User login
Many Physicians Unaware of Costs for Lab Tests, Procedures
Sometimes, simply knowing what a test costs can make all the difference.
Many physicians have sheepishly admitted that they know little about the price tags attached to the procedures and tests they order on a routine basis—or how that might impact their patients financially. In Medscape’s Physician Compensation Report for 2012, only 38% of surveyed doctors said they regularly discussed the cost of treatment with their patients. The following year, the rate had dropped to 30%.
One medical resident, Neel Shah, MD, MPP discovered how important those discussions can be.
After a woman admitted to the ED tested positive on a pregnancy test, a follow-up hormone test warned of potential trouble with her pregnancy, and Dr. Shah asked her to return to the hospital for an ultrasound.
“She refused to come in until I could tell her how much the ultrasound would cost,” he recalls. Other providers had told him that bringing up costs with patients would decrease their trust, because they didn’t want doctors to focus on anything but providing care. “With her, it was very clear that my inability to tell her what things cost actually eroded her trust in me and, in her mind, she was being reasonable,” he says.

–Neel Shah, MD, MPP
Dr. Shah had already grown disillusioned in medical school, watching providers around him make clinical decisions without regard to the cost for patients, and he took a hiatus to study politics at Harvard’s Kennedy School of Government. When he and a collaborator subsequently launched the nonprofit organization Costs of Care to point out the downsides of that lack of transparency, however, they received a less-than-enthusiastic reception from some quarters.
“If you’re trying to tell doctors or clinicians in general that we ought to be doing things differently, as a young person, it’s not a great way to make friends,” says
Dr. Shah, who is now an assistant professor at Harvard Medical School in Boston.
The group gained traction as its cost-awareness manifesto began to resonate with the public, however, and the essays on its site have been picked up by multiple media groups. Dr. Shah’s own experience with his pregnant patient, however, made one of the strongest impressions on him.
Getting an answer to her about the cost of an ultrasound took nearly 24 hours, he recalls, “because nobody around me knew.” In the interim, he fretted that his patient might have an ectopic pregnancy and bleed to death. She didn’t, but the outcome could have been very different, he says.
“That really struck home for me, for sure,” he adds. “I think about that all the time.”
Sometimes, simply knowing what a test costs can make all the difference.
Many physicians have sheepishly admitted that they know little about the price tags attached to the procedures and tests they order on a routine basis—or how that might impact their patients financially. In Medscape’s Physician Compensation Report for 2012, only 38% of surveyed doctors said they regularly discussed the cost of treatment with their patients. The following year, the rate had dropped to 30%.
One medical resident, Neel Shah, MD, MPP discovered how important those discussions can be.
After a woman admitted to the ED tested positive on a pregnancy test, a follow-up hormone test warned of potential trouble with her pregnancy, and Dr. Shah asked her to return to the hospital for an ultrasound.
“She refused to come in until I could tell her how much the ultrasound would cost,” he recalls. Other providers had told him that bringing up costs with patients would decrease their trust, because they didn’t want doctors to focus on anything but providing care. “With her, it was very clear that my inability to tell her what things cost actually eroded her trust in me and, in her mind, she was being reasonable,” he says.

–Neel Shah, MD, MPP
Dr. Shah had already grown disillusioned in medical school, watching providers around him make clinical decisions without regard to the cost for patients, and he took a hiatus to study politics at Harvard’s Kennedy School of Government. When he and a collaborator subsequently launched the nonprofit organization Costs of Care to point out the downsides of that lack of transparency, however, they received a less-than-enthusiastic reception from some quarters.
“If you’re trying to tell doctors or clinicians in general that we ought to be doing things differently, as a young person, it’s not a great way to make friends,” says
Dr. Shah, who is now an assistant professor at Harvard Medical School in Boston.
The group gained traction as its cost-awareness manifesto began to resonate with the public, however, and the essays on its site have been picked up by multiple media groups. Dr. Shah’s own experience with his pregnant patient, however, made one of the strongest impressions on him.
Getting an answer to her about the cost of an ultrasound took nearly 24 hours, he recalls, “because nobody around me knew.” In the interim, he fretted that his patient might have an ectopic pregnancy and bleed to death. She didn’t, but the outcome could have been very different, he says.
“That really struck home for me, for sure,” he adds. “I think about that all the time.”
Sometimes, simply knowing what a test costs can make all the difference.
Many physicians have sheepishly admitted that they know little about the price tags attached to the procedures and tests they order on a routine basis—or how that might impact their patients financially. In Medscape’s Physician Compensation Report for 2012, only 38% of surveyed doctors said they regularly discussed the cost of treatment with their patients. The following year, the rate had dropped to 30%.
One medical resident, Neel Shah, MD, MPP discovered how important those discussions can be.
After a woman admitted to the ED tested positive on a pregnancy test, a follow-up hormone test warned of potential trouble with her pregnancy, and Dr. Shah asked her to return to the hospital for an ultrasound.
“She refused to come in until I could tell her how much the ultrasound would cost,” he recalls. Other providers had told him that bringing up costs with patients would decrease their trust, because they didn’t want doctors to focus on anything but providing care. “With her, it was very clear that my inability to tell her what things cost actually eroded her trust in me and, in her mind, she was being reasonable,” he says.

–Neel Shah, MD, MPP
Dr. Shah had already grown disillusioned in medical school, watching providers around him make clinical decisions without regard to the cost for patients, and he took a hiatus to study politics at Harvard’s Kennedy School of Government. When he and a collaborator subsequently launched the nonprofit organization Costs of Care to point out the downsides of that lack of transparency, however, they received a less-than-enthusiastic reception from some quarters.
“If you’re trying to tell doctors or clinicians in general that we ought to be doing things differently, as a young person, it’s not a great way to make friends,” says
Dr. Shah, who is now an assistant professor at Harvard Medical School in Boston.
