User login
23-year-old woman • fever, fatigue, and sore throat • scleral icterus and hepatosplenomegaly • Dx?
THE CASE
A 23-year-old woman sought care from her primary care physician (PCP) after being sick for 7 days. The illness started with a headache and fatigue, and by Day 6, she also had fever, chills, sore throat, nausea, a poor appetite, and intractable vomiting. The patient had no significant medical history and was socially isolating due to the COVID-19 pandemic. She had no known sick contacts or recent sexual activity and did not use any illicit drugs.
On examination, her vital signs were normal although she appeared ill and diaphoretic. A shallow tonsil ulcer and tonsillar adenopathy were present. Laboratory tests included a complete blood count (CBC), comprehensive metabolic panel, Monospot test, and Epstein-Barr virus (EBV) antibody test. Results were notable for leukocytosis with atypical lymphocytes on her CBC. Her Monospot test and EBV immunoglobulin (Ig) M antibody were positive, and her EBV IgG antibody was negative. She was given a diagnosis of infectious mononucleosis (IM) and told to get adequate rest, drink a lot of fluids, and take ibuprofen or acetaminophen for pain control.
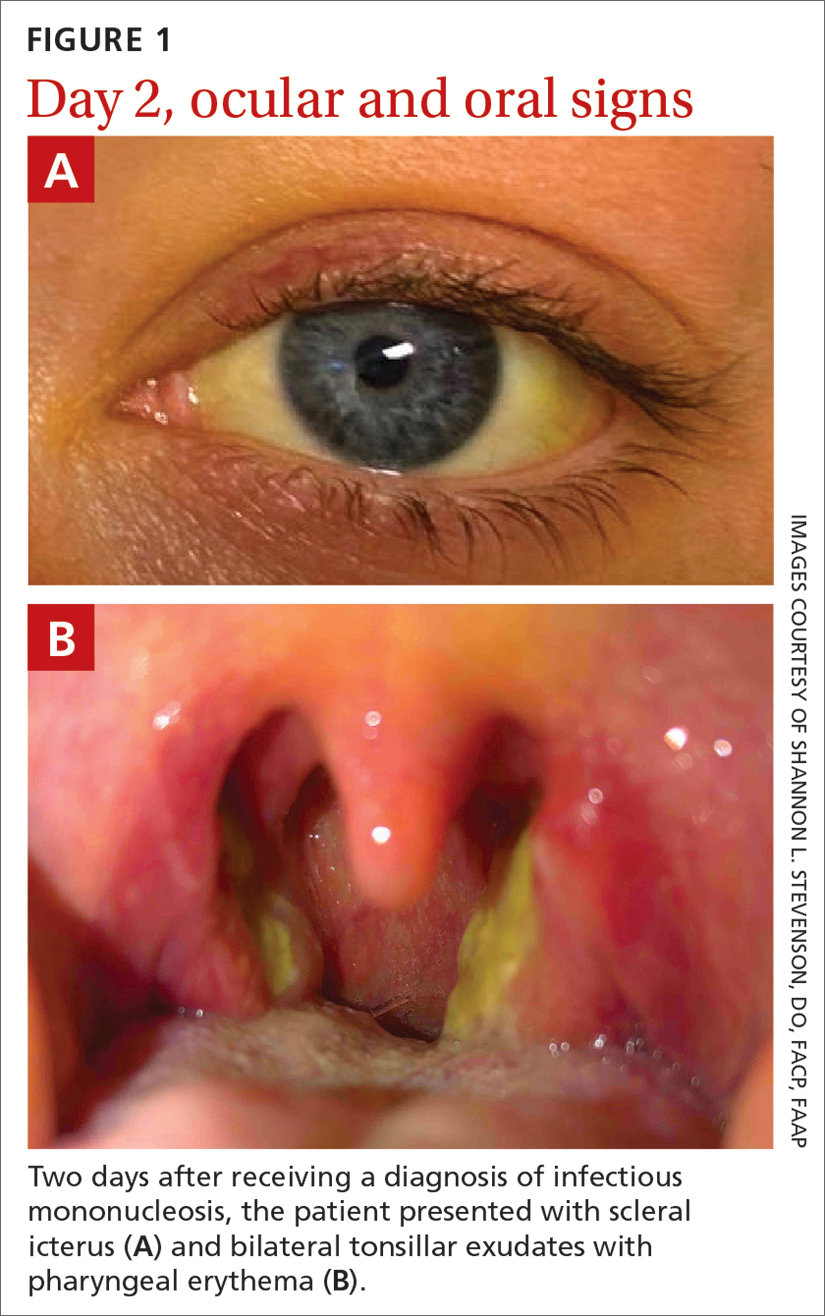
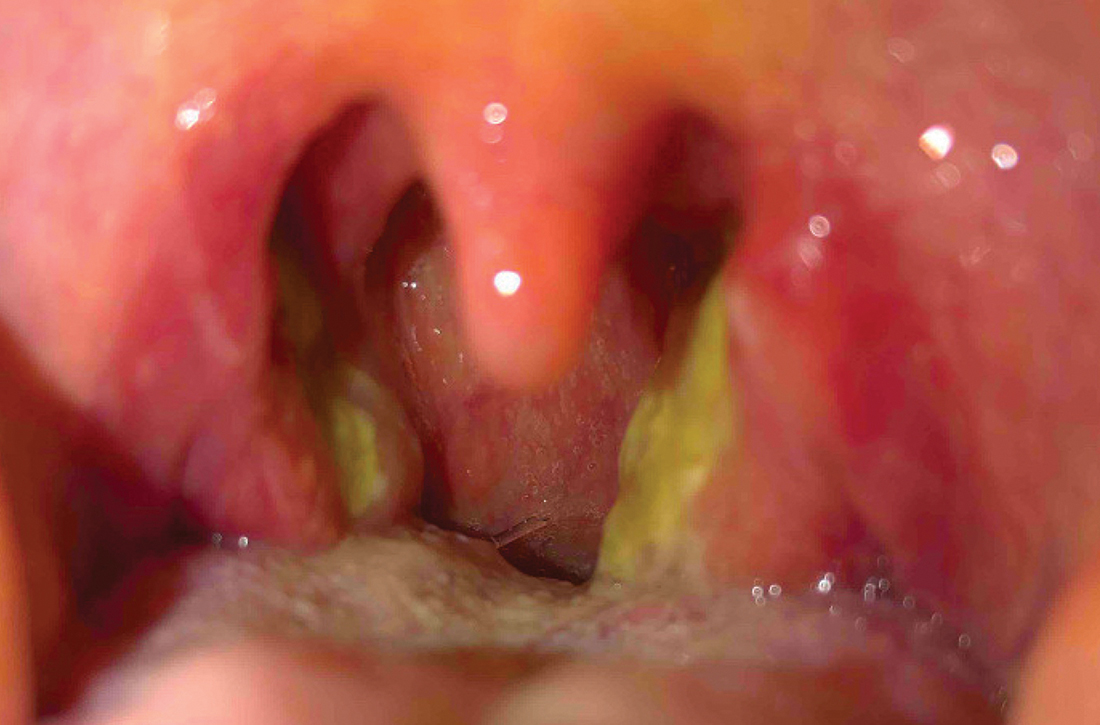
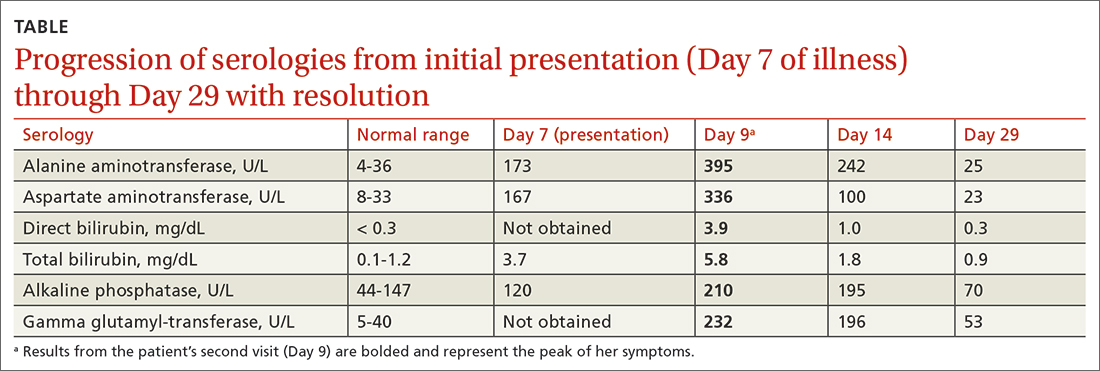
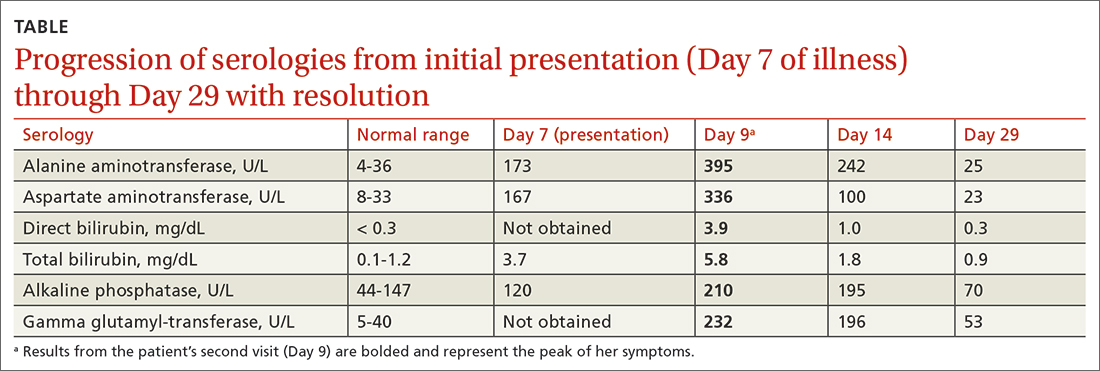
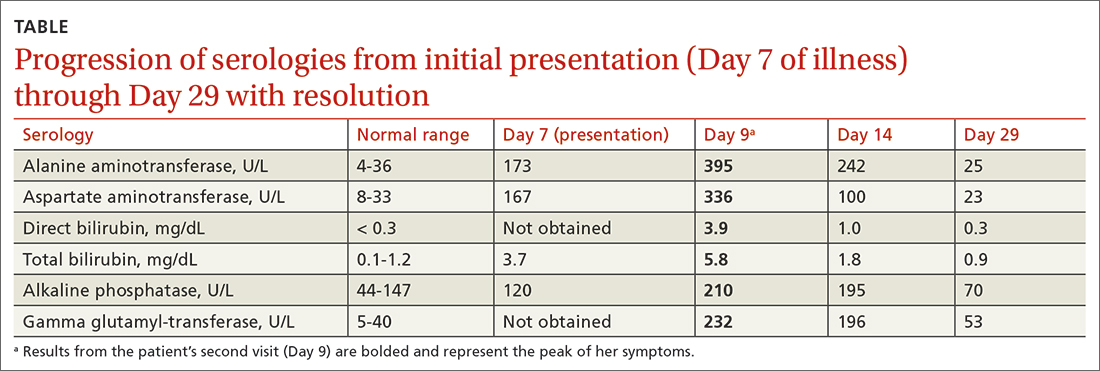
