User login
Clarion Call
A specialty without a disease: It was a major hangup for the field of hospital medicine in the early days. We’d hurdled many of the traditional barriers to specialty status—research fellowships, textbooks, an active society, a growing body of research, and thousands of practitioners focusing their practice on the hospital setting. However, despite several examples of site-defined specialties like emergency and critical-care medicine, cynics clung to the time-honored need for a specialty to own an organ, or at least a disease.
Early SHM efforts made a strong push to make VTE our disease—both its treatment and, more importantly, its prevention. It was a laudable effort, one that has saved many thousands of lives and limbs. It made sense for hospitalists to tackle VTE; it’s an incapacitating disease that affects many, is largely preventable, and had no strong inpatient advocate. While hematologists were the obvious “owner” of this disease, they were neither available nor able to redesign the inpatient systems of care necessary to thwart this illness. Hospitalists, invested in this issue by consequence of direct care of many at-risk patients and through commitment to improving hospital systems, came to own VTE prevention.
The Next Frontier: Stroke
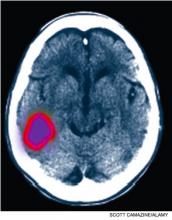
It is time hospitalists apply this experience to the management of an even more incapacitating, largely preventable disease looking for an inpatient steward: stroke. A stroke occurs in the U.S. every 40 seconds, with disabling sequelae that often are avoidable with rapid detection and treatment. This is especially true when we are given the clarion call of a transient ischemic attack (TIA). The problem is that most American hospitals are not kingpins of efficiency—the key ingredient of the processes necessary to improve stroke outcomes. Furthermore, while our neurologic colleagues are the obvious group to lead the deployment of stroke QI programs, there just aren’t enough of them to do so.
Hospitalists provide a significant amount of neurologic care. One study notes that TIA and stroke were among the most commonly cared-for diseases by hospitalists.1 This places us in a prime position to take the lead and own this disease in collaboration with our neurology colleagues. Just as with reliable VTE prevention, the key to effective stroke care requires effective systems engineering in conjunction with disease-specific expertise.
Rapid Care for Acute Medical Crisis
EDs are equipped with stroke pathways to efficiently evaluate, triage, scan, and intervene for patients who present with stroke symptoms. While most hospitals have a long way to go to perfect these systems, some hospitals—mostly in large, urban centers—have achieved the appropriate level of ED efficiency. These hospitals are recognized by The Joint Commission accreditation as stroke centers. As a result, patients who present to these hospitals with stroke symptoms often receive thrombolytics—a disease- and life-altering therapy—within the appropriate, but very limited, time window for benefit.
But what happens if that same patient develops those same signs and symptoms in the hospital? Will they get the same level of efficient evaluation, triage, scanning, and intervention that occurs in the ED? This is more than an academic question. Fifteen percent of all strokes are heralded by transient neurologic deficits, so many of the estimated 300,000 annual TIA patients are admitted to the hospital. What’s the reason for the admission? To facilitate the diagnostic workup, monitor for stroke symptoms and apply timely interventions should this occur.
But are we equipped to provide this kind of timely care in the hospital?
Case Study
Let’s take a 70-year-old diabetic male who presents with 45 minutes of aphasia and right-side arm weakness that resolve prior to presentation to the ED. If the patient is hypertensive on admission, the ABCD tool would suggest that he has a risk of stroke that approximates 20% in 90 days.2 Importantly, nearly half of that risk is in the first 48 hours. In other words, he has about a 10% risk of having a stroke in the next two days. Thus, we rightly admit him for monitoring in order to react quickly to any new signs and symptoms.
The problem is that most hospitals don’t have a system to efficiently manage patients who develop new stroke symptoms in the hospital. Does your hospital have an inpatient stroke pathway? That is, for a patient who has stroke onset while already in the hospital:
- Are the nurses aware of stroke signs and symptoms?
- Do nurses have a phone number to call to initiate an evaluation?
- Is there a team with stroke expertise immediately available to respond to those calls?
- Is there a priority path to get the patient promptly transported to the CT scanner for brain imaging with immediate radiology interpretation?
- How fast can thrombolytics be delivered, and is there an inpatient neurologist available 24/7 to assist?
The goal is 25 minutes from first recognition of symptoms to CT scan, and 60 minutes to complete evaluation and commencement of treatment. What percentage of your inpatient units could meet that goal? Could they do it any day of the week, at any time of the day or night?
ED systems had to be developed and implemented to ensure that appropriate candidates receive thrombolytic therapy in a timely manner. If those systems are not in place outside your hospital’s ED, then inpatient stroke cases are likely to miss the window of opportunity for thrombolytics. Ironically, they might have been better off going home and coming to the ED with any new symptoms. As a hospitalist, that is a sobering thought.
Hospitalist Ownership
It takes more than hospitalists being on-site to improve stroke outcomes. Processes need to be sharpened, roles defined, and outcomes monitored and acted upon to further sharpen the process. All of this plays to the strengths of hospitalists and should be undertaken with the vigor afforded to VTE prevention. This will take recognition that there’s a problem with the system, a dedication of resources, and a commitment to relentlessly work to improve and streamline the processes of stroke care.
In other words, it takes ownership. TH
Dr. Glasheen is associate professor of medicine and director of the hospital medicine group and hospitalist training program at the University of Colorado Denver. Ethan Cumbler, MD, contributed to this article. Dr. Cumbler is assistant professor of medicine at UC Denver and a member of the university’s Hospital Stroke Council.
This column represents the opinions of the author and is not intended to reflect an official position of SHM.
References
- Glasheen JJ, Epstein KR, Siegal E, Kutner J, Prochazka AV. The spectrum of community-based hospitalist practice: a call to tailor internal medicine residency training. Arch Intern Med. 2007;167(7):727-728.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292.
A specialty without a disease: It was a major hangup for the field of hospital medicine in the early days. We’d hurdled many of the traditional barriers to specialty status—research fellowships, textbooks, an active society, a growing body of research, and thousands of practitioners focusing their practice on the hospital setting. However, despite several examples of site-defined specialties like emergency and critical-care medicine, cynics clung to the time-honored need for a specialty to own an organ, or at least a disease.
Early SHM efforts made a strong push to make VTE our disease—both its treatment and, more importantly, its prevention. It was a laudable effort, one that has saved many thousands of lives and limbs. It made sense for hospitalists to tackle VTE; it’s an incapacitating disease that affects many, is largely preventable, and had no strong inpatient advocate. While hematologists were the obvious “owner” of this disease, they were neither available nor able to redesign the inpatient systems of care necessary to thwart this illness. Hospitalists, invested in this issue by consequence of direct care of many at-risk patients and through commitment to improving hospital systems, came to own VTE prevention.
The Next Frontier: Stroke
It is time hospitalists apply this experience to the management of an even more incapacitating, largely preventable disease looking for an inpatient steward: stroke. A stroke occurs in the U.S. every 40 seconds, with disabling sequelae that often are avoidable with rapid detection and treatment. This is especially true when we are given the clarion call of a transient ischemic attack (TIA). The problem is that most American hospitals are not kingpins of efficiency—the key ingredient of the processes necessary to improve stroke outcomes. Furthermore, while our neurologic colleagues are the obvious group to lead the deployment of stroke QI programs, there just aren’t enough of them to do so.
Hospitalists provide a significant amount of neurologic care. One study notes that TIA and stroke were among the most commonly cared-for diseases by hospitalists.1 This places us in a prime position to take the lead and own this disease in collaboration with our neurology colleagues. Just as with reliable VTE prevention, the key to effective stroke care requires effective systems engineering in conjunction with disease-specific expertise.
Rapid Care for Acute Medical Crisis
EDs are equipped with stroke pathways to efficiently evaluate, triage, scan, and intervene for patients who present with stroke symptoms. While most hospitals have a long way to go to perfect these systems, some hospitals—mostly in large, urban centers—have achieved the appropriate level of ED efficiency. These hospitals are recognized by The Joint Commission accreditation as stroke centers. As a result, patients who present to these hospitals with stroke symptoms often receive thrombolytics—a disease- and life-altering therapy—within the appropriate, but very limited, time window for benefit.
But what happens if that same patient develops those same signs and symptoms in the hospital? Will they get the same level of efficient evaluation, triage, scanning, and intervention that occurs in the ED? This is more than an academic question. Fifteen percent of all strokes are heralded by transient neurologic deficits, so many of the estimated 300,000 annual TIA patients are admitted to the hospital. What’s the reason for the admission? To facilitate the diagnostic workup, monitor for stroke symptoms and apply timely interventions should this occur.
But are we equipped to provide this kind of timely care in the hospital?
Case Study
Let’s take a 70-year-old diabetic male who presents with 45 minutes of aphasia and right-side arm weakness that resolve prior to presentation to the ED. If the patient is hypertensive on admission, the ABCD tool would suggest that he has a risk of stroke that approximates 20% in 90 days.2 Importantly, nearly half of that risk is in the first 48 hours. In other words, he has about a 10% risk of having a stroke in the next two days. Thus, we rightly admit him for monitoring in order to react quickly to any new signs and symptoms.
The problem is that most hospitals don’t have a system to efficiently manage patients who develop new stroke symptoms in the hospital. Does your hospital have an inpatient stroke pathway? That is, for a patient who has stroke onset while already in the hospital:
- Are the nurses aware of stroke signs and symptoms?
- Do nurses have a phone number to call to initiate an evaluation?
- Is there a team with stroke expertise immediately available to respond to those calls?
- Is there a priority path to get the patient promptly transported to the CT scanner for brain imaging with immediate radiology interpretation?
- How fast can thrombolytics be delivered, and is there an inpatient neurologist available 24/7 to assist?
The goal is 25 minutes from first recognition of symptoms to CT scan, and 60 minutes to complete evaluation and commencement of treatment. What percentage of your inpatient units could meet that goal? Could they do it any day of the week, at any time of the day or night?
ED systems had to be developed and implemented to ensure that appropriate candidates receive thrombolytic therapy in a timely manner. If those systems are not in place outside your hospital’s ED, then inpatient stroke cases are likely to miss the window of opportunity for thrombolytics. Ironically, they might have been better off going home and coming to the ED with any new symptoms. As a hospitalist, that is a sobering thought.
Hospitalist Ownership
It takes more than hospitalists being on-site to improve stroke outcomes. Processes need to be sharpened, roles defined, and outcomes monitored and acted upon to further sharpen the process. All of this plays to the strengths of hospitalists and should be undertaken with the vigor afforded to VTE prevention. This will take recognition that there’s a problem with the system, a dedication of resources, and a commitment to relentlessly work to improve and streamline the processes of stroke care.
In other words, it takes ownership. TH
Dr. Glasheen is associate professor of medicine and director of the hospital medicine group and hospitalist training program at the University of Colorado Denver. Ethan Cumbler, MD, contributed to this article. Dr. Cumbler is assistant professor of medicine at UC Denver and a member of the university’s Hospital Stroke Council.
This column represents the opinions of the author and is not intended to reflect an official position of SHM.
References
- Glasheen JJ, Epstein KR, Siegal E, Kutner J, Prochazka AV. The spectrum of community-based hospitalist practice: a call to tailor internal medicine residency training. Arch Intern Med. 2007;167(7):727-728.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292.
A specialty without a disease: It was a major hangup for the field of hospital medicine in the early days. We’d hurdled many of the traditional barriers to specialty status—research fellowships, textbooks, an active society, a growing body of research, and thousands of practitioners focusing their practice on the hospital setting. However, despite several examples of site-defined specialties like emergency and critical-care medicine, cynics clung to the time-honored need for a specialty to own an organ, or at least a disease.
Early SHM efforts made a strong push to make VTE our disease—both its treatment and, more importantly, its prevention. It was a laudable effort, one that has saved many thousands of lives and limbs. It made sense for hospitalists to tackle VTE; it’s an incapacitating disease that affects many, is largely preventable, and had no strong inpatient advocate. While hematologists were the obvious “owner” of this disease, they were neither available nor able to redesign the inpatient systems of care necessary to thwart this illness. Hospitalists, invested in this issue by consequence of direct care of many at-risk patients and through commitment to improving hospital systems, came to own VTE prevention.
The Next Frontier: Stroke
It is time hospitalists apply this experience to the management of an even more incapacitating, largely preventable disease looking for an inpatient steward: stroke. A stroke occurs in the U.S. every 40 seconds, with disabling sequelae that often are avoidable with rapid detection and treatment. This is especially true when we are given the clarion call of a transient ischemic attack (TIA). The problem is that most American hospitals are not kingpins of efficiency—the key ingredient of the processes necessary to improve stroke outcomes. Furthermore, while our neurologic colleagues are the obvious group to lead the deployment of stroke QI programs, there just aren’t enough of them to do so.
Hospitalists provide a significant amount of neurologic care. One study notes that TIA and stroke were among the most commonly cared-for diseases by hospitalists.1 This places us in a prime position to take the lead and own this disease in collaboration with our neurology colleagues. Just as with reliable VTE prevention, the key to effective stroke care requires effective systems engineering in conjunction with disease-specific expertise.
Rapid Care for Acute Medical Crisis
EDs are equipped with stroke pathways to efficiently evaluate, triage, scan, and intervene for patients who present with stroke symptoms. While most hospitals have a long way to go to perfect these systems, some hospitals—mostly in large, urban centers—have achieved the appropriate level of ED efficiency. These hospitals are recognized by The Joint Commission accreditation as stroke centers. As a result, patients who present to these hospitals with stroke symptoms often receive thrombolytics—a disease- and life-altering therapy—within the appropriate, but very limited, time window for benefit.
But what happens if that same patient develops those same signs and symptoms in the hospital? Will they get the same level of efficient evaluation, triage, scanning, and intervention that occurs in the ED? This is more than an academic question. Fifteen percent of all strokes are heralded by transient neurologic deficits, so many of the estimated 300,000 annual TIA patients are admitted to the hospital. What’s the reason for the admission? To facilitate the diagnostic workup, monitor for stroke symptoms and apply timely interventions should this occur.
But are we equipped to provide this kind of timely care in the hospital?
Case Study
Let’s take a 70-year-old diabetic male who presents with 45 minutes of aphasia and right-side arm weakness that resolve prior to presentation to the ED. If the patient is hypertensive on admission, the ABCD tool would suggest that he has a risk of stroke that approximates 20% in 90 days.2 Importantly, nearly half of that risk is in the first 48 hours. In other words, he has about a 10% risk of having a stroke in the next two days. Thus, we rightly admit him for monitoring in order to react quickly to any new signs and symptoms.
The problem is that most hospitals don’t have a system to efficiently manage patients who develop new stroke symptoms in the hospital. Does your hospital have an inpatient stroke pathway? That is, for a patient who has stroke onset while already in the hospital:
- Are the nurses aware of stroke signs and symptoms?
- Do nurses have a phone number to call to initiate an evaluation?
- Is there a team with stroke expertise immediately available to respond to those calls?
- Is there a priority path to get the patient promptly transported to the CT scanner for brain imaging with immediate radiology interpretation?
- How fast can thrombolytics be delivered, and is there an inpatient neurologist available 24/7 to assist?
The goal is 25 minutes from first recognition of symptoms to CT scan, and 60 minutes to complete evaluation and commencement of treatment. What percentage of your inpatient units could meet that goal? Could they do it any day of the week, at any time of the day or night?
ED systems had to be developed and implemented to ensure that appropriate candidates receive thrombolytic therapy in a timely manner. If those systems are not in place outside your hospital’s ED, then inpatient stroke cases are likely to miss the window of opportunity for thrombolytics. Ironically, they might have been better off going home and coming to the ED with any new symptoms. As a hospitalist, that is a sobering thought.
Hospitalist Ownership
It takes more than hospitalists being on-site to improve stroke outcomes. Processes need to be sharpened, roles defined, and outcomes monitored and acted upon to further sharpen the process. All of this plays to the strengths of hospitalists and should be undertaken with the vigor afforded to VTE prevention. This will take recognition that there’s a problem with the system, a dedication of resources, and a commitment to relentlessly work to improve and streamline the processes of stroke care.
In other words, it takes ownership. TH
Dr. Glasheen is associate professor of medicine and director of the hospital medicine group and hospitalist training program at the University of Colorado Denver. Ethan Cumbler, MD, contributed to this article. Dr. Cumbler is assistant professor of medicine at UC Denver and a member of the university’s Hospital Stroke Council.
This column represents the opinions of the author and is not intended to reflect an official position of SHM.
References
- Glasheen JJ, Epstein KR, Siegal E, Kutner J, Prochazka AV. The spectrum of community-based hospitalist practice: a call to tailor internal medicine residency training. Arch Intern Med. 2007;167(7):727-728.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283-292.
Bundling Bedlam
Even if you receive your salary as an employee of your hospital or hospitalist group, you should keep a close eye on discussions taking place in Washington about reshaping the way hospital care is paid for. It seems that every 10 to 20 years, a seismic tremor starts on Capitol Hill and fundamentally shakes up the way healthcare is funded. It starts with Medicare, then quickly is adopted by private insurers; it not only changes the distribution of dollars, but the new incentives also drive the way medicine is practiced.
In the 1960s, change began with President Johnson and the development of Medicare and Medicaid. It was the first time specific populations—seniors and the poor—were “entitled” to healthcare coverage. In essence, Johnson created the largest “insurance company” in the country, and it became the tail that wagged the dog.
In the 1970s, President Nixon pushed through support for HMOs, and capitation and managed care spread well beyond the Kaisers of the world. This system incentivized controlling costs, because the total amount was capped, while maintaining an acceptable level of quality. For the first time, doing more did not generate more money.
In the 1980s, diagnosis-related groups (DRGs) changed Medicare payments to hospitals from cost-plus billings to a bundled fee for an episode of care. This motivated hospitals to work with their physicians—sometimes driven by protocols and case managers—to efficiently manage resources and length of stay (LOS). Between capitation, case rates, and DRGs, hospitals have had to refashion themselves to be leaner and more efficient.
Today, with national thought leaders like John Wennberg and Elliot Fisher at Dartmouth and Brent James at Intermountain revealing the many variations in the way healthcare is practiced—and throwing around statistics like “40% of healthcare is wasteful”—it is no wonder that as President Obama and Congress look to add 47 million uninsured persons to the system and try to reduce variation and increase accountabilities, there is every indication that radical changes will be made to the payment system.
One of these newfangled approaches is the bundling of payment for an episode of care to include both the facility charges (e.g., hospital care) and the professional charges (e.g., physician care). Bundling can be a good thing or a worrisome approach, depending on where you sit in this dialogue and how bundling is actually implemented.
Background on Bundling
The motivation of the government—and, by extension, all insurers—is that efforts to control what they pay per unit for a visit, a procedure, or even an entire hospitalization has not curbed costs or led to a satisfactory level of performance. With respect to hospitalized patients, Obama has stated that he wants to eliminate waste by reducing unnecessary readmissions to the tune of $6.8 billion annually. Furthermore, Medicare officials want to look for strategies that either keep people out of the ED post-discharge or at least eliminate Medicare’s need to pay for this care, which they feel is unnecessary and avoidable.
By bundling payment for a specific admission (e.g., decompensated heart failure or pneumonia) and including the facility and professional-care fees, both during hospitalization and for a period of time (e.g., 30 days post-discharge) and providing incentives for best performance, the insurer (i.e., Medicare) can hand off responsibility to the hospitals and the doctors to figure it all out. There is nothing like the accountability of knowing “this is all you are going to get,” or “if you want more, you have to meet these standards,” to motivate professionals to reshape their system to improve their discharge process, engage the outpatient physicians, and do the job right the first time. This can play to HM’s strengths, and SHM already has started developing and implementing change in the discharge process through Project BOOST (Better Outcomes for Older Adults through Safe Transitions, www.hospitalmedicine.org/boost).
Potential Problems
One key concern is not knowing who—or what—will control the dollars once Medicare sets the bundled payment. Right now, hospitals receive the DRG payment and physicians bill for their own professional services. In the future, will all the money flow to the hospital? How will these dollars be distributed? Who determines who will be awarded performance bonuses?
In California and other states with significant managed-care populations and large medical groups, there is real-life experience with setting up efficient physician-hospital organizations (PHOs) to solve these issues. Some take the form of independent physician associations (IPAs), which represent the physicians in PHOs. There is no reason PHOs cannot be developed to administrate these bundled funds, and hospitalists, who are seeing an increasing number of hospitalized patients on medicine and surgery, should be key leaders in such PHO arrangements.
But HM is not a monolith in this discussion. The diversity in how HM groups are organized, their relationship with their hospitals, and how hospitalists or their groups receive funding can, and will, influence the group’s perspective on this issue. Hospitalist groups that are independent from their hospitals, or those that rely on referrals from primary-care physicians (PCPs) or the ED, might be justifiably concerned about all of “their” money having to flow through the hospital. Hospitalists who are employed by a hospital might be concerned that they will need to develop new metrics to justify their salaries and bonuses. HM groups that contract with the hospital might be concerned that a change in the flow of funding from Medicare to the hospital might make their contractual arrangements more difficult.
For those who battle with hospital administration over hospital support of their HM group, they might find bundling alleviates the need for the current use of Part A dollars to support hospitalists, because the new bundling of Part A (current payments for hospital facility charges) and Part B (current payment for physicians’ professional services) can allow for a more professional discussion, based on the value hospitalists bring. The need for subsidies or support could diminish or vanish.
Change Is Coming
No matter your perspective or viewpoint, one reality is coming into focus: This president and this Congress will make sweeping changes, and it appears from our conversations with Sen. Max Baucus (D-Mont.), chair of the powerful Senate Finance Committee (see “Medicine’s Change Agent,” May 2009, p. 18), that bundling and value-based purchasing will be part of healthcare reform.
With this in mind, SHM’s Public Policy Committee is actively engaged in trying to shape bundling in a way that fits emerging changes in the care of hospitalized patients. We want a system that works for the way healthcare will be practiced in the future, not a Band-Aid on the system of the past. This is very important stuff. Hospitalists will be affected by reform because so many of our patients are on Medicare and our compensation is generated by patient care in the hospital.
SHM has created an easy-to-use, Web-based system to send a message to members of Congress through a partnership with Capwiz. Visit www.hospitalmedicine.org/beheard to get started.
While the uncertainty of healthcare reform and, more specifically, payment reform is at times frightening, mainly because it is so sweeping and at this point so undefined, HM has been forged in the cauldron of change and ambiguity. Hospitalists are positioned as well as any health professionals to seize the opportunities that a new system will provide. And SHM will do its part to help shape the new reality and assist our members in creating successful strategies in this new environment. TH
Dr. Wellikson is CEO of SHM.
Even if you receive your salary as an employee of your hospital or hospitalist group, you should keep a close eye on discussions taking place in Washington about reshaping the way hospital care is paid for. It seems that every 10 to 20 years, a seismic tremor starts on Capitol Hill and fundamentally shakes up the way healthcare is funded. It starts with Medicare, then quickly is adopted by private insurers; it not only changes the distribution of dollars, but the new incentives also drive the way medicine is practiced.
In the 1960s, change began with President Johnson and the development of Medicare and Medicaid. It was the first time specific populations—seniors and the poor—were “entitled” to healthcare coverage. In essence, Johnson created the largest “insurance company” in the country, and it became the tail that wagged the dog.
In the 1970s, President Nixon pushed through support for HMOs, and capitation and managed care spread well beyond the Kaisers of the world. This system incentivized controlling costs, because the total amount was capped, while maintaining an acceptable level of quality. For the first time, doing more did not generate more money.
In the 1980s, diagnosis-related groups (DRGs) changed Medicare payments to hospitals from cost-plus billings to a bundled fee for an episode of care. This motivated hospitals to work with their physicians—sometimes driven by protocols and case managers—to efficiently manage resources and length of stay (LOS). Between capitation, case rates, and DRGs, hospitals have had to refashion themselves to be leaner and more efficient.
Today, with national thought leaders like John Wennberg and Elliot Fisher at Dartmouth and Brent James at Intermountain revealing the many variations in the way healthcare is practiced—and throwing around statistics like “40% of healthcare is wasteful”—it is no wonder that as President Obama and Congress look to add 47 million uninsured persons to the system and try to reduce variation and increase accountabilities, there is every indication that radical changes will be made to the payment system.
