User login
Case Report: Sudden Chest Pain Following an Asthma Attack
Case
A 20-year-old woman with a history of asthma and cigarette smoking presented to the ED twice within the same week. At the initial presentation, the patient stated that she had been experiencing symptoms of an upper respiratory infection over the past 4 days which had progressed to difficulty breathing. She further noted that these symptoms were also consistent with childhood asthma exacerbations. In addition to childhood asthma, the patient’s medical history included chronic dermatitis, for which she had been taking oral doxycycline daily.
The patient was treated with intravenous (IV) corticosteroids and an albuterol/atrovent nebulizer. Based on significant response to treatment and improvement, she was discharged on a 5-day steroid burst and albuterol meter-dose inhaler. She was also counseled to continue taking doxycycline daily for the chronic dermatitis.
Two days after discharge, the patient returned to the ED with episodes of coughing followed by worsening shortness of breath and sharp chest pain that radiated into her neck and back, which she described as unbearable. Neither the pain nor shortness of breath responded to albuterol.
The patient’s vital signs at this second presentation were: blood pressure, 144/88 mm Hg; heart rate, 98 beats/minute; respiratory rate, 28 breaths/minute; and temperature, 97.8˚ F. Oxygen (O2) saturation was 94% on room air. On physical examination, the patient was uncomfortable and in mild distress. She was visibly tachypneic with diminished breath sounds, but no wheezing, rales, or rhonchi were appreciated on auscultation. Cardiac auscultation was likewise normal. The patient had a visceral sense of pain on palpation of her anterior chest wall, but no crepitus was appreciated. Both an electrocardiogram and chest X-ray (CXR) were normal, but laboratory evaluation revealed a white blood cell count of 18.4 u/L (4.0-11.0).
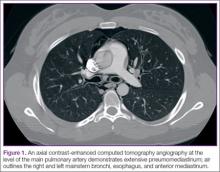
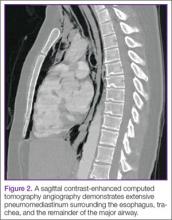
An assessment based on Well’s criteria showed the patient to be at a moderate risk for pulmonary embolism (PE), and a computed tomography angiography (CTA) of the chest was obtained. The CTA was negative for PE but showed significant pneumomediastinum (Figures 1 and 2). Upon repeat examination, crepitus was palpated on the anterior right neck, correlating with the CTA findings.
The patient was admitted to the inpatient ward for observation and continued support, and she was given IV analgesics and supplemental O2 via nasal cannula. Due to the considerable amount of air surrounding her heart, she was considered at high-risk for disease progression. Since she had been on continuous doxycycline therapy, the inpatient team performed a gastrografin swallow study to rule out esophageal perforation. The results of this test were negative, further supporting asthma exacerbation as the etiology for the pneumomediastinum. As cigarette smoking was a contributing risk factor, she was also counseled on tobacco cessation.
During her inpatient stay, the patient completed the 5-day course of oral corticosteroids that had been prescribed at her first ED visit, and was weaned-off supplemental O2. After an uncomplicated clinical course and full resolution of symptoms, she was discharged on hospital day 3 with an albuterol hydrofluoroalkane inhaler to be used as needed; she was also advised to continue taking doxycycline as prescribed for her dermatologic condition. The patient was followed in the outpatient setting on a routine basis; to date, she has remained asymptomatic with no sequelae.
