User login
Cardiovascular Research Foundation: Transcatheter Cardiovascular Therapeutics (TCT)
VIDEO: Identifying preexisting conditions crucial before pneumonectomy, even for benign disease
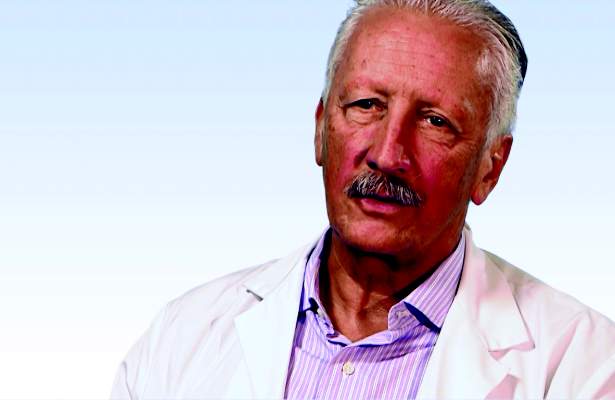
BOSTON – When performing pneumonectomy on patients with benign disease, it is important to be aware of specific preexisting conditions that could complicate surgery before bringing patients into the operating room.
“Sometimes the usual, standard operative procedure is not appropriate, given the circumstances of a particular patient, [and] typically, these pneumonectomies for benign disease are very challenging operations because the inflamed lung is usually quite densely adherent to the inside of the chest cavity,” explained Dr. G. Alex Patterson of Washington University in St. Louis.
In an interview at the Focus on Thoracic Surgery: Technical Challenges and Complications meeting sponsored by the American Association for Thoracic Surgeons, Dr. Patterson talked about the challenges associated with pneumonectomies for benign disease and how surgeons can safely navigate them.
Dr. Patterson had no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – When performing pneumonectomy on patients with benign disease, it is important to be aware of specific preexisting conditions that could complicate surgery before bringing patients into the operating room.
“Sometimes the usual, standard operative procedure is not appropriate, given the circumstances of a particular patient, [and] typically, these pneumonectomies for benign disease are very challenging operations because the inflamed lung is usually quite densely adherent to the inside of the chest cavity,” explained Dr. G. Alex Patterson of Washington University in St. Louis.
In an interview at the Focus on Thoracic Surgery: Technical Challenges and Complications meeting sponsored by the American Association for Thoracic Surgeons, Dr. Patterson talked about the challenges associated with pneumonectomies for benign disease and how surgeons can safely navigate them.
Dr. Patterson had no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – When performing pneumonectomy on patients with benign disease, it is important to be aware of specific preexisting conditions that could complicate surgery before bringing patients into the operating room.
“Sometimes the usual, standard operative procedure is not appropriate, given the circumstances of a particular patient, [and] typically, these pneumonectomies for benign disease are very challenging operations because the inflamed lung is usually quite densely adherent to the inside of the chest cavity,” explained Dr. G. Alex Patterson of Washington University in St. Louis.
In an interview at the Focus on Thoracic Surgery: Technical Challenges and Complications meeting sponsored by the American Association for Thoracic Surgeons, Dr. Patterson talked about the challenges associated with pneumonectomies for benign disease and how surgeons can safely navigate them.
Dr. Patterson had no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT AATS FOCUS ON THORACIC SURGERY
VIDEO: Drug-coated balloons offer in-stent restenosis option
SAN FRANCISCO – Drug-coated balloons have become a widely used option in Europe for treating coronary in-stent restenosis, and the scoring-balloon pretreatment tested in ISAR-DESIRE 4 appeared to boost the efficacy of a drug-coated balloon in a clinically meaningful way, Dr. Marco Valgimigli said in an interview at the Transcatheter Cardiovascular Therapeutics annual meeting.
When patients develop restenosis within a coronary stent, many times it’s because the stent was not properly expanded during initial placement. An advantage to a drug-coated balloon is that it pairs well with therapeutic reexpansion of the existing stent to its proper, fully open position.
In addition, this approach spares the patient from receiving a second stent inside the first stent, said Dr. Valgimigli, an interventional cardiologist at Inselspital in Bern, Switzerland.
Often when patients develop in-stent restenosis, it tends to keep recurring. And when that happens, eventually the only remaining option for effective revascularization of the patient’s coronary arteries is coronary bypass surgery.
Pretreating in-stent restenosis with a scoring balloon prior to treatment with a drug-coated balloon improved efficacy in the ISAR-DESIRE 4 trial by a modest amount. But if this treatment strategy can successfully defer or obviate just a few cases that might otherwise require coronary bypass surgery, then using the scoring balloon is a reasonable approach, Dr. Valgimigli said at the meeting, sponsored by the Cardiovascular Research Foundation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
SAN FRANCISCO – Drug-coated balloons have become a widely used option in Europe for treating coronary in-stent restenosis, and the scoring-balloon pretreatment tested in ISAR-DESIRE 4 appeared to boost the efficacy of a drug-coated balloon in a clinically meaningful way, Dr. Marco Valgimigli said in an interview at the Transcatheter Cardiovascular Therapeutics annual meeting.
When patients develop restenosis within a coronary stent, many times it’s because the stent was not properly expanded during initial placement. An advantage to a drug-coated balloon is that it pairs well with therapeutic reexpansion of the existing stent to its proper, fully open position.
In addition, this approach spares the patient from receiving a second stent inside the first stent, said Dr. Valgimigli, an interventional cardiologist at Inselspital in Bern, Switzerland.
Often when patients develop in-stent restenosis, it tends to keep recurring. And when that happens, eventually the only remaining option for effective revascularization of the patient’s coronary arteries is coronary bypass surgery.
Pretreating in-stent restenosis with a scoring balloon prior to treatment with a drug-coated balloon improved efficacy in the ISAR-DESIRE 4 trial by a modest amount. But if this treatment strategy can successfully defer or obviate just a few cases that might otherwise require coronary bypass surgery, then using the scoring balloon is a reasonable approach, Dr. Valgimigli said at the meeting, sponsored by the Cardiovascular Research Foundation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
SAN FRANCISCO – Drug-coated balloons have become a widely used option in Europe for treating coronary in-stent restenosis, and the scoring-balloon pretreatment tested in ISAR-DESIRE 4 appeared to boost the efficacy of a drug-coated balloon in a clinically meaningful way, Dr. Marco Valgimigli said in an interview at the Transcatheter Cardiovascular Therapeutics annual meeting.
When patients develop restenosis within a coronary stent, many times it’s because the stent was not properly expanded during initial placement. An advantage to a drug-coated balloon is that it pairs well with therapeutic reexpansion of the existing stent to its proper, fully open position.
In addition, this approach spares the patient from receiving a second stent inside the first stent, said Dr. Valgimigli, an interventional cardiologist at Inselspital in Bern, Switzerland.
Often when patients develop in-stent restenosis, it tends to keep recurring. And when that happens, eventually the only remaining option for effective revascularization of the patient’s coronary arteries is coronary bypass surgery.
Pretreating in-stent restenosis with a scoring balloon prior to treatment with a drug-coated balloon improved efficacy in the ISAR-DESIRE 4 trial by a modest amount. But if this treatment strategy can successfully defer or obviate just a few cases that might otherwise require coronary bypass surgery, then using the scoring balloon is a reasonable approach, Dr. Valgimigli said at the meeting, sponsored by the Cardiovascular Research Foundation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM TCT 2015
TCT: TAVR outcomes show further improvement
SAN FRANCISCO – The safety and efficacy of transcatheter aortic valve replacement keeps improving, with 1-year follow-up now available for two most-advanced systems on the U.S. market showing unprecedentedly low mortality and stroke rates in high-risk patients.
Continued improvements in safety and efficacy had cardiologists declaring that transcatheter aortic valve replacement (TAVR) is now the preferred strategy over surgery.
TAVR “should have a class I indication for high-risk patients as an alternative to surgery. That change needs to be made” based on the new data reported at the Transcatheter Cardiovascular Therapeutics annual meeting, said Dr. Martin B. Leon, director of the Center for Interventional Vascular Therapy of Columbia University in New York. TAVR currently has a class IIa recommendation as a “reasonable alternative” to surgery in patients at high surgical risk in the latest U.S. recommendations for treating aortic stenosis that came out in 2014.
One-year follow-up of 492 high-risk or inoperable patients who underwent TAVR with the SAPIEN 3 device system – the newest model from the SAPIEN series of TAVR systems and one of two next-generation systems now on the U.S. market – showed a 14% overall mortality rate and 2% stroke rate, Dr. Howard C. Herrmann reported at the meeting sponsored by the Cardiovascular Research Foundation. A combination of factors likely explained these strikingly low rates, including more refined patient selection, new device features, improved placement techniques, and more extensive operator experience, said Dr. Herrmann, professor and director of the cardiac catheterization laboratory at the University of Pennsylvania in Philadelphia.
The 1-year mortality rate of 14% in the SAPIEN3 (Safety and Performance Study of the Edwards SAPIEN 3 Transcatheter Heart Valve) study ran roughly half the rate seen in the large-scale test of the first-generation SAPIEN TAVR system, a study that began nearly 10 years ago (N Engl J Med. 2011 Jun 9;364[23]:2187-98). The 30-day results from this unblinded series of more than 500 patients treated with the SAPIEN 3 system, reported last Spring, led to Food and Drug Administration approval of the SAPIEN 3 system for U.S. marketing last June.“Our confidence in calling TAVR the preferred strategy just gets stronger when we have data like these,” commented Dr. Jeffrey J. Popma, professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
“The data show that TAVR is getting better,” said Dr. Samir Kapadia, professor and head of interventional cardiology at the Cleveland Clinic in Cleveland.
Similar 1-year results, though from many fewer patients, also came out at the meeting for the other next-generation TAVR system on the U.S. market, Evolut R, also approved by the FDA last June. Those data showed a 1-year mortality rate of 7% and a disabling stroke rate of 3% among 60 patients who had been treated with the Evolut R TAVR system.
Another notable finding from the SAPIEN 3 results was a moderate paravalvular leak (PVL) rate of 3% after 30 days and 4% after 1 year. No patients had a severe PVL at either 30 days or 1 year; the mild PVL rate at 1 year was 34%, and 62% had none or trace PVL. “The PVL rates are really dramatic,” commented Dr. Popma.
An analysis that correlated PVL severity at 30 days and mortality at 1 year showed that mild PVL linked with 14% mortality, essentially identical to the 12% mortality in patients with no or trace PVL after 30 days. In contrast, the 16 patients with moderate PVL after 30 days had a substantially increased 38% 1-year mortality, highlighting a patient subset that needs additional interventions.
“We need to look at these cases carefully” and determine what issues are causing more severe PVLs, said Dr. Herrmann. “We need to have no moderate PVLs.”
SAPIEN3 was sponsored by Edwards Lifesciences. Dr. Herrmann has received honoraria and research grants from Edwards as well as research grants from several other companies. He also own equity in Microinterventional Devices. Dr. Popma has been a consultant to Abbott Laboratories, Boston Scientific, and STENTYS, and he has been a speaker for Medtronic, Abbott Laboratories, Boston Scientific, Covidien, Cook Medical, and Direct Flow. Dr. Leon has been a consultant to Edwards. Dr. Kapadia had no disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – The safety and efficacy of transcatheter aortic valve replacement keeps improving, with 1-year follow-up now available for two most-advanced systems on the U.S. market showing unprecedentedly low mortality and stroke rates in high-risk patients.
Continued improvements in safety and efficacy had cardiologists declaring that transcatheter aortic valve replacement (TAVR) is now the preferred strategy over surgery.
TAVR “should have a class I indication for high-risk patients as an alternative to surgery. That change needs to be made” based on the new data reported at the Transcatheter Cardiovascular Therapeutics annual meeting, said Dr. Martin B. Leon, director of the Center for Interventional Vascular Therapy of Columbia University in New York. TAVR currently has a class IIa recommendation as a “reasonable alternative” to surgery in patients at high surgical risk in the latest U.S. recommendations for treating aortic stenosis that came out in 2014.
One-year follow-up of 492 high-risk or inoperable patients who underwent TAVR with the SAPIEN 3 device system – the newest model from the SAPIEN series of TAVR systems and one of two next-generation systems now on the U.S. market – showed a 14% overall mortality rate and 2% stroke rate, Dr. Howard C. Herrmann reported at the meeting sponsored by the Cardiovascular Research Foundation. A combination of factors likely explained these strikingly low rates, including more refined patient selection, new device features, improved placement techniques, and more extensive operator experience, said Dr. Herrmann, professor and director of the cardiac catheterization laboratory at the University of Pennsylvania in Philadelphia.
