User login
Planned Parenthood videos explain sexual consent to young adults
Planned Parenthood Federation of America has released a series of videos geared to teens and young adults that explains and provides examples of giving, hearing, and asking for consent; addressing both verbal and nonverbal cues; and fostering healthy communication around sex and relationships.
The videos are intended to inform and ultimately reduce sexual assault by ensuring that sex is safe and mutually consensual, Dr. Leslie Kantor, vice president of education at Planned Parenthood Federation of America, said in a statement. They can be a valuable resource for teens because consent is often hard to demonstrate; even though there has been emphasis on telling people that they must obtain consent in a sexual encounter, there are few examples illustrating what it looks like, said Dr. Kantor.
“To address sexual assault in this country and move us toward a healthy culture of consent, young people must understand consent and have the skills to engage in healthy communication around sex and relationships. Open, honest communication between partners is necessary to ensure that sex is safe and mutually consensual, which is a skill that can be learned. Education about consent is sexual assault prevention,” Dr. Kantor wrote.
The four-part video series can be viewed in its entirety on Planned Parenthood’s YouTube channel, and lesson plans that accompany the videos can be obtained by emailing education@ppfa.org. Young people can find more information about consent on PlannedParenthood.org’s Info for Teens page and submit questions to Planned Parenthood’s Tumblr, Facebook, and Twitter pages.
Planned Parenthood Federation of America has released a series of videos geared to teens and young adults that explains and provides examples of giving, hearing, and asking for consent; addressing both verbal and nonverbal cues; and fostering healthy communication around sex and relationships.
The videos are intended to inform and ultimately reduce sexual assault by ensuring that sex is safe and mutually consensual, Dr. Leslie Kantor, vice president of education at Planned Parenthood Federation of America, said in a statement. They can be a valuable resource for teens because consent is often hard to demonstrate; even though there has been emphasis on telling people that they must obtain consent in a sexual encounter, there are few examples illustrating what it looks like, said Dr. Kantor.
“To address sexual assault in this country and move us toward a healthy culture of consent, young people must understand consent and have the skills to engage in healthy communication around sex and relationships. Open, honest communication between partners is necessary to ensure that sex is safe and mutually consensual, which is a skill that can be learned. Education about consent is sexual assault prevention,” Dr. Kantor wrote.
The four-part video series can be viewed in its entirety on Planned Parenthood’s YouTube channel, and lesson plans that accompany the videos can be obtained by emailing education@ppfa.org. Young people can find more information about consent on PlannedParenthood.org’s Info for Teens page and submit questions to Planned Parenthood’s Tumblr, Facebook, and Twitter pages.
Planned Parenthood Federation of America has released a series of videos geared to teens and young adults that explains and provides examples of giving, hearing, and asking for consent; addressing both verbal and nonverbal cues; and fostering healthy communication around sex and relationships.
The videos are intended to inform and ultimately reduce sexual assault by ensuring that sex is safe and mutually consensual, Dr. Leslie Kantor, vice president of education at Planned Parenthood Federation of America, said in a statement. They can be a valuable resource for teens because consent is often hard to demonstrate; even though there has been emphasis on telling people that they must obtain consent in a sexual encounter, there are few examples illustrating what it looks like, said Dr. Kantor.
“To address sexual assault in this country and move us toward a healthy culture of consent, young people must understand consent and have the skills to engage in healthy communication around sex and relationships. Open, honest communication between partners is necessary to ensure that sex is safe and mutually consensual, which is a skill that can be learned. Education about consent is sexual assault prevention,” Dr. Kantor wrote.
The four-part video series can be viewed in its entirety on Planned Parenthood’s YouTube channel, and lesson plans that accompany the videos can be obtained by emailing education@ppfa.org. Young people can find more information about consent on PlannedParenthood.org’s Info for Teens page and submit questions to Planned Parenthood’s Tumblr, Facebook, and Twitter pages.
Bipolar phenotype affects present, future self-image
Higher positivity ratings for current self-images were associated with lower depression and anxiety scores among young adults with Bipolar Spectrum Disorder (BPSD), suggesting that BPSD phenotype can shape the relationship between affect and current and future self-images.
As reported in the Journal of Affective Disorders, lead author Dr. Martina Di Simplicio of MRC Cognition and Brain Sciences Unit, Cambridge, England, and her associates assessed a nonclinical sample of 47 participants (66% female; mean age, 23) for hypomanic experiences and BPSD vulnerability, split into two groups based on their Mood Disorders Questionnaire (MDQ) score. Seventy-five percent of the participants in the high MDQ group generated at least one negative current self-image, compared with 48% of participants in the low MDQ group (P = .055).