The group gained traction as its cost-awareness manifesto began to resonate with the public, however, and the essays on its site have been picked up by multiple media groups. Dr. Shah’s own experience with his pregnant patient, however, made one of the strongest impressions on him.
Getting an answer to her about the cost of an ultrasound took nearly 24 hours, he recalls, “because nobody around me knew.” In the interim, he fretted that his patient might have an ectopic pregnancy and bleed to death. She didn’t, but the outcome could have been very different, he says.
“That really struck home for me, for sure,” he adds. “I think about that all the time.”
Insufficient Time for Patients May Add to Healthcare Waste
Reform advocates agree that a doctor’s time is a scarce resource that can contribute to waste when it is stretched too thin.
“It’s not just about overtreatment; it’s about getting the right treatment, and the right treatment depends on the right diagnosis, and the right diagnosis depends on really taking the time to think carefully with the patient about what’s going on,” says Vineet Arora, MD, MAPP, FHM, a hospitalist and researcher at the University of Chicago. A doctor “pulled in 10 different ways in the hospital” simply may not have the bandwidth to devote sufficient time to a complex patient; ordering a test can then seem like an enticing way to save some time.
Although electronic health records may have simplified the process for ordering CT scans and other tests, Dr. Arora says, they sometimes supersede important conversations that should take place with radiologists or other specialists about whether those tests are truly necessary. Meanwhile, providers face a proliferation of reporting duties. Recent surveys, in fact, suggest that doctors are “drowning” in paperwork and computer-based reporting requirements. Placing additional demands on a doctor’s time, Dr. Arora says, can limit his or her availability for other duties.
With hospitalists caring for increasingly complex patients with more complicated therapeutics, UCSF’s Christopher Moriates, MD, agrees that insufficient time can be an important barrier to change. It is not, however, insurmountable. If the ethos of medicine is “First, do no harm,” he says, it’s critical for doctors to remember that waste is harm.
“If we’re really going to stand by that,” he says, “then it rises to be something that we really need to take on.”
Reform advocates agree that a doctor’s time is a scarce resource that can contribute to waste when it is stretched too thin.
“It’s not just about overtreatment; it’s about getting the right treatment, and the right treatment depends on the right diagnosis, and the right diagnosis depends on really taking the time to think carefully with the patient about what’s going on,” says Vineet Arora, MD, MAPP, FHM, a hospitalist and researcher at the University of Chicago. A doctor “pulled in 10 different ways in the hospital” simply may not have the bandwidth to devote sufficient time to a complex patient; ordering a test can then seem like an enticing way to save some time.
Although electronic health records may have simplified the process for ordering CT scans and other tests, Dr. Arora says, they sometimes supersede important conversations that should take place with radiologists or other specialists about whether those tests are truly necessary. Meanwhile, providers face a proliferation of reporting duties. Recent surveys, in fact, suggest that doctors are “drowning” in paperwork and computer-based reporting requirements. Placing additional demands on a doctor’s time, Dr. Arora says, can limit his or her availability for other duties.
With hospitalists caring for increasingly complex patients with more complicated therapeutics, UCSF’s Christopher Moriates, MD, agrees that insufficient time can be an important barrier to change. It is not, however, insurmountable. If the ethos of medicine is “First, do no harm,” he says, it’s critical for doctors to remember that waste is harm.
“If we’re really going to stand by that,” he says, “then it rises to be something that we really need to take on.”
Reform advocates agree that a doctor’s time is a scarce resource that can contribute to waste when it is stretched too thin.
“It’s not just about overtreatment; it’s about getting the right treatment, and the right treatment depends on the right diagnosis, and the right diagnosis depends on really taking the time to think carefully with the patient about what’s going on,” says Vineet Arora, MD, MAPP, FHM, a hospitalist and researcher at the University of Chicago. A doctor “pulled in 10 different ways in the hospital” simply may not have the bandwidth to devote sufficient time to a complex patient; ordering a test can then seem like an enticing way to save some time.
Although electronic health records may have simplified the process for ordering CT scans and other tests, Dr. Arora says, they sometimes supersede important conversations that should take place with radiologists or other specialists about whether those tests are truly necessary. Meanwhile, providers face a proliferation of reporting duties. Recent surveys, in fact, suggest that doctors are “drowning” in paperwork and computer-based reporting requirements. Placing additional demands on a doctor’s time, Dr. Arora says, can limit his or her availability for other duties.
With hospitalists caring for increasingly complex patients with more complicated therapeutics, UCSF’s Christopher Moriates, MD, agrees that insufficient time can be an important barrier to change. It is not, however, insurmountable. If the ethos of medicine is “First, do no harm,” he says, it’s critical for doctors to remember that waste is harm.
“If we’re really going to stand by that,” he says, “then it rises to be something that we really need to take on.”
Tips for Reducing Medical Device Alarm Fatigue
In April 2013, The Joint Commission issued a Sentinel Event Alert that provided hospitals with recommendations for assessing their individual circumstances and developing a systematic, coordinated approach regarding medical device alarms.
The recommendations correspond with those of the Association for the Advancement of Medical Instrumentation (AAMI) and ECRI Institute. Most of the information and guidance provided in these alerts is drawn from The Joint Commission’s Sentinel Event Database, a voluntary reporting system for serious adverse events in healthcare.
The recommendations include the following:
- Create a process for safe alarm management and response in high-risk areas;
- Inventory alarm-equipped medical devices used for high-risk areas and conditions, and identify default alarm settings;
- Have guidelines for tailoring alarm settings and limits for individual patients; and
- Inspect, check, and maintain alarm-equipped devices.
The Joint Commission alert also recommended training and education for all clinical care team members on safe alarm management and response in high-risk areas. Organizations should also consider ways to reduce nuisance alarm signals.
“Patient harm and death that is caused by factors related to alarm management has persisted as the top patient safety issue,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill.
In addition to the alert and existing accreditation standards regarding alarm safety, The Joint Commission issued 2014 National Patient Safety Goals to help healthcare organizations address this issue.
