User login
Hypertensive chronic kidney disease in African Americans: Strategies for improving care
“Healthy citizens are the greatest asset any country can have.”
—Winston Churchill
Diabetes and high blood pressure take a toll on the kidneys, especially in African Americans. To prevent chronic kidney disease (CKD) and to slow or stop its progression, the same principles apply in African Americans as in other patients—ie, vigilance for the onset of proteinuria, aggressive control of blood pressure, drug treatment to block the renin-angiotensin system, and attention to lifestyle factors (Table 1). However, we need to try to do better in the care of African Americans.
The purpose of this article is to review recent evidence- and consensus-based recommendations and to present a practical approach for the evaluation and treatment of CKD in African Americans.
CKD DEFINED
In 2002, the National Kidney Foundation1 defined CKD as either:
- Kidney damage for 3 or more months, as defined by structural or functional abnormalities of the kidney, with or without a decreased glomerular filtration rate (GFR), manifested either by pathologic abnormalities or by markers of kidney damage, including abnormalities in the composition of the blood or urine (eg, proteinuria), or abnormalities in imaging tests; or
- A GFR less than 60 mL/min/1.73 m2 for 3 or more months, with or without kidney damage.
The definition divides CKD into five progressive stages according to the GFR:
- Stage 1 (kidney damage with normal or increased GFR): GFR ≥ 90 mL/min/1.73m2
- Stage 2 (kidney damage with mildly decreased GFR): GFR 60–89
- Stage 3 (moderately decreased GFR): GFR 30–59
- Stage 4 (severely decreased GFR): GFR 15–29
- Stage 5 (kidney failure): GFR < 15 or dialysis.
Because the definition includes markers of kidney damage such as albuminuria, it allows CKD to be detected in its earliest stages, when the estimated GFR might still be well within normal limits.
CKD APPEARS EARLIER, PROGRESSES FASTER IN AFRICAN AMERICANS
“Not everything that counts can be counted, and not everything that can be counted counts.”
—Albert Einstein
CKD with or without a sustained reduction in the estimated GFR affects about one in every nine American adults.2 Its course varies depending on the cause and also from patient to patient, even in those with the same cause of CKD.
In general, the prevalence of early CKD is comparable across racial and ethnic groups in the United States, but CKD progresses to end-stage renal disease far more rapidly in minority populations, with rates nearly four times higher in black Americans than in white Americans.3 Also, the onset of CKD is earlier in African Americans.
HYPERTENSION AND DIABETES AS REASONS FOR THE DISPARITIES
Part of the reason for these differences is that minority populations have higher rates of diabetes and hypertension, and these diseases tend to be more severe in these groups. Poverty, less access to health care, exposure to environmental toxins, and genetic variation may also contribute.4–7
Compared with whites, blacks have higher rates of diabetes and hypertension and earlier onset of these diseases, poorer control, and higher rates of complications such as CKD, stroke, and heart disease.8,9 The higher rate of hypertension and the lower rate of blood pressure control in African Americans with CKD may contribute to the more rapid progression of CKD to end-stage renal disease.
In the Chronic Renal Insufficiency Cohort, 10 a racially and ethnically diverse group of 3,612 adults with a broad spectrum of renal disease severity, 93% of African Americans had hypertension at baseline compared with 80% of whites. In addition, African Americans were 18% less likely to have their blood pressure controlled to 140/90 mm Hg (the rates of control were 76% vs 60%), and 28% were less likely to have it controlled to 130/80 mm Hg (56% vs 38%).10 These factors may partially explain the faster progression to end-stage renal disease in African Americans with CKD.
Despite the potential efficacy of strict control of serum glucose levels and blood pressure,11 the high rate of poor blood pressure control has contributed to the epidemic of diabetic nephropathy, especially among African Americans. Fortunately, hypertension control in the general population, while still not ideal, has improved from 27% in 1988–1994 to 50% in 2007–2008 and is now similar across racial and ethnic groups.12 This, hopefully, is a preface for improved hypertension-related outcomes for all Americans over the next decade.
OTHER REASONS FOR THE DISPARITIES
“There are no unnatural or supernatural phenomena, only a very large gap in our knowledge of what is natural.”
—Edgar Mitchell, Apollo 14 astronaut
Proteinuria
Proteinuria is another key cardiorenal risk factor prevalent in African Americans.
Knight et al,13 analyzing data from the Third National Health and Nutrition Examination Survey, found that people with high-normal blood pressure (systolic pressure 130–139 mm Hg or diastolic pressure 85–89 mm Hg) were twice as likely to have microalbuminuria (odds ratio 2.13, 95% confidence interval [CI] 1.51–3.01) compared with people with optimal blood pressure (systolic pressure < 120 mm Hg and diastolic pressure < 80 mm Hg). Compared with whites as the reference group, Mexican Americans had slightly but not statistically significantly higher odds of microalbuminuria (odds ratio 1.16; 95% CI 0.90–1.51), and African Americans had significantly higher odds (odds ratio 1.30; 95% CI 1.04–1.64).
The incidence of hypertension-related end-stage renal disease is nearly five times higher in African Americans than in whites, and the rate of hypertension-related end-stage renal disease is 15 times higher in African American men ages 24 to 44 than in whites of the same ages.3 The greater risk of proteinuria in African Americans at any given level of higher blood pressure is thought to contribute in part to these disparate rates.
The renin-angiotensin system
The renin-angiotensin system plays a role in modulating hypertension and mediating hypertension-related complications. Hypertensive African Americans are more likely than hypertensive whites to have low-renin, salt-sensitive hypertension. Therein lies a paradox.
Since the renin-angiotensin system promotes the progression of CKD, we would expect patients with low-renin hypertension to have a lower risk of hypertension-related endorgan damage than patients with high-renin hypertension. However, many African Americans (who as a group have high rates of sodium sensitivity and low plasma renin levels) experience more severe hypertension-related end-organ complications such as proteinuria and cardiorenal disease.14
A reason for this paradox may be that the circulating renin-angiotensin system is separate from the intrarenal one. Supporting this theory is the observation that up-regulation of the intrarenal renin-angiotensin system accompanies renal interstitial inflammation and oxidative stress in the kidneys and cardiovascular tissues of salt-sensitive rats fed a high-salt diet.15 In other experiments in salt-sensitive rats, renin-angiotensin system blockade reversed endothelial dysfunction, attenuated proteinuria, and reduced renal injury independent of blood pressure changes even though the animals had low circulating renin levels.16
These findings imply that drugs that block the renin-angiotensin system, ie, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, could still be a rational therapy for CKD patients with low-renin hypertension, particularly African Americans, in whom local up-regulation of the renin-angiotensin system in the kidney could exacerbate both diabetic and hypertensive CKD.17 Although these drugs may not lower blood pressure as much in low-renin hypertension as in high-renin hypertension, they may still afford the same cardiorenal protection.
Genetic factors
Variations in the MYH9 and APOL1 genes on chromosome 22 have recently been found in genome-wide admixture mapping studies and may explain as much as 70% of the differences in the rates of nondiabetic end-stage renal disease between white and black Americans.7,18,19 In addition, genetic variations may modulate differences in blood-pressure response to antihypertensive medications across racial and ethnic groups,20 complicating treatment recommendations and clinical outcomes in our increasingly diverse nation.
Comment. The pathophysiologic basis for the variability in the course of CKD is probably multifactorial and is still poorly understood. Nevertheless, we may be able to delay the progression of CKD and prevent its complications with specific therapeutic and life-style interventions.
Race and ethnicity are associated with sociocultural and biologic variations that influence the risk and progression of CKD. Understanding these factors for minority populations can help in targeting interventions to attenuate the disproportionately high rates of CKD progression and complications.
The pathophysiologic reason African Americans have a greater prevalence of end-stage renal disease and a more rapid progression of CKD is complex and probably involves the interplay of biological, behavioral, and environmental factors such as salt intake, stress levels, and exposure to heavy metals.21
TRIALS OF ANTIHYPERTENSIVE THERAPY IN AFRICAN AMERICANS WITH CKD
“If we knew what we were doing, it wouldn’t be called research.”
—Albert Einstein
Until recently, trials of antihypertensive therapy in patients with CKD did not include adequate numbers of African American participants, but the following clinical trials have added to our knowledge (Table 2).22–26
African American Study of Kidney Disease and Hypertension (AASK)
The African American Study of Kidney Disease and Hypertension (AASK),22,23 with 1,094 patients, was the largest prospective study of CKD to date designed to focus on African Americans.
