User login
VIDEO: Consider combining treatments when body sculpting
LAS VEGAS – Currently, there are available treatments that are effective in contouring the body, Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Some devices can help patients looking for reductions of trouble spots, such as around the abdomen, and are safe and effective, said Dr. Zachary of the University of California, Irvine. However, they are not a realistic option for obese or overweight patients, he added.
In addition, other treatments can be combined with body sculpting devices to optimize results, particularly when removing fat in the submental area, he noted.
Dr. Zachary disclosed relationships with Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Currently, there are available treatments that are effective in contouring the body, Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Some devices can help patients looking for reductions of trouble spots, such as around the abdomen, and are safe and effective, said Dr. Zachary of the University of California, Irvine. However, they are not a realistic option for obese or overweight patients, he added.
In addition, other treatments can be combined with body sculpting devices to optimize results, particularly when removing fat in the submental area, he noted.
Dr. Zachary disclosed relationships with Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Currently, there are available treatments that are effective in contouring the body, Christopher B. Zachary, MD, said in a video interview at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Some devices can help patients looking for reductions of trouble spots, such as around the abdomen, and are safe and effective, said Dr. Zachary of the University of California, Irvine. However, they are not a realistic option for obese or overweight patients, he added.
In addition, other treatments can be combined with body sculpting devices to optimize results, particularly when removing fat in the submental area, he noted.
Dr. Zachary disclosed relationships with Solta, Zeltiq, Sciton, DUSA, Zimmer, Cutera, Alma, and Amway.
SDEF and this news organization are owned by the same parent company.
AT SDEF LAS VEGAS DERMATOLOGY SEMINAR
Recommending efficacious cleansers for your patients
Cleansing is one of the most important steps in any skin care routine, but the surfeit of products on the market can lead to patients selecting an inappropriate cleanser for their skin type. This can engender various adverse cutaneous effects, including xerosis, flaking, acne, and flare-ups of chronic skin conditions such as eczema and rosacea. For example, acne medications are better tolerated when the proper cleanser is used. Cleanser choice is particularly important for individuals with dry skin who have an impaired barrier and those with sensitive skin who are susceptible to inflammation. The following discussion focuses on the factors that practitioners should address with patients when recommending cleansing products to help them maximize their outcomes and maintain clear, healthy-looking skin.
TYPES OF CLEANSERS
Foaming agents
Anionic surface acting agents (surfactants or detergents) produce foam and display the greatest cleansing potency. (Table 1). Because these detergents remove lipids from the skin’s surface and protective bilayer membrane barrier, they should only be used only by individuals with increased sebum production. Ingredients in this category injure the skin barrier and make the skin more susceptible to irritant reactions.1 For example, the widely used compound sodium lauryl sulfate (SLS), which strips lipids from the skin, irritates the skin to such an extent that it is used in research labs to hinder the skin barrier to test “barrier repair products.” The “sulfate- free” trend originates from the irritation caused by SLS. The barrier disruption caused by SLS can be used to intentionally damage the skin barrier to allow increased penetration of chemical peeling products and other therapeutic agents. An alternative to SLS is sodium laureth sulfate (or sodium lauryl ether sulfate, also known as SLES), which exhibits foaming attributes but is less likely than SLS to cause irritation. We often use a foaming cleanser in our practice prior to injectable procedures to ensure that makeup and debris are removed from the skin, and to decrease the time needed for topical lidocaine to penetrate into the skin. If you adopt this strategy, you should follow the injectable procedure with a barrier repair moisturizer.
Nonfoaming agents
These agents were developed through efforts to reduce detergent irritancy. This class of cleansers includes superfatted soaps, combination bars (“combars”), syndet bars (composed of synthetic surfactants) and compounds that deposit lipids on the skin, such as creams, lotions and oils. Cream, milk, cold creams, and oil cleansers fall into this category. These products usually have a neutral pH, and include ingredients such as alkyl glyceryl, ether sulfonate, alpha olefin sulfonates, betaines, sulfosuccinates, sodium cocoyl monoglyceride sulfate, and sodium cocoyl isethionate. Organic nonfoaming agents are also available, and may include saponins, a large family of structurally related compounds derived from plant, and sucrose laurate. Nonfoaming cleansers are most appropriate for dry skin types. Oily skin types often report that they “do not feel clean” when they use these cleansers.
Hydroxy acid cleansers
Alpha hydroxy acids (AHAs) are well suited for use by individuals with dry skin because hydroxy acids act as humectants (water-soluble materials with high water absorption capabilities). These hydrophilic cleansers provide exfoliation, and are appropriate for individuals with dry skin and acne because their low pH contributes to an inhospitable microbiome for Propionibacterium acnes, making it harder for the bacteria to thrive. Importantly, the exfoliating activity imparted by hydroxy acids sets the stage for better penetration into the stratum corneum by ingredients applied subsequent to the cleanser. Alpha hydroxy acid cleansers do not dry out the skin the way that salicylic acid cleansers do because their hydrophilic nature makes them unable to penetrate through sebum.
