopenia. Thus, we could consider her as having EV, as a low CD4 count is a known association. Her immunodeficient state could possibly be attributed to the chromosomal translocation; however, the genetic loci surrounding the chromosomal translocation have not been identified to date, leaving this hypothesis unsubstantiated. Nevertheless, in our otherwise healthy patient, no explanation was found as to why a cell-mediated deficiency would selectively favor a cutaneous HPV infection. According to Zavattaro et al,5 a possible cause could be the presence of additional genetic or environmental factors in the patient that predisposed her to this particular infection.
Every patient with EV requires close lifelong observation for skin cancer and education regarding strict sun avoidance and protection.1 Treatment options for the lesions include topical therapies with imiquimod 5%, immunomodulators, and salicylic acid16,17; oral isotretinoin18; and combinations of acitretin and interferon alfa.19 Physical ablative procedures also have been proposed, including cryotherapy with liquid nitrogen, electrosurgery, surgical excision, and laser therapies.20
Topical immunotherapy with SADBE initially was used to treat refractory alopecia areata and also has been described in the treatment of recalcitrant warts.21-24 Historically, 2,4-dinitrochlorobenzene was used for contact immunotherapy in wart management but is now avoided due to its mutagenic potential.25 Squaric acid dibutylester and diphenylcyclopropenone currently are the favored contact sensitizers, with a resolution rate of 60% reported in refractory warts.26
Topical immunotherapy involves sensitization of the patient with high-concentration (2%) SADBE on a small surface area until an eczematous dermatitis appears. The rash indicates sensitization has been achieved, and then a lower-concentration SADBE is applied to the warts. Observation of mild contact dermatitis should not be an indication to stop treatment, as this effect is an integral part of therapeutic response. No serious side effects were reported to SADBE; erythema, desquamation, edema, itching, and burning were described.23
The mechanism of action of SADBE is not clear. The most common proposed theory is the induction of a type IV hypersensitivity reaction in the warts, leading to their destruction. Other authors suggest that wart resolution is caused by a nonspecific inflammatory reaction. An argument in favor of the latter hypothesis is the spontaneous regression of untreated warts in patients treated with SADBE at a remote site, suggesting a mechanism of action beyond a simple cell-mediated process.23
Epidermodysplasia verruciformis should be included in the differential diagnosis for any eruptive, warty, papular, and plaque-type lesions that appear in immunocompromised individuals. Moreover, the diagnosis of idiopathic CD4+ T-cell lymphocytopenia should be considered in any patient with a CD4 count deficit presenting with widespread viral, fungal, or mycobacterial infection with negative HIV test. Appropriate evaluation of the absolute CD4+ counts also should be performed. In our case, it was hypothesized that the patient’s balanced chromosomal translocation was related to her lymphopenia and EV, though this correlation has yet to be confirmed. However, it is notable that her son carried the same translocation and has a normal white blood cell count and no evidence of flat warts. This case demonstrates the success of contact immunotherapy in treating these widespread and often recalcitrant lesions.
1. Vohra S, Sharma NL, Shanker V, et al. Autosomal dominant epidermodysplasia verruciformis: a clinicotherapeutic experience in two cases. Indian J Dermatol Venereol Leprol. 2010;76:557-561.
2. Dell’Oste V, Azzimonti B, De Andrea M, et al. High beta-HPV DNA loads and strong seroreactivity are present in epidermodysplasia verruciformis. J Invest Dermatol. 2009;129:1026-1034.
3. Orth G. Epidermodysplasia verruciformis: a model for understanding the oncogenicity of human papillomavirus. Ciba Found Symp. 1986;120:157-174.
4. Michael KM, Waterboer T, Pfister H, et al. Seroreactivity of 38 human papillomavirus types in epidermodysplasia verruciformis patients, relatives, and controls. J Invest Dermatol. 2010;130:841-848.
5. Zavattaro E, Azzimonti B, Mondini M, et al. Identification of defective Fas function and variation of the perforin gene in an epidermodysplasia verruciformis patient lacking EVER1 and EVER2 mutations. J Invest Dermatol. 2008;128:732-735.
6. Majewski S, Jabłońska S. Epidermodysplasia verruciformis as a model of human papillomavirus-induced genetic cancer of the skin. Arch Dermatol. 1995;131:1312-1318.
7. Robati RM, Marefat A, Saeedi M, et al. Four familial cases of epidermodysplasia verruciformis: mother and three sons. Dermatol Online J. 2009;15:8.
