User login
Dual fractional laser offers advantages for facial rejuvenation
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
AT THE ODAC CONFERENCE
Understand form and function to make the most of fillers
LAS VEGAS – Combining the right products and anatomical knowledge translates patient concerns into better outcomes when using fillers, according to Burt Steffes, MD, a dermatologist in Fond du Lac, Wisc.
“If you understand differences in products, you’ll get better results and minimize complications” for different areas, Dr. Steffes said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
The physical properties of different fillers impact the results, he pointed out. For example, G prime, a measure of elasticity, varies among fillers; a filler with a higher G prime is more contour stable and is designed to lift tissue, while a product with a lower G prime is designed to spread through tissues and move more naturally with the face.
However, “lift capacity using G prime is only useful across products in the entire family and make up,” Dr. Steffes noted. A recent Allergan-sponsored study emphasized that “product performance is a complex interaction of various properties and tissue interactions not just G prime,” he said (Dermatol Surg, 2015;41:S373-81).
Determining the most effective filler to use depends on the location and area to be corrected.
• Tear troughs: Dr. Steffes recommends avoiding hydrophilic products; he prefers Belotero, Restylane, or Restylane Silk.
• Lips: More flexible products such as Juvederm, Restylane, or Belotero can provide patients with the desired result, he noted.
• Nasolabial fold: Juvederm, Restylane, or Radiesse are appropriate choices likely to produce favorable outcomes, Dr. Steffes said.
• Lateral and midface atrophy: For greater lift and cohesivity in these patients, Dr. Steffes considers Perlane, Voluma, Radiesse, or Sculptra as options.
“Fillers are a great way to help people look and feel better,” but complications occur, so be prepared, he said. “You have to know how to recognize and manage complications.”
Proper management starts with staff education. Provide instruction and training to staff (including reception) on how to recognize impending problems. “Have a written protocol available, and keep nitroglycerin paste, hyaluronidase, and aspirin on hand,” he advised.
Cases of swelling may require hyaluronidase to correct, as may lumps and bumps, Dr. Steffes said. Bruising may be managed with ice packs after the fact, but can often be avoided or minimized by using blunt tip cannulas, slow injections, small aliquots, and small-gauge needles, he added.
In cases of extreme complications such as vascular occlusion, start by massaging the area with nitroglycerin paste, and administer hyaluronidase if necessary, he said. However, be sure to proceed carefully if using hyaluronidase in patients with an allergy to bee stings; use it only in an emergency in these patients and treat anaphylaxis if necessary, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Combining the right products and anatomical knowledge translates patient concerns into better outcomes when using fillers, according to Burt Steffes, MD, a dermatologist in Fond du Lac, Wisc.
“If you understand differences in products, you’ll get better results and minimize complications” for different areas, Dr. Steffes said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
The physical properties of different fillers impact the results, he pointed out. For example, G prime, a measure of elasticity, varies among fillers; a filler with a higher G prime is more contour stable and is designed to lift tissue, while a product with a lower G prime is designed to spread through tissues and move more naturally with the face.
However, “lift capacity using G prime is only useful across products in the entire family and make up,” Dr. Steffes noted. A recent Allergan-sponsored study emphasized that “product performance is a complex interaction of various properties and tissue interactions not just G prime,” he said (Dermatol Surg, 2015;41:S373-81).
Determining the most effective filler to use depends on the location and area to be corrected.
• Tear troughs: Dr. Steffes recommends avoiding hydrophilic products; he prefers Belotero, Restylane, or Restylane Silk.
• Lips: More flexible products such as Juvederm, Restylane, or Belotero can provide patients with the desired result, he noted.
• Nasolabial fold: Juvederm, Restylane, or Radiesse are appropriate choices likely to produce favorable outcomes, Dr. Steffes said.
• Lateral and midface atrophy: For greater lift and cohesivity in these patients, Dr. Steffes considers Perlane, Voluma, Radiesse, or Sculptra as options.
“Fillers are a great way to help people look and feel better,” but complications occur, so be prepared, he said. “You have to know how to recognize and manage complications.”
Proper management starts with staff education. Provide instruction and training to staff (including reception) on how to recognize impending problems. “Have a written protocol available, and keep nitroglycerin paste, hyaluronidase, and aspirin on hand,” he advised.
Cases of swelling may require hyaluronidase to correct, as may lumps and bumps, Dr. Steffes said. Bruising may be managed with ice packs after the fact, but can often be avoided or minimized by using blunt tip cannulas, slow injections, small aliquots, and small-gauge needles, he added.
In cases of extreme complications such as vascular occlusion, start by massaging the area with nitroglycerin paste, and administer hyaluronidase if necessary, he said. However, be sure to proceed carefully if using hyaluronidase in patients with an allergy to bee stings; use it only in an emergency in these patients and treat anaphylaxis if necessary, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Combining the right products and anatomical knowledge translates patient concerns into better outcomes when using fillers, according to Burt Steffes, MD, a dermatologist in Fond du Lac, Wisc.
“If you understand differences in products, you’ll get better results and minimize complications” for different areas, Dr. Steffes said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
The physical properties of different fillers impact the results, he pointed out. For example, G prime, a measure of elasticity, varies among fillers; a filler with a higher G prime is more contour stable and is designed to lift tissue, while a product with a lower G prime is designed to spread through tissues and move more naturally with the face.
However, “lift capacity using G prime is only useful across products in the entire family and make up,” Dr. Steffes noted. A recent Allergan-sponsored study emphasized that “product performance is a complex interaction of various properties and tissue interactions not just G prime,” he said (Dermatol Surg, 2015;41:S373-81).
Determining the most effective filler to use depends on the location and area to be corrected.
• Tear troughs: Dr. Steffes recommends avoiding hydrophilic products; he prefers Belotero, Restylane, or Restylane Silk.
• Lips: More flexible products such as Juvederm, Restylane, or Belotero can provide patients with the desired result, he noted.
• Nasolabial fold: Juvederm, Restylane, or Radiesse are appropriate choices likely to produce favorable outcomes, Dr. Steffes said.
• Lateral and midface atrophy: For greater lift and cohesivity in these patients, Dr. Steffes considers Perlane, Voluma, Radiesse, or Sculptra as options.
“Fillers are a great way to help people look and feel better,” but complications occur, so be prepared, he said. “You have to know how to recognize and manage complications.”
Proper management starts with staff education. Provide instruction and training to staff (including reception) on how to recognize impending problems. “Have a written protocol available, and keep nitroglycerin paste, hyaluronidase, and aspirin on hand,” he advised.
Cases of swelling may require hyaluronidase to correct, as may lumps and bumps, Dr. Steffes said. Bruising may be managed with ice packs after the fact, but can often be avoided or minimized by using blunt tip cannulas, slow injections, small aliquots, and small-gauge needles, he added.
In cases of extreme complications such as vascular occlusion, start by massaging the area with nitroglycerin paste, and administer hyaluronidase if necessary, he said. However, be sure to proceed carefully if using hyaluronidase in patients with an allergy to bee stings; use it only in an emergency in these patients and treat anaphylaxis if necessary, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Simple tips optimize toxin treatments
LAS VEGAS – Listening to patients is the “first and most important step” toward using neuromodulators successfully, according to Burt Steffes, MD.
Clinicians armed with a thorough knowledge of anatomy and the available products can use neuromodulators successfully for a range of aging concerns including the glabellar complex, crow’s feet, marionette lines, smoker’s lines, a dimpled chin, and platysmal bands, Dr. Steffes, a dermatologist in Fond du Lac, Wisc., said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
When diluting toxins, be consistent for best results, he advised. “Pick a concentration you like and stick with it,” he said. Establishing realistic expectations and taking preprocedure photos are essential for optimizing results, he added.
