User login
American Association for the Surgery of Trauma (AAST): Annual Meeting
Pneumonia most deadly emergency surgery complication
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
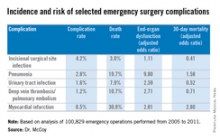
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
 |
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.
 |
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.
 |
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
Key clinical point: Target pneumonia for prevention after emergency general surgery.
Major finding: Emergency operations account for only 15% of all operations but more than half of postoperative deaths. Of the studied complications, pneumonia was associated with the greatest number of deaths after emergency general surgery.
Data source: Analysis of 100,829 emergency surgery cases in the American College of Surgeons National Surgical Quality Improvement Program database.
Disclosures: Dr. McCoy had no financial conflicts to disclose.
Splenectomy rare after first 24 hours in trauma, early trial results show
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
PHILADELPHIA – Delayed splenectomy for delayed splenic rupture is a feared complication of forgoing surgery on a blunt spleen injury, but early results of the Splenic Injury Outcomes Trial show that the vast majority of trauma patients rarely need splenectomy after the first 24 hours, and the use of angiography and CT to monitor healing of the spleen in asymptomatic patients may not be necessary in most cases.
Dr. Ben Zarzaur of Indiana University, Indianapolis, reported on early results from the Splenic Injury Outcomes Trial study of 383 patients from 11 level 1 trauma centers. The aim of the study is to provide a snapshot of how trauma surgeons manage critically injured patients with a spleen injury. He presented the findings at the annual meeting of the American Association for the Surgery of Trauma, which sponsored the trial.
“Out of that cohort, the in-hospital risk of splenectomy after the first 24 hours was about 3.6%, and after discharge the risk out to 6 months was 0.27%,” Dr. Zarzaur reported. In all, 12 patients had their spleens removed within 10 days of injury, and 4 patients died of causes not spleen related. The trial followed 87% of enrolled patients for up to 6 months after treatment.
One goal of the trial was to determine if the use of angiography and follow-up CT were necessary in monitoring the spleen in critically injured patients. The findings may help clarify management of patients with grade 1 injuries, Dr. Zarzaur said. “These patients likely don’t need any further interventions, because no [individuals with] grade 1 injuries had a splenectomy after the first 24 hours,” he said.
“Patients probably need close observation for 10-14 days after blunt spleen injury, and that can occur as an inpatient or can be done as an outpatient with very explicit instructions to return to the hospital if they have signs or symptoms of bleeding,” he said.
The trial also evaluated whether embolization made a difference in salvaging spleens. “There was no statistical difference in splenectomy rates in patients who were embolized versus those who were not,” Dr. Zarzaur said. He noted, however, that in more patients with grade 3 injuries or greater, the incidence of splenectomy was lower after embolization, but it was not statistically significant. “With regard to angiography embolization, it’s likely helpful. There are probably some high-risk patient populations, and we should concentrate on those in order to maximize the benefit and minimize the risk of patients with blunt splenic injury,” he said.
“There are about 39,000 spleen injuries a year, about 35,000 of which will be managed nonoperatively successfully over 24 hours,” Dr. Zarzaur said after his presentation. “So if we do the calculations for all injury grades, if we do angiography in these patients at the rates we saw in the study, we would save 84 additional spleens. If we concentrate on just higher-grade injuries – just grades 3 to 5 – we might save an additional 274 spleens a year. I think we have to ask ourselves, is that worth all the effort and cost and radiation exposure of angiography?”
That’s not a question the trial authors can answer at this point, Dr. Zarzaur said. A larger randomized clinical trial would be in order to get there, so he said the next step for him and the Splenic Injury Outcomes Trial coauthors is to put together a protocol for that.
Dr. Zarzaur reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Follow-up angiography and CT may not be necessary for trauma patients with blunt spleen injury because of the low rates of splenectomy after 24 hours.
Major finding: Only 3.6% of trauma patients required in-hospital splenectomy between 24 hours and 9 days after surgery; the vast majority were discharged with spleen intact.
Data source: Splenic Injury Outcomes Trial, a prospective study involving 383 patients at 11 level 1 trauma centers.
Disclosures: Dr. Zarzaur reported having no relevant financial disclosures.
PROOVIT registry results make case for expansion
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at aastproovit@yahoo.com.
Dr. DuBose reported having no relevant financial disclosures.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at aastproovit@yahoo.com.
Dr. DuBose reported having no relevant financial disclosures.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at aastproovit@yahoo.com.
Dr. DuBose reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Gathering previously uncollected information on management of trauma-related vascular injuries can inform treatment and may improve outcomes.
Major finding: The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
Data source: The AAST PROOVIT registry involving 13 Level 1 and 1 Level 2 trauma centers with data on 542 injuries.
Disclosures: Dr. DuBose reported having no relevant financial disclosures.
Antihypertension drugs may have clotting protection in obese trauma patients
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
PHILADELPHIA – Antihypertension drugs may have a protective effect in obese trauma victims, while a better understanding of how obesity influences blood clotting may help trauma surgeons target treatment more effectively, according to early results from two trials involving obese patients.
“With the growing incidence of obesity, coupled with the increased incidence of trauma injury worldwide, elucidating the intimate associations between these two disease states is critical,” Dr. Lucy Kornblith of the University of California, San Francisco, said, reporting on a prospective analysis that determined that obese trauma victims have clotting properties superior to normal patients.
In another paper, investigators at the Washington University, St. Louis evaluated obese trauma victims who took ACE inhibitors or angiotensin receptor blocker (ARB) drugs before injury. “Obese patients who were not on ACE inhibitors or ARB drugs did develop organ failure, while those obese patients who took those medications did not,” Dr. Robert D. Winfield reported at the annual meeting of the American Association for the Surgery of Trauma.
The Washington University trial involved 1,932 patients, 94 of whom took the hypertension drugs and had body mass index (BMI) data available, a group that included 55 obese individuals. Obese subjects on the drugs had Marshall Multiple Organ Dysfunction and Denver-2 Postinjury Multiple Organ Failure trauma scores similar to nonobese patients either taking or not taking the drugs, 5.83 and 2.45, respectively, Dr. Winfield said.
He explained the drugs may enable cells in obese individuals to express more CD47, a cell surface marker that plays a role in monocyte maturation. “What we see in those obese patients taking ACE-I or ARB preinjury is not a perfect response, but it is better,” he said. “We see more cells expressing CD47, and as a result, we see improved cell maturation and tracking and the ability to battle, in particular, secondary insults.”
The next step involves animal research to see if ACE-I and ARB use before and after injury can modulate the immune response, which Washington University and the American College of Surgeons are funding, according to Dr. Winfield.