Two days later, she returned to her PCP with scleral icterus (FIGURE 1A), increasingly tender cervical lymphadenopathy, and left-side abdominal pain. Her liver function tests (LFTs) had worsened (TABLE). An abdominal ultrasound revealed mild diffuse decreased hepatic echogenicity and prominent periportal echogenicity, likely related to diffuse hepatic parenchymal disease, as well as splenomegaly and a mildly thickened gallbladder with no gallstones. She also had severe throat discomfort, with bilateral tonsillar exudates and pharyngeal erythema (FIGURE 1B).
THE DIAGNOSIS
Based on her symptoms and the results of her physical examination, LFTs, EBV serologic assays, and abdominal ultrasound, this patient was given a diagnosis of acute EBV hepatitis.
DISCUSSION
EBV infection, which is the most common cause of IM, causes asymptomatic liver enzyme abnormalities in 80% to 90% of patients.1-3 Although not common, patients can develop acute EBV hepatitis and require hospitalization.4
Be aware of potential complications. Prompt assessment of elevated liver enzymes and accurate diagnosis are key.5 Although acute EBV hepatitis is usually self-limiting, there can be serious gastrointestinal complications such as splenic rupture, liver failure due to acute and/or chronic EBV infection, autoimmune hepatitis, and hepatocellular carcinoma.2 It’s rare for EBV hepatitis to lead to acute liver failure,but when that occurs, it can be fatal.6-9 One case series revealed that while primary EBV infection accounts for less than 1% of adult acute liver failure cases, it has a high case fatality rate of 50%.9