Dr. Steffes shared the following tips for successful toxin treatments:
• Horizontal forehead rhytids. Check the brow position and stay approximately 2 cm above the eyebrows. Be conservative with the amount of product used to avoid the frozen look. In cases of upper eyelid ptosis, “improvement can be achieved with apraclonidine 0.5% drops,” he said.
• Glabellar complex. Dr. Steffes said he usually uses 10-30 units. Avoid blood vessels to avoid bruising, he said, “and ask patients to scowl” to identify the exact location for injections.
• Crow’s feet. Treatment of crow’s feet means managing an area “of great variability,” Dr. Steffes said. He advised using superficial injections to minimize bruising, while staying 2 cm from the orbital rim and adjusting to match the patient’s rhytid pattern. He recommends 1-2 units placed 1 cm below the lower eyelid margin at the mid-pupillary line to decrease the bunching of the lower eyelid.
• Platysmal bands. Managing volume is the key to successful treatment of platysmal bands, said Dr. Steffes. “Injecting too much product into the neck can lead to asymmetry” he cautioned. Pinch the platysmal band between the fingers and inject intramuscularly, using 2 units per injection. “Use conservative amounts and adjust in two weeks if needed,” he said.
Be sure that all patients make follow-up appointments before they leave the office after a procedure, and schedule new patients for follow-up in 2 weeks, said Dr. Steffes. Instruct all patients to contact your office immediately for any concerns including bruising that may be managed within the first 24-48 hours with a low-fluence 595-nm, 532-nm, or 1,064-nm laser, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Listening to patients is the “first and most important step” toward using neuromodulators successfully, according to Burt Steffes, MD.
Clinicians armed with a thorough knowledge of anatomy and the available products can use neuromodulators successfully for a range of aging concerns including the glabellar complex, crow’s feet, marionette lines, smoker’s lines, a dimpled chin, and platysmal bands, Dr. Steffes, a dermatologist in Fond du Lac, Wisc., said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
When diluting toxins, be consistent for best results, he advised. “Pick a concentration you like and stick with it,” he said. Establishing realistic expectations and taking preprocedure photos are essential for optimizing results, he added.
Dr. Steffes shared the following tips for successful toxin treatments:
• Horizontal forehead rhytids. Check the brow position and stay approximately 2 cm above the eyebrows. Be conservative with the amount of product used to avoid the frozen look. In cases of upper eyelid ptosis, “improvement can be achieved with apraclonidine 0.5% drops,” he said.
• Glabellar complex. Dr. Steffes said he usually uses 10-30 units. Avoid blood vessels to avoid bruising, he said, “and ask patients to scowl” to identify the exact location for injections.
• Crow’s feet. Treatment of crow’s feet means managing an area “of great variability,” Dr. Steffes said. He advised using superficial injections to minimize bruising, while staying 2 cm from the orbital rim and adjusting to match the patient’s rhytid pattern. He recommends 1-2 units placed 1 cm below the lower eyelid margin at the mid-pupillary line to decrease the bunching of the lower eyelid.
• Platysmal bands. Managing volume is the key to successful treatment of platysmal bands, said Dr. Steffes. “Injecting too much product into the neck can lead to asymmetry” he cautioned. Pinch the platysmal band between the fingers and inject intramuscularly, using 2 units per injection. “Use conservative amounts and adjust in two weeks if needed,” he said.
Be sure that all patients make follow-up appointments before they leave the office after a procedure, and schedule new patients for follow-up in 2 weeks, said Dr. Steffes. Instruct all patients to contact your office immediately for any concerns including bruising that may be managed within the first 24-48 hours with a low-fluence 595-nm, 532-nm, or 1,064-nm laser, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Listening to patients is the “first and most important step” toward using neuromodulators successfully, according to Burt Steffes, MD.
Clinicians armed with a thorough knowledge of anatomy and the available products can use neuromodulators successfully for a range of aging concerns including the glabellar complex, crow’s feet, marionette lines, smoker’s lines, a dimpled chin, and platysmal bands, Dr. Steffes, a dermatologist in Fond du Lac, Wisc., said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
When diluting toxins, be consistent for best results, he advised. “Pick a concentration you like and stick with it,” he said. Establishing realistic expectations and taking preprocedure photos are essential for optimizing results, he added.
Dr. Steffes shared the following tips for successful toxin treatments:
• Horizontal forehead rhytids. Check the brow position and stay approximately 2 cm above the eyebrows. Be conservative with the amount of product used to avoid the frozen look. In cases of upper eyelid ptosis, “improvement can be achieved with apraclonidine 0.5% drops,” he said.
• Glabellar complex. Dr. Steffes said he usually uses 10-30 units. Avoid blood vessels to avoid bruising, he said, “and ask patients to scowl” to identify the exact location for injections.
• Crow’s feet. Treatment of crow’s feet means managing an area “of great variability,” Dr. Steffes said. He advised using superficial injections to minimize bruising, while staying 2 cm from the orbital rim and adjusting to match the patient’s rhytid pattern. He recommends 1-2 units placed 1 cm below the lower eyelid margin at the mid-pupillary line to decrease the bunching of the lower eyelid.
• Platysmal bands. Managing volume is the key to successful treatment of platysmal bands, said Dr. Steffes. “Injecting too much product into the neck can lead to asymmetry” he cautioned. Pinch the platysmal band between the fingers and inject intramuscularly, using 2 units per injection. “Use conservative amounts and adjust in two weeks if needed,” he said.
Be sure that all patients make follow-up appointments before they leave the office after a procedure, and schedule new patients for follow-up in 2 weeks, said Dr. Steffes. Instruct all patients to contact your office immediately for any concerns including bruising that may be managed within the first 24-48 hours with a low-fluence 595-nm, 532-nm, or 1,064-nm laser, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
VIDEO: For facial resurfacing, revisit CO2 lasers
LAS VEGAS – Patients can enjoy positive results from facial resurfacing with fractionated lasers, but they don’t always yield the same benefits as the traditional CO2 laser, Christopher Zachary, M.D., said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
“A lot of us are going back to using traditional laser resurfacing” for the patients who need it, such as those with many wrinkles, crepey skin, and extensive sun damage, Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine, said in a video interview.
“Those patients are not going to have an optimal result, even with the most aggressive of fractionated ablative lasers, as compared to the traditional laser resurfacing,” he added.
Dr. Zachary disclosed relationships with multiple companies, including Solta, Zeltiq, Scion, Amway, and Candela. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Patients can enjoy positive results from facial resurfacing with fractionated lasers, but they don’t always yield the same benefits as the traditional CO2 laser, Christopher Zachary, M.D., said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
“A lot of us are going back to using traditional laser resurfacing” for the patients who need it, such as those with many wrinkles, crepey skin, and extensive sun damage, Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine, said in a video interview.
“Those patients are not going to have an optimal result, even with the most aggressive of fractionated ablative lasers, as compared to the traditional laser resurfacing,” he added.
Dr. Zachary disclosed relationships with multiple companies, including Solta, Zeltiq, Scion, Amway, and Candela. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Patients can enjoy positive results from facial resurfacing with fractionated lasers, but they don’t always yield the same benefits as the traditional CO2 laser, Christopher Zachary, M.D., said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
“A lot of us are going back to using traditional laser resurfacing” for the patients who need it, such as those with many wrinkles, crepey skin, and extensive sun damage, Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine, said in a video interview.
“Those patients are not going to have an optimal result, even with the most aggressive of fractionated ablative lasers, as compared to the traditional laser resurfacing,” he added.
Dr. Zachary disclosed relationships with multiple companies, including Solta, Zeltiq, Scion, Amway, and Candela. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
VIDEO: Bulk matters in body sculpting
LAS VEGAS – Both heating and cooling techniques can provide effective results for patients seeking to improve their appearance with body sculpting, Christopher Zachary, MD, said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Whether the clinician chooses devices that use radiofrequency, laser, or cryolipolysis to target fat, the key is bulk treatment, Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine, said in a video interview.