One of these newfangled approaches is the bundling of payment for an episode of care to include both the facility charges (e.g., hospital care) and the professional charges (e.g., physician care). Bundling can be a good thing or a worrisome approach, depending on where you sit in this dialogue and how bundling is actually implemented.
Background on Bundling
The motivation of the government—and, by extension, all insurers—is that efforts to control what they pay per unit for a visit, a procedure, or even an entire hospitalization has not curbed costs or led to a satisfactory level of performance. With respect to hospitalized patients, Obama has stated that he wants to eliminate waste by reducing unnecessary readmissions to the tune of $6.8 billion annually. Furthermore, Medicare officials want to look for strategies that either keep people out of the ED post-discharge or at least eliminate Medicare’s need to pay for this care, which they feel is unnecessary and avoidable.
By bundling payment for a specific admission (e.g., decompensated heart failure or pneumonia) and including the facility and professional-care fees, both during hospitalization and for a period of time (e.g., 30 days post-discharge) and providing incentives for best performance, the insurer (i.e., Medicare) can hand off responsibility to the hospitals and the doctors to figure it all out. There is nothing like the accountability of knowing “this is all you are going to get,” or “if you want more, you have to meet these standards,” to motivate professionals to reshape their system to improve their discharge process, engage the outpatient physicians, and do the job right the first time. This can play to HM’s strengths, and SHM already has started developing and implementing change in the discharge process through Project BOOST (Better Outcomes for Older Adults through Safe Transitions, www.hospitalmedicine.org/boost).
Potential Problems
One key concern is not knowing who—or what—will control the dollars once Medicare sets the bundled payment. Right now, hospitals receive the DRG payment and physicians bill for their own professional services. In the future, will all the money flow to the hospital? How will these dollars be distributed? Who determines who will be awarded performance bonuses?
In California and other states with significant managed-care populations and large medical groups, there is real-life experience with setting up efficient physician-hospital organizations (PHOs) to solve these issues. Some take the form of independent physician associations (IPAs), which represent the physicians in PHOs. There is no reason PHOs cannot be developed to administrate these bundled funds, and hospitalists, who are seeing an increasing number of hospitalized patients on medicine and surgery, should be key leaders in such PHO arrangements.
But HM is not a monolith in this discussion. The diversity in how HM groups are organized, their relationship with their hospitals, and how hospitalists or their groups receive funding can, and will, influence the group’s perspective on this issue. Hospitalist groups that are independent from their hospitals, or those that rely on referrals from primary-care physicians (PCPs) or the ED, might be justifiably concerned about all of “their” money having to flow through the hospital. Hospitalists who are employed by a hospital might be concerned that they will need to develop new metrics to justify their salaries and bonuses. HM groups that contract with the hospital might be concerned that a change in the flow of funding from Medicare to the hospital might make their contractual arrangements more difficult.
For those who battle with hospital administration over hospital support of their HM group, they might find bundling alleviates the need for the current use of Part A dollars to support hospitalists, because the new bundling of Part A (current payments for hospital facility charges) and Part B (current payment for physicians’ professional services) can allow for a more professional discussion, based on the value hospitalists bring. The need for subsidies or support could diminish or vanish.
Change Is Coming
No matter your perspective or viewpoint, one reality is coming into focus: This president and this Congress will make sweeping changes, and it appears from our conversations with Sen. Max Baucus (D-Mont.), chair of the powerful Senate Finance Committee (see “Medicine’s Change Agent,” May 2009, p. 18), that bundling and value-based purchasing will be part of healthcare reform.
With this in mind, SHM’s Public Policy Committee is actively engaged in trying to shape bundling in a way that fits emerging changes in the care of hospitalized patients. We want a system that works for the way healthcare will be practiced in the future, not a Band-Aid on the system of the past. This is very important stuff. Hospitalists will be affected by reform because so many of our patients are on Medicare and our compensation is generated by patient care in the hospital.
SHM has created an easy-to-use, Web-based system to send a message to members of Congress through a partnership with Capwiz. Visit www.hospitalmedicine.org/beheard to get started.
While the uncertainty of healthcare reform and, more specifically, payment reform is at times frightening, mainly because it is so sweeping and at this point so undefined, HM has been forged in the cauldron of change and ambiguity. Hospitalists are positioned as well as any health professionals to seize the opportunities that a new system will provide. And SHM will do its part to help shape the new reality and assist our members in creating successful strategies in this new environment. TH
Dr. Wellikson is CEO of SHM.
Even if you receive your salary as an employee of your hospital or hospitalist group, you should keep a close eye on discussions taking place in Washington about reshaping the way hospital care is paid for. It seems that every 10 to 20 years, a seismic tremor starts on Capitol Hill and fundamentally shakes up the way healthcare is funded. It starts with Medicare, then quickly is adopted by private insurers; it not only changes the distribution of dollars, but the new incentives also drive the way medicine is practiced.
In the 1960s, change began with President Johnson and the development of Medicare and Medicaid. It was the first time specific populations—seniors and the poor—were “entitled” to healthcare coverage. In essence, Johnson created the largest “insurance company” in the country, and it became the tail that wagged the dog.
In the 1970s, President Nixon pushed through support for HMOs, and capitation and managed care spread well beyond the Kaisers of the world. This system incentivized controlling costs, because the total amount was capped, while maintaining an acceptable level of quality. For the first time, doing more did not generate more money.
In the 1980s, diagnosis-related groups (DRGs) changed Medicare payments to hospitals from cost-plus billings to a bundled fee for an episode of care. This motivated hospitals to work with their physicians—sometimes driven by protocols and case managers—to efficiently manage resources and length of stay (LOS). Between capitation, case rates, and DRGs, hospitals have had to refashion themselves to be leaner and more efficient.
Today, with national thought leaders like John Wennberg and Elliot Fisher at Dartmouth and Brent James at Intermountain revealing the many variations in the way healthcare is practiced—and throwing around statistics like “40% of healthcare is wasteful”—it is no wonder that as President Obama and Congress look to add 47 million uninsured persons to the system and try to reduce variation and increase accountabilities, there is every indication that radical changes will be made to the payment system.
One of these newfangled approaches is the bundling of payment for an episode of care to include both the facility charges (e.g., hospital care) and the professional charges (e.g., physician care). Bundling can be a good thing or a worrisome approach, depending on where you sit in this dialogue and how bundling is actually implemented.
Background on Bundling
The motivation of the government—and, by extension, all insurers—is that efforts to control what they pay per unit for a visit, a procedure, or even an entire hospitalization has not curbed costs or led to a satisfactory level of performance. With respect to hospitalized patients, Obama has stated that he wants to eliminate waste by reducing unnecessary readmissions to the tune of $6.8 billion annually. Furthermore, Medicare officials want to look for strategies that either keep people out of the ED post-discharge or at least eliminate Medicare’s need to pay for this care, which they feel is unnecessary and avoidable.
By bundling payment for a specific admission (e.g., decompensated heart failure or pneumonia) and including the facility and professional-care fees, both during hospitalization and for a period of time (e.g., 30 days post-discharge) and providing incentives for best performance, the insurer (i.e., Medicare) can hand off responsibility to the hospitals and the doctors to figure it all out. There is nothing like the accountability of knowing “this is all you are going to get,” or “if you want more, you have to meet these standards,” to motivate professionals to reshape their system to improve their discharge process, engage the outpatient physicians, and do the job right the first time. This can play to HM’s strengths, and SHM already has started developing and implementing change in the discharge process through Project BOOST (Better Outcomes for Older Adults through Safe Transitions, www.hospitalmedicine.org/boost).
Potential Problems
One key concern is not knowing who—or what—will control the dollars once Medicare sets the bundled payment. Right now, hospitals receive the DRG payment and physicians bill for their own professional services. In the future, will all the money flow to the hospital? How will these dollars be distributed? Who determines who will be awarded performance bonuses?
In California and other states with significant managed-care populations and large medical groups, there is real-life experience with setting up efficient physician-hospital organizations (PHOs) to solve these issues. Some take the form of independent physician associations (IPAs), which represent the physicians in PHOs. There is no reason PHOs cannot be developed to administrate these bundled funds, and hospitalists, who are seeing an increasing number of hospitalized patients on medicine and surgery, should be key leaders in such PHO arrangements.
But HM is not a monolith in this discussion. The diversity in how HM groups are organized, their relationship with their hospitals, and how hospitalists or their groups receive funding can, and will, influence the group’s perspective on this issue. Hospitalist groups that are independent from their hospitals, or those that rely on referrals from primary-care physicians (PCPs) or the ED, might be justifiably concerned about all of “their” money having to flow through the hospital. Hospitalists who are employed by a hospital might be concerned that they will need to develop new metrics to justify their salaries and bonuses. HM groups that contract with the hospital might be concerned that a change in the flow of funding from Medicare to the hospital might make their contractual arrangements more difficult.
For those who battle with hospital administration over hospital support of their HM group, they might find bundling alleviates the need for the current use of Part A dollars to support hospitalists, because the new bundling of Part A (current payments for hospital facility charges) and Part B (current payment for physicians’ professional services) can allow for a more professional discussion, based on the value hospitalists bring. The need for subsidies or support could diminish or vanish.
Change Is Coming
No matter your perspective or viewpoint, one reality is coming into focus: This president and this Congress will make sweeping changes, and it appears from our conversations with Sen. Max Baucus (D-Mont.), chair of the powerful Senate Finance Committee (see “Medicine’s Change Agent,” May 2009, p. 18), that bundling and value-based purchasing will be part of healthcare reform.
With this in mind, SHM’s Public Policy Committee is actively engaged in trying to shape bundling in a way that fits emerging changes in the care of hospitalized patients. We want a system that works for the way healthcare will be practiced in the future, not a Band-Aid on the system of the past. This is very important stuff. Hospitalists will be affected by reform because so many of our patients are on Medicare and our compensation is generated by patient care in the hospital.
SHM has created an easy-to-use, Web-based system to send a message to members of Congress through a partnership with Capwiz. Visit www.hospitalmedicine.org/beheard to get started.
While the uncertainty of healthcare reform and, more specifically, payment reform is at times frightening, mainly because it is so sweeping and at this point so undefined, HM has been forged in the cauldron of change and ambiguity. Hospitalists are positioned as well as any health professionals to seize the opportunities that a new system will provide. And SHM will do its part to help shape the new reality and assist our members in creating successful strategies in this new environment. TH
Dr. Wellikson is CEO of SHM.
Grassroots Mentorship
Indu Michael remembers the one-page medical field survey she filled out around this time last year. A pre-med student at the University of California at Los Angeles, she provided the correct job descriptions for surgeons, pediatricians, OB/GYNs, psychiatrists, and internal medicine physicians. Only one medical specialty stumped her.
“I had no idea what a hospitalist did,” says Michael, 21, a senior.
The anonymous survey was part of the application and interview process for the Undergraduate Preceptorship in Internal Medicine (UPIM), a program that was launched last summer at UCLA Medical Center. By the time Michael finished the three-week program in early September, she had a complete understanding of what hospitalists do. She also says she’s leaning toward an internal medicine (IM) career—and might become a hospitalist.
“I’m seriously thinking [Hem-Onc] may not be the direction I want to take,” Michael says. “I realized oncologists are mainly consultative doctors and it’s really the general medicine team that does the medicine.”
Those kind of comments are music to Nasim Afsar-manesh’s ear. Dr. Afsar-manesh, a hospitalist and assistant clinical professor at UCLA, developed the UPIM program from scratch as a way to expose pre-med undergrads to internal medicine. The ultimate goal, of course, is steering them toward an internist career. She is well aware of medical students’ declining interest in IM, and she believes outreach to undergrads and first-year medical students will help reverse the trend.
“Undergraduates are like sponges,” Dr. Afsar-manesh says. “They are so genuinely excited about the possibilities of getting to do this stuff. … You can appeal to their idealism.” She created the program because “the general field of medicine has become so complex that students who are thinking about making it a career don’t have a good chance to see what the day-to-day practicing of medicine is like.”
HM Test Drive
Michael was one of seven students in the inaugural UPIM session. The program is open to UCLA undergrads who volunteer at least 80 hours at the medical center and pre-med students at the California Institute of Technology, where Dr. Afsar-manesh received her undergraduate degree. Seventeen students applied for the first session; the seven who were selected were chosen based on their motivation, maturity, and enthusiasm for medicine. The plan is simple: UPIM aims to offer an early spark of excitement that will stay with students and serve as positive reinforcement as they proceed through medical school and confront the challenges of an IM career.
UPIM participants were integrated into teams of attendings, residents, and medical school students, and they spent time on hospital units and subspecialty consult services. The undergrads observed residents in their patient evaluations, daily rounds, and discussions with patient families. They witnessed a number of procedures, including central-line placement and bone-marrow biopsies. Although the attendings and residents weren’t required to teach the undergrads, many volunteered a significant amount of their time, Dr. Afsar-manesh says. Some of the students spent night shifts at the hospital.
“The students felt they had participated in something special. They felt the experience had overshadowed anything they had previously done,” says Dr. Afsar-manesh, a member of SHM’s Young Physicians Committee. “I think it’s a program that can really quickly grow.”
Every Friday, undergrads participated in a teaching session, during which they had to present a medically, socially, or ethically challenging case from the previous week. They received lectures on common HM topics, such as coronary artery disease, hypertension, and diabetes mellitus. The sessions featured guest speakers who touched on career options in IM and HM, research careers, tips for getting into medical school, and international health issues.
“I loved the patient interaction, as well as discussing a case with fellow students. I didn’t even mind the long hours,” says Stacey Yudin, 23, a senior pre-med student at UCLA. “While on rounds, medical students and doctors took the time to explain concepts while we were scurrying from patient to patient. The program gave me the opportunity to test-drive my dream. We always test-drive a car before we hand over thousands of dollars for it. Shouldn’t future medical students be able to at least safely experience the practice of medicine?”
Round Two: Upgrade
This summer, Dr. Afsar-manesh is improving the student presentation and guest speaker component of the Friday sessions. She will add QI and patient-safety sessions. But the biggest change to the program is expansion, as she and fellow UCLA hospitalist Ed Ha, MD, will offer a summer session for medical students between their first and second years.
Dr. Afsar-manesh also is busy reaching out to other academic IM and HM programs interested in establishing a preceptorship program. So far, she’s made headway with 10 institutions, including Northwestern University, Stanford University, the University of Michigan Health System, and a handful of the campuses within the University of California system. She’s invited the institutions to participate in a research collaborative to combine their data on program results. “We ultimately need to see how many participants will go into IM and compare that to the national numbers. That will take years,” she says.
Uphill Battle
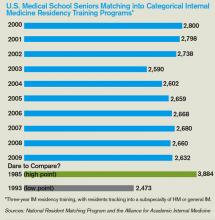
Mark Schwartz, MD, an associate professor in the division of general IM at New York University’s School of Medicine, believes UPIM and programs like it will help—even if only marginally—address the declining interest in IM careers among medical students.
“It will take more than tinkering around in the educational environment,” says Dr. Schwartz, who believes workforce planning, changes in reimbursement, and redesigning medical practices are essential to recruiting medical students to internal medicine (see “A Good Start, But Not Enough”).
Nevertheless, SHM is ready to support a combined IM/HM preceptorship program that targets medical school students in their first and second years, says Larry Wellikson, MD, FHM, CEO of SHM. The society already has assigned staff to manage the project and named Dr. Afsar-manesh as the lead physician. The plan is to track preceptorship participants as they make their way through medical school and residency, and see if the program changes their attitudes toward IM careers.
Even though the number of medical students who aspire to hospitalist careers continues to increase every year, SHM believes it must move to counteract the lackluster IM numbers, because that is where most medical students are introduced to HM, Dr. Wellikson says. “The problem of people not picking internal medicine could affect hospital medicine down the road,” he says. “We can’t sit passively by and see who picks to be a hospitalist. We believe we need to be active.”
One of the last things Dr. Afsar-manesh did at the conclusion of the inaugural UPIM program was collect the students’ e-mail addresses and phone numbers so she can stay in touch and track their career paths. The UPIM survey results give her hope: After UPIM, 100% of the students were “extremely confident” in their decision to pursue medicine; 57% indicated they were “very likely” to consider IM as a specialty; and 47% were “very likely” to think about HM.
“This program is a great way to encourage students to enter into internal medicine,” Yudin says. “I am sure that all my subsequent experiences working in a hospital will be measured against my first experience rounding with the IM department.” It seems as though the student took the words right out of the doctor’s mouth. TH
Lisa Ryan is a freelance writer based in New Jersey.
Reference
- Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154-1164.
Indu Michael remembers the one-page medical field survey she filled out around this time last year. A pre-med student at the University of California at Los Angeles, she provided the correct job descriptions for surgeons, pediatricians, OB/GYNs, psychiatrists, and internal medicine physicians. Only one medical specialty stumped her.
“I had no idea what a hospitalist did,” says Michael, 21, a senior.
The anonymous survey was part of the application and interview process for the Undergraduate Preceptorship in Internal Medicine (UPIM), a program that was launched last summer at UCLA Medical Center. By the time Michael finished the three-week program in early September, she had a complete understanding of what hospitalists do. She also says she’s leaning toward an internal medicine (IM) career—and might become a hospitalist.
“I’m seriously thinking [Hem-Onc] may not be the direction I want to take,” Michael says. “I realized oncologists are mainly consultative doctors and it’s really the general medicine team that does the medicine.”
Those kind of comments are music to Nasim Afsar-manesh’s ear. Dr. Afsar-manesh, a hospitalist and assistant clinical professor at UCLA, developed the UPIM program from scratch as a way to expose pre-med undergrads to internal medicine. The ultimate goal, of course, is steering them toward an internist career. She is well aware of medical students’ declining interest in IM, and she believes outreach to undergrads and first-year medical students will help reverse the trend.
“Undergraduates are like sponges,” Dr. Afsar-manesh says. “They are so genuinely excited about the possibilities of getting to do this stuff. … You can appeal to their idealism.” She created the program because “the general field of medicine has become so complex that students who are thinking about making it a career don’t have a good chance to see what the day-to-day practicing of medicine is like.”
HM Test Drive
Michael was one of seven students in the inaugural UPIM session. The program is open to UCLA undergrads who volunteer at least 80 hours at the medical center and pre-med students at the California Institute of Technology, where Dr. Afsar-manesh received her undergraduate degree. Seventeen students applied for the first session; the seven who were selected were chosen based on their motivation, maturity, and enthusiasm for medicine. The plan is simple: UPIM aims to offer an early spark of excitement that will stay with students and serve as positive reinforcement as they proceed through medical school and confront the challenges of an IM career.
UPIM participants were integrated into teams of attendings, residents, and medical school students, and they spent time on hospital units and subspecialty consult services. The undergrads observed residents in their patient evaluations, daily rounds, and discussions with patient families. They witnessed a number of procedures, including central-line placement and bone-marrow biopsies. Although the attendings and residents weren’t required to teach the undergrads, many volunteered a significant amount of their time, Dr. Afsar-manesh says. Some of the students spent night shifts at the hospital.
“The students felt they had participated in something special. They felt the experience had overshadowed anything they had previously done,” says Dr. Afsar-manesh, a member of SHM’s Young Physicians Committee. “I think it’s a program that can really quickly grow.”
Every Friday, undergrads participated in a teaching session, during which they had to present a medically, socially, or ethically challenging case from the previous week. They received lectures on common HM topics, such as coronary artery disease, hypertension, and diabetes mellitus. The sessions featured guest speakers who touched on career options in IM and HM, research careers, tips for getting into medical school, and international health issues.
“I loved the patient interaction, as well as discussing a case with fellow students. I didn’t even mind the long hours,” says Stacey Yudin, 23, a senior pre-med student at UCLA. “While on rounds, medical students and doctors took the time to explain concepts while we were scurrying from patient to patient. The program gave me the opportunity to test-drive my dream. We always test-drive a car before we hand over thousands of dollars for it. Shouldn’t future medical students be able to at least safely experience the practice of medicine?”
Round Two: Upgrade
This summer, Dr. Afsar-manesh is improving the student presentation and guest speaker component of the Friday sessions. She will add QI and patient-safety sessions. But the biggest change to the program is expansion, as she and fellow UCLA hospitalist Ed Ha, MD, will offer a summer session for medical students between their first and second years.
Dr. Afsar-manesh also is busy reaching out to other academic IM and HM programs interested in establishing a preceptorship program. So far, she’s made headway with 10 institutions, including Northwestern University, Stanford University, the University of Michigan Health System, and a handful of the campuses within the University of California system. She’s invited the institutions to participate in a research collaborative to combine their data on program results. “We ultimately need to see how many participants will go into IM and compare that to the national numbers. That will take years,” she says.
Uphill Battle
Mark Schwartz, MD, an associate professor in the division of general IM at New York University’s School of Medicine, believes UPIM and programs like it will help—even if only marginally—address the declining interest in IM careers among medical students.
“It will take more than tinkering around in the educational environment,” says Dr. Schwartz, who believes workforce planning, changes in reimbursement, and redesigning medical practices are essential to recruiting medical students to internal medicine (see “A Good Start, But Not Enough”).
Nevertheless, SHM is ready to support a combined IM/HM preceptorship program that targets medical school students in their first and second years, says Larry Wellikson, MD, FHM, CEO of SHM. The society already has assigned staff to manage the project and named Dr. Afsar-manesh as the lead physician. The plan is to track preceptorship participants as they make their way through medical school and residency, and see if the program changes their attitudes toward IM careers.
Even though the number of medical students who aspire to hospitalist careers continues to increase every year, SHM believes it must move to counteract the lackluster IM numbers, because that is where most medical students are introduced to HM, Dr. Wellikson says. “The problem of people not picking internal medicine could affect hospital medicine down the road,” he says. “We can’t sit passively by and see who picks to be a hospitalist. We believe we need to be active.”
One of the last things Dr. Afsar-manesh did at the conclusion of the inaugural UPIM program was collect the students’ e-mail addresses and phone numbers so she can stay in touch and track their career paths. The UPIM survey results give her hope: After UPIM, 100% of the students were “extremely confident” in their decision to pursue medicine; 57% indicated they were “very likely” to consider IM as a specialty; and 47% were “very likely” to think about HM.
“This program is a great way to encourage students to enter into internal medicine,” Yudin says. “I am sure that all my subsequent experiences working in a hospital will be measured against my first experience rounding with the IM department.” It seems as though the student took the words right out of the doctor’s mouth. TH
Lisa Ryan is a freelance writer based in New Jersey.
Reference
- Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154-1164.
Indu Michael remembers the one-page medical field survey she filled out around this time last year. A pre-med student at the University of California at Los Angeles, she provided the correct job descriptions for surgeons, pediatricians, OB/GYNs, psychiatrists, and internal medicine physicians. Only one medical specialty stumped her.
“I had no idea what a hospitalist did,” says Michael, 21, a senior.
The anonymous survey was part of the application and interview process for the Undergraduate Preceptorship in Internal Medicine (UPIM), a program that was launched last summer at UCLA Medical Center. By the time Michael finished the three-week program in early September, she had a complete understanding of what hospitalists do. She also says she’s leaning toward an internal medicine (IM) career—and might become a hospitalist.
“I’m seriously thinking [Hem-Onc] may not be the direction I want to take,” Michael says. “I realized oncologists are mainly consultative doctors and it’s really the general medicine team that does the medicine.”
Those kind of comments are music to Nasim Afsar-manesh’s ear. Dr. Afsar-manesh, a hospitalist and assistant clinical professor at UCLA, developed the UPIM program from scratch as a way to expose pre-med undergrads to internal medicine. The ultimate goal, of course, is steering them toward an internist career. She is well aware of medical students’ declining interest in IM, and she believes outreach to undergrads and first-year medical students will help reverse the trend.
“Undergraduates are like sponges,” Dr. Afsar-manesh says. “They are so genuinely excited about the possibilities of getting to do this stuff. … You can appeal to their idealism.” She created the program because “the general field of medicine has become so complex that students who are thinking about making it a career don’t have a good chance to see what the day-to-day practicing of medicine is like.”
