User login
A 32-year-old woman came to the rescue mission clinic with her 2 sons because she had red eyes and a runny nose. Her sons both had symptoms highly suggestive of viral upper respiratory infection. They lived in a homeless shelter.
The patient stated she did not use contact lenses or have any eye trauma, itching, photophobia, loss or change of vision, eye pain, eye discharge, or previous episodes of pinkeye. She had no other medical problems or history of allergies.
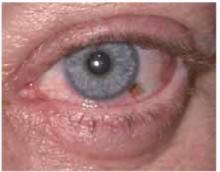
On physical exam, her vital signs were normal. She had conjunctival injection, without purulent discharge or limbal blush (Figures 1 and 2). Eyelids were mildly erythematous with no cobble-stoning. Pupils were equal, round, and reactive to light. The anterior chamber by flashlight exam from the side did not show a narrow angle. Visual acuity was normal by Snellen exam. She had clear nasal discharge and bilateral preauricular lymphadenopathy.
In addition, she had a brown macule under the left iris on the conjunctiva. The patient said this had been present since childhood and it had not changed.
FIGURE 1
Red eyes
FIGURE 2
Brown macule
What is the differential iagnosis?
What about the brown macule?
Are any diagnostic tests Necessary for either condition?
Differential diagnosis
The differential diagnosis of a red eye includes:
- Conjunctivitis
- Uveitis
- Acute glaucoma
- Corneal disease or foreign body trauma
- Scleritis and episcleritis.1
For this patient, conjunctivitis is the most likely diagnosis. The absence of eye pain or loss of vision makes uveitis, acute glaucoma, or corneal disease (including foreign-body trauma) less likely. The round shape of the pupil and the absence of the limbal blush also make uveitis less likely. The pattern of injection does not match the wedge-shaped inflammation of episcleritis or the depth of scleritis.
Diagnosis: viral conjunctivitis
This patient has viral conjunctivitis. Conjunctivitis can be infectious, allergic, chemical/irritative, or autoimmune in origin. The most common infectious agents are viral—specifically, the adenoviruses. Other infectious agents include bacteria (Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae), chlamydia, and herpes simplex virus.
Both infectious and allergic conjunctivitis are common. In this patient, the presence of nasal discharge, preauricular lymphadenopathy, and the lack of pruritus make viral infection more likely than allergic. Conjunctivitis that is bilateral without purulent discharge is more likely to be viral than bacterial.
What about the brown macule?
This patient also had a brown macule on her conjunctiva. The differential diagnosis of pigmented areas on the conjunctiva includes nevus, racial melanosis, primary acquired melanosis, secondary pigmentary deposition, and ocular melanoma.2 These conditions (besides ocular melanoma) are benign.
Although ocular melanoma is the most common primary intraocular malignancy in adults, and the second most likely location for primary melanoma after the skin, it is still exceedingly rare. In the Causasian population, it has an average annual incidence of 6 cases per million, with approximately 1200 cases diagnosed each year. Ocular melanoma occurs in the uvea much more commonly than in the conjunctiva, at a ratio of 35:1. Conjunctival melanomas have a propensity for regional spread to the lymph nodes analogous to cutaneous disease, with 10-year survival rates of more than 80%.3
In this case, the patient had this dark spot since childhood and had noted no growth or change. It was consistent with a conjunctival nevus and did not need biopsy.
Diagnostic tests: only for cases that do not respond
When viral conjunctivitis is suspected, no laboratory tests are routinely recommended. Bacterial and viral cultures may be helpful to establish the diagnosis in cases that do not resolve or when patients have recurrent episodes. Infections that do not respond to empiric treatment should be cultured for the suspected organisms (bacteria, chlamydia, or herpes simplex). When chlamydial conjunctivitis is suspected, the diagnosis should be confirmed by means of an immunodiagnostic test (direct fluorescent antibody [DFA]) or culture (level of evidence [LOE]=1a).4
A fluorescein exam is helpful in cases with a question of corneal involvement from foreign-body trauma, herpes simplex, or epidemic kerato-conjunctivitis. Herpes simplex infections have a dendritic pattern of ulceration, and epidemic keratoconjunctivitis infections cause multiple small areas of increased fluorescein uptake.
