User login
Why young hemophiliacs skip prophylaxis

Some young hemophilia patients may not be sticking to their prophylaxis regimens for psychosocial reasons, according to research published in PLOS ONE.
The study included 78 hemophilia patients, ages 12 to 25, treated at 13 centers in England and Wales.
“This research has a specific focus on young people rather than including patients of all age groups,” said study author Sandra Van Os, a PhD student at the University of Hertfordshire in Hatfield, UK.
“This is important since young people are likely to have had a very different experience than the older generations due to the revolutionary improvements in treatment achieved during the past 2 decades. Another key issue is rather than asking parents or healthcare professionals to estimate adherence as previous studies have done, this study asked young people directly.”
The results showed that 18% of the patients did not adhere to their prophylaxis regimens. Most non-adherence was due to forgetting treatment rather than intentionally skipping it.
But there were a few psychosocial reasons for non-adherence. Patients reported non-adherence due to a lack of social support and the perceived impact of prophylaxis on their everyday lives.
Patients also lacked understanding about the effectiveness of prophylaxis and its importance in treating hemophilia.
The patients were more likely to adhere to treatment when they perceived the need for prophylaxis to be greater than their concern over taking it.
And the study suggested a strong emotional reaction to a bleed may encourage young people to adhere to their treatment regimen.
“Interestingly, the findings suggest that, in addition to social support and treatment beliefs, emotional responses in relation to hemophilia, such as fear, anger, or distress, may also contribute to better adherence,” van Os said.
“It is important that patients receive sufficient and appropriate social support in order to stay on track with their treatment. It will also be beneficial to reduce potential concerns about prophylaxis and to assess whether patients understand their treatment sufficiently well and the role they themselves have to play in its effectiveness.”
This research was supported by external, peer-reviewed funding from the Bayer Haemophilia Awards Programme (Caregiver Award awarded to van Os). ![]()

Some young hemophilia patients may not be sticking to their prophylaxis regimens for psychosocial reasons, according to research published in PLOS ONE.
The study included 78 hemophilia patients, ages 12 to 25, treated at 13 centers in England and Wales.
“This research has a specific focus on young people rather than including patients of all age groups,” said study author Sandra Van Os, a PhD student at the University of Hertfordshire in Hatfield, UK.
“This is important since young people are likely to have had a very different experience than the older generations due to the revolutionary improvements in treatment achieved during the past 2 decades. Another key issue is rather than asking parents or healthcare professionals to estimate adherence as previous studies have done, this study asked young people directly.”
The results showed that 18% of the patients did not adhere to their prophylaxis regimens. Most non-adherence was due to forgetting treatment rather than intentionally skipping it.
But there were a few psychosocial reasons for non-adherence. Patients reported non-adherence due to a lack of social support and the perceived impact of prophylaxis on their everyday lives.
Patients also lacked understanding about the effectiveness of prophylaxis and its importance in treating hemophilia.
The patients were more likely to adhere to treatment when they perceived the need for prophylaxis to be greater than their concern over taking it.
And the study suggested a strong emotional reaction to a bleed may encourage young people to adhere to their treatment regimen.
“Interestingly, the findings suggest that, in addition to social support and treatment beliefs, emotional responses in relation to hemophilia, such as fear, anger, or distress, may also contribute to better adherence,” van Os said.
“It is important that patients receive sufficient and appropriate social support in order to stay on track with their treatment. It will also be beneficial to reduce potential concerns about prophylaxis and to assess whether patients understand their treatment sufficiently well and the role they themselves have to play in its effectiveness.”
This research was supported by external, peer-reviewed funding from the Bayer Haemophilia Awards Programme (Caregiver Award awarded to van Os). ![]()

Some young hemophilia patients may not be sticking to their prophylaxis regimens for psychosocial reasons, according to research published in PLOS ONE.
The study included 78 hemophilia patients, ages 12 to 25, treated at 13 centers in England and Wales.
“This research has a specific focus on young people rather than including patients of all age groups,” said study author Sandra Van Os, a PhD student at the University of Hertfordshire in Hatfield, UK.
“This is important since young people are likely to have had a very different experience than the older generations due to the revolutionary improvements in treatment achieved during the past 2 decades. Another key issue is rather than asking parents or healthcare professionals to estimate adherence as previous studies have done, this study asked young people directly.”
The results showed that 18% of the patients did not adhere to their prophylaxis regimens. Most non-adherence was due to forgetting treatment rather than intentionally skipping it.
But there were a few psychosocial reasons for non-adherence. Patients reported non-adherence due to a lack of social support and the perceived impact of prophylaxis on their everyday lives.
Patients also lacked understanding about the effectiveness of prophylaxis and its importance in treating hemophilia.
The patients were more likely to adhere to treatment when they perceived the need for prophylaxis to be greater than their concern over taking it.
And the study suggested a strong emotional reaction to a bleed may encourage young people to adhere to their treatment regimen.
“Interestingly, the findings suggest that, in addition to social support and treatment beliefs, emotional responses in relation to hemophilia, such as fear, anger, or distress, may also contribute to better adherence,” van Os said.
“It is important that patients receive sufficient and appropriate social support in order to stay on track with their treatment. It will also be beneficial to reduce potential concerns about prophylaxis and to assess whether patients understand their treatment sufficiently well and the role they themselves have to play in its effectiveness.”
This research was supported by external, peer-reviewed funding from the Bayer Haemophilia Awards Programme (Caregiver Award awarded to van Os). ![]()
Donor CAR T cells bridge to HSCT in infants with ALL

treated with UCART19
Photo courtesy of GOSH
New research suggests that “universal,” donor-derived, chimeric antigen receptor (CAR) T cells may be a viable treatment option for very young children who do not have sufficient healthy T cells for autologous CAR T-cell therapy.
The universal CAR T-cell therapy, known as UCART19, was given to 2 infants with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) who had previously
exhausted all other treatment options.
Both infants achieved remission after UCART19 and were able to proceed to transplant.
Both were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19, respectively.
Waseem Qasim, MBBS, PhD, of University College London’s Institute of Child Health and Great Ormond Street Hospital (GOSH) in London, UK, and his colleagues reported these results in Science Translational Medicine.
About the therapy
UCART19 consists of donor T cells modified using transcription activator-like effector nucleases. The cells are programmed to target CD19 and be insensitive to alemtuzumab. That way, a patient can receive alemtuzumab to prevent rejection of HLA-mismatched cells.
UCART19 was under development by Cellectis but is now being developed by Servier and Pfizer Inc. Pfizer has exclusive rights to develop and commercialize UCART19 in the US, while Servier retains exclusive rights for all other countries.
In Science Translational Medicine, Dr Qasim and his colleagues reported results in the first patients ever treated with UCART19. That research was funded, in part, by Cellectis.
Subject 1
The first patient was an 11-month-old, mixed-race infant with high-risk, t(11;19), CD19+ B-ALL. She had already failed chemotherapy, an allogeneic hematopoietic stem cell transplant (HSCT), and blinatumomab.
Prior to UCART19, she received a dose of vincristine and asparaginase and 7 days of dexamethasone, followed by cytoreduction with fludarabine, cyclophosphamide, and alemtuzumab. She then received a single dose of UCART19 (4.6 × 106/kg).
The patient had neutrophil recovery by day 30, although this was dependent on granulocyte colony-stimulating factor. After that, she developed multilineage cytopenia that persisted until she underwent a second allogeneic HSCT.
Prior to the second HSCT, the patient achieved cytogenetic and molecular remission but also developed grade 2 skin graft-vs-host disease. This was managed with systemic steroids.
The child received rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, thiotepa, and total body irradiation, followed by an HSCT from the original mismatched, unrelated donor.
The child achieved a complete remission and has remained minimal residual disease-negative, with full donor chimerism and normalized lymphocyte profiles, at 18 months after UCART19.
Results with this patient were previously reported by GOSH in November 2015 and at the 2015 ASH Annual Meeting.
Subject 2
The second patient was a 16-month-old Caucasian infant who had been diagnosed at 4 weeks of age with high-risk, congenital, mixed lineage leukemia–rearranged B-ALL.
She had already undergone HSCT from a matched, unrelated donor but relapsed. She did not respond to subsequent blinatumomab.
After these failed treatments, the patient received fludarabine, cyclophosphamide, and alemtuzumab, followed by a single infusion of UCART19 (4.0 × 106/kg).
She developed an erythematous rash after treatment, but this was immediately responsive to topical steroids.
The child achieved donor-derived neutrophil recovery and went on to receive a transplant from the same matched, unrelated donor as her previous HSCT.
The child received the transplant within 10 weeks of UCART19 therapy, after receiving rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
At 12 months after UCART19, the child remains minimal residual disease-negative and “clinically well.”
“Both infants who have had this treatment have been at home for some time and are doing well,” Dr Qasim said. “We continue to monitor them closely, and, while we have reduced the frequency of their hospital visits and checks, we will still need to keep an eye on them for some time.”
Dr Qasim added that there are phase 1 trials of UCART19 underway for children and adults with chronic lymphocytic leukemia and acute lymphoblastic leukemia. ![]()

