User login
Targeting tachycardia: Diagnostic tips and tools
•Analyze P wave axis, morphology, and timing for help in diagnosing narrow QRS complex tachycardia. C
•Review the modes of onset and termination for clues to the specific type of tachycardia, including features such as the rate of acceleration and the response to medication and the Valsalva maneuver. C
•Compare a baseline 12-lead EKG with one taken during an episode of tachycardia, looking for clues to the mechanism of the arrhythmia. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sinus tachycardia educational video for patients
Courtesy of: WirelessDx
Go to http://www.wirelessdx.com/sinustachycardia.htm

Narrow QRS complex tachycardias—rhythms with a rate >100 beats per minute (bpm) and a QRS duration <120 ms—are frequently encountered in both inpatient and outpatient settings. Therapeutic strategy ranges from simple reassurance to acute inpatient intervention, depending on the specific arrhythmia.
Early and accurate diagnosis is paramount to avoid unnecessary testing, ensure timely management, and prevent complications and long-term adverse outcomes. While most narrow QRS complex tachycardias are easily diagnosed, some pose a diagnostic challenge.

This review can help. We start with a summary of the various types of narrow QRS complex tachycardias, accompanied in some cases with 12-lead electrocardiogram (EKG) strips. Next, we highlight key characteristics to consider in the differential and provide an algorithm to help you zero in on the diagnosis.
Narrow QRS complex tachycardias: What you’ll find
Narrow QRS complex tachycardias fall into 2 broad categories: those that are sinus node-generated, and those that are not. Here’s a look at both.
Sinus node-generated tachycardias
Sinus node tachycardia (FIGURE 1), the most common arrhythmia,1 is an appropriate response to physiologic or emotional stress or disease processes. It is defined as a heart rate >100 bpm with the presence of P waves of normal sinus morphology on a 12-lead EKG.
FIGURE 1
Sinus tachycardia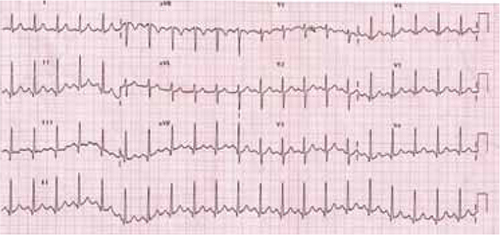
The P waves show normal sinus morphology. Note superior-to-inferior axis with positive P deflections in leads II, III, and aVF.
Inappropriate sinus tachycardia is a nonparoxysmal arrhythmia with a resting daytime heart rate >100 bpm (or an average heart rate >90 bpm over a 24-hour period), normal P wave morphology, and an exaggerated response to physical activity.2,3 What distinguishes it from simple sinus tachycardia is the disproportionate degree of the arrhythmia to the level of physiologic stress.
Inappropriate sinus tachycardia is a diagnosis of exclusion, established only after other reversible pathologic or pharmacologic causes of tachycardia, such as hyperthyroidism, pheochromocytoma, infection, or theophylline toxicity, have been ruled out. Possible mechanisms may include autonomic dysfunction with increased cardiac sympathetic or reduced vagal output.4
Paroxysmal orthostatic tachycardia syndrome (POTS) is an abnormal sinus tachycardia response to an upright position.5,6 It is diagnosed by a heart rate ≥120 bpm or an increase ≥30 bpm within 5 minutes of standing up or being on a tilt table, with simultaneous development of orthostatic symptoms, such as dizziness, light-headedness, or even syncope, without the corresponding drop in blood pressure. Symptoms usually resolve after the patient assumes a supine position. The presentation may overlap with that of inappropriate sinus tachycardia, although patients with POTS usually develop autonomic symptoms such as constipation, tremor, or heat/cold intolerance, as well.7,8
Sinus node reentry tachycardia is a paroxysmal tachycardia with a normal P wave on a 12-lead EKG. The paroxysmal nature of the arrhythmia and a positive response to atropine and vagal maneuvers, as well as identification by electrophysiologic studies, differentiate this condition from inappropriate sinus tachycardia.9
Nonsinus node-generated tachycardias
Focal atrial tachycardia (FIGURE 2) is caused by an automatic, triggered, or microreentrant mechanism that can be localized to a specific area of atrial tissue.10 The diagnosis can often be made by a careful review of the EKG, which will reveal P waves that differ from those of the sinus beat.11 This can be tricky, however, as a P wave on a 12-lead EKG from a focal point close to the sinoatrial node may resemble that of a normal sinus rhythm.
FIGURE 2
Focal atrial tachycardia
The P waves differ from those of the sinus beat. Note the positive P wave in lead aVR.
The atrial rate associated with this condition can vary from 120 to 300 bpm, depending on the focus, and may be associated with variable degrees of atrioventricular (AV) block. The crista terminalis in the right atrium and pulmonary vein ostia are frequent origins of focal atrial arrhythmias.12,13
Multifocal atrial tachycardia (FIGURE 3) is a supraventricular arrhythmia with ≥3 different P wave morphologies, as well as varying PR and RR intervals on the 12-lead EKG. It is typically associated with lung disorders but may occur in patients with other conditions, such as theophylline toxicity.14
FIGURE 3
Multifocal atrial tachycardia
The P waves have varied morphologies; the PR and RR intervals also vary, which is best seen in lead V1.
Atrioventricular nodal reentrant tachycardia (AVNRT), a reentrant form of narrow QRS complex tachycardia, is based on a dual (slow and fast) pathway of the compact AV node (FIGURE 4). In the typical form—constituting 90% of cases15—antegrade conduction is via the slow pathway and retrograde conduction is via the fast pathway.16 In the atypical form, it’s the other way around.
FIGURE 4
Atrioventricular nodal reentrant tachycardia
Note the “pseudo S” waves, which is best seen in leads II, III, and aVF. This represents retrograde activation of the atria with an inferior-to-superior axis. The RP interval is very short.
Orthodromic atrioventricular reciprocating tachycardia (AVRT), or Wolff-Parkinson-White syndrome, is a narrow QRS complex tachycardia in which antegrade conduction is via the AV node and retrograde conduction is via an accessory pathway (bundle of Kent). The accessory pathway consists of a band of muscle tissue that connects the atrium directly to the ventricles, allowing electrical impulses to bypass the AV node. Antidromic AVRT, a wide QRS complex tachycardia, is the most common supraventricular arrhythmia in patients with accessory pathways.17
Atrial fibrillation (FIGURE 5), the most common arrhythmia for which medical treatment is required,18 is an irregular rhythm with an undulating baseline.19
FIGURE 5
Atrial fibrillation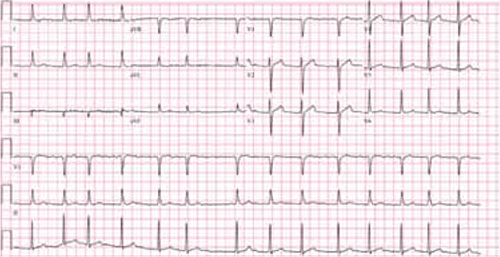
This strip shows an irregularly irregular rhythm with no distinct P waves. The undulating baseline represents fibrillatory waves.