Management: conjunctivitis usually self-limiting
Typical viral conjunctivitis caused by the adenoviruses or other common viruses (not herpes) does not require medication. Warm compresses may be recommended to reduce discomfort. Infectious conjunctivitis caused by bacteria are also usually self-limiting; however, a recent meta-analysis indicates that treatment with antibiotics can shorten the clinical duration (LOE=1a).5
Appropriate medications for bacterial conjunctivitis include 0.3% tobramycin or gentamycin, 10% sodium sulfacetamide, or erythromycin ophthalmic ointment. If herpetic keratoconjuntivitis is suspected, prompt ophthalmologic referral is indicated.1
Patient’s treatment and outcome
This patient was managed with reassurance and symptomatic treatment of her viral respiratory illness. Her red eyes and upper respiratory infection both resolved spontaneously within 1 week.
As her nevus had not changed in many years, she was instructed to continue to watch the nevus and report any changes to a physician for evaluation. If the lesion changed in the future, she should be referred to an ophthalmologist.
- Erythromycin (ophthalmic) • Ilotycin
- Gentamycin (ophthalmic) • Garamycin, Genoptic Liquifilm, Genoptic SOP, Gentacidin, Gentafair, Gentak, Ocu-Mycin, Spectro-Genta
- Sulfacetamide (ophthalmic) • AK-Sulf, Bleph-10, Cetamide, Isopto Cetamide, Ocusulf-10, Sodium Sulamyd, Sulf-10
- Tobramycin (ophthalmic) • AKTob, Tobrex
Correspondence
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: usatine@uthscsa.edu.
1. Ricketson CW. Conjunctivitis in 5-minute clinical consult. Dambro, MR (ed). InfoRetriever [electronic database]. Charlottesville, Va: InfoPOEMs, Inc; 2004.
2. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
3. Hurst EA, Harbour JW, Cornelius LA. Ocular melanoma: a review and the relationship to cutaneous melanoma. Arch Dermatol 2003;139:1067-1073.
4. American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. Available at: www.aao.org/aao/education/library/ppp/index.cfm. Accessed on February 3, 2004.
5. Sheikh A, Hurwitz B, Cave J. Antibiotics versus placebo for acute bacterial conjunctivitis (Cochrane Review). In: The Cochrane Library, Issue 4, 2003.
A 32-year-old woman came to the rescue mission clinic with her 2 sons because she had red eyes and a runny nose. Her sons both had symptoms highly suggestive of viral upper respiratory infection. They lived in a homeless shelter.
The patient stated she did not use contact lenses or have any eye trauma, itching, photophobia, loss or change of vision, eye pain, eye discharge, or previous episodes of pinkeye. She had no other medical problems or history of allergies.
On physical exam, her vital signs were normal. She had conjunctival injection, without purulent discharge or limbal blush (Figures 1 and 2). Eyelids were mildly erythematous with no cobble-stoning. Pupils were equal, round, and reactive to light. The anterior chamber by flashlight exam from the side did not show a narrow angle. Visual acuity was normal by Snellen exam. She had clear nasal discharge and bilateral preauricular lymphadenopathy.
In addition, she had a brown macule under the left iris on the conjunctiva. The patient said this had been present since childhood and it had not changed.
FIGURE 1
Red eyes
FIGURE 2
Brown macule
What is the differential iagnosis?
What about the brown macule?
Are any diagnostic tests Necessary for either condition?