HM Test Drive
Michael was one of seven students in the inaugural UPIM session. The program is open to UCLA undergrads who volunteer at least 80 hours at the medical center and pre-med students at the California Institute of Technology, where Dr. Afsar-manesh received her undergraduate degree. Seventeen students applied for the first session; the seven who were selected were chosen based on their motivation, maturity, and enthusiasm for medicine. The plan is simple: UPIM aims to offer an early spark of excitement that will stay with students and serve as positive reinforcement as they proceed through medical school and confront the challenges of an IM career.
UPIM participants were integrated into teams of attendings, residents, and medical school students, and they spent time on hospital units and subspecialty consult services. The undergrads observed residents in their patient evaluations, daily rounds, and discussions with patient families. They witnessed a number of procedures, including central-line placement and bone-marrow biopsies. Although the attendings and residents weren’t required to teach the undergrads, many volunteered a significant amount of their time, Dr. Afsar-manesh says. Some of the students spent night shifts at the hospital.
“The students felt they had participated in something special. They felt the experience had overshadowed anything they had previously done,” says Dr. Afsar-manesh, a member of SHM’s Young Physicians Committee. “I think it’s a program that can really quickly grow.”
Every Friday, undergrads participated in a teaching session, during which they had to present a medically, socially, or ethically challenging case from the previous week. They received lectures on common HM topics, such as coronary artery disease, hypertension, and diabetes mellitus. The sessions featured guest speakers who touched on career options in IM and HM, research careers, tips for getting into medical school, and international health issues.
“I loved the patient interaction, as well as discussing a case with fellow students. I didn’t even mind the long hours,” says Stacey Yudin, 23, a senior pre-med student at UCLA. “While on rounds, medical students and doctors took the time to explain concepts while we were scurrying from patient to patient. The program gave me the opportunity to test-drive my dream. We always test-drive a car before we hand over thousands of dollars for it. Shouldn’t future medical students be able to at least safely experience the practice of medicine?”
Round Two: Upgrade
This summer, Dr. Afsar-manesh is improving the student presentation and guest speaker component of the Friday sessions. She will add QI and patient-safety sessions. But the biggest change to the program is expansion, as she and fellow UCLA hospitalist Ed Ha, MD, will offer a summer session for medical students between their first and second years.
Dr. Afsar-manesh also is busy reaching out to other academic IM and HM programs interested in establishing a preceptorship program. So far, she’s made headway with 10 institutions, including Northwestern University, Stanford University, the University of Michigan Health System, and a handful of the campuses within the University of California system. She’s invited the institutions to participate in a research collaborative to combine their data on program results. “We ultimately need to see how many participants will go into IM and compare that to the national numbers. That will take years,” she says.
Uphill Battle
Mark Schwartz, MD, an associate professor in the division of general IM at New York University’s School of Medicine, believes UPIM and programs like it will help—even if only marginally—address the declining interest in IM careers among medical students.
“It will take more than tinkering around in the educational environment,” says Dr. Schwartz, who believes workforce planning, changes in reimbursement, and redesigning medical practices are essential to recruiting medical students to internal medicine (see “A Good Start, But Not Enough”).
Nevertheless, SHM is ready to support a combined IM/HM preceptorship program that targets medical school students in their first and second years, says Larry Wellikson, MD, FHM, CEO of SHM. The society already has assigned staff to manage the project and named Dr. Afsar-manesh as the lead physician. The plan is to track preceptorship participants as they make their way through medical school and residency, and see if the program changes their attitudes toward IM careers.
Even though the number of medical students who aspire to hospitalist careers continues to increase every year, SHM believes it must move to counteract the lackluster IM numbers, because that is where most medical students are introduced to HM, Dr. Wellikson says. “The problem of people not picking internal medicine could affect hospital medicine down the road,” he says. “We can’t sit passively by and see who picks to be a hospitalist. We believe we need to be active.”
One of the last things Dr. Afsar-manesh did at the conclusion of the inaugural UPIM program was collect the students’ e-mail addresses and phone numbers so she can stay in touch and track their career paths. The UPIM survey results give her hope: After UPIM, 100% of the students were “extremely confident” in their decision to pursue medicine; 57% indicated they were “very likely” to consider IM as a specialty; and 47% were “very likely” to think about HM.
“This program is a great way to encourage students to enter into internal medicine,” Yudin says. “I am sure that all my subsequent experiences working in a hospital will be measured against my first experience rounding with the IM department.” It seems as though the student took the words right out of the doctor’s mouth. TH
Lisa Ryan is a freelance writer based in New Jersey.
Reference
- Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154-1164.
Code Correctly
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
Medicare: Enroll Early
Some healthcare providers probably missed an important change buried within the 2009 Medicare Physician Fee Schedule: New rules for physician enrollment have drastically reduced the period for retroactive billing. Effective April 1, physicians enrolling or re-enrolling with Medicare can only submit a bill for services provided up to 30 days prior to the effective date, rather than for the prior 27 months.
Those who miss this deadline will be denied reimbursement for services to Medicare patients seen before the deadline. And those who move to a new job (“change of location,” in Medicare parlance) and fail to update their address within 30 days risk a two-year suspension from receiving Medicare payments.
What It Means
Essentially, HM group leaders must make sure they are ready to credential a new hire long before they start working. Before now, groups had months to get new hires enrolled in the Medicare system; now, with just 30 days to enroll, you need to start your credentialing and enrollment process early—before the physician’s start date, if possible.
“In a nutshell, groups are going to have to be more proactive than ever before in getting paperwork submitted for new providers,” says Derise Woods, operations project manager for Knoxville, Tenn.-based TeamHealth. “The situation we often face is that the provider is found and placed, and sometimes the paperwork does not get submitted right away. The natural focus is to get them on board and then get them up and running.”
If that is the case in your group, you should create a checklist for enrollment in Medicare and for other payors. Then, as soon as your new hire signs the contract, require them to submit all available information (e.g., DEA number and proof of board certification).
Woods says the rule states that “retroactive billing can start from the provider’s start date or from the date the enrollment is received at [Medicare], whichever is later.”
Even if you don’t capture all the necessary information, enroll the new physician as soon as possible. According to the Centers for Medicare & Medicaid Services (CMS), incomplete applications will be denied, but the date of the original filing will be preserved. So if a hospitalist begins working for your group Sept. 1, and you submit the enrollment application Sept. 7, the hospitalist can bill retroactively starting Sept. 7, even if that application is kicked back to you for more information and doesn’t get resolved for several weeks.
—Derise Woods, TeamHealth, Knoxville, Tenn.
Large and Small Groups
Missing the new enrollment deadline means reimbursement losses. Hospitalists provide services to a significant number of Medicare patients, so cutting back on retroactive billing could hurt the bottom line. “In most [HM] instances where Medicare is a large portion of income, this has potential to disrupt a practice,” Woods says, noting TeamHealth has yet to see the impact of the new enrollment rules.
Which entity incurs the loss of Medicare payments depends on your program’s payment structure. “For instance, TeamHealth contracts with our providers and pays them an hourly rate,” says Woods, explaining that the third-party contractor will suffer any loss of fees. “In a hospital-based program, the hospital might bill for the provider—and that provider may not get paid.”
Smaller HM groups might not have as much experience with these changes simply because they don’t hire physicians as often. “I did not know about this,” says Heidi Tessler, MD, president of the Colorado Hospitalist Company in Denver. “We contract with a billing company [for physician enrollments], and we would have been caught flat-footed with our next hire.”
Small groups could end up scrambling when they need to fill a position, especially if it’s a quick turnover. Groups that outsource their recruiting and billing should plan to communicate with those companies to expedite the enrollment process, Woods says.
TeamHealth, the largest provider of hospital-based clinical outsourcing in the U.S., has made numerous changes to accommodate the new enrollment rules, all the way up to a new business development group. “They now take this new rule into consideration when we are planning to start providing service,” Woods says. “Our recruiters are helping. They are ensuring that new providers fill out their paperwork and get it in. Understandably, physicians can let paperwork sit for a number of days.”
The good news is CMS has made it easier—and faster—to enroll through a Web-based portal called PECOS (Provider Enrollment, Chain, and Ownership System), which can be accessed at www.cms.hhs.gov/MedicareProviderSupEnroll/.
Central Source
SHM has consolidated essential sources on the new rules to include:
- Medicare’s all-inclusive Web section on provider enrollment is www.cms.hhs.gov/medicareprovidersupenroll.
- The CMS manual on enrollment is at www.cms.hhs.gov. Click on “manuals,” then “Internet-only manuals”; select “Publication 100-08, Program Integrity Manual,” then “Chapter 10.”
- AMA provides an overview on its Web site, and, with the Medical Group Management Association (MGMA), has developed a toolkit to guide physicians through the new rules. “The toolkit is probably the best resource available,” says Leslie Flores, principal in Nelson/Flores Associates, a national hospitalist management consulting firm and director of SHM’s Practice Management Institute. AMA and MGMA members can access the toolkit at www.mgma.com/policy/default.aspx?id=5712.
“SHM wants to make sure we communicate these new rules to our members,” says Flores, “and provide direction to resources they can use.” Check www.hospitalmedicine.org for the latest links and information. TH
Jane Jerrard is a freelance writer based in Chicago.
Some healthcare providers probably missed an important change buried within the 2009 Medicare Physician Fee Schedule: New rules for physician enrollment have drastically reduced the period for retroactive billing. Effective April 1, physicians enrolling or re-enrolling with Medicare can only submit a bill for services provided up to 30 days prior to the effective date, rather than for the prior 27 months.
Those who miss this deadline will be denied reimbursement for services to Medicare patients seen before the deadline. And those who move to a new job (“change of location,” in Medicare parlance) and fail to update their address within 30 days risk a two-year suspension from receiving Medicare payments.
What It Means
Essentially, HM group leaders must make sure they are ready to credential a new hire long before they start working. Before now, groups had months to get new hires enrolled in the Medicare system; now, with just 30 days to enroll, you need to start your credentialing and enrollment process early—before the physician’s start date, if possible.
“In a nutshell, groups are going to have to be more proactive than ever before in getting paperwork submitted for new providers,” says Derise Woods, operations project manager for Knoxville, Tenn.-based TeamHealth. “The situation we often face is that the provider is found and placed, and sometimes the paperwork does not get submitted right away. The natural focus is to get them on board and then get them up and running.”
If that is the case in your group, you should create a checklist for enrollment in Medicare and for other payors. Then, as soon as your new hire signs the contract, require them to submit all available information (e.g., DEA number and proof of board certification).
Woods says the rule states that “retroactive billing can start from the provider’s start date or from the date the enrollment is received at [Medicare], whichever is later.”
Even if you don’t capture all the necessary information, enroll the new physician as soon as possible. According to the Centers for Medicare & Medicaid Services (CMS), incomplete applications will be denied, but the date of the original filing will be preserved. So if a hospitalist begins working for your group Sept. 1, and you submit the enrollment application Sept. 7, the hospitalist can bill retroactively starting Sept. 7, even if that application is kicked back to you for more information and doesn’t get resolved for several weeks.
—Derise Woods, TeamHealth, Knoxville, Tenn.
Large and Small Groups
Missing the new enrollment deadline means reimbursement losses. Hospitalists provide services to a significant number of Medicare patients, so cutting back on retroactive billing could hurt the bottom line. “In most [HM] instances where Medicare is a large portion of income, this has potential to disrupt a practice,” Woods says, noting TeamHealth has yet to see the impact of the new enrollment rules.
Which entity incurs the loss of Medicare payments depends on your program’s payment structure. “For instance, TeamHealth contracts with our providers and pays them an hourly rate,” says Woods, explaining that the third-party contractor will suffer any loss of fees. “In a hospital-based program, the hospital might bill for the provider—and that provider may not get paid.”
Smaller HM groups might not have as much experience with these changes simply because they don’t hire physicians as often. “I did not know about this,” says Heidi Tessler, MD, president of the Colorado Hospitalist Company in Denver. “We contract with a billing company [for physician enrollments], and we would have been caught flat-footed with our next hire.”
Small groups could end up scrambling when they need to fill a position, especially if it’s a quick turnover. Groups that outsource their recruiting and billing should plan to communicate with those companies to expedite the enrollment process, Woods says.
TeamHealth, the largest provider of hospital-based clinical outsourcing in the U.S., has made numerous changes to accommodate the new enrollment rules, all the way up to a new business development group. “They now take this new rule into consideration when we are planning to start providing service,” Woods says. “Our recruiters are helping. They are ensuring that new providers fill out their paperwork and get it in. Understandably, physicians can let paperwork sit for a number of days.”
The good news is CMS has made it easier—and faster—to enroll through a Web-based portal called PECOS (Provider Enrollment, Chain, and Ownership System), which can be accessed at www.cms.hhs.gov/MedicareProviderSupEnroll/.
Central Source
SHM has consolidated essential sources on the new rules to include:
- Medicare’s all-inclusive Web section on provider enrollment is www.cms.hhs.gov/medicareprovidersupenroll.
- The CMS manual on enrollment is at www.cms.hhs.gov. Click on “manuals,” then “Internet-only manuals”; select “Publication 100-08, Program Integrity Manual,” then “Chapter 10.”
- AMA provides an overview on its Web site, and, with the Medical Group Management Association (MGMA), has developed a toolkit to guide physicians through the new rules. “The toolkit is probably the best resource available,” says Leslie Flores, principal in Nelson/Flores Associates, a national hospitalist management consulting firm and director of SHM’s Practice Management Institute. AMA and MGMA members can access the toolkit at www.mgma.com/policy/default.aspx?id=5712.
“SHM wants to make sure we communicate these new rules to our members,” says Flores, “and provide direction to resources they can use.” Check www.hospitalmedicine.org for the latest links and information. TH
Jane Jerrard is a freelance writer based in Chicago.
Some healthcare providers probably missed an important change buried within the 2009 Medicare Physician Fee Schedule: New rules for physician enrollment have drastically reduced the period for retroactive billing. Effective April 1, physicians enrolling or re-enrolling with Medicare can only submit a bill for services provided up to 30 days prior to the effective date, rather than for the prior 27 months.
Those who miss this deadline will be denied reimbursement for services to Medicare patients seen before the deadline. And those who move to a new job (“change of location,” in Medicare parlance) and fail to update their address within 30 days risk a two-year suspension from receiving Medicare payments.
What It Means
Essentially, HM group leaders must make sure they are ready to credential a new hire long before they start working. Before now, groups had months to get new hires enrolled in the Medicare system; now, with just 30 days to enroll, you need to start your credentialing and enrollment process early—before the physician’s start date, if possible.
“In a nutshell, groups are going to have to be more proactive than ever before in getting paperwork submitted for new providers,” says Derise Woods, operations project manager for Knoxville, Tenn.-based TeamHealth. “The situation we often face is that the provider is found and placed, and sometimes the paperwork does not get submitted right away. The natural focus is to get them on board and then get them up and running.”
If that is the case in your group, you should create a checklist for enrollment in Medicare and for other payors. Then, as soon as your new hire signs the contract, require them to submit all available information (e.g., DEA number and proof of board certification).
Woods says the rule states that “retroactive billing can start from the provider’s start date or from the date the enrollment is received at [Medicare], whichever is later.”
Even if you don’t capture all the necessary information, enroll the new physician as soon as possible. According to the Centers for Medicare & Medicaid Services (CMS), incomplete applications will be denied, but the date of the original filing will be preserved. So if a hospitalist begins working for your group Sept. 1, and you submit the enrollment application Sept. 7, the hospitalist can bill retroactively starting Sept. 7, even if that application is kicked back to you for more information and doesn’t get resolved for several weeks.
—Derise Woods, TeamHealth, Knoxville, Tenn.
Large and Small Groups
Missing the new enrollment deadline means reimbursement losses. Hospitalists provide services to a significant number of Medicare patients, so cutting back on retroactive billing could hurt the bottom line. “In most [HM] instances where Medicare is a large portion of income, this has potential to disrupt a practice,” Woods says, noting TeamHealth has yet to see the impact of the new enrollment rules.
Which entity incurs the loss of Medicare payments depends on your program’s payment structure. “For instance, TeamHealth contracts with our providers and pays them an hourly rate,” says Woods, explaining that the third-party contractor will suffer any loss of fees. “In a hospital-based program, the hospital might bill for the provider—and that provider may not get paid.”
Smaller HM groups might not have as much experience with these changes simply because they don’t hire physicians as often. “I did not know about this,” says Heidi Tessler, MD, president of the Colorado Hospitalist Company in Denver. “We contract with a billing company [for physician enrollments], and we would have been caught flat-footed with our next hire.”
Small groups could end up scrambling when they need to fill a position, especially if it’s a quick turnover. Groups that outsource their recruiting and billing should plan to communicate with those companies to expedite the enrollment process, Woods says.
TeamHealth, the largest provider of hospital-based clinical outsourcing in the U.S., has made numerous changes to accommodate the new enrollment rules, all the way up to a new business development group. “They now take this new rule into consideration when we are planning to start providing service,” Woods says. “Our recruiters are helping. They are ensuring that new providers fill out their paperwork and get it in. Understandably, physicians can let paperwork sit for a number of days.”
The good news is CMS has made it easier—and faster—to enroll through a Web-based portal called PECOS (Provider Enrollment, Chain, and Ownership System), which can be accessed at www.cms.hhs.gov/MedicareProviderSupEnroll/.
Central Source
SHM has consolidated essential sources on the new rules to include:
- Medicare’s all-inclusive Web section on provider enrollment is www.cms.hhs.gov/medicareprovidersupenroll.
- The CMS manual on enrollment is at www.cms.hhs.gov. Click on “manuals,” then “Internet-only manuals”; select “Publication 100-08, Program Integrity Manual,” then “Chapter 10.”
- AMA provides an overview on its Web site, and, with the Medical Group Management Association (MGMA), has developed a toolkit to guide physicians through the new rules. “The toolkit is probably the best resource available,” says Leslie Flores, principal in Nelson/Flores Associates, a national hospitalist management consulting firm and director of SHM’s Practice Management Institute. AMA and MGMA members can access the toolkit at www.mgma.com/policy/default.aspx?id=5712.
“SHM wants to make sure we communicate these new rules to our members,” says Flores, “and provide direction to resources they can use.” Check www.hospitalmedicine.org for the latest links and information. TH
Jane Jerrard is a freelance writer based in Chicago.
What is the best empiric therapy for community-acquired cellulitis?
Case
A previously healthy 55-year-old white female presents to the ED with a three-day history of pain and erythema in her right hand. Examination reveals fluctuance as well. She is diagnosed with an abscess with surrounding cellulitis. The abscess is incised, drained, and cultured, and she is sent home on oral trimethoprim/sulfamethoxazole. The following day, her cellulitis has worsened. She is hospitalized and commenced on intravenous vancomycin. What is the best empiric therapy for community-acquired cellulitis?
Background
Cellulitis is defined as a skin and soft-tissue infection (SSTI), which develops as a result of bacterial entry via breaches in the skin barrier. Typically, it involves the dermis and subcutaneous tissue, and is associated with local tenderness, erythema, swelling and fever. Cellulitis usually affects the lower extremities, but can affect other locations resulting in diagnoses such as periorbital, abdominal wall, buccal, and perianal cellulitis.1,2
Gram-positive organisms, especially Staphylococcus aureus and beta hemolytic streptococci, are the most common causes of cellulitis. Although it is less common, cellulitis can be caused by gram-negative organisms. The recent significant increase in the prevalence of SSTIs due to community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) has led to changes in the selection of antibiotics that were most commonly utilized to empirically treat cellulitis.
The diagnosis of cellulitis is based primarily on clinical manifestations. Due to low diagnostic yields, blood cultures, needle aspiration, or punch biopsy, specimens usually are not helpful in the setting of simple cellulitis.3 Therefore, antibiotic therapy is almost universally started empirically. Starting appropriate initial antibiotic therapy improves patient outcomes by reducing mortality rates, length of stay, and inpatient costs.4
Cellulitis incidence is about two cases per 1,000 patient-years.5 This rather high incidence, coupled with escalating rates of SSTIs due to CA-MRSA, demands reliable and cost-effective treatment strategies for the management of community-acquired cellulitis.
Review of the Data
The treatment of community-acquired cellulitis was straightforward until the past decade, as physicians saw a significant increase in CA-MRSA incidence.6 MRSA was reported initially in 1961, only two years after methicillin was introduced into clinical practice.7,8 Subsequently, MRSA prevalence increased dramatically, and by the beginning of this decade, more than 50% of the Staphylococcus aureus hospital strains were resistant to methicillin.8 Furthermore, 60% to 80% of community-acquired Staphylococcus aureus strains in the U.S. are methicillin-resistant.8
The two major types of MRSA infections are healthcare-acquired (HA-MRSA) and community-acquired (CA-MRSA). The HA-MRSA infection group is further subdivided into those strains that develop during a period of hospitalization, and those that develop following contact with healthcare facilities (e.g., hospitalization or surgery within the previous year). This subgroup includes HA-MRSA infections in hemodialysis patients, residents of long-term care facilities, and individuals who have a vascular catheter or other indwelling device.9,10
CA-MRSA infections, on the other hand, occur in individuals who have not had any contact with healthcare facilities. Higher rates of CA-MRSA infection are observed in settings where individuals have close contact with each other, including military trainees, athletes involved in contact sports, patients age 65 and older, men who have sex with other men, and parenteral substance abusers.8,11-13 However, in view of the high prevalence of CA-MRSA in the U.S., most patients, including those without any apparent risk factors, are at risk.8
HA-MRSA has the ability to survive on inanimate objects for extended time periods, increasing the likelihood of transmission to persons who come into contact with those objects. Although evidence has not confirmed that CA-MRSA has a similar capacity, it seems plausible that such spread does contribute to the propagation of CA-MRSA.12
The increasing importance of CA-MRSA also is evident in hospital settings, where it is replacing HA-MRSA as the most common type of Staphylococcus aureus. Since CA-MRSA tends to be susceptible to a larger number of antibiotics than HA-MRSA is, this has led to a reduced incidence of multidrug resistance. Fortunately, unlike HA-MRSA, CA-MRSA is susceptible to non-beta-lactam antibiotics, including tetracyclines, sulfonamides, and clindamycin.9
CA-MRSA most often causes SSTIs, and a tender abscess is a typical presentation.8 Patients commonly misinterpret early skin lesions as an insect or spider bite.12,14 When cutaneous CA-MRSA presents as an abscess, an incision and drainage procedure is essential for adequate treatment of the infection. For some CA-MRSA infections, particularly those characterized by the presence of a relatively small abscess, it might be adequate to do only an incision and drainage procedure, and not administer antibiotics.8,15 However, in most instances, especially when there is an area of cellulitis around the abscess, the initiation of antibiotic therapy improves patients’ clinical outcomes.9,16
When there is no apparent drainable purulent fluid collection, which often occurs with cellulitis, antibiotics should be the mainstay of therapy. The decision about which antibiotic to start can present some challenges, because the organism causing the cellulitis usually is not identified. This is because blood cultures are positive in less than 5% of cases. Also, positive culture results from needle aspiration are only helpful from 5% to 40% of the time. Meanwhile, culture of punch biopsy specimens yields a pathogen in only 20% to 30% of cases.3,17-19
Due to increased CA-MRSA incidence, cephalexin should not be prescribed to treat cellulitis in the outpatient setting because it does not provide coverage for the pathogen.13 Instead, oral antibiotics (e.g., clindamycin or trimethoprim/sulfamethoxazole) should be prescribed. Doxycycline, minocycline, rifampin (usually prescribed in combination with fusidic acid to prevent resistance development), and linezolid are additional therapeutic options.
Trimethoprim/sulfamethoxazole and clindamycin have several advantages: good oral bioavailability, familiarity to physicians, and general affordability. A disadvantage to using both trimethoprim/sulfamethoxazole and doxycycline is that they provide inadequate coverage for group A streptococci, which are a common cause of cellulitis. Therefore, the simultaneous use of a beta-lactam antibiotic with either of these medications may improve outcomes for “nonpurulent” cellulitis.13,15 Linezolid has proven effective for skin and SSTI caused by MRSA, even though it is not bactericidal.