8. Ramoz N, Rueda LA, Bouadjar B, et al. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet. 2002;32:579-581.
9. Azzimonti B, Mondini M, De Andrea M, et al. CD8+ T-cell lymphocytopenia and lack of EVER mutations in a patient with clinically and virologically typical epidermodysplasia verruciformis. Arch Dermatol. 2005;141:1323-1325.
10. Androphy EJ, Dvoretzky I, Lowy DR. X-linked inheritance of epidermodysplasia verruciformis. genetic and virologic studies of a kindred. Arch Dermatol. 1985;121:864-868.
11. Tobin E, Rohwedder A, Holland SM, et al. Recurrent ‘sterile’ verrucous cyst abscesses and epidermodysplasia verruciformis-like eruption associated with idiopathic CD4 lymphopenia. Br J Dermatol. 2003;149:627-633.
12. Obalek S, Favre M, Szymanczyk J, et al. Human papillomavirus (HPV) types specific of epidermodysplasia verruciformis detected in warts induced by HPV3 or HPV3-related types in immunosuppressed patients. J Invest Dermatol. 1992;98:936-941.
13. Berk DR, Bruckner AL, Lu D. Epidermodysplasia verruciform-like lesions in an HIV patient. Dermatol Online J. 2009;15:1.
14. Vu J, Wallace GR, Singh R, et al. Common variable immunodeficiency syndrome associated with epidermodysplasia verruciformis. Am J Clin Dermatol. 2007;8:307-310.
15. Gul U, Soylu S, Yavuzer R. Epidermodysplasia verruciformis associated with IgM deficiency. Indian J Dermatol Venereol Leprol. 2007;73:420-422.
16. De Oliveira WR, Festa Neto C, Rady PL, et al. Clinical aspects of epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol. 2003;17:394-398.
17. Jablonska S, Majewski S. Epidermodysplasia verruciformis: what’s new? J Eur Acad Dermatol Venereol. 2003;17:381-382.
18. Rallis E, Papatheodorou G, Bimpakis E, et al. Systemic low-dose isotretinoin maintains remission status in epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol. 2008;22:523-525.
19. Anadolu R, Oskay T, Erdem C, et al. Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol. 2001;45:296-299.
20. Fang F, Zhao L, Jiang MJ, et al. Epidermodysplasia verruciformis with severe hand and foot deformity successfully treated with surgical excision. J Plast Reconstr Aesthet Surg. 2008;61:338-341.
21. Huang W, Morrell D. Successful treatment of recalcitrant warts with topical squaric acid in immunosuppressed child. Pediatr Dermatol. 2008;25:275-276.
22. Hama N, Hatamochi A, Hayashi S, et al. Usefulness of topical immunotherapy with squaric acid dibutylester for refractory common warts on the face and neck. J Dermatol. 2009;36:660-662.
23. Micali G, Nasca MR, Tedeschi A, et al. Use of squaric acid dibutylester (SADBE) for cutaneous warts in children. Pediatr Dermatol. 2000;17:315-318.
24. Mastrolonardo M, Lopalco PL, Diaferio A. Topical immunotherapy with contact sensitizers: a model to study the natural history of delayedhypersensitivity. Contact Dermatitis. 2002;47:210-214.
25. Lewis HM. Topical immunotherapy of refractory warts. Cutis. 1973;12:863-869.
26. Weisshaar E, Neumann HJ, Gollnick H. Successful treatment of disseminated facial verrucae with contact immunotherapy. Eur J Dermatol. 1998;8:488-491.
Epidermodysplasia verruciformis (EV) is an uncommon autosomal-recessive inherited disorder characterized by disseminated cutaneous warts in predisposed patients who are highly susceptible to genus â-papillomavirus infections. Squaric acid dibutylester (SADBE) is a contact sensitizer agent that has gained general acceptance over the years for the treatment of a variety of dermatologic diseases, including alopecia areata and cutaneous warts. We report the case of a 40-year-old woman with a balanced chromosomal translocation and lymphocytopenia who presented with the sole clinical finding of refractory multiple flat warts that had been present for 25 years. After failed attempts at therapy with oral isotretinoin, cryotherapy with topical trichloroacetic acid, and topical tretinoin, the lesions were successfully eradicated with topical SADBE with prior sensitization.