Atrial flutter is a reentrant tachycardia originating in either atrium, with regular flutter (F) waves on a 12-lead EKG (FIGURE 6). A counterclockwise propagating isthmus-dependent atrial flutter originating in the right atrium produces the typical “sawtooth” pattern of negative F waves in the inferior electrocardiographic leads.
FIGURE 6
Atrial flutter
Note the regular flutter waves (“sawtooth waves”) best seen in lead II with variable AV conduction.
Junctional ectopic tachycardia is a rare arrhythmia caused by increased automaticity within the bundle of His.20,21 It is typically diagnosed in childhood and usually presents as a narrow QRS tachycardia with AV dissociation,22 but retrograde conduction to the atrium has also been found.21
How to approach the differential diagnosis
There are a number of characteristics to consider in the differential diagnosis of a patient with narrow QRS complex tachycardia (ALGORITHM).1,23-29 These include:
- rhythm regularity
- P wave axis and morphology
- relative duration of RP and PR intervals
- P wave position relative to the QRS complex
- ST elevation in lead aVR
- onset and termination mode.
ALGORITHM
Narrow QRS complex tachycardia: Zeroing in on the diagnosis1,23-29
AVNRT, atrioventricular nodal reentrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; EKG, electrocardiogram; MAT, multifocal atrial tachycardia.
*Or technically poor EKG.
Rhythm regularity is a key consideration. An irregular rhythm and the absence of P waves (or the presence of fibrillatory waves) characterizes atrial fibrillation; irregularity and ≥3 different P wave morphologies is suggestive of multifocal atrial tachycardia. Other possibilities include frequent premature atrial contractions or a sinoatrial or AV nodal conduction block.
AV dissociation is rarely seen in narrow QRS complex tachycardia. Its presence raises the possibility of junctional ectopic tachycardia, ventricular tachycardia, or complete AV node block.
P wave axis and morphology can help with both the differentiation and the origin of narrow QRS complex tachycardias. A superior-to-inferior axis of P waves (positivity in leads II, III, and aVF) is seen in sinus node-generated tachycardias and sometimes in focal atrial tachycardia. An inferior-superior P wave axis (negativity in leads II, III, and aVF) is observed in AVNRT, AVRT, and a subset of focal atrial tachycardia.23,24
The specific P wave axis and morphology in focal atrial tachycardia depends on the site of atrial automaticity. If the origin is near the sinus node region or high in the atrium, the result would be a superior-to-inferior P wave axis; if it originates lower in the atrium, the resulting atrial depolarization would be an inferior-to-superior axis.23,24
Relative duration of RP and PR intervals can help to differentiate narrow QRS complex tachycardias based on the timing of the P wave with respect to adjacent QRS complexes. Those in which the RP interval is longer than the PR interval are called long RP tachycardias and include sinus tachycardia, intra-atrial tachycardia, atypical AVNRT, and AVRT with a slowly conducting ventriculoatrial pathway.25,26
Short RP tachycardias are characterized by an RP interval that’s shorter than the PR interval. Only 2 arrhythmias present as short RP tachycardias: AVNRT and AVRT.27 If the RP interval is <70 ms, AVNRT is the likely diagnosis.28
P wave position. A careful review of the position of the P wave with respect to the QRS complex can provide additional help in distinguishing between AVNRT and AVRT. In 66% of AVNRTs, the P wave is hidden within the QRS complex;29 in 30%, a retrograde P wave closely follows the QRS complex, creating a “pseudo-S” wave; and 4% of the time, the P wave precedes the QRS complex.
In AVRT, a retrograde P wave follows the QRS complex. This creates a potential dilemma in differentiating 30% of AVNRTs from AVRT. In AVNRT, the retrograde P wave typically appears very close to the QRS complex, creating a pseudo-S wave. In the orthodromic AVRT, there is usually a separation between the QRS and retrograde P wave. In general, if the RP interval is <70 ms, the arrhythmia is usually due to typical AVNRT.28
ST segment elevation in lead aVR on a 12-lead EKG in a supraventricular tachycardia is about 70% sensitive and 70% to 83% specific for a diagnosis of AVRT.30,31 ST depression of more than 2 mm or T wave inversion is more common in AVRT than in AVNRT.32 QRS alternans, which refers to variations in QRS amplitude or direction with every other beat, has been reported to be indicative of AVRT, 33,34 but may in fact be a rate-dependent phenomenon that has little to do with the mechanism of tachycardias.35
Onset and termination and other indicators. Still uncertain? Patterns of arrhythmias and modes of onset and termination may provide additional help with the differential diagnosis.
Sinus tachycardias and atrial tachycardias frequently demonstrate a “warm up” in rate, for instance, while AVNRT and AVRT are often triggered by premature atrial contractions. A positive response to the Valsalva maneuver or to adenosine is typically characteristic of reentrant tachycardias using the AV node, such as AVNRT and AVRT.
Comparing a baseline 12-lead EKG with an EKG taken during an episode of tachycardia often provides further information about the mechanism of the arrhythmia. The presence of pre-excitation, the morphology of P waves, and the lack of retrograde P waves on a baseline EKG can be useful in narrowing the differential diagnosis.
Figures courtesy of: University of Buffalo and Buffalo General Hospital.
CORRESPONDENCE Vipul Gupta, MD, MPH, State University of New York at Buffalo, 131 Biomedical Education Building, Buffalo, NY 14214;
1. Yusuf S, Camm AJ. Deciphering the sinus tachycardias. Clin Cardiol. 2005;28:267-276.
2. Lee RJ, Shinbane JS. Inappropriate sinus tachycardia. Diagnosis and treatment. Cardiol Clin. 1997;15:599-605.
3. Morillo CA, Klein GJ, Thakur RK, et al. Mechanism of ‘inappropriate’ sinus tachycardia. Circulation. 1994;90:873-877.
4. Bauernfeind RA, Amat-y-Leon F, Dhingra RC, et al. Chronic nonparoxysmal sinus tachycardia in otherwise healthy persons. Ann Intern Med. 1979;91:702-710.
5. Low PA, Opfer-Gehrking TL, Textor SC, et al. Postural tachycardia syndrome (POTS). Neurology. 1995;45(suppl 5):S19-S25.
6. Raj SR. The postural tachycardia syndrome (POTS): pathophysiology, diagnosis & management. Indian Pacing Electrophysiol J. 2006;6:84-99.
7. Grubb BP, Kanjwal MY, Kosinski DJ. Review: the postural orthostatic tachycardia syndrome. J Interv Card Electrophysiol. 2001;5:9-16.
8. Kanjwal MY, Kosinski DJ, Grubb BP. Treatment of postural orthostatic tachycardia syndrome and inappropriate sinus tachycardia. Curr Cardiol Rep. 2003;5:402-406.
