User login
The health care ‘iron triangle’
To the Editor: In his article, Dr. Lehman1 argued that because the Patient Protection and Affordable Care Act (PPACA) attempts to break the healthcare “iron triangle” by simultaneously improving access and quality while reducing costs, it may paradoxically make the situation worse on all three fronts. However, this line of argument fails to provide a comparison—that is, worse compared to what? While Dr. Lehman does not suggest a comparison, two come to mind that could be implied from his arguments: 1) doing nothing, or 2) targeting reform at only two sides of the triangle.
Prior to the PPACA, the US healthcare system had serious problems with access, quality, and cost.2 While it is true that any reform could potentially be worse than doing nothing, none of the three seemed to be getting any better under the status quo. Both candidates for president in 2008 agreed that doing nothing was no longer an option.3,4 Alternatively, trying to improve two legs of the triangle (say, access and quality) while acknowledging that the third (cost) would suffer would have been just as politically untenable.
The true explanation for how the PPACA could expect to (and may still) improve access and quality while reducing healthcare costs (compared to no reform) is that the PPACA is not a single intervention, as is obvious from the 2,000-plus pages of the law. No single component of the law needs to do all three. For example, expanding Medicaid improves access and quality (especially for those without prior coverage) but undoubtedly raises costs. On the other hand, accountable care organizations should decrease costs by incentivizing providers to be more efficient and reduce waste (and ideally would also improve quality).5 Given the low bar set prior to implementation of the PPACA, it was not a stretch to have expected any major reform to improve (not fix) our problems with access, quality, and cost.
- Lehman EP. The health care ‘iron triangle’ and the Patient Protection and Affordable Care Act. Cleve Clin J Med 2015; 82:73–80.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008; 27:759–769.
- McCain J. Access to quality and affordable health care for every American. N Engl J Med 2008; 359:1537–1541.
- Obama B. Modern health care for all Americans. N Engl J Med 2008; 359:1537–1541.
- Shortell SM, Casalino LP. Health care reform requires accountable care systems. JAMA 2008; 300:95–97.
To the Editor: In his article, Dr. Lehman1 argued that because the Patient Protection and Affordable Care Act (PPACA) attempts to break the healthcare “iron triangle” by simultaneously improving access and quality while reducing costs, it may paradoxically make the situation worse on all three fronts. However, this line of argument fails to provide a comparison—that is, worse compared to what? While Dr. Lehman does not suggest a comparison, two come to mind that could be implied from his arguments: 1) doing nothing, or 2) targeting reform at only two sides of the triangle.
Prior to the PPACA, the US healthcare system had serious problems with access, quality, and cost.2 While it is true that any reform could potentially be worse than doing nothing, none of the three seemed to be getting any better under the status quo. Both candidates for president in 2008 agreed that doing nothing was no longer an option.3,4 Alternatively, trying to improve two legs of the triangle (say, access and quality) while acknowledging that the third (cost) would suffer would have been just as politically untenable.
The true explanation for how the PPACA could expect to (and may still) improve access and quality while reducing healthcare costs (compared to no reform) is that the PPACA is not a single intervention, as is obvious from the 2,000-plus pages of the law. No single component of the law needs to do all three. For example, expanding Medicaid improves access and quality (especially for those without prior coverage) but undoubtedly raises costs. On the other hand, accountable care organizations should decrease costs by incentivizing providers to be more efficient and reduce waste (and ideally would also improve quality).5 Given the low bar set prior to implementation of the PPACA, it was not a stretch to have expected any major reform to improve (not fix) our problems with access, quality, and cost.
To the Editor: In his article, Dr. Lehman1 argued that because the Patient Protection and Affordable Care Act (PPACA) attempts to break the healthcare “iron triangle” by simultaneously improving access and quality while reducing costs, it may paradoxically make the situation worse on all three fronts. However, this line of argument fails to provide a comparison—that is, worse compared to what? While Dr. Lehman does not suggest a comparison, two come to mind that could be implied from his arguments: 1) doing nothing, or 2) targeting reform at only two sides of the triangle.
Prior to the PPACA, the US healthcare system had serious problems with access, quality, and cost.2 While it is true that any reform could potentially be worse than doing nothing, none of the three seemed to be getting any better under the status quo. Both candidates for president in 2008 agreed that doing nothing was no longer an option.3,4 Alternatively, trying to improve two legs of the triangle (say, access and quality) while acknowledging that the third (cost) would suffer would have been just as politically untenable.
The true explanation for how the PPACA could expect to (and may still) improve access and quality while reducing healthcare costs (compared to no reform) is that the PPACA is not a single intervention, as is obvious from the 2,000-plus pages of the law. No single component of the law needs to do all three. For example, expanding Medicaid improves access and quality (especially for those without prior coverage) but undoubtedly raises costs. On the other hand, accountable care organizations should decrease costs by incentivizing providers to be more efficient and reduce waste (and ideally would also improve quality).5 Given the low bar set prior to implementation of the PPACA, it was not a stretch to have expected any major reform to improve (not fix) our problems with access, quality, and cost.
- Lehman EP. The health care ‘iron triangle’ and the Patient Protection and Affordable Care Act. Cleve Clin J Med 2015; 82:73–80.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008; 27:759–769.
- McCain J. Access to quality and affordable health care for every American. N Engl J Med 2008; 359:1537–1541.
- Obama B. Modern health care for all Americans. N Engl J Med 2008; 359:1537–1541.
- Shortell SM, Casalino LP. Health care reform requires accountable care systems. JAMA 2008; 300:95–97.
- Lehman EP. The health care ‘iron triangle’ and the Patient Protection and Affordable Care Act. Cleve Clin J Med 2015; 82:73–80.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008; 27:759–769.
- McCain J. Access to quality and affordable health care for every American. N Engl J Med 2008; 359:1537–1541.
- Obama B. Modern health care for all Americans. N Engl J Med 2008; 359:1537–1541.
- Shortell SM, Casalino LP. Health care reform requires accountable care systems. JAMA 2008; 300:95–97.
In reply: The health care ‘iron triangle’
In Reply: Many of the statements made by Dr. Riggs are indisputable. The conclusions drawn from these insights, however, are questionable.
The Patient Protection and Affordable Care Act (PPACA) was introduced under the premise that a patchwork of policies would improve access and quality of care while decreasing overall health expenditures. Dr. Riggs suggests that, since individual components are targeted toward some of these issues, the net effect of the PPACA is its breaking of the healthcare iron triangle.
Nothing could be further from the truth. This line of reasoning requires that the left hand knows not what the right hand is doing, and that each hand (ie, each component of the PPACA) can ignore the effects of the other, with each proclaiming success in its efforts. It is disingenuous to suggest that the PPACA, on the whole, improves upon the problems of access, quality, and cost if each of the program’s tenets addresses only one or two of the triangle’s vertices.
The PPACA suffers from its own lofty expectations. Rather than being a transformative law that shifts a paradigm, the PPACA is simply an evolution of an existing, broken system, cobbling together components everyone readily agrees are dysfunctional. It expands Medicaid, an insufficiently funded program for the most economically and medically disadvantaged Americans. It subsidizes private health insurance, which, for all its advantages, is likely responsible for the overconsumption of discounted healthcare. And it promotes the unproven concept of accountable care organizations, with no rational expectation that this approach would be superior to preferred provider organizations or health maintenance organizations. It is illogical to expect the sum of many broken parts to yield a superior outcome.
Dr. Riggs notes that trying to improve two legs of the triangle (increased access and improved quality) while acknowledging rising costs is politically untenable. On this point, he is absolutely correct. Discussing the harsh reality that healthcare is a scarce commodity is a political nonstarter. Until Americans demand—and politicians provide—difficult answers to the question of how we will provide healthcare in the 21st century, simultaneously improving delivery of care on all three fronts remains a fantasy. Barring truly transformative change, the iron triangle continues to rule the economics of American healthcare.
In Reply: Many of the statements made by Dr. Riggs are indisputable. The conclusions drawn from these insights, however, are questionable.
The Patient Protection and Affordable Care Act (PPACA) was introduced under the premise that a patchwork of policies would improve access and quality of care while decreasing overall health expenditures. Dr. Riggs suggests that, since individual components are targeted toward some of these issues, the net effect of the PPACA is its breaking of the healthcare iron triangle.
Nothing could be further from the truth. This line of reasoning requires that the left hand knows not what the right hand is doing, and that each hand (ie, each component of the PPACA) can ignore the effects of the other, with each proclaiming success in its efforts. It is disingenuous to suggest that the PPACA, on the whole, improves upon the problems of access, quality, and cost if each of the program’s tenets addresses only one or two of the triangle’s vertices.
The PPACA suffers from its own lofty expectations. Rather than being a transformative law that shifts a paradigm, the PPACA is simply an evolution of an existing, broken system, cobbling together components everyone readily agrees are dysfunctional. It expands Medicaid, an insufficiently funded program for the most economically and medically disadvantaged Americans. It subsidizes private health insurance, which, for all its advantages, is likely responsible for the overconsumption of discounted healthcare. And it promotes the unproven concept of accountable care organizations, with no rational expectation that this approach would be superior to preferred provider organizations or health maintenance organizations. It is illogical to expect the sum of many broken parts to yield a superior outcome.
Dr. Riggs notes that trying to improve two legs of the triangle (increased access and improved quality) while acknowledging rising costs is politically untenable. On this point, he is absolutely correct. Discussing the harsh reality that healthcare is a scarce commodity is a political nonstarter. Until Americans demand—and politicians provide—difficult answers to the question of how we will provide healthcare in the 21st century, simultaneously improving delivery of care on all three fronts remains a fantasy. Barring truly transformative change, the iron triangle continues to rule the economics of American healthcare.
In Reply: Many of the statements made by Dr. Riggs are indisputable. The conclusions drawn from these insights, however, are questionable.
The Patient Protection and Affordable Care Act (PPACA) was introduced under the premise that a patchwork of policies would improve access and quality of care while decreasing overall health expenditures. Dr. Riggs suggests that, since individual components are targeted toward some of these issues, the net effect of the PPACA is its breaking of the healthcare iron triangle.
Nothing could be further from the truth. This line of reasoning requires that the left hand knows not what the right hand is doing, and that each hand (ie, each component of the PPACA) can ignore the effects of the other, with each proclaiming success in its efforts. It is disingenuous to suggest that the PPACA, on the whole, improves upon the problems of access, quality, and cost if each of the program’s tenets addresses only one or two of the triangle’s vertices.
The PPACA suffers from its own lofty expectations. Rather than being a transformative law that shifts a paradigm, the PPACA is simply an evolution of an existing, broken system, cobbling together components everyone readily agrees are dysfunctional. It expands Medicaid, an insufficiently funded program for the most economically and medically disadvantaged Americans. It subsidizes private health insurance, which, for all its advantages, is likely responsible for the overconsumption of discounted healthcare. And it promotes the unproven concept of accountable care organizations, with no rational expectation that this approach would be superior to preferred provider organizations or health maintenance organizations. It is illogical to expect the sum of many broken parts to yield a superior outcome.
Dr. Riggs notes that trying to improve two legs of the triangle (increased access and improved quality) while acknowledging rising costs is politically untenable. On this point, he is absolutely correct. Discussing the harsh reality that healthcare is a scarce commodity is a political nonstarter. Until Americans demand—and politicians provide—difficult answers to the question of how we will provide healthcare in the 21st century, simultaneously improving delivery of care on all three fronts remains a fantasy. Barring truly transformative change, the iron triangle continues to rule the economics of American healthcare.
Alcoholic hepatitis: An important consideration
To the Editor: I read with keen interest the high-quality review of the pathogenesis, diagnosis, and management of alcoholic hepatitis by Dugum et al.1 They clearly emphasized the high morbidity and mortality rates associated with this condition.
An important consideration for healthcare practitioners is that the presentation of alcoholic hepatitis can mimic an infectious process, eg, presenting with fever and an elevated white blood cell count. Indeed, clinicians should be vigilant and should routinely evaluate for an underlying infection in patients with suspected alcoholic hepatitis, because patients with liver disease are immunocompromised and several problems can potentially coexist in any given patient.
Therefore, clinicians should focus on the clinical history and examination (vital signs, mental status examination, presence of ascites) and should screen for common coinfections such as urinary tract infection and pneumonia with a white blood cell count with differential and other tests. Of particular importance, patients with ascites should undergo diagnostic abdominal paracentesis,2 and empiric antimicrobial therapy for spontaneous bacterial peritonitis should be considered on a case-by-case basis.3
- Dugum M, Zein N, McCullough A, Hanouneh I. Alcoholic hepatitis: challenges in diagnosis and management. Cleve Clin J Med 2015; 82:226–236.
- Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013; 57:1651–1653.
- Lutz P, Nischalke HD, Strassburg CP, Spengler U. Spontaneous bacterial peritonitis: the clinical challenge of a leaky gut and a cirrhotic liver. World J Hepatol 2015; 7:304–314.