The 1-year mortality rate of 14% in the SAPIEN3 (Safety and Performance Study of the Edwards SAPIEN 3 Transcatheter Heart Valve) study ran roughly half the rate seen in the large-scale test of the first-generation SAPIEN TAVR system, a study that began nearly 10 years ago (N Engl J Med. 2011 Jun 9;364[23]:2187-98). The 30-day results from this unblinded series of more than 500 patients treated with the SAPIEN 3 system, reported last Spring, led to Food and Drug Administration approval of the SAPIEN 3 system for U.S. marketing last June.“Our confidence in calling TAVR the preferred strategy just gets stronger when we have data like these,” commented Dr. Jeffrey J. Popma, professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
“The data show that TAVR is getting better,” said Dr. Samir Kapadia, professor and head of interventional cardiology at the Cleveland Clinic in Cleveland.
Similar 1-year results, though from many fewer patients, also came out at the meeting for the other next-generation TAVR system on the U.S. market, Evolut R, also approved by the FDA last June. Those data showed a 1-year mortality rate of 7% and a disabling stroke rate of 3% among 60 patients who had been treated with the Evolut R TAVR system.
Another notable finding from the SAPIEN 3 results was a moderate paravalvular leak (PVL) rate of 3% after 30 days and 4% after 1 year. No patients had a severe PVL at either 30 days or 1 year; the mild PVL rate at 1 year was 34%, and 62% had none or trace PVL. “The PVL rates are really dramatic,” commented Dr. Popma.
An analysis that correlated PVL severity at 30 days and mortality at 1 year showed that mild PVL linked with 14% mortality, essentially identical to the 12% mortality in patients with no or trace PVL after 30 days. In contrast, the 16 patients with moderate PVL after 30 days had a substantially increased 38% 1-year mortality, highlighting a patient subset that needs additional interventions.
“We need to look at these cases carefully” and determine what issues are causing more severe PVLs, said Dr. Herrmann. “We need to have no moderate PVLs.”
SAPIEN3 was sponsored by Edwards Lifesciences. Dr. Herrmann has received honoraria and research grants from Edwards as well as research grants from several other companies. He also own equity in Microinterventional Devices. Dr. Popma has been a consultant to Abbott Laboratories, Boston Scientific, and STENTYS, and he has been a speaker for Medtronic, Abbott Laboratories, Boston Scientific, Covidien, Cook Medical, and Direct Flow. Dr. Leon has been a consultant to Edwards. Dr. Kapadia had no disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – The safety and efficacy of transcatheter aortic valve replacement keeps improving, with 1-year follow-up now available for two most-advanced systems on the U.S. market showing unprecedentedly low mortality and stroke rates in high-risk patients.
Continued improvements in safety and efficacy had cardiologists declaring that transcatheter aortic valve replacement (TAVR) is now the preferred strategy over surgery.
TAVR “should have a class I indication for high-risk patients as an alternative to surgery. That change needs to be made” based on the new data reported at the Transcatheter Cardiovascular Therapeutics annual meeting, said Dr. Martin B. Leon, director of the Center for Interventional Vascular Therapy of Columbia University in New York. TAVR currently has a class IIa recommendation as a “reasonable alternative” to surgery in patients at high surgical risk in the latest U.S. recommendations for treating aortic stenosis that came out in 2014.
One-year follow-up of 492 high-risk or inoperable patients who underwent TAVR with the SAPIEN 3 device system – the newest model from the SAPIEN series of TAVR systems and one of two next-generation systems now on the U.S. market – showed a 14% overall mortality rate and 2% stroke rate, Dr. Howard C. Herrmann reported at the meeting sponsored by the Cardiovascular Research Foundation. A combination of factors likely explained these strikingly low rates, including more refined patient selection, new device features, improved placement techniques, and more extensive operator experience, said Dr. Herrmann, professor and director of the cardiac catheterization laboratory at the University of Pennsylvania in Philadelphia.
The 1-year mortality rate of 14% in the SAPIEN3 (Safety and Performance Study of the Edwards SAPIEN 3 Transcatheter Heart Valve) study ran roughly half the rate seen in the large-scale test of the first-generation SAPIEN TAVR system, a study that began nearly 10 years ago (N Engl J Med. 2011 Jun 9;364[23]:2187-98). The 30-day results from this unblinded series of more than 500 patients treated with the SAPIEN 3 system, reported last Spring, led to Food and Drug Administration approval of the SAPIEN 3 system for U.S. marketing last June.“Our confidence in calling TAVR the preferred strategy just gets stronger when we have data like these,” commented Dr. Jeffrey J. Popma, professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
“The data show that TAVR is getting better,” said Dr. Samir Kapadia, professor and head of interventional cardiology at the Cleveland Clinic in Cleveland.
Similar 1-year results, though from many fewer patients, also came out at the meeting for the other next-generation TAVR system on the U.S. market, Evolut R, also approved by the FDA last June. Those data showed a 1-year mortality rate of 7% and a disabling stroke rate of 3% among 60 patients who had been treated with the Evolut R TAVR system.
Another notable finding from the SAPIEN 3 results was a moderate paravalvular leak (PVL) rate of 3% after 30 days and 4% after 1 year. No patients had a severe PVL at either 30 days or 1 year; the mild PVL rate at 1 year was 34%, and 62% had none or trace PVL. “The PVL rates are really dramatic,” commented Dr. Popma.
An analysis that correlated PVL severity at 30 days and mortality at 1 year showed that mild PVL linked with 14% mortality, essentially identical to the 12% mortality in patients with no or trace PVL after 30 days. In contrast, the 16 patients with moderate PVL after 30 days had a substantially increased 38% 1-year mortality, highlighting a patient subset that needs additional interventions.
“We need to look at these cases carefully” and determine what issues are causing more severe PVLs, said Dr. Herrmann. “We need to have no moderate PVLs.”
SAPIEN3 was sponsored by Edwards Lifesciences. Dr. Herrmann has received honoraria and research grants from Edwards as well as research grants from several other companies. He also own equity in Microinterventional Devices. Dr. Popma has been a consultant to Abbott Laboratories, Boston Scientific, and STENTYS, and he has been a speaker for Medtronic, Abbott Laboratories, Boston Scientific, Covidien, Cook Medical, and Direct Flow. Dr. Leon has been a consultant to Edwards. Dr. Kapadia had no disclosures.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point: A next-generation TAVR device showed excellent safety with 1-year follow-up of almost 500 patients.
Major finding: High-risk recipients of the SAPIEN 3 TAVR system had 1-year mortality of 14% and a 2% rate of disabling stroke.
Data source: SAPIEN3, an unblinded, single-arm study with 583 patients enrolled at 29 U.S. sites.
Disclosures: SAPIEN3 was sponsored by Edwards Lifesciences. Dr. Herrmann has received honoraria and research grants from Edwards as well as research grants from several other companies. He also own equity in Microinterventional Devices.
TCT: SAPIEN XT TAVR system gains valve-in-valve indication
SAN FRANCISCO – Food and Drug Administration approval of the SAPIEN XT transcatheter aortic valve for the valve-in-valve indication in high–surgical risk patients means that, officially, there are now two options for transcatheter replacement of a faulty prosthetic aortic valve.
CoreValve, the competing device for transcatheter aortic valve replacement (TAVR) in U.S. practice, received FDA approval for the valve-in-valve indication in March.
Researchers reported the data behind SAPIEN XT’s approval from two U.S. registries with a total of 197 high-risk patients at the Transcatheter Cardiovascular Therapeutics annual meeting on Oct. 16, the same day the FDA approval was announced by Edwards Lifesciences. The mortality rate was 4% after 30 days and 13% after 1 year, and the 1-year stroke rate was 4%, Dr. Danny Dvir said at the meeting.
One feature of the 1-year survival data that Dr. Dvir called “quite amazing” was the absence of any deaths during the first 30 days post TAVR with the SAPIEN XT system, and 7% at 1 year among the 100 patients treated during the final 8 months of the registry, who comprised the second half of patients enrolled in the registry. “I think we learned how to choose the right patients for this procedure,” said Dr. Dvir, an interventional cardiologist at St. Paul’s Hospital in Vancouver, B.C.
Given the risk from replacing a failed bioprosthetic valve by open surgery, “TAVR is becoming the preferred approach to valve-in-valve,” commented Dr. Ajay J. Kirtane, director of the cardiac catheterization laboratories at Columbia University in New York.
The registry results also highlighted a key limitation of the SAPIEN XT valve: patients with a bioprosthetic valve with a relatively narrow inner diameter of 21 mm or less.
Because the SAPIEN series of valves are balloon expandable and designed to sit directly in the aortic-valve annulus, the inner diameter of an existing bioprothesis can limit the TAVR options. The CoreValve, self-expanding valves sit in a supravalvular location and better fit through a narrow-frame existing valve.
This geometric limitation means that SAPIEN XT cannot work in patients with existing valves less than 21 mm in inner diameter, and the registry excluded such patients, who generally comprise about 10% of all patients with severe aortic stenosis.
In addition, among the 28% of patients enrolled in the registry who had an existing valve diameter of 21 mm, the 1-year mortality rate was strikingly high – 20% – compared with an 11% mortality rate in patients with existing valve diameters of 23 or 25 mm, Dr. Dvir reported.
“If a patient had a smaller inner diameter I’d definitely go with the supravalvular valve. For a bigger valve you have more choices,” commented Dr. Axel H.P. Linke, codirector of cardiology at the Heart Center at the University of Leipzig (Germany).
“It’s not fair to extrapolate these findings with SAPIEN XT to smaller [existing bioprosthetic] valves. There is the ability to go to lower inner diameters” using CoreValve, commented Dr. Jeffrey J. Popma, who led the U.S. CoreValve studies and is professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
The two sequential valve-in-valve U.S. registries for SAPIEN XT ran as part of the PARTNER 2 trial, designed to test the safety and efficacy of SAPIEN XT in patients undergoing TAVR for a de novo aortic valve. The 197 patients in the full registry averaged 79 years of age, 60% were men, their average Society of Thoracic Surgeons mortality risk score was 9.7%, 50% had atrial fibrillation, 95% had New York Heart Association class III or IV symptoms, and baseline screening identified one-third of the patients as frail.
The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems. Dr. Kirtane has received research grants from Boston Scientific, St. Jude, Eli Lilly, GlaxoSmithKline, Abiomed, and Abbott Vascular. Dr. Linke has been a consultant to Boston Scientific, St. Jude, Bard, Edwards, and Medtronic and owns equity in Claret. Dr. Popma has been principal investigator of the CoreValve studies, has been a consultant to Abbott Vascular, Boston Scientific, and Director Flow; he owns equity in Direct Flow, and he has received research grants from Abbott Vascular, Medtronic, Boston Scientific, and Cook Medical.
On Twitter @mitchelzoler
Transcatheter aortic valve replacement is on track to be the preferred treatment for aortic valve-in-valve replacement. How many surgeons are eager to do a reoperation on an aortic valve?
 |
Dr. David L. Brown |
Transcatheter valve replacement is the best way to treat aortic valve-in-valve disease. The results reported by Dr. Dvir further support that notion. One attraction of the balloon-expandable TAVR valve is that it greatly reduces the risk of annular rupture. But it is important to use a TAVR valve that is right sized. If the existing bioprosthesis is narrow then you have no choice but to use a self-expanding valve.
We had already been placing the SAPIEN XT, as well as SAPIEN 3 valves before XT received the valve-in-valve indication. In the past, when we did this we were never sure if the procedure would receive insurance coverage, but now XT should be covered because of the FDA approval, so this is a huge deal for us. It eliminates our economic uncertainty.
Dr. David L. Brown is director of interventional cardiology at the Heart Hospital Baylor Plano, Texas. He had no disclosures. He made these comments as a discussant at the meeting and in an interview.
Transcatheter aortic valve replacement is on track to be the preferred treatment for aortic valve-in-valve replacement. How many surgeons are eager to do a reoperation on an aortic valve?
 |
Dr. David L. Brown |
Transcatheter valve replacement is the best way to treat aortic valve-in-valve disease. The results reported by Dr. Dvir further support that notion. One attraction of the balloon-expandable TAVR valve is that it greatly reduces the risk of annular rupture. But it is important to use a TAVR valve that is right sized. If the existing bioprosthesis is narrow then you have no choice but to use a self-expanding valve.
