User login
Genesis and exodus of the healthcare industry
He looked upon the earth so filled with misery and pox
On Cro‐Magnon Neurosurgeons taking tumors out with rocks
With the blood banks run by leeches and their pterodactyl nursing
And observed This can't be healthcare these mere creatures are rehearsing
What shall we do when their lifespan will exceed eleven years?
When they no longer drink from toilet pits or make hearts from used pig ears?
There will need to be a better way to care for newer ills
A time when broadband wireless will be cheaper than their pills
He came up with a brilliant plan to revolutionize the health
To advance all medical outcomes and thereby spread the wealth
But for some strange combination of wisdom, luck, and quirk
He devised sufficient stakeholders to ensure this could not work
So a King might hire a knight to wipe out enemies with his lance
Then buy a plan to pay the cost of repairing his chain mail pants
Then along will come men with crosses of Blue who can manage that so much smarter
By inventing rules that convert poor fools from heroic docs to martyrs
He made tiny things that hide in meat and cause nasty cramps and rashes
That leave only the fittest alive to run in the royal 50 yard dashes
He made plants with spikes and purple leaves that can make one very sick
Then companies who turn green goop to gold that can flow thru a needle stick
He made medical schools to teach more tools, taking 10 years from students' lives
Then ruined careers with malpractice fears if they forget to wash their knives.
He made men whose pockets are filled with stuff from frivolous medical suits
When the experts forget the proper dosing of Peruvian medicinal fruits
He made routine birth a hazardous game between midwife, mom, and fetus
He made people who dress in masks and gloves to bravely retrieve and greet us
Then if anything goes wrong because one more time he throws snake eyes on the dice
He made lawyers to ensure that at least someone benefits while everyone else paid the price
Then along came the buildings with gadgets and learning, to find things we can't hope to fix
And those who get paid to know how NOT to pay the providers of care to the sick
He made organized giants that make tablets and gizmos from the minds of the cream of the crop
And made multiple races with all different faces whose subjective complaints will not stop
But alas came the gadgets, the photons and diodes, the software, the web and the data
Then the standards, the knowledge bases, multiuser interfaces, all in perpetual BETA
To automate the arcane, declare real what is feigned, and make INPUT like losing a toe
Then the last fatal strawhe made privacy laws to ensure they can't share what they know
Oh what have I done, this is really no fun, they now live to one hundred and thirty
But there's no more MDs and the few with degrees refuse to get their hands dirty
Next time when I try to take research to practice I'll start with a real I.O.M.
Evidence galore, so when we screw up once more I can put all the blame right on them
He looked upon the earth so filled with misery and pox
On Cro‐Magnon Neurosurgeons taking tumors out with rocks
With the blood banks run by leeches and their pterodactyl nursing
And observed This can't be healthcare these mere creatures are rehearsing
What shall we do when their lifespan will exceed eleven years?
When they no longer drink from toilet pits or make hearts from used pig ears?
There will need to be a better way to care for newer ills
A time when broadband wireless will be cheaper than their pills
He came up with a brilliant plan to revolutionize the health
To advance all medical outcomes and thereby spread the wealth
But for some strange combination of wisdom, luck, and quirk
He devised sufficient stakeholders to ensure this could not work
So a King might hire a knight to wipe out enemies with his lance
Then buy a plan to pay the cost of repairing his chain mail pants
Then along will come men with crosses of Blue who can manage that so much smarter
By inventing rules that convert poor fools from heroic docs to martyrs
He made tiny things that hide in meat and cause nasty cramps and rashes
That leave only the fittest alive to run in the royal 50 yard dashes
He made plants with spikes and purple leaves that can make one very sick
Then companies who turn green goop to gold that can flow thru a needle stick
He made medical schools to teach more tools, taking 10 years from students' lives
Then ruined careers with malpractice fears if they forget to wash their knives.
He made men whose pockets are filled with stuff from frivolous medical suits
When the experts forget the proper dosing of Peruvian medicinal fruits
He made routine birth a hazardous game between midwife, mom, and fetus
He made people who dress in masks and gloves to bravely retrieve and greet us
Then if anything goes wrong because one more time he throws snake eyes on the dice
He made lawyers to ensure that at least someone benefits while everyone else paid the price
Then along came the buildings with gadgets and learning, to find things we can't hope to fix
And those who get paid to know how NOT to pay the providers of care to the sick
He made organized giants that make tablets and gizmos from the minds of the cream of the crop
And made multiple races with all different faces whose subjective complaints will not stop
But alas came the gadgets, the photons and diodes, the software, the web and the data
Then the standards, the knowledge bases, multiuser interfaces, all in perpetual BETA
To automate the arcane, declare real what is feigned, and make INPUT like losing a toe
Then the last fatal strawhe made privacy laws to ensure they can't share what they know
Oh what have I done, this is really no fun, they now live to one hundred and thirty
But there's no more MDs and the few with degrees refuse to get their hands dirty
Next time when I try to take research to practice I'll start with a real I.O.M.
Evidence galore, so when we screw up once more I can put all the blame right on them
He looked upon the earth so filled with misery and pox
On Cro‐Magnon Neurosurgeons taking tumors out with rocks
With the blood banks run by leeches and their pterodactyl nursing
And observed This can't be healthcare these mere creatures are rehearsing
What shall we do when their lifespan will exceed eleven years?
When they no longer drink from toilet pits or make hearts from used pig ears?
There will need to be a better way to care for newer ills
A time when broadband wireless will be cheaper than their pills
He came up with a brilliant plan to revolutionize the health
To advance all medical outcomes and thereby spread the wealth
But for some strange combination of wisdom, luck, and quirk
He devised sufficient stakeholders to ensure this could not work
So a King might hire a knight to wipe out enemies with his lance
Then buy a plan to pay the cost of repairing his chain mail pants
Then along will come men with crosses of Blue who can manage that so much smarter
By inventing rules that convert poor fools from heroic docs to martyrs
He made tiny things that hide in meat and cause nasty cramps and rashes
That leave only the fittest alive to run in the royal 50 yard dashes
He made plants with spikes and purple leaves that can make one very sick
Then companies who turn green goop to gold that can flow thru a needle stick
He made medical schools to teach more tools, taking 10 years from students' lives
Then ruined careers with malpractice fears if they forget to wash their knives.
He made men whose pockets are filled with stuff from frivolous medical suits
When the experts forget the proper dosing of Peruvian medicinal fruits
He made routine birth a hazardous game between midwife, mom, and fetus
He made people who dress in masks and gloves to bravely retrieve and greet us
Then if anything goes wrong because one more time he throws snake eyes on the dice
He made lawyers to ensure that at least someone benefits while everyone else paid the price
Then along came the buildings with gadgets and learning, to find things we can't hope to fix
And those who get paid to know how NOT to pay the providers of care to the sick
He made organized giants that make tablets and gizmos from the minds of the cream of the crop
And made multiple races with all different faces whose subjective complaints will not stop
But alas came the gadgets, the photons and diodes, the software, the web and the data
Then the standards, the knowledge bases, multiuser interfaces, all in perpetual BETA
To automate the arcane, declare real what is feigned, and make INPUT like losing a toe
Then the last fatal strawhe made privacy laws to ensure they can't share what they know
Oh what have I done, this is really no fun, they now live to one hundred and thirty
But there's no more MDs and the few with degrees refuse to get their hands dirty
Next time when I try to take research to practice I'll start with a real I.O.M.
Evidence galore, so when we screw up once more I can put all the blame right on them
Rapid Response: A QI Conundrum
Many in‐hospital cardiac arrests and other adverse events are heralded by warning signs that are evident in the preceding 6 to 8 hours.1 By promptly intervening before further deterioration occurs, rapid response teams (RRTs) are designed to decrease unexpected intensive care unit (ICU) transfers, cardiac arrests, and inpatient mortality. While implementing RRTs is 1 of the 6 initiatives recommended by the Institute for Healthcare Improvement,2 data supporting their effectiveness is equivocal.3, 4
In October 2006, at Denver Health Medical Center, an academic, safety net hospital, we initiated a rapid response systemclinical triggers program (RRS‐CTP).5 In our RRS‐CTP, an abrupt change in patient status (Figure 1) triggers a mandatory call by the patient's nurse to the primary team, which is then required to perform an immediate bedside evaluation. By incorporating the primary team into the RRT‐CTP, we sought to preserve as much continuity of care as possible. Also, since the same house staff compose our cardiopulmonary arrest or cor team, and staff the ICUs and non‐ICU hospital wards, we did not feel that creating a separate RRT was an efficient use of resources. Our nurses have undergone extensive education about the necessity of a prompt bedside evaluation and have been instructed and empowered to escalate concerns to senior physicians if needed. We present a case that illustrates challenges to both implementing an RRS and measuring its potential benefits.
Case
A 59‐year‐old woman with a history of bipolar mood disorder was admitted for altered mental status. At presentation, she had signs of acute mania with normal vital signs. After initial laboratory workup, her altered mental status was felt to be multifactorial due to urinary tract infection, hypernatremia (attributed to lithium‐induced nephrogenic diabetes insipidus), and acute mania (attributed to medication discontinuation). Because she was slow to recover from the acute mania, her hospital stay was prolonged. From admission, the patient was treated with heparin 5000 units subcutaneously twice daily for venous thromboembolism prophylaxis.
On hospital day 7, at 21:32, the patient was noted to have asymptomatic tachycardia at 149 beats per minute and a new oxygen requirement of 3 L/minute. The cross‐cover team was called; however, although criteria were met, the RRS‐CTP was not activated and a bedside evaluation was not performed. A chest X‐ray was found to be normal and, with the exception of the oxygen requirement, her vital signs normalized by 23:45. No further diagnostic testing was performed at the time.
The next morning, at 11:58, the patient was found to have a blood pressure of 60/40 mmHg and heart rate of 42 beats per minute. The RRS‐CTP was activated. The primary team arrived at the bedside at 12:00 and found the patient to be alert, oriented, and without complaints. Her respiratory rate was 30/minute, and her oxygen saturation was 86% on 3 L/minute. An arterial blood gas analysis demonstrated acute respiratory alkalosis with hypoxemia and an electrocardiogram showed sinus tachycardia with a new S1Q3T3 pattern. A computed tomography angiogram revealed a large, nearly occlusive pulmonary embolus (PE) filling an enlarged right pulmonary artery, as well as thrombus within the left main pulmonary artery. She was transferred to the medical ICU and alteplase was administered. The patient survived and was discharged in good clinical condition.
Discussion
Despite the strong theoretical benefit of the RRT concept, a recent review by Ranji et al.4 concluded that RRTs had not yet been shown to improve patient outcomes. In contrast to dedicated RRTs, this case illustrates a different type of RRS that was designed to address abrupt changes in patient status, while maintaining continuity of care and efficiently utilizing resources.
If one considers an RRS to have both afferent (criteria recognition) and efferent (RRT or primary team response) limbs, the afferent limb must be consistently activated in order to obtain the efferent limb's response.6 The greatest opportunities to improve RRSs are thought to lie in the afferent limb.3 Our RRS‐CTP was not triggered in 1 of 2 instances in which criteria for mandatory initiation of the system were met. This is consistent with the findings of the Medical Early Response Intervention and Therapy (MERIT) trial, in which RRTs were called in only 41% of the patients meeting criteria and subsequently having adverse events,7 and with the ongoing monitoring of the use of the system at our hospital. Had the cross‐covering team seen the patient at the bedside initially, the PE might have been diagnosed while the patient was hemodynamically stable, giving the patient nearly a 3‐fold lower relative mortality.8 When the RRS‐CTP was activated, a prompt bedside evaluation occurred, allowing for lytic therapy to be administered before cardiopulmonary arrest (attendant mortality of 90%).9
While rapid response criteria were originally based upon published sensitivity analyses, more recent studies suggest that these criteria lack diagnostic accuracy. As demonstrated by Cretikos et al,10 to reach a sensitivity of 70%, the corresponding specificity would be only 86%. Given that the prevalence of adverse events in the MERIT trial was only 0.6%, the resulting positive predictive value (PPV) of rapid response call criteria is 3%. Accordingly, 33 calls would be needed to prevent 1 unplanned ICU transfer, cardiac arrest, or death. Nurses' attempts to minimize false‐positive calls may help explain the low call rates for patients meeting RRT criteria. The 2 avenues to increase the PPV of criteria are:
-
Increase the prevalence of disease in the population screened by risk factor stratification.
-
Increase the specificity of the call criteria, which has been limited by the associated decrease in sensitivity.10
Regarding the efferent response limb of RRS, our case demonstrates that the primary team (rather than a separate group of caregivers), when alerted appropriately, can effectively respond to critical changes in patient status. Accordingly, our data show that since the inception of the program, cardiopulmonary arrests have decreased from a mean of 4.1 per month to 2.3 per month (P = 0.03).
Many clinical trials of RRTs would not capture the success demonstrated in this case. For example, due to the low prevalence of events, the MERIT trial used a composite endpoint that included unplanned ICU transfers, cardiac arrests, and mortality. Because our patient still required an unplanned ICU transfer after being evaluated by the responding team, she would have been counted as a system failure.
Conclusion
While local needs should inform the type of RRS implemented, this case illustrates one of the major obstacles ubiquitous to RRS implementation: failure of system activation. With appropriate activation, an RRS‐CTP can meet RRS goals while maintaining continuity of care and maximizing existing resources. This case also illustrates the difficulty of achieving a statistically relevant outcome, while demonstrating the potential benefits of evolving RRSs.
- ,,,,.Rapid response teams—do they make a difference.Dimens Crit Care Nurs.2007;26(6):253–260.
- Institute for Healthcare Improvement. 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1IHI. Accessed February2009.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,,.Effects of rapid response systems on clinical outcomes: review and meta‐analyses.J Hosp Med.2007;2:422–432.
- ,,.Clinical triggers and rapid response escalation criteria.Patient Saf Qual Healthc.2007;4(2):12–13. Available at: http://www.psqh.com/archives.html. Accessed February 2009.
- ,,, et al.Use of medical emergency team responses to reduce hospital cardiopulmonary arrest.Qual Saf Health Care.2004;13:251–254.
- MERIT Study Investigators.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365:2091–2097.
- ,,.Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER).Lancet.1999;353(9162):1386–1389.
- ,,,.Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest.Chest.1990;97(2):413–419.
- ,,,,,.The objective medical emergency team activation criteria: a case–control study.Resuscitation.2007;73:62–72.
Many in‐hospital cardiac arrests and other adverse events are heralded by warning signs that are evident in the preceding 6 to 8 hours.1 By promptly intervening before further deterioration occurs, rapid response teams (RRTs) are designed to decrease unexpected intensive care unit (ICU) transfers, cardiac arrests, and inpatient mortality. While implementing RRTs is 1 of the 6 initiatives recommended by the Institute for Healthcare Improvement,2 data supporting their effectiveness is equivocal.3, 4
In October 2006, at Denver Health Medical Center, an academic, safety net hospital, we initiated a rapid response systemclinical triggers program (RRS‐CTP).5 In our RRS‐CTP, an abrupt change in patient status (Figure 1) triggers a mandatory call by the patient's nurse to the primary team, which is then required to perform an immediate bedside evaluation. By incorporating the primary team into the RRT‐CTP, we sought to preserve as much continuity of care as possible. Also, since the same house staff compose our cardiopulmonary arrest or cor team, and staff the ICUs and non‐ICU hospital wards, we did not feel that creating a separate RRT was an efficient use of resources. Our nurses have undergone extensive education about the necessity of a prompt bedside evaluation and have been instructed and empowered to escalate concerns to senior physicians if needed. We present a case that illustrates challenges to both implementing an RRS and measuring its potential benefits.
Case
A 59‐year‐old woman with a history of bipolar mood disorder was admitted for altered mental status. At presentation, she had signs of acute mania with normal vital signs. After initial laboratory workup, her altered mental status was felt to be multifactorial due to urinary tract infection, hypernatremia (attributed to lithium‐induced nephrogenic diabetes insipidus), and acute mania (attributed to medication discontinuation). Because she was slow to recover from the acute mania, her hospital stay was prolonged. From admission, the patient was treated with heparin 5000 units subcutaneously twice daily for venous thromboembolism prophylaxis.
On hospital day 7, at 21:32, the patient was noted to have asymptomatic tachycardia at 149 beats per minute and a new oxygen requirement of 3 L/minute. The cross‐cover team was called; however, although criteria were met, the RRS‐CTP was not activated and a bedside evaluation was not performed. A chest X‐ray was found to be normal and, with the exception of the oxygen requirement, her vital signs normalized by 23:45. No further diagnostic testing was performed at the time.
The next morning, at 11:58, the patient was found to have a blood pressure of 60/40 mmHg and heart rate of 42 beats per minute. The RRS‐CTP was activated. The primary team arrived at the bedside at 12:00 and found the patient to be alert, oriented, and without complaints. Her respiratory rate was 30/minute, and her oxygen saturation was 86% on 3 L/minute. An arterial blood gas analysis demonstrated acute respiratory alkalosis with hypoxemia and an electrocardiogram showed sinus tachycardia with a new S1Q3T3 pattern. A computed tomography angiogram revealed a large, nearly occlusive pulmonary embolus (PE) filling an enlarged right pulmonary artery, as well as thrombus within the left main pulmonary artery. She was transferred to the medical ICU and alteplase was administered. The patient survived and was discharged in good clinical condition.
Discussion
Despite the strong theoretical benefit of the RRT concept, a recent review by Ranji et al.4 concluded that RRTs had not yet been shown to improve patient outcomes. In contrast to dedicated RRTs, this case illustrates a different type of RRS that was designed to address abrupt changes in patient status, while maintaining continuity of care and efficiently utilizing resources.