Case Report
A 40-year-old woman presented with multiple flat warts on the bilateral arms and legs of 25 years’ duration (Figure 1) that had been unsuccessfully treated by an outside physician with imiquimod cream 5% and tazarotene gel 0.1%. Her medical history was remarkable for recurrent upper respiratory tract infections, urinary tract infections, yeast infections, and otitis media. She also reported a history of 6 spontaneous miscarriages that had been attributed to a balanced chromosomal translocation between chromosomes 12 and 14.
  |
Laboratory evaluation revealed leukopenia, lymphopenia, and hypogammaglobulinemia, with a white blood cell count of 3600/μL (reference range, 4500–11,000/mL), a lymphocyte count of 12.1% (20%–45%), absolute CD4 count of 77 cells/μL (490–1740 cells/μL), absolute CD8 count of 56 cells/mL (180–1170 cells/μL), and serum IgM level of 17 mg/dL (48–271 mg/dL). Human immunodeficiency virus (HIV) titers were negative.
On physical examination numerous pink, flat-topped papules were noted on the forehead and bilateral arms and legs. Histologic analysis of a tangential plane biopsy of a lesion on the right leg revealed hyperkeratosis of the stratum corneum and epidermal hyperplasia (Figure 2). The epidermis also showed focal papillomatosis with areas of hypergranulosis and viropathic changes; these findings were consistent with a diagnosis of verruca plana. Human papillomavirus (HPV) DNA typing by polymerase chain reaction from the verrucous lesions showed HPV type 20, which has been associated with EV. Based on the patient’s clinical findings and HPV subtype, she was diagnosed with atypical EV.
Subsequent treatment with liquid nitrogen, tretinoin cream 0.1%, and topical trichloroacetic acid 50% failed. She received oral isotretinoin at a dosage of 80 mg daily for 9 months, but the lesions persisted and she developed alopecia and ankle stiffness; therefore, the isotretinoin was discontinued. Candida antigen testing revealed that the patient was anergic, and SADBE sensitization was subsequently initiated. Squaric acid dibutylester was utilized as a sensitizing agent, and it was formulated as 2% and 0.2% solutions in acetone, supplied in 20-mL tinted glass bottles.
Squaric acid dibutylester solution 2% under occlusion was applied to a test area on the right forearm. Three days later, results indicated prominent erythema and inflammation at the application site. Two weeks later, a chronic dermatitic response was noted at the test site (Figure 3). Squaric acid dibutylester 0.2% was then applied to an affected area on the right shin and was kept under occlusion for 48 hours. One month later, no notable changes in the lesions were observed, and no further treatments were performed. Three months later, the patient returned for evaluation and it was noted that the flat warts on the right shin that had been treated with SADBE 0.2% 4 months prior had resolved (Figure 4). Subsequently, it was noted that all of the lesions had regressed, even those that had not been treated with SADBE.
Comment
Epidermodysplasia verruciformis is a rare genodermatosis caused by a group of phylogenetically related viruses1 belonging to the β-papillomavirus genus.2,3 It is characterized by a combination of pityriasis versicolor–like lesions, reddish verrucalike plaques, and seborrheic keratosis–like plaques,1,4 preferentially on sun-exposed areas.5 The lesions undergo malignant transformation in 30% to 60% of patients,3,6 especially into squamous cell carcinomas.7 The most frequent HPV types found in EV skin lesions are 5, 8, 9, 12, 14, 15, 17, and 19 to 25; types 5 and 8 are found in 90% of cutaneous squamous cell carcinomas in EV patients.2 Human papillomavirus type 20, the type identified in our patient, has been isolated from warts in EV patients,1,2 though it is not the most common type. It has been shown that more than one HPV type could be present concurrently in the same EV patient,1 which necessitates close follow-up for skin cancer evaluation in all EV patients, as oncogenic strains may be present in some lesions.
  |
Epidermodysplasia verruciformis has no particular predisposition for race or geographic location.1,7 It usually is inherited in an autosomal-recessive fashion1,4,7 and has been linked to mutations in 2 EV genes located on chromosome 17: EVER1/TCM6 and EVER2/TCM8.8 However, approximately 25% of EV cases are not associated with these gene mutations,5,9 as demonstrated in our patient. Autosomal-dominant or X-linked mutations also have been reported.10 In our case, a chromosomal abnormality in the form of a balanced chromosomal translocation was present, which is unique. A connection between EV and balanced chromosomal translocation cannot be excluded and warrants further investigation.