treated with UCART19
Photo courtesy of GOSH
New research suggests that “universal,” donor-derived, chimeric antigen receptor (CAR) T cells may be a viable treatment option for very young children who do not have sufficient healthy T cells for autologous CAR T-cell therapy.
The universal CAR T-cell therapy, known as UCART19, was given to 2 infants with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) who had previously
exhausted all other treatment options.
Both infants achieved remission after UCART19 and were able to proceed to transplant.
Both were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19, respectively.
Waseem Qasim, MBBS, PhD, of University College London’s Institute of Child Health and Great Ormond Street Hospital (GOSH) in London, UK, and his colleagues reported these results in Science Translational Medicine.
About the therapy
UCART19 consists of donor T cells modified using transcription activator-like effector nucleases. The cells are programmed to target CD19 and be insensitive to alemtuzumab. That way, a patient can receive alemtuzumab to prevent rejection of HLA-mismatched cells.
UCART19 was under development by Cellectis but is now being developed by Servier and Pfizer Inc. Pfizer has exclusive rights to develop and commercialize UCART19 in the US, while Servier retains exclusive rights for all other countries.
In Science Translational Medicine, Dr Qasim and his colleagues reported results in the first patients ever treated with UCART19. That research was funded, in part, by Cellectis.
Subject 1
The first patient was an 11-month-old, mixed-race infant with high-risk, t(11;19), CD19+ B-ALL. She had already failed chemotherapy, an allogeneic hematopoietic stem cell transplant (HSCT), and blinatumomab.
Prior to UCART19, she received a dose of vincristine and asparaginase and 7 days of dexamethasone, followed by cytoreduction with fludarabine, cyclophosphamide, and alemtuzumab. She then received a single dose of UCART19 (4.6 × 106/kg).
The patient had neutrophil recovery by day 30, although this was dependent on granulocyte colony-stimulating factor. After that, she developed multilineage cytopenia that persisted until she underwent a second allogeneic HSCT.
Prior to the second HSCT, the patient achieved cytogenetic and molecular remission but also developed grade 2 skin graft-vs-host disease. This was managed with systemic steroids.
The child received rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, thiotepa, and total body irradiation, followed by an HSCT from the original mismatched, unrelated donor.
The child achieved a complete remission and has remained minimal residual disease-negative, with full donor chimerism and normalized lymphocyte profiles, at 18 months after UCART19.
Results with this patient were previously reported by GOSH in November 2015 and at the 2015 ASH Annual Meeting.
Subject 2
The second patient was a 16-month-old Caucasian infant who had been diagnosed at 4 weeks of age with high-risk, congenital, mixed lineage leukemia–rearranged B-ALL.
She had already undergone HSCT from a matched, unrelated donor but relapsed. She did not respond to subsequent blinatumomab.
After these failed treatments, the patient received fludarabine, cyclophosphamide, and alemtuzumab, followed by a single infusion of UCART19 (4.0 × 106/kg).
She developed an erythematous rash after treatment, but this was immediately responsive to topical steroids.
The child achieved donor-derived neutrophil recovery and went on to receive a transplant from the same matched, unrelated donor as her previous HSCT.
The child received the transplant within 10 weeks of UCART19 therapy, after receiving rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
At 12 months after UCART19, the child remains minimal residual disease-negative and “clinically well.”
“Both infants who have had this treatment have been at home for some time and are doing well,” Dr Qasim said. “We continue to monitor them closely, and, while we have reduced the frequency of their hospital visits and checks, we will still need to keep an eye on them for some time.”
Dr Qasim added that there are phase 1 trials of UCART19 underway for children and adults with chronic lymphocytic leukemia and acute lymphoblastic leukemia. ![]()

treated with UCART19
Photo courtesy of GOSH
New research suggests that “universal,” donor-derived, chimeric antigen receptor (CAR) T cells may be a viable treatment option for very young children who do not have sufficient healthy T cells for autologous CAR T-cell therapy.
The universal CAR T-cell therapy, known as UCART19, was given to 2 infants with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) who had previously
exhausted all other treatment options.
Both infants achieved remission after UCART19 and were able to proceed to transplant.
Both were still alive and leukemia-free at last follow-up—12 months and 18 months after UCART19, respectively.
Waseem Qasim, MBBS, PhD, of University College London’s Institute of Child Health and Great Ormond Street Hospital (GOSH) in London, UK, and his colleagues reported these results in Science Translational Medicine.
About the therapy
UCART19 consists of donor T cells modified using transcription activator-like effector nucleases. The cells are programmed to target CD19 and be insensitive to alemtuzumab. That way, a patient can receive alemtuzumab to prevent rejection of HLA-mismatched cells.
UCART19 was under development by Cellectis but is now being developed by Servier and Pfizer Inc. Pfizer has exclusive rights to develop and commercialize UCART19 in the US, while Servier retains exclusive rights for all other countries.
In Science Translational Medicine, Dr Qasim and his colleagues reported results in the first patients ever treated with UCART19. That research was funded, in part, by Cellectis.
Subject 1
The first patient was an 11-month-old, mixed-race infant with high-risk, t(11;19), CD19+ B-ALL. She had already failed chemotherapy, an allogeneic hematopoietic stem cell transplant (HSCT), and blinatumomab.
Prior to UCART19, she received a dose of vincristine and asparaginase and 7 days of dexamethasone, followed by cytoreduction with fludarabine, cyclophosphamide, and alemtuzumab. She then received a single dose of UCART19 (4.6 × 106/kg).
The patient had neutrophil recovery by day 30, although this was dependent on granulocyte colony-stimulating factor. After that, she developed multilineage cytopenia that persisted until she underwent a second allogeneic HSCT.
Prior to the second HSCT, the patient achieved cytogenetic and molecular remission but also developed grade 2 skin graft-vs-host disease. This was managed with systemic steroids.
The child received rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, thiotepa, and total body irradiation, followed by an HSCT from the original mismatched, unrelated donor.
The child achieved a complete remission and has remained minimal residual disease-negative, with full donor chimerism and normalized lymphocyte profiles, at 18 months after UCART19.
Results with this patient were previously reported by GOSH in November 2015 and at the 2015 ASH Annual Meeting.
Subject 2
The second patient was a 16-month-old Caucasian infant who had been diagnosed at 4 weeks of age with high-risk, congenital, mixed lineage leukemia–rearranged B-ALL.
She had already undergone HSCT from a matched, unrelated donor but relapsed. She did not respond to subsequent blinatumomab.
After these failed treatments, the patient received fludarabine, cyclophosphamide, and alemtuzumab, followed by a single infusion of UCART19 (4.0 × 106/kg).
She developed an erythematous rash after treatment, but this was immediately responsive to topical steroids.
The child achieved donor-derived neutrophil recovery and went on to receive a transplant from the same matched, unrelated donor as her previous HSCT.
The child received the transplant within 10 weeks of UCART19 therapy, after receiving rituximab and conditioning with antithymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
At 12 months after UCART19, the child remains minimal residual disease-negative and “clinically well.”
“Both infants who have had this treatment have been at home for some time and are doing well,” Dr Qasim said. “We continue to monitor them closely, and, while we have reduced the frequency of their hospital visits and checks, we will still need to keep an eye on them for some time.”
Dr Qasim added that there are phase 1 trials of UCART19 underway for children and adults with chronic lymphocytic leukemia and acute lymphoblastic leukemia. ![]()
Roche launches new blood analyzer

Photo by Graham Colm
Roche has announced the launch of its cobas m 511 integrated hematology analyzer in countries that recognize the CE mark.*
The cobas m 511 combines 3 components of the hematology testing process—a digital morphology analyzer, cell counter, and classifier—into a single system that prepares, stains, and analyzes microscopy blood slides.
Roche said cobas m 511 provides greater accuracy and consistency than current technologies by identifying, counting, isolating, and categorizing blood cells, then presenting the digital images of all these cell types.
The company said this automation and digitalization reduces the need for resource-intensive manual microscope reviews, supports clinicians to share challenging cases around the world, and enables the delivery of quicker results, which ultimately aid patient diagnoses.
The cobas m 511 uses Bloodhound® technology for printing, staining, and imaging. This technology uses 30 µL of blood to print a monolayer onto the slide, stains for further analysis of the morphology, and enables classification of cells displayed on a viewing station.
Unlike the indirect methods commonly used in blood analysis today, the cobas m 511 images individual cells directly.
Based on these direct images, the Bloodhound® technology counts, analyzes morphology, and then classifies every cell in the viewing area to provide a standard complete blood count and 5-part differential and reticulocyte count.
While hematologists will continue to have the option of looking at slides under their microscopes, the cobas m 511 provides cell-by-cell images that, in many cases, may eliminate the need for microscopic review.
“With this launch, patients will benefit from a faster and more accurate diagnosis of blood diseases as diverse as anemia and leukemia,” said Roland Diggelmann, CEO of Roche Diagnostics.
“We are entering a new area of innovation with Roche in hematology testing, supporting customers with integrated and efficient laboratory solutions, which deliver increased medical value.” ![]()
*Local product availability may vary independently from CE mark approval. The cobas m 511 integrated hematology analyzer is not available in countries with previously agreed third-party vendor agreements.

Photo by Graham Colm
Roche has announced the launch of its cobas m 511 integrated hematology analyzer in countries that recognize the CE mark.*
The cobas m 511 combines 3 components of the hematology testing process—a digital morphology analyzer, cell counter, and classifier—into a single system that prepares, stains, and analyzes microscopy blood slides.
Roche said cobas m 511 provides greater accuracy and consistency than current technologies by identifying, counting, isolating, and categorizing blood cells, then presenting the digital images of all these cell types.
The company said this automation and digitalization reduces the need for resource-intensive manual microscope reviews, supports clinicians to share challenging cases around the world, and enables the delivery of quicker results, which ultimately aid patient diagnoses.
The cobas m 511 uses Bloodhound® technology for printing, staining, and imaging. This technology uses 30 µL of blood to print a monolayer onto the slide, stains for further analysis of the morphology, and enables classification of cells displayed on a viewing station.
Unlike the indirect methods commonly used in blood analysis today, the cobas m 511 images individual cells directly.
Based on these direct images, the Bloodhound® technology counts, analyzes morphology, and then classifies every cell in the viewing area to provide a standard complete blood count and 5-part differential and reticulocyte count.
While hematologists will continue to have the option of looking at slides under their microscopes, the cobas m 511 provides cell-by-cell images that, in many cases, may eliminate the need for microscopic review.
“With this launch, patients will benefit from a faster and more accurate diagnosis of blood diseases as diverse as anemia and leukemia,” said Roland Diggelmann, CEO of Roche Diagnostics.
“We are entering a new area of innovation with Roche in hematology testing, supporting customers with integrated and efficient laboratory solutions, which deliver increased medical value.” ![]()
*Local product availability may vary independently from CE mark approval. The cobas m 511 integrated hematology analyzer is not available in countries with previously agreed third-party vendor agreements.

