User login
Fever, petechiae, and joint pain
A 59-year-old woman presented to our emergency department with a rash, severe acute pain in her left hip and lower back, and dyspnea on exertion. She denied having a headache and her mental status was at baseline. The woman reported exposure to rats and snakes one week prior to presentation, and mentioned getting bitten by a rat multiple times on the back of both of her hands while feeding it to her son’s pet snake. The patient had a history of a left hip replacement, with a revision and bone graft 5 years earlier.
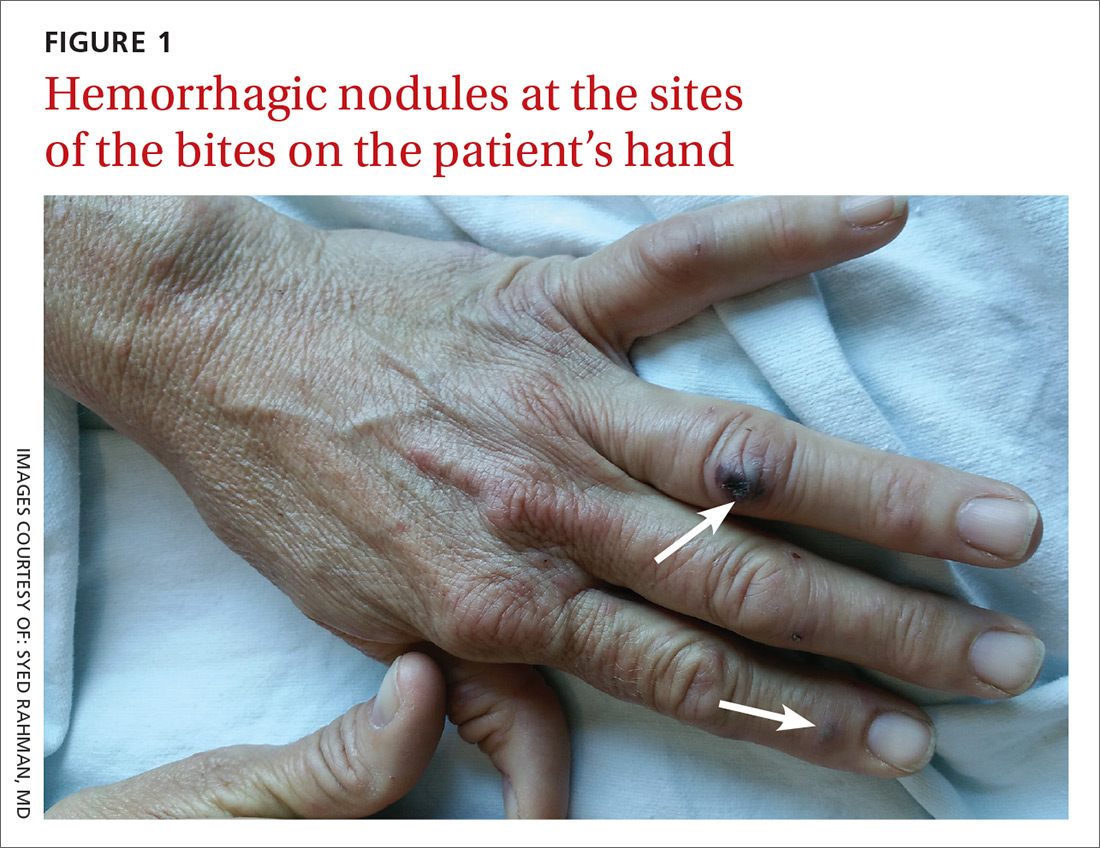
The patient had a fever of 103° F during the physical examination. She had erythematous papules and central hemorrhagic eschars at the sites of the bites (FIGURE 1). She also had nonblanching petechiae on both of her lower legs (FIGURE 2) and on the dorsal and palmar aspects of her hands.