9. Simmers TA, Sreeram N. Sinoatrial reentry tachycardia: a review. Indian Pacing Electrophysiol J. 2003;3:109-116.
10. Saoudi N, Cosío F, Waldo A, et al. Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical bases. Eur Heart J. 2001;22:1162-1182.
11. Teh AW, Kistler PM, Kalman JM. Using the 12-lead ECG to localize the origin of ventricular and atrial tachycardias: part 1.J Cardiovasc Electrophysiol. 2009;20:706-709.
12. Roberts-Thomson KC, Kistler PM, Kalman JM. Focal atrial tachycardia I: clinical features, diagnosis, mechanisms, and anatomic location. Pacing Clin Electrophysiol. 2006;29:643-652.
13. Rosso R, Kistler PM. Focal atrial tachycardia. Heart. 2010;96:181-185.
14. Schwartz M, Rodman D, Lowenstein SR. Recognition and treatment of multifocal atrial tachycardia: a critical review. J Emerg Med. 1994;12:353-360.
15. Kwaku KF, Josephson ME. Typical AVNRT-an update on mechanisms and therapy. Cardiol Electrophysiol Rev. 2002;6:414-421.
16. Nawata H, Yamamoto N, Hirao K, et al. Heterogeneity of anterograde fast-pathway and retrograde slow-pathway conduction patterns in patients with the fast-slow form of atrioventricular nodal reentrant tachycardia. J Am Coll Cardiol. 1998;32:1731-1740.
17. Fox DJ, Tischenko A, Krahn AD, et al. Supraventricular tachycardia. Mayo Clin Proc. 2008;83:1400-1411.
18. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention. JAMA. 2001;285:2370-2375.
19. Falk RH. Atrial fibrillation. N Engl J Med. 2001;344:1067-1078.
20. Garson A, Gillette PC. Junctional ectopic tachycardia in children: electrocardiography, electrophysiology and pharmacologic response. Am J Cardiol. 1979;44:298-302.
21. Villain E, Vetter VL, Garcia JM, et al. Evolving concepts in the management of congenital junctional ectopic tachycardia. A multicenter study. Circulation. 1990;81:1544-1549.
22. Sarubbi B, Vergara P, D’Alto M, et al. Congenital junctional ectopic tachycardia: presentation and outcome. Indian Pacing Electrophysiol J. 2003;3:143-147.
23. Tada H, Nogami A, Naito S, et al. Simple electrocardiographic criteria for identifying the site of origin of focal right atrial tachycardia. Pacing Clin Electrophysiol. 2006;21:2431-2439.
24. Kistler PM, Roberts-Thomson KC, Haqqani HM, et al. P wave morphology in focal atrial tachycardia. J Am Coll Cardiol. 2006;48:1010-1017.
25. Divakara Menon SM, Healey JS, Nair GM, et al. A case of long-RP tachycardia. J Cardiovasc Electrophysiol. 2009;20:702-704.
26. Lerman BB, Greenberg M, Overholt ED, et al. Differential electrophysiologic properties of decremental retrograde pathways in long RP’ tachycardia. Circulation. 1987;76:21-31.
27. Zipes DP. Clinical application of the electrocardiogram. J Am Coll Cardiol. 2000;36:1746-1748.
28. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias-executive summary. Circulation. 2003;108:1871-1909.
29. Farre J, Wellens HJJ. The value of electrocardiogram in diagnosing site of origin and mechanism of supraventricular tachycardia Wellens HJJ, Kulbertus HE, eds. What’s New in Electrocardiography. Boston, Mass: Martinus Nijhoff; 1981:131.
30. Ho YL, Lin LY, Lin JL, et al. Usefulness of ST-segment elevation in lead aVR during tachycardia for determining the mechanism of narrow QRS complex tachycardia. Am J Cardiol. 2003;92:1424-1428.
31. Zhong YM, Guo JH, Hou AJ, et al. A modified electrocardiographic algorithm for differentiating typical atrioventricular node reentrant tachycardia from atrioventricular reciprocating tachycardia mediated by concealed accessory pathway. Int J Clin Pract. 2006;60:1371-1377.
32. Riva SI, Della Bella P, Fassini G, et al. Value of analysis of ST segment changes during tachycardia in determining type of narrow QRS complex tachycardia. J Am Coll Cardiol. 1996;27:1480-1485.
33. Green M, Heddle B, Dassen W, et al. Value of QRS alteration in determining the site of origin of narrow QRS supraventricular tachycardia. Circulation. 1983;68:368-373.
34. Kalbfleisch SJ, el-Atassi R, Calkins H, et al. Differentiation of paroxysmal narrow QRS complex tachycardias using the 12-lead electrocardiogram. J Am Coll Cardiol. 1993;21:85-89.
35. Morady F. Significance of QRS alternans during narrow QRS tachycardias. Pacing Clin Electrophysiol. 1991;14:2193-2198.
•Analyze P wave axis, morphology, and timing for help in diagnosing narrow QRS complex tachycardia. C
•Review the modes of onset and termination for clues to the specific type of tachycardia, including features such as the rate of acceleration and the response to medication and the Valsalva maneuver. C
•Compare a baseline 12-lead EKG with one taken during an episode of tachycardia, looking for clues to the mechanism of the arrhythmia. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sinus tachycardia educational video for patients
Courtesy of: WirelessDx
Go to http://www.wirelessdx.com/sinustachycardia.htm

Narrow QRS complex tachycardias—rhythms with a rate >100 beats per minute (bpm) and a QRS duration <120 ms—are frequently encountered in both inpatient and outpatient settings. Therapeutic strategy ranges from simple reassurance to acute inpatient intervention, depending on the specific arrhythmia.
Early and accurate diagnosis is paramount to avoid unnecessary testing, ensure timely management, and prevent complications and long-term adverse outcomes. While most narrow QRS complex tachycardias are easily diagnosed, some pose a diagnostic challenge.

This review can help. We start with a summary of the various types of narrow QRS complex tachycardias, accompanied in some cases with 12-lead electrocardiogram (EKG) strips. Next, we highlight key characteristics to consider in the differential and provide an algorithm to help you zero in on the diagnosis.
Narrow QRS complex tachycardias: What you’ll find
Narrow QRS complex tachycardias fall into 2 broad categories: those that are sinus node-generated, and those that are not. Here’s a look at both.
Sinus node-generated tachycardias
Sinus node tachycardia (FIGURE 1), the most common arrhythmia,1 is an appropriate response to physiologic or emotional stress or disease processes. It is defined as a heart rate >100 bpm with the presence of P waves of normal sinus morphology on a 12-lead EKG.
FIGURE 1
Sinus tachycardia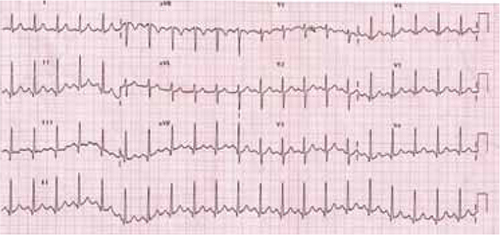
The P waves show normal sinus morphology. Note superior-to-inferior axis with positive P deflections in leads II, III, and aVF.