The UCSF study did not draw any definitive conclusion of the overall benefits or drawbacks of hypercoagulability in the obese after injury, Dr. Kornblith said, although it did suggest one significant deleterious effect in multivariate analysis. “We found that for every 5 kg/m2 increase in BMI, there was an 85% increase in the odds of developing a clinically significant thromboembolic complication,” she said.
The study, using data from “Inflammation and the Host Response to Injury” database, evaluated 377 patients with an average BMI of 25.8 kg/m2, about a quarter of whom were obese (average BMI 33 kg/m2). Obese patients had higher admission platelet counts (302.69 x 103mcL vs. 268.58 x 103mcL) and factor IX (134% vs. 119% activity), and lower D-dimer counts (1.88 vs. 4.00 mc/mL) than did normal weight patients. Thromboelastography measured stronger clot and higher levels of functional fibrinogen on admission in obese patients. These findings of hypercoagulability in the obese patients existed out to 24-120 hours after injury.
Dr. Kornblith acknowledged several limitations to the study. “We do not do a screening duplex ultrasound for DVTs [deep vein thromboses] at our institution,” she said. “There may also be a much higher incidence of nonclinically significant clots in this population; however, based on this, if anything, our numbers are really an underestimate reflecting only those that were clinically significant.”
More work needs to be done, Dr. Kornblith noted. “It is known that excess adipose tissue is far from inert, and it plays a cardinal role in the biology and physiology of obesity,” she said. “Untangling the complex interaction of inflammation, coagulation, and injury will really help contribute to a better understanding of the clinical outcome differences seen in obese patients after injury and may help with targeted treatment of this at-risk group.”
Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
FROM AATS ANNUAL MEETING
Key clinical point: ACE-I and ARB medications may help obese trauma patients maintain trauma scores similar to nonobese patients.
Major finding: Obese patients who took ACE inhibitors or ARB drugs before their injuries had trauma scores similar to nonobese trauma patients, while obese patients in a prospective study displayed hypercoagulability, compared with that of normal weight patients.
Data source: Analysis of data from Inflammation and the Host Response to Injury database, and prospective analysis of demographic, outcomes and laboratory measures of 377 patients of varying BMI.
Disclosures: Dr. Kornblith and Dr. Winfield reported having no financial disclosures.
Whole blood autotransfusion linked to fewer fluids, lower costs
PHILADELPHIA – Early whole-blood autotransfusion of severely injured trauma victims’ own blood, while employed frequently in the military, has been rare in civilian populations, but a recent trial has found it to be safe, effective, and less costly than customary allogeneic transfusions.
Dr. Peter Rhee, chief of trauma, critical care, burns, and emergency surgery at the University of Arizona Medical Center, Tucson, reported on results from a 6-year retrospective study at the annual meeting of the American Association for the Surgery of Trauma. The study evaluated 272 trauma patients in two centers in Tucson and Los Angeles County who required transfusions upon presentation in the emergency department.
“We did this because there is a lot of concern in animal and also human ex vivo laboratory type experiments [regarding] complications from coagulopathy and possibly even increasing the inflammatory processes. So we looked at those types of complications and found that there were no clinically significant complications we could identify in regard to coagulopathy or inflammatory processes with AT [autotransfusion],” Dr. Rhee said.
“But what we also found was that since getting a patient’s own blood back costs less, hospital costs would also be less.”
Patients who underwent AT vs. no AT received significantly less allogeneic packed red blood cells (10.3 vs. 12.1 units), platelets (5.2 vs. 7.9 units), and fresh frozen plasma (6.1 vs. 8.2 units) than patients who did not undergo transfusion.
The investigators reported that AT cost approximately $8,794 per patient vs. $10,7427 for allogeneic transfusions. Hospital costs ($42,156 vs. $43,963) were also lower without any appreciable difference in outcomes.
The trial population was split evenly between those receiving AT and those who did not. Demographics and injury characteristics were similar between the two groups.
“Autologous autotransfusion of blood collected through the chest tube was safe, is associated reduced allogeneic transfusion, and is associated with decreased hospital costs,” Dr. Rhee said. “I think this trial provides safety data for us to go on and do a larger prospective, multicenter study.”
Dr. Rhee reported having no relevant financial disclosures.
PHILADELPHIA – Early whole-blood autotransfusion of severely injured trauma victims’ own blood, while employed frequently in the military, has been rare in civilian populations, but a recent trial has found it to be safe, effective, and less costly than customary allogeneic transfusions.
Dr. Peter Rhee, chief of trauma, critical care, burns, and emergency surgery at the University of Arizona Medical Center, Tucson, reported on results from a 6-year retrospective study at the annual meeting of the American Association for the Surgery of Trauma. The study evaluated 272 trauma patients in two centers in Tucson and Los Angeles County who required transfusions upon presentation in the emergency department.
“We did this because there is a lot of concern in animal and also human ex vivo laboratory type experiments [regarding] complications from coagulopathy and possibly even increasing the inflammatory processes. So we looked at those types of complications and found that there were no clinically significant complications we could identify in regard to coagulopathy or inflammatory processes with AT [autotransfusion],” Dr. Rhee said.
“But what we also found was that since getting a patient’s own blood back costs less, hospital costs would also be less.”
Patients who underwent AT vs. no AT received significantly less allogeneic packed red blood cells (10.3 vs. 12.1 units), platelets (5.2 vs. 7.9 units), and fresh frozen plasma (6.1 vs. 8.2 units) than patients who did not undergo transfusion.
The investigators reported that AT cost approximately $8,794 per patient vs. $10,7427 for allogeneic transfusions. Hospital costs ($42,156 vs. $43,963) were also lower without any appreciable difference in outcomes.
The trial population was split evenly between those receiving AT and those who did not. Demographics and injury characteristics were similar between the two groups.
“Autologous autotransfusion of blood collected through the chest tube was safe, is associated reduced allogeneic transfusion, and is associated with decreased hospital costs,” Dr. Rhee said. “I think this trial provides safety data for us to go on and do a larger prospective, multicenter study.”
Dr. Rhee reported having no relevant financial disclosures.
PHILADELPHIA – Early whole-blood autotransfusion of severely injured trauma victims’ own blood, while employed frequently in the military, has been rare in civilian populations, but a recent trial has found it to be safe, effective, and less costly than customary allogeneic transfusions.
Dr. Peter Rhee, chief of trauma, critical care, burns, and emergency surgery at the University of Arizona Medical Center, Tucson, reported on results from a 6-year retrospective study at the annual meeting of the American Association for the Surgery of Trauma. The study evaluated 272 trauma patients in two centers in Tucson and Los Angeles County who required transfusions upon presentation in the emergency department.
“We did this because there is a lot of concern in animal and also human ex vivo laboratory type experiments [regarding] complications from coagulopathy and possibly even increasing the inflammatory processes. So we looked at those types of complications and found that there were no clinically significant complications we could identify in regard to coagulopathy or inflammatory processes with AT [autotransfusion],” Dr. Rhee said.