Excellent oral bioavailability of this drug is an attractive characteristic, as it facilitates the transition from the use of intravenous to oral antibiotic therapy later in a patient’s hospital course. Although oral linezolid has been studied in clinical trials and provides good coverage for MRSA, its use in the outpatient setting is relatively limited, largely due to its significant cost.20 In 2008, the cost of 10 days of treatment with oral linezolid was $1,286.80. In comparison, the generic trimethoprim/sulfamethox-azole cost $9.40, and generic clindamycin cost $95.10.8 The lack of routine availability in many outpatient pharmacies also hinders the widespread use of linezolid.13
To date, with the exception of linezolid, no randomized, prospective clinical trials clearly demonstrate the efficacy of the oral agents that are commonly used for the outpatient treatment of cellulitis.20
When patients require hospitalization for the optimal treatment of cellulitis, it is important to select a parenteral antibiotic that provides coverage for MRSA.8 Vancomycin, daptomycin, linezolid, and tigecycline are the most commonly used agents.6
In the inpatient setting, failure to initiate appropriate medical therapy can result in longer hospital admissions, which significantly increase inpatient costs. Inadequate antibiotic therapy creates a significant financial burden and has been associated with increased mortality.4 Historically, vancomycin is used whenever a MRSA infection is suspected. However, there is concern about the declining efficacy of vancomycin related to a gradual increase in the rate of relative resistance—a minimal inhibitory concentration (MIC) increase—in MRSA strains. This MIC creep is noted in some medical centers and can lead to a failure to respond to vancomycin.13,20
Daptomycin is rapidly bactericidal against MRSA; in some institutions, its use may be preferred over vancomycin because the former antibiotic is associated with a significantly more rapid clinical response, which may shorten the required length of hospitalization.21 The once-daily dosing requirement for daptomycin allows for ease of use in both hospital and outpatient settings, and therefore may facilitate early hospital discharge or prevent the need for hospitalization altogether. Clinical experience also suggests potential economic advantages with the use of daptomycin.22
Tigecycline is a bacteriostatic antibiotic that achieves low serum concentrations. However, it penetrates the skin well and has a similar effectiveness to combination therapy with vancomycin and aztreonam. Thus far, tigecycline is not widely used for the treatment of MRSA infections, and it has been suggested that it may be preferred for polymicrobial infections or for patients who exhibit allergies to more commonly used agents.8
When selecting an antibiotic therapy, cost considerations play an important role in the decision-making process. For intravenous agents commonly used to treat CA-MRSA infections, the 2008 cost for 10 days of treatment with generic vancomycin was $182.80; daptomycin cost $1,660.80. For tigecycline and linezolid, the same duration of treatment cost $1,362 and $1,560, respectively.8
Back to the Case
Our patient, an otherwise healthy female, presented with no apparent risk factors for developing a CA-MRSA SSTI. However, more detailed history revealed that she regularly used sports equipment at her local fitness center. Based on her clinical presentation and concerns about the high local prevalence of CA-MRSA, an incision and drainage procedure was performed, and she was started empirically on IV vancomycin. She had a positive clinical response to this treatment.
Wound culture results confirmed CA-MRSA abscess and cellulitis, susceptible to trimethoprim/sulfamethoxazole. She was discharged on the oral formulation of this antibiotic to complete a 10-day course of treatment, including the days she received intravenous antibiotics.
Few well-designed trials have compared different lengths of cellulitis therapy. Most authorities recommend five to 10 days of treatment; however, longer courses might be required for more severe or complicated diseases.
Bottom line
Because of the high prevalence of CA-MRSA, initial antibiotic therapy for the treatment of community-acquired cellulitis must provide coverage for this organism. TH
Dr. Clarke is a hospitalist and clinical instructor at Emory University School of Medicine, Atlanta. Dr. Dressler is associate professor and director of education, section of hospital medicine, and associate program director of the J. Willis Hurst Internal Medicine Residency Program. Dr. Purohit is an instructor in clinical medicine at Emory University School of Medicine.
References
- Barzilai A, Choen HA. Isolation of group A streptococci from children with perianal cellulitis and from their siblings. Pediatr Infect Dis J. 1998;17(4):358-360.
- Thorsteinsdottir B, Tleyjeh IM, Baddour LM. Abdominal wall cellulitis in the morbidly obese. Scand J Infect Dis. 2005;37(8):605-608.
- Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004;350(9):904-912.
- Edelsberg J, Berger A, Weber DJ, et al. Clinical and economic consequences of failure of initial antibiotic therapy for hospitalized patients with complicated skin and skin-structure infections. Infect Control Hosp Epidemiol. 2008;29(2):160-169.
- McNamara DR, Tleyjeh IM, Berbari EF, et al. Incidence of lower extremity cellulitis: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2007;82(7):817-821.
- Moellering RC. Current treatment options for community-acquired methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2008;46(7):1032-1037.
- Chambers HF. The changing epidemiology of Staphylococcus aureus. Emerg Infect Dis. 2001;7(2):178-182.
- Moellering RC. A 39-year-old man with a skin infection. JAMA. 2008;299(1):79-87
- Ruhe J, Smith N, Bradsher RW, Menon A. Community-onset methicillin-resistant Staphylococcus aureus skin and soft tissue infections: impact of antimicrobial therapy on outcome. Clin Infect Dis. 2007;44(6):777-784.
- David MZ, Glikman D, Crawford SE, et al. What is community-associated methicillin-resistant Staphylococcus aureus? J Infect Dis. 2008;197(9):1235-1243.
- Iyer S, Jones DH. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: a retrospective analysis of clinical presentation and treatment of a local outbreak. J Am Acad Dermatol. 2004;50(6):854-858.
- Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison—Mississippi, 2000. MMWR Morb Mortal Wkly Rep. 2001;50(42):919-922.
- Daum RS. Clinical practice. Skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. N Engl J Med. 2007;357(4):380-390.
- Dominguez TJ. It’s not a spider bite, it’s community-acquired methicillin-resistant Staphylococcus aureus. J Am Board Fam Pract. 2004;17(3):220-226.
- Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666-674.
- Jetton L. Therapy for methicillin-resistant Staphylococcus aureus. N Engl J Med. 2006;355(20):2153-2155.
- Hook EW, Hooton TM, Horton CA, et al. Microbiologic evaluation of cutaneous cellulitis in adults. Arch Intern Med. 1986;146(2):295-297.
- Duvanel T, Auckenthaler R, Rohner P, Harms M, Saurat JH. Quantitative cultures of biopsy specimens from cutaneous cellulitis. Arch Intern Med. 1989;149(2):293-296.
- Newell PM, Norden CW. Value of needle aspiration in bacteriologic diagnosis of cellulitis in adults. J Clin Microbiol. 1988; 26(3):401-404.
- Loffler CA, Macdougall C. Update on prevalence and treatment of methicillin-resistant Staphylococcus aureus infections. Expert Rev Anti Infect Ther. 2007;5(6):961-981.
- Davis SL, McKinnon PS, Hall LM, et al. Daptomycin versus vancomycin for complicated skin and skin structure infections: clinical and economic outcomes. Pharmacotherapy. 2007;27(12):1611-1618.
- Seaton RA. Daptomycin: rationale and role in the management of skin and soft tissue infections. J Antimicrob Chemother. 2008;62(Suppl 3):iii15-23.
Case
A previously healthy 55-year-old white female presents to the ED with a three-day history of pain and erythema in her right hand. Examination reveals fluctuance as well. She is diagnosed with an abscess with surrounding cellulitis. The abscess is incised, drained, and cultured, and she is sent home on oral trimethoprim/sulfamethoxazole. The following day, her cellulitis has worsened. She is hospitalized and commenced on intravenous vancomycin. What is the best empiric therapy for community-acquired cellulitis?
Background
Cellulitis is defined as a skin and soft-tissue infection (SSTI), which develops as a result of bacterial entry via breaches in the skin barrier. Typically, it involves the dermis and subcutaneous tissue, and is associated with local tenderness, erythema, swelling and fever. Cellulitis usually affects the lower extremities, but can affect other locations resulting in diagnoses such as periorbital, abdominal wall, buccal, and perianal cellulitis.1,2
Gram-positive organisms, especially Staphylococcus aureus and beta hemolytic streptococci, are the most common causes of cellulitis. Although it is less common, cellulitis can be caused by gram-negative organisms. The recent significant increase in the prevalence of SSTIs due to community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) has led to changes in the selection of antibiotics that were most commonly utilized to empirically treat cellulitis.
The diagnosis of cellulitis is based primarily on clinical manifestations. Due to low diagnostic yields, blood cultures, needle aspiration, or punch biopsy, specimens usually are not helpful in the setting of simple cellulitis.3 Therefore, antibiotic therapy is almost universally started empirically. Starting appropriate initial antibiotic therapy improves patient outcomes by reducing mortality rates, length of stay, and inpatient costs.4
Cellulitis incidence is about two cases per 1,000 patient-years.5 This rather high incidence, coupled with escalating rates of SSTIs due to CA-MRSA, demands reliable and cost-effective treatment strategies for the management of community-acquired cellulitis.
Review of the Data
The treatment of community-acquired cellulitis was straightforward until the past decade, as physicians saw a significant increase in CA-MRSA incidence.6 MRSA was reported initially in 1961, only two years after methicillin was introduced into clinical practice.7,8 Subsequently, MRSA prevalence increased dramatically, and by the beginning of this decade, more than 50% of the Staphylococcus aureus hospital strains were resistant to methicillin.8 Furthermore, 60% to 80% of community-acquired Staphylococcus aureus strains in the U.S. are methicillin-resistant.8
The two major types of MRSA infections are healthcare-acquired (HA-MRSA) and community-acquired (CA-MRSA). The HA-MRSA infection group is further subdivided into those strains that develop during a period of hospitalization, and those that develop following contact with healthcare facilities (e.g., hospitalization or surgery within the previous year). This subgroup includes HA-MRSA infections in hemodialysis patients, residents of long-term care facilities, and individuals who have a vascular catheter or other indwelling device.9,10
CA-MRSA infections, on the other hand, occur in individuals who have not had any contact with healthcare facilities. Higher rates of CA-MRSA infection are observed in settings where individuals have close contact with each other, including military trainees, athletes involved in contact sports, patients age 65 and older, men who have sex with other men, and parenteral substance abusers.8,11-13 However, in view of the high prevalence of CA-MRSA in the U.S., most patients, including those without any apparent risk factors, are at risk.8
HA-MRSA has the ability to survive on inanimate objects for extended time periods, increasing the likelihood of transmission to persons who come into contact with those objects. Although evidence has not confirmed that CA-MRSA has a similar capacity, it seems plausible that such spread does contribute to the propagation of CA-MRSA.12
The increasing importance of CA-MRSA also is evident in hospital settings, where it is replacing HA-MRSA as the most common type of Staphylococcus aureus. Since CA-MRSA tends to be susceptible to a larger number of antibiotics than HA-MRSA is, this has led to a reduced incidence of multidrug resistance. Fortunately, unlike HA-MRSA, CA-MRSA is susceptible to non-beta-lactam antibiotics, including tetracyclines, sulfonamides, and clindamycin.9
CA-MRSA most often causes SSTIs, and a tender abscess is a typical presentation.8 Patients commonly misinterpret early skin lesions as an insect or spider bite.12,14 When cutaneous CA-MRSA presents as an abscess, an incision and drainage procedure is essential for adequate treatment of the infection. For some CA-MRSA infections, particularly those characterized by the presence of a relatively small abscess, it might be adequate to do only an incision and drainage procedure, and not administer antibiotics.8,15 However, in most instances, especially when there is an area of cellulitis around the abscess, the initiation of antibiotic therapy improves patients’ clinical outcomes.9,16
When there is no apparent drainable purulent fluid collection, which often occurs with cellulitis, antibiotics should be the mainstay of therapy. The decision about which antibiotic to start can present some challenges, because the organism causing the cellulitis usually is not identified. This is because blood cultures are positive in less than 5% of cases. Also, positive culture results from needle aspiration are only helpful from 5% to 40% of the time. Meanwhile, culture of punch biopsy specimens yields a pathogen in only 20% to 30% of cases.3,17-19
Due to increased CA-MRSA incidence, cephalexin should not be prescribed to treat cellulitis in the outpatient setting because it does not provide coverage for the pathogen.13 Instead, oral antibiotics (e.g., clindamycin or trimethoprim/sulfamethoxazole) should be prescribed. Doxycycline, minocycline, rifampin (usually prescribed in combination with fusidic acid to prevent resistance development), and linezolid are additional therapeutic options.
Trimethoprim/sulfamethoxazole and clindamycin have several advantages: good oral bioavailability, familiarity to physicians, and general affordability. A disadvantage to using both trimethoprim/sulfamethoxazole and doxycycline is that they provide inadequate coverage for group A streptococci, which are a common cause of cellulitis. Therefore, the simultaneous use of a beta-lactam antibiotic with either of these medications may improve outcomes for “nonpurulent” cellulitis.13,15 Linezolid has proven effective for skin and SSTI caused by MRSA, even though it is not bactericidal.
Excellent oral bioavailability of this drug is an attractive characteristic, as it facilitates the transition from the use of intravenous to oral antibiotic therapy later in a patient’s hospital course. Although oral linezolid has been studied in clinical trials and provides good coverage for MRSA, its use in the outpatient setting is relatively limited, largely due to its significant cost.20 In 2008, the cost of 10 days of treatment with oral linezolid was $1,286.80. In comparison, the generic trimethoprim/sulfamethox-azole cost $9.40, and generic clindamycin cost $95.10.8 The lack of routine availability in many outpatient pharmacies also hinders the widespread use of linezolid.13
To date, with the exception of linezolid, no randomized, prospective clinical trials clearly demonstrate the efficacy of the oral agents that are commonly used for the outpatient treatment of cellulitis.20
When patients require hospitalization for the optimal treatment of cellulitis, it is important to select a parenteral antibiotic that provides coverage for MRSA.8 Vancomycin, daptomycin, linezolid, and tigecycline are the most commonly used agents.6
In the inpatient setting, failure to initiate appropriate medical therapy can result in longer hospital admissions, which significantly increase inpatient costs. Inadequate antibiotic therapy creates a significant financial burden and has been associated with increased mortality.4 Historically, vancomycin is used whenever a MRSA infection is suspected. However, there is concern about the declining efficacy of vancomycin related to a gradual increase in the rate of relative resistance—a minimal inhibitory concentration (MIC) increase—in MRSA strains. This MIC creep is noted in some medical centers and can lead to a failure to respond to vancomycin.13,20
Daptomycin is rapidly bactericidal against MRSA; in some institutions, its use may be preferred over vancomycin because the former antibiotic is associated with a significantly more rapid clinical response, which may shorten the required length of hospitalization.21 The once-daily dosing requirement for daptomycin allows for ease of use in both hospital and outpatient settings, and therefore may facilitate early hospital discharge or prevent the need for hospitalization altogether. Clinical experience also suggests potential economic advantages with the use of daptomycin.22
Tigecycline is a bacteriostatic antibiotic that achieves low serum concentrations. However, it penetrates the skin well and has a similar effectiveness to combination therapy with vancomycin and aztreonam. Thus far, tigecycline is not widely used for the treatment of MRSA infections, and it has been suggested that it may be preferred for polymicrobial infections or for patients who exhibit allergies to more commonly used agents.8
When selecting an antibiotic therapy, cost considerations play an important role in the decision-making process. For intravenous agents commonly used to treat CA-MRSA infections, the 2008 cost for 10 days of treatment with generic vancomycin was $182.80; daptomycin cost $1,660.80. For tigecycline and linezolid, the same duration of treatment cost $1,362 and $1,560, respectively.8
Back to the Case
Our patient, an otherwise healthy female, presented with no apparent risk factors for developing a CA-MRSA SSTI. However, more detailed history revealed that she regularly used sports equipment at her local fitness center. Based on her clinical presentation and concerns about the high local prevalence of CA-MRSA, an incision and drainage procedure was performed, and she was started empirically on IV vancomycin. She had a positive clinical response to this treatment.
Wound culture results confirmed CA-MRSA abscess and cellulitis, susceptible to trimethoprim/sulfamethoxazole. She was discharged on the oral formulation of this antibiotic to complete a 10-day course of treatment, including the days she received intravenous antibiotics.
Few well-designed trials have compared different lengths of cellulitis therapy. Most authorities recommend five to 10 days of treatment; however, longer courses might be required for more severe or complicated diseases.
Bottom line
Because of the high prevalence of CA-MRSA, initial antibiotic therapy for the treatment of community-acquired cellulitis must provide coverage for this organism. TH
Dr. Clarke is a hospitalist and clinical instructor at Emory University School of Medicine, Atlanta. Dr. Dressler is associate professor and director of education, section of hospital medicine, and associate program director of the J. Willis Hurst Internal Medicine Residency Program. Dr. Purohit is an instructor in clinical medicine at Emory University School of Medicine.
References
- Barzilai A, Choen HA. Isolation of group A streptococci from children with perianal cellulitis and from their siblings. Pediatr Infect Dis J. 1998;17(4):358-360.
- Thorsteinsdottir B, Tleyjeh IM, Baddour LM. Abdominal wall cellulitis in the morbidly obese. Scand J Infect Dis. 2005;37(8):605-608.
- Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004;350(9):904-912.
- Edelsberg J, Berger A, Weber DJ, et al. Clinical and economic consequences of failure of initial antibiotic therapy for hospitalized patients with complicated skin and skin-structure infections. Infect Control Hosp Epidemiol. 2008;29(2):160-169.
- McNamara DR, Tleyjeh IM, Berbari EF, et al. Incidence of lower extremity cellulitis: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2007;82(7):817-821.
- Moellering RC. Current treatment options for community-acquired methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2008;46(7):1032-1037.
- Chambers HF. The changing epidemiology of Staphylococcus aureus. Emerg Infect Dis. 2001;7(2):178-182.
- Moellering RC. A 39-year-old man with a skin infection. JAMA. 2008;299(1):79-87
- Ruhe J, Smith N, Bradsher RW, Menon A. Community-onset methicillin-resistant Staphylococcus aureus skin and soft tissue infections: impact of antimicrobial therapy on outcome. Clin Infect Dis. 2007;44(6):777-784.
- David MZ, Glikman D, Crawford SE, et al. What is community-associated methicillin-resistant Staphylococcus aureus? J Infect Dis. 2008;197(9):1235-1243.
- Iyer S, Jones DH. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: a retrospective analysis of clinical presentation and treatment of a local outbreak. J Am Acad Dermatol. 2004;50(6):854-858.
- Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison—Mississippi, 2000. MMWR Morb Mortal Wkly Rep. 2001;50(42):919-922.
- Daum RS. Clinical practice. Skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. N Engl J Med. 2007;357(4):380-390.
- Dominguez TJ. It’s not a spider bite, it’s community-acquired methicillin-resistant Staphylococcus aureus. J Am Board Fam Pract. 2004;17(3):220-226.
- Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666-674.
- Jetton L. Therapy for methicillin-resistant Staphylococcus aureus. N Engl J Med. 2006;355(20):2153-2155.
- Hook EW, Hooton TM, Horton CA, et al. Microbiologic evaluation of cutaneous cellulitis in adults. Arch Intern Med. 1986;146(2):295-297.
- Duvanel T, Auckenthaler R, Rohner P, Harms M, Saurat JH. Quantitative cultures of biopsy specimens from cutaneous cellulitis. Arch Intern Med. 1989;149(2):293-296.
- Newell PM, Norden CW. Value of needle aspiration in bacteriologic diagnosis of cellulitis in adults. J Clin Microbiol. 1988; 26(3):401-404.
- Loffler CA, Macdougall C. Update on prevalence and treatment of methicillin-resistant Staphylococcus aureus infections. Expert Rev Anti Infect Ther. 2007;5(6):961-981.
- Davis SL, McKinnon PS, Hall LM, et al. Daptomycin versus vancomycin for complicated skin and skin structure infections: clinical and economic outcomes. Pharmacotherapy. 2007;27(12):1611-1618.
- Seaton RA. Daptomycin: rationale and role in the management of skin and soft tissue infections. J Antimicrob Chemother. 2008;62(Suppl 3):iii15-23.
Case
A previously healthy 55-year-old white female presents to the ED with a three-day history of pain and erythema in her right hand. Examination reveals fluctuance as well. She is diagnosed with an abscess with surrounding cellulitis. The abscess is incised, drained, and cultured, and she is sent home on oral trimethoprim/sulfamethoxazole. The following day, her cellulitis has worsened. She is hospitalized and commenced on intravenous vancomycin. What is the best empiric therapy for community-acquired cellulitis?
Background
Cellulitis is defined as a skin and soft-tissue infection (SSTI), which develops as a result of bacterial entry via breaches in the skin barrier. Typically, it involves the dermis and subcutaneous tissue, and is associated with local tenderness, erythema, swelling and fever. Cellulitis usually affects the lower extremities, but can affect other locations resulting in diagnoses such as periorbital, abdominal wall, buccal, and perianal cellulitis.1,2
Gram-positive organisms, especially Staphylococcus aureus and beta hemolytic streptococci, are the most common causes of cellulitis. Although it is less common, cellulitis can be caused by gram-negative organisms. The recent significant increase in the prevalence of SSTIs due to community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) has led to changes in the selection of antibiotics that were most commonly utilized to empirically treat cellulitis.
The diagnosis of cellulitis is based primarily on clinical manifestations. Due to low diagnostic yields, blood cultures, needle aspiration, or punch biopsy, specimens usually are not helpful in the setting of simple cellulitis.3 Therefore, antibiotic therapy is almost universally started empirically. Starting appropriate initial antibiotic therapy improves patient outcomes by reducing mortality rates, length of stay, and inpatient costs.4
Cellulitis incidence is about two cases per 1,000 patient-years.5 This rather high incidence, coupled with escalating rates of SSTIs due to CA-MRSA, demands reliable and cost-effective treatment strategies for the management of community-acquired cellulitis.
Review of the Data
The treatment of community-acquired cellulitis was straightforward until the past decade, as physicians saw a significant increase in CA-MRSA incidence.6 MRSA was reported initially in 1961, only two years after methicillin was introduced into clinical practice.7,8 Subsequently, MRSA prevalence increased dramatically, and by the beginning of this decade, more than 50% of the Staphylococcus aureus hospital strains were resistant to methicillin.8 Furthermore, 60% to 80% of community-acquired Staphylococcus aureus strains in the U.S. are methicillin-resistant.8
The two major types of MRSA infections are healthcare-acquired (HA-MRSA) and community-acquired (CA-MRSA). The HA-MRSA infection group is further subdivided into those strains that develop during a period of hospitalization, and those that develop following contact with healthcare facilities (e.g., hospitalization or surgery within the previous year). This subgroup includes HA-MRSA infections in hemodialysis patients, residents of long-term care facilities, and individuals who have a vascular catheter or other indwelling device.9,10
CA-MRSA infections, on the other hand, occur in individuals who have not had any contact with healthcare facilities. Higher rates of CA-MRSA infection are observed in settings where individuals have close contact with each other, including military trainees, athletes involved in contact sports, patients age 65 and older, men who have sex with other men, and parenteral substance abusers.8,11-13 However, in view of the high prevalence of CA-MRSA in the U.S., most patients, including those without any apparent risk factors, are at risk.8
HA-MRSA has the ability to survive on inanimate objects for extended time periods, increasing the likelihood of transmission to persons who come into contact with those objects. Although evidence has not confirmed that CA-MRSA has a similar capacity, it seems plausible that such spread does contribute to the propagation of CA-MRSA.12
The increasing importance of CA-MRSA also is evident in hospital settings, where it is replacing HA-MRSA as the most common type of Staphylococcus aureus. Since CA-MRSA tends to be susceptible to a larger number of antibiotics than HA-MRSA is, this has led to a reduced incidence of multidrug resistance. Fortunately, unlike HA-MRSA, CA-MRSA is susceptible to non-beta-lactam antibiotics, including tetracyclines, sulfonamides, and clindamycin.9
CA-MRSA most often causes SSTIs, and a tender abscess is a typical presentation.8 Patients commonly misinterpret early skin lesions as an insect or spider bite.12,14 When cutaneous CA-MRSA presents as an abscess, an incision and drainage procedure is essential for adequate treatment of the infection. For some CA-MRSA infections, particularly those characterized by the presence of a relatively small abscess, it might be adequate to do only an incision and drainage procedure, and not administer antibiotics.8,15 However, in most instances, especially when there is an area of cellulitis around the abscess, the initiation of antibiotic therapy improves patients’ clinical outcomes.9,16
When there is no apparent drainable purulent fluid collection, which often occurs with cellulitis, antibiotics should be the mainstay of therapy. The decision about which antibiotic to start can present some challenges, because the organism causing the cellulitis usually is not identified. This is because blood cultures are positive in less than 5% of cases. Also, positive culture results from needle aspiration are only helpful from 5% to 40% of the time. Meanwhile, culture of punch biopsy specimens yields a pathogen in only 20% to 30% of cases.3,17-19
Due to increased CA-MRSA incidence, cephalexin should not be prescribed to treat cellulitis in the outpatient setting because it does not provide coverage for the pathogen.13 Instead, oral antibiotics (e.g., clindamycin or trimethoprim/sulfamethoxazole) should be prescribed. Doxycycline, minocycline, rifampin (usually prescribed in combination with fusidic acid to prevent resistance development), and linezolid are additional therapeutic options.
