User login
Recurrent Pyogenic Granuloma With a Satellite Lesion
Pyogenic granuloma (PG)(also known as a telangiectatic granuloma, eruptive hemangioma, granulation tissue-type hemangioma, granuloma gravidarum, lobular capillary hemangioma, and pregnancy tumor) is a common tumorlike growth of the oral mucosa or skin that is considered to be nonneoplastic in nature.1 Pyogenic granuloma is considered to be a reactive tumorlike lesion that arises in response to various stimuli, including chronic low-grade irritation,2 traumatic injury,2 hormonal factors, certain kinds of drugs (ie, retinoid, antiretroviral, oncologic agents), and iatrogenic stimulations in dental practice (eg, guided tissue regeneration).3 Clinically, oral PG presents as a smooth or lobulated exophytic lesion manifesting as a small erythematous growth on a pedunculated or sometimes sessile base that usually is hemorrhagic.4,5
Hullihen6 was the first clinician to report about PG in the English-language literature in 1844, but the term pyogenic granuloma or granuloma pyogenicum was introduced by Hartzell7 in 1904. Before the use of the term pyogenic granuloma, these lesions were known as Botryomycosis hominis because they were thought to be caused by infection from either staphylococci or streptococci.5 Today, the literature is clear that the term pyogenic granuloma is a misnomer because it is not a true granuloma. In actuality, PG is a capillary hemangioma of lobular subtype, which is the reason the lesions often are prone to bleeding.5 The term pyogenic, which means pus producing, is misleading because there is no pus present in lesions of PG from any specific infection.5
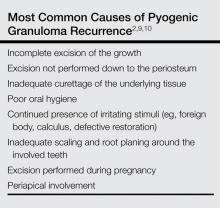
Pyogenic granuloma may occur in patients of all ages but predominantly in the second decade of life in young adult females.8 The size of PG lesions varies but rarely exceeds 2.5 cm in diameter. Pyogenic granuloma of the oral mucosa commonly involves the gingiva (75% of all cases).8 The lips, tongue, and buccal mucosa are the next most common sites. Lesions are slightly more common on the maxillary gingiva than the mandibular gingiva; anterior areas are more frequently affected than posterior areas. Also, these lesions are much more common on the facial aspect of the gingiva than the lingual aspect; some extend between the teeth and involve both the facial and lingual gingiva.8 After excision, recurrence occurs in up to 16% of lesions,9,10 requiring re-excision. Recurrence is believed to occur due to a variety of factors (Table).2,9,10
We report the case of 30-year-old woman who presented with PG in the anterior palatal region during pregnancy that recurred with a satellite lesion 1 year following surgical excision.
Case Report
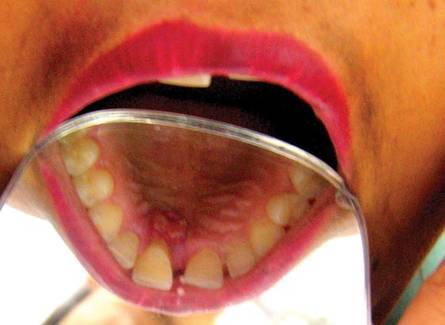
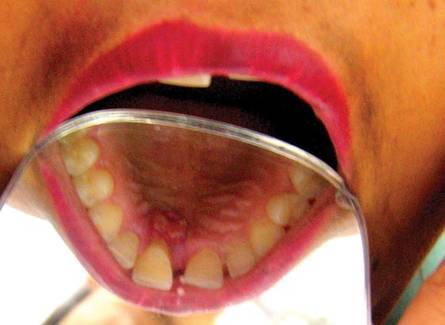
A 30-year-old woman presented to the department of periodontics for evaluation of a growth on the gums of the upper jaw of 3 months’ duration. The patient was in the third trimester of pregnancy (7 months). Intraoral examination revealed a 3×3-cm growth in the anterior palatal region that was firm in consistency and nontender with a pedunculated base (Figure 1). The patient had poor oral hygiene. The growth initially was small in size but had grown rapidly in the last few days. The patient reported no history of oral trauma, infection, or surgery.