The patient’s lab work showed mild normocytic anemia with a hemoglobin level of 11.4 g/dL (normal, 12-16 g/dL) and a platelet count of 129,000/mcL (normal, 130,000-400,000/mcL). Her white blood cell count, chemistries, brain natriuretic peptide test, and chest x-ray were normal.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Rat bite fever
Based on the patient’s symptoms, history, and lab work, we concluded that this was a case of rat bite fever. RBF is a zoonotic systemic illness caused by infection from either the gram-negative bacillus Streptobacillus moniliformis, commonly found in the United States, or the gram-negative rod Spirillum minus, commonly seen in Asia. Anyone with exposure to rats is at risk for RBF, especially pet shop employees, lab workers, and people living in areas with rat infestations.1
The rash associated with RBF can be petechial, purpuric, or maculopapular, but the presence of hemorrhagic nodules and ulcers at the site of the bite is especially indicative of the illness. The rash often involves the hands and feet, including the palms and soles.
To make the diagnosis of RBF, a careful history and a high index of suspicion are important. Fever and rigor are often the first symptoms to appear, beginning 3 to 10 days after the bite. Three to 4 days after the onset of fever, up to 75% of patients will develop a rash.2 Joint and muscle aches are also common, as is a migrating pattern of arthritis.2,3
Rule out other infections related to animal exposure
The differential diagnosis for RBF includes other animal-related infections, such as those from snake bites, leptospirosis, rabies, and pasteurellosis.
Symptoms associated with snake bite injuries appear rapidly after the bite and vary with the type of snake toxin. Hemotoxic symptoms may include intense pain, edema, petechiae, and ecchymosis from coagulopathy. Neurotoxic symptoms may include ptosis, weakness, and paresthesias. All snake bites should be treated with supportive care, and antivenin is indicated when symptoms or history indicate a bite from a venomous snake. Venomous snakes are rarely intentionally kept as pets.2
Leptospirosis is a zoonotic bacterial infection that may be spread through the urine of rats, dogs, or other mammals. Symptoms may be mild and limited to conjunctivitis, vomiting, and fever; life-threatening symptoms include hemorrhage and kidney failure. A petechial rash is not typical.4 Beta-lactam antibiotics are the treatment of choice.
Rabies is a viral infection that occurs after exposure to infected animals (most commonly raccoons, bats, skunks, and foxes). Symptoms include fever and mental status changes that can lead to death; rash is not a typical symptom. Exposed patients should receive post-exposure prophylaxis with immune globulin or a rabies vaccine.5
Pasteurellosis may also cause hemorrhagic nodules at the site of the bite or scratch, but bites are typically caused by larger animals such as dogs and livestock. Other symptoms include fever, sepsis, and osteomyelitis. Treatment includes amoxicillin-clavulanate or a fluoroquinolone-clindamycin combination.6
In cases of high suspicion, special culture tubes may be needed
Blood cultures and cerebrospinal fluid cultures are often falsely negative. Special culture tubes without polyanethol sulfonate preservative, which inhibits the growth of S moniliformis, may be required in cases of high suspicion. S moniliformis polymerase chain reaction may be available in some specialized labs.7,8
Treatment options include 7 to 10 days of antibiotic therapy with oral penicillin 500 mg 4 times daily, amoxicillin-clavulanate 875/125 mg twice daily, or oral doxycycline 100 mg every 12 hours.9
RBF may be fatal if not treated.3 Complications may include bacteremia, septicemia, meningitis, and endocarditis.
Our patient received empiric intravenous ceftriaxone 1 g every 24 hours and her fever and joint pain resolved within 48 hours. On Day 3 she was discharged home to complete a 10-day course of oral amoxicillin-clavulanate 875/125 mg. Her primary care physician reported that the rash resolved and the patient made a full recovery.
CORRESPONDENCE
Kate Rowland, MD, MS, Rush-Copley Family Medicine Residency, 2020 Ogden Ave. Suite 325, Aurora, IL 60504; krowland@rushcopley.com.