Trimethoprim/sulfamethoxazole and clindamycin have several advantages: good oral bioavailability, familiarity to physicians, and general affordability. A disadvantage to using both trimethoprim/sulfamethoxazole and doxycycline is that they provide inadequate coverage for group A streptococci, which are a common cause of cellulitis. Therefore, the simultaneous use of a beta-lactam antibiotic with either of these medications may improve outcomes for “nonpurulent” cellulitis.13,15 Linezolid has proven effective for skin and SSTI caused by MRSA, even though it is not bactericidal.
Excellent oral bioavailability of this drug is an attractive characteristic, as it facilitates the transition from the use of intravenous to oral antibiotic therapy later in a patient’s hospital course. Although oral linezolid has been studied in clinical trials and provides good coverage for MRSA, its use in the outpatient setting is relatively limited, largely due to its significant cost.20 In 2008, the cost of 10 days of treatment with oral linezolid was $1,286.80. In comparison, the generic trimethoprim/sulfamethox-azole cost $9.40, and generic clindamycin cost $95.10.8 The lack of routine availability in many outpatient pharmacies also hinders the widespread use of linezolid.13
To date, with the exception of linezolid, no randomized, prospective clinical trials clearly demonstrate the efficacy of the oral agents that are commonly used for the outpatient treatment of cellulitis.20
When patients require hospitalization for the optimal treatment of cellulitis, it is important to select a parenteral antibiotic that provides coverage for MRSA.8 Vancomycin, daptomycin, linezolid, and tigecycline are the most commonly used agents.6
In the inpatient setting, failure to initiate appropriate medical therapy can result in longer hospital admissions, which significantly increase inpatient costs. Inadequate antibiotic therapy creates a significant financial burden and has been associated with increased mortality.4 Historically, vancomycin is used whenever a MRSA infection is suspected. However, there is concern about the declining efficacy of vancomycin related to a gradual increase in the rate of relative resistance—a minimal inhibitory concentration (MIC) increase—in MRSA strains. This MIC creep is noted in some medical centers and can lead to a failure to respond to vancomycin.13,20
Daptomycin is rapidly bactericidal against MRSA; in some institutions, its use may be preferred over vancomycin because the former antibiotic is associated with a significantly more rapid clinical response, which may shorten the required length of hospitalization.21 The once-daily dosing requirement for daptomycin allows for ease of use in both hospital and outpatient settings, and therefore may facilitate early hospital discharge or prevent the need for hospitalization altogether. Clinical experience also suggests potential economic advantages with the use of daptomycin.22
Tigecycline is a bacteriostatic antibiotic that achieves low serum concentrations. However, it penetrates the skin well and has a similar effectiveness to combination therapy with vancomycin and aztreonam. Thus far, tigecycline is not widely used for the treatment of MRSA infections, and it has been suggested that it may be preferred for polymicrobial infections or for patients who exhibit allergies to more commonly used agents.8
When selecting an antibiotic therapy, cost considerations play an important role in the decision-making process. For intravenous agents commonly used to treat CA-MRSA infections, the 2008 cost for 10 days of treatment with generic vancomycin was $182.80; daptomycin cost $1,660.80. For tigecycline and linezolid, the same duration of treatment cost $1,362 and $1,560, respectively.8
Back to the Case
Our patient, an otherwise healthy female, presented with no apparent risk factors for developing a CA-MRSA SSTI. However, more detailed history revealed that she regularly used sports equipment at her local fitness center. Based on her clinical presentation and concerns about the high local prevalence of CA-MRSA, an incision and drainage procedure was performed, and she was started empirically on IV vancomycin. She had a positive clinical response to this treatment.
Wound culture results confirmed CA-MRSA abscess and cellulitis, susceptible to trimethoprim/sulfamethoxazole. She was discharged on the oral formulation of this antibiotic to complete a 10-day course of treatment, including the days she received intravenous antibiotics.
Few well-designed trials have compared different lengths of cellulitis therapy. Most authorities recommend five to 10 days of treatment; however, longer courses might be required for more severe or complicated diseases.
Bottom line
Because of the high prevalence of CA-MRSA, initial antibiotic therapy for the treatment of community-acquired cellulitis must provide coverage for this organism. TH
Dr. Clarke is a hospitalist and clinical instructor at Emory University School of Medicine, Atlanta. Dr. Dressler is associate professor and director of education, section of hospital medicine, and associate program director of the J. Willis Hurst Internal Medicine Residency Program. Dr. Purohit is an instructor in clinical medicine at Emory University School of Medicine.
References
- Barzilai A, Choen HA. Isolation of group A streptococci from children with perianal cellulitis and from their siblings. Pediatr Infect Dis J. 1998;17(4):358-360.
- Thorsteinsdottir B, Tleyjeh IM, Baddour LM. Abdominal wall cellulitis in the morbidly obese. Scand J Infect Dis. 2005;37(8):605-608.
- Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004;350(9):904-912.
- Edelsberg J, Berger A, Weber DJ, et al. Clinical and economic consequences of failure of initial antibiotic therapy for hospitalized patients with complicated skin and skin-structure infections. Infect Control Hosp Epidemiol. 2008;29(2):160-169.
- McNamara DR, Tleyjeh IM, Berbari EF, et al. Incidence of lower extremity cellulitis: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2007;82(7):817-821.
- Moellering RC. Current treatment options for community-acquired methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2008;46(7):1032-1037.
- Chambers HF. The changing epidemiology of Staphylococcus aureus. Emerg Infect Dis. 2001;7(2):178-182.
- Moellering RC. A 39-year-old man with a skin infection. JAMA. 2008;299(1):79-87
- Ruhe J, Smith N, Bradsher RW, Menon A. Community-onset methicillin-resistant Staphylococcus aureus skin and soft tissue infections: impact of antimicrobial therapy on outcome. Clin Infect Dis. 2007;44(6):777-784.
- David MZ, Glikman D, Crawford SE, et al. What is community-associated methicillin-resistant Staphylococcus aureus? J Infect Dis. 2008;197(9):1235-1243.
- Iyer S, Jones DH. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: a retrospective analysis of clinical presentation and treatment of a local outbreak. J Am Acad Dermatol. 2004;50(6):854-858.
- Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison—Mississippi, 2000. MMWR Morb Mortal Wkly Rep. 2001;50(42):919-922.
- Daum RS. Clinical practice. Skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. N Engl J Med. 2007;357(4):380-390.
- Dominguez TJ. It’s not a spider bite, it’s community-acquired methicillin-resistant Staphylococcus aureus. J Am Board Fam Pract. 2004;17(3):220-226.
- Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666-674.
- Jetton L. Therapy for methicillin-resistant Staphylococcus aureus. N Engl J Med. 2006;355(20):2153-2155.
- Hook EW, Hooton TM, Horton CA, et al. Microbiologic evaluation of cutaneous cellulitis in adults. Arch Intern Med. 1986;146(2):295-297.
- Duvanel T, Auckenthaler R, Rohner P, Harms M, Saurat JH. Quantitative cultures of biopsy specimens from cutaneous cellulitis. Arch Intern Med. 1989;149(2):293-296.
- Newell PM, Norden CW. Value of needle aspiration in bacteriologic diagnosis of cellulitis in adults. J Clin Microbiol. 1988; 26(3):401-404.
- Loffler CA, Macdougall C. Update on prevalence and treatment of methicillin-resistant Staphylococcus aureus infections. Expert Rev Anti Infect Ther. 2007;5(6):961-981.
- Davis SL, McKinnon PS, Hall LM, et al. Daptomycin versus vancomycin for complicated skin and skin structure infections: clinical and economic outcomes. Pharmacotherapy. 2007;27(12):1611-1618.
- Seaton RA. Daptomycin: rationale and role in the management of skin and soft tissue infections. J Antimicrob Chemother. 2008;62(Suppl 3):iii15-23.
Increased Attention
According to the American Diabetes Association, a normal fasting plasma glucose (FPG) level is less than 100 mg/dl; impaired fasting glucose (IFG) is defined as an FPG from 100 to 125 mg/dl; and any patient with an FPG greater than or equal to 126 mg/dL carries a provisional diagnosis of diabetes.1 When the oral glucose tolerance test is used for evaluation, similar definitions exist. Patients with IFG or impaired glucose tolerance (IGT) have “pre-diabetes,” and are at a high risk for developing diabetes. Elevated blood glucose levels can have major consequences, particularly in high-risk populations.2
Macrovascular and microvascular complications, impaired wound healing, and a compromised immune system can occur in the setting of sustained, elevated blood glucose concentrations. Aside from patients with diabetes who have elevated blood glucose levels, schizophrenic patients might be predisposed to glucose intolerance and diabetes independent of treatment.3
It is not known whether IGT seen in schizophrenics is due to lifestyle risk factors (e.g., smoking, poor diet, being overweight, lack of exercise) or some genetic or biological component of the disease. However, this is complicated by the fact that many of these patients are treated with second-generation antipsychotics (SGAs), which might increase the risk of developing diabetes.4 Because of this, a warning regarding the risk of developing hyperglycemia and diabetes was mandated by the Food and Drug Administration (FDA) for SGA manufacturers.5
Hyperglycemia symptoms include polyuria, polydipsia, weight loss (sometimes with polyphagia), and blurred vision. Impairment of growth and susceptibility to certain infections might occur with chronic hyperglycemia. Hyperglycemia with ketoacidosis or the nonketotic hyperosmolar syndrome are acute, life-threatening consequences of uncontrolled diabetes. It is important for hospitalists and other healthcare professionals to be aware of drugs that can cause hyperglycemia or impair glucose tolerance. In some cases, the drug can be continued; in other cases, an alternate agent should be provided if necessary for patient management.
Certain drugs and drug classes known to cause hyperglycemia include: thiazide diuretics, glucocorticoids, oral contraceptives and sex hormones (e.g., testosterone), protease inhibitors, SGAs, thyroid hormone, phenytoin, niacin/nicotinic acid, diazoxide, and alfa-interferon.1-3,6
Limited evidence exists for some other agents/classes, including: asparaginase, beta-agonists, beta-blockers, calcium channel blockers, clonidine, cyclosporine, levodopa, lithium, minoxidil, phenothiazines, and others.7 The Seventh Report of the Joint National Committee (JNC 7) recommends thiazide diuretics as a first-line treatment for most patients with Stage 1 hypertension, alone or in combination for patients with diabetes.8 These thiazide doses tend to be smaller and, therefore, tend to have minimal effects on blood glucose levels.
In 2004, a consensus guideline was developed on antipsychotic drugs, obesity, and diabetes.9 It describes baseline and followup monitoring of patients treated with SGAs. The baseline includes personal/family history, weight/body mass index, waist circumference, blood pressure, FPG, and a fasting lipid profile. Monitoring of these parameters is then designated at specified times throughout treatment (e.g., weeks four, eight, 12, etc.). Haupt et al recently compared monitoring of lipids and glucose in a population of insured patients receiving SGAs in a retrospective cohort of patients pre- and post-guideline.10 Baseline lipid and glucose testing rates increased minimally post-guideline versus pre-guideline.
The results of this study demonstrate that even though monitoring guidelines to prevent potentially adverse outcomes in a patient population at high risk for developing adverse outcomes are available, clinicians do not always follow them. In order to improve patient outcomes, identified at-risk populations (e.g., patients receiving SGAs) need to be more closely evaluated and monitored throughout therapy to prevent IGT and/or diabetes. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2009;32:S62-S67.
- Luna B, Feinglos MN. Drug-induced hyperglycemia. JAMA. 2001;286:1945-1948.
- Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(Suppl 1):20-27.
- Tahir R. Metabolic effects of atypical antipsychotics. US Pharm. 2007;32:HS3-HS14.
- Warning about hyperglycemia and atypical antipsychotic drugs. U.S. Food & Drug Administration Web site. Available at: www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/printer.cfm?id=229. Accessed March 31, 2009.
- Kaufman MB, Simionatto C. A review of protease inhibitor-induced hyperglycemia. Pharmacotherapy. 1999;19:114-117.
- Pandit MK, Burke J, Gustafson AB, Minocha A, Peiris AN. Drug-induced disorders of glucose tolerance. Ann Intern Med. 1993;118:529-539.
- Chobanian AV, Bakris GL, Clack HR, et al. The seventh report of the joint national committee on prevention, detection, evaluations, and treatment of high blood pressure. JAMA. 2003;289:2560-2572.
- American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596-601.
- Haupt DW, Rosenblatt LC, Kim E, Baker RA, Whitehead R, Newcomer JW. Prevalence and predictors of lipid and glucose monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166:345-353.
- FDA approves generic treatment for emesis. Drug Store News Web site. Available at: www.drugstorenews.com/story.aspx?id=96143. Accessed March 6, 2009.
- Aurobindo Pharma gets tentative approval from US FDA for tenofovir disoproxil fumarate tabs. RTT News Web site. Available at: www.rttnews.com/ArticleView.aspx?id=860423. Accessed March 4, 2009.
- Teva announces approval and launch of generic Topamax tablets.Teva Web site. Available at: www.tevapharm.com/pr/2009/pr_835.asp. Accessed March 30, 2009.
- FDA approves Symbicort for chronic obstructive pulmonary disease (COPD). AstraZeneca Web site. Available at: www.astrazeneca-us.com/about-astrazenecaus/newsroom/all/4939997?itemId=4939997. Accessed June 5, 2009.
- Copaxone approved by the FDA for patients with a first clinical event suggestive of multiple sclerosis. Teva Web site. Available at: www.tevapharm.com/pr/2009/ pr_826.asp? Accessed June 5, 2009.
- Todoruk M. FDA approves new use for Wyeth’s Tygacil antibiotic. Available at: www.firstwordplus.com/Fws.do?articleid=CF71DE6056CE4120A295243AE2D6EC00. Accessed March 25, 2009.
- FDA Web site. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2009/021821s013s017s018lbl.pdf. Accessed June 5, 2009.
- Transdermal drug patches with metallic backings. FDA Web site. Available at: www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm111493.htm. Accessed June 5, 2009.
- FDA warns about risk of wearing medicated patches during MRIs. FDA Web site. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149537.htm. Accessed March 6, 2009.
- FDA requires boxed warning and risk mitigation strategy for metoclopramide-containing drugs. FDA Web site. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149533.htm. Accessed March 4, 2009.
- Zonisamide (marketed as Zonegran, and generics). FDA Web site. Available at: www.fda.gov/ForConsumers/ConsumerUpdates/ucm095251.htm. Accessed March 4, 2009.
According to the American Diabetes Association, a normal fasting plasma glucose (FPG) level is less than 100 mg/dl; impaired fasting glucose (IFG) is defined as an FPG from 100 to 125 mg/dl; and any patient with an FPG greater than or equal to 126 mg/dL carries a provisional diagnosis of diabetes.1 When the oral glucose tolerance test is used for evaluation, similar definitions exist. Patients with IFG or impaired glucose tolerance (IGT) have “pre-diabetes,” and are at a high risk for developing diabetes. Elevated blood glucose levels can have major consequences, particularly in high-risk populations.2
Macrovascular and microvascular complications, impaired wound healing, and a compromised immune system can occur in the setting of sustained, elevated blood glucose concentrations. Aside from patients with diabetes who have elevated blood glucose levels, schizophrenic patients might be predisposed to glucose intolerance and diabetes independent of treatment.3
It is not known whether IGT seen in schizophrenics is due to lifestyle risk factors (e.g., smoking, poor diet, being overweight, lack of exercise) or some genetic or biological component of the disease. However, this is complicated by the fact that many of these patients are treated with second-generation antipsychotics (SGAs), which might increase the risk of developing diabetes.4 Because of this, a warning regarding the risk of developing hyperglycemia and diabetes was mandated by the Food and Drug Administration (FDA) for SGA manufacturers.5
Hyperglycemia symptoms include polyuria, polydipsia, weight loss (sometimes with polyphagia), and blurred vision. Impairment of growth and susceptibility to certain infections might occur with chronic hyperglycemia. Hyperglycemia with ketoacidosis or the nonketotic hyperosmolar syndrome are acute, life-threatening consequences of uncontrolled diabetes. It is important for hospitalists and other healthcare professionals to be aware of drugs that can cause hyperglycemia or impair glucose tolerance. In some cases, the drug can be continued; in other cases, an alternate agent should be provided if necessary for patient management.
Certain drugs and drug classes known to cause hyperglycemia include: thiazide diuretics, glucocorticoids, oral contraceptives and sex hormones (e.g., testosterone), protease inhibitors, SGAs, thyroid hormone, phenytoin, niacin/nicotinic acid, diazoxide, and alfa-interferon.1-3,6
Limited evidence exists for some other agents/classes, including: asparaginase, beta-agonists, beta-blockers, calcium channel blockers, clonidine, cyclosporine, levodopa, lithium, minoxidil, phenothiazines, and others.7 The Seventh Report of the Joint National Committee (JNC 7) recommends thiazide diuretics as a first-line treatment for most patients with Stage 1 hypertension, alone or in combination for patients with diabetes.8 These thiazide doses tend to be smaller and, therefore, tend to have minimal effects on blood glucose levels.
In 2004, a consensus guideline was developed on antipsychotic drugs, obesity, and diabetes.9 It describes baseline and followup monitoring of patients treated with SGAs. The baseline includes personal/family history, weight/body mass index, waist circumference, blood pressure, FPG, and a fasting lipid profile. Monitoring of these parameters is then designated at specified times throughout treatment (e.g., weeks four, eight, 12, etc.). Haupt et al recently compared monitoring of lipids and glucose in a population of insured patients receiving SGAs in a retrospective cohort of patients pre- and post-guideline.10 Baseline lipid and glucose testing rates increased minimally post-guideline versus pre-guideline.
The results of this study demonstrate that even though monitoring guidelines to prevent potentially adverse outcomes in a patient population at high risk for developing adverse outcomes are available, clinicians do not always follow them. In order to improve patient outcomes, identified at-risk populations (e.g., patients receiving SGAs) need to be more closely evaluated and monitored throughout therapy to prevent IGT and/or diabetes. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2009;32:S62-S67.
- Luna B, Feinglos MN. Drug-induced hyperglycemia. JAMA. 2001;286:1945-1948.
- Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(Suppl 1):20-27.
- Tahir R. Metabolic effects of atypical antipsychotics. US Pharm. 2007;32:HS3-HS14.
- Warning about hyperglycemia and atypical antipsychotic drugs. U.S. Food & Drug Administration Web site. Available at: www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/printer.cfm?id=229. Accessed March 31, 2009.
- Kaufman MB, Simionatto C. A review of protease inhibitor-induced hyperglycemia. Pharmacotherapy. 1999;19:114-117.
- Pandit MK, Burke J, Gustafson AB, Minocha A, Peiris AN. Drug-induced disorders of glucose tolerance. Ann Intern Med. 1993;118:529-539.
- Chobanian AV, Bakris GL, Clack HR, et al. The seventh report of the joint national committee on prevention, detection, evaluations, and treatment of high blood pressure. JAMA. 2003;289:2560-2572.
- American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596-601.
- Haupt DW, Rosenblatt LC, Kim E, Baker RA, Whitehead R, Newcomer JW. Prevalence and predictors of lipid and glucose monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166:345-353.
- FDA approves generic treatment for emesis. Drug Store News Web site. Available at: www.drugstorenews.com/story.aspx?id=96143. Accessed March 6, 2009.
- Aurobindo Pharma gets tentative approval from US FDA for tenofovir disoproxil fumarate tabs. RTT News Web site. Available at: www.rttnews.com/ArticleView.aspx?id=860423. Accessed March 4, 2009.
- Teva announces approval and launch of generic Topamax tablets.Teva Web site. Available at: www.tevapharm.com/pr/2009/pr_835.asp. Accessed March 30, 2009.
- FDA approves Symbicort for chronic obstructive pulmonary disease (COPD). AstraZeneca Web site. Available at: www.astrazeneca-us.com/about-astrazenecaus/newsroom/all/4939997?itemId=4939997. Accessed June 5, 2009.
- Copaxone approved by the FDA for patients with a first clinical event suggestive of multiple sclerosis. Teva Web site. Available at: www.tevapharm.com/pr/2009/ pr_826.asp? Accessed June 5, 2009.
- Todoruk M. FDA approves new use for Wyeth’s Tygacil antibiotic. Available at: www.firstwordplus.com/Fws.do?articleid=CF71DE6056CE4120A295243AE2D6EC00. Accessed March 25, 2009.
- FDA Web site. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2009/021821s013s017s018lbl.pdf. Accessed June 5, 2009.
- Transdermal drug patches with metallic backings. FDA Web site. Available at: www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm111493.htm. Accessed June 5, 2009.
- FDA warns about risk of wearing medicated patches during MRIs. FDA Web site. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149537.htm. Accessed March 6, 2009.
- FDA requires boxed warning and risk mitigation strategy for metoclopramide-containing drugs. FDA Web site. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149533.htm. Accessed March 4, 2009.
- Zonisamide (marketed as Zonegran, and generics). FDA Web site. Available at: www.fda.gov/ForConsumers/ConsumerUpdates/ucm095251.htm. Accessed March 4, 2009.
According to the American Diabetes Association, a normal fasting plasma glucose (FPG) level is less than 100 mg/dl; impaired fasting glucose (IFG) is defined as an FPG from 100 to 125 mg/dl; and any patient with an FPG greater than or equal to 126 mg/dL carries a provisional diagnosis of diabetes.1 When the oral glucose tolerance test is used for evaluation, similar definitions exist. Patients with IFG or impaired glucose tolerance (IGT) have “pre-diabetes,” and are at a high risk for developing diabetes. Elevated blood glucose levels can have major consequences, particularly in high-risk populations.2
Macrovascular and microvascular complications, impaired wound healing, and a compromised immune system can occur in the setting of sustained, elevated blood glucose concentrations. Aside from patients with diabetes who have elevated blood glucose levels, schizophrenic patients might be predisposed to glucose intolerance and diabetes independent of treatment.3
It is not known whether IGT seen in schizophrenics is due to lifestyle risk factors (e.g., smoking, poor diet, being overweight, lack of exercise) or some genetic or biological component of the disease. However, this is complicated by the fact that many of these patients are treated with second-generation antipsychotics (SGAs), which might increase the risk of developing diabetes.4 Because of this, a warning regarding the risk of developing hyperglycemia and diabetes was mandated by the Food and Drug Administration (FDA) for SGA manufacturers.5
Hyperglycemia symptoms include polyuria, polydipsia, weight loss (sometimes with polyphagia), and blurred vision. Impairment of growth and susceptibility to certain infections might occur with chronic hyperglycemia. Hyperglycemia with ketoacidosis or the nonketotic hyperosmolar syndrome are acute, life-threatening consequences of uncontrolled diabetes. It is important for hospitalists and other healthcare professionals to be aware of drugs that can cause hyperglycemia or impair glucose tolerance. In some cases, the drug can be continued; in other cases, an alternate agent should be provided if necessary for patient management.