We had already been placing the SAPIEN XT, as well as SAPIEN 3 valves before XT received the valve-in-valve indication. In the past, when we did this we were never sure if the procedure would receive insurance coverage, but now XT should be covered because of the FDA approval, so this is a huge deal for us. It eliminates our economic uncertainty.
Dr. David L. Brown is director of interventional cardiology at the Heart Hospital Baylor Plano, Texas. He had no disclosures. He made these comments as a discussant at the meeting and in an interview.
Transcatheter aortic valve replacement is on track to be the preferred treatment for aortic valve-in-valve replacement. How many surgeons are eager to do a reoperation on an aortic valve?
 |
Dr. David L. Brown |
Transcatheter valve replacement is the best way to treat aortic valve-in-valve disease. The results reported by Dr. Dvir further support that notion. One attraction of the balloon-expandable TAVR valve is that it greatly reduces the risk of annular rupture. But it is important to use a TAVR valve that is right sized. If the existing bioprosthesis is narrow then you have no choice but to use a self-expanding valve.
We had already been placing the SAPIEN XT, as well as SAPIEN 3 valves before XT received the valve-in-valve indication. In the past, when we did this we were never sure if the procedure would receive insurance coverage, but now XT should be covered because of the FDA approval, so this is a huge deal for us. It eliminates our economic uncertainty.
Dr. David L. Brown is director of interventional cardiology at the Heart Hospital Baylor Plano, Texas. He had no disclosures. He made these comments as a discussant at the meeting and in an interview.
SAN FRANCISCO – Food and Drug Administration approval of the SAPIEN XT transcatheter aortic valve for the valve-in-valve indication in high–surgical risk patients means that, officially, there are now two options for transcatheter replacement of a faulty prosthetic aortic valve.
CoreValve, the competing device for transcatheter aortic valve replacement (TAVR) in U.S. practice, received FDA approval for the valve-in-valve indication in March.
Researchers reported the data behind SAPIEN XT’s approval from two U.S. registries with a total of 197 high-risk patients at the Transcatheter Cardiovascular Therapeutics annual meeting on Oct. 16, the same day the FDA approval was announced by Edwards Lifesciences. The mortality rate was 4% after 30 days and 13% after 1 year, and the 1-year stroke rate was 4%, Dr. Danny Dvir said at the meeting.
One feature of the 1-year survival data that Dr. Dvir called “quite amazing” was the absence of any deaths during the first 30 days post TAVR with the SAPIEN XT system, and 7% at 1 year among the 100 patients treated during the final 8 months of the registry, who comprised the second half of patients enrolled in the registry. “I think we learned how to choose the right patients for this procedure,” said Dr. Dvir, an interventional cardiologist at St. Paul’s Hospital in Vancouver, B.C.
Given the risk from replacing a failed bioprosthetic valve by open surgery, “TAVR is becoming the preferred approach to valve-in-valve,” commented Dr. Ajay J. Kirtane, director of the cardiac catheterization laboratories at Columbia University in New York.
The registry results also highlighted a key limitation of the SAPIEN XT valve: patients with a bioprosthetic valve with a relatively narrow inner diameter of 21 mm or less.
Because the SAPIEN series of valves are balloon expandable and designed to sit directly in the aortic-valve annulus, the inner diameter of an existing bioprothesis can limit the TAVR options. The CoreValve, self-expanding valves sit in a supravalvular location and better fit through a narrow-frame existing valve.
This geometric limitation means that SAPIEN XT cannot work in patients with existing valves less than 21 mm in inner diameter, and the registry excluded such patients, who generally comprise about 10% of all patients with severe aortic stenosis.
In addition, among the 28% of patients enrolled in the registry who had an existing valve diameter of 21 mm, the 1-year mortality rate was strikingly high – 20% – compared with an 11% mortality rate in patients with existing valve diameters of 23 or 25 mm, Dr. Dvir reported.
“If a patient had a smaller inner diameter I’d definitely go with the supravalvular valve. For a bigger valve you have more choices,” commented Dr. Axel H.P. Linke, codirector of cardiology at the Heart Center at the University of Leipzig (Germany).
“It’s not fair to extrapolate these findings with SAPIEN XT to smaller [existing bioprosthetic] valves. There is the ability to go to lower inner diameters” using CoreValve, commented Dr. Jeffrey J. Popma, who led the U.S. CoreValve studies and is professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
The two sequential valve-in-valve U.S. registries for SAPIEN XT ran as part of the PARTNER 2 trial, designed to test the safety and efficacy of SAPIEN XT in patients undergoing TAVR for a de novo aortic valve. The 197 patients in the full registry averaged 79 years of age, 60% were men, their average Society of Thoracic Surgeons mortality risk score was 9.7%, 50% had atrial fibrillation, 95% had New York Heart Association class III or IV symptoms, and baseline screening identified one-third of the patients as frail.
The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems. Dr. Kirtane has received research grants from Boston Scientific, St. Jude, Eli Lilly, GlaxoSmithKline, Abiomed, and Abbott Vascular. Dr. Linke has been a consultant to Boston Scientific, St. Jude, Bard, Edwards, and Medtronic and owns equity in Claret. Dr. Popma has been principal investigator of the CoreValve studies, has been a consultant to Abbott Vascular, Boston Scientific, and Director Flow; he owns equity in Direct Flow, and he has received research grants from Abbott Vascular, Medtronic, Boston Scientific, and Cook Medical.
On Twitter @mitchelzoler
SAN FRANCISCO – Food and Drug Administration approval of the SAPIEN XT transcatheter aortic valve for the valve-in-valve indication in high–surgical risk patients means that, officially, there are now two options for transcatheter replacement of a faulty prosthetic aortic valve.
CoreValve, the competing device for transcatheter aortic valve replacement (TAVR) in U.S. practice, received FDA approval for the valve-in-valve indication in March.
Researchers reported the data behind SAPIEN XT’s approval from two U.S. registries with a total of 197 high-risk patients at the Transcatheter Cardiovascular Therapeutics annual meeting on Oct. 16, the same day the FDA approval was announced by Edwards Lifesciences. The mortality rate was 4% after 30 days and 13% after 1 year, and the 1-year stroke rate was 4%, Dr. Danny Dvir said at the meeting.
One feature of the 1-year survival data that Dr. Dvir called “quite amazing” was the absence of any deaths during the first 30 days post TAVR with the SAPIEN XT system, and 7% at 1 year among the 100 patients treated during the final 8 months of the registry, who comprised the second half of patients enrolled in the registry. “I think we learned how to choose the right patients for this procedure,” said Dr. Dvir, an interventional cardiologist at St. Paul’s Hospital in Vancouver, B.C.
Given the risk from replacing a failed bioprosthetic valve by open surgery, “TAVR is becoming the preferred approach to valve-in-valve,” commented Dr. Ajay J. Kirtane, director of the cardiac catheterization laboratories at Columbia University in New York.
The registry results also highlighted a key limitation of the SAPIEN XT valve: patients with a bioprosthetic valve with a relatively narrow inner diameter of 21 mm or less.
Because the SAPIEN series of valves are balloon expandable and designed to sit directly in the aortic-valve annulus, the inner diameter of an existing bioprothesis can limit the TAVR options. The CoreValve, self-expanding valves sit in a supravalvular location and better fit through a narrow-frame existing valve.
This geometric limitation means that SAPIEN XT cannot work in patients with existing valves less than 21 mm in inner diameter, and the registry excluded such patients, who generally comprise about 10% of all patients with severe aortic stenosis.
In addition, among the 28% of patients enrolled in the registry who had an existing valve diameter of 21 mm, the 1-year mortality rate was strikingly high – 20% – compared with an 11% mortality rate in patients with existing valve diameters of 23 or 25 mm, Dr. Dvir reported.
“If a patient had a smaller inner diameter I’d definitely go with the supravalvular valve. For a bigger valve you have more choices,” commented Dr. Axel H.P. Linke, codirector of cardiology at the Heart Center at the University of Leipzig (Germany).
“It’s not fair to extrapolate these findings with SAPIEN XT to smaller [existing bioprosthetic] valves. There is the ability to go to lower inner diameters” using CoreValve, commented Dr. Jeffrey J. Popma, who led the U.S. CoreValve studies and is professor at Harvard Medical School and director of interventional cardiology at Beth Israel Deaconess Medical Center in Boston.
The two sequential valve-in-valve U.S. registries for SAPIEN XT ran as part of the PARTNER 2 trial, designed to test the safety and efficacy of SAPIEN XT in patients undergoing TAVR for a de novo aortic valve. The 197 patients in the full registry averaged 79 years of age, 60% were men, their average Society of Thoracic Surgeons mortality risk score was 9.7%, 50% had atrial fibrillation, 95% had New York Heart Association class III or IV symptoms, and baseline screening identified one-third of the patients as frail.
The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems. Dr. Kirtane has received research grants from Boston Scientific, St. Jude, Eli Lilly, GlaxoSmithKline, Abiomed, and Abbott Vascular. Dr. Linke has been a consultant to Boston Scientific, St. Jude, Bard, Edwards, and Medtronic and owns equity in Claret. Dr. Popma has been principal investigator of the CoreValve studies, has been a consultant to Abbott Vascular, Boston Scientific, and Director Flow; he owns equity in Direct Flow, and he has received research grants from Abbott Vascular, Medtronic, Boston Scientific, and Cook Medical.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point:The SAPIEN XT balloon-expandable system for transcatheter aortic valve replacement received FDA approval for valve-in-valve use in high-risk patients.
Major finding: High-risk patients treated for aortic valve-in-replacement with SAPIEN XT had a 13% 1-year mortality rate.
Data source: The PARTNER 2 trial valve-in-valve registry and extended registry, a multicenter center based primarily in the United States with 197 high-risk patients.
Disclosures: The PARTNER 2 trial valve-in-valve registry and extended registry are sponsored by Edwards Lifesciences, which markets the SAPIEN XT system. Dr. Dvir has been a consultant to Edwards and to Medtronic, the company that markets the CoreValve systems.
TCT: Differing sirolimus absorption rates, similar outcomes in PANDA III
SAN FRANCISCO – Two sirolimus-eluting stents with differing elution an absorption kinetics were equally effective in the prospective, randomized PANDA III trial.
The sirolimus in the BuMA stent is completely absorbed in 3 months, while that in the Excel stent takes 6-9 months to be absorbed.
The target lesion failure rate, defined as a composite of cardiac death, target vessel myocardial infarction, or ischemia-driven target lesion revascularization, was the same at 6.4% in 1,175 patients randomized to receive the BuMA device, and 1,175 randomized to receive the Excel device. Cardiac death occurred in 1.2% and 1.3% of patients in the groups, respectively; target vessel myocardial infarction occurred in 4.3% and 4.9%; and ischemia-driven target lesion revascularization occurred in 1.9% and 1.2%, respectively, Dr. Bo Xu of Fu Wai Hospital, Beijing, explained at the Transcatheter Cardiovascular Therapeutics annual meeting.
However, the definite/probable stent thrombosis rate at 1 year was 0.5% in the BuMA patients, and 1.3% in the Excel patients in the intention to treat population. The difference was statistically significant.
BuMA and Excel – neither of which are available in the United States – are both bioresorbable, polymer-based metallic stents, but they have varying elution and absorption kinetics: The BuMA sirolimus-eluting stent (SES) is a poly lactic-co-glycolic acid (PLGA) polymer-based stent incorporating an electrografting base layer between the polymer and stent strut, securing adhesion for the PLGA coating. The BuMA sirolimus is 100% eluted within 30 days, and the polymer is completely absorbed within 3 months, Dr. Xu said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
“In contrast, the [polylactic acid, or PLA] polymer-based Excel SES elutes sirolimus completely within 180 days, and the PLA polymer is completely absorbed within 6-9 months,” he said.
Both stents elute sirolimus from stainless steel platforms, which means that major differences in effects are likely attributable to the polymer and elution kinetics, he noted.
In a previous small study (the BuMA-OCT trial, EuroIntervention 2014;10[7]:806-14) involving 80 patients who were randomized to receive either the BuMA or the Excel stent, the BuMA stent was found to be superior at 3 months (strut coverage proportion, 94.2% vs. 90.0%). The current study enrolled all comers to determine whether BuMA is noninferior or superior to the Excel SES for the primary endpoint of 1 year target lesion failure.