1. Centers for Disease Control and Prevention. Rat-bite fever (RBF). Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/rat-bite-fever/index.html. Accessed December 1, 2015.
2. Elliott SP. Rat bite fever and Streptobacillus moniliformis. Clin Microbiol Rev. 2007;20:13-22.
3. Juckett G, Hancox JG. Venomous snakebites in the United States: management review and update. Am Fam Physician. 2002;65:1367-1374.
4. Rabinowitz PM, Gordon Z, Odofin L. Pet-related infections. Am Fam Physician. 2007;76:1314-1322.
5. Fishbein DB, Robinson LE. Rabies. N Engl J Med. 1993;329:1632-1638.
6. Wilson BA, Ho M. Pasteurella multocida: from zoonosis to cellular microbiology. Clin Microbiol Rev. 2013;26:631-655.
7. Eng J. Effect of sodium polyanethol sulfonate in blood cultures. J Clin Microbiol. 1975;1:119-123.
8. Nakagomi D, Deguchi N, Yagasaki A, et al. Rat-bite fever identified by polymerase chain reaction detection of Streptobacillus moniliformis DNA. J Dermatol. 2008;35:667-670.
9. Bush LM, Perez MT. Rat-bite fever. In: The Merck Manual of Diagnosis and Therapy. Whitehouse Station, NJ: Merck Sharp & Dohme Corp.; 2011.
A 59-year-old woman presented to our emergency department with a rash, severe acute pain in her left hip and lower back, and dyspnea on exertion. She denied having a headache and her mental status was at baseline. The woman reported exposure to rats and snakes one week prior to presentation, and mentioned getting bitten by a rat multiple times on the back of both of her hands while feeding it to her son’s pet snake. The patient had a history of a left hip replacement, with a revision and bone graft 5 years earlier.
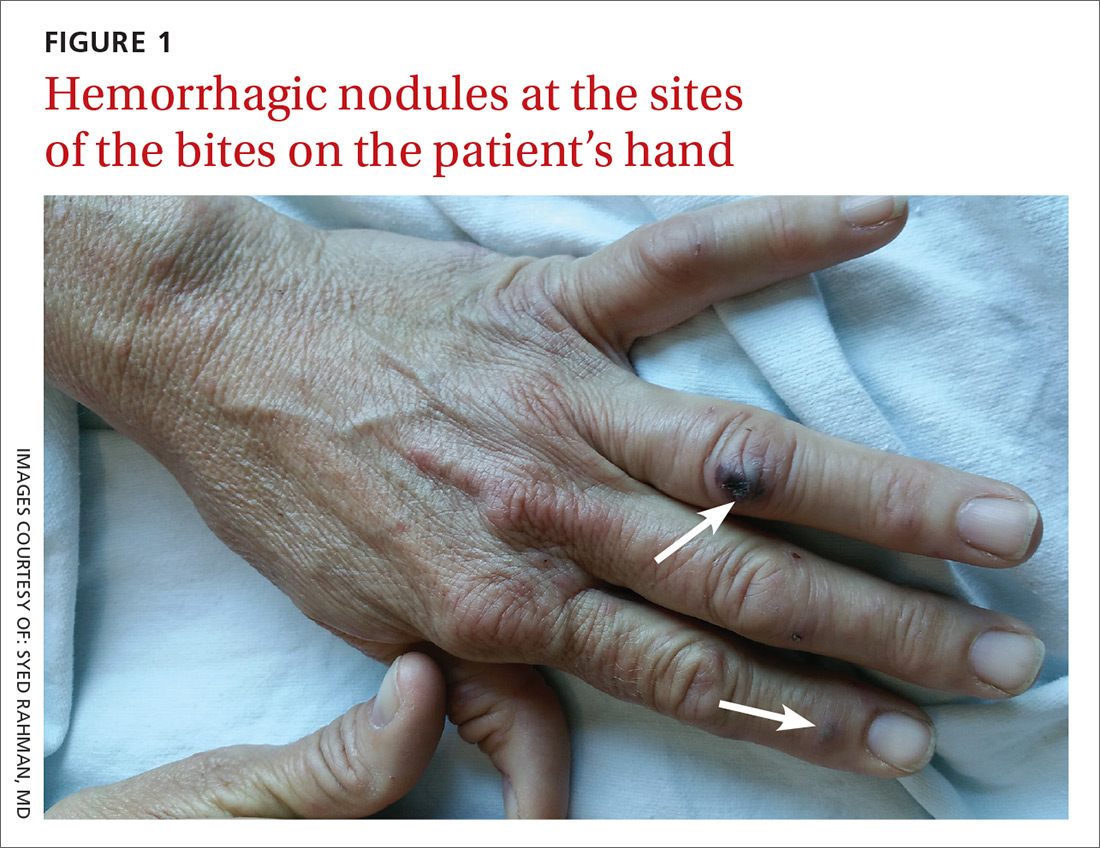
The patient had a fever of 103° F during the physical examination. She had erythematous papules and central hemorrhagic eschars at the sites of the bites (FIGURE 1). She also had nonblanching petechiae on both of her lower legs (FIGURE 2) and on the dorsal and palmar aspects of her hands.

The patient’s lab work showed mild normocytic anemia with a hemoglobin level of 11.4 g/dL (normal, 12-16 g/dL) and a platelet count of 129,000/mcL (normal, 130,000-400,000/mcL). Her white blood cell count, chemistries, brain natriuretic peptide test, and chest x-ray were normal.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Rat bite fever