If one considers an RRS to have both afferent (criteria recognition) and efferent (RRT or primary team response) limbs, the afferent limb must be consistently activated in order to obtain the efferent limb's response.6 The greatest opportunities to improve RRSs are thought to lie in the afferent limb.3 Our RRS‐CTP was not triggered in 1 of 2 instances in which criteria for mandatory initiation of the system were met. This is consistent with the findings of the Medical Early Response Intervention and Therapy (MERIT) trial, in which RRTs were called in only 41% of the patients meeting criteria and subsequently having adverse events,7 and with the ongoing monitoring of the use of the system at our hospital. Had the cross‐covering team seen the patient at the bedside initially, the PE might have been diagnosed while the patient was hemodynamically stable, giving the patient nearly a 3‐fold lower relative mortality.8 When the RRS‐CTP was activated, a prompt bedside evaluation occurred, allowing for lytic therapy to be administered before cardiopulmonary arrest (attendant mortality of 90%).9
While rapid response criteria were originally based upon published sensitivity analyses, more recent studies suggest that these criteria lack diagnostic accuracy. As demonstrated by Cretikos et al,10 to reach a sensitivity of 70%, the corresponding specificity would be only 86%. Given that the prevalence of adverse events in the MERIT trial was only 0.6%, the resulting positive predictive value (PPV) of rapid response call criteria is 3%. Accordingly, 33 calls would be needed to prevent 1 unplanned ICU transfer, cardiac arrest, or death. Nurses' attempts to minimize false‐positive calls may help explain the low call rates for patients meeting RRT criteria. The 2 avenues to increase the PPV of criteria are:
-
Increase the prevalence of disease in the population screened by risk factor stratification.
-
Increase the specificity of the call criteria, which has been limited by the associated decrease in sensitivity.10
Regarding the efferent response limb of RRS, our case demonstrates that the primary team (rather than a separate group of caregivers), when alerted appropriately, can effectively respond to critical changes in patient status. Accordingly, our data show that since the inception of the program, cardiopulmonary arrests have decreased from a mean of 4.1 per month to 2.3 per month (P = 0.03).
Many clinical trials of RRTs would not capture the success demonstrated in this case. For example, due to the low prevalence of events, the MERIT trial used a composite endpoint that included unplanned ICU transfers, cardiac arrests, and mortality. Because our patient still required an unplanned ICU transfer after being evaluated by the responding team, she would have been counted as a system failure.
Conclusion
While local needs should inform the type of RRS implemented, this case illustrates one of the major obstacles ubiquitous to RRS implementation: failure of system activation. With appropriate activation, an RRS‐CTP can meet RRS goals while maintaining continuity of care and maximizing existing resources. This case also illustrates the difficulty of achieving a statistically relevant outcome, while demonstrating the potential benefits of evolving RRSs.
Many in‐hospital cardiac arrests and other adverse events are heralded by warning signs that are evident in the preceding 6 to 8 hours.1 By promptly intervening before further deterioration occurs, rapid response teams (RRTs) are designed to decrease unexpected intensive care unit (ICU) transfers, cardiac arrests, and inpatient mortality. While implementing RRTs is 1 of the 6 initiatives recommended by the Institute for Healthcare Improvement,2 data supporting their effectiveness is equivocal.3, 4
In October 2006, at Denver Health Medical Center, an academic, safety net hospital, we initiated a rapid response systemclinical triggers program (RRS‐CTP).5 In our RRS‐CTP, an abrupt change in patient status (Figure 1) triggers a mandatory call by the patient's nurse to the primary team, which is then required to perform an immediate bedside evaluation. By incorporating the primary team into the RRT‐CTP, we sought to preserve as much continuity of care as possible. Also, since the same house staff compose our cardiopulmonary arrest or cor team, and staff the ICUs and non‐ICU hospital wards, we did not feel that creating a separate RRT was an efficient use of resources. Our nurses have undergone extensive education about the necessity of a prompt bedside evaluation and have been instructed and empowered to escalate concerns to senior physicians if needed. We present a case that illustrates challenges to both implementing an RRS and measuring its potential benefits.
Case
A 59‐year‐old woman with a history of bipolar mood disorder was admitted for altered mental status. At presentation, she had signs of acute mania with normal vital signs. After initial laboratory workup, her altered mental status was felt to be multifactorial due to urinary tract infection, hypernatremia (attributed to lithium‐induced nephrogenic diabetes insipidus), and acute mania (attributed to medication discontinuation). Because she was slow to recover from the acute mania, her hospital stay was prolonged. From admission, the patient was treated with heparin 5000 units subcutaneously twice daily for venous thromboembolism prophylaxis.
On hospital day 7, at 21:32, the patient was noted to have asymptomatic tachycardia at 149 beats per minute and a new oxygen requirement of 3 L/minute. The cross‐cover team was called; however, although criteria were met, the RRS‐CTP was not activated and a bedside evaluation was not performed. A chest X‐ray was found to be normal and, with the exception of the oxygen requirement, her vital signs normalized by 23:45. No further diagnostic testing was performed at the time.
The next morning, at 11:58, the patient was found to have a blood pressure of 60/40 mmHg and heart rate of 42 beats per minute. The RRS‐CTP was activated. The primary team arrived at the bedside at 12:00 and found the patient to be alert, oriented, and without complaints. Her respiratory rate was 30/minute, and her oxygen saturation was 86% on 3 L/minute. An arterial blood gas analysis demonstrated acute respiratory alkalosis with hypoxemia and an electrocardiogram showed sinus tachycardia with a new S1Q3T3 pattern. A computed tomography angiogram revealed a large, nearly occlusive pulmonary embolus (PE) filling an enlarged right pulmonary artery, as well as thrombus within the left main pulmonary artery. She was transferred to the medical ICU and alteplase was administered. The patient survived and was discharged in good clinical condition.
Discussion
Despite the strong theoretical benefit of the RRT concept, a recent review by Ranji et al.4 concluded that RRTs had not yet been shown to improve patient outcomes. In contrast to dedicated RRTs, this case illustrates a different type of RRS that was designed to address abrupt changes in patient status, while maintaining continuity of care and efficiently utilizing resources.
If one considers an RRS to have both afferent (criteria recognition) and efferent (RRT or primary team response) limbs, the afferent limb must be consistently activated in order to obtain the efferent limb's response.6 The greatest opportunities to improve RRSs are thought to lie in the afferent limb.3 Our RRS‐CTP was not triggered in 1 of 2 instances in which criteria for mandatory initiation of the system were met. This is consistent with the findings of the Medical Early Response Intervention and Therapy (MERIT) trial, in which RRTs were called in only 41% of the patients meeting criteria and subsequently having adverse events,7 and with the ongoing monitoring of the use of the system at our hospital. Had the cross‐covering team seen the patient at the bedside initially, the PE might have been diagnosed while the patient was hemodynamically stable, giving the patient nearly a 3‐fold lower relative mortality.8 When the RRS‐CTP was activated, a prompt bedside evaluation occurred, allowing for lytic therapy to be administered before cardiopulmonary arrest (attendant mortality of 90%).9
While rapid response criteria were originally based upon published sensitivity analyses, more recent studies suggest that these criteria lack diagnostic accuracy. As demonstrated by Cretikos et al,10 to reach a sensitivity of 70%, the corresponding specificity would be only 86%. Given that the prevalence of adverse events in the MERIT trial was only 0.6%, the resulting positive predictive value (PPV) of rapid response call criteria is 3%. Accordingly, 33 calls would be needed to prevent 1 unplanned ICU transfer, cardiac arrest, or death. Nurses' attempts to minimize false‐positive calls may help explain the low call rates for patients meeting RRT criteria. The 2 avenues to increase the PPV of criteria are:
-
Increase the prevalence of disease in the population screened by risk factor stratification.
-
Increase the specificity of the call criteria, which has been limited by the associated decrease in sensitivity.10
Regarding the efferent response limb of RRS, our case demonstrates that the primary team (rather than a separate group of caregivers), when alerted appropriately, can effectively respond to critical changes in patient status. Accordingly, our data show that since the inception of the program, cardiopulmonary arrests have decreased from a mean of 4.1 per month to 2.3 per month (P = 0.03).
Many clinical trials of RRTs would not capture the success demonstrated in this case. For example, due to the low prevalence of events, the MERIT trial used a composite endpoint that included unplanned ICU transfers, cardiac arrests, and mortality. Because our patient still required an unplanned ICU transfer after being evaluated by the responding team, she would have been counted as a system failure.
Conclusion
While local needs should inform the type of RRS implemented, this case illustrates one of the major obstacles ubiquitous to RRS implementation: failure of system activation. With appropriate activation, an RRS‐CTP can meet RRS goals while maintaining continuity of care and maximizing existing resources. This case also illustrates the difficulty of achieving a statistically relevant outcome, while demonstrating the potential benefits of evolving RRSs.
- ,,,,.Rapid response teams—do they make a difference.Dimens Crit Care Nurs.2007;26(6):253–260.
- Institute for Healthcare Improvement. 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1IHI. Accessed February2009.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,,.Effects of rapid response systems on clinical outcomes: review and meta‐analyses.J Hosp Med.2007;2:422–432.
- ,,.Clinical triggers and rapid response escalation criteria.Patient Saf Qual Healthc.2007;4(2):12–13. Available at: http://www.psqh.com/archives.html. Accessed February 2009.
- ,,, et al.Use of medical emergency team responses to reduce hospital cardiopulmonary arrest.Qual Saf Health Care.2004;13:251–254.
- MERIT Study Investigators.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365:2091–2097.
- ,,.Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER).Lancet.1999;353(9162):1386–1389.
- ,,,.Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest.Chest.1990;97(2):413–419.
- ,,,,,.The objective medical emergency team activation criteria: a case–control study.Resuscitation.2007;73:62–72.
- ,,,,.Rapid response teams—do they make a difference.Dimens Crit Care Nurs.2007;26(6):253–260.
- Institute for Healthcare Improvement. 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1IHI. Accessed February2009.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,,.Effects of rapid response systems on clinical outcomes: review and meta‐analyses.J Hosp Med.2007;2:422–432.
- ,,.Clinical triggers and rapid response escalation criteria.Patient Saf Qual Healthc.2007;4(2):12–13. Available at: http://www.psqh.com/archives.html. Accessed February 2009.
- ,,, et al.Use of medical emergency team responses to reduce hospital cardiopulmonary arrest.Qual Saf Health Care.2004;13:251–254.
- MERIT Study Investigators.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365:2091–2097.
- ,,.Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER).Lancet.1999;353(9162):1386–1389.
- ,,,.Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest.Chest.1990;97(2):413–419.
- ,,,,,.The objective medical emergency team activation criteria: a case–control study.Resuscitation.2007;73:62–72.
The Accidental Hospitalist
David Yu, MD, learned early on the value of being flexible. While attending Washington University in St. Louis, he found his calling when he changed his major from economics to biology. When the malpractice insurance crisis forced him to close his private practice, he embraced an opportunity to launch a program devoted to the “newfangled concept” of hospital medicine.
“I’m kind of like the accidental tourist,” says Dr. Yu, medical director of hospitalist services at the 372-bed Decatur Memorial Hospital in Decatur, Ill., and clinical assistant professor of family and community medicine at Southern Illinois University School of Medicine in Carbondale. “I didn’t really go to college with the mind-set of being a doctor, and when I became a doctor, there was no such thing as a hospitalist. … I went where the current took me and, fortunately, here I am.”
Question: What prompted the switch from economics to pre-med/biology?
Answer: When I got to the upper-level econ classes, I realized why the economy is the way it is: because nobody can understand how it works. My sister was in medical school. She really liked it and she talked me into it.
Q: You spent nine years in traditional practice. Why did you become a hospitalist?
A: In 2004, my malpractice insurance rate shot up 400% without any active lawsuits, so I had to close my practice. I had the choice of joining another traditional group, or Decatur (Memorial Hospital) was starting a new hospitalist program. To quote “The Godfather,” they made me an offer I couldn’t refuse.
Q: How did your experience in traditional practice prepare you for your role as a hospitalist?
A: I had been surrounded by incredible specialists. I saw how they interacted with me and how they treated my patients. As hospitalists, we are serving our patients, but really our clientele is the physicians we admit for. When I made the switch, I really had an idea of how a hospitalist should serve traditional practice.
Q: What is that service model?
A: It comes down to what I call the three A’s: You have to be available, you have to be able, and you have to be amicable. One of the problems in our field is a lot of hospitalists complain they’re treated like residents. They say they don’t get respect. They feel mistreated. That’s the wrong attitude. You can’t just ask for respect or demand it. You have to develop relationships.
Q: When Decatur’s hospitalist program started, you were on your own. Now there are seven physicians, two physician assistants, and a practice manager. How rewarding has it been to see it grow?
We have to find ways to help hospitalists take more ownership in their patients and their program. ... With our schedule, you can’t pawn off your responsibility to the nocturnist or the weekend guy.
—David Yu, MD, Decatur (Ill.)
Memorial Hospital
A: It’s been very rewarding. I’m honored to have been chosen as a member of Team Hospitalist, and I’m honored to be a committee member for SHM’s Non-Physician Provider Committee. Those are personal honors, but they are reflections on the success of the program. It’s an honor for the entire Decatur Memorial Hospital, and the administration, that a program started four and a half years ago, indirectly, has received national recognition.
Q: You implemented a one-week-on, one-week-off schedule for your hospitalists as a way to decrease signouts. How did that come about?
A: Signouts have been the bane of medical mistakes. Instead of having signouts twice a day, we have one physician on call for that entire week for his or her patients. It’s patient-centric versus schedule-centric. Physicians leave the hospital when their work is done, instead of looking at the clock and waiting to sign out at a certain time like a factory worker. It treats hospitalists not as shift workers but as attending physicians. It gives them due respect that they can manage their own patients responsibly.
Q: Do you think the schedule improves the quality of patient care?
A: The continuity of care is incredible. If you are admitted and discharged between Mondays, you have one hospitalist in charge of your entire case, instead of multiple physicians being on call for you. That increases patient satisfaction, reduces medical errors, and eliminates the need for unnecessary tests when new physicians take over. I’m also a huge believer that scheduling brings out the best and worst in hospitalists.
Q: How does it bring out the best in them?
A: As medical directors, we have to find ways to help hospitalists take more ownership in their patients and their program. If they’re thinking, “My shift is ending and I’m going to be off and I can hand this issue off to the next doctor,” that can have a tremendous effect on the quality of care and the way a hospitalist delivers medicine. With our schedule, you can’t pawn off your responsibility to the nocturnist or the weekend guy. … If something goes wrong or if the ball gets dropped, there’s no one else to blame it on.
Q: You developed a system at Decatur through which patient discharge summaries are sent electronically to primary-care physicians, often before the patient leaves the hospital. Have the primaries been receptive?
A: Absolutely. Communication is the mother’s milk of hospitalists. Some hospitalist programs are very large, they’re very busy, or there’s no incentive for them to do this because they’re the only game in town. But I practice in a mid-size community and I know all of these doctors. My reputation is my bond. I have to provide good service.
Q: What do you enjoy most about your role as a hospitalist?
A: I love solving problems for a patient. I also love how the relationship builds. You introduce yourself to a patient and their family as a hospitalist and they’re thinking, “Who the heck are you?” For a few seconds, it’s like meeting someone on a blind date. And when they’re discharged, they tell you they had a pleasant experience and they appreciate your help. It’s a courtship at a rapid pace.
Q: What do you consider to be your biggest challenge?
A: Recruitment; the administration asking us to take on more responsibilities; burnout. … We’re a typical hospitalist program; I think the problems are pretty universal.
Q: How do you address those challenges?
A: As medical director, you’re always navigating political and personal minefields. It comes back to developing relationships. The only way to earn goodwill is to give and provide service. That’s a problem some hospitalist programs run into. They want to instantly demand respect. You can’t demand it; you have to earn it. Sometimes hospitalists feel dumped on. Those are opportunities … to provide service in a willing and positive way instead of complaining. I’m not saying you have to be a whipping boy, but there are times when you have to give a little to get a little. That’s where the wisdom of the medical director comes in and sets the whole tone.
Q: What’s ahead for the academic side of your career?
A: We’re considering the possibility of starting a family practice fellowship program for attending residents who finish but want to go into the field of hospital medicine and want additional training. It’s not a done deal, but it’s an exciting possibility.
Q: How so?
A: Every medical director says they have a hard time recruiting. One way we can help solve the problem is by producing more hospitalists. We can’t just complain. We have to increase the pool of professionals interested in our model, train them, and get them integrated into our system.
Q: What advice would you give a student who is considering going that route?
A: You have to be a good communicator, you have to enjoy taking care of very sick people, and you have to enjoy solving very complex problems. You can’t just do it for the lifestyle. If you do, you won’t be happy in the long run. If I ask a medical student or resident why they want to be a hospitalist and they say, “I like the one-week-on, one-week-off schedule,” I tell them, “If that’s the reason you’re considering it, you really should reconsider.” TH
Mark Leiser is a freelance writer in New Jersey.
David Yu, MD, learned early on the value of being flexible. While attending Washington University in St. Louis, he found his calling when he changed his major from economics to biology. When the malpractice insurance crisis forced him to close his private practice, he embraced an opportunity to launch a program devoted to the “newfangled concept” of hospital medicine.
“I’m kind of like the accidental tourist,” says Dr. Yu, medical director of hospitalist services at the 372-bed Decatur Memorial Hospital in Decatur, Ill., and clinical assistant professor of family and community medicine at Southern Illinois University School of Medicine in Carbondale. “I didn’t really go to college with the mind-set of being a doctor, and when I became a doctor, there was no such thing as a hospitalist. … I went where the current took me and, fortunately, here I am.”
Question: What prompted the switch from economics to pre-med/biology?
Answer: When I got to the upper-level econ classes, I realized why the economy is the way it is: because nobody can understand how it works. My sister was in medical school. She really liked it and she talked me into it.
Q: You spent nine years in traditional practice. Why did you become a hospitalist?
A: In 2004, my malpractice insurance rate shot up 400% without any active lawsuits, so I had to close my practice. I had the choice of joining another traditional group, or Decatur (Memorial Hospital) was starting a new hospitalist program. To quote “The Godfather,” they made me an offer I couldn’t refuse.
Q: How did your experience in traditional practice prepare you for your role as a hospitalist?
A: I had been surrounded by incredible specialists. I saw how they interacted with me and how they treated my patients. As hospitalists, we are serving our patients, but really our clientele is the physicians we admit for. When I made the switch, I really had an idea of how a hospitalist should serve traditional practice.
Q: What is that service model?
