User login
A 72-year-old woman is admitted with fever and shortness of breath. Chest radiography demonstrates a consolidation in the right lower lobe, and ceftriaxone and azithromycin are given to treat community-acquired pneumonia. After initial improvement she develops abdominal discomfort and profuse diarrhea on day 5 of hospitalization. What stool testing should be ordered?
Most cases of diarrhea in hospitalized patients are not due to infection, but the most common infectious cause is Clostridium difficile. In the absence of unusual circumstances such as a norovirus outbreak or diarrhea in an immunocompromised patient, testing for C difficile is the only recommended assay. A multistep algorithm with a combination of antigen detection and nucleic acid amplification techniques provides the best sensitivity and specificity. Repeated testing after an initially negative test and performing a test of cure are of limited utility and incur added costs, and thus are not recommended.
CAUSES OF DIARRHEA IN THE HOSPITAL
Diarrhea is defined as at least 1 day with three or more unformed stools or a significant increase in stool frequency above baseline.
Nosocomial diarrhea is an acute episode of diarrhea in a hospitalized patient that was not present on admission and that arises after 3 days of hospitalization. It is fairly common, developing in 12% to 32% of patients at some point during their hospitalization.1
Most cases of nosocomial diarrhea are not due to infection, but rather secondary to enteral feeding, medications, and underlying illness. C difficile is the most common infectious cause and accounts for 10% to 20% of all cases of nosocomial diarrhea.2 Other pathogens associated with nosocomial diarrhea are unusual, although outbreaks of norovirus in healthcare facilities have occurred,3 and isolated cases of Klebsiella oxytoca causing acute abdominal pain, bloody diarrhea, and leukocytosis after exposure to antibiotics have been reported.1
RECOMMENDED TESTING
The evaluation of a hospitalized patient in whom diarrhea develops should initially focus on the clinical presentation, with attention to signs of sepsis. Stable patients with mild symptoms may respond to withdrawal of the offending agent (if any), while patients with moderate or severe symptoms (including those with fever, hypotension, leukocytosis, acute kidney injury, or a decreased serum bicarbonate level) should be tested for C difficile infection (Figure 1).
In general, stool testing should adhere to the “3-day rule”—ie, fecal specimens from patients with diarrhea that develops after 3 days of hospitalization have a very low yield when cultured for standard bacteria or examined for ova and parasites. Thus, only testing for C difficile infection should be ordered.4
In an outbreak of norovirus, especially if vomiting is present, norovirus testing by reverse transcriptase polymerase chain reaction (PCR) could be considered.
Fecal white blood cell testing should not be ordered, as it neither sensitive nor specific.5
Immunocompromised patients (such as those with organ transplants or late-stage human immunodeficiency virus infection) occasionally contract diarrhea due to causes other than C difficile, and consultation with a gastroenterologist or an infectious diseases physician could be considered if diarrhea persists and no cause is apparent.
In the rare situation when a patient is hospitalized after very recent overseas travel and then contracts diarrhea, causes of traveler’s diarrhea should be considered.
TESTING FOR C DIFFICILE INFECTION
A number of diagnostic tests for C difficile infection are available.
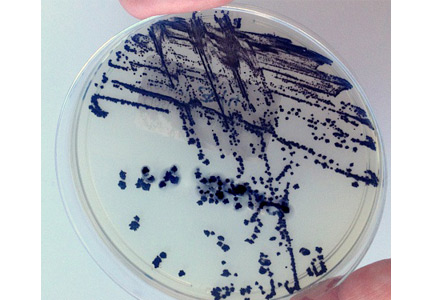
Toxigenic culture (culture followed by detection of a toxigenic isolate) and C difficile cytotoxin neutralization assay are considered the reference standards, having high sensitivity and specificity. However, both are time- and labor-intensive, with turnaround times of at least 2 to 3 days and up to 9 days, limiting their clinical utility and resulting in delay in both diagnosis and implementation of infection control measures.2,6
Enzyme immunoassays (EIAs) are faster. EIAs are available to detect glutamate dehydrogenase (GDH) and toxins A and B, all produced by C difficile. The GDH EIA is 92% sensitive and 93% specific but should not be used alone as it does not distinguish between toxigenic and nontoxigenic strains of C difficile.2,6 The toxin A/B EIA is 97% specific, but since its sensitivity may be as low as 73%, it too should not be used alone.6
Nucleic acid amplification tests such as PCR and loop-mediated isothermal amplification (LAMP) identify toxigenic C difficile by detecting tcdA, tcdB, or tcdC genes, which regulate toxin production. These tests have sensitivities and specificities well over 90%.6
Since molecular tests (ie, nucleic acid amplification tests) for C difficile infection became available in 2009, they have been widely adopted and are commercially available.7 Facilities that use them have reported a 50% to 100% increase in C difficile infection rates,7 but the increase may not be real. Rather, it may reflect increased detection of colonization by the more-sensitive tests.
