User login
Paid Parental Leave: Impact on Maternal Mental Health and Child Wellbeing
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Topical Roflumilast Effective in 4 Weeks for Atopic Dermatitis in Young Children
SAN DIEGO — Treatment with (AD), according to the results of a phase 3 study reported at the annual meeting of the American Academy of Dermatology.
Among patients treated with roflumilast cream, 0.05%, 25.4% reached the primary endpoint of “clear” or “almost clear” plus a two-grade improvement from baseline at week 4 vs 10.7% among those in the vehicle group (P < .0001) in a phase 3 randomized controlled trial of children. The findings were released in a late-breaker session at the meeting.
Roflumilast cream, 0.3% (Zoryve), is approved by the Food and Drug Administration (FDA) for treating psoriasis in patients 6 years and older, and lower doses are being evaluated for AD: 0.15% for adults and children ages 6 and older, and 0.05% for ages 2-5. Roflumilast is a phosphodiesterase-4 inhibitor. In 2023, the FDA accepted a supplemental drug application from the manufacturer, Arcutis, for roflumilast, 0.15%, for treating AD in patients ages 6 and older, based on the results from two recently published phase 3 trials, INTEGUMENT-1 and INTEGUMENT-2.
The study of younger children, INTEGUMENT-PED, recruited 652 patients aged 2-5 with mild to moderate AD, with a Validated Investigator Global Assessment scale for AD (vlGA-AD) score of 2 or 3, a mean body surface area of 22% overall (range, 3%-82%), and an Eczema Area and Severity Index (EASI) score of at least 5. Of the patients enrolled, 437 were assigned to 0.05% roflumilast cream, applied once a day for 4 weeks (mean age, 3.3 years; 51.6% male; 67.4% White; 15.6% Black; 8.5% Asian; 8.5% other or more than one race; 80.5% not Latino/Hispanic). The remaining 215 children were assigned to vehicle cream and had similar characteristics.
About 52% of the patients in both groups had an inadequate response, intolerance, or contraindications to topical corticosteroids (and about 17% for topical calcineurin inhibitors and about 9% for crisaborole).
The proportions of patients who reached “clear” (0) or “almost clear” (1) on the vlGA-AD scale were 35.4% and 14.6%, respectively, at week 4 (P < .0001) for roflumilast and vehicle, respectively, according to the lead author of the study, Lawrence M. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, who presented the results at the meeting. In addition, 39.4% and 20.6% achieved an EASI-75 (a secondary endpoint), respectively (P < .0001), and itch also improved within 24 hours of starting treatment.
With regard to safety, 29.7% of patients taking roflumilast had treatment-emergent adverse effects (including upper respiratory tract infections in 4.1%) vs 21.9% of those in the vehicle arm (including upper respiratory tract infections in 1.4%). Reports of pain at the administration site were low (1.6% for roflumilast vs 1.9% for vehicle). Only one patient, a 2-year-old girl, had a treatment-emergent serious adverse event. The child, who was in the roflumilast group, had cellulitis involving noneczematous skin and was treated with antibiotics in the hospital for 3 days. The event was not attributed to roflumilast, which was stopped for 5 days, according to Dr. Eichenfield.
In an interview, Fairfield, Connecticut–based dermatologist Brittany Craiglow, MD, who was not involved in the study, said topical roflumilast would be an “important” new treatment because there are still few nonsteroidal options for the treatment of AD in children under 12. “The excellent local tolerability combined with early improvements in itch and skin clearance will make this a particularly attractive option, if approved,” she said.
Dr. Eichenfield disclosed multiple relationships with various drugmakers. He and several other study authors are investigators and/or consultants for Arcutis and received grants/research funding and/or honoraria. Two authors are Arcutis employees. Other disclosure information for the authors was not immediately available. Dr. Craiglow had no disclosures.
A version of this article appeared on Medscape.com .
SAN DIEGO — Treatment with (AD), according to the results of a phase 3 study reported at the annual meeting of the American Academy of Dermatology.
Among patients treated with roflumilast cream, 0.05%, 25.4% reached the primary endpoint of “clear” or “almost clear” plus a two-grade improvement from baseline at week 4 vs 10.7% among those in the vehicle group (P < .0001) in a phase 3 randomized controlled trial of children. The findings were released in a late-breaker session at the meeting.
Roflumilast cream, 0.3% (Zoryve), is approved by the Food and Drug Administration (FDA) for treating psoriasis in patients 6 years and older, and lower doses are being evaluated for AD: 0.15% for adults and children ages 6 and older, and 0.05% for ages 2-5. Roflumilast is a phosphodiesterase-4 inhibitor. In 2023, the FDA accepted a supplemental drug application from the manufacturer, Arcutis, for roflumilast, 0.15%, for treating AD in patients ages 6 and older, based on the results from two recently published phase 3 trials, INTEGUMENT-1 and INTEGUMENT-2.
The study of younger children, INTEGUMENT-PED, recruited 652 patients aged 2-5 with mild to moderate AD, with a Validated Investigator Global Assessment scale for AD (vlGA-AD) score of 2 or 3, a mean body surface area of 22% overall (range, 3%-82%), and an Eczema Area and Severity Index (EASI) score of at least 5. Of the patients enrolled, 437 were assigned to 0.05% roflumilast cream, applied once a day for 4 weeks (mean age, 3.3 years; 51.6% male; 67.4% White; 15.6% Black; 8.5% Asian; 8.5% other or more than one race; 80.5% not Latino/Hispanic). The remaining 215 children were assigned to vehicle cream and had similar characteristics.
About 52% of the patients in both groups had an inadequate response, intolerance, or contraindications to topical corticosteroids (and about 17% for topical calcineurin inhibitors and about 9% for crisaborole).
The proportions of patients who reached “clear” (0) or “almost clear” (1) on the vlGA-AD scale were 35.4% and 14.6%, respectively, at week 4 (P < .0001) for roflumilast and vehicle, respectively, according to the lead author of the study, Lawrence M. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, who presented the results at the meeting. In addition, 39.4% and 20.6% achieved an EASI-75 (a secondary endpoint), respectively (P < .0001), and itch also improved within 24 hours of starting treatment.
With regard to safety, 29.7% of patients taking roflumilast had treatment-emergent adverse effects (including upper respiratory tract infections in 4.1%) vs 21.9% of those in the vehicle arm (including upper respiratory tract infections in 1.4%). Reports of pain at the administration site were low (1.6% for roflumilast vs 1.9% for vehicle). Only one patient, a 2-year-old girl, had a treatment-emergent serious adverse event. The child, who was in the roflumilast group, had cellulitis involving noneczematous skin and was treated with antibiotics in the hospital for 3 days. The event was not attributed to roflumilast, which was stopped for 5 days, according to Dr. Eichenfield.
In an interview, Fairfield, Connecticut–based dermatologist Brittany Craiglow, MD, who was not involved in the study, said topical roflumilast would be an “important” new treatment because there are still few nonsteroidal options for the treatment of AD in children under 12. “The excellent local tolerability combined with early improvements in itch and skin clearance will make this a particularly attractive option, if approved,” she said.
Dr. Eichenfield disclosed multiple relationships with various drugmakers. He and several other study authors are investigators and/or consultants for Arcutis and received grants/research funding and/or honoraria. Two authors are Arcutis employees. Other disclosure information for the authors was not immediately available. Dr. Craiglow had no disclosures.
A version of this article appeared on Medscape.com .
SAN DIEGO — Treatment with (AD), according to the results of a phase 3 study reported at the annual meeting of the American Academy of Dermatology.
Among patients treated with roflumilast cream, 0.05%, 25.4% reached the primary endpoint of “clear” or “almost clear” plus a two-grade improvement from baseline at week 4 vs 10.7% among those in the vehicle group (P < .0001) in a phase 3 randomized controlled trial of children. The findings were released in a late-breaker session at the meeting.
Roflumilast cream, 0.3% (Zoryve), is approved by the Food and Drug Administration (FDA) for treating psoriasis in patients 6 years and older, and lower doses are being evaluated for AD: 0.15% for adults and children ages 6 and older, and 0.05% for ages 2-5. Roflumilast is a phosphodiesterase-4 inhibitor. In 2023, the FDA accepted a supplemental drug application from the manufacturer, Arcutis, for roflumilast, 0.15%, for treating AD in patients ages 6 and older, based on the results from two recently published phase 3 trials, INTEGUMENT-1 and INTEGUMENT-2.
The study of younger children, INTEGUMENT-PED, recruited 652 patients aged 2-5 with mild to moderate AD, with a Validated Investigator Global Assessment scale for AD (vlGA-AD) score of 2 or 3, a mean body surface area of 22% overall (range, 3%-82%), and an Eczema Area and Severity Index (EASI) score of at least 5. Of the patients enrolled, 437 were assigned to 0.05% roflumilast cream, applied once a day for 4 weeks (mean age, 3.3 years; 51.6% male; 67.4% White; 15.6% Black; 8.5% Asian; 8.5% other or more than one race; 80.5% not Latino/Hispanic). The remaining 215 children were assigned to vehicle cream and had similar characteristics.
About 52% of the patients in both groups had an inadequate response, intolerance, or contraindications to topical corticosteroids (and about 17% for topical calcineurin inhibitors and about 9% for crisaborole).
The proportions of patients who reached “clear” (0) or “almost clear” (1) on the vlGA-AD scale were 35.4% and 14.6%, respectively, at week 4 (P < .0001) for roflumilast and vehicle, respectively, according to the lead author of the study, Lawrence M. Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, who presented the results at the meeting. In addition, 39.4% and 20.6% achieved an EASI-75 (a secondary endpoint), respectively (P < .0001), and itch also improved within 24 hours of starting treatment.