“But what we also found was that since getting a patient’s own blood back costs less, hospital costs would also be less.”
Patients who underwent AT vs. no AT received significantly less allogeneic packed red blood cells (10.3 vs. 12.1 units), platelets (5.2 vs. 7.9 units), and fresh frozen plasma (6.1 vs. 8.2 units) than patients who did not undergo transfusion.
The investigators reported that AT cost approximately $8,794 per patient vs. $10,7427 for allogeneic transfusions. Hospital costs ($42,156 vs. $43,963) were also lower without any appreciable difference in outcomes.
The trial population was split evenly between those receiving AT and those who did not. Demographics and injury characteristics were similar between the two groups.
“Autologous autotransfusion of blood collected through the chest tube was safe, is associated reduced allogeneic transfusion, and is associated with decreased hospital costs,” Dr. Rhee said. “I think this trial provides safety data for us to go on and do a larger prospective, multicenter study.”
Dr. Rhee reported having no relevant financial disclosures.
Key clinical point: Autotransfusion appears to be safe and cost-effective in trauma patients.
Major finding: Patients who underwent autotransfusion (AT) vs. no AT received significantly less allogeneic packed red blood cells (10.3 vs. 12.1 units), platelets (5.2 vs. 7.9 units), and fresh frozen plasma (6.1 vs. 8.2 units) than patients who did not undergo transfusion. Therapy expenses ($8,794 vs. $10,427) and hospital costs ($42,156 vs. $43,963) were also lower without any appreciable difference in outcomes.
Data source: Six-year, multi-institutional, retrospective study of 272 trauma patients, evenly divided between receiving AT and not receiving AT.
Disclosures: Dr. Rhee reported having no relevant financial disclosures.
Same-day combined ERCP and cholecystectomy: achievable and cost effective
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
FROM THE AAST ANNUAL MEETING
Key clinical point: Scheduling both ERCP and cholecystectomy on the same day reduces hospital stays and saves money.
Major finding: Patients who had preoperative endoscopic retrograde cholangiopancreatography (ERCP) on the same day as cholecystectomy had 3-day hospital stays compared to 5 days for patients who had the procedures on separate days.
Data source: Single-center retrospective study of 240 patients from 2010 to 2014.
Disclosures: Dr. Wild reported having no relevant financial disclosures.
Protocol for small-bowel obstruction
PHILADELPHIA – Closely monitoring patients admitted for small bowel obstruction every 4 hours and starting them on intravenous fluids, bowel rest, and nasogastric tube decompression may aid in quickly differentiating partial and complete SBO and direct them into targeted treatment earlier, according to investigators at the University of Florida Health, Gainesville.
“Despite the prevalence of small bowel obstruction and the fact that we’ve been dealing with it for more than a century, we still do not have a general consensus on how to differentiate between partial bowel obstruction and complete obstruction,” Dr. Janeen Jordan said at the annual meeting of the American Association for the Surgery of Trauma. Dr. Jordan reported on a study involving 91 patients admitted for SBO over 1 year at the University of Florida Health.
Early differentiation of partial vs. complete bowel obstruction and early intervention were goals of the protocol, Dr. Jordan said. “We really wanted to get them to surgery within 3 days with hopes of decreasing our bowel resection rate, hospital length of stay and, of course, mortality,” she said.
She outlined the protocol her institution used in symptomatic patients with x-ray findings positive for SBO: admission for intravenous fluid resuscitation, bowel rest, nasogastric tube decompression, and exams every 4 hours. Once stabilized, patients received a CT scan with only intravenous contrast to confirm the diagnosis. “If there was any suggestion of bowel compromise such as pneumatosis, mesenteric edema, or suggestion of a closed-loop obstruction, they were evaluated immediately for operation,” Dr. Jordan said. “If patients had none of those findings or had fecalization, which suggests a chronic problem instead of an acute issue, those patients were admitted for bowel decompression and IV fluid resuscitation.”
After resuscitation, patients with peritonitis or CT imaging positive for bowel compromise had exploratory surgery. All other patients received an osmotically active, water-soluble contrast agent and diagnostic imaging at 4, 8, 12 and 24 hours. If contrast did not reach the colon in 24 hours, the patient underwent exploratory surgery.
Twenty-six patients went directly to the OR without entering the protocol, 58% of whom required bowel resection, Dr. Jordan said. Among the 75 patients in the protocol, 43% required surgery. The average time to surgery was within 1 day for those not on the protocol and 2 days for those managed with contrast. Demographics between the two groups were similar, although the nonprotocol patients were more likely to have bowel wall thickening on CT scan.
The analysis also compared patients who received contrast and those who did not, and further broke that down into patients who had surgery vs. nonoperative management in each group. “Giving them contrast didn’t increase hospital length of stay,” Dr. Jordan said. “And the patients who didn’t get surgery had an overall hospital length of stay of 3-4 days; if they had surgery, regardless whether or not they received contrast, their hospital length of stay was approximately 10 days.” Additionally, the length of time for the contrast to reach the colon was predictive of who would fail at eating or drinking by mouth or have recurrent symptoms before discharge.
Discussant Dr. Clay Cothren Burlew of Denver Health said she found the concept of a protocol for patients with symptoms of SBO “incredibly appealing.” However, she added, “Patients without overt clinical signs of peritonitis mandating operative intervention are often fraught with challenges. Questions of the timing of intervention to bring about resolution have never really been met. It’s a gray zone in surgery.”
Dr. Martin Schreiber of Oregon Health & Science University, Portland, questioned the cost involved in imaging without contrast. “Instead of doing a CT scan without enteral contrast and then doing an upper GI, why not do the CT with enteral contrast and then do your follow-up x-rays to see if contrast reaches the colon? Skip a step and save lots of money.”
Dr. Ronald Maier of the University of Washington, Seattle, pointed out the protocol seeks to rule out surgery for a patient population that’s unlikely to have surgery anyway. “We know, as many studies have presented, 85% of these people – if you never operate on them – go home without an operation and they do fine,” he said. “So you’re hunting for the 15%, and yet in your protocol you operate on nearly half of them.”
Previously published studies that linked interventions after 3 days in the hospital with higher bowel resection and mortality determined the timing of surgery in the protocol, Dr. Jordan said. However, she admitted that the rate of surgery was lower at the end of the study period than at the beginning.
Dr. Jordan reported having no financial disclosures.
PHILADELPHIA – Closely monitoring patients admitted for small bowel obstruction every 4 hours and starting them on intravenous fluids, bowel rest, and nasogastric tube decompression may aid in quickly differentiating partial and complete SBO and direct them into targeted treatment earlier, according to investigators at the University of Florida Health, Gainesville.