Inappropriate sinus tachycardia is a nonparoxysmal arrhythmia with a resting daytime heart rate >100 bpm (or an average heart rate >90 bpm over a 24-hour period), normal P wave morphology, and an exaggerated response to physical activity.2,3 What distinguishes it from simple sinus tachycardia is the disproportionate degree of the arrhythmia to the level of physiologic stress.
Inappropriate sinus tachycardia is a diagnosis of exclusion, established only after other reversible pathologic or pharmacologic causes of tachycardia, such as hyperthyroidism, pheochromocytoma, infection, or theophylline toxicity, have been ruled out. Possible mechanisms may include autonomic dysfunction with increased cardiac sympathetic or reduced vagal output.4
Paroxysmal orthostatic tachycardia syndrome (POTS) is an abnormal sinus tachycardia response to an upright position.5,6 It is diagnosed by a heart rate ≥120 bpm or an increase ≥30 bpm within 5 minutes of standing up or being on a tilt table, with simultaneous development of orthostatic symptoms, such as dizziness, light-headedness, or even syncope, without the corresponding drop in blood pressure. Symptoms usually resolve after the patient assumes a supine position. The presentation may overlap with that of inappropriate sinus tachycardia, although patients with POTS usually develop autonomic symptoms such as constipation, tremor, or heat/cold intolerance, as well.7,8
Sinus node reentry tachycardia is a paroxysmal tachycardia with a normal P wave on a 12-lead EKG. The paroxysmal nature of the arrhythmia and a positive response to atropine and vagal maneuvers, as well as identification by electrophysiologic studies, differentiate this condition from inappropriate sinus tachycardia.9
Nonsinus node-generated tachycardias
Focal atrial tachycardia (FIGURE 2) is caused by an automatic, triggered, or microreentrant mechanism that can be localized to a specific area of atrial tissue.10 The diagnosis can often be made by a careful review of the EKG, which will reveal P waves that differ from those of the sinus beat.11 This can be tricky, however, as a P wave on a 12-lead EKG from a focal point close to the sinoatrial node may resemble that of a normal sinus rhythm.
FIGURE 2
Focal atrial tachycardia
The P waves differ from those of the sinus beat. Note the positive P wave in lead aVR.
The atrial rate associated with this condition can vary from 120 to 300 bpm, depending on the focus, and may be associated with variable degrees of atrioventricular (AV) block. The crista terminalis in the right atrium and pulmonary vein ostia are frequent origins of focal atrial arrhythmias.12,13
Multifocal atrial tachycardia (FIGURE 3) is a supraventricular arrhythmia with ≥3 different P wave morphologies, as well as varying PR and RR intervals on the 12-lead EKG. It is typically associated with lung disorders but may occur in patients with other conditions, such as theophylline toxicity.14
FIGURE 3
Multifocal atrial tachycardia
The P waves have varied morphologies; the PR and RR intervals also vary, which is best seen in lead V1.
Atrioventricular nodal reentrant tachycardia (AVNRT), a reentrant form of narrow QRS complex tachycardia, is based on a dual (slow and fast) pathway of the compact AV node (FIGURE 4). In the typical form—constituting 90% of cases15—antegrade conduction is via the slow pathway and retrograde conduction is via the fast pathway.16 In the atypical form, it’s the other way around.
FIGURE 4
Atrioventricular nodal reentrant tachycardia
Note the “pseudo S” waves, which is best seen in leads II, III, and aVF. This represents retrograde activation of the atria with an inferior-to-superior axis. The RP interval is very short.
Orthodromic atrioventricular reciprocating tachycardia (AVRT), or Wolff-Parkinson-White syndrome, is a narrow QRS complex tachycardia in which antegrade conduction is via the AV node and retrograde conduction is via an accessory pathway (bundle of Kent). The accessory pathway consists of a band of muscle tissue that connects the atrium directly to the ventricles, allowing electrical impulses to bypass the AV node. Antidromic AVRT, a wide QRS complex tachycardia, is the most common supraventricular arrhythmia in patients with accessory pathways.17
Atrial fibrillation (FIGURE 5), the most common arrhythmia for which medical treatment is required,18 is an irregular rhythm with an undulating baseline.19
FIGURE 5
Atrial fibrillation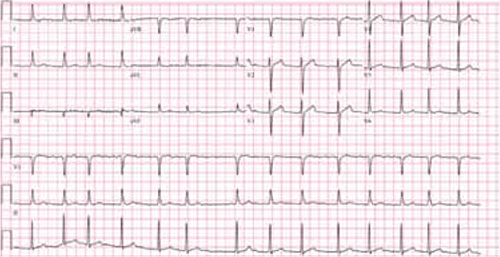
This strip shows an irregularly irregular rhythm with no distinct P waves. The undulating baseline represents fibrillatory waves.
Atrial flutter is a reentrant tachycardia originating in either atrium, with regular flutter (F) waves on a 12-lead EKG (FIGURE 6). A counterclockwise propagating isthmus-dependent atrial flutter originating in the right atrium produces the typical “sawtooth” pattern of negative F waves in the inferior electrocardiographic leads.
FIGURE 6
Atrial flutter
Note the regular flutter waves (“sawtooth waves”) best seen in lead II with variable AV conduction.
Junctional ectopic tachycardia is a rare arrhythmia caused by increased automaticity within the bundle of His.20,21 It is typically diagnosed in childhood and usually presents as a narrow QRS tachycardia with AV dissociation,22 but retrograde conduction to the atrium has also been found.21
How to approach the differential diagnosis
There are a number of characteristics to consider in the differential diagnosis of a patient with narrow QRS complex tachycardia (ALGORITHM).1,23-29 These include:
- rhythm regularity
- P wave axis and morphology
- relative duration of RP and PR intervals
- P wave position relative to the QRS complex
- ST elevation in lead aVR
- onset and termination mode.
ALGORITHM
Narrow QRS complex tachycardia: Zeroing in on the diagnosis1,23-29
AVNRT, atrioventricular nodal reentrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; EKG, electrocardiogram; MAT, multifocal atrial tachycardia.
*Or technically poor EKG.
Rhythm regularity is a key consideration. An irregular rhythm and the absence of P waves (or the presence of fibrillatory waves) characterizes atrial fibrillation; irregularity and ≥3 different P wave morphologies is suggestive of multifocal atrial tachycardia. Other possibilities include frequent premature atrial contractions or a sinoatrial or AV nodal conduction block.
AV dissociation is rarely seen in narrow QRS complex tachycardia. Its presence raises the possibility of junctional ectopic tachycardia, ventricular tachycardia, or complete AV node block.
