User login
Preventive B-Lynch suture effective in women at high postpartum hemorrhage risk
Key clinical point: Preventive B-Lynch suture seemed safe and effective in preventing excessive maternal hemorrhage in patients at a high risk for postpartum hemorrhage.
Major finding: Overall, 92% of patients who underwent the B-Lynch suture procedure showed no apparent postoperative bleeding within 2 hours after the cesarean section (CS), with 24 patients requiring intraoperative or postoperative blood transfusion, none requiring hysterectomy, and only 1 patient with a twin pregnancy requiring additional treatment because of secondary postpartum hemorrhage 5 days after the CS. Adverse events seemed unrelated to the procedure.
Study details: Findings are from a retrospective study including 663 patients who underwent CS, of which 38 patients underwent the preventive B-Lynch suture procedure before excessive blood loss occurred during CS.
Disclosures: No source of funding was reported. The authors declared no conflicts of interest.
Source: Kuwabara M et al. Effectiveness of preventive B-Lynch sutures in patients at a high risk of postpartum hemorrhage. J Obstet Gynaecol Res. 2022 (Sep 11). Doi: 10.1111/jog.15415
Key clinical point: Preventive B-Lynch suture seemed safe and effective in preventing excessive maternal hemorrhage in patients at a high risk for postpartum hemorrhage.
Major finding: Overall, 92% of patients who underwent the B-Lynch suture procedure showed no apparent postoperative bleeding within 2 hours after the cesarean section (CS), with 24 patients requiring intraoperative or postoperative blood transfusion, none requiring hysterectomy, and only 1 patient with a twin pregnancy requiring additional treatment because of secondary postpartum hemorrhage 5 days after the CS. Adverse events seemed unrelated to the procedure.
Study details: Findings are from a retrospective study including 663 patients who underwent CS, of which 38 patients underwent the preventive B-Lynch suture procedure before excessive blood loss occurred during CS.
Disclosures: No source of funding was reported. The authors declared no conflicts of interest.
Source: Kuwabara M et al. Effectiveness of preventive B-Lynch sutures in patients at a high risk of postpartum hemorrhage. J Obstet Gynaecol Res. 2022 (Sep 11). Doi: 10.1111/jog.15415
Key clinical point: Preventive B-Lynch suture seemed safe and effective in preventing excessive maternal hemorrhage in patients at a high risk for postpartum hemorrhage.
Major finding: Overall, 92% of patients who underwent the B-Lynch suture procedure showed no apparent postoperative bleeding within 2 hours after the cesarean section (CS), with 24 patients requiring intraoperative or postoperative blood transfusion, none requiring hysterectomy, and only 1 patient with a twin pregnancy requiring additional treatment because of secondary postpartum hemorrhage 5 days after the CS. Adverse events seemed unrelated to the procedure.
Study details: Findings are from a retrospective study including 663 patients who underwent CS, of which 38 patients underwent the preventive B-Lynch suture procedure before excessive blood loss occurred during CS.
Disclosures: No source of funding was reported. The authors declared no conflicts of interest.
Source: Kuwabara M et al. Effectiveness of preventive B-Lynch sutures in patients at a high risk of postpartum hemorrhage. J Obstet Gynaecol Res. 2022 (Sep 11). Doi: 10.1111/jog.15415
Risk for severe birth injury higher with breech vs cephalic vaginal delivery
Key clinical point: Birth injuries are rare with breech vaginal delivery (VD); however, severe birth injury incidence is nearly 2-times higher with breech VD compared with cephalic VD, with brachial plexus palsy (BPP) being more common with breech vs cephalic VD.
Major finding: The incidence of severe birth injury with breech VD, cephalic VD, and cesarean section with breech presentation were 0.76/100, 0.31/100, and 0.059/100 live births, respectively. BPP occurred more frequently with breech VD (0.6% of live births) than with cephalic VD (0.3% of live births).
Study details: The data come from a retrospective study including 650,528 neonates who were delivered by breech VD (0.7%), breech cesarean section (2.6%), or cephalic VD (96.7%).
Disclosures: This study was partly funded by competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital, Finland. The authors declared no conflicts of interest.
Source: Kekki M et al. Birth injury in breech delivery: A nationwide population-based cohort study in Finland. Arch Gynecol Obstet. 2022 (Sep 8). Doi: 10.1007/s00404-022-06772-1
Key clinical point: Birth injuries are rare with breech vaginal delivery (VD); however, severe birth injury incidence is nearly 2-times higher with breech VD compared with cephalic VD, with brachial plexus palsy (BPP) being more common with breech vs cephalic VD.
Major finding: The incidence of severe birth injury with breech VD, cephalic VD, and cesarean section with breech presentation were 0.76/100, 0.31/100, and 0.059/100 live births, respectively. BPP occurred more frequently with breech VD (0.6% of live births) than with cephalic VD (0.3% of live births).
Study details: The data come from a retrospective study including 650,528 neonates who were delivered by breech VD (0.7%), breech cesarean section (2.6%), or cephalic VD (96.7%).
Disclosures: This study was partly funded by competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital, Finland. The authors declared no conflicts of interest.
Source: Kekki M et al. Birth injury in breech delivery: A nationwide population-based cohort study in Finland. Arch Gynecol Obstet. 2022 (Sep 8). Doi: 10.1007/s00404-022-06772-1
Key clinical point: Birth injuries are rare with breech vaginal delivery (VD); however, severe birth injury incidence is nearly 2-times higher with breech VD compared with cephalic VD, with brachial plexus palsy (BPP) being more common with breech vs cephalic VD.