“Despite the prevalence of small bowel obstruction and the fact that we’ve been dealing with it for more than a century, we still do not have a general consensus on how to differentiate between partial bowel obstruction and complete obstruction,” Dr. Janeen Jordan said at the annual meeting of the American Association for the Surgery of Trauma. Dr. Jordan reported on a study involving 91 patients admitted for SBO over 1 year at the University of Florida Health.
Early differentiation of partial vs. complete bowel obstruction and early intervention were goals of the protocol, Dr. Jordan said. “We really wanted to get them to surgery within 3 days with hopes of decreasing our bowel resection rate, hospital length of stay and, of course, mortality,” she said.
She outlined the protocol her institution used in symptomatic patients with x-ray findings positive for SBO: admission for intravenous fluid resuscitation, bowel rest, nasogastric tube decompression, and exams every 4 hours. Once stabilized, patients received a CT scan with only intravenous contrast to confirm the diagnosis. “If there was any suggestion of bowel compromise such as pneumatosis, mesenteric edema, or suggestion of a closed-loop obstruction, they were evaluated immediately for operation,” Dr. Jordan said. “If patients had none of those findings or had fecalization, which suggests a chronic problem instead of an acute issue, those patients were admitted for bowel decompression and IV fluid resuscitation.”
After resuscitation, patients with peritonitis or CT imaging positive for bowel compromise had exploratory surgery. All other patients received an osmotically active, water-soluble contrast agent and diagnostic imaging at 4, 8, 12 and 24 hours. If contrast did not reach the colon in 24 hours, the patient underwent exploratory surgery.
Twenty-six patients went directly to the OR without entering the protocol, 58% of whom required bowel resection, Dr. Jordan said. Among the 75 patients in the protocol, 43% required surgery. The average time to surgery was within 1 day for those not on the protocol and 2 days for those managed with contrast. Demographics between the two groups were similar, although the nonprotocol patients were more likely to have bowel wall thickening on CT scan.
The analysis also compared patients who received contrast and those who did not, and further broke that down into patients who had surgery vs. nonoperative management in each group. “Giving them contrast didn’t increase hospital length of stay,” Dr. Jordan said. “And the patients who didn’t get surgery had an overall hospital length of stay of 3-4 days; if they had surgery, regardless whether or not they received contrast, their hospital length of stay was approximately 10 days.” Additionally, the length of time for the contrast to reach the colon was predictive of who would fail at eating or drinking by mouth or have recurrent symptoms before discharge.
Discussant Dr. Clay Cothren Burlew of Denver Health said she found the concept of a protocol for patients with symptoms of SBO “incredibly appealing.” However, she added, “Patients without overt clinical signs of peritonitis mandating operative intervention are often fraught with challenges. Questions of the timing of intervention to bring about resolution have never really been met. It’s a gray zone in surgery.”
Dr. Martin Schreiber of Oregon Health & Science University, Portland, questioned the cost involved in imaging without contrast. “Instead of doing a CT scan without enteral contrast and then doing an upper GI, why not do the CT with enteral contrast and then do your follow-up x-rays to see if contrast reaches the colon? Skip a step and save lots of money.”
Dr. Ronald Maier of the University of Washington, Seattle, pointed out the protocol seeks to rule out surgery for a patient population that’s unlikely to have surgery anyway. “We know, as many studies have presented, 85% of these people – if you never operate on them – go home without an operation and they do fine,” he said. “So you’re hunting for the 15%, and yet in your protocol you operate on nearly half of them.”
Previously published studies that linked interventions after 3 days in the hospital with higher bowel resection and mortality determined the timing of surgery in the protocol, Dr. Jordan said. However, she admitted that the rate of surgery was lower at the end of the study period than at the beginning.
Dr. Jordan reported having no financial disclosures.
PHILADELPHIA – Closely monitoring patients admitted for small bowel obstruction every 4 hours and starting them on intravenous fluids, bowel rest, and nasogastric tube decompression may aid in quickly differentiating partial and complete SBO and direct them into targeted treatment earlier, according to investigators at the University of Florida Health, Gainesville.
“Despite the prevalence of small bowel obstruction and the fact that we’ve been dealing with it for more than a century, we still do not have a general consensus on how to differentiate between partial bowel obstruction and complete obstruction,” Dr. Janeen Jordan said at the annual meeting of the American Association for the Surgery of Trauma. Dr. Jordan reported on a study involving 91 patients admitted for SBO over 1 year at the University of Florida Health.
Early differentiation of partial vs. complete bowel obstruction and early intervention were goals of the protocol, Dr. Jordan said. “We really wanted to get them to surgery within 3 days with hopes of decreasing our bowel resection rate, hospital length of stay and, of course, mortality,” she said.
She outlined the protocol her institution used in symptomatic patients with x-ray findings positive for SBO: admission for intravenous fluid resuscitation, bowel rest, nasogastric tube decompression, and exams every 4 hours. Once stabilized, patients received a CT scan with only intravenous contrast to confirm the diagnosis. “If there was any suggestion of bowel compromise such as pneumatosis, mesenteric edema, or suggestion of a closed-loop obstruction, they were evaluated immediately for operation,” Dr. Jordan said. “If patients had none of those findings or had fecalization, which suggests a chronic problem instead of an acute issue, those patients were admitted for bowel decompression and IV fluid resuscitation.”
After resuscitation, patients with peritonitis or CT imaging positive for bowel compromise had exploratory surgery. All other patients received an osmotically active, water-soluble contrast agent and diagnostic imaging at 4, 8, 12 and 24 hours. If contrast did not reach the colon in 24 hours, the patient underwent exploratory surgery.
Twenty-six patients went directly to the OR without entering the protocol, 58% of whom required bowel resection, Dr. Jordan said. Among the 75 patients in the protocol, 43% required surgery. The average time to surgery was within 1 day for those not on the protocol and 2 days for those managed with contrast. Demographics between the two groups were similar, although the nonprotocol patients were more likely to have bowel wall thickening on CT scan.
The analysis also compared patients who received contrast and those who did not, and further broke that down into patients who had surgery vs. nonoperative management in each group. “Giving them contrast didn’t increase hospital length of stay,” Dr. Jordan said. “And the patients who didn’t get surgery had an overall hospital length of stay of 3-4 days; if they had surgery, regardless whether or not they received contrast, their hospital length of stay was approximately 10 days.” Additionally, the length of time for the contrast to reach the colon was predictive of who would fail at eating or drinking by mouth or have recurrent symptoms before discharge.
Discussant Dr. Clay Cothren Burlew of Denver Health said she found the concept of a protocol for patients with symptoms of SBO “incredibly appealing.” However, she added, “Patients without overt clinical signs of peritonitis mandating operative intervention are often fraught with challenges. Questions of the timing of intervention to bring about resolution have never really been met. It’s a gray zone in surgery.”