Treatment for patients with EBV hepatitis is usually supportive and includes rest, analgesia, and avoidance of vigorous activity for 1 month to reduce the risk for splenic rupture.1 In patients with nausea and vomiting, intravenous fluids may be necessary and can be administered at an outpatient infusion center. For individuals with severe tonsillar hypertrophy, prednisone (40-60 mg/d for 2-3 days, with subsequent tapering over 1-2 weeks) is indicated to prevent airway obstruction.1 Acyclovir may be used to reduce EBV viral shedding; however, it has no significant clinical impact.1
Continue to: Patients who are hemodynamially stable...
Patients who are hemodynamically stable and have appropriate access to follow-up care can be managed at home.2 If follow-up cannot occur remotely within 1 week or the patient’s clinical status begins to worsen (ie, the patient’s liver enzymes or bilirubin levels dramatically increase), hospitalization is necessary.10
Through shared decision-making, our patient was treated as an outpatient based on her hemodynamic stability and her ability to closely follow up in the clinic and by phone and to access an outpatient infusion center. She was reexamined within 2 days and given ondansetron 8 mg IV with 2 L of normal saline at our outpatient infusion center. We also prescribed ibuprofen (400 mg every 6 hours as needed) for analgesia and issued the standard recommendations that she avoid contact sports (for at least 6 weeks) and excessive alcohol consumption.