Major finding: The incidence of severe birth injury with breech VD, cephalic VD, and cesarean section with breech presentation were 0.76/100, 0.31/100, and 0.059/100 live births, respectively. BPP occurred more frequently with breech VD (0.6% of live births) than with cephalic VD (0.3% of live births).
Study details: The data come from a retrospective study including 650,528 neonates who were delivered by breech VD (0.7%), breech cesarean section (2.6%), or cephalic VD (96.7%).
Disclosures: This study was partly funded by competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital, Finland. The authors declared no conflicts of interest.
Source: Kekki M et al. Birth injury in breech delivery: A nationwide population-based cohort study in Finland. Arch Gynecol Obstet. 2022 (Sep 8). Doi: 10.1007/s00404-022-06772-1
Preterm preeclampsia associated with persistent cardiovascular morbidity
Key clinical point: A majority of women with preterm preeclampsia showed persistent cardiovascular morbidity at 6 months postpartum, which may have significant implications to long-term cardiovascular health.
Major finding: At 6 months postpartum, diastolic dysfunction, increased total vascular resistance (TVR), and persistent left ventricular remodeling were observed in 61%, 75%, and 41% of women, respectively, with 46% of women with no pre-existing hypertension having de novo hypertension and only 5% of women having a completely normal echocardiogram. A significant association was observed between prolonged preeclampsia duration and increased TVR at 6 months (P = .02).
Study details: Findings are from a sub-study of PICk-UP trial involving 44 postnatal women with preterm preeclampsia who delivered before 37 weeks.
Disclosures: This study was funded by the Medical Research Council, UK. The authors declared no competing financial interests.
Source: Ormesher L et al. Postnatal cardiovascular morbidity following preterm pre-eclampsia: An observational study. Pregnancy Hypertens. 2022;30:68-81 (Aug 17). Doi: 10.1016/j.preghy.2022.08.007
Key clinical point: A majority of women with preterm preeclampsia showed persistent cardiovascular morbidity at 6 months postpartum, which may have significant implications to long-term cardiovascular health.
Major finding: At 6 months postpartum, diastolic dysfunction, increased total vascular resistance (TVR), and persistent left ventricular remodeling were observed in 61%, 75%, and 41% of women, respectively, with 46% of women with no pre-existing hypertension having de novo hypertension and only 5% of women having a completely normal echocardiogram. A significant association was observed between prolonged preeclampsia duration and increased TVR at 6 months (P = .02).
Study details: Findings are from a sub-study of PICk-UP trial involving 44 postnatal women with preterm preeclampsia who delivered before 37 weeks.
Disclosures: This study was funded by the Medical Research Council, UK. The authors declared no competing financial interests.
Source: Ormesher L et al. Postnatal cardiovascular morbidity following preterm pre-eclampsia: An observational study. Pregnancy Hypertens. 2022;30:68-81 (Aug 17). Doi: 10.1016/j.preghy.2022.08.007
Key clinical point: A majority of women with preterm preeclampsia showed persistent cardiovascular morbidity at 6 months postpartum, which may have significant implications to long-term cardiovascular health.
Major finding: At 6 months postpartum, diastolic dysfunction, increased total vascular resistance (TVR), and persistent left ventricular remodeling were observed in 61%, 75%, and 41% of women, respectively, with 46% of women with no pre-existing hypertension having de novo hypertension and only 5% of women having a completely normal echocardiogram. A significant association was observed between prolonged preeclampsia duration and increased TVR at 6 months (P = .02).
Study details: Findings are from a sub-study of PICk-UP trial involving 44 postnatal women with preterm preeclampsia who delivered before 37 weeks.
Disclosures: This study was funded by the Medical Research Council, UK. The authors declared no competing financial interests.
Source: Ormesher L et al. Postnatal cardiovascular morbidity following preterm pre-eclampsia: An observational study. Pregnancy Hypertens. 2022;30:68-81 (Aug 17). Doi: 10.1016/j.preghy.2022.08.007
Consistent increase in incidence of acute high-risk chest pain diseases during pregnancy and puerperium
Key clinical point: The incidence of acute high-risk chest pain (AHRCP) diseases during pregnancy and puerperium has increased consistently over a decade, with advanced maternal age being a significant risk factor.
Major finding: The incidence of AHRCP diseases during pregnancy and puerperium increased from 79.92/100,000 hospitalizations in 2008 to 114.79/100,000 hospitalizations in 2017 (Ptrend < .0001), with pulmonary embolism (86.5%) occurring 10-fold and 26-fold more frequently than acute myocardial infarction (9.6%) and aortic dissection (3.3%), respectively. Maternal age over 45 years was a significant risk factor (odds ratio 4.25; 95% CI 3.80-4.75).
Study details: Findings are from an observational analysis of 41,174,101 patients hospitalized for pregnancy and puerperium, of which 40,285 were diagnosed with AHRCP diseases.
Disclosures: This study was supported by the 3-Year Action Plan for Strengthening Public Health System in Shanghai (2020–2022) and other sources. The authors declared no conflicts of interest.
Source: Wu S et al. Incidence and outcomes of acute high-risk chest pain diseases during pregnancy and puerperium. Front Cardiovasc Med. 2022;9:968964 (Aug 11). Doi: 10.3389/fcvm.2022.968964
Key clinical point: The incidence of acute high-risk chest pain (AHRCP) diseases during pregnancy and puerperium has increased consistently over a decade, with advanced maternal age being a significant risk factor.