Epidermodysplasia verruciformis has been associated with decreased cell-mediated immunity.1,7 However, nonimmunologic factors likely contribute considering the rarity of EV-like eruptions in immunodeficiency disorders11 as well as its frequent coinfection with HPV type 312 and its association with EVER1/TCM6 and EVER2/TCM8.8 Epidermodysplasia verruciformis–like lesions have been reported in several immunosuppressed states, including HIV infection,13 combined variable immunodeficiency syndrome,14 IgM deficiency,15 and CD4+ T-cell lymphocytopenia.11 Our patient’s findings fit the latter diagnostic criteria, as she had a chronically low CD4 count of 77 cells/μL, negative HIV titers, and absence of alternative explanation to the lymphopenia. Thus, we could consider her as having EV, as a low CD4 count is a known association. Her immunodeficient state could possibly be attributed to the chromosomal translocation; however, the genetic loci surrounding the chromosomal translocation have not been identified to date, leaving this hypothesis unsubstantiated. Nevertheless, in our otherwise healthy patient, no explanation was found as to why a cell-mediated deficiency would selectively favor a cutaneous HPV infection. According to Zavattaro et al,5 a possible cause could be the presence of additional genetic or environmental factors in the patient that predisposed her to this particular infection.
Every patient with EV requires close lifelong observation for skin cancer and education regarding strict sun avoidance and protection.1 Treatment options for the lesions include topical therapies with imiquimod 5%, immunomodulators, and salicylic acid16,17; oral isotretinoin18; and combinations of acitretin and interferon alfa.19 Physical ablative procedures also have been proposed, including cryotherapy with liquid nitrogen, electrosurgery, surgical excision, and laser therapies.20
Topical immunotherapy with SADBE initially was used to treat refractory alopecia areata and also has been described in the treatment of recalcitrant warts.21-24 Historically, 2,4-dinitrochlorobenzene was used for contact immunotherapy in wart management but is now avoided due to its mutagenic potential.25 Squaric acid dibutylester and diphenylcyclopropenone currently are the favored contact sensitizers, with a resolution rate of 60% reported in refractory warts.26
Topical immunotherapy involves sensitization of the patient with high-concentration (2%) SADBE on a small surface area until an eczematous dermatitis appears. The rash indicates sensitization has been achieved, and then a lower-concentration SADBE is applied to the warts. Observation of mild contact dermatitis should not be an indication to stop treatment, as this effect is an integral part of therapeutic response. No serious side effects were reported to SADBE; erythema, desquamation, edema, itching, and burning were described.23
The mechanism of action of SADBE is not clear. The most common proposed theory is the induction of a type IV hypersensitivity reaction in the warts, leading to their destruction. Other authors suggest that wart resolution is caused by a nonspecific inflammatory reaction. An argument in favor of the latter hypothesis is the spontaneous regression of untreated warts in patients treated with SADBE at a remote site, suggesting a mechanism of action beyond a simple cell-mediated process.23
Epidermodysplasia verruciformis should be included in the differential diagnosis for any eruptive, warty, papular, and plaque-type lesions that appear in immunocompromised individuals. Moreover, the diagnosis of idiopathic CD4+ T-cell lymphocytopenia should be considered in any patient with a CD4 count deficit presenting with widespread viral, fungal, or mycobacterial infection with negative HIV test. Appropriate evaluation of the absolute CD4+ counts also should be performed. In our case, it was hypothesized that the patient’s balanced chromosomal translocation was related to her lymphopenia and EV, though this correlation has yet to be confirmed. However, it is notable that her son carried the same translocation and has a normal white blood cell count and no evidence of flat warts. This case demonstrates the success of contact immunotherapy in treating these widespread and often recalcitrant lesions.
Epidermodysplasia verruciformis (EV) is an uncommon autosomal-recessive inherited disorder characterized by disseminated cutaneous warts in predisposed patients who are highly susceptible to genus â-papillomavirus infections. Squaric acid dibutylester (SADBE) is a contact sensitizer agent that has gained general acceptance over the years for the treatment of a variety of dermatologic diseases, including alopecia areata and cutaneous warts. We report the case of a 40-year-old woman with a balanced chromosomal translocation and lymphocytopenia who presented with the sole clinical finding of refractory multiple flat warts that had been present for 25 years. After failed attempts at therapy with oral isotretinoin, cryotherapy with topical trichloroacetic acid, and topical tretinoin, the lesions were successfully eradicated with topical SADBE with prior sensitization.