The investigators noted that, for those with high MDQ scores, the relationship between affect and perception of the stability of negative self-images is different compared with those with low MDQ scores. And while 75% participants in the BPSD phenotype group were likely to endorse negative images of the current self (compared with less than 50% of the group without hypomanic experiences, almost none of the patients from either group had negative images of the future self).
“BPSD phenotype presents with both alterations and resilience in how self-images and mood shape each other. Further investigations could elucidate how this relationship is affected by illness progression and offer targets for early interventions based on experimental cognitive models,” the investigators wrote.
Read the article in Journal of Affective Disorders (doi: 10.1016/j.jad.2015.08.042).
Higher positivity ratings for current self-images were associated with lower depression and anxiety scores among young adults with Bipolar Spectrum Disorder (BPSD), suggesting that BPSD phenotype can shape the relationship between affect and current and future self-images.
As reported in the Journal of Affective Disorders, lead author Dr. Martina Di Simplicio of MRC Cognition and Brain Sciences Unit, Cambridge, England, and her associates assessed a nonclinical sample of 47 participants (66% female; mean age, 23) for hypomanic experiences and BPSD vulnerability, split into two groups based on their Mood Disorders Questionnaire (MDQ) score. Seventy-five percent of the participants in the high MDQ group generated at least one negative current self-image, compared with 48% of participants in the low MDQ group (P = .055).
The investigators noted that, for those with high MDQ scores, the relationship between affect and perception of the stability of negative self-images is different compared with those with low MDQ scores. And while 75% participants in the BPSD phenotype group were likely to endorse negative images of the current self (compared with less than 50% of the group without hypomanic experiences, almost none of the patients from either group had negative images of the future self).
“BPSD phenotype presents with both alterations and resilience in how self-images and mood shape each other. Further investigations could elucidate how this relationship is affected by illness progression and offer targets for early interventions based on experimental cognitive models,” the investigators wrote.
Read the article in Journal of Affective Disorders (doi: 10.1016/j.jad.2015.08.042).
Higher positivity ratings for current self-images were associated with lower depression and anxiety scores among young adults with Bipolar Spectrum Disorder (BPSD), suggesting that BPSD phenotype can shape the relationship between affect and current and future self-images.
As reported in the Journal of Affective Disorders, lead author Dr. Martina Di Simplicio of MRC Cognition and Brain Sciences Unit, Cambridge, England, and her associates assessed a nonclinical sample of 47 participants (66% female; mean age, 23) for hypomanic experiences and BPSD vulnerability, split into two groups based on their Mood Disorders Questionnaire (MDQ) score. Seventy-five percent of the participants in the high MDQ group generated at least one negative current self-image, compared with 48% of participants in the low MDQ group (P = .055).
The investigators noted that, for those with high MDQ scores, the relationship between affect and perception of the stability of negative self-images is different compared with those with low MDQ scores. And while 75% participants in the BPSD phenotype group were likely to endorse negative images of the current self (compared with less than 50% of the group without hypomanic experiences, almost none of the patients from either group had negative images of the future self).
“BPSD phenotype presents with both alterations and resilience in how self-images and mood shape each other. Further investigations could elucidate how this relationship is affected by illness progression and offer targets for early interventions based on experimental cognitive models,” the investigators wrote.
Read the article in Journal of Affective Disorders (doi: 10.1016/j.jad.2015.08.042).
FROM THE JOURNAL OF AFFECTIVE DISORDERS
MBDA score can help to predict RA radiographic progression
Multibiomarker disease activity scores were significantly associated with joint damage after 1 year in rheumatoid arthritis patients taking nonbiologic disease-modifying antirheumatic drug therapy even after adjustment for several established risk factors for joint damage in an observational study.
Lead author Dr. Wanying Li of Crescendo Bioscience and associates determined multibiomarker disease activity (MBDA) scores during 271 visits in 163 patients with established rheumatoid arthritis who received nonbiologic disease-modifying antirheumatic drug therapy. The MBDA combines the serum concentrations of 12 biomarkers via a validated algorithm to quantify disease activity. The patients had a mean MBDA score of 43 (possible range 1-100), a mean age of 55 years, and two-thirds were female. Rheumatoid factor and anti-CCP each was positive in two-thirds of patients.
The investigators noted that radiographic progression – both joint space narrowing and joint erosion – was infrequent during the following year when MBDA scores were low, but the frequency and severity of radiographic progression increased as MBDA scores became higher. Progression was not observed for all patients with MBDA scores greater than 44 – the optimal score threshold for predicting progression – but the risk of progression continued to increase within the high MBDA range. The MBDA score remained significantly associated with subsequent joint damage after adjusting for 28-joint swollen joint count, 28-joint disease activity score using C-reactive protein (CRP), CRP, total Sharp van der Heijde score, and serologic status.