Dr. Martin Schreiber of Oregon Health & Science University, Portland, questioned the cost involved in imaging without contrast. “Instead of doing a CT scan without enteral contrast and then doing an upper GI, why not do the CT with enteral contrast and then do your follow-up x-rays to see if contrast reaches the colon? Skip a step and save lots of money.”
Dr. Ronald Maier of the University of Washington, Seattle, pointed out the protocol seeks to rule out surgery for a patient population that’s unlikely to have surgery anyway. “We know, as many studies have presented, 85% of these people – if you never operate on them – go home without an operation and they do fine,” he said. “So you’re hunting for the 15%, and yet in your protocol you operate on nearly half of them.”
Previously published studies that linked interventions after 3 days in the hospital with higher bowel resection and mortality determined the timing of surgery in the protocol, Dr. Jordan said. However, she admitted that the rate of surgery was lower at the end of the study period than at the beginning.
Dr. Jordan reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Protocol clarifies targeted treatment in SBO management.
Major finding: A quarter of patients with small bowel obstruction went directly to surgery based on imaging or exam findings, half of whom required bowel resection. The remainder were managed on a protocol to differentiate partial and complete bowl obstruction, 45% of whom needed surgery. Those in the protocol went to surgery within 2 days vs. 1 day for those not in the protocol.
Data source: Single-institution experience involved 101 admissions admitted for SBO over 1 year.
Disclosures: Dr. Jordan reported having no financial disclosures.
CTA before visceral arteriography improves bleed identification, localization
PHILADELPHIA – A protocol that employed CT angiography instead of or along with nuclear bleeding scans before visceral arteriography in patients with lower gastrointestinal hemorrhage helped localize bleeds more accurately and reduced the need for subsequent imaging studies, compared with VA alone, a single-center study found.
“CTA rather than a nuclear bleeding scan [NBS] prior to visceral arteriography is associated with fewer imaging studies but better localization of bleeding; if patients do receive more contrast, we did not observe any change in the renal function as a result,” Dr. Christina Jacovides of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the American Association for the Surgery of Trauma.
The study evaluated 161 patients over an 8-year observation period: 78 from 2005 to 2009, before the protocol was implemented; and 83 under the protocol.
“We saw that this protocol effectively changed the pre-VA approach from bleeding scans to CTA,” Dr. Jacovides said.
Lower gastrointestinal hemorrhage carries “substantial” morbidity, in the words of the study authors, so developing tools that can locate the bleeding and target treatment is critical in reducing deaths and complications, Dr. Jacovides said. “Bleeding scans have been demonstrated to be highly sensitive but have had poor localization, whereas CTA has also been demonstrated to be highly sensitive and provides localization similar to that seen with VA,” she said.
In the study, obtaining visceral arteriography without any imaging beforehand identified bleeding in 62% of cases, versus 94% with pre-VA imaging consisting of either CTA, NBS, or both. CTA only before VA resulted in more imaging studies than VA alone (2.5 vs. 1.3), but was also more than twice as likely to find bleeding (92% vs. 43%). Bleed localization rates were similar between VA only and pre-VA CTA.
When compared to NBS, CTA only before VA resulted in fewer imaging studies (2.1 vs. 2.5 for NBS) and similar rates of finding bleeding (around 94% for both), but significantly higher rates of bleed localization on VA (45.7% for CTA vs. 26.4% for NBS), according to the study findings. Embolization rates among the different protocols also varied, from 23% for NBS to 40% for CTA only before VA. The study did not evaluate costs.
How the university’s protocol affected renal function drew the attention of discussant Dr. Leslie Kobayashi,of the University of California, San Diego, who noted that creatinine levels were actually higher in the VA-only group. “This would suggest to me that patient factors such as severity of hemorrhage, presence of shock, and location of comorbidities are most associated with increases in creatinine rather than the actual contrast bolus or contrast dose,” she said. However, the study did not include a multivariate analysis to determine if CT contrast was associated with a rise in creatinine, Dr. Jacovides said.
Dr. Hasan Alam of the University of Michigan Health System, Ann Arbor, acknowledged that CTA before VA may be viable in hemodynamically stable patients, but not so for those with more critical injuries. “The problem is sometimes logistics, because you have to go to two different places for the CTA and VA, so a time factor is involved,” he said. “So if you have a sick patient who is robustly or briskly bleeding, who’s hypotensive, for those 5%-10% of patients, that causes a delay.”
Dr. Jacovides noted that at least among the patients who received pre-VA imaging, the protocol at the University of Pennsylvania actually got those patients to treatment quicker. “We did find that among patients who underwent CTA only instead of NBS, the time from the first scan to first VA was significantly reduced; it was about 1,200 minutes on bleeding scans and about 530 minutes with CTA on average,” she said.
Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
PHILADELPHIA – A protocol that employed CT angiography instead of or along with nuclear bleeding scans before visceral arteriography in patients with lower gastrointestinal hemorrhage helped localize bleeds more accurately and reduced the need for subsequent imaging studies, compared with VA alone, a single-center study found.
“CTA rather than a nuclear bleeding scan [NBS] prior to visceral arteriography is associated with fewer imaging studies but better localization of bleeding; if patients do receive more contrast, we did not observe any change in the renal function as a result,” Dr. Christina Jacovides of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the American Association for the Surgery of Trauma.
The study evaluated 161 patients over an 8-year observation period: 78 from 2005 to 2009, before the protocol was implemented; and 83 under the protocol.
“We saw that this protocol effectively changed the pre-VA approach from bleeding scans to CTA,” Dr. Jacovides said.
Lower gastrointestinal hemorrhage carries “substantial” morbidity, in the words of the study authors, so developing tools that can locate the bleeding and target treatment is critical in reducing deaths and complications, Dr. Jacovides said. “Bleeding scans have been demonstrated to be highly sensitive but have had poor localization, whereas CTA has also been demonstrated to be highly sensitive and provides localization similar to that seen with VA,” she said.
In the study, obtaining visceral arteriography without any imaging beforehand identified bleeding in 62% of cases, versus 94% with pre-VA imaging consisting of either CTA, NBS, or both. CTA only before VA resulted in more imaging studies than VA alone (2.5 vs. 1.3), but was also more than twice as likely to find bleeding (92% vs. 43%). Bleed localization rates were similar between VA only and pre-VA CTA.
When compared to NBS, CTA only before VA resulted in fewer imaging studies (2.1 vs. 2.5 for NBS) and similar rates of finding bleeding (around 94% for both), but significantly higher rates of bleed localization on VA (45.7% for CTA vs. 26.4% for NBS), according to the study findings. Embolization rates among the different protocols also varied, from 23% for NBS to 40% for CTA only before VA. The study did not evaluate costs.