Case Report
A 40-year-old woman presented with multiple flat warts on the bilateral arms and legs of 25 years’ duration (Figure 1) that had been unsuccessfully treated by an outside physician with imiquimod cream 5% and tazarotene gel 0.1%. Her medical history was remarkable for recurrent upper respiratory tract infections, urinary tract infections, yeast infections, and otitis media. She also reported a history of 6 spontaneous miscarriages that had been attributed to a balanced chromosomal translocation between chromosomes 12 and 14.
  |
Laboratory evaluation revealed leukopenia, lymphopenia, and hypogammaglobulinemia, with a white blood cell count of 3600/μL (reference range, 4500–11,000/mL), a lymphocyte count of 12.1% (20%–45%), absolute CD4 count of 77 cells/μL (490–1740 cells/μL), absolute CD8 count of 56 cells/mL (180–1170 cells/μL), and serum IgM level of 17 mg/dL (48–271 mg/dL). Human immunodeficiency virus (HIV) titers were negative.
On physical examination numerous pink, flat-topped papules were noted on the forehead and bilateral arms and legs. Histologic analysis of a tangential plane biopsy of a lesion on the right leg revealed hyperkeratosis of the stratum corneum and epidermal hyperplasia (Figure 2). The epidermis also showed focal papillomatosis with areas of hypergranulosis and viropathic changes; these findings were consistent with a diagnosis of verruca plana. Human papillomavirus (HPV) DNA typing by polymerase chain reaction from the verrucous lesions showed HPV type 20, which has been associated with EV. Based on the patient’s clinical findings and HPV subtype, she was diagnosed with atypical EV.
Subsequent treatment with liquid nitrogen, tretinoin cream 0.1%, and topical trichloroacetic acid 50% failed. She received oral isotretinoin at a dosage of 80 mg daily for 9 months, but the lesions persisted and she developed alopecia and ankle stiffness; therefore, the isotretinoin was discontinued. Candida antigen testing revealed that the patient was anergic, and SADBE sensitization was subsequently initiated. Squaric acid dibutylester was utilized as a sensitizing agent, and it was formulated as 2% and 0.2% solutions in acetone, supplied in 20-mL tinted glass bottles.
Squaric acid dibutylester solution 2% under occlusion was applied to a test area on the right forearm. Three days later, results indicated prominent erythema and inflammation at the application site. Two weeks later, a chronic dermatitic response was noted at the test site (Figure 3). Squaric acid dibutylester 0.2% was then applied to an affected area on the right shin and was kept under occlusion for 48 hours. One month later, no notable changes in the lesions were observed, and no further treatments were performed. Three months later, the patient returned for evaluation and it was noted that the flat warts on the right shin that had been treated with SADBE 0.2% 4 months prior had resolved (Figure 4). Subsequently, it was noted that all of the lesions had regressed, even those that had not been treated with SADBE.
Comment
Epidermodysplasia verruciformis is a rare genodermatosis caused by a group of phylogenetically related viruses1 belonging to the β-papillomavirus genus.2,3 It is characterized by a combination of pityriasis versicolor–like lesions, reddish verrucalike plaques, and seborrheic keratosis–like plaques,1,4 preferentially on sun-exposed areas.5 The lesions undergo malignant transformation in 30% to 60% of patients,3,6 especially into squamous cell carcinomas.7 The most frequent HPV types found in EV skin lesions are 5, 8, 9, 12, 14, 15, 17, and 19 to 25; types 5 and 8 are found in 90% of cutaneous squamous cell carcinomas in EV patients.2 Human papillomavirus type 20, the type identified in our patient, has been isolated from warts in EV patients,1,2 though it is not the most common type. It has been shown that more than one HPV type could be present concurrently in the same EV patient,1 which necessitates close follow-up for skin cancer evaluation in all EV patients, as oncogenic strains may be present in some lesions.
  |
Epidermodysplasia verruciformis has no particular predisposition for race or geographic location.1,7 It usually is inherited in an autosomal-recessive fashion1,4,7 and has been linked to mutations in 2 EV genes located on chromosome 17: EVER1/TCM6 and EVER2/TCM8.8 However, approximately 25% of EV cases are not associated with these gene mutations,5,9 as demonstrated in our patient. Autosomal-dominant or X-linked mutations also have been reported.10 In our case, a chromosomal abnormality in the form of a balanced chromosomal translocation was present, which is unique. A connection between EV and balanced chromosomal translocation cannot be excluded and warrants further investigation.