Based on the patient’s symptoms, history, and lab work, we concluded that this was a case of rat bite fever. RBF is a zoonotic systemic illness caused by infection from either the gram-negative bacillus Streptobacillus moniliformis, commonly found in the United States, or the gram-negative rod Spirillum minus, commonly seen in Asia. Anyone with exposure to rats is at risk for RBF, especially pet shop employees, lab workers, and people living in areas with rat infestations.1
The rash associated with RBF can be petechial, purpuric, or maculopapular, but the presence of hemorrhagic nodules and ulcers at the site of the bite is especially indicative of the illness. The rash often involves the hands and feet, including the palms and soles.
To make the diagnosis of RBF, a careful history and a high index of suspicion are important. Fever and rigor are often the first symptoms to appear, beginning 3 to 10 days after the bite. Three to 4 days after the onset of fever, up to 75% of patients will develop a rash.2 Joint and muscle aches are also common, as is a migrating pattern of arthritis.2,3
Rule out other infections related to animal exposure
The differential diagnosis for RBF includes other animal-related infections, such as those from snake bites, leptospirosis, rabies, and pasteurellosis.
Symptoms associated with snake bite injuries appear rapidly after the bite and vary with the type of snake toxin. Hemotoxic symptoms may include intense pain, edema, petechiae, and ecchymosis from coagulopathy. Neurotoxic symptoms may include ptosis, weakness, and paresthesias. All snake bites should be treated with supportive care, and antivenin is indicated when symptoms or history indicate a bite from a venomous snake. Venomous snakes are rarely intentionally kept as pets.2
Leptospirosis is a zoonotic bacterial infection that may be spread through the urine of rats, dogs, or other mammals. Symptoms may be mild and limited to conjunctivitis, vomiting, and fever; life-threatening symptoms include hemorrhage and kidney failure. A petechial rash is not typical.4 Beta-lactam antibiotics are the treatment of choice.