Differential diagnosis
The differential diagnosis of a red eye includes:
- Conjunctivitis
- Uveitis
- Acute glaucoma
- Corneal disease or foreign body trauma
- Scleritis and episcleritis.1
For this patient, conjunctivitis is the most likely diagnosis. The absence of eye pain or loss of vision makes uveitis, acute glaucoma, or corneal disease (including foreign-body trauma) less likely. The round shape of the pupil and the absence of the limbal blush also make uveitis less likely. The pattern of injection does not match the wedge-shaped inflammation of episcleritis or the depth of scleritis.
Diagnosis: viral conjunctivitis
This patient has viral conjunctivitis. Conjunctivitis can be infectious, allergic, chemical/irritative, or autoimmune in origin. The most common infectious agents are viral—specifically, the adenoviruses. Other infectious agents include bacteria (Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae), chlamydia, and herpes simplex virus.
Both infectious and allergic conjunctivitis are common. In this patient, the presence of nasal discharge, preauricular lymphadenopathy, and the lack of pruritus make viral infection more likely than allergic. Conjunctivitis that is bilateral without purulent discharge is more likely to be viral than bacterial.
What about the brown macule?
This patient also had a brown macule on her conjunctiva. The differential diagnosis of pigmented areas on the conjunctiva includes nevus, racial melanosis, primary acquired melanosis, secondary pigmentary deposition, and ocular melanoma.2 These conditions (besides ocular melanoma) are benign.
Although ocular melanoma is the most common primary intraocular malignancy in adults, and the second most likely location for primary melanoma after the skin, it is still exceedingly rare. In the Causasian population, it has an average annual incidence of 6 cases per million, with approximately 1200 cases diagnosed each year. Ocular melanoma occurs in the uvea much more commonly than in the conjunctiva, at a ratio of 35:1. Conjunctival melanomas have a propensity for regional spread to the lymph nodes analogous to cutaneous disease, with 10-year survival rates of more than 80%.3
In this case, the patient had this dark spot since childhood and had noted no growth or change. It was consistent with a conjunctival nevus and did not need biopsy.
Diagnostic tests: only for cases that do not respond
When viral conjunctivitis is suspected, no laboratory tests are routinely recommended. Bacterial and viral cultures may be helpful to establish the diagnosis in cases that do not resolve or when patients have recurrent episodes. Infections that do not respond to empiric treatment should be cultured for the suspected organisms (bacteria, chlamydia, or herpes simplex). When chlamydial conjunctivitis is suspected, the diagnosis should be confirmed by means of an immunodiagnostic test (direct fluorescent antibody [DFA]) or culture (level of evidence [LOE]=1a).4
A fluorescein exam is helpful in cases with a question of corneal involvement from foreign-body trauma, herpes simplex, or epidemic kerato-conjunctivitis. Herpes simplex infections have a dendritic pattern of ulceration, and epidemic keratoconjunctivitis infections cause multiple small areas of increased fluorescein uptake.
Management: conjunctivitis usually self-limiting
Typical viral conjunctivitis caused by the adenoviruses or other common viruses (not herpes) does not require medication. Warm compresses may be recommended to reduce discomfort. Infectious conjunctivitis caused by bacteria are also usually self-limiting; however, a recent meta-analysis indicates that treatment with antibiotics can shorten the clinical duration (LOE=1a).5
Appropriate medications for bacterial conjunctivitis include 0.3% tobramycin or gentamycin, 10% sodium sulfacetamide, or erythromycin ophthalmic ointment. If herpetic keratoconjuntivitis is suspected, prompt ophthalmologic referral is indicated.1
Patient’s treatment and outcome
This patient was managed with reassurance and symptomatic treatment of her viral respiratory illness. Her red eyes and upper respiratory infection both resolved spontaneously within 1 week.
As her nevus had not changed in many years, she was instructed to continue to watch the nevus and report any changes to a physician for evaluation. If the lesion changed in the future, she should be referred to an ophthalmologist.