On Day 11, the patient followed up with her PCP by telephone. The patient was started on oral prednisone (40 mg/d for 3 days with taper over the next week as symptoms improved) for her severe throat discomfort, exudates, difficulty swallowing, and muffled voice. By Day 14, her aminotransferase levels began to decrease (TABLE), and her symptoms steadily improved thereafter.
THE TAKEAWAY
When a patient presents with unexplained elevated liver enzymes or cholestasis, it is important to assess for signs and symptoms of EBV hepatitis. Although EBV hepatitis is typically self-limiting, it can have serious complications or be fatal. Prompt initiation of outpatient management may avoid these complications and hospitalization.
CORRESPONDENCE
Lydia J. Schneider, MD, 225 East Chicago Avenue, Chicago, IL 60611; lydia.schneider315@gmail.com
1. Cohen JI. Chapter 189: Epstein-Barr virus infections, including infectious mononucleosis. In: Jameson JL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. McGraw Hill; 2020. Accessed March 21, 2023. accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=192024765
2. Crum NF. Epstein Barr virus hepatitis: case series and review. South Med J. 2006;99:544-547. doi: 10.1097/01.smj.0000216469.04854.2a
3. Bunchorntavakul C, Reddy KR. Epstein-Barr virus and cytomegalovirus infections of the liver. Gastroenterol Clin North Am. 2020;49:331-346. doi: 10.1016/j.gtc.2020.01.008
4. Leonardsson H, Hreinsson JP, Löve A, et al. Hepatitis due to Epstein-Barr virus and cytomegalovirus: clinical features and outcomes. Scand J Gastroenterol. 2017;52:893-897. doi: 10.1080/ 00365521.2017.1319972
5. Banker L, Bowman PE. Epstein-Barr virus: forgotten etiology of hepatic injury. Clinical Advisor. September 23, 2021. Accessed April 18, 2023. www.clinicaladvisor.com/home/topics/infectious-diseases-information-center/epstein-barr-virus-etiology-hepatic-injury/
6. Fugl A, Lykkegaard Andersen C. Epstein-Barr virus and its association with disease: a review of relevance to general practice. BMC Fam Pract. 2019;20:62. doi: 10.1186/s12875-019-0954-3
7. Markin RS, Linder J, Zuerlein K, et al. Hepatitis in fatal infectious mononucleosis. Gastroenterology. 1987;93:1210-1217. doi: 10.1016/0016-5085(87)90246-0
8. Zhang W, Chen B, Chen Y, et al. Epstein-Barr virus-associated acute liver failure present in a 67-year-old immunocompetent female. Gastroenterology Res. 2016;9:74-78.
9. Mellinğer J, Rossaro L, Naugler W, et al. Epstein-Barr virus (EBV) related acute liver failure: a case series from the US Acute Liver Failure Study Group. Dig Dis Sci. 2014;59:1630-1637. doi: 10.1007/s10620-014-3029-2
10. Uluğ M, Kemal Celen M, Ayaz C, et al. Acute hepatitis: a rare complication of Epstein-Barr virus (EBV) infection. J Infect Dev Ctries. 2010;4:668-673. doi: 10.3855/jidc.871
THE CASE
A 23-year-old woman sought care from her primary care physician (PCP) after being sick for 7 days. The illness started with a headache and fatigue, and by Day 6, she also had fever, chills, sore throat, nausea, a poor appetite, and intractable vomiting. The patient had no significant medical history and was socially isolating due to the COVID-19 pandemic. She had no known sick contacts or recent sexual activity and did not use any illicit drugs.
On examination, her vital signs were normal although she appeared ill and diaphoretic. A shallow tonsil ulcer and tonsillar adenopathy were present. Laboratory tests included a complete blood count (CBC), comprehensive metabolic panel, Monospot test, and Epstein-Barr virus (EBV) antibody test. Results were notable for leukocytosis with atypical lymphocytes on her CBC. Her Monospot test and EBV immunoglobulin (Ig) M antibody were positive, and her EBV IgG antibody was negative. She was given a diagnosis of infectious mononucleosis (IM) and told to get adequate rest, drink a lot of fluids, and take ibuprofen or acetaminophen for pain control.