Pneumomediastinum
Also referred to as mediastinal emphysema, pneumomediastinum manifests as free air surrounding the mediastinal structures.1-7 This condition most commonly occurs in middle-aged men; though rare, 25% of all cases have been linked to existing pulmonary disease.1,6,8,9 Patients with pneumomediastinum typically present with pleuritic chest pain (often radiating to the neck and back), dyspnea, dysphonia, and dysphagia.1,2,5,7-9
Risk Factors
Pneumomediastinum is usually associated with asthma exacerbations; however, it has also been linked to increases in intrathoracic pressure, extension of subcutaneous emphysema from superior structures (eg, cervical region), esophageal lesions, as well as use and/or withdrawal symptoms of certain drugs (eg, cocaine).1,2,4,6,8
When considering primary pulmonary disease, the pathophysiological process is driven by a pressure gradient between the pulmonary interstitium and the alveoli. The force transference causes alveolar rupture, allowing air to escape into the interstitium.9 In asthma, obstruction in the minor airways leads to air-trapping and barotrauma of distal airways, resulting in the aforementioned alveolar rupture.2 Once in the lung interstitium, the free air flows along the pressure gradient through the hilum from the pulmonary parenchyma in a centripetal direction before entering the mediastinum (Macklin effect).2,9
Pneumomediastinum is not exclusive to asthma and subsequent alveolar barotrauma. There are reported instances of gas-producing microorganisms within the mediastinum as well as perforated mucosal structures—specifically the esophagus (of which doxycycline is a risk factor) and tracheobronchial tree, which have also manifested as mediastinal emphysema.6,9
One of the most life-threatening causes of pneumomediastinum is Boerhaave syndrome in which there is a spontaneous rupture of the esophagus.3 In addition, as previously mentioned, numerous illicit drugs (eg, cocaine, marijuana, ecstasy) have been implicated in pneumomediastinum—with cocaine posing the greatest risk.8,9 Perna et al8 relate cocaine-related pneumomediastinum to the direct toxic effects of the drug on the lung parenchyma in the acute phases of use and not due to pressure variations resulting from the Valsalva maneuver necessary to inhale the drug.
Predisposing risk factors for mediastinal emphysema include preexisting pulmonary disease (eg, chronic obstructive pulmonary disease, asthma) and a history of smoking.5,6,8,9 Precipitating risks include recent exercise, significant upper respiratory infection, forceful straining (eg, cough, emesis, childbirth), and diabetic ketoacidosis.6,8,9 Unlikely sources that have also been implicated are those related to surgical procedures, such as arthroscopy, adenotonsillectomy, instrumentation, and recreational activities (eg, scuba diving, playing wind instruments).3,6
Diagnosis
The diagnosis is often made clinically and confirmed radiographically.2,7 Physical examination findings vary by the extent of the mediastinal emphysema. Common findings include the Hamman sign, which has been described as classic “crunching, crackling, bubbling, and rasping sounds synchronous with peak heart beat” on auscultation.2,5,8 Air from the mediastinum may dissect into the skin, particularly in the superior structures of the neck and face, resulting in a subcutaneous emphysema described as a palpable crunching sound.2
Imaging
Obtaining a plain CXR is an acceptable standard of practice. Pneumomediastinum has been described as either a “classic hyperlucency” or, as Chiu et al5 have described, as “lucent streaks or bubbles of gas that outline mediastinal structures” on a posteroanterior and lateral film, implying damage to luminal structures of the intrathoracic cavity.2,4,5,7,9 This lucency has been further described as an outline of the inner pleura of mediastinal structures, which is a defined crease lateral to the pulmonary artery and arch of the aorta along the cardiac border (best visualized on a lateral view image).5,7 A scant amount of air, however, may not be visualized on a plain film.2,4,5,9 Therefore, the literature supports a thoracic CT as the gold standard for its greater sensitivity in visualizing a small pneumomediastinum.2,9
Treatment
Since pneumomediastinum is typically a self-limited disease, treatment is often conservative management with specific consideration to the patient’s age, severity of symptoms, underlying cause, and comorbidities.2,10 Treatment should include rest, supplemental O2, and analgesia.5,7,9 Hospitalization for an observation period of 2 to 5 days is recommended, with one study reporting an average length of stay as 3 days or until resolution of symptoms.8,9
Disposition is best determined by the patient’s clinical course; however, the risk of progression warrants observation for serial follow-up examinations and possibly repeat imaging as well as access to acute intervention, if required. Though rare, several serious comorbid conditions have been reported, including hypertensive episodes, bilateral pneumothoraxes, and even cardiac compression (or tension pneumomediastinum) limiting cardiac output and leading to cardiac arrest.2,4 Following discharge, there has been no clinical study reporting recurrence of pneumomediastinum; therefore, close clinical follow-up is not necessarily indicated.4,9
Conclusion
Pneumomediastinum is a rare complication of acute and chronic pulmonary and extrapulmonary diseases. As seen in this case presentation, the condition is typically associated with asthma exacerbations. Patients often present with chest pain, dyspnea, dysphonia, and dysphagia. Although diagnosis may be confirmed using plain CRX, CTA is the preferred modality due to its higher sensitivity in visualizing mild pneumomediastinum. While the risk of mortality is present, the condition generally follows a stable clinical course with minimal risk of long-term morbidity.