In a prospective, observational, cohort study,7 1,416 hospitalized patients with diarrhea that developed 72 hours after hospitalization were tested for C difficile infection by both toxin EIA and PCR. Those with positive results on both tests had a longer duration of diarrhea, more C difficile infection-related complications, more C difficile infection-related deaths, and greater risk of diarrhea during follow-up. For those who had negative results on toxin EIA testing, the results of PCR testing made no difference, and neither did treatment for C difficile infection, suggesting that most patients with negative toxin test results do not need treatment for C difficile even if PCR testing is positive.
In light of the limited sensitivity of some toxin EIAs and the increased identification of asymptomatic colonization with nucleic acid amplification testing, the optimal approach may be to combine rapid testing methods. Algorithms that include nucleic acid amplification testing have the best sensitivity (68% to 100%) and specificity (92% to 100%).7 Clinical guidelines suggest using a GDH EIA as the initial step, and then confirming positive results with either nucleic acid amplification testing alone or toxin EIA followed by nucleic acid amplification testing if the toxin EIA is negative.8 However, the best diagnostic approach remains controversial, and multistep algorithms may be impractical in some laboratories.
Knowledge of the laboratory test used can help clinicians appreciate the limitations of specimen testing. Table 1 outlines some of the performance characteristics of the available assays.9–11
The preferred approach at our institution is a multistep algorithm using both the GDH and toxin EIAs in the initial step, followed by a LAMP assay for the C difficile toxin genes in cases of discordant EIA results.
Repeat testing after an initial negative test may be positive in fewer than 5% of cases, can increase the chance of false-positive results, does not improve sensitivity and negative predictive values, and is therefore not recommended.2,8 Similarly, a test of cure after symptoms resolve is not recommended, as the toxin EIA can be positive for up to 30 days after resolution of symptoms, and a positive nucleic acid amplification test may only reflect colonization.2,8
RETURNING TO OUR PATIENT
Returning to the patient hospitalized with community-acquired pneumonia, C difficile infection is the most likely cause of her diarrhea. If her respiratory symptoms have improved, then cessation of ceftriaxone and azithromycin should be considered because she has completed 5 days of therapy. In addition, given her profuse diarrhea, testing for C difficile is recommended with a multistep approach.
- Polage CR, Solnick JV, Cohen SH. Nosocomial diarrhea: evaluation and treatment of causes other than Clostridum difficile. Clin Infect Dis 2012; 55:982–989.
- Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 2010; 31:431–455.
- Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: infection control interventions found effective. Epidemiol Infect 2012; 140:1151–1160.
- Guerrant RL, Van Gilder T, Steiner TS, et al; Infectious Diseases Society of America. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis 2001; 32:331–351.
- Savola KL, Baron EJ, Tompkins LS, Passaro DJ. Fecal leukocyte stain has diagnostic value for outpatients but not inpatients. Clin Microbiol 2001; 39:266–269.
- Bagdasarian N, Rao, K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA 2015; 313:398–408.
- Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med 2015; 175:1792–1801.
- Surawica CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 2013; 108:478–498.
- Staneck JL, Weckbah LS, Allen SD, et al. Multicenter evaluation of four methods for Clostridium difficile detection: immunocard C. difficile, cytotoxin assay, culture, and latex agglutination. J Clin Microbiol 1996; 34:2718–2721.
- Novak-Weekley SM, Marlow EM, Miller JM, et al. Clostridium difficile testing in the clinical laboratory by use of multiple testing algorithms. J Clin Microbiol 2010; 48:889–893.