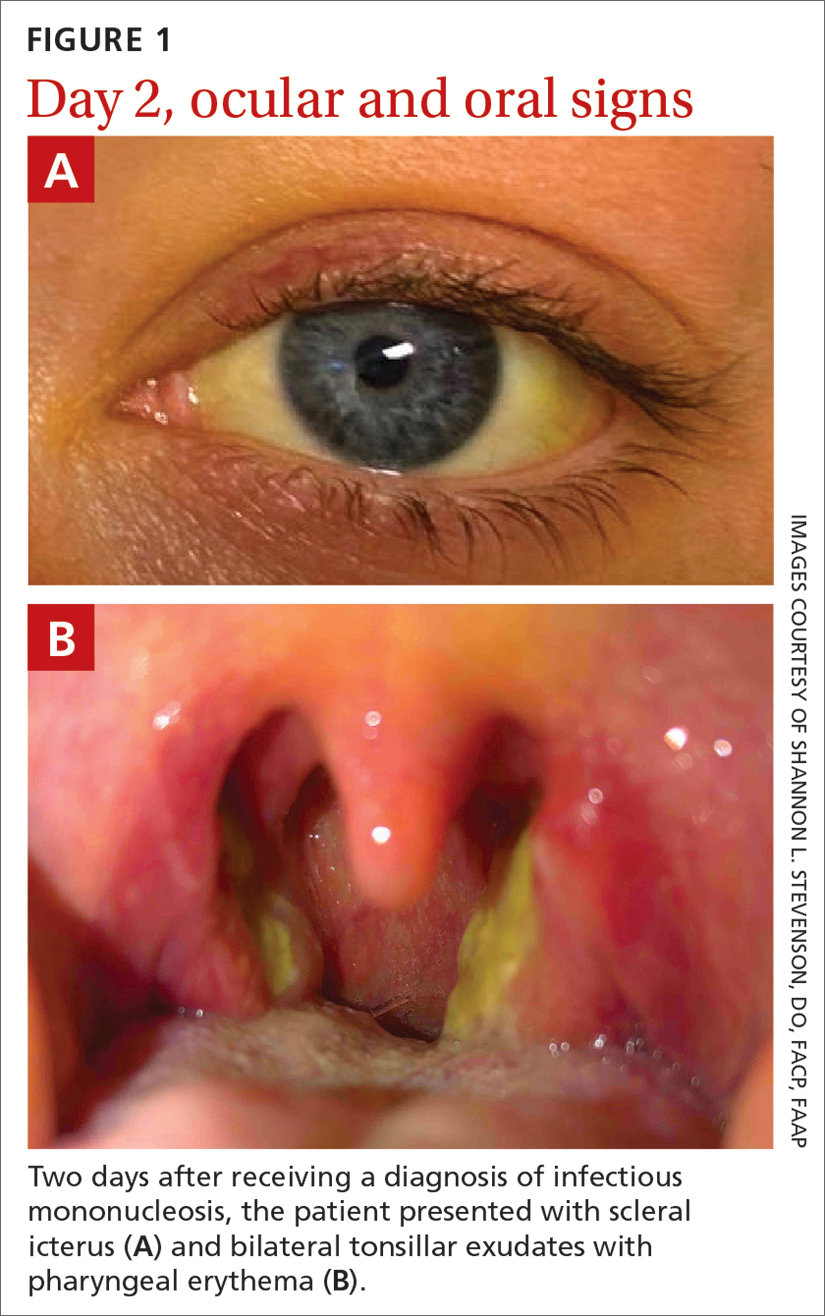
Two days later, she returned to her PCP with scleral icterus (FIGURE 1A), increasingly tender cervical lymphadenopathy, and left-side abdominal pain. Her liver function tests (LFTs) had worsened (TABLE). An abdominal ultrasound revealed mild diffuse decreased hepatic echogenicity and prominent periportal echogenicity, likely related to diffuse hepatic parenchymal disease, as well as splenomegaly and a mildly thickened gallbladder with no gallstones. She also had severe throat discomfort, with bilateral tonsillar exudates and pharyngeal erythema (FIGURE 1B).
THE DIAGNOSIS
Based on her symptoms and the results of her physical examination, LFTs, EBV serologic assays, and abdominal ultrasound, this patient was given a diagnosis of acute EBV hepatitis.
DISCUSSION
EBV infection, which is the most common cause of IM, causes asymptomatic liver enzyme abnormalities in 80% to 90% of patients.1-3 Although not common, patients can develop acute EBV hepatitis and require hospitalization.4
Be aware of potential complications. Prompt assessment of elevated liver enzymes and accurate diagnosis are key.5 Although acute EBV hepatitis is usually self-limiting, there can be serious gastrointestinal complications such as splenic rupture, liver failure due to acute and/or chronic EBV infection, autoimmune hepatitis, and hepatocellular carcinoma.2 It’s rare for EBV hepatitis to lead to acute liver failure,but when that occurs, it can be fatal.6-9 One case series revealed that while primary EBV infection accounts for less than 1% of adult acute liver failure cases, it has a high case fatality rate of 50%.9
Treatment for patients with EBV hepatitis is usually supportive and includes rest, analgesia, and avoidance of vigorous activity for 1 month to reduce the risk for splenic rupture.1 In patients with nausea and vomiting, intravenous fluids may be necessary and can be administered at an outpatient infusion center. For individuals with severe tonsillar hypertrophy, prednisone (40-60 mg/d for 2-3 days, with subsequent tapering over 1-2 weeks) is indicated to prevent airway obstruction.1 Acyclovir may be used to reduce EBV viral shedding; however, it has no significant clinical impact.1
Continue to: Patients who are hemodynamially stable...