AASK examined the effects of two levels of blood-pressure control:
- Standard, with a goal blood pressure of 135–140/85–90 mm Hg (mean arterial pressure 102–107 mm Hg)
- Intensive, with a goal of 120/80 mm Hg or less (mean arterial pressure ≤ 92 mm Hg).
In a two-by two factorial design, patients were also randomized to receive one of three antihypertensive drugs as initial therapy:
- The ACE inhibitor ramipril (Altace)
- The sustained-release beta-blocker metoprolol succinate (Toprol XL)
- The calcium channel blocker amlodipine (Norvasc).
To enter the study, patients had to be African American, have at least one diastolic pressure reading of 95 mm Hg or greater during the screening period, and have a measured GFR between 20 and 65 mL/min/1.83 m2. They could not have diabetes, substantial proteinuria (> 2.5 g/day), or other causes of CKD.22
AASK was distinct from many of the larger hypertension trials in which secondary analyses of outcomes in patients with CKD were performed in that it was implicit in the design that most, if not all, study participants had substantial GFR reduction and would need diuretic therapy.
At baseline, after blood pressure medications had been tapered to define eligibility and then reintroduced before randomization, 20.0% of the patients in the intensive blood pressure goal group had pressure lower than 140/90 mm Hg, and this increased to 78.9% by 14 months after randomization. In the standard goal group, the numbers were 21.5% at baseline but only 41.8% at 14 months.23 In spite of this difference, the rate of decline in GFR (the main clinical outcome measure) was the same in both groups.
However, the class of drug did make a difference. Secondary clinical outcomes, including the composite end point of development of end-stage renal disease, doubling of serum creatinine, or death, were less frequent in the ACE inhibitor group than in the beta-blocker and calcium channel blocker groups. As anticipated and consistent with real world practice, nearly 90% of all participants received concomitant diuretic therapy to achieve target blood pressure levels.
Comments. AASK showed that blood pressure can be controlled in African Americans who have CKD and that clinical cardiorenal outcomes can be improved by using an ACE inhibitor as initial therapy rather than a beta-blocker or calcium channel blocker, with diuretics and other agents added as needed.
AASK cohort phase
After completing the trial phase, patients were invited to enroll in a cohort phase in which the blood pressure target was less than 130/80 mm Hg. The combined follow-up period was 8.8 to 12.2 years.24
During the trial phase, the mean blood pressure was 130/78 mm Hg in the intensive group and 141/86 mm Hg in the standard group. During the cohort phase, the mean blood pressures were 131/78 mm Hg and 134/78 mm Hg, respectively, in these groups.
In both phases, there was no significant difference between groups in clinical outcomes (hazard ratio in the intensive-control group 0.91, P = .27). However, the groups differed when stratified by baseline level of proteinuria (P = .02 for the interaction), with a potential benefit of a blood pressure target lower than 130/80 mm Hg in patients with a protein-to-creatinine ratio of more than 0.22 (hazard ratio 0.73, P = .01).24
Comment. Given that many African Americans with hypertension and CKD have a protein-to-creatinine ratio of more than 0.22, these findings support a practical approach in clinical practice for a target blood pressure less than 130/80 mm Hg, using a first-line combination of a renin-angiotensin system inhibitor and a diuretic.
RENAAL study
The Reduction of Endpoints in NIDDM With the Angiotensin II Antagonist Losartan (RENAAL) study25 included 1,513 patients, of whom 15% were African American and 18% were Hispanic; all had type 2 diabetes mellitus and nephropathy. They were randomized to receive the angiotensin II receptor antagonist losartan (Cozaar) or placebo in addition to other antihypertensive drugs.
At 3.4 years, the blood pressure was about 141/74 mm Hg in both groups. A post hoc analysis found lower rates of albuminuria and end-stage renal disease in the group treated with losartan,25 with no racial or ethnic differences in its renoprotective effect.
Comments. While these findings support the recommendation of inhibiting the renin-angiotensin system for improving clinical outcomes in diabetic nephropathy in racial and ethnic minorities, the AASK study also proved a second important point. These patients required intense blood pressure management for several years in a clinical trial environment, which may be difficult to do in many clinical practice models.
To be cost-effective in today’s health care environment, such care will likely be limited to larger group practices or health care plans with large comprehensive covered populations. Payers and providers need to be willing to invest in intense early care in such high-risk subgroups with the understanding that they could recognize downstream gains from long-term improved outcomes. However, even in these settings, the ability to provide effective care to high-risk subgroups without generating significant financial losses remains a concern.
ALLHAT
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)26 enrolled more than 33,000 hypertensive patients at high risk, of whom 32% were black, 16% were Hispanic, and 36% had diabetes. Their mean serum creatinine level was 1 mg/dL. Follow-up was for up to 8 years. At year 5, the mean blood pressure was 135/75 mm Hg.
In a secondary analysis, patients were stratified by GFR:
- Normal (> 90 mL/min/1.73 m2; n = 8,126)
- Mild reduction (60–89 mL/min/1.73 m2; n = 18,109)
- Moderate-severe reduction (< 60 mL/min/1.73 m2; n = 5,662).
In all three groups, amlodipine, lisinopril (Zestril), and chlorthalidone were equivalent as initial monotherapy in reducing the rate of the composite end point of end-stage renal disease or 50% or greater decrement in GFR.
Comments. The combined AASK, RENAAL, and ALLHAT findings are consistent with the practical recommendation of a diuretic, renin-angiotensin system inhibitor, or both, as initial therapy for blood pressure control in African American patients who have CKD, with a target blood pressure of less than 130/80 mm Hg.
A COMPREHENSIVE APPROACH TO CHRONIC KIDNEY DISEASE CARE
“It is much more important to know what sort of a patient has a disease, than what sort of disease a patient has.”
—William Osler
Many of the risk factors for cardiovascular disease in African Americans are behavioral and modifiable. These include too much salt and fat in the diet, too little physical activity, excessive alcohol intake, and smoking.
Education is key, to identify and communicate the risk attributable to health beliefs and behaviors, particularly in patients with known cardiovascular disease, and to encourage the patient to be proactive in risk-reduction strategies (Table 1). However, effective communication depends on compassion and concern by the health care provider to engender a sense of trust.27 Other health care professionals such as dietitians, pharmacists, and social workers as well as family members can reinforce messages and improve communication with the patient to optimize outcomes.
The International Society on Hypertension in Blacks recommends a blood pressure target of less than 130/80 mm Hg in blacks with elevated blood pressure and target-organ damage. The authors suggest monotherapy with a diuretic or calcium channel blocker if the blood pressure is 10 mm Hg or less above target levels. When blood pressure is more than 15/10 mm Hg above target, two-drug therapy is recommended, either with a calcium channel blocker plus a renin-angiotensin system blocker or, alternatively, in edematous or volume-overload states, with a thiazide diuretic plus a renin-angiotensin system blocker.28,29
The Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease of the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative recommend starting anti-hypertensive therapy with an ACE inhibitor or an angiotensin receptor blocker for most patients with CKD, regardless of ethnicity, recognizing that many will require combination therapy.30 Evaluation of the response to therapy should include not only checking that the blood pressure is at or below the recommended target of 130/80 mm Hg, but also assessing for complications and monitoring the change in the level of proteinuria, which is a powerful predictor of progression of hypertensive kidney disease in all patients at any given GFR.31
OUR RECOMMENDATIONS
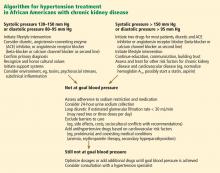
African Americans with hypertension and kidney disease require an aggressive and comprehensive approach to slow the progression of kidney disease and its complications, often necessitating aggressive care of the primary cause and the use of two or more antihypertensive agents to control blood pressure, proteinuria, or both (Figure 1).32
We recommend that the initial evaluation of patients with hypertension include a screening for albuminuria and that the initial therapy for hypertension or proteinuria in all patients with CKD include renin-angiotensin system inhibition with a diuretic, because this combination appears most effective to achieve blood pressure control and to confer additional cardiorenal protection beyond that offered by blood-pressure control alone. Although some studies have reported that African Americans have lower blood-pressure response rates than whites to renin-angiotensin system inhibition, 18 it is nevertheless beneficial for clinical outcomes in this group, especially in the presence of proteinuria, a hallmark of hypertension-related CKD in African Americans. Thus, until more data are available, ethnicity should not be the primary criterion for selecting a given class of antihypertensive therapy, especially in patients with hypertensive nephropathy.
