User login
Case Report: Spontaneous Retroperitoneal Bleeding Masking as Left Lower Quadrant Abdominal Pain
Case
A 76-year-old woman with worsening intermittent lower left quadrant abdominal pain was brought to the ED by her daughter, who stated that her mother’s pain had started 2 days prior to presentation. The patient described the pain, which was present with movement and at rest, as sharp and radiating to the left hip, left lower back, and left inner thigh. She denied shortness of breath, chest pain, fever, chills, nausea, and vomiting. The patient initially reported having diarrhea, but further inquiry revealed that her stools had been softer than usual but not watery or more frequent.
One week before presentation, the patient had been treated at another hospital for myocardial infarction (MI) and new-onset atrial fibrillation. During this hospital stay, she had declined diagnostic cardiac catheterization and was started on warfarin and enoxaparin at discharge. Other than a history of hypertension, the patient had been in good health prior to the MI and atrial fibrillation. Her regular medications included metoprolol, lisinopril, and aspirin.
On physical examination, she was alert and oriented, but appeared to be in mild distress. The patient was an obese, elderly female with a body mass index of 35.2 kg/m2. Her vital signs were: temperature, 98.4˚F; blood pressure, 180/74 mm Hg; heart rate, 69 beats/minute; and respiratory rate, 18 breaths/minute. No respiratory distress was noted, and her oxygen saturation was 99% on room air.
The head, ears, eyes, nose, and throat examination was normal, with a normocephalic and atraumatic head. The patient’s neck was supple and without jugular vein distension or tracheal deviation. A cardiopulmonary examination revealed breath sounds with normal effort and no rales, wheezes, or rhonchi; no murmurs, rubs, or gallops were heard on auscultation. The patient’s abdomen was soft, without rebound tenderness, distention, or guarding, and bowel sounds were normal and appreciated on auscultation. She had tenderness to palpation in the left lower quadrant.
On musculoskeletal examination, the patient’s hips had normal range of motion and there was equal +5/5 strength bilaterally in the hips and lower extremities. The remainder of the examination of her lower extremities was without rash, erythema, or edema, and there were no lesions or rashes elsewhere on the skin. No focal deficits were noted on neurological examination.
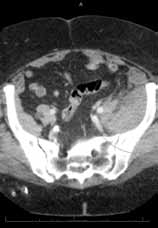
The patient was admitted to the hospital with a request for cardiology and surgical consultations. Upon inpatient admission and evaluation, the warfarin and enoxaparin were stopped, and the surgical team elected for conservative management of the retroperitoneal bleed. The patient had stable Hgb levels on serial complete blood-cell counts.
A renal ultrasound was ordered to investigate the low-density lesion in the left kidney revealed a left renal cyst. It is, however, unlikely the renal cyst was contributory to the retroperitoneal bleed. As the patient remained hemodynamically stable and her pain abated, she was discharged on hospital day 4.
Discussion
Overview
Spontaneous retroperitoneal bleeding is a rare but potentially life-threatening occurrence that is most commonly seen in patients on anticoagulation therapy, those with bleeding disorders, and those on hemodialysis.1 Patients with spontaneous retroperitoneal bleeding present with a variety of symptoms including abdominal pain, hip and upper thigh pain, back pain, and hypotension.2,3 In one observational cohort study, the nonspecific nature of symptoms led to misdiagnosis in 10.1% of the cases.3 The patient in this case exhibited several of the abovementioned symptoms and complaints.
The literature concerning spontaneous retroperitoneal bleeding is limited and consists of mainly case reports and case series. Warfarin, clopidogrel, unfractionated and low-molecular weight heparin use have all been reported in patients with retroperitoneal bleeding,4 and various studies have placed the incidence of this distinct entity to be between 0.6% to 6.6%.5,6
Spontaneous Versus Iatrogenic Retroperitoneal Bleeding
By definition, spontaneous retroperitoneal bleeding occurs without trauma, surgery, invasive procedures, and abdominal aortic aneurysm.3 Iatrogenic retroperitoneal bleeding, however, is a rare but known complication of catheterization procedures involving the femoral region, with an increased risk in female patients.7 Based on this increased incidence, the patient in this case was specifically asked whether she had undergone any procedures during her latest admission, including cardiac catheterization, which she denied.
In contrast, spontaneous retroperitoneal hemorrhage has an unclear pathogenesis. Some authors have suggested unrecognized minor trauma such as coughing as a possible cause.8 The patient in this case was asked on hospital day 2 if she had experienced a history of cough the week prior to presentation to the ED, to which she stated she had not.