Rabies is a viral infection that occurs after exposure to infected animals (most commonly raccoons, bats, skunks, and foxes). Symptoms include fever and mental status changes that can lead to death; rash is not a typical symptom. Exposed patients should receive post-exposure prophylaxis with immune globulin or a rabies vaccine.5
Pasteurellosis may also cause hemorrhagic nodules at the site of the bite or scratch, but bites are typically caused by larger animals such as dogs and livestock. Other symptoms include fever, sepsis, and osteomyelitis. Treatment includes amoxicillin-clavulanate or a fluoroquinolone-clindamycin combination.6
In cases of high suspicion, special culture tubes may be needed
Blood cultures and cerebrospinal fluid cultures are often falsely negative. Special culture tubes without polyanethol sulfonate preservative, which inhibits the growth of S moniliformis, may be required in cases of high suspicion. S moniliformis polymerase chain reaction may be available in some specialized labs.7,8
Treatment options include 7 to 10 days of antibiotic therapy with oral penicillin 500 mg 4 times daily, amoxicillin-clavulanate 875/125 mg twice daily, or oral doxycycline 100 mg every 12 hours.9
RBF may be fatal if not treated.3 Complications may include bacteremia, septicemia, meningitis, and endocarditis.
Our patient received empiric intravenous ceftriaxone 1 g every 24 hours and her fever and joint pain resolved within 48 hours. On Day 3 she was discharged home to complete a 10-day course of oral amoxicillin-clavulanate 875/125 mg. Her primary care physician reported that the rash resolved and the patient made a full recovery.
CORRESPONDENCE
Kate Rowland, MD, MS, Rush-Copley Family Medicine Residency, 2020 Ogden Ave. Suite 325, Aurora, IL 60504; krowland@rushcopley.com.
A 59-year-old woman presented to our emergency department with a rash, severe acute pain in her left hip and lower back, and dyspnea on exertion. She denied having a headache and her mental status was at baseline. The woman reported exposure to rats and snakes one week prior to presentation, and mentioned getting bitten by a rat multiple times on the back of both of her hands while feeding it to her son’s pet snake. The patient had a history of a left hip replacement, with a revision and bone graft 5 years earlier.
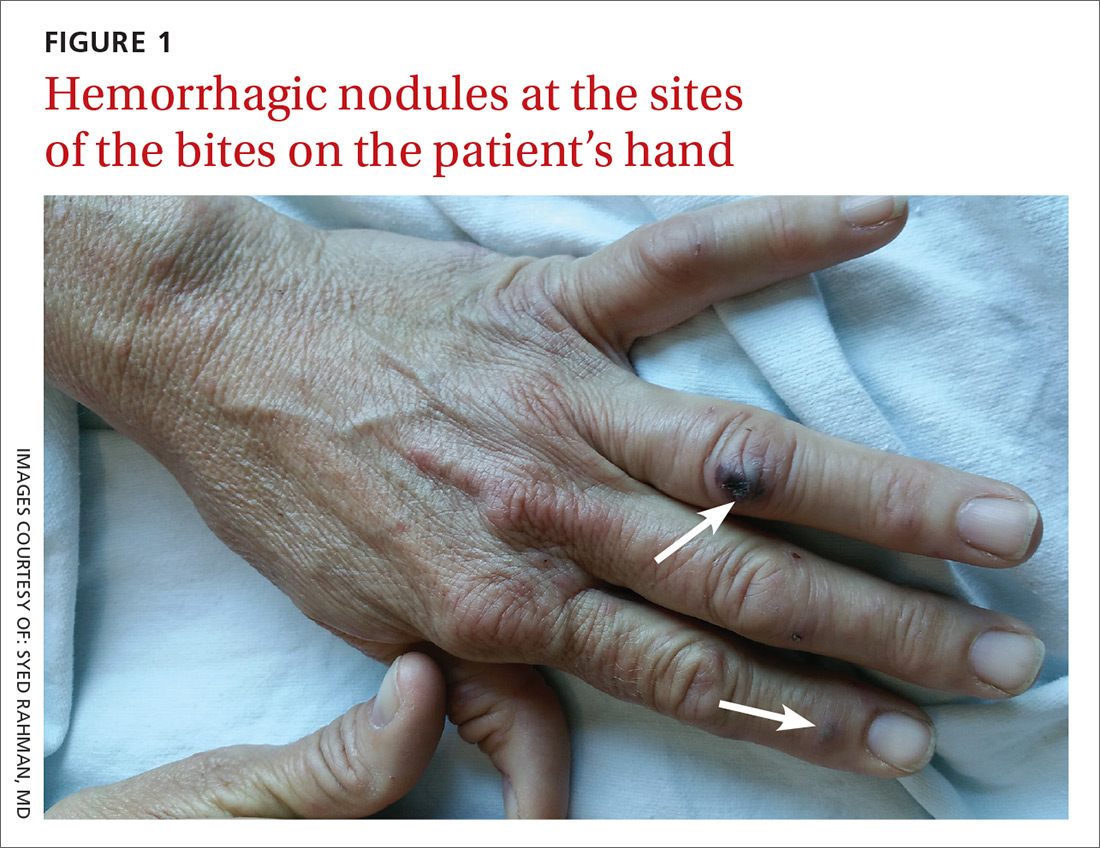
The patient had a fever of 103° F during the physical examination. She had erythematous papules and central hemorrhagic eschars at the sites of the bites (FIGURE 1). She also had nonblanching petechiae on both of her lower legs (FIGURE 2) and on the dorsal and palmar aspects of her hands.