Major finding: The incidence of AHRCP diseases during pregnancy and puerperium increased from 79.92/100,000 hospitalizations in 2008 to 114.79/100,000 hospitalizations in 2017 (Ptrend < .0001), with pulmonary embolism (86.5%) occurring 10-fold and 26-fold more frequently than acute myocardial infarction (9.6%) and aortic dissection (3.3%), respectively. Maternal age over 45 years was a significant risk factor (odds ratio 4.25; 95% CI 3.80-4.75).
Study details: Findings are from an observational analysis of 41,174,101 patients hospitalized for pregnancy and puerperium, of which 40,285 were diagnosed with AHRCP diseases.
Disclosures: This study was supported by the 3-Year Action Plan for Strengthening Public Health System in Shanghai (2020–2022) and other sources. The authors declared no conflicts of interest.
Source: Wu S et al. Incidence and outcomes of acute high-risk chest pain diseases during pregnancy and puerperium. Front Cardiovasc Med. 2022;9:968964 (Aug 11). Doi: 10.3389/fcvm.2022.968964
Key clinical point: The incidence of acute high-risk chest pain (AHRCP) diseases during pregnancy and puerperium has increased consistently over a decade, with advanced maternal age being a significant risk factor.
Major finding: The incidence of AHRCP diseases during pregnancy and puerperium increased from 79.92/100,000 hospitalizations in 2008 to 114.79/100,000 hospitalizations in 2017 (Ptrend < .0001), with pulmonary embolism (86.5%) occurring 10-fold and 26-fold more frequently than acute myocardial infarction (9.6%) and aortic dissection (3.3%), respectively. Maternal age over 45 years was a significant risk factor (odds ratio 4.25; 95% CI 3.80-4.75).
Study details: Findings are from an observational analysis of 41,174,101 patients hospitalized for pregnancy and puerperium, of which 40,285 were diagnosed with AHRCP diseases.
Disclosures: This study was supported by the 3-Year Action Plan for Strengthening Public Health System in Shanghai (2020–2022) and other sources. The authors declared no conflicts of interest.
Source: Wu S et al. Incidence and outcomes of acute high-risk chest pain diseases during pregnancy and puerperium. Front Cardiovasc Med. 2022;9:968964 (Aug 11). Doi: 10.3389/fcvm.2022.968964
Evidence spanning 2 decades reveals trend changes in risk factors for postpartum hemorrhage
Key clinical point: Analysis over 2 decades demonstrated trend changes in individual contribution of risk factors for postpartum hemorrhage, with perineal or vaginal tears increasing, large for gestational age neonate decreasing, and other risk factors remaining stable.
Major finding: The incidence of postpartum hemorrhage increased from 0.5% in 1988 to 0.6% in 2014. Among risk factors for postpartum hemorrhage, perineal or vaginal tear demonstrated a rising trend (P = .01), delivery of large for gestational age neonate demonstrated a declining trend (P < .001), and other risk factors, such as preeclampsia, vacuum extraction delivery, and retained placenta, remained stable during the study period.
Study details: Findings are from a population-based, retrospective, nested, case-control study including 285,992 pregnancies, of which 1684 were complicated by postpartum hemorrhage.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Sade S et al. Trend changes in the individual contribution of risk factors for postpartum hemorrhage over more than two decades. Matern Child Health J. 2022 (Aug 24). Doi: 10.1007/s10995-022-03461-y
Key clinical point: Analysis over 2 decades demonstrated trend changes in individual contribution of risk factors for postpartum hemorrhage, with perineal or vaginal tears increasing, large for gestational age neonate decreasing, and other risk factors remaining stable.
Major finding: The incidence of postpartum hemorrhage increased from 0.5% in 1988 to 0.6% in 2014. Among risk factors for postpartum hemorrhage, perineal or vaginal tear demonstrated a rising trend (P = .01), delivery of large for gestational age neonate demonstrated a declining trend (P < .001), and other risk factors, such as preeclampsia, vacuum extraction delivery, and retained placenta, remained stable during the study period.
Study details: Findings are from a population-based, retrospective, nested, case-control study including 285,992 pregnancies, of which 1684 were complicated by postpartum hemorrhage.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Sade S et al. Trend changes in the individual contribution of risk factors for postpartum hemorrhage over more than two decades. Matern Child Health J. 2022 (Aug 24). Doi: 10.1007/s10995-022-03461-y
Key clinical point: Analysis over 2 decades demonstrated trend changes in individual contribution of risk factors for postpartum hemorrhage, with perineal or vaginal tears increasing, large for gestational age neonate decreasing, and other risk factors remaining stable.
Major finding: The incidence of postpartum hemorrhage increased from 0.5% in 1988 to 0.6% in 2014. Among risk factors for postpartum hemorrhage, perineal or vaginal tear demonstrated a rising trend (P = .01), delivery of large for gestational age neonate demonstrated a declining trend (P < .001), and other risk factors, such as preeclampsia, vacuum extraction delivery, and retained placenta, remained stable during the study period.
Study details: Findings are from a population-based, retrospective, nested, case-control study including 285,992 pregnancies, of which 1684 were complicated by postpartum hemorrhage.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Sade S et al. Trend changes in the individual contribution of risk factors for postpartum hemorrhage over more than two decades. Matern Child Health J. 2022 (Aug 24). Doi: 10.1007/s10995-022-03461-y
Risk factors for intrauterine tamponade failure in women with postpartum hemorrhage
Key clinical point: Cesarean delivery, preeclampsia, and uterine rupture were independently associated with a higher risk for intrauterine tamponade failure in women with deliveries complicated by postpartum hemorrhage.