To the Editor: I read with keen interest the high-quality review of the pathogenesis, diagnosis, and management of alcoholic hepatitis by Dugum et al.1 They clearly emphasized the high morbidity and mortality rates associated with this condition.
An important consideration for healthcare practitioners is that the presentation of alcoholic hepatitis can mimic an infectious process, eg, presenting with fever and an elevated white blood cell count. Indeed, clinicians should be vigilant and should routinely evaluate for an underlying infection in patients with suspected alcoholic hepatitis, because patients with liver disease are immunocompromised and several problems can potentially coexist in any given patient.
Therefore, clinicians should focus on the clinical history and examination (vital signs, mental status examination, presence of ascites) and should screen for common coinfections such as urinary tract infection and pneumonia with a white blood cell count with differential and other tests. Of particular importance, patients with ascites should undergo diagnostic abdominal paracentesis,2 and empiric antimicrobial therapy for spontaneous bacterial peritonitis should be considered on a case-by-case basis.3
To the Editor: I read with keen interest the high-quality review of the pathogenesis, diagnosis, and management of alcoholic hepatitis by Dugum et al.1 They clearly emphasized the high morbidity and mortality rates associated with this condition.
An important consideration for healthcare practitioners is that the presentation of alcoholic hepatitis can mimic an infectious process, eg, presenting with fever and an elevated white blood cell count. Indeed, clinicians should be vigilant and should routinely evaluate for an underlying infection in patients with suspected alcoholic hepatitis, because patients with liver disease are immunocompromised and several problems can potentially coexist in any given patient.
Therefore, clinicians should focus on the clinical history and examination (vital signs, mental status examination, presence of ascites) and should screen for common coinfections such as urinary tract infection and pneumonia with a white blood cell count with differential and other tests. Of particular importance, patients with ascites should undergo diagnostic abdominal paracentesis,2 and empiric antimicrobial therapy for spontaneous bacterial peritonitis should be considered on a case-by-case basis.3
- Dugum M, Zein N, McCullough A, Hanouneh I. Alcoholic hepatitis: challenges in diagnosis and management. Cleve Clin J Med 2015; 82:226–236.
- Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013; 57:1651–1653.
- Lutz P, Nischalke HD, Strassburg CP, Spengler U. Spontaneous bacterial peritonitis: the clinical challenge of a leaky gut and a cirrhotic liver. World J Hepatol 2015; 7:304–314.
- Dugum M, Zein N, McCullough A, Hanouneh I. Alcoholic hepatitis: challenges in diagnosis and management. Cleve Clin J Med 2015; 82:226–236.
- Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013; 57:1651–1653.
- Lutz P, Nischalke HD, Strassburg CP, Spengler U. Spontaneous bacterial peritonitis: the clinical challenge of a leaky gut and a cirrhotic liver. World J Hepatol 2015; 7:304–314.
In reply: Alcoholic hepatitis: An important consideration
In Reply: We thank Dr. Mirrakhimov for his interest in our article1 and for his comments on the importance of infection evaluation and treatment in patients with alcoholic hepatitis. We agree with the points he has raised and emphasized several of them in our article. We highlighted the need to evaluate for infections in these patients, as about a quarter of them are infected at the time of presentation.2
Importantly, patients with alcoholic hepatitis frequently have systemic inflammatory response syndrome criteria, which can be related to the overall inflammatory state of the disease itself or can reflect an active bacterial infection. Therefore, clinical monitoring for symptoms and signs of infection is crucial, and screening for infections is warranted on admission as well as repeatedly during the hospital stay for patients who experience clinical deterioration.3 Obtaining blood and urine cultures and performing paracentesis in patients with ascites to evaluate for bacterial peritonitis are required. Indeed, infections are a leading cause of death in patients with severe alcoholic hepatitis, both directly and indirectly by predisposing to multiorgan failure.4
Another factor to consider is the increased susceptibility to infection in these patients treated with corticosteroids. A study by Louvet et al2 showed that nonresponse to corticosteroids is the main factor contributing to the development of infection during treatment with corticosteroids, suggesting that infection is likely a consequence of the absence of improvement in liver function. More recently, results of the Steroids or Pentoxifylline for Alcoholic Hepatitis trial (which evaluated the treatment effect of prednisolone and pentoxifylline in the management of severe alcoholic hepatitis) showed that despite the higher rates of infections in patients treated with prednisolone, the mortality rates attributed to infections were similar across the treatment groups, regardless of whether prednisolone was administered.4
Finally, it is important to emphasize that criteria to initiate empiric antibiotics in patients with alcoholic hepatitis are currently lacking, and the decision to start antibiotics empirically in patients without a clear infection is largely based on the clinician’s assessment.
- Dugum M, Zein N, McCullough A, Hanouneh I. Alcoholic hepatitis: challenges in diagnosis and management. Cleve Clin J Med 2015; 82:226–236.
- Louvet A, Wartel F, Castel H, et al. Infection in patients with severe alcoholic hepatitis treated with steroids: early response to therapy is the key factor. Gastroenterology 2009; 137:541–548.
- European Association for the Study of Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol 2012; 57:399–420.
- Thursz MR, Richardson P, Allison M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med 2015; 372:1619–1628.
In Reply: We thank Dr. Mirrakhimov for his interest in our article1 and for his comments on the importance of infection evaluation and treatment in patients with alcoholic hepatitis. We agree with the points he has raised and emphasized several of them in our article. We highlighted the need to evaluate for infections in these patients, as about a quarter of them are infected at the time of presentation.2
Importantly, patients with alcoholic hepatitis frequently have systemic inflammatory response syndrome criteria, which can be related to the overall inflammatory state of the disease itself or can reflect an active bacterial infection. Therefore, clinical monitoring for symptoms and signs of infection is crucial, and screening for infections is warranted on admission as well as repeatedly during the hospital stay for patients who experience clinical deterioration.3 Obtaining blood and urine cultures and performing paracentesis in patients with ascites to evaluate for bacterial peritonitis are required. Indeed, infections are a leading cause of death in patients with severe alcoholic hepatitis, both directly and indirectly by predisposing to multiorgan failure.4
Another factor to consider is the increased susceptibility to infection in these patients treated with corticosteroids. A study by Louvet et al2 showed that nonresponse to corticosteroids is the main factor contributing to the development of infection during treatment with corticosteroids, suggesting that infection is likely a consequence of the absence of improvement in liver function. More recently, results of the Steroids or Pentoxifylline for Alcoholic Hepatitis trial (which evaluated the treatment effect of prednisolone and pentoxifylline in the management of severe alcoholic hepatitis) showed that despite the higher rates of infections in patients treated with prednisolone, the mortality rates attributed to infections were similar across the treatment groups, regardless of whether prednisolone was administered.4
Finally, it is important to emphasize that criteria to initiate empiric antibiotics in patients with alcoholic hepatitis are currently lacking, and the decision to start antibiotics empirically in patients without a clear infection is largely based on the clinician’s assessment.
In Reply: We thank Dr. Mirrakhimov for his interest in our article1 and for his comments on the importance of infection evaluation and treatment in patients with alcoholic hepatitis. We agree with the points he has raised and emphasized several of them in our article. We highlighted the need to evaluate for infections in these patients, as about a quarter of them are infected at the time of presentation.2
Importantly, patients with alcoholic hepatitis frequently have systemic inflammatory response syndrome criteria, which can be related to the overall inflammatory state of the disease itself or can reflect an active bacterial infection. Therefore, clinical monitoring for symptoms and signs of infection is crucial, and screening for infections is warranted on admission as well as repeatedly during the hospital stay for patients who experience clinical deterioration.3 Obtaining blood and urine cultures and performing paracentesis in patients with ascites to evaluate for bacterial peritonitis are required. Indeed, infections are a leading cause of death in patients with severe alcoholic hepatitis, both directly and indirectly by predisposing to multiorgan failure.4
Another factor to consider is the increased susceptibility to infection in these patients treated with corticosteroids. A study by Louvet et al2 showed that nonresponse to corticosteroids is the main factor contributing to the development of infection during treatment with corticosteroids, suggesting that infection is likely a consequence of the absence of improvement in liver function. More recently, results of the Steroids or Pentoxifylline for Alcoholic Hepatitis trial (which evaluated the treatment effect of prednisolone and pentoxifylline in the management of severe alcoholic hepatitis) showed that despite the higher rates of infections in patients treated with prednisolone, the mortality rates attributed to infections were similar across the treatment groups, regardless of whether prednisolone was administered.4
Finally, it is important to emphasize that criteria to initiate empiric antibiotics in patients with alcoholic hepatitis are currently lacking, and the decision to start antibiotics empirically in patients without a clear infection is largely based on the clinician’s assessment.
- Dugum M, Zein N, McCullough A, Hanouneh I. Alcoholic hepatitis: challenges in diagnosis and management. Cleve Clin J Med 2015; 82:226–236.
- Louvet A, Wartel F, Castel H, et al. Infection in patients with severe alcoholic hepatitis treated with steroids: early response to therapy is the key factor. Gastroenterology 2009; 137:541–548.
- European Association for the Study of Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol 2012; 57:399–420.
- Thursz MR, Richardson P, Allison M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med 2015; 372:1619–1628.
- Dugum M, Zein N, McCullough A, Hanouneh I. Alcoholic hepatitis: challenges in diagnosis and management. Cleve Clin J Med 2015; 82:226–236.
- Louvet A, Wartel F, Castel H, et al. Infection in patients with severe alcoholic hepatitis treated with steroids: early response to therapy is the key factor. Gastroenterology 2009; 137:541–548.
- European Association for the Study of Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol 2012; 57:399–420.
- Thursz MR, Richardson P, Allison M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med 2015; 372:1619–1628.
Missed case of group A strep results in amputation ... More
Missed case of group A strep results in amputation of limbs
A 53-YEAR-OLD WOMAN went to the emergency department (ED) with severe abdominal pain, a rapid heartbeat, and a 101.3° F fever. After 9 hours, the ED physician discharged her around midnight with instructions to contact her gynecologist in the morning for “fibroid issues.” Later that day, the patient collapsed at home and was transported back to the hospital. She was treated for septic shock from a group A Streptococcus infection and had all 4 of her limbs amputated.
Older patients with a fever and no definite source of infection must be handled with great caution.
PLAINTIFF’S CLAIM The ED physician, who discharged the patient with a 102.9° F fever, should have spotted the infection and should have spent more time with her—given the complexity of her case. The physician should have given the patient alternative diagnoses, which would have prompted her to pursue other treatment.
THE DEFENSE The defendants denied any negligence.
VERDICT $25.3 million Wisconsin verdict.
COMMENT Although we are not given many details of this case, I suspect there was a fairly thorough work-up with no specific source of infection discovered. While this was an emergency medicine case, it is a strong reminder that older patients with a fever and no definite source of infection must be handled with great caution.
Patient dies following "routine" warfarin change
AN 80-YEAR-OLD WOMAN was taking warfarin for chronic pulmonary emboli. She saw her physician for a follow-up visit after being hospitalized for heart failure and shortness of breath. He ordered lab work, which revealed an elevated international normalized ratio (INR) of 3.7. The physician e-mailed a nurse to contact the patient and tell her to reduce her warfarin dosage. The nurse documented that she told the patient and called in a new prescription. Five days later, the patient was admitted to the hospital with a significantly elevated INR and a spinal bleed that caused paralysis. The patient was transferred to a nursing home, where she died 6 months after her initial follow-up visit.
PLANTIFF’S CLAIM The physician’s instructions were ambiguous, and a repeat INR should have been performed in 2 or 3 days. The nurse did not properly instruct the decedent and should have notified the family and the visiting nurse of the medication change.
THE DEFENSE The instructions the physician gave were correct and the appropriate plan was to repeat the INR in 13 days. The decedent had managed her warfarin through 11 previous dose changes, so there was no reason to notify the family or visiting nurse.
VERDICT $40,000 settlement.
COMMENT This case is a reminder of the difficulties one can encounter with warfarin dose adjustments. In view of the small settlement, it does not appear there was much physician liability. Most patients do not bleed with an INR of 3.7. It certainly would have been prudent to recheck in 2 to 3 days, however.
Severe headache, but no CT scan results in death
A HOSPITALIZED 57-YEAR-OLD MAN complained of a severe headache that he described as a 10 on a scale of 1 to 10. At the time, he was taking warfarin. After 6 days, he died from a brain herniation and hemorrhage.
PLAINTIFF’S CLAIM Despite the patient’s complaint of severe headache, the physician failed to order a computed tomography scan of the head.
THE DEFENSE The patient’s headaches had waxed and waned and were associated with a fever of recent onset. There were no focal neurologic deficits to suggest that there was any problem with the brain. The brain hemorrhage was a sudden and acute event.
VERDICT $250,000 Illinois verdict.