The findings demonstrate noninferiority of the BuMA SES. Further, the BuMA SES was associated with a lower incidence of stent thrombosis, compared with the Excel SES, consistent with the previous findings of enhanced strut coverage with this device, Dr. Xu said, adding that longer follow-up is needed to further understand the long-term effects of this emerging stent technology.
Discussant Dr. David J. Cohen of St. Luke’s Mid America Heart Institute, Kansas City, applauded the study design and inclusion of all comers, but noted that the findings don’t have immediate clinical implications in the United States since neither is available here. They do, however, shed some light on the two stents used in the trial, he said.
“The only difference was stent thrombosis, which was somewhat borderline in the intention-to-treat population, and has to at least be taken as a word of caution. We don’t know if this is because the new stent with the bioabsorbable polymer is better than other things we have, or if the comparator stent is worse, since it’s not a comparator that’s widely used, he said.
Panda III was funded by a research grant from SinoMed. Dr. Xu reported having no disclosures.
SAN FRANCISCO – Two sirolimus-eluting stents with differing elution an absorption kinetics were equally effective in the prospective, randomized PANDA III trial.
The sirolimus in the BuMA stent is completely absorbed in 3 months, while that in the Excel stent takes 6-9 months to be absorbed.
The target lesion failure rate, defined as a composite of cardiac death, target vessel myocardial infarction, or ischemia-driven target lesion revascularization, was the same at 6.4% in 1,175 patients randomized to receive the BuMA device, and 1,175 randomized to receive the Excel device. Cardiac death occurred in 1.2% and 1.3% of patients in the groups, respectively; target vessel myocardial infarction occurred in 4.3% and 4.9%; and ischemia-driven target lesion revascularization occurred in 1.9% and 1.2%, respectively, Dr. Bo Xu of Fu Wai Hospital, Beijing, explained at the Transcatheter Cardiovascular Therapeutics annual meeting.
However, the definite/probable stent thrombosis rate at 1 year was 0.5% in the BuMA patients, and 1.3% in the Excel patients in the intention to treat population. The difference was statistically significant.
BuMA and Excel – neither of which are available in the United States – are both bioresorbable, polymer-based metallic stents, but they have varying elution and absorption kinetics: The BuMA sirolimus-eluting stent (SES) is a poly lactic-co-glycolic acid (PLGA) polymer-based stent incorporating an electrografting base layer between the polymer and stent strut, securing adhesion for the PLGA coating. The BuMA sirolimus is 100% eluted within 30 days, and the polymer is completely absorbed within 3 months, Dr. Xu said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
“In contrast, the [polylactic acid, or PLA] polymer-based Excel SES elutes sirolimus completely within 180 days, and the PLA polymer is completely absorbed within 6-9 months,” he said.
Both stents elute sirolimus from stainless steel platforms, which means that major differences in effects are likely attributable to the polymer and elution kinetics, he noted.
In a previous small study (the BuMA-OCT trial, EuroIntervention 2014;10[7]:806-14) involving 80 patients who were randomized to receive either the BuMA or the Excel stent, the BuMA stent was found to be superior at 3 months (strut coverage proportion, 94.2% vs. 90.0%). The current study enrolled all comers to determine whether BuMA is noninferior or superior to the Excel SES for the primary endpoint of 1 year target lesion failure.
The findings demonstrate noninferiority of the BuMA SES. Further, the BuMA SES was associated with a lower incidence of stent thrombosis, compared with the Excel SES, consistent with the previous findings of enhanced strut coverage with this device, Dr. Xu said, adding that longer follow-up is needed to further understand the long-term effects of this emerging stent technology.
Discussant Dr. David J. Cohen of St. Luke’s Mid America Heart Institute, Kansas City, applauded the study design and inclusion of all comers, but noted that the findings don’t have immediate clinical implications in the United States since neither is available here. They do, however, shed some light on the two stents used in the trial, he said.
“The only difference was stent thrombosis, which was somewhat borderline in the intention-to-treat population, and has to at least be taken as a word of caution. We don’t know if this is because the new stent with the bioabsorbable polymer is better than other things we have, or if the comparator stent is worse, since it’s not a comparator that’s widely used, he said.
Panda III was funded by a research grant from SinoMed. Dr. Xu reported having no disclosures.
SAN FRANCISCO – Two sirolimus-eluting stents with differing elution an absorption kinetics were equally effective in the prospective, randomized PANDA III trial.
The sirolimus in the BuMA stent is completely absorbed in 3 months, while that in the Excel stent takes 6-9 months to be absorbed.
The target lesion failure rate, defined as a composite of cardiac death, target vessel myocardial infarction, or ischemia-driven target lesion revascularization, was the same at 6.4% in 1,175 patients randomized to receive the BuMA device, and 1,175 randomized to receive the Excel device. Cardiac death occurred in 1.2% and 1.3% of patients in the groups, respectively; target vessel myocardial infarction occurred in 4.3% and 4.9%; and ischemia-driven target lesion revascularization occurred in 1.9% and 1.2%, respectively, Dr. Bo Xu of Fu Wai Hospital, Beijing, explained at the Transcatheter Cardiovascular Therapeutics annual meeting.
However, the definite/probable stent thrombosis rate at 1 year was 0.5% in the BuMA patients, and 1.3% in the Excel patients in the intention to treat population. The difference was statistically significant.
BuMA and Excel – neither of which are available in the United States – are both bioresorbable, polymer-based metallic stents, but they have varying elution and absorption kinetics: The BuMA sirolimus-eluting stent (SES) is a poly lactic-co-glycolic acid (PLGA) polymer-based stent incorporating an electrografting base layer between the polymer and stent strut, securing adhesion for the PLGA coating. The BuMA sirolimus is 100% eluted within 30 days, and the polymer is completely absorbed within 3 months, Dr. Xu said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
“In contrast, the [polylactic acid, or PLA] polymer-based Excel SES elutes sirolimus completely within 180 days, and the PLA polymer is completely absorbed within 6-9 months,” he said.
Both stents elute sirolimus from stainless steel platforms, which means that major differences in effects are likely attributable to the polymer and elution kinetics, he noted.
In a previous small study (the BuMA-OCT trial, EuroIntervention 2014;10[7]:806-14) involving 80 patients who were randomized to receive either the BuMA or the Excel stent, the BuMA stent was found to be superior at 3 months (strut coverage proportion, 94.2% vs. 90.0%). The current study enrolled all comers to determine whether BuMA is noninferior or superior to the Excel SES for the primary endpoint of 1 year target lesion failure.
The findings demonstrate noninferiority of the BuMA SES. Further, the BuMA SES was associated with a lower incidence of stent thrombosis, compared with the Excel SES, consistent with the previous findings of enhanced strut coverage with this device, Dr. Xu said, adding that longer follow-up is needed to further understand the long-term effects of this emerging stent technology.
Discussant Dr. David J. Cohen of St. Luke’s Mid America Heart Institute, Kansas City, applauded the study design and inclusion of all comers, but noted that the findings don’t have immediate clinical implications in the United States since neither is available here. They do, however, shed some light on the two stents used in the trial, he said.
“The only difference was stent thrombosis, which was somewhat borderline in the intention-to-treat population, and has to at least be taken as a word of caution. We don’t know if this is because the new stent with the bioabsorbable polymer is better than other things we have, or if the comparator stent is worse, since it’s not a comparator that’s widely used, he said.
Panda III was funded by a research grant from SinoMed. Dr. Xu reported having no disclosures.
AT TCT 2015
Key clinical point: Two sirolimus-eluting stents with differing elution an absorption kinetics were equally effective in the prospective, randomized PANDA III trial.
Major finding: The target lesion failure rate was 6.4% in both the BuMA Group and the Excel stent groups.
Data source: The prospective, randomized PANDA III trial involving 2,350 patients.
Disclosures: Panda III was funded by a research grant from SinoMed. Dr. Xu reported having no disclosures.
TCT: Everolimus stents best paclitaxel for diabetes patients
SAN FRANCISCO – Everolimus-eluting stents were more effective than were paclitaxel-eluting stents in diabetes patients with coronary artery disease who underwent percutaneous coronary intervention (PCI) in the randomized, multicenter TUXEDO-India trial.
The everolimus-eluting stents were shown to be superior to paclitaxel-eluting stents on several endpoints, including target-vessel failure, myocardial infarction, and stent thrombosis at 1 year Dr. Upendra Kaul reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Target vessel failure – the study’s primary endpoint, defined as a composite of cardiac death, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization – occurred in 5.6% of 914 patients randomized to the paclitaxel-eluting stent group, compared with 2.9% of 916 randomized to the everolimus-eluting stent group (relative risk, 1.89), Dr. Kaul of Fortis Escorts Heart Institute, New Delhi, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation.
The rate of spontaneous MI was 3.2% vs. 1.2% in the groups, respectively, and the rate of stent thrombosis was 2.1% vs. 0.4%. Target-vessel revascularization and target-lesion revascularization rates in both groups were 3.4% vs. 1.2% with paclitaxel- and everolimus-eluting stents, respectively, he said, noting that the superiority of everolimus-eluting stents was maintained in insulin-requiring patients.
The findings, which were published online simultaneously (N Engl J Med. 2015 Oct. 14;doi: 10.1056/NEJMoa1510188), effectively end the debate regarding whether paclitaxel-eluting stents are the better choice in diabetes patients with coronary artery disease.
Paclitaxel-eluting stents are generally accepted to be inferior to limus-eluting stents in most patients, but data from numerous trials have been conflicting as to whether that is true in diabetes patients.
“In the absence of a dedicated adequately powered study, a definitive answer is not possible,” Dr. Kaul said.
The findings from TUXEDO, the largest trial to compare paclitaxel- and everolimus-eluting stents head to head in diabetes patients, support “the current worldwide practice of use of new-generation limus-eluting stents, even in patients with insulin-requiring diabetes,” he said.
The findings raise questions about the results of prior coronary artery bypass grafting vs. stenting trials that show superiority of CABG, because first-generation stents, which are inferior to everolimus-eluting stents, were used as comparators in those trials, he noted.
Indeed, current guidelines for bypass surgery and PCI are based upon the findings of those trials, and while the TUXEDO findings don’t invalidate those prior studies, they do raise questions about whether the differences in favor of bypass surgery are much smaller than believed in the setting of modern stent use, commented Dr. Bernard J. Gersh of the Mayo Clinic, Rochester, Minn.
The TUXEDO-India trial was supported by Boston Scientific.
SAN FRANCISCO – Everolimus-eluting stents were more effective than were paclitaxel-eluting stents in diabetes patients with coronary artery disease who underwent percutaneous coronary intervention (PCI) in the randomized, multicenter TUXEDO-India trial.
The everolimus-eluting stents were shown to be superior to paclitaxel-eluting stents on several endpoints, including target-vessel failure, myocardial infarction, and stent thrombosis at 1 year Dr. Upendra Kaul reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Target vessel failure – the study’s primary endpoint, defined as a composite of cardiac death, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization – occurred in 5.6% of 914 patients randomized to the paclitaxel-eluting stent group, compared with 2.9% of 916 randomized to the everolimus-eluting stent group (relative risk, 1.89), Dr. Kaul of Fortis Escorts Heart Institute, New Delhi, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation.
The rate of spontaneous MI was 3.2% vs. 1.2% in the groups, respectively, and the rate of stent thrombosis was 2.1% vs. 0.4%. Target-vessel revascularization and target-lesion revascularization rates in both groups were 3.4% vs. 1.2% with paclitaxel- and everolimus-eluting stents, respectively, he said, noting that the superiority of everolimus-eluting stents was maintained in insulin-requiring patients.
The findings, which were published online simultaneously (N Engl J Med. 2015 Oct. 14;doi: 10.1056/NEJMoa1510188), effectively end the debate regarding whether paclitaxel-eluting stents are the better choice in diabetes patients with coronary artery disease.
Paclitaxel-eluting stents are generally accepted to be inferior to limus-eluting stents in most patients, but data from numerous trials have been conflicting as to whether that is true in diabetes patients.
“In the absence of a dedicated adequately powered study, a definitive answer is not possible,” Dr. Kaul said.
The findings from TUXEDO, the largest trial to compare paclitaxel- and everolimus-eluting stents head to head in diabetes patients, support “the current worldwide practice of use of new-generation limus-eluting stents, even in patients with insulin-requiring diabetes,” he said.