How the university’s protocol affected renal function drew the attention of discussant Dr. Leslie Kobayashi,of the University of California, San Diego, who noted that creatinine levels were actually higher in the VA-only group. “This would suggest to me that patient factors such as severity of hemorrhage, presence of shock, and location of comorbidities are most associated with increases in creatinine rather than the actual contrast bolus or contrast dose,” she said. However, the study did not include a multivariate analysis to determine if CT contrast was associated with a rise in creatinine, Dr. Jacovides said.
Dr. Hasan Alam of the University of Michigan Health System, Ann Arbor, acknowledged that CTA before VA may be viable in hemodynamically stable patients, but not so for those with more critical injuries. “The problem is sometimes logistics, because you have to go to two different places for the CTA and VA, so a time factor is involved,” he said. “So if you have a sick patient who is robustly or briskly bleeding, who’s hypotensive, for those 5%-10% of patients, that causes a delay.”
Dr. Jacovides noted that at least among the patients who received pre-VA imaging, the protocol at the University of Pennsylvania actually got those patients to treatment quicker. “We did find that among patients who underwent CTA only instead of NBS, the time from the first scan to first VA was significantly reduced; it was about 1,200 minutes on bleeding scans and about 530 minutes with CTA on average,” she said.
Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
PHILADELPHIA – A protocol that employed CT angiography instead of or along with nuclear bleeding scans before visceral arteriography in patients with lower gastrointestinal hemorrhage helped localize bleeds more accurately and reduced the need for subsequent imaging studies, compared with VA alone, a single-center study found.
“CTA rather than a nuclear bleeding scan [NBS] prior to visceral arteriography is associated with fewer imaging studies but better localization of bleeding; if patients do receive more contrast, we did not observe any change in the renal function as a result,” Dr. Christina Jacovides of the University of Pennsylvania, Philadelphia, reported at the annual meeting of the American Association for the Surgery of Trauma.
The study evaluated 161 patients over an 8-year observation period: 78 from 2005 to 2009, before the protocol was implemented; and 83 under the protocol.
“We saw that this protocol effectively changed the pre-VA approach from bleeding scans to CTA,” Dr. Jacovides said.
Lower gastrointestinal hemorrhage carries “substantial” morbidity, in the words of the study authors, so developing tools that can locate the bleeding and target treatment is critical in reducing deaths and complications, Dr. Jacovides said. “Bleeding scans have been demonstrated to be highly sensitive but have had poor localization, whereas CTA has also been demonstrated to be highly sensitive and provides localization similar to that seen with VA,” she said.
In the study, obtaining visceral arteriography without any imaging beforehand identified bleeding in 62% of cases, versus 94% with pre-VA imaging consisting of either CTA, NBS, or both. CTA only before VA resulted in more imaging studies than VA alone (2.5 vs. 1.3), but was also more than twice as likely to find bleeding (92% vs. 43%). Bleed localization rates were similar between VA only and pre-VA CTA.
When compared to NBS, CTA only before VA resulted in fewer imaging studies (2.1 vs. 2.5 for NBS) and similar rates of finding bleeding (around 94% for both), but significantly higher rates of bleed localization on VA (45.7% for CTA vs. 26.4% for NBS), according to the study findings. Embolization rates among the different protocols also varied, from 23% for NBS to 40% for CTA only before VA. The study did not evaluate costs.
How the university’s protocol affected renal function drew the attention of discussant Dr. Leslie Kobayashi,of the University of California, San Diego, who noted that creatinine levels were actually higher in the VA-only group. “This would suggest to me that patient factors such as severity of hemorrhage, presence of shock, and location of comorbidities are most associated with increases in creatinine rather than the actual contrast bolus or contrast dose,” she said. However, the study did not include a multivariate analysis to determine if CT contrast was associated with a rise in creatinine, Dr. Jacovides said.
Dr. Hasan Alam of the University of Michigan Health System, Ann Arbor, acknowledged that CTA before VA may be viable in hemodynamically stable patients, but not so for those with more critical injuries. “The problem is sometimes logistics, because you have to go to two different places for the CTA and VA, so a time factor is involved,” he said. “So if you have a sick patient who is robustly or briskly bleeding, who’s hypotensive, for those 5%-10% of patients, that causes a delay.”
Dr. Jacovides noted that at least among the patients who received pre-VA imaging, the protocol at the University of Pennsylvania actually got those patients to treatment quicker. “We did find that among patients who underwent CTA only instead of NBS, the time from the first scan to first VA was significantly reduced; it was about 1,200 minutes on bleeding scans and about 530 minutes with CTA on average,” she said.
Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
AT THE AAST ANNUAL MEETING
Key clinical point: In patients with lower GI hemorrhage, performing CT angiography before visceral arteriography can improve diagnostic accuracy and reduce radiation exposure.
Major finding: CTA before VA vs. VA alone was more than twice as likely to find bleeds and reduce fluoroscopy times without affecting kidney function, and without subjecting patients to the radiation of a nuclear bleeding scan. The ability of CTA before VA to find bleeding was comparable to that of an NBS, with an ability to localize bleeding about 60% better than that of an NBS.
Data source: Single-center review of an interventional radiology database of 161 patients after implementation of institutional policy.
Disclosures: Dr. Jacovides reported having no relevant financial disclosures. She is a surgical intern at Thomas Jefferson University Hospital, Philadelphia, and completed this research as a medical student at the University of Pennsylvania, where the senior authors are in the division of traumatology, surgical critical care, and emergency surgery.
Repeat CT selectively in children with traumatic brain injuries
SAN FRANCISCO – Repeat CT scans in children with mild traumatic brain injury were not justified when done routinely but may be warranted for epidural hematomas, according to a retrospective study of 120 patients.
A comparison of the 106 patients who underwent repeat CT scans and the 14 who did not found that the two groups did not differ significantly based on their Injury Severity Score (ISS), the mechanism of injury, or the type of brain injury. Neurologic symptoms did not worsen in patients who did not get a repeat CT scan, none of whom needed surgery, Dr. Jarett K. Howe and his associates reported.
Repeat CT scans showed injury progression in 7 patients (7%), including 2 with subarachnoid hemorrhage and 5 with epidural hematoma –a third of the 15 epidural hematomas in the study. Two patients with epidural hematoma required craniotomy, one of whom showed worsening of clinical symptoms. All 106 patients who had repeat CT scans were discharged without sequelae, said Dr. Howe of Cardinal Glennon Children’s Medical Center, St. Louis University.
The investigators analyzed records for 435 children admitted with traumatic brain injury (TBI) between July 2004 and July 2012 who had CT evidence of an intracranial hemorrhage and a Glasgow Coma Scale score of 14-15, 120 of whom had complete data and met no exclusion criteria.