Major Howell is a physician assistant, department of emergency medicine, Wright-Patterson Medical Center, Wright-Patterson Air Force Base, Ohio. Captain Pennington is an emergency medicine physician, department of emergency medicine, Wright-Patterson Medical Center, Wright-Patterson Air Force Base, Ohio.
Acknowledgement:The authors wish to extend special thanks to Dr Nurani Kester, department of emergency medicine, San Antonio Military Medical Center, Fort Sam Houston, Texas; and to Dr Luke Simonet, department of radiology, David Grant United States Air Force Medical Center, Travis Air Force Base, California.
Disclosure: The authors report no conflicts of interest.
- Dajer-Fadel WL, Argüero-Sanchez R, Ibarra-Pérez C, Navarro-Reynoso F. Systemic review of spontaneous pneumomediastinium: a survey of 22 years’ data. Asian Cardiovasc Thorac Ann. 2014;22(8):997-1002.
- Karakaya Z, Demir S, Sagay SS, Karakaya O, Ozdinç S. Bilateral spontaneous pneumothorax, pneumomediastinum, and subcutaenous emphyesema: rare and fatal complications of asthma. Case Rep Emerg Med. 2012;2012:242579.
- Kogan I, Celli B. Pneumomediastinum in a 63-year-old woman with asthma exacerbation. Chest. 2000;117(6):1778-1781.
- Momin AU, Chung DA, John LC. Childhood asthma predisposes to spontaneous pneumomediastinum. Emerg Med J. 2004;21(5):630-631.
- Chiu CY, Wong KS, Yao TC, Huang JL. Asthmatic versus non-asthmatic spontaneous pneumomediastinum in children. Asian Pac J Allergy Immunol. 2005;23(1):19-22.
- Akinyemi R, Ogah O, Akisanya C, et al. Pneumomediastinum and subcutaneous emphysema complicating acute exacerbation of bronchial asthma. Ann Ib Postgrad Med. 2007:5(2):78-79.
- Firinci F, Ozgürler F, Doğan M, Koçyigit A, Mete E. Spontaneous pneumomediastinum in childhood: report of an adolescent case diagnose with asthma. Tuberk Toraks. 2014;62(3):253-254.
- Perna V, Vilá E, Guelbenzu J, Amat, I. Penumomediastinum: is this really a benign entity? When it can be considered as spontaenous? Our experience in 47 adult patients? Eur J Cardiothorac Surg. 2010;37(3):573-575.
- Macia I, Moya J, Ramos R, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg. 2007;31(6):1110-1114.
- Mahajan P, AI Maslamani NJ, Purayil, NK. Rare case of pneumorrhachis, pneumomediastinum, pneumothorax, and surgical emphysema secondary to bronchial asthma. Int Med Case Rep J. 2014;7:35-39.
Case
A 20-year-old woman with a history of asthma and cigarette smoking presented to the ED twice within the same week. At the initial presentation, the patient stated that she had been experiencing symptoms of an upper respiratory infection over the past 4 days which had progressed to difficulty breathing. She further noted that these symptoms were also consistent with childhood asthma exacerbations. In addition to childhood asthma, the patient’s medical history included chronic dermatitis, for which she had been taking oral doxycycline daily.
The patient was treated with intravenous (IV) corticosteroids and an albuterol/atrovent nebulizer. Based on significant response to treatment and improvement, she was discharged on a 5-day steroid burst and albuterol meter-dose inhaler. She was also counseled to continue taking doxycycline daily for the chronic dermatitis.
Two days after discharge, the patient returned to the ED with episodes of coughing followed by worsening shortness of breath and sharp chest pain that radiated into her neck and back, which she described as unbearable. Neither the pain nor shortness of breath responded to albuterol.