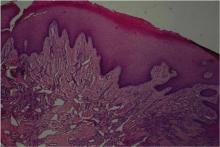
Intraoral radiography showed bone loss around the maxillary central incisors. A provisional diagnosis of PG was made. The differential diagnosis included peripheral giant cell granuloma, peripheral ossifying fibroma, metastatic cancer, hemangioma, conventional granulation tissue, hyperplastic gingival inflammation, Kaposi sarcoma, bacillary angiomatosis, angiosarcoma, and non-Hodgkin lymphoma. Initial therapy consisting of scaling and root planing was performed, and the patient was advised to return after the birth of the baby for excision of the growth. Surgical excision was performed 6 months after initial presentation (3 months after delivery) and the lesion was submitted for histopathologic examination, which revealed a parakeratinized, hyperplastic, stratified squamous epithelium overlying the connective tissue stroma that consisted of collagenous tissue interspersed with many small and large endothelium-lined blood vessels and moderate to dense inflammatory infiltrates, indicative of PG (Figure 2).
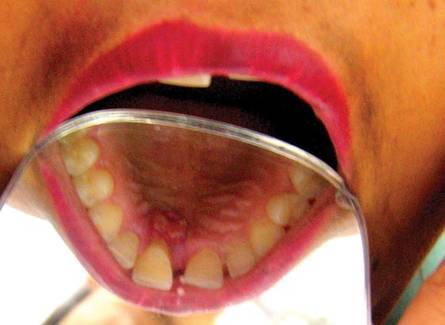
The patient was followed for 3 months without recurrence of the lesion (Figure 3). One year later the patient presented with recurrence of the lesion (Figure 4). Intraoral examination revealed 2 larger growths at the same location that caused disturbance in the patient’s speech and mastication. Additionally, a small growth also was noted on the labial aspect of the maxillary right canine (Figure 5). Scaling and root planing was done on all lesions. The lesions were re-excised and submitted for histopathologic examination. Histopathologic findings were similar to the prior biopsy. The right maxillary central incisor was nonresponsive to electric pulp testing; therefore, endodontic treatment was performed. Uneventful healing of the surgical sites was noted 2 weeks following excision. No recurrence was reported after 1 year of follow-up (Figure 6), and the patient continues to remain disease free 3 years later.
|  | |

|  |
Comment
Pyogenic granuloma occurs in 0.2% to 9.6% of all pregnancies, highlighting the underlying hormonal changes in this patient population.1 In our patient, the initial lesion may have occurred due to the hormonal changes of pregnancy coupled with poor oral hygiene. Pyogenic granulomas that are excised during pregnancy are known to recur,9,10 and excision is only advised in this patient population if the lesion is causing disturbance in speech and mastication.9 In our patient, excision was performed following delivery because the initial lesion had not caused any disturbance in speech or mastication. Cases of larger PGs that do interfere with the patient’s speech and mastication may necessitate early excision prior to delivery.11 In our patient, thorough scaling and root planing around the involved teeth was done before excision of the lesion by the dentist. Despite taking these precautions to reduce the chances of recurrence, the lesion recurred 1 year following excision. Recurrence of PG after excision has been noted in up to 16% of cases.2 Profuse bleeding in our patient was encountered during excision of the initial lesion and was controlled using pressure packs and local hemostatic agents. It is possible that some small portions of the lesion were not excised due to the profuse bleeding. Bleeding during excision of PGs is expected; therefore, aids to achieve hemostasis (eg, pressure packs, local hemostatic agents, electrocautery) should be available. In spite of educating and motivating the patient to practice good oral hygiene, her oral hygiene status was poor, which could be an important factor in the recurrence of the lesion at the primary site and also may explain the occurrence of an additional growth/satellite lesion around the maxillary right canine. Occurrence of satellite lesions or additional lesions following excision of PG has been reported in the literature.12,13 However, the presence of additional lesions in the oral cavity or gingiva rarely has been reported.