The patient’s lab work showed mild normocytic anemia with a hemoglobin level of 11.4 g/dL (normal, 12-16 g/dL) and a platelet count of 129,000/mcL (normal, 130,000-400,000/mcL). Her white blood cell count, chemistries, brain natriuretic peptide test, and chest x-ray were normal.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Rat bite fever
Based on the patient’s symptoms, history, and lab work, we concluded that this was a case of rat bite fever. RBF is a zoonotic systemic illness caused by infection from either the gram-negative bacillus Streptobacillus moniliformis, commonly found in the United States, or the gram-negative rod Spirillum minus, commonly seen in Asia. Anyone with exposure to rats is at risk for RBF, especially pet shop employees, lab workers, and people living in areas with rat infestations.1
The rash associated with RBF can be petechial, purpuric, or maculopapular, but the presence of hemorrhagic nodules and ulcers at the site of the bite is especially indicative of the illness. The rash often involves the hands and feet, including the palms and soles.
To make the diagnosis of RBF, a careful history and a high index of suspicion are important. Fever and rigor are often the first symptoms to appear, beginning 3 to 10 days after the bite. Three to 4 days after the onset of fever, up to 75% of patients will develop a rash.2 Joint and muscle aches are also common, as is a migrating pattern of arthritis.2,3
Rule out other infections related to animal exposure
The differential diagnosis for RBF includes other animal-related infections, such as those from snake bites, leptospirosis, rabies, and pasteurellosis.
Symptoms associated with snake bite injuries appear rapidly after the bite and vary with the type of snake toxin. Hemotoxic symptoms may include intense pain, edema, petechiae, and ecchymosis from coagulopathy. Neurotoxic symptoms may include ptosis, weakness, and paresthesias. All snake bites should be treated with supportive care, and antivenin is indicated when symptoms or history indicate a bite from a venomous snake. Venomous snakes are rarely intentionally kept as pets.2
Leptospirosis is a zoonotic bacterial infection that may be spread through the urine of rats, dogs, or other mammals. Symptoms may be mild and limited to conjunctivitis, vomiting, and fever; life-threatening symptoms include hemorrhage and kidney failure. A petechial rash is not typical.4 Beta-lactam antibiotics are the treatment of choice.