Photo by Graham Colm
Roche has announced the launch of its cobas m 511 integrated hematology analyzer in countries that recognize the CE mark.*
The cobas m 511 combines 3 components of the hematology testing process—a digital morphology analyzer, cell counter, and classifier—into a single system that prepares, stains, and analyzes microscopy blood slides.
Roche said cobas m 511 provides greater accuracy and consistency than current technologies by identifying, counting, isolating, and categorizing blood cells, then presenting the digital images of all these cell types.
The company said this automation and digitalization reduces the need for resource-intensive manual microscope reviews, supports clinicians to share challenging cases around the world, and enables the delivery of quicker results, which ultimately aid patient diagnoses.
The cobas m 511 uses Bloodhound® technology for printing, staining, and imaging. This technology uses 30 µL of blood to print a monolayer onto the slide, stains for further analysis of the morphology, and enables classification of cells displayed on a viewing station.
Unlike the indirect methods commonly used in blood analysis today, the cobas m 511 images individual cells directly.
Based on these direct images, the Bloodhound® technology counts, analyzes morphology, and then classifies every cell in the viewing area to provide a standard complete blood count and 5-part differential and reticulocyte count.
While hematologists will continue to have the option of looking at slides under their microscopes, the cobas m 511 provides cell-by-cell images that, in many cases, may eliminate the need for microscopic review.
“With this launch, patients will benefit from a faster and more accurate diagnosis of blood diseases as diverse as anemia and leukemia,” said Roland Diggelmann, CEO of Roche Diagnostics.
“We are entering a new area of innovation with Roche in hematology testing, supporting customers with integrated and efficient laboratory solutions, which deliver increased medical value.” ![]()
*Local product availability may vary independently from CE mark approval. The cobas m 511 integrated hematology analyzer is not available in countries with previously agreed third-party vendor agreements.
Anticoagulants often unnecessary after surgery, analysis suggests

Many surgical patients may be receiving anticoagulants they don’t need, according to research published in Annals of Surgery.
The study challenges standard of care guidelines, which recommend that all general surgery patients receive treatment to prevent venous thromboembolism (VTE).
The new findings suggest that anticoagulants may be unnecessary for most surgical patients and could even be harmful to some.
“A ‘one-size-fits-all approach’ doesn’t always make sense,” said study author Christopher Pannucci, MD, of the University of Utah in Salt Lake City.
“A healthy 35-year-old is very different from someone who is 85 and has a history of clots. Our research indicates that there could be a substantial number of people who are being over-treated.”
Dr Pannucci and his colleagues reviewed data from 13 studies to determine which surgical patients were most likely, and least likely, to benefit from anticoagulants. There was data on VTE events in 11 studies (n=14,776) and data on clinically relevant bleeding in 8 studies (n=7590).
In most of the studies, patients received mechanical VTE prophylaxis, which meant elastic compression and/or sequential compression devices.
Some studies compared mechanical prophylaxis to anticoagulants, including heparin, low-molecular-weight heparin, direct factor Xa inhibitors, direct thrombin inhibitors, warfarin, dextran, and aspirin.
The studies included a broad range of surgical patients, from individuals with few VTE risk factors to those with multiple risk factors, such as obesity, advanced age, and personal or family history of VTE.
The patients were divided into 1 of 5 categories indicating overall VTE risk. Assessment was based on the Caprini score.
VTE risk without anticoagulant treatment
There were 11 studies in which some patients did not receive anticoagulants (n=6085).
Among these patients, those who were classified as having the highest risk of VTE were 14 times more likely to develop VTE than patients in the low-risk category—10.7% vs 0.7%.
These findings were independent of surgery type.
“It was eye-opening to see that there is this huge variability in risk among the overall group of patients that walk into your office,” Dr Pannucci said. “Unless you consider a patient’s risk based on their individual factors, you would never know.”
VTE outcomes by risk score
When given, anticoagulants did significantly reduce the risk of VTE for the overall study population and for high-risk patients.
The odds ratios (ORs) were 0.66 (P=0.001) for the overall population, 0.60 (P=0.04) for patients with Caprini scores of 7 to 8, and 0.41 (P=0.0002) for patients with scores higher than 8.
Unfortunately, anticoagulants did not make a significant difference in VTE rates for mid- or low-risk patients.
The ORs were 0.45 (P=0.31) for patients with Caprini scores of 0 to 2, 1.31 (P=0.57) for patients with scores of 3 to 4, and 0.96 (P=0.85) for patients with scores of 5 to 6.
Risk of bleeding
Anticoagulants significantly increased clinically relevant bleeding for the overall population. The OR was 1.69 (P=0.006).
Patients who received anticoagulants were not significantly more likely to have clinically relevant bleeding if they had risk scores of 0 to 2 (OR=2.47, P=0.61), 3 to 4 (OR=1.05, P=0.87), 5 to 6 (OR=2.10, P=0.06), 7 to 8 (OR=3.15, P=0.16), or >8 (OR=2.31, P=0.16).
“For the first time, we have data that prophylaxis for the highest-risk groups is beneficial, and data that suggests that lower-risk patients may need no prophylaxis,” said study author Peter Henke, MD, of the University of Michigan in Ann Arbor.
He and his colleagues noted, however, that prospective studies are needed to confirm these findings. ![]()

Many surgical patients may be receiving anticoagulants they don’t need, according to research published in Annals of Surgery.
The study challenges standard of care guidelines, which recommend that all general surgery patients receive treatment to prevent venous thromboembolism (VTE).
The new findings suggest that anticoagulants may be unnecessary for most surgical patients and could even be harmful to some.
“A ‘one-size-fits-all approach’ doesn’t always make sense,” said study author Christopher Pannucci, MD, of the University of Utah in Salt Lake City.
“A healthy 35-year-old is very different from someone who is 85 and has a history of clots. Our research indicates that there could be a substantial number of people who are being over-treated.”
Dr Pannucci and his colleagues reviewed data from 13 studies to determine which surgical patients were most likely, and least likely, to benefit from anticoagulants. There was data on VTE events in 11 studies (n=14,776) and data on clinically relevant bleeding in 8 studies (n=7590).
In most of the studies, patients received mechanical VTE prophylaxis, which meant elastic compression and/or sequential compression devices.
Some studies compared mechanical prophylaxis to anticoagulants, including heparin, low-molecular-weight heparin, direct factor Xa inhibitors, direct thrombin inhibitors, warfarin, dextran, and aspirin.
The studies included a broad range of surgical patients, from individuals with few VTE risk factors to those with multiple risk factors, such as obesity, advanced age, and personal or family history of VTE.
The patients were divided into 1 of 5 categories indicating overall VTE risk. Assessment was based on the Caprini score.
VTE risk without anticoagulant treatment
There were 11 studies in which some patients did not receive anticoagulants (n=6085).
Among these patients, those who were classified as having the highest risk of VTE were 14 times more likely to develop VTE than patients in the low-risk category—10.7% vs 0.7%.
These findings were independent of surgery type.
“It was eye-opening to see that there is this huge variability in risk among the overall group of patients that walk into your office,” Dr Pannucci said. “Unless you consider a patient’s risk based on their individual factors, you would never know.”
VTE outcomes by risk score
When given, anticoagulants did significantly reduce the risk of VTE for the overall study population and for high-risk patients.
The odds ratios (ORs) were 0.66 (P=0.001) for the overall population, 0.60 (P=0.04) for patients with Caprini scores of 7 to 8, and 0.41 (P=0.0002) for patients with scores higher than 8.
Unfortunately, anticoagulants did not make a significant difference in VTE rates for mid- or low-risk patients.
The ORs were 0.45 (P=0.31) for patients with Caprini scores of 0 to 2, 1.31 (P=0.57) for patients with scores of 3 to 4, and 0.96 (P=0.85) for patients with scores of 5 to 6.
Risk of bleeding
Anticoagulants significantly increased clinically relevant bleeding for the overall population. The OR was 1.69 (P=0.006).
Patients who received anticoagulants were not significantly more likely to have clinically relevant bleeding if they had risk scores of 0 to 2 (OR=2.47, P=0.61), 3 to 4 (OR=1.05, P=0.87), 5 to 6 (OR=2.10, P=0.06), 7 to 8 (OR=3.15, P=0.16), or >8 (OR=2.31, P=0.16).
“For the first time, we have data that prophylaxis for the highest-risk groups is beneficial, and data that suggests that lower-risk patients may need no prophylaxis,” said study author Peter Henke, MD, of the University of Michigan in Ann Arbor.
He and his colleagues noted, however, that prospective studies are needed to confirm these findings. ![]()