Beginning in January 2014, hospitals were required to identify the most important alarms to manage based on their own internal situations. In phase 2, beginning in January 2016, hospitals will be expected to develop and implement specific components of alarm policies and procedures that address such items as clinically appropriate settings, when settings can be changed, and who is allowed to make such changes. Requirements only apply to organizations accredited by The Joint Commission.
In April 2013, The Joint Commission issued a Sentinel Event Alert that provided hospitals with recommendations for assessing their individual circumstances and developing a systematic, coordinated approach regarding medical device alarms.
The recommendations correspond with those of the Association for the Advancement of Medical Instrumentation (AAMI) and ECRI Institute. Most of the information and guidance provided in these alerts is drawn from The Joint Commission’s Sentinel Event Database, a voluntary reporting system for serious adverse events in healthcare.
The recommendations include the following:
- Create a process for safe alarm management and response in high-risk areas;
- Inventory alarm-equipped medical devices used for high-risk areas and conditions, and identify default alarm settings;
- Have guidelines for tailoring alarm settings and limits for individual patients; and
- Inspect, check, and maintain alarm-equipped devices.
The Joint Commission alert also recommended training and education for all clinical care team members on safe alarm management and response in high-risk areas. Organizations should also consider ways to reduce nuisance alarm signals.
“Patient harm and death that is caused by factors related to alarm management has persisted as the top patient safety issue,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill.
In addition to the alert and existing accreditation standards regarding alarm safety, The Joint Commission issued 2014 National Patient Safety Goals to help healthcare organizations address this issue.
Beginning in January 2014, hospitals were required to identify the most important alarms to manage based on their own internal situations. In phase 2, beginning in January 2016, hospitals will be expected to develop and implement specific components of alarm policies and procedures that address such items as clinically appropriate settings, when settings can be changed, and who is allowed to make such changes. Requirements only apply to organizations accredited by The Joint Commission.
In April 2013, The Joint Commission issued a Sentinel Event Alert that provided hospitals with recommendations for assessing their individual circumstances and developing a systematic, coordinated approach regarding medical device alarms.
The recommendations correspond with those of the Association for the Advancement of Medical Instrumentation (AAMI) and ECRI Institute. Most of the information and guidance provided in these alerts is drawn from The Joint Commission’s Sentinel Event Database, a voluntary reporting system for serious adverse events in healthcare.
The recommendations include the following:
- Create a process for safe alarm management and response in high-risk areas;
- Inventory alarm-equipped medical devices used for high-risk areas and conditions, and identify default alarm settings;
- Have guidelines for tailoring alarm settings and limits for individual patients; and
- Inspect, check, and maintain alarm-equipped devices.
The Joint Commission alert also recommended training and education for all clinical care team members on safe alarm management and response in high-risk areas. Organizations should also consider ways to reduce nuisance alarm signals.
“Patient harm and death that is caused by factors related to alarm management has persisted as the top patient safety issue,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill.
In addition to the alert and existing accreditation standards regarding alarm safety, The Joint Commission issued 2014 National Patient Safety Goals to help healthcare organizations address this issue.
Beginning in January 2014, hospitals were required to identify the most important alarms to manage based on their own internal situations. In phase 2, beginning in January 2016, hospitals will be expected to develop and implement specific components of alarm policies and procedures that address such items as clinically appropriate settings, when settings can be changed, and who is allowed to make such changes. Requirements only apply to organizations accredited by The Joint Commission.
Observation Status Bill in Senate Doesn’t Solve Policy Problem
As you may have heard, H.R. 876, a bill unanimously passed in the House recently, requires a hospital to give adequate oral and written notification of a patient’s observation status. The bill has now moved to the Senate.
“Notice of Observation Treatment and Implication for Care Eligibility Act,” known as the NOTICE Act, was sponsored by Rep. Lloyd Doggett (D-Texas) and co-sponsored by Rep. Earl Blumenauer (D-Ore.), Rep. Charles Rangel (D-N.Y.), and Rep. Todd Young (R-Ind.), all known to be admirable patient care advocates.
The bill proposes requiring that any patient who has been classified as observation status for more than 24 hours be given oral and written notice within 36 hours of that classification. That notice must include the reason for and implications of that status, including lack of coverage for services and cost sharing under Medicare Part B, as well as the name and title of the hospital staff who gave the oral notification. Written notification must be signed by the patient or, if the patient refuses, by the staff who presented it.
Although it is essential that patients are aware of observation status and its implications, this bill would not solve the underlying problem and would only create divisions between patients and the staff caring for them. Two issues stand out:
- Observation status is not currently a medical determination; and
- Hospitalized medical patients should not be considered outpatients.
When a patient is admitted to the hospital, acute inpatient versus observation status is often assigned by a non-clinician in the form of a “verbal” order before the attending hospitalist meets or even hears of the patient. This order must be signed promptly by that hospitalist to prevent penalization for lack of medical record compliance. Increasingly, more of these orders are for observation status, as hospitals fear bounty-hunting recovery audit contractors (RACs) in pursuit of “Medicare fraud.”
Under H.R. 876, the situation is further intensified for both clinicians and patients. Picture yourself in the middle of a busy day at your hospital, admitting and discharging patients, stabilizing critically ill patients, and discussing goals of care with patients given life-altering diagnoses. Your pager goes off.
“Mrs. H. on 6th Floor East wants to talk to you right away,” the conversation starts. Mrs. H is in tears, and her family is angry. “We were just told that Grandma is observation status, not admitted to the hospital! This makes no sense!”
Forty-five minutes later, you have agreed, commiserated, and let them know you have absolutely no control over the designation. To you, Mrs. H. is medically ill enough to require hospitalization, and she and her family agree, but Medicare regulations and fear of RAC audits keep her on observation status. What have you accomplished during that time?