With regard to safety, 29.7% of patients taking roflumilast had treatment-emergent adverse effects (including upper respiratory tract infections in 4.1%) vs 21.9% of those in the vehicle arm (including upper respiratory tract infections in 1.4%). Reports of pain at the administration site were low (1.6% for roflumilast vs 1.9% for vehicle). Only one patient, a 2-year-old girl, had a treatment-emergent serious adverse event. The child, who was in the roflumilast group, had cellulitis involving noneczematous skin and was treated with antibiotics in the hospital for 3 days. The event was not attributed to roflumilast, which was stopped for 5 days, according to Dr. Eichenfield.
In an interview, Fairfield, Connecticut–based dermatologist Brittany Craiglow, MD, who was not involved in the study, said topical roflumilast would be an “important” new treatment because there are still few nonsteroidal options for the treatment of AD in children under 12. “The excellent local tolerability combined with early improvements in itch and skin clearance will make this a particularly attractive option, if approved,” she said.
Dr. Eichenfield disclosed multiple relationships with various drugmakers. He and several other study authors are investigators and/or consultants for Arcutis and received grants/research funding and/or honoraria. Two authors are Arcutis employees. Other disclosure information for the authors was not immediately available. Dr. Craiglow had no disclosures.
A version of this article appeared on Medscape.com .
FROM AAD 2024
New Research Dissects Transgenerational Obesity and Diabetes
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
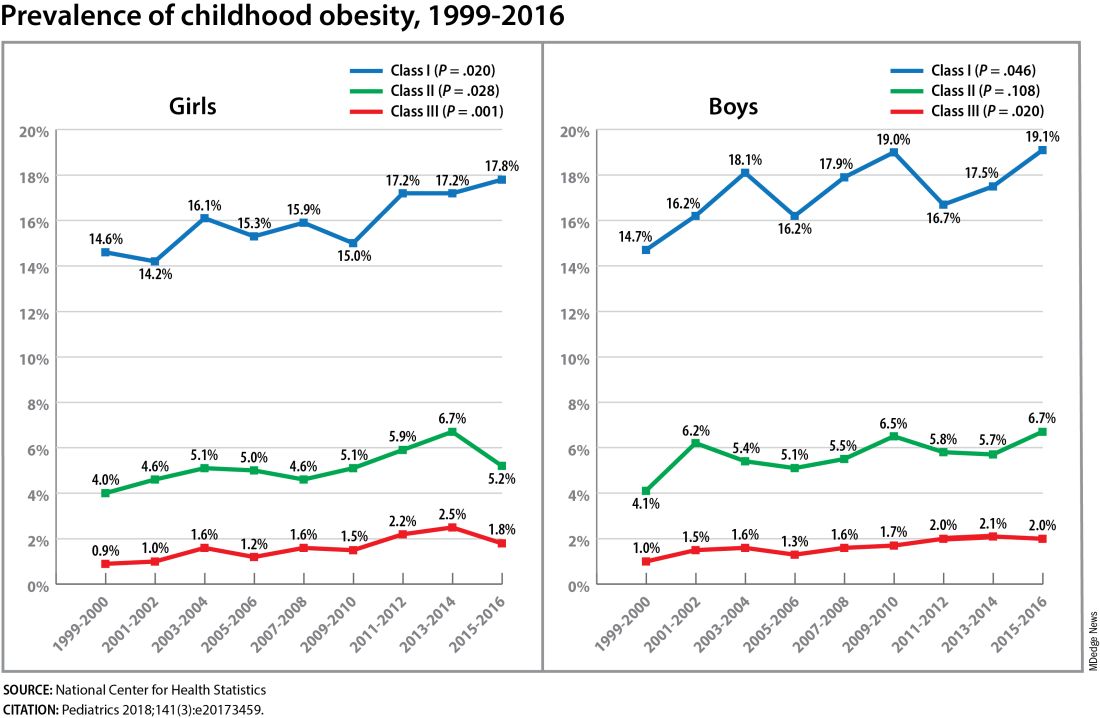
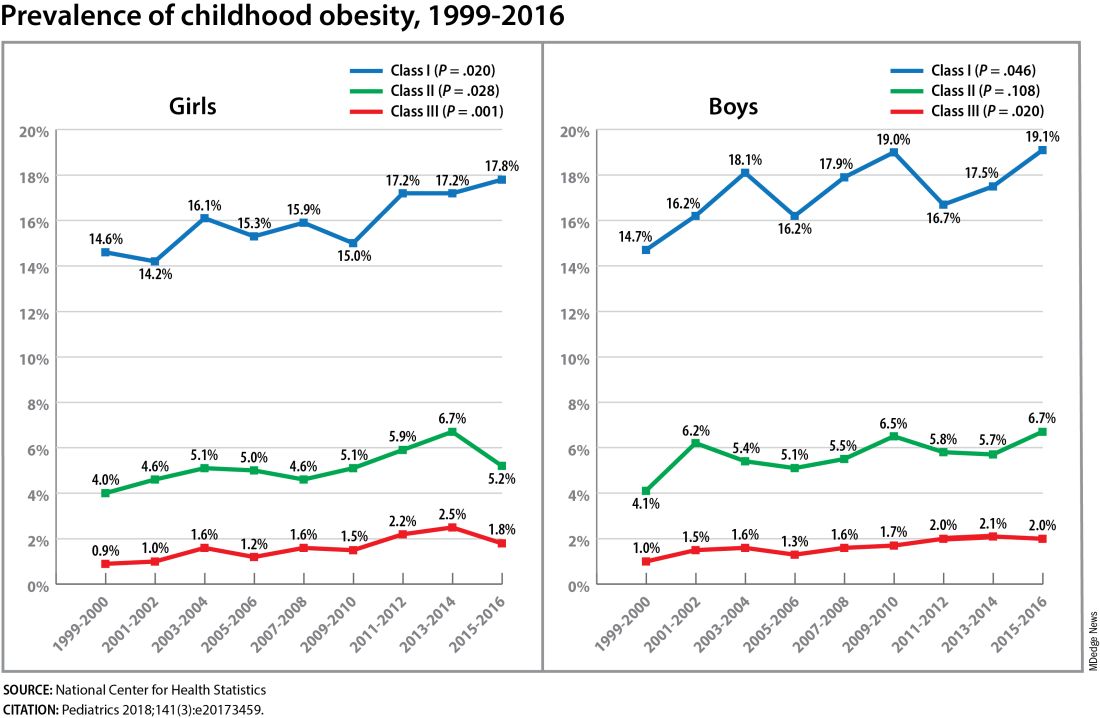
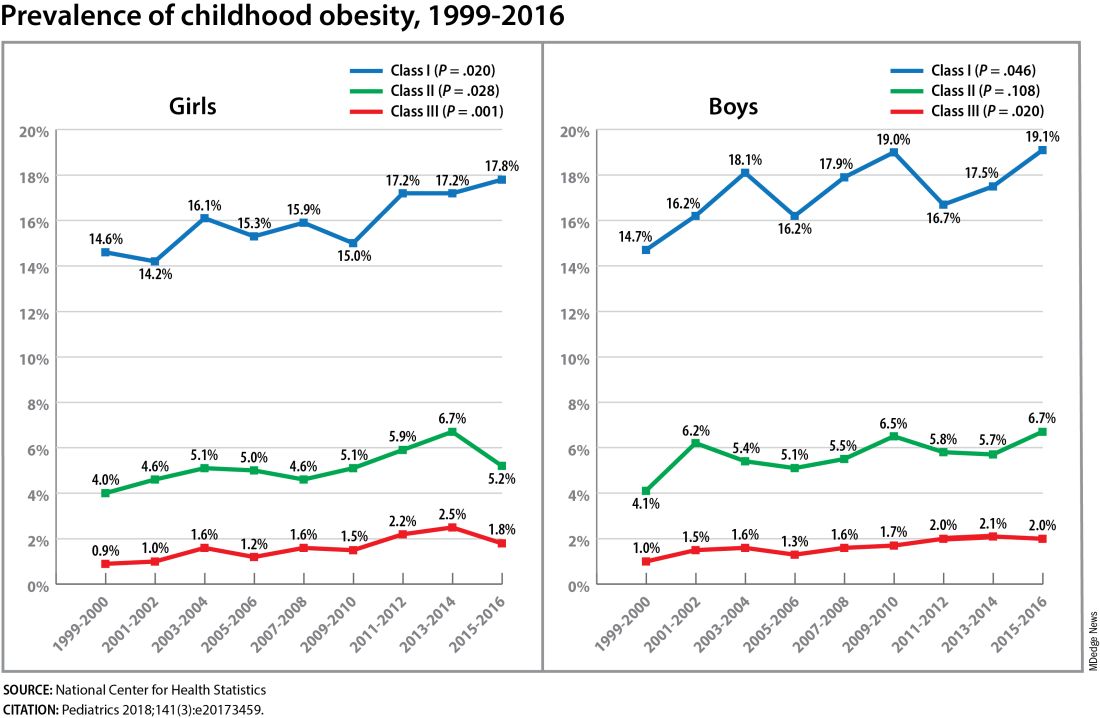
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1).
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1).
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1).
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FROM DPSG-NA 2023
Web-Based Aid Educates Women on Tubal Sterilization
Although tubal sterilization is common, especially among those with lower income and education levels, misunderstandings persist about the reversibility of the procedure, and previous studies suggest that many pregnant individuals are not making well-informed decisions, wrote Sonya Borrero, MD, of the University of Pittsburgh, and colleagues.
In a study published in JAMA Network Open, the researchers randomized 350 pregnant individuals with Medicaid insurance to usual care or usual care plus a web-based decision aid in English or Spanish called MyDecision/MiDecisión that included written, audio, and video information about tubal sterilization. The tool also included an interactive table comparing tubal sterilization to other contraceptive options, exercises to clarify patients’ values, knowledge checks, and a final summary report.