“These findings suggest that the MBDA score may be able to complement conventional tools for assessing RA patients during DMARD therapy and to help determine which patients need treatment intensification to prevent progressive joint damage,” the authors wrote.
Read the full article in Rheumatology (doi: 10.1093/rheumatology/kev341).
Multibiomarker disease activity scores were significantly associated with joint damage after 1 year in rheumatoid arthritis patients taking nonbiologic disease-modifying antirheumatic drug therapy even after adjustment for several established risk factors for joint damage in an observational study.
Lead author Dr. Wanying Li of Crescendo Bioscience and associates determined multibiomarker disease activity (MBDA) scores during 271 visits in 163 patients with established rheumatoid arthritis who received nonbiologic disease-modifying antirheumatic drug therapy. The MBDA combines the serum concentrations of 12 biomarkers via a validated algorithm to quantify disease activity. The patients had a mean MBDA score of 43 (possible range 1-100), a mean age of 55 years, and two-thirds were female. Rheumatoid factor and anti-CCP each was positive in two-thirds of patients.
The investigators noted that radiographic progression – both joint space narrowing and joint erosion – was infrequent during the following year when MBDA scores were low, but the frequency and severity of radiographic progression increased as MBDA scores became higher. Progression was not observed for all patients with MBDA scores greater than 44 – the optimal score threshold for predicting progression – but the risk of progression continued to increase within the high MBDA range. The MBDA score remained significantly associated with subsequent joint damage after adjusting for 28-joint swollen joint count, 28-joint disease activity score using C-reactive protein (CRP), CRP, total Sharp van der Heijde score, and serologic status.
“These findings suggest that the MBDA score may be able to complement conventional tools for assessing RA patients during DMARD therapy and to help determine which patients need treatment intensification to prevent progressive joint damage,” the authors wrote.
Read the full article in Rheumatology (doi: 10.1093/rheumatology/kev341).
Multibiomarker disease activity scores were significantly associated with joint damage after 1 year in rheumatoid arthritis patients taking nonbiologic disease-modifying antirheumatic drug therapy even after adjustment for several established risk factors for joint damage in an observational study.
Lead author Dr. Wanying Li of Crescendo Bioscience and associates determined multibiomarker disease activity (MBDA) scores during 271 visits in 163 patients with established rheumatoid arthritis who received nonbiologic disease-modifying antirheumatic drug therapy. The MBDA combines the serum concentrations of 12 biomarkers via a validated algorithm to quantify disease activity. The patients had a mean MBDA score of 43 (possible range 1-100), a mean age of 55 years, and two-thirds were female. Rheumatoid factor and anti-CCP each was positive in two-thirds of patients.
The investigators noted that radiographic progression – both joint space narrowing and joint erosion – was infrequent during the following year when MBDA scores were low, but the frequency and severity of radiographic progression increased as MBDA scores became higher. Progression was not observed for all patients with MBDA scores greater than 44 – the optimal score threshold for predicting progression – but the risk of progression continued to increase within the high MBDA range. The MBDA score remained significantly associated with subsequent joint damage after adjusting for 28-joint swollen joint count, 28-joint disease activity score using C-reactive protein (CRP), CRP, total Sharp van der Heijde score, and serologic status.
“These findings suggest that the MBDA score may be able to complement conventional tools for assessing RA patients during DMARD therapy and to help determine which patients need treatment intensification to prevent progressive joint damage,” the authors wrote.
Read the full article in Rheumatology (doi: 10.1093/rheumatology/kev341).
FROM RHEUMATOLOGY
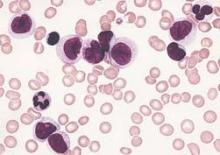
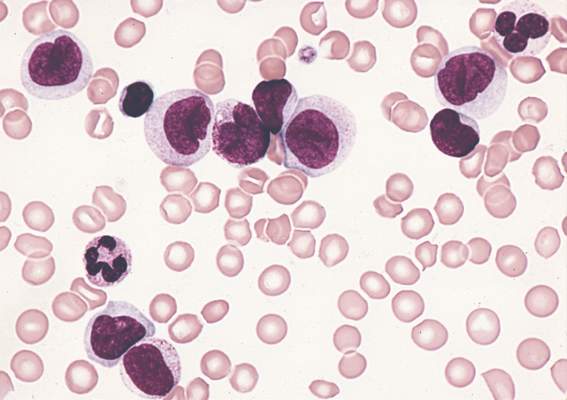
Advances in AML understanding could translate to improved therapy
An understanding of the various molecular differences between acute myeloid leukemia (AML) particles is guiding the search for new drug combinations targeting a variety of AML cellular processes, according to research published in the New England Journal of Medicine.