The patient’s vital signs at this second presentation were: blood pressure, 144/88 mm Hg; heart rate, 98 beats/minute; respiratory rate, 28 breaths/minute; and temperature, 97.8˚ F. Oxygen (O2) saturation was 94% on room air. On physical examination, the patient was uncomfortable and in mild distress. She was visibly tachypneic with diminished breath sounds, but no wheezing, rales, or rhonchi were appreciated on auscultation. Cardiac auscultation was likewise normal. The patient had a visceral sense of pain on palpation of her anterior chest wall, but no crepitus was appreciated. Both an electrocardiogram and chest X-ray (CXR) were normal, but laboratory evaluation revealed a white blood cell count of 18.4 u/L (4.0-11.0).
An assessment based on Well’s criteria showed the patient to be at a moderate risk for pulmonary embolism (PE), and a computed tomography angiography (CTA) of the chest was obtained. The CTA was negative for PE but showed significant pneumomediastinum (Figures 1 and 2). Upon repeat examination, crepitus was palpated on the anterior right neck, correlating with the CTA findings.
The patient was admitted to the inpatient ward for observation and continued support, and she was given IV analgesics and supplemental O2 via nasal cannula. Due to the considerable amount of air surrounding her heart, she was considered at high-risk for disease progression. Since she had been on continuous doxycycline therapy, the inpatient team performed a gastrografin swallow study to rule out esophageal perforation. The results of this test were negative, further supporting asthma exacerbation as the etiology for the pneumomediastinum. As cigarette smoking was a contributing risk factor, she was also counseled on tobacco cessation.
During her inpatient stay, the patient completed the 5-day course of oral corticosteroids that had been prescribed at her first ED visit, and was weaned-off supplemental O2. After an uncomplicated clinical course and full resolution of symptoms, she was discharged on hospital day 3 with an albuterol hydrofluoroalkane inhaler to be used as needed; she was also advised to continue taking doxycycline as prescribed for her dermatologic condition. The patient was followed in the outpatient setting on a routine basis; to date, she has remained asymptomatic with no sequelae.
Pneumomediastinum
Also referred to as mediastinal emphysema, pneumomediastinum manifests as free air surrounding the mediastinal structures.1-7 This condition most commonly occurs in middle-aged men; though rare, 25% of all cases have been linked to existing pulmonary disease.1,6,8,9 Patients with pneumomediastinum typically present with pleuritic chest pain (often radiating to the neck and back), dyspnea, dysphonia, and dysphagia.1,2,5,7-9
Risk Factors
Pneumomediastinum is usually associated with asthma exacerbations; however, it has also been linked to increases in intrathoracic pressure, extension of subcutaneous emphysema from superior structures (eg, cervical region), esophageal lesions, as well as use and/or withdrawal symptoms of certain drugs (eg, cocaine).1,2,4,6,8
When considering primary pulmonary disease, the pathophysiological process is driven by a pressure gradient between the pulmonary interstitium and the alveoli. The force transference causes alveolar rupture, allowing air to escape into the interstitium.9 In asthma, obstruction in the minor airways leads to air-trapping and barotrauma of distal airways, resulting in the aforementioned alveolar rupture.2 Once in the lung interstitium, the free air flows along the pressure gradient through the hilum from the pulmonary parenchyma in a centripetal direction before entering the mediastinum (Macklin effect).2,9
Pneumomediastinum is not exclusive to asthma and subsequent alveolar barotrauma. There are reported instances of gas-producing microorganisms within the mediastinum as well as perforated mucosal structures—specifically the esophagus (of which doxycycline is a risk factor) and tracheobronchial tree, which have also manifested as mediastinal emphysema.6,9
One of the most life-threatening causes of pneumomediastinum is Boerhaave syndrome in which there is a spontaneous rupture of the esophagus.3 In addition, as previously mentioned, numerous illicit drugs (eg, cocaine, marijuana, ecstasy) have been implicated in pneumomediastinum—with cocaine posing the greatest risk.8,9 Perna et al8 relate cocaine-related pneumomediastinum to the direct toxic effects of the drug on the lung parenchyma in the acute phases of use and not due to pressure variations resulting from the Valsalva maneuver necessary to inhale the drug.