H.R. 876 is not the problem, and it is clearly well intentioned. I regularly inform patients when I’m aware of their observation status, because it’s a lousy situation for the patient. We should all be doing as much.
But H.R. 876 is not the solution, either, because it does not address the core problems with observation policy. Now is the time for us all to step forward, voicing our support of SHM as it works to change observation status as we now know it. It is not an easy task. The ultimate goal is to be able to consider all hospitalized medical patients what they really are: inpatients.
Dr. Johnson is clinical associate professor in the department of internal medicine at the University of Iowa Carver College of Medicine. She is a member of the SHM Public Policy Committee and was one of the authors of the SHM PPC white paper on observation status released in July 2014.
As you may have heard, H.R. 876, a bill unanimously passed in the House recently, requires a hospital to give adequate oral and written notification of a patient’s observation status. The bill has now moved to the Senate.
“Notice of Observation Treatment and Implication for Care Eligibility Act,” known as the NOTICE Act, was sponsored by Rep. Lloyd Doggett (D-Texas) and co-sponsored by Rep. Earl Blumenauer (D-Ore.), Rep. Charles Rangel (D-N.Y.), and Rep. Todd Young (R-Ind.), all known to be admirable patient care advocates.
The bill proposes requiring that any patient who has been classified as observation status for more than 24 hours be given oral and written notice within 36 hours of that classification. That notice must include the reason for and implications of that status, including lack of coverage for services and cost sharing under Medicare Part B, as well as the name and title of the hospital staff who gave the oral notification. Written notification must be signed by the patient or, if the patient refuses, by the staff who presented it.
Although it is essential that patients are aware of observation status and its implications, this bill would not solve the underlying problem and would only create divisions between patients and the staff caring for them. Two issues stand out:
- Observation status is not currently a medical determination; and
- Hospitalized medical patients should not be considered outpatients.
When a patient is admitted to the hospital, acute inpatient versus observation status is often assigned by a non-clinician in the form of a “verbal” order before the attending hospitalist meets or even hears of the patient. This order must be signed promptly by that hospitalist to prevent penalization for lack of medical record compliance. Increasingly, more of these orders are for observation status, as hospitals fear bounty-hunting recovery audit contractors (RACs) in pursuit of “Medicare fraud.”
Under H.R. 876, the situation is further intensified for both clinicians and patients. Picture yourself in the middle of a busy day at your hospital, admitting and discharging patients, stabilizing critically ill patients, and discussing goals of care with patients given life-altering diagnoses. Your pager goes off.
“Mrs. H. on 6th Floor East wants to talk to you right away,” the conversation starts. Mrs. H is in tears, and her family is angry. “We were just told that Grandma is observation status, not admitted to the hospital! This makes no sense!”
Forty-five minutes later, you have agreed, commiserated, and let them know you have absolutely no control over the designation. To you, Mrs. H. is medically ill enough to require hospitalization, and she and her family agree, but Medicare regulations and fear of RAC audits keep her on observation status. What have you accomplished during that time?
H.R. 876 is not the problem, and it is clearly well intentioned. I regularly inform patients when I’m aware of their observation status, because it’s a lousy situation for the patient. We should all be doing as much.
But H.R. 876 is not the solution, either, because it does not address the core problems with observation policy. Now is the time for us all to step forward, voicing our support of SHM as it works to change observation status as we now know it. It is not an easy task. The ultimate goal is to be able to consider all hospitalized medical patients what they really are: inpatients.
Dr. Johnson is clinical associate professor in the department of internal medicine at the University of Iowa Carver College of Medicine. She is a member of the SHM Public Policy Committee and was one of the authors of the SHM PPC white paper on observation status released in July 2014.
As you may have heard, H.R. 876, a bill unanimously passed in the House recently, requires a hospital to give adequate oral and written notification of a patient’s observation status. The bill has now moved to the Senate.
“Notice of Observation Treatment and Implication for Care Eligibility Act,” known as the NOTICE Act, was sponsored by Rep. Lloyd Doggett (D-Texas) and co-sponsored by Rep. Earl Blumenauer (D-Ore.), Rep. Charles Rangel (D-N.Y.), and Rep. Todd Young (R-Ind.), all known to be admirable patient care advocates.
The bill proposes requiring that any patient who has been classified as observation status for more than 24 hours be given oral and written notice within 36 hours of that classification. That notice must include the reason for and implications of that status, including lack of coverage for services and cost sharing under Medicare Part B, as well as the name and title of the hospital staff who gave the oral notification. Written notification must be signed by the patient or, if the patient refuses, by the staff who presented it.
Although it is essential that patients are aware of observation status and its implications, this bill would not solve the underlying problem and would only create divisions between patients and the staff caring for them. Two issues stand out:
- Observation status is not currently a medical determination; and
- Hospitalized medical patients should not be considered outpatients.
When a patient is admitted to the hospital, acute inpatient versus observation status is often assigned by a non-clinician in the form of a “verbal” order before the attending hospitalist meets or even hears of the patient. This order must be signed promptly by that hospitalist to prevent penalization for lack of medical record compliance. Increasingly, more of these orders are for observation status, as hospitals fear bounty-hunting recovery audit contractors (RACs) in pursuit of “Medicare fraud.”
Under H.R. 876, the situation is further intensified for both clinicians and patients. Picture yourself in the middle of a busy day at your hospital, admitting and discharging patients, stabilizing critically ill patients, and discussing goals of care with patients given life-altering diagnoses. Your pager goes off.
“Mrs. H. on 6th Floor East wants to talk to you right away,” the conversation starts. Mrs. H is in tears, and her family is angry. “We were just told that Grandma is observation status, not admitted to the hospital! This makes no sense!”
Forty-five minutes later, you have agreed, commiserated, and let them know you have absolutely no control over the designation. To you, Mrs. H. is medically ill enough to require hospitalization, and she and her family agree, but Medicare regulations and fear of RAC audits keep her on observation status. What have you accomplished during that time?