Risk Factors
More recent case reports focus on renal or adrenal tumors as a potential source of spontaneous retroperitoneal bleeding. Although this patient did have a renal cyst in left kidney, its contribution to the retroperitoneal bleed is unknown and thought to be only incidental.
A retrospective chart review of 119 identified patients with spontaneous retroperitoneal bleeds sought to identify reliable predictors of early diagnosis. Ivascu et al2 found that elderly patients on both anticoagulation and antiplatelet therapy were at the highest risk. Shah et al9 echoed the sentiment of severity in their retrospective review which showed that those on combined anticoagulant and antiplatelet therapy were more likely to require intensive care unit (ICU) admission and had longer ICU stays.
Conclusion
Unlike hemorrhages in other locations in the body, retroperitoneal bleeding can be difficult to diagnose since patients often present with nonspecific symptoms such as lower abdominal pain. Clinicians should therefore maintain a high index of suspicion, especially in patients who are on anticoagulation therapy, who have a coagulopathy, or who are on hemodialysis. Delay or failure to diagnose this condition may lead to significant morbidity and mortality.
Dr Lui is a resident, department of emergency medicine, Henry Ford Wyandotte Hospital, Wyandotte, Michigan. Dr Boehm is the emergency medicine residency program director in the graduate medical education department, Saint Mary Mercy Hospital, livonia, Michigan; and is an emergency physician at the Emergency physicians Medical Group, ann arbor, Michigan.
- Bhasin HK, Dana CL. Spontaneous retroperitoneal hemorrhage in chronically hemodialyzed patients. Nephron. 1978; 22(4-6):322-327.
- Ivascu FA, Janczyk RJ, Bair HA, Bendick PJ, Howells GA. Spontaneous retroperitoneal hemorrhage. Am J Surg. 2005;189(3):345-347.
- Sunga, KL, Bellolio MF, Gilmore RM, Cabrera D. Spontaneous retroperitoneal hematoma: etiology, characteristics, management, and outcome. J Emer Med. 2012;43(2):e157-e161.
- Ernits M, Mohan PS, Fares LG 2nd, Hardy H 3rd. A retroperitoneal bleed induced by enoxaparin therapy. Am Surg. 2005;71(5):430-433.
- Mant MJ, O’Brien BD, Thong KL, Hammond GW, Birtwhistle RV, Grace MG. Haemorrhagic complications of heparin therapy. Lancet. 1977;1(8022):1133-1135.
- Forfar JC. A 7-year analysis of haemorrhage in patients on long-term anticoagulant treatment. Br Heart J. 1979;42(2):128-132.
- Sajnani N, Bogart DB. Retroperitoneal hemorrhage as a complication of percutaneous intervention: report of 2 cases and review of the literature. Open Cardiovasc Med J. 2013;7:16-22.
- Berná JD, Zuazu I, Madrigal M, García-Medina V, Fernández C, Guirado F. Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging. 2000;25(3):230-234.
- Shah, RD, Nagar S, Shanley CJ, Janczyk RJ. Factors affecting the severity of spontaneous retroperitoneal hemorrhage in anticoagulated patients. Am J Surg.
Case
A 76-year-old woman with worsening intermittent lower left quadrant abdominal pain was brought to the ED by her daughter, who stated that her mother’s pain had started 2 days prior to presentation. The patient described the pain, which was present with movement and at rest, as sharp and radiating to the left hip, left lower back, and left inner thigh. She denied shortness of breath, chest pain, fever, chills, nausea, and vomiting. The patient initially reported having diarrhea, but further inquiry revealed that her stools had been softer than usual but not watery or more frequent.
One week before presentation, the patient had been treated at another hospital for myocardial infarction (MI) and new-onset atrial fibrillation. During this hospital stay, she had declined diagnostic cardiac catheterization and was started on warfarin and enoxaparin at discharge. Other than a history of hypertension, the patient had been in good health prior to the MI and atrial fibrillation. Her regular medications included metoprolol, lisinopril, and aspirin.
On physical examination, she was alert and oriented, but appeared to be in mild distress. The patient was an obese, elderly female with a body mass index of 35.2 kg/m2. Her vital signs were: temperature, 98.4˚F; blood pressure, 180/74 mm Hg; heart rate, 69 beats/minute; and respiratory rate, 18 breaths/minute. No respiratory distress was noted, and her oxygen saturation was 99% on room air.