- Schroeder LF, Robilotti E, Peterson LR, Banaei N, Dowdy DW. Economic evaluation of laboratory testing strategies for hospital-associated Clostridium difficle infection. J Clin Microbiol 2014; 52:489–496.
A 72-year-old woman is admitted with fever and shortness of breath. Chest radiography demonstrates a consolidation in the right lower lobe, and ceftriaxone and azithromycin are given to treat community-acquired pneumonia. After initial improvement she develops abdominal discomfort and profuse diarrhea on day 5 of hospitalization. What stool testing should be ordered?
Most cases of diarrhea in hospitalized patients are not due to infection, but the most common infectious cause is Clostridium difficile. In the absence of unusual circumstances such as a norovirus outbreak or diarrhea in an immunocompromised patient, testing for C difficile is the only recommended assay. A multistep algorithm with a combination of antigen detection and nucleic acid amplification techniques provides the best sensitivity and specificity. Repeated testing after an initially negative test and performing a test of cure are of limited utility and incur added costs, and thus are not recommended.
CAUSES OF DIARRHEA IN THE HOSPITAL
Diarrhea is defined as at least 1 day with three or more unformed stools or a significant increase in stool frequency above baseline.
Nosocomial diarrhea is an acute episode of diarrhea in a hospitalized patient that was not present on admission and that arises after 3 days of hospitalization. It is fairly common, developing in 12% to 32% of patients at some point during their hospitalization.1
Most cases of nosocomial diarrhea are not due to infection, but rather secondary to enteral feeding, medications, and underlying illness. C difficile is the most common infectious cause and accounts for 10% to 20% of all cases of nosocomial diarrhea.2 Other pathogens associated with nosocomial diarrhea are unusual, although outbreaks of norovirus in healthcare facilities have occurred,3 and isolated cases of Klebsiella oxytoca causing acute abdominal pain, bloody diarrhea, and leukocytosis after exposure to antibiotics have been reported.1
RECOMMENDED TESTING
The evaluation of a hospitalized patient in whom diarrhea develops should initially focus on the clinical presentation, with attention to signs of sepsis. Stable patients with mild symptoms may respond to withdrawal of the offending agent (if any), while patients with moderate or severe symptoms (including those with fever, hypotension, leukocytosis, acute kidney injury, or a decreased serum bicarbonate level) should be tested for C difficile infection (Figure 1).
In general, stool testing should adhere to the “3-day rule”—ie, fecal specimens from patients with diarrhea that develops after 3 days of hospitalization have a very low yield when cultured for standard bacteria or examined for ova and parasites. Thus, only testing for C difficile infection should be ordered.4
In an outbreak of norovirus, especially if vomiting is present, norovirus testing by reverse transcriptase polymerase chain reaction (PCR) could be considered.
Fecal white blood cell testing should not be ordered, as it neither sensitive nor specific.5
Immunocompromised patients (such as those with organ transplants or late-stage human immunodeficiency virus infection) occasionally contract diarrhea due to causes other than C difficile, and consultation with a gastroenterologist or an infectious diseases physician could be considered if diarrhea persists and no cause is apparent.
In the rare situation when a patient is hospitalized after very recent overseas travel and then contracts diarrhea, causes of traveler’s diarrhea should be considered.
TESTING FOR C DIFFICILE INFECTION
A number of diagnostic tests for C difficile infection are available.
Toxigenic culture (culture followed by detection of a toxigenic isolate) and C difficile cytotoxin neutralization assay are considered the reference standards, having high sensitivity and specificity. However, both are time- and labor-intensive, with turnaround times of at least 2 to 3 days and up to 9 days, limiting their clinical utility and resulting in delay in both diagnosis and implementation of infection control measures.2,6
Enzyme immunoassays (EIAs) are faster. EIAs are available to detect glutamate dehydrogenase (GDH) and toxins A and B, all produced by C difficile. The GDH EIA is 92% sensitive and 93% specific but should not be used alone as it does not distinguish between toxigenic and nontoxigenic strains of C difficile.2,6 The toxin A/B EIA is 97% specific, but since its sensitivity may be as low as 73%, it too should not be used alone.6
Nucleic acid amplification tests such as PCR and loop-mediated isothermal amplification (LAMP) identify toxigenic C difficile by detecting tcdA, tcdB, or tcdC genes, which regulate toxin production. These tests have sensitivities and specificities well over 90%.6
Since molecular tests (ie, nucleic acid amplification tests) for C difficile infection became available in 2009, they have been widely adopted and are commercially available.7 Facilities that use them have reported a 50% to 100% increase in C difficile infection rates,7 but the increase may not be real. Rather, it may reflect increased detection of colonization by the more-sensitive tests.