Certain drugs and drug classes known to cause hyperglycemia include: thiazide diuretics, glucocorticoids, oral contraceptives and sex hormones (e.g., testosterone), protease inhibitors, SGAs, thyroid hormone, phenytoin, niacin/nicotinic acid, diazoxide, and alfa-interferon.1-3,6
Limited evidence exists for some other agents/classes, including: asparaginase, beta-agonists, beta-blockers, calcium channel blockers, clonidine, cyclosporine, levodopa, lithium, minoxidil, phenothiazines, and others.7 The Seventh Report of the Joint National Committee (JNC 7) recommends thiazide diuretics as a first-line treatment for most patients with Stage 1 hypertension, alone or in combination for patients with diabetes.8 These thiazide doses tend to be smaller and, therefore, tend to have minimal effects on blood glucose levels.
In 2004, a consensus guideline was developed on antipsychotic drugs, obesity, and diabetes.9 It describes baseline and followup monitoring of patients treated with SGAs. The baseline includes personal/family history, weight/body mass index, waist circumference, blood pressure, FPG, and a fasting lipid profile. Monitoring of these parameters is then designated at specified times throughout treatment (e.g., weeks four, eight, 12, etc.). Haupt et al recently compared monitoring of lipids and glucose in a population of insured patients receiving SGAs in a retrospective cohort of patients pre- and post-guideline.10 Baseline lipid and glucose testing rates increased minimally post-guideline versus pre-guideline.
The results of this study demonstrate that even though monitoring guidelines to prevent potentially adverse outcomes in a patient population at high risk for developing adverse outcomes are available, clinicians do not always follow them. In order to improve patient outcomes, identified at-risk populations (e.g., patients receiving SGAs) need to be more closely evaluated and monitored throughout therapy to prevent IGT and/or diabetes. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2009;32:S62-S67.
- Luna B, Feinglos MN. Drug-induced hyperglycemia. JAMA. 2001;286:1945-1948.
- Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(Suppl 1):20-27.
- Tahir R. Metabolic effects of atypical antipsychotics. US Pharm. 2007;32:HS3-HS14.
- Warning about hyperglycemia and atypical antipsychotic drugs. U.S. Food & Drug Administration Web site. Available at: www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/printer.cfm?id=229. Accessed March 31, 2009.
- Kaufman MB, Simionatto C. A review of protease inhibitor-induced hyperglycemia. Pharmacotherapy. 1999;19:114-117.
- Pandit MK, Burke J, Gustafson AB, Minocha A, Peiris AN. Drug-induced disorders of glucose tolerance. Ann Intern Med. 1993;118:529-539.
- Chobanian AV, Bakris GL, Clack HR, et al. The seventh report of the joint national committee on prevention, detection, evaluations, and treatment of high blood pressure. JAMA. 2003;289:2560-2572.
- American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596-601.
- Haupt DW, Rosenblatt LC, Kim E, Baker RA, Whitehead R, Newcomer JW. Prevalence and predictors of lipid and glucose monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166:345-353.
- FDA approves generic treatment for emesis. Drug Store News Web site. Available at: www.drugstorenews.com/story.aspx?id=96143. Accessed March 6, 2009.
- Aurobindo Pharma gets tentative approval from US FDA for tenofovir disoproxil fumarate tabs. RTT News Web site. Available at: www.rttnews.com/ArticleView.aspx?id=860423. Accessed March 4, 2009.
- Teva announces approval and launch of generic Topamax tablets.Teva Web site. Available at: www.tevapharm.com/pr/2009/pr_835.asp. Accessed March 30, 2009.
- FDA approves Symbicort for chronic obstructive pulmonary disease (COPD). AstraZeneca Web site. Available at: www.astrazeneca-us.com/about-astrazenecaus/newsroom/all/4939997?itemId=4939997. Accessed June 5, 2009.
- Copaxone approved by the FDA for patients with a first clinical event suggestive of multiple sclerosis. Teva Web site. Available at: www.tevapharm.com/pr/2009/ pr_826.asp? Accessed June 5, 2009.
- Todoruk M. FDA approves new use for Wyeth’s Tygacil antibiotic. Available at: www.firstwordplus.com/Fws.do?articleid=CF71DE6056CE4120A295243AE2D6EC00. Accessed March 25, 2009.
- FDA Web site. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2009/021821s013s017s018lbl.pdf. Accessed June 5, 2009.
- Transdermal drug patches with metallic backings. FDA Web site. Available at: www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm111493.htm. Accessed June 5, 2009.
- FDA warns about risk of wearing medicated patches during MRIs. FDA Web site. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149537.htm. Accessed March 6, 2009.
- FDA requires boxed warning and risk mitigation strategy for metoclopramide-containing drugs. FDA Web site. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149533.htm. Accessed March 4, 2009.
- Zonisamide (marketed as Zonegran, and generics). FDA Web site. Available at: www.fda.gov/ForConsumers/ConsumerUpdates/ucm095251.htm. Accessed March 4, 2009.
In the Literature
In This Edition
Literature at a Glance: A guide to this month’s studies
- PPI use with clopidrogrel in ACS.
- Chlorhexidine sponge use reduces line infections.
- Extended thienopyridine use does not benefit DES patients.
- CABG is revascularization choice for severe CAD.
- Pre-treated CVC use reduces bloodstream infections.
- Hospitalist use grows in U.S.
- Sepsis order set improves outcomes.
- Admission day predicts acute PE mortality.
PPI Use with Clopidogrel in Acute Coronary Syndrome Is Associated with Readmissions and Mortality
Clinical question: Does concomitant use of clopidogrel and a proton pump inhibitor (PPI) following hospitalization for acute coronary syndrome (ACS) lead to adverse outcomes?
Background: Prophylactic PPIs often are prescribed with clopidogrel to reduce the risk of gastrointestinal bleeding. Mechanistic studies have shown that omeprazole decreases the platelet-inhibitory effect of clopidogrel, raising concerns that PPIs might interfere with clopidogrel’s beneficial effects. The clinical significance of this finding is unknown.
Study design: Retrospective cohort study.
Setting: 127 VA hospitals.
Synopsis: Investigators used data from the Cardiac Care Follow-up Clinical Study and VA pharmacy records to examine 8,205 male veterans who were hospitalized for ACS and treated with clopidogrel. Patients who filled prescriptions for both clopidogrel and a PPI were at significantly higher risk for death or readmission with ACS compared with those who filled prescriptions for clopidogrel only (adjusted odds ratio, 1.25; 95% confidence interval, 1.11-1.41). Patients who filled prescriptions for PPIs alone had similar risk for adverse events as those who took neither medication.
Subanalyses found similarly increased risk among patients prescribed omeprazole and rabeprazole, but those taking lanzoprazole and pantoprazole were not examined due to the small sample size. Although causality cannot be inferred from this observational study, and the risk associated with combined clopidigrel and PPI use appeared small, alternatives for gastric acid reduction exist. Thus, it may be prudent to restrict PPI use to patients who have a clear indication for their use until more definitive clinical trials can be conducted.
Bottom line: Among patients who are treated with clopidogrel for ACS, PPIs should be reserved for patients with a clear indication for gastric acid reduction and who cannot use alternative therapies.
Citation: Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301(9):937-944.
Chlorhexidine-Impregnated Sponge Use Reduces Line Infections
Clinical question: Does dressing vascular catheters with chlorhexidine gluconate-impregnated sponges (CHGIS) reduce rates of catheter-related infections, and are dressing changes every seven days inferior to every three days?
Background: Process improvement strategies—including educating providers, strictly adhering to sterile technique, and promptly removing unnecessary catheters—greatly decrease catheter-related infections. It is unclear if CHGIS dressings offer additional benefit. Also uncertain is whether weekly dressing changes are as safe as changing dressings every three days.
Study design: A 2x2 factorial, assessor-blinded, randomized controlled trial.
Setting: ICUs in three university hospitals and two general hospitals in France.
Synopsis: 1,636 French adults expected to require arterial and central venous catheters for >48 hours were randomly assigned to one of four groups. Each group received either CHGIS dressings or standard dressings, and each group had dressing changes every three or seven days. Dressings were changed sooner if soiled or nonadherent. CHGIS dressings were associated with fewer catheter-related infections than standard dressings (0.6 vs. 1.4 infections per 1,000 catheter days; P=0.03). No significant difference in rates of catheter colonization existed between the three-day and seven-day dressing change strategies (10.4 vs. 11 events per 1,000 catheter days, P>0.05).
Although microbiology assessors were blinded to patients’ status, the ICU staff was not, potentially creating experimenter bias. Approximately 30% of the venous catheters and 40% of the arterial catheters were in a femoral site. Secondary analyses found higher rates of severe dermatitis among patients with CHGIS dressings but no difference in minimal bactericidal concentration (MBC) or colonizing organisms. Preliminary calculations suggested CHGIS dressings could be cost-effective.
Bottom line: Among critically ill adults, CHGIS catheter dressings may marginally reduce catheter-related infection rates, but further evaluation is needed before this technology can be adopted widely.
Citation: Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically-ill adults: a randomized controlled trial. JAMA. 2009;301(12):1231-1241.
Thienopyridine Use Six Months after Sirolimus-Eluting Stent Implant-ation Offers No Benefit
Clinical question: What are the relative contributions of aspirin and thienopyridine on preventing stent thrombosis in patients with sirolimus-eluting stents?
Background: There are no randomized clinical trials addressing the optimal duration, or the risks associated with discontinuation, of dual-antiplatelet therapy after drug-eluting stent (DES) implantation. Nevertheless, many patients continue to be maintained on dual-antiplatelet therapy beyond one year of their index DES implantation.
Study design: Prospective multicenter observational study.
Setting: Hospitals in Japan.
Synopsis: This study observed 10,778 Japanese patients undergoing sirolimus-eluting stent implantation. Patients discontinuing both thienopyridine and aspirin had a significantly higher rate of stent thrombosis than those who continued both medications for up to 18 months. However, discontinuation of thienopyridine alone was not associated with an excess risk of stent thrombosis. Additionally, a landmark analysis of patients who were free of events at six months showed rates of death for myocardial infarction (MI) at 24 months were 4.1% for patients taking thienopyridine and 4.1% for patients not taking thienopyridine (P=0.99). Ticlodipine was the thienopyridine used by more than 95% of patients.
Hospitalists should be aware that the role thienopyridine therapy plays in reducing stent thrombosis beyond one month after implantation has not been well addressed.
Bottom line: Discontinuation of thienopyridine therapy after six months while maintaining aspirin therapy is not associated with increased risk of stent thrombosis in patients with sirolimus-eluting stents.
Citation: Kimura T, Morimoto T, Nakagawa Y, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009;119(7):987-995.
Compared with PCI, CABG Results in Lower Rates of Major Adverse Events in Severe CAD Patients
Clinical question: What is the optimal revascularization strategy for previously untreated severe coronary artery disease (CAD)?
Background: Coronary artery bypass grafting (CABG) is the treatment of choice in three-vessel and left-main CAD. However, percutaneous coronary intervention (PCI) with drug-eluting stents often is utilized despite the lack of adequately powered randomized trials.
Study design: Prospective multicenter randomized clinical trial.
Setting: 85 hospitals in Europe and the U.S.
Synopsis: 1,800 patients with an average age of 65 and previously untreated three-vessel or left-main CAD amenable to therapy with both PCI and CABG were randomized to CABG or PCI. The primary combined endpoint was a major adverse cardiac or cerebrovascular event, defined as death, stroke, MI, or repeat revascularization. PCI was associated with a significantly higher rate of major adverse cardiac or cerebrovascular events, due mostly to a higher rate of repeat revascularization (13.5% vs. 5.9%, P<0.001). At 12 months, the two groups had similar rates of death from any cause or MI, and similar rates of the combined endpoint of death from any cause, stroke, or MI; however, the rate of stroke was 1.6% higher in the CABG group.
Hospitalists should continue to favor CABG over PCI but give consideration to the risks involved with such an intervention.
Bottom line: CABG remains the revascularization choice in patients with severe CAD.
Citation: Serruys PW, Morice MC, Kappetein AP, et al. Percuta-neous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961-972.
Pre-Medicated Central Venous Catheters Reduce Risk of Catheter-Related Bloodstream Infections
Clinical question: Does pre-treating central venous catheters with anti-infective agents prevent catheter-related bloodstream infections?
Background: Use of central venous catheters (CVC) is associated with catheter-related bloodstream infection (CRBSI), with CRBSI-related mortality rates as high as 25%. Previous reviews have indicated that CVCs coated or impregnated with anti-infectives may reduce CRBSI incidence. This review integrates new trial data with information from prior reviews.
Study design: Meta-analysis of 27 randomized controlled trials.
Setting: Meta-analysis.
Synopsis: The authors report CVCs pre-treated with anti-infectives (AI-CVCs) are clinically effective in reducing the risk of CRBSI. The odds of having a CRBSI with a treated CVC versus an untreated CVC are 0.49 to 1 (95% CI, 0.37–0.64, 27 studies, fixed effects). The study also finds the use of AI-CVCs might provide a large cost savings in Great Britain. Because the findings are based on a meta-analysis, they are limited by the quality, context, and consistency of the original studies. The authors note that many of the studies had unsatisfactory descriptions of methodology. The current study is unable to separate the risk reduction attributable to AI-CVC versus that attributable to other infection control practices. Also, original data is insufficient to assess the benefits of AI-CVCs placed for longer than 12 days.
To summarize, AI-CVCs may present a means to reduce CRBSI, but more investigation of its role within infection control protocols is needed, as is investigation of longer duration of treatment.
Bottom line: Central venous catheters pre-treated with anti-infectives significantly reduce catheter-related bloodstream infections.
Citation: Hockenhull JC, Dwan KM, Smith GW, et al. The clinical effectiveness of central venous catheters treated with anti-infective agents in preventing catheter-related bloodstream infections: a systematic review. Crit Care Med. 2009;37(2):702-712.
Fivefold Increase in Hospitalists in the U.S. from 1995 to 2006
Clinical question: What is the growth rate of hospitalists and hospitalist-provided care?
Background: Survey data has shown a sharp increase in the number of hospitalists, but until now there have not been any national or population-based data on the growth of hospitalist care.
Study design: Descriptive analysis.
Setting: Medicare-enrolled patients.
Synopsis: The study is based on national Medicare data from 2.1 million admissions involving 990,785 patients in 5,800 hospitals and 120,226 general internists. It represents 5% of inpatient Medicare claims generated by general internists. The authors define “hospitalist” as a general internist who generates >90% of his or her claims from the care of hospitalized patients.
U.S. hospitals have seen substantial growth in hospitalists over the period examined. The nation saw a 500% increase in the number of general-internist hospitalists, and a 28% increase (to 37.1% in 2006 from 9.1% in 1995) in the number of Medicare patients who received care from a hospitalist. The odds that a hospitalized Medicare patient received care from a hospitalist increased 29.2% per year from 1997 to 2006. The percentage of hospitals with at least three hospitalists rose to 47.1% in 2006 from 11.6% in 1995.
This analysis might actually have underestimated HM’s growth. Analysis of Medicare claims does not identify pediatric hospitalists and hospitalists who work exclusively within HMOs. This analysis also did not include family practitioners or internal-medicine subspecialists who are hospitalists.
Bottom line: Medicare claims data confirm survey data findings: Hospitalists and hospitalist care has grown sharply over the last decade.
Citation: Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102-1012.
Standardized Order Set for Bacteremic Sepsis Improves LOS and Mortality
Clinical question: Does a standardized order set for bacteremic sepsis impact patient management and outcomes?
Background: Prompt cardiovascular resuscitation and appropriate antibiotics decrease morbidity and mortality in bacteremic sepsis. This study examined whether hospitalwide, standardized sepsis order set improved management and outcomes.
Study design: Retrospective, before-and-after study design.
Setting: 1,200-bed academic medical center.
Synopsis: Two hundred patients with bacteremic severe sepsis were randomly selected from 18 months before the order set was introduced, and 200 were selected from 18 months after the order set was introduced. Primary outcomes measured were quantity of fluid administered and appropriate initial antibiotics. Secondary outcomes measured were hospital mortality and length of stay. Patients in the “after” group received more intravenous fluid (1627±1862 ml vs. 2054±2237 ml, P=.04), more appropriate antibiotics (53.0% vs. 65.5%, P=.01), had shorter hospital stays (28.7±30.1 days vs. 22.4±20.9 days, P=.02), and decreased in-house mortality (55.0% vs. 39.5%, P =<0.01).
The retrospective design of the study limited its ability to determine causal relationship. Extensive education may have contributed to the change (Hawthorne effect). Management in the ICU and ED, not the hospital wards, was the primary reason for mortality difference.
Bottom line: A standardized order set for bacteremic sepsis was associated with increased compliance with evidence-based treatment and improved outcomes. Hospitalists should promptly treat bacteremic sepsis with appropriate fluid resuscitation and antibiotics.
Citation: Thiel SW, Asghar MF, Micek ST, Reichley RM, Doherty JA, Kollef MH. Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis. Crit Care Med. 2009;37(3):819-824.
Admission Day of the Week Predicts Mortality in Patients with Acute Pulmonary Embolus
Clinical question: Do weekend pulmonary embolus (PE) admissions have worse outcomes than weekday admissions?
Background: Studies of patients with acute cardiovascular diagnoses (e.g., stroke, cardiac arrest) have shown higher short-term mortality and longer length of stay (LOS) for weekend versus weekday admissions. PE diagnosis is complex, requiring timely testing and experienced staff who are sometimes unavailable on weekends. Optimal anticoagulation therapy also depends on provider skill.
Study design: Retrospective observational study.
Setting: 186 private Pennsylvania hospitals, January 2000 through November 2002.
Synopsis: Using the Pennsylvania Health Care Cost Containment Council database, the authors reviewed 15,531 records of patients with a primary or secondary PE diagnosis code. The primary outcome was all-cause mortality over 30 days; LOS was the secondary outcome.
Weekend admissions in the highest severity of illness risk class had higher 30-day mortality than weekday admissions. Weekend admissions were significantly more likely than weekday admissions to be clinically unstable and to have abnormal lab parameters. Adjusted for severity of illness risk class, overall mortality was 1.4% higher for weekend versus weekday admissions. All excess mortality came from the sickest group of patients. LOS did not differ.
Less-experienced caregivers or delayed diagnostic testing may play a role in poor outcomes. Patients admitted on weekends might receive delayed care from the first onset of symptoms. This is important because timely therapy has been shown to influence outcomes in acute PE. Reasons for these observed differences should be explored further to help provide more consistent PE management, regardless of admission day.
Bottom line: The sickest patients with PE admitted on weekends experienced small but significantly greater 30-day mortality compared with those admitted on weekdays.
Citation: Aujesky D, Jimenez D, Mor M, Geng M, Fine M, Ibrahim S. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119:962-968. TH
In This Edition
Literature at a Glance: A guide to this month’s studies
- PPI use with clopidrogrel in ACS.
- Chlorhexidine sponge use reduces line infections.
- Extended thienopyridine use does not benefit DES patients.
- CABG is revascularization choice for severe CAD.
- Pre-treated CVC use reduces bloodstream infections.
- Hospitalist use grows in U.S.
- Sepsis order set improves outcomes.
- Admission day predicts acute PE mortality.
PPI Use with Clopidogrel in Acute Coronary Syndrome Is Associated with Readmissions and Mortality
Clinical question: Does concomitant use of clopidogrel and a proton pump inhibitor (PPI) following hospitalization for acute coronary syndrome (ACS) lead to adverse outcomes?
Background: Prophylactic PPIs often are prescribed with clopidogrel to reduce the risk of gastrointestinal bleeding. Mechanistic studies have shown that omeprazole decreases the platelet-inhibitory effect of clopidogrel, raising concerns that PPIs might interfere with clopidogrel’s beneficial effects. The clinical significance of this finding is unknown.
Study design: Retrospective cohort study.
Setting: 127 VA hospitals.
Synopsis: Investigators used data from the Cardiac Care Follow-up Clinical Study and VA pharmacy records to examine 8,205 male veterans who were hospitalized for ACS and treated with clopidogrel. Patients who filled prescriptions for both clopidogrel and a PPI were at significantly higher risk for death or readmission with ACS compared with those who filled prescriptions for clopidogrel only (adjusted odds ratio, 1.25; 95% confidence interval, 1.11-1.41). Patients who filled prescriptions for PPIs alone had similar risk for adverse events as those who took neither medication.
Subanalyses found similarly increased risk among patients prescribed omeprazole and rabeprazole, but those taking lanzoprazole and pantoprazole were not examined due to the small sample size. Although causality cannot be inferred from this observational study, and the risk associated with combined clopidigrel and PPI use appeared small, alternatives for gastric acid reduction exist. Thus, it may be prudent to restrict PPI use to patients who have a clear indication for their use until more definitive clinical trials can be conducted.
Bottom line: Among patients who are treated with clopidogrel for ACS, PPIs should be reserved for patients with a clear indication for gastric acid reduction and who cannot use alternative therapies.
Citation: Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301(9):937-944.
Chlorhexidine-Impregnated Sponge Use Reduces Line Infections
Clinical question: Does dressing vascular catheters with chlorhexidine gluconate-impregnated sponges (CHGIS) reduce rates of catheter-related infections, and are dressing changes every seven days inferior to every three days?
Background: Process improvement strategies—including educating providers, strictly adhering to sterile technique, and promptly removing unnecessary catheters—greatly decrease catheter-related infections. It is unclear if CHGIS dressings offer additional benefit. Also uncertain is whether weekly dressing changes are as safe as changing dressings every three days.
Study design: A 2x2 factorial, assessor-blinded, randomized controlled trial.
Setting: ICUs in three university hospitals and two general hospitals in France.
Synopsis: 1,636 French adults expected to require arterial and central venous catheters for >48 hours were randomly assigned to one of four groups. Each group received either CHGIS dressings or standard dressings, and each group had dressing changes every three or seven days. Dressings were changed sooner if soiled or nonadherent. CHGIS dressings were associated with fewer catheter-related infections than standard dressings (0.6 vs. 1.4 infections per 1,000 catheter days; P=0.03). No significant difference in rates of catheter colonization existed between the three-day and seven-day dressing change strategies (10.4 vs. 11 events per 1,000 catheter days, P>0.05).
Although microbiology assessors were blinded to patients’ status, the ICU staff was not, potentially creating experimenter bias. Approximately 30% of the venous catheters and 40% of the arterial catheters were in a femoral site. Secondary analyses found higher rates of severe dermatitis among patients with CHGIS dressings but no difference in minimal bactericidal concentration (MBC) or colonizing organisms. Preliminary calculations suggested CHGIS dressings could be cost-effective.
Bottom line: Among critically ill adults, CHGIS catheter dressings may marginally reduce catheter-related infection rates, but further evaluation is needed before this technology can be adopted widely.
Citation: Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically-ill adults: a randomized controlled trial. JAMA. 2009;301(12):1231-1241.
Thienopyridine Use Six Months after Sirolimus-Eluting Stent Implant-ation Offers No Benefit
Clinical question: What are the relative contributions of aspirin and thienopyridine on preventing stent thrombosis in patients with sirolimus-eluting stents?
Background: There are no randomized clinical trials addressing the optimal duration, or the risks associated with discontinuation, of dual-antiplatelet therapy after drug-eluting stent (DES) implantation. Nevertheless, many patients continue to be maintained on dual-antiplatelet therapy beyond one year of their index DES implantation.
Study design: Prospective multicenter observational study.
Setting: Hospitals in Japan.