Patients who are hemodynamically stable and have appropriate access to follow-up care can be managed at home.2 If follow-up cannot occur remotely within 1 week or the patient’s clinical status begins to worsen (ie, the patient’s liver enzymes or bilirubin levels dramatically increase), hospitalization is necessary.10
Through shared decision-making, our patient was treated as an outpatient based on her hemodynamic stability and her ability to closely follow up in the clinic and by phone and to access an outpatient infusion center. She was reexamined within 2 days and given ondansetron 8 mg IV with 2 L of normal saline at our outpatient infusion center. We also prescribed ibuprofen (400 mg every 6 hours as needed) for analgesia and issued the standard recommendations that she avoid contact sports (for at least 6 weeks) and excessive alcohol consumption.
On Day 11, the patient followed up with her PCP by telephone. The patient was started on oral prednisone (40 mg/d for 3 days with taper over the next week as symptoms improved) for her severe throat discomfort, exudates, difficulty swallowing, and muffled voice. By Day 14, her aminotransferase levels began to decrease (TABLE), and her symptoms steadily improved thereafter.
THE TAKEAWAY
When a patient presents with unexplained elevated liver enzymes or cholestasis, it is important to assess for signs and symptoms of EBV hepatitis. Although EBV hepatitis is typically self-limiting, it can have serious complications or be fatal. Prompt initiation of outpatient management may avoid these complications and hospitalization.
CORRESPONDENCE
Lydia J. Schneider, MD, 225 East Chicago Avenue, Chicago, IL 60611; lydia.schneider315@gmail.com
THE CASE
A 23-year-old woman sought care from her primary care physician (PCP) after being sick for 7 days. The illness started with a headache and fatigue, and by Day 6, she also had fever, chills, sore throat, nausea, a poor appetite, and intractable vomiting. The patient had no significant medical history and was socially isolating due to the COVID-19 pandemic. She had no known sick contacts or recent sexual activity and did not use any illicit drugs.
On examination, her vital signs were normal although she appeared ill and diaphoretic. A shallow tonsil ulcer and tonsillar adenopathy were present. Laboratory tests included a complete blood count (CBC), comprehensive metabolic panel, Monospot test, and Epstein-Barr virus (EBV) antibody test. Results were notable for leukocytosis with atypical lymphocytes on her CBC. Her Monospot test and EBV immunoglobulin (Ig) M antibody were positive, and her EBV IgG antibody was negative. She was given a diagnosis of infectious mononucleosis (IM) and told to get adequate rest, drink a lot of fluids, and take ibuprofen or acetaminophen for pain control.
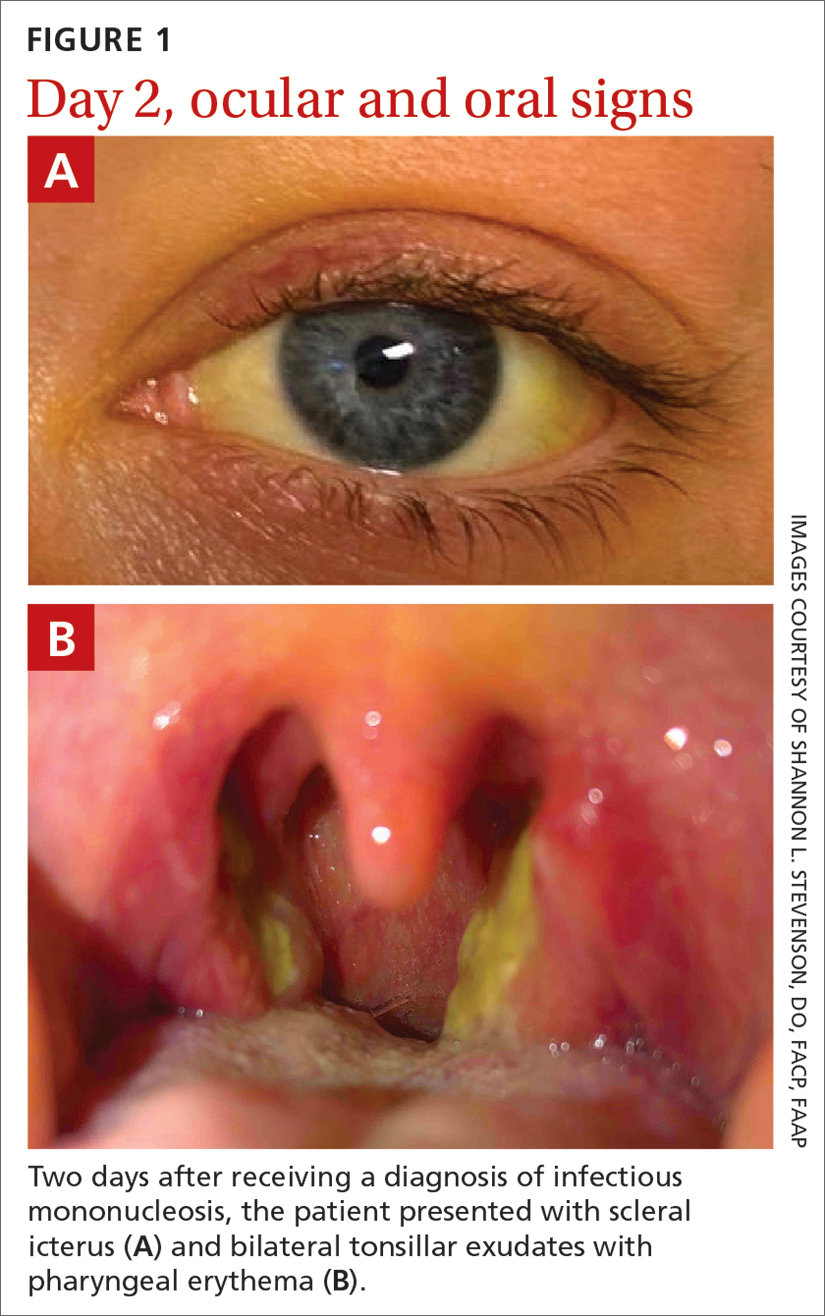
Two days later, she returned to her PCP with scleral icterus (FIGURE 1A), increasingly tender cervical lymphadenopathy, and left-side abdominal pain. Her liver function tests (LFTs) had worsened (TABLE). An abdominal ultrasound revealed mild diffuse decreased hepatic echogenicity and prominent periportal echogenicity, likely related to diffuse hepatic parenchymal disease, as well as splenomegaly and a mildly thickened gallbladder with no gallstones. She also had severe throat discomfort, with bilateral tonsillar exudates and pharyngeal erythema (FIGURE 1B).