H.R. 876 is not the problem, and it is clearly well intentioned. I regularly inform patients when I’m aware of their observation status, because it’s a lousy situation for the patient. We should all be doing as much.
But H.R. 876 is not the solution, either, because it does not address the core problems with observation policy. Now is the time for us all to step forward, voicing our support of SHM as it works to change observation status as we now know it. It is not an easy task. The ultimate goal is to be able to consider all hospitalized medical patients what they really are: inpatients.
Dr. Johnson is clinical associate professor in the department of internal medicine at the University of Iowa Carver College of Medicine. She is a member of the SHM Public Policy Committee and was one of the authors of the SHM PPC white paper on observation status released in July 2014.
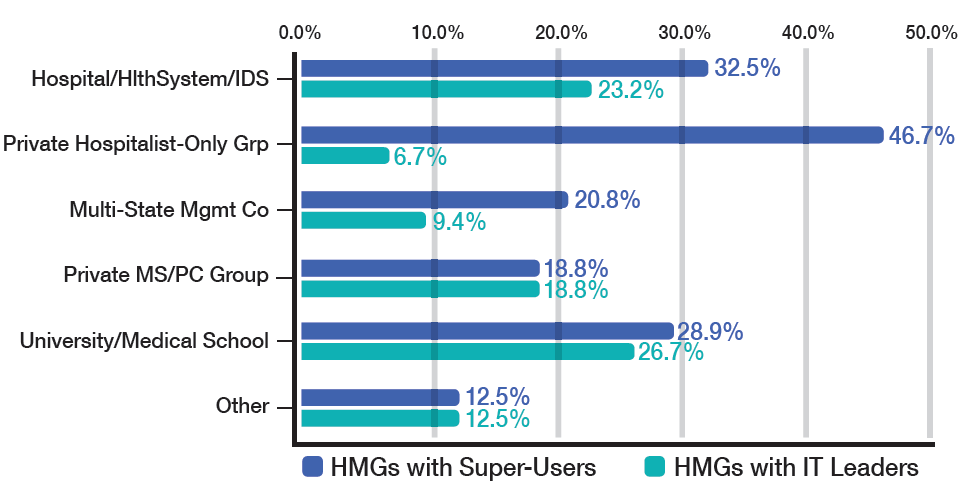
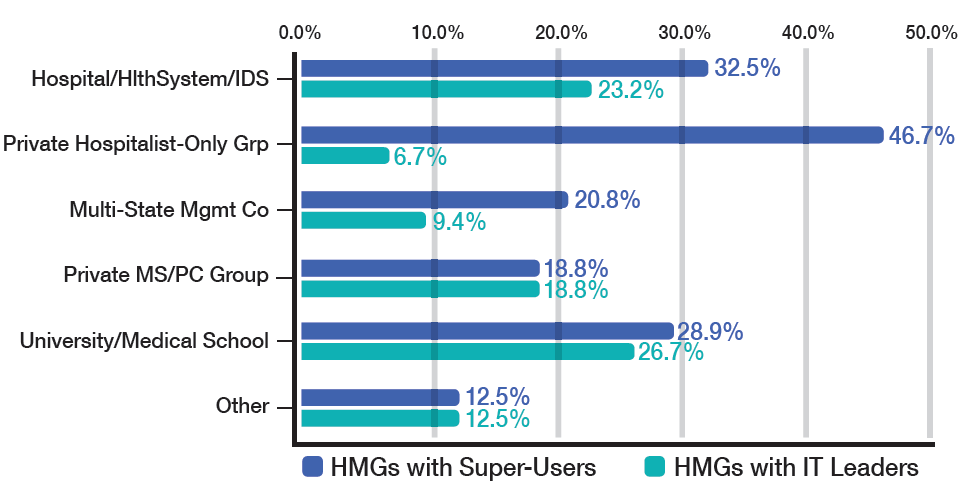
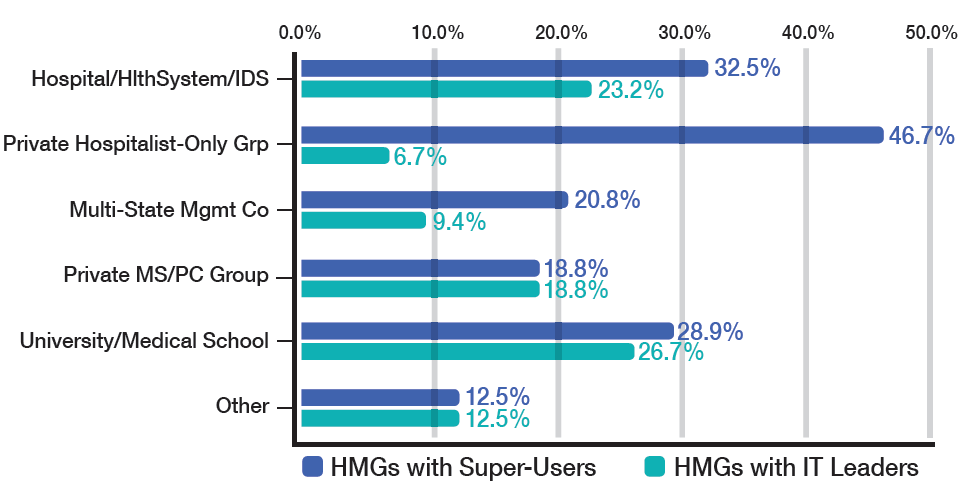
Society of Hospital Medicine Engagement Benchmarking Service Available
SHM’s new Engagement Benchmarking Service helps hospital medicine groups (HMGs) better understand how to engage their physicians for increased retention and performance. Now, SHM is offering the service free to SHM members as a way to build a database and familiarize HMGs with the value of the service. For details, visit www.hospitalmedicine.org/engage.
SHM’s new Engagement Benchmarking Service helps hospital medicine groups (HMGs) better understand how to engage their physicians for increased retention and performance. Now, SHM is offering the service free to SHM members as a way to build a database and familiarize HMGs with the value of the service. For details, visit www.hospitalmedicine.org/engage.