P wave axis and morphology can help with both the differentiation and the origin of narrow QRS complex tachycardias. A superior-to-inferior axis of P waves (positivity in leads II, III, and aVF) is seen in sinus node-generated tachycardias and sometimes in focal atrial tachycardia. An inferior-superior P wave axis (negativity in leads II, III, and aVF) is observed in AVNRT, AVRT, and a subset of focal atrial tachycardia.23,24
The specific P wave axis and morphology in focal atrial tachycardia depends on the site of atrial automaticity. If the origin is near the sinus node region or high in the atrium, the result would be a superior-to-inferior P wave axis; if it originates lower in the atrium, the resulting atrial depolarization would be an inferior-to-superior axis.23,24
Relative duration of RP and PR intervals can help to differentiate narrow QRS complex tachycardias based on the timing of the P wave with respect to adjacent QRS complexes. Those in which the RP interval is longer than the PR interval are called long RP tachycardias and include sinus tachycardia, intra-atrial tachycardia, atypical AVNRT, and AVRT with a slowly conducting ventriculoatrial pathway.25,26
Short RP tachycardias are characterized by an RP interval that’s shorter than the PR interval. Only 2 arrhythmias present as short RP tachycardias: AVNRT and AVRT.27 If the RP interval is <70 ms, AVNRT is the likely diagnosis.28
P wave position. A careful review of the position of the P wave with respect to the QRS complex can provide additional help in distinguishing between AVNRT and AVRT. In 66% of AVNRTs, the P wave is hidden within the QRS complex;29 in 30%, a retrograde P wave closely follows the QRS complex, creating a “pseudo-S” wave; and 4% of the time, the P wave precedes the QRS complex.
In AVRT, a retrograde P wave follows the QRS complex. This creates a potential dilemma in differentiating 30% of AVNRTs from AVRT. In AVNRT, the retrograde P wave typically appears very close to the QRS complex, creating a pseudo-S wave. In the orthodromic AVRT, there is usually a separation between the QRS and retrograde P wave. In general, if the RP interval is <70 ms, the arrhythmia is usually due to typical AVNRT.28
ST segment elevation in lead aVR on a 12-lead EKG in a supraventricular tachycardia is about 70% sensitive and 70% to 83% specific for a diagnosis of AVRT.30,31 ST depression of more than 2 mm or T wave inversion is more common in AVRT than in AVNRT.32 QRS alternans, which refers to variations in QRS amplitude or direction with every other beat, has been reported to be indicative of AVRT, 33,34 but may in fact be a rate-dependent phenomenon that has little to do with the mechanism of tachycardias.35
Onset and termination and other indicators. Still uncertain? Patterns of arrhythmias and modes of onset and termination may provide additional help with the differential diagnosis.
Sinus tachycardias and atrial tachycardias frequently demonstrate a “warm up” in rate, for instance, while AVNRT and AVRT are often triggered by premature atrial contractions. A positive response to the Valsalva maneuver or to adenosine is typically characteristic of reentrant tachycardias using the AV node, such as AVNRT and AVRT.
Comparing a baseline 12-lead EKG with an EKG taken during an episode of tachycardia often provides further information about the mechanism of the arrhythmia. The presence of pre-excitation, the morphology of P waves, and the lack of retrograde P waves on a baseline EKG can be useful in narrowing the differential diagnosis.
Figures courtesy of: University of Buffalo and Buffalo General Hospital.
CORRESPONDENCE Vipul Gupta, MD, MPH, State University of New York at Buffalo, 131 Biomedical Education Building, Buffalo, NY 14214;
•Analyze P wave axis, morphology, and timing for help in diagnosing narrow QRS complex tachycardia. C
•Review the modes of onset and termination for clues to the specific type of tachycardia, including features such as the rate of acceleration and the response to medication and the Valsalva maneuver. C
•Compare a baseline 12-lead EKG with one taken during an episode of tachycardia, looking for clues to the mechanism of the arrhythmia. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sinus tachycardia educational video for patients
Courtesy of: WirelessDx
Go to http://www.wirelessdx.com/sinustachycardia.htm

Narrow QRS complex tachycardias—rhythms with a rate >100 beats per minute (bpm) and a QRS duration <120 ms—are frequently encountered in both inpatient and outpatient settings. Therapeutic strategy ranges from simple reassurance to acute inpatient intervention, depending on the specific arrhythmia.
Early and accurate diagnosis is paramount to avoid unnecessary testing, ensure timely management, and prevent complications and long-term adverse outcomes. While most narrow QRS complex tachycardias are easily diagnosed, some pose a diagnostic challenge.

This review can help. We start with a summary of the various types of narrow QRS complex tachycardias, accompanied in some cases with 12-lead electrocardiogram (EKG) strips. Next, we highlight key characteristics to consider in the differential and provide an algorithm to help you zero in on the diagnosis.
Narrow QRS complex tachycardias: What you’ll find
Narrow QRS complex tachycardias fall into 2 broad categories: those that are sinus node-generated, and those that are not. Here’s a look at both.
Sinus node-generated tachycardias
Sinus node tachycardia (FIGURE 1), the most common arrhythmia,1 is an appropriate response to physiologic or emotional stress or disease processes. It is defined as a heart rate >100 bpm with the presence of P waves of normal sinus morphology on a 12-lead EKG.
FIGURE 1
Sinus tachycardia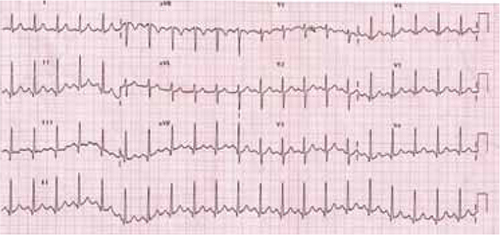
The P waves show normal sinus morphology. Note superior-to-inferior axis with positive P deflections in leads II, III, and aVF.
Inappropriate sinus tachycardia is a nonparoxysmal arrhythmia with a resting daytime heart rate >100 bpm (or an average heart rate >90 bpm over a 24-hour period), normal P wave morphology, and an exaggerated response to physical activity.2,3 What distinguishes it from simple sinus tachycardia is the disproportionate degree of the arrhythmia to the level of physiologic stress.
Inappropriate sinus tachycardia is a diagnosis of exclusion, established only after other reversible pathologic or pharmacologic causes of tachycardia, such as hyperthyroidism, pheochromocytoma, infection, or theophylline toxicity, have been ruled out. Possible mechanisms may include autonomic dysfunction with increased cardiac sympathetic or reduced vagal output.4
Paroxysmal orthostatic tachycardia syndrome (POTS) is an abnormal sinus tachycardia response to an upright position.5,6 It is diagnosed by a heart rate ≥120 bpm or an increase ≥30 bpm within 5 minutes of standing up or being on a tilt table, with simultaneous development of orthostatic symptoms, such as dizziness, light-headedness, or even syncope, without the corresponding drop in blood pressure. Symptoms usually resolve after the patient assumes a supine position. The presentation may overlap with that of inappropriate sinus tachycardia, although patients with POTS usually develop autonomic symptoms such as constipation, tremor, or heat/cold intolerance, as well.7,8
Sinus node reentry tachycardia is a paroxysmal tachycardia with a normal P wave on a 12-lead EKG. The paroxysmal nature of the arrhythmia and a positive response to atropine and vagal maneuvers, as well as identification by electrophysiologic studies, differentiate this condition from inappropriate sinus tachycardia.9
Nonsinus node-generated tachycardias
Focal atrial tachycardia (FIGURE 2) is caused by an automatic, triggered, or microreentrant mechanism that can be localized to a specific area of atrial tissue.10 The diagnosis can often be made by a careful review of the EKG, which will reveal P waves that differ from those of the sinus beat.11 This can be tricky, however, as a P wave on a 12-lead EKG from a focal point close to the sinoatrial node may resemble that of a normal sinus rhythm.