The overall treatment decision should be guided by individual response, coexisting risk factors, and potential cultural and socioeconomic considerations such as cost of medications and insurance coverage, which affect adherence to both pharmacologic and nonpharmacologic interventions.33
Future studies should strive for adequate representation of racial and ethnic minority populations in order to enhance the evidence base for CKD treatment as we move toward using personalized medicine approaches in an increasingly diverse society.34
Acknowledgment: Support for this paper was provided in part by NIH grants RR026138 and MD000182.
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39(suppl 1):S1–S266.
- Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA 2007; 298:2038–2047.
- US Renal Data System. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2010.
- Norris K, Nissenson AR. Race, gender, and socioeconomic disparities in CKD in the United States. J Am Soc Nephrol 2008; 19:1261–1270.
- Norris KC, Agodoa LY. Unraveling the racial disparities associated with kidney disease. Kidney Int 2005; 68:914–924.
- Powe NR. To have and have not: health and health care disparities in chronic kidney disease. Kidney Int 2003; 64:763–772.
- Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 2010; 329:841–845.
- Rosamond W, Flegal K, Furie K, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008; 117:e25–e146.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Muntner P, Anderson A, Charleston J, et al; Chronic Renal Insufficiency Cohort (CRIC) Study Investigators. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 2010; 55:441–451.
- Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317:703–713.
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303:2043–2050.
- Knight EL, Kramer HM, Curhan GC. High-normal blood pressure and microalbuminuria. Am J Kidney Dis 2003; 41:588–595.
- Luft FC, Grim CE, Fineberg N, Weinberger MC. Effects of volume expansion and contraction in normotensive whites, blacks, and subjects of different ages. Circulation 1979; 59:643–650.
- Chandramohan G, Bai Y, Norris K, Rodriguez-Iturbe B, Vaziri ND. Effects of dietary salt on intrarenal angiotensin system, NAD(P)H oxidase, COX-2, MCP-1 and PAI-1 expressions and NF-kappaB activity in salt-sensitive and -resistant rat kidneys. Am J Nephrol 2008; 28:158–167.
- Hayakawa H, Coffee K, Raij L. Endothelial dysfunction and cardiorenal injury in experimental salt-sensitive hypertension: effects of antihypertensive therapy. Circulation 1997; 96:2407–2413.
- Norris KC, Tareen N, Martins D, Vaziri ND. Implications of ethnicity for the treatment of hypertensive kidney disease, with an emphasis on African Americans. Nat Clin Pract Nephrol 2008; 4:538–549.
- Kao WH, Klag MJ, Meoni LA, et al; Family Investigation of Nephropathy and Diabetes Research Group. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet 2008; 40:1185–1192.
- Freedman BI, Kopp JB, Langefeld CD, et al. The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. J Am Soc Nephrol 2010; 21:1422–1426.
- Materson BJ, Reda DJ, Cushman WC, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med 1993; 328:914–921. Erratum in N Engl J Med 1994; 330:1689.
- Norris KC, Francis CK. Gender and ethnic differences and considerations in cardiovascular risk assessment and prevention in African Americans. In:Wong N, Gardin JM, Black HR, editors. Practical Strategies in Preventing Heart Disease. New York, NY: McGraw-Hill; 2004:415–440.
- Wright JT, Bakris G, Greene T, et al; African American Study of Kidney Disease and Hypertension Study Group. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002; 288:2421–2431. Erratum in JAMA 2006; 295:2726.
- Wright JT, Agodoa L, Contreras G, et al; African American Study of Kidney Disease and Hypertension Study Group. Successful blood pressure control in the African American Study of Kidney Disease and Hypertension. Arch Intern Med 2002; 162:1636–1643.
- Appel LJ, Wright JT, Greene T, et al; AASK Collaborative Research Group. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med 2010; 363:918–929.
- de Zeeuw D, Ramjit D, Zhang Z, et al. Renal risk and renoprotection among ethnic groups with type 2 diabetic nephropathy: a post hoc analysis of RENAAL. Kidney Int 2006; 69:1675–1682.
- Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005; 165:936–946.
- Barrier PA, Li JT, Jensen NM. Two words to improve physician-patient communication: what else? Mayo Clin Proc 2003; 78:211–214.
- Flack JM, Sica DA, Bakris G, et al; International Society on Hypertension in Blacks. Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension 2010; 56:780–800.
- Wright JT, Agodoa LY, Appel L, et al. New recommendations for treating hypertension in black patients: evidence and/or consensus? Hypertension 2010; 56:801–803.
- National Kidney Foundation. K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease: executive summary. Am J Kid Dis 2004; 43(suppl 1):S16–S33.
- Lea J, Greene T, Hebert L, et al. The relationship between magnitude of proteinuria reduction and risk of end-stage renal disease: results of the African American study of kidney disease and hypertension. Arch Intern Med 2005; 165:947–953.
- Bakris GL, Williams M, Dworkin L, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis 2000; 36:646–661.
- Martins D, Norris K. Hypertension treatment in African Americans: physiology is less important than sociology. Cleve Clin J Med 2004; 71:735–743.
- Cooper RS, Psaty BM. Should ethnicity serve as the basis for clinical trial design? Diversity and inclusiveness should remain the guiding principles for clinical trials. Circulation 2005; 112:3660–3665.
“Healthy citizens are the greatest asset any country can have.”
—Winston Churchill
Diabetes and high blood pressure take a toll on the kidneys, especially in African Americans. To prevent chronic kidney disease (CKD) and to slow or stop its progression, the same principles apply in African Americans as in other patients—ie, vigilance for the onset of proteinuria, aggressive control of blood pressure, drug treatment to block the renin-angiotensin system, and attention to lifestyle factors (Table 1). However, we need to try to do better in the care of African Americans.
The purpose of this article is to review recent evidence- and consensus-based recommendations and to present a practical approach for the evaluation and treatment of CKD in African Americans.
CKD DEFINED
In 2002, the National Kidney Foundation1 defined CKD as either:
- Kidney damage for 3 or more months, as defined by structural or functional abnormalities of the kidney, with or without a decreased glomerular filtration rate (GFR), manifested either by pathologic abnormalities or by markers of kidney damage, including abnormalities in the composition of the blood or urine (eg, proteinuria), or abnormalities in imaging tests; or
- A GFR less than 60 mL/min/1.73 m2 for 3 or more months, with or without kidney damage.
The definition divides CKD into five progressive stages according to the GFR:
- Stage 1 (kidney damage with normal or increased GFR): GFR ≥ 90 mL/min/1.73m2
- Stage 2 (kidney damage with mildly decreased GFR): GFR 60–89
- Stage 3 (moderately decreased GFR): GFR 30–59
- Stage 4 (severely decreased GFR): GFR 15–29
- Stage 5 (kidney failure): GFR < 15 or dialysis.
Because the definition includes markers of kidney damage such as albuminuria, it allows CKD to be detected in its earliest stages, when the estimated GFR might still be well within normal limits.
CKD APPEARS EARLIER, PROGRESSES FASTER IN AFRICAN AMERICANS
“Not everything that counts can be counted, and not everything that can be counted counts.”
—Albert Einstein
CKD with or without a sustained reduction in the estimated GFR affects about one in every nine American adults.2 Its course varies depending on the cause and also from patient to patient, even in those with the same cause of CKD.
In general, the prevalence of early CKD is comparable across racial and ethnic groups in the United States, but CKD progresses to end-stage renal disease far more rapidly in minority populations, with rates nearly four times higher in black Americans than in white Americans.3 Also, the onset of CKD is earlier in African Americans.
HYPERTENSION AND DIABETES AS REASONS FOR THE DISPARITIES
Part of the reason for these differences is that minority populations have higher rates of diabetes and hypertension, and these diseases tend to be more severe in these groups. Poverty, less access to health care, exposure to environmental toxins, and genetic variation may also contribute.4–7
Compared with whites, blacks have higher rates of diabetes and hypertension and earlier onset of these diseases, poorer control, and higher rates of complications such as CKD, stroke, and heart disease.8,9 The higher rate of hypertension and the lower rate of blood pressure control in African Americans with CKD may contribute to the more rapid progression of CKD to end-stage renal disease.