When cooling or heating the fat, “it has to been done in bulk; it has to be done for a certain length of time,” he said, noting that treatment times vary with devices, from 5 to 60 minutes. “I can’t stress enough the importance of bulk cooling or bulk heating,” which induce a chronic reaction “that results in localized fat reduction,” he added.
Dr. Zachary disclosed relationships with multiple companies, including Solta, Zeltiq, Scion, Amway, and Candela. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Both heating and cooling techniques can provide effective results for patients seeking to improve their appearance with body sculpting, Christopher Zachary, MD, said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Whether the clinician chooses devices that use radiofrequency, laser, or cryolipolysis to target fat, the key is bulk treatment, Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine, said in a video interview.
When cooling or heating the fat, “it has to been done in bulk; it has to be done for a certain length of time,” he said, noting that treatment times vary with devices, from 5 to 60 minutes. “I can’t stress enough the importance of bulk cooling or bulk heating,” which induce a chronic reaction “that results in localized fat reduction,” he added.
Dr. Zachary disclosed relationships with multiple companies, including Solta, Zeltiq, Scion, Amway, and Candela. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Both heating and cooling techniques can provide effective results for patients seeking to improve their appearance with body sculpting, Christopher Zachary, MD, said at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
Whether the clinician chooses devices that use radiofrequency, laser, or cryolipolysis to target fat, the key is bulk treatment, Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine, said in a video interview.
When cooling or heating the fat, “it has to been done in bulk; it has to be done for a certain length of time,” he said, noting that treatment times vary with devices, from 5 to 60 minutes. “I can’t stress enough the importance of bulk cooling or bulk heating,” which induce a chronic reaction “that results in localized fat reduction,” he added.
Dr. Zachary disclosed relationships with multiple companies, including Solta, Zeltiq, Scion, Amway, and Candela. SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
Highlights from the ASDS Annual Conference 2016
At this year’s American Society for Dermatologic Surgery (ASDS) annual meeting, many of the hot topics pertained to tightening and smoothness of the skin. More naturally derived skin care products were discussed, as well as skin-tightening devices, techniques for improving fat, microneedling, devices for improving cellulite, and some of the newer injectable fillers on the market.
Of all of these, the use of microneedling with and without radiofrequency energy to improve acne scars, rhytids, and pore size was the most prominent emerging trend. Microneedling devices with radiofrequency also are being used for skin tightening, in addition to improving skin texture.
There were also presentations on improvements in acne scars with a number of techniques, including fractional ablative and nonablative lasers, subcision, microneedling, and fillers.
Controversies addressed at the meeting included whether or not dermatologists should use the same lasers with different Food and Drug Administration–approved hand pieces for vaginal rejuvenation. In addition, controversies over whether Mohs surgeons should undergo board examination were discussed.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com.
At this year’s American Society for Dermatologic Surgery (ASDS) annual meeting, many of the hot topics pertained to tightening and smoothness of the skin. More naturally derived skin care products were discussed, as well as skin-tightening devices, techniques for improving fat, microneedling, devices for improving cellulite, and some of the newer injectable fillers on the market.
Of all of these, the use of microneedling with and without radiofrequency energy to improve acne scars, rhytids, and pore size was the most prominent emerging trend. Microneedling devices with radiofrequency also are being used for skin tightening, in addition to improving skin texture.
There were also presentations on improvements in acne scars with a number of techniques, including fractional ablative and nonablative lasers, subcision, microneedling, and fillers.
Controversies addressed at the meeting included whether or not dermatologists should use the same lasers with different Food and Drug Administration–approved hand pieces for vaginal rejuvenation. In addition, controversies over whether Mohs surgeons should undergo board examination were discussed.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com.
At this year’s American Society for Dermatologic Surgery (ASDS) annual meeting, many of the hot topics pertained to tightening and smoothness of the skin. More naturally derived skin care products were discussed, as well as skin-tightening devices, techniques for improving fat, microneedling, devices for improving cellulite, and some of the newer injectable fillers on the market.
Of all of these, the use of microneedling with and without radiofrequency energy to improve acne scars, rhytids, and pore size was the most prominent emerging trend. Microneedling devices with radiofrequency also are being used for skin tightening, in addition to improving skin texture.
There were also presentations on improvements in acne scars with a number of techniques, including fractional ablative and nonablative lasers, subcision, microneedling, and fillers.
Controversies addressed at the meeting included whether or not dermatologists should use the same lasers with different Food and Drug Administration–approved hand pieces for vaginal rejuvenation. In addition, controversies over whether Mohs surgeons should undergo board examination were discussed.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com.
Postinflammatory erythema
The troubling, frustrating part of acne: the persistent acne scars that are often a prolonged battle for most of our patients. We have many techniques to deal with postinflammatory hyperpigmentation (PIH). However, postinflammatory erythema (PIE), the erythematous scars often seen in acne and other inflammatory skin conditions, is not well understood. And despite its pervasive nature, very little data exist that identify its etiology and effective treatment options.
Inflammatory acne scars are not all the same. PIH, often seen with Fitzpatrick skin types III-VI, is related to brown spots, not red spots. Hyperpigmentation is caused by an excess production of melanin. There are treatments for PIH in our armamentarium – such as microdermabrasion, chemical peels, hydroquinone, and vitamin C – that inhibit melanogenesis and blend the skin discoloration.
In contrast, PIE is characterized by pink, red, and sometimes purple-appearing vascular neogenesis seen most often with skin types I-III after an inflammatory skin condition resolves, and is often seen in cystic acne.
The term postinflammatory erythema was initially introduced in the dermatology literature in 2013 by Bae-Harboe et al. to describe erythema often seen after the resolution of inflammatory acne or other inflammatory skin conditions.1 It is not to be confused with the erythema and telangiectasias seen in erythematotelangiectatic rosacea, which is a separate entity.
In my practice, microneedling has also been effective in reducing PIE. Although this may seem counterintuitive because of the bleeding associated with the microneedling process, microneedling-induced skin tissue injury and neocollagenesis have been clinically shown to improve the abnormal vascular proliferation that occurs in PIE. Similar techniques can be used with fractional resurfacing lasers. However, no studies have specifically evaluated the erythematous component of acne scars treated with fractionated lasers.
Topical preparations containing brimonidine (Mirvaso), azelaic acid, and green tea, as well as oral nicotinamide, can have a temporary effect on reducing skin erythema.
However, very little data or clinical studies are available on treatments for PIE, and there are no well-studied preparations with long-term efficacy data. Studies are needed to provide better clinical guidelines for treatment methods and alternatives to treatments, including topical and systemic medications.
References
1. J Clin Aesthet Dermatol. 2013 Sep;6(9):46-7.
2. J Am Acad Dermatol. 2009 May;60(5):801-7.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@frontlinemedcom.com.
The troubling, frustrating part of acne: the persistent acne scars that are often a prolonged battle for most of our patients. We have many techniques to deal with postinflammatory hyperpigmentation (PIH). However, postinflammatory erythema (PIE), the erythematous scars often seen in acne and other inflammatory skin conditions, is not well understood. And despite its pervasive nature, very little data exist that identify its etiology and effective treatment options.
Inflammatory acne scars are not all the same. PIH, often seen with Fitzpatrick skin types III-VI, is related to brown spots, not red spots. Hyperpigmentation is caused by an excess production of melanin. There are treatments for PIH in our armamentarium – such as microdermabrasion, chemical peels, hydroquinone, and vitamin C – that inhibit melanogenesis and blend the skin discoloration.
In contrast, PIE is characterized by pink, red, and sometimes purple-appearing vascular neogenesis seen most often with skin types I-III after an inflammatory skin condition resolves, and is often seen in cystic acne.