After a brief overview of disease classification and prognostic factors for AML, the authors, led by Dr. Hartmut Döhner of University Hospital Ulm in Germany, described a number of new treatment strategies. These approaches include directly addressing mutant proteins by targeting mutation-specific dependencies, developing inhibitors that could cut down on the occurrence of mutations in receptor tyrosine kinase genes, and developing new epigenetic therapies based on targeting specific mutant metabolic enzymes such as IDH1 and IDH2.
Other strategies, such as antibody therapy that focuses on the development of new monoclonal antibodies targeting CD33, and new formulations of older cytotoxic agents, also are being developed or are in clinical trial stages; however, many of these developments have not yet been translated into clinical practice, the researchers noted.
“New compounds hold promise to improve treatment outcomes; however, it is unlikely that any of these compounds, when used as single agents, will cure the disease. A major challenge will be to identify predictors for a response to specific agents, which will allow for the rational design of combinatorial therapies,” they wrote.
Dr. Döhner and a coauthor disclosed ties with several pharmaceutical companies.
Read the article here.
An understanding of the various molecular differences between acute myeloid leukemia (AML) particles is guiding the search for new drug combinations targeting a variety of AML cellular processes, according to research published in the New England Journal of Medicine.
After a brief overview of disease classification and prognostic factors for AML, the authors, led by Dr. Hartmut Döhner of University Hospital Ulm in Germany, described a number of new treatment strategies. These approaches include directly addressing mutant proteins by targeting mutation-specific dependencies, developing inhibitors that could cut down on the occurrence of mutations in receptor tyrosine kinase genes, and developing new epigenetic therapies based on targeting specific mutant metabolic enzymes such as IDH1 and IDH2.
Other strategies, such as antibody therapy that focuses on the development of new monoclonal antibodies targeting CD33, and new formulations of older cytotoxic agents, also are being developed or are in clinical trial stages; however, many of these developments have not yet been translated into clinical practice, the researchers noted.
“New compounds hold promise to improve treatment outcomes; however, it is unlikely that any of these compounds, when used as single agents, will cure the disease. A major challenge will be to identify predictors for a response to specific agents, which will allow for the rational design of combinatorial therapies,” they wrote.
Dr. Döhner and a coauthor disclosed ties with several pharmaceutical companies.
Read the article here.
An understanding of the various molecular differences between acute myeloid leukemia (AML) particles is guiding the search for new drug combinations targeting a variety of AML cellular processes, according to research published in the New England Journal of Medicine.
After a brief overview of disease classification and prognostic factors for AML, the authors, led by Dr. Hartmut Döhner of University Hospital Ulm in Germany, described a number of new treatment strategies. These approaches include directly addressing mutant proteins by targeting mutation-specific dependencies, developing inhibitors that could cut down on the occurrence of mutations in receptor tyrosine kinase genes, and developing new epigenetic therapies based on targeting specific mutant metabolic enzymes such as IDH1 and IDH2.
Other strategies, such as antibody therapy that focuses on the development of new monoclonal antibodies targeting CD33, and new formulations of older cytotoxic agents, also are being developed or are in clinical trial stages; however, many of these developments have not yet been translated into clinical practice, the researchers noted.
“New compounds hold promise to improve treatment outcomes; however, it is unlikely that any of these compounds, when used as single agents, will cure the disease. A major challenge will be to identify predictors for a response to specific agents, which will allow for the rational design of combinatorial therapies,” they wrote.
Dr. Döhner and a coauthor disclosed ties with several pharmaceutical companies.
Read the article here.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Respiratory problems make adenotonsillectomy recovery worse for kids
Respiratory compromise and secondary hemorrhage were the most common early side effects in children who had adenotonsillectomies; children with obstructive sleep apnea (OSA) have nearly five times more respiratory complications after surgery than children without OSA, a multistudy review concluded.
Graziela De Luca Canto, Ph.D., of the Federal University of Santa Catarina, Brazil, and her associates performed a data review by identifying 1,254 different citations found via electronic database searches; after eliminations, only 23 studies were included in the final analysis. Although children with OSA have nearly five times more respiratory complications after adenotonsillectomy than their peers, (odds ratio, 4.90), they are less likely to have postoperative bleeding, compared with children without OSA (OR, 0.41). Among both groups, the most frequent complication was respiratory compromise (9.4%), followed by secondary hemorrhage (2.6%).