COMMENT Have a high index of suspicion for intracranial hemorrhage in patients taking warfarin with severe headache. What more needs to be said?
Missed case of group A strep results in amputation of limbs
A 53-YEAR-OLD WOMAN went to the emergency department (ED) with severe abdominal pain, a rapid heartbeat, and a 101.3° F fever. After 9 hours, the ED physician discharged her around midnight with instructions to contact her gynecologist in the morning for “fibroid issues.” Later that day, the patient collapsed at home and was transported back to the hospital. She was treated for septic shock from a group A Streptococcus infection and had all 4 of her limbs amputated.
Older patients with a fever and no definite source of infection must be handled with great caution.
PLAINTIFF’S CLAIM The ED physician, who discharged the patient with a 102.9° F fever, should have spotted the infection and should have spent more time with her—given the complexity of her case. The physician should have given the patient alternative diagnoses, which would have prompted her to pursue other treatment.
THE DEFENSE The defendants denied any negligence.
VERDICT $25.3 million Wisconsin verdict.
COMMENT Although we are not given many details of this case, I suspect there was a fairly thorough work-up with no specific source of infection discovered. While this was an emergency medicine case, it is a strong reminder that older patients with a fever and no definite source of infection must be handled with great caution.
Patient dies following "routine" warfarin change
AN 80-YEAR-OLD WOMAN was taking warfarin for chronic pulmonary emboli. She saw her physician for a follow-up visit after being hospitalized for heart failure and shortness of breath. He ordered lab work, which revealed an elevated international normalized ratio (INR) of 3.7. The physician e-mailed a nurse to contact the patient and tell her to reduce her warfarin dosage. The nurse documented that she told the patient and called in a new prescription. Five days later, the patient was admitted to the hospital with a significantly elevated INR and a spinal bleed that caused paralysis. The patient was transferred to a nursing home, where she died 6 months after her initial follow-up visit.
PLANTIFF’S CLAIM The physician’s instructions were ambiguous, and a repeat INR should have been performed in 2 or 3 days. The nurse did not properly instruct the decedent and should have notified the family and the visiting nurse of the medication change.
THE DEFENSE The instructions the physician gave were correct and the appropriate plan was to repeat the INR in 13 days. The decedent had managed her warfarin through 11 previous dose changes, so there was no reason to notify the family or visiting nurse.
VERDICT $40,000 settlement.
COMMENT This case is a reminder of the difficulties one can encounter with warfarin dose adjustments. In view of the small settlement, it does not appear there was much physician liability. Most patients do not bleed with an INR of 3.7. It certainly would have been prudent to recheck in 2 to 3 days, however.
Severe headache, but no CT scan results in death
A HOSPITALIZED 57-YEAR-OLD MAN complained of a severe headache that he described as a 10 on a scale of 1 to 10. At the time, he was taking warfarin. After 6 days, he died from a brain herniation and hemorrhage.
PLAINTIFF’S CLAIM Despite the patient’s complaint of severe headache, the physician failed to order a computed tomography scan of the head.
THE DEFENSE The patient’s headaches had waxed and waned and were associated with a fever of recent onset. There were no focal neurologic deficits to suggest that there was any problem with the brain. The brain hemorrhage was a sudden and acute event.
VERDICT $250,000 Illinois verdict.
COMMENT Have a high index of suspicion for intracranial hemorrhage in patients taking warfarin with severe headache. What more needs to be said?
Missed case of group A strep results in amputation of limbs
A 53-YEAR-OLD WOMAN went to the emergency department (ED) with severe abdominal pain, a rapid heartbeat, and a 101.3° F fever. After 9 hours, the ED physician discharged her around midnight with instructions to contact her gynecologist in the morning for “fibroid issues.” Later that day, the patient collapsed at home and was transported back to the hospital. She was treated for septic shock from a group A Streptococcus infection and had all 4 of her limbs amputated.
Older patients with a fever and no definite source of infection must be handled with great caution.
PLAINTIFF’S CLAIM The ED physician, who discharged the patient with a 102.9° F fever, should have spotted the infection and should have spent more time with her—given the complexity of her case. The physician should have given the patient alternative diagnoses, which would have prompted her to pursue other treatment.
THE DEFENSE The defendants denied any negligence.
VERDICT $25.3 million Wisconsin verdict.
COMMENT Although we are not given many details of this case, I suspect there was a fairly thorough work-up with no specific source of infection discovered. While this was an emergency medicine case, it is a strong reminder that older patients with a fever and no definite source of infection must be handled with great caution.
Patient dies following "routine" warfarin change
AN 80-YEAR-OLD WOMAN was taking warfarin for chronic pulmonary emboli. She saw her physician for a follow-up visit after being hospitalized for heart failure and shortness of breath. He ordered lab work, which revealed an elevated international normalized ratio (INR) of 3.7. The physician e-mailed a nurse to contact the patient and tell her to reduce her warfarin dosage. The nurse documented that she told the patient and called in a new prescription. Five days later, the patient was admitted to the hospital with a significantly elevated INR and a spinal bleed that caused paralysis. The patient was transferred to a nursing home, where she died 6 months after her initial follow-up visit.
PLANTIFF’S CLAIM The physician’s instructions were ambiguous, and a repeat INR should have been performed in 2 or 3 days. The nurse did not properly instruct the decedent and should have notified the family and the visiting nurse of the medication change.
THE DEFENSE The instructions the physician gave were correct and the appropriate plan was to repeat the INR in 13 days. The decedent had managed her warfarin through 11 previous dose changes, so there was no reason to notify the family or visiting nurse.
VERDICT $40,000 settlement.
COMMENT This case is a reminder of the difficulties one can encounter with warfarin dose adjustments. In view of the small settlement, it does not appear there was much physician liability. Most patients do not bleed with an INR of 3.7. It certainly would have been prudent to recheck in 2 to 3 days, however.
Severe headache, but no CT scan results in death
A HOSPITALIZED 57-YEAR-OLD MAN complained of a severe headache that he described as a 10 on a scale of 1 to 10. At the time, he was taking warfarin. After 6 days, he died from a brain herniation and hemorrhage.
PLAINTIFF’S CLAIM Despite the patient’s complaint of severe headache, the physician failed to order a computed tomography scan of the head.
THE DEFENSE The patient’s headaches had waxed and waned and were associated with a fever of recent onset. There were no focal neurologic deficits to suggest that there was any problem with the brain. The brain hemorrhage was a sudden and acute event.
VERDICT $250,000 Illinois verdict.
COMMENT Have a high index of suspicion for intracranial hemorrhage in patients taking warfarin with severe headache. What more needs to be said?
Hospitalist Consults on Psychiatric Patients Concern Nurses
I am a psychiatric nurse and am concerned about the new group of hospitalists who are taking over all the new ED patients:
- Are signing off to the nursing staff or in the electronic health record (EHR); they do not speak with the attending psychiatrist;
- Are not monitoring their own medications, including Coumadin or insulin (from what some other nurses have reported);
- Require that, if we need to speak with one, we are to call the triage hospitalist, who typically says that they can’t do anything because they didn’t start the medication and they don’t know the patient.
Many of our patients are very ill, not only psychiatrically but also medically. We feel the hospital has placed us and the patients in jeopardy. Is this typical? Do other hospitalist groups manage their patients like the ones I have described?
–Sincerely,
Psych Nurse Caught in the Middle
Dr. Hospitalist responds:
Since you mention that the “new group” of hospitalists is caring for “all the new ED patients,” I’m assuming the patients are being assigned to the hospitalist group because they are unassigned and either don’t have a primary care physician (who would direct them to a specific hospitalist) or the group is the only one in the hospital and receives all patients admitted through the ED who require admission to a hospitalist service. After all, if either you or the PCP is dissatisfied with the group and there were other groups to choose from, you would simply call another group.
I’ll address your concerns individually:
Although signing off from a consult in the EHR is fairly common, especially in busy practices, the process is usually mutually agreed upon by the clinicians involved. If the attending psychiatrist would like a call from the hospitalists before they sign off, then he or she should make that known to the group.
On most occasions, the sign-off does not occur until the hospitalist/consultant feels the patient is stable and the clinicians involved can handle “basic medical issues.” There are many patients in the hospital on insulin, Coumadin, and anti-hypertensive medications; if the hospitalist followed all of them throughout their entire hospitalization, there would be no time for the new consults. It is customary to follow patients until they are stable (e.g. the blood sugars are not markedly fluctuating and there is good sliding scale coverage, or the PT/INR [prothrombin time/international normalized ratio] has been relatively unchanged for several days). To do otherwise might also alert the CMS auditors to check the “medical necessity” for the ongoing visits.
While most large hospitalist programs have a designated triage person who receives all the calls from the ED, the other providers, and the transfer service, that person can usually answer basic patient care questions. If the person is very busy, or if the problem is more complex and the original consultant is not available, there is always someone covering for that person or the consult service to answer questions, since this is a very common occurrence.
Consults are meant to answer a specific question or assist with complex medical management issues. In order for the arrangement to work, both parties have to agree to well-defined parameters, and, at some point, there should be mutually agreed upon closure.
If no such arrangement exists, I would discuss the issue with the hospitalist director.
I am a psychiatric nurse and am concerned about the new group of hospitalists who are taking over all the new ED patients:
- Are signing off to the nursing staff or in the electronic health record (EHR); they do not speak with the attending psychiatrist;
- Are not monitoring their own medications, including Coumadin or insulin (from what some other nurses have reported);
- Require that, if we need to speak with one, we are to call the triage hospitalist, who typically says that they can’t do anything because they didn’t start the medication and they don’t know the patient.
Many of our patients are very ill, not only psychiatrically but also medically. We feel the hospital has placed us and the patients in jeopardy. Is this typical? Do other hospitalist groups manage their patients like the ones I have described?
–Sincerely,
Psych Nurse Caught in the Middle
Dr. Hospitalist responds:
Since you mention that the “new group” of hospitalists is caring for “all the new ED patients,” I’m assuming the patients are being assigned to the hospitalist group because they are unassigned and either don’t have a primary care physician (who would direct them to a specific hospitalist) or the group is the only one in the hospital and receives all patients admitted through the ED who require admission to a hospitalist service. After all, if either you or the PCP is dissatisfied with the group and there were other groups to choose from, you would simply call another group.
I’ll address your concerns individually:
Although signing off from a consult in the EHR is fairly common, especially in busy practices, the process is usually mutually agreed upon by the clinicians involved. If the attending psychiatrist would like a call from the hospitalists before they sign off, then he or she should make that known to the group.
On most occasions, the sign-off does not occur until the hospitalist/consultant feels the patient is stable and the clinicians involved can handle “basic medical issues.” There are many patients in the hospital on insulin, Coumadin, and anti-hypertensive medications; if the hospitalist followed all of them throughout their entire hospitalization, there would be no time for the new consults. It is customary to follow patients until they are stable (e.g. the blood sugars are not markedly fluctuating and there is good sliding scale coverage, or the PT/INR [prothrombin time/international normalized ratio] has been relatively unchanged for several days). To do otherwise might also alert the CMS auditors to check the “medical necessity” for the ongoing visits.
While most large hospitalist programs have a designated triage person who receives all the calls from the ED, the other providers, and the transfer service, that person can usually answer basic patient care questions. If the person is very busy, or if the problem is more complex and the original consultant is not available, there is always someone covering for that person or the consult service to answer questions, since this is a very common occurrence.
Consults are meant to answer a specific question or assist with complex medical management issues. In order for the arrangement to work, both parties have to agree to well-defined parameters, and, at some point, there should be mutually agreed upon closure.
If no such arrangement exists, I would discuss the issue with the hospitalist director.
I am a psychiatric nurse and am concerned about the new group of hospitalists who are taking over all the new ED patients:
- Are signing off to the nursing staff or in the electronic health record (EHR); they do not speak with the attending psychiatrist;
- Are not monitoring their own medications, including Coumadin or insulin (from what some other nurses have reported);
- Require that, if we need to speak with one, we are to call the triage hospitalist, who typically says that they can’t do anything because they didn’t start the medication and they don’t know the patient.
Many of our patients are very ill, not only psychiatrically but also medically. We feel the hospital has placed us and the patients in jeopardy. Is this typical? Do other hospitalist groups manage their patients like the ones I have described?
–Sincerely,
Psych Nurse Caught in the Middle
Dr. Hospitalist responds:
Since you mention that the “new group” of hospitalists is caring for “all the new ED patients,” I’m assuming the patients are being assigned to the hospitalist group because they are unassigned and either don’t have a primary care physician (who would direct them to a specific hospitalist) or the group is the only one in the hospital and receives all patients admitted through the ED who require admission to a hospitalist service. After all, if either you or the PCP is dissatisfied with the group and there were other groups to choose from, you would simply call another group.