Epidermodysplasia verruciformis has been associated with decreased cell-mediated immunity.1,7 However, nonimmunologic factors likely contribute considering the rarity of EV-like eruptions in immunodeficiency disorders11 as well as its frequent coinfection with HPV type 312 and its association with EVER1/TCM6 and EVER2/TCM8.8 Epidermodysplasia verruciformis–like lesions have been reported in several immunosuppressed states, including HIV infection,13 combined variable immunodeficiency syndrome,14 IgM deficiency,15 and CD4+ T-cell lymphocytopenia.11 Our patient’s findings fit the latter diagnostic criteria, as she had a chronically low CD4 count of 77 cells/μL, negative HIV titers, and absence of alternative explanation to the lymphopenia. Thus, we could consider her as having EV, as a low CD4 count is a known association. Her immunodeficient state could possibly be attributed to the chromosomal translocation; however, the genetic loci surrounding the chromosomal translocation have not been identified to date, leaving this hypothesis unsubstantiated. Nevertheless, in our otherwise healthy patient, no explanation was found as to why a cell-mediated deficiency would selectively favor a cutaneous HPV infection. According to Zavattaro et al,5 a possible cause could be the presence of additional genetic or environmental factors in the patient that predisposed her to this particular infection.
Every patient with EV requires close lifelong observation for skin cancer and education regarding strict sun avoidance and protection.1 Treatment options for the lesions include topical therapies with imiquimod 5%, immunomodulators, and salicylic acid16,17; oral isotretinoin18; and combinations of acitretin and interferon alfa.19 Physical ablative procedures also have been proposed, including cryotherapy with liquid nitrogen, electrosurgery, surgical excision, and laser therapies.20
Topical immunotherapy with SADBE initially was used to treat refractory alopecia areata and also has been described in the treatment of recalcitrant warts.21-24 Historically, 2,4-dinitrochlorobenzene was used for contact immunotherapy in wart management but is now avoided due to its mutagenic potential.25 Squaric acid dibutylester and diphenylcyclopropenone currently are the favored contact sensitizers, with a resolution rate of 60% reported in refractory warts.26
Topical immunotherapy involves sensitization of the patient with high-concentration (2%) SADBE on a small surface area until an eczematous dermatitis appears. The rash indicates sensitization has been achieved, and then a lower-concentration SADBE is applied to the warts. Observation of mild contact dermatitis should not be an indication to stop treatment, as this effect is an integral part of therapeutic response. No serious side effects were reported to SADBE; erythema, desquamation, edema, itching, and burning were described.23
The mechanism of action of SADBE is not clear. The most common proposed theory is the induction of a type IV hypersensitivity reaction in the warts, leading to their destruction. Other authors suggest that wart resolution is caused by a nonspecific inflammatory reaction. An argument in favor of the latter hypothesis is the spontaneous regression of untreated warts in patients treated with SADBE at a remote site, suggesting a mechanism of action beyond a simple cell-mediated process.23
Epidermodysplasia verruciformis should be included in the differential diagnosis for any eruptive, warty, papular, and plaque-type lesions that appear in immunocompromised individuals. Moreover, the diagnosis of idiopathic CD4+ T-cell lymphocytopenia should be considered in any patient with a CD4 count deficit presenting with widespread viral, fungal, or mycobacterial infection with negative HIV test. Appropriate evaluation of the absolute CD4+ counts also should be performed. In our case, it was hypothesized that the patient’s balanced chromosomal translocation was related to her lymphopenia and EV, though this correlation has yet to be confirmed. However, it is notable that her son carried the same translocation and has a normal white blood cell count and no evidence of flat warts. This case demonstrates the success of contact immunotherapy in treating these widespread and often recalcitrant lesions.
1. Vohra S, Sharma NL, Shanker V, et al. Autosomal dominant epidermodysplasia verruciformis: a clinicotherapeutic experience in two cases. Indian J Dermatol Venereol Leprol. 2010;76:557-561.
2. Dell’Oste V, Azzimonti B, De Andrea M, et al. High beta-HPV DNA loads and strong seroreactivity are present in epidermodysplasia verruciformis. J Invest Dermatol. 2009;129:1026-1034.
3. Orth G. Epidermodysplasia verruciformis: a model for understanding the oncogenicity of human papillomavirus. Ciba Found Symp. 1986;120:157-174.
4. Michael KM, Waterboer T, Pfister H, et al. Seroreactivity of 38 human papillomavirus types in epidermodysplasia verruciformis patients, relatives, and controls. J Invest Dermatol. 2010;130:841-848.
5. Zavattaro E, Azzimonti B, Mondini M, et al. Identification of defective Fas function and variation of the perforin gene in an epidermodysplasia verruciformis patient lacking EVER1 and EVER2 mutations. J Invest Dermatol. 2008;128:732-735.
6. Majewski S, Jabłońska S. Epidermodysplasia verruciformis as a model of human papillomavirus-induced genetic cancer of the skin. Arch Dermatol. 1995;131:1312-1318.