In a prospective, observational, cohort study,7 1,416 hospitalized patients with diarrhea that developed 72 hours after hospitalization were tested for C difficile infection by both toxin EIA and PCR. Those with positive results on both tests had a longer duration of diarrhea, more C difficile infection-related complications, more C difficile infection-related deaths, and greater risk of diarrhea during follow-up. For those who had negative results on toxin EIA testing, the results of PCR testing made no difference, and neither did treatment for C difficile infection, suggesting that most patients with negative toxin test results do not need treatment for C difficile even if PCR testing is positive.
In light of the limited sensitivity of some toxin EIAs and the increased identification of asymptomatic colonization with nucleic acid amplification testing, the optimal approach may be to combine rapid testing methods. Algorithms that include nucleic acid amplification testing have the best sensitivity (68% to 100%) and specificity (92% to 100%).7 Clinical guidelines suggest using a GDH EIA as the initial step, and then confirming positive results with either nucleic acid amplification testing alone or toxin EIA followed by nucleic acid amplification testing if the toxin EIA is negative.8 However, the best diagnostic approach remains controversial, and multistep algorithms may be impractical in some laboratories.
Knowledge of the laboratory test used can help clinicians appreciate the limitations of specimen testing. Table 1 outlines some of the performance characteristics of the available assays.9–11
The preferred approach at our institution is a multistep algorithm using both the GDH and toxin EIAs in the initial step, followed by a LAMP assay for the C difficile toxin genes in cases of discordant EIA results.
Repeat testing after an initial negative test may be positive in fewer than 5% of cases, can increase the chance of false-positive results, does not improve sensitivity and negative predictive values, and is therefore not recommended.2,8 Similarly, a test of cure after symptoms resolve is not recommended, as the toxin EIA can be positive for up to 30 days after resolution of symptoms, and a positive nucleic acid amplification test may only reflect colonization.2,8
RETURNING TO OUR PATIENT
Returning to the patient hospitalized with community-acquired pneumonia, C difficile infection is the most likely cause of her diarrhea. If her respiratory symptoms have improved, then cessation of ceftriaxone and azithromycin should be considered because she has completed 5 days of therapy. In addition, given her profuse diarrhea, testing for C difficile is recommended with a multistep approach.
A 72-year-old woman is admitted with fever and shortness of breath. Chest radiography demonstrates a consolidation in the right lower lobe, and ceftriaxone and azithromycin are given to treat community-acquired pneumonia. After initial improvement she develops abdominal discomfort and profuse diarrhea on day 5 of hospitalization. What stool testing should be ordered?
Most cases of diarrhea in hospitalized patients are not due to infection, but the most common infectious cause is Clostridium difficile. In the absence of unusual circumstances such as a norovirus outbreak or diarrhea in an immunocompromised patient, testing for C difficile is the only recommended assay. A multistep algorithm with a combination of antigen detection and nucleic acid amplification techniques provides the best sensitivity and specificity. Repeated testing after an initially negative test and performing a test of cure are of limited utility and incur added costs, and thus are not recommended.
CAUSES OF DIARRHEA IN THE HOSPITAL
Diarrhea is defined as at least 1 day with three or more unformed stools or a significant increase in stool frequency above baseline.