I’ll address your concerns individually:
Although signing off from a consult in the EHR is fairly common, especially in busy practices, the process is usually mutually agreed upon by the clinicians involved. If the attending psychiatrist would like a call from the hospitalists before they sign off, then he or she should make that known to the group.
On most occasions, the sign-off does not occur until the hospitalist/consultant feels the patient is stable and the clinicians involved can handle “basic medical issues.” There are many patients in the hospital on insulin, Coumadin, and anti-hypertensive medications; if the hospitalist followed all of them throughout their entire hospitalization, there would be no time for the new consults. It is customary to follow patients until they are stable (e.g. the blood sugars are not markedly fluctuating and there is good sliding scale coverage, or the PT/INR [prothrombin time/international normalized ratio] has been relatively unchanged for several days). To do otherwise might also alert the CMS auditors to check the “medical necessity” for the ongoing visits.
While most large hospitalist programs have a designated triage person who receives all the calls from the ED, the other providers, and the transfer service, that person can usually answer basic patient care questions. If the person is very busy, or if the problem is more complex and the original consultant is not available, there is always someone covering for that person or the consult service to answer questions, since this is a very common occurrence.
Consults are meant to answer a specific question or assist with complex medical management issues. In order for the arrangement to work, both parties have to agree to well-defined parameters, and, at some point, there should be mutually agreed upon closure.
If no such arrangement exists, I would discuss the issue with the hospitalist director.
VIDEO: Rituximab-refractory indolent NHL yields to combo treatment
CHICAGO – Progression-free survival for patients with rituximab-refractory indolent non-Hodgkin’s lymphomas was effectively doubled with a combination of obinutuzumab and bendamustine, compared with bendamustine alone.
Dr. Laura Helen Sehn from the British Columbia (Canada) Cancer Agency in Vancouver, says that the study, the GADOLIN trial. “is remarkable, because it does demonstrate the first randomized evidence of a clinical benefit of a novel anti-CD20 monoclonal antibiody for patients who are rituximab refractory.”
She described the study’s key findings at the annual meeting of the American Society of Clinical Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Progression-free survival for patients with rituximab-refractory indolent non-Hodgkin’s lymphomas was effectively doubled with a combination of obinutuzumab and bendamustine, compared with bendamustine alone.
Dr. Laura Helen Sehn from the British Columbia (Canada) Cancer Agency in Vancouver, says that the study, the GADOLIN trial. “is remarkable, because it does demonstrate the first randomized evidence of a clinical benefit of a novel anti-CD20 monoclonal antibiody for patients who are rituximab refractory.”
She described the study’s key findings at the annual meeting of the American Society of Clinical Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Progression-free survival for patients with rituximab-refractory indolent non-Hodgkin’s lymphomas was effectively doubled with a combination of obinutuzumab and bendamustine, compared with bendamustine alone.
Dr. Laura Helen Sehn from the British Columbia (Canada) Cancer Agency in Vancouver, says that the study, the GADOLIN trial. “is remarkable, because it does demonstrate the first randomized evidence of a clinical benefit of a novel anti-CD20 monoclonal antibiody for patients who are rituximab refractory.”
She described the study’s key findings at the annual meeting of the American Society of Clinical Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASCO 2015
Inhibitor may fulfill unmet need in MF

© ASCO/Zach Boyden-Holmes
CHICAGO—The JAK2/FLT3 inhibitor pacritinib may fulfill an unmet need in the treatment of myelofibrosis (MF), according to a speaker at the 2015 ASCO Annual Meeting.
Results of the phase 3 PERSIST-1 trial indicate that pacritinib is safe and effective for MF patients with thrombocytopenia.
“Thrombocytopenia is a common feature in people with advanced [MF], and current treatment options have not been able to concurrently improve splenomegaly symptoms and cytopenias in these patients,” said study investigator Ruben A. Mesa, MD, of the Mayo Clinic Cancer Center in Scottsdale, Arizona.
But PERSIST-1 showed that pacritinib can accomplish this. And the drug proved more effective than best available therapy (BAT), excluding JAK inhibitors, in reducing spleen volume and alleviating MF symptoms in the entire cohort of MF patients.
Dr Mesa presented these results at ASCO as abstract LBA7006. The study was funded by CTI BioPharma Corp., the company developing pacritinib.
The trial included 327 patients who were randomized to receive pacritinib (n=220) or BAT (n=107).
Patients in the BAT arm received therapies that are routinely prescribed off-label for MF, such as erythropoietin-stimulating agents, immunomodulatory drugs, and hydroxyurea. Ruxolitinib was intentionally excluded from this trial because the study included patients with thrombocytopenia.
Dr Mesa said the patients’ baseline characteristics “demonstrate a group of individuals with advanced myelofibrosis, a heavy percentage of those with primary myelofibrosis, the vast majority having intermediate-2 or high-risk disease, with very significant splenomegaly, and the vast majority having the JAK2 mutation.”
“About half the individuals were anemic or transfusion-dependent,” he noted. “And a full third were thrombocytopenic, under 100,000 [platelets/µL], with 16% under 50,000 [platelets/µL]. This was the first phase 3 study of myelofibrosis that allowed individuals with a platelet count of less than 100,000 to be enrolled.”
Fifty-six percent of patients remained on pacritinib at the time of analysis, as did 8% of patients on BAT. Seventy-nine percent of patients crossed over from the BAT arm to the pacritinib arm.
Spleen reduction
The study’s primary endpoint was a reduction in spleen volume of 35% or greater.
In the intent-to-treat (ITT) population, 19.1% of patients in the pacritinib arm met this endpoint, as did 4.7% of patients in the BAT arm (P=0.0003). In the evaluable population—165 patients in the pacritinib arm and 85 patients in the BAT arm—the rates were 25% and 5.9%, respectively (P=0.0001).
Dr Mesa noted that pacritinib was able to reduce spleen volume in all subgroups of patients, including those with thrombocytopenia.
“Both the group [with platelet counts] under 100,000 as well as under 50,000 uniquely responded only on the pacritinib arm, with no responses on the BAT arm,” he said.
In the ITT population, 16.7% of patients with platelet counts under 100,000/µL and 22.9% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values, in the comparison with the BAT arm, were 0.0451 and 0.0086, respectively.
In the evaluable population, 23.5% of patients with platelet counts under 100,000/µL and 33.3% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values were 0.0370 and 0.0072, respectively.
“It is too early to know if pacritinib has an impact on survival, but that is clearly our expectation [based on the spleen responses observed],” Dr Mesa said.
TSS and transfusion
The study’s secondary endpoint was the proportion of patients with a 50% or greater reduction in Total Symptom Score (TSS) from baseline to week 24. TSS was measured by patient responses on the Myeloproliferative Neoplasm Symptom Assessment Form.
In the ITT population, 24.5% of pacritinib-treated patients and 6.5% of BAT-treated patients had a 50% or greater reduction in TSS score (P<0.0001). In the evaluable population, 40.9% and 9.9% of patients, respectively (P<0.0001), met this endpoint.
Dr Mesa also pointed out that 25.7% of pacritinib-treated patients who were severely anemic and transfusion-dependent—requiring at least 6 units of blood in the 90 days prior to study entry—became transfusion independent. But none of the BAT-treated patients did so (P<0.043).
Adverse events
“The most common adverse events [in the pacritinib arm] were consistent with the earlier studies,” Dr Mesa said. “Gastrointestinal toxicities were most common, although typically at low grades.”
“As expected, we saw very few individuals with any significant thrombocytopenia or anemia as drug-emergent. There were individuals who enrolled in the study as a grade 4, so some of those remained.”
The most common adverse events of any grade were diarrhea (53.2% in the pacritinib arm and 12.3% in the BAT arm), nausea (26.8% vs 6.6%), anemia (22.3% vs 19.8%), thrombocytopenia (16.8% vs 13.2%), and vomiting (15.9% vs 5.7%).
Ten percent of patients in the pacritinib arm required dose reductions due to adverse events. Diarrhea prompted dose interruptions in 13 patients and discontinuation in 3 patients. But pacritinib-associated diarrhea typically resolved in a little over a week.
“Based on these preliminary results, pacritinib may represent a very important agent for individuals with advanced disease and may have an impact on the disease course,” Dr Mesa concluded. ![]()

© ASCO/Zach Boyden-Holmes
CHICAGO—The JAK2/FLT3 inhibitor pacritinib may fulfill an unmet need in the treatment of myelofibrosis (MF), according to a speaker at the 2015 ASCO Annual Meeting.
Results of the phase 3 PERSIST-1 trial indicate that pacritinib is safe and effective for MF patients with thrombocytopenia.
“Thrombocytopenia is a common feature in people with advanced [MF], and current treatment options have not been able to concurrently improve splenomegaly symptoms and cytopenias in these patients,” said study investigator Ruben A. Mesa, MD, of the Mayo Clinic Cancer Center in Scottsdale, Arizona.
But PERSIST-1 showed that pacritinib can accomplish this. And the drug proved more effective than best available therapy (BAT), excluding JAK inhibitors, in reducing spleen volume and alleviating MF symptoms in the entire cohort of MF patients.
Dr Mesa presented these results at ASCO as abstract LBA7006. The study was funded by CTI BioPharma Corp., the company developing pacritinib.
The trial included 327 patients who were randomized to receive pacritinib (n=220) or BAT (n=107).
Patients in the BAT arm received therapies that are routinely prescribed off-label for MF, such as erythropoietin-stimulating agents, immunomodulatory drugs, and hydroxyurea. Ruxolitinib was intentionally excluded from this trial because the study included patients with thrombocytopenia.
Dr Mesa said the patients’ baseline characteristics “demonstrate a group of individuals with advanced myelofibrosis, a heavy percentage of those with primary myelofibrosis, the vast majority having intermediate-2 or high-risk disease, with very significant splenomegaly, and the vast majority having the JAK2 mutation.”
“About half the individuals were anemic or transfusion-dependent,” he noted. “And a full third were thrombocytopenic, under 100,000 [platelets/µL], with 16% under 50,000 [platelets/µL]. This was the first phase 3 study of myelofibrosis that allowed individuals with a platelet count of less than 100,000 to be enrolled.”
Fifty-six percent of patients remained on pacritinib at the time of analysis, as did 8% of patients on BAT. Seventy-nine percent of patients crossed over from the BAT arm to the pacritinib arm.
Spleen reduction
The study’s primary endpoint was a reduction in spleen volume of 35% or greater.
In the intent-to-treat (ITT) population, 19.1% of patients in the pacritinib arm met this endpoint, as did 4.7% of patients in the BAT arm (P=0.0003). In the evaluable population—165 patients in the pacritinib arm and 85 patients in the BAT arm—the rates were 25% and 5.9%, respectively (P=0.0001).
Dr Mesa noted that pacritinib was able to reduce spleen volume in all subgroups of patients, including those with thrombocytopenia.
“Both the group [with platelet counts] under 100,000 as well as under 50,000 uniquely responded only on the pacritinib arm, with no responses on the BAT arm,” he said.
In the ITT population, 16.7% of patients with platelet counts under 100,000/µL and 22.9% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values, in the comparison with the BAT arm, were 0.0451 and 0.0086, respectively.
In the evaluable population, 23.5% of patients with platelet counts under 100,000/µL and 33.3% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values were 0.0370 and 0.0072, respectively.
“It is too early to know if pacritinib has an impact on survival, but that is clearly our expectation [based on the spleen responses observed],” Dr Mesa said.
TSS and transfusion
The study’s secondary endpoint was the proportion of patients with a 50% or greater reduction in Total Symptom Score (TSS) from baseline to week 24. TSS was measured by patient responses on the Myeloproliferative Neoplasm Symptom Assessment Form.
In the ITT population, 24.5% of pacritinib-treated patients and 6.5% of BAT-treated patients had a 50% or greater reduction in TSS score (P<0.0001). In the evaluable population, 40.9% and 9.9% of patients, respectively (P<0.0001), met this endpoint.
Dr Mesa also pointed out that 25.7% of pacritinib-treated patients who were severely anemic and transfusion-dependent—requiring at least 6 units of blood in the 90 days prior to study entry—became transfusion independent. But none of the BAT-treated patients did so (P<0.043).
Adverse events
“The most common adverse events [in the pacritinib arm] were consistent with the earlier studies,” Dr Mesa said. “Gastrointestinal toxicities were most common, although typically at low grades.”
“As expected, we saw very few individuals with any significant thrombocytopenia or anemia as drug-emergent. There were individuals who enrolled in the study as a grade 4, so some of those remained.”
The most common adverse events of any grade were diarrhea (53.2% in the pacritinib arm and 12.3% in the BAT arm), nausea (26.8% vs 6.6%), anemia (22.3% vs 19.8%), thrombocytopenia (16.8% vs 13.2%), and vomiting (15.9% vs 5.7%).