Major finding: Intrauterine tamponade failure rate was 11.1%. The risk for intrauterine tamponade failure was higher in women with cesarean delivery (adjusted odds ratio [aOR] 4.2; 95% CI 2.9-6.0), preeclampsia (aOR 2.3; 95% CI 1.3-3.9), and uterine rupture (aOR 14.1; 95% CI 2.4-83.0).
Study details: Findings are from a population-based retrospective cohort study including 1761 women with deliveries complicated by postpartum hemorrhage who underwent intrauterine tamponade within 24 hours of postpartum hemorrhage to manage persistent bleeding.
Disclosures: This study did not report any source of funding. No conflicts of interest were declared.
Source: Gibier M et al. Risk factors for intrauterine tamponade failure in postpartum hemorrhage. Obstet Gynecol. 2022;140(3):439-446 (Aug 3). Doi: 10.1097/AOG.0000000000004888
Key clinical point: Cesarean delivery, preeclampsia, and uterine rupture were independently associated with a higher risk for intrauterine tamponade failure in women with deliveries complicated by postpartum hemorrhage.
Major finding: Intrauterine tamponade failure rate was 11.1%. The risk for intrauterine tamponade failure was higher in women with cesarean delivery (adjusted odds ratio [aOR] 4.2; 95% CI 2.9-6.0), preeclampsia (aOR 2.3; 95% CI 1.3-3.9), and uterine rupture (aOR 14.1; 95% CI 2.4-83.0).
Study details: Findings are from a population-based retrospective cohort study including 1761 women with deliveries complicated by postpartum hemorrhage who underwent intrauterine tamponade within 24 hours of postpartum hemorrhage to manage persistent bleeding.
Disclosures: This study did not report any source of funding. No conflicts of interest were declared.
Source: Gibier M et al. Risk factors for intrauterine tamponade failure in postpartum hemorrhage. Obstet Gynecol. 2022;140(3):439-446 (Aug 3). Doi: 10.1097/AOG.0000000000004888
Key clinical point: Cesarean delivery, preeclampsia, and uterine rupture were independently associated with a higher risk for intrauterine tamponade failure in women with deliveries complicated by postpartum hemorrhage.
Major finding: Intrauterine tamponade failure rate was 11.1%. The risk for intrauterine tamponade failure was higher in women with cesarean delivery (adjusted odds ratio [aOR] 4.2; 95% CI 2.9-6.0), preeclampsia (aOR 2.3; 95% CI 1.3-3.9), and uterine rupture (aOR 14.1; 95% CI 2.4-83.0).
Study details: Findings are from a population-based retrospective cohort study including 1761 women with deliveries complicated by postpartum hemorrhage who underwent intrauterine tamponade within 24 hours of postpartum hemorrhage to manage persistent bleeding.
Disclosures: This study did not report any source of funding. No conflicts of interest were declared.
Source: Gibier M et al. Risk factors for intrauterine tamponade failure in postpartum hemorrhage. Obstet Gynecol. 2022;140(3):439-446 (Aug 3). Doi: 10.1097/AOG.0000000000004888
Labetalol vs nifedipine associated with higher rates of postpartum readmission for hypertension
Key clinical point: The chances of postpartum readmission for hypertension were significantly higher among patients discharged with labetalol vs nifedipine after delivery, irrespective of the severity of their hypertensive disorder of pregnancy.
Major finding: Compared with nifedipine, the chances of postpartum readmission for hypertension were higher with labetalol (adjusted odds ratio [aOR] 1.63, 95% CI 1.43-1.85), with the risk being persistent among patients with mild (aOR 1.57; 95% CI 1.29-1.93) and severe (aOR 1.63, 95% CI 1.43-1.85) hypertensive disorders.
Study details: This study evaluated 24,477 patients who were discharged with nifedipine (36.8%), labetalol (57.7%), or both medications (5.6%) after delivery.
Disclosures: This study did not report any source of funding. DJ Lyell declared receiving payment from various sources.
Source: Do SC et al. Postpartum readmission for hypertension after discharge on labetalol or nifedipine. Obstet Gynecol. 2022;140(4):591-598 (Sep 8). Doi: 10.1097/AOG.0000000000004918
Key clinical point: The chances of postpartum readmission for hypertension were significantly higher among patients discharged with labetalol vs nifedipine after delivery, irrespective of the severity of their hypertensive disorder of pregnancy.
Major finding: Compared with nifedipine, the chances of postpartum readmission for hypertension were higher with labetalol (adjusted odds ratio [aOR] 1.63, 95% CI 1.43-1.85), with the risk being persistent among patients with mild (aOR 1.57; 95% CI 1.29-1.93) and severe (aOR 1.63, 95% CI 1.43-1.85) hypertensive disorders.
Study details: This study evaluated 24,477 patients who were discharged with nifedipine (36.8%), labetalol (57.7%), or both medications (5.6%) after delivery.
Disclosures: This study did not report any source of funding. DJ Lyell declared receiving payment from various sources.
Source: Do SC et al. Postpartum readmission for hypertension after discharge on labetalol or nifedipine. Obstet Gynecol. 2022;140(4):591-598 (Sep 8). Doi: 10.1097/AOG.0000000000004918
Key clinical point: The chances of postpartum readmission for hypertension were significantly higher among patients discharged with labetalol vs nifedipine after delivery, irrespective of the severity of their hypertensive disorder of pregnancy.