7. Robati RM, Marefat A, Saeedi M, et al. Four familial cases of epidermodysplasia verruciformis: mother and three sons. Dermatol Online J. 2009;15:8.
8. Ramoz N, Rueda LA, Bouadjar B, et al. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet. 2002;32:579-581.
9. Azzimonti B, Mondini M, De Andrea M, et al. CD8+ T-cell lymphocytopenia and lack of EVER mutations in a patient with clinically and virologically typical epidermodysplasia verruciformis. Arch Dermatol. 2005;141:1323-1325.
10. Androphy EJ, Dvoretzky I, Lowy DR. X-linked inheritance of epidermodysplasia verruciformis. genetic and virologic studies of a kindred. Arch Dermatol. 1985;121:864-868.
11. Tobin E, Rohwedder A, Holland SM, et al. Recurrent ‘sterile’ verrucous cyst abscesses and epidermodysplasia verruciformis-like eruption associated with idiopathic CD4 lymphopenia. Br J Dermatol. 2003;149:627-633.
12. Obalek S, Favre M, Szymanczyk J, et al. Human papillomavirus (HPV) types specific of epidermodysplasia verruciformis detected in warts induced by HPV3 or HPV3-related types in immunosuppressed patients. J Invest Dermatol. 1992;98:936-941.
13. Berk DR, Bruckner AL, Lu D. Epidermodysplasia verruciform-like lesions in an HIV patient. Dermatol Online J. 2009;15:1.
14. Vu J, Wallace GR, Singh R, et al. Common variable immunodeficiency syndrome associated with epidermodysplasia verruciformis. Am J Clin Dermatol. 2007;8:307-310.
15. Gul U, Soylu S, Yavuzer R. Epidermodysplasia verruciformis associated with IgM deficiency. Indian J Dermatol Venereol Leprol. 2007;73:420-422.
16. De Oliveira WR, Festa Neto C, Rady PL, et al. Clinical aspects of epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol. 2003;17:394-398.
17. Jablonska S, Majewski S. Epidermodysplasia verruciformis: what’s new? J Eur Acad Dermatol Venereol. 2003;17:381-382.
18. Rallis E, Papatheodorou G, Bimpakis E, et al. Systemic low-dose isotretinoin maintains remission status in epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol. 2008;22:523-525.
19. Anadolu R, Oskay T, Erdem C, et al. Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol. 2001;45:296-299.
20. Fang F, Zhao L, Jiang MJ, et al. Epidermodysplasia verruciformis with severe hand and foot deformity successfully treated with surgical excision. J Plast Reconstr Aesthet Surg. 2008;61:338-341.
21. Huang W, Morrell D. Successful treatment of recalcitrant warts with topical squaric acid in immunosuppressed child. Pediatr Dermatol. 2008;25:275-276.
22. Hama N, Hatamochi A, Hayashi S, et al. Usefulness of topical immunotherapy with squaric acid dibutylester for refractory common warts on the face and neck. J Dermatol. 2009;36:660-662.
23. Micali G, Nasca MR, Tedeschi A, et al. Use of squaric acid dibutylester (SADBE) for cutaneous warts in children. Pediatr Dermatol. 2000;17:315-318.
24. Mastrolonardo M, Lopalco PL, Diaferio A. Topical immunotherapy with contact sensitizers: a model to study the natural history of delayedhypersensitivity. Contact Dermatitis. 2002;47:210-214.
25. Lewis HM. Topical immunotherapy of refractory warts. Cutis. 1973;12:863-869.
26. Weisshaar E, Neumann HJ, Gollnick H. Successful treatment of disseminated facial verrucae with contact immunotherapy. Eur J Dermatol. 1998;8:488-491.
1. Vohra S, Sharma NL, Shanker V, et al. Autosomal dominant epidermodysplasia verruciformis: a clinicotherapeutic experience in two cases. Indian J Dermatol Venereol Leprol. 2010;76:557-561.
2. Dell’Oste V, Azzimonti B, De Andrea M, et al. High beta-HPV DNA loads and strong seroreactivity are present in epidermodysplasia verruciformis. J Invest Dermatol. 2009;129:1026-1034.
3. Orth G. Epidermodysplasia verruciformis: a model for understanding the oncogenicity of human papillomavirus. Ciba Found Symp. 1986;120:157-174.
4. Michael KM, Waterboer T, Pfister H, et al. Seroreactivity of 38 human papillomavirus types in epidermodysplasia verruciformis patients, relatives, and controls. J Invest Dermatol. 2010;130:841-848.