Ten percent of patients in the pacritinib arm required dose reductions due to adverse events. Diarrhea prompted dose interruptions in 13 patients and discontinuation in 3 patients. But pacritinib-associated diarrhea typically resolved in a little over a week.
“Based on these preliminary results, pacritinib may represent a very important agent for individuals with advanced disease and may have an impact on the disease course,” Dr Mesa concluded. ![]()

© ASCO/Zach Boyden-Holmes
CHICAGO—The JAK2/FLT3 inhibitor pacritinib may fulfill an unmet need in the treatment of myelofibrosis (MF), according to a speaker at the 2015 ASCO Annual Meeting.
Results of the phase 3 PERSIST-1 trial indicate that pacritinib is safe and effective for MF patients with thrombocytopenia.
“Thrombocytopenia is a common feature in people with advanced [MF], and current treatment options have not been able to concurrently improve splenomegaly symptoms and cytopenias in these patients,” said study investigator Ruben A. Mesa, MD, of the Mayo Clinic Cancer Center in Scottsdale, Arizona.
But PERSIST-1 showed that pacritinib can accomplish this. And the drug proved more effective than best available therapy (BAT), excluding JAK inhibitors, in reducing spleen volume and alleviating MF symptoms in the entire cohort of MF patients.
Dr Mesa presented these results at ASCO as abstract LBA7006. The study was funded by CTI BioPharma Corp., the company developing pacritinib.
The trial included 327 patients who were randomized to receive pacritinib (n=220) or BAT (n=107).
Patients in the BAT arm received therapies that are routinely prescribed off-label for MF, such as erythropoietin-stimulating agents, immunomodulatory drugs, and hydroxyurea. Ruxolitinib was intentionally excluded from this trial because the study included patients with thrombocytopenia.
Dr Mesa said the patients’ baseline characteristics “demonstrate a group of individuals with advanced myelofibrosis, a heavy percentage of those with primary myelofibrosis, the vast majority having intermediate-2 or high-risk disease, with very significant splenomegaly, and the vast majority having the JAK2 mutation.”
“About half the individuals were anemic or transfusion-dependent,” he noted. “And a full third were thrombocytopenic, under 100,000 [platelets/µL], with 16% under 50,000 [platelets/µL]. This was the first phase 3 study of myelofibrosis that allowed individuals with a platelet count of less than 100,000 to be enrolled.”
Fifty-six percent of patients remained on pacritinib at the time of analysis, as did 8% of patients on BAT. Seventy-nine percent of patients crossed over from the BAT arm to the pacritinib arm.
Spleen reduction
The study’s primary endpoint was a reduction in spleen volume of 35% or greater.
In the intent-to-treat (ITT) population, 19.1% of patients in the pacritinib arm met this endpoint, as did 4.7% of patients in the BAT arm (P=0.0003). In the evaluable population—165 patients in the pacritinib arm and 85 patients in the BAT arm—the rates were 25% and 5.9%, respectively (P=0.0001).
Dr Mesa noted that pacritinib was able to reduce spleen volume in all subgroups of patients, including those with thrombocytopenia.
“Both the group [with platelet counts] under 100,000 as well as under 50,000 uniquely responded only on the pacritinib arm, with no responses on the BAT arm,” he said.
In the ITT population, 16.7% of patients with platelet counts under 100,000/µL and 22.9% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values, in the comparison with the BAT arm, were 0.0451 and 0.0086, respectively.
In the evaluable population, 23.5% of patients with platelet counts under 100,000/µL and 33.3% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values were 0.0370 and 0.0072, respectively.
“It is too early to know if pacritinib has an impact on survival, but that is clearly our expectation [based on the spleen responses observed],” Dr Mesa said.
TSS and transfusion
The study’s secondary endpoint was the proportion of patients with a 50% or greater reduction in Total Symptom Score (TSS) from baseline to week 24. TSS was measured by patient responses on the Myeloproliferative Neoplasm Symptom Assessment Form.
In the ITT population, 24.5% of pacritinib-treated patients and 6.5% of BAT-treated patients had a 50% or greater reduction in TSS score (P<0.0001). In the evaluable population, 40.9% and 9.9% of patients, respectively (P<0.0001), met this endpoint.
Dr Mesa also pointed out that 25.7% of pacritinib-treated patients who were severely anemic and transfusion-dependent—requiring at least 6 units of blood in the 90 days prior to study entry—became transfusion independent. But none of the BAT-treated patients did so (P<0.043).
Adverse events
“The most common adverse events [in the pacritinib arm] were consistent with the earlier studies,” Dr Mesa said. “Gastrointestinal toxicities were most common, although typically at low grades.”
“As expected, we saw very few individuals with any significant thrombocytopenia or anemia as drug-emergent. There were individuals who enrolled in the study as a grade 4, so some of those remained.”
The most common adverse events of any grade were diarrhea (53.2% in the pacritinib arm and 12.3% in the BAT arm), nausea (26.8% vs 6.6%), anemia (22.3% vs 19.8%), thrombocytopenia (16.8% vs 13.2%), and vomiting (15.9% vs 5.7%).
Ten percent of patients in the pacritinib arm required dose reductions due to adverse events. Diarrhea prompted dose interruptions in 13 patients and discontinuation in 3 patients. But pacritinib-associated diarrhea typically resolved in a little over a week.
“Based on these preliminary results, pacritinib may represent a very important agent for individuals with advanced disease and may have an impact on the disease course,” Dr Mesa concluded. ![]()
Malpractice Counsel
Hypoglycemia
A 44-year-old-man with type 1 diabetes mellitus (DM) was transported to the ED via emergency medical services (EMS) with a chief complaint of hypoglycemia. His wife stated the patient had been acting strangely prior to presentation. She further noted that after checking his blood sugar, which was 19 mg/dL, she gave her husband an oral glucose tablet with some water before calling EMS.
Upon arrival to the ED, the patient was triaged and designated as an urgent level III. At that time, he was alert and oriented, with a blood glucose level of 66 mg/dL. The patient was examined by a physician assistant (PA) within 15 minutes of his arrival. When interviewed by the PA, the patient described feelings of weakness, dizziness, and lightheadedness. The PA attributed these symptoms to the patient’s hypoglycemic state and ordered him a food tray. The patient was then observed for approximately 2 hours, during which time repeat blood-glucose testing revealed a level of 438 mg/dL. Approximately 20 minutes later, another blood-glucose test showed a level of 400 mg/dL. The patient felt well, appeared back to baseline, and expressed the desire to go home. At discharge, the PA instructed the patient to reduce his insulin by 20% and to follow up with his primary care physician (PCP) that same week.
Approximately 3 hours after discharge, the patient was found unresponsive by his wife, and EMS was again called. When EMS arrived at the patient’s house, his blood glucose level was 85 mg/dL. At presentation to the ED, the patient was unresponsive and without a pulse. Despite approximately 30 minutes of intensive resuscitative efforts, the code was called and the patient was pronounced dead.
The family sued the hospital, the emergency physician (EP), and the PA. They claimed the triage nurse failed to obtain an adequate history of the patient’s recent glucometer checks, previous hypoglycemic episodes, the amount and time of his last dose of insulin, and when and how much food he had recently ingested. The plaintiff further argued that that PA failed to obtain an electrocardiogram (ECG) to determine if the patient’s heart rhythm had been affected by his hypoglycemic state. The plaintiff also claimed the PA should have notified the patient’s PCP that the patient was in the ED, so that he could be admitted.
The defendants denied any negligence and argued the patient’s death was due to a sudden cardiac event, which was unrelated to the low-blood sugar levels. The defense contended that the patient’s enlarged heart and preexisting cardiovascular disease, hypertension, hypercholesterolemia, poorly controlled type 1 DM, history of alcohol abuse, and documented evidence of medication noncompliance were the cause of death. According to published accounts, a defense verdict was returned.
Discussion
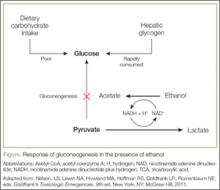
It seems that rarely a shift goes by without a patient presenting with diabetes-associated complications such as hyperglycemia or hypoglycemia. While the jury reached the correct conclusion in this case, it does serve as a reminder that cases of hypoglycemia should not be treated lightly, and the EP must attempt to determine its cause.
The most commonly accepted definition of hypoglycemia is a blood-glucose level <50 mg/dL with associated symptoms. The causes of hypoglycemia in patients treated with insulin typically involves inadequate or no food intake, or accidental administration of too much insulin or the wrong type of insulin.1
The differential diagnosis, however, needs to be more than just these two conditions. Since insulin is cleared by the kidneys, and patients with DM are at increased risk for kidney disease, acute renal failure should be considered in the differential. Other conditions to consider include infection, acute coronary syndromes, or unusual physical or mental stress.2
As with every patient presenting to the ED, patients with DM require a good history taking and physical examination. Additional testing, such as an ECG, troponin level, and kidney function test, should be performed based on the history and physical examination. Once the cause is determined, the majority of these patients can be treated with either intravenous (IV) or oral medications, observed, and discharged home with follow-up instructions.
Diabetic patients presenting with hypoglycemia due to a sulfonylurea agent or a long-acting insulin are in a completely different category. Because of the longer half-life of these agents, such patients will usually require admission to the hospital for serial glucose monitoring and treatment.2 On occasion, patients with diabetic hypoglycemia and who are on a regular form of insulin will also require hospital admission. Those at highest risk are patients with DM aged 80 years and older.1
Hyperkalemia
A 59-year-old man presented to the ED complaining of generalized weakness, the onset of which he stated had developed gradually over the previous 3 days. He denied chest pain, shortness of breath, or nausea and vomiting. His medical history was significant only for renal insufficiency. The patient was on no medications and denied alcohol or tobacco use.
On physical examination, the patient had normal vital signs, including normal pulse oximetry. Similarly, the heart, lung, and abdominal examinations were all normal. On neurological examination, the patient had 5/5 motor strength in all four extremities and exhibited a normal gait.
The EP ordered an ECG, complete blood count (CBC), basic metabolic panel, urinalysis, and a chest X-ray (CXR). Laboratory evaluation showed an elevated potassium level of 6 mEq/L. The results of the CBC, urinalysis, and CXR were all reported as normal. (Unfortunately, there was no published information on the results of the BUN, creatinine, serum bicarbonate, or ECG findings.)
Based on the patient’s elevated potassium level, the EP ordered sodium polystyrene (Kayexalate) orally and arranged for admission to the hospital. The sodium polystyrene was administered to the patient approximately 1 hour after it was ordered. While waiting for an inpatient bed, the patient experienced a cardiac arrest and died in the ED.
The family sued the EP and hospital for failure to properly respond to the patient’s elevated potassium level. The hospital denied any negligence, and the defense argued that the death was not related to any electrolyte abnormality, but was due to a respiratory arrest that led to the cardiac arrest. The defendants also maintained the sodium polystyrene had been administered in a timely manner. At trial, a defense verdict was returned.
Discussion
Hyperkalemia has been variably defined as serum potassium concentrations >5 mEq/L, >5.5 mEq/L, or >6 mEq/L.1 Symptoms of hyperkalemia include generalized muscle weakness (as seen in this patient), muscle cramps, paresthesias, nausea, vomiting, and/or diarrhea. However, it is the cardiac manifestations (eg, ventricular arrhythmias, complete heart block, asystole) associated with hyperkalemia that are most concerning.
There are numerous causes of hyperkalemia, including medications, renal failure, digitalis toxicity, and metabolic acidosis. Therefore, it is important for the EP to identify the etiology in order to definitively treat the hyperkalemia.
Traditionally, it has been taught that hyperkalemia only requires treatment if abnormalities on the ECG are noted. Classic findings seen on ECG include prolonged PR interval, peaked T waves,2 shortened QT interval, QRS widening, and a sinusoidal wave pattern. Once fictitious or hemolysis has been ruled out as the etiology, most EPs will initiate treatment above a specific threshold value (frequently 6 mEq/L),
Since it is the cardiac effects of hyperkalemia that can result in death, the initial treatment must be directed toward cardiac membrane stabilization. This is best accomplished by the administration of calcium gluconate 10% IV. This medication has a rapid onset of action (typically 1-3 minutes) and helps prevent the development of cardiac arrhythmias. Additional measures, which involve moving potassium intracellullarly, include sodium bicarbonate IV and insulin with glucose IV.
Actual removal of potassium from the body involves either the administration sodium polystyrene sulfonate or hemodialysis. Sodium polystyrene sulfonate, which is an ion-exchange resin designed to exchange sodium for potassium in the colon, can be given either orally or as an enema. Even though sodium polystyrene sulfonate has been approved for the treatment of hyperkalemia since 1958, it does not take effect for 1 to 2 hours after administration; there is also growing evidence questioning its efficacy and safety.3 In addition, sodium polystyrene sulfonate can exacerbate volume overload due to the associated increase in serum sodium. Therefore, hemodialysis is the most effective treatment for hyperkalemia, and is the treatment of choice for unstable patients with hyperkalemia and acute or chronic renal failure.