The term postinflammatory erythema was initially introduced in the dermatology literature in 2013 by Bae-Harboe et al. to describe erythema often seen after the resolution of inflammatory acne or other inflammatory skin conditions.1 It is not to be confused with the erythema and telangiectasias seen in erythematotelangiectatic rosacea, which is a separate entity.
In my practice, microneedling has also been effective in reducing PIE. Although this may seem counterintuitive because of the bleeding associated with the microneedling process, microneedling-induced skin tissue injury and neocollagenesis have been clinically shown to improve the abnormal vascular proliferation that occurs in PIE. Similar techniques can be used with fractional resurfacing lasers. However, no studies have specifically evaluated the erythematous component of acne scars treated with fractionated lasers.
Topical preparations containing brimonidine (Mirvaso), azelaic acid, and green tea, as well as oral nicotinamide, can have a temporary effect on reducing skin erythema.
However, very little data or clinical studies are available on treatments for PIE, and there are no well-studied preparations with long-term efficacy data. Studies are needed to provide better clinical guidelines for treatment methods and alternatives to treatments, including topical and systemic medications.
References
1. J Clin Aesthet Dermatol. 2013 Sep;6(9):46-7.
2. J Am Acad Dermatol. 2009 May;60(5):801-7.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@frontlinemedcom.com.
The troubling, frustrating part of acne: the persistent acne scars that are often a prolonged battle for most of our patients. We have many techniques to deal with postinflammatory hyperpigmentation (PIH). However, postinflammatory erythema (PIE), the erythematous scars often seen in acne and other inflammatory skin conditions, is not well understood. And despite its pervasive nature, very little data exist that identify its etiology and effective treatment options.
Inflammatory acne scars are not all the same. PIH, often seen with Fitzpatrick skin types III-VI, is related to brown spots, not red spots. Hyperpigmentation is caused by an excess production of melanin. There are treatments for PIH in our armamentarium – such as microdermabrasion, chemical peels, hydroquinone, and vitamin C – that inhibit melanogenesis and blend the skin discoloration.
In contrast, PIE is characterized by pink, red, and sometimes purple-appearing vascular neogenesis seen most often with skin types I-III after an inflammatory skin condition resolves, and is often seen in cystic acne.
The term postinflammatory erythema was initially introduced in the dermatology literature in 2013 by Bae-Harboe et al. to describe erythema often seen after the resolution of inflammatory acne or other inflammatory skin conditions.1 It is not to be confused with the erythema and telangiectasias seen in erythematotelangiectatic rosacea, which is a separate entity.
In my practice, microneedling has also been effective in reducing PIE. Although this may seem counterintuitive because of the bleeding associated with the microneedling process, microneedling-induced skin tissue injury and neocollagenesis have been clinically shown to improve the abnormal vascular proliferation that occurs in PIE. Similar techniques can be used with fractional resurfacing lasers. However, no studies have specifically evaluated the erythematous component of acne scars treated with fractionated lasers.
Topical preparations containing brimonidine (Mirvaso), azelaic acid, and green tea, as well as oral nicotinamide, can have a temporary effect on reducing skin erythema.
However, very little data or clinical studies are available on treatments for PIE, and there are no well-studied preparations with long-term efficacy data. Studies are needed to provide better clinical guidelines for treatment methods and alternatives to treatments, including topical and systemic medications.
References
1. J Clin Aesthet Dermatol. 2013 Sep;6(9):46-7.
2. J Am Acad Dermatol. 2009 May;60(5):801-7.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@frontlinemedcom.com.
Aesthetic dermatology: What do we know so far about Volbella?
On May 31, 2016, the Food and Drug Administration approved Juvéderm Volbella XC for use in the lips for lip augmentation and for correction of perioral rhytids, in adults over the age of 21. In the U.S. pivotal clinical trial of 168 patients, Juvederm Volbella XC was found to increase lip fullness and soften the appearance of perioral rhytids in two-thirds through 1 year.
Like its previously approved predecessor Juvéderm Voluma XC, approved for the mid-face/cheek area, Juvéderm Volbella XC is composed of hyaluronic acid (HA) using Vycross technology. Vycross technology blends different molecular weights of hyaluronic acid together, allowing for longer duration of the product. Unlike Juvéderm Voluma XC (20 mg/mL), Juvéderm Volbella XC is a lower-concentration HA (15 mg/mL) and has a lower G prime and cohesivity, allowing more horizontal spread as opposed to a lift, which makes it more appropriate for injection into the lips and superficial perioral lines.1
Juvéderm Volbella XC will not be available for use in the United States until October 2016. However, the product was first approved in Europe in 2011, and subsequently in Latin America, the Middle East, Asia Pacific, and Canada. What has been the experience of our neighboring colleagues?
In a randomized, prospective, 12-month controlled European study of 280 patients comparing Volbella to a nonanimal stabilized hyaluronic acid (NASHA), Volbella was found to be noninferior to NASHA at 3 months.2 Improvements in lip fullness, perioral lines, and oral commissures for Volbella were statistically significant at 6 and 12 months. Acute swelling was also noted to be less.
In a German 62-patient study with primary endpoints of satisfaction with improvement and look and feel of the lips, a high degree of subject satisfaction with aesthetic improvement in the lips, as well as with their natural look and feel, was noted among 83.6% and 75%-93%, respectively.3
In a retrospective chart review of 400 patients in Israel, where Volbella was injected into tear troughs (disclaimer: not approved for tear troughs in the United States) and/or lips, 17 patients (4.25%) developed prolonged inflammatory cutaneous reactions, lasting up to 11 months, which recurred (with an average number of 3.17 episodes) and occurred late (with an average onset of 8.41 weeks after the injection).4 The reactions were treated with antibiotics and hyaluronidase injections. The finding in this published report is higher than the 0.02% of delayed-onset inflammatory reaction previously reported with HA fillers.
With a full armamentarium of HA and non-HA fillers on the market, we are lucky to have many options to select from to treat aesthetic concerns of patients. For lip and perioral enhancement in the United States, Restylane, Juvéderm, Belotero, and now Volbella are all excellent options. As the dermal filler portfolio available internationally is larger than that in the United States, much can be learned from the experience of our international colleagues.
References
1. Plast Reconstr Surg. 2015 Nov;136(5 Suppl):139S-48S.
2. J Drugs Dermatol. 2015 Dec;14(12):1444-52.
3. J Cosmet Dermatol. 2014 Jun;13(2):125-34.
4. Dermatol Surg. 2016 Jan;42(1):31-7.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com. Dr. Wesley has no disclosures with regard to Volbella; she participated in clinical trials for Juvéderm Voluma. Dr. Talakoub is a national trainer for Juvéderm manufacturer Allergan for all its injectables.
On May 31, 2016, the Food and Drug Administration approved Juvéderm Volbella XC for use in the lips for lip augmentation and for correction of perioral rhytids, in adults over the age of 21. In the U.S. pivotal clinical trial of 168 patients, Juvederm Volbella XC was found to increase lip fullness and soften the appearance of perioral rhytids in two-thirds through 1 year.
Like its previously approved predecessor Juvéderm Voluma XC, approved for the mid-face/cheek area, Juvéderm Volbella XC is composed of hyaluronic acid (HA) using Vycross technology. Vycross technology blends different molecular weights of hyaluronic acid together, allowing for longer duration of the product. Unlike Juvéderm Voluma XC (20 mg/mL), Juvéderm Volbella XC is a lower-concentration HA (15 mg/mL) and has a lower G prime and cohesivity, allowing more horizontal spread as opposed to a lift, which makes it more appropriate for injection into the lips and superficial perioral lines.1
Juvéderm Volbella XC will not be available for use in the United States until October 2016. However, the product was first approved in Europe in 2011, and subsequently in Latin America, the Middle East, Asia Pacific, and Canada. What has been the experience of our neighboring colleagues?