Major finding: Compared with nifedipine, the chances of postpartum readmission for hypertension were higher with labetalol (adjusted odds ratio [aOR] 1.63, 95% CI 1.43-1.85), with the risk being persistent among patients with mild (aOR 1.57; 95% CI 1.29-1.93) and severe (aOR 1.63, 95% CI 1.43-1.85) hypertensive disorders.
Study details: This study evaluated 24,477 patients who were discharged with nifedipine (36.8%), labetalol (57.7%), or both medications (5.6%) after delivery.
Disclosures: This study did not report any source of funding. DJ Lyell declared receiving payment from various sources.
Source: Do SC et al. Postpartum readmission for hypertension after discharge on labetalol or nifedipine. Obstet Gynecol. 2022;140(4):591-598 (Sep 8). Doi: 10.1097/AOG.0000000000004918
Simulation training on management of shoulder dystocia reduces incidence of permanent BPBI
Key clinical point: Weekly 3-hour simulation-based training of midwives and doctors on shoulder dystocia (SD) management significantly reduced the incidence of permanent brachial plexus birth injury (BPBI).
Major finding: Despite an increase in the incidence of SD cases (0.1% vs 0.3%; P < .001) and risk factors in pre-training vs post-training period, the incidence of permanent BPBI decreased significantly (0.05% vs 0.02%; P < .001), with the risk for permanent BPBI among those with SD reducing (43.5% vs 6.0%; P < .001) and the rate of successful posterior arm delivery increasing (11.3% vs 23.4%; P = .04) significantly after the implementation of systematic simulation-based training.
Study details: Findings are from a retrospective observational study including 113,785 vertex deliveries performed by a team of doctors and midwives after receiving the weekly 3-hour simulation-based training.
Disclosures: This study was funded by Helsinki University State Research Funding. No conflicts of interest were declared.
Source: Kaijomaa M et al. Impact of simulation training on the management of shoulder dystocia and incidence of permanent brachial plexus birth injury: An observational study. BJOG. 2022 (Aug 10). Doi: 10.1111/1471-0528.17278
Key clinical point: Weekly 3-hour simulation-based training of midwives and doctors on shoulder dystocia (SD) management significantly reduced the incidence of permanent brachial plexus birth injury (BPBI).
Major finding: Despite an increase in the incidence of SD cases (0.1% vs 0.3%; P < .001) and risk factors in pre-training vs post-training period, the incidence of permanent BPBI decreased significantly (0.05% vs 0.02%; P < .001), with the risk for permanent BPBI among those with SD reducing (43.5% vs 6.0%; P < .001) and the rate of successful posterior arm delivery increasing (11.3% vs 23.4%; P = .04) significantly after the implementation of systematic simulation-based training.
Study details: Findings are from a retrospective observational study including 113,785 vertex deliveries performed by a team of doctors and midwives after receiving the weekly 3-hour simulation-based training.
Disclosures: This study was funded by Helsinki University State Research Funding. No conflicts of interest were declared.
Source: Kaijomaa M et al. Impact of simulation training on the management of shoulder dystocia and incidence of permanent brachial plexus birth injury: An observational study. BJOG. 2022 (Aug 10). Doi: 10.1111/1471-0528.17278
Key clinical point: Weekly 3-hour simulation-based training of midwives and doctors on shoulder dystocia (SD) management significantly reduced the incidence of permanent brachial plexus birth injury (BPBI).
Major finding: Despite an increase in the incidence of SD cases (0.1% vs 0.3%; P < .001) and risk factors in pre-training vs post-training period, the incidence of permanent BPBI decreased significantly (0.05% vs 0.02%; P < .001), with the risk for permanent BPBI among those with SD reducing (43.5% vs 6.0%; P < .001) and the rate of successful posterior arm delivery increasing (11.3% vs 23.4%; P = .04) significantly after the implementation of systematic simulation-based training.
Study details: Findings are from a retrospective observational study including 113,785 vertex deliveries performed by a team of doctors and midwives after receiving the weekly 3-hour simulation-based training.
Disclosures: This study was funded by Helsinki University State Research Funding. No conflicts of interest were declared.
Source: Kaijomaa M et al. Impact of simulation training on the management of shoulder dystocia and incidence of permanent brachial plexus birth injury: An observational study. BJOG. 2022 (Aug 10). Doi: 10.1111/1471-0528.17278
November 2022 - ICYMI
Gastroenterology
August 2022
Johnson-Laghi KA, Mattar MC. Integrating cognitive apprenticeship into gastroenterology clinical training. Gastroenterology. 2022 Aug;163(2):364-7. doi: 10.1053/j.gastro.2022.06.013.
Wood LD et al. Pancreatic cancer: Pathogenesis, screening, diagnosis, and treatment. Gastroenterology. 2022 Aug;163(2):386-402.e1. doi: 10.1053/j.gastro.2022.03.056.
Calderwood AH and Robertson DJ. Stopping surveillance in gastrointestinal conditions: Thoughts on the scope of the problem and potential solutions. Gastroenterology. 2022 Aug;163(2):345-9. doi: 10.1053/j.gastro.2022.04.009.
September 2022
Donnangelo LL et al. Disclosure and reflection after an adverse event: Tips for training and practice. Gastroenterology. 2022 Sep;163(3):568-71. doi: 10.1053/j.gastro.2022.07.003.
Chey WD et al. Vonoprazan triple and dual therapy for Helicobacter pylori infection in the United States and Europe: Randomized clinical trial. Gastroenterology. 2022 Sep;163(3):608-19. doi: 10.1053/j.gastro.2022.05.055.