Reference - Hypoglycemia
- Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5): 678-686.
- Jalili M: Type 2 Diabetes Mellitus. In: Tintinalli JE, et al, eds. Tintinalli’s Emergency Medicine – A Comprehensive Study Guide, 7th ed. New York; McGraw Hill Medical; 2011:1419.
Reference - Hyperkalemia
- Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510-1513.
- Welch A, Maroz N, Wingo CS. Hyperkalemia: getting to the heart of the matter. Nephrol Dial Transplant. 2013;28(1):15-16.
- Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010; 21(5):73-735.
Hypoglycemia
A 44-year-old-man with type 1 diabetes mellitus (DM) was transported to the ED via emergency medical services (EMS) with a chief complaint of hypoglycemia. His wife stated the patient had been acting strangely prior to presentation. She further noted that after checking his blood sugar, which was 19 mg/dL, she gave her husband an oral glucose tablet with some water before calling EMS.
Upon arrival to the ED, the patient was triaged and designated as an urgent level III. At that time, he was alert and oriented, with a blood glucose level of 66 mg/dL. The patient was examined by a physician assistant (PA) within 15 minutes of his arrival. When interviewed by the PA, the patient described feelings of weakness, dizziness, and lightheadedness. The PA attributed these symptoms to the patient’s hypoglycemic state and ordered him a food tray. The patient was then observed for approximately 2 hours, during which time repeat blood-glucose testing revealed a level of 438 mg/dL. Approximately 20 minutes later, another blood-glucose test showed a level of 400 mg/dL. The patient felt well, appeared back to baseline, and expressed the desire to go home. At discharge, the PA instructed the patient to reduce his insulin by 20% and to follow up with his primary care physician (PCP) that same week.
Approximately 3 hours after discharge, the patient was found unresponsive by his wife, and EMS was again called. When EMS arrived at the patient’s house, his blood glucose level was 85 mg/dL. At presentation to the ED, the patient was unresponsive and without a pulse. Despite approximately 30 minutes of intensive resuscitative efforts, the code was called and the patient was pronounced dead.
The family sued the hospital, the emergency physician (EP), and the PA. They claimed the triage nurse failed to obtain an adequate history of the patient’s recent glucometer checks, previous hypoglycemic episodes, the amount and time of his last dose of insulin, and when and how much food he had recently ingested. The plaintiff further argued that that PA failed to obtain an electrocardiogram (ECG) to determine if the patient’s heart rhythm had been affected by his hypoglycemic state. The plaintiff also claimed the PA should have notified the patient’s PCP that the patient was in the ED, so that he could be admitted.
The defendants denied any negligence and argued the patient’s death was due to a sudden cardiac event, which was unrelated to the low-blood sugar levels. The defense contended that the patient’s enlarged heart and preexisting cardiovascular disease, hypertension, hypercholesterolemia, poorly controlled type 1 DM, history of alcohol abuse, and documented evidence of medication noncompliance were the cause of death. According to published accounts, a defense verdict was returned.
Discussion
It seems that rarely a shift goes by without a patient presenting with diabetes-associated complications such as hyperglycemia or hypoglycemia. While the jury reached the correct conclusion in this case, it does serve as a reminder that cases of hypoglycemia should not be treated lightly, and the EP must attempt to determine its cause.
The most commonly accepted definition of hypoglycemia is a blood-glucose level <50 mg/dL with associated symptoms. The causes of hypoglycemia in patients treated with insulin typically involves inadequate or no food intake, or accidental administration of too much insulin or the wrong type of insulin.1
The differential diagnosis, however, needs to be more than just these two conditions. Since insulin is cleared by the kidneys, and patients with DM are at increased risk for kidney disease, acute renal failure should be considered in the differential. Other conditions to consider include infection, acute coronary syndromes, or unusual physical or mental stress.2
As with every patient presenting to the ED, patients with DM require a good history taking and physical examination. Additional testing, such as an ECG, troponin level, and kidney function test, should be performed based on the history and physical examination. Once the cause is determined, the majority of these patients can be treated with either intravenous (IV) or oral medications, observed, and discharged home with follow-up instructions.
Diabetic patients presenting with hypoglycemia due to a sulfonylurea agent or a long-acting insulin are in a completely different category. Because of the longer half-life of these agents, such patients will usually require admission to the hospital for serial glucose monitoring and treatment.2 On occasion, patients with diabetic hypoglycemia and who are on a regular form of insulin will also require hospital admission. Those at highest risk are patients with DM aged 80 years and older.1
Hyperkalemia
A 59-year-old man presented to the ED complaining of generalized weakness, the onset of which he stated had developed gradually over the previous 3 days. He denied chest pain, shortness of breath, or nausea and vomiting. His medical history was significant only for renal insufficiency. The patient was on no medications and denied alcohol or tobacco use.
On physical examination, the patient had normal vital signs, including normal pulse oximetry. Similarly, the heart, lung, and abdominal examinations were all normal. On neurological examination, the patient had 5/5 motor strength in all four extremities and exhibited a normal gait.
The EP ordered an ECG, complete blood count (CBC), basic metabolic panel, urinalysis, and a chest X-ray (CXR). Laboratory evaluation showed an elevated potassium level of 6 mEq/L. The results of the CBC, urinalysis, and CXR were all reported as normal. (Unfortunately, there was no published information on the results of the BUN, creatinine, serum bicarbonate, or ECG findings.)
Based on the patient’s elevated potassium level, the EP ordered sodium polystyrene (Kayexalate) orally and arranged for admission to the hospital. The sodium polystyrene was administered to the patient approximately 1 hour after it was ordered. While waiting for an inpatient bed, the patient experienced a cardiac arrest and died in the ED.
The family sued the EP and hospital for failure to properly respond to the patient’s elevated potassium level. The hospital denied any negligence, and the defense argued that the death was not related to any electrolyte abnormality, but was due to a respiratory arrest that led to the cardiac arrest. The defendants also maintained the sodium polystyrene had been administered in a timely manner. At trial, a defense verdict was returned.
Discussion
Hyperkalemia has been variably defined as serum potassium concentrations >5 mEq/L, >5.5 mEq/L, or >6 mEq/L.1 Symptoms of hyperkalemia include generalized muscle weakness (as seen in this patient), muscle cramps, paresthesias, nausea, vomiting, and/or diarrhea. However, it is the cardiac manifestations (eg, ventricular arrhythmias, complete heart block, asystole) associated with hyperkalemia that are most concerning.
There are numerous causes of hyperkalemia, including medications, renal failure, digitalis toxicity, and metabolic acidosis. Therefore, it is important for the EP to identify the etiology in order to definitively treat the hyperkalemia.
Traditionally, it has been taught that hyperkalemia only requires treatment if abnormalities on the ECG are noted. Classic findings seen on ECG include prolonged PR interval, peaked T waves,2 shortened QT interval, QRS widening, and a sinusoidal wave pattern. Once fictitious or hemolysis has been ruled out as the etiology, most EPs will initiate treatment above a specific threshold value (frequently 6 mEq/L),
Since it is the cardiac effects of hyperkalemia that can result in death, the initial treatment must be directed toward cardiac membrane stabilization. This is best accomplished by the administration of calcium gluconate 10% IV. This medication has a rapid onset of action (typically 1-3 minutes) and helps prevent the development of cardiac arrhythmias. Additional measures, which involve moving potassium intracellullarly, include sodium bicarbonate IV and insulin with glucose IV.
Actual removal of potassium from the body involves either the administration sodium polystyrene sulfonate or hemodialysis. Sodium polystyrene sulfonate, which is an ion-exchange resin designed to exchange sodium for potassium in the colon, can be given either orally or as an enema. Even though sodium polystyrene sulfonate has been approved for the treatment of hyperkalemia since 1958, it does not take effect for 1 to 2 hours after administration; there is also growing evidence questioning its efficacy and safety.3 In addition, sodium polystyrene sulfonate can exacerbate volume overload due to the associated increase in serum sodium. Therefore, hemodialysis is the most effective treatment for hyperkalemia, and is the treatment of choice for unstable patients with hyperkalemia and acute or chronic renal failure.
Hypoglycemia
A 44-year-old-man with type 1 diabetes mellitus (DM) was transported to the ED via emergency medical services (EMS) with a chief complaint of hypoglycemia. His wife stated the patient had been acting strangely prior to presentation. She further noted that after checking his blood sugar, which was 19 mg/dL, she gave her husband an oral glucose tablet with some water before calling EMS.
Upon arrival to the ED, the patient was triaged and designated as an urgent level III. At that time, he was alert and oriented, with a blood glucose level of 66 mg/dL. The patient was examined by a physician assistant (PA) within 15 minutes of his arrival. When interviewed by the PA, the patient described feelings of weakness, dizziness, and lightheadedness. The PA attributed these symptoms to the patient’s hypoglycemic state and ordered him a food tray. The patient was then observed for approximately 2 hours, during which time repeat blood-glucose testing revealed a level of 438 mg/dL. Approximately 20 minutes later, another blood-glucose test showed a level of 400 mg/dL. The patient felt well, appeared back to baseline, and expressed the desire to go home. At discharge, the PA instructed the patient to reduce his insulin by 20% and to follow up with his primary care physician (PCP) that same week.
Approximately 3 hours after discharge, the patient was found unresponsive by his wife, and EMS was again called. When EMS arrived at the patient’s house, his blood glucose level was 85 mg/dL. At presentation to the ED, the patient was unresponsive and without a pulse. Despite approximately 30 minutes of intensive resuscitative efforts, the code was called and the patient was pronounced dead.
The family sued the hospital, the emergency physician (EP), and the PA. They claimed the triage nurse failed to obtain an adequate history of the patient’s recent glucometer checks, previous hypoglycemic episodes, the amount and time of his last dose of insulin, and when and how much food he had recently ingested. The plaintiff further argued that that PA failed to obtain an electrocardiogram (ECG) to determine if the patient’s heart rhythm had been affected by his hypoglycemic state. The plaintiff also claimed the PA should have notified the patient’s PCP that the patient was in the ED, so that he could be admitted.
The defendants denied any negligence and argued the patient’s death was due to a sudden cardiac event, which was unrelated to the low-blood sugar levels. The defense contended that the patient’s enlarged heart and preexisting cardiovascular disease, hypertension, hypercholesterolemia, poorly controlled type 1 DM, history of alcohol abuse, and documented evidence of medication noncompliance were the cause of death. According to published accounts, a defense verdict was returned.
Discussion
It seems that rarely a shift goes by without a patient presenting with diabetes-associated complications such as hyperglycemia or hypoglycemia. While the jury reached the correct conclusion in this case, it does serve as a reminder that cases of hypoglycemia should not be treated lightly, and the EP must attempt to determine its cause.
The most commonly accepted definition of hypoglycemia is a blood-glucose level <50 mg/dL with associated symptoms. The causes of hypoglycemia in patients treated with insulin typically involves inadequate or no food intake, or accidental administration of too much insulin or the wrong type of insulin.1
The differential diagnosis, however, needs to be more than just these two conditions. Since insulin is cleared by the kidneys, and patients with DM are at increased risk for kidney disease, acute renal failure should be considered in the differential. Other conditions to consider include infection, acute coronary syndromes, or unusual physical or mental stress.2
As with every patient presenting to the ED, patients with DM require a good history taking and physical examination. Additional testing, such as an ECG, troponin level, and kidney function test, should be performed based on the history and physical examination. Once the cause is determined, the majority of these patients can be treated with either intravenous (IV) or oral medications, observed, and discharged home with follow-up instructions.
Diabetic patients presenting with hypoglycemia due to a sulfonylurea agent or a long-acting insulin are in a completely different category. Because of the longer half-life of these agents, such patients will usually require admission to the hospital for serial glucose monitoring and treatment.2 On occasion, patients with diabetic hypoglycemia and who are on a regular form of insulin will also require hospital admission. Those at highest risk are patients with DM aged 80 years and older.1
Hyperkalemia
A 59-year-old man presented to the ED complaining of generalized weakness, the onset of which he stated had developed gradually over the previous 3 days. He denied chest pain, shortness of breath, or nausea and vomiting. His medical history was significant only for renal insufficiency. The patient was on no medications and denied alcohol or tobacco use.
On physical examination, the patient had normal vital signs, including normal pulse oximetry. Similarly, the heart, lung, and abdominal examinations were all normal. On neurological examination, the patient had 5/5 motor strength in all four extremities and exhibited a normal gait.
The EP ordered an ECG, complete blood count (CBC), basic metabolic panel, urinalysis, and a chest X-ray (CXR). Laboratory evaluation showed an elevated potassium level of 6 mEq/L. The results of the CBC, urinalysis, and CXR were all reported as normal. (Unfortunately, there was no published information on the results of the BUN, creatinine, serum bicarbonate, or ECG findings.)