A: It comes down to what I call the three A’s: You have to be available, you have to be able, and you have to be amicable. One of the problems in our field is a lot of hospitalists complain they’re treated like residents. They say they don’t get respect. They feel mistreated. That’s the wrong attitude. You can’t just ask for respect or demand it. You have to develop relationships.
Q: When Decatur’s hospitalist program started, you were on your own. Now there are seven physicians, two physician assistants, and a practice manager. How rewarding has it been to see it grow?
We have to find ways to help hospitalists take more ownership in their patients and their program. ... With our schedule, you can’t pawn off your responsibility to the nocturnist or the weekend guy.
—David Yu, MD, Decatur (Ill.)
Memorial Hospital
A: It’s been very rewarding. I’m honored to have been chosen as a member of Team Hospitalist, and I’m honored to be a committee member for SHM’s Non-Physician Provider Committee. Those are personal honors, but they are reflections on the success of the program. It’s an honor for the entire Decatur Memorial Hospital, and the administration, that a program started four and a half years ago, indirectly, has received national recognition.
Q: You implemented a one-week-on, one-week-off schedule for your hospitalists as a way to decrease signouts. How did that come about?
A: Signouts have been the bane of medical mistakes. Instead of having signouts twice a day, we have one physician on call for that entire week for his or her patients. It’s patient-centric versus schedule-centric. Physicians leave the hospital when their work is done, instead of looking at the clock and waiting to sign out at a certain time like a factory worker. It treats hospitalists not as shift workers but as attending physicians. It gives them due respect that they can manage their own patients responsibly.
Q: Do you think the schedule improves the quality of patient care?
A: The continuity of care is incredible. If you are admitted and discharged between Mondays, you have one hospitalist in charge of your entire case, instead of multiple physicians being on call for you. That increases patient satisfaction, reduces medical errors, and eliminates the need for unnecessary tests when new physicians take over. I’m also a huge believer that scheduling brings out the best and worst in hospitalists.
Q: How does it bring out the best in them?
A: As medical directors, we have to find ways to help hospitalists take more ownership in their patients and their program. If they’re thinking, “My shift is ending and I’m going to be off and I can hand this issue off to the next doctor,” that can have a tremendous effect on the quality of care and the way a hospitalist delivers medicine. With our schedule, you can’t pawn off your responsibility to the nocturnist or the weekend guy. … If something goes wrong or if the ball gets dropped, there’s no one else to blame it on.
Q: You developed a system at Decatur through which patient discharge summaries are sent electronically to primary-care physicians, often before the patient leaves the hospital. Have the primaries been receptive?
A: Absolutely. Communication is the mother’s milk of hospitalists. Some hospitalist programs are very large, they’re very busy, or there’s no incentive for them to do this because they’re the only game in town. But I practice in a mid-size community and I know all of these doctors. My reputation is my bond. I have to provide good service.
Q: What do you enjoy most about your role as a hospitalist?
A: I love solving problems for a patient. I also love how the relationship builds. You introduce yourself to a patient and their family as a hospitalist and they’re thinking, “Who the heck are you?” For a few seconds, it’s like meeting someone on a blind date. And when they’re discharged, they tell you they had a pleasant experience and they appreciate your help. It’s a courtship at a rapid pace.
Q: What do you consider to be your biggest challenge?
A: Recruitment; the administration asking us to take on more responsibilities; burnout. … We’re a typical hospitalist program; I think the problems are pretty universal.
Q: How do you address those challenges?
A: As medical director, you’re always navigating political and personal minefields. It comes back to developing relationships. The only way to earn goodwill is to give and provide service. That’s a problem some hospitalist programs run into. They want to instantly demand respect. You can’t demand it; you have to earn it. Sometimes hospitalists feel dumped on. Those are opportunities … to provide service in a willing and positive way instead of complaining. I’m not saying you have to be a whipping boy, but there are times when you have to give a little to get a little. That’s where the wisdom of the medical director comes in and sets the whole tone.
Q: What’s ahead for the academic side of your career?
A: We’re considering the possibility of starting a family practice fellowship program for attending residents who finish but want to go into the field of hospital medicine and want additional training. It’s not a done deal, but it’s an exciting possibility.
Q: How so?
A: Every medical director says they have a hard time recruiting. One way we can help solve the problem is by producing more hospitalists. We can’t just complain. We have to increase the pool of professionals interested in our model, train them, and get them integrated into our system.
Q: What advice would you give a student who is considering going that route?
A: You have to be a good communicator, you have to enjoy taking care of very sick people, and you have to enjoy solving very complex problems. You can’t just do it for the lifestyle. If you do, you won’t be happy in the long run. If I ask a medical student or resident why they want to be a hospitalist and they say, “I like the one-week-on, one-week-off schedule,” I tell them, “If that’s the reason you’re considering it, you really should reconsider.” TH
Mark Leiser is a freelance writer in New Jersey.
David Yu, MD, learned early on the value of being flexible. While attending Washington University in St. Louis, he found his calling when he changed his major from economics to biology. When the malpractice insurance crisis forced him to close his private practice, he embraced an opportunity to launch a program devoted to the “newfangled concept” of hospital medicine.
“I’m kind of like the accidental tourist,” says Dr. Yu, medical director of hospitalist services at the 372-bed Decatur Memorial Hospital in Decatur, Ill., and clinical assistant professor of family and community medicine at Southern Illinois University School of Medicine in Carbondale. “I didn’t really go to college with the mind-set of being a doctor, and when I became a doctor, there was no such thing as a hospitalist. … I went where the current took me and, fortunately, here I am.”
Question: What prompted the switch from economics to pre-med/biology?
Answer: When I got to the upper-level econ classes, I realized why the economy is the way it is: because nobody can understand how it works. My sister was in medical school. She really liked it and she talked me into it.
Q: You spent nine years in traditional practice. Why did you become a hospitalist?
A: In 2004, my malpractice insurance rate shot up 400% without any active lawsuits, so I had to close my practice. I had the choice of joining another traditional group, or Decatur (Memorial Hospital) was starting a new hospitalist program. To quote “The Godfather,” they made me an offer I couldn’t refuse.
Q: How did your experience in traditional practice prepare you for your role as a hospitalist?
A: I had been surrounded by incredible specialists. I saw how they interacted with me and how they treated my patients. As hospitalists, we are serving our patients, but really our clientele is the physicians we admit for. When I made the switch, I really had an idea of how a hospitalist should serve traditional practice.
Q: What is that service model?
A: It comes down to what I call the three A’s: You have to be available, you have to be able, and you have to be amicable. One of the problems in our field is a lot of hospitalists complain they’re treated like residents. They say they don’t get respect. They feel mistreated. That’s the wrong attitude. You can’t just ask for respect or demand it. You have to develop relationships.
Q: When Decatur’s hospitalist program started, you were on your own. Now there are seven physicians, two physician assistants, and a practice manager. How rewarding has it been to see it grow?
We have to find ways to help hospitalists take more ownership in their patients and their program. ... With our schedule, you can’t pawn off your responsibility to the nocturnist or the weekend guy.
—David Yu, MD, Decatur (Ill.)
Memorial Hospital
A: It’s been very rewarding. I’m honored to have been chosen as a member of Team Hospitalist, and I’m honored to be a committee member for SHM’s Non-Physician Provider Committee. Those are personal honors, but they are reflections on the success of the program. It’s an honor for the entire Decatur Memorial Hospital, and the administration, that a program started four and a half years ago, indirectly, has received national recognition.
Q: You implemented a one-week-on, one-week-off schedule for your hospitalists as a way to decrease signouts. How did that come about?
A: Signouts have been the bane of medical mistakes. Instead of having signouts twice a day, we have one physician on call for that entire week for his or her patients. It’s patient-centric versus schedule-centric. Physicians leave the hospital when their work is done, instead of looking at the clock and waiting to sign out at a certain time like a factory worker. It treats hospitalists not as shift workers but as attending physicians. It gives them due respect that they can manage their own patients responsibly.
Q: Do you think the schedule improves the quality of patient care?
A: The continuity of care is incredible. If you are admitted and discharged between Mondays, you have one hospitalist in charge of your entire case, instead of multiple physicians being on call for you. That increases patient satisfaction, reduces medical errors, and eliminates the need for unnecessary tests when new physicians take over. I’m also a huge believer that scheduling brings out the best and worst in hospitalists.
Q: How does it bring out the best in them?
A: As medical directors, we have to find ways to help hospitalists take more ownership in their patients and their program. If they’re thinking, “My shift is ending and I’m going to be off and I can hand this issue off to the next doctor,” that can have a tremendous effect on the quality of care and the way a hospitalist delivers medicine. With our schedule, you can’t pawn off your responsibility to the nocturnist or the weekend guy. … If something goes wrong or if the ball gets dropped, there’s no one else to blame it on.
Q: You developed a system at Decatur through which patient discharge summaries are sent electronically to primary-care physicians, often before the patient leaves the hospital. Have the primaries been receptive?
A: Absolutely. Communication is the mother’s milk of hospitalists. Some hospitalist programs are very large, they’re very busy, or there’s no incentive for them to do this because they’re the only game in town. But I practice in a mid-size community and I know all of these doctors. My reputation is my bond. I have to provide good service.
Q: What do you enjoy most about your role as a hospitalist?
A: I love solving problems for a patient. I also love how the relationship builds. You introduce yourself to a patient and their family as a hospitalist and they’re thinking, “Who the heck are you?” For a few seconds, it’s like meeting someone on a blind date. And when they’re discharged, they tell you they had a pleasant experience and they appreciate your help. It’s a courtship at a rapid pace.
Q: What do you consider to be your biggest challenge?
A: Recruitment; the administration asking us to take on more responsibilities; burnout. … We’re a typical hospitalist program; I think the problems are pretty universal.
Q: How do you address those challenges?
A: As medical director, you’re always navigating political and personal minefields. It comes back to developing relationships. The only way to earn goodwill is to give and provide service. That’s a problem some hospitalist programs run into. They want to instantly demand respect. You can’t demand it; you have to earn it. Sometimes hospitalists feel dumped on. Those are opportunities … to provide service in a willing and positive way instead of complaining. I’m not saying you have to be a whipping boy, but there are times when you have to give a little to get a little. That’s where the wisdom of the medical director comes in and sets the whole tone.
Q: What’s ahead for the academic side of your career?
A: We’re considering the possibility of starting a family practice fellowship program for attending residents who finish but want to go into the field of hospital medicine and want additional training. It’s not a done deal, but it’s an exciting possibility.
Q: How so?
A: Every medical director says they have a hard time recruiting. One way we can help solve the problem is by producing more hospitalists. We can’t just complain. We have to increase the pool of professionals interested in our model, train them, and get them integrated into our system.
Q: What advice would you give a student who is considering going that route?
A: You have to be a good communicator, you have to enjoy taking care of very sick people, and you have to enjoy solving very complex problems. You can’t just do it for the lifestyle. If you do, you won’t be happy in the long run. If I ask a medical student or resident why they want to be a hospitalist and they say, “I like the one-week-on, one-week-off schedule,” I tell them, “If that’s the reason you’re considering it, you really should reconsider.” TH
Mark Leiser is a freelance writer in New Jersey.
Palliative-Care Payment
Many hospitalists provide palliative-care services to patients at the request of physicians within their own groups or from other specialists. Varying factors affect how hospitalists report these services—namely, the nature of the request and the type of service provided. Palliative-care programs can be quite costly as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives is pertinent.
Nature of the Request
Members of a palliative-care team often are called on to provide management options to assist in reducing pain and suffering associated with both terminal and nonterminal disease, thereby improving a patient’s quality of life. When a palliative-care specialist is asked to provide an opinion or advice, the initial service could qualify as a consultation. However, all requirements must be met in order to report the service as an inpatient consultation (codes 99251-99255).
There must be a written request from a qualified healthcare provider involved in the patient’s care (e.g., a physician, resident, or nurse practitioner). In the inpatient setting, this request can be documented as a physician order or in the assessment of the requesting provider’s progress note. Standing orders for consultation are not permitted. Ideally, the requesting provider should identify the reason for a consult to support the medical necessity of the service.
Additionally, the palliative-care physician renders and documents the service, then reports findings to the requesting physician. The consultant’s required written report does not have to be sent separately to the requesting physician. Because the requesting physician and the consultant share a common medical record in an inpatient setting, the consultant’s inpatient progress note suffices the “written report” requirement.
One concern about billing consultations involves the nature of the request. If the requesting physician documents the need for an opinion or advice from the palliative-care specialist, the service can be reported as a consultation. If, however, the request states consult for “medical management” or “palliative management,” it’s less likely that payors will consider the service a consultation. In the latter situation, it appears as if the requesting physician is not seeking an opinion or advice from the consultant to incorporate into his own plan of care for the patient and would rather the consultant take over that portion of patient care.
Recently revised billing policies prevent the consultant from billing consults under these circumstances. Without a sufficient request for consultation, the palliative-care specialist can only report “subsequent” hospital care services.1 Language that better supports the consultative nature of the request is:
- Consult for an opinion or advice on palliative measures;
- Consult for evaluation of palliative options; and
- Consult palliative care for treatment options.
Proper Documentation
The requesting physician can be in the same or different provider group as the consultant. The consultant must possess expertise in an area beyond that of the requesting provider. Because the specialty designation for most hospitalists is internal medicine, palliative-care claims could be scrutinized more closely. This does not necessarily occur when the requesting provider has a different two-digit specialty designation (e.g., internal medicine and gastroenterology).2 Scrutiny is more likely to occur when the requesting provider has the same internal-medicine designation as the palliative-care consultant, even if they are in different provider groups.
Payor concern escalates when physicians of the same designated specialty submit claims for the same patient on the same date. Having different primary diagnosis codes attached to each visit level does not necessarily help. The payor is likely to deny the second claim received, pending a review of documentation. If this happens, the provider who received the denial should submit a copy of both progress notes for the date in question. Hopefully, the distinction between the services is demonstrated in the documentation.
Service Type
Palliative services might involve obtaining and documenting the standard key components for visit-level selection: history, exam, and medical decision-making.3 However, the palliative-care specialist might spend more time providing counseling or coordination of care for a patient and family. When this occurs, the palliative-care specialist should not forget about the guidelines for reporting time-based services.4 Inpatient services may be reported on the basis of time, as long as a face-to-face service between the provider and the patient occurs. Consider the total time spent face to face with the patient, and the time spent obtaining, discussing, and coordinating patient care, while you are in the patient’s unit or floor.
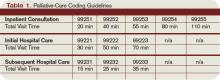
As a reminder, document the total time, the amount of time spent counseling, and the details of discussion and coordination. The physician may count the time spent counseling the patient’s family regarding the treatment and care, as long as the focus is not emotional support for the family, the meeting takes place in the patient’s unit or floor, and the patient is present, unless there is medically supported reason for which the patient is unable to participate (e.g., cognitive impairment). The palliative-care specialist can then select the visit level based on time.5 (See Table 1, above.) TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.10. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26, Section 10.8. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c26.pdf. Accessed Jan. 30, 2009.
3. Centers for Medicare and Medicaid Services. Documentation Guidelines for Evaluation and Management Services. CMS Web site. Available at: www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp. Accessed Jan. 30, 2009.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Many hospitalists provide palliative-care services to patients at the request of physicians within their own groups or from other specialists. Varying factors affect how hospitalists report these services—namely, the nature of the request and the type of service provided. Palliative-care programs can be quite costly as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives is pertinent.
Nature of the Request
Members of a palliative-care team often are called on to provide management options to assist in reducing pain and suffering associated with both terminal and nonterminal disease, thereby improving a patient’s quality of life. When a palliative-care specialist is asked to provide an opinion or advice, the initial service could qualify as a consultation. However, all requirements must be met in order to report the service as an inpatient consultation (codes 99251-99255).
There must be a written request from a qualified healthcare provider involved in the patient’s care (e.g., a physician, resident, or nurse practitioner). In the inpatient setting, this request can be documented as a physician order or in the assessment of the requesting provider’s progress note. Standing orders for consultation are not permitted. Ideally, the requesting provider should identify the reason for a consult to support the medical necessity of the service.
Additionally, the palliative-care physician renders and documents the service, then reports findings to the requesting physician. The consultant’s required written report does not have to be sent separately to the requesting physician. Because the requesting physician and the consultant share a common medical record in an inpatient setting, the consultant’s inpatient progress note suffices the “written report” requirement.
One concern about billing consultations involves the nature of the request. If the requesting physician documents the need for an opinion or advice from the palliative-care specialist, the service can be reported as a consultation. If, however, the request states consult for “medical management” or “palliative management,” it’s less likely that payors will consider the service a consultation. In the latter situation, it appears as if the requesting physician is not seeking an opinion or advice from the consultant to incorporate into his own plan of care for the patient and would rather the consultant take over that portion of patient care.
Recently revised billing policies prevent the consultant from billing consults under these circumstances. Without a sufficient request for consultation, the palliative-care specialist can only report “subsequent” hospital care services.1 Language that better supports the consultative nature of the request is:
- Consult for an opinion or advice on palliative measures;
- Consult for evaluation of palliative options; and
- Consult palliative care for treatment options.
Proper Documentation
The requesting physician can be in the same or different provider group as the consultant. The consultant must possess expertise in an area beyond that of the requesting provider. Because the specialty designation for most hospitalists is internal medicine, palliative-care claims could be scrutinized more closely. This does not necessarily occur when the requesting provider has a different two-digit specialty designation (e.g., internal medicine and gastroenterology).2 Scrutiny is more likely to occur when the requesting provider has the same internal-medicine designation as the palliative-care consultant, even if they are in different provider groups.
Payor concern escalates when physicians of the same designated specialty submit claims for the same patient on the same date. Having different primary diagnosis codes attached to each visit level does not necessarily help. The payor is likely to deny the second claim received, pending a review of documentation. If this happens, the provider who received the denial should submit a copy of both progress notes for the date in question. Hopefully, the distinction between the services is demonstrated in the documentation.