The two primary outcomes were knowledge of tubal sterilization based on a 10-question true/false test and decisional conflict about contraceptive choices using the low-literacy Decision Conflict Scale. The participants ranged in age from 21 to 45 years, with a mean age of 29.7 years. Participants were randomized prior to 24 weeks’ gestation, and those in the intervention group completed the intervention immediately using a personal device or a university device in the clinical setting. Further assessments occurred by phone during the third trimester and at 3 months postpartum.
Participants in the decision aid group showed significantly greater knowledge of tubal sterilization compared with controls, with a mean of 76.5% correct responses to the knowledge questions, vs. 55.6% in the control group (P < .001). Decisional conflict scores also were significantly lower in the intervention group compared with controls (mean 12.7 vs. 18.7, P = .002).
The most dramatic knowledge gap related to permanence of tubal sterilization; 90.1% of participants in the intervention group answered correctly that the procedure is not easily reversible, compared to 39.3% of the controls. Similarly, 86.6% of the intervention group responded correctly that the tubes do not “come untied” spontaneously, vs. 33.7% of controls (P < .001 for both).
The findings were limited by several factors including the focus only on pregnant Medicaid patients, the presentation of the decision tool only at a point early in pregnancy, which may have been too soon for some participants to consider tubal sterilization, and a lack of data on long-term satisfaction or regret about tubal sterilization decisions, the researchers noted.
However, the knowledge differences between the intervention and control groups remained significant at the third trimester assessment, they said.
More research is needed in other populations and using other time points, but the current study results suggest that use of the MyDecision/MiDecisión tool in a real-world clinical setting at the actual time of decision-making could improve knowledge and inform patients’ choices, the researchers concluded. Improved patient education also could inform policy decisions about the potential elimination of the 30-day waiting period for sterilization procedures, they said.
The study was supported by the National Institute on Minority Health and Health Disparities. The researchers had no financial conflicts to disclose.
Although tubal sterilization is common, especially among those with lower income and education levels, misunderstandings persist about the reversibility of the procedure, and previous studies suggest that many pregnant individuals are not making well-informed decisions, wrote Sonya Borrero, MD, of the University of Pittsburgh, and colleagues.
In a study published in JAMA Network Open, the researchers randomized 350 pregnant individuals with Medicaid insurance to usual care or usual care plus a web-based decision aid in English or Spanish called MyDecision/MiDecisión that included written, audio, and video information about tubal sterilization. The tool also included an interactive table comparing tubal sterilization to other contraceptive options, exercises to clarify patients’ values, knowledge checks, and a final summary report.
The two primary outcomes were knowledge of tubal sterilization based on a 10-question true/false test and decisional conflict about contraceptive choices using the low-literacy Decision Conflict Scale. The participants ranged in age from 21 to 45 years, with a mean age of 29.7 years. Participants were randomized prior to 24 weeks’ gestation, and those in the intervention group completed the intervention immediately using a personal device or a university device in the clinical setting. Further assessments occurred by phone during the third trimester and at 3 months postpartum.
Participants in the decision aid group showed significantly greater knowledge of tubal sterilization compared with controls, with a mean of 76.5% correct responses to the knowledge questions, vs. 55.6% in the control group (P < .001). Decisional conflict scores also were significantly lower in the intervention group compared with controls (mean 12.7 vs. 18.7, P = .002).
The most dramatic knowledge gap related to permanence of tubal sterilization; 90.1% of participants in the intervention group answered correctly that the procedure is not easily reversible, compared to 39.3% of the controls. Similarly, 86.6% of the intervention group responded correctly that the tubes do not “come untied” spontaneously, vs. 33.7% of controls (P < .001 for both).
The findings were limited by several factors including the focus only on pregnant Medicaid patients, the presentation of the decision tool only at a point early in pregnancy, which may have been too soon for some participants to consider tubal sterilization, and a lack of data on long-term satisfaction or regret about tubal sterilization decisions, the researchers noted.
However, the knowledge differences between the intervention and control groups remained significant at the third trimester assessment, they said.
More research is needed in other populations and using other time points, but the current study results suggest that use of the MyDecision/MiDecisión tool in a real-world clinical setting at the actual time of decision-making could improve knowledge and inform patients’ choices, the researchers concluded. Improved patient education also could inform policy decisions about the potential elimination of the 30-day waiting period for sterilization procedures, they said.
The study was supported by the National Institute on Minority Health and Health Disparities. The researchers had no financial conflicts to disclose.
Although tubal sterilization is common, especially among those with lower income and education levels, misunderstandings persist about the reversibility of the procedure, and previous studies suggest that many pregnant individuals are not making well-informed decisions, wrote Sonya Borrero, MD, of the University of Pittsburgh, and colleagues.
In a study published in JAMA Network Open, the researchers randomized 350 pregnant individuals with Medicaid insurance to usual care or usual care plus a web-based decision aid in English or Spanish called MyDecision/MiDecisión that included written, audio, and video information about tubal sterilization. The tool also included an interactive table comparing tubal sterilization to other contraceptive options, exercises to clarify patients’ values, knowledge checks, and a final summary report.
The two primary outcomes were knowledge of tubal sterilization based on a 10-question true/false test and decisional conflict about contraceptive choices using the low-literacy Decision Conflict Scale. The participants ranged in age from 21 to 45 years, with a mean age of 29.7 years. Participants were randomized prior to 24 weeks’ gestation, and those in the intervention group completed the intervention immediately using a personal device or a university device in the clinical setting. Further assessments occurred by phone during the third trimester and at 3 months postpartum.
Participants in the decision aid group showed significantly greater knowledge of tubal sterilization compared with controls, with a mean of 76.5% correct responses to the knowledge questions, vs. 55.6% in the control group (P < .001). Decisional conflict scores also were significantly lower in the intervention group compared with controls (mean 12.7 vs. 18.7, P = .002).
The most dramatic knowledge gap related to permanence of tubal sterilization; 90.1% of participants in the intervention group answered correctly that the procedure is not easily reversible, compared to 39.3% of the controls. Similarly, 86.6% of the intervention group responded correctly that the tubes do not “come untied” spontaneously, vs. 33.7% of controls (P < .001 for both).
The findings were limited by several factors including the focus only on pregnant Medicaid patients, the presentation of the decision tool only at a point early in pregnancy, which may have been too soon for some participants to consider tubal sterilization, and a lack of data on long-term satisfaction or regret about tubal sterilization decisions, the researchers noted.
However, the knowledge differences between the intervention and control groups remained significant at the third trimester assessment, they said.
More research is needed in other populations and using other time points, but the current study results suggest that use of the MyDecision/MiDecisión tool in a real-world clinical setting at the actual time of decision-making could improve knowledge and inform patients’ choices, the researchers concluded. Improved patient education also could inform policy decisions about the potential elimination of the 30-day waiting period for sterilization procedures, they said.
The study was supported by the National Institute on Minority Health and Health Disparities. The researchers had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
No Excess Cancer Risk Seen with Non-TNF Inhibitor Biologics in RA
TOPLINE:
Treatment of patients with rheumatoid arthritis (RA) with non–tumor necrosis factor inhibitor (TNFi) biologic disease-modifying antirheumatic drugs (bDMARDs) may not pose an increased risk for cancer, compared with TNFis and conventional synthetic DMARDs.
METHODOLOGY:
- Previous research has presented conflicting results on the association between non-TNFi bDMARDs and the risk for cancer, with abatacept drawing particular attention owing to its mode of action.
- By utilizing information from Danish registers (January 2006-December 2020), researchers compared the risk for cancer in 14,944 patients with RA (age > 18 years) who were initiated on non-TNFi bDMARDs (tocilizumab/sarilumab, abatacept, or rituximab), TNFis, or were in the conventional synthetic DMARDs (bDMARD-naive) group.
- The patient population contributed to 21,982 treatment initiations, which corresponded to 1457, 1016, 690, 7458, and 11,361 treatment initiations for the tocilizumab/sarilumab, abatacept, rituximab, TNFi, and bDMARD-naive groups, respectively.
- Patients were followed up until a diagnosis was obtained for cancer, death, emigration, the initiation of a different bDMARD or a targeted synthetic DMARD, or the end of the study, whichever was earlier.
- The primary outcome was defined as any primary cancer diagnosis (except nonmelanoma skin cancer).
TAKEAWAY:
- The risk for overall cancer was not significantly higher in the tocilizumab/sarilumab-, abatacept-, or rituximab-initiated groups than in the TNFi-treated and bDMARD-naive groups.
- The likelihood of cancer appeared to be higher in patients with more than 5 years of exposure to abatacept than in the TNFi-treated (hazard ratio [HR], 1.41; 95% CI, 0.60-2.60) and bDMARD-naive groups (HR, 1.14; 95% CI, 0.51-2.33). However, the results were not statistically significant.
- Treatment with rituximab may be associated with a lower risk for hematologic cancers than for TNFi-treated (HR, 0.09; 95% CI, 0.00-2.06) or bDMARD-naive groups (HR, 0.13; 95% CI, 0.00-1.89), although the findings did not show statistical significance.
IN PRACTICE:
The authors wrote, “bDMARD-associated cancer risk remains a clinically important research question, and more future studies specifically investigating non-TNFi bDMARDs in terms of cancer risk in patients with RA are warranted.”
SOURCE:
The investigation, led by Rasmus Westermann, MD, of Aalborg University Hospital, Aalborg, Denmark, was published online on March 7 in Rheumatology.
LIMITATIONS:
Many patients received more than one type of non-TNFi bDMARD treatment during the study. Because the temporal relationship of DMARD treatment with cancer was not certain, potential carcinogenic treatment effects could not be distinguished. Limited data were available on cancer risk factors.