The head, ears, eyes, nose, and throat examination was normal, with a normocephalic and atraumatic head. The patient’s neck was supple and without jugular vein distension or tracheal deviation. A cardiopulmonary examination revealed breath sounds with normal effort and no rales, wheezes, or rhonchi; no murmurs, rubs, or gallops were heard on auscultation. The patient’s abdomen was soft, without rebound tenderness, distention, or guarding, and bowel sounds were normal and appreciated on auscultation. She had tenderness to palpation in the left lower quadrant.
On musculoskeletal examination, the patient’s hips had normal range of motion and there was equal +5/5 strength bilaterally in the hips and lower extremities. The remainder of the examination of her lower extremities was without rash, erythema, or edema, and there were no lesions or rashes elsewhere on the skin. No focal deficits were noted on neurological examination.
The patient was admitted to the hospital with a request for cardiology and surgical consultations. Upon inpatient admission and evaluation, the warfarin and enoxaparin were stopped, and the surgical team elected for conservative management of the retroperitoneal bleed. The patient had stable Hgb levels on serial complete blood-cell counts.
A renal ultrasound was ordered to investigate the low-density lesion in the left kidney revealed a left renal cyst. It is, however, unlikely the renal cyst was contributory to the retroperitoneal bleed. As the patient remained hemodynamically stable and her pain abated, she was discharged on hospital day 4.
Discussion
Overview
Spontaneous retroperitoneal bleeding is a rare but potentially life-threatening occurrence that is most commonly seen in patients on anticoagulation therapy, those with bleeding disorders, and those on hemodialysis.1 Patients with spontaneous retroperitoneal bleeding present with a variety of symptoms including abdominal pain, hip and upper thigh pain, back pain, and hypotension.2,3 In one observational cohort study, the nonspecific nature of symptoms led to misdiagnosis in 10.1% of the cases.3 The patient in this case exhibited several of the abovementioned symptoms and complaints.
The literature concerning spontaneous retroperitoneal bleeding is limited and consists of mainly case reports and case series. Warfarin, clopidogrel, unfractionated and low-molecular weight heparin use have all been reported in patients with retroperitoneal bleeding,4 and various studies have placed the incidence of this distinct entity to be between 0.6% to 6.6%.5,6
Spontaneous Versus Iatrogenic Retroperitoneal Bleeding
By definition, spontaneous retroperitoneal bleeding occurs without trauma, surgery, invasive procedures, and abdominal aortic aneurysm.3 Iatrogenic retroperitoneal bleeding, however, is a rare but known complication of catheterization procedures involving the femoral region, with an increased risk in female patients.7 Based on this increased incidence, the patient in this case was specifically asked whether she had undergone any procedures during her latest admission, including cardiac catheterization, which she denied.
In contrast, spontaneous retroperitoneal hemorrhage has an unclear pathogenesis. Some authors have suggested unrecognized minor trauma such as coughing as a possible cause.8 The patient in this case was asked on hospital day 2 if she had experienced a history of cough the week prior to presentation to the ED, to which she stated she had not.
Risk Factors
More recent case reports focus on renal or adrenal tumors as a potential source of spontaneous retroperitoneal bleeding. Although this patient did have a renal cyst in left kidney, its contribution to the retroperitoneal bleed is unknown and thought to be only incidental.
A retrospective chart review of 119 identified patients with spontaneous retroperitoneal bleeds sought to identify reliable predictors of early diagnosis. Ivascu et al2 found that elderly patients on both anticoagulation and antiplatelet therapy were at the highest risk. Shah et al9 echoed the sentiment of severity in their retrospective review which showed that those on combined anticoagulant and antiplatelet therapy were more likely to require intensive care unit (ICU) admission and had longer ICU stays.
Conclusion
Unlike hemorrhages in other locations in the body, retroperitoneal bleeding can be difficult to diagnose since patients often present with nonspecific symptoms such as lower abdominal pain. Clinicians should therefore maintain a high index of suspicion, especially in patients who are on anticoagulation therapy, who have a coagulopathy, or who are on hemodialysis. Delay or failure to diagnose this condition may lead to significant morbidity and mortality.
Dr Lui is a resident, department of emergency medicine, Henry Ford Wyandotte Hospital, Wyandotte, Michigan. Dr Boehm is the emergency medicine residency program director in the graduate medical education department, Saint Mary Mercy Hospital, livonia, Michigan; and is an emergency physician at the Emergency physicians Medical Group, ann arbor, Michigan.