Service Type
Palliative services might involve obtaining and documenting the standard key components for visit-level selection: history, exam, and medical decision-making.3 However, the palliative-care specialist might spend more time providing counseling or coordination of care for a patient and family. When this occurs, the palliative-care specialist should not forget about the guidelines for reporting time-based services.4 Inpatient services may be reported on the basis of time, as long as a face-to-face service between the provider and the patient occurs. Consider the total time spent face to face with the patient, and the time spent obtaining, discussing, and coordinating patient care, while you are in the patient’s unit or floor.
As a reminder, document the total time, the amount of time spent counseling, and the details of discussion and coordination. The physician may count the time spent counseling the patient’s family regarding the treatment and care, as long as the focus is not emotional support for the family, the meeting takes place in the patient’s unit or floor, and the patient is present, unless there is medically supported reason for which the patient is unable to participate (e.g., cognitive impairment). The palliative-care specialist can then select the visit level based on time.5 (See Table 1, above.) TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.10. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26, Section 10.8. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c26.pdf. Accessed Jan. 30, 2009.
3. Centers for Medicare and Medicaid Services. Documentation Guidelines for Evaluation and Management Services. CMS Web site. Available at: www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp. Accessed Jan. 30, 2009.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Many hospitalists provide palliative-care services to patients at the request of physicians within their own groups or from other specialists. Varying factors affect how hospitalists report these services—namely, the nature of the request and the type of service provided. Palliative-care programs can be quite costly as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives is pertinent.
Nature of the Request
Members of a palliative-care team often are called on to provide management options to assist in reducing pain and suffering associated with both terminal and nonterminal disease, thereby improving a patient’s quality of life. When a palliative-care specialist is asked to provide an opinion or advice, the initial service could qualify as a consultation. However, all requirements must be met in order to report the service as an inpatient consultation (codes 99251-99255).
There must be a written request from a qualified healthcare provider involved in the patient’s care (e.g., a physician, resident, or nurse practitioner). In the inpatient setting, this request can be documented as a physician order or in the assessment of the requesting provider’s progress note. Standing orders for consultation are not permitted. Ideally, the requesting provider should identify the reason for a consult to support the medical necessity of the service.
Additionally, the palliative-care physician renders and documents the service, then reports findings to the requesting physician. The consultant’s required written report does not have to be sent separately to the requesting physician. Because the requesting physician and the consultant share a common medical record in an inpatient setting, the consultant’s inpatient progress note suffices the “written report” requirement.
One concern about billing consultations involves the nature of the request. If the requesting physician documents the need for an opinion or advice from the palliative-care specialist, the service can be reported as a consultation. If, however, the request states consult for “medical management” or “palliative management,” it’s less likely that payors will consider the service a consultation. In the latter situation, it appears as if the requesting physician is not seeking an opinion or advice from the consultant to incorporate into his own plan of care for the patient and would rather the consultant take over that portion of patient care.
Recently revised billing policies prevent the consultant from billing consults under these circumstances. Without a sufficient request for consultation, the palliative-care specialist can only report “subsequent” hospital care services.1 Language that better supports the consultative nature of the request is:
- Consult for an opinion or advice on palliative measures;
- Consult for evaluation of palliative options; and
- Consult palliative care for treatment options.
Proper Documentation
The requesting physician can be in the same or different provider group as the consultant. The consultant must possess expertise in an area beyond that of the requesting provider. Because the specialty designation for most hospitalists is internal medicine, palliative-care claims could be scrutinized more closely. This does not necessarily occur when the requesting provider has a different two-digit specialty designation (e.g., internal medicine and gastroenterology).2 Scrutiny is more likely to occur when the requesting provider has the same internal-medicine designation as the palliative-care consultant, even if they are in different provider groups.
Payor concern escalates when physicians of the same designated specialty submit claims for the same patient on the same date. Having different primary diagnosis codes attached to each visit level does not necessarily help. The payor is likely to deny the second claim received, pending a review of documentation. If this happens, the provider who received the denial should submit a copy of both progress notes for the date in question. Hopefully, the distinction between the services is demonstrated in the documentation.
Service Type
Palliative services might involve obtaining and documenting the standard key components for visit-level selection: history, exam, and medical decision-making.3 However, the palliative-care specialist might spend more time providing counseling or coordination of care for a patient and family. When this occurs, the palliative-care specialist should not forget about the guidelines for reporting time-based services.4 Inpatient services may be reported on the basis of time, as long as a face-to-face service between the provider and the patient occurs. Consider the total time spent face to face with the patient, and the time spent obtaining, discussing, and coordinating patient care, while you are in the patient’s unit or floor.
As a reminder, document the total time, the amount of time spent counseling, and the details of discussion and coordination. The physician may count the time spent counseling the patient’s family regarding the treatment and care, as long as the focus is not emotional support for the family, the meeting takes place in the patient’s unit or floor, and the patient is present, unless there is medically supported reason for which the patient is unable to participate (e.g., cognitive impairment). The palliative-care specialist can then select the visit level based on time.5 (See Table 1, above.) TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.10. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 26, Section 10.8. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c26.pdf. Accessed Jan. 30, 2009.
3. Centers for Medicare and Medicaid Services. Documentation Guidelines for Evaluation and Management Services. CMS Web site. Available at: www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp. Accessed Jan. 30, 2009.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 30, 2009.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
A Pivotal Year for Policy
Change is in the air. With a new ad-ministration promising to be a change agent, an overhauled Congress, and a seemingly unanimous national interest in tackling healthcare reform, what changes can hospital medicine expect in 2009?
“I think there’s certainly the political will and interest now,” says Eric Siegal, MD, chair of SHM’s Public Policy Committee. “We haven’t had enough political will to ‘go big’ until recently. Now that we have it, the trillion-dollar question is where the money will come from.”
With that in mind, let’s explore three of the hottest healthcare issues:
Comprehensive Healthcare Reform
Providing healthcare coverage to all or most Americans was a centerpiece of President Obama’s campaign and a significant part of a proposal published by Senate Finance Committee Chairman Max Baucus (D-Mont.). Any actual reform will come through legislation, which will have to spell out who is covered and how, and where the money will come from. Any legislation will have to pass both the House and the Senate before Obama can sign it into law.
“The Democrats have certainly said [healthcare reform] is going to happen. Obama has talked about it … but how bipartisan will the effort be?” Dr. Siegal says. “This is too big and important for unilateral action; any durable healthcare reform must have bipartisan support. I do think that everyone can agree that the healthcare system is going to bankrupt itself if we don’t make changes.”
Dr. Siegal is skeptical that a major reform bill of any stripe will be passed anytime soon. “Given the depth of the recession and the projected cost of the stimulus package, my guess is that we will not see significant healthcare reform legislation passed in 2009,” he predicts. “However, I think that 2009 is still going to be an important year in that Congress will lay much of the foundation for new legislation. My guess is that 2010 is the year to look for major healthcare reform. And we want to make sure that the reform that happens is in the best interests of healthcare and of hospitalists.”
Less encompassing aspects of healthcare reform, the “easy stuff,” should have enough votes to pass in 2009, Dr. Siegal says. A good example is the State Children’s Health Insurance Program (SCHIP), which was passed the first week of February and increases the number of children eligible for free medical coverage from 7 million to 11 million. “SCHIP was as close to a slam dunk as possible.”
Major overhauls to the system, such as the healthcare exchange outlined in Sen. Baucus’ proposal or a major reworking of Medicare, may come about further down the road. “Those are going to take a lot of time, energy, and money,” Dr. Siegal says, “and I think that Congress has bigger fish to fry right now.”
Physician Fee Schedule
Last summer, physician fees paid by Medicare were slashed by 10.6% and then restored—with a 1.1% increase—when Congress overrode a presidential veto. SHM members were among the many physicians who fought the fee cut with letters and e-mails to Congress. However, the current fee schedule is short-lived: A 20% fee cut is scheduled for 2010. Will hospitalists and others have to go through the same battle all over again to maintain their Medicare payments?
Bradley Flansbaum, DO, MPH, chief of the hospitalist section at Lenox Hill Hospital in New York City and a member of SHM’s Public Policy Committee, points out “there are some proposals to modify the SGR [sustainable growth rate] formula, so this may not be the hot issue it was in 2008.” The SGR is used to set reimbursement rates for specific services and have been targeted by numerous stakeholders as flawed.
Regardless of the reimbursement formula, the Centers for Medicare and Medicaid Services (CMS) physician fee schedule might become less crucial to hospitalists’ income. “In the context of healthcare reform, you have to wonder if fee-for-service is even going to be relevant,” Dr. Flansbaum explains. “I think that Congress and MedPAC will think things through and admit that we can’t keep Band-Aiding a broken system.”
A major system overhaul might be looming. “This may not happen this year,” he says, “but I think that if Congress needs to avert the pay cut, then they will say they’re doing this one more time, with the caveat that payment will be drastically different” in the near future.
Delivery System Reform
A third hot topic for 2009 is legislation and consideration of changes in the healthcare delivery system, including payment reform, healthcare information technology, and improving care coordination.
“We think that payment reform is central to reshaping the healthcare system,” Dr. Siegal says.
As for moving toward a fee-for-quality system: “Well, there’s politics and there’s policy,” Dr. Flansbaum says. “Politics says we need to reward quality. However, the policy is that the methods of measuring quality haven’t evolved to the point where we can go forward. Everything is in beta-testing right now; we’re not ready to make any sweeping decisions. The delivery system has to be well-thought-out. It’s complicated.”
For example, in 2008, the CMS published a proposed inpatient prospective payment system rule, which included additional categories of hospital-acquired conditions that would no longer carry higher Medicare payments. The list caused industry alarm because some of the conditions—including Clostridium difficile-associated disease (see “Clostridium Difficile Infection: Are We Doing Enough,” p. 12)—were seen as only partially preventable in hospitalized patients or not entirely hospital-acquired.
The lesson learned? Any reform to healthcare delivery must be carefully considered, along with input from the medical community. “Healthcare is 16% of the gross domestic product. You don’t take that and spin it around in one day,” Dr. Flansbaum says. “It’s best to approach reform slowly and really think it through.”
Even so, there is no guarantee that reform legislation will make it through Congress.
“Another aspect to consider is that there are ideological differences between Democrats and Republicans,” Dr. Flansbaum adds. “ … Many Republicans are miles away from [Democrats] ideologically. Further still, with Daschle’s exit, it is unclear how his replacement will approach any overhaul.”
Of course, nobody has a crystal ball. This year may bring forth less drastic changes than hospital medicine is predicting. Then again, considering the economic and political climate, reform could take place faster than seems possible.
Only time will tell. TH
Jane Jerrard is a medical writer based in Chicago.
Change is in the air. With a new ad-ministration promising to be a change agent, an overhauled Congress, and a seemingly unanimous national interest in tackling healthcare reform, what changes can hospital medicine expect in 2009?
“I think there’s certainly the political will and interest now,” says Eric Siegal, MD, chair of SHM’s Public Policy Committee. “We haven’t had enough political will to ‘go big’ until recently. Now that we have it, the trillion-dollar question is where the money will come from.”
With that in mind, let’s explore three of the hottest healthcare issues:
Comprehensive Healthcare Reform
Providing healthcare coverage to all or most Americans was a centerpiece of President Obama’s campaign and a significant part of a proposal published by Senate Finance Committee Chairman Max Baucus (D-Mont.). Any actual reform will come through legislation, which will have to spell out who is covered and how, and where the money will come from. Any legislation will have to pass both the House and the Senate before Obama can sign it into law.
“The Democrats have certainly said [healthcare reform] is going to happen. Obama has talked about it … but how bipartisan will the effort be?” Dr. Siegal says. “This is too big and important for unilateral action; any durable healthcare reform must have bipartisan support. I do think that everyone can agree that the healthcare system is going to bankrupt itself if we don’t make changes.”
Dr. Siegal is skeptical that a major reform bill of any stripe will be passed anytime soon. “Given the depth of the recession and the projected cost of the stimulus package, my guess is that we will not see significant healthcare reform legislation passed in 2009,” he predicts. “However, I think that 2009 is still going to be an important year in that Congress will lay much of the foundation for new legislation. My guess is that 2010 is the year to look for major healthcare reform. And we want to make sure that the reform that happens is in the best interests of healthcare and of hospitalists.”
Less encompassing aspects of healthcare reform, the “easy stuff,” should have enough votes to pass in 2009, Dr. Siegal says. A good example is the State Children’s Health Insurance Program (SCHIP), which was passed the first week of February and increases the number of children eligible for free medical coverage from 7 million to 11 million. “SCHIP was as close to a slam dunk as possible.”
Major overhauls to the system, such as the healthcare exchange outlined in Sen. Baucus’ proposal or a major reworking of Medicare, may come about further down the road. “Those are going to take a lot of time, energy, and money,” Dr. Siegal says, “and I think that Congress has bigger fish to fry right now.”
Physician Fee Schedule
Last summer, physician fees paid by Medicare were slashed by 10.6% and then restored—with a 1.1% increase—when Congress overrode a presidential veto. SHM members were among the many physicians who fought the fee cut with letters and e-mails to Congress. However, the current fee schedule is short-lived: A 20% fee cut is scheduled for 2010. Will hospitalists and others have to go through the same battle all over again to maintain their Medicare payments?
Bradley Flansbaum, DO, MPH, chief of the hospitalist section at Lenox Hill Hospital in New York City and a member of SHM’s Public Policy Committee, points out “there are some proposals to modify the SGR [sustainable growth rate] formula, so this may not be the hot issue it was in 2008.” The SGR is used to set reimbursement rates for specific services and have been targeted by numerous stakeholders as flawed.
Regardless of the reimbursement formula, the Centers for Medicare and Medicaid Services (CMS) physician fee schedule might become less crucial to hospitalists’ income. “In the context of healthcare reform, you have to wonder if fee-for-service is even going to be relevant,” Dr. Flansbaum explains. “I think that Congress and MedPAC will think things through and admit that we can’t keep Band-Aiding a broken system.”
A major system overhaul might be looming. “This may not happen this year,” he says, “but I think that if Congress needs to avert the pay cut, then they will say they’re doing this one more time, with the caveat that payment will be drastically different” in the near future.
Delivery System Reform
A third hot topic for 2009 is legislation and consideration of changes in the healthcare delivery system, including payment reform, healthcare information technology, and improving care coordination.
“We think that payment reform is central to reshaping the healthcare system,” Dr. Siegal says.
As for moving toward a fee-for-quality system: “Well, there’s politics and there’s policy,” Dr. Flansbaum says. “Politics says we need to reward quality. However, the policy is that the methods of measuring quality haven’t evolved to the point where we can go forward. Everything is in beta-testing right now; we’re not ready to make any sweeping decisions. The delivery system has to be well-thought-out. It’s complicated.”
For example, in 2008, the CMS published a proposed inpatient prospective payment system rule, which included additional categories of hospital-acquired conditions that would no longer carry higher Medicare payments. The list caused industry alarm because some of the conditions—including Clostridium difficile-associated disease (see “Clostridium Difficile Infection: Are We Doing Enough,” p. 12)—were seen as only partially preventable in hospitalized patients or not entirely hospital-acquired.
The lesson learned? Any reform to healthcare delivery must be carefully considered, along with input from the medical community. “Healthcare is 16% of the gross domestic product. You don’t take that and spin it around in one day,” Dr. Flansbaum says. “It’s best to approach reform slowly and really think it through.”
Even so, there is no guarantee that reform legislation will make it through Congress.
“Another aspect to consider is that there are ideological differences between Democrats and Republicans,” Dr. Flansbaum adds. “ … Many Republicans are miles away from [Democrats] ideologically. Further still, with Daschle’s exit, it is unclear how his replacement will approach any overhaul.”
Of course, nobody has a crystal ball. This year may bring forth less drastic changes than hospital medicine is predicting. Then again, considering the economic and political climate, reform could take place faster than seems possible.
Only time will tell. TH
Jane Jerrard is a medical writer based in Chicago.
Change is in the air. With a new ad-ministration promising to be a change agent, an overhauled Congress, and a seemingly unanimous national interest in tackling healthcare reform, what changes can hospital medicine expect in 2009?
“I think there’s certainly the political will and interest now,” says Eric Siegal, MD, chair of SHM’s Public Policy Committee. “We haven’t had enough political will to ‘go big’ until recently. Now that we have it, the trillion-dollar question is where the money will come from.”
With that in mind, let’s explore three of the hottest healthcare issues:
Comprehensive Healthcare Reform
Providing healthcare coverage to all or most Americans was a centerpiece of President Obama’s campaign and a significant part of a proposal published by Senate Finance Committee Chairman Max Baucus (D-Mont.). Any actual reform will come through legislation, which will have to spell out who is covered and how, and where the money will come from. Any legislation will have to pass both the House and the Senate before Obama can sign it into law.
“The Democrats have certainly said [healthcare reform] is going to happen. Obama has talked about it … but how bipartisan will the effort be?” Dr. Siegal says. “This is too big and important for unilateral action; any durable healthcare reform must have bipartisan support. I do think that everyone can agree that the healthcare system is going to bankrupt itself if we don’t make changes.”
Dr. Siegal is skeptical that a major reform bill of any stripe will be passed anytime soon. “Given the depth of the recession and the projected cost of the stimulus package, my guess is that we will not see significant healthcare reform legislation passed in 2009,” he predicts. “However, I think that 2009 is still going to be an important year in that Congress will lay much of the foundation for new legislation. My guess is that 2010 is the year to look for major healthcare reform. And we want to make sure that the reform that happens is in the best interests of healthcare and of hospitalists.”
Less encompassing aspects of healthcare reform, the “easy stuff,” should have enough votes to pass in 2009, Dr. Siegal says. A good example is the State Children’s Health Insurance Program (SCHIP), which was passed the first week of February and increases the number of children eligible for free medical coverage from 7 million to 11 million. “SCHIP was as close to a slam dunk as possible.”
Major overhauls to the system, such as the healthcare exchange outlined in Sen. Baucus’ proposal or a major reworking of Medicare, may come about further down the road. “Those are going to take a lot of time, energy, and money,” Dr. Siegal says, “and I think that Congress has bigger fish to fry right now.”
Physician Fee Schedule
Last summer, physician fees paid by Medicare were slashed by 10.6% and then restored—with a 1.1% increase—when Congress overrode a presidential veto. SHM members were among the many physicians who fought the fee cut with letters and e-mails to Congress. However, the current fee schedule is short-lived: A 20% fee cut is scheduled for 2010. Will hospitalists and others have to go through the same battle all over again to maintain their Medicare payments?