Children who got a repeat CT scan were significantly older (8 years of age) than those who didn’t (3 years), Dr. Howe reported at the annual meeting of the American Association for the Surgery of Trauma. "This is particularly interesting since CT scan usage is often justified by the difficulty in examining a young child," he said.
The mean Injury Severity Score was similar between groups: 15 in those scanned and 13 in those not scanned.
Although the type of injury did not influence the likelihood of repeat CT, all 15 patients with epidural hematoma got a repeat CT scan (100%), he noted. Repeat CT scans also were ordered in 94% of patients with subdural hematoma, 71% with contusion, 88% with intraparenchymal hemorrhage, 77% with subarachnoid hemorrhage, and 67% with intraventricular hemorrhage.
The TBIs were caused primarily by falls or motor vehicle accidents but also by assaults, sports, or being hit by a car as a pedestrian.
Every year in the United States approximately 642,000 children are evaluated in emergency departments for TBI, 65,000 are admitted, and 7,400 die of TBI. As many as 70% of these children get imaged, with head CT, the diagnostic modality of choice, Dr. Howe said. A total of 4%-8% of children undergoing a CT will have a skull or intracranial abnormality, and less than 1% will have an injury requiring neurosurgical intervention.
Radiation from the CT scan, however, may cause a fatal cancer later on in 1 of every 1,200 children scanned, an extrapolation of historical data from Hiroshima, Japan suggests, he said.
"A majority of our children with minor physiologic insults can be managed without repeat imaging," he said. The investigators now are organizing a multi-institutional study to validate the findings.
A previous prospective study that evaluated 42,412 children with head injuries found that 90% had isolated head trauma and 97% had a Glasgow Coma Scale score of 15 upon arrival in emergency rooms. Still, 35% underwent head CT scans, which identified TBI in 5%, and 0.4% underwent surgery. No patients died (Lancet 2009;374:1160-70).
Previous studies in adults also suggest that repeat CT is not necessary for mild TBI because patients requiring intervention will show deterioration on physical exam, Dr. Howe added. Repeat CT showed injury progression in 21% of 179 adults in one study, only 7 of whom needed surgical intervention (J. Trauma 2006;60:494-9).
Dr. Howe reported having no financial disclosures.
On Twitter @sherryboschert
Intuitively, this makes sense, and it’s something we want to believe.
No patient in the selective CT group developed progression of neurologic symptoms or required delayed intervention. In contrast, 7% of children undergoing scheduled or routine CT demonstrated progression, and a majority had epidural hematoma. Two required operative intervention, both as a result of expanding epidural hematoma. From this, the authors conclude that routine or scheduled CT is not indicated in absence of progression or epidural hematoma.
As I understand it, the purpose for repeat CT is to detect progression and the need for intervention. A consistent observation in a review of the literature demonstrates a wide discrepancy in the reported rates of CT progression with or without neurologic progression. Can we safely observe all lesions other than subdural hematoma and obtain CT only if neurologic symptoms progress? If so, for how long do we observe these patients?
The study has a limited number of patients. An appropriately powered noninferiority study to show a new treatment, selective CT, is not worse than existing CT would require nearly 6,000 patients in each arm.
The study provides a description of the lesions noted on CT in the two groups by type, yet it is difficult to determine if the two groups were truly comparable, since there’s a great deal of variability between lesions. Further complicating the analysis is not only the type of lesion but the location of the lesion. Outcomes between supratentorial and posterior fossa lesions can be significantly different regardless of the volume of blood. The findings also could have been influenced by the volume of blood and the time from initial injury to evaluation and imaging.
Dr. Denis D. Bensard is chief of pediatric surgery and trauma at Denver Health Medical Center. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
Intuitively, this makes sense, and it’s something we want to believe.
No patient in the selective CT group developed progression of neurologic symptoms or required delayed intervention. In contrast, 7% of children undergoing scheduled or routine CT demonstrated progression, and a majority had epidural hematoma. Two required operative intervention, both as a result of expanding epidural hematoma. From this, the authors conclude that routine or scheduled CT is not indicated in absence of progression or epidural hematoma.
As I understand it, the purpose for repeat CT is to detect progression and the need for intervention. A consistent observation in a review of the literature demonstrates a wide discrepancy in the reported rates of CT progression with or without neurologic progression. Can we safely observe all lesions other than subdural hematoma and obtain CT only if neurologic symptoms progress? If so, for how long do we observe these patients?
The study has a limited number of patients. An appropriately powered noninferiority study to show a new treatment, selective CT, is not worse than existing CT would require nearly 6,000 patients in each arm.
The study provides a description of the lesions noted on CT in the two groups by type, yet it is difficult to determine if the two groups were truly comparable, since there’s a great deal of variability between lesions. Further complicating the analysis is not only the type of lesion but the location of the lesion. Outcomes between supratentorial and posterior fossa lesions can be significantly different regardless of the volume of blood. The findings also could have been influenced by the volume of blood and the time from initial injury to evaluation and imaging.
Dr. Denis D. Bensard is chief of pediatric surgery and trauma at Denver Health Medical Center. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
Intuitively, this makes sense, and it’s something we want to believe.
No patient in the selective CT group developed progression of neurologic symptoms or required delayed intervention. In contrast, 7% of children undergoing scheduled or routine CT demonstrated progression, and a majority had epidural hematoma. Two required operative intervention, both as a result of expanding epidural hematoma. From this, the authors conclude that routine or scheduled CT is not indicated in absence of progression or epidural hematoma.
As I understand it, the purpose for repeat CT is to detect progression and the need for intervention. A consistent observation in a review of the literature demonstrates a wide discrepancy in the reported rates of CT progression with or without neurologic progression. Can we safely observe all lesions other than subdural hematoma and obtain CT only if neurologic symptoms progress? If so, for how long do we observe these patients?
The study has a limited number of patients. An appropriately powered noninferiority study to show a new treatment, selective CT, is not worse than existing CT would require nearly 6,000 patients in each arm.
The study provides a description of the lesions noted on CT in the two groups by type, yet it is difficult to determine if the two groups were truly comparable, since there’s a great deal of variability between lesions. Further complicating the analysis is not only the type of lesion but the location of the lesion. Outcomes between supratentorial and posterior fossa lesions can be significantly different regardless of the volume of blood. The findings also could have been influenced by the volume of blood and the time from initial injury to evaluation and imaging.
Dr. Denis D. Bensard is chief of pediatric surgery and trauma at Denver Health Medical Center. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Repeat CT scans in children with mild traumatic brain injury were not justified when done routinely but may be warranted for epidural hematomas, according to a retrospective study of 120 patients.