Many surgical patients may be receiving anticoagulants they don’t need, according to research published in Annals of Surgery.
The study challenges standard of care guidelines, which recommend that all general surgery patients receive treatment to prevent venous thromboembolism (VTE).
The new findings suggest that anticoagulants may be unnecessary for most surgical patients and could even be harmful to some.
“A ‘one-size-fits-all approach’ doesn’t always make sense,” said study author Christopher Pannucci, MD, of the University of Utah in Salt Lake City.
“A healthy 35-year-old is very different from someone who is 85 and has a history of clots. Our research indicates that there could be a substantial number of people who are being over-treated.”
Dr Pannucci and his colleagues reviewed data from 13 studies to determine which surgical patients were most likely, and least likely, to benefit from anticoagulants. There was data on VTE events in 11 studies (n=14,776) and data on clinically relevant bleeding in 8 studies (n=7590).
In most of the studies, patients received mechanical VTE prophylaxis, which meant elastic compression and/or sequential compression devices.
Some studies compared mechanical prophylaxis to anticoagulants, including heparin, low-molecular-weight heparin, direct factor Xa inhibitors, direct thrombin inhibitors, warfarin, dextran, and aspirin.
The studies included a broad range of surgical patients, from individuals with few VTE risk factors to those with multiple risk factors, such as obesity, advanced age, and personal or family history of VTE.
The patients were divided into 1 of 5 categories indicating overall VTE risk. Assessment was based on the Caprini score.
VTE risk without anticoagulant treatment
There were 11 studies in which some patients did not receive anticoagulants (n=6085).
Among these patients, those who were classified as having the highest risk of VTE were 14 times more likely to develop VTE than patients in the low-risk category—10.7% vs 0.7%.
These findings were independent of surgery type.
“It was eye-opening to see that there is this huge variability in risk among the overall group of patients that walk into your office,” Dr Pannucci said. “Unless you consider a patient’s risk based on their individual factors, you would never know.”
VTE outcomes by risk score
When given, anticoagulants did significantly reduce the risk of VTE for the overall study population and for high-risk patients.
The odds ratios (ORs) were 0.66 (P=0.001) for the overall population, 0.60 (P=0.04) for patients with Caprini scores of 7 to 8, and 0.41 (P=0.0002) for patients with scores higher than 8.
Unfortunately, anticoagulants did not make a significant difference in VTE rates for mid- or low-risk patients.
The ORs were 0.45 (P=0.31) for patients with Caprini scores of 0 to 2, 1.31 (P=0.57) for patients with scores of 3 to 4, and 0.96 (P=0.85) for patients with scores of 5 to 6.
Risk of bleeding
Anticoagulants significantly increased clinically relevant bleeding for the overall population. The OR was 1.69 (P=0.006).
Patients who received anticoagulants were not significantly more likely to have clinically relevant bleeding if they had risk scores of 0 to 2 (OR=2.47, P=0.61), 3 to 4 (OR=1.05, P=0.87), 5 to 6 (OR=2.10, P=0.06), 7 to 8 (OR=3.15, P=0.16), or >8 (OR=2.31, P=0.16).
“For the first time, we have data that prophylaxis for the highest-risk groups is beneficial, and data that suggests that lower-risk patients may need no prophylaxis,” said study author Peter Henke, MD, of the University of Michigan in Ann Arbor.
He and his colleagues noted, however, that prospective studies are needed to confirm these findings. ![]()
Study quantifies 5-year survival rates for blood cancers

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954. ![]()

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954. ![]()

chemotherapy
Photo by Rhoda Baer
A new study shows that 5-year survival rates for US patients with hematologic malignancies have increased greatly since the 1950s, but there is still room for improvement, particularly for patients with acute myeloid leukemia (AML).
Researchers found the absolute difference in improvement for 5-year survival from 1950-1954 to 2008-2013 ranged from 38.2% for non-Hodgkin lymphoma (NHL) to 56.6% for Hodgkin lymphoma.
And although the 5-year survival rate for Hodgkin lymphoma patients reached 86.6% for 2008-2013, the 5-year survival rate for patients with AML only reached 27.4%.
This study also revealed large disparities in overall cancer mortality rates between different counties across the country.
Ali H. Mokdad, PhD, of the Institute for Health Metrics and Evaluation in Seattle, Washington, and his colleagues reported these findings in JAMA.
Overall cancer deaths
The researchers found there were 19,511,910 cancer deaths recorded in the US between 1980 and 2014. Cancer mortality decreased by 20.1% between 1980 and 2014, from 240.2 deaths per 100,000 people to 192.0 deaths per 100,000 people.
In 1980, cancer mortality ranged from 130.6 per 100,000 in Summit County, Colorado, to 386.9 per 100,000 in North Slope Borough, Alaska.
In 2014, cancer mortality ranged from 70.7 per 100,000 in Summit County, Colorado, to 503.1 per 100,000 in Union County, Florida.
“Such significant disparities among US counties is unacceptable,” Dr Mokdad said. “Every person should have access to early screenings for cancer, as well as adequate treatment.”
Mortality rates for hematologic malignancies
In 2014, the mortality rates, per 100,000 people, for hematologic malignancies were:
- 0.4 for Hodgkin lymphoma (rank out of all cancers, 27)
- 8.3 for NHL (rank, 7)
- 3.9 for multiple myeloma (rank, 16)
- 9.0 for all leukemias (rank, 6)
- 0.7 for acute lymphoid leukemia (ALL)
- 2.6 for chronic lymphoid leukemia (CLL)
- 5.1 for AML
- 0.6 for chronic myeloid leukemia (CML).
The leukemia subtypes were not assigned a rank.
5-year survival rates for hematologic malignancies
Hodgkin lymphoma
- 30% for 1950-54
- 68.6% for 1973-77
- 72.1% for 1978-82
- 86.6% for 2008-2013
- Absolute difference (between the first and latest year of data), 56.6%.
NHL
- 33% for 1950-54
- 45.3% for 1973-77
- 48.7% for 1978-82
- 71.2% for 2008-2013
- Absolute difference, 38.2%.
Multiple myeloma
- 6% for 1950-54
- 23.4% for 1973-77
- 26.6% for 1978-82
- 49.8% for 2008-2013
- Absolute difference, 43.8%.
Leukemia
- 10% for 1950-54
- 34% for 1973-77
- 36.3% for 1978-82
- 60.1% for 2008-2013
- Absolute difference, 50.1%.
ALL
- 39.2% for 1973-77
- 50.5% for 1978-82
- 68.1% for 2008-2013
- Absolute difference, 28.9%.
CLL
- 67% for 1973-77
- 66.3% for 1978-82
- 82.5% for 2008-2013
- Absolute difference, 15.5%.
AML
- 6.2% for 1973-77
- 7.9% for 1978-82
- 27.4% for 2008-2013
- Absolute difference, 21.2%.
CML
- 21.1% for 1973-77
- 25.8% for 1978-82
- 66.4% for 2008-2013
- Absolute difference, 45.3%.
For the leukemia subtypes, there was no data for 1950 to 1954. ![]()
Health Canada expands indication for lenalidomide

Photo courtesy of Celgene
Health Canada has expanded the approved indication for lenalidomide (Revlimid®) to include the treatment of patients with multiple myeloma (MM).
Lenalidomide is now approved for use in combination with dexamethasone to treat patients newly diagnosed with MM who are not eligible for stem cell transplant.
Lenalidomide was previously approved in Canada for the treatment of patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes associated with a deletion 5q cytogenetic abnormality, with or without additional cytogenetic abnormalities.
Lenalidomide is a product of Celgene Corporation.
“The expanded indication of Revlimid® provides [MM] patients with a treatment much earlier in their disease and offers this patient population an all-oral, melphalan-free option for a disease that continues to be difficult to treat,” said Donna Reece, MD, of Princess Margaret Hospital in Toronto, Ontario, Canada.
The expanded approval of lenalidomide is based on safety and efficacy results from the phase 3 FIRST trial. Updated results from this study were published in the Journal of Clinical Oncology last November.
The trial included 1623 patients with newly diagnosed MM who were not eligible for stem cell transplant.
Patients were randomized to receive:
- Lenalidomide and low-dose dexamethasone (Rd) in 28-day cycles until disease progression (n=535)
- 18 cycles of Rd (Rd18) for 72 weeks (n=541)
- Melphalan, prednisone, and thalidomide (MPT) for 72 weeks (n=547).
In the intent-to-treat population, the overall response rate was 81% for the continuous Rd group, 79% for the Rd18 group, and 67% in the MPT group. The complete response rates were 21%, 20%, and 12%, respectively.
The median progression-free survival (PFS) was 26.0 months in the continuous Rd group, 21.0 months in the Rd18 group, and 21.9 months in the MPT group. At 4 years, the PFS rates were 33%, 14%, and 13%, respectively.
The median overall survival (OS) was 58.9 months in the continuous Rd group, 56.7 months in the Rd18 group, and 48.5 months in the MPT group. At 4 years, the OS rates were 60%, 57%, and 51%, respectively.
The most frequent grade 3/4 hematologic treatment-emergent adverse events were neutropenia and anemia. The rate of grade 3/4 neutropenia was higher in the MPT group than the continuous Rd or Rd18 groups.
Infections were the most common grade 3/4 non-hematologic treatment-emergent adverse events. The rate of grade 3/4 infections was higher in the Rd groups than the MPT group.
“With this new clinical evidence, we know that keeping newly diagnosed multiple myeloma patients on Revlimid® may help delay disease progression and reduce the risk of death,” Dr Reece said. “As such, we are looking forward to having Revlimid® as a key option in the first-line setting for the appropriate patients.” ![]()