Bradley Flansbaum, DO, MPH, chief of the hospitalist section at Lenox Hill Hospital in New York City and a member of SHM’s Public Policy Committee, points out “there are some proposals to modify the SGR [sustainable growth rate] formula, so this may not be the hot issue it was in 2008.” The SGR is used to set reimbursement rates for specific services and have been targeted by numerous stakeholders as flawed.
Regardless of the reimbursement formula, the Centers for Medicare and Medicaid Services (CMS) physician fee schedule might become less crucial to hospitalists’ income. “In the context of healthcare reform, you have to wonder if fee-for-service is even going to be relevant,” Dr. Flansbaum explains. “I think that Congress and MedPAC will think things through and admit that we can’t keep Band-Aiding a broken system.”
A major system overhaul might be looming. “This may not happen this year,” he says, “but I think that if Congress needs to avert the pay cut, then they will say they’re doing this one more time, with the caveat that payment will be drastically different” in the near future.
Delivery System Reform
A third hot topic for 2009 is legislation and consideration of changes in the healthcare delivery system, including payment reform, healthcare information technology, and improving care coordination.
“We think that payment reform is central to reshaping the healthcare system,” Dr. Siegal says.
As for moving toward a fee-for-quality system: “Well, there’s politics and there’s policy,” Dr. Flansbaum says. “Politics says we need to reward quality. However, the policy is that the methods of measuring quality haven’t evolved to the point where we can go forward. Everything is in beta-testing right now; we’re not ready to make any sweeping decisions. The delivery system has to be well-thought-out. It’s complicated.”
For example, in 2008, the CMS published a proposed inpatient prospective payment system rule, which included additional categories of hospital-acquired conditions that would no longer carry higher Medicare payments. The list caused industry alarm because some of the conditions—including Clostridium difficile-associated disease (see “Clostridium Difficile Infection: Are We Doing Enough,” p. 12)—were seen as only partially preventable in hospitalized patients or not entirely hospital-acquired.
The lesson learned? Any reform to healthcare delivery must be carefully considered, along with input from the medical community. “Healthcare is 16% of the gross domestic product. You don’t take that and spin it around in one day,” Dr. Flansbaum says. “It’s best to approach reform slowly and really think it through.”
Even so, there is no guarantee that reform legislation will make it through Congress.
“Another aspect to consider is that there are ideological differences between Democrats and Republicans,” Dr. Flansbaum adds. “ … Many Republicans are miles away from [Democrats] ideologically. Further still, with Daschle’s exit, it is unclear how his replacement will approach any overhaul.”
Of course, nobody has a crystal ball. This year may bring forth less drastic changes than hospital medicine is predicting. Then again, considering the economic and political climate, reform could take place faster than seems possible.
Only time will tell. TH
Jane Jerrard is a medical writer based in Chicago.
Appearance Counts
Your physical appearance—the image and demeanor you present in your work environment—plays an important role in your career. If you aspire to a leadership position or are looking for a new job, be sure to examine your outward style as carefully as you craft your curriculum vitae.
“This is a huge, woefully unexplored way that physicians relate to the world,” says Mary Frances Lyons, MD, an executive search consultant with Witt/Kiefer in St. Louis. “Let’s call it body language. It’s the attitude or deportment you show. If you’re not the most corporate person in the world, you can still appear to be open, enthusiastic about your work, and have integrity.”
Kindergarten Revisited
Dr. Lyons frequently coaches physician executives before job interviews. She instructs many of them in the basics: standing up straight, making eye contact, smiling, and having a firm handshake. “This is literally your chance to connect with other people,” she says. “Send a signal that you want to connect, that you’re open, and you’ll bring that out in them as well.”
Her advice may seem simplistic, and she agrees. “You can literally learn this stuff in kindergarten—but many physicians don’t do it,” she says. “Their currency of credibility is how smart they are, and they rely on that. The truth is that no one in medical school ever teaches physicians that a large part of their medical success is how they interact with and relate to others—including patients, their boss, payers, and colleagues.” As a clinician, you can get by with minimal social skills or attention to your demeanor, but Dr. Lyons warns, “If you want to move up the food chain, this is professionally important.”
Typically, hospitalists are insulated from the traditional office dress code (i.e., suits and ties and heels), but doctors are not immune to the basic standards of workplace appearance. “For better or for worse, hospital medicine groups are not corporate,” Dr. Lyons points out. “The question is, how do you become corporate enough to get the job offer or the promotion?”
Look the Part
If you want a higher-level position, whether you’re aiming for a promotion, interviewing for an important committee position, or seeking a new job, consider the impression you make before you open your mouth.
“Your style and attitude is more important than how you dress,” Dr. Lyons says. “However, appearance-wise, you want to look professional and serious … not somber. Be appropriate and nondescript; you don’t want interesting clothes or clothes that make a statement. You want people to think, ‘What a professional person,’ not ‘Wow, I really love those earrings.’ ”
When you have an important interview or meeting, wear a dark business suit. Pantsuits are fine for women, Dr. Lyons says. “You can never, ever go wrong with a suit,” she says. “You don’t want the people interviewing you to be better dressed than you. Your appearance signals how you’ll present yourself to patients.”
Ultimately, a physician’s behavior and professional interactions are significant considerations in the hiring process, says Kenneth Simone, DO, owner of Hospitalist and Practice Solutions in Veazie, Maine, and author of the upcoming book “Hospitalist Recruitment and Retention: Building a Hospital Medicine Program.” “It will affect relationships with all stakeholders in the healthcare system. Furthermore, if the hospitalist’s professional relationship with the nursing staff and other hospital staff disintegrates, it can affect patient care.”
Listen Up
During a job interview, promotional interview, or committee chair interview, the balance between how much you say and when you stop talking can reveal much about your attitude. Hiring managers look for leaders who can listen as well as they direct. “Doctors have no idea how to listen,” Dr. Lyons says. “I sometimes recommend that a client limit himself or herself to three sentences to answer a question.” Dr. Simone agrees. “A job candidate should discuss their professional and personal interests when queried but should refrain from dominating the discussion. It should be an interactive exchange,” he says.
Dr. Lyons recommends preparing for an interview by putting together a three- to five-minute presentation about who you are as a professional. Your interviewers will already have your resume, so avoid recounting what they already know. “If you’re having trouble with these things, put on your interview suit, then videotape yourself giving your presentation,” Dr. Lyons says. “Watch it and ask yourself, ‘Would I hire this person?’ It’s a grim exercise, but it’s effective.”
Consider your demeanor and make changes that allow you to show off your personal strengths and your ability to connect. Simple changes—upgrades, if you will—can lift you above your competition. “If concerns arise with one candidate, the rule of thumb is to avoid taking a chance on hiring a potential problem physician,” Dr. Simone says. “Recruitment is expensive. It has been estimated that making an incorrect [hire] can cost a program up to $100,000, when you consider expenses such as headhunter fees, sign-on bonus, moving expenses, and advertising, in addition to lost revenues for the program while staff participate in the recruitment process and lost productivity when the program is down one provider.”
A good attitude, openness to others, and a professional demeanor can bolster your career path. As Dr. Lyons points out, “If you don’t interview well, other people will make all the major decisions for your career. Physicians have not been taught to interview well. The good news is, it’s not that hard.” TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Your physical appearance—the image and demeanor you present in your work environment—plays an important role in your career. If you aspire to a leadership position or are looking for a new job, be sure to examine your outward style as carefully as you craft your curriculum vitae.
“This is a huge, woefully unexplored way that physicians relate to the world,” says Mary Frances Lyons, MD, an executive search consultant with Witt/Kiefer in St. Louis. “Let’s call it body language. It’s the attitude or deportment you show. If you’re not the most corporate person in the world, you can still appear to be open, enthusiastic about your work, and have integrity.”
Kindergarten Revisited
Dr. Lyons frequently coaches physician executives before job interviews. She instructs many of them in the basics: standing up straight, making eye contact, smiling, and having a firm handshake. “This is literally your chance to connect with other people,” she says. “Send a signal that you want to connect, that you’re open, and you’ll bring that out in them as well.”
Her advice may seem simplistic, and she agrees. “You can literally learn this stuff in kindergarten—but many physicians don’t do it,” she says. “Their currency of credibility is how smart they are, and they rely on that. The truth is that no one in medical school ever teaches physicians that a large part of their medical success is how they interact with and relate to others—including patients, their boss, payers, and colleagues.” As a clinician, you can get by with minimal social skills or attention to your demeanor, but Dr. Lyons warns, “If you want to move up the food chain, this is professionally important.”
Typically, hospitalists are insulated from the traditional office dress code (i.e., suits and ties and heels), but doctors are not immune to the basic standards of workplace appearance. “For better or for worse, hospital medicine groups are not corporate,” Dr. Lyons points out. “The question is, how do you become corporate enough to get the job offer or the promotion?”
Look the Part
If you want a higher-level position, whether you’re aiming for a promotion, interviewing for an important committee position, or seeking a new job, consider the impression you make before you open your mouth.
“Your style and attitude is more important than how you dress,” Dr. Lyons says. “However, appearance-wise, you want to look professional and serious … not somber. Be appropriate and nondescript; you don’t want interesting clothes or clothes that make a statement. You want people to think, ‘What a professional person,’ not ‘Wow, I really love those earrings.’ ”
When you have an important interview or meeting, wear a dark business suit. Pantsuits are fine for women, Dr. Lyons says. “You can never, ever go wrong with a suit,” she says. “You don’t want the people interviewing you to be better dressed than you. Your appearance signals how you’ll present yourself to patients.”
Ultimately, a physician’s behavior and professional interactions are significant considerations in the hiring process, says Kenneth Simone, DO, owner of Hospitalist and Practice Solutions in Veazie, Maine, and author of the upcoming book “Hospitalist Recruitment and Retention: Building a Hospital Medicine Program.” “It will affect relationships with all stakeholders in the healthcare system. Furthermore, if the hospitalist’s professional relationship with the nursing staff and other hospital staff disintegrates, it can affect patient care.”
Listen Up
During a job interview, promotional interview, or committee chair interview, the balance between how much you say and when you stop talking can reveal much about your attitude. Hiring managers look for leaders who can listen as well as they direct. “Doctors have no idea how to listen,” Dr. Lyons says. “I sometimes recommend that a client limit himself or herself to three sentences to answer a question.” Dr. Simone agrees. “A job candidate should discuss their professional and personal interests when queried but should refrain from dominating the discussion. It should be an interactive exchange,” he says.
Dr. Lyons recommends preparing for an interview by putting together a three- to five-minute presentation about who you are as a professional. Your interviewers will already have your resume, so avoid recounting what they already know. “If you’re having trouble with these things, put on your interview suit, then videotape yourself giving your presentation,” Dr. Lyons says. “Watch it and ask yourself, ‘Would I hire this person?’ It’s a grim exercise, but it’s effective.”
Consider your demeanor and make changes that allow you to show off your personal strengths and your ability to connect. Simple changes—upgrades, if you will—can lift you above your competition. “If concerns arise with one candidate, the rule of thumb is to avoid taking a chance on hiring a potential problem physician,” Dr. Simone says. “Recruitment is expensive. It has been estimated that making an incorrect [hire] can cost a program up to $100,000, when you consider expenses such as headhunter fees, sign-on bonus, moving expenses, and advertising, in addition to lost revenues for the program while staff participate in the recruitment process and lost productivity when the program is down one provider.”
A good attitude, openness to others, and a professional demeanor can bolster your career path. As Dr. Lyons points out, “If you don’t interview well, other people will make all the major decisions for your career. Physicians have not been taught to interview well. The good news is, it’s not that hard.” TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Your physical appearance—the image and demeanor you present in your work environment—plays an important role in your career. If you aspire to a leadership position or are looking for a new job, be sure to examine your outward style as carefully as you craft your curriculum vitae.
“This is a huge, woefully unexplored way that physicians relate to the world,” says Mary Frances Lyons, MD, an executive search consultant with Witt/Kiefer in St. Louis. “Let’s call it body language. It’s the attitude or deportment you show. If you’re not the most corporate person in the world, you can still appear to be open, enthusiastic about your work, and have integrity.”
Kindergarten Revisited
Dr. Lyons frequently coaches physician executives before job interviews. She instructs many of them in the basics: standing up straight, making eye contact, smiling, and having a firm handshake. “This is literally your chance to connect with other people,” she says. “Send a signal that you want to connect, that you’re open, and you’ll bring that out in them as well.”
Her advice may seem simplistic, and she agrees. “You can literally learn this stuff in kindergarten—but many physicians don’t do it,” she says. “Their currency of credibility is how smart they are, and they rely on that. The truth is that no one in medical school ever teaches physicians that a large part of their medical success is how they interact with and relate to others—including patients, their boss, payers, and colleagues.” As a clinician, you can get by with minimal social skills or attention to your demeanor, but Dr. Lyons warns, “If you want to move up the food chain, this is professionally important.”
Typically, hospitalists are insulated from the traditional office dress code (i.e., suits and ties and heels), but doctors are not immune to the basic standards of workplace appearance. “For better or for worse, hospital medicine groups are not corporate,” Dr. Lyons points out. “The question is, how do you become corporate enough to get the job offer or the promotion?”
Look the Part
If you want a higher-level position, whether you’re aiming for a promotion, interviewing for an important committee position, or seeking a new job, consider the impression you make before you open your mouth.
“Your style and attitude is more important than how you dress,” Dr. Lyons says. “However, appearance-wise, you want to look professional and serious … not somber. Be appropriate and nondescript; you don’t want interesting clothes or clothes that make a statement. You want people to think, ‘What a professional person,’ not ‘Wow, I really love those earrings.’ ”
When you have an important interview or meeting, wear a dark business suit. Pantsuits are fine for women, Dr. Lyons says. “You can never, ever go wrong with a suit,” she says. “You don’t want the people interviewing you to be better dressed than you. Your appearance signals how you’ll present yourself to patients.”
Ultimately, a physician’s behavior and professional interactions are significant considerations in the hiring process, says Kenneth Simone, DO, owner of Hospitalist and Practice Solutions in Veazie, Maine, and author of the upcoming book “Hospitalist Recruitment and Retention: Building a Hospital Medicine Program.” “It will affect relationships with all stakeholders in the healthcare system. Furthermore, if the hospitalist’s professional relationship with the nursing staff and other hospital staff disintegrates, it can affect patient care.”
Listen Up
During a job interview, promotional interview, or committee chair interview, the balance between how much you say and when you stop talking can reveal much about your attitude. Hiring managers look for leaders who can listen as well as they direct. “Doctors have no idea how to listen,” Dr. Lyons says. “I sometimes recommend that a client limit himself or herself to three sentences to answer a question.” Dr. Simone agrees. “A job candidate should discuss their professional and personal interests when queried but should refrain from dominating the discussion. It should be an interactive exchange,” he says.
Dr. Lyons recommends preparing for an interview by putting together a three- to five-minute presentation about who you are as a professional. Your interviewers will already have your resume, so avoid recounting what they already know. “If you’re having trouble with these things, put on your interview suit, then videotape yourself giving your presentation,” Dr. Lyons says. “Watch it and ask yourself, ‘Would I hire this person?’ It’s a grim exercise, but it’s effective.”
Consider your demeanor and make changes that allow you to show off your personal strengths and your ability to connect. Simple changes—upgrades, if you will—can lift you above your competition. “If concerns arise with one candidate, the rule of thumb is to avoid taking a chance on hiring a potential problem physician,” Dr. Simone says. “Recruitment is expensive. It has been estimated that making an incorrect [hire] can cost a program up to $100,000, when you consider expenses such as headhunter fees, sign-on bonus, moving expenses, and advertising, in addition to lost revenues for the program while staff participate in the recruitment process and lost productivity when the program is down one provider.”
A good attitude, openness to others, and a professional demeanor can bolster your career path. As Dr. Lyons points out, “If you don’t interview well, other people will make all the major decisions for your career. Physicians have not been taught to interview well. The good news is, it’s not that hard.” TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
C. Difficile Infection: Are We Doing Enough?
The worst of the nationwide Clostri-dium difficile epidemic is yet to come. The current, highly virulent NAP1/027 strain has reached all 50 states and Canada, with a total burden estimated at more than 500,000 annual cases.1
The economic burden associated with managing C. difficile-associated disease (CDAD) in Massachusetts hospitals over a two-year period was estimated at $51.2 million and associated with 55,380 inpatient days.2 A retrospective review (n=3,692) identified a mean cost per stay for a first hospitalization with a primary CDAD diagnosis at $10,212. This was associated with a mean length of stay (LOS) of 6.4 days. For patients with a secondary CDAD diagnosis, the LOS was estimated at 15.7 days, most likely due to time spent in the intensive-care unit (ICU) and not likely related to CDAD management. The CDAD-related increased LOS in these patients was estimated to be an additional 2.95 days, with an additional cost of $13,675.
More recently, CDAD-associated costs were noted to be more than $7,000 per case, according to data from 439 cases evaluated by two statistical methods.3
Bacillus Background
C. difficile is a spore-forming, gram-positive, anaerobic bacillus that has become one of the most significant causes of hospitalization-associated diarrhea in adults.4 The number of infections occurring with the more virulent strain is disquieting. It is associated with a spectrum of illnesses, which include uncomplicated diarrhea presenting as mild, watery stools, life-threatening pseudomembranous colitis, and toxic megacolon, leading to sepsis and death.
CDAD might be an unrecognized and under-reported cause of death in the U.S.5 From 1999 to 2004, CDAD was reported as a cause of death for 24,642 people and an underlying cause of death for an additional 12,264 people.6 The median patient age was 82.
As an aside, CDAD is the older terminology for what is now being referred to as C. difficile infection (CDI).
CDI is predominantly seen as a nosocomial or long-term-care facility concern, although community-acquired infections have been reported.7 Risk factors include previous antimicrobial use, particularly with clindamycin, fluoroquinolones, cephalosporins, ampicillin, or ß-lactams. Other risk factors include use of immunosuppressants or chemotherapeutic agents, advanced age, surgery, exposure to gastric acid suppressants, host immunity, and serious underlying illnesses or comorbidities.8,9 Gastric acid suppressant use outside a healthcare facility might be a significant risk factor for outpatient CDI.