SHM’s new Engagement Benchmarking Service helps hospital medicine groups (HMGs) better understand how to engage their physicians for increased retention and performance. Now, SHM is offering the service free to SHM members as a way to build a database and familiarize HMGs with the value of the service. For details, visit www.hospitalmedicine.org/engage.
Hospital Medicine Exchange Posts Top Topics Among Hospitalists
More than 7,000 hospitalists have logged in to HMX to ask questions and share successes. These are the top topics hospitalists are discussing on HMX:
- PICC Line in IV Drug Users;
- Hospitalists Who Do Procedures;
- Census Cap Policies;
- Case Logs for Treating Patients on the Floors; and
- Medication Reconciliation.
Join the discussion—or start your own—today at www.hmxchange.org.
More than 7,000 hospitalists have logged in to HMX to ask questions and share successes. These are the top topics hospitalists are discussing on HMX:
- PICC Line in IV Drug Users;
- Hospitalists Who Do Procedures;
- Census Cap Policies;
- Case Logs for Treating Patients on the Floors; and
- Medication Reconciliation.
Join the discussion—or start your own—today at www.hmxchange.org.
More than 7,000 hospitalists have logged in to HMX to ask questions and share successes. These are the top topics hospitalists are discussing on HMX:
- PICC Line in IV Drug Users;
- Hospitalists Who Do Procedures;
- Census Cap Policies;
- Case Logs for Treating Patients on the Floors; and
- Medication Reconciliation.
Join the discussion—or start your own—today at www.hmxchange.org.
Society of Hospital Medicine Programs Help Improve Your Hospital
New Patient Experience Community and Resources
SHM’s new Patient Experience Committee has begun convening resources and people to help hospitalists address the patient experience. In addition to new resources on the SHM website, SHM has set up an HMX community specifically dedicated to the many issues related to the experience of patients in the hospital. To get involved, visit www.hospitalmedicine.org/patientexperience.
Project BOOST On-Demand Webinar Available
It’s never too late—or too early—to think about improving processes to reduce readmissions. SHM’s Project BOOST now accepts program applications throughout the year, and the recent webinar with Project BOOST program leaders is now available for free online. www.hospitalmedicine.org/boost.
Glycemic Control Implementation Guide available in June.
Glycemic control and the management of diabetic patients can be challenging for hospitalists. That’s why SHM is presenting the new Glycemic Control Implementation Guide. Recent webinars are available, too, at www.hospitalmedicine.org/qi.
Free CME on Acute Coronary Syndrome
Approximately 1.7 million patients are hospitalized for acute coronary syndrome (ACS), and 600,000 die because of an acute myocardial infarction. Now, SHM is presenting a free self-directed web-based activity designed to help hospitalists evaluate practices and strategies to affect outcomes. For details, visit www.hospitalmedicine.org/qi.
This educational initiative is supported by an educational grant from AstraZeneca.
New Patient Experience Community and Resources
SHM’s new Patient Experience Committee has begun convening resources and people to help hospitalists address the patient experience. In addition to new resources on the SHM website, SHM has set up an HMX community specifically dedicated to the many issues related to the experience of patients in the hospital. To get involved, visit www.hospitalmedicine.org/patientexperience.
Project BOOST On-Demand Webinar Available
It’s never too late—or too early—to think about improving processes to reduce readmissions. SHM’s Project BOOST now accepts program applications throughout the year, and the recent webinar with Project BOOST program leaders is now available for free online. www.hospitalmedicine.org/boost.
Glycemic Control Implementation Guide available in June.
Glycemic control and the management of diabetic patients can be challenging for hospitalists. That’s why SHM is presenting the new Glycemic Control Implementation Guide. Recent webinars are available, too, at www.hospitalmedicine.org/qi.
Free CME on Acute Coronary Syndrome
Approximately 1.7 million patients are hospitalized for acute coronary syndrome (ACS), and 600,000 die because of an acute myocardial infarction. Now, SHM is presenting a free self-directed web-based activity designed to help hospitalists evaluate practices and strategies to affect outcomes. For details, visit www.hospitalmedicine.org/qi.
This educational initiative is supported by an educational grant from AstraZeneca.
New Patient Experience Community and Resources
SHM’s new Patient Experience Committee has begun convening resources and people to help hospitalists address the patient experience. In addition to new resources on the SHM website, SHM has set up an HMX community specifically dedicated to the many issues related to the experience of patients in the hospital. To get involved, visit www.hospitalmedicine.org/patientexperience.
Project BOOST On-Demand Webinar Available
It’s never too late—or too early—to think about improving processes to reduce readmissions. SHM’s Project BOOST now accepts program applications throughout the year, and the recent webinar with Project BOOST program leaders is now available for free online. www.hospitalmedicine.org/boost.
Glycemic Control Implementation Guide available in June.
Glycemic control and the management of diabetic patients can be challenging for hospitalists. That’s why SHM is presenting the new Glycemic Control Implementation Guide. Recent webinars are available, too, at www.hospitalmedicine.org/qi.
Free CME on Acute Coronary Syndrome
Approximately 1.7 million patients are hospitalized for acute coronary syndrome (ACS), and 600,000 die because of an acute myocardial infarction. Now, SHM is presenting a free self-directed web-based activity designed to help hospitalists evaluate practices and strategies to affect outcomes. For details, visit www.hospitalmedicine.org/qi.
This educational initiative is supported by an educational grant from AstraZeneca.
Society of Hospital Medicine Events for Hospitalists in 2015
Pediatric Hospital Medicine
July 23-26, San Antonio
PHM 2015 will also feature a mobile conference app for online access to the agenda and many other features. To register, visit www.phmmeeting.org.
Academic Hospitalist Academy
Oct. 7-10, Englewood, Colo.