Photo courtesy of Celgene
Health Canada has expanded the approved indication for lenalidomide (Revlimid®) to include the treatment of patients with multiple myeloma (MM).
Lenalidomide is now approved for use in combination with dexamethasone to treat patients newly diagnosed with MM who are not eligible for stem cell transplant.
Lenalidomide was previously approved in Canada for the treatment of patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes associated with a deletion 5q cytogenetic abnormality, with or without additional cytogenetic abnormalities.
Lenalidomide is a product of Celgene Corporation.
“The expanded indication of Revlimid® provides [MM] patients with a treatment much earlier in their disease and offers this patient population an all-oral, melphalan-free option for a disease that continues to be difficult to treat,” said Donna Reece, MD, of Princess Margaret Hospital in Toronto, Ontario, Canada.
The expanded approval of lenalidomide is based on safety and efficacy results from the phase 3 FIRST trial. Updated results from this study were published in the Journal of Clinical Oncology last November.
The trial included 1623 patients with newly diagnosed MM who were not eligible for stem cell transplant.
Patients were randomized to receive:
- Lenalidomide and low-dose dexamethasone (Rd) in 28-day cycles until disease progression (n=535)
- 18 cycles of Rd (Rd18) for 72 weeks (n=541)
- Melphalan, prednisone, and thalidomide (MPT) for 72 weeks (n=547).
In the intent-to-treat population, the overall response rate was 81% for the continuous Rd group, 79% for the Rd18 group, and 67% in the MPT group. The complete response rates were 21%, 20%, and 12%, respectively.
The median progression-free survival (PFS) was 26.0 months in the continuous Rd group, 21.0 months in the Rd18 group, and 21.9 months in the MPT group. At 4 years, the PFS rates were 33%, 14%, and 13%, respectively.
The median overall survival (OS) was 58.9 months in the continuous Rd group, 56.7 months in the Rd18 group, and 48.5 months in the MPT group. At 4 years, the OS rates were 60%, 57%, and 51%, respectively.
The most frequent grade 3/4 hematologic treatment-emergent adverse events were neutropenia and anemia. The rate of grade 3/4 neutropenia was higher in the MPT group than the continuous Rd or Rd18 groups.
Infections were the most common grade 3/4 non-hematologic treatment-emergent adverse events. The rate of grade 3/4 infections was higher in the Rd groups than the MPT group.
“With this new clinical evidence, we know that keeping newly diagnosed multiple myeloma patients on Revlimid® may help delay disease progression and reduce the risk of death,” Dr Reece said. “As such, we are looking forward to having Revlimid® as a key option in the first-line setting for the appropriate patients.” ![]()

Photo courtesy of Celgene
Health Canada has expanded the approved indication for lenalidomide (Revlimid®) to include the treatment of patients with multiple myeloma (MM).
Lenalidomide is now approved for use in combination with dexamethasone to treat patients newly diagnosed with MM who are not eligible for stem cell transplant.
Lenalidomide was previously approved in Canada for the treatment of patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes associated with a deletion 5q cytogenetic abnormality, with or without additional cytogenetic abnormalities.
Lenalidomide is a product of Celgene Corporation.
“The expanded indication of Revlimid® provides [MM] patients with a treatment much earlier in their disease and offers this patient population an all-oral, melphalan-free option for a disease that continues to be difficult to treat,” said Donna Reece, MD, of Princess Margaret Hospital in Toronto, Ontario, Canada.
The expanded approval of lenalidomide is based on safety and efficacy results from the phase 3 FIRST trial. Updated results from this study were published in the Journal of Clinical Oncology last November.
The trial included 1623 patients with newly diagnosed MM who were not eligible for stem cell transplant.
Patients were randomized to receive:
- Lenalidomide and low-dose dexamethasone (Rd) in 28-day cycles until disease progression (n=535)
- 18 cycles of Rd (Rd18) for 72 weeks (n=541)
- Melphalan, prednisone, and thalidomide (MPT) for 72 weeks (n=547).
In the intent-to-treat population, the overall response rate was 81% for the continuous Rd group, 79% for the Rd18 group, and 67% in the MPT group. The complete response rates were 21%, 20%, and 12%, respectively.
The median progression-free survival (PFS) was 26.0 months in the continuous Rd group, 21.0 months in the Rd18 group, and 21.9 months in the MPT group. At 4 years, the PFS rates were 33%, 14%, and 13%, respectively.
The median overall survival (OS) was 58.9 months in the continuous Rd group, 56.7 months in the Rd18 group, and 48.5 months in the MPT group. At 4 years, the OS rates were 60%, 57%, and 51%, respectively.
The most frequent grade 3/4 hematologic treatment-emergent adverse events were neutropenia and anemia. The rate of grade 3/4 neutropenia was higher in the MPT group than the continuous Rd or Rd18 groups.
Infections were the most common grade 3/4 non-hematologic treatment-emergent adverse events. The rate of grade 3/4 infections was higher in the Rd groups than the MPT group.
“With this new clinical evidence, we know that keeping newly diagnosed multiple myeloma patients on Revlimid® may help delay disease progression and reduce the risk of death,” Dr Reece said. “As such, we are looking forward to having Revlimid® as a key option in the first-line setting for the appropriate patients.” ![]()
Improving the efficacy of obinutuzumab

Preclinical research suggests that immune stimulation through Toll-like receptor 7 (TLR7) agonism can enhance the efficacy of obinutuzumab in lymphoma.
Researchers found that combining the anti-CD20 monoclonal antibody obinutuzumab with the TLR7 agonist R848 improved survival in lab mice with lymphoma.
The combination also demonstrated efficacy against chronic lymphocytic leukemia (CLL) cells in vitro.
Tim Illidge, PhD, MBBS, of the University of Manchester in the UK, and his colleagues reported these findings in the journal Leukemia.
The research was funded by the Kay Kendall Leukaemia Fund and Cancer Research UK in collaboration with Roche Pharmaceutical Research and Early Development.
The researchers said they initially found that R848 activates immune cells in vivo and enhances obinutuzumab-mediated antitumor effector mechanisms in vitro.
The team therefore went on to test R848 and obinutuzumab in C57Bl/6 mice bearing human CD20+ lymphoma (EL4). The mice received obinutuzumab modified to express the murine glycoengineered IgG2a Fc region (m2a) starting 1 day after tumor inoculation and systemic R848 once weekly for 4 weeks.
The researchers found that monotherapy with either obinutuzumab or R848 significantly improved survival compared to control (P<0.0001), but only 8% to 15% of mice that received monotherapy were long-term survivors (living more than 90 days).
Mice that received obinutuzumab in combination with R848 had significantly better survival than mice that received either monotherapy (P<0.0001). And about 70% of mice receiving the combination remained tumor-free out to 95 days.
Furthermore, long-term survivors that had received the combination treatment were protected from tumor re-challenge.
The researchers also tested the combination in a second model—human CD20 transgenic mice, which express the human CD20 antigen on normal B cells. The team said this model is more akin to the clinical situation.
The mice received treatment 7 days after the inoculation of EL4hCD20 cells. Mice that received obinutuzumab monotherapy had significantly better survival than control mice (P=0.02), but there were no long-term survivors. For mice that received R848 monotherapy, survival was not significantly different from that of controls.
Mice that received R848 in combination with obinutuzumab had significantly better survival than mice that received obinutuzumab alone (P=0.003).
In fact, 6 of the 12 mice that received the combination were long-term survivors. And 5 of these mice rejected tumor re-challenge.
“We were excited when we discovered that combining obinutuzumab with TLR7 activation significantly enhanced survival of animals with lymphoma by effectively eradicating tumors,” Dr Illidge said. “Clearly, more work needs to be done to assess the impact of this combination on humans, but this study is, nevertheless, very promising.”
The researchers said the primary antitumor activity of the combination is dependent on natural killer cells and CD4 helper T cells but not on CD8 killer T cells.
“While the combination therapy was highly effective, CD8 killer T cells did not play a major role in the therapy,” said Eleanor Cheadle, PhD, also of the University of Manchester.
“Given the important role that killer T cells can play in long-term protection from tumor regrowth, we are looking at ways to enhance activation of these cells after obinutuzumab therapy.”
The researchers also found that, in vitro, R848 significantly enhanced natural killer cell-mediated antibody-dependent cellular cytotoxicity against obinutuzumab-opsonized CLL cells and significantly increased non-specific, antibody-independent killing of CLL cells. ![]()

Preclinical research suggests that immune stimulation through Toll-like receptor 7 (TLR7) agonism can enhance the efficacy of obinutuzumab in lymphoma.
Researchers found that combining the anti-CD20 monoclonal antibody obinutuzumab with the TLR7 agonist R848 improved survival in lab mice with lymphoma.
The combination also demonstrated efficacy against chronic lymphocytic leukemia (CLL) cells in vitro.
Tim Illidge, PhD, MBBS, of the University of Manchester in the UK, and his colleagues reported these findings in the journal Leukemia.
The research was funded by the Kay Kendall Leukaemia Fund and Cancer Research UK in collaboration with Roche Pharmaceutical Research and Early Development.
The researchers said they initially found that R848 activates immune cells in vivo and enhances obinutuzumab-mediated antitumor effector mechanisms in vitro.
The team therefore went on to test R848 and obinutuzumab in C57Bl/6 mice bearing human CD20+ lymphoma (EL4). The mice received obinutuzumab modified to express the murine glycoengineered IgG2a Fc region (m2a) starting 1 day after tumor inoculation and systemic R848 once weekly for 4 weeks.
The researchers found that monotherapy with either obinutuzumab or R848 significantly improved survival compared to control (P<0.0001), but only 8% to 15% of mice that received monotherapy were long-term survivors (living more than 90 days).
Mice that received obinutuzumab in combination with R848 had significantly better survival than mice that received either monotherapy (P<0.0001). And about 70% of mice receiving the combination remained tumor-free out to 95 days.
Furthermore, long-term survivors that had received the combination treatment were protected from tumor re-challenge.
The researchers also tested the combination in a second model—human CD20 transgenic mice, which express the human CD20 antigen on normal B cells. The team said this model is more akin to the clinical situation.
The mice received treatment 7 days after the inoculation of EL4hCD20 cells. Mice that received obinutuzumab monotherapy had significantly better survival than control mice (P=0.02), but there were no long-term survivors. For mice that received R848 monotherapy, survival was not significantly different from that of controls.
Mice that received R848 in combination with obinutuzumab had significantly better survival than mice that received obinutuzumab alone (P=0.003).
In fact, 6 of the 12 mice that received the combination were long-term survivors. And 5 of these mice rejected tumor re-challenge.
“We were excited when we discovered that combining obinutuzumab with TLR7 activation significantly enhanced survival of animals with lymphoma by effectively eradicating tumors,” Dr Illidge said. “Clearly, more work needs to be done to assess the impact of this combination on humans, but this study is, nevertheless, very promising.”
The researchers said the primary antitumor activity of the combination is dependent on natural killer cells and CD4 helper T cells but not on CD8 killer T cells.
“While the combination therapy was highly effective, CD8 killer T cells did not play a major role in the therapy,” said Eleanor Cheadle, PhD, also of the University of Manchester.
“Given the important role that killer T cells can play in long-term protection from tumor regrowth, we are looking at ways to enhance activation of these cells after obinutuzumab therapy.”
The researchers also found that, in vitro, R848 significantly enhanced natural killer cell-mediated antibody-dependent cellular cytotoxicity against obinutuzumab-opsonized CLL cells and significantly increased non-specific, antibody-independent killing of CLL cells. ![]()