Prevention
Healthcare-facility-based CDI prevention strategies include discontinuing any suspected antibiotic, as this alone has been known to resolve CDI in up to 25% of patients. C. difficile spores are resistant to bactericidal effects of alcohol and most hospital disinfectants. Therefore, additional prevention measures should include:
- Meticulous and proper hand hygiene for healthcare workers, patients, and visitors;
- Utilizing soap and water and avoiding alcohol-based rubs that are not sporicidal;
- Environmental cleaning with sporicidal cleaning agents;
- Placing patients under contact isolation infection control procedures until resolution of the diarrhea; and
- Adopting antibiotic restriction policies to limit excessive antimicrobial use.
Two additional principles include not giving prophylactic antimicrobials for patients at high risk of developing CDI and not treating or attempting to decolonize asymptomatic C. difficile carriers. The Centers for Disease Control recently developed a patient-safety initiative to assist healthcare facilities in dealing with multidrug-resistant organisms (MDRO) and CDAD.10
Management
General management strategies for CDI patients include:
- Discontinuing all unnecessary antimicrobials or utilizing lower-risk agents when able;
- Monitoring volume status and electrolytes and appropriately replete when necessary;
- Avoiding anti-diarrheal agents, such as loperamide, atropine, or diphenoxylate, as these agents do not allow the toxin to be excreted and can worsen symptoms and lead to serious complications;
- Encouraging patient hand hygiene through use of soap and water;
- Possibly avoiding the use of lactose-containing foods;
- Possibly discontinuing proton pump inhibitors and other acid suppressants; and
- Administering specific anti-Clostridial antibiotics, if necessary, based on infection severity.
Severe CDI causes volume depletion, electrolyte imbalances, and hypotension, as well as renal impairment, hemodynamic instability, leukocytosis, toxic megacolon, and death. Severe diarrhea associated with this form of CDI might include 10 or more loose stools per day. A surgical consultation should be obtained for a complete evaluation in the most severe cases, as patients may require colectomy.
Recent reports suggest oral (OP) vancomycin be considered as first-line therapy for severe CDI. Intravenous (IV) vancomycin should not be used, because it does not reach high enough stool levels to treat the infection. Vancomycin should be dosed at 500 mg four times daily for 10 to 14 days (severe CDI) and 125 mg four times daily for 10 to 14 days in cases of mild to moderate CDI; alternatively, the duration of treatment can be extended for several days after the diarrhea resolves. This usually occurs within a few days after commencing treatment.
The treatment of choice for mild to moderate CDI is metronidazole. It is dosed at either 500 mg PO three times daily or 250 mg PO four times daily. Oral metronidazole achieves higher stool concentrations than IV metronidazole, so it is the preferred route for CDI management.
Metronidazole can cause nausea and a metallic taste. It also interacts with warfarin, so the international normalized ratio (INR) must be followed. Concomitant administration of alcohol can lead to a reaction similar to that associated with use of Antabuse. The drug should not be used in pregnant women or children. Metronidazole and vancomycin usually are equally effective for treating mild to moderate CDI, but some resistance has been noted. Vancomycin PO currently is available only as a branded drug with a high cost, but this may soon change.11
Recurrence
Recurrence can occur in approximately 20% of patients within 60 days, and these patients can be treated with the same antibiotics as were previously utilized. Subsequent recurrences can be managed with pulse dosing, or by tapering the dose at the end of therapy. Due to a lack of controlled studies, the use of probiotics, such as Lactobacillus, in the prevention of CDI cannot be routinely recommended.12 However, Lactobacillus-containing products generally are considered safe in immunocompetent individuals.
The Future
Generic oral vancomycin is on the horizon and a number of agents are currently undergoing phase 3 clinical trials for CDI management. These include rifaximin, nitazoxanide, and rifampin in combination with current agents.13-16 For now, prevention is key. Utilize some of the measures noted above to prevent this potentially serious, nosocomial infection. For infected patients, current treatments are effective and new ones will be here soon. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1.Walker EP. ICAAC-IDSA: C. difficile epidemic continues to worsen. MedPage Web site. Available at: www.medpagetoday.com/MeetingCoverage/ ICAAC/11518. Accessed Jan. 13, 2009.
2.O’Brien JA, Lahue BJ, Caro JJ, Davidson DM. The emerging infectious challenge of Clostridium difficile-associated disease in Massachusetts hospitals: clinical and economic consequences. Infect Control Hosp Epidemiol. 2007;28:1219-1227.
3.Dubberke ER, Reske RA, Olsen MA, McDonald C, Fraser VJ. Short- and long-term attributable costs of Clostridium difficile-associated disease in nonsurgical patients. Clin Infect Dis. 2008;46:497-504.
4.Jodlowski TZ, Oehler R, Kam LW, Melnychuk I. Emerging therapies in the treatment of Clostridium difficile-associated disease. Ann Pharmacother. 2006;40:2164-2169.
5.Redelings MD, Sorvillo F, Mascola L. Increase in Clostridium difficile-related mortality rates, United States, 1999-2004. Emerg Infect Dis. 2007;13:1417-1419.
6.The national healthcare safety network protocol multi-drug-resistant organism and Clostridium difficile-associated disease module version 4.1. CDC Web site. Available at: www.cdc.gov/ncidod/dhqp/ pdf/nhsn/MDRO_CDADprotocolv41Dec08final.pdf. Accessed Jan. 14, 2009.
7.Severe Clostridium difficile-associated disease in populations previously at low risk—four states, 2005. CDC Web site. Available at www.cdc.gov/mmwr/preview/mmwrhtml/mm5447a1.htm. Accessed Jan. 14, 2009.
8.Lawrence SJ. Contemporary management of Clostridium difficile-associated disease. IDSE Web site. Available at: www.idse.net/download/079idse0907WM.pdf. Accessed Jan. 14, 2009.
9.Dubberke ER, Gerding DN, Classen D, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29:S81-S92.
10.Multidrug-resistant organisms (MDRO) and Clostridium difficile-associated disease (CDAD) module. CDC Web site. Available at: www.cdc.gov/ncidod/dhqp/nhsn_MDRO_CDAD.html. Accessed Jan. 14, 2009.
11.ViroPharma files FOIA complaint seeking administrative record for vancocin. ViroPharma Inc. Web site. Available at: phx.corporateir.net/phoenix.zhtml?c=92320&p=irol-newsArticle&ID=1237649. Published Dec. 18, 2008. Accessed Jan. 14, 2009.
12.Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ. 2007;6. Available at: www.bmj.com/cgi/reprint/bmj.39231.599815.55v1. Accessed Jan. 14, 2009.
13. A trial to compare xifaxan to vancomycin for the treatment of Clostridium difficile-associated diarrhea (CDAD). National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/ NCT00269399?term=rifaximin+and+clostridium&rank=1. Accessed Jan. 10, 2009.
14. Efficacy of metronidazole versus metronidazole and rifampin in CDAD treatment. National Institutes of Health Web site. Available at www.clinicaltrials.gov/ct2/show/NCT00182429?term=rifampin+and+cdad&rank=1. Accessed Jan. 10, 2009.
15. Compassionate use of nitazoxanide for the treatment of Clostridium difficile infection. National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/NCT00304356?term=Nitazoxanide+and+clostridium&rank=2. Accessed Jan. 10, 2009.
16. Vancomycin vs. nitazoxanide to treat recurrent C. difficile colitis. National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/NCT00304889?term=Nitazoxanide+and+vancomycin&rank=2. Accessed Jan. 10, 2009.
The worst of the nationwide Clostri-dium difficile epidemic is yet to come. The current, highly virulent NAP1/027 strain has reached all 50 states and Canada, with a total burden estimated at more than 500,000 annual cases.1
The economic burden associated with managing C. difficile-associated disease (CDAD) in Massachusetts hospitals over a two-year period was estimated at $51.2 million and associated with 55,380 inpatient days.2 A retrospective review (n=3,692) identified a mean cost per stay for a first hospitalization with a primary CDAD diagnosis at $10,212. This was associated with a mean length of stay (LOS) of 6.4 days. For patients with a secondary CDAD diagnosis, the LOS was estimated at 15.7 days, most likely due to time spent in the intensive-care unit (ICU) and not likely related to CDAD management. The CDAD-related increased LOS in these patients was estimated to be an additional 2.95 days, with an additional cost of $13,675.
More recently, CDAD-associated costs were noted to be more than $7,000 per case, according to data from 439 cases evaluated by two statistical methods.3
Bacillus Background
C. difficile is a spore-forming, gram-positive, anaerobic bacillus that has become one of the most significant causes of hospitalization-associated diarrhea in adults.4 The number of infections occurring with the more virulent strain is disquieting. It is associated with a spectrum of illnesses, which include uncomplicated diarrhea presenting as mild, watery stools, life-threatening pseudomembranous colitis, and toxic megacolon, leading to sepsis and death.
CDAD might be an unrecognized and under-reported cause of death in the U.S.5 From 1999 to 2004, CDAD was reported as a cause of death for 24,642 people and an underlying cause of death for an additional 12,264 people.6 The median patient age was 82.
As an aside, CDAD is the older terminology for what is now being referred to as C. difficile infection (CDI).
CDI is predominantly seen as a nosocomial or long-term-care facility concern, although community-acquired infections have been reported.7 Risk factors include previous antimicrobial use, particularly with clindamycin, fluoroquinolones, cephalosporins, ampicillin, or ß-lactams. Other risk factors include use of immunosuppressants or chemotherapeutic agents, advanced age, surgery, exposure to gastric acid suppressants, host immunity, and serious underlying illnesses or comorbidities.8,9 Gastric acid suppressant use outside a healthcare facility might be a significant risk factor for outpatient CDI.
Prevention
Healthcare-facility-based CDI prevention strategies include discontinuing any suspected antibiotic, as this alone has been known to resolve CDI in up to 25% of patients. C. difficile spores are resistant to bactericidal effects of alcohol and most hospital disinfectants. Therefore, additional prevention measures should include:
- Meticulous and proper hand hygiene for healthcare workers, patients, and visitors;
- Utilizing soap and water and avoiding alcohol-based rubs that are not sporicidal;
- Environmental cleaning with sporicidal cleaning agents;
- Placing patients under contact isolation infection control procedures until resolution of the diarrhea; and
- Adopting antibiotic restriction policies to limit excessive antimicrobial use.
Two additional principles include not giving prophylactic antimicrobials for patients at high risk of developing CDI and not treating or attempting to decolonize asymptomatic C. difficile carriers. The Centers for Disease Control recently developed a patient-safety initiative to assist healthcare facilities in dealing with multidrug-resistant organisms (MDRO) and CDAD.10
Management
General management strategies for CDI patients include:
- Discontinuing all unnecessary antimicrobials or utilizing lower-risk agents when able;
- Monitoring volume status and electrolytes and appropriately replete when necessary;
- Avoiding anti-diarrheal agents, such as loperamide, atropine, or diphenoxylate, as these agents do not allow the toxin to be excreted and can worsen symptoms and lead to serious complications;
- Encouraging patient hand hygiene through use of soap and water;
- Possibly avoiding the use of lactose-containing foods;
- Possibly discontinuing proton pump inhibitors and other acid suppressants; and
- Administering specific anti-Clostridial antibiotics, if necessary, based on infection severity.
Severe CDI causes volume depletion, electrolyte imbalances, and hypotension, as well as renal impairment, hemodynamic instability, leukocytosis, toxic megacolon, and death. Severe diarrhea associated with this form of CDI might include 10 or more loose stools per day. A surgical consultation should be obtained for a complete evaluation in the most severe cases, as patients may require colectomy.
Recent reports suggest oral (OP) vancomycin be considered as first-line therapy for severe CDI. Intravenous (IV) vancomycin should not be used, because it does not reach high enough stool levels to treat the infection. Vancomycin should be dosed at 500 mg four times daily for 10 to 14 days (severe CDI) and 125 mg four times daily for 10 to 14 days in cases of mild to moderate CDI; alternatively, the duration of treatment can be extended for several days after the diarrhea resolves. This usually occurs within a few days after commencing treatment.
The treatment of choice for mild to moderate CDI is metronidazole. It is dosed at either 500 mg PO three times daily or 250 mg PO four times daily. Oral metronidazole achieves higher stool concentrations than IV metronidazole, so it is the preferred route for CDI management.
Metronidazole can cause nausea and a metallic taste. It also interacts with warfarin, so the international normalized ratio (INR) must be followed. Concomitant administration of alcohol can lead to a reaction similar to that associated with use of Antabuse. The drug should not be used in pregnant women or children. Metronidazole and vancomycin usually are equally effective for treating mild to moderate CDI, but some resistance has been noted. Vancomycin PO currently is available only as a branded drug with a high cost, but this may soon change.11
Recurrence
Recurrence can occur in approximately 20% of patients within 60 days, and these patients can be treated with the same antibiotics as were previously utilized. Subsequent recurrences can be managed with pulse dosing, or by tapering the dose at the end of therapy. Due to a lack of controlled studies, the use of probiotics, such as Lactobacillus, in the prevention of CDI cannot be routinely recommended.12 However, Lactobacillus-containing products generally are considered safe in immunocompetent individuals.
The Future
Generic oral vancomycin is on the horizon and a number of agents are currently undergoing phase 3 clinical trials for CDI management. These include rifaximin, nitazoxanide, and rifampin in combination with current agents.13-16 For now, prevention is key. Utilize some of the measures noted above to prevent this potentially serious, nosocomial infection. For infected patients, current treatments are effective and new ones will be here soon. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1.Walker EP. ICAAC-IDSA: C. difficile epidemic continues to worsen. MedPage Web site. Available at: www.medpagetoday.com/MeetingCoverage/ ICAAC/11518. Accessed Jan. 13, 2009.
2.O’Brien JA, Lahue BJ, Caro JJ, Davidson DM. The emerging infectious challenge of Clostridium difficile-associated disease in Massachusetts hospitals: clinical and economic consequences. Infect Control Hosp Epidemiol. 2007;28:1219-1227.
3.Dubberke ER, Reske RA, Olsen MA, McDonald C, Fraser VJ. Short- and long-term attributable costs of Clostridium difficile-associated disease in nonsurgical patients. Clin Infect Dis. 2008;46:497-504.
4.Jodlowski TZ, Oehler R, Kam LW, Melnychuk I. Emerging therapies in the treatment of Clostridium difficile-associated disease. Ann Pharmacother. 2006;40:2164-2169.
5.Redelings MD, Sorvillo F, Mascola L. Increase in Clostridium difficile-related mortality rates, United States, 1999-2004. Emerg Infect Dis. 2007;13:1417-1419.
6.The national healthcare safety network protocol multi-drug-resistant organism and Clostridium difficile-associated disease module version 4.1. CDC Web site. Available at: www.cdc.gov/ncidod/dhqp/ pdf/nhsn/MDRO_CDADprotocolv41Dec08final.pdf. Accessed Jan. 14, 2009.
7.Severe Clostridium difficile-associated disease in populations previously at low risk—four states, 2005. CDC Web site. Available at www.cdc.gov/mmwr/preview/mmwrhtml/mm5447a1.htm. Accessed Jan. 14, 2009.
8.Lawrence SJ. Contemporary management of Clostridium difficile-associated disease. IDSE Web site. Available at: www.idse.net/download/079idse0907WM.pdf. Accessed Jan. 14, 2009.
9.Dubberke ER, Gerding DN, Classen D, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29:S81-S92.
10.Multidrug-resistant organisms (MDRO) and Clostridium difficile-associated disease (CDAD) module. CDC Web site. Available at: www.cdc.gov/ncidod/dhqp/nhsn_MDRO_CDAD.html. Accessed Jan. 14, 2009.
11.ViroPharma files FOIA complaint seeking administrative record for vancocin. ViroPharma Inc. Web site. Available at: phx.corporateir.net/phoenix.zhtml?c=92320&p=irol-newsArticle&ID=1237649. Published Dec. 18, 2008. Accessed Jan. 14, 2009.
12.Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ. 2007;6. Available at: www.bmj.com/cgi/reprint/bmj.39231.599815.55v1. Accessed Jan. 14, 2009.
13. A trial to compare xifaxan to vancomycin for the treatment of Clostridium difficile-associated diarrhea (CDAD). National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/ NCT00269399?term=rifaximin+and+clostridium&rank=1. Accessed Jan. 10, 2009.
14. Efficacy of metronidazole versus metronidazole and rifampin in CDAD treatment. National Institutes of Health Web site. Available at www.clinicaltrials.gov/ct2/show/NCT00182429?term=rifampin+and+cdad&rank=1. Accessed Jan. 10, 2009.
15. Compassionate use of nitazoxanide for the treatment of Clostridium difficile infection. National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/NCT00304356?term=Nitazoxanide+and+clostridium&rank=2. Accessed Jan. 10, 2009.
16. Vancomycin vs. nitazoxanide to treat recurrent C. difficile colitis. National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/NCT00304889?term=Nitazoxanide+and+vancomycin&rank=2. Accessed Jan. 10, 2009.
The worst of the nationwide Clostri-dium difficile epidemic is yet to come. The current, highly virulent NAP1/027 strain has reached all 50 states and Canada, with a total burden estimated at more than 500,000 annual cases.1
The economic burden associated with managing C. difficile-associated disease (CDAD) in Massachusetts hospitals over a two-year period was estimated at $51.2 million and associated with 55,380 inpatient days.2 A retrospective review (n=3,692) identified a mean cost per stay for a first hospitalization with a primary CDAD diagnosis at $10,212. This was associated with a mean length of stay (LOS) of 6.4 days. For patients with a secondary CDAD diagnosis, the LOS was estimated at 15.7 days, most likely due to time spent in the intensive-care unit (ICU) and not likely related to CDAD management. The CDAD-related increased LOS in these patients was estimated to be an additional 2.95 days, with an additional cost of $13,675.