In a randomized, prospective, 12-month controlled European study of 280 patients comparing Volbella to a nonanimal stabilized hyaluronic acid (NASHA), Volbella was found to be noninferior to NASHA at 3 months.2 Improvements in lip fullness, perioral lines, and oral commissures for Volbella were statistically significant at 6 and 12 months. Acute swelling was also noted to be less.
In a German 62-patient study with primary endpoints of satisfaction with improvement and look and feel of the lips, a high degree of subject satisfaction with aesthetic improvement in the lips, as well as with their natural look and feel, was noted among 83.6% and 75%-93%, respectively.3
In a retrospective chart review of 400 patients in Israel, where Volbella was injected into tear troughs (disclaimer: not approved for tear troughs in the United States) and/or lips, 17 patients (4.25%) developed prolonged inflammatory cutaneous reactions, lasting up to 11 months, which recurred (with an average number of 3.17 episodes) and occurred late (with an average onset of 8.41 weeks after the injection).4 The reactions were treated with antibiotics and hyaluronidase injections. The finding in this published report is higher than the 0.02% of delayed-onset inflammatory reaction previously reported with HA fillers.
With a full armamentarium of HA and non-HA fillers on the market, we are lucky to have many options to select from to treat aesthetic concerns of patients. For lip and perioral enhancement in the United States, Restylane, Juvéderm, Belotero, and now Volbella are all excellent options. As the dermal filler portfolio available internationally is larger than that in the United States, much can be learned from the experience of our international colleagues.
References
1. Plast Reconstr Surg. 2015 Nov;136(5 Suppl):139S-48S.
2. J Drugs Dermatol. 2015 Dec;14(12):1444-52.
3. J Cosmet Dermatol. 2014 Jun;13(2):125-34.
4. Dermatol Surg. 2016 Jan;42(1):31-7.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com. Dr. Wesley has no disclosures with regard to Volbella; she participated in clinical trials for Juvéderm Voluma. Dr. Talakoub is a national trainer for Juvéderm manufacturer Allergan for all its injectables.
On May 31, 2016, the Food and Drug Administration approved Juvéderm Volbella XC for use in the lips for lip augmentation and for correction of perioral rhytids, in adults over the age of 21. In the U.S. pivotal clinical trial of 168 patients, Juvederm Volbella XC was found to increase lip fullness and soften the appearance of perioral rhytids in two-thirds through 1 year.
Like its previously approved predecessor Juvéderm Voluma XC, approved for the mid-face/cheek area, Juvéderm Volbella XC is composed of hyaluronic acid (HA) using Vycross technology. Vycross technology blends different molecular weights of hyaluronic acid together, allowing for longer duration of the product. Unlike Juvéderm Voluma XC (20 mg/mL), Juvéderm Volbella XC is a lower-concentration HA (15 mg/mL) and has a lower G prime and cohesivity, allowing more horizontal spread as opposed to a lift, which makes it more appropriate for injection into the lips and superficial perioral lines.1
Juvéderm Volbella XC will not be available for use in the United States until October 2016. However, the product was first approved in Europe in 2011, and subsequently in Latin America, the Middle East, Asia Pacific, and Canada. What has been the experience of our neighboring colleagues?
In a randomized, prospective, 12-month controlled European study of 280 patients comparing Volbella to a nonanimal stabilized hyaluronic acid (NASHA), Volbella was found to be noninferior to NASHA at 3 months.2 Improvements in lip fullness, perioral lines, and oral commissures for Volbella were statistically significant at 6 and 12 months. Acute swelling was also noted to be less.
In a German 62-patient study with primary endpoints of satisfaction with improvement and look and feel of the lips, a high degree of subject satisfaction with aesthetic improvement in the lips, as well as with their natural look and feel, was noted among 83.6% and 75%-93%, respectively.3
In a retrospective chart review of 400 patients in Israel, where Volbella was injected into tear troughs (disclaimer: not approved for tear troughs in the United States) and/or lips, 17 patients (4.25%) developed prolonged inflammatory cutaneous reactions, lasting up to 11 months, which recurred (with an average number of 3.17 episodes) and occurred late (with an average onset of 8.41 weeks after the injection).4 The reactions were treated with antibiotics and hyaluronidase injections. The finding in this published report is higher than the 0.02% of delayed-onset inflammatory reaction previously reported with HA fillers.
With a full armamentarium of HA and non-HA fillers on the market, we are lucky to have many options to select from to treat aesthetic concerns of patients. For lip and perioral enhancement in the United States, Restylane, Juvéderm, Belotero, and now Volbella are all excellent options. As the dermal filler portfolio available internationally is larger than that in the United States, much can be learned from the experience of our international colleagues.
References
1. Plast Reconstr Surg. 2015 Nov;136(5 Suppl):139S-48S.
2. J Drugs Dermatol. 2015 Dec;14(12):1444-52.
3. J Cosmet Dermatol. 2014 Jun;13(2):125-34.
4. Dermatol Surg. 2016 Jan;42(1):31-7.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com. Dr. Wesley has no disclosures with regard to Volbella; she participated in clinical trials for Juvéderm Voluma. Dr. Talakoub is a national trainer for Juvéderm manufacturer Allergan for all its injectables.
Color correcting – for skin blemishes
One of the most frustrating problems we encounter is helping patients with skin issues that we cannot immediately fix or cure. Teaching them the art of concealing skin blemishes gives patients a sense of relief. Color correction is an art and requires an understanding of basic color theory and Fitzpatrick skin type.
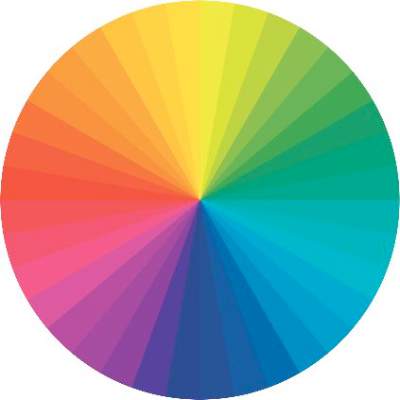
On the color wheel, each color sits directly across from another color, making them complementary colors.
If we look at red, the color opposing it is green. When red and green are combined, they neutralize each other. One of the greatest dermatologists of all time and my mentor, Timothy Berger, MD, taught me that in dermatology color “hue” is a clue to understanding morphology. Everything that is red cannot just be called “erythematous.” There is orange/red (pityriasis rosea, tinea versicolor, seborrheic dermatitis), deep red (cellulitis, Sweet’s syndrome, acne scars, rosacea, psoriasis), purple/red (vasculitis, lichen planus (LP), veins, under-eye circles), brown/red (pigmented purpura, pigmented acne scars, sarcoid).
The combination of the underlying pathology, morphology, and Fitzpatrick type is both a clue to diagnosis and a pallet for skin concealers. We can use the following techniques to help patients color correct skin imperfections:
Red: rosacea, acne scars, acne
Green-based concealers and primers are the best option to significantly reduce the redness. While green primers and correctors tend to be great for Fitzpatrick skin types I-III, a yellow-based concealer/corrector can help to cover redness on those with skin types IV-VI.
Blue: periorbital veins
If you are dealing with blue-toned skin lesions, such as periorbital veins, the ideal corrector is one with a peach or orange undertones. For skin types I-III, a peach/salmon corrector works best, whereas skin types IV-VI requires an orange-toned corrector.
Purple: under-eye circles, LP, postprocedure bruising
If under-eye circles tend to have a more purple hue to them, a yellow-based corrector works best for skin types I-III. For skin types IV-VI skin types, you will need a corrector with a red undertone.
Yellow: bruising
Purple/lavender correctors are best suited for eliminating yellow tones from the face. Purple also combats sallow undertones of the skin.