Preclinical research suggests that immune stimulation through Toll-like receptor 7 (TLR7) agonism can enhance the efficacy of obinutuzumab in lymphoma.
Researchers found that combining the anti-CD20 monoclonal antibody obinutuzumab with the TLR7 agonist R848 improved survival in lab mice with lymphoma.
The combination also demonstrated efficacy against chronic lymphocytic leukemia (CLL) cells in vitro.
Tim Illidge, PhD, MBBS, of the University of Manchester in the UK, and his colleagues reported these findings in the journal Leukemia.
The research was funded by the Kay Kendall Leukaemia Fund and Cancer Research UK in collaboration with Roche Pharmaceutical Research and Early Development.
The researchers said they initially found that R848 activates immune cells in vivo and enhances obinutuzumab-mediated antitumor effector mechanisms in vitro.
The team therefore went on to test R848 and obinutuzumab in C57Bl/6 mice bearing human CD20+ lymphoma (EL4). The mice received obinutuzumab modified to express the murine glycoengineered IgG2a Fc region (m2a) starting 1 day after tumor inoculation and systemic R848 once weekly for 4 weeks.
The researchers found that monotherapy with either obinutuzumab or R848 significantly improved survival compared to control (P<0.0001), but only 8% to 15% of mice that received monotherapy were long-term survivors (living more than 90 days).
Mice that received obinutuzumab in combination with R848 had significantly better survival than mice that received either monotherapy (P<0.0001). And about 70% of mice receiving the combination remained tumor-free out to 95 days.
Furthermore, long-term survivors that had received the combination treatment were protected from tumor re-challenge.
The researchers also tested the combination in a second model—human CD20 transgenic mice, which express the human CD20 antigen on normal B cells. The team said this model is more akin to the clinical situation.
The mice received treatment 7 days after the inoculation of EL4hCD20 cells. Mice that received obinutuzumab monotherapy had significantly better survival than control mice (P=0.02), but there were no long-term survivors. For mice that received R848 monotherapy, survival was not significantly different from that of controls.
Mice that received R848 in combination with obinutuzumab had significantly better survival than mice that received obinutuzumab alone (P=0.003).
In fact, 6 of the 12 mice that received the combination were long-term survivors. And 5 of these mice rejected tumor re-challenge.
“We were excited when we discovered that combining obinutuzumab with TLR7 activation significantly enhanced survival of animals with lymphoma by effectively eradicating tumors,” Dr Illidge said. “Clearly, more work needs to be done to assess the impact of this combination on humans, but this study is, nevertheless, very promising.”
The researchers said the primary antitumor activity of the combination is dependent on natural killer cells and CD4 helper T cells but not on CD8 killer T cells.
“While the combination therapy was highly effective, CD8 killer T cells did not play a major role in the therapy,” said Eleanor Cheadle, PhD, also of the University of Manchester.
“Given the important role that killer T cells can play in long-term protection from tumor regrowth, we are looking at ways to enhance activation of these cells after obinutuzumab therapy.”
The researchers also found that, in vitro, R848 significantly enhanced natural killer cell-mediated antibody-dependent cellular cytotoxicity against obinutuzumab-opsonized CLL cells and significantly increased non-specific, antibody-independent killing of CLL cells.
CMA report reveals successes and shortcomings

The European Medicines Agency (EMA) has released a report showing both successes and room for improvement regarding conditional marketing authorizations (CMAs).
CMA is one of the tools available to regulators to support the development of and early access to drugs that address unmet medical needs of patients in the European Union.
Drugs are granted CMA if the public health benefit of their immediate availability is thought to outweigh the risk of an authorization on the basis of less comprehensive data than normally required.
A CMA is valid for 1 year. As part of the authorization, the drug’s developer is obliged to carry out further studies to obtain complete data.
The EMA’s Committee for Medicinal Products for Human Use (CHMP) assesses the data generated by these specific post-authorization obligations at least annually to ensure the balance of benefits and risks of the drug continues to remain positive.
At the end of its assessment, the CHMP issues a recommendation regarding the renewal of the CMA or its conversion into a standard marketing authorization.
Overview
The EMA’s report summarizes the experience with CMAs from the first use of this authorization type in 2006 until June 30, 2016.
During this time, a total of 30 drugs have received a CMA, including several
hematology drugs—Adcetris (brentuximab vedotin),
Arzerra (ofatumumab), Blincyto (blinatumomab), Bosulif (bosutinib), Darzalex (daratumumab), and Pixuvri (pixantrone).
Eleven CMAs have been converted into standard marketing authorizations (including Arzerra’s CMA), 2 have been withdrawn for commercial reasons, and 17 are still conditional authorizations.
None of the drugs that still have CMAs have been authorized for more than 5 years. And none of the CMAs issued since 2006 have had to be revoked or suspended.
Successes
According to the EMA’s analysis, marketing authorization holders comply with the specific obligations imposed by the agency.
More than 90% of completed specific obligations did not result in major changes of scope, and about 70% of specific obligations did not require an extension to the originally specified timelines.
The report shows that it took an average of 4 years to generate the additional data needed and to convert a CMA into a full marketing authorization.
This suggests patients with life-threatening or seriously debilitating conditions had access to promising drugs much earlier than they would have under standard authorization.
Areas for improvement
The EMA’s analysis also revealed room for improvement.
The report showed that, relatively frequently, CMA was first
considered only during the assessment of the drug application, which meant granting a CMA took longer than intended.
Therefore, the EMA recommends that drug developers engage in early dialogue with the EMA
and prospectively plan to apply for a CMA.
The agency said this should support
prompt assessment of such applications and could also facilitate prompt
completion of additional studies and timely availability of
comprehensive data.
The EMA said another area for improvement is engaging other stakeholders involved in bringing drugs to patients—in particular, Health Technology Assessment bodies—to facilitate the generation of all data needed for decision-making through one development program.

The European Medicines Agency (EMA) has released a report showing both successes and room for improvement regarding conditional marketing authorizations (CMAs).
CMA is one of the tools available to regulators to support the development of and early access to drugs that address unmet medical needs of patients in the European Union.
Drugs are granted CMA if the public health benefit of their immediate availability is thought to outweigh the risk of an authorization on the basis of less comprehensive data than normally required.
A CMA is valid for 1 year. As part of the authorization, the drug’s developer is obliged to carry out further studies to obtain complete data.
The EMA’s Committee for Medicinal Products for Human Use (CHMP) assesses the data generated by these specific post-authorization obligations at least annually to ensure the balance of benefits and risks of the drug continues to remain positive.
At the end of its assessment, the CHMP issues a recommendation regarding the renewal of the CMA or its conversion into a standard marketing authorization.
Overview
The EMA’s report summarizes the experience with CMAs from the first use of this authorization type in 2006 until June 30, 2016.
During this time, a total of 30 drugs have received a CMA, including several
hematology drugs—Adcetris (brentuximab vedotin),
Arzerra (ofatumumab), Blincyto (blinatumomab), Bosulif (bosutinib), Darzalex (daratumumab), and Pixuvri (pixantrone).
Eleven CMAs have been converted into standard marketing authorizations (including Arzerra’s CMA), 2 have been withdrawn for commercial reasons, and 17 are still conditional authorizations.
None of the drugs that still have CMAs have been authorized for more than 5 years. And none of the CMAs issued since 2006 have had to be revoked or suspended.
Successes
According to the EMA’s analysis, marketing authorization holders comply with the specific obligations imposed by the agency.
More than 90% of completed specific obligations did not result in major changes of scope, and about 70% of specific obligations did not require an extension to the originally specified timelines.
The report shows that it took an average of 4 years to generate the additional data needed and to convert a CMA into a full marketing authorization.
This suggests patients with life-threatening or seriously debilitating conditions had access to promising drugs much earlier than they would have under standard authorization.
Areas for improvement
The EMA’s analysis also revealed room for improvement.
The report showed that, relatively frequently, CMA was first
considered only during the assessment of the drug application, which meant granting a CMA took longer than intended.
Therefore, the EMA recommends that drug developers engage in early dialogue with the EMA
and prospectively plan to apply for a CMA.
The agency said this should support
prompt assessment of such applications and could also facilitate prompt
completion of additional studies and timely availability of
comprehensive data.
The EMA said another area for improvement is engaging other stakeholders involved in bringing drugs to patients—in particular, Health Technology Assessment bodies—to facilitate the generation of all data needed for decision-making through one development program.