Pyogenic granuloma is common on the gingiva, especially in pregnant women, and recurrence following excision is not rare. If causes of recurrence, such as chronic irritation factors, are resolved and excision is done with some amount of normal adjacent tissue down to the periosteum, chances of recurrence decrease.
1. Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006;48:167-175.
2. Neville BW, Damm DD, Allen CM, et al. Soft tissue tumors: pyogenic granuloma. In: Neville BW, Damm DD, Allen CM, et al, eds. Oral and Maxillofacial Pathology. 3rd ed. St. Louis, MO: Saunders Elsevier; 2008:517-519.
3. Fowler EB, Cuenin MF, Thompson SH, et al. Pyogenic granuloma associated with guided tissue regeneration: a case report. J Periodontol. 1996;67:1011-1015.
4. Kolte AP, Kolte RA, Shrirao TS. Focal fibrous overgrowths: a case series and review of literature. Contemp Clin Dent. 2010;1:271-274.
5. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16:79-82.
6. Hullihen SP. Case of aneurism by anastomosis of the superior maxillae. Am J Dent Sc. 1844;4:160-162.
7. Hartzell MB. Granuloma pyogenicum. J Cutan Dis Syph. 1904;22:520-525.
8. Krishnapillai R, Punnoose K, Angadi PV, et al. Oral pyogenic granuloma—a review of 215 cases in a South Indian Teaching Hospital, Karnataka, over a period of 20 years [published online ahead of print January 26, 2012]. Oral Maxillofac Surg. 2012;16:305-309.
9. Oettinger-Barak O, Machtei EE, Ofer BI, et al. Pregnancy tumor occurring twice in the same individual: report of a case and hormone receptors study. Quintessence Int. 2006;37:213-218.
10. Ong MA, Chai WL, Ngeow WC. Recurrent gigantic pyogenic granuloma disturbing speech and mastication: a case report and literature review. Ann Acad Med Singapore. 1998;27:258-261.
11. Lindenmüller IH, Noll P, Mameghani T, et al. CO2 laser-assisted treatment of a giant pyogenic granuloma of the gingiva. Int J Dent Hyg. 2010;8:249-252.
12. Allen RK, Rodman OG. Pyogenic granuloma recurrent with satellite lesions. J Dermatol Surg Oncol. 1979;5:490-493.
13. Fisher I. Recurrent multiple pyogenic granuloma with multiple satellites. features of Masson’s hemangioma. Cutis. 1977;20:201-205.
Pyogenic granuloma (PG)(also known as a telangiectatic granuloma, eruptive hemangioma, granulation tissue-type hemangioma, granuloma gravidarum, lobular capillary hemangioma, and pregnancy tumor) is a common tumorlike growth of the oral mucosa or skin that is considered to be nonneoplastic in nature.1 Pyogenic granuloma is considered to be a reactive tumorlike lesion that arises in response to various stimuli, including chronic low-grade irritation,2 traumatic injury,2 hormonal factors, certain kinds of drugs (ie, retinoid, antiretroviral, oncologic agents), and iatrogenic stimulations in dental practice (eg, guided tissue regeneration).3 Clinically, oral PG presents as a smooth or lobulated exophytic lesion manifesting as a small erythematous growth on a pedunculated or sometimes sessile base that usually is hemorrhagic.4,5
Hullihen6 was the first clinician to report about PG in the English-language literature in 1844, but the term pyogenic granuloma or granuloma pyogenicum was introduced by Hartzell7 in 1904. Before the use of the term pyogenic granuloma, these lesions were known as Botryomycosis hominis because they were thought to be caused by infection from either staphylococci or streptococci.5 Today, the literature is clear that the term pyogenic granuloma is a misnomer because it is not a true granuloma. In actuality, PG is a capillary hemangioma of lobular subtype, which is the reason the lesions often are prone to bleeding.5 The term pyogenic, which means pus producing, is misleading because there is no pus present in lesions of PG from any specific infection.5
Pyogenic granuloma may occur in patients of all ages but predominantly in the second decade of life in young adult females.8 The size of PG lesions varies but rarely exceeds 2.5 cm in diameter. Pyogenic granuloma of the oral mucosa commonly involves the gingiva (75% of all cases).8 The lips, tongue, and buccal mucosa are the next most common sites. Lesions are slightly more common on the maxillary gingiva than the mandibular gingiva; anterior areas are more frequently affected than posterior areas. Also, these lesions are much more common on the facial aspect of the gingiva than the lingual aspect; some extend between the teeth and involve both the facial and lingual gingiva.8 After excision, recurrence occurs in up to 16% of lesions,9,10 requiring re-excision. Recurrence is believed to occur due to a variety of factors (Table).2,9,10
We report the case of 30-year-old woman who presented with PG in the anterior palatal region during pregnancy that recurred with a satellite lesion 1 year following surgical excision.