Brown: lentigines, melasma, seborrheic keratosis, post-inflammatory hyperpigmentation, nevi, café au lait spots
Brown is actually the hardest of all colors to correct. The deeper the pigment (ashy dermatitis, melasma) the more gray the areas appear with skin concealers. The more superficial the pigment (ephelides, lentigines), the easier it is to correct. Generally speaking, peach toned concealers work best, not beige or brown. The corrector, however, should be lighter than the skin tone or the lesion itself will appear darker.
Helping patients conceal imperfections with these simple guidelines is a great way to help relieve some anxiety and help our patients fell more confident in their skin.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@frontlinemedcom.com.
One of the most frustrating problems we encounter is helping patients with skin issues that we cannot immediately fix or cure. Teaching them the art of concealing skin blemishes gives patients a sense of relief. Color correction is an art and requires an understanding of basic color theory and Fitzpatrick skin type.
On the color wheel, each color sits directly across from another color, making them complementary colors.
If we look at red, the color opposing it is green. When red and green are combined, they neutralize each other. One of the greatest dermatologists of all time and my mentor, Timothy Berger, MD, taught me that in dermatology color “hue” is a clue to understanding morphology. Everything that is red cannot just be called “erythematous.” There is orange/red (pityriasis rosea, tinea versicolor, seborrheic dermatitis), deep red (cellulitis, Sweet’s syndrome, acne scars, rosacea, psoriasis), purple/red (vasculitis, lichen planus (LP), veins, under-eye circles), brown/red (pigmented purpura, pigmented acne scars, sarcoid).
The combination of the underlying pathology, morphology, and Fitzpatrick type is both a clue to diagnosis and a pallet for skin concealers. We can use the following techniques to help patients color correct skin imperfections:
Red: rosacea, acne scars, acne
Green-based concealers and primers are the best option to significantly reduce the redness. While green primers and correctors tend to be great for Fitzpatrick skin types I-III, a yellow-based concealer/corrector can help to cover redness on those with skin types IV-VI.
Blue: periorbital veins
If you are dealing with blue-toned skin lesions, such as periorbital veins, the ideal corrector is one with a peach or orange undertones. For skin types I-III, a peach/salmon corrector works best, whereas skin types IV-VI requires an orange-toned corrector.
Purple: under-eye circles, LP, postprocedure bruising
If under-eye circles tend to have a more purple hue to them, a yellow-based corrector works best for skin types I-III. For skin types IV-VI skin types, you will need a corrector with a red undertone.
Yellow: bruising
Purple/lavender correctors are best suited for eliminating yellow tones from the face. Purple also combats sallow undertones of the skin.
Brown: lentigines, melasma, seborrheic keratosis, post-inflammatory hyperpigmentation, nevi, café au lait spots
Brown is actually the hardest of all colors to correct. The deeper the pigment (ashy dermatitis, melasma) the more gray the areas appear with skin concealers. The more superficial the pigment (ephelides, lentigines), the easier it is to correct. Generally speaking, peach toned concealers work best, not beige or brown. The corrector, however, should be lighter than the skin tone or the lesion itself will appear darker.
Helping patients conceal imperfections with these simple guidelines is a great way to help relieve some anxiety and help our patients fell more confident in their skin.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@frontlinemedcom.com.
One of the most frustrating problems we encounter is helping patients with skin issues that we cannot immediately fix or cure. Teaching them the art of concealing skin blemishes gives patients a sense of relief. Color correction is an art and requires an understanding of basic color theory and Fitzpatrick skin type.
On the color wheel, each color sits directly across from another color, making them complementary colors.
If we look at red, the color opposing it is green. When red and green are combined, they neutralize each other. One of the greatest dermatologists of all time and my mentor, Timothy Berger, MD, taught me that in dermatology color “hue” is a clue to understanding morphology. Everything that is red cannot just be called “erythematous.” There is orange/red (pityriasis rosea, tinea versicolor, seborrheic dermatitis), deep red (cellulitis, Sweet’s syndrome, acne scars, rosacea, psoriasis), purple/red (vasculitis, lichen planus (LP), veins, under-eye circles), brown/red (pigmented purpura, pigmented acne scars, sarcoid).
The combination of the underlying pathology, morphology, and Fitzpatrick type is both a clue to diagnosis and a pallet for skin concealers. We can use the following techniques to help patients color correct skin imperfections:
Red: rosacea, acne scars, acne
Green-based concealers and primers are the best option to significantly reduce the redness. While green primers and correctors tend to be great for Fitzpatrick skin types I-III, a yellow-based concealer/corrector can help to cover redness on those with skin types IV-VI.
Blue: periorbital veins
If you are dealing with blue-toned skin lesions, such as periorbital veins, the ideal corrector is one with a peach or orange undertones. For skin types I-III, a peach/salmon corrector works best, whereas skin types IV-VI requires an orange-toned corrector.
Purple: under-eye circles, LP, postprocedure bruising
If under-eye circles tend to have a more purple hue to them, a yellow-based corrector works best for skin types I-III. For skin types IV-VI skin types, you will need a corrector with a red undertone.
Yellow: bruising
Purple/lavender correctors are best suited for eliminating yellow tones from the face. Purple also combats sallow undertones of the skin.
Brown: lentigines, melasma, seborrheic keratosis, post-inflammatory hyperpigmentation, nevi, café au lait spots
Brown is actually the hardest of all colors to correct. The deeper the pigment (ashy dermatitis, melasma) the more gray the areas appear with skin concealers. The more superficial the pigment (ephelides, lentigines), the easier it is to correct. Generally speaking, peach toned concealers work best, not beige or brown. The corrector, however, should be lighter than the skin tone or the lesion itself will appear darker.
Helping patients conceal imperfections with these simple guidelines is a great way to help relieve some anxiety and help our patients fell more confident in their skin.
Dr. Talakoub and Dr. Wesley are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at dermnews@frontlinemedcom.com.
Laser and electrocautery plume
A recent publication by Chuang et al. carefully characterizes the content of smoke (or plume) created from laser hair removal.1 At the University of California, Los Angeles, discarded terminal hairs from the trunk and extremities were collected from two adult volunteers. The hair samples were sealed in glass gas chromatography chambers and treated with either an 810-nm diode laser (Lightsheer, Lumenis) or 755-nm alexandrite laser (Gentlelase, Candela). During laser hair removal (LHR) treatment, two 6-L negative-pressure canisters were used to capture 30 seconds of laser plume, and a portable condensation particle counter was used to measure ultrafine particulates (less than 1 mcm). Ultrafine particle concentrations were measured within the treatment room, within the waiting room, and outside the building. The laser plume was then analyzed by gas chromatography–mass spectrometry (GC-MS) at the Boston University department of chemistry.
Analysis with GC-MS identified 377 chemical compounds. Sixty-two of the compounds exhibited strong absorption peaks, of which 13 are known or suspected carcinogens (including benzene, ethylbenzene, benzeneacetonitrile, acetonitrile, quinoline, isoquinoline, sterene, diethyl phthalate, 2-methylpyridine, naphthalene carbonitrile, and propene) and more than 20 are known environmental toxins causing acute toxic effects on exposure (including carbon monoxide, p-xylene, phenol, toluene, benzaldehyde, benzenedicarboxylic acid [phthalic acid], and long-chain and cyclic hydrocarbons).
During LHR, the portable condensation particle counters documented an eightfold increase, compared with the ambient room baseline level of ultrafine particle concentrations (ambient room baseline, 15,300 particles per cubic centimeter [ppc]; LHR with smoke evacuator, 129,376 ppc), even when a smoke evacuator was in close proximity (5.0 cm) to the procedure site. When the smoke evacuator was turned off for 30 seconds, there was a more than 26-fold increase in particulate count, compared with ambient baseline levels (ambient baseline, 15,300 ppc; LHR without smoke evacuator for 30 seconds, 435,888 ppc).