More recently, CDAD-associated costs were noted to be more than $7,000 per case, according to data from 439 cases evaluated by two statistical methods.3
Bacillus Background
C. difficile is a spore-forming, gram-positive, anaerobic bacillus that has become one of the most significant causes of hospitalization-associated diarrhea in adults.4 The number of infections occurring with the more virulent strain is disquieting. It is associated with a spectrum of illnesses, which include uncomplicated diarrhea presenting as mild, watery stools, life-threatening pseudomembranous colitis, and toxic megacolon, leading to sepsis and death.
CDAD might be an unrecognized and under-reported cause of death in the U.S.5 From 1999 to 2004, CDAD was reported as a cause of death for 24,642 people and an underlying cause of death for an additional 12,264 people.6 The median patient age was 82.
As an aside, CDAD is the older terminology for what is now being referred to as C. difficile infection (CDI).
CDI is predominantly seen as a nosocomial or long-term-care facility concern, although community-acquired infections have been reported.7 Risk factors include previous antimicrobial use, particularly with clindamycin, fluoroquinolones, cephalosporins, ampicillin, or ß-lactams. Other risk factors include use of immunosuppressants or chemotherapeutic agents, advanced age, surgery, exposure to gastric acid suppressants, host immunity, and serious underlying illnesses or comorbidities.8,9 Gastric acid suppressant use outside a healthcare facility might be a significant risk factor for outpatient CDI.
Prevention
Healthcare-facility-based CDI prevention strategies include discontinuing any suspected antibiotic, as this alone has been known to resolve CDI in up to 25% of patients. C. difficile spores are resistant to bactericidal effects of alcohol and most hospital disinfectants. Therefore, additional prevention measures should include:
- Meticulous and proper hand hygiene for healthcare workers, patients, and visitors;
- Utilizing soap and water and avoiding alcohol-based rubs that are not sporicidal;
- Environmental cleaning with sporicidal cleaning agents;
- Placing patients under contact isolation infection control procedures until resolution of the diarrhea; and
- Adopting antibiotic restriction policies to limit excessive antimicrobial use.
Two additional principles include not giving prophylactic antimicrobials for patients at high risk of developing CDI and not treating or attempting to decolonize asymptomatic C. difficile carriers. The Centers for Disease Control recently developed a patient-safety initiative to assist healthcare facilities in dealing with multidrug-resistant organisms (MDRO) and CDAD.10
Management
General management strategies for CDI patients include:
- Discontinuing all unnecessary antimicrobials or utilizing lower-risk agents when able;
- Monitoring volume status and electrolytes and appropriately replete when necessary;
- Avoiding anti-diarrheal agents, such as loperamide, atropine, or diphenoxylate, as these agents do not allow the toxin to be excreted and can worsen symptoms and lead to serious complications;
- Encouraging patient hand hygiene through use of soap and water;
- Possibly avoiding the use of lactose-containing foods;
- Possibly discontinuing proton pump inhibitors and other acid suppressants; and
- Administering specific anti-Clostridial antibiotics, if necessary, based on infection severity.
Severe CDI causes volume depletion, electrolyte imbalances, and hypotension, as well as renal impairment, hemodynamic instability, leukocytosis, toxic megacolon, and death. Severe diarrhea associated with this form of CDI might include 10 or more loose stools per day. A surgical consultation should be obtained for a complete evaluation in the most severe cases, as patients may require colectomy.
Recent reports suggest oral (OP) vancomycin be considered as first-line therapy for severe CDI. Intravenous (IV) vancomycin should not be used, because it does not reach high enough stool levels to treat the infection. Vancomycin should be dosed at 500 mg four times daily for 10 to 14 days (severe CDI) and 125 mg four times daily for 10 to 14 days in cases of mild to moderate CDI; alternatively, the duration of treatment can be extended for several days after the diarrhea resolves. This usually occurs within a few days after commencing treatment.
The treatment of choice for mild to moderate CDI is metronidazole. It is dosed at either 500 mg PO three times daily or 250 mg PO four times daily. Oral metronidazole achieves higher stool concentrations than IV metronidazole, so it is the preferred route for CDI management.
Metronidazole can cause nausea and a metallic taste. It also interacts with warfarin, so the international normalized ratio (INR) must be followed. Concomitant administration of alcohol can lead to a reaction similar to that associated with use of Antabuse. The drug should not be used in pregnant women or children. Metronidazole and vancomycin usually are equally effective for treating mild to moderate CDI, but some resistance has been noted. Vancomycin PO currently is available only as a branded drug with a high cost, but this may soon change.11
Recurrence
Recurrence can occur in approximately 20% of patients within 60 days, and these patients can be treated with the same antibiotics as were previously utilized. Subsequent recurrences can be managed with pulse dosing, or by tapering the dose at the end of therapy. Due to a lack of controlled studies, the use of probiotics, such as Lactobacillus, in the prevention of CDI cannot be routinely recommended.12 However, Lactobacillus-containing products generally are considered safe in immunocompetent individuals.
The Future
Generic oral vancomycin is on the horizon and a number of agents are currently undergoing phase 3 clinical trials for CDI management. These include rifaximin, nitazoxanide, and rifampin in combination with current agents.13-16 For now, prevention is key. Utilize some of the measures noted above to prevent this potentially serious, nosocomial infection. For infected patients, current treatments are effective and new ones will be here soon. TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1.Walker EP. ICAAC-IDSA: C. difficile epidemic continues to worsen. MedPage Web site. Available at: www.medpagetoday.com/MeetingCoverage/ ICAAC/11518. Accessed Jan. 13, 2009.
2.O’Brien JA, Lahue BJ, Caro JJ, Davidson DM. The emerging infectious challenge of Clostridium difficile-associated disease in Massachusetts hospitals: clinical and economic consequences. Infect Control Hosp Epidemiol. 2007;28:1219-1227.
3.Dubberke ER, Reske RA, Olsen MA, McDonald C, Fraser VJ. Short- and long-term attributable costs of Clostridium difficile-associated disease in nonsurgical patients. Clin Infect Dis. 2008;46:497-504.
4.Jodlowski TZ, Oehler R, Kam LW, Melnychuk I. Emerging therapies in the treatment of Clostridium difficile-associated disease. Ann Pharmacother. 2006;40:2164-2169.
5.Redelings MD, Sorvillo F, Mascola L. Increase in Clostridium difficile-related mortality rates, United States, 1999-2004. Emerg Infect Dis. 2007;13:1417-1419.
6.The national healthcare safety network protocol multi-drug-resistant organism and Clostridium difficile-associated disease module version 4.1. CDC Web site. Available at: www.cdc.gov/ncidod/dhqp/ pdf/nhsn/MDRO_CDADprotocolv41Dec08final.pdf. Accessed Jan. 14, 2009.
7.Severe Clostridium difficile-associated disease in populations previously at low risk—four states, 2005. CDC Web site. Available at www.cdc.gov/mmwr/preview/mmwrhtml/mm5447a1.htm. Accessed Jan. 14, 2009.
8.Lawrence SJ. Contemporary management of Clostridium difficile-associated disease. IDSE Web site. Available at: www.idse.net/download/079idse0907WM.pdf. Accessed Jan. 14, 2009.
9.Dubberke ER, Gerding DN, Classen D, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29:S81-S92.
10.Multidrug-resistant organisms (MDRO) and Clostridium difficile-associated disease (CDAD) module. CDC Web site. Available at: www.cdc.gov/ncidod/dhqp/nhsn_MDRO_CDAD.html. Accessed Jan. 14, 2009.
11.ViroPharma files FOIA complaint seeking administrative record for vancocin. ViroPharma Inc. Web site. Available at: phx.corporateir.net/phoenix.zhtml?c=92320&p=irol-newsArticle&ID=1237649. Published Dec. 18, 2008. Accessed Jan. 14, 2009.
12.Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ. 2007;6. Available at: www.bmj.com/cgi/reprint/bmj.39231.599815.55v1. Accessed Jan. 14, 2009.
13. A trial to compare xifaxan to vancomycin for the treatment of Clostridium difficile-associated diarrhea (CDAD). National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/ NCT00269399?term=rifaximin+and+clostridium&rank=1. Accessed Jan. 10, 2009.
14. Efficacy of metronidazole versus metronidazole and rifampin in CDAD treatment. National Institutes of Health Web site. Available at www.clinicaltrials.gov/ct2/show/NCT00182429?term=rifampin+and+cdad&rank=1. Accessed Jan. 10, 2009.
15. Compassionate use of nitazoxanide for the treatment of Clostridium difficile infection. National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/NCT00304356?term=Nitazoxanide+and+clostridium&rank=2. Accessed Jan. 10, 2009.
16. Vancomycin vs. nitazoxanide to treat recurrent C. difficile colitis. National Institutes of Health Web site. Available at: www.clinicaltrials.gov/ct2/show/NCT00304889?term=Nitazoxanide+and+vancomycin&rank=2. Accessed Jan. 10, 2009.
SHM National Conference Expands to Four Days
With the total number of hospitalists in the U.S. nearing 28,000 and hospitalists now working in four out of every five large hospitals, the issues affecting hospitalists continue to expand and become more complex.
That’s the rationale behind expanding SHM’s national conference, “Hospital Medicine 2009,” to a four-day schedule. Previous SHM annual conferences were limited to three days; HM09 runs May 14-17 in Chicago.
“Hospitalists are continually looking for opportunities for professional development, and we’re expecting another record-breaking attendance,” says Todd Von Deak, SHM’s vice president for membership and marketing. “We’re thrilled that we can offer additional courses and still give attendees plenty of time for other sessions and networking with thousands of hospitalists and colleagues. Ultimately, the expansion makes it easier for hospitalists to bring best practices back to their hospitals and patients.”
HM09 will feature keynotes from a pair of leaders in healthcare quality:
- Mark R. Chassin, MD, MPP, MPH, president of The Joint Commission and an expert on improving the safety and quality of healthcare; and
- Robert M. Wachter, MD, professor and chief of the division of hospital medicine at the University of California San Francisco, a former SHM president, and author of the blog “Wachter’s World”.
With the total number of hospitalists in the U.S. nearing 28,000 and hospitalists now working in four out of every five large hospitals, the issues affecting hospitalists continue to expand and become more complex.
That’s the rationale behind expanding SHM’s national conference, “Hospital Medicine 2009,” to a four-day schedule. Previous SHM annual conferences were limited to three days; HM09 runs May 14-17 in Chicago.
“Hospitalists are continually looking for opportunities for professional development, and we’re expecting another record-breaking attendance,” says Todd Von Deak, SHM’s vice president for membership and marketing. “We’re thrilled that we can offer additional courses and still give attendees plenty of time for other sessions and networking with thousands of hospitalists and colleagues. Ultimately, the expansion makes it easier for hospitalists to bring best practices back to their hospitals and patients.”
HM09 will feature keynotes from a pair of leaders in healthcare quality:
- Mark R. Chassin, MD, MPP, MPH, president of The Joint Commission and an expert on improving the safety and quality of healthcare; and
- Robert M. Wachter, MD, professor and chief of the division of hospital medicine at the University of California San Francisco, a former SHM president, and author of the blog “Wachter’s World”.
With the total number of hospitalists in the U.S. nearing 28,000 and hospitalists now working in four out of every five large hospitals, the issues affecting hospitalists continue to expand and become more complex.
That’s the rationale behind expanding SHM’s national conference, “Hospital Medicine 2009,” to a four-day schedule. Previous SHM annual conferences were limited to three days; HM09 runs May 14-17 in Chicago.
“Hospitalists are continually looking for opportunities for professional development, and we’re expecting another record-breaking attendance,” says Todd Von Deak, SHM’s vice president for membership and marketing. “We’re thrilled that we can offer additional courses and still give attendees plenty of time for other sessions and networking with thousands of hospitalists and colleagues. Ultimately, the expansion makes it easier for hospitalists to bring best practices back to their hospitals and patients.”
HM09 will feature keynotes from a pair of leaders in healthcare quality:
- Mark R. Chassin, MD, MPP, MPH, president of The Joint Commission and an expert on improving the safety and quality of healthcare; and
- Robert M. Wachter, MD, professor and chief of the division of hospital medicine at the University of California San Francisco, a former SHM president, and author of the blog “Wachter’s World”.
VTE Awareness Month
Jason Stein, MD, knows he could walk into almost any nursing unit in any hospital in the country, ask a simple question, and get blank stares in return.
“I would ask, ‘Which patients here in the nursing unit don’t have an order for VTE prophylaxis?’ ” says Dr. Stein, associate director for quality improvement and assistant professor of medicine at Emory University School of Medicine in Atlanta. “And they would tell me, ‘What kind of place do you think this is? How can we possibly know that?’ ”
It’s not idle chat. Venous thromboembolism (VTE) is a condition known throughout HM for three things: It runs rampant in hospitals; it can be deadly; and it’s easily preventable.
This month, SHM—along with dozens of other healthcare organizations, including the Agency for Healthcare Research Quality (AHRQ)—is highlighting the dangers of VTE and deep vein thrombosis (DVT), and promoting best practices to prevent them.
“SHM’s leadership of awareness efforts and championing VTE [prevention] has played an important role in keeping this on everybody’s mind,” Dr. Stein says.
VTE: A Hospital-Based Epidemic
Although it is easy to target at-risk populations and prevent it, VTE is widespread and dangerous.
“By published estimates, each year VTE kills more people than HIV, car accidents, and breast cancer combined,” says Gregory A. Maynard, MD, Ms, chief of the division of hospital medicine and clinical professor of medicine at the University of California at San Diego.
The risk of VTE in hospital patients should give hospitalists and their colleagues pause. Here’s why:
- According to the American Heart Association, more than 200,000 cases of VTE are reported each year, and VTE occurs for the first time in approximately 100 out of every 100,000 persons each year;
- Research published last year in The Lancet estimates 52% of hospitalized patients are at risk for VTE;
- 1 in 3 VTE patients experiences a pulmonary embolism;
- 30% of new VTE patients die within three days;
- 20% of new VTE patients die suddenly from pulmonary embolus; and
- DVT is responsible for approximately 8,000 hospital discharges every year. Pulmonary embolism accounts for nearly 100,000.
Risk Factors and Prevention
In a hospital setting, VTE risk factors are especially straightforward to monitor and prevent, but Dr. Maynard sees room for improvement.
“We don’t need to do better things; we need to do things better,” he told colleagues at a recent grand rounds. “Pharmacologic prophylaxis is the preferred way to prevent VTE in the hospital, which can reduce DVT and pulmonary embolism by 50% to 65%.”
Most hospital patients have at least one of these VTE risk factors, which are sorted into three categories:
- Stasis: conditions such as advanced age, immobility, paralysis, or stroke;
- Hypercoaguability: smoking, pregnancy, cancer, or sepsis; and
- Endothelial damage: surgery, prior VTE, central lines, or trauma.
Because the potential VTE risk is so high in hospital patients, the assessment must go hand in hand with prophylaxis, says Dr. Maynard and other hospitalists working with VTE.
Recent research has shown that prescribing medications to prevent VTE before it begins is safe, effective, and cost-effective.
The Hospitalist’s Role
The responsibility for VTE risk assessment and prevention often falls to hospitalists. In its online VTE Resource Room, SHM provides information for hospitalists working to assess and prevent VTE in their patients. It also provides a complete toolkit for hospitalists interested in addressing VTE prevention systematically throughout their hospitals. The toolkit is part of a comprehensive VTE Prevention Collaborative, which provides real-world mentoring and materials to hospitalists as they develop VTE monitoring and prevention programs.
“In 2005, when SHM set up the Quality Improvement resource room, we began with VTE prophylaxis,” Dr. Stein says. “VTE is the No. 1 cause of preventable death in hospitals, and preventing it is a fundamentally simple thing for hospitalists to do. We’re trying to get physicians to order a shot in the abdomen once a day. … If we can’t do that, we’re in trouble. On the flipside, if we can figure that out, we can derive mechanisms that we can apply to more complex problems in care.”
Together with SHM, Drs. Stein and Maynard have pioneered a two-pronged approach known as “measure-vention.” The underlying principal of measure-vention is that monitoring for VTE risk in real time can empower hospital staff to remedy issues in real time. In most hospitals, VTE risk can only be measured retrospectively through quality improvement data, which can take months to collect.
SHM and Dr. Stein have implemented an information technology approach at five of Emory’s hospitals. Each facility assesses patients who don’t have VTE prophylaxis every hour. The data is distributed to nursing stations, where nurses and other providers can apply VTE interventions within minutes. The program has driven Emory’s VTE prophylaxis rates to more than 90%, and Dr. Stein is working to make the program exportable to other hospitals, with the help of funding and assistance from SHM.
“As the leader of the VTE prevention program at Emory hospitals, I hear lots of stories about preventable VTE—not just about patients, but from friends of friends and family members,” he says. “It’s extraordinary.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Jason Stein, MD, knows he could walk into almost any nursing unit in any hospital in the country, ask a simple question, and get blank stares in return.
“I would ask, ‘Which patients here in the nursing unit don’t have an order for VTE prophylaxis?’ ” says Dr. Stein, associate director for quality improvement and assistant professor of medicine at Emory University School of Medicine in Atlanta. “And they would tell me, ‘What kind of place do you think this is? How can we possibly know that?’ ”
It’s not idle chat. Venous thromboembolism (VTE) is a condition known throughout HM for three things: It runs rampant in hospitals; it can be deadly; and it’s easily preventable.
This month, SHM—along with dozens of other healthcare organizations, including the Agency for Healthcare Research Quality (AHRQ)—is highlighting the dangers of VTE and deep vein thrombosis (DVT), and promoting best practices to prevent them.
“SHM’s leadership of awareness efforts and championing VTE [prevention] has played an important role in keeping this on everybody’s mind,” Dr. Stein says.
VTE: A Hospital-Based Epidemic
Although it is easy to target at-risk populations and prevent it, VTE is widespread and dangerous.
“By published estimates, each year VTE kills more people than HIV, car accidents, and breast cancer combined,” says Gregory A. Maynard, MD, Ms, chief of the division of hospital medicine and clinical professor of medicine at the University of California at San Diego.