Bushyhead D and Quigley EMM. Small intestinal bacterial overgrowth-pathophysiology and its implications for definition and management. Gastroenterology. 2022 Sep;163(3):593-607. doi: 10.1053/j.gastro.2022.04.002.
Long MT et al. AGA Clinical practice update: Diagnosis and management of nonalcoholic fatty liver disease in lean individuals: Expert review. Gastroenterology. 2022 Sep;163(3):764-74.e1. doi: 10.1053/j.gastro.2022.06.023.
CGH
August 2022
Lennon AM and Vege SS. Pancreatic cyst surveillance. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1663-7.e1. doi: 10.1016/j.cgh.2022.03.002.
Crockett SD et al. Large Polyp Study Group Consortium. Clip closure does not reduce risk of bleeding after resection of large serrated polyps: Results from a randomized trial. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1757-17--65.e4. doi: 10.1016/j.cgh.2021.12.036.
Martin P et al. Treatment algorithm for managing chronic hepatitis b virus infection in the United States: 2021 update. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1766-75. doi: 10.1016/j.cgh.2021.07.036.
September 2022
Pawlak KM et al. How to train the next generation to provide high-quality peer-reviews. Clin Gastroenterol Hepatol. 2022 Sep;20(9):1902-6. doi: 10.1016/j.cgh.2022.05.018.
Choung RS et al. Collagenous gastritis: Characteristics and response to topical budesonide. Clin Gastroenterol Hepatol. 2022 Sep;20(9):1977-85.e1. doi: 10.1016/j.cgh.2021.11.033.
Basnayake C et al. Long-term outcome of multidisciplinary versus standard gastroenterologist care for functional gastrointestinal disorders: A randomized trial. Clin Gastroenterol Hepatol. 2022 Sep;20(9):2102-11.e9. doi: 10.1016/j.cgh.2021.12.005.
Deutsch-Link S et al. Alcohol-associated liver disease mortality increased from 2017 to 2020 and accelerated during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2022 Sep;20(9):2142-4.e2. doi: 10.1016/j.cgh.2022.03.017.
TIGE
Nakamatsu, Dai et al. Safety of cold snare polypectomy for small colorectal polyps in patients receiving antithrombotic therapy. Tech Innov Gastrointest Endosc. 2022 Apr 8;24[3]:246-53. doi: 10.1016/j.tige.2022.03.008.
Gastro Hep Advances
Brindusa Truta et al. Outcomes of continuation vs. discontinuation of adalimumab therapy during third trimester of pregnancy in inflammatory bowel disease. Gastro Hep Advances. 2022 Jan 1;1[5]:785-91. doi: 10.1016/j.gastha.2022.04.009.
Gastroenterology
August 2022
Johnson-Laghi KA, Mattar MC. Integrating cognitive apprenticeship into gastroenterology clinical training. Gastroenterology. 2022 Aug;163(2):364-7. doi: 10.1053/j.gastro.2022.06.013.
Wood LD et al. Pancreatic cancer: Pathogenesis, screening, diagnosis, and treatment. Gastroenterology. 2022 Aug;163(2):386-402.e1. doi: 10.1053/j.gastro.2022.03.056.
Calderwood AH and Robertson DJ. Stopping surveillance in gastrointestinal conditions: Thoughts on the scope of the problem and potential solutions. Gastroenterology. 2022 Aug;163(2):345-9. doi: 10.1053/j.gastro.2022.04.009.
September 2022
Donnangelo LL et al. Disclosure and reflection after an adverse event: Tips for training and practice. Gastroenterology. 2022 Sep;163(3):568-71. doi: 10.1053/j.gastro.2022.07.003.
Chey WD et al. Vonoprazan triple and dual therapy for Helicobacter pylori infection in the United States and Europe: Randomized clinical trial. Gastroenterology. 2022 Sep;163(3):608-19. doi: 10.1053/j.gastro.2022.05.055.
Bushyhead D and Quigley EMM. Small intestinal bacterial overgrowth-pathophysiology and its implications for definition and management. Gastroenterology. 2022 Sep;163(3):593-607. doi: 10.1053/j.gastro.2022.04.002.
Long MT et al. AGA Clinical practice update: Diagnosis and management of nonalcoholic fatty liver disease in lean individuals: Expert review. Gastroenterology. 2022 Sep;163(3):764-74.e1. doi: 10.1053/j.gastro.2022.06.023.
CGH
August 2022
Lennon AM and Vege SS. Pancreatic cyst surveillance. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1663-7.e1. doi: 10.1016/j.cgh.2022.03.002.
Crockett SD et al. Large Polyp Study Group Consortium. Clip closure does not reduce risk of bleeding after resection of large serrated polyps: Results from a randomized trial. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1757-17--65.e4. doi: 10.1016/j.cgh.2021.12.036.
Martin P et al. Treatment algorithm for managing chronic hepatitis b virus infection in the United States: 2021 update. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1766-75. doi: 10.1016/j.cgh.2021.07.036.
September 2022
Pawlak KM et al. How to train the next generation to provide high-quality peer-reviews. Clin Gastroenterol Hepatol. 2022 Sep;20(9):1902-6. doi: 10.1016/j.cgh.2022.05.018.
Choung RS et al. Collagenous gastritis: Characteristics and response to topical budesonide. Clin Gastroenterol Hepatol. 2022 Sep;20(9):1977-85.e1. doi: 10.1016/j.cgh.2021.11.033.