Salicylic acid (SA) cleansers are a member of the aspirin family and therefore confer anti-inflammatory properties. Salicylic acid is lipophilic and can penetrate through the sebum derived lipids into pores. They are the most effective cleansers to unclog pores. Therefore, SA cleansers are ideal for use by individuals with oily, sensitive skin prone to acne, seborrheic dermatitis, or rosacea. The exfoliation yielded by salicylic acid also enhances skin barrier penetration by ingredients applied after its use and is well tolerated by individuals with oily skin. Dry skin types, especially those on retinoids and benzoyl peroxide, will not tolerate SA as well as they will AHA cleansers.
Antibacterial cleansers
Antibacterial cleansers contain ingredients that reduce P. acnes and other types of bacteria on the skin. These products include benzoyl peroxide (BP), silver, hypochlorous acid, and sodium hypochlorite. Benzoyl peroxide can be highly irritating and is not well tolerated by patients with dry skin. Silver has a long history, having been used as an antibacterial agent since the times of King Herod. On the other hand, hypochlorous acid and sodium hypochlorite are novel entrants in the cleansing realm, particularly for individuals with acne. In fact, sodium hypochlorite is formulated to be mild enough for daily use while still sufficiently effective for acne-prone skin.
CLEANSER CHOICE BY SKIN ISSUE
Acne
Recommending the right cleanser for acne-prone skin first depends on whether the patient has oily or dry skin. Individuals with dry skin and acne cannot tolerate drying acne medications. Choosing the correct cleanser and moisturizer can help acne patients be more compliant with the acne treatment plan because of fewer side effects. Dry skin acne types often need two different cleansers. For the morning cleanser, AHA cleansers such as glycolic acid are effective at managing dry. acne-prone skin because glycolic acid has a relatively low pH. P. acnes is less likely to grow on skin with a lower pH.
Hydroxy acids help prevent clogged pores and exfoliate dead skin, which helps prevent acne comedones. Glycolic acid also serves as a humectant ingredient. Creamy cleansers should be used once daily, preferably at night for patients who use makeup since these products are effective at makeup removal. Foaming cleansers should never be used on dry, acne-prone skin. Individuals with the acne subtype of sensitive skin should avoid using scrubs, loofahs, and other forms of mechanical exfoliation.
Patients with oily skin and acne are easier to treat than are dry types because they can better tolerate acne medications. I recommend a salicylic acid cleanser in the morning to unclog pores. The anti-inflammatory properties of salicylic acid help prevent the formation of papules and pustules that characterize acne. Twice-daily use of salicylic acid by patients with oily skin and acne may feel too drying when combined with acne medications such as a retinoid and benzoyl peroxide. If this is the case, a foaming cleanser can be used in the evening to remove dirt, makeup, sunscreen, and debris that can clog pores and exacerbate acne.
Rosacea
Most dry skin type rosacea patients flush red when they wash their face, even if they only use water. The friction alone is enough to cause them to react. Rosacea patients can skip the morning cleanse to help reduce this skin irritation and flushing. Instead they should apply their a.m. anti-redness products followed by a sunscreen appropriate for their skin type. In the evening, a soothing, nonfoaming cleanser with anti-inflammatory ingredients is the best choice to remove makeup, sunscreen, and any built-up dirt or bacteria from the skin’s surface. This should be followed by an anti-redness product that targets the inflammation caused by rosacea.
Anti-inflammatory ingredients that can be found in soothing cleansers and moisturizers for rosacea prone skin include argan oil, green tea, feverfew, chamomile, licorice extract, and aloe.
Patients with very oily skin who have rosacea need to cleanse twice daily to remove excess oil to prevent comedones and acne lesions. A foaming cleanser that contains anti-inflammatory ingredients such as green tea, feverfew, licorice extract, aloe, niacinamide, green tea, and salicylic acid are a good choice for oily rosacea prone skin types.
All rosacea patients should be counseled to avoid mechanical exfoliation, including cleansing scrubs, chemical exfoliants, and abrasive loofahs or cloths.
Eczema
Patients with eczema should choose the same nonfoaming cleansers recommended for dry skin. For patients with frequent skin infections, hypochlorite and silver are beneficial ingredients found in cleansers to help decrease skin bacteria and prevent infections. Foaming cleansers should never be used in eczema prone types.
Conclusion
Cleansers play an important role in skin care because they affect the skin barrier, pH of the skin, presence of bacteria, condition of the pores, and penetration of the post cleanser–applied ingredients. Knowing which cleansing product to use based on a patient’s skin type is critical to recommending the proper ingredients so that patients can achieve and maintain healthy skin.