The findings raise questions about the results of prior coronary artery bypass grafting vs. stenting trials that show superiority of CABG, because first-generation stents, which are inferior to everolimus-eluting stents, were used as comparators in those trials, he noted.
Indeed, current guidelines for bypass surgery and PCI are based upon the findings of those trials, and while the TUXEDO findings don’t invalidate those prior studies, they do raise questions about whether the differences in favor of bypass surgery are much smaller than believed in the setting of modern stent use, commented Dr. Bernard J. Gersh of the Mayo Clinic, Rochester, Minn.
The TUXEDO-India trial was supported by Boston Scientific.
SAN FRANCISCO – Everolimus-eluting stents were more effective than were paclitaxel-eluting stents in diabetes patients with coronary artery disease who underwent percutaneous coronary intervention (PCI) in the randomized, multicenter TUXEDO-India trial.
The everolimus-eluting stents were shown to be superior to paclitaxel-eluting stents on several endpoints, including target-vessel failure, myocardial infarction, and stent thrombosis at 1 year Dr. Upendra Kaul reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Target vessel failure – the study’s primary endpoint, defined as a composite of cardiac death, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization – occurred in 5.6% of 914 patients randomized to the paclitaxel-eluting stent group, compared with 2.9% of 916 randomized to the everolimus-eluting stent group (relative risk, 1.89), Dr. Kaul of Fortis Escorts Heart Institute, New Delhi, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation.
The rate of spontaneous MI was 3.2% vs. 1.2% in the groups, respectively, and the rate of stent thrombosis was 2.1% vs. 0.4%. Target-vessel revascularization and target-lesion revascularization rates in both groups were 3.4% vs. 1.2% with paclitaxel- and everolimus-eluting stents, respectively, he said, noting that the superiority of everolimus-eluting stents was maintained in insulin-requiring patients.
The findings, which were published online simultaneously (N Engl J Med. 2015 Oct. 14;doi: 10.1056/NEJMoa1510188), effectively end the debate regarding whether paclitaxel-eluting stents are the better choice in diabetes patients with coronary artery disease.
Paclitaxel-eluting stents are generally accepted to be inferior to limus-eluting stents in most patients, but data from numerous trials have been conflicting as to whether that is true in diabetes patients.
“In the absence of a dedicated adequately powered study, a definitive answer is not possible,” Dr. Kaul said.
The findings from TUXEDO, the largest trial to compare paclitaxel- and everolimus-eluting stents head to head in diabetes patients, support “the current worldwide practice of use of new-generation limus-eluting stents, even in patients with insulin-requiring diabetes,” he said.
The findings raise questions about the results of prior coronary artery bypass grafting vs. stenting trials that show superiority of CABG, because first-generation stents, which are inferior to everolimus-eluting stents, were used as comparators in those trials, he noted.
Indeed, current guidelines for bypass surgery and PCI are based upon the findings of those trials, and while the TUXEDO findings don’t invalidate those prior studies, they do raise questions about whether the differences in favor of bypass surgery are much smaller than believed in the setting of modern stent use, commented Dr. Bernard J. Gersh of the Mayo Clinic, Rochester, Minn.
The TUXEDO-India trial was supported by Boston Scientific.
AT TCT 2015
Key clinical point: Paclitaxel-eluting stents did not meet criterion for noninferiority to everolimus-eluting stents in diabetes mellitus patients with CAD who were undergoing PCI in the TUXEDO-India trial.
Major finding: Target vessel failure occurred in 5.6% vs. 2.9% of patients in the paclitaxel- vs. everolimus-eluting stent group (relative risk, 1.89).
Data source: The randomized, multicenter TUXEDO-India trial in 1,830 patients.
Disclosures: The TUXEDO-India trial was supported by Boston Scientific.
For subacute STEMI, thrombectomy adds no benefit to PCI
The addition of thrombectomy to percutaneous coronary intervention didn’t improve cardiac flow or clinical endpoints any more than PCI alone in patients with a subacute ST-elevation myocardial infarction.
Thrombosis aspiration decreased microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass, Dr. Steffan Desch said at the Transcatheter Cardiovascular Therapeutics annual meeting. There were also no significant differences in infarct size, myocardial salvage, or left ventricular ejection fraction, he said at the meeting sponsored by the Cardiovascular Research Foundation.
“Routine manual thrombectomy and aspiration didn’t show any significant reduction in microvascular obstruction on imaging,” said Dr. Desch of University Heart Center, Lübeck, Germany. “This finding was supported by a variety of secondary endpoints, none of them significantly beneficial.”
The study, which was simultaneously published online (JACC Cardiovasc Interv. 2015. doi: 10.1016/j.jcin.2015.09.010), gives the first firm evidence that clot removal is not particularly helpful to patients who present late after symptom onset. With a mean development time of 28 hours, thrombi in this cohort were more mature, with higher fibrin content than the typically soft material seen in patients with acute ST-elevation myocardial infarction (STEMI). When the clot becomes denser and more organized, it is likely less suitable for aspiration, he said.
The cohort comprised 152 patients who presented in a 12- to 48-hour window after onset of symptoms. They were randomized to either standard PCI or to clot aspiration followed by PCI. The primary outcome was the extent of major vessel occlusion on magnetic resonance imaging conducted 1-4 days after the intervention. Secondary outcomes included infarct size, myocardial salvage, and left ventricular volume and ejection fraction.
Patients were a mean of 66 years old, with typical baseline characteristics. Most were men; hypertension was common (about 70%). About half had signs of ongoing ischemia at admission. The door-to-balloon time was 78 minutes in the combination therapy group and 62 minutes in the PCI-only group. Most (62.5%) had a complete occlusion of the culprit vessel.
In addition to providing no benefit in microvascular occlusion, aspiration did not significantly improve TIMI flow grade above that achieved with PCI only. After the intervention, 78% of those in the thrombectomy group and 69% of those in the PCI group achieved a TIMI flow grade 3. Nor was there a significant difference in myocardial blush grade (70% vs. 65%). When troponin T values were used to assess enzymatic infarct size, they were similar in both groups at 24 and 48 hours.
Clinical outcomes were similar as well. All-cause mortality was 3% in the aspiration group and 5% in the PCI-only group; cardiovascular death occurred in 3% and 4%, respectively. There were no reinfarctions and no stent thromboses. One stroke occurred in a patient who underwent PCI alone.
Dr. Desch noted in the published article that the study took all comers, rather than selecting for specific patient characteristics. Therefore, he said “it is possible that thrombus aspiration might only be advantageous in specific subsets of patients such as those with large thrombus burden, total occlusion or reduced flow.”
The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
The addition of thrombectomy to percutaneous coronary intervention didn’t improve cardiac flow or clinical endpoints any more than PCI alone in patients with a subacute ST-elevation myocardial infarction.
Thrombosis aspiration decreased microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass, Dr. Steffan Desch said at the Transcatheter Cardiovascular Therapeutics annual meeting. There were also no significant differences in infarct size, myocardial salvage, or left ventricular ejection fraction, he said at the meeting sponsored by the Cardiovascular Research Foundation.
“Routine manual thrombectomy and aspiration didn’t show any significant reduction in microvascular obstruction on imaging,” said Dr. Desch of University Heart Center, Lübeck, Germany. “This finding was supported by a variety of secondary endpoints, none of them significantly beneficial.”
The study, which was simultaneously published online (JACC Cardiovasc Interv. 2015. doi: 10.1016/j.jcin.2015.09.010), gives the first firm evidence that clot removal is not particularly helpful to patients who present late after symptom onset. With a mean development time of 28 hours, thrombi in this cohort were more mature, with higher fibrin content than the typically soft material seen in patients with acute ST-elevation myocardial infarction (STEMI). When the clot becomes denser and more organized, it is likely less suitable for aspiration, he said.
The cohort comprised 152 patients who presented in a 12- to 48-hour window after onset of symptoms. They were randomized to either standard PCI or to clot aspiration followed by PCI. The primary outcome was the extent of major vessel occlusion on magnetic resonance imaging conducted 1-4 days after the intervention. Secondary outcomes included infarct size, myocardial salvage, and left ventricular volume and ejection fraction.
Patients were a mean of 66 years old, with typical baseline characteristics. Most were men; hypertension was common (about 70%). About half had signs of ongoing ischemia at admission. The door-to-balloon time was 78 minutes in the combination therapy group and 62 minutes in the PCI-only group. Most (62.5%) had a complete occlusion of the culprit vessel.
In addition to providing no benefit in microvascular occlusion, aspiration did not significantly improve TIMI flow grade above that achieved with PCI only. After the intervention, 78% of those in the thrombectomy group and 69% of those in the PCI group achieved a TIMI flow grade 3. Nor was there a significant difference in myocardial blush grade (70% vs. 65%). When troponin T values were used to assess enzymatic infarct size, they were similar in both groups at 24 and 48 hours.
Clinical outcomes were similar as well. All-cause mortality was 3% in the aspiration group and 5% in the PCI-only group; cardiovascular death occurred in 3% and 4%, respectively. There were no reinfarctions and no stent thromboses. One stroke occurred in a patient who underwent PCI alone.
Dr. Desch noted in the published article that the study took all comers, rather than selecting for specific patient characteristics. Therefore, he said “it is possible that thrombus aspiration might only be advantageous in specific subsets of patients such as those with large thrombus burden, total occlusion or reduced flow.”
The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
The addition of thrombectomy to percutaneous coronary intervention didn’t improve cardiac flow or clinical endpoints any more than PCI alone in patients with a subacute ST-elevation myocardial infarction.
Thrombosis aspiration decreased microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass, Dr. Steffan Desch said at the Transcatheter Cardiovascular Therapeutics annual meeting. There were also no significant differences in infarct size, myocardial salvage, or left ventricular ejection fraction, he said at the meeting sponsored by the Cardiovascular Research Foundation.
“Routine manual thrombectomy and aspiration didn’t show any significant reduction in microvascular obstruction on imaging,” said Dr. Desch of University Heart Center, Lübeck, Germany. “This finding was supported by a variety of secondary endpoints, none of them significantly beneficial.”
The study, which was simultaneously published online (JACC Cardiovasc Interv. 2015. doi: 10.1016/j.jcin.2015.09.010), gives the first firm evidence that clot removal is not particularly helpful to patients who present late after symptom onset. With a mean development time of 28 hours, thrombi in this cohort were more mature, with higher fibrin content than the typically soft material seen in patients with acute ST-elevation myocardial infarction (STEMI). When the clot becomes denser and more organized, it is likely less suitable for aspiration, he said.
The cohort comprised 152 patients who presented in a 12- to 48-hour window after onset of symptoms. They were randomized to either standard PCI or to clot aspiration followed by PCI. The primary outcome was the extent of major vessel occlusion on magnetic resonance imaging conducted 1-4 days after the intervention. Secondary outcomes included infarct size, myocardial salvage, and left ventricular volume and ejection fraction.
Patients were a mean of 66 years old, with typical baseline characteristics. Most were men; hypertension was common (about 70%). About half had signs of ongoing ischemia at admission. The door-to-balloon time was 78 minutes in the combination therapy group and 62 minutes in the PCI-only group. Most (62.5%) had a complete occlusion of the culprit vessel.
In addition to providing no benefit in microvascular occlusion, aspiration did not significantly improve TIMI flow grade above that achieved with PCI only. After the intervention, 78% of those in the thrombectomy group and 69% of those in the PCI group achieved a TIMI flow grade 3. Nor was there a significant difference in myocardial blush grade (70% vs. 65%). When troponin T values were used to assess enzymatic infarct size, they were similar in both groups at 24 and 48 hours.
Clinical outcomes were similar as well. All-cause mortality was 3% in the aspiration group and 5% in the PCI-only group; cardiovascular death occurred in 3% and 4%, respectively. There were no reinfarctions and no stent thromboses. One stroke occurred in a patient who underwent PCI alone.
Dr. Desch noted in the published article that the study took all comers, rather than selecting for specific patient characteristics. Therefore, he said “it is possible that thrombus aspiration might only be advantageous in specific subsets of patients such as those with large thrombus burden, total occlusion or reduced flow.”
The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
AT TCT 2015
Key clinical point: Thrombus aspiration doesn’t reduce microvascular obstruction in subacute STEMI patients undergoing PCI late after symptom onset.
Major finding: Thrombosis aspiration improved microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass – and conferred no other indications of clinical benefit.