Basnayake C et al. Long-term outcome of multidisciplinary versus standard gastroenterologist care for functional gastrointestinal disorders: A randomized trial. Clin Gastroenterol Hepatol. 2022 Sep;20(9):2102-11.e9. doi: 10.1016/j.cgh.2021.12.005.
Deutsch-Link S et al. Alcohol-associated liver disease mortality increased from 2017 to 2020 and accelerated during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2022 Sep;20(9):2142-4.e2. doi: 10.1016/j.cgh.2022.03.017.
TIGE
Nakamatsu, Dai et al. Safety of cold snare polypectomy for small colorectal polyps in patients receiving antithrombotic therapy. Tech Innov Gastrointest Endosc. 2022 Apr 8;24[3]:246-53. doi: 10.1016/j.tige.2022.03.008.
Gastro Hep Advances
Brindusa Truta et al. Outcomes of continuation vs. discontinuation of adalimumab therapy during third trimester of pregnancy in inflammatory bowel disease. Gastro Hep Advances. 2022 Jan 1;1[5]:785-91. doi: 10.1016/j.gastha.2022.04.009.
Gastroenterology
August 2022
Johnson-Laghi KA, Mattar MC. Integrating cognitive apprenticeship into gastroenterology clinical training. Gastroenterology. 2022 Aug;163(2):364-7. doi: 10.1053/j.gastro.2022.06.013.
Wood LD et al. Pancreatic cancer: Pathogenesis, screening, diagnosis, and treatment. Gastroenterology. 2022 Aug;163(2):386-402.e1. doi: 10.1053/j.gastro.2022.03.056.
Calderwood AH and Robertson DJ. Stopping surveillance in gastrointestinal conditions: Thoughts on the scope of the problem and potential solutions. Gastroenterology. 2022 Aug;163(2):345-9. doi: 10.1053/j.gastro.2022.04.009.
September 2022
Donnangelo LL et al. Disclosure and reflection after an adverse event: Tips for training and practice. Gastroenterology. 2022 Sep;163(3):568-71. doi: 10.1053/j.gastro.2022.07.003.
Chey WD et al. Vonoprazan triple and dual therapy for Helicobacter pylori infection in the United States and Europe: Randomized clinical trial. Gastroenterology. 2022 Sep;163(3):608-19. doi: 10.1053/j.gastro.2022.05.055.
Bushyhead D and Quigley EMM. Small intestinal bacterial overgrowth-pathophysiology and its implications for definition and management. Gastroenterology. 2022 Sep;163(3):593-607. doi: 10.1053/j.gastro.2022.04.002.
Long MT et al. AGA Clinical practice update: Diagnosis and management of nonalcoholic fatty liver disease in lean individuals: Expert review. Gastroenterology. 2022 Sep;163(3):764-74.e1. doi: 10.1053/j.gastro.2022.06.023.
CGH
August 2022
Lennon AM and Vege SS. Pancreatic cyst surveillance. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1663-7.e1. doi: 10.1016/j.cgh.2022.03.002.
Crockett SD et al. Large Polyp Study Group Consortium. Clip closure does not reduce risk of bleeding after resection of large serrated polyps: Results from a randomized trial. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1757-17--65.e4. doi: 10.1016/j.cgh.2021.12.036.
Martin P et al. Treatment algorithm for managing chronic hepatitis b virus infection in the United States: 2021 update. Clin Gastroenterol Hepatol. 2022 Aug;20(8):1766-75. doi: 10.1016/j.cgh.2021.07.036.
September 2022
Pawlak KM et al. How to train the next generation to provide high-quality peer-reviews. Clin Gastroenterol Hepatol. 2022 Sep;20(9):1902-6. doi: 10.1016/j.cgh.2022.05.018.
Choung RS et al. Collagenous gastritis: Characteristics and response to topical budesonide. Clin Gastroenterol Hepatol. 2022 Sep;20(9):1977-85.e1. doi: 10.1016/j.cgh.2021.11.033.
Basnayake C et al. Long-term outcome of multidisciplinary versus standard gastroenterologist care for functional gastrointestinal disorders: A randomized trial. Clin Gastroenterol Hepatol. 2022 Sep;20(9):2102-11.e9. doi: 10.1016/j.cgh.2021.12.005.
Deutsch-Link S et al. Alcohol-associated liver disease mortality increased from 2017 to 2020 and accelerated during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2022 Sep;20(9):2142-4.e2. doi: 10.1016/j.cgh.2022.03.017.
TIGE
Nakamatsu, Dai et al. Safety of cold snare polypectomy for small colorectal polyps in patients receiving antithrombotic therapy. Tech Innov Gastrointest Endosc. 2022 Apr 8;24[3]:246-53. doi: 10.1016/j.tige.2022.03.008.
Gastro Hep Advances
Brindusa Truta et al. Outcomes of continuation vs. discontinuation of adalimumab therapy during third trimester of pregnancy in inflammatory bowel disease. Gastro Hep Advances. 2022 Jan 1;1[5]:785-91. doi: 10.1016/j.gastha.2022.04.009.