Synopsis: This study observed 10,778 Japanese patients undergoing sirolimus-eluting stent implantation. Patients discontinuing both thienopyridine and aspirin had a significantly higher rate of stent thrombosis than those who continued both medications for up to 18 months. However, discontinuation of thienopyridine alone was not associated with an excess risk of stent thrombosis. Additionally, a landmark analysis of patients who were free of events at six months showed rates of death for myocardial infarction (MI) at 24 months were 4.1% for patients taking thienopyridine and 4.1% for patients not taking thienopyridine (P=0.99). Ticlodipine was the thienopyridine used by more than 95% of patients.
Hospitalists should be aware that the role thienopyridine therapy plays in reducing stent thrombosis beyond one month after implantation has not been well addressed.
Bottom line: Discontinuation of thienopyridine therapy after six months while maintaining aspirin therapy is not associated with increased risk of stent thrombosis in patients with sirolimus-eluting stents.
Citation: Kimura T, Morimoto T, Nakagawa Y, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009;119(7):987-995.
Compared with PCI, CABG Results in Lower Rates of Major Adverse Events in Severe CAD Patients
Clinical question: What is the optimal revascularization strategy for previously untreated severe coronary artery disease (CAD)?
Background: Coronary artery bypass grafting (CABG) is the treatment of choice in three-vessel and left-main CAD. However, percutaneous coronary intervention (PCI) with drug-eluting stents often is utilized despite the lack of adequately powered randomized trials.
Study design: Prospective multicenter randomized clinical trial.
Setting: 85 hospitals in Europe and the U.S.
Synopsis: 1,800 patients with an average age of 65 and previously untreated three-vessel or left-main CAD amenable to therapy with both PCI and CABG were randomized to CABG or PCI. The primary combined endpoint was a major adverse cardiac or cerebrovascular event, defined as death, stroke, MI, or repeat revascularization. PCI was associated with a significantly higher rate of major adverse cardiac or cerebrovascular events, due mostly to a higher rate of repeat revascularization (13.5% vs. 5.9%, P<0.001). At 12 months, the two groups had similar rates of death from any cause or MI, and similar rates of the combined endpoint of death from any cause, stroke, or MI; however, the rate of stroke was 1.6% higher in the CABG group.
Hospitalists should continue to favor CABG over PCI but give consideration to the risks involved with such an intervention.
Bottom line: CABG remains the revascularization choice in patients with severe CAD.
Citation: Serruys PW, Morice MC, Kappetein AP, et al. Percuta-neous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961-972.
Pre-Medicated Central Venous Catheters Reduce Risk of Catheter-Related Bloodstream Infections
Clinical question: Does pre-treating central venous catheters with anti-infective agents prevent catheter-related bloodstream infections?
Background: Use of central venous catheters (CVC) is associated with catheter-related bloodstream infection (CRBSI), with CRBSI-related mortality rates as high as 25%. Previous reviews have indicated that CVCs coated or impregnated with anti-infectives may reduce CRBSI incidence. This review integrates new trial data with information from prior reviews.
Study design: Meta-analysis of 27 randomized controlled trials.
Setting: Meta-analysis.
Synopsis: The authors report CVCs pre-treated with anti-infectives (AI-CVCs) are clinically effective in reducing the risk of CRBSI. The odds of having a CRBSI with a treated CVC versus an untreated CVC are 0.49 to 1 (95% CI, 0.37–0.64, 27 studies, fixed effects). The study also finds the use of AI-CVCs might provide a large cost savings in Great Britain. Because the findings are based on a meta-analysis, they are limited by the quality, context, and consistency of the original studies. The authors note that many of the studies had unsatisfactory descriptions of methodology. The current study is unable to separate the risk reduction attributable to AI-CVC versus that attributable to other infection control practices. Also, original data is insufficient to assess the benefits of AI-CVCs placed for longer than 12 days.
To summarize, AI-CVCs may present a means to reduce CRBSI, but more investigation of its role within infection control protocols is needed, as is investigation of longer duration of treatment.
Bottom line: Central venous catheters pre-treated with anti-infectives significantly reduce catheter-related bloodstream infections.
Citation: Hockenhull JC, Dwan KM, Smith GW, et al. The clinical effectiveness of central venous catheters treated with anti-infective agents in preventing catheter-related bloodstream infections: a systematic review. Crit Care Med. 2009;37(2):702-712.
Fivefold Increase in Hospitalists in the U.S. from 1995 to 2006
Clinical question: What is the growth rate of hospitalists and hospitalist-provided care?
Background: Survey data has shown a sharp increase in the number of hospitalists, but until now there have not been any national or population-based data on the growth of hospitalist care.
Study design: Descriptive analysis.
Setting: Medicare-enrolled patients.
Synopsis: The study is based on national Medicare data from 2.1 million admissions involving 990,785 patients in 5,800 hospitals and 120,226 general internists. It represents 5% of inpatient Medicare claims generated by general internists. The authors define “hospitalist” as a general internist who generates >90% of his or her claims from the care of hospitalized patients.
U.S. hospitals have seen substantial growth in hospitalists over the period examined. The nation saw a 500% increase in the number of general-internist hospitalists, and a 28% increase (to 37.1% in 2006 from 9.1% in 1995) in the number of Medicare patients who received care from a hospitalist. The odds that a hospitalized Medicare patient received care from a hospitalist increased 29.2% per year from 1997 to 2006. The percentage of hospitals with at least three hospitalists rose to 47.1% in 2006 from 11.6% in 1995.
This analysis might actually have underestimated HM’s growth. Analysis of Medicare claims does not identify pediatric hospitalists and hospitalists who work exclusively within HMOs. This analysis also did not include family practitioners or internal-medicine subspecialists who are hospitalists.
Bottom line: Medicare claims data confirm survey data findings: Hospitalists and hospitalist care has grown sharply over the last decade.
Citation: Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102-1012.
Standardized Order Set for Bacteremic Sepsis Improves LOS and Mortality
Clinical question: Does a standardized order set for bacteremic sepsis impact patient management and outcomes?
Background: Prompt cardiovascular resuscitation and appropriate antibiotics decrease morbidity and mortality in bacteremic sepsis. This study examined whether hospitalwide, standardized sepsis order set improved management and outcomes.
Study design: Retrospective, before-and-after study design.
Setting: 1,200-bed academic medical center.
Synopsis: Two hundred patients with bacteremic severe sepsis were randomly selected from 18 months before the order set was introduced, and 200 were selected from 18 months after the order set was introduced. Primary outcomes measured were quantity of fluid administered and appropriate initial antibiotics. Secondary outcomes measured were hospital mortality and length of stay. Patients in the “after” group received more intravenous fluid (1627±1862 ml vs. 2054±2237 ml, P=.04), more appropriate antibiotics (53.0% vs. 65.5%, P=.01), had shorter hospital stays (28.7±30.1 days vs. 22.4±20.9 days, P=.02), and decreased in-house mortality (55.0% vs. 39.5%, P =<0.01).
The retrospective design of the study limited its ability to determine causal relationship. Extensive education may have contributed to the change (Hawthorne effect). Management in the ICU and ED, not the hospital wards, was the primary reason for mortality difference.
Bottom line: A standardized order set for bacteremic sepsis was associated with increased compliance with evidence-based treatment and improved outcomes. Hospitalists should promptly treat bacteremic sepsis with appropriate fluid resuscitation and antibiotics.
Citation: Thiel SW, Asghar MF, Micek ST, Reichley RM, Doherty JA, Kollef MH. Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis. Crit Care Med. 2009;37(3):819-824.
Admission Day of the Week Predicts Mortality in Patients with Acute Pulmonary Embolus
Clinical question: Do weekend pulmonary embolus (PE) admissions have worse outcomes than weekday admissions?
Background: Studies of patients with acute cardiovascular diagnoses (e.g., stroke, cardiac arrest) have shown higher short-term mortality and longer length of stay (LOS) for weekend versus weekday admissions. PE diagnosis is complex, requiring timely testing and experienced staff who are sometimes unavailable on weekends. Optimal anticoagulation therapy also depends on provider skill.
Study design: Retrospective observational study.
Setting: 186 private Pennsylvania hospitals, January 2000 through November 2002.
Synopsis: Using the Pennsylvania Health Care Cost Containment Council database, the authors reviewed 15,531 records of patients with a primary or secondary PE diagnosis code. The primary outcome was all-cause mortality over 30 days; LOS was the secondary outcome.
Weekend admissions in the highest severity of illness risk class had higher 30-day mortality than weekday admissions. Weekend admissions were significantly more likely than weekday admissions to be clinically unstable and to have abnormal lab parameters. Adjusted for severity of illness risk class, overall mortality was 1.4% higher for weekend versus weekday admissions. All excess mortality came from the sickest group of patients. LOS did not differ.
Less-experienced caregivers or delayed diagnostic testing may play a role in poor outcomes. Patients admitted on weekends might receive delayed care from the first onset of symptoms. This is important because timely therapy has been shown to influence outcomes in acute PE. Reasons for these observed differences should be explored further to help provide more consistent PE management, regardless of admission day.
Bottom line: The sickest patients with PE admitted on weekends experienced small but significantly greater 30-day mortality compared with those admitted on weekdays.
Citation: Aujesky D, Jimenez D, Mor M, Geng M, Fine M, Ibrahim S. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119:962-968. TH
In This Edition
Literature at a Glance: A guide to this month’s studies
- PPI use with clopidrogrel in ACS.
- Chlorhexidine sponge use reduces line infections.
- Extended thienopyridine use does not benefit DES patients.
- CABG is revascularization choice for severe CAD.
- Pre-treated CVC use reduces bloodstream infections.
- Hospitalist use grows in U.S.
- Sepsis order set improves outcomes.
- Admission day predicts acute PE mortality.
PPI Use with Clopidogrel in Acute Coronary Syndrome Is Associated with Readmissions and Mortality
Clinical question: Does concomitant use of clopidogrel and a proton pump inhibitor (PPI) following hospitalization for acute coronary syndrome (ACS) lead to adverse outcomes?
Background: Prophylactic PPIs often are prescribed with clopidogrel to reduce the risk of gastrointestinal bleeding. Mechanistic studies have shown that omeprazole decreases the platelet-inhibitory effect of clopidogrel, raising concerns that PPIs might interfere with clopidogrel’s beneficial effects. The clinical significance of this finding is unknown.
Study design: Retrospective cohort study.
Setting: 127 VA hospitals.
Synopsis: Investigators used data from the Cardiac Care Follow-up Clinical Study and VA pharmacy records to examine 8,205 male veterans who were hospitalized for ACS and treated with clopidogrel. Patients who filled prescriptions for both clopidogrel and a PPI were at significantly higher risk for death or readmission with ACS compared with those who filled prescriptions for clopidogrel only (adjusted odds ratio, 1.25; 95% confidence interval, 1.11-1.41). Patients who filled prescriptions for PPIs alone had similar risk for adverse events as those who took neither medication.
Subanalyses found similarly increased risk among patients prescribed omeprazole and rabeprazole, but those taking lanzoprazole and pantoprazole were not examined due to the small sample size. Although causality cannot be inferred from this observational study, and the risk associated with combined clopidigrel and PPI use appeared small, alternatives for gastric acid reduction exist. Thus, it may be prudent to restrict PPI use to patients who have a clear indication for their use until more definitive clinical trials can be conducted.
Bottom line: Among patients who are treated with clopidogrel for ACS, PPIs should be reserved for patients with a clear indication for gastric acid reduction and who cannot use alternative therapies.
Citation: Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301(9):937-944.
Chlorhexidine-Impregnated Sponge Use Reduces Line Infections
Clinical question: Does dressing vascular catheters with chlorhexidine gluconate-impregnated sponges (CHGIS) reduce rates of catheter-related infections, and are dressing changes every seven days inferior to every three days?
Background: Process improvement strategies—including educating providers, strictly adhering to sterile technique, and promptly removing unnecessary catheters—greatly decrease catheter-related infections. It is unclear if CHGIS dressings offer additional benefit. Also uncertain is whether weekly dressing changes are as safe as changing dressings every three days.
Study design: A 2x2 factorial, assessor-blinded, randomized controlled trial.
Setting: ICUs in three university hospitals and two general hospitals in France.
Synopsis: 1,636 French adults expected to require arterial and central venous catheters for >48 hours were randomly assigned to one of four groups. Each group received either CHGIS dressings or standard dressings, and each group had dressing changes every three or seven days. Dressings were changed sooner if soiled or nonadherent. CHGIS dressings were associated with fewer catheter-related infections than standard dressings (0.6 vs. 1.4 infections per 1,000 catheter days; P=0.03). No significant difference in rates of catheter colonization existed between the three-day and seven-day dressing change strategies (10.4 vs. 11 events per 1,000 catheter days, P>0.05).
Although microbiology assessors were blinded to patients’ status, the ICU staff was not, potentially creating experimenter bias. Approximately 30% of the venous catheters and 40% of the arterial catheters were in a femoral site. Secondary analyses found higher rates of severe dermatitis among patients with CHGIS dressings but no difference in minimal bactericidal concentration (MBC) or colonizing organisms. Preliminary calculations suggested CHGIS dressings could be cost-effective.
Bottom line: Among critically ill adults, CHGIS catheter dressings may marginally reduce catheter-related infection rates, but further evaluation is needed before this technology can be adopted widely.
Citation: Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically-ill adults: a randomized controlled trial. JAMA. 2009;301(12):1231-1241.
Thienopyridine Use Six Months after Sirolimus-Eluting Stent Implant-ation Offers No Benefit
Clinical question: What are the relative contributions of aspirin and thienopyridine on preventing stent thrombosis in patients with sirolimus-eluting stents?
Background: There are no randomized clinical trials addressing the optimal duration, or the risks associated with discontinuation, of dual-antiplatelet therapy after drug-eluting stent (DES) implantation. Nevertheless, many patients continue to be maintained on dual-antiplatelet therapy beyond one year of their index DES implantation.
Study design: Prospective multicenter observational study.
Setting: Hospitals in Japan.
Synopsis: This study observed 10,778 Japanese patients undergoing sirolimus-eluting stent implantation. Patients discontinuing both thienopyridine and aspirin had a significantly higher rate of stent thrombosis than those who continued both medications for up to 18 months. However, discontinuation of thienopyridine alone was not associated with an excess risk of stent thrombosis. Additionally, a landmark analysis of patients who were free of events at six months showed rates of death for myocardial infarction (MI) at 24 months were 4.1% for patients taking thienopyridine and 4.1% for patients not taking thienopyridine (P=0.99). Ticlodipine was the thienopyridine used by more than 95% of patients.
Hospitalists should be aware that the role thienopyridine therapy plays in reducing stent thrombosis beyond one month after implantation has not been well addressed.
Bottom line: Discontinuation of thienopyridine therapy after six months while maintaining aspirin therapy is not associated with increased risk of stent thrombosis in patients with sirolimus-eluting stents.
Citation: Kimura T, Morimoto T, Nakagawa Y, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009;119(7):987-995.
Compared with PCI, CABG Results in Lower Rates of Major Adverse Events in Severe CAD Patients
Clinical question: What is the optimal revascularization strategy for previously untreated severe coronary artery disease (CAD)?
Background: Coronary artery bypass grafting (CABG) is the treatment of choice in three-vessel and left-main CAD. However, percutaneous coronary intervention (PCI) with drug-eluting stents often is utilized despite the lack of adequately powered randomized trials.
Study design: Prospective multicenter randomized clinical trial.
Setting: 85 hospitals in Europe and the U.S.
Synopsis: 1,800 patients with an average age of 65 and previously untreated three-vessel or left-main CAD amenable to therapy with both PCI and CABG were randomized to CABG or PCI. The primary combined endpoint was a major adverse cardiac or cerebrovascular event, defined as death, stroke, MI, or repeat revascularization. PCI was associated with a significantly higher rate of major adverse cardiac or cerebrovascular events, due mostly to a higher rate of repeat revascularization (13.5% vs. 5.9%, P<0.001). At 12 months, the two groups had similar rates of death from any cause or MI, and similar rates of the combined endpoint of death from any cause, stroke, or MI; however, the rate of stroke was 1.6% higher in the CABG group.
Hospitalists should continue to favor CABG over PCI but give consideration to the risks involved with such an intervention.
Bottom line: CABG remains the revascularization choice in patients with severe CAD.
Citation: Serruys PW, Morice MC, Kappetein AP, et al. Percuta-neous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961-972.
Pre-Medicated Central Venous Catheters Reduce Risk of Catheter-Related Bloodstream Infections
Clinical question: Does pre-treating central venous catheters with anti-infective agents prevent catheter-related bloodstream infections?
Background: Use of central venous catheters (CVC) is associated with catheter-related bloodstream infection (CRBSI), with CRBSI-related mortality rates as high as 25%. Previous reviews have indicated that CVCs coated or impregnated with anti-infectives may reduce CRBSI incidence. This review integrates new trial data with information from prior reviews.
Study design: Meta-analysis of 27 randomized controlled trials.
Setting: Meta-analysis.
Synopsis: The authors report CVCs pre-treated with anti-infectives (AI-CVCs) are clinically effective in reducing the risk of CRBSI. The odds of having a CRBSI with a treated CVC versus an untreated CVC are 0.49 to 1 (95% CI, 0.37–0.64, 27 studies, fixed effects). The study also finds the use of AI-CVCs might provide a large cost savings in Great Britain. Because the findings are based on a meta-analysis, they are limited by the quality, context, and consistency of the original studies. The authors note that many of the studies had unsatisfactory descriptions of methodology. The current study is unable to separate the risk reduction attributable to AI-CVC versus that attributable to other infection control practices. Also, original data is insufficient to assess the benefits of AI-CVCs placed for longer than 12 days.
To summarize, AI-CVCs may present a means to reduce CRBSI, but more investigation of its role within infection control protocols is needed, as is investigation of longer duration of treatment.
Bottom line: Central venous catheters pre-treated with anti-infectives significantly reduce catheter-related bloodstream infections.
Citation: Hockenhull JC, Dwan KM, Smith GW, et al. The clinical effectiveness of central venous catheters treated with anti-infective agents in preventing catheter-related bloodstream infections: a systematic review. Crit Care Med. 2009;37(2):702-712.
Fivefold Increase in Hospitalists in the U.S. from 1995 to 2006
Clinical question: What is the growth rate of hospitalists and hospitalist-provided care?
Background: Survey data has shown a sharp increase in the number of hospitalists, but until now there have not been any national or population-based data on the growth of hospitalist care.
Study design: Descriptive analysis.
Setting: Medicare-enrolled patients.
Synopsis: The study is based on national Medicare data from 2.1 million admissions involving 990,785 patients in 5,800 hospitals and 120,226 general internists. It represents 5% of inpatient Medicare claims generated by general internists. The authors define “hospitalist” as a general internist who generates >90% of his or her claims from the care of hospitalized patients.
U.S. hospitals have seen substantial growth in hospitalists over the period examined. The nation saw a 500% increase in the number of general-internist hospitalists, and a 28% increase (to 37.1% in 2006 from 9.1% in 1995) in the number of Medicare patients who received care from a hospitalist. The odds that a hospitalized Medicare patient received care from a hospitalist increased 29.2% per year from 1997 to 2006. The percentage of hospitals with at least three hospitalists rose to 47.1% in 2006 from 11.6% in 1995.
This analysis might actually have underestimated HM’s growth. Analysis of Medicare claims does not identify pediatric hospitalists and hospitalists who work exclusively within HMOs. This analysis also did not include family practitioners or internal-medicine subspecialists who are hospitalists.
Bottom line: Medicare claims data confirm survey data findings: Hospitalists and hospitalist care has grown sharply over the last decade.
Citation: Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102-1012.
Standardized Order Set for Bacteremic Sepsis Improves LOS and Mortality
Clinical question: Does a standardized order set for bacteremic sepsis impact patient management and outcomes?
Background: Prompt cardiovascular resuscitation and appropriate antibiotics decrease morbidity and mortality in bacteremic sepsis. This study examined whether hospitalwide, standardized sepsis order set improved management and outcomes.
Study design: Retrospective, before-and-after study design.
Setting: 1,200-bed academic medical center.
Synopsis: Two hundred patients with bacteremic severe sepsis were randomly selected from 18 months before the order set was introduced, and 200 were selected from 18 months after the order set was introduced. Primary outcomes measured were quantity of fluid administered and appropriate initial antibiotics. Secondary outcomes measured were hospital mortality and length of stay. Patients in the “after” group received more intravenous fluid (1627±1862 ml vs. 2054±2237 ml, P=.04), more appropriate antibiotics (53.0% vs. 65.5%, P=.01), had shorter hospital stays (28.7±30.1 days vs. 22.4±20.9 days, P=.02), and decreased in-house mortality (55.0% vs. 39.5%, P =<0.01).
The retrospective design of the study limited its ability to determine causal relationship. Extensive education may have contributed to the change (Hawthorne effect). Management in the ICU and ED, not the hospital wards, was the primary reason for mortality difference.
Bottom line: A standardized order set for bacteremic sepsis was associated with increased compliance with evidence-based treatment and improved outcomes. Hospitalists should promptly treat bacteremic sepsis with appropriate fluid resuscitation and antibiotics.
Citation: Thiel SW, Asghar MF, Micek ST, Reichley RM, Doherty JA, Kollef MH. Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis. Crit Care Med. 2009;37(3):819-824.
Admission Day of the Week Predicts Mortality in Patients with Acute Pulmonary Embolus
Clinical question: Do weekend pulmonary embolus (PE) admissions have worse outcomes than weekday admissions?
Background: Studies of patients with acute cardiovascular diagnoses (e.g., stroke, cardiac arrest) have shown higher short-term mortality and longer length of stay (LOS) for weekend versus weekday admissions. PE diagnosis is complex, requiring timely testing and experienced staff who are sometimes unavailable on weekends. Optimal anticoagulation therapy also depends on provider skill.
Study design: Retrospective observational study.
Setting: 186 private Pennsylvania hospitals, January 2000 through November 2002.
Synopsis: Using the Pennsylvania Health Care Cost Containment Council database, the authors reviewed 15,531 records of patients with a primary or secondary PE diagnosis code. The primary outcome was all-cause mortality over 30 days; LOS was the secondary outcome.
Weekend admissions in the highest severity of illness risk class had higher 30-day mortality than weekday admissions. Weekend admissions were significantly more likely than weekday admissions to be clinically unstable and to have abnormal lab parameters. Adjusted for severity of illness risk class, overall mortality was 1.4% higher for weekend versus weekday admissions. All excess mortality came from the sickest group of patients. LOS did not differ.
Less-experienced caregivers or delayed diagnostic testing may play a role in poor outcomes. Patients admitted on weekends might receive delayed care from the first onset of symptoms. This is important because timely therapy has been shown to influence outcomes in acute PE. Reasons for these observed differences should be explored further to help provide more consistent PE management, regardless of admission day.
Bottom line: The sickest patients with PE admitted on weekends experienced small but significantly greater 30-day mortality compared with those admitted on weekdays.
Citation: Aujesky D, Jimenez D, Mor M, Geng M, Fine M, Ibrahim S. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119:962-968. TH
Healthcare Trailblazers
Younger generations blaze new paths through the American economy. Fifteen years ago, Generation X was fresh out of college and flush with the unimagined potential of the Internet. They helped change the way the world shared information and conducted business. The impact of such innovation and enthusiasm for new technology is still felt today.
The healthcare sector possesses pioneers of its own, many with the same kind of drive and vision as the dot-com entrepreneurs of the 1990s. Fifteen years from now, today’s young hospitalists—shaped by ever-changing demands and healthcare hurdles—will be recognized as an authority in the new ways patient care is delivered.
—Brian Markoff, MD, FHM, associate professor of medicine, Mount Sinai Hospitalist Group, New York City
Bijo Chacko, MD, FHM, former chair of SHM’s Young Physicians Committee, sees energy in the newest generation of hospitalists. He also sees great potential from residents who are finishing their training and considering their job options. Until recently, SHM’s Young Physicians Committee operated as a task force. The group’s growth and increased young-physician representation throughout the society prompted SHM leadership to promote the task force to full committee status.