FIGURE 2
Focal atrial tachycardia
The P waves differ from those of the sinus beat. Note the positive P wave in lead aVR.
The atrial rate associated with this condition can vary from 120 to 300 bpm, depending on the focus, and may be associated with variable degrees of atrioventricular (AV) block. The crista terminalis in the right atrium and pulmonary vein ostia are frequent origins of focal atrial arrhythmias.12,13
Multifocal atrial tachycardia (FIGURE 3) is a supraventricular arrhythmia with ≥3 different P wave morphologies, as well as varying PR and RR intervals on the 12-lead EKG. It is typically associated with lung disorders but may occur in patients with other conditions, such as theophylline toxicity.14
FIGURE 3
Multifocal atrial tachycardia
The P waves have varied morphologies; the PR and RR intervals also vary, which is best seen in lead V1.
Atrioventricular nodal reentrant tachycardia (AVNRT), a reentrant form of narrow QRS complex tachycardia, is based on a dual (slow and fast) pathway of the compact AV node (FIGURE 4). In the typical form—constituting 90% of cases15—antegrade conduction is via the slow pathway and retrograde conduction is via the fast pathway.16 In the atypical form, it’s the other way around.
FIGURE 4
Atrioventricular nodal reentrant tachycardia
Note the “pseudo S” waves, which is best seen in leads II, III, and aVF. This represents retrograde activation of the atria with an inferior-to-superior axis. The RP interval is very short.
Orthodromic atrioventricular reciprocating tachycardia (AVRT), or Wolff-Parkinson-White syndrome, is a narrow QRS complex tachycardia in which antegrade conduction is via the AV node and retrograde conduction is via an accessory pathway (bundle of Kent). The accessory pathway consists of a band of muscle tissue that connects the atrium directly to the ventricles, allowing electrical impulses to bypass the AV node. Antidromic AVRT, a wide QRS complex tachycardia, is the most common supraventricular arrhythmia in patients with accessory pathways.17
Atrial fibrillation (FIGURE 5), the most common arrhythmia for which medical treatment is required,18 is an irregular rhythm with an undulating baseline.19
FIGURE 5
Atrial fibrillation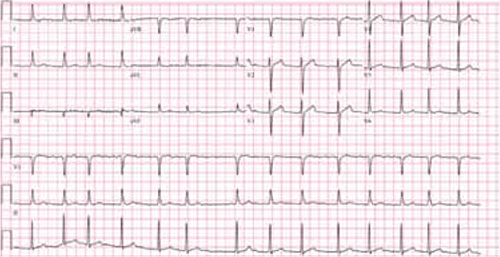
This strip shows an irregularly irregular rhythm with no distinct P waves. The undulating baseline represents fibrillatory waves.
Atrial flutter is a reentrant tachycardia originating in either atrium, with regular flutter (F) waves on a 12-lead EKG (FIGURE 6). A counterclockwise propagating isthmus-dependent atrial flutter originating in the right atrium produces the typical “sawtooth” pattern of negative F waves in the inferior electrocardiographic leads.
FIGURE 6
Atrial flutter
Note the regular flutter waves (“sawtooth waves”) best seen in lead II with variable AV conduction.
Junctional ectopic tachycardia is a rare arrhythmia caused by increased automaticity within the bundle of His.20,21 It is typically diagnosed in childhood and usually presents as a narrow QRS tachycardia with AV dissociation,22 but retrograde conduction to the atrium has also been found.21
How to approach the differential diagnosis
There are a number of characteristics to consider in the differential diagnosis of a patient with narrow QRS complex tachycardia (ALGORITHM).1,23-29 These include:
- rhythm regularity
- P wave axis and morphology
- relative duration of RP and PR intervals
- P wave position relative to the QRS complex
- ST elevation in lead aVR
- onset and termination mode.
ALGORITHM
Narrow QRS complex tachycardia: Zeroing in on the diagnosis1,23-29
AVNRT, atrioventricular nodal reentrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; EKG, electrocardiogram; MAT, multifocal atrial tachycardia.
*Or technically poor EKG.
Rhythm regularity is a key consideration. An irregular rhythm and the absence of P waves (or the presence of fibrillatory waves) characterizes atrial fibrillation; irregularity and ≥3 different P wave morphologies is suggestive of multifocal atrial tachycardia. Other possibilities include frequent premature atrial contractions or a sinoatrial or AV nodal conduction block.
AV dissociation is rarely seen in narrow QRS complex tachycardia. Its presence raises the possibility of junctional ectopic tachycardia, ventricular tachycardia, or complete AV node block.
P wave axis and morphology can help with both the differentiation and the origin of narrow QRS complex tachycardias. A superior-to-inferior axis of P waves (positivity in leads II, III, and aVF) is seen in sinus node-generated tachycardias and sometimes in focal atrial tachycardia. An inferior-superior P wave axis (negativity in leads II, III, and aVF) is observed in AVNRT, AVRT, and a subset of focal atrial tachycardia.23,24
The specific P wave axis and morphology in focal atrial tachycardia depends on the site of atrial automaticity. If the origin is near the sinus node region or high in the atrium, the result would be a superior-to-inferior P wave axis; if it originates lower in the atrium, the resulting atrial depolarization would be an inferior-to-superior axis.23,24
Relative duration of RP and PR intervals can help to differentiate narrow QRS complex tachycardias based on the timing of the P wave with respect to adjacent QRS complexes. Those in which the RP interval is longer than the PR interval are called long RP tachycardias and include sinus tachycardia, intra-atrial tachycardia, atypical AVNRT, and AVRT with a slowly conducting ventriculoatrial pathway.25,26
Short RP tachycardias are characterized by an RP interval that’s shorter than the PR interval. Only 2 arrhythmias present as short RP tachycardias: AVNRT and AVRT.27 If the RP interval is <70 ms, AVNRT is the likely diagnosis.28
P wave position. A careful review of the position of the P wave with respect to the QRS complex can provide additional help in distinguishing between AVNRT and AVRT. In 66% of AVNRTs, the P wave is hidden within the QRS complex;29 in 30%, a retrograde P wave closely follows the QRS complex, creating a “pseudo-S” wave; and 4% of the time, the P wave precedes the QRS complex.