The risk of VTE in hospital patients should give hospitalists and their colleagues pause. Here’s why:
- According to the American Heart Association, more than 200,000 cases of VTE are reported each year, and VTE occurs for the first time in approximately 100 out of every 100,000 persons each year;
- Research published last year in The Lancet estimates 52% of hospitalized patients are at risk for VTE;
- 1 in 3 VTE patients experiences a pulmonary embolism;
- 30% of new VTE patients die within three days;
- 20% of new VTE patients die suddenly from pulmonary embolus; and
- DVT is responsible for approximately 8,000 hospital discharges every year. Pulmonary embolism accounts for nearly 100,000.
Risk Factors and Prevention
In a hospital setting, VTE risk factors are especially straightforward to monitor and prevent, but Dr. Maynard sees room for improvement.
“We don’t need to do better things; we need to do things better,” he told colleagues at a recent grand rounds. “Pharmacologic prophylaxis is the preferred way to prevent VTE in the hospital, which can reduce DVT and pulmonary embolism by 50% to 65%.”
Most hospital patients have at least one of these VTE risk factors, which are sorted into three categories:
- Stasis: conditions such as advanced age, immobility, paralysis, or stroke;
- Hypercoaguability: smoking, pregnancy, cancer, or sepsis; and
- Endothelial damage: surgery, prior VTE, central lines, or trauma.
Because the potential VTE risk is so high in hospital patients, the assessment must go hand in hand with prophylaxis, says Dr. Maynard and other hospitalists working with VTE.
Recent research has shown that prescribing medications to prevent VTE before it begins is safe, effective, and cost-effective.
The Hospitalist’s Role
The responsibility for VTE risk assessment and prevention often falls to hospitalists. In its online VTE Resource Room, SHM provides information for hospitalists working to assess and prevent VTE in their patients. It also provides a complete toolkit for hospitalists interested in addressing VTE prevention systematically throughout their hospitals. The toolkit is part of a comprehensive VTE Prevention Collaborative, which provides real-world mentoring and materials to hospitalists as they develop VTE monitoring and prevention programs.
“In 2005, when SHM set up the Quality Improvement resource room, we began with VTE prophylaxis,” Dr. Stein says. “VTE is the No. 1 cause of preventable death in hospitals, and preventing it is a fundamentally simple thing for hospitalists to do. We’re trying to get physicians to order a shot in the abdomen once a day. … If we can’t do that, we’re in trouble. On the flipside, if we can figure that out, we can derive mechanisms that we can apply to more complex problems in care.”
Together with SHM, Drs. Stein and Maynard have pioneered a two-pronged approach known as “measure-vention.” The underlying principal of measure-vention is that monitoring for VTE risk in real time can empower hospital staff to remedy issues in real time. In most hospitals, VTE risk can only be measured retrospectively through quality improvement data, which can take months to collect.
SHM and Dr. Stein have implemented an information technology approach at five of Emory’s hospitals. Each facility assesses patients who don’t have VTE prophylaxis every hour. The data is distributed to nursing stations, where nurses and other providers can apply VTE interventions within minutes. The program has driven Emory’s VTE prophylaxis rates to more than 90%, and Dr. Stein is working to make the program exportable to other hospitals, with the help of funding and assistance from SHM.
“As the leader of the VTE prevention program at Emory hospitals, I hear lots of stories about preventable VTE—not just about patients, but from friends of friends and family members,” he says. “It’s extraordinary.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Jason Stein, MD, knows he could walk into almost any nursing unit in any hospital in the country, ask a simple question, and get blank stares in return.
“I would ask, ‘Which patients here in the nursing unit don’t have an order for VTE prophylaxis?’ ” says Dr. Stein, associate director for quality improvement and assistant professor of medicine at Emory University School of Medicine in Atlanta. “And they would tell me, ‘What kind of place do you think this is? How can we possibly know that?’ ”
It’s not idle chat. Venous thromboembolism (VTE) is a condition known throughout HM for three things: It runs rampant in hospitals; it can be deadly; and it’s easily preventable.
This month, SHM—along with dozens of other healthcare organizations, including the Agency for Healthcare Research Quality (AHRQ)—is highlighting the dangers of VTE and deep vein thrombosis (DVT), and promoting best practices to prevent them.
“SHM’s leadership of awareness efforts and championing VTE [prevention] has played an important role in keeping this on everybody’s mind,” Dr. Stein says.
VTE: A Hospital-Based Epidemic
Although it is easy to target at-risk populations and prevent it, VTE is widespread and dangerous.
“By published estimates, each year VTE kills more people than HIV, car accidents, and breast cancer combined,” says Gregory A. Maynard, MD, Ms, chief of the division of hospital medicine and clinical professor of medicine at the University of California at San Diego.
The risk of VTE in hospital patients should give hospitalists and their colleagues pause. Here’s why:
- According to the American Heart Association, more than 200,000 cases of VTE are reported each year, and VTE occurs for the first time in approximately 100 out of every 100,000 persons each year;
- Research published last year in The Lancet estimates 52% of hospitalized patients are at risk for VTE;
- 1 in 3 VTE patients experiences a pulmonary embolism;
- 30% of new VTE patients die within three days;
- 20% of new VTE patients die suddenly from pulmonary embolus; and
- DVT is responsible for approximately 8,000 hospital discharges every year. Pulmonary embolism accounts for nearly 100,000.
Risk Factors and Prevention
In a hospital setting, VTE risk factors are especially straightforward to monitor and prevent, but Dr. Maynard sees room for improvement.
“We don’t need to do better things; we need to do things better,” he told colleagues at a recent grand rounds. “Pharmacologic prophylaxis is the preferred way to prevent VTE in the hospital, which can reduce DVT and pulmonary embolism by 50% to 65%.”
Most hospital patients have at least one of these VTE risk factors, which are sorted into three categories:
- Stasis: conditions such as advanced age, immobility, paralysis, or stroke;
- Hypercoaguability: smoking, pregnancy, cancer, or sepsis; and
- Endothelial damage: surgery, prior VTE, central lines, or trauma.
Because the potential VTE risk is so high in hospital patients, the assessment must go hand in hand with prophylaxis, says Dr. Maynard and other hospitalists working with VTE.
Recent research has shown that prescribing medications to prevent VTE before it begins is safe, effective, and cost-effective.
The Hospitalist’s Role
The responsibility for VTE risk assessment and prevention often falls to hospitalists. In its online VTE Resource Room, SHM provides information for hospitalists working to assess and prevent VTE in their patients. It also provides a complete toolkit for hospitalists interested in addressing VTE prevention systematically throughout their hospitals. The toolkit is part of a comprehensive VTE Prevention Collaborative, which provides real-world mentoring and materials to hospitalists as they develop VTE monitoring and prevention programs.
“In 2005, when SHM set up the Quality Improvement resource room, we began with VTE prophylaxis,” Dr. Stein says. “VTE is the No. 1 cause of preventable death in hospitals, and preventing it is a fundamentally simple thing for hospitalists to do. We’re trying to get physicians to order a shot in the abdomen once a day. … If we can’t do that, we’re in trouble. On the flipside, if we can figure that out, we can derive mechanisms that we can apply to more complex problems in care.”
Together with SHM, Drs. Stein and Maynard have pioneered a two-pronged approach known as “measure-vention.” The underlying principal of measure-vention is that monitoring for VTE risk in real time can empower hospital staff to remedy issues in real time. In most hospitals, VTE risk can only be measured retrospectively through quality improvement data, which can take months to collect.
SHM and Dr. Stein have implemented an information technology approach at five of Emory’s hospitals. Each facility assesses patients who don’t have VTE prophylaxis every hour. The data is distributed to nursing stations, where nurses and other providers can apply VTE interventions within minutes. The program has driven Emory’s VTE prophylaxis rates to more than 90%, and Dr. Stein is working to make the program exportable to other hospitals, with the help of funding and assistance from SHM.
“As the leader of the VTE prevention program at Emory hospitals, I hear lots of stories about preventable VTE—not just about patients, but from friends of friends and family members,” he says. “It’s extraordinary.” TH
Brendon Shank is a freelance writer based in Philadelphia.
Politics & Publishing Pitfalls
Wouldn’t you know it? The same day the February issue of The Hospitalist was being shipped to the post office, former Sen. Tom Daschle—President Obama’s “chosen one” to spearhead healthcare reform— surprised us all. Embroiled in a tax and ethics scandal, Daschle up and withdrew his nomination for secretary of the Department of Health and Human Services (HHS). Considering our February cover story outlines Obama and Daschle’s plan for comprehensive healthcare reform—and the magazine cover has a nice picture of Obama with Daschle in the background—the timing couldn’t have been … better.
In publishing circles, it’s one of those slow-motion moments. You know, the kind of moment sitcoms rewind and show from three different angles. Do they really think we need to see Cosmo Kramer trip and fall three times? I got it.
It’s not as if we declared Thomas Dewey the next president of the United States. If nothing else, consider the February issue a collector’s item. Once I’m done writing this column, I’m going to FedEx a box of February issues to Daschle’s office. I hope he hangs one on the wall—a reminder of how close he came to history.
The fact of the matter is, I’m guessing Daschle’s departure will do little to slow Obama’s push for healthcare reform. Case in point: The day after Daschle withdrew his nomination, the House of Representatives approved legislation to provide federally funded healthcare to 4 million more Americans by expanding the State Children’s Health Insurance Program, or SCHIP (see “2009: A Pivotal Year for Policy,” p. 14). The president’s first healthcare reform legislation passed Congress by a pair of two-thirds votes and will inject $35 billion into the program over the next five years. More importantly, the fact that the legislation was signed into law on Day 15 of the new administration signals Obama’s commitment to comprehensive healthcare reform.
Most in the HM community fully support the president on the idea that it’s time to change the way healthcare is delivered, revamp the way providers are paid for their services, and eliminate the term “uninsured.” Unfortunately, the president’s tidal wave of support for healthcare reform is being chipped away by a wayward economy and missteps in the confirmation process. A similar message was conveyed during a policy report to SHM’s board of directors in late January in Washington, D.C. Key HM issues, such as bundling and coordination of care, appear to be on the traditional route within the legislative process. Translation: a slower one rife with political obstacles.
At press time, Obama had not put forth a new HHS nominee. Some names thrown into the ring: Jeanne Lambrew, PhD, a deputy health adviser to Obama and Daschle’s former right hand; Rep. Rosa DeLauro (D-Conn.); and Sen. Max Baucus (D-Mont.), chairman of the Senate Finance Committee. And a possibility from the other side of the aisle: Mitt Romney, former Massachusetts governor and presidential candidate. (OK, the Romney mention is a shout-out to the blogosphere. Massachusetts physicians would lay siege to the White House if Romney were nominated.)
Pundits are calling for an individual with many of Daschle’s key attributes: expertise in the healthcare system, knowledge of the inner workings of Washington, and confluence—not to mention influence—with the president in healthcare issues. From the looks of things—and knowing that Daschle’s place in the Obama cabinet was considered a slam dunk—the president will have the unenviable task of replacing the person he thought was most capable of being the “lead architect” to implement “our healthcare plan,” as he said in the Dec. 11 news conference introducing Daschle as his HHS nominee.
Although the task is great and the process delayed, it’s unlikely the healthcare debate is going to slide to the back burner. Although healthcare reform ideology spans the full spectrum—politically, philosophically, and economically—the healthcare debate is alive and kicking in this new administration.
We’ll just have to make sure the next HHS leader is confirmed before The Hospitalist shines the spotlight on them. TH
Jason Carris is editor of The Hospitalist.
Wouldn’t you know it? The same day the February issue of The Hospitalist was being shipped to the post office, former Sen. Tom Daschle—President Obama’s “chosen one” to spearhead healthcare reform— surprised us all. Embroiled in a tax and ethics scandal, Daschle up and withdrew his nomination for secretary of the Department of Health and Human Services (HHS). Considering our February cover story outlines Obama and Daschle’s plan for comprehensive healthcare reform—and the magazine cover has a nice picture of Obama with Daschle in the background—the timing couldn’t have been … better.
In publishing circles, it’s one of those slow-motion moments. You know, the kind of moment sitcoms rewind and show from three different angles. Do they really think we need to see Cosmo Kramer trip and fall three times? I got it.
It’s not as if we declared Thomas Dewey the next president of the United States. If nothing else, consider the February issue a collector’s item. Once I’m done writing this column, I’m going to FedEx a box of February issues to Daschle’s office. I hope he hangs one on the wall—a reminder of how close he came to history.
The fact of the matter is, I’m guessing Daschle’s departure will do little to slow Obama’s push for healthcare reform. Case in point: The day after Daschle withdrew his nomination, the House of Representatives approved legislation to provide federally funded healthcare to 4 million more Americans by expanding the State Children’s Health Insurance Program, or SCHIP (see “2009: A Pivotal Year for Policy,” p. 14). The president’s first healthcare reform legislation passed Congress by a pair of two-thirds votes and will inject $35 billion into the program over the next five years. More importantly, the fact that the legislation was signed into law on Day 15 of the new administration signals Obama’s commitment to comprehensive healthcare reform.
Most in the HM community fully support the president on the idea that it’s time to change the way healthcare is delivered, revamp the way providers are paid for their services, and eliminate the term “uninsured.” Unfortunately, the president’s tidal wave of support for healthcare reform is being chipped away by a wayward economy and missteps in the confirmation process. A similar message was conveyed during a policy report to SHM’s board of directors in late January in Washington, D.C. Key HM issues, such as bundling and coordination of care, appear to be on the traditional route within the legislative process. Translation: a slower one rife with political obstacles.
At press time, Obama had not put forth a new HHS nominee. Some names thrown into the ring: Jeanne Lambrew, PhD, a deputy health adviser to Obama and Daschle’s former right hand; Rep. Rosa DeLauro (D-Conn.); and Sen. Max Baucus (D-Mont.), chairman of the Senate Finance Committee. And a possibility from the other side of the aisle: Mitt Romney, former Massachusetts governor and presidential candidate. (OK, the Romney mention is a shout-out to the blogosphere. Massachusetts physicians would lay siege to the White House if Romney were nominated.)
Pundits are calling for an individual with many of Daschle’s key attributes: expertise in the healthcare system, knowledge of the inner workings of Washington, and confluence—not to mention influence—with the president in healthcare issues. From the looks of things—and knowing that Daschle’s place in the Obama cabinet was considered a slam dunk—the president will have the unenviable task of replacing the person he thought was most capable of being the “lead architect” to implement “our healthcare plan,” as he said in the Dec. 11 news conference introducing Daschle as his HHS nominee.
Although the task is great and the process delayed, it’s unlikely the healthcare debate is going to slide to the back burner. Although healthcare reform ideology spans the full spectrum—politically, philosophically, and economically—the healthcare debate is alive and kicking in this new administration.
We’ll just have to make sure the next HHS leader is confirmed before The Hospitalist shines the spotlight on them. TH
Jason Carris is editor of The Hospitalist.
Wouldn’t you know it? The same day the February issue of The Hospitalist was being shipped to the post office, former Sen. Tom Daschle—President Obama’s “chosen one” to spearhead healthcare reform— surprised us all. Embroiled in a tax and ethics scandal, Daschle up and withdrew his nomination for secretary of the Department of Health and Human Services (HHS). Considering our February cover story outlines Obama and Daschle’s plan for comprehensive healthcare reform—and the magazine cover has a nice picture of Obama with Daschle in the background—the timing couldn’t have been … better.
In publishing circles, it’s one of those slow-motion moments. You know, the kind of moment sitcoms rewind and show from three different angles. Do they really think we need to see Cosmo Kramer trip and fall three times? I got it.
It’s not as if we declared Thomas Dewey the next president of the United States. If nothing else, consider the February issue a collector’s item. Once I’m done writing this column, I’m going to FedEx a box of February issues to Daschle’s office. I hope he hangs one on the wall—a reminder of how close he came to history.
The fact of the matter is, I’m guessing Daschle’s departure will do little to slow Obama’s push for healthcare reform. Case in point: The day after Daschle withdrew his nomination, the House of Representatives approved legislation to provide federally funded healthcare to 4 million more Americans by expanding the State Children’s Health Insurance Program, or SCHIP (see “2009: A Pivotal Year for Policy,” p. 14). The president’s first healthcare reform legislation passed Congress by a pair of two-thirds votes and will inject $35 billion into the program over the next five years. More importantly, the fact that the legislation was signed into law on Day 15 of the new administration signals Obama’s commitment to comprehensive healthcare reform.
Most in the HM community fully support the president on the idea that it’s time to change the way healthcare is delivered, revamp the way providers are paid for their services, and eliminate the term “uninsured.” Unfortunately, the president’s tidal wave of support for healthcare reform is being chipped away by a wayward economy and missteps in the confirmation process. A similar message was conveyed during a policy report to SHM’s board of directors in late January in Washington, D.C. Key HM issues, such as bundling and coordination of care, appear to be on the traditional route within the legislative process. Translation: a slower one rife with political obstacles.
At press time, Obama had not put forth a new HHS nominee. Some names thrown into the ring: Jeanne Lambrew, PhD, a deputy health adviser to Obama and Daschle’s former right hand; Rep. Rosa DeLauro (D-Conn.); and Sen. Max Baucus (D-Mont.), chairman of the Senate Finance Committee. And a possibility from the other side of the aisle: Mitt Romney, former Massachusetts governor and presidential candidate. (OK, the Romney mention is a shout-out to the blogosphere. Massachusetts physicians would lay siege to the White House if Romney were nominated.)
Pundits are calling for an individual with many of Daschle’s key attributes: expertise in the healthcare system, knowledge of the inner workings of Washington, and confluence—not to mention influence—with the president in healthcare issues. From the looks of things—and knowing that Daschle’s place in the Obama cabinet was considered a slam dunk—the president will have the unenviable task of replacing the person he thought was most capable of being the “lead architect” to implement “our healthcare plan,” as he said in the Dec. 11 news conference introducing Daschle as his HHS nominee.
Although the task is great and the process delayed, it’s unlikely the healthcare debate is going to slide to the back burner. Although healthcare reform ideology spans the full spectrum—politically, philosophically, and economically—the healthcare debate is alive and kicking in this new administration.
We’ll just have to make sure the next HHS leader is confirmed before The Hospitalist shines the spotlight on them. TH
Jason Carris is editor of The Hospitalist.