5. Zavattaro E, Azzimonti B, Mondini M, et al. Identification of defective Fas function and variation of the perforin gene in an epidermodysplasia verruciformis patient lacking EVER1 and EVER2 mutations. J Invest Dermatol. 2008;128:732-735.
6. Majewski S, Jabłońska S. Epidermodysplasia verruciformis as a model of human papillomavirus-induced genetic cancer of the skin. Arch Dermatol. 1995;131:1312-1318.
7. Robati RM, Marefat A, Saeedi M, et al. Four familial cases of epidermodysplasia verruciformis: mother and three sons. Dermatol Online J. 2009;15:8.
8. Ramoz N, Rueda LA, Bouadjar B, et al. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat Genet. 2002;32:579-581.
9. Azzimonti B, Mondini M, De Andrea M, et al. CD8+ T-cell lymphocytopenia and lack of EVER mutations in a patient with clinically and virologically typical epidermodysplasia verruciformis. Arch Dermatol. 2005;141:1323-1325.
10. Androphy EJ, Dvoretzky I, Lowy DR. X-linked inheritance of epidermodysplasia verruciformis. genetic and virologic studies of a kindred. Arch Dermatol. 1985;121:864-868.
11. Tobin E, Rohwedder A, Holland SM, et al. Recurrent ‘sterile’ verrucous cyst abscesses and epidermodysplasia verruciformis-like eruption associated with idiopathic CD4 lymphopenia. Br J Dermatol. 2003;149:627-633.
12. Obalek S, Favre M, Szymanczyk J, et al. Human papillomavirus (HPV) types specific of epidermodysplasia verruciformis detected in warts induced by HPV3 or HPV3-related types in immunosuppressed patients. J Invest Dermatol. 1992;98:936-941.
13. Berk DR, Bruckner AL, Lu D. Epidermodysplasia verruciform-like lesions in an HIV patient. Dermatol Online J. 2009;15:1.
14. Vu J, Wallace GR, Singh R, et al. Common variable immunodeficiency syndrome associated with epidermodysplasia verruciformis. Am J Clin Dermatol. 2007;8:307-310.
15. Gul U, Soylu S, Yavuzer R. Epidermodysplasia verruciformis associated with IgM deficiency. Indian J Dermatol Venereol Leprol. 2007;73:420-422.
16. De Oliveira WR, Festa Neto C, Rady PL, et al. Clinical aspects of epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol. 2003;17:394-398.
17. Jablonska S, Majewski S. Epidermodysplasia verruciformis: what’s new? J Eur Acad Dermatol Venereol. 2003;17:381-382.
18. Rallis E, Papatheodorou G, Bimpakis E, et al. Systemic low-dose isotretinoin maintains remission status in epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol. 2008;22:523-525.
19. Anadolu R, Oskay T, Erdem C, et al. Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol. 2001;45:296-299.
20. Fang F, Zhao L, Jiang MJ, et al. Epidermodysplasia verruciformis with severe hand and foot deformity successfully treated with surgical excision. J Plast Reconstr Aesthet Surg. 2008;61:338-341.
21. Huang W, Morrell D. Successful treatment of recalcitrant warts with topical squaric acid in immunosuppressed child. Pediatr Dermatol. 2008;25:275-276.
22. Hama N, Hatamochi A, Hayashi S, et al. Usefulness of topical immunotherapy with squaric acid dibutylester for refractory common warts on the face and neck. J Dermatol. 2009;36:660-662.
23. Micali G, Nasca MR, Tedeschi A, et al. Use of squaric acid dibutylester (SADBE) for cutaneous warts in children. Pediatr Dermatol. 2000;17:315-318.
24. Mastrolonardo M, Lopalco PL, Diaferio A. Topical immunotherapy with contact sensitizers: a model to study the natural history of delayedhypersensitivity. Contact Dermatitis. 2002;47:210-214.
25. Lewis HM. Topical immunotherapy of refractory warts. Cutis. 1973;12:863-869.
26. Weisshaar E, Neumann HJ, Gollnick H. Successful treatment of disseminated facial verrucae with contact immunotherapy. Eur J Dermatol. 1998;8:488-491.
Practice Points
- Epidermodysplasia verruciformis (EV) is a rare immune deficiency. Associated warts are difficult to treat.
- Topical immunotherapy with squaric acid dibutylester (SADBE) has successfully treated long-standing warts in an EV patient.
- Consider immunotherapy with a contact sensitizer such as SADBE to treat resistant warts, even in immune deficiency patients.