![]()
Adult Hospital Medicine Boot Camp for Physician Assistants and Nurse Practitioners
Oct. 14-18, Phoenix
![]()
Leadership Academy
Oct. 19-22, Austin
![]()
Pediatric Hospital Medicine
July 23-26, San Antonio
PHM 2015 will also feature a mobile conference app for online access to the agenda and many other features. To register, visit www.phmmeeting.org.
Academic Hospitalist Academy
Oct. 7-10, Englewood, Colo.
![]()
Adult Hospital Medicine Boot Camp for Physician Assistants and Nurse Practitioners
Oct. 14-18, Phoenix
![]()
Leadership Academy
Oct. 19-22, Austin
![]()
Pediatric Hospital Medicine
July 23-26, San Antonio
PHM 2015 will also feature a mobile conference app for online access to the agenda and many other features. To register, visit www.phmmeeting.org.
Academic Hospitalist Academy
Oct. 7-10, Englewood, Colo.
![]()
Adult Hospital Medicine Boot Camp for Physician Assistants and Nurse Practitioners
Oct. 14-18, Phoenix
![]()
Leadership Academy
Oct. 19-22, Austin
![]()
Society of Hospital Medicine Learning Portal Adds Programs
Free CME is available to all SHM members, and new modules are added all the time. Here’s a sampling of the most recent online modules:
- Observation or Inpatient? Challenges and Successes in Implementing the Two-Midnight Rule.
- Primer for Hospitalists on Skilled Nursing Facilities: SHM’s first educational initiative, directed at a rapidly growing segment of work for hospitalists, post-acute care (PAC).
- Organizational Knowledge and Leadership Skills 2015.
- Patient Safety Principles 2015.
- Quality Measurement and Stakeholder Interest 2015.
Free CME is available to all SHM members, and new modules are added all the time. Here’s a sampling of the most recent online modules:
- Observation or Inpatient? Challenges and Successes in Implementing the Two-Midnight Rule.
- Primer for Hospitalists on Skilled Nursing Facilities: SHM’s first educational initiative, directed at a rapidly growing segment of work for hospitalists, post-acute care (PAC).
- Organizational Knowledge and Leadership Skills 2015.
- Patient Safety Principles 2015.
- Quality Measurement and Stakeholder Interest 2015.
Free CME is available to all SHM members, and new modules are added all the time. Here’s a sampling of the most recent online modules:
- Observation or Inpatient? Challenges and Successes in Implementing the Two-Midnight Rule.
- Primer for Hospitalists on Skilled Nursing Facilities: SHM’s first educational initiative, directed at a rapidly growing segment of work for hospitalists, post-acute care (PAC).
- Organizational Knowledge and Leadership Skills 2015.
- Patient Safety Principles 2015.
- Quality Measurement and Stakeholder Interest 2015.
Veteran's Affairs Education Programs Develop Hospitalist Leaders
The Veterans Health Administration (VHA) is entrusted with three key missions: clinical care, research, and education. Although clinical care and research receive much of the publicity, the role that the VHA plays in education remains critically important to both current and future healthcare providers.
As one of the statutory requirements of the Department of Veterans Affairs (VA), the VHA runs multiple training programs, encompassing many types of healthcare providers, under the aegis of the Office of Academic Affiliations (OAA). Started after World War II, OAA was founded on the premise of joining each VA hospital with a medical school. For more than 60 years, these agreements have grown and flourished, and VHA facilities currently have affiliation agreements with 130 of the 141 accredited allopathic and 22 of the 29 accredited osteopathic medical schools in the United States. In partnership with these academic institutions, VHA trained more than 40,000 graduate medical learners (residents and fellows) and more than 21,000 medical students in 2013 alone. This makes VHA the nation’s single largest provider of medical education. Currently, more than 65% of all U.S. physicians have completed some portion of their training in a VHA setting.
A core piece of the VHA, OAA continues to innovate as it grows. For example, as the country moves toward patient-centered medical homes, VHA has developed its own version: patient aligned care teams (PACTs). Accordingly, OAA has been overseeing the development of “Academic” PACTs to better understand how to incorporate trainees into these new systems of care.
Along the same lines, there are three post-graduate training programs of particular interest to hospitalists: the Chief Resident in Quality and Patient Safety (CRQS) program, the Patient Safety Fellowship Program, and the VA National Quality Scholars Fellowship Program (NQSFP). All of these have rigorous educational components that are coordinated through the National Center for Patient Safety.
The CRQS program was developed to support additional chief residents who would be dedicated to educating housestaff and students about quality improvement and patient safety. As of July 1, 2015, there will be 58 such chief residents at VAs across the country. These positions are open to any residency that has at least eight other VA-funded resident positions in the program. Currently, there are CRQSs from internal medicine, surgery, anesthesia, and psychiatry.
The Patient Safety Fellowship is a one-year interdisciplinary program that includes nurses, pharmacists, and psychologists, as well as the physician fellows. This program is offered at six VA Medical Centers across the county and focuses on patient safety improvement science and leadership development.
Since 1999, the NQSFP has produced fellows that are leaders in QI scholarship and implementation. It is a two-year fellowship for post-graduate nurses and physicians and occurs at eight sites across the U.S.
These programs offer graduating residents who are interested in safety and quality opportunities to develop skills in research, implementation, and education. These are especially beneficial for hospitalists who may wish to pursue leadership roles in quality and safety at the program, institution, or healthcare system level.
The VA’s commitment to medical education starts at the level of medical school and continues through its post-graduate programs, many of which may well produce hospitalist leaders of the future.
Dr. Fletcher is associate program director for the internal medicine residency program at the Clement J. Zablocki VA Medical Center and the Medical College of Wisconsin in Madison. Dr. Bates is graduate medical education site director for internal medicine at Baylor College of Medicine at the Michael E. DeBakey VA Medical Center in Houston.