Predisposing risk factors for mediastinal emphysema include preexisting pulmonary disease (eg, chronic obstructive pulmonary disease, asthma) and a history of smoking.5,6,8,9 Precipitating risks include recent exercise, significant upper respiratory infection, forceful straining (eg, cough, emesis, childbirth), and diabetic ketoacidosis.6,8,9 Unlikely sources that have also been implicated are those related to surgical procedures, such as arthroscopy, adenotonsillectomy, instrumentation, and recreational activities (eg, scuba diving, playing wind instruments).3,6
Diagnosis
The diagnosis is often made clinically and confirmed radiographically.2,7 Physical examination findings vary by the extent of the mediastinal emphysema. Common findings include the Hamman sign, which has been described as classic “crunching, crackling, bubbling, and rasping sounds synchronous with peak heart beat” on auscultation.2,5,8 Air from the mediastinum may dissect into the skin, particularly in the superior structures of the neck and face, resulting in a subcutaneous emphysema described as a palpable crunching sound.2
Imaging
Obtaining a plain CXR is an acceptable standard of practice. Pneumomediastinum has been described as either a “classic hyperlucency” or, as Chiu et al5 have described, as “lucent streaks or bubbles of gas that outline mediastinal structures” on a posteroanterior and lateral film, implying damage to luminal structures of the intrathoracic cavity.2,4,5,7,9 This lucency has been further described as an outline of the inner pleura of mediastinal structures, which is a defined crease lateral to the pulmonary artery and arch of the aorta along the cardiac border (best visualized on a lateral view image).5,7 A scant amount of air, however, may not be visualized on a plain film.2,4,5,9 Therefore, the literature supports a thoracic CT as the gold standard for its greater sensitivity in visualizing a small pneumomediastinum.2,9
Treatment
Since pneumomediastinum is typically a self-limited disease, treatment is often conservative management with specific consideration to the patient’s age, severity of symptoms, underlying cause, and comorbidities.2,10 Treatment should include rest, supplemental O2, and analgesia.5,7,9 Hospitalization for an observation period of 2 to 5 days is recommended, with one study reporting an average length of stay as 3 days or until resolution of symptoms.8,9
Disposition is best determined by the patient’s clinical course; however, the risk of progression warrants observation for serial follow-up examinations and possibly repeat imaging as well as access to acute intervention, if required. Though rare, several serious comorbid conditions have been reported, including hypertensive episodes, bilateral pneumothoraxes, and even cardiac compression (or tension pneumomediastinum) limiting cardiac output and leading to cardiac arrest.2,4 Following discharge, there has been no clinical study reporting recurrence of pneumomediastinum; therefore, close clinical follow-up is not necessarily indicated.4,9
Conclusion
Pneumomediastinum is a rare complication of acute and chronic pulmonary and extrapulmonary diseases. As seen in this case presentation, the condition is typically associated with asthma exacerbations. Patients often present with chest pain, dyspnea, dysphonia, and dysphagia. Although diagnosis may be confirmed using plain CRX, CTA is the preferred modality due to its higher sensitivity in visualizing mild pneumomediastinum. While the risk of mortality is present, the condition generally follows a stable clinical course with minimal risk of long-term morbidity.
Major Howell is a physician assistant, department of emergency medicine, Wright-Patterson Medical Center, Wright-Patterson Air Force Base, Ohio. Captain Pennington is an emergency medicine physician, department of emergency medicine, Wright-Patterson Medical Center, Wright-Patterson Air Force Base, Ohio.
Acknowledgement:The authors wish to extend special thanks to Dr Nurani Kester, department of emergency medicine, San Antonio Military Medical Center, Fort Sam Houston, Texas; and to Dr Luke Simonet, department of radiology, David Grant United States Air Force Medical Center, Travis Air Force Base, California.
Disclosure: The authors report no conflicts of interest.
Case
A 20-year-old woman with a history of asthma and cigarette smoking presented to the ED twice within the same week. At the initial presentation, the patient stated that she had been experiencing symptoms of an upper respiratory infection over the past 4 days which had progressed to difficulty breathing. She further noted that these symptoms were also consistent with childhood asthma exacerbations. In addition to childhood asthma, the patient’s medical history included chronic dermatitis, for which she had been taking oral doxycycline daily.
The patient was treated with intravenous (IV) corticosteroids and an albuterol/atrovent nebulizer. Based on significant response to treatment and improvement, she was discharged on a 5-day steroid burst and albuterol meter-dose inhaler. She was also counseled to continue taking doxycycline daily for the chronic dermatitis.