The European Medicines Agency (EMA) has released a report showing both successes and room for improvement regarding conditional marketing authorizations (CMAs).
CMA is one of the tools available to regulators to support the development of and early access to drugs that address unmet medical needs of patients in the European Union.
Drugs are granted CMA if the public health benefit of their immediate availability is thought to outweigh the risk of an authorization on the basis of less comprehensive data than normally required.
A CMA is valid for 1 year. As part of the authorization, the drug’s developer is obliged to carry out further studies to obtain complete data.
The EMA’s Committee for Medicinal Products for Human Use (CHMP) assesses the data generated by these specific post-authorization obligations at least annually to ensure the balance of benefits and risks of the drug continues to remain positive.
At the end of its assessment, the CHMP issues a recommendation regarding the renewal of the CMA or its conversion into a standard marketing authorization.
Overview
The EMA’s report summarizes the experience with CMAs from the first use of this authorization type in 2006 until June 30, 2016.
During this time, a total of 30 drugs have received a CMA, including several
hematology drugs—Adcetris (brentuximab vedotin),
Arzerra (ofatumumab), Blincyto (blinatumomab), Bosulif (bosutinib), Darzalex (daratumumab), and Pixuvri (pixantrone).
Eleven CMAs have been converted into standard marketing authorizations (including Arzerra’s CMA), 2 have been withdrawn for commercial reasons, and 17 are still conditional authorizations.
None of the drugs that still have CMAs have been authorized for more than 5 years. And none of the CMAs issued since 2006 have had to be revoked or suspended.
Successes
According to the EMA’s analysis, marketing authorization holders comply with the specific obligations imposed by the agency.
More than 90% of completed specific obligations did not result in major changes of scope, and about 70% of specific obligations did not require an extension to the originally specified timelines.
The report shows that it took an average of 4 years to generate the additional data needed and to convert a CMA into a full marketing authorization.
This suggests patients with life-threatening or seriously debilitating conditions had access to promising drugs much earlier than they would have under standard authorization.
Areas for improvement
The EMA’s analysis also revealed room for improvement.
The report showed that, relatively frequently, CMA was first
considered only during the assessment of the drug application, which meant granting a CMA took longer than intended.
Therefore, the EMA recommends that drug developers engage in early dialogue with the EMA
and prospectively plan to apply for a CMA.
The agency said this should support
prompt assessment of such applications and could also facilitate prompt
completion of additional studies and timely availability of
comprehensive data.
The EMA said another area for improvement is engaging other stakeholders involved in bringing drugs to patients—in particular, Health Technology Assessment bodies—to facilitate the generation of all data needed for decision-making through one development program.
Iron-fortified nutrition bars combat anemia in India

Consuming an iron-fortified nutrition bar daily for a few months can fight anemia without producing side effects, according to research published in the American Journal of Clinical Nutrition.
Anemic
women in India who consumed an iron-fortified nutrition bar each day for 90 days
were much more likely to experience increases in hemoglobin and
hematocrit and to be cured of their anemia than women who did not consume
such bars.
Rajvi Mehta, a medical student at Duke University in Durham, North Carolina, developed the nutrition bars used in this study, known as GudNesS bars.
The bars are made with iron-rich, natural, local (to India), and culturally accepted ingredients. They contain the World Health Organization’s daily recommended dose of iron.
In 2011, Mehta worked with nutritionists and physicians in India to establish a social venture there called Let’s Be Well Red (LBWR) to begin large-scale production of the bars.
The study, conducted from March to August 2014 in Mumbai and Navi Mumbai, India, involved 179 anemic, non-pregnant participants of reproductive age (18-35) at 10 demographically diverse sites.
The sites were randomly placed in either a control group or an intervention group.
Women in the intervention group received 1 iron-fortified nutrition bar (containing 14 mg Fe) daily for 90 days, and women in the control group received nothing. Baseline characteristics were comparable between the groups.
Each group underwent 3 blood tests during the 90-day follow-up period—at 15 days, 45 days, and 90 days—to measure their hemoglobin and hematocrit.
Seventy-six percent of subjects (n=136) completed all follow-up assessments (65 intervention and 71 control subjects).
The primary outcomes were 90-day changes from baseline in hemoglobin concentrations and hematocrit percentages.
The researchers said the mean hemoglobin and hematocrit increases after 90 days were greater for the intervention group than the control group, at 1.4 g/dL and 2.7%, respectively.
And subjects in the intervention group had a much greater decrease in anemia than those in the control group. At 90 days, 29.2% of subjects in the intervention group still had anemia, compared to 98.6% of those in the control group. The odds ratio was 0.007.
The researchers said no side effects were reported.
“We are encouraged by the results of this study, which show a positive connection between consuming an iron-fortified nutrition bar and a reduction in anemia prevalence,” said study author Elizabeth Turner, PhD, of Duke University.
“It appears to be a practical and well-tolerated solution to a significant health challenge in India.”
Let’s Be Well Red is currently operating in 3 locations in India and produces 100,000 bars each year that it distributes throughout the country.
“Anemia is a debilitating condition that can have severe health consequences,” Mehta said. “I am thrilled that my colleagues and I were able to develop a solution that has proven to be effective among a high-risk population. Making an impact in global health has long been a goal of mine.”

Consuming an iron-fortified nutrition bar daily for a few months can fight anemia without producing side effects, according to research published in the American Journal of Clinical Nutrition.
Anemic
women in India who consumed an iron-fortified nutrition bar each day for 90 days
were much more likely to experience increases in hemoglobin and
hematocrit and to be cured of their anemia than women who did not consume
such bars.
Rajvi Mehta, a medical student at Duke University in Durham, North Carolina, developed the nutrition bars used in this study, known as GudNesS bars.
The bars are made with iron-rich, natural, local (to India), and culturally accepted ingredients. They contain the World Health Organization’s daily recommended dose of iron.
In 2011, Mehta worked with nutritionists and physicians in India to establish a social venture there called Let’s Be Well Red (LBWR) to begin large-scale production of the bars.
The study, conducted from March to August 2014 in Mumbai and Navi Mumbai, India, involved 179 anemic, non-pregnant participants of reproductive age (18-35) at 10 demographically diverse sites.
The sites were randomly placed in either a control group or an intervention group.
Women in the intervention group received 1 iron-fortified nutrition bar (containing 14 mg Fe) daily for 90 days, and women in the control group received nothing. Baseline characteristics were comparable between the groups.
Each group underwent 3 blood tests during the 90-day follow-up period—at 15 days, 45 days, and 90 days—to measure their hemoglobin and hematocrit.
Seventy-six percent of subjects (n=136) completed all follow-up assessments (65 intervention and 71 control subjects).
The primary outcomes were 90-day changes from baseline in hemoglobin concentrations and hematocrit percentages.
The researchers said the mean hemoglobin and hematocrit increases after 90 days were greater for the intervention group than the control group, at 1.4 g/dL and 2.7%, respectively.
And subjects in the intervention group had a much greater decrease in anemia than those in the control group. At 90 days, 29.2% of subjects in the intervention group still had anemia, compared to 98.6% of those in the control group. The odds ratio was 0.007.
The researchers said no side effects were reported.
“We are encouraged by the results of this study, which show a positive connection between consuming an iron-fortified nutrition bar and a reduction in anemia prevalence,” said study author Elizabeth Turner, PhD, of Duke University.
“It appears to be a practical and well-tolerated solution to a significant health challenge in India.”
Let’s Be Well Red is currently operating in 3 locations in India and produces 100,000 bars each year that it distributes throughout the country.
“Anemia is a debilitating condition that can have severe health consequences,” Mehta said. “I am thrilled that my colleagues and I were able to develop a solution that has proven to be effective among a high-risk population. Making an impact in global health has long been a goal of mine.”