The Veterans Health Administration (VHA) is entrusted with three key missions: clinical care, research, and education. Although clinical care and research receive much of the publicity, the role that the VHA plays in education remains critically important to both current and future healthcare providers.
As one of the statutory requirements of the Department of Veterans Affairs (VA), the VHA runs multiple training programs, encompassing many types of healthcare providers, under the aegis of the Office of Academic Affiliations (OAA). Started after World War II, OAA was founded on the premise of joining each VA hospital with a medical school. For more than 60 years, these agreements have grown and flourished, and VHA facilities currently have affiliation agreements with 130 of the 141 accredited allopathic and 22 of the 29 accredited osteopathic medical schools in the United States. In partnership with these academic institutions, VHA trained more than 40,000 graduate medical learners (residents and fellows) and more than 21,000 medical students in 2013 alone. This makes VHA the nation’s single largest provider of medical education. Currently, more than 65% of all U.S. physicians have completed some portion of their training in a VHA setting.
A core piece of the VHA, OAA continues to innovate as it grows. For example, as the country moves toward patient-centered medical homes, VHA has developed its own version: patient aligned care teams (PACTs). Accordingly, OAA has been overseeing the development of “Academic” PACTs to better understand how to incorporate trainees into these new systems of care.
Along the same lines, there are three post-graduate training programs of particular interest to hospitalists: the Chief Resident in Quality and Patient Safety (CRQS) program, the Patient Safety Fellowship Program, and the VA National Quality Scholars Fellowship Program (NQSFP). All of these have rigorous educational components that are coordinated through the National Center for Patient Safety.
The CRQS program was developed to support additional chief residents who would be dedicated to educating housestaff and students about quality improvement and patient safety. As of July 1, 2015, there will be 58 such chief residents at VAs across the country. These positions are open to any residency that has at least eight other VA-funded resident positions in the program. Currently, there are CRQSs from internal medicine, surgery, anesthesia, and psychiatry.
The Patient Safety Fellowship is a one-year interdisciplinary program that includes nurses, pharmacists, and psychologists, as well as the physician fellows. This program is offered at six VA Medical Centers across the county and focuses on patient safety improvement science and leadership development.
Since 1999, the NQSFP has produced fellows that are leaders in QI scholarship and implementation. It is a two-year fellowship for post-graduate nurses and physicians and occurs at eight sites across the U.S.
These programs offer graduating residents who are interested in safety and quality opportunities to develop skills in research, implementation, and education. These are especially beneficial for hospitalists who may wish to pursue leadership roles in quality and safety at the program, institution, or healthcare system level.
The VA’s commitment to medical education starts at the level of medical school and continues through its post-graduate programs, many of which may well produce hospitalist leaders of the future.
Dr. Fletcher is associate program director for the internal medicine residency program at the Clement J. Zablocki VA Medical Center and the Medical College of Wisconsin in Madison. Dr. Bates is graduate medical education site director for internal medicine at Baylor College of Medicine at the Michael E. DeBakey VA Medical Center in Houston.
The Veterans Health Administration (VHA) is entrusted with three key missions: clinical care, research, and education. Although clinical care and research receive much of the publicity, the role that the VHA plays in education remains critically important to both current and future healthcare providers.
As one of the statutory requirements of the Department of Veterans Affairs (VA), the VHA runs multiple training programs, encompassing many types of healthcare providers, under the aegis of the Office of Academic Affiliations (OAA). Started after World War II, OAA was founded on the premise of joining each VA hospital with a medical school. For more than 60 years, these agreements have grown and flourished, and VHA facilities currently have affiliation agreements with 130 of the 141 accredited allopathic and 22 of the 29 accredited osteopathic medical schools in the United States. In partnership with these academic institutions, VHA trained more than 40,000 graduate medical learners (residents and fellows) and more than 21,000 medical students in 2013 alone. This makes VHA the nation’s single largest provider of medical education. Currently, more than 65% of all U.S. physicians have completed some portion of their training in a VHA setting.
A core piece of the VHA, OAA continues to innovate as it grows. For example, as the country moves toward patient-centered medical homes, VHA has developed its own version: patient aligned care teams (PACTs). Accordingly, OAA has been overseeing the development of “Academic” PACTs to better understand how to incorporate trainees into these new systems of care.
Along the same lines, there are three post-graduate training programs of particular interest to hospitalists: the Chief Resident in Quality and Patient Safety (CRQS) program, the Patient Safety Fellowship Program, and the VA National Quality Scholars Fellowship Program (NQSFP). All of these have rigorous educational components that are coordinated through the National Center for Patient Safety.
The CRQS program was developed to support additional chief residents who would be dedicated to educating housestaff and students about quality improvement and patient safety. As of July 1, 2015, there will be 58 such chief residents at VAs across the country. These positions are open to any residency that has at least eight other VA-funded resident positions in the program. Currently, there are CRQSs from internal medicine, surgery, anesthesia, and psychiatry.
The Patient Safety Fellowship is a one-year interdisciplinary program that includes nurses, pharmacists, and psychologists, as well as the physician fellows. This program is offered at six VA Medical Centers across the county and focuses on patient safety improvement science and leadership development.
Since 1999, the NQSFP has produced fellows that are leaders in QI scholarship and implementation. It is a two-year fellowship for post-graduate nurses and physicians and occurs at eight sites across the U.S.
These programs offer graduating residents who are interested in safety and quality opportunities to develop skills in research, implementation, and education. These are especially beneficial for hospitalists who may wish to pursue leadership roles in quality and safety at the program, institution, or healthcare system level.
The VA’s commitment to medical education starts at the level of medical school and continues through its post-graduate programs, many of which may well produce hospitalist leaders of the future.
Dr. Fletcher is associate program director for the internal medicine residency program at the Clement J. Zablocki VA Medical Center and the Medical College of Wisconsin in Madison. Dr. Bates is graduate medical education site director for internal medicine at Baylor College of Medicine at the Michael E. DeBakey VA Medical Center in Houston.