“The wonderful thing is that we have received lots of input from around the country and dramatically increased membership in the past few years,” says Dr. Chacko, hospital medicine medical director for Preferred Health Partners in New York City. “We have moved from simply gathering information about young physicians in hospital medicine to actively disseminating it, including the new Resident’s Corner [department in The Hospitalist]. It addresses the needs of residents and introduces them to the nuances and specifics of hospital medicine.”
The demand for information has spurred the launch of a young physicians section (www.hospitalmedicine.org/youngdoctor) on SHM’s Web site. Combined with SHM’s online career center (www.hospitalmedicine.org/careercenter), the new microsites provide young physicians a broad range of information about the specialty and—most importantly—HM career options.
Natural Progression
Four out of five large hospitals now use hospitalists, and as more hospitals implement HM programs, more residents will be exposed to the hospitalist model of care. For residents, the allure of an HM career is broad and deep. In many ways, HM is the logical extension of residency training. Brian Markoff, MD, FHM, a hospitalist and associate professor of medicine at Mount Sinai Hospitalist Group in New York City, was a chief resident when he founded the hospitalist program at the University of California at Davis Health System in Sacramento in 1998.
“Creating the hospitalist program at UC-Davis was pretty easy,” Dr. Markoff says. “All of the program’s founders were chief residents at the time. The people involved were warm to the idea, and we could teach without being in the fellowship program. Residents are already very comfortable treating patients in the hospital setting.”
Dr. Markoff says practicing hospitalists are a positive influence on residents who are still undecided on a career path. “If you’re a good role model, they’ll be interested in hospital medicine,” he says.
Diversity of Patients, Issues, Settings
Dr. Markoff and others caution that HM encompasses more than an expansion of a resident’s standard roles and responsibilities. “We’re not just super-residents,” he says. “We’re highly trained specialists in the care of hospitalized patients and the process of making care in hospital better.”
Medical conditions, patient issues, and administrative situations that often are outside a resident’s scope quickly come into focus for a new hospitalist. When Mona Patel, DO, associate director of hospitalist services at Staten Island University Hospital in New York, chose an HM career five years ago, the diversity in opportunities was a major draw. Like many hospitalists, she knew she would enjoy the type of care she provides to patients.
“I liked the acuity of the patients and disease processes; it was much more interesting and exciting for me than ongoing outpatient care of chronic diseases,” Dr. Patel says. “I liked the interaction with the hospital house staff and lots of consultants. If I had questions about a patient, I could easily consult with a specialist within the hospital.”
In addition to providing bedside care, new hospitalists often find themselves at the forefront of a monumental change in how healthcare is provided nationwide. Quality improvement (QI) initiatives, such as reducing preventable diseases in the hospital and reducing readmission rates, attracted Bryan Huang, MD, to hospital medicine at the University of California at San Diego.
“When I interviewed at UCSD, I was very interested in quality improvement,” says Dr. Huang, an assistant clinical professor at UCSD’s Division of Hospital Medicine. “UCSD is well known for glycemic control and VTE prophylaxis. We’re now working on quality improvement for treating delirium and hospital discharge.”
His experience as an academic hospitalist has opened up the QI world to him. “Before this job, I was almost not familiar at all with quality improvement,” Dr. Huang says. “As a resident, I did some quality-improvement work, but not much. Quality improvement was missing from residency training, but it’s getting better.”
Dr. Patel says HM’s biggest selling point is the variety of settings available to a new hospitalist. She’s been working for the past two years in an academic hospital program in a community hospital setting with 20 hospitalists. Before that, she worked in private practice as a hospitalist. Now, when she talks with residents, she talks about their options.
“It’s really important that you figure out what kind of setting you want,” Dr. Patel says. “Hospital medicine has a diversity of settings, from a small community hospital where you do a broad range of inpatient care to a larger academic teaching environment or a private practice group.”
Leadership Opportunities
The continuing demand for hospitalists affords young physicians who are considering an HM career additional freedom in the job market. In comparison to more traditional primary-care models, hospitalist jobs offer flexible hours and competitive salaries.
Dr. Chacko points to another benefit that is a direct result of the high demand for hospitalists: increased opportunities to launch management careers. The average age of a hospitalist is 37 and the average age of an HM group leader is 41, according to SHM’s 2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement.
“That’s not that much of a difference,” Dr. Chacko says. “Early-career hospitalists find ample leadership opportunities in the specialty. There are lots of opportunities for young hospitalists.”
How to Get Started
Because most teaching hospitals have hospitalists, most residents are exposed to HM. Many hospitalists relish the opportunity to mentor and provide early-career counseling. “Sometimes, a resident will ask to grab coffee and learn more about hospital medicine,” Dr. Huang says. “I tell them what my job is like. Many ask, ‘How do I get started looking for a job?’ I tell them that connections really help. Word of mouth is very important, so I refer people to other people.”
Margaret Fang, MD, MPH, FHM, assistant professor of medicine at the University of California at San Francisco’s division of hospital medicine and a founding member of the Young Physicians Committee, recommends that residents begin with a vision and work backward. “On a broad level, if you’re a resident, you should think about where you want to be in five years,” she says. “Look around your hospital and find a few people whose job you want.”
For some young physicians, looking ahead five years could mean being part of the healthcare revolution of tomorrow. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM elects board members
SHM has elected three new members to its Board of Directors and re-elected two members. Board members are nominated and elected by the membership and serve a three-year term.The newly elected members of the board are:



Re-elected board members:


Younger generations blaze new paths through the American economy. Fifteen years ago, Generation X was fresh out of college and flush with the unimagined potential of the Internet. They helped change the way the world shared information and conducted business. The impact of such innovation and enthusiasm for new technology is still felt today.
The healthcare sector possesses pioneers of its own, many with the same kind of drive and vision as the dot-com entrepreneurs of the 1990s. Fifteen years from now, today’s young hospitalists—shaped by ever-changing demands and healthcare hurdles—will be recognized as an authority in the new ways patient care is delivered.
—Brian Markoff, MD, FHM, associate professor of medicine, Mount Sinai Hospitalist Group, New York City
Bijo Chacko, MD, FHM, former chair of SHM’s Young Physicians Committee, sees energy in the newest generation of hospitalists. He also sees great potential from residents who are finishing their training and considering their job options. Until recently, SHM’s Young Physicians Committee operated as a task force. The group’s growth and increased young-physician representation throughout the society prompted SHM leadership to promote the task force to full committee status.
“The wonderful thing is that we have received lots of input from around the country and dramatically increased membership in the past few years,” says Dr. Chacko, hospital medicine medical director for Preferred Health Partners in New York City. “We have moved from simply gathering information about young physicians in hospital medicine to actively disseminating it, including the new Resident’s Corner [department in The Hospitalist]. It addresses the needs of residents and introduces them to the nuances and specifics of hospital medicine.”
The demand for information has spurred the launch of a young physicians section (www.hospitalmedicine.org/youngdoctor) on SHM’s Web site. Combined with SHM’s online career center (www.hospitalmedicine.org/careercenter), the new microsites provide young physicians a broad range of information about the specialty and—most importantly—HM career options.
Natural Progression
Four out of five large hospitals now use hospitalists, and as more hospitals implement HM programs, more residents will be exposed to the hospitalist model of care. For residents, the allure of an HM career is broad and deep. In many ways, HM is the logical extension of residency training. Brian Markoff, MD, FHM, a hospitalist and associate professor of medicine at Mount Sinai Hospitalist Group in New York City, was a chief resident when he founded the hospitalist program at the University of California at Davis Health System in Sacramento in 1998.
“Creating the hospitalist program at UC-Davis was pretty easy,” Dr. Markoff says. “All of the program’s founders were chief residents at the time. The people involved were warm to the idea, and we could teach without being in the fellowship program. Residents are already very comfortable treating patients in the hospital setting.”
Dr. Markoff says practicing hospitalists are a positive influence on residents who are still undecided on a career path. “If you’re a good role model, they’ll be interested in hospital medicine,” he says.
Diversity of Patients, Issues, Settings
Dr. Markoff and others caution that HM encompasses more than an expansion of a resident’s standard roles and responsibilities. “We’re not just super-residents,” he says. “We’re highly trained specialists in the care of hospitalized patients and the process of making care in hospital better.”
Medical conditions, patient issues, and administrative situations that often are outside a resident’s scope quickly come into focus for a new hospitalist. When Mona Patel, DO, associate director of hospitalist services at Staten Island University Hospital in New York, chose an HM career five years ago, the diversity in opportunities was a major draw. Like many hospitalists, she knew she would enjoy the type of care she provides to patients.
“I liked the acuity of the patients and disease processes; it was much more interesting and exciting for me than ongoing outpatient care of chronic diseases,” Dr. Patel says. “I liked the interaction with the hospital house staff and lots of consultants. If I had questions about a patient, I could easily consult with a specialist within the hospital.”
In addition to providing bedside care, new hospitalists often find themselves at the forefront of a monumental change in how healthcare is provided nationwide. Quality improvement (QI) initiatives, such as reducing preventable diseases in the hospital and reducing readmission rates, attracted Bryan Huang, MD, to hospital medicine at the University of California at San Diego.
“When I interviewed at UCSD, I was very interested in quality improvement,” says Dr. Huang, an assistant clinical professor at UCSD’s Division of Hospital Medicine. “UCSD is well known for glycemic control and VTE prophylaxis. We’re now working on quality improvement for treating delirium and hospital discharge.”
His experience as an academic hospitalist has opened up the QI world to him. “Before this job, I was almost not familiar at all with quality improvement,” Dr. Huang says. “As a resident, I did some quality-improvement work, but not much. Quality improvement was missing from residency training, but it’s getting better.”
Dr. Patel says HM’s biggest selling point is the variety of settings available to a new hospitalist. She’s been working for the past two years in an academic hospital program in a community hospital setting with 20 hospitalists. Before that, she worked in private practice as a hospitalist. Now, when she talks with residents, she talks about their options.
“It’s really important that you figure out what kind of setting you want,” Dr. Patel says. “Hospital medicine has a diversity of settings, from a small community hospital where you do a broad range of inpatient care to a larger academic teaching environment or a private practice group.”
Leadership Opportunities
The continuing demand for hospitalists affords young physicians who are considering an HM career additional freedom in the job market. In comparison to more traditional primary-care models, hospitalist jobs offer flexible hours and competitive salaries.
Dr. Chacko points to another benefit that is a direct result of the high demand for hospitalists: increased opportunities to launch management careers. The average age of a hospitalist is 37 and the average age of an HM group leader is 41, according to SHM’s 2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement.
“That’s not that much of a difference,” Dr. Chacko says. “Early-career hospitalists find ample leadership opportunities in the specialty. There are lots of opportunities for young hospitalists.”
How to Get Started
Because most teaching hospitals have hospitalists, most residents are exposed to HM. Many hospitalists relish the opportunity to mentor and provide early-career counseling. “Sometimes, a resident will ask to grab coffee and learn more about hospital medicine,” Dr. Huang says. “I tell them what my job is like. Many ask, ‘How do I get started looking for a job?’ I tell them that connections really help. Word of mouth is very important, so I refer people to other people.”
Margaret Fang, MD, MPH, FHM, assistant professor of medicine at the University of California at San Francisco’s division of hospital medicine and a founding member of the Young Physicians Committee, recommends that residents begin with a vision and work backward. “On a broad level, if you’re a resident, you should think about where you want to be in five years,” she says. “Look around your hospital and find a few people whose job you want.”
For some young physicians, looking ahead five years could mean being part of the healthcare revolution of tomorrow. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM elects board members
SHM has elected three new members to its Board of Directors and re-elected two members. Board members are nominated and elected by the membership and serve a three-year term.The newly elected members of the board are:



Re-elected board members:


Younger generations blaze new paths through the American economy. Fifteen years ago, Generation X was fresh out of college and flush with the unimagined potential of the Internet. They helped change the way the world shared information and conducted business. The impact of such innovation and enthusiasm for new technology is still felt today.
The healthcare sector possesses pioneers of its own, many with the same kind of drive and vision as the dot-com entrepreneurs of the 1990s. Fifteen years from now, today’s young hospitalists—shaped by ever-changing demands and healthcare hurdles—will be recognized as an authority in the new ways patient care is delivered.
—Brian Markoff, MD, FHM, associate professor of medicine, Mount Sinai Hospitalist Group, New York City
Bijo Chacko, MD, FHM, former chair of SHM’s Young Physicians Committee, sees energy in the newest generation of hospitalists. He also sees great potential from residents who are finishing their training and considering their job options. Until recently, SHM’s Young Physicians Committee operated as a task force. The group’s growth and increased young-physician representation throughout the society prompted SHM leadership to promote the task force to full committee status.
“The wonderful thing is that we have received lots of input from around the country and dramatically increased membership in the past few years,” says Dr. Chacko, hospital medicine medical director for Preferred Health Partners in New York City. “We have moved from simply gathering information about young physicians in hospital medicine to actively disseminating it, including the new Resident’s Corner [department in The Hospitalist]. It addresses the needs of residents and introduces them to the nuances and specifics of hospital medicine.”
The demand for information has spurred the launch of a young physicians section (www.hospitalmedicine.org/youngdoctor) on SHM’s Web site. Combined with SHM’s online career center (www.hospitalmedicine.org/careercenter), the new microsites provide young physicians a broad range of information about the specialty and—most importantly—HM career options.
Natural Progression
Four out of five large hospitals now use hospitalists, and as more hospitals implement HM programs, more residents will be exposed to the hospitalist model of care. For residents, the allure of an HM career is broad and deep. In many ways, HM is the logical extension of residency training. Brian Markoff, MD, FHM, a hospitalist and associate professor of medicine at Mount Sinai Hospitalist Group in New York City, was a chief resident when he founded the hospitalist program at the University of California at Davis Health System in Sacramento in 1998.
“Creating the hospitalist program at UC-Davis was pretty easy,” Dr. Markoff says. “All of the program’s founders were chief residents at the time. The people involved were warm to the idea, and we could teach without being in the fellowship program. Residents are already very comfortable treating patients in the hospital setting.”
Dr. Markoff says practicing hospitalists are a positive influence on residents who are still undecided on a career path. “If you’re a good role model, they’ll be interested in hospital medicine,” he says.
Diversity of Patients, Issues, Settings
Dr. Markoff and others caution that HM encompasses more than an expansion of a resident’s standard roles and responsibilities. “We’re not just super-residents,” he says. “We’re highly trained specialists in the care of hospitalized patients and the process of making care in hospital better.”
Medical conditions, patient issues, and administrative situations that often are outside a resident’s scope quickly come into focus for a new hospitalist. When Mona Patel, DO, associate director of hospitalist services at Staten Island University Hospital in New York, chose an HM career five years ago, the diversity in opportunities was a major draw. Like many hospitalists, she knew she would enjoy the type of care she provides to patients.
“I liked the acuity of the patients and disease processes; it was much more interesting and exciting for me than ongoing outpatient care of chronic diseases,” Dr. Patel says. “I liked the interaction with the hospital house staff and lots of consultants. If I had questions about a patient, I could easily consult with a specialist within the hospital.”
In addition to providing bedside care, new hospitalists often find themselves at the forefront of a monumental change in how healthcare is provided nationwide. Quality improvement (QI) initiatives, such as reducing preventable diseases in the hospital and reducing readmission rates, attracted Bryan Huang, MD, to hospital medicine at the University of California at San Diego.
“When I interviewed at UCSD, I was very interested in quality improvement,” says Dr. Huang, an assistant clinical professor at UCSD’s Division of Hospital Medicine. “UCSD is well known for glycemic control and VTE prophylaxis. We’re now working on quality improvement for treating delirium and hospital discharge.”
His experience as an academic hospitalist has opened up the QI world to him. “Before this job, I was almost not familiar at all with quality improvement,” Dr. Huang says. “As a resident, I did some quality-improvement work, but not much. Quality improvement was missing from residency training, but it’s getting better.”
Dr. Patel says HM’s biggest selling point is the variety of settings available to a new hospitalist. She’s been working for the past two years in an academic hospital program in a community hospital setting with 20 hospitalists. Before that, she worked in private practice as a hospitalist. Now, when she talks with residents, she talks about their options.
“It’s really important that you figure out what kind of setting you want,” Dr. Patel says. “Hospital medicine has a diversity of settings, from a small community hospital where you do a broad range of inpatient care to a larger academic teaching environment or a private practice group.”
Leadership Opportunities
The continuing demand for hospitalists affords young physicians who are considering an HM career additional freedom in the job market. In comparison to more traditional primary-care models, hospitalist jobs offer flexible hours and competitive salaries.
Dr. Chacko points to another benefit that is a direct result of the high demand for hospitalists: increased opportunities to launch management careers. The average age of a hospitalist is 37 and the average age of an HM group leader is 41, according to SHM’s 2007-2008 Bi-Annual Survey on the State of the Hospital Medicine Movement.
“That’s not that much of a difference,” Dr. Chacko says. “Early-career hospitalists find ample leadership opportunities in the specialty. There are lots of opportunities for young hospitalists.”
How to Get Started
Because most teaching hospitals have hospitalists, most residents are exposed to HM. Many hospitalists relish the opportunity to mentor and provide early-career counseling. “Sometimes, a resident will ask to grab coffee and learn more about hospital medicine,” Dr. Huang says. “I tell them what my job is like. Many ask, ‘How do I get started looking for a job?’ I tell them that connections really help. Word of mouth is very important, so I refer people to other people.”
Margaret Fang, MD, MPH, FHM, assistant professor of medicine at the University of California at San Francisco’s division of hospital medicine and a founding member of the Young Physicians Committee, recommends that residents begin with a vision and work backward. “On a broad level, if you’re a resident, you should think about where you want to be in five years,” she says. “Look around your hospital and find a few people whose job you want.”
For some young physicians, looking ahead five years could mean being part of the healthcare revolution of tomorrow. TH
Brendon Shank is a freelance writer based in Philadelphia.
SHM elects board members
SHM has elected three new members to its Board of Directors and re-elected two members. Board members are nominated and elected by the membership and serve a three-year term.The newly elected members of the board are:



Re-elected board members:


Use Metrics to Identify Documentation and Coding Errors
Use Metrics to Identify Documentation and Coding Errors
I am the leader of a hospitalist group. We have a number of recent graduates in our group, and I have a feeling that not everyone is billing correctly. Do you have any suggestions on how I can remedy this problem?
D. Perman, MD, Augusta, Ga.
Dr. Hospitalist responds:
I would not be surprised if your suspicions are correct. Unfortunately, many young physicians do not have a firm grasp on the rules and regulations surrounding coding and documentation. But before you set out to find a remedy, you need to identify and understand the problem.
I suggest you start by collecting data. This is easily done by involving your administrative staff and billing service. Create individual and group dashboards to help you and the individual physicians examine the data. Determine whether the doctors in your group are submitting a bill with each clinical encounter. Measure the number of days between the date of service and the date they submit the bill. Create metrics and put them on the dashboard. For example, one could measure bills submitted divided by clinical encounters; another would calculate the percent of bills submitted within 72 hours of the service date.
Next, look at the individual and group code distributions. Assuming that all members of your group have a similar job description and see the same groups of patients, the code distribution should be similar. For example, the percentage of Level 3, Level 2, and Level 1 initial admission codes should be similar among all members of your group. A disparity would suggest that one or more physicians is not documenting and coding correctly.
Use your dashboard to compare individual and group distribution. In my group, I provide each physician with the metrics on their personal distribution of codes for the fiscal year, along with their distribution of codes from previous years. When I do this, I also provide each physician with our group’s distribution of codes for the current as well as previous years. This allows individual physicians to compare historical trends for themselves and the entire group. I do not share individual data with others in the group.
Lastly, provide the distribution of codes for internal-medicine physicians from Medicare. This information is available at www.cms.hhs.gov/pqri/. It is important to note that I am not holding up the Medicare data or our group data as the standard; it is merely a reflection of how other internists in our group and across the country are billing.
This data is intended to supplement, not replace, our annual training on documentation, coding, and compliance. I have found that pushing this data to our physicians has helped them understand the importance of creating a system to ensure that all bills are submitted and coded appropriately to the level of service and documentation. TH
Use Metrics to Identify Documentation and Coding Errors
I am the leader of a hospitalist group. We have a number of recent graduates in our group, and I have a feeling that not everyone is billing correctly. Do you have any suggestions on how I can remedy this problem?
D. Perman, MD, Augusta, Ga.
Dr. Hospitalist responds:
I would not be surprised if your suspicions are correct. Unfortunately, many young physicians do not have a firm grasp on the rules and regulations surrounding coding and documentation. But before you set out to find a remedy, you need to identify and understand the problem.
I suggest you start by collecting data. This is easily done by involving your administrative staff and billing service. Create individual and group dashboards to help you and the individual physicians examine the data. Determine whether the doctors in your group are submitting a bill with each clinical encounter. Measure the number of days between the date of service and the date they submit the bill. Create metrics and put them on the dashboard. For example, one could measure bills submitted divided by clinical encounters; another would calculate the percent of bills submitted within 72 hours of the service date.
Next, look at the individual and group code distributions. Assuming that all members of your group have a similar job description and see the same groups of patients, the code distribution should be similar. For example, the percentage of Level 3, Level 2, and Level 1 initial admission codes should be similar among all members of your group. A disparity would suggest that one or more physicians is not documenting and coding correctly.
Use your dashboard to compare individual and group distribution. In my group, I provide each physician with the metrics on their personal distribution of codes for the fiscal year, along with their distribution of codes from previous years. When I do this, I also provide each physician with our group’s distribution of codes for the current as well as previous years. This allows individual physicians to compare historical trends for themselves and the entire group. I do not share individual data with others in the group.
Lastly, provide the distribution of codes for internal-medicine physicians from Medicare. This information is available at www.cms.hhs.gov/pqri/. It is important to note that I am not holding up the Medicare data or our group data as the standard; it is merely a reflection of how other internists in our group and across the country are billing.
This data is intended to supplement, not replace, our annual training on documentation, coding, and compliance. I have found that pushing this data to our physicians has helped them understand the importance of creating a system to ensure that all bills are submitted and coded appropriately to the level of service and documentation. TH
Use Metrics to Identify Documentation and Coding Errors
I am the leader of a hospitalist group. We have a number of recent graduates in our group, and I have a feeling that not everyone is billing correctly. Do you have any suggestions on how I can remedy this problem?
D. Perman, MD, Augusta, Ga.
Dr. Hospitalist responds:
I would not be surprised if your suspicions are correct. Unfortunately, many young physicians do not have a firm grasp on the rules and regulations surrounding coding and documentation. But before you set out to find a remedy, you need to identify and understand the problem.
I suggest you start by collecting data. This is easily done by involving your administrative staff and billing service. Create individual and group dashboards to help you and the individual physicians examine the data. Determine whether the doctors in your group are submitting a bill with each clinical encounter. Measure the number of days between the date of service and the date they submit the bill. Create metrics and put them on the dashboard. For example, one could measure bills submitted divided by clinical encounters; another would calculate the percent of bills submitted within 72 hours of the service date.
Next, look at the individual and group code distributions. Assuming that all members of your group have a similar job description and see the same groups of patients, the code distribution should be similar. For example, the percentage of Level 3, Level 2, and Level 1 initial admission codes should be similar among all members of your group. A disparity would suggest that one or more physicians is not documenting and coding correctly.
Use your dashboard to compare individual and group distribution. In my group, I provide each physician with the metrics on their personal distribution of codes for the fiscal year, along with their distribution of codes from previous years. When I do this, I also provide each physician with our group’s distribution of codes for the current as well as previous years. This allows individual physicians to compare historical trends for themselves and the entire group. I do not share individual data with others in the group.
Lastly, provide the distribution of codes for internal-medicine physicians from Medicare. This information is available at www.cms.hhs.gov/pqri/. It is important to note that I am not holding up the Medicare data or our group data as the standard; it is merely a reflection of how other internists in our group and across the country are billing.
This data is intended to supplement, not replace, our annual training on documentation, coding, and compliance. I have found that pushing this data to our physicians has helped them understand the importance of creating a system to ensure that all bills are submitted and coded appropriately to the level of service and documentation. TH