Case Report
A 30-year-old woman presented to the department of periodontics for evaluation of a growth on the gums of the upper jaw of 3 months’ duration. The patient was in the third trimester of pregnancy (7 months). Intraoral examination revealed a 3×3-cm growth in the anterior palatal region that was firm in consistency and nontender with a pedunculated base (Figure 1). The patient had poor oral hygiene. The growth initially was small in size but had grown rapidly in the last few days. The patient reported no history of oral trauma, infection, or surgery.
Intraoral radiography showed bone loss around the maxillary central incisors. A provisional diagnosis of PG was made. The differential diagnosis included peripheral giant cell granuloma, peripheral ossifying fibroma, metastatic cancer, hemangioma, conventional granulation tissue, hyperplastic gingival inflammation, Kaposi sarcoma, bacillary angiomatosis, angiosarcoma, and non-Hodgkin lymphoma. Initial therapy consisting of scaling and root planing was performed, and the patient was advised to return after the birth of the baby for excision of the growth. Surgical excision was performed 6 months after initial presentation (3 months after delivery) and the lesion was submitted for histopathologic examination, which revealed a parakeratinized, hyperplastic, stratified squamous epithelium overlying the connective tissue stroma that consisted of collagenous tissue interspersed with many small and large endothelium-lined blood vessels and moderate to dense inflammatory infiltrates, indicative of PG (Figure 2).
The patient was followed for 3 months without recurrence of the lesion (Figure 3). One year later the patient presented with recurrence of the lesion (Figure 4). Intraoral examination revealed 2 larger growths at the same location that caused disturbance in the patient’s speech and mastication. Additionally, a small growth also was noted on the labial aspect of the maxillary right canine (Figure 5). Scaling and root planing was done on all lesions. The lesions were re-excised and submitted for histopathologic examination. Histopathologic findings were similar to the prior biopsy. The right maxillary central incisor was nonresponsive to electric pulp testing; therefore, endodontic treatment was performed. Uneventful healing of the surgical sites was noted 2 weeks following excision. No recurrence was reported after 1 year of follow-up (Figure 6), and the patient continues to remain disease free 3 years later.
|  | |

|  |
Comment
Pyogenic granuloma occurs in 0.2% to 9.6% of all pregnancies, highlighting the underlying hormonal changes in this patient population.1 In our patient, the initial lesion may have occurred due to the hormonal changes of pregnancy coupled with poor oral hygiene. Pyogenic granulomas that are excised during pregnancy are known to recur,9,10 and excision is only advised in this patient population if the lesion is causing disturbance in speech and mastication.9 In our patient, excision was performed following delivery because the initial lesion had not caused any disturbance in speech or mastication. Cases of larger PGs that do interfere with the patient’s speech and mastication may necessitate early excision prior to delivery.11 In our patient, thorough scaling and root planing around the involved teeth was done before excision of the lesion by the dentist. Despite taking these precautions to reduce the chances of recurrence, the lesion recurred 1 year following excision. Recurrence of PG after excision has been noted in up to 16% of cases.2 Profuse bleeding in our patient was encountered during excision of the initial lesion and was controlled using pressure packs and local hemostatic agents. It is possible that some small portions of the lesion were not excised due to the profuse bleeding. Bleeding during excision of PGs is expected; therefore, aids to achieve hemostasis (eg, pressure packs, local hemostatic agents, electrocautery) should be available. In spite of educating and motivating the patient to practice good oral hygiene, her oral hygiene status was poor, which could be an important factor in the recurrence of the lesion at the primary site and also may explain the occurrence of an additional growth/satellite lesion around the maxillary right canine. Occurrence of satellite lesions or additional lesions following excision of PG has been reported in the literature.12,13 However, the presence of additional lesions in the oral cavity or gingiva rarely has been reported.