Based on the patient’s elevated potassium level, the EP ordered sodium polystyrene (Kayexalate) orally and arranged for admission to the hospital. The sodium polystyrene was administered to the patient approximately 1 hour after it was ordered. While waiting for an inpatient bed, the patient experienced a cardiac arrest and died in the ED.
The family sued the EP and hospital for failure to properly respond to the patient’s elevated potassium level. The hospital denied any negligence, and the defense argued that the death was not related to any electrolyte abnormality, but was due to a respiratory arrest that led to the cardiac arrest. The defendants also maintained the sodium polystyrene had been administered in a timely manner. At trial, a defense verdict was returned.
Discussion
Hyperkalemia has been variably defined as serum potassium concentrations >5 mEq/L, >5.5 mEq/L, or >6 mEq/L.1 Symptoms of hyperkalemia include generalized muscle weakness (as seen in this patient), muscle cramps, paresthesias, nausea, vomiting, and/or diarrhea. However, it is the cardiac manifestations (eg, ventricular arrhythmias, complete heart block, asystole) associated with hyperkalemia that are most concerning.
There are numerous causes of hyperkalemia, including medications, renal failure, digitalis toxicity, and metabolic acidosis. Therefore, it is important for the EP to identify the etiology in order to definitively treat the hyperkalemia.
Traditionally, it has been taught that hyperkalemia only requires treatment if abnormalities on the ECG are noted. Classic findings seen on ECG include prolonged PR interval, peaked T waves,2 shortened QT interval, QRS widening, and a sinusoidal wave pattern. Once fictitious or hemolysis has been ruled out as the etiology, most EPs will initiate treatment above a specific threshold value (frequently 6 mEq/L),
Since it is the cardiac effects of hyperkalemia that can result in death, the initial treatment must be directed toward cardiac membrane stabilization. This is best accomplished by the administration of calcium gluconate 10% IV. This medication has a rapid onset of action (typically 1-3 minutes) and helps prevent the development of cardiac arrhythmias. Additional measures, which involve moving potassium intracellullarly, include sodium bicarbonate IV and insulin with glucose IV.
Actual removal of potassium from the body involves either the administration sodium polystyrene sulfonate or hemodialysis. Sodium polystyrene sulfonate, which is an ion-exchange resin designed to exchange sodium for potassium in the colon, can be given either orally or as an enema. Even though sodium polystyrene sulfonate has been approved for the treatment of hyperkalemia since 1958, it does not take effect for 1 to 2 hours after administration; there is also growing evidence questioning its efficacy and safety.3 In addition, sodium polystyrene sulfonate can exacerbate volume overload due to the associated increase in serum sodium. Therefore, hemodialysis is the most effective treatment for hyperkalemia, and is the treatment of choice for unstable patients with hyperkalemia and acute or chronic renal failure.
Reference - Hypoglycemia
- Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5): 678-686.
- Jalili M: Type 2 Diabetes Mellitus. In: Tintinalli JE, et al, eds. Tintinalli’s Emergency Medicine – A Comprehensive Study Guide, 7th ed. New York; McGraw Hill Medical; 2011:1419.
Reference - Hyperkalemia
- Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510-1513.
- Welch A, Maroz N, Wingo CS. Hyperkalemia: getting to the heart of the matter. Nephrol Dial Transplant. 2013;28(1):15-16.
- Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010; 21(5):73-735.
Reference - Hypoglycemia
- Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174(5): 678-686.
- Jalili M: Type 2 Diabetes Mellitus. In: Tintinalli JE, et al, eds. Tintinalli’s Emergency Medicine – A Comprehensive Study Guide, 7th ed. New York; McGraw Hill Medical; 2011:1419.
Reference - Hyperkalemia
- Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510-1513.
- Welch A, Maroz N, Wingo CS. Hyperkalemia: getting to the heart of the matter. Nephrol Dial Transplant. 2013;28(1):15-16.
- Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective? J Am Soc Nephrol. 2010; 21(5):73-735.
Case Studies in Toxicology: Babies and Booze—Pediatric Considerations in the Management of Ethanol Intoxication
Case
A previously healthy 4-month-old girl was brought into the ED for concerns of alcohol ingestion. Reportedly, the infant’s father reconstituted 4 ounces of powdered formula using what he thought was water from an unmarked bottle in his refrigerator. He later realized that the bottle contained rum, although he still let the child finish the 4 ounces of formula in the hopes that she would vomit—which did not occur.
Upon arrival to the ED, the infant’s vital signs were: blood pressure, 100/61 mm Hg; heart rate, 155 beats/minute; respiratory rate, 36 breaths/minute; and temperature, normal. Oxygen saturation was 98% on room air. A rapid bedside blood glucose test was 89 mg/dL. The infant’s physical examination was unremarkable. She appeared active but hungry, had a strong cry, and had a developmentally appropriate gross neurological examination.
How does ethanol exposure in children typically occur?
Recent reports from the American Association of Poison Control Centers’ National Poison Data System demonstrate that ethanol exposures comprise 1% to 3% of total exposures in children aged ≤5 years.
The most common sources are ethanol-containing beverages, mouthwash, and cologne/perfume.1 Ethanol can also be found as a solvent for certain pediatric liquid medications (eg, ranitidine) or in flavor extracts (eg, vanilla extract, orange extract). Any clear alcohol (eg, vodka, gin, rum) stored in an accessible site, such as a refrigerator, may be mistaken for water. In many reports, a caregiver unintentionally used the alcohol to reconstitute formula; however, intentional provision of alcohol to toddlers, usually as a sedative, is a recurring concern.2
What are the clinical concerns in children with ethanol intoxication?
Under usual conditions, a normal serum glucose concentration is maintained from ingested carbohydrates and via glycogenolysis of hepatic glycogen stores. Such glycogen reserves can sustain normal blood glucose concentrations for several hours in adults but for a shorter period in children. Once glycogen is depleted, as is common after an overnight fast, glucose can be generated through gluconeogenesis.
However, in the presence of ethanol (Figure), the excessive reducing potential (ie, NADH) that results from ethanol metabolism shunts pyruvate away from the gluconeogenic pathway (toward lactate), inhibiting glucose production. Unlike adults, children and infants, who have relatively low glycogen reserves, are at significant risk for hypoglycemia following ethanol exposure. This represents the largest contributor to morbidity and mortality of children with ethanol intoxication.3 Patients with hypoglycemia can have a highly variable clinical presentation including agitation, seizures, focality, or coma.4
Case Continuation
Intravenous (IV) access was obtained, and the patient was placed on a dextrose-containing fluid at 1.5 times the maintenance flow rate. Pertinent laboratory studies revealed a serum glucose level of 90 mg/dL, normal electrolyte panel, and an initial blood alcohol concentration of 337 mg/dL (approximately 30 minutes postingestion).
How do children with ethanol intoxication present?
While there is some variation in clinical effects among nontolerant adults, acute ethanol intoxication with a serum concentration >250 mg/dL is frequently associated with stupor, respiratory depression, and hypotension. A concentration >400 mg/dL may be associated with coma or apnea. Although similar clinical effects are expected in adolescents and children, infants often have counterintuitive clinical findings.
To date, eight cases of significant infant ethanol exposure exist in the literature (age range, 29 days to 9 months; ethanol concentration, 183-524 mg/dL). Respiratory depression was absent in all cases.5-9 In all but two cases, the neurological examination revealed only subtle decreases in interaction or tone. The remaining two children were described as obtunded and flaccid (ethanol levels, 405 mg/dL and 524 mg/dL, respectively) and were intubated for airway protection despite normal respiratory rates.7,10
The incongruence between the clinical findings (both the neurological examination and respiratory effects) and the ethanol concentration is difficult to explain. It may be due to age-related neurological immaturity or a limited ability to perform the required detailed neurological examinations in children. In particular, the relatively preserved level of consciousness, despite an otherwise coma-inducing ethanol concentration, is unique to infants. Accordingly, there should be a low threshold to check ethanol concentrations in infants presenting with apparent life-threatening events, altered mental status, decreased tone, or unexplained hypoglycemia or hypothermia.
What is the estimated time to sobriety in infants?
Ethanol is eliminated via a hepatic enzymatic oxidation pathway that becomes saturated at low serum levels. In nontolerant adults, this results in a zero-order kinetic elimination pattern with an ethanol elimination rate of approximately 20 mg/dL per hour. Anecdotally, it had been thought that children clear ethanol at roughly double this rate via unclear mechanisms. However, a review of published kinetic data suggests the actual rate of clearance may not differ substantially from adults (range, 19-34 mg/dL per hour).5-7,10,11
Case Conclusion
The patient was transferred to a tertiary care pediatric hospital for continued management, where the markedly elevated serum ethanol concentration was confirmed. She was maintained on a dextrose-containing IV fluid and observed overnight without development of any complications. Serial serum ethanol concentrations were performed and complete clearance was achieved approximately 20 hours postingestion, suggesting a metabolic rate of 16 mg/dL per hour. The infant was discharged home with supervision by child protective services.
Dr Boroughf is a toxicology fellow, department of emergency medicine, Albert Einstein Medical Center, Philadelphia, Pennsylvania. Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at the New York University School of Medicine and the New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board. Dr Henretig is an attending toxicologist, department of emergency medicine, Children’s Hospital of Philadelphia, Pennsylvania.
- Mowry JB, Spyker DA, Cantilena LR Jr, Bailey JE, Ford M. 2012 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. Clin Toxicol (Phila). 2013;51(10):949-1229.
- Wood JN, Pecker LH, Russo ME, Henretig F, Christian CW. Evaluation and referral for child maltreatment in pediatric poisoning victims. Child Abuse Negl. 2012;36(4):362-369.
- Lamminpää A. Alcohol intoxication in childhood and adolescence. Alcohol Alcohol. 1995;30(1):5-12.
- Malouf R, Brust JC. Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol.1985;17(5):421-430.
- Chikava K, Lower DR, Frangiskakis SH, Sepulveda JL, Virji MA, Rao KN. Acute ethanol intoxication in a 7-month old-infant. Pediatr Dev Pathol. 2004;7(4):400-402.
- Ford JB, Wayment MT, Albertson TE, Owen KP, Radke JB, Sutter ME. Elimination kinetics of ethanol in a 5-week-old infant and a literature review of infant ethanol pharmacokinetics. Case Rep Med. 2013;2013:250716. doi:10.1155/2013/250716
- McCormick T, Levine M, Knox O, Claudius I. Ethanol ingestion in two infants under 2 months old: a previously unreported cause of ALTE. Pediatrics. 2013;131(2);e604-e607.
- Fong HF, Muller AA. An unexpected clinical course in a 29-day-old infant with ethanol exposure. Pediatr Emerg Care. 2014;30(2):111-113.
- Iyer SS, Haupt A, Henretig FM. Pick your poison: straight from the spring? Ped Emerg Care. 2009;25(3):194-196.
- Edmunds SM, Ajizian SJ, Liguori A. Acute obtundation in a 9-month-old patient: ethanol ingestion. Pediatr Emerg Care. 2014;30(10):739-741.
- Simon HK, Cox JM, Sucov A, Linakis JG. Serum ethanol clearance in intoxicated children and adolescents presenting to the ED. Acad Emerg Med. 1994;1(6):520-524.
Case
A previously healthy 4-month-old girl was brought into the ED for concerns of alcohol ingestion. Reportedly, the infant’s father reconstituted 4 ounces of powdered formula using what he thought was water from an unmarked bottle in his refrigerator. He later realized that the bottle contained rum, although he still let the child finish the 4 ounces of formula in the hopes that she would vomit—which did not occur.
Upon arrival to the ED, the infant’s vital signs were: blood pressure, 100/61 mm Hg; heart rate, 155 beats/minute; respiratory rate, 36 breaths/minute; and temperature, normal. Oxygen saturation was 98% on room air. A rapid bedside blood glucose test was 89 mg/dL. The infant’s physical examination was unremarkable. She appeared active but hungry, had a strong cry, and had a developmentally appropriate gross neurological examination.
How does ethanol exposure in children typically occur?
Recent reports from the American Association of Poison Control Centers’ National Poison Data System demonstrate that ethanol exposures comprise 1% to 3% of total exposures in children aged ≤5 years.
The most common sources are ethanol-containing beverages, mouthwash, and cologne/perfume.1 Ethanol can also be found as a solvent for certain pediatric liquid medications (eg, ranitidine) or in flavor extracts (eg, vanilla extract, orange extract). Any clear alcohol (eg, vodka, gin, rum) stored in an accessible site, such as a refrigerator, may be mistaken for water. In many reports, a caregiver unintentionally used the alcohol to reconstitute formula; however, intentional provision of alcohol to toddlers, usually as a sedative, is a recurring concern.2
What are the clinical concerns in children with ethanol intoxication?