THE DIAGNOSIS
Based on her symptoms and the results of her physical examination, LFTs, EBV serologic assays, and abdominal ultrasound, this patient was given a diagnosis of acute EBV hepatitis.
DISCUSSION
EBV infection, which is the most common cause of IM, causes asymptomatic liver enzyme abnormalities in 80% to 90% of patients.1-3 Although not common, patients can develop acute EBV hepatitis and require hospitalization.4
Be aware of potential complications. Prompt assessment of elevated liver enzymes and accurate diagnosis are key.5 Although acute EBV hepatitis is usually self-limiting, there can be serious gastrointestinal complications such as splenic rupture, liver failure due to acute and/or chronic EBV infection, autoimmune hepatitis, and hepatocellular carcinoma.2 It’s rare for EBV hepatitis to lead to acute liver failure,but when that occurs, it can be fatal.6-9 One case series revealed that while primary EBV infection accounts for less than 1% of adult acute liver failure cases, it has a high case fatality rate of 50%.9
Treatment for patients with EBV hepatitis is usually supportive and includes rest, analgesia, and avoidance of vigorous activity for 1 month to reduce the risk for splenic rupture.1 In patients with nausea and vomiting, intravenous fluids may be necessary and can be administered at an outpatient infusion center. For individuals with severe tonsillar hypertrophy, prednisone (40-60 mg/d for 2-3 days, with subsequent tapering over 1-2 weeks) is indicated to prevent airway obstruction.1 Acyclovir may be used to reduce EBV viral shedding; however, it has no significant clinical impact.1
Continue to: Patients who are hemodynamially stable...
Patients who are hemodynamically stable and have appropriate access to follow-up care can be managed at home.2 If follow-up cannot occur remotely within 1 week or the patient’s clinical status begins to worsen (ie, the patient’s liver enzymes or bilirubin levels dramatically increase), hospitalization is necessary.10
Through shared decision-making, our patient was treated as an outpatient based on her hemodynamic stability and her ability to closely follow up in the clinic and by phone and to access an outpatient infusion center. She was reexamined within 2 days and given ondansetron 8 mg IV with 2 L of normal saline at our outpatient infusion center. We also prescribed ibuprofen (400 mg every 6 hours as needed) for analgesia and issued the standard recommendations that she avoid contact sports (for at least 6 weeks) and excessive alcohol consumption.
On Day 11, the patient followed up with her PCP by telephone. The patient was started on oral prednisone (40 mg/d for 3 days with taper over the next week as symptoms improved) for her severe throat discomfort, exudates, difficulty swallowing, and muffled voice. By Day 14, her aminotransferase levels began to decrease (TABLE), and her symptoms steadily improved thereafter.
THE TAKEAWAY
When a patient presents with unexplained elevated liver enzymes or cholestasis, it is important to assess for signs and symptoms of EBV hepatitis. Although EBV hepatitis is typically self-limiting, it can have serious complications or be fatal. Prompt initiation of outpatient management may avoid these complications and hospitalization.