Nosocomial diarrhea is an acute episode of diarrhea in a hospitalized patient that was not present on admission and that arises after 3 days of hospitalization. It is fairly common, developing in 12% to 32% of patients at some point during their hospitalization.1
Most cases of nosocomial diarrhea are not due to infection, but rather secondary to enteral feeding, medications, and underlying illness. C difficile is the most common infectious cause and accounts for 10% to 20% of all cases of nosocomial diarrhea.2 Other pathogens associated with nosocomial diarrhea are unusual, although outbreaks of norovirus in healthcare facilities have occurred,3 and isolated cases of Klebsiella oxytoca causing acute abdominal pain, bloody diarrhea, and leukocytosis after exposure to antibiotics have been reported.1
RECOMMENDED TESTING
The evaluation of a hospitalized patient in whom diarrhea develops should initially focus on the clinical presentation, with attention to signs of sepsis. Stable patients with mild symptoms may respond to withdrawal of the offending agent (if any), while patients with moderate or severe symptoms (including those with fever, hypotension, leukocytosis, acute kidney injury, or a decreased serum bicarbonate level) should be tested for C difficile infection (Figure 1).
In general, stool testing should adhere to the “3-day rule”—ie, fecal specimens from patients with diarrhea that develops after 3 days of hospitalization have a very low yield when cultured for standard bacteria or examined for ova and parasites. Thus, only testing for C difficile infection should be ordered.4
In an outbreak of norovirus, especially if vomiting is present, norovirus testing by reverse transcriptase polymerase chain reaction (PCR) could be considered.
Fecal white blood cell testing should not be ordered, as it neither sensitive nor specific.5
Immunocompromised patients (such as those with organ transplants or late-stage human immunodeficiency virus infection) occasionally contract diarrhea due to causes other than C difficile, and consultation with a gastroenterologist or an infectious diseases physician could be considered if diarrhea persists and no cause is apparent.
In the rare situation when a patient is hospitalized after very recent overseas travel and then contracts diarrhea, causes of traveler’s diarrhea should be considered.
TESTING FOR C DIFFICILE INFECTION
A number of diagnostic tests for C difficile infection are available.
Toxigenic culture (culture followed by detection of a toxigenic isolate) and C difficile cytotoxin neutralization assay are considered the reference standards, having high sensitivity and specificity. However, both are time- and labor-intensive, with turnaround times of at least 2 to 3 days and up to 9 days, limiting their clinical utility and resulting in delay in both diagnosis and implementation of infection control measures.2,6
Enzyme immunoassays (EIAs) are faster. EIAs are available to detect glutamate dehydrogenase (GDH) and toxins A and B, all produced by C difficile. The GDH EIA is 92% sensitive and 93% specific but should not be used alone as it does not distinguish between toxigenic and nontoxigenic strains of C difficile.2,6 The toxin A/B EIA is 97% specific, but since its sensitivity may be as low as 73%, it too should not be used alone.6
Nucleic acid amplification tests such as PCR and loop-mediated isothermal amplification (LAMP) identify toxigenic C difficile by detecting tcdA, tcdB, or tcdC genes, which regulate toxin production. These tests have sensitivities and specificities well over 90%.6
Since molecular tests (ie, nucleic acid amplification tests) for C difficile infection became available in 2009, they have been widely adopted and are commercially available.7 Facilities that use them have reported a 50% to 100% increase in C difficile infection rates,7 but the increase may not be real. Rather, it may reflect increased detection of colonization by the more-sensitive tests.
In a prospective, observational, cohort study,7 1,416 hospitalized patients with diarrhea that developed 72 hours after hospitalization were tested for C difficile infection by both toxin EIA and PCR. Those with positive results on both tests had a longer duration of diarrhea, more C difficile infection-related complications, more C difficile infection-related deaths, and greater risk of diarrhea during follow-up. For those who had negative results on toxin EIA testing, the results of PCR testing made no difference, and neither did treatment for C difficile infection, suggesting that most patients with negative toxin test results do not need treatment for C difficile even if PCR testing is positive.
In light of the limited sensitivity of some toxin EIAs and the increased identification of asymptomatic colonization with nucleic acid amplification testing, the optimal approach may be to combine rapid testing methods. Algorithms that include nucleic acid amplification testing have the best sensitivity (68% to 100%) and specificity (92% to 100%).7 Clinical guidelines suggest using a GDH EIA as the initial step, and then confirming positive results with either nucleic acid amplification testing alone or toxin EIA followed by nucleic acid amplification testing if the toxin EIA is negative.8 However, the best diagnostic approach remains controversial, and multistep algorithms may be impractical in some laboratories.