Data source: The study randomized 152 patients with late-presentation STEMI to PCI alone or to thrombectomy plus PCI.
Disclosures: The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
TCT: Scoring balloon boosts efficacy against in-stent restenosis
SAN FRANCISCO – Drug-coated balloons are an option in Europe for treating in-stent restenosis in coronary arteries, and new results from a randomized trial with 252 German patients showed that the efficacy of a drug-coated balloon for treating restenosis jumped significantly when preceded by prepping the in-stent restenosis with a scoring-balloon inflation.
“Neointimal modification with a scoring balloon significantly improved the antirestenotic efficacy of a paclitaxel-coated balloon” measured by angiography 6-8 months after the intervention, Dr. Robert A. Byrne said at the at the Transcatheter Cardiovascular Therapeutics annual meeting.
Using a scoring balloon first led to an average 35% diameter stenosis in the treated segment at follow-up angiography, compared with a 40% average diameter stenosis at follow-up in patients treated with a paclitaxel-coated balloon alone, without the scoring-balloon first.
“We feel that even this modest increased benefit might be relevant for practice,” said Dr. Byrne, an interventional cardiologist at the German Heart Center in Munich. “This is a challenging patient group, particularly patients who develop restenosis inside a drug-eluting stent. Even small gains are worth pursuing.” All patients enrolled in the study had their restenosis inside a drug-eluting stent.
“It was a modest benefit,” but the alternative to treating in-stent restenosis with a drug-eluting balloon is using a stent, which creates a stent-in-stent situation and has relatively poor outcomes, commented Dr. David J. Cohen, director of cardiovascular research at Saint Luke’s Mid America Heart Institute in Kansas City. Dr. Cohen noted that, as of now, no drug-coated balloon has received approval for U.S. marketing.
“The most important message was that if you treat in-stent restenosis with a drug-coated balloon, then lesion preparation is the most important step,” commented Dr. Bruno Scheller, professor and interventional cardiologist at the University Clinic of Saarland in Homburg, Germany.
The ISAR-DESIRE 4 (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug Eluting Stent In-Stent Restenosis 4) trial enrolled 252 patients with restenosis inside a drug-eluting coronary stent at four German centers during June 2012–December 2014. Patients averaged 69 years old, about 85% were men, and about 42% had diabetes. The study randomized patients to pretreatment with either a scoring balloon or a conventional balloon. After that, all lesions received treatment with a paclitaxel-coated balloon (Pantera Lux).
The study’s primary endpoint was average-diameter stenosis on follow-up angiography 6-8 months after treatment. Scoring balloon pretreatment produced a five percentage-point decline in the diameter stenosis at follow-up. In addition, the secondary outcome of binary restenosis – the percentage of patients with at least 50% diameter stenosis at follow-up – occurred at a 19% rate in the 125 patients pretreated with a scoring balloon and a 32% rate in the 127 control patients pretreated with a conventional balloon, Dr. Byrne reported at the meeting, sponsored by the Cardiovascular Research Foundation.
Scoring-balloon pretreatment also produced a trend toward fewer patients undergoing a new revascularization procedure during 1 year of clinical follow-up, with a 17% revascularization rate among patients pretreated with a scoring balloon and a 23% rate among the controls. The primary safety outcome, the combined rate of death and nonfatal MIs during 1-year clinical follow-up, occurred at an identical 3% rate in both treatment arms.
The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen. Dr. Cohen has been a consultant to Abbott Vascular and Medtronic, a speaker for AstraZeneca, and he has received research grants from nine companies. Dr. Scheller has several patents involving drug-coated balloons.
On Twitter @mitchelzoler
Stenosis often forms within a stent because initial placement failed to open the stent to its optimal diameter. In these cases, treating the stenosis with a second stent inside the first does not make sense. The more attractive alternative is to treat the stenosis with a couple of balloons, with one balloon aimed at retreating the existing stent to open it more optimally.
 |
Dr. Marco Valgimigli |
Until now, studies designed to show the efficacy of a drug-coated balloon in treating in-stent restenosis have generally not been of high quality, and in Europe, drug-coated balloons have been more expensive than drug-eluting stents and are often not reimbursed by medical coverage programs. But the results from ISAR-DESIRE 4 may change that because they are convincing.
The incremental benefit produced by first using a scoring balloon highlights the importance of preparing a coronary stenosis before treating it with a drug-coated balloon. The effect of the scoring balloon on further opening the existing stent may have been as important or more important than the scoring itself.
Regardless of the exact mechanism of benefit, the treatment method tested in ISAR-DESIRE 4 showed a small but significant incremental benefit from scoring pretreatment, and the benefit was large enough to warrant adoption. In-stent restenosis is very challenging to treat, so any significant gain in efficacy is welcome. It is very important to treat the restenosis optimally the first time, because it is often refractory and keeps recurring and when this happens, the only alternative is coronary bypass surgery. The approach that succeeded in ISAR-DESIRE 4 is worth trying if it can prevent some patients from needing bypass surgery.
Dr. Marco Valgimigli is an interventional cardiologist at Inselspital University Hospital in Bern, Switzerland. He made these comments in an interview. He had no disclosures.
Stenosis often forms within a stent because initial placement failed to open the stent to its optimal diameter. In these cases, treating the stenosis with a second stent inside the first does not make sense. The more attractive alternative is to treat the stenosis with a couple of balloons, with one balloon aimed at retreating the existing stent to open it more optimally.
 |
Dr. Marco Valgimigli |
Until now, studies designed to show the efficacy of a drug-coated balloon in treating in-stent restenosis have generally not been of high quality, and in Europe, drug-coated balloons have been more expensive than drug-eluting stents and are often not reimbursed by medical coverage programs. But the results from ISAR-DESIRE 4 may change that because they are convincing.
The incremental benefit produced by first using a scoring balloon highlights the importance of preparing a coronary stenosis before treating it with a drug-coated balloon. The effect of the scoring balloon on further opening the existing stent may have been as important or more important than the scoring itself.
Regardless of the exact mechanism of benefit, the treatment method tested in ISAR-DESIRE 4 showed a small but significant incremental benefit from scoring pretreatment, and the benefit was large enough to warrant adoption. In-stent restenosis is very challenging to treat, so any significant gain in efficacy is welcome. It is very important to treat the restenosis optimally the first time, because it is often refractory and keeps recurring and when this happens, the only alternative is coronary bypass surgery. The approach that succeeded in ISAR-DESIRE 4 is worth trying if it can prevent some patients from needing bypass surgery.
Dr. Marco Valgimigli is an interventional cardiologist at Inselspital University Hospital in Bern, Switzerland. He made these comments in an interview. He had no disclosures.
Stenosis often forms within a stent because initial placement failed to open the stent to its optimal diameter. In these cases, treating the stenosis with a second stent inside the first does not make sense. The more attractive alternative is to treat the stenosis with a couple of balloons, with one balloon aimed at retreating the existing stent to open it more optimally.
 |
Dr. Marco Valgimigli |
Until now, studies designed to show the efficacy of a drug-coated balloon in treating in-stent restenosis have generally not been of high quality, and in Europe, drug-coated balloons have been more expensive than drug-eluting stents and are often not reimbursed by medical coverage programs. But the results from ISAR-DESIRE 4 may change that because they are convincing.
The incremental benefit produced by first using a scoring balloon highlights the importance of preparing a coronary stenosis before treating it with a drug-coated balloon. The effect of the scoring balloon on further opening the existing stent may have been as important or more important than the scoring itself.
Regardless of the exact mechanism of benefit, the treatment method tested in ISAR-DESIRE 4 showed a small but significant incremental benefit from scoring pretreatment, and the benefit was large enough to warrant adoption. In-stent restenosis is very challenging to treat, so any significant gain in efficacy is welcome. It is very important to treat the restenosis optimally the first time, because it is often refractory and keeps recurring and when this happens, the only alternative is coronary bypass surgery. The approach that succeeded in ISAR-DESIRE 4 is worth trying if it can prevent some patients from needing bypass surgery.
Dr. Marco Valgimigli is an interventional cardiologist at Inselspital University Hospital in Bern, Switzerland. He made these comments in an interview. He had no disclosures.
SAN FRANCISCO – Drug-coated balloons are an option in Europe for treating in-stent restenosis in coronary arteries, and new results from a randomized trial with 252 German patients showed that the efficacy of a drug-coated balloon for treating restenosis jumped significantly when preceded by prepping the in-stent restenosis with a scoring-balloon inflation.
“Neointimal modification with a scoring balloon significantly improved the antirestenotic efficacy of a paclitaxel-coated balloon” measured by angiography 6-8 months after the intervention, Dr. Robert A. Byrne said at the at the Transcatheter Cardiovascular Therapeutics annual meeting.
Using a scoring balloon first led to an average 35% diameter stenosis in the treated segment at follow-up angiography, compared with a 40% average diameter stenosis at follow-up in patients treated with a paclitaxel-coated balloon alone, without the scoring-balloon first.
“We feel that even this modest increased benefit might be relevant for practice,” said Dr. Byrne, an interventional cardiologist at the German Heart Center in Munich. “This is a challenging patient group, particularly patients who develop restenosis inside a drug-eluting stent. Even small gains are worth pursuing.” All patients enrolled in the study had their restenosis inside a drug-eluting stent.
“It was a modest benefit,” but the alternative to treating in-stent restenosis with a drug-eluting balloon is using a stent, which creates a stent-in-stent situation and has relatively poor outcomes, commented Dr. David J. Cohen, director of cardiovascular research at Saint Luke’s Mid America Heart Institute in Kansas City. Dr. Cohen noted that, as of now, no drug-coated balloon has received approval for U.S. marketing.
“The most important message was that if you treat in-stent restenosis with a drug-coated balloon, then lesion preparation is the most important step,” commented Dr. Bruno Scheller, professor and interventional cardiologist at the University Clinic of Saarland in Homburg, Germany.
The ISAR-DESIRE 4 (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug Eluting Stent In-Stent Restenosis 4) trial enrolled 252 patients with restenosis inside a drug-eluting coronary stent at four German centers during June 2012–December 2014. Patients averaged 69 years old, about 85% were men, and about 42% had diabetes. The study randomized patients to pretreatment with either a scoring balloon or a conventional balloon. After that, all lesions received treatment with a paclitaxel-coated balloon (Pantera Lux).
The study’s primary endpoint was average-diameter stenosis on follow-up angiography 6-8 months after treatment. Scoring balloon pretreatment produced a five percentage-point decline in the diameter stenosis at follow-up. In addition, the secondary outcome of binary restenosis – the percentage of patients with at least 50% diameter stenosis at follow-up – occurred at a 19% rate in the 125 patients pretreated with a scoring balloon and a 32% rate in the 127 control patients pretreated with a conventional balloon, Dr. Byrne reported at the meeting, sponsored by the Cardiovascular Research Foundation.
Scoring-balloon pretreatment also produced a trend toward fewer patients undergoing a new revascularization procedure during 1 year of clinical follow-up, with a 17% revascularization rate among patients pretreated with a scoring balloon and a 23% rate among the controls. The primary safety outcome, the combined rate of death and nonfatal MIs during 1-year clinical follow-up, occurred at an identical 3% rate in both treatment arms.
The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen. Dr. Cohen has been a consultant to Abbott Vascular and Medtronic, a speaker for AstraZeneca, and he has received research grants from nine companies. Dr. Scheller has several patents involving drug-coated balloons.
On Twitter @mitchelzoler
SAN FRANCISCO – Drug-coated balloons are an option in Europe for treating in-stent restenosis in coronary arteries, and new results from a randomized trial with 252 German patients showed that the efficacy of a drug-coated balloon for treating restenosis jumped significantly when preceded by prepping the in-stent restenosis with a scoring-balloon inflation.
“Neointimal modification with a scoring balloon significantly improved the antirestenotic efficacy of a paclitaxel-coated balloon” measured by angiography 6-8 months after the intervention, Dr. Robert A. Byrne said at the at the Transcatheter Cardiovascular Therapeutics annual meeting.
Using a scoring balloon first led to an average 35% diameter stenosis in the treated segment at follow-up angiography, compared with a 40% average diameter stenosis at follow-up in patients treated with a paclitaxel-coated balloon alone, without the scoring-balloon first.
“We feel that even this modest increased benefit might be relevant for practice,” said Dr. Byrne, an interventional cardiologist at the German Heart Center in Munich. “This is a challenging patient group, particularly patients who develop restenosis inside a drug-eluting stent. Even small gains are worth pursuing.” All patients enrolled in the study had their restenosis inside a drug-eluting stent.