Pyogenic granuloma is common on the gingiva, especially in pregnant women, and recurrence following excision is not rare. If causes of recurrence, such as chronic irritation factors, are resolved and excision is done with some amount of normal adjacent tissue down to the periosteum, chances of recurrence decrease.
Pyogenic granuloma (PG)(also known as a telangiectatic granuloma, eruptive hemangioma, granulation tissue-type hemangioma, granuloma gravidarum, lobular capillary hemangioma, and pregnancy tumor) is a common tumorlike growth of the oral mucosa or skin that is considered to be nonneoplastic in nature.1 Pyogenic granuloma is considered to be a reactive tumorlike lesion that arises in response to various stimuli, including chronic low-grade irritation,2 traumatic injury,2 hormonal factors, certain kinds of drugs (ie, retinoid, antiretroviral, oncologic agents), and iatrogenic stimulations in dental practice (eg, guided tissue regeneration).3 Clinically, oral PG presents as a smooth or lobulated exophytic lesion manifesting as a small erythematous growth on a pedunculated or sometimes sessile base that usually is hemorrhagic.4,5
Hullihen6 was the first clinician to report about PG in the English-language literature in 1844, but the term pyogenic granuloma or granuloma pyogenicum was introduced by Hartzell7 in 1904. Before the use of the term pyogenic granuloma, these lesions were known as Botryomycosis hominis because they were thought to be caused by infection from either staphylococci or streptococci.5 Today, the literature is clear that the term pyogenic granuloma is a misnomer because it is not a true granuloma. In actuality, PG is a capillary hemangioma of lobular subtype, which is the reason the lesions often are prone to bleeding.5 The term pyogenic, which means pus producing, is misleading because there is no pus present in lesions of PG from any specific infection.5
Pyogenic granuloma may occur in patients of all ages but predominantly in the second decade of life in young adult females.8 The size of PG lesions varies but rarely exceeds 2.5 cm in diameter. Pyogenic granuloma of the oral mucosa commonly involves the gingiva (75% of all cases).8 The lips, tongue, and buccal mucosa are the next most common sites. Lesions are slightly more common on the maxillary gingiva than the mandibular gingiva; anterior areas are more frequently affected than posterior areas. Also, these lesions are much more common on the facial aspect of the gingiva than the lingual aspect; some extend between the teeth and involve both the facial and lingual gingiva.8 After excision, recurrence occurs in up to 16% of lesions,9,10 requiring re-excision. Recurrence is believed to occur due to a variety of factors (Table).2,9,10
We report the case of 30-year-old woman who presented with PG in the anterior palatal region during pregnancy that recurred with a satellite lesion 1 year following surgical excision.
Case Report
A 30-year-old woman presented to the department of periodontics for evaluation of a growth on the gums of the upper jaw of 3 months’ duration. The patient was in the third trimester of pregnancy (7 months). Intraoral examination revealed a 3×3-cm growth in the anterior palatal region that was firm in consistency and nontender with a pedunculated base (Figure 1). The patient had poor oral hygiene. The growth initially was small in size but had grown rapidly in the last few days. The patient reported no history of oral trauma, infection, or surgery.