It has long been known that smoke created from electrocautery also may impose a risk on the health care worker. In 2011, Lewin et al. published a comprehensive review of the risk that surgical smoke and laser imposes on the dermatologist.2 At this time, most of the laser data was for the plume created by ablative CO2 lasers. In their review, it was stated that surgical smoke is composed of 95% water and 5% particulate matter (made up of chemicals, blood and tissue particles, viruses, and bacteria). The size of the particulate matter is dictated by the device used, with electrosurgical units creating particles of roughly 0.07 mcm and lasers liberating particles of 0.31 mcm. The size of liberated particles is important as those smaller than 100 mcm in diameter remain airborne, and particles less than 2 mcm are deposited in the bronchioles and alveoli.
Electrocautery plume is composed mostly of hydrocarbons, phenols, nitriles, and fatty acids, but most notably carbon monoxide, acrylonitrile, hydrogen cyanide, and benzene, which may have carcinogenic potential. On the mucosa of the canine tongue, the mutagenic effect of the smoke from 1 g of cauterized tissue with laser and electrocautery was equivalent to those from three or six cigarettes, respectively. Pulmonary changes also may occur. Blood vessel hypertrophy, alveolar congestion, and emphysematous changes were seen in rats after plume created from both electrocautery and Nd:Yag ablation of porcine skin. In that study, pulmonary changes were less severe in rats exposed to surgical smoke collected with single- and double-filtered smoke evacuators than unfiltered smoke.
Infection also poses a risk, with bovine papillomavirus and HPV detected in CO2 laser plume as early as 1988. In 1995, Gloster and Roenigk at the Mayo Clinic conducted a comparative study using questionnaires sent to members of the American Society for Laser Surgeons and the American Society of Dermatologic Surgery.3 The comparison groups were CO2 laser surgeons and two large groups of patients in the community with a diagnosis of warts. Analysis revealed that CO2 laser surgeons had a statistically significant greater risk of acquiring nasopharyngeal warts but were less likely to acquire plantar, genital, and perianal warts than the Mayo Clinic patient group did, demonstrating that laser plume is a likely means by which HPV can be transmitted to the upper airway, suggesting that those using lasers to treat HPV lesions are at greater risk. Staphylococcus, Corynebacterium, and Neisseria also have been detected during laser resurfacing.
Traditional surgical masks are able to capture particles greater than 5 mcm but offer no protection against particulate matter produced by electrosurgical and laser devices liberating byproducts less than 1 mcm. Laser masks or high-filtration masks provide greater protection than do standard surgical masks and are able to filter particles to 1.1 mcm; however, it has been shown that approximately 77% of particulate matter in surgical smoke is 1.1 mcm and smaller. Smoke evacuators consist of a suction unit (vacuum pump), filter, hose, and inlet nozzle. The smoke evacuator should have a capture velocity of approximately 30-45 m/min at the inlet nozzle. As the effectiveness of the smoke evacuator decreases with farther distance away from the procedure site, the current study of laser plume from LHR recommends that the smoke evacuator be placed within 5 cm of plume generation.4 In a study of warts treated with CO2 laser or electrocoagulation, smoke evacuators are 98.6% effective when placed 1 cm from the treatment site, with efficacy decreasing to 50% when moved to 2 cm from the treatment site.
As our specialty likely conducts the highest proportion of laser and electrosurgical procedures of any specialty, current recommendations for electrocautery, laser resurfacing, and LHR should include adequate air filtration and the use of high-filtration masks and smoke evacuators by the health care practitioner.
References
1. JAMA Dermatol. 2016 Jul 6. doi: 10.1001/jamadermatol.2016.2097. [Epub ahead of print]
2. J Am Acad Dermatol. 2011 Sep;65(3):636-41.
3. J Am Acad Dermatol. 1995 Mar;32(3):436-41.
4. J Am Acad Dermatol. 1989 Jul;21(1):41-9.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com.
A recent publication by Chuang et al. carefully characterizes the content of smoke (or plume) created from laser hair removal.1 At the University of California, Los Angeles, discarded terminal hairs from the trunk and extremities were collected from two adult volunteers. The hair samples were sealed in glass gas chromatography chambers and treated with either an 810-nm diode laser (Lightsheer, Lumenis) or 755-nm alexandrite laser (Gentlelase, Candela). During laser hair removal (LHR) treatment, two 6-L negative-pressure canisters were used to capture 30 seconds of laser plume, and a portable condensation particle counter was used to measure ultrafine particulates (less than 1 mcm). Ultrafine particle concentrations were measured within the treatment room, within the waiting room, and outside the building. The laser plume was then analyzed by gas chromatography–mass spectrometry (GC-MS) at the Boston University department of chemistry.
Analysis with GC-MS identified 377 chemical compounds. Sixty-two of the compounds exhibited strong absorption peaks, of which 13 are known or suspected carcinogens (including benzene, ethylbenzene, benzeneacetonitrile, acetonitrile, quinoline, isoquinoline, sterene, diethyl phthalate, 2-methylpyridine, naphthalene carbonitrile, and propene) and more than 20 are known environmental toxins causing acute toxic effects on exposure (including carbon monoxide, p-xylene, phenol, toluene, benzaldehyde, benzenedicarboxylic acid [phthalic acid], and long-chain and cyclic hydrocarbons).
During LHR, the portable condensation particle counters documented an eightfold increase, compared with the ambient room baseline level of ultrafine particle concentrations (ambient room baseline, 15,300 particles per cubic centimeter [ppc]; LHR with smoke evacuator, 129,376 ppc), even when a smoke evacuator was in close proximity (5.0 cm) to the procedure site. When the smoke evacuator was turned off for 30 seconds, there was a more than 26-fold increase in particulate count, compared with ambient baseline levels (ambient baseline, 15,300 ppc; LHR without smoke evacuator for 30 seconds, 435,888 ppc).
It has long been known that smoke created from electrocautery also may impose a risk on the health care worker. In 2011, Lewin et al. published a comprehensive review of the risk that surgical smoke and laser imposes on the dermatologist.2 At this time, most of the laser data was for the plume created by ablative CO2 lasers. In their review, it was stated that surgical smoke is composed of 95% water and 5% particulate matter (made up of chemicals, blood and tissue particles, viruses, and bacteria). The size of the particulate matter is dictated by the device used, with electrosurgical units creating particles of roughly 0.07 mcm and lasers liberating particles of 0.31 mcm. The size of liberated particles is important as those smaller than 100 mcm in diameter remain airborne, and particles less than 2 mcm are deposited in the bronchioles and alveoli.
Electrocautery plume is composed mostly of hydrocarbons, phenols, nitriles, and fatty acids, but most notably carbon monoxide, acrylonitrile, hydrogen cyanide, and benzene, which may have carcinogenic potential. On the mucosa of the canine tongue, the mutagenic effect of the smoke from 1 g of cauterized tissue with laser and electrocautery was equivalent to those from three or six cigarettes, respectively. Pulmonary changes also may occur. Blood vessel hypertrophy, alveolar congestion, and emphysematous changes were seen in rats after plume created from both electrocautery and Nd:Yag ablation of porcine skin. In that study, pulmonary changes were less severe in rats exposed to surgical smoke collected with single- and double-filtered smoke evacuators than unfiltered smoke.
Infection also poses a risk, with bovine papillomavirus and HPV detected in CO2 laser plume as early as 1988. In 1995, Gloster and Roenigk at the Mayo Clinic conducted a comparative study using questionnaires sent to members of the American Society for Laser Surgeons and the American Society of Dermatologic Surgery.3 The comparison groups were CO2 laser surgeons and two large groups of patients in the community with a diagnosis of warts. Analysis revealed that CO2 laser surgeons had a statistically significant greater risk of acquiring nasopharyngeal warts but were less likely to acquire plantar, genital, and perianal warts than the Mayo Clinic patient group did, demonstrating that laser plume is a likely means by which HPV can be transmitted to the upper airway, suggesting that those using lasers to treat HPV lesions are at greater risk. Staphylococcus, Corynebacterium, and Neisseria also have been detected during laser resurfacing.