Under usual conditions, a normal serum glucose concentration is maintained from ingested carbohydrates and via glycogenolysis of hepatic glycogen stores. Such glycogen reserves can sustain normal blood glucose concentrations for several hours in adults but for a shorter period in children. Once glycogen is depleted, as is common after an overnight fast, glucose can be generated through gluconeogenesis.
However, in the presence of ethanol (Figure), the excessive reducing potential (ie, NADH) that results from ethanol metabolism shunts pyruvate away from the gluconeogenic pathway (toward lactate), inhibiting glucose production. Unlike adults, children and infants, who have relatively low glycogen reserves, are at significant risk for hypoglycemia following ethanol exposure. This represents the largest contributor to morbidity and mortality of children with ethanol intoxication.3 Patients with hypoglycemia can have a highly variable clinical presentation including agitation, seizures, focality, or coma.4
Case Continuation
Intravenous (IV) access was obtained, and the patient was placed on a dextrose-containing fluid at 1.5 times the maintenance flow rate. Pertinent laboratory studies revealed a serum glucose level of 90 mg/dL, normal electrolyte panel, and an initial blood alcohol concentration of 337 mg/dL (approximately 30 minutes postingestion).
How do children with ethanol intoxication present?
While there is some variation in clinical effects among nontolerant adults, acute ethanol intoxication with a serum concentration >250 mg/dL is frequently associated with stupor, respiratory depression, and hypotension. A concentration >400 mg/dL may be associated with coma or apnea. Although similar clinical effects are expected in adolescents and children, infants often have counterintuitive clinical findings.
To date, eight cases of significant infant ethanol exposure exist in the literature (age range, 29 days to 9 months; ethanol concentration, 183-524 mg/dL). Respiratory depression was absent in all cases.5-9 In all but two cases, the neurological examination revealed only subtle decreases in interaction or tone. The remaining two children were described as obtunded and flaccid (ethanol levels, 405 mg/dL and 524 mg/dL, respectively) and were intubated for airway protection despite normal respiratory rates.7,10
The incongruence between the clinical findings (both the neurological examination and respiratory effects) and the ethanol concentration is difficult to explain. It may be due to age-related neurological immaturity or a limited ability to perform the required detailed neurological examinations in children. In particular, the relatively preserved level of consciousness, despite an otherwise coma-inducing ethanol concentration, is unique to infants. Accordingly, there should be a low threshold to check ethanol concentrations in infants presenting with apparent life-threatening events, altered mental status, decreased tone, or unexplained hypoglycemia or hypothermia.
What is the estimated time to sobriety in infants?
Ethanol is eliminated via a hepatic enzymatic oxidation pathway that becomes saturated at low serum levels. In nontolerant adults, this results in a zero-order kinetic elimination pattern with an ethanol elimination rate of approximately 20 mg/dL per hour. Anecdotally, it had been thought that children clear ethanol at roughly double this rate via unclear mechanisms. However, a review of published kinetic data suggests the actual rate of clearance may not differ substantially from adults (range, 19-34 mg/dL per hour).5-7,10,11
Case Conclusion
The patient was transferred to a tertiary care pediatric hospital for continued management, where the markedly elevated serum ethanol concentration was confirmed. She was maintained on a dextrose-containing IV fluid and observed overnight without development of any complications. Serial serum ethanol concentrations were performed and complete clearance was achieved approximately 20 hours postingestion, suggesting a metabolic rate of 16 mg/dL per hour. The infant was discharged home with supervision by child protective services.
Dr Boroughf is a toxicology fellow, department of emergency medicine, Albert Einstein Medical Center, Philadelphia, Pennsylvania. Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at the New York University School of Medicine and the New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board. Dr Henretig is an attending toxicologist, department of emergency medicine, Children’s Hospital of Philadelphia, Pennsylvania.
Case
A previously healthy 4-month-old girl was brought into the ED for concerns of alcohol ingestion. Reportedly, the infant’s father reconstituted 4 ounces of powdered formula using what he thought was water from an unmarked bottle in his refrigerator. He later realized that the bottle contained rum, although he still let the child finish the 4 ounces of formula in the hopes that she would vomit—which did not occur.
Upon arrival to the ED, the infant’s vital signs were: blood pressure, 100/61 mm Hg; heart rate, 155 beats/minute; respiratory rate, 36 breaths/minute; and temperature, normal. Oxygen saturation was 98% on room air. A rapid bedside blood glucose test was 89 mg/dL. The infant’s physical examination was unremarkable. She appeared active but hungry, had a strong cry, and had a developmentally appropriate gross neurological examination.
How does ethanol exposure in children typically occur?
Recent reports from the American Association of Poison Control Centers’ National Poison Data System demonstrate that ethanol exposures comprise 1% to 3% of total exposures in children aged ≤5 years.
The most common sources are ethanol-containing beverages, mouthwash, and cologne/perfume.1 Ethanol can also be found as a solvent for certain pediatric liquid medications (eg, ranitidine) or in flavor extracts (eg, vanilla extract, orange extract). Any clear alcohol (eg, vodka, gin, rum) stored in an accessible site, such as a refrigerator, may be mistaken for water. In many reports, a caregiver unintentionally used the alcohol to reconstitute formula; however, intentional provision of alcohol to toddlers, usually as a sedative, is a recurring concern.2
What are the clinical concerns in children with ethanol intoxication?
Under usual conditions, a normal serum glucose concentration is maintained from ingested carbohydrates and via glycogenolysis of hepatic glycogen stores. Such glycogen reserves can sustain normal blood glucose concentrations for several hours in adults but for a shorter period in children. Once glycogen is depleted, as is common after an overnight fast, glucose can be generated through gluconeogenesis.
However, in the presence of ethanol (Figure), the excessive reducing potential (ie, NADH) that results from ethanol metabolism shunts pyruvate away from the gluconeogenic pathway (toward lactate), inhibiting glucose production. Unlike adults, children and infants, who have relatively low glycogen reserves, are at significant risk for hypoglycemia following ethanol exposure. This represents the largest contributor to morbidity and mortality of children with ethanol intoxication.3 Patients with hypoglycemia can have a highly variable clinical presentation including agitation, seizures, focality, or coma.4
Case Continuation
Intravenous (IV) access was obtained, and the patient was placed on a dextrose-containing fluid at 1.5 times the maintenance flow rate. Pertinent laboratory studies revealed a serum glucose level of 90 mg/dL, normal electrolyte panel, and an initial blood alcohol concentration of 337 mg/dL (approximately 30 minutes postingestion).
How do children with ethanol intoxication present?
While there is some variation in clinical effects among nontolerant adults, acute ethanol intoxication with a serum concentration >250 mg/dL is frequently associated with stupor, respiratory depression, and hypotension. A concentration >400 mg/dL may be associated with coma or apnea. Although similar clinical effects are expected in adolescents and children, infants often have counterintuitive clinical findings.
To date, eight cases of significant infant ethanol exposure exist in the literature (age range, 29 days to 9 months; ethanol concentration, 183-524 mg/dL). Respiratory depression was absent in all cases.5-9 In all but two cases, the neurological examination revealed only subtle decreases in interaction or tone. The remaining two children were described as obtunded and flaccid (ethanol levels, 405 mg/dL and 524 mg/dL, respectively) and were intubated for airway protection despite normal respiratory rates.7,10
The incongruence between the clinical findings (both the neurological examination and respiratory effects) and the ethanol concentration is difficult to explain. It may be due to age-related neurological immaturity or a limited ability to perform the required detailed neurological examinations in children. In particular, the relatively preserved level of consciousness, despite an otherwise coma-inducing ethanol concentration, is unique to infants. Accordingly, there should be a low threshold to check ethanol concentrations in infants presenting with apparent life-threatening events, altered mental status, decreased tone, or unexplained hypoglycemia or hypothermia.
What is the estimated time to sobriety in infants?
Ethanol is eliminated via a hepatic enzymatic oxidation pathway that becomes saturated at low serum levels. In nontolerant adults, this results in a zero-order kinetic elimination pattern with an ethanol elimination rate of approximately 20 mg/dL per hour. Anecdotally, it had been thought that children clear ethanol at roughly double this rate via unclear mechanisms. However, a review of published kinetic data suggests the actual rate of clearance may not differ substantially from adults (range, 19-34 mg/dL per hour).5-7,10,11
Case Conclusion
The patient was transferred to a tertiary care pediatric hospital for continued management, where the markedly elevated serum ethanol concentration was confirmed. She was maintained on a dextrose-containing IV fluid and observed overnight without development of any complications. Serial serum ethanol concentrations were performed and complete clearance was achieved approximately 20 hours postingestion, suggesting a metabolic rate of 16 mg/dL per hour. The infant was discharged home with supervision by child protective services.
Dr Boroughf is a toxicology fellow, department of emergency medicine, Albert Einstein Medical Center, Philadelphia, Pennsylvania. Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at the New York University School of Medicine and the New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board. Dr Henretig is an attending toxicologist, department of emergency medicine, Children’s Hospital of Philadelphia, Pennsylvania.
- Mowry JB, Spyker DA, Cantilena LR Jr, Bailey JE, Ford M. 2012 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. Clin Toxicol (Phila). 2013;51(10):949-1229.
- Wood JN, Pecker LH, Russo ME, Henretig F, Christian CW. Evaluation and referral for child maltreatment in pediatric poisoning victims. Child Abuse Negl. 2012;36(4):362-369.
- Lamminpää A. Alcohol intoxication in childhood and adolescence. Alcohol Alcohol. 1995;30(1):5-12.
- Malouf R, Brust JC. Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol.1985;17(5):421-430.
- Chikava K, Lower DR, Frangiskakis SH, Sepulveda JL, Virji MA, Rao KN. Acute ethanol intoxication in a 7-month old-infant. Pediatr Dev Pathol. 2004;7(4):400-402.
- Ford JB, Wayment MT, Albertson TE, Owen KP, Radke JB, Sutter ME. Elimination kinetics of ethanol in a 5-week-old infant and a literature review of infant ethanol pharmacokinetics. Case Rep Med. 2013;2013:250716. doi:10.1155/2013/250716
- McCormick T, Levine M, Knox O, Claudius I. Ethanol ingestion in two infants under 2 months old: a previously unreported cause of ALTE. Pediatrics. 2013;131(2);e604-e607.
- Fong HF, Muller AA. An unexpected clinical course in a 29-day-old infant with ethanol exposure. Pediatr Emerg Care. 2014;30(2):111-113.
- Iyer SS, Haupt A, Henretig FM. Pick your poison: straight from the spring? Ped Emerg Care. 2009;25(3):194-196.
- Edmunds SM, Ajizian SJ, Liguori A. Acute obtundation in a 9-month-old patient: ethanol ingestion. Pediatr Emerg Care. 2014;30(10):739-741.
- Simon HK, Cox JM, Sucov A, Linakis JG. Serum ethanol clearance in intoxicated children and adolescents presenting to the ED. Acad Emerg Med. 1994;1(6):520-524.
- Mowry JB, Spyker DA, Cantilena LR Jr, Bailey JE, Ford M. 2012 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. Clin Toxicol (Phila). 2013;51(10):949-1229.
- Wood JN, Pecker LH, Russo ME, Henretig F, Christian CW. Evaluation and referral for child maltreatment in pediatric poisoning victims. Child Abuse Negl. 2012;36(4):362-369.
- Lamminpää A. Alcohol intoxication in childhood and adolescence. Alcohol Alcohol. 1995;30(1):5-12.
- Malouf R, Brust JC. Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol.1985;17(5):421-430.
- Chikava K, Lower DR, Frangiskakis SH, Sepulveda JL, Virji MA, Rao KN. Acute ethanol intoxication in a 7-month old-infant. Pediatr Dev Pathol. 2004;7(4):400-402.
- Ford JB, Wayment MT, Albertson TE, Owen KP, Radke JB, Sutter ME. Elimination kinetics of ethanol in a 5-week-old infant and a literature review of infant ethanol pharmacokinetics. Case Rep Med. 2013;2013:250716. doi:10.1155/2013/250716
- McCormick T, Levine M, Knox O, Claudius I. Ethanol ingestion in two infants under 2 months old: a previously unreported cause of ALTE. Pediatrics. 2013;131(2);e604-e607.
- Fong HF, Muller AA. An unexpected clinical course in a 29-day-old infant with ethanol exposure. Pediatr Emerg Care. 2014;30(2):111-113.
- Iyer SS, Haupt A, Henretig FM. Pick your poison: straight from the spring? Ped Emerg Care. 2009;25(3):194-196.
- Edmunds SM, Ajizian SJ, Liguori A. Acute obtundation in a 9-month-old patient: ethanol ingestion. Pediatr Emerg Care. 2014;30(10):739-741.
- Simon HK, Cox JM, Sucov A, Linakis JG. Serum ethanol clearance in intoxicated children and adolescents presenting to the ED. Acad Emerg Med. 1994;1(6):520-524.