In the Chronic Renal Insufficiency Cohort, 10 a racially and ethnically diverse group of 3,612 adults with a broad spectrum of renal disease severity, 93% of African Americans had hypertension at baseline compared with 80% of whites. In addition, African Americans were 18% less likely to have their blood pressure controlled to 140/90 mm Hg (the rates of control were 76% vs 60%), and 28% were less likely to have it controlled to 130/80 mm Hg (56% vs 38%).10 These factors may partially explain the faster progression to end-stage renal disease in African Americans with CKD.
Despite the potential efficacy of strict control of serum glucose levels and blood pressure,11 the high rate of poor blood pressure control has contributed to the epidemic of diabetic nephropathy, especially among African Americans. Fortunately, hypertension control in the general population, while still not ideal, has improved from 27% in 1988–1994 to 50% in 2007–2008 and is now similar across racial and ethnic groups.12 This, hopefully, is a preface for improved hypertension-related outcomes for all Americans over the next decade.
OTHER REASONS FOR THE DISPARITIES
“There are no unnatural or supernatural phenomena, only a very large gap in our knowledge of what is natural.”
—Edgar Mitchell, Apollo 14 astronaut
Proteinuria
Proteinuria is another key cardiorenal risk factor prevalent in African Americans.
Knight et al,13 analyzing data from the Third National Health and Nutrition Examination Survey, found that people with high-normal blood pressure (systolic pressure 130–139 mm Hg or diastolic pressure 85–89 mm Hg) were twice as likely to have microalbuminuria (odds ratio 2.13, 95% confidence interval [CI] 1.51–3.01) compared with people with optimal blood pressure (systolic pressure < 120 mm Hg and diastolic pressure < 80 mm Hg). Compared with whites as the reference group, Mexican Americans had slightly but not statistically significantly higher odds of microalbuminuria (odds ratio 1.16; 95% CI 0.90–1.51), and African Americans had significantly higher odds (odds ratio 1.30; 95% CI 1.04–1.64).
The incidence of hypertension-related end-stage renal disease is nearly five times higher in African Americans than in whites, and the rate of hypertension-related end-stage renal disease is 15 times higher in African American men ages 24 to 44 than in whites of the same ages.3 The greater risk of proteinuria in African Americans at any given level of higher blood pressure is thought to contribute in part to these disparate rates.
The renin-angiotensin system
The renin-angiotensin system plays a role in modulating hypertension and mediating hypertension-related complications. Hypertensive African Americans are more likely than hypertensive whites to have low-renin, salt-sensitive hypertension. Therein lies a paradox.
Since the renin-angiotensin system promotes the progression of CKD, we would expect patients with low-renin hypertension to have a lower risk of hypertension-related endorgan damage than patients with high-renin hypertension. However, many African Americans (who as a group have high rates of sodium sensitivity and low plasma renin levels) experience more severe hypertension-related end-organ complications such as proteinuria and cardiorenal disease.14
A reason for this paradox may be that the circulating renin-angiotensin system is separate from the intrarenal one. Supporting this theory is the observation that up-regulation of the intrarenal renin-angiotensin system accompanies renal interstitial inflammation and oxidative stress in the kidneys and cardiovascular tissues of salt-sensitive rats fed a high-salt diet.15 In other experiments in salt-sensitive rats, renin-angiotensin system blockade reversed endothelial dysfunction, attenuated proteinuria, and reduced renal injury independent of blood pressure changes even though the animals had low circulating renin levels.16
These findings imply that drugs that block the renin-angiotensin system, ie, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, could still be a rational therapy for CKD patients with low-renin hypertension, particularly African Americans, in whom local up-regulation of the renin-angiotensin system in the kidney could exacerbate both diabetic and hypertensive CKD.17 Although these drugs may not lower blood pressure as much in low-renin hypertension as in high-renin hypertension, they may still afford the same cardiorenal protection.
Genetic factors
Variations in the MYH9 and APOL1 genes on chromosome 22 have recently been found in genome-wide admixture mapping studies and may explain as much as 70% of the differences in the rates of nondiabetic end-stage renal disease between white and black Americans.7,18,19 In addition, genetic variations may modulate differences in blood-pressure response to antihypertensive medications across racial and ethnic groups,20 complicating treatment recommendations and clinical outcomes in our increasingly diverse nation.
Comment. The pathophysiologic basis for the variability in the course of CKD is probably multifactorial and is still poorly understood. Nevertheless, we may be able to delay the progression of CKD and prevent its complications with specific therapeutic and life-style interventions.
Race and ethnicity are associated with sociocultural and biologic variations that influence the risk and progression of CKD. Understanding these factors for minority populations can help in targeting interventions to attenuate the disproportionately high rates of CKD progression and complications.
The pathophysiologic reason African Americans have a greater prevalence of end-stage renal disease and a more rapid progression of CKD is complex and probably involves the interplay of biological, behavioral, and environmental factors such as salt intake, stress levels, and exposure to heavy metals.21
TRIALS OF ANTIHYPERTENSIVE THERAPY IN AFRICAN AMERICANS WITH CKD
“If we knew what we were doing, it wouldn’t be called research.”
—Albert Einstein
Until recently, trials of antihypertensive therapy in patients with CKD did not include adequate numbers of African American participants, but the following clinical trials have added to our knowledge (Table 2).22–26
African American Study of Kidney Disease and Hypertension (AASK)
The African American Study of Kidney Disease and Hypertension (AASK),22,23 with 1,094 patients, was the largest prospective study of CKD to date designed to focus on African Americans.
AASK examined the effects of two levels of blood-pressure control:
- Standard, with a goal blood pressure of 135–140/85–90 mm Hg (mean arterial pressure 102–107 mm Hg)
- Intensive, with a goal of 120/80 mm Hg or less (mean arterial pressure ≤ 92 mm Hg).
In a two-by two factorial design, patients were also randomized to receive one of three antihypertensive drugs as initial therapy:
- The ACE inhibitor ramipril (Altace)
- The sustained-release beta-blocker metoprolol succinate (Toprol XL)
- The calcium channel blocker amlodipine (Norvasc).
To enter the study, patients had to be African American, have at least one diastolic pressure reading of 95 mm Hg or greater during the screening period, and have a measured GFR between 20 and 65 mL/min/1.83 m2. They could not have diabetes, substantial proteinuria (> 2.5 g/day), or other causes of CKD.22
AASK was distinct from many of the larger hypertension trials in which secondary analyses of outcomes in patients with CKD were performed in that it was implicit in the design that most, if not all, study participants had substantial GFR reduction and would need diuretic therapy.
At baseline, after blood pressure medications had been tapered to define eligibility and then reintroduced before randomization, 20.0% of the patients in the intensive blood pressure goal group had pressure lower than 140/90 mm Hg, and this increased to 78.9% by 14 months after randomization. In the standard goal group, the numbers were 21.5% at baseline but only 41.8% at 14 months.23 In spite of this difference, the rate of decline in GFR (the main clinical outcome measure) was the same in both groups.
However, the class of drug did make a difference. Secondary clinical outcomes, including the composite end point of development of end-stage renal disease, doubling of serum creatinine, or death, were less frequent in the ACE inhibitor group than in the beta-blocker and calcium channel blocker groups. As anticipated and consistent with real world practice, nearly 90% of all participants received concomitant diuretic therapy to achieve target blood pressure levels.
Comments. AASK showed that blood pressure can be controlled in African Americans who have CKD and that clinical cardiorenal outcomes can be improved by using an ACE inhibitor as initial therapy rather than a beta-blocker or calcium channel blocker, with diuretics and other agents added as needed.
AASK cohort phase
After completing the trial phase, patients were invited to enroll in a cohort phase in which the blood pressure target was less than 130/80 mm Hg. The combined follow-up period was 8.8 to 12.2 years.24
During the trial phase, the mean blood pressure was 130/78 mm Hg in the intensive group and 141/86 mm Hg in the standard group. During the cohort phase, the mean blood pressures were 131/78 mm Hg and 134/78 mm Hg, respectively, in these groups.