Traditional surgical masks are able to capture particles greater than 5 mcm but offer no protection against particulate matter produced by electrosurgical and laser devices liberating byproducts less than 1 mcm. Laser masks or high-filtration masks provide greater protection than do standard surgical masks and are able to filter particles to 1.1 mcm; however, it has been shown that approximately 77% of particulate matter in surgical smoke is 1.1 mcm and smaller. Smoke evacuators consist of a suction unit (vacuum pump), filter, hose, and inlet nozzle. The smoke evacuator should have a capture velocity of approximately 30-45 m/min at the inlet nozzle. As the effectiveness of the smoke evacuator decreases with farther distance away from the procedure site, the current study of laser plume from LHR recommends that the smoke evacuator be placed within 5 cm of plume generation.4 In a study of warts treated with CO2 laser or electrocoagulation, smoke evacuators are 98.6% effective when placed 1 cm from the treatment site, with efficacy decreasing to 50% when moved to 2 cm from the treatment site.
As our specialty likely conducts the highest proportion of laser and electrosurgical procedures of any specialty, current recommendations for electrocautery, laser resurfacing, and LHR should include adequate air filtration and the use of high-filtration masks and smoke evacuators by the health care practitioner.
References
1. JAMA Dermatol. 2016 Jul 6. doi: 10.1001/jamadermatol.2016.2097. [Epub ahead of print]
2. J Am Acad Dermatol. 2011 Sep;65(3):636-41.
3. J Am Acad Dermatol. 1995 Mar;32(3):436-41.
4. J Am Acad Dermatol. 1989 Jul;21(1):41-9.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com.
A recent publication by Chuang et al. carefully characterizes the content of smoke (or plume) created from laser hair removal.1 At the University of California, Los Angeles, discarded terminal hairs from the trunk and extremities were collected from two adult volunteers. The hair samples were sealed in glass gas chromatography chambers and treated with either an 810-nm diode laser (Lightsheer, Lumenis) or 755-nm alexandrite laser (Gentlelase, Candela). During laser hair removal (LHR) treatment, two 6-L negative-pressure canisters were used to capture 30 seconds of laser plume, and a portable condensation particle counter was used to measure ultrafine particulates (less than 1 mcm). Ultrafine particle concentrations were measured within the treatment room, within the waiting room, and outside the building. The laser plume was then analyzed by gas chromatography–mass spectrometry (GC-MS) at the Boston University department of chemistry.
Analysis with GC-MS identified 377 chemical compounds. Sixty-two of the compounds exhibited strong absorption peaks, of which 13 are known or suspected carcinogens (including benzene, ethylbenzene, benzeneacetonitrile, acetonitrile, quinoline, isoquinoline, sterene, diethyl phthalate, 2-methylpyridine, naphthalene carbonitrile, and propene) and more than 20 are known environmental toxins causing acute toxic effects on exposure (including carbon monoxide, p-xylene, phenol, toluene, benzaldehyde, benzenedicarboxylic acid [phthalic acid], and long-chain and cyclic hydrocarbons).
During LHR, the portable condensation particle counters documented an eightfold increase, compared with the ambient room baseline level of ultrafine particle concentrations (ambient room baseline, 15,300 particles per cubic centimeter [ppc]; LHR with smoke evacuator, 129,376 ppc), even when a smoke evacuator was in close proximity (5.0 cm) to the procedure site. When the smoke evacuator was turned off for 30 seconds, there was a more than 26-fold increase in particulate count, compared with ambient baseline levels (ambient baseline, 15,300 ppc; LHR without smoke evacuator for 30 seconds, 435,888 ppc).
It has long been known that smoke created from electrocautery also may impose a risk on the health care worker. In 2011, Lewin et al. published a comprehensive review of the risk that surgical smoke and laser imposes on the dermatologist.2 At this time, most of the laser data was for the plume created by ablative CO2 lasers. In their review, it was stated that surgical smoke is composed of 95% water and 5% particulate matter (made up of chemicals, blood and tissue particles, viruses, and bacteria). The size of the particulate matter is dictated by the device used, with electrosurgical units creating particles of roughly 0.07 mcm and lasers liberating particles of 0.31 mcm. The size of liberated particles is important as those smaller than 100 mcm in diameter remain airborne, and particles less than 2 mcm are deposited in the bronchioles and alveoli.
Electrocautery plume is composed mostly of hydrocarbons, phenols, nitriles, and fatty acids, but most notably carbon monoxide, acrylonitrile, hydrogen cyanide, and benzene, which may have carcinogenic potential. On the mucosa of the canine tongue, the mutagenic effect of the smoke from 1 g of cauterized tissue with laser and electrocautery was equivalent to those from three or six cigarettes, respectively. Pulmonary changes also may occur. Blood vessel hypertrophy, alveolar congestion, and emphysematous changes were seen in rats after plume created from both electrocautery and Nd:Yag ablation of porcine skin. In that study, pulmonary changes were less severe in rats exposed to surgical smoke collected with single- and double-filtered smoke evacuators than unfiltered smoke.
Infection also poses a risk, with bovine papillomavirus and HPV detected in CO2 laser plume as early as 1988. In 1995, Gloster and Roenigk at the Mayo Clinic conducted a comparative study using questionnaires sent to members of the American Society for Laser Surgeons and the American Society of Dermatologic Surgery.3 The comparison groups were CO2 laser surgeons and two large groups of patients in the community with a diagnosis of warts. Analysis revealed that CO2 laser surgeons had a statistically significant greater risk of acquiring nasopharyngeal warts but were less likely to acquire plantar, genital, and perianal warts than the Mayo Clinic patient group did, demonstrating that laser plume is a likely means by which HPV can be transmitted to the upper airway, suggesting that those using lasers to treat HPV lesions are at greater risk. Staphylococcus, Corynebacterium, and Neisseria also have been detected during laser resurfacing.
Traditional surgical masks are able to capture particles greater than 5 mcm but offer no protection against particulate matter produced by electrosurgical and laser devices liberating byproducts less than 1 mcm. Laser masks or high-filtration masks provide greater protection than do standard surgical masks and are able to filter particles to 1.1 mcm; however, it has been shown that approximately 77% of particulate matter in surgical smoke is 1.1 mcm and smaller. Smoke evacuators consist of a suction unit (vacuum pump), filter, hose, and inlet nozzle. The smoke evacuator should have a capture velocity of approximately 30-45 m/min at the inlet nozzle. As the effectiveness of the smoke evacuator decreases with farther distance away from the procedure site, the current study of laser plume from LHR recommends that the smoke evacuator be placed within 5 cm of plume generation.4 In a study of warts treated with CO2 laser or electrocoagulation, smoke evacuators are 98.6% effective when placed 1 cm from the treatment site, with efficacy decreasing to 50% when moved to 2 cm from the treatment site.
As our specialty likely conducts the highest proportion of laser and electrosurgical procedures of any specialty, current recommendations for electrocautery, laser resurfacing, and LHR should include adequate air filtration and the use of high-filtration masks and smoke evacuators by the health care practitioner.
References
1. JAMA Dermatol. 2016 Jul 6. doi: 10.1001/jamadermatol.2016.2097. [Epub ahead of print]
2. J Am Acad Dermatol. 2011 Sep;65(3):636-41.
3. J Am Acad Dermatol. 1995 Mar;32(3):436-41.
4. J Am Acad Dermatol. 1989 Jul;21(1):41-9.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at dermnews@frontlinemedcom.com.