DISCLOSURES:
The study was supported by the Danish Rheumatism Association and the Danish Cancer Society. Some authors reported financial relationships with pharmaceutical companies outside of the submitted work.
A version of this article appeared on Medscape.com.
TOPLINE:
Treatment of patients with rheumatoid arthritis (RA) with non–tumor necrosis factor inhibitor (TNFi) biologic disease-modifying antirheumatic drugs (bDMARDs) may not pose an increased risk for cancer, compared with TNFis and conventional synthetic DMARDs.
METHODOLOGY:
- Previous research has presented conflicting results on the association between non-TNFi bDMARDs and the risk for cancer, with abatacept drawing particular attention owing to its mode of action.
- By utilizing information from Danish registers (January 2006-December 2020), researchers compared the risk for cancer in 14,944 patients with RA (age > 18 years) who were initiated on non-TNFi bDMARDs (tocilizumab/sarilumab, abatacept, or rituximab), TNFis, or were in the conventional synthetic DMARDs (bDMARD-naive) group.
- The patient population contributed to 21,982 treatment initiations, which corresponded to 1457, 1016, 690, 7458, and 11,361 treatment initiations for the tocilizumab/sarilumab, abatacept, rituximab, TNFi, and bDMARD-naive groups, respectively.
- Patients were followed up until a diagnosis was obtained for cancer, death, emigration, the initiation of a different bDMARD or a targeted synthetic DMARD, or the end of the study, whichever was earlier.
- The primary outcome was defined as any primary cancer diagnosis (except nonmelanoma skin cancer).
TAKEAWAY:
- The risk for overall cancer was not significantly higher in the tocilizumab/sarilumab-, abatacept-, or rituximab-initiated groups than in the TNFi-treated and bDMARD-naive groups.
- The likelihood of cancer appeared to be higher in patients with more than 5 years of exposure to abatacept than in the TNFi-treated (hazard ratio [HR], 1.41; 95% CI, 0.60-2.60) and bDMARD-naive groups (HR, 1.14; 95% CI, 0.51-2.33). However, the results were not statistically significant.
- Treatment with rituximab may be associated with a lower risk for hematologic cancers than for TNFi-treated (HR, 0.09; 95% CI, 0.00-2.06) or bDMARD-naive groups (HR, 0.13; 95% CI, 0.00-1.89), although the findings did not show statistical significance.
IN PRACTICE:
The authors wrote, “bDMARD-associated cancer risk remains a clinically important research question, and more future studies specifically investigating non-TNFi bDMARDs in terms of cancer risk in patients with RA are warranted.”
SOURCE:
The investigation, led by Rasmus Westermann, MD, of Aalborg University Hospital, Aalborg, Denmark, was published online on March 7 in Rheumatology.
LIMITATIONS:
Many patients received more than one type of non-TNFi bDMARD treatment during the study. Because the temporal relationship of DMARD treatment with cancer was not certain, potential carcinogenic treatment effects could not be distinguished. Limited data were available on cancer risk factors.
DISCLOSURES:
The study was supported by the Danish Rheumatism Association and the Danish Cancer Society. Some authors reported financial relationships with pharmaceutical companies outside of the submitted work.
A version of this article appeared on Medscape.com.
TOPLINE:
Treatment of patients with rheumatoid arthritis (RA) with non–tumor necrosis factor inhibitor (TNFi) biologic disease-modifying antirheumatic drugs (bDMARDs) may not pose an increased risk for cancer, compared with TNFis and conventional synthetic DMARDs.
METHODOLOGY:
- Previous research has presented conflicting results on the association between non-TNFi bDMARDs and the risk for cancer, with abatacept drawing particular attention owing to its mode of action.
- By utilizing information from Danish registers (January 2006-December 2020), researchers compared the risk for cancer in 14,944 patients with RA (age > 18 years) who were initiated on non-TNFi bDMARDs (tocilizumab/sarilumab, abatacept, or rituximab), TNFis, or were in the conventional synthetic DMARDs (bDMARD-naive) group.
- The patient population contributed to 21,982 treatment initiations, which corresponded to 1457, 1016, 690, 7458, and 11,361 treatment initiations for the tocilizumab/sarilumab, abatacept, rituximab, TNFi, and bDMARD-naive groups, respectively.
- Patients were followed up until a diagnosis was obtained for cancer, death, emigration, the initiation of a different bDMARD or a targeted synthetic DMARD, or the end of the study, whichever was earlier.
- The primary outcome was defined as any primary cancer diagnosis (except nonmelanoma skin cancer).
TAKEAWAY:
- The risk for overall cancer was not significantly higher in the tocilizumab/sarilumab-, abatacept-, or rituximab-initiated groups than in the TNFi-treated and bDMARD-naive groups.
- The likelihood of cancer appeared to be higher in patients with more than 5 years of exposure to abatacept than in the TNFi-treated (hazard ratio [HR], 1.41; 95% CI, 0.60-2.60) and bDMARD-naive groups (HR, 1.14; 95% CI, 0.51-2.33). However, the results were not statistically significant.
- Treatment with rituximab may be associated with a lower risk for hematologic cancers than for TNFi-treated (HR, 0.09; 95% CI, 0.00-2.06) or bDMARD-naive groups (HR, 0.13; 95% CI, 0.00-1.89), although the findings did not show statistical significance.
IN PRACTICE:
The authors wrote, “bDMARD-associated cancer risk remains a clinically important research question, and more future studies specifically investigating non-TNFi bDMARDs in terms of cancer risk in patients with RA are warranted.”
SOURCE:
The investigation, led by Rasmus Westermann, MD, of Aalborg University Hospital, Aalborg, Denmark, was published online on March 7 in Rheumatology.
LIMITATIONS:
Many patients received more than one type of non-TNFi bDMARD treatment during the study. Because the temporal relationship of DMARD treatment with cancer was not certain, potential carcinogenic treatment effects could not be distinguished. Limited data were available on cancer risk factors.
DISCLOSURES:
The study was supported by the Danish Rheumatism Association and the Danish Cancer Society. Some authors reported financial relationships with pharmaceutical companies outside of the submitted work.
A version of this article appeared on Medscape.com.
Early Diagnosis Improves Clinical Outcomes in Psoriatic Arthritis
TOPLINE:
An earlier diagnosis of psoriatic arthritis (PsA) following symptom onset increases the likelihood of achieving improved clinical outcomes, highlighting the presence of a diagnostic window of opportunity in PsA.
METHODOLOGY:
- A diagnostic delay in PsA leads to increased joint erosions and functional impairment; however, whether a “window of opportunity” (< 12 weeks) exists in PsA requires further evaluation.
- Researchers assessed the impact of diagnostic delay on clinical outcomes in 708 newly diagnosed, disease-modifying antirheumatic drug-naive patients with PsA from the Dutch southwest Early PsA cohort.
- Total diagnostic delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist.
- On the basis of the total diagnostic delay, patients were categorized into those with a short delay of < 12 weeks (n = 136), intermediate delay of 12 weeks to 1 year (n = 237), and a long delay of > 1 year (n = 335).
- The groups were compared for clinical (Minimal Disease Activity [MDA] and Disease Activity index for Psoriatic Arthritis [DAPSA] remission) and patient-reported outcomes during 3 years of follow-up.
TAKEAWAY:
- The probability of achieving MDA was higher in patients with a short vs long diagnostic delay (odds ratio [OR], 2.55; 95% CI, 1.37-4.76).
- Compared with patients in the long diagnostic delay group, those in the short (OR, 2.35; 95% CI, 1.32-4.19) and intermediate (OR, 1.94; 95% CI, 1.19-3.15) diagnostic delay groups were more likely to achieve DAPSA remission.
- Compared with patients in the long diagnostic delay group, those in the short (estimated mean difference [Δ], −1.09; 95% CI, −1.88 to −0.30) or intermediate (Δ, −0.85; 95% CI, −1.50 to −0.19) groups had slightly less tender joints.
IN PRACTICE:
“A delay of > 1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population” in this study, wrote the authors, adding that for better long-term outcomes, “it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.”
SOURCE:
This study, led by Selinde V.J. Snoeck Henkemans, MD, of the department of rheumatology at Erasmus University Medical Center, Rotterdam, the Netherlands, was published online February 27, 2024, in RMD Open.
LIMITATIONS:
The study’s dropout rates (25%-31% across groups) may have influenced the findings. Patients with a long diagnostic delay might have dropped out owing to treatment dissatisfaction, and those with a short or intermediate delay might have dropped out due to inactive disease.
DISCLOSURES:
This study did not declare any specific source of funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
An earlier diagnosis of psoriatic arthritis (PsA) following symptom onset increases the likelihood of achieving improved clinical outcomes, highlighting the presence of a diagnostic window of opportunity in PsA.
METHODOLOGY:
- A diagnostic delay in PsA leads to increased joint erosions and functional impairment; however, whether a “window of opportunity” (< 12 weeks) exists in PsA requires further evaluation.
- Researchers assessed the impact of diagnostic delay on clinical outcomes in 708 newly diagnosed, disease-modifying antirheumatic drug-naive patients with PsA from the Dutch southwest Early PsA cohort.
- Total diagnostic delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist.
- On the basis of the total diagnostic delay, patients were categorized into those with a short delay of < 12 weeks (n = 136), intermediate delay of 12 weeks to 1 year (n = 237), and a long delay of > 1 year (n = 335).
- The groups were compared for clinical (Minimal Disease Activity [MDA] and Disease Activity index for Psoriatic Arthritis [DAPSA] remission) and patient-reported outcomes during 3 years of follow-up.
TAKEAWAY:
- The probability of achieving MDA was higher in patients with a short vs long diagnostic delay (odds ratio [OR], 2.55; 95% CI, 1.37-4.76).