In both phases, there was no significant difference between groups in clinical outcomes (hazard ratio in the intensive-control group 0.91, P = .27). However, the groups differed when stratified by baseline level of proteinuria (P = .02 for the interaction), with a potential benefit of a blood pressure target lower than 130/80 mm Hg in patients with a protein-to-creatinine ratio of more than 0.22 (hazard ratio 0.73, P = .01).24
Comment. Given that many African Americans with hypertension and CKD have a protein-to-creatinine ratio of more than 0.22, these findings support a practical approach in clinical practice for a target blood pressure less than 130/80 mm Hg, using a first-line combination of a renin-angiotensin system inhibitor and a diuretic.
RENAAL study
The Reduction of Endpoints in NIDDM With the Angiotensin II Antagonist Losartan (RENAAL) study25 included 1,513 patients, of whom 15% were African American and 18% were Hispanic; all had type 2 diabetes mellitus and nephropathy. They were randomized to receive the angiotensin II receptor antagonist losartan (Cozaar) or placebo in addition to other antihypertensive drugs.
At 3.4 years, the blood pressure was about 141/74 mm Hg in both groups. A post hoc analysis found lower rates of albuminuria and end-stage renal disease in the group treated with losartan,25 with no racial or ethnic differences in its renoprotective effect.
Comments. While these findings support the recommendation of inhibiting the renin-angiotensin system for improving clinical outcomes in diabetic nephropathy in racial and ethnic minorities, the AASK study also proved a second important point. These patients required intense blood pressure management for several years in a clinical trial environment, which may be difficult to do in many clinical practice models.
To be cost-effective in today’s health care environment, such care will likely be limited to larger group practices or health care plans with large comprehensive covered populations. Payers and providers need to be willing to invest in intense early care in such high-risk subgroups with the understanding that they could recognize downstream gains from long-term improved outcomes. However, even in these settings, the ability to provide effective care to high-risk subgroups without generating significant financial losses remains a concern.
ALLHAT
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)26 enrolled more than 33,000 hypertensive patients at high risk, of whom 32% were black, 16% were Hispanic, and 36% had diabetes. Their mean serum creatinine level was 1 mg/dL. Follow-up was for up to 8 years. At year 5, the mean blood pressure was 135/75 mm Hg.
In a secondary analysis, patients were stratified by GFR:
- Normal (> 90 mL/min/1.73 m2; n = 8,126)
- Mild reduction (60–89 mL/min/1.73 m2; n = 18,109)
- Moderate-severe reduction (< 60 mL/min/1.73 m2; n = 5,662).
In all three groups, amlodipine, lisinopril (Zestril), and chlorthalidone were equivalent as initial monotherapy in reducing the rate of the composite end point of end-stage renal disease or 50% or greater decrement in GFR.
Comments. The combined AASK, RENAAL, and ALLHAT findings are consistent with the practical recommendation of a diuretic, renin-angiotensin system inhibitor, or both, as initial therapy for blood pressure control in African American patients who have CKD, with a target blood pressure of less than 130/80 mm Hg.
A COMPREHENSIVE APPROACH TO CHRONIC KIDNEY DISEASE CARE
“It is much more important to know what sort of a patient has a disease, than what sort of disease a patient has.”
—William Osler
Many of the risk factors for cardiovascular disease in African Americans are behavioral and modifiable. These include too much salt and fat in the diet, too little physical activity, excessive alcohol intake, and smoking.
Education is key, to identify and communicate the risk attributable to health beliefs and behaviors, particularly in patients with known cardiovascular disease, and to encourage the patient to be proactive in risk-reduction strategies (Table 1). However, effective communication depends on compassion and concern by the health care provider to engender a sense of trust.27 Other health care professionals such as dietitians, pharmacists, and social workers as well as family members can reinforce messages and improve communication with the patient to optimize outcomes.
The International Society on Hypertension in Blacks recommends a blood pressure target of less than 130/80 mm Hg in blacks with elevated blood pressure and target-organ damage. The authors suggest monotherapy with a diuretic or calcium channel blocker if the blood pressure is 10 mm Hg or less above target levels. When blood pressure is more than 15/10 mm Hg above target, two-drug therapy is recommended, either with a calcium channel blocker plus a renin-angiotensin system blocker or, alternatively, in edematous or volume-overload states, with a thiazide diuretic plus a renin-angiotensin system blocker.28,29
The Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease of the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative recommend starting anti-hypertensive therapy with an ACE inhibitor or an angiotensin receptor blocker for most patients with CKD, regardless of ethnicity, recognizing that many will require combination therapy.30 Evaluation of the response to therapy should include not only checking that the blood pressure is at or below the recommended target of 130/80 mm Hg, but also assessing for complications and monitoring the change in the level of proteinuria, which is a powerful predictor of progression of hypertensive kidney disease in all patients at any given GFR.31
OUR RECOMMENDATIONS
African Americans with hypertension and kidney disease require an aggressive and comprehensive approach to slow the progression of kidney disease and its complications, often necessitating aggressive care of the primary cause and the use of two or more antihypertensive agents to control blood pressure, proteinuria, or both (Figure 1).32
We recommend that the initial evaluation of patients with hypertension include a screening for albuminuria and that the initial therapy for hypertension or proteinuria in all patients with CKD include renin-angiotensin system inhibition with a diuretic, because this combination appears most effective to achieve blood pressure control and to confer additional cardiorenal protection beyond that offered by blood-pressure control alone. Although some studies have reported that African Americans have lower blood-pressure response rates than whites to renin-angiotensin system inhibition, 18 it is nevertheless beneficial for clinical outcomes in this group, especially in the presence of proteinuria, a hallmark of hypertension-related CKD in African Americans. Thus, until more data are available, ethnicity should not be the primary criterion for selecting a given class of antihypertensive therapy, especially in patients with hypertensive nephropathy.
The overall treatment decision should be guided by individual response, coexisting risk factors, and potential cultural and socioeconomic considerations such as cost of medications and insurance coverage, which affect adherence to both pharmacologic and nonpharmacologic interventions.33
Future studies should strive for adequate representation of racial and ethnic minority populations in order to enhance the evidence base for CKD treatment as we move toward using personalized medicine approaches in an increasingly diverse society.34
Acknowledgment: Support for this paper was provided in part by NIH grants RR026138 and MD000182.
“Healthy citizens are the greatest asset any country can have.”
—Winston Churchill
Diabetes and high blood pressure take a toll on the kidneys, especially in African Americans. To prevent chronic kidney disease (CKD) and to slow or stop its progression, the same principles apply in African Americans as in other patients—ie, vigilance for the onset of proteinuria, aggressive control of blood pressure, drug treatment to block the renin-angiotensin system, and attention to lifestyle factors (Table 1). However, we need to try to do better in the care of African Americans.
The purpose of this article is to review recent evidence- and consensus-based recommendations and to present a practical approach for the evaluation and treatment of CKD in African Americans.
CKD DEFINED
In 2002, the National Kidney Foundation1 defined CKD as either:
- Kidney damage for 3 or more months, as defined by structural or functional abnormalities of the kidney, with or without a decreased glomerular filtration rate (GFR), manifested either by pathologic abnormalities or by markers of kidney damage, including abnormalities in the composition of the blood or urine (eg, proteinuria), or abnormalities in imaging tests; or
- A GFR less than 60 mL/min/1.73 m2 for 3 or more months, with or without kidney damage.
The definition divides CKD into five progressive stages according to the GFR:
- Stage 1 (kidney damage with normal or increased GFR): GFR ≥ 90 mL/min/1.73m2
- Stage 2 (kidney damage with mildly decreased GFR): GFR 60–89
- Stage 3 (moderately decreased GFR): GFR 30–59
- Stage 4 (severely decreased GFR): GFR 15–29
- Stage 5 (kidney failure): GFR < 15 or dialysis.
Because the definition includes markers of kidney damage such as albuminuria, it allows CKD to be detected in its earliest stages, when the estimated GFR might still be well within normal limits.
CKD APPEARS EARLIER, PROGRESSES FASTER IN AFRICAN AMERICANS
“Not everything that counts can be counted, and not everything that can be counted counts.”
—Albert Einstein
CKD with or without a sustained reduction in the estimated GFR affects about one in every nine American adults.2 Its course varies depending on the cause and also from patient to patient, even in those with the same cause of CKD.
In general, the prevalence of early CKD is comparable across racial and ethnic groups in the United States, but CKD progresses to end-stage renal disease far more rapidly in minority populations, with rates nearly four times higher in black Americans than in white Americans.3 Also, the onset of CKD is earlier in African Americans.