Case
A 76-year-old woman with worsening intermittent lower left quadrant abdominal pain was brought to the ED by her daughter, who stated that her mother’s pain had started 2 days prior to presentation. The patient described the pain, which was present with movement and at rest, as sharp and radiating to the left hip, left lower back, and left inner thigh. She denied shortness of breath, chest pain, fever, chills, nausea, and vomiting. The patient initially reported having diarrhea, but further inquiry revealed that her stools had been softer than usual but not watery or more frequent.
One week before presentation, the patient had been treated at another hospital for myocardial infarction (MI) and new-onset atrial fibrillation. During this hospital stay, she had declined diagnostic cardiac catheterization and was started on warfarin and enoxaparin at discharge. Other than a history of hypertension, the patient had been in good health prior to the MI and atrial fibrillation. Her regular medications included metoprolol, lisinopril, and aspirin.
On physical examination, she was alert and oriented, but appeared to be in mild distress. The patient was an obese, elderly female with a body mass index of 35.2 kg/m2. Her vital signs were: temperature, 98.4˚F; blood pressure, 180/74 mm Hg; heart rate, 69 beats/minute; and respiratory rate, 18 breaths/minute. No respiratory distress was noted, and her oxygen saturation was 99% on room air.
The head, ears, eyes, nose, and throat examination was normal, with a normocephalic and atraumatic head. The patient’s neck was supple and without jugular vein distension or tracheal deviation. A cardiopulmonary examination revealed breath sounds with normal effort and no rales, wheezes, or rhonchi; no murmurs, rubs, or gallops were heard on auscultation. The patient’s abdomen was soft, without rebound tenderness, distention, or guarding, and bowel sounds were normal and appreciated on auscultation. She had tenderness to palpation in the left lower quadrant.
On musculoskeletal examination, the patient’s hips had normal range of motion and there was equal +5/5 strength bilaterally in the hips and lower extremities. The remainder of the examination of her lower extremities was without rash, erythema, or edema, and there were no lesions or rashes elsewhere on the skin. No focal deficits were noted on neurological examination.
The patient was admitted to the hospital with a request for cardiology and surgical consultations. Upon inpatient admission and evaluation, the warfarin and enoxaparin were stopped, and the surgical team elected for conservative management of the retroperitoneal bleed. The patient had stable Hgb levels on serial complete blood-cell counts.
A renal ultrasound was ordered to investigate the low-density lesion in the left kidney revealed a left renal cyst. It is, however, unlikely the renal cyst was contributory to the retroperitoneal bleed. As the patient remained hemodynamically stable and her pain abated, she was discharged on hospital day 4.
Discussion
Overview
Spontaneous retroperitoneal bleeding is a rare but potentially life-threatening occurrence that is most commonly seen in patients on anticoagulation therapy, those with bleeding disorders, and those on hemodialysis.1 Patients with spontaneous retroperitoneal bleeding present with a variety of symptoms including abdominal pain, hip and upper thigh pain, back pain, and hypotension.2,3 In one observational cohort study, the nonspecific nature of symptoms led to misdiagnosis in 10.1% of the cases.3 The patient in this case exhibited several of the abovementioned symptoms and complaints.
The literature concerning spontaneous retroperitoneal bleeding is limited and consists of mainly case reports and case series. Warfarin, clopidogrel, unfractionated and low-molecular weight heparin use have all been reported in patients with retroperitoneal bleeding,4 and various studies have placed the incidence of this distinct entity to be between 0.6% to 6.6%.5,6
Spontaneous Versus Iatrogenic Retroperitoneal Bleeding
By definition, spontaneous retroperitoneal bleeding occurs without trauma, surgery, invasive procedures, and abdominal aortic aneurysm.3 Iatrogenic retroperitoneal bleeding, however, is a rare but known complication of catheterization procedures involving the femoral region, with an increased risk in female patients.7 Based on this increased incidence, the patient in this case was specifically asked whether she had undergone any procedures during her latest admission, including cardiac catheterization, which she denied.
In contrast, spontaneous retroperitoneal hemorrhage has an unclear pathogenesis. Some authors have suggested unrecognized minor trauma such as coughing as a possible cause.8 The patient in this case was asked on hospital day 2 if she had experienced a history of cough the week prior to presentation to the ED, to which she stated she had not.
Risk Factors
More recent case reports focus on renal or adrenal tumors as a potential source of spontaneous retroperitoneal bleeding. Although this patient did have a renal cyst in left kidney, its contribution to the retroperitoneal bleed is unknown and thought to be only incidental.