- Compared with patients in the long diagnostic delay group, those in the short (OR, 2.35; 95% CI, 1.32-4.19) and intermediate (OR, 1.94; 95% CI, 1.19-3.15) diagnostic delay groups were more likely to achieve DAPSA remission.
- Compared with patients in the long diagnostic delay group, those in the short (estimated mean difference [Δ], −1.09; 95% CI, −1.88 to −0.30) or intermediate (Δ, −0.85; 95% CI, −1.50 to −0.19) groups had slightly less tender joints.
IN PRACTICE:
“A delay of > 1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population” in this study, wrote the authors, adding that for better long-term outcomes, “it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.”
SOURCE:
This study, led by Selinde V.J. Snoeck Henkemans, MD, of the department of rheumatology at Erasmus University Medical Center, Rotterdam, the Netherlands, was published online February 27, 2024, in RMD Open.
LIMITATIONS:
The study’s dropout rates (25%-31% across groups) may have influenced the findings. Patients with a long diagnostic delay might have dropped out owing to treatment dissatisfaction, and those with a short or intermediate delay might have dropped out due to inactive disease.
DISCLOSURES:
This study did not declare any specific source of funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
An earlier diagnosis of psoriatic arthritis (PsA) following symptom onset increases the likelihood of achieving improved clinical outcomes, highlighting the presence of a diagnostic window of opportunity in PsA.
METHODOLOGY:
- A diagnostic delay in PsA leads to increased joint erosions and functional impairment; however, whether a “window of opportunity” (< 12 weeks) exists in PsA requires further evaluation.
- Researchers assessed the impact of diagnostic delay on clinical outcomes in 708 newly diagnosed, disease-modifying antirheumatic drug-naive patients with PsA from the Dutch southwest Early PsA cohort.
- Total diagnostic delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist.
- On the basis of the total diagnostic delay, patients were categorized into those with a short delay of < 12 weeks (n = 136), intermediate delay of 12 weeks to 1 year (n = 237), and a long delay of > 1 year (n = 335).
- The groups were compared for clinical (Minimal Disease Activity [MDA] and Disease Activity index for Psoriatic Arthritis [DAPSA] remission) and patient-reported outcomes during 3 years of follow-up.
TAKEAWAY:
- The probability of achieving MDA was higher in patients with a short vs long diagnostic delay (odds ratio [OR], 2.55; 95% CI, 1.37-4.76).
- Compared with patients in the long diagnostic delay group, those in the short (OR, 2.35; 95% CI, 1.32-4.19) and intermediate (OR, 1.94; 95% CI, 1.19-3.15) diagnostic delay groups were more likely to achieve DAPSA remission.
- Compared with patients in the long diagnostic delay group, those in the short (estimated mean difference [Δ], −1.09; 95% CI, −1.88 to −0.30) or intermediate (Δ, −0.85; 95% CI, −1.50 to −0.19) groups had slightly less tender joints.
IN PRACTICE:
“A delay of > 1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population” in this study, wrote the authors, adding that for better long-term outcomes, “it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.”
SOURCE:
This study, led by Selinde V.J. Snoeck Henkemans, MD, of the department of rheumatology at Erasmus University Medical Center, Rotterdam, the Netherlands, was published online February 27, 2024, in RMD Open.
LIMITATIONS:
The study’s dropout rates (25%-31% across groups) may have influenced the findings. Patients with a long diagnostic delay might have dropped out owing to treatment dissatisfaction, and those with a short or intermediate delay might have dropped out due to inactive disease.
DISCLOSURES:
This study did not declare any specific source of funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Can a Stroke Be Caused by Cervical Manipulation?
Cervical manipulations have been associated with vascular complications. While the incidence of carotid dissections does not seem to have increased, the question remains open for vertebral artery injuries. We must remain vigilant!
Resorting to joint manipulation for neck pain is not unusual. Currently, cervical manipulation remains a popular first-line treatment for cervicodynia or headaches. Although evidence exists showing that specific joint mobilization can improve this type of symptomatology, there is a possibility that it may risk damaging the cervical arteries and causing ischemic stroke through arterial dissection.
Epidemiologically, internal carotid artery dissection is a relatively rare event with an estimated annual incidence of 1.72 per 100,000 individuals (those most likely to be diagnosed being obviously those leading to hospitalization for stroke) but represents one of the most common causes of stroke in young and middle-aged adults. Faced with case reports that may raise concerns and hypotheses about an associated risk, two studies have sought to delve into the issue.
No Increased Carotid Risk Identified
The first study, of a case-cross design, identified all incident cases of ischemic stroke in the territory of the internal carotid artery admitted to the hospital over a 9-year period using administrative healthcare data, the cases being used as their own control by sampling control periods before the date of the index stroke. Thus, 15,523 cases were compared with 62,092 control periods using exposure windows of 1, 3, 7, and 14 days before the stroke. The study also compared post-medical consultation and post-chiropractic consultation outcomes, knowing that as a first-line for complaints of neck pain or headache, patients often turn to one of these two types of primary care clinicians.
However, data analysis shows, among subjects aged under 45 years, positive associations for both different consultations in cases of subsequent carotid stroke (but no association for those aged over 45 years). These associations tended to increase when analyses were limited to visits for diagnoses of neck pain and headaches. Nevertheless, there was no significant difference between risk estimates after chiropractic or general medical consultation.
A notable limitation of this work is that it did not focus on strokes due to vertebral artery dissections that run through the transverse foramina of the cervical vertebrae.
A Screening Test Lacking Precision
More recently, the International Federation of Orthopedic Manual Physical Therapists has looked into the subject to refine the assessment of the risk for vascular complications in patients seeking physiotherapy/osteopathy care for neck pain and/or headaches. Through a cross-sectional study involving 150 patients, it tested a vascular complication risk index (from high to low grade, based on history taking and clinical examination), developed to estimate the risk for the presence of vascular rather than musculoskeletal pathology, to determine whether or not there is a contraindication to cervical manipulation.
However, the developed index had only low sensitivity (0.50; 95% CI, 0.39-0.61) and moderate specificity (0.63; 95% CI, 0.51-0.75), knowing that the reference test was a consensus medical decision made by a vascular neurologist, an interventional neurologist, and a neuroradiologist (based on clinical data and cervical MRI). Similarly, positive and negative likelihood ratios were low at 1.36 (95% CI, 0.93-1.99) and 0.79 (95% CI, 0.60-1.05), respectively.
In conclusion, the data from the case-cross study did not seem to demonstrate an excess risk for stroke in the territory of the internal carotid artery after cervical joint manipulations. Associations between cervical manipulation sessions or medical consultations and carotid strokes appear similar and could have been due to the fact that patients with early symptoms related to arterial dissection seek care before developing their stroke.
However, it is regrettable that the study did not focus on vertebral artery dissections, which are anatomically more exposed to cervical chiropractic sessions. Nevertheless, because indices defined from joint tests and medical history are insufficient to identify patients “at risk or in the process of arterial dissection,” and because stroke can result in severe disability, practitioners managing patients with neck pain cannot take this type of complication lightly.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Cervical manipulations have been associated with vascular complications. While the incidence of carotid dissections does not seem to have increased, the question remains open for vertebral artery injuries. We must remain vigilant!
Resorting to joint manipulation for neck pain is not unusual. Currently, cervical manipulation remains a popular first-line treatment for cervicodynia or headaches. Although evidence exists showing that specific joint mobilization can improve this type of symptomatology, there is a possibility that it may risk damaging the cervical arteries and causing ischemic stroke through arterial dissection.
Epidemiologically, internal carotid artery dissection is a relatively rare event with an estimated annual incidence of 1.72 per 100,000 individuals (those most likely to be diagnosed being obviously those leading to hospitalization for stroke) but represents one of the most common causes of stroke in young and middle-aged adults. Faced with case reports that may raise concerns and hypotheses about an associated risk, two studies have sought to delve into the issue.
No Increased Carotid Risk Identified
The first study, of a case-cross design, identified all incident cases of ischemic stroke in the territory of the internal carotid artery admitted to the hospital over a 9-year period using administrative healthcare data, the cases being used as their own control by sampling control periods before the date of the index stroke. Thus, 15,523 cases were compared with 62,092 control periods using exposure windows of 1, 3, 7, and 14 days before the stroke. The study also compared post-medical consultation and post-chiropractic consultation outcomes, knowing that as a first-line for complaints of neck pain or headache, patients often turn to one of these two types of primary care clinicians.
However, data analysis shows, among subjects aged under 45 years, positive associations for both different consultations in cases of subsequent carotid stroke (but no association for those aged over 45 years). These associations tended to increase when analyses were limited to visits for diagnoses of neck pain and headaches. Nevertheless, there was no significant difference between risk estimates after chiropractic or general medical consultation.
A notable limitation of this work is that it did not focus on strokes due to vertebral artery dissections that run through the transverse foramina of the cervical vertebrae.
A Screening Test Lacking Precision
More recently, the International Federation of Orthopedic Manual Physical Therapists has looked into the subject to refine the assessment of the risk for vascular complications in patients seeking physiotherapy/osteopathy care for neck pain and/or headaches. Through a cross-sectional study involving 150 patients, it tested a vascular complication risk index (from high to low grade, based on history taking and clinical examination), developed to estimate the risk for the presence of vascular rather than musculoskeletal pathology, to determine whether or not there is a contraindication to cervical manipulation.
However, the developed index had only low sensitivity (0.50; 95% CI, 0.39-0.61) and moderate specificity (0.63; 95% CI, 0.51-0.75), knowing that the reference test was a consensus medical decision made by a vascular neurologist, an interventional neurologist, and a neuroradiologist (based on clinical data and cervical MRI). Similarly, positive and negative likelihood ratios were low at 1.36 (95% CI, 0.93-1.99) and 0.79 (95% CI, 0.60-1.05), respectively.