“It was a modest benefit,” but the alternative to treating in-stent restenosis with a drug-eluting balloon is using a stent, which creates a stent-in-stent situation and has relatively poor outcomes, commented Dr. David J. Cohen, director of cardiovascular research at Saint Luke’s Mid America Heart Institute in Kansas City. Dr. Cohen noted that, as of now, no drug-coated balloon has received approval for U.S. marketing.
“The most important message was that if you treat in-stent restenosis with a drug-coated balloon, then lesion preparation is the most important step,” commented Dr. Bruno Scheller, professor and interventional cardiologist at the University Clinic of Saarland in Homburg, Germany.
The ISAR-DESIRE 4 (Intracoronary Stenting and Angiographic Results: Optimizing Treatment of Drug Eluting Stent In-Stent Restenosis 4) trial enrolled 252 patients with restenosis inside a drug-eluting coronary stent at four German centers during June 2012–December 2014. Patients averaged 69 years old, about 85% were men, and about 42% had diabetes. The study randomized patients to pretreatment with either a scoring balloon or a conventional balloon. After that, all lesions received treatment with a paclitaxel-coated balloon (Pantera Lux).
The study’s primary endpoint was average-diameter stenosis on follow-up angiography 6-8 months after treatment. Scoring balloon pretreatment produced a five percentage-point decline in the diameter stenosis at follow-up. In addition, the secondary outcome of binary restenosis – the percentage of patients with at least 50% diameter stenosis at follow-up – occurred at a 19% rate in the 125 patients pretreated with a scoring balloon and a 32% rate in the 127 control patients pretreated with a conventional balloon, Dr. Byrne reported at the meeting, sponsored by the Cardiovascular Research Foundation.
Scoring-balloon pretreatment also produced a trend toward fewer patients undergoing a new revascularization procedure during 1 year of clinical follow-up, with a 17% revascularization rate among patients pretreated with a scoring balloon and a 23% rate among the controls. The primary safety outcome, the combined rate of death and nonfatal MIs during 1-year clinical follow-up, occurred at an identical 3% rate in both treatment arms.
The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen. Dr. Cohen has been a consultant to Abbott Vascular and Medtronic, a speaker for AstraZeneca, and he has received research grants from nine companies. Dr. Scheller has several patents involving drug-coated balloons.
On Twitter @mitchelzoler
AT TCT 2015
Key clinical point: Pretreating in-stent restenosis with a scoring balloon before using a drug-coated balloon significantly boosted efficacy.
Major finding: After 6 months, average diameter stenosis following paclitaxel-coated balloon treatment was 35% with a scoring balloon and 40% without.
Data source: ISAR-DESIRE 4, a randomized trial of 252 patients at four German centers.
Disclosures: The ISAR-DESIRE 4 trial was cosponsored by Biotronik, which markets the paclitaxel-coated balloon (Pantera Lux) used in the trial. Dr. Byrne said that he has received speaking fees from Biotronik and from Boston Scientific and B. Braun Melsungen.
TCT: CTO treatment after MI doesn’t benefit LV function
SAN FRANCISCO – Recanalization of a chronic total occlusion in a noninfarct-related artery within a week after primary percutaneous coronary intervention was safe and feasible but did not improve overall left ventricular ejection fraction or LV end diastolic volume in the randomized, prospective EXPLORE trial.
At 4 months after primary percutaneous coronary intervention (pPCI), cardiac magnetic resonance imaging showed that left ventricular ejection fraction (LVEF) was similar in 136 patients who underwent chronic total occlusion percutaneous coronary intervention (CTO-PCI) and 144 who did not undergo CTO-PCI (44.1 and 44.8, respectively) within 1 week after the pPCI, Dr. Jose P.S. Henriques reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
LV end diastolic volume also was similar in the two groups (215.6 and 212.8, respectively), Dr. Henriques of the Academic Medical Center, Amsterdam, said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
A subgroup analysis, however, showed that LVEF did improve significantly with CTO-PCI in 69 patients whose CTOs were located in the left anterior descending (LAD) artery, compared with 211 patients with non-LAD CTOs (treatment effect, 6.8 vs. –3.2), Dr. Henriques said.
Patients enrolled in the EXPLORE trial had a mean age of 60 years, and most were men (89% in the CTO-PCI group and 82% in the non-CTO-PCI group). The two groups were well balanced with respect to clinical and demographic characteristics. Of note, both groups had a high rate of triple-vessel disease with greater than 70% stenosis and high rates of multiple CTOs (9% and 14%), he said.
Of those who underwent CTO-PCI, 6 had multiple CTO arteries treated, 124 were treated using an antegrade-only technique, 23 were treated using a retrograde technique, and 5 were treated using Crossboss/Stingray. The self-reported PCI success rates was 80%, but this was downgraded to 72% based on core lab adjudication.
About 10% of ST-segment–elevation myocardial infarction (STEMI) patients have a noninfarct-related artery CTO, but randomized controlled data on management are lacking.
“We don’t know how to treat them or what to do with these patients. What we do know is that the observed mortality in multivessel-disease patients vs. single vessel–disease patients is mainly driven by confirmed total occlusion. Also, the observed reduced LV function in multivessel-disease patients vs. single vessel–disease patients is also mainly driven by chronic total occlusion,” Dr. Henriques said.
“The EXPLORE trial is the first randomized controlled trial on the impact of PCI of CTO on LV function and clinical outcome in post-STEMI patients,” he said.
The findings suggest that CTO-PCI for a post-STEMI CTO located in the LAD may improve LV function and potentially improve clinical outcome in the long term, he concluded.
Dr. Henriques reported receiving grant or research support from Abbott Vascular, Abiomed, Biotronik, and B.Braun.
SAN FRANCISCO – Recanalization of a chronic total occlusion in a noninfarct-related artery within a week after primary percutaneous coronary intervention was safe and feasible but did not improve overall left ventricular ejection fraction or LV end diastolic volume in the randomized, prospective EXPLORE trial.
At 4 months after primary percutaneous coronary intervention (pPCI), cardiac magnetic resonance imaging showed that left ventricular ejection fraction (LVEF) was similar in 136 patients who underwent chronic total occlusion percutaneous coronary intervention (CTO-PCI) and 144 who did not undergo CTO-PCI (44.1 and 44.8, respectively) within 1 week after the pPCI, Dr. Jose P.S. Henriques reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
LV end diastolic volume also was similar in the two groups (215.6 and 212.8, respectively), Dr. Henriques of the Academic Medical Center, Amsterdam, said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
A subgroup analysis, however, showed that LVEF did improve significantly with CTO-PCI in 69 patients whose CTOs were located in the left anterior descending (LAD) artery, compared with 211 patients with non-LAD CTOs (treatment effect, 6.8 vs. –3.2), Dr. Henriques said.
Patients enrolled in the EXPLORE trial had a mean age of 60 years, and most were men (89% in the CTO-PCI group and 82% in the non-CTO-PCI group). The two groups were well balanced with respect to clinical and demographic characteristics. Of note, both groups had a high rate of triple-vessel disease with greater than 70% stenosis and high rates of multiple CTOs (9% and 14%), he said.
Of those who underwent CTO-PCI, 6 had multiple CTO arteries treated, 124 were treated using an antegrade-only technique, 23 were treated using a retrograde technique, and 5 were treated using Crossboss/Stingray. The self-reported PCI success rates was 80%, but this was downgraded to 72% based on core lab adjudication.
About 10% of ST-segment–elevation myocardial infarction (STEMI) patients have a noninfarct-related artery CTO, but randomized controlled data on management are lacking.
“We don’t know how to treat them or what to do with these patients. What we do know is that the observed mortality in multivessel-disease patients vs. single vessel–disease patients is mainly driven by confirmed total occlusion. Also, the observed reduced LV function in multivessel-disease patients vs. single vessel–disease patients is also mainly driven by chronic total occlusion,” Dr. Henriques said.
“The EXPLORE trial is the first randomized controlled trial on the impact of PCI of CTO on LV function and clinical outcome in post-STEMI patients,” he said.
The findings suggest that CTO-PCI for a post-STEMI CTO located in the LAD may improve LV function and potentially improve clinical outcome in the long term, he concluded.
Dr. Henriques reported receiving grant or research support from Abbott Vascular, Abiomed, Biotronik, and B.Braun.
SAN FRANCISCO – Recanalization of a chronic total occlusion in a noninfarct-related artery within a week after primary percutaneous coronary intervention was safe and feasible but did not improve overall left ventricular ejection fraction or LV end diastolic volume in the randomized, prospective EXPLORE trial.
At 4 months after primary percutaneous coronary intervention (pPCI), cardiac magnetic resonance imaging showed that left ventricular ejection fraction (LVEF) was similar in 136 patients who underwent chronic total occlusion percutaneous coronary intervention (CTO-PCI) and 144 who did not undergo CTO-PCI (44.1 and 44.8, respectively) within 1 week after the pPCI, Dr. Jose P.S. Henriques reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
LV end diastolic volume also was similar in the two groups (215.6 and 212.8, respectively), Dr. Henriques of the Academic Medical Center, Amsterdam, said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
A subgroup analysis, however, showed that LVEF did improve significantly with CTO-PCI in 69 patients whose CTOs were located in the left anterior descending (LAD) artery, compared with 211 patients with non-LAD CTOs (treatment effect, 6.8 vs. –3.2), Dr. Henriques said.
Patients enrolled in the EXPLORE trial had a mean age of 60 years, and most were men (89% in the CTO-PCI group and 82% in the non-CTO-PCI group). The two groups were well balanced with respect to clinical and demographic characteristics. Of note, both groups had a high rate of triple-vessel disease with greater than 70% stenosis and high rates of multiple CTOs (9% and 14%), he said.
Of those who underwent CTO-PCI, 6 had multiple CTO arteries treated, 124 were treated using an antegrade-only technique, 23 were treated using a retrograde technique, and 5 were treated using Crossboss/Stingray. The self-reported PCI success rates was 80%, but this was downgraded to 72% based on core lab adjudication.
About 10% of ST-segment–elevation myocardial infarction (STEMI) patients have a noninfarct-related artery CTO, but randomized controlled data on management are lacking.
“We don’t know how to treat them or what to do with these patients. What we do know is that the observed mortality in multivessel-disease patients vs. single vessel–disease patients is mainly driven by confirmed total occlusion. Also, the observed reduced LV function in multivessel-disease patients vs. single vessel–disease patients is also mainly driven by chronic total occlusion,” Dr. Henriques said.
“The EXPLORE trial is the first randomized controlled trial on the impact of PCI of CTO on LV function and clinical outcome in post-STEMI patients,” he said.
The findings suggest that CTO-PCI for a post-STEMI CTO located in the LAD may improve LV function and potentially improve clinical outcome in the long term, he concluded.
Dr. Henriques reported receiving grant or research support from Abbott Vascular, Abiomed, Biotronik, and B.Braun.
AT TCT 2015
Key clinical point: Recanalization of a chronic total occlusion in a noninfarct-related artery within a week after primary percutaneous coronary intervention was safe and feasible.
Major finding: LVEF improved significantly with CTO-PCI in patients with LAD artery CTOs vs. non-LAD CTOs (treatment effect, 6.8 vs. –3.2).
Data source: The randomized, prospective EXPLORE Trial of 280 patients.
Disclosures: Dr. Henriques reported receiving grant or research support from Abbott Vascular, Abiomed, Biotronik, and B.Braun.
TCT: Novel drug-coated stent bests bare-metal in patients at high bleeding risk
A novel drug-coated stent halved the need for repeat revascularization and had a superior safety profile, compared with a bare-metal stent, in patients with a high risk of bleeding in the LEADERS FREE trial.
The results could mean that these typically older, sicker patients in whom dual antiplatelet therapy is contraindicated because of hemorrhage risk now have a wider range of revascularization options, said lead investigator Dr. Philip Urban.
“Patients who have a high risk of bleeding during percutaneous coronary intervention (PCI) are often excluded from stent and drug trials but constitute a rapidly growing proportion of PCI candidates, and they suffer high event rates,” said Dr. Urban, director of interventional cardiology at La Tour Hospital in Geneva. As the life expectancy increases, the implications are profound because roughly one-fifth of all PCI patients globally could be candidates for this type of treatment.