Consuming an iron-fortified nutrition bar daily for a few months can fight anemia without producing side effects, according to research published in the American Journal of Clinical Nutrition.
Anemic
women in India who consumed an iron-fortified nutrition bar each day for 90 days
were much more likely to experience increases in hemoglobin and
hematocrit and to be cured of their anemia than women who did not consume
such bars.
Rajvi Mehta, a medical student at Duke University in Durham, North Carolina, developed the nutrition bars used in this study, known as GudNesS bars.
The bars are made with iron-rich, natural, local (to India), and culturally accepted ingredients. They contain the World Health Organization’s daily recommended dose of iron.
In 2011, Mehta worked with nutritionists and physicians in India to establish a social venture there called Let’s Be Well Red (LBWR) to begin large-scale production of the bars.
The study, conducted from March to August 2014 in Mumbai and Navi Mumbai, India, involved 179 anemic, non-pregnant participants of reproductive age (18-35) at 10 demographically diverse sites.
The sites were randomly placed in either a control group or an intervention group.
Women in the intervention group received 1 iron-fortified nutrition bar (containing 14 mg Fe) daily for 90 days, and women in the control group received nothing. Baseline characteristics were comparable between the groups.
Each group underwent 3 blood tests during the 90-day follow-up period—at 15 days, 45 days, and 90 days—to measure their hemoglobin and hematocrit.
Seventy-six percent of subjects (n=136) completed all follow-up assessments (65 intervention and 71 control subjects).
The primary outcomes were 90-day changes from baseline in hemoglobin concentrations and hematocrit percentages.
The researchers said the mean hemoglobin and hematocrit increases after 90 days were greater for the intervention group than the control group, at 1.4 g/dL and 2.7%, respectively.
And subjects in the intervention group had a much greater decrease in anemia than those in the control group. At 90 days, 29.2% of subjects in the intervention group still had anemia, compared to 98.6% of those in the control group. The odds ratio was 0.007.
The researchers said no side effects were reported.
“We are encouraged by the results of this study, which show a positive connection between consuming an iron-fortified nutrition bar and a reduction in anemia prevalence,” said study author Elizabeth Turner, PhD, of Duke University.
“It appears to be a practical and well-tolerated solution to a significant health challenge in India.”
Let’s Be Well Red is currently operating in 3 locations in India and produces 100,000 bars each year that it distributes throughout the country.
“Anemia is a debilitating condition that can have severe health consequences,” Mehta said. “I am thrilled that my colleagues and I were able to develop a solution that has proven to be effective among a high-risk population. Making an impact in global health has long been a goal of mine.”
New recommendations for pediatric AMKL
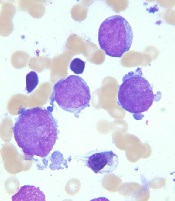
Image courtesy of St. Jude
Children’s Research Hospital
and Tina Motroni
Research has revealed genetic alterations that may prove useful for predicting treatment outcomes in pediatric patients with acute megakaryoblastic leukemia (AMKL) who do not have Down syndrome.
The study suggests that 3
genetic alterations can be used to identify high-risk patients who may benefit
from allogeneic stem cell transplant, and 1 alteration may identify
low-risk patients who require less chemotherapy than their peers.
Researchers said these findings, published in Nature Genetics, support revised diagnostic screening and treatment recommendations for pediatric AMKL.
“Because long-term survival for pediatric AMKL patients without Down syndrome is poor, just 14% to 34%, the standard recommendation by many pediatric oncologists has been to treat all patients with allogeneic stem cell transplantation during their first remission,” said study author Tanja Gruber, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“In this study, we identified several genetic alterations that are important predictors of treatment success. All newly identified pediatric AMKL patients without Down syndrome should be screened for these prognostic indicators at diagnosis. The results will help identify which patients need allogeneic stem cell transplants during their first remission and which do not.”
This study involved next-generation sequencing of the whole exome or RNA of 99 AMKL patients without Down syndrome (75 pediatric and 24 adult patients). Along with the sequencing data, researchers analyzed patients’ gene expression and long-term survival.
Results
The results showed that non-Down syndrome pediatric AMKL can be divided into 7 subgroups based on the underlying genetic alteration, pattern of gene expression, and treatment outcome.
The subgroups include the newly identified HOX subgroup. About 15% of the pediatric patients in this study were in the HOX subgroup, which is characterized by several different HOX fusion genes.
The researchers also identified cooperating mutations that help fuel AMKL in different subgroups. The cooperating mutations include changes in the RB1 gene and recurring mutations in the RAS and JAK pathways.
In addition, the study showed that 3 genetic alterations—CBFA2T3-GLIS2, KMT2A rearrangements, and NUP98-KDM5A—are associated with reduced survival in pediatric AMKL subtypes.
The researchers said patients with these alterations may benefit from allogeneic stem cell transplants, so non-Down syndrome pediatric AMKL patients should be screened for these alterations at diagnosis.
The team also recommended testing AMKL patients for mutations in the GATA1 gene. GATA1 mutations are a hallmark of AMKL in children with Down syndrome, who almost always survive the leukemia. In this study, AMKL patients with GATA1 mutations and no fusion gene had the same favorable outcomes.
“The results raise the possibility that pediatric AMKL patients without Down syndrome who have mutations in GATA1 may benefit from the same reduced chemotherapy used to treat the leukemia in patients with Down syndrome,” Dr Gruber said.
These revised diagnostic screening and treatment recommendations are being implemented at St. Jude.
This study also showed that adults with AMKL lacked recurrent fusion genes. The most common mutations found in the adult patients were in TP53 (21%), cohesin genes (17%), splicing factor genes (17%), ASXL genes (17%), and DNMT3A (13%). About 4% had GATA1 mutations.
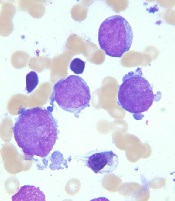
Image courtesy of St. Jude
Children’s Research Hospital
and Tina Motroni
Research has revealed genetic alterations that may prove useful for predicting treatment outcomes in pediatric patients with acute megakaryoblastic leukemia (AMKL) who do not have Down syndrome.
The study suggests that 3
genetic alterations can be used to identify high-risk patients who may benefit
from allogeneic stem cell transplant, and 1 alteration may identify
low-risk patients who require less chemotherapy than their peers.
Researchers said these findings, published in Nature Genetics, support revised diagnostic screening and treatment recommendations for pediatric AMKL.
“Because long-term survival for pediatric AMKL patients without Down syndrome is poor, just 14% to 34%, the standard recommendation by many pediatric oncologists has been to treat all patients with allogeneic stem cell transplantation during their first remission,” said study author Tanja Gruber, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“In this study, we identified several genetic alterations that are important predictors of treatment success. All newly identified pediatric AMKL patients without Down syndrome should be screened for these prognostic indicators at diagnosis. The results will help identify which patients need allogeneic stem cell transplants during their first remission and which do not.”
This study involved next-generation sequencing of the whole exome or RNA of 99 AMKL patients without Down syndrome (75 pediatric and 24 adult patients). Along with the sequencing data, researchers analyzed patients’ gene expression and long-term survival.
Results
The results showed that non-Down syndrome pediatric AMKL can be divided into 7 subgroups based on the underlying genetic alteration, pattern of gene expression, and treatment outcome.
The subgroups include the newly identified HOX subgroup. About 15% of the pediatric patients in this study were in the HOX subgroup, which is characterized by several different HOX fusion genes.
The researchers also identified cooperating mutations that help fuel AMKL in different subgroups. The cooperating mutations include changes in the RB1 gene and recurring mutations in the RAS and JAK pathways.
In addition, the study showed that 3 genetic alterations—CBFA2T3-GLIS2, KMT2A rearrangements, and NUP98-KDM5A—are associated with reduced survival in pediatric AMKL subtypes.
The researchers said patients with these alterations may benefit from allogeneic stem cell transplants, so non-Down syndrome pediatric AMKL patients should be screened for these alterations at diagnosis.
The team also recommended testing AMKL patients for mutations in the GATA1 gene. GATA1 mutations are a hallmark of AMKL in children with Down syndrome, who almost always survive the leukemia. In this study, AMKL patients with GATA1 mutations and no fusion gene had the same favorable outcomes.
“The results raise the possibility that pediatric AMKL patients without Down syndrome who have mutations in GATA1 may benefit from the same reduced chemotherapy used to treat the leukemia in patients with Down syndrome,” Dr Gruber said.
These revised diagnostic screening and treatment recommendations are being implemented at St. Jude.
This study also showed that adults with AMKL lacked recurrent fusion genes. The most common mutations found in the adult patients were in TP53 (21%), cohesin genes (17%), splicing factor genes (17%), ASXL genes (17%), and DNMT3A (13%). About 4% had GATA1 mutations.
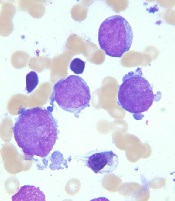
Image courtesy of St. Jude
Children’s Research Hospital
and Tina Motroni
Research has revealed genetic alterations that may prove useful for predicting treatment outcomes in pediatric patients with acute megakaryoblastic leukemia (AMKL) who do not have Down syndrome.
The study suggests that 3
genetic alterations can be used to identify high-risk patients who may benefit
from allogeneic stem cell transplant, and 1 alteration may identify
low-risk patients who require less chemotherapy than their peers.
Researchers said these findings, published in Nature Genetics, support revised diagnostic screening and treatment recommendations for pediatric AMKL.
“Because long-term survival for pediatric AMKL patients without Down syndrome is poor, just 14% to 34%, the standard recommendation by many pediatric oncologists has been to treat all patients with allogeneic stem cell transplantation during their first remission,” said study author Tanja Gruber, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“In this study, we identified several genetic alterations that are important predictors of treatment success. All newly identified pediatric AMKL patients without Down syndrome should be screened for these prognostic indicators at diagnosis. The results will help identify which patients need allogeneic stem cell transplants during their first remission and which do not.”
This study involved next-generation sequencing of the whole exome or RNA of 99 AMKL patients without Down syndrome (75 pediatric and 24 adult patients). Along with the sequencing data, researchers analyzed patients’ gene expression and long-term survival.
Results
The results showed that non-Down syndrome pediatric AMKL can be divided into 7 subgroups based on the underlying genetic alteration, pattern of gene expression, and treatment outcome.
The subgroups include the newly identified HOX subgroup. About 15% of the pediatric patients in this study were in the HOX subgroup, which is characterized by several different HOX fusion genes.
The researchers also identified cooperating mutations that help fuel AMKL in different subgroups. The cooperating mutations include changes in the RB1 gene and recurring mutations in the RAS and JAK pathways.
In addition, the study showed that 3 genetic alterations—CBFA2T3-GLIS2, KMT2A rearrangements, and NUP98-KDM5A—are associated with reduced survival in pediatric AMKL subtypes.
The researchers said patients with these alterations may benefit from allogeneic stem cell transplants, so non-Down syndrome pediatric AMKL patients should be screened for these alterations at diagnosis.
The team also recommended testing AMKL patients for mutations in the GATA1 gene. GATA1 mutations are a hallmark of AMKL in children with Down syndrome, who almost always survive the leukemia. In this study, AMKL patients with GATA1 mutations and no fusion gene had the same favorable outcomes.
“The results raise the possibility that pediatric AMKL patients without Down syndrome who have mutations in GATA1 may benefit from the same reduced chemotherapy used to treat the leukemia in patients with Down syndrome,” Dr Gruber said.
These revised diagnostic screening and treatment recommendations are being implemented at St. Jude.
This study also showed that adults with AMKL lacked recurrent fusion genes. The most common mutations found in the adult patients were in TP53 (21%), cohesin genes (17%), splicing factor genes (17%), ASXL genes (17%), and DNMT3A (13%). About 4% had GATA1 mutations.