In conclusion, the data from the case-cross study did not seem to demonstrate an excess risk for stroke in the territory of the internal carotid artery after cervical joint manipulations. Associations between cervical manipulation sessions or medical consultations and carotid strokes appear similar and could have been due to the fact that patients with early symptoms related to arterial dissection seek care before developing their stroke.
However, it is regrettable that the study did not focus on vertebral artery dissections, which are anatomically more exposed to cervical chiropractic sessions. Nevertheless, because indices defined from joint tests and medical history are insufficient to identify patients “at risk or in the process of arterial dissection,” and because stroke can result in severe disability, practitioners managing patients with neck pain cannot take this type of complication lightly.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Cervical manipulations have been associated with vascular complications. While the incidence of carotid dissections does not seem to have increased, the question remains open for vertebral artery injuries. We must remain vigilant!
Resorting to joint manipulation for neck pain is not unusual. Currently, cervical manipulation remains a popular first-line treatment for cervicodynia or headaches. Although evidence exists showing that specific joint mobilization can improve this type of symptomatology, there is a possibility that it may risk damaging the cervical arteries and causing ischemic stroke through arterial dissection.
Epidemiologically, internal carotid artery dissection is a relatively rare event with an estimated annual incidence of 1.72 per 100,000 individuals (those most likely to be diagnosed being obviously those leading to hospitalization for stroke) but represents one of the most common causes of stroke in young and middle-aged adults. Faced with case reports that may raise concerns and hypotheses about an associated risk, two studies have sought to delve into the issue.
No Increased Carotid Risk Identified
The first study, of a case-cross design, identified all incident cases of ischemic stroke in the territory of the internal carotid artery admitted to the hospital over a 9-year period using administrative healthcare data, the cases being used as their own control by sampling control periods before the date of the index stroke. Thus, 15,523 cases were compared with 62,092 control periods using exposure windows of 1, 3, 7, and 14 days before the stroke. The study also compared post-medical consultation and post-chiropractic consultation outcomes, knowing that as a first-line for complaints of neck pain or headache, patients often turn to one of these two types of primary care clinicians.
However, data analysis shows, among subjects aged under 45 years, positive associations for both different consultations in cases of subsequent carotid stroke (but no association for those aged over 45 years). These associations tended to increase when analyses were limited to visits for diagnoses of neck pain and headaches. Nevertheless, there was no significant difference between risk estimates after chiropractic or general medical consultation.
A notable limitation of this work is that it did not focus on strokes due to vertebral artery dissections that run through the transverse foramina of the cervical vertebrae.
A Screening Test Lacking Precision
More recently, the International Federation of Orthopedic Manual Physical Therapists has looked into the subject to refine the assessment of the risk for vascular complications in patients seeking physiotherapy/osteopathy care for neck pain and/or headaches. Through a cross-sectional study involving 150 patients, it tested a vascular complication risk index (from high to low grade, based on history taking and clinical examination), developed to estimate the risk for the presence of vascular rather than musculoskeletal pathology, to determine whether or not there is a contraindication to cervical manipulation.
However, the developed index had only low sensitivity (0.50; 95% CI, 0.39-0.61) and moderate specificity (0.63; 95% CI, 0.51-0.75), knowing that the reference test was a consensus medical decision made by a vascular neurologist, an interventional neurologist, and a neuroradiologist (based on clinical data and cervical MRI). Similarly, positive and negative likelihood ratios were low at 1.36 (95% CI, 0.93-1.99) and 0.79 (95% CI, 0.60-1.05), respectively.
In conclusion, the data from the case-cross study did not seem to demonstrate an excess risk for stroke in the territory of the internal carotid artery after cervical joint manipulations. Associations between cervical manipulation sessions or medical consultations and carotid strokes appear similar and could have been due to the fact that patients with early symptoms related to arterial dissection seek care before developing their stroke.
However, it is regrettable that the study did not focus on vertebral artery dissections, which are anatomically more exposed to cervical chiropractic sessions. Nevertheless, because indices defined from joint tests and medical history are insufficient to identify patients “at risk or in the process of arterial dissection,” and because stroke can result in severe disability, practitioners managing patients with neck pain cannot take this type of complication lightly.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
QOL Not Harmed With Add-On Pembrolizumab in Cervical Cancer
according to patient-reported outcome analyses from the KEYNOTE-A18 trial.
Progression-free survival data from the trial, reported at the 2023 meeting of the European Society for Medical Oncology, showed a 30% reduction in the risk for progression (P =.002) with the addition of pembrolizumab vs placebo, as well as favorable overall survival trends, reported Leslie Randall, MD, with VCU Health in Richmond, Virginia. Now the new analyses bring the “voices of the patients from this large phase 3 study.”
“I think the data can put us at ease and give patients a measure of comfort because there was no detriment in the quality of life,” said Dr. Randall, who presented the data on March 17 at the Society of Gynecologic Oncology (SGO) 2024 conference.
The phase 3 KEYNOTE-A18 trial enrolled 1060 patients new to treatment who had either stage 1B2-2B disease with lymph node involvement or stage 3-4A disease. They were randomly allocated to receive pembrolizumab or placebo plus concurrent chemoradiotherapy.
Patient-reported outcome instruments used in the study were the European Organization for Research and Treatment of Cancer (EORTC) 30-item quality-of-life (QOL) core questionnaire (QLQ-C30), the EORTC cervical cancer–specific module (QLQ-CX24), and the EuroQol EQ-5D-5L visual analog scale (VAS).
Prespecified secondary study endpoints were changes from baseline to week 36 in QLQ-C30 global health status/QOL (GHS/QOL) and physical functioning, and the QLQ-CX24 symptom-experience scale.
At baseline, patient-reported outcome scores were similar between treatment groups. Patients in both treatment groups had an initial decrease in QLQ-C30 GHS/QOL and physical functioning subscale and EQ-5D-5L VAS scores at weeks 3 and 6, but these improved relative to baseline at week 12 and subsequent weeks.
A similar number of patients in the pembrolizumab and placebo groups had improved or stable scores for QLQ-C30 GHS/QOL (76% vs 75%), QLQ-C30 physical functioning (77% vs 77%), QLQ-CX24 symptom experience (85% vs 85%) and EQ-5D-5L VAS (73% vs 76%).
Across all QOL instruments evaluated, there were no meaningful differences in patient-reported outcomes among patients who received pembrolizumab compared with those who received placebo, said Dr. Randall.
The improvement in progression-free survival, coupled with the patient-reported outcomes showing no additional harms to quality of life, support pembrolizumab plus concurrent chemoradiotherapy as a “new standard of care” for patients with high-risk locally advanced cervical cancer, she told attendees.
“We have had stunning success in cervical cancer treatments over the past 10-15 years, and now we see that the addition of pembrolizumab to standard chemotherapy not only improves outcome but very importantly does not significantly impact the quality of life in our patients,” said study discussant R. Wendel Naumann, MD, Atrium Health Levine Cancer Institute, Charlotte, North Carolina.
Funding for KEYNOTE-A18 was provided by Merck. Dr. Randall has disclosed relationships with Seagen/Genmab, Merck, GSK, ImmunoGen, AstraZeneca, and On Target Laboratories. Dr. Naumann has no relevant disclosures.
A version of this article appeared on Medscape.com.
according to patient-reported outcome analyses from the KEYNOTE-A18 trial.
Progression-free survival data from the trial, reported at the 2023 meeting of the European Society for Medical Oncology, showed a 30% reduction in the risk for progression (P =.002) with the addition of pembrolizumab vs placebo, as well as favorable overall survival trends, reported Leslie Randall, MD, with VCU Health in Richmond, Virginia. Now the new analyses bring the “voices of the patients from this large phase 3 study.”
“I think the data can put us at ease and give patients a measure of comfort because there was no detriment in the quality of life,” said Dr. Randall, who presented the data on March 17 at the Society of Gynecologic Oncology (SGO) 2024 conference.
The phase 3 KEYNOTE-A18 trial enrolled 1060 patients new to treatment who had either stage 1B2-2B disease with lymph node involvement or stage 3-4A disease. They were randomly allocated to receive pembrolizumab or placebo plus concurrent chemoradiotherapy.
Patient-reported outcome instruments used in the study were the European Organization for Research and Treatment of Cancer (EORTC) 30-item quality-of-life (QOL) core questionnaire (QLQ-C30), the EORTC cervical cancer–specific module (QLQ-CX24), and the EuroQol EQ-5D-5L visual analog scale (VAS).
Prespecified secondary study endpoints were changes from baseline to week 36 in QLQ-C30 global health status/QOL (GHS/QOL) and physical functioning, and the QLQ-CX24 symptom-experience scale.
At baseline, patient-reported outcome scores were similar between treatment groups. Patients in both treatment groups had an initial decrease in QLQ-C30 GHS/QOL and physical functioning subscale and EQ-5D-5L VAS scores at weeks 3 and 6, but these improved relative to baseline at week 12 and subsequent weeks.
A similar number of patients in the pembrolizumab and placebo groups had improved or stable scores for QLQ-C30 GHS/QOL (76% vs 75%), QLQ-C30 physical functioning (77% vs 77%), QLQ-CX24 symptom experience (85% vs 85%) and EQ-5D-5L VAS (73% vs 76%).
Across all QOL instruments evaluated, there were no meaningful differences in patient-reported outcomes among patients who received pembrolizumab compared with those who received placebo, said Dr. Randall.
The improvement in progression-free survival, coupled with the patient-reported outcomes showing no additional harms to quality of life, support pembrolizumab plus concurrent chemoradiotherapy as a “new standard of care” for patients with high-risk locally advanced cervical cancer, she told attendees.