HYPERTENSION AND DIABETES AS REASONS FOR THE DISPARITIES
Part of the reason for these differences is that minority populations have higher rates of diabetes and hypertension, and these diseases tend to be more severe in these groups. Poverty, less access to health care, exposure to environmental toxins, and genetic variation may also contribute.4–7
Compared with whites, blacks have higher rates of diabetes and hypertension and earlier onset of these diseases, poorer control, and higher rates of complications such as CKD, stroke, and heart disease.8,9 The higher rate of hypertension and the lower rate of blood pressure control in African Americans with CKD may contribute to the more rapid progression of CKD to end-stage renal disease.
In the Chronic Renal Insufficiency Cohort, 10 a racially and ethnically diverse group of 3,612 adults with a broad spectrum of renal disease severity, 93% of African Americans had hypertension at baseline compared with 80% of whites. In addition, African Americans were 18% less likely to have their blood pressure controlled to 140/90 mm Hg (the rates of control were 76% vs 60%), and 28% were less likely to have it controlled to 130/80 mm Hg (56% vs 38%).10 These factors may partially explain the faster progression to end-stage renal disease in African Americans with CKD.
Despite the potential efficacy of strict control of serum glucose levels and blood pressure,11 the high rate of poor blood pressure control has contributed to the epidemic of diabetic nephropathy, especially among African Americans. Fortunately, hypertension control in the general population, while still not ideal, has improved from 27% in 1988–1994 to 50% in 2007–2008 and is now similar across racial and ethnic groups.12 This, hopefully, is a preface for improved hypertension-related outcomes for all Americans over the next decade.
OTHER REASONS FOR THE DISPARITIES
“There are no unnatural or supernatural phenomena, only a very large gap in our knowledge of what is natural.”
—Edgar Mitchell, Apollo 14 astronaut
Proteinuria
Proteinuria is another key cardiorenal risk factor prevalent in African Americans.
Knight et al,13 analyzing data from the Third National Health and Nutrition Examination Survey, found that people with high-normal blood pressure (systolic pressure 130–139 mm Hg or diastolic pressure 85–89 mm Hg) were twice as likely to have microalbuminuria (odds ratio 2.13, 95% confidence interval [CI] 1.51–3.01) compared with people with optimal blood pressure (systolic pressure < 120 mm Hg and diastolic pressure < 80 mm Hg). Compared with whites as the reference group, Mexican Americans had slightly but not statistically significantly higher odds of microalbuminuria (odds ratio 1.16; 95% CI 0.90–1.51), and African Americans had significantly higher odds (odds ratio 1.30; 95% CI 1.04–1.64).
The incidence of hypertension-related end-stage renal disease is nearly five times higher in African Americans than in whites, and the rate of hypertension-related end-stage renal disease is 15 times higher in African American men ages 24 to 44 than in whites of the same ages.3 The greater risk of proteinuria in African Americans at any given level of higher blood pressure is thought to contribute in part to these disparate rates.
The renin-angiotensin system
The renin-angiotensin system plays a role in modulating hypertension and mediating hypertension-related complications. Hypertensive African Americans are more likely than hypertensive whites to have low-renin, salt-sensitive hypertension. Therein lies a paradox.
Since the renin-angiotensin system promotes the progression of CKD, we would expect patients with low-renin hypertension to have a lower risk of hypertension-related endorgan damage than patients with high-renin hypertension. However, many African Americans (who as a group have high rates of sodium sensitivity and low plasma renin levels) experience more severe hypertension-related end-organ complications such as proteinuria and cardiorenal disease.14
A reason for this paradox may be that the circulating renin-angiotensin system is separate from the intrarenal one. Supporting this theory is the observation that up-regulation of the intrarenal renin-angiotensin system accompanies renal interstitial inflammation and oxidative stress in the kidneys and cardiovascular tissues of salt-sensitive rats fed a high-salt diet.15 In other experiments in salt-sensitive rats, renin-angiotensin system blockade reversed endothelial dysfunction, attenuated proteinuria, and reduced renal injury independent of blood pressure changes even though the animals had low circulating renin levels.16
These findings imply that drugs that block the renin-angiotensin system, ie, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, could still be a rational therapy for CKD patients with low-renin hypertension, particularly African Americans, in whom local up-regulation of the renin-angiotensin system in the kidney could exacerbate both diabetic and hypertensive CKD.17 Although these drugs may not lower blood pressure as much in low-renin hypertension as in high-renin hypertension, they may still afford the same cardiorenal protection.
Genetic factors
Variations in the MYH9 and APOL1 genes on chromosome 22 have recently been found in genome-wide admixture mapping studies and may explain as much as 70% of the differences in the rates of nondiabetic end-stage renal disease between white and black Americans.7,18,19 In addition, genetic variations may modulate differences in blood-pressure response to antihypertensive medications across racial and ethnic groups,20 complicating treatment recommendations and clinical outcomes in our increasingly diverse nation.
Comment. The pathophysiologic basis for the variability in the course of CKD is probably multifactorial and is still poorly understood. Nevertheless, we may be able to delay the progression of CKD and prevent its complications with specific therapeutic and life-style interventions.
Race and ethnicity are associated with sociocultural and biologic variations that influence the risk and progression of CKD. Understanding these factors for minority populations can help in targeting interventions to attenuate the disproportionately high rates of CKD progression and complications.
The pathophysiologic reason African Americans have a greater prevalence of end-stage renal disease and a more rapid progression of CKD is complex and probably involves the interplay of biological, behavioral, and environmental factors such as salt intake, stress levels, and exposure to heavy metals.21
TRIALS OF ANTIHYPERTENSIVE THERAPY IN AFRICAN AMERICANS WITH CKD
“If we knew what we were doing, it wouldn’t be called research.”
—Albert Einstein
Until recently, trials of antihypertensive therapy in patients with CKD did not include adequate numbers of African American participants, but the following clinical trials have added to our knowledge (Table 2).22–26
African American Study of Kidney Disease and Hypertension (AASK)
The African American Study of Kidney Disease and Hypertension (AASK),22,23 with 1,094 patients, was the largest prospective study of CKD to date designed to focus on African Americans.
AASK examined the effects of two levels of blood-pressure control:
- Standard, with a goal blood pressure of 135–140/85–90 mm Hg (mean arterial pressure 102–107 mm Hg)
- Intensive, with a goal of 120/80 mm Hg or less (mean arterial pressure ≤ 92 mm Hg).
In a two-by two factorial design, patients were also randomized to receive one of three antihypertensive drugs as initial therapy:
- The ACE inhibitor ramipril (Altace)
- The sustained-release beta-blocker metoprolol succinate (Toprol XL)
- The calcium channel blocker amlodipine (Norvasc).
To enter the study, patients had to be African American, have at least one diastolic pressure reading of 95 mm Hg or greater during the screening period, and have a measured GFR between 20 and 65 mL/min/1.83 m2. They could not have diabetes, substantial proteinuria (> 2.5 g/day), or other causes of CKD.22
AASK was distinct from many of the larger hypertension trials in which secondary analyses of outcomes in patients with CKD were performed in that it was implicit in the design that most, if not all, study participants had substantial GFR reduction and would need diuretic therapy.
At baseline, after blood pressure medications had been tapered to define eligibility and then reintroduced before randomization, 20.0% of the patients in the intensive blood pressure goal group had pressure lower than 140/90 mm Hg, and this increased to 78.9% by 14 months after randomization. In the standard goal group, the numbers were 21.5% at baseline but only 41.8% at 14 months.23 In spite of this difference, the rate of decline in GFR (the main clinical outcome measure) was the same in both groups.
However, the class of drug did make a difference. Secondary clinical outcomes, including the composite end point of development of end-stage renal disease, doubling of serum creatinine, or death, were less frequent in the ACE inhibitor group than in the beta-blocker and calcium channel blocker groups. As anticipated and consistent with real world practice, nearly 90% of all participants received concomitant diuretic therapy to achieve target blood pressure levels.
Comments. AASK showed that blood pressure can be controlled in African Americans who have CKD and that clinical cardiorenal outcomes can be improved by using an ACE inhibitor as initial therapy rather than a beta-blocker or calcium channel blocker, with diuretics and other agents added as needed.
AASK cohort phase
After completing the trial phase, patients were invited to enroll in a cohort phase in which the blood pressure target was less than 130/80 mm Hg. The combined follow-up period was 8.8 to 12.2 years.24
During the trial phase, the mean blood pressure was 130/78 mm Hg in the intensive group and 141/86 mm Hg in the standard group. During the cohort phase, the mean blood pressures were 131/78 mm Hg and 134/78 mm Hg, respectively, in these groups.