Two days after discharge, the patient returned to the ED with episodes of coughing followed by worsening shortness of breath and sharp chest pain that radiated into her neck and back, which she described as unbearable. Neither the pain nor shortness of breath responded to albuterol.
The patient’s vital signs at this second presentation were: blood pressure, 144/88 mm Hg; heart rate, 98 beats/minute; respiratory rate, 28 breaths/minute; and temperature, 97.8˚ F. Oxygen (O2) saturation was 94% on room air. On physical examination, the patient was uncomfortable and in mild distress. She was visibly tachypneic with diminished breath sounds, but no wheezing, rales, or rhonchi were appreciated on auscultation. Cardiac auscultation was likewise normal. The patient had a visceral sense of pain on palpation of her anterior chest wall, but no crepitus was appreciated. Both an electrocardiogram and chest X-ray (CXR) were normal, but laboratory evaluation revealed a white blood cell count of 18.4 u/L (4.0-11.0).
An assessment based on Well’s criteria showed the patient to be at a moderate risk for pulmonary embolism (PE), and a computed tomography angiography (CTA) of the chest was obtained. The CTA was negative for PE but showed significant pneumomediastinum (Figures 1 and 2). Upon repeat examination, crepitus was palpated on the anterior right neck, correlating with the CTA findings.
The patient was admitted to the inpatient ward for observation and continued support, and she was given IV analgesics and supplemental O2 via nasal cannula. Due to the considerable amount of air surrounding her heart, she was considered at high-risk for disease progression. Since she had been on continuous doxycycline therapy, the inpatient team performed a gastrografin swallow study to rule out esophageal perforation. The results of this test were negative, further supporting asthma exacerbation as the etiology for the pneumomediastinum. As cigarette smoking was a contributing risk factor, she was also counseled on tobacco cessation.
During her inpatient stay, the patient completed the 5-day course of oral corticosteroids that had been prescribed at her first ED visit, and was weaned-off supplemental O2. After an uncomplicated clinical course and full resolution of symptoms, she was discharged on hospital day 3 with an albuterol hydrofluoroalkane inhaler to be used as needed; she was also advised to continue taking doxycycline as prescribed for her dermatologic condition. The patient was followed in the outpatient setting on a routine basis; to date, she has remained asymptomatic with no sequelae.
Pneumomediastinum
Also referred to as mediastinal emphysema, pneumomediastinum manifests as free air surrounding the mediastinal structures.1-7 This condition most commonly occurs in middle-aged men; though rare, 25% of all cases have been linked to existing pulmonary disease.1,6,8,9 Patients with pneumomediastinum typically present with pleuritic chest pain (often radiating to the neck and back), dyspnea, dysphonia, and dysphagia.1,2,5,7-9
Risk Factors
Pneumomediastinum is usually associated with asthma exacerbations; however, it has also been linked to increases in intrathoracic pressure, extension of subcutaneous emphysema from superior structures (eg, cervical region), esophageal lesions, as well as use and/or withdrawal symptoms of certain drugs (eg, cocaine).1,2,4,6,8
When considering primary pulmonary disease, the pathophysiological process is driven by a pressure gradient between the pulmonary interstitium and the alveoli. The force transference causes alveolar rupture, allowing air to escape into the interstitium.9 In asthma, obstruction in the minor airways leads to air-trapping and barotrauma of distal airways, resulting in the aforementioned alveolar rupture.2 Once in the lung interstitium, the free air flows along the pressure gradient through the hilum from the pulmonary parenchyma in a centripetal direction before entering the mediastinum (Macklin effect).2,9
Pneumomediastinum is not exclusive to asthma and subsequent alveolar barotrauma. There are reported instances of gas-producing microorganisms within the mediastinum as well as perforated mucosal structures—specifically the esophagus (of which doxycycline is a risk factor) and tracheobronchial tree, which have also manifested as mediastinal emphysema.6,9
One of the most life-threatening causes of pneumomediastinum is Boerhaave syndrome in which there is a spontaneous rupture of the esophagus.3 In addition, as previously mentioned, numerous illicit drugs (eg, cocaine, marijuana, ecstasy) have been implicated in pneumomediastinum—with cocaine posing the greatest risk.8,9 Perna et al8 relate cocaine-related pneumomediastinum to the direct toxic effects of the drug on the lung parenchyma in the acute phases of use and not due to pressure variations resulting from the Valsalva maneuver necessary to inhale the drug.