Because children with OSA are more likely to require supplemental oxygen, oral or nasal airway insertion, or assisted ventilation in the immediate postoperative period than their peers, the authors suggested that anesthesiologists would be wise to screen patients for snoring, airway dysfunction, and other airway anatomic disorders before performing surgery.
“Children with OSA are clearly at higher anesthetic risk than are patients with normal upper airway function. … Despite the pressure to reduce costs, both surgeons and anesthesiologists should improve screening procedures, perhaps develop alternate surgical approaches, to decrease the risks,” the investigators wrote.
Read the full article in Pediatrics 2015 (doi: 10.1542/peds.2015-1283).
Respiratory compromise and secondary hemorrhage were the most common early side effects in children who had adenotonsillectomies; children with obstructive sleep apnea (OSA) have nearly five times more respiratory complications after surgery than children without OSA, a multistudy review concluded.
Graziela De Luca Canto, Ph.D., of the Federal University of Santa Catarina, Brazil, and her associates performed a data review by identifying 1,254 different citations found via electronic database searches; after eliminations, only 23 studies were included in the final analysis. Although children with OSA have nearly five times more respiratory complications after adenotonsillectomy than their peers, (odds ratio, 4.90), they are less likely to have postoperative bleeding, compared with children without OSA (OR, 0.41). Among both groups, the most frequent complication was respiratory compromise (9.4%), followed by secondary hemorrhage (2.6%).
Because children with OSA are more likely to require supplemental oxygen, oral or nasal airway insertion, or assisted ventilation in the immediate postoperative period than their peers, the authors suggested that anesthesiologists would be wise to screen patients for snoring, airway dysfunction, and other airway anatomic disorders before performing surgery.
“Children with OSA are clearly at higher anesthetic risk than are patients with normal upper airway function. … Despite the pressure to reduce costs, both surgeons and anesthesiologists should improve screening procedures, perhaps develop alternate surgical approaches, to decrease the risks,” the investigators wrote.
Read the full article in Pediatrics 2015 (doi: 10.1542/peds.2015-1283).
Respiratory compromise and secondary hemorrhage were the most common early side effects in children who had adenotonsillectomies; children with obstructive sleep apnea (OSA) have nearly five times more respiratory complications after surgery than children without OSA, a multistudy review concluded.
Graziela De Luca Canto, Ph.D., of the Federal University of Santa Catarina, Brazil, and her associates performed a data review by identifying 1,254 different citations found via electronic database searches; after eliminations, only 23 studies were included in the final analysis. Although children with OSA have nearly five times more respiratory complications after adenotonsillectomy than their peers, (odds ratio, 4.90), they are less likely to have postoperative bleeding, compared with children without OSA (OR, 0.41). Among both groups, the most frequent complication was respiratory compromise (9.4%), followed by secondary hemorrhage (2.6%).
Because children with OSA are more likely to require supplemental oxygen, oral or nasal airway insertion, or assisted ventilation in the immediate postoperative period than their peers, the authors suggested that anesthesiologists would be wise to screen patients for snoring, airway dysfunction, and other airway anatomic disorders before performing surgery.
“Children with OSA are clearly at higher anesthetic risk than are patients with normal upper airway function. … Despite the pressure to reduce costs, both surgeons and anesthesiologists should improve screening procedures, perhaps develop alternate surgical approaches, to decrease the risks,” the investigators wrote.
Read the full article in Pediatrics 2015 (doi: 10.1542/peds.2015-1283).
FROM PEDIATRICS
Uptick in Health Care Workers Getting Flu Shots in 2014-2015 Season
Overall, 77.3% of health care personnel reported receiving an influenza vaccination during the 2014-2015 season, with the highest vaccination coverage was reported in work sites with employer requirements for vaccination, according to an investigation published in MMWR (2015 Sep 18;64[36]:993-9).
Vaccination data came from an opt-in Internet panel survey conducted by Abt Associates for the Centers for Disease Control and Prevention, and included questions on demographic characteristics, occupation, work setting, self-reported influenza vaccination, and employer vaccination policies. Results from 1,914 survey responses were analyzed. The overall health care personnel (HCP) influenza vaccination coverage estimate for the 2014-2015 season was 77.3%, compared with 75.2% for the 2013-2014 season. When compared with the 2013-2014 season, coverage in 2014-2015 was higher among pharmacists (95.3% vs. 85.7%), assistants/aides (64.4% vs. 57.7%), and nonclinical personnel (75.2% vs. 68.6%). Coverage among other clinical personnel decreased from 87.4% in 2013-2014 to 81.3% in 2014-2015, while other categories experienced little change between the two time periods.