A retrospective chart review of 119 identified patients with spontaneous retroperitoneal bleeds sought to identify reliable predictors of early diagnosis. Ivascu et al2 found that elderly patients on both anticoagulation and antiplatelet therapy were at the highest risk. Shah et al9 echoed the sentiment of severity in their retrospective review which showed that those on combined anticoagulant and antiplatelet therapy were more likely to require intensive care unit (ICU) admission and had longer ICU stays.
Conclusion
Unlike hemorrhages in other locations in the body, retroperitoneal bleeding can be difficult to diagnose since patients often present with nonspecific symptoms such as lower abdominal pain. Clinicians should therefore maintain a high index of suspicion, especially in patients who are on anticoagulation therapy, who have a coagulopathy, or who are on hemodialysis. Delay or failure to diagnose this condition may lead to significant morbidity and mortality.
Dr Lui is a resident, department of emergency medicine, Henry Ford Wyandotte Hospital, Wyandotte, Michigan. Dr Boehm is the emergency medicine residency program director in the graduate medical education department, Saint Mary Mercy Hospital, livonia, Michigan; and is an emergency physician at the Emergency physicians Medical Group, ann arbor, Michigan.
- Bhasin HK, Dana CL. Spontaneous retroperitoneal hemorrhage in chronically hemodialyzed patients. Nephron. 1978; 22(4-6):322-327.
- Ivascu FA, Janczyk RJ, Bair HA, Bendick PJ, Howells GA. Spontaneous retroperitoneal hemorrhage. Am J Surg. 2005;189(3):345-347.
- Sunga, KL, Bellolio MF, Gilmore RM, Cabrera D. Spontaneous retroperitoneal hematoma: etiology, characteristics, management, and outcome. J Emer Med. 2012;43(2):e157-e161.
- Ernits M, Mohan PS, Fares LG 2nd, Hardy H 3rd. A retroperitoneal bleed induced by enoxaparin therapy. Am Surg. 2005;71(5):430-433.
- Mant MJ, O’Brien BD, Thong KL, Hammond GW, Birtwhistle RV, Grace MG. Haemorrhagic complications of heparin therapy. Lancet. 1977;1(8022):1133-1135.
- Forfar JC. A 7-year analysis of haemorrhage in patients on long-term anticoagulant treatment. Br Heart J. 1979;42(2):128-132.
- Sajnani N, Bogart DB. Retroperitoneal hemorrhage as a complication of percutaneous intervention: report of 2 cases and review of the literature. Open Cardiovasc Med J. 2013;7:16-22.
- Berná JD, Zuazu I, Madrigal M, García-Medina V, Fernández C, Guirado F. Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging. 2000;25(3):230-234.
- Shah, RD, Nagar S, Shanley CJ, Janczyk RJ. Factors affecting the severity of spontaneous retroperitoneal hemorrhage in anticoagulated patients. Am J Surg.
- Bhasin HK, Dana CL. Spontaneous retroperitoneal hemorrhage in chronically hemodialyzed patients. Nephron. 1978; 22(4-6):322-327.
- Ivascu FA, Janczyk RJ, Bair HA, Bendick PJ, Howells GA. Spontaneous retroperitoneal hemorrhage. Am J Surg. 2005;189(3):345-347.
- Sunga, KL, Bellolio MF, Gilmore RM, Cabrera D. Spontaneous retroperitoneal hematoma: etiology, characteristics, management, and outcome. J Emer Med. 2012;43(2):e157-e161.
- Ernits M, Mohan PS, Fares LG 2nd, Hardy H 3rd. A retroperitoneal bleed induced by enoxaparin therapy. Am Surg. 2005;71(5):430-433.
- Mant MJ, O’Brien BD, Thong KL, Hammond GW, Birtwhistle RV, Grace MG. Haemorrhagic complications of heparin therapy. Lancet. 1977;1(8022):1133-1135.
- Forfar JC. A 7-year analysis of haemorrhage in patients on long-term anticoagulant treatment. Br Heart J. 1979;42(2):128-132.
- Sajnani N, Bogart DB. Retroperitoneal hemorrhage as a complication of percutaneous intervention: report of 2 cases and review of the literature. Open Cardiovasc Med J. 2013;7:16-22.
- Berná JD, Zuazu I, Madrigal M, García-Medina V, Fernández C, Guirado F. Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging. 2000;25(3):230-234.
- Shah, RD, Nagar S, Shanley CJ, Janczyk RJ. Factors affecting the severity of spontaneous retroperitoneal hemorrhage in anticoagulated patients. Am J Surg.