In AVRT, a retrograde P wave follows the QRS complex. This creates a potential dilemma in differentiating 30% of AVNRTs from AVRT. In AVNRT, the retrograde P wave typically appears very close to the QRS complex, creating a pseudo-S wave. In the orthodromic AVRT, there is usually a separation between the QRS and retrograde P wave. In general, if the RP interval is <70 ms, the arrhythmia is usually due to typical AVNRT.28
ST segment elevation in lead aVR on a 12-lead EKG in a supraventricular tachycardia is about 70% sensitive and 70% to 83% specific for a diagnosis of AVRT.30,31 ST depression of more than 2 mm or T wave inversion is more common in AVRT than in AVNRT.32 QRS alternans, which refers to variations in QRS amplitude or direction with every other beat, has been reported to be indicative of AVRT, 33,34 but may in fact be a rate-dependent phenomenon that has little to do with the mechanism of tachycardias.35
Onset and termination and other indicators. Still uncertain? Patterns of arrhythmias and modes of onset and termination may provide additional help with the differential diagnosis.
Sinus tachycardias and atrial tachycardias frequently demonstrate a “warm up” in rate, for instance, while AVNRT and AVRT are often triggered by premature atrial contractions. A positive response to the Valsalva maneuver or to adenosine is typically characteristic of reentrant tachycardias using the AV node, such as AVNRT and AVRT.
Comparing a baseline 12-lead EKG with an EKG taken during an episode of tachycardia often provides further information about the mechanism of the arrhythmia. The presence of pre-excitation, the morphology of P waves, and the lack of retrograde P waves on a baseline EKG can be useful in narrowing the differential diagnosis.
Figures courtesy of: University of Buffalo and Buffalo General Hospital.
CORRESPONDENCE Vipul Gupta, MD, MPH, State University of New York at Buffalo, 131 Biomedical Education Building, Buffalo, NY 14214;
1. Yusuf S, Camm AJ. Deciphering the sinus tachycardias. Clin Cardiol. 2005;28:267-276.
2. Lee RJ, Shinbane JS. Inappropriate sinus tachycardia. Diagnosis and treatment. Cardiol Clin. 1997;15:599-605.
3. Morillo CA, Klein GJ, Thakur RK, et al. Mechanism of ‘inappropriate’ sinus tachycardia. Circulation. 1994;90:873-877.
4. Bauernfeind RA, Amat-y-Leon F, Dhingra RC, et al. Chronic nonparoxysmal sinus tachycardia in otherwise healthy persons. Ann Intern Med. 1979;91:702-710.
5. Low PA, Opfer-Gehrking TL, Textor SC, et al. Postural tachycardia syndrome (POTS). Neurology. 1995;45(suppl 5):S19-S25.
6. Raj SR. The postural tachycardia syndrome (POTS): pathophysiology, diagnosis & management. Indian Pacing Electrophysiol J. 2006;6:84-99.
7. Grubb BP, Kanjwal MY, Kosinski DJ. Review: the postural orthostatic tachycardia syndrome. J Interv Card Electrophysiol. 2001;5:9-16.
8. Kanjwal MY, Kosinski DJ, Grubb BP. Treatment of postural orthostatic tachycardia syndrome and inappropriate sinus tachycardia. Curr Cardiol Rep. 2003;5:402-406.
9. Simmers TA, Sreeram N. Sinoatrial reentry tachycardia: a review. Indian Pacing Electrophysiol J. 2003;3:109-116.
10. Saoudi N, Cosío F, Waldo A, et al. Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical bases. Eur Heart J. 2001;22:1162-1182.
11. Teh AW, Kistler PM, Kalman JM. Using the 12-lead ECG to localize the origin of ventricular and atrial tachycardias: part 1.J Cardiovasc Electrophysiol. 2009;20:706-709.
12. Roberts-Thomson KC, Kistler PM, Kalman JM. Focal atrial tachycardia I: clinical features, diagnosis, mechanisms, and anatomic location. Pacing Clin Electrophysiol. 2006;29:643-652.
13. Rosso R, Kistler PM. Focal atrial tachycardia. Heart. 2010;96:181-185.
14. Schwartz M, Rodman D, Lowenstein SR. Recognition and treatment of multifocal atrial tachycardia: a critical review. J Emerg Med. 1994;12:353-360.
15. Kwaku KF, Josephson ME. Typical AVNRT-an update on mechanisms and therapy. Cardiol Electrophysiol Rev. 2002;6:414-421.
16. Nawata H, Yamamoto N, Hirao K, et al. Heterogeneity of anterograde fast-pathway and retrograde slow-pathway conduction patterns in patients with the fast-slow form of atrioventricular nodal reentrant tachycardia. J Am Coll Cardiol. 1998;32:1731-1740.
17. Fox DJ, Tischenko A, Krahn AD, et al. Supraventricular tachycardia. Mayo Clin Proc. 2008;83:1400-1411.
18. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention. JAMA. 2001;285:2370-2375.
19. Falk RH. Atrial fibrillation. N Engl J Med. 2001;344:1067-1078.
20. Garson A, Gillette PC. Junctional ectopic tachycardia in children: electrocardiography, electrophysiology and pharmacologic response. Am J Cardiol. 1979;44:298-302.
21. Villain E, Vetter VL, Garcia JM, et al. Evolving concepts in the management of congenital junctional ectopic tachycardia. A multicenter study. Circulation. 1990;81:1544-1549.
22. Sarubbi B, Vergara P, D’Alto M, et al. Congenital junctional ectopic tachycardia: presentation and outcome. Indian Pacing Electrophysiol J. 2003;3:143-147.
23. Tada H, Nogami A, Naito S, et al. Simple electrocardiographic criteria for identifying the site of origin of focal right atrial tachycardia. Pacing Clin Electrophysiol. 2006;21:2431-2439.
24. Kistler PM, Roberts-Thomson KC, Haqqani HM, et al. P wave morphology in focal atrial tachycardia. J Am Coll Cardiol. 2006;48:1010-1017.
25. Divakara Menon SM, Healey JS, Nair GM, et al. A case of long-RP tachycardia. J Cardiovasc Electrophysiol. 2009;20:702-704.
26. Lerman BB, Greenberg M, Overholt ED, et al. Differential electrophysiologic properties of decremental retrograde pathways in long RP’ tachycardia. Circulation. 1987;76:21-31.
27. Zipes DP. Clinical application of the electrocardiogram. J Am Coll Cardiol. 2000;36:1746-1748.
28. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias-executive summary. Circulation. 2003;108:1871-1909.
29. Farre J, Wellens HJJ. The value of electrocardiogram in diagnosing site of origin and mechanism of supraventricular tachycardia Wellens HJJ, Kulbertus HE, eds. What’s New in Electrocardiography. Boston, Mass: Martinus Nijhoff; 1981:131.
30. Ho YL, Lin LY, Lin JL, et al. Usefulness of ST-segment elevation in lead aVR during tachycardia for determining the mechanism of narrow QRS complex tachycardia. Am J Cardiol. 2003;92:1424-1428.
31. Zhong YM, Guo JH, Hou AJ, et al. A modified electrocardiographic algorithm for differentiating typical atrioventricular node reentrant tachycardia from atrioventricular reciprocating tachycardia mediated by concealed accessory pathway. Int J Clin Pract. 2006;60:1371-1377.