Knowledge of the laboratory test used can help clinicians appreciate the limitations of specimen testing. Table 1 outlines some of the performance characteristics of the available assays.9–11
The preferred approach at our institution is a multistep algorithm using both the GDH and toxin EIAs in the initial step, followed by a LAMP assay for the C difficile toxin genes in cases of discordant EIA results.
Repeat testing after an initial negative test may be positive in fewer than 5% of cases, can increase the chance of false-positive results, does not improve sensitivity and negative predictive values, and is therefore not recommended.2,8 Similarly, a test of cure after symptoms resolve is not recommended, as the toxin EIA can be positive for up to 30 days after resolution of symptoms, and a positive nucleic acid amplification test may only reflect colonization.2,8
RETURNING TO OUR PATIENT
Returning to the patient hospitalized with community-acquired pneumonia, C difficile infection is the most likely cause of her diarrhea. If her respiratory symptoms have improved, then cessation of ceftriaxone and azithromycin should be considered because she has completed 5 days of therapy. In addition, given her profuse diarrhea, testing for C difficile is recommended with a multistep approach.
- Polage CR, Solnick JV, Cohen SH. Nosocomial diarrhea: evaluation and treatment of causes other than Clostridum difficile. Clin Infect Dis 2012; 55:982–989.
- Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 2010; 31:431–455.
- Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: infection control interventions found effective. Epidemiol Infect 2012; 140:1151–1160.
- Guerrant RL, Van Gilder T, Steiner TS, et al; Infectious Diseases Society of America. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis 2001; 32:331–351.
- Savola KL, Baron EJ, Tompkins LS, Passaro DJ. Fecal leukocyte stain has diagnostic value for outpatients but not inpatients. Clin Microbiol 2001; 39:266–269.
- Bagdasarian N, Rao, K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA 2015; 313:398–408.
- Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med 2015; 175:1792–1801.
- Surawica CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 2013; 108:478–498.
- Staneck JL, Weckbah LS, Allen SD, et al. Multicenter evaluation of four methods for Clostridium difficile detection: immunocard C. difficile, cytotoxin assay, culture, and latex agglutination. J Clin Microbiol 1996; 34:2718–2721.
- Novak-Weekley SM, Marlow EM, Miller JM, et al. Clostridium difficile testing in the clinical laboratory by use of multiple testing algorithms. J Clin Microbiol 2010; 48:889–893.
- Schroeder LF, Robilotti E, Peterson LR, Banaei N, Dowdy DW. Economic evaluation of laboratory testing strategies for hospital-associated Clostridium difficle infection. J Clin Microbiol 2014; 52:489–496.
- Polage CR, Solnick JV, Cohen SH. Nosocomial diarrhea: evaluation and treatment of causes other than Clostridum difficile. Clin Infect Dis 2012; 55:982–989.
- Cohen SH, Gerding DN, Johnson S, et al; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 2010; 31:431–455.
- Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: infection control interventions found effective. Epidemiol Infect 2012; 140:1151–1160.
- Guerrant RL, Van Gilder T, Steiner TS, et al; Infectious Diseases Society of America. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis 2001; 32:331–351.
- Savola KL, Baron EJ, Tompkins LS, Passaro DJ. Fecal leukocyte stain has diagnostic value for outpatients but not inpatients. Clin Microbiol 2001; 39:266–269.
- Bagdasarian N, Rao, K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA 2015; 313:398–408.
- Polage CR, Gyorke CE, Kennedy MA, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med 2015; 175:1792–1801.
- Surawica CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 2013; 108:478–498.
- Staneck JL, Weckbah LS, Allen SD, et al. Multicenter evaluation of four methods for Clostridium difficile detection: immunocard C. difficile, cytotoxin assay, culture, and latex agglutination. J Clin Microbiol 1996; 34:2718–2721.
- Novak-Weekley SM, Marlow EM, Miller JM, et al. Clostridium difficile testing in the clinical laboratory by use of multiple testing algorithms. J Clin Microbiol 2010; 48:889–893.
- Schroeder LF, Robilotti E, Peterson LR, Banaei N, Dowdy DW. Economic evaluation of laboratory testing strategies for hospital-associated Clostridium difficle infection. J Clin Microbiol 2014; 52:489–496.