Table 1. Ingredients used in foaming cleansers
Acyl glycinates
Acylglutamates
Alkyl acyl isethionates
Alkyl carboxylates
Alkyl ether sulfates
Alkyl ethoxy sulfates
Alkyl phosphates
Alkyl sulfates
Alkyl sulfonates
Alkyl sulfosuccinates
Alkyl taurates
Reference
Cleansing is one of the most important steps in any skin care routine, but the surfeit of products on the market can lead to patients selecting an inappropriate cleanser for their skin type. This can engender various adverse cutaneous effects, including xerosis, flaking, acne, and flare-ups of chronic skin conditions such as eczema and rosacea. For example, acne medications are better tolerated when the proper cleanser is used. Cleanser choice is particularly important for individuals with dry skin who have an impaired barrier and those with sensitive skin who are susceptible to inflammation. The following discussion focuses on the factors that practitioners should address with patients when recommending cleansing products to help them maximize their outcomes and maintain clear, healthy-looking skin.
TYPES OF CLEANSERS
Foaming agents
Anionic surface acting agents (surfactants or detergents) produce foam and display the greatest cleansing potency. (Table 1). Because these detergents remove lipids from the skin’s surface and protective bilayer membrane barrier, they should only be used only by individuals with increased sebum production. Ingredients in this category injure the skin barrier and make the skin more susceptible to irritant reactions.1 For example, the widely used compound sodium lauryl sulfate (SLS), which strips lipids from the skin, irritates the skin to such an extent that it is used in research labs to hinder the skin barrier to test “barrier repair products.” The “sulfate- free” trend originates from the irritation caused by SLS. The barrier disruption caused by SLS can be used to intentionally damage the skin barrier to allow increased penetration of chemical peeling products and other therapeutic agents. An alternative to SLS is sodium laureth sulfate (or sodium lauryl ether sulfate, also known as SLES), which exhibits foaming attributes but is less likely than SLS to cause irritation. We often use a foaming cleanser in our practice prior to injectable procedures to ensure that makeup and debris are removed from the skin, and to decrease the time needed for topical lidocaine to penetrate into the skin. If you adopt this strategy, you should follow the injectable procedure with a barrier repair moisturizer.
Nonfoaming agents
These agents were developed through efforts to reduce detergent irritancy. This class of cleansers includes superfatted soaps, combination bars (“combars”), syndet bars (composed of synthetic surfactants) and compounds that deposit lipids on the skin, such as creams, lotions and oils. Cream, milk, cold creams, and oil cleansers fall into this category. These products usually have a neutral pH, and include ingredients such as alkyl glyceryl, ether sulfonate, alpha olefin sulfonates, betaines, sulfosuccinates, sodium cocoyl monoglyceride sulfate, and sodium cocoyl isethionate. Organic nonfoaming agents are also available, and may include saponins, a large family of structurally related compounds derived from plant, and sucrose laurate. Nonfoaming cleansers are most appropriate for dry skin types. Oily skin types often report that they “do not feel clean” when they use these cleansers.
Hydroxy acid cleansers
Alpha hydroxy acids (AHAs) are well suited for use by individuals with dry skin because hydroxy acids act as humectants (water-soluble materials with high water absorption capabilities). These hydrophilic cleansers provide exfoliation, and are appropriate for individuals with dry skin and acne because their low pH contributes to an inhospitable microbiome for Propionibacterium acnes, making it harder for the bacteria to thrive. Importantly, the exfoliating activity imparted by hydroxy acids sets the stage for better penetration into the stratum corneum by ingredients applied subsequent to the cleanser. Alpha hydroxy acid cleansers do not dry out the skin the way that salicylic acid cleansers do because their hydrophilic nature makes them unable to penetrate through sebum.
Salicylic acid (SA) cleansers are a member of the aspirin family and therefore confer anti-inflammatory properties. Salicylic acid is lipophilic and can penetrate through the sebum derived lipids into pores. They are the most effective cleansers to unclog pores. Therefore, SA cleansers are ideal for use by individuals with oily, sensitive skin prone to acne, seborrheic dermatitis, or rosacea. The exfoliation yielded by salicylic acid also enhances skin barrier penetration by ingredients applied after its use and is well tolerated by individuals with oily skin. Dry skin types, especially those on retinoids and benzoyl peroxide, will not tolerate SA as well as they will AHA cleansers.
Antibacterial cleansers
Antibacterial cleansers contain ingredients that reduce P. acnes and other types of bacteria on the skin. These products include benzoyl peroxide (BP), silver, hypochlorous acid, and sodium hypochlorite. Benzoyl peroxide can be highly irritating and is not well tolerated by patients with dry skin. Silver has a long history, having been used as an antibacterial agent since the times of King Herod. On the other hand, hypochlorous acid and sodium hypochlorite