- Erythromycin (ophthalmic) • Ilotycin
- Gentamycin (ophthalmic) • Garamycin, Genoptic Liquifilm, Genoptic SOP, Gentacidin, Gentafair, Gentak, Ocu-Mycin, Spectro-Genta
- Sulfacetamide (ophthalmic) • AK-Sulf, Bleph-10, Cetamide, Isopto Cetamide, Ocusulf-10, Sodium Sulamyd, Sulf-10
- Tobramycin (ophthalmic) • AKTob, Tobrex
Correspondence
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: usatine@uthscsa.edu.
A 32-year-old woman came to the rescue mission clinic with her 2 sons because she had red eyes and a runny nose. Her sons both had symptoms highly suggestive of viral upper respiratory infection. They lived in a homeless shelter.
The patient stated she did not use contact lenses or have any eye trauma, itching, photophobia, loss or change of vision, eye pain, eye discharge, or previous episodes of pinkeye. She had no other medical problems or history of allergies.
On physical exam, her vital signs were normal. She had conjunctival injection, without purulent discharge or limbal blush (Figures 1 and 2). Eyelids were mildly erythematous with no cobble-stoning. Pupils were equal, round, and reactive to light. The anterior chamber by flashlight exam from the side did not show a narrow angle. Visual acuity was normal by Snellen exam. She had clear nasal discharge and bilateral preauricular lymphadenopathy.
In addition, she had a brown macule under the left iris on the conjunctiva. The patient said this had been present since childhood and it had not changed.
FIGURE 1
Red eyes
FIGURE 2
Brown macule
What is the differential iagnosis?
What about the brown macule?
Are any diagnostic tests Necessary for either condition?
Differential diagnosis
The differential diagnosis of a red eye includes:
- Conjunctivitis
- Uveitis
- Acute glaucoma
- Corneal disease or foreign body trauma
- Scleritis and episcleritis.1
For this patient, conjunctivitis is the most likely diagnosis. The absence of eye pain or loss of vision makes uveitis, acute glaucoma, or corneal disease (including foreign-body trauma) less likely. The round shape of the pupil and the absence of the limbal blush also make uveitis less likely. The pattern of injection does not match the wedge-shaped inflammation of episcleritis or the depth of scleritis.
Diagnosis: viral conjunctivitis
This patient has viral conjunctivitis. Conjunctivitis can be infectious, allergic, chemical/irritative, or autoimmune in origin. The most common infectious agents are viral—specifically, the adenoviruses. Other infectious agents include bacteria (Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae), chlamydia, and herpes simplex virus.
Both infectious and allergic conjunctivitis are common. In this patient, the presence of nasal discharge, preauricular lymphadenopathy, and the lack of pruritus make viral infection more likely than allergic. Conjunctivitis that is bilateral without purulent discharge is more likely to be viral than bacterial.
What about the brown macule?
This patient also had a brown macule on her conjunctiva. The differential diagnosis of pigmented areas on the conjunctiva includes nevus, racial melanosis, primary acquired melanosis, secondary pigmentary deposition, and ocular melanoma.2 These conditions (besides ocular melanoma) are benign.
Although ocular melanoma is the most common primary intraocular malignancy in adults, and the second most likely location for primary melanoma after the skin, it is still exceedingly rare. In the Causasian population, it has an average annual incidence of 6 cases per million, with approximately 1200 cases diagnosed each year. Ocular melanoma occurs in the uvea much more commonly than in the conjunctiva, at a ratio of 35:1. Conjunctival melanomas have a propensity for regional spread to the lymph nodes analogous to cutaneous disease, with 10-year survival rates of more than 80%.3
In this case, the patient had this dark spot since childhood and had noted no growth or change. It was consistent with a conjunctival nevus and did not need biopsy.