The data were presented at the Transcatheter Cardiovascular Therapeutics annual meeting, which was sponsored by the Cardiovascular Research Foundation. The results also were published online (N Engl J Med. 2015 Oct 14. doi: 10.1056/NEJMoa1503943).
“I hope these results will change practice as early as next week in Europe and elsewhere,” he said. The device is currently CE marked in Europe and is available in some parts of Asia. A clinical trial for the device is currently in the preliminary stages in the United States.
The current standard for PCI in patients at high risk for hemorrhage is to use bare-metal, instead of drug-eluting, stents. Although this protocol lowers the potential risk for bleeding and other complications often caused by extended dual antiplatelet therapy (DAPT), it exposes these patients to a higher risk of restenosis.
Rather than use a drug delivery polymer, the Biolimus A9-coated BioFreedom (Biosensors International) is polymer free and uses a stainless steel stent microstructured to hold a proprietary lipophilic drug on its outer surface. The drug is absorbed by the body within a month of placement.
The first of its kind, the double-blinded LEADERS FREE trial randomly assigned 2,466 PCI patients at high risk for bleeding to receive either the test stent or the standard platform Gazelle bare-metal stent. The procedures were performed at nearly 70 participating sites around the world, excluding the United States. More than half of all patients were accessed transradially, which was preferable to transfemoral access, according to Dr. Urban, because of the lower associated bleeding rates.
All patients were given 1 month of antiplatelet therapy after their intervention: about two-thirds of each group received DAPT and one-third received triple antiplatelet therapy. All were then switched to aspirin alone for 1 year.
At 390 days, there was nearly a 50% reduction in the need for repeat revascularization in the 1,221 patients receiving the drug-coated stent (5.1%), compared with 1,221 receiving the bare-metal stent (9.8%), with the difference reaching statistical significance for superiority for this primary efficacy endpoint (P < .001 for superiority).
Patients in the study arm also had a 29% reduction in risk of cardiac death, myocardial infarction, or stent thrombosis, the primary safety endpoint. At 390 days, these events occurred in 9.4% of the drug coated–stent patients, compared with 12.9% of the controls, a statistically significant difference for both noninferiority (P < .0001) and superiority (P = .005).
The study was done in patients typically excluded from such a trial, although, according to Dr. Urban, the PCI procedures performed were no more complex than usual. More than half the patients, three-quarters of whom were men in their mid- to late-70s, also had a range of comorbidities such as diabetes, kidney disease, and atrial fibrillation. Patients taking anticoagulants, those who had experienced a stroke within the past year, those expected to have major surgery within the year, and those who had undergone cancer treatment within the past 3 years also were included.
Bleeding events in the year following did not differ significantly between groups: 18.1% in the study group and 19.1% of controls had BARC 1-5 bleeding; 13.9% in the test arm and 14.7% of controls had BARC 2-5 events; and 7.2% in the study group and 7.3% of controls experienced BARC 3-5 events.
In the past, Dr. Urban had theorized that the trial would help to quantify not only risk for hemorrhage, but also the thrombotic risk in this patient population. In an interview, Dr. Urban said that, while the stent thrombosis rate was nearly identical in both groups in the trial, “the safety advantage of the drug-coated stent was especially apparent in the more thrombotic milieu.”
LEADERS FREE was underwritten by Biosensors International, maker of the BioFreedom stent. Dr. Urban and several of his coinvestigators disclosed relationships with device makers, including Edward Lifesciences, Terumo, Abbott Vascular, and Quest Medical.
On Twitter @whitneymcknight
A novel drug-coated stent halved the need for repeat revascularization and had a superior safety profile, compared with a bare-metal stent, in patients with a high risk of bleeding in the LEADERS FREE trial.
The results could mean that these typically older, sicker patients in whom dual antiplatelet therapy is contraindicated because of hemorrhage risk now have a wider range of revascularization options, said lead investigator Dr. Philip Urban.
“Patients who have a high risk of bleeding during percutaneous coronary intervention (PCI) are often excluded from stent and drug trials but constitute a rapidly growing proportion of PCI candidates, and they suffer high event rates,” said Dr. Urban, director of interventional cardiology at La Tour Hospital in Geneva. As the life expectancy increases, the implications are profound because roughly one-fifth of all PCI patients globally could be candidates for this type of treatment.
The data were presented at the Transcatheter Cardiovascular Therapeutics annual meeting, which was sponsored by the Cardiovascular Research Foundation. The results also were published online (N Engl J Med. 2015 Oct 14. doi: 10.1056/NEJMoa1503943).
“I hope these results will change practice as early as next week in Europe and elsewhere,” he said. The device is currently CE marked in Europe and is available in some parts of Asia. A clinical trial for the device is currently in the preliminary stages in the United States.
The current standard for PCI in patients at high risk for hemorrhage is to use bare-metal, instead of drug-eluting, stents. Although this protocol lowers the potential risk for bleeding and other complications often caused by extended dual antiplatelet therapy (DAPT), it exposes these patients to a higher risk of restenosis.
Rather than use a drug delivery polymer, the Biolimus A9-coated BioFreedom (Biosensors International) is polymer free and uses a stainless steel stent microstructured to hold a proprietary lipophilic drug on its outer surface. The drug is absorbed by the body within a month of placement.
The first of its kind, the double-blinded LEADERS FREE trial randomly assigned 2,466 PCI patients at high risk for bleeding to receive either the test stent or the standard platform Gazelle bare-metal stent. The procedures were performed at nearly 70 participating sites around the world, excluding the United States. More than half of all patients were accessed transradially, which was preferable to transfemoral access, according to Dr. Urban, because of the lower associated bleeding rates.
All patients were given 1 month of antiplatelet therapy after their intervention: about two-thirds of each group received DAPT and one-third received triple antiplatelet therapy. All were then switched to aspirin alone for 1 year.
At 390 days, there was nearly a 50% reduction in the need for repeat revascularization in the 1,221 patients receiving the drug-coated stent (5.1%), compared with 1,221 receiving the bare-metal stent (9.8%), with the difference reaching statistical significance for superiority for this primary efficacy endpoint (P < .001 for superiority).
Patients in the study arm also had a 29% reduction in risk of cardiac death, myocardial infarction, or stent thrombosis, the primary safety endpoint. At 390 days, these events occurred in 9.4% of the drug coated–stent patients, compared with 12.9% of the controls, a statistically significant difference for both noninferiority (P < .0001) and superiority (P = .005).
The study was done in patients typically excluded from such a trial, although, according to Dr. Urban, the PCI procedures performed were no more complex than usual. More than half the patients, three-quarters of whom were men in their mid- to late-70s, also had a range of comorbidities such as diabetes, kidney disease, and atrial fibrillation. Patients taking anticoagulants, those who had experienced a stroke within the past year, those expected to have major surgery within the year, and those who had undergone cancer treatment within the past 3 years also were included.
Bleeding events in the year following did not differ significantly between groups: 18.1% in the study group and 19.1% of controls had BARC 1-5 bleeding; 13.9% in the test arm and 14.7% of controls had BARC 2-5 events; and 7.2% in the study group and 7.3% of controls experienced BARC 3-5 events.
In the past, Dr. Urban had theorized that the trial would help to quantify not only risk for hemorrhage, but also the thrombotic risk in this patient population. In an interview, Dr. Urban said that, while the stent thrombosis rate was nearly identical in both groups in the trial, “the safety advantage of the drug-coated stent was especially apparent in the more thrombotic milieu.”
LEADERS FREE was underwritten by Biosensors International, maker of the BioFreedom stent. Dr. Urban and several of his coinvestigators disclosed relationships with device makers, including Edward Lifesciences, Terumo, Abbott Vascular, and Quest Medical.
On Twitter @whitneymcknight
A novel drug-coated stent halved the need for repeat revascularization and had a superior safety profile, compared with a bare-metal stent, in patients with a high risk of bleeding in the LEADERS FREE trial.
The results could mean that these typically older, sicker patients in whom dual antiplatelet therapy is contraindicated because of hemorrhage risk now have a wider range of revascularization options, said lead investigator Dr. Philip Urban.
“Patients who have a high risk of bleeding during percutaneous coronary intervention (PCI) are often excluded from stent and drug trials but constitute a rapidly growing proportion of PCI candidates, and they suffer high event rates,” said Dr. Urban, director of interventional cardiology at La Tour Hospital in Geneva. As the life expectancy increases, the implications are profound because roughly one-fifth of all PCI patients globally could be candidates for this type of treatment.
The data were presented at the Transcatheter Cardiovascular Therapeutics annual meeting, which was sponsored by the Cardiovascular Research Foundation. The results also were published online (N Engl J Med. 2015 Oct 14. doi: 10.1056/NEJMoa1503943).
“I hope these results will change practice as early as next week in Europe and elsewhere,” he said. The device is currently CE marked in Europe and is available in some parts of Asia. A clinical trial for the device is currently in the preliminary stages in the United States.
The current standard for PCI in patients at high risk for hemorrhage is to use bare-metal, instead of drug-eluting, stents. Although this protocol lowers the potential risk for bleeding and other complications often caused by extended dual antiplatelet therapy (DAPT), it exposes these patients to a higher risk of restenosis.
Rather than use a drug delivery polymer, the Biolimus A9-coated BioFreedom (Biosensors International) is polymer free and uses a stainless steel stent microstructured to hold a proprietary lipophilic drug on its outer surface. The drug is absorbed by the body within a month of placement.
The first of its kind, the double-blinded LEADERS FREE trial randomly assigned 2,466 PCI patients at high risk for bleeding to receive either the test stent or the standard platform Gazelle bare-metal stent. The procedures were performed at nearly 70 participating sites around the world, excluding the United States. More than half of all patients were accessed transradially, which was preferable to transfemoral access, according to Dr. Urban, because of the lower associated bleeding rates.
All patients were given 1 month of antiplatelet therapy after their intervention: about two-thirds of each group received DAPT and one-third received triple antiplatelet therapy. All were then switched to aspirin alone for 1 year.
At 390 days, there was nearly a 50% reduction in the need for repeat revascularization in the 1,221 patients receiving the drug-coated stent (5.1%), compared with 1,221 receiving the bare-metal stent (9.8%), with the difference reaching statistical significance for superiority for this primary efficacy endpoint (P < .001 for superiority).
Patients in the study arm also had a 29% reduction in risk of cardiac death, myocardial infarction, or stent thrombosis, the primary safety endpoint. At 390 days, these events occurred in 9.4% of the drug coated–stent patients, compared with 12.9% of the controls, a statistically significant difference for both noninferiority (P < .0001) and superiority (P = .005).
The study was done in patients typically excluded from such a trial, although, according to Dr. Urban, the PCI procedures performed were no more complex than usual. More than half the patients, three-quarters of whom were men in their mid- to late-70s, also had a range of comorbidities such as diabetes, kidney disease, and atrial fibrillation. Patients taking anticoagulants, those who had experienced a stroke within the past year, those expected to have major surgery within the year, and those who had undergone cancer treatment within the past 3 years also were included.
Bleeding events in the year following did not differ significantly between groups: 18.1% in the study group and 19.1% of controls had BARC 1-5 bleeding; 13.9% in the test arm and 14.7% of controls had BARC 2-5 events; and 7.2% in the study group and 7.3% of controls experienced BARC 3-5 events.
In the past, Dr. Urban had theorized that the trial would help to quantify not only risk for hemorrhage, but also the thrombotic risk in this patient population. In an interview, Dr. Urban said that, while the stent thrombosis rate was nearly identical in both groups in the trial, “the safety advantage of the drug-coated stent was especially apparent in the more thrombotic milieu.”
LEADERS FREE was underwritten by Biosensors International, maker of the BioFreedom stent. Dr. Urban and several of his coinvestigators disclosed relationships with device makers, including Edward Lifesciences, Terumo, Abbott Vascular, and Quest Medical.
On Twitter @whitneymcknight
AT TCT 2015
Key clinical point: Older, sicker acute coronary syndrome patients at higher risk for hemorrhage may now have more PCI options.
Major finding: At 390 days, 5.1% of PCI patients given a drug-coated stent plus 1 month of DAPT required revascularization, compared with 9.8% of the bare metal–stented control group given 1 month of DAPT; 9.4% of those given a drug-coated stent plus 1 month DAPT had adverse events vs. 12.9% of controls.
Data source: LEADERS FREE is a prospective, double-blinded, randomized controlled trial of 2,466 PCI patients at high risk for bleeding.
Disclosures: The study was underwritten by Biosensors International, maker of the BioFreedom stent.