The team of researchers, led by Carla L. Black, Ph.D., of the National Center for Immunization and Respiratory Diseases, CDC, noted that among HCP whose employers did not require vaccination, vaccination coverage among those who worked in locations where their employer made vaccination available on-site at no cost for more than 1 day was 83.9%, compared with coverage of 73.6% among those who worked in locations where their employer made vaccination available at no cost for 1 day only, and 59.5% among those who worked in locations where their employer did not provide influenza vaccination on-site at no cost but actively promoted vaccination through other mechanisms.
“These findings support recommendations for a comprehensive strategy that includes easy access to vaccination at no cost on multiple days, along with promotion of vaccination, to increase HCP influenza vaccination coverage,” the authors wrote.
Read the full report here: http://www.cdc.gov/mmwr/.
Overall, 77.3% of health care personnel reported receiving an influenza vaccination during the 2014-2015 season, with the highest vaccination coverage was reported in work sites with employer requirements for vaccination, according to an investigation published in MMWR (2015 Sep 18;64[36]:993-9).
Vaccination data came from an opt-in Internet panel survey conducted by Abt Associates for the Centers for Disease Control and Prevention, and included questions on demographic characteristics, occupation, work setting, self-reported influenza vaccination, and employer vaccination policies. Results from 1,914 survey responses were analyzed. The overall health care personnel (HCP) influenza vaccination coverage estimate for the 2014-2015 season was 77.3%, compared with 75.2% for the 2013-2014 season. When compared with the 2013-2014 season, coverage in 2014-2015 was higher among pharmacists (95.3% vs. 85.7%), assistants/aides (64.4% vs. 57.7%), and nonclinical personnel (75.2% vs. 68.6%). Coverage among other clinical personnel decreased from 87.4% in 2013-2014 to 81.3% in 2014-2015, while other categories experienced little change between the two time periods.
The team of researchers, led by Carla L. Black, Ph.D., of the National Center for Immunization and Respiratory Diseases, CDC, noted that among HCP whose employers did not require vaccination, vaccination coverage among those who worked in locations where their employer made vaccination available on-site at no cost for more than 1 day was 83.9%, compared with coverage of 73.6% among those who worked in locations where their employer made vaccination available at no cost for 1 day only, and 59.5% among those who worked in locations where their employer did not provide influenza vaccination on-site at no cost but actively promoted vaccination through other mechanisms.
“These findings support recommendations for a comprehensive strategy that includes easy access to vaccination at no cost on multiple days, along with promotion of vaccination, to increase HCP influenza vaccination coverage,” the authors wrote.
Read the full report here: http://www.cdc.gov/mmwr/.
Overall, 77.3% of health care personnel reported receiving an influenza vaccination during the 2014-2015 season, with the highest vaccination coverage was reported in work sites with employer requirements for vaccination, according to an investigation published in MMWR (2015 Sep 18;64[36]:993-9).
Vaccination data came from an opt-in Internet panel survey conducted by Abt Associates for the Centers for Disease Control and Prevention, and included questions on demographic characteristics, occupation, work setting, self-reported influenza vaccination, and employer vaccination policies. Results from 1,914 survey responses were analyzed. The overall health care personnel (HCP) influenza vaccination coverage estimate for the 2014-2015 season was 77.3%, compared with 75.2% for the 2013-2014 season. When compared with the 2013-2014 season, coverage in 2014-2015 was higher among pharmacists (95.3% vs. 85.7%), assistants/aides (64.4% vs. 57.7%), and nonclinical personnel (75.2% vs. 68.6%). Coverage among other clinical personnel decreased from 87.4% in 2013-2014 to 81.3% in 2014-2015, while other categories experienced little change between the two time periods.
The team of researchers, led by Carla L. Black, Ph.D., of the National Center for Immunization and Respiratory Diseases, CDC, noted that among HCP whose employers did not require vaccination, vaccination coverage among those who worked in locations where their employer made vaccination available on-site at no cost for more than 1 day was 83.9%, compared with coverage of 73.6% among those who worked in locations where their employer made vaccination available at no cost for 1 day only, and 59.5% among those who worked in locations where their employer did not provide influenza vaccination on-site at no cost but actively promoted vaccination through other mechanisms.
“These findings support recommendations for a comprehensive strategy that includes easy access to vaccination at no cost on multiple days, along with promotion of vaccination, to increase HCP influenza vaccination coverage,” the authors wrote.