The role of repeat uterine curettage in postmolar gestational trophoblastic neoplasia
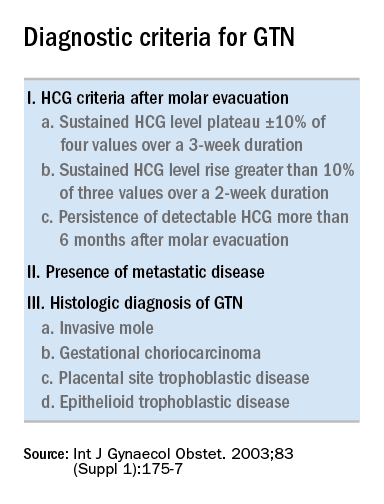
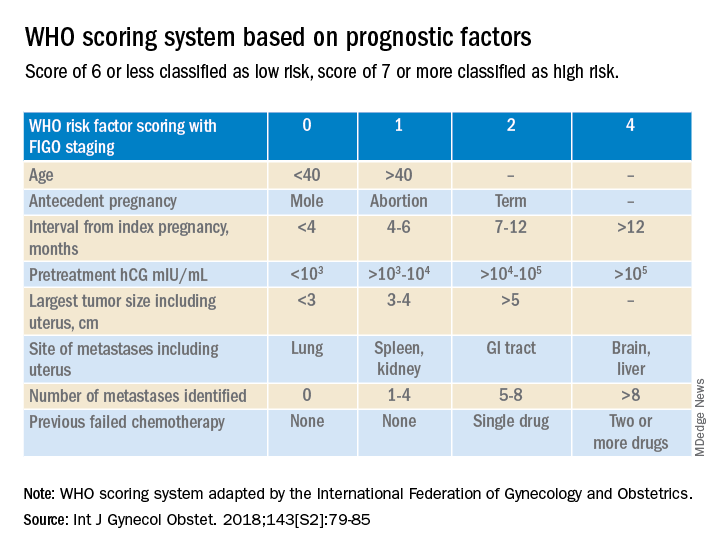
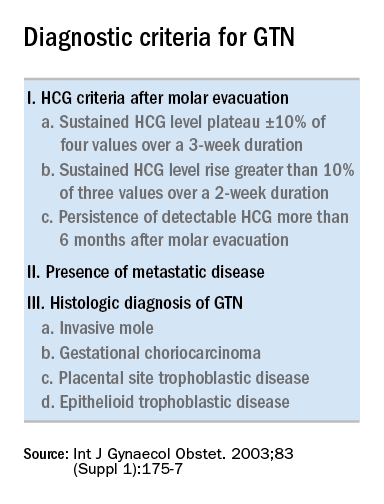
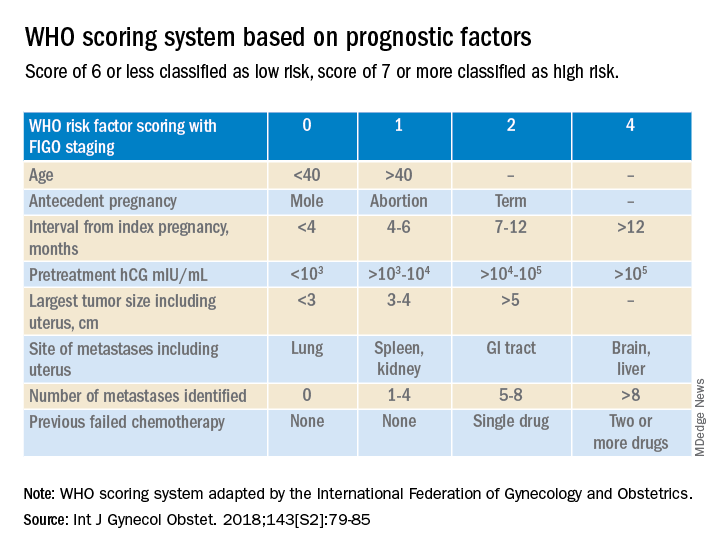
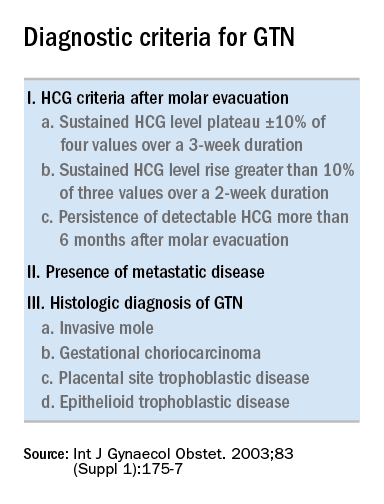
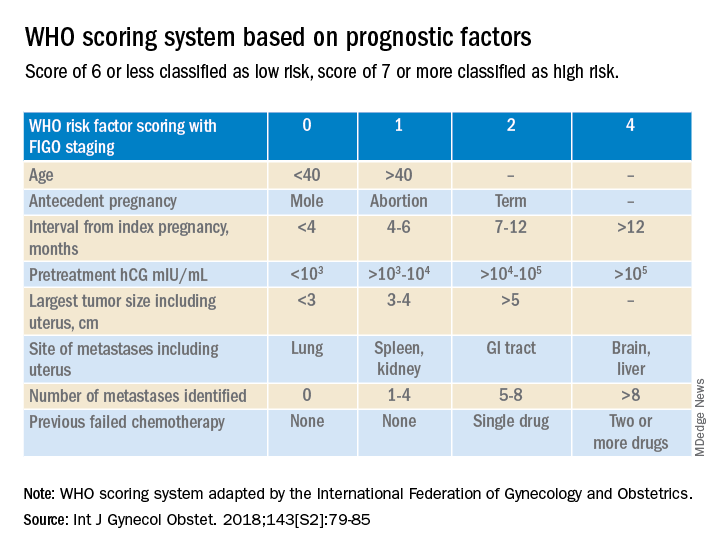
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