CORRESPONDENCE
Lydia J. Schneider, MD, 225 East Chicago Avenue, Chicago, IL 60611; lydia.schneider315@gmail.com
1. Cohen JI. Chapter 189: Epstein-Barr virus infections, including infectious mononucleosis. In: Jameson JL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. McGraw Hill; 2020. Accessed March 21, 2023. accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=192024765
2. Crum NF. Epstein Barr virus hepatitis: case series and review. South Med J. 2006;99:544-547. doi: 10.1097/01.smj.0000216469.04854.2a
3. Bunchorntavakul C, Reddy KR. Epstein-Barr virus and cytomegalovirus infections of the liver. Gastroenterol Clin North Am. 2020;49:331-346. doi: 10.1016/j.gtc.2020.01.008
4. Leonardsson H, Hreinsson JP, Löve A, et al. Hepatitis due to Epstein-Barr virus and cytomegalovirus: clinical features and outcomes. Scand J Gastroenterol. 2017;52:893-897. doi: 10.1080/ 00365521.2017.1319972
5. Banker L, Bowman PE. Epstein-Barr virus: forgotten etiology of hepatic injury. Clinical Advisor. September 23, 2021. Accessed April 18, 2023. www.clinicaladvisor.com/home/topics/infectious-diseases-information-center/epstein-barr-virus-etiology-hepatic-injury/
6. Fugl A, Lykkegaard Andersen C. Epstein-Barr virus and its association with disease: a review of relevance to general practice. BMC Fam Pract. 2019;20:62. doi: 10.1186/s12875-019-0954-3
7. Markin RS, Linder J, Zuerlein K, et al. Hepatitis in fatal infectious mononucleosis. Gastroenterology. 1987;93:1210-1217. doi: 10.1016/0016-5085(87)90246-0
8. Zhang W, Chen B, Chen Y, et al. Epstein-Barr virus-associated acute liver failure present in a 67-year-old immunocompetent female. Gastroenterology Res. 2016;9:74-78.
9. Mellinğer J, Rossaro L, Naugler W, et al. Epstein-Barr virus (EBV) related acute liver failure: a case series from the US Acute Liver Failure Study Group. Dig Dis Sci. 2014;59:1630-1637. doi: 10.1007/s10620-014-3029-2
10. Uluğ M, Kemal Celen M, Ayaz C, et al. Acute hepatitis: a rare complication of Epstein-Barr virus (EBV) infection. J Infect Dev Ctries. 2010;4:668-673. doi: 10.3855/jidc.871
1. Cohen JI. Chapter 189: Epstein-Barr virus infections, including infectious mononucleosis. In: Jameson JL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. McGraw Hill; 2020. Accessed March 21, 2023. accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=192024765
2. Crum NF. Epstein Barr virus hepatitis: case series and review. South Med J. 2006;99:544-547. doi: 10.1097/01.smj.0000216469.04854.2a
3. Bunchorntavakul C, Reddy KR. Epstein-Barr virus and cytomegalovirus infections of the liver. Gastroenterol Clin North Am. 2020;49:331-346. doi: 10.1016/j.gtc.2020.01.008
4. Leonardsson H, Hreinsson JP, Löve A, et al. Hepatitis due to Epstein-Barr virus and cytomegalovirus: clinical features and outcomes. Scand J Gastroenterol. 2017;52:893-897. doi: 10.1080/ 00365521.2017.1319972
5. Banker L, Bowman PE. Epstein-Barr virus: forgotten etiology of hepatic injury. Clinical Advisor. September 23, 2021. Accessed April 18, 2023. www.clinicaladvisor.com/home/topics/infectious-diseases-information-center/epstein-barr-virus-etiology-hepatic-injury/
6. Fugl A, Lykkegaard Andersen C. Epstein-Barr virus and its association with disease: a review of relevance to general practice. BMC Fam Pract. 2019;20:62. doi: 10.1186/s12875-019-0954-3
7. Markin RS, Linder J, Zuerlein K, et al. Hepatitis in fatal infectious mononucleosis. Gastroenterology. 1987;93:1210-1217. doi: 10.1016/0016-5085(87)90246-0
8. Zhang W, Chen B, Chen Y, et al. Epstein-Barr virus-associated acute liver failure present in a 67-year-old immunocompetent female. Gastroenterology Res. 2016;9:74-78.
9. Mellinğer J, Rossaro L, Naugler W, et al. Epstein-Barr virus (EBV) related acute liver failure: a case series from the US Acute Liver Failure Study Group. Dig Dis Sci. 2014;59:1630-1637. doi: 10.1007/s10620-014-3029-2
10. Uluğ M, Kemal Celen M, Ayaz C, et al. Acute hepatitis: a rare complication of Epstein-Barr virus (EBV) infection. J Infect Dev Ctries. 2010;4:668-673. doi: 10.3855/jidc.871
► Fever, fatigue, and sore throat
► Scleral icterus and hepatosplenomegaly