Read the full report here: http://www.cdc.gov/mmwr/.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Uptick in health care workers getting flu shots in 2014-2015 season
Overall, 77.3% of health care personnel reported receiving an influenza vaccination during the 2014-2015 season, with the highest vaccination coverage was reported in work sites with employer requirements for vaccination, according to an investigation published in MMWR (2015 Sep 18;64[36]:993-9).
Vaccination data came from an opt-in Internet panel survey conducted by Abt Associates for the Centers for Disease Control and Prevention, and included questions on demographic characteristics, occupation, work setting, self-reported influenza vaccination, and employer vaccination policies. Results from 1,914 survey responses were analyzed. The overall health care personnel (HCP) influenza vaccination coverage estimate for the 2014-2015 season was 77.3%, compared with 75.2% for the 2013-2014 season. When compared with the 2013-2014 season, coverage in 2014-2015 was higher among pharmacists (95.3% vs. 85.7%), assistants/aides (64.4% vs. 57.7%), and nonclinical personnel (75.2% vs. 68.6%). Coverage among other clinical personnel decreased from 87.4% in 2013-2014 to 81.3% in 2014-2015, while other categories experienced little change between the two time periods.
The team of researchers, led by Carla L. Black, Ph.D., of the National Center for Immunization and Respiratory Diseases, CDC, noted that among HCP whose employers did not require vaccination, vaccination coverage among those who worked in locations where their employer made vaccination available on-site at no cost for more than 1 day was 83.9%, compared with coverage of 73.6% among those who worked in locations where their employer made vaccination available at no cost for 1 day only, and 59.5% among those who worked in locations where their employer did not provide influenza vaccination on-site at no cost but actively promoted vaccination through other mechanisms.
“These findings support recommendations for a comprehensive strategy that includes easy access to vaccination at no cost on multiple days, along with promotion of vaccination, to increase HCP influenza vaccination coverage,” the authors wrote.
Read the full report here: http://www.cdc.gov/mmwr/.
Overall, 77.3% of health care personnel reported receiving an influenza vaccination during the 2014-2015 season, with the highest vaccination coverage was reported in work sites with employer requirements for vaccination, according to an investigation published in MMWR (2015 Sep 18;64[36]:993-9).
Vaccination data came from an opt-in Internet panel survey conducted by Abt Associates for the Centers for Disease Control and Prevention, and included questions on demographic characteristics, occupation, work setting, self-reported influenza vaccination, and employer vaccination policies. Results from 1,914 survey responses were analyzed. The overall health care personnel (HCP) influenza vaccination coverage estimate for the 2014-2015 season was 77.3%, compared with 75.2% for the 2013-2014 season. When compared with the 2013-2014 season, coverage in 2014-2015 was higher among pharmacists (95.3% vs. 85.7%), assistants/aides (64.4% vs. 57.7%), and nonclinical personnel (75.2% vs. 68.6%). Coverage among other clinical personnel decreased from 87.4% in 2013-2014 to 81.3% in 2014-2015, while other categories experienced little change between the two time periods.
The team of researchers, led by Carla L. Black, Ph.D., of the National Center for Immunization and Respiratory Diseases, CDC, noted that among HCP whose employers did not require vaccination, vaccination coverage among those who worked in locations where their employer made vaccination available on-site at no cost for more than 1 day was 83.9%, compared with coverage of 73.6% among those who worked in locations where their employer made vaccination available at no cost for 1 day only, and 59.5% among those who worked in locations where their employer did not provide influenza vaccination on-site at no cost but actively promoted vaccination through other mechanisms.
“These findings support recommendations for a comprehensive strategy that includes easy access to vaccination at no cost on multiple days, along with promotion of vaccination, to increase HCP influenza vaccination coverage,” the authors wrote.
Read the full report here: http://www.cdc.gov/mmwr/.
Overall, 77.3% of health care personnel reported receiving an influenza vaccination during the 2014-2015 season, with the highest vaccination coverage was reported in work sites with employer requirements for vaccination, according to an investigation published in MMWR (2015 Sep 18;64[36]:993-9).
Vaccination data came from an opt-in Internet panel survey conducted by Abt Associates for the Centers for Disease Control and Prevention, and included questions on demographic characteristics, occupation, work setting, self-reported influenza vaccination, and employer vaccination policies. Results from 1,914 survey responses were analyzed. The overall health care personnel (HCP) influenza vaccination coverage estimate for the 2014-2015 season was 77.3%, compared with 75.2% for the 2013-2014 season. When compared with the 2013-2014 season, coverage in 2014-2015 was higher among pharmacists (95.3% vs. 85.7%), assistants/aides (64.4% vs. 57.7%), and nonclinical personnel (75.2% vs. 68.6%). Coverage among other clinical personnel decreased from 87.4% in 2013-2014 to 81.3% in 2014-2015, while other categories experienced little change between the two time periods.