In both phases, there was no significant difference between groups in clinical outcomes (hazard ratio in the intensive-control group 0.91, P = .27). However, the groups differed when stratified by baseline level of proteinuria (P = .02 for the interaction), with a potential benefit of a blood pressure target lower than 130/80 mm Hg in patients with a protein-to-creatinine ratio of more than 0.22 (hazard ratio 0.73, P = .01).24
Comment. Given that many African Americans with hypertension and CKD have a protein-to-creatinine ratio of more than 0.22, these findings support a practical approach in clinical practice for a target blood pressure less than 130/80 mm Hg, using a first-line combination of a renin-angiotensin system inhibitor and a diuretic.
RENAAL study
The Reduction of Endpoints in NIDDM With the Angiotensin II Antagonist Losartan (RENAAL) study25 included 1,513 patients, of whom 15% were African American and 18% were Hispanic; all had type 2 diabetes mellitus and nephropathy. They were randomized to receive the angiotensin II receptor antagonist losartan (Cozaar) or placebo in addition to other antihypertensive drugs.
At 3.4 years, the blood pressure was about 141/74 mm Hg in both groups. A post hoc analysis found lower rates of albuminuria and end-stage renal disease in the group treated with losartan,25 with no racial or ethnic differences in its renoprotective effect.
Comments. While these findings support the recommendation of inhibiting the renin-angiotensin system for improving clinical outcomes in diabetic nephropathy in racial and ethnic minorities, the AASK study also proved a second important point. These patients required intense blood pressure management for several years in a clinical trial environment, which may be difficult to do in many clinical practice models.
To be cost-effective in today’s health care environment, such care will likely be limited to larger group practices or health care plans with large comprehensive covered populations. Payers and providers need to be willing to invest in intense early care in such high-risk subgroups with the understanding that they could recognize downstream gains from long-term improved outcomes. However, even in these settings, the ability to provide effective care to high-risk subgroups without generating significant financial losses remains a concern.
ALLHAT
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)26 enrolled more than 33,000 hypertensive patients at high risk, of whom 32% were black, 16% were Hispanic, and 36% had diabetes. Their mean serum creatinine level was 1 mg/dL. Follow-up was for up to 8 years. At year 5, the mean blood pressure was 135/75 mm Hg.
In a secondary analysis, patients were stratified by GFR:
- Normal (> 90 mL/min/1.73 m2; n = 8,126)
- Mild reduction (60–89 mL/min/1.73 m2; n = 18,109)
- Moderate-severe reduction (< 60 mL/min/1.73 m2; n = 5,662).
In all three groups, amlodipine, lisinopril (Zestril), and chlorthalidone were equivalent as initial monotherapy in reducing the rate of the composite end point of end-stage renal disease or 50% or greater decrement in GFR.
Comments. The combined AASK, RENAAL, and ALLHAT findings are consistent with the practical recommendation of a diuretic, renin-angiotensin system inhibitor, or both, as initial therapy for blood pressure control in African American patients who have CKD, with a target blood pressure of less than 130/80 mm Hg.
A COMPREHENSIVE APPROACH TO CHRONIC KIDNEY DISEASE CARE
“It is much more important to know what sort of a patient has a disease, than what sort of disease a patient has.”
—William Osler
Many of the risk factors for cardiovascular disease in African Americans are behavioral and modifiable. These include too much salt and fat in the diet, too little physical activity, excessive alcohol intake, and smoking.
Education is key, to identify and communicate the risk attributable to health beliefs and behaviors, particularly in patients with known cardiovascular disease, and to encourage the patient to be proactive in risk-reduction strategies (Table 1). However, effective communication depends on compassion and concern by the health care provider to engender a sense of trust.27 Other health care professionals such as dietitians, pharmacists, and social workers as well as family members can reinforce messages and improve communication with the patient to optimize outcomes.
The International Society on Hypertension in Blacks recommends a blood pressure target of less than 130/80 mm Hg in blacks with elevated blood pressure and target-organ damage. The authors suggest monotherapy with a diuretic or calcium channel blocker if the blood pressure is 10 mm Hg or less above target levels. When blood pressure is more than 15/10 mm Hg above target, two-drug therapy is recommended, either with a calcium channel blocker plus a renin-angiotensin system blocker or, alternatively, in edematous or volume-overload states, with a thiazide diuretic plus a renin-angiotensin system blocker.28,29
The Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease of the National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative recommend starting anti-hypertensive therapy with an ACE inhibitor or an angiotensin receptor blocker for most patients with CKD, regardless of ethnicity, recognizing that many will require combination therapy.30 Evaluation of the response to therapy should include not only checking that the blood pressure is at or below the recommended target of 130/80 mm Hg, but also assessing for complications and monitoring the change in the level of proteinuria, which is a powerful predictor of progression of hypertensive kidney disease in all patients at any given GFR.31
OUR RECOMMENDATIONS
African Americans with hypertension and kidney disease require an aggressive and comprehensive approach to slow the progression of kidney disease and its complications, often necessitating aggressive care of the primary cause and the use of two or more antihypertensive agents to control blood pressure, proteinuria, or both (Figure 1).32
We recommend that the initial evaluation of patients with hypertension include a screening for albuminuria and that the initial therapy for hypertension or proteinuria in all patients with CKD include renin-angiotensin system inhibition with a diuretic, because this combination appears most effective to achieve blood pressure control and to confer additional cardiorenal protection beyond that offered by blood-pressure control alone. Although some studies have reported that African Americans have lower blood-pressure response rates than whites to renin-angiotensin system inhibition, 18 it is nevertheless beneficial for clinical outcomes in this group, especially in the presence of proteinuria, a hallmark of hypertension-related CKD in African Americans. Thus, until more data are available, ethnicity should not be the primary criterion for selecting a given class of antihypertensive therapy, especially in patients with hypertensive nephropathy.
The overall treatment decision should be guided by individual response, coexisting risk factors, and potential cultural and socioeconomic considerations such as cost of medications and insurance coverage, which affect adherence to both pharmacologic and nonpharmacologic interventions.33
Future studies should strive for adequate representation of racial and ethnic minority populations in order to enhance the evidence base for CKD treatment as we move toward using personalized medicine approaches in an increasingly diverse society.34
Acknowledgment: Support for this paper was provided in part by NIH grants RR026138 and MD000182.
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39(suppl 1):S1–S266.
- Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA 2007; 298:2038–2047.
- US Renal Data System. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2010.
- Norris K, Nissenson AR. Race, gender, and socioeconomic disparities in CKD in the United States. J Am Soc Nephrol 2008; 19:1261–1270.
- Norris KC, Agodoa LY. Unraveling the racial disparities associated with kidney disease. Kidney Int 2005; 68:914–924.
- Powe NR. To have and have not: health and health care disparities in chronic kidney disease. Kidney Int 2003; 64:763–772.
- Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 2010; 329:841–845.
- Rosamond W, Flegal K, Furie K, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008; 117:e25–e146.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Muntner P, Anderson A, Charleston J, et al; Chronic Renal Insufficiency Cohort (CRIC) Study Investigators. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 2010; 55:441–451.
- Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317:703–713.
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303:2043–2050.
- Knight EL, Kramer HM, Curhan GC. High-normal blood pressure and microalbuminuria. Am J Kidney Dis 2003; 41:588–595.
- Luft FC, Grim CE, Fineberg N, Weinberger MC. Effects of volume expansion and contraction in normotensive whites, blacks, and subjects of different ages. Circulation 1979; 59:643–650.
- Chandramohan G, Bai Y, Norris K, Rodriguez-Iturbe B, Vaziri ND. Effects of dietary salt on intrarenal angiotensin system, NAD(P)H oxidase, COX-2, MCP-1 and PAI-1 expressions and NF-kappaB activity in salt-sensitive and -resistant rat kidneys. Am J Nephrol 2008; 28:158–167.
- Hayakawa H, Coffee K, Raij L. Endothelial dysfunction and cardiorenal injury in experimental salt-sensitive hypertension: effects of antihypertensive therapy. Circulation 1997; 96:2407–2413.