Predisposing risk factors for mediastinal emphysema include preexisting pulmonary disease (eg, chronic obstructive pulmonary disease, asthma) and a history of smoking.5,6,8,9 Precipitating risks include recent exercise, significant upper respiratory infection, forceful straining (eg, cough, emesis, childbirth), and diabetic ketoacidosis.6,8,9 Unlikely sources that have also been implicated are those related to surgical procedures, such as arthroscopy, adenotonsillectomy, instrumentation, and recreational activities (eg, scuba diving, playing wind instruments).3,6
Diagnosis
The diagnosis is often made clinically and confirmed radiographically.2,7 Physical examination findings vary by the extent of the mediastinal emphysema. Common findings include the Hamman sign, which has been described as classic “crunching, crackling, bubbling, and rasping sounds synchronous with peak heart beat” on auscultation.2,5,8 Air from the mediastinum may dissect into the skin, particularly in the superior structures of the neck and face, resulting in a subcutaneous emphysema described as a palpable crunching sound.2
Imaging
Obtaining a plain CXR is an acceptable standard of practice. Pneumomediastinum has been described as either a “classic hyperlucency” or, as Chiu et al5 have described, as “lucent streaks or bubbles of gas that outline mediastinal structures” on a posteroanterior and lateral film, implying damage to luminal structures of the intrathoracic cavity.2,4,5,7,9 This lucency has been further described as an outline of the inner pleura of mediastinal structures, which is a defined crease lateral to the pulmonary artery and arch of the aorta along the cardiac border (best visualized on a lateral view image).5,7 A scant amount of air, however, may not be visualized on a plain film.2,4,5,9 Therefore, the literature supports a thoracic CT as the gold standard for its greater sensitivity in visualizing a small pneumomediastinum.2,9
Treatment
Since pneumomediastinum is typically a self-limited disease, treatment is often conservative management with specific consideration to the patient’s age, severity of symptoms, underlying cause, and comorbidities.2,10 Treatment should include rest, supplemental O2, and analgesia.5,7,9 Hospitalization for an observation period of 2 to 5 days is recommended, with one study reporting an average length of stay as 3 days or until resolution of symptoms.8,9
Disposition is best determined by the patient’s clinical course; however, the risk of progression warrants observation for serial follow-up examinations and possibly repeat imaging as well as access to acute intervention, if required. Though rare, several serious comorbid conditions have been reported, including hypertensive episodes, bilateral pneumothoraxes, and even cardiac compression (or tension pneumomediastinum) limiting cardiac output and leading to cardiac arrest.2,4 Following discharge, there has been no clinical study reporting recurrence of pneumomediastinum; therefore, close clinical follow-up is not necessarily indicated.4,9
Conclusion
Pneumomediastinum is a rare complication of acute and chronic pulmonary and extrapulmonary diseases. As seen in this case presentation, the condition is typically associated with asthma exacerbations. Patients often present with chest pain, dyspnea, dysphonia, and dysphagia. Although diagnosis may be confirmed using plain CRX, CTA is the preferred modality due to its higher sensitivity in visualizing mild pneumomediastinum. While the risk of mortality is present, the condition generally follows a stable clinical course with minimal risk of long-term morbidity.
Major Howell is a physician assistant, department of emergency medicine, Wright-Patterson Medical Center, Wright-Patterson Air Force Base, Ohio. Captain Pennington is an emergency medicine physician, department of emergency medicine, Wright-Patterson Medical Center, Wright-Patterson Air Force Base, Ohio.
Acknowledgement:The authors wish to extend special thanks to Dr Nurani Kester, department of emergency medicine, San Antonio Military Medical Center, Fort Sam Houston, Texas; and to Dr Luke Simonet, department of radiology, David Grant United States Air Force Medical Center, Travis Air Force Base, California.
Disclosure: The authors report no conflicts of interest.