Diagnostic tests: only for cases that do not respond
When viral conjunctivitis is suspected, no laboratory tests are routinely recommended. Bacterial and viral cultures may be helpful to establish the diagnosis in cases that do not resolve or when patients have recurrent episodes. Infections that do not respond to empiric treatment should be cultured for the suspected organisms (bacteria, chlamydia, or herpes simplex). When chlamydial conjunctivitis is suspected, the diagnosis should be confirmed by means of an immunodiagnostic test (direct fluorescent antibody [DFA]) or culture (level of evidence [LOE]=1a).4
A fluorescein exam is helpful in cases with a question of corneal involvement from foreign-body trauma, herpes simplex, or epidemic kerato-conjunctivitis. Herpes simplex infections have a dendritic pattern of ulceration, and epidemic keratoconjunctivitis infections cause multiple small areas of increased fluorescein uptake.
Management: conjunctivitis usually self-limiting
Typical viral conjunctivitis caused by the adenoviruses or other common viruses (not herpes) does not require medication. Warm compresses may be recommended to reduce discomfort. Infectious conjunctivitis caused by bacteria are also usually self-limiting; however, a recent meta-analysis indicates that treatment with antibiotics can shorten the clinical duration (LOE=1a).5
Appropriate medications for bacterial conjunctivitis include 0.3% tobramycin or gentamycin, 10% sodium sulfacetamide, or erythromycin ophthalmic ointment. If herpetic keratoconjuntivitis is suspected, prompt ophthalmologic referral is indicated.1
Patient’s treatment and outcome
This patient was managed with reassurance and symptomatic treatment of her viral respiratory illness. Her red eyes and upper respiratory infection both resolved spontaneously within 1 week.
As her nevus had not changed in many years, she was instructed to continue to watch the nevus and report any changes to a physician for evaluation. If the lesion changed in the future, she should be referred to an ophthalmologist.
- Erythromycin (ophthalmic) • Ilotycin
- Gentamycin (ophthalmic) • Garamycin, Genoptic Liquifilm, Genoptic SOP, Gentacidin, Gentafair, Gentak, Ocu-Mycin, Spectro-Genta
- Sulfacetamide (ophthalmic) • AK-Sulf, Bleph-10, Cetamide, Isopto Cetamide, Ocusulf-10, Sodium Sulamyd, Sulf-10
- Tobramycin (ophthalmic) • AKTob, Tobrex
Correspondence
Richard P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900. E-mail: usatine@uthscsa.edu.
1. Ricketson CW. Conjunctivitis in 5-minute clinical consult. Dambro, MR (ed). InfoRetriever [electronic database]. Charlottesville, Va: InfoPOEMs, Inc; 2004.
2. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
3. Hurst EA, Harbour JW, Cornelius LA. Ocular melanoma: a review and the relationship to cutaneous melanoma. Arch Dermatol 2003;139:1067-1073.
4. American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. Available at: www.aao.org/aao/education/library/ppp/index.cfm. Accessed on February 3, 2004.
5. Sheikh A, Hurwitz B, Cave J. Antibiotics versus placebo for acute bacterial conjunctivitis (Cochrane Review). In: The Cochrane Library, Issue 4, 2003.
1. Ricketson CW. Conjunctivitis in 5-minute clinical consult. Dambro, MR (ed). InfoRetriever [electronic database]. Charlottesville, Va: InfoPOEMs, Inc; 2004.
2. Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol 2004;49:3-24.
3. Hurst EA, Harbour JW, Cornelius LA. Ocular melanoma: a review and the relationship to cutaneous melanoma. Arch Dermatol 2003;139:1067-1073.
4. American Academy of Ophthalmology. Preferred Practice Patterns. Conjunctivitis. Available at: www.aao.org/aao/education/library/ppp/index.cfm. Accessed on February 3, 2004.
5. Sheikh A, Hurwitz B, Cave J. Antibiotics versus placebo for acute bacterial conjunctivitis (Cochrane Review). In: The Cochrane Library, Issue 4, 2003.