- Norris KC, Tareen N, Martins D, Vaziri ND. Implications of ethnicity for the treatment of hypertensive kidney disease, with an emphasis on African Americans. Nat Clin Pract Nephrol 2008; 4:538–549.
- Kao WH, Klag MJ, Meoni LA, et al; Family Investigation of Nephropathy and Diabetes Research Group. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet 2008; 40:1185–1192.
- Freedman BI, Kopp JB, Langefeld CD, et al. The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. J Am Soc Nephrol 2010; 21:1422–1426.
- Materson BJ, Reda DJ, Cushman WC, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med 1993; 328:914–921. Erratum in N Engl J Med 1994; 330:1689.
- Norris KC, Francis CK. Gender and ethnic differences and considerations in cardiovascular risk assessment and prevention in African Americans. In:Wong N, Gardin JM, Black HR, editors. Practical Strategies in Preventing Heart Disease. New York, NY: McGraw-Hill; 2004:415–440.
- Wright JT, Bakris G, Greene T, et al; African American Study of Kidney Disease and Hypertension Study Group. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002; 288:2421–2431. Erratum in JAMA 2006; 295:2726.
- Wright JT, Agodoa L, Contreras G, et al; African American Study of Kidney Disease and Hypertension Study Group. Successful blood pressure control in the African American Study of Kidney Disease and Hypertension. Arch Intern Med 2002; 162:1636–1643.
- Appel LJ, Wright JT, Greene T, et al; AASK Collaborative Research Group. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med 2010; 363:918–929.
- de Zeeuw D, Ramjit D, Zhang Z, et al. Renal risk and renoprotection among ethnic groups with type 2 diabetic nephropathy: a post hoc analysis of RENAAL. Kidney Int 2006; 69:1675–1682.
- Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005; 165:936–946.
- Barrier PA, Li JT, Jensen NM. Two words to improve physician-patient communication: what else? Mayo Clin Proc 2003; 78:211–214.
- Flack JM, Sica DA, Bakris G, et al; International Society on Hypertension in Blacks. Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension 2010; 56:780–800.
- Wright JT, Agodoa LY, Appel L, et al. New recommendations for treating hypertension in black patients: evidence and/or consensus? Hypertension 2010; 56:801–803.
- National Kidney Foundation. K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease: executive summary. Am J Kid Dis 2004; 43(suppl 1):S16–S33.
- Lea J, Greene T, Hebert L, et al. The relationship between magnitude of proteinuria reduction and risk of end-stage renal disease: results of the African American study of kidney disease and hypertension. Arch Intern Med 2005; 165:947–953.
- Bakris GL, Williams M, Dworkin L, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis 2000; 36:646–661.
- Martins D, Norris K. Hypertension treatment in African Americans: physiology is less important than sociology. Cleve Clin J Med 2004; 71:735–743.
- Cooper RS, Psaty BM. Should ethnicity serve as the basis for clinical trial design? Diversity and inclusiveness should remain the guiding principles for clinical trials. Circulation 2005; 112:3660–3665.
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39(suppl 1):S1–S266.
- Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA 2007; 298:2038–2047.
- US Renal Data System. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2010.
- Norris K, Nissenson AR. Race, gender, and socioeconomic disparities in CKD in the United States. J Am Soc Nephrol 2008; 19:1261–1270.
- Norris KC, Agodoa LY. Unraveling the racial disparities associated with kidney disease. Kidney Int 2005; 68:914–924.
- Powe NR. To have and have not: health and health care disparities in chronic kidney disease. Kidney Int 2003; 64:763–772.
- Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 2010; 329:841–845.
- Rosamond W, Flegal K, Furie K, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008; 117:e25–e146.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Muntner P, Anderson A, Charleston J, et al; Chronic Renal Insufficiency Cohort (CRIC) Study Investigators. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 2010; 55:441–451.
- Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317:703–713.
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303:2043–2050.
- Knight EL, Kramer HM, Curhan GC. High-normal blood pressure and microalbuminuria. Am J Kidney Dis 2003; 41:588–595.
- Luft FC, Grim CE, Fineberg N, Weinberger MC. Effects of volume expansion and contraction in normotensive whites, blacks, and subjects of different ages. Circulation 1979; 59:643–650.
- Chandramohan G, Bai Y, Norris K, Rodriguez-Iturbe B, Vaziri ND. Effects of dietary salt on intrarenal angiotensin system, NAD(P)H oxidase, COX-2, MCP-1 and PAI-1 expressions and NF-kappaB activity in salt-sensitive and -resistant rat kidneys. Am J Nephrol 2008; 28:158–167.
- Hayakawa H, Coffee K, Raij L. Endothelial dysfunction and cardiorenal injury in experimental salt-sensitive hypertension: effects of antihypertensive therapy. Circulation 1997; 96:2407–2413.
- Norris KC, Tareen N, Martins D, Vaziri ND. Implications of ethnicity for the treatment of hypertensive kidney disease, with an emphasis on African Americans. Nat Clin Pract Nephrol 2008; 4:538–549.
- Kao WH, Klag MJ, Meoni LA, et al; Family Investigation of Nephropathy and Diabetes Research Group. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet 2008; 40:1185–1192.
- Freedman BI, Kopp JB, Langefeld CD, et al. The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. J Am Soc Nephrol 2010; 21:1422–1426.
- Materson BJ, Reda DJ, Cushman WC, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med 1993; 328:914–921. Erratum in N Engl J Med 1994; 330:1689.
- Norris KC, Francis CK. Gender and ethnic differences and considerations in cardiovascular risk assessment and prevention in African Americans. In:Wong N, Gardin JM, Black HR, editors. Practical Strategies in Preventing Heart Disease. New York, NY: McGraw-Hill; 2004:415–440.
- Wright JT, Bakris G, Greene T, et al; African American Study of Kidney Disease and Hypertension Study Group. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002; 288:2421–2431. Erratum in JAMA 2006; 295:2726.
- Wright JT, Agodoa L, Contreras G, et al; African American Study of Kidney Disease and Hypertension Study Group. Successful blood pressure control in the African American Study of Kidney Disease and Hypertension. Arch Intern Med 2002; 162:1636–1643.
- Appel LJ, Wright JT, Greene T, et al; AASK Collaborative Research Group. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med 2010; 363:918–929.
- de Zeeuw D, Ramjit D, Zhang Z, et al. Renal risk and renoprotection among ethnic groups with type 2 diabetic nephropathy: a post hoc analysis of RENAAL. Kidney Int 2006; 69:1675–1682.
- Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005; 165:936–946.
- Barrier PA, Li JT, Jensen NM. Two words to improve physician-patient communication: what else? Mayo Clin Proc 2003; 78:211–214.
- Flack JM, Sica DA, Bakris G, et al; International Society on Hypertension in Blacks. Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension 2010; 56:780–800.
- Wright JT, Agodoa LY, Appel L, et al. New recommendations for treating hypertension in black patients: evidence and/or consensus? Hypertension 2010; 56:801–803.
- National Kidney Foundation. K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease: executive summary. Am J Kid Dis 2004; 43(suppl 1):S16–S33.
- Lea J, Greene T, Hebert L, et al. The relationship between magnitude of proteinuria reduction and risk of end-stage renal disease: results of the African American study of kidney disease and hypertension. Arch Intern Med 2005; 165:947–953.
- Bakris GL, Williams M, Dworkin L, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis 2000; 36:646–661.
- Martins D, Norris K. Hypertension treatment in African Americans: physiology is less important than sociology. Cleve Clin J Med 2004; 71:735–743.
- Cooper RS, Psaty BM. Should ethnicity serve as the basis for clinical trial design? Diversity and inclusiveness should remain the guiding principles for clinical trials. Circulation 2005; 112:3660–3665.
KEY POINTS
- To provide optimal care for African Americans, we need to be sensitive to factors that may pose barriers to care, such as poverty, unemployment, lack of insurance, low education level, lack of family support, inaccurate health beliefs, and unhealthy behaviors.
- If we detect CKD earlier, we can better implement strategies to prevent its progression, refer the patient to specialists, and possibly arrange for preemptive kidney transplantation if needed.
- Progression of CKD can be prevented or slowed by controlling blood pressure, proteinuria, and blood glucose. However, CKD progresses in a subset of patients despite evidence-based therapy to target goals.
- African Americans with hypertensive CKD and proteinuria should receive a diuretic, a renin-angiotensin system inhibitor, or both as initial therapy, with a target blood pressure of less than 130/80 mm Hg.