- Dajer-Fadel WL, Argüero-Sanchez R, Ibarra-Pérez C, Navarro-Reynoso F. Systemic review of spontaneous pneumomediastinium: a survey of 22 years’ data. Asian Cardiovasc Thorac Ann. 2014;22(8):997-1002.
- Karakaya Z, Demir S, Sagay SS, Karakaya O, Ozdinç S. Bilateral spontaneous pneumothorax, pneumomediastinum, and subcutaenous emphyesema: rare and fatal complications of asthma. Case Rep Emerg Med. 2012;2012:242579.
- Kogan I, Celli B. Pneumomediastinum in a 63-year-old woman with asthma exacerbation. Chest. 2000;117(6):1778-1781.
- Momin AU, Chung DA, John LC. Childhood asthma predisposes to spontaneous pneumomediastinum. Emerg Med J. 2004;21(5):630-631.
- Chiu CY, Wong KS, Yao TC, Huang JL. Asthmatic versus non-asthmatic spontaneous pneumomediastinum in children. Asian Pac J Allergy Immunol. 2005;23(1):19-22.
- Akinyemi R, Ogah O, Akisanya C, et al. Pneumomediastinum and subcutaneous emphysema complicating acute exacerbation of bronchial asthma. Ann Ib Postgrad Med. 2007:5(2):78-79.
- Firinci F, Ozgürler F, Doğan M, Koçyigit A, Mete E. Spontaneous pneumomediastinum in childhood: report of an adolescent case diagnose with asthma. Tuberk Toraks. 2014;62(3):253-254.
- Perna V, Vilá E, Guelbenzu J, Amat, I. Penumomediastinum: is this really a benign entity? When it can be considered as spontaenous? Our experience in 47 adult patients? Eur J Cardiothorac Surg. 2010;37(3):573-575.
- Macia I, Moya J, Ramos R, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg. 2007;31(6):1110-1114.
- Mahajan P, AI Maslamani NJ, Purayil, NK. Rare case of pneumorrhachis, pneumomediastinum, pneumothorax, and surgical emphysema secondary to bronchial asthma. Int Med Case Rep J. 2014;7:35-39.
- Dajer-Fadel WL, Argüero-Sanchez R, Ibarra-Pérez C, Navarro-Reynoso F. Systemic review of spontaneous pneumomediastinium: a survey of 22 years’ data. Asian Cardiovasc Thorac Ann. 2014;22(8):997-1002.
- Karakaya Z, Demir S, Sagay SS, Karakaya O, Ozdinç S. Bilateral spontaneous pneumothorax, pneumomediastinum, and subcutaenous emphyesema: rare and fatal complications of asthma. Case Rep Emerg Med. 2012;2012:242579.
- Kogan I, Celli B. Pneumomediastinum in a 63-year-old woman with asthma exacerbation. Chest. 2000;117(6):1778-1781.
- Momin AU, Chung DA, John LC. Childhood asthma predisposes to spontaneous pneumomediastinum. Emerg Med J. 2004;21(5):630-631.
- Chiu CY, Wong KS, Yao TC, Huang JL. Asthmatic versus non-asthmatic spontaneous pneumomediastinum in children. Asian Pac J Allergy Immunol. 2005;23(1):19-22.
- Akinyemi R, Ogah O, Akisanya C, et al. Pneumomediastinum and subcutaneous emphysema complicating acute exacerbation of bronchial asthma. Ann Ib Postgrad Med. 2007:5(2):78-79.
- Firinci F, Ozgürler F, Doğan M, Koçyigit A, Mete E. Spontaneous pneumomediastinum in childhood: report of an adolescent case diagnose with asthma. Tuberk Toraks. 2014;62(3):253-254.
- Perna V, Vilá E, Guelbenzu J, Amat, I. Penumomediastinum: is this really a benign entity? When it can be considered as spontaenous? Our experience in 47 adult patients? Eur J Cardiothorac Surg. 2010;37(3):573-575.
- Macia I, Moya J, Ramos R, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg. 2007;31(6):1110-1114.
- Mahajan P, AI Maslamani NJ, Purayil, NK. Rare case of pneumorrhachis, pneumomediastinum, pneumothorax, and surgical emphysema secondary to bronchial asthma. Int Med Case Rep J. 2014;7:35-39.