A comparison of the 106 patients who underwent repeat CT scans and the 14 who did not found that the two groups did not differ significantly based on their Injury Severity Score (ISS), the mechanism of injury, or the type of brain injury. Neurologic symptoms did not worsen in patients who did not get a repeat CT scan, none of whom needed surgery, Dr. Jarett K. Howe and his associates reported.
Repeat CT scans showed injury progression in 7 patients (7%), including 2 with subarachnoid hemorrhage and 5 with epidural hematoma –a third of the 15 epidural hematomas in the study. Two patients with epidural hematoma required craniotomy, one of whom showed worsening of clinical symptoms. All 106 patients who had repeat CT scans were discharged without sequelae, said Dr. Howe of Cardinal Glennon Children’s Medical Center, St. Louis University.
The investigators analyzed records for 435 children admitted with traumatic brain injury (TBI) between July 2004 and July 2012 who had CT evidence of an intracranial hemorrhage and a Glasgow Coma Scale score of 14-15, 120 of whom had complete data and met no exclusion criteria.
Children who got a repeat CT scan were significantly older (8 years of age) than those who didn’t (3 years), Dr. Howe reported at the annual meeting of the American Association for the Surgery of Trauma. "This is particularly interesting since CT scan usage is often justified by the difficulty in examining a young child," he said.
The mean Injury Severity Score was similar between groups: 15 in those scanned and 13 in those not scanned.
Although the type of injury did not influence the likelihood of repeat CT, all 15 patients with epidural hematoma got a repeat CT scan (100%), he noted. Repeat CT scans also were ordered in 94% of patients with subdural hematoma, 71% with contusion, 88% with intraparenchymal hemorrhage, 77% with subarachnoid hemorrhage, and 67% with intraventricular hemorrhage.
The TBIs were caused primarily by falls or motor vehicle accidents but also by assaults, sports, or being hit by a car as a pedestrian.
Every year in the United States approximately 642,000 children are evaluated in emergency departments for TBI, 65,000 are admitted, and 7,400 die of TBI. As many as 70% of these children get imaged, with head CT, the diagnostic modality of choice, Dr. Howe said. A total of 4%-8% of children undergoing a CT will have a skull or intracranial abnormality, and less than 1% will have an injury requiring neurosurgical intervention.
Radiation from the CT scan, however, may cause a fatal cancer later on in 1 of every 1,200 children scanned, an extrapolation of historical data from Hiroshima, Japan suggests, he said.
"A majority of our children with minor physiologic insults can be managed without repeat imaging," he said. The investigators now are organizing a multi-institutional study to validate the findings.
A previous prospective study that evaluated 42,412 children with head injuries found that 90% had isolated head trauma and 97% had a Glasgow Coma Scale score of 15 upon arrival in emergency rooms. Still, 35% underwent head CT scans, which identified TBI in 5%, and 0.4% underwent surgery. No patients died (Lancet 2009;374:1160-70).
Previous studies in adults also suggest that repeat CT is not necessary for mild TBI because patients requiring intervention will show deterioration on physical exam, Dr. Howe added. Repeat CT showed injury progression in 21% of 179 adults in one study, only 7 of whom needed surgical intervention (J. Trauma 2006;60:494-9).
Dr. Howe reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Repeat CT scans in children with mild traumatic brain injury were not justified when done routinely but may be warranted for epidural hematomas, according to a retrospective study of 120 patients.
A comparison of the 106 patients who underwent repeat CT scans and the 14 who did not found that the two groups did not differ significantly based on their Injury Severity Score (ISS), the mechanism of injury, or the type of brain injury. Neurologic symptoms did not worsen in patients who did not get a repeat CT scan, none of whom needed surgery, Dr. Jarett K. Howe and his associates reported.
Repeat CT scans showed injury progression in 7 patients (7%), including 2 with subarachnoid hemorrhage and 5 with epidural hematoma –a third of the 15 epidural hematomas in the study. Two patients with epidural hematoma required craniotomy, one of whom showed worsening of clinical symptoms. All 106 patients who had repeat CT scans were discharged without sequelae, said Dr. Howe of Cardinal Glennon Children’s Medical Center, St. Louis University.
The investigators analyzed records for 435 children admitted with traumatic brain injury (TBI) between July 2004 and July 2012 who had CT evidence of an intracranial hemorrhage and a Glasgow Coma Scale score of 14-15, 120 of whom had complete data and met no exclusion criteria.
Children who got a repeat CT scan were significantly older (8 years of age) than those who didn’t (3 years), Dr. Howe reported at the annual meeting of the American Association for the Surgery of Trauma. "This is particularly interesting since CT scan usage is often justified by the difficulty in examining a young child," he said.
The mean Injury Severity Score was similar between groups: 15 in those scanned and 13 in those not scanned.
Although the type of injury did not influence the likelihood of repeat CT, all 15 patients with epidural hematoma got a repeat CT scan (100%), he noted. Repeat CT scans also were ordered in 94% of patients with subdural hematoma, 71% with contusion, 88% with intraparenchymal hemorrhage, 77% with subarachnoid hemorrhage, and 67% with intraventricular hemorrhage.
The TBIs were caused primarily by falls or motor vehicle accidents but also by assaults, sports, or being hit by a car as a pedestrian.
Every year in the United States approximately 642,000 children are evaluated in emergency departments for TBI, 65,000 are admitted, and 7,400 die of TBI. As many as 70% of these children get imaged, with head CT, the diagnostic modality of choice, Dr. Howe said. A total of 4%-8% of children undergoing a CT will have a skull or intracranial abnormality, and less than 1% will have an injury requiring neurosurgical intervention.
Radiation from the CT scan, however, may cause a fatal cancer later on in 1 of every 1,200 children scanned, an extrapolation of historical data from Hiroshima, Japan suggests, he said.
"A majority of our children with minor physiologic insults can be managed without repeat imaging," he said. The investigators now are organizing a multi-institutional study to validate the findings.
A previous prospective study that evaluated 42,412 children with head injuries found that 90% had isolated head trauma and 97% had a Glasgow Coma Scale score of 15 upon arrival in emergency rooms. Still, 35% underwent head CT scans, which identified TBI in 5%, and 0.4% underwent surgery. No patients died (Lancet 2009;374:1160-70).
Previous studies in adults also suggest that repeat CT is not necessary for mild TBI because patients requiring intervention will show deterioration on physical exam, Dr. Howe added. Repeat CT showed injury progression in 21% of 179 adults in one study, only 7 of whom needed surgical intervention (J. Trauma 2006;60:494-9).
Dr. Howe reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Two of 106 children with mild TBI who had repeat CT scans underwent craniotomy (2%), 1 of whom had worsening clinical symptoms.
Data source: Retrospective review of 120 children evaluated for mild TBI at one institution.
Disclosures: Dr. Howe reported having no financial disclosures.