“We have had stunning success in cervical cancer treatments over the past 10-15 years, and now we see that the addition of pembrolizumab to standard chemotherapy not only improves outcome but very importantly does not significantly impact the quality of life in our patients,” said study discussant R. Wendel Naumann, MD, Atrium Health Levine Cancer Institute, Charlotte, North Carolina.
Funding for KEYNOTE-A18 was provided by Merck. Dr. Randall has disclosed relationships with Seagen/Genmab, Merck, GSK, ImmunoGen, AstraZeneca, and On Target Laboratories. Dr. Naumann has no relevant disclosures.
A version of this article appeared on Medscape.com.
according to patient-reported outcome analyses from the KEYNOTE-A18 trial.
Progression-free survival data from the trial, reported at the 2023 meeting of the European Society for Medical Oncology, showed a 30% reduction in the risk for progression (P =.002) with the addition of pembrolizumab vs placebo, as well as favorable overall survival trends, reported Leslie Randall, MD, with VCU Health in Richmond, Virginia. Now the new analyses bring the “voices of the patients from this large phase 3 study.”
“I think the data can put us at ease and give patients a measure of comfort because there was no detriment in the quality of life,” said Dr. Randall, who presented the data on March 17 at the Society of Gynecologic Oncology (SGO) 2024 conference.
The phase 3 KEYNOTE-A18 trial enrolled 1060 patients new to treatment who had either stage 1B2-2B disease with lymph node involvement or stage 3-4A disease. They were randomly allocated to receive pembrolizumab or placebo plus concurrent chemoradiotherapy.
Patient-reported outcome instruments used in the study were the European Organization for Research and Treatment of Cancer (EORTC) 30-item quality-of-life (QOL) core questionnaire (QLQ-C30), the EORTC cervical cancer–specific module (QLQ-CX24), and the EuroQol EQ-5D-5L visual analog scale (VAS).
Prespecified secondary study endpoints were changes from baseline to week 36 in QLQ-C30 global health status/QOL (GHS/QOL) and physical functioning, and the QLQ-CX24 symptom-experience scale.
At baseline, patient-reported outcome scores were similar between treatment groups. Patients in both treatment groups had an initial decrease in QLQ-C30 GHS/QOL and physical functioning subscale and EQ-5D-5L VAS scores at weeks 3 and 6, but these improved relative to baseline at week 12 and subsequent weeks.
A similar number of patients in the pembrolizumab and placebo groups had improved or stable scores for QLQ-C30 GHS/QOL (76% vs 75%), QLQ-C30 physical functioning (77% vs 77%), QLQ-CX24 symptom experience (85% vs 85%) and EQ-5D-5L VAS (73% vs 76%).
Across all QOL instruments evaluated, there were no meaningful differences in patient-reported outcomes among patients who received pembrolizumab compared with those who received placebo, said Dr. Randall.
The improvement in progression-free survival, coupled with the patient-reported outcomes showing no additional harms to quality of life, support pembrolizumab plus concurrent chemoradiotherapy as a “new standard of care” for patients with high-risk locally advanced cervical cancer, she told attendees.
“We have had stunning success in cervical cancer treatments over the past 10-15 years, and now we see that the addition of pembrolizumab to standard chemotherapy not only improves outcome but very importantly does not significantly impact the quality of life in our patients,” said study discussant R. Wendel Naumann, MD, Atrium Health Levine Cancer Institute, Charlotte, North Carolina.
Funding for KEYNOTE-A18 was provided by Merck. Dr. Randall has disclosed relationships with Seagen/Genmab, Merck, GSK, ImmunoGen, AstraZeneca, and On Target Laboratories. Dr. Naumann has no relevant disclosures.
A version of this article appeared on Medscape.com.
Primary Biliary Cholangitis: Managing a Progressive Liver Disease
Primary biliary cholangitis is a rare progressive autoimmune liver disease that specifically targets biliary epithelial cells. In this article, Dr. Kowdley describes prognostic markers of disease, current and investigational medical therapies, liver transplant, and focusing on maximizing favorable long-term outcomes.
Primary biliary cholangitis is a rare progressive autoimmune liver disease that specifically targets biliary epithelial cells. In this article, Dr. Kowdley describes prognostic markers of disease, current and investigational medical therapies, liver transplant, and focusing on maximizing favorable long-term outcomes.
Primary biliary cholangitis is a rare progressive autoimmune liver disease that specifically targets biliary epithelial cells. In this article, Dr. Kowdley describes prognostic markers of disease, current and investigational medical therapies, liver transplant, and focusing on maximizing favorable long-term outcomes.
Rheumatology Workforce May Have Grown, But It’s Still Not Enough
The number of clinically active rheumatology providers in the United States grew more than 20% from 2009 to 2019, according to a new analysis.
The number of advanced practice providers (APPs) in rheumatology more than doubled during that same time. However, these numerical increases are not enough to meet the projected demand in care, the authors reported.
“Even though we found growth, and if that same growth continued, we’d still be well below the projected needs for the overall aging population of the United States,” lead author Melissa Mannion, MD, MSPH, a pediatric rheumatologist at the University of Alabama at Birmingham, said in an interview.
In a 2015 workforce study by the American College of Rheumatology (ACR), researchers projected that the supply of rheumatologists would decrease by 25% from 2015 to 2030, with an estimated shortage of over 4000 clinical full-time equivalent (cFTE) rheumatology providers.
While the previous study’s findings seem to contrast with this newest analysis, Dr. Dr. Mannion said the findings are complementary, with both studies using different data sources.
The newest findings were published online on February 24 in Arthritis & Rheumatology.
Leveraging Medicare Data
The ACR study estimated the adult rheumatology workforce and cFTEs using both primary and secondary sources, including published data from the American Medical Association and other professional societies, as well as electronic surveys of ACR members and rheumatology fellows in training.
By contrast, this newest study identified rheumatology providers using Medicare administrative data from 2006 to 2020, supplemented by national provider identifier taxonomy codes. Rheumatologists were considered “clinically active” if they provided care for at least five patients in 1 year. To account for rheumatology fellows, who can be categorized as internal medicine physicians, researchers also included internists who prescribed biologic or targeted synthetic disease-modifying antirheumatic drugs (DMARDs) to more than 10 patients a year.
The count also included APPs, both nurse practitioners (NPs) and physician assistants (PAs), who were attached to practices with only rheumatologists, internists, or one other specialty. Like physicians, APPs were included in the count if they prescribed more than 10 patients biologic or targeted synthetic DMARDs in a calendar year and billed at least five patients with a rheumatic condition per year.
Researchers also estimated the number of cFTEs for 2019, using a variety of assumptions to generate an upper and lower range.
Different Numbers, Complementary Conclusions
For the 2019 calendar year, researchers counted 5667 clinically active rheumatologists and 379 NPs/PAs.
This represented a 23% increase in rheumatologists and a 141% increase in the number of APPs in the rheumatology workforce from 2009. The active rheumatology workforce increased by about 100 providers per year over the study period, although growth flattened off in more recent years.
The estimated cFTEs for 2019 ranged from 3457 to 5396, which are “comparable” to the projected 2020 cFTE estimates made in the ACR 2015 workforce study: 3888 to 5777 cFTEs.
Daniel Battafarano, DO, chair of the ACR Workforce Solutions Committee, agreed with Dr. Mannion that these findings complement each other, telling a similar story “but with different numbers,” he told this news organization. Dr. Battafarano, a professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Maryland, led the ACR workforce study.
“Both studies project estimates of rheumatology providers and workforce trends, but neither study can claim accurate numbers of rheumatology providers due to the true limitation of either workforce study model,” he said.
The ACR study began with a higher count of rheumatologists, estimating 6013 practicing providers in 2015, while Dr. Mannion’s team calculated 5474 providers for the same year. The ACR study projected that provider numbers would fall to 5886 by 2020, which was higher than the 2019 count in this most recent study.
Dr. Battafarano noted that the studies also dealt with different time frames: While the ACR study used 2015 data to project trends in 5-year increments, this most recent study looked trends in the previous decade.
“We found an increase over time, although toward the end of our study — from 2019 to 2020 — we did have a drop off in number of providers, so maybe we are finding the beginning of what [the ACR researchers] anticipated, or maybe that will be corrected in the future,” Dr. Dr. Mannion said. “I think that our estimates really coordinate with what they found just using a different data source.”
Geographic Disparities and Solutions
The new study also highlighted the scarcity of rheumatology providers in rural counties, which was also an important take away from the 2015 ACR study. In the new analysis, researchers found that 95% of rheumatology practices were in urban settings, which did not change over the study period. Most counties in the United States had fewer than 30 rheumatologists per 1 million adults, with 93% of rural counties having zero adult rheumatologists. In comparison, 48% of urban counties had no adult rheumatologists.
“There’s not enough people, and they’re in very specific locations,” Dr. Dr. Mannion said. “Both things make it harder for people to get care.”
Dr. Battafarano noted that leveraging APPs would be key to increasing patient access to care moving forward — a resource that has more than doubled in the past decade, according to Dr. Dr. Mannion’s analysis.
“Recruiting a significant number of APPs into rheumatology practice should be a primary goal to increase the rheumatology workforce,” he said. Other potential solutions, he added, include employing telemedicine and educating primary care providers on rheumatic disease to help them comanage these conditions with rheumatologists.
This study was partially funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Mannion was supported by the Rheumatology Research Foundation Norman B. Gaylis, MD Clinical Research Award, paid to her institution. Dr. Battafarano had no relevant disclosures.
A version of this article appeared on Medscape.com.
The number of clinically active rheumatology providers in the United States grew more than 20% from 2009 to 2019, according to a new analysis.