The team of researchers, led by Carla L. Black, Ph.D., of the National Center for Immunization and Respiratory Diseases, CDC, noted that among HCP whose employers did not require vaccination, vaccination coverage among those who worked in locations where their employer made vaccination available on-site at no cost for more than 1 day was 83.9%, compared with coverage of 73.6% among those who worked in locations where their employer made vaccination available at no cost for 1 day only, and 59.5% among those who worked in locations where their employer did not provide influenza vaccination on-site at no cost but actively promoted vaccination through other mechanisms.
“These findings support recommendations for a comprehensive strategy that includes easy access to vaccination at no cost on multiple days, along with promotion of vaccination, to increase HCP influenza vaccination coverage,” the authors wrote.
Read the full report here: http://www.cdc.gov/mmwr/.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Executive attention deficits often persist in euthymic bipolar disorder
Euthymic bipolar disorder patients have impaired executive control (greater interference), reduced vigilance, slower overall reaction times, and poorer accuracy scores compared with healthy controls, a recent research article shows.
Lead author Andrea Marotta, Ph.D., of the University of Rome, and colleagues compared a sample of euthymic bipolar disorder patients and age-matched healthy controls, and had both groups complete the Attention Network Test for Interactions and Vigilance (ANTI-V), a neurocognitive test that assesses the efficiency of attentional networks and measures orienting, executive and alerting networks, and vigilance (tonic alerting). Although the bipolar disorder patients exhibited normal phasic alerting and orienting, they performed worse on alerting and executive control, the authors found.
“Our results show that deficits in executive attention and sustained attention often persist in [bipolar disorder] patients even after complete remission of affective symptoms, thus suggesting that cognitive enhancing treatments programmed to improve these deficits could contribute to improve their functional recovery,” they wrote.
Read the full article in Psychiatry Research (2015 Sept 30;229[1-2]:490-6. doi: 10.1016/jpsychres.2015.06.026).
Euthymic bipolar disorder patients have impaired executive control (greater interference), reduced vigilance, slower overall reaction times, and poorer accuracy scores compared with healthy controls, a recent research article shows.
Lead author Andrea Marotta, Ph.D., of the University of Rome, and colleagues compared a sample of euthymic bipolar disorder patients and age-matched healthy controls, and had both groups complete the Attention Network Test for Interactions and Vigilance (ANTI-V), a neurocognitive test that assesses the efficiency of attentional networks and measures orienting, executive and alerting networks, and vigilance (tonic alerting). Although the bipolar disorder patients exhibited normal phasic alerting and orienting, they performed worse on alerting and executive control, the authors found.
“Our results show that deficits in executive attention and sustained attention often persist in [bipolar disorder] patients even after complete remission of affective symptoms, thus suggesting that cognitive enhancing treatments programmed to improve these deficits could contribute to improve their functional recovery,” they wrote.
Read the full article in Psychiatry Research (2015 Sept 30;229[1-2]:490-6. doi: 10.1016/jpsychres.2015.06.026).
Euthymic bipolar disorder patients have impaired executive control (greater interference), reduced vigilance, slower overall reaction times, and poorer accuracy scores compared with healthy controls, a recent research article shows.
Lead author Andrea Marotta, Ph.D., of the University of Rome, and colleagues compared a sample of euthymic bipolar disorder patients and age-matched healthy controls, and had both groups complete the Attention Network Test for Interactions and Vigilance (ANTI-V), a neurocognitive test that assesses the efficiency of attentional networks and measures orienting, executive and alerting networks, and vigilance (tonic alerting). Although the bipolar disorder patients exhibited normal phasic alerting and orienting, they performed worse on alerting and executive control, the authors found.
“Our results show that deficits in executive attention and sustained attention often persist in [bipolar disorder] patients even after complete remission of affective symptoms, thus suggesting that cognitive enhancing treatments programmed to improve these deficits could contribute to improve their functional recovery,” they wrote.
Read the full article in Psychiatry Research (2015 Sept 30;229[1-2]:490-6. doi: 10.1016/jpsychres.2015.06.026).
FROM PSYCHIATRY RESEARCH
Clinicians Rarely Talk to Teens About E-cigarettes
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
FROM THE JOURNAL OF ADOLESCENT HEALTH
Physicians rarely talk to teens about e-cigarettes
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
FROM THE JOURNAL OF ADOLESCENT HEALTH