Rabies is a viral infection that occurs after exposure to infected animals (most commonly raccoons, bats, skunks, and foxes). Symptoms include fever and mental status changes that can lead to death; rash is not a typical symptom. Exposed patients should receive post-exposure prophylaxis with immune globulin or a rabies vaccine.5
Pasteurellosis may also cause hemorrhagic nodules at the site of the bite or scratch, but bites are typically caused by larger animals such as dogs and livestock. Other symptoms include fever, sepsis, and osteomyelitis. Treatment includes amoxicillin-clavulanate or a fluoroquinolone-clindamycin combination.6
In cases of high suspicion, special culture tubes may be needed
Blood cultures and cerebrospinal fluid cultures are often falsely negative. Special culture tubes without polyanethol sulfonate preservative, which inhibits the growth of S moniliformis, may be required in cases of high suspicion. S moniliformis polymerase chain reaction may be available in some specialized labs.7,8
Treatment options include 7 to 10 days of antibiotic therapy with oral penicillin 500 mg 4 times daily, amoxicillin-clavulanate 875/125 mg twice daily, or oral doxycycline 100 mg every 12 hours.9
RBF may be fatal if not treated.3 Complications may include bacteremia, septicemia, meningitis, and endocarditis.
Our patient received empiric intravenous ceftriaxone 1 g every 24 hours and her fever and joint pain resolved within 48 hours. On Day 3 she was discharged home to complete a 10-day course of oral amoxicillin-clavulanate 875/125 mg. Her primary care physician reported that the rash resolved and the patient made a full recovery.
CORRESPONDENCE
Kate Rowland, MD, MS, Rush-Copley Family Medicine Residency, 2020 Ogden Ave. Suite 325, Aurora, IL 60504; krowland@rushcopley.com.
1. Centers for Disease Control and Prevention. Rat-bite fever (RBF). Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/rat-bite-fever/index.html. Accessed December 1, 2015.
2. Elliott SP. Rat bite fever and Streptobacillus moniliformis. Clin Microbiol Rev. 2007;20:13-22.
3. Juckett G, Hancox JG. Venomous snakebites in the United States: management review and update. Am Fam Physician. 2002;65:1367-1374.
4. Rabinowitz PM, Gordon Z, Odofin L. Pet-related infections. Am Fam Physician. 2007;76:1314-1322.
5. Fishbein DB, Robinson LE. Rabies. N Engl J Med. 1993;329:1632-1638.
6. Wilson BA, Ho M. Pasteurella multocida: from zoonosis to cellular microbiology. Clin Microbiol Rev. 2013;26:631-655.
7. Eng J. Effect of sodium polyanethol sulfonate in blood cultures. J Clin Microbiol. 1975;1:119-123.
8. Nakagomi D, Deguchi N, Yagasaki A, et al. Rat-bite fever identified by polymerase chain reaction detection of Streptobacillus moniliformis DNA. J Dermatol. 2008;35:667-670.
9. Bush LM, Perez MT. Rat-bite fever. In: The Merck Manual of Diagnosis and Therapy. Whitehouse Station, NJ: Merck Sharp & Dohme Corp.; 2011.
1. Centers for Disease Control and Prevention. Rat-bite fever (RBF). Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/rat-bite-fever/index.html. Accessed December 1, 2015.
2. Elliott SP. Rat bite fever and Streptobacillus moniliformis. Clin Microbiol Rev. 2007;20:13-22.
3. Juckett G, Hancox JG. Venomous snakebites in the United States: management review and update. Am Fam Physician. 2002;65:1367-1374.
4. Rabinowitz PM, Gordon Z, Odofin L. Pet-related infections. Am Fam Physician. 2007;76:1314-1322.
5. Fishbein DB, Robinson LE. Rabies. N Engl J Med. 1993;329:1632-1638.
6. Wilson BA, Ho M. Pasteurella multocida: from zoonosis to cellular microbiology. Clin Microbiol Rev. 2013;26:631-655.
7. Eng J. Effect of sodium polyanethol sulfonate in blood cultures. J Clin Microbiol. 1975;1:119-123.
8. Nakagomi D, Deguchi N, Yagasaki A, et al. Rat-bite fever identified by polymerase chain reaction detection of Streptobacillus moniliformis DNA. J Dermatol. 2008;35:667-670.
9. Bush LM, Perez MT. Rat-bite fever. In: The Merck Manual of Diagnosis and Therapy. Whitehouse Station, NJ: Merck Sharp & Dohme Corp.; 2011.