32. Riva SI, Della Bella P, Fassini G, et al. Value of analysis of ST segment changes during tachycardia in determining type of narrow QRS complex tachycardia. J Am Coll Cardiol. 1996;27:1480-1485.
33. Green M, Heddle B, Dassen W, et al. Value of QRS alteration in determining the site of origin of narrow QRS supraventricular tachycardia. Circulation. 1983;68:368-373.
34. Kalbfleisch SJ, el-Atassi R, Calkins H, et al. Differentiation of paroxysmal narrow QRS complex tachycardias using the 12-lead electrocardiogram. J Am Coll Cardiol. 1993;21:85-89.
35. Morady F. Significance of QRS alternans during narrow QRS tachycardias. Pacing Clin Electrophysiol. 1991;14:2193-2198.
1. Yusuf S, Camm AJ. Deciphering the sinus tachycardias. Clin Cardiol. 2005;28:267-276.
2. Lee RJ, Shinbane JS. Inappropriate sinus tachycardia. Diagnosis and treatment. Cardiol Clin. 1997;15:599-605.
3. Morillo CA, Klein GJ, Thakur RK, et al. Mechanism of ‘inappropriate’ sinus tachycardia. Circulation. 1994;90:873-877.
4. Bauernfeind RA, Amat-y-Leon F, Dhingra RC, et al. Chronic nonparoxysmal sinus tachycardia in otherwise healthy persons. Ann Intern Med. 1979;91:702-710.
5. Low PA, Opfer-Gehrking TL, Textor SC, et al. Postural tachycardia syndrome (POTS). Neurology. 1995;45(suppl 5):S19-S25.
6. Raj SR. The postural tachycardia syndrome (POTS): pathophysiology, diagnosis & management. Indian Pacing Electrophysiol J. 2006;6:84-99.
7. Grubb BP, Kanjwal MY, Kosinski DJ. Review: the postural orthostatic tachycardia syndrome. J Interv Card Electrophysiol. 2001;5:9-16.
8. Kanjwal MY, Kosinski DJ, Grubb BP. Treatment of postural orthostatic tachycardia syndrome and inappropriate sinus tachycardia. Curr Cardiol Rep. 2003;5:402-406.
9. Simmers TA, Sreeram N. Sinoatrial reentry tachycardia: a review. Indian Pacing Electrophysiol J. 2003;3:109-116.
10. Saoudi N, Cosío F, Waldo A, et al. Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical bases. Eur Heart J. 2001;22:1162-1182.
11. Teh AW, Kistler PM, Kalman JM. Using the 12-lead ECG to localize the origin of ventricular and atrial tachycardias: part 1.J Cardiovasc Electrophysiol. 2009;20:706-709.
12. Roberts-Thomson KC, Kistler PM, Kalman JM. Focal atrial tachycardia I: clinical features, diagnosis, mechanisms, and anatomic location. Pacing Clin Electrophysiol. 2006;29:643-652.
13. Rosso R, Kistler PM. Focal atrial tachycardia. Heart. 2010;96:181-185.
14. Schwartz M, Rodman D, Lowenstein SR. Recognition and treatment of multifocal atrial tachycardia: a critical review. J Emerg Med. 1994;12:353-360.
15. Kwaku KF, Josephson ME. Typical AVNRT-an update on mechanisms and therapy. Cardiol Electrophysiol Rev. 2002;6:414-421.
16. Nawata H, Yamamoto N, Hirao K, et al. Heterogeneity of anterograde fast-pathway and retrograde slow-pathway conduction patterns in patients with the fast-slow form of atrioventricular nodal reentrant tachycardia. J Am Coll Cardiol. 1998;32:1731-1740.
17. Fox DJ, Tischenko A, Krahn AD, et al. Supraventricular tachycardia. Mayo Clin Proc. 2008;83:1400-1411.
18. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention. JAMA. 2001;285:2370-2375.
19. Falk RH. Atrial fibrillation. N Engl J Med. 2001;344:1067-1078.
20. Garson A, Gillette PC. Junctional ectopic tachycardia in children: electrocardiography, electrophysiology and pharmacologic response. Am J Cardiol. 1979;44:298-302.
21. Villain E, Vetter VL, Garcia JM, et al. Evolving concepts in the management of congenital junctional ectopic tachycardia. A multicenter study. Circulation. 1990;81:1544-1549.
22. Sarubbi B, Vergara P, D’Alto M, et al. Congenital junctional ectopic tachycardia: presentation and outcome. Indian Pacing Electrophysiol J. 2003;3:143-147.
23. Tada H, Nogami A, Naito S, et al. Simple electrocardiographic criteria for identifying the site of origin of focal right atrial tachycardia. Pacing Clin Electrophysiol. 2006;21:2431-2439.
24. Kistler PM, Roberts-Thomson KC, Haqqani HM, et al. P wave morphology in focal atrial tachycardia. J Am Coll Cardiol. 2006;48:1010-1017.
25. Divakara Menon SM, Healey JS, Nair GM, et al. A case of long-RP tachycardia. J Cardiovasc Electrophysiol. 2009;20:702-704.
26. Lerman BB, Greenberg M, Overholt ED, et al. Differential electrophysiologic properties of decremental retrograde pathways in long RP’ tachycardia. Circulation. 1987;76:21-31.
27. Zipes DP. Clinical application of the electrocardiogram. J Am Coll Cardiol. 2000;36:1746-1748.
28. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias-executive summary. Circulation. 2003;108:1871-1909.
29. Farre J, Wellens HJJ. The value of electrocardiogram in diagnosing site of origin and mechanism of supraventricular tachycardia Wellens HJJ, Kulbertus HE, eds. What’s New in Electrocardiography. Boston, Mass: Martinus Nijhoff; 1981:131.
30. Ho YL, Lin LY, Lin JL, et al. Usefulness of ST-segment elevation in lead aVR during tachycardia for determining the mechanism of narrow QRS complex tachycardia. Am J Cardiol. 2003;92:1424-1428.
31. Zhong YM, Guo JH, Hou AJ, et al. A modified electrocardiographic algorithm for differentiating typical atrioventricular node reentrant tachycardia from atrioventricular reciprocating tachycardia mediated by concealed accessory pathway. Int J Clin Pract. 2006;60:1371-1377.
32. Riva SI, Della Bella P, Fassini G, et al. Value of analysis of ST segment changes during tachycardia in determining type of narrow QRS complex tachycardia. J Am Coll Cardiol. 1996;27:1480-1485.
33. Green M, Heddle B, Dassen W, et al. Value of QRS alteration in determining the site of origin of narrow QRS supraventricular tachycardia. Circulation. 1983;68:368-373.
34. Kalbfleisch SJ, el-Atassi R, Calkins H, et al. Differentiation of paroxysmal narrow QRS complex tachycardias using the 12-lead electrocardiogram. J Am Coll Cardiol. 1993;21:85-89.
35. Morady F. Significance of QRS alternans during narrow QRS tachycardias. Pacing Clin Electrophysiol. 1991;14:2193-2198.