Intraoral radiography showed bone loss around the maxillary central incisors. A provisional diagnosis of PG was made. The differential diagnosis included peripheral giant cell granuloma, peripheral ossifying fibroma, metastatic cancer, hemangioma, conventional granulation tissue, hyperplastic gingival inflammation, Kaposi sarcoma, bacillary angiomatosis, angiosarcoma, and non-Hodgkin lymphoma. Initial therapy consisting of scaling and root planing was performed, and the patient was advised to return after the birth of the baby for excision of the growth. Surgical excision was performed 6 months after initial presentation (3 months after delivery) and the lesion was submitted for histopathologic examination, which revealed a parakeratinized, hyperplastic, stratified squamous epithelium overlying the connective tissue stroma that consisted of collagenous tissue interspersed with many small and large endothelium-lined blood vessels and moderate to dense inflammatory infiltrates, indicative of PG (Figure 2).
The patient was followed for 3 months without recurrence of the lesion (Figure 3). One year later the patient presented with recurrence of the lesion (Figure 4). Intraoral examination revealed 2 larger growths at the same location that caused disturbance in the patient’s speech and mastication. Additionally, a small growth also was noted on the labial aspect of the maxillary right canine (Figure 5). Scaling and root planing was done on all lesions. The lesions were re-excised and submitted for histopathologic examination. Histopathologic findings were similar to the prior biopsy. The right maxillary central incisor was nonresponsive to electric pulp testing; therefore, endodontic treatment was performed. Uneventful healing of the surgical sites was noted 2 weeks following excision. No recurrence was reported after 1 year of follow-up (Figure 6), and the patient continues to remain disease free 3 years later.
|  | |

|  |
Comment
Pyogenic granuloma occurs in 0.2% to 9.6% of all pregnancies, highlighting the underlying hormonal changes in this patient population.1 In our patient, the initial lesion may have occurred due to the hormonal changes of pregnancy coupled with poor oral hygiene. Pyogenic granulomas that are excised during pregnancy are known to recur,9,10 and excision is only advised in this patient population if the lesion is causing disturbance in speech and mastication.9 In our patient, excision was performed following delivery because the initial lesion had not caused any disturbance in speech or mastication. Cases of larger PGs that do interfere with the patient’s speech and mastication may necessitate early excision prior to delivery.11 In our patient, thorough scaling and root planing around the involved teeth was done before excision of the lesion by the dentist. Despite taking these precautions to reduce the chances of recurrence, the lesion recurred 1 year following excision. Recurrence of PG after excision has been noted in up to 16% of cases.2 Profuse bleeding in our patient was encountered during excision of the initial lesion and was controlled using pressure packs and local hemostatic agents. It is possible that some small portions of the lesion were not excised due to the profuse bleeding. Bleeding during excision of PGs is expected; therefore, aids to achieve hemostasis (eg, pressure packs, local hemostatic agents, electrocautery) should be available. In spite of educating and motivating the patient to practice good oral hygiene, her oral hygiene status was poor, which could be an important factor in the recurrence of the lesion at the primary site and also may explain the occurrence of an additional growth/satellite lesion around the maxillary right canine. Occurrence of satellite lesions or additional lesions following excision of PG has been reported in the literature.12,13 However, the presence of additional lesions in the oral cavity or gingiva rarely has been reported.
Pyogenic granuloma is common on the gingiva, especially in pregnant women, and recurrence following excision is not rare. If causes of recurrence, such as chronic irritation factors, are resolved and excision is done with some amount of normal adjacent tissue down to the periosteum, chances of recurrence decrease.
1. Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006;48:167-175.
2. Neville BW, Damm DD, Allen CM, et al. Soft tissue tumors: pyogenic granuloma. In: Neville BW, Damm DD, Allen CM, et al, eds. Oral and Maxillofacial Pathology. 3rd ed. St. Louis, MO: Saunders Elsevier; 2008:517-519.
3. Fowler EB, Cuenin MF, Thompson SH, et al. Pyogenic granuloma associated with guided tissue regeneration: a case report. J Periodontol. 1996;67:1011-1015.
4. Kolte AP, Kolte RA, Shrirao TS. Focal fibrous overgrowths: a case series and review of literature. Contemp Clin Dent. 2010;1:271-274.
5. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16:79-82.