The number of advanced practice providers (APPs) in rheumatology more than doubled during that same time. However, these numerical increases are not enough to meet the projected demand in care, the authors reported.
“Even though we found growth, and if that same growth continued, we’d still be well below the projected needs for the overall aging population of the United States,” lead author Melissa Mannion, MD, MSPH, a pediatric rheumatologist at the University of Alabama at Birmingham, said in an interview.
In a 2015 workforce study by the American College of Rheumatology (ACR), researchers projected that the supply of rheumatologists would decrease by 25% from 2015 to 2030, with an estimated shortage of over 4000 clinical full-time equivalent (cFTE) rheumatology providers.
While the previous study’s findings seem to contrast with this newest analysis, Dr. Dr. Mannion said the findings are complementary, with both studies using different data sources.
The newest findings were published online on February 24 in Arthritis & Rheumatology.
Leveraging Medicare Data
The ACR study estimated the adult rheumatology workforce and cFTEs using both primary and secondary sources, including published data from the American Medical Association and other professional societies, as well as electronic surveys of ACR members and rheumatology fellows in training.
By contrast, this newest study identified rheumatology providers using Medicare administrative data from 2006 to 2020, supplemented by national provider identifier taxonomy codes. Rheumatologists were considered “clinically active” if they provided care for at least five patients in 1 year. To account for rheumatology fellows, who can be categorized as internal medicine physicians, researchers also included internists who prescribed biologic or targeted synthetic disease-modifying antirheumatic drugs (DMARDs) to more than 10 patients a year.
The count also included APPs, both nurse practitioners (NPs) and physician assistants (PAs), who were attached to practices with only rheumatologists, internists, or one other specialty. Like physicians, APPs were included in the count if they prescribed more than 10 patients biologic or targeted synthetic DMARDs in a calendar year and billed at least five patients with a rheumatic condition per year.
Researchers also estimated the number of cFTEs for 2019, using a variety of assumptions to generate an upper and lower range.
Different Numbers, Complementary Conclusions
For the 2019 calendar year, researchers counted 5667 clinically active rheumatologists and 379 NPs/PAs.
This represented a 23% increase in rheumatologists and a 141% increase in the number of APPs in the rheumatology workforce from 2009. The active rheumatology workforce increased by about 100 providers per year over the study period, although growth flattened off in more recent years.
The estimated cFTEs for 2019 ranged from 3457 to 5396, which are “comparable” to the projected 2020 cFTE estimates made in the ACR 2015 workforce study: 3888 to 5777 cFTEs.
Daniel Battafarano, DO, chair of the ACR Workforce Solutions Committee, agreed with Dr. Mannion that these findings complement each other, telling a similar story “but with different numbers,” he told this news organization. Dr. Battafarano, a professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Maryland, led the ACR workforce study.
“Both studies project estimates of rheumatology providers and workforce trends, but neither study can claim accurate numbers of rheumatology providers due to the true limitation of either workforce study model,” he said.
The ACR study began with a higher count of rheumatologists, estimating 6013 practicing providers in 2015, while Dr. Mannion’s team calculated 5474 providers for the same year. The ACR study projected that provider numbers would fall to 5886 by 2020, which was higher than the 2019 count in this most recent study.
Dr. Battafarano noted that the studies also dealt with different time frames: While the ACR study used 2015 data to project trends in 5-year increments, this most recent study looked trends in the previous decade.
“We found an increase over time, although toward the end of our study — from 2019 to 2020 — we did have a drop off in number of providers, so maybe we are finding the beginning of what [the ACR researchers] anticipated, or maybe that will be corrected in the future,” Dr. Dr. Mannion said. “I think that our estimates really coordinate with what they found just using a different data source.”
Geographic Disparities and Solutions
The new study also highlighted the scarcity of rheumatology providers in rural counties, which was also an important take away from the 2015 ACR study. In the new analysis, researchers found that 95% of rheumatology practices were in urban settings, which did not change over the study period. Most counties in the United States had fewer than 30 rheumatologists per 1 million adults, with 93% of rural counties having zero adult rheumatologists. In comparison, 48% of urban counties had no adult rheumatologists.
“There’s not enough people, and they’re in very specific locations,” Dr. Dr. Mannion said. “Both things make it harder for people to get care.”
Dr. Battafarano noted that leveraging APPs would be key to increasing patient access to care moving forward — a resource that has more than doubled in the past decade, according to Dr. Dr. Mannion’s analysis.
“Recruiting a significant number of APPs into rheumatology practice should be a primary goal to increase the rheumatology workforce,” he said. Other potential solutions, he added, include employing telemedicine and educating primary care providers on rheumatic disease to help them comanage these conditions with rheumatologists.
This study was partially funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Mannion was supported by the Rheumatology Research Foundation Norman B. Gaylis, MD Clinical Research Award, paid to her institution. Dr. Battafarano had no relevant disclosures.
A version of this article appeared on Medscape.com.
The number of clinically active rheumatology providers in the United States grew more than 20% from 2009 to 2019, according to a new analysis.
The number of advanced practice providers (APPs) in rheumatology more than doubled during that same time. However, these numerical increases are not enough to meet the projected demand in care, the authors reported.
“Even though we found growth, and if that same growth continued, we’d still be well below the projected needs for the overall aging population of the United States,” lead author Melissa Mannion, MD, MSPH, a pediatric rheumatologist at the University of Alabama at Birmingham, said in an interview.
In a 2015 workforce study by the American College of Rheumatology (ACR), researchers projected that the supply of rheumatologists would decrease by 25% from 2015 to 2030, with an estimated shortage of over 4000 clinical full-time equivalent (cFTE) rheumatology providers.
While the previous study’s findings seem to contrast with this newest analysis, Dr. Dr. Mannion said the findings are complementary, with both studies using different data sources.
The newest findings were published online on February 24 in Arthritis & Rheumatology.
Leveraging Medicare Data
The ACR study estimated the adult rheumatology workforce and cFTEs using both primary and secondary sources, including published data from the American Medical Association and other professional societies, as well as electronic surveys of ACR members and rheumatology fellows in training.
By contrast, this newest study identified rheumatology providers using Medicare administrative data from 2006 to 2020, supplemented by national provider identifier taxonomy codes. Rheumatologists were considered “clinically active” if they provided care for at least five patients in 1 year. To account for rheumatology fellows, who can be categorized as internal medicine physicians, researchers also included internists who prescribed biologic or targeted synthetic disease-modifying antirheumatic drugs (DMARDs) to more than 10 patients a year.
The count also included APPs, both nurse practitioners (NPs) and physician assistants (PAs), who were attached to practices with only rheumatologists, internists, or one other specialty. Like physicians, APPs were included in the count if they prescribed more than 10 patients biologic or targeted synthetic DMARDs in a calendar year and billed at least five patients with a rheumatic condition per year.
Researchers also estimated the number of cFTEs for 2019, using a variety of assumptions to generate an upper and lower range.
Different Numbers, Complementary Conclusions
For the 2019 calendar year, researchers counted 5667 clinically active rheumatologists and 379 NPs/PAs.
This represented a 23% increase in rheumatologists and a 141% increase in the number of APPs in the rheumatology workforce from 2009. The active rheumatology workforce increased by about 100 providers per year over the study period, although growth flattened off in more recent years.
The estimated cFTEs for 2019 ranged from 3457 to 5396, which are “comparable” to the projected 2020 cFTE estimates made in the ACR 2015 workforce study: 3888 to 5777 cFTEs.
Daniel Battafarano, DO, chair of the ACR Workforce Solutions Committee, agreed with Dr. Mannion that these findings complement each other, telling a similar story “but with different numbers,” he told this news organization. Dr. Battafarano, a professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Maryland, led the ACR workforce study.
“Both studies project estimates of rheumatology providers and workforce trends, but neither study can claim accurate numbers of rheumatology providers due to the true limitation of either workforce study model,” he said.
The ACR study began with a higher count of rheumatologists, estimating 6013 practicing providers in 2015, while Dr. Mannion’s team calculated 5474 providers for the same year. The ACR study projected that provider numbers would fall to 5886 by 2020, which was higher than the 2019 count in this most recent study.
Dr. Battafarano noted that the studies also dealt with different time frames: While the ACR study used 2015 data to project trends in 5-year increments, this most recent study looked trends in the previous decade.
“We found an increase over time, although toward the end of our study — from 2019 to 2020 — we did have a drop off in number of providers, so maybe we are finding the beginning of what [the ACR researchers] anticipated, or maybe that will be corrected in the future,” Dr. Dr. Mannion said. “I think that our estimates really coordinate with what they found just using a different data source.”
Geographic Disparities and Solutions
The new study also highlighted the scarcity of rheumatology providers in rural counties, which was also an important take away from the 2015 ACR study. In the new analysis, researchers found that 95% of rheumatology practices were in urban settings, which did not change over the study period. Most counties in the United States had fewer than 30 rheumatologists per 1 million adults, with 93% of rural counties having zero adult rheumatologists. In comparison, 48% of urban counties had no adult rheumatologists.
“There’s not enough people, and they’re in very specific locations,” Dr. Dr. Mannion said. “Both things make it harder for people to get care.”
Dr. Battafarano noted that leveraging APPs would be key to increasing patient access to care moving forward — a resource that has more than doubled in the past decade, according to Dr. Dr. Mannion’s analysis.
“Recruiting a significant number of APPs into rheumatology practice should be a primary goal to increase the rheumatology workforce,” he said. Other potential solutions, he added, include employing telemedicine and educating primary care providers on rheumatic disease to help them comanage these conditions with rheumatologists.
This study was partially funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Mannion was supported by the Rheumatology Research Foundation Norman B. Gaylis, MD Clinical Research Award, paid to her institution. Dr. Battafarano had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM ARTHRITIS & RHEUMATOLOGY