6. Hullihen SP. Case of aneurism by anastomosis of the superior maxillae. Am J Dent Sc. 1844;4:160-162.
7. Hartzell MB. Granuloma pyogenicum. J Cutan Dis Syph. 1904;22:520-525.
8. Krishnapillai R, Punnoose K, Angadi PV, et al. Oral pyogenic granuloma—a review of 215 cases in a South Indian Teaching Hospital, Karnataka, over a period of 20 years [published online ahead of print January 26, 2012]. Oral Maxillofac Surg. 2012;16:305-309.
9. Oettinger-Barak O, Machtei EE, Ofer BI, et al. Pregnancy tumor occurring twice in the same individual: report of a case and hormone receptors study. Quintessence Int. 2006;37:213-218.
10. Ong MA, Chai WL, Ngeow WC. Recurrent gigantic pyogenic granuloma disturbing speech and mastication: a case report and literature review. Ann Acad Med Singapore. 1998;27:258-261.
11. Lindenmüller IH, Noll P, Mameghani T, et al. CO2 laser-assisted treatment of a giant pyogenic granuloma of the gingiva. Int J Dent Hyg. 2010;8:249-252.
12. Allen RK, Rodman OG. Pyogenic granuloma recurrent with satellite lesions. J Dermatol Surg Oncol. 1979;5:490-493.
13. Fisher I. Recurrent multiple pyogenic granuloma with multiple satellites. features of Masson’s hemangioma. Cutis. 1977;20:201-205.
1. Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006;48:167-175.
2. Neville BW, Damm DD, Allen CM, et al. Soft tissue tumors: pyogenic granuloma. In: Neville BW, Damm DD, Allen CM, et al, eds. Oral and Maxillofacial Pathology. 3rd ed. St. Louis, MO: Saunders Elsevier; 2008:517-519.
3. Fowler EB, Cuenin MF, Thompson SH, et al. Pyogenic granuloma associated with guided tissue regeneration: a case report. J Periodontol. 1996;67:1011-1015.
4. Kolte AP, Kolte RA, Shrirao TS. Focal fibrous overgrowths: a case series and review of literature. Contemp Clin Dent. 2010;1:271-274.
5. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16:79-82.
6. Hullihen SP. Case of aneurism by anastomosis of the superior maxillae. Am J Dent Sc. 1844;4:160-162.
7. Hartzell MB. Granuloma pyogenicum. J Cutan Dis Syph. 1904;22:520-525.
8. Krishnapillai R, Punnoose K, Angadi PV, et al. Oral pyogenic granuloma—a review of 215 cases in a South Indian Teaching Hospital, Karnataka, over a period of 20 years [published online ahead of print January 26, 2012]. Oral Maxillofac Surg. 2012;16:305-309.
9. Oettinger-Barak O, Machtei EE, Ofer BI, et al. Pregnancy tumor occurring twice in the same individual: report of a case and hormone receptors study. Quintessence Int. 2006;37:213-218.
10. Ong MA, Chai WL, Ngeow WC. Recurrent gigantic pyogenic granuloma disturbing speech and mastication: a case report and literature review. Ann Acad Med Singapore. 1998;27:258-261.
11. Lindenmüller IH, Noll P, Mameghani T, et al. CO2 laser-assisted treatment of a giant pyogenic granuloma of the gingiva. Int J Dent Hyg. 2010;8:249-252.
12. Allen RK, Rodman OG. Pyogenic granuloma recurrent with satellite lesions. J Dermatol Surg Oncol. 1979;5:490-493.
13. Fisher I. Recurrent multiple pyogenic granuloma with multiple satellites. features of Masson’s hemangioma. Cutis. 1977;20:201-205.
Practice Points
- Pyogenic granulomas (PGs) need to be excised down to the periosteum to decrease the chances of recurrence.
- Bleeding during excision of PGs is expected; therefore, aids to achieve hemostasis (eg, pressure packs, local hemostatic agents, electrocautery) should be available.
- The underlying cause for the lesion (ie, infection, trauma, irritation) has to be identified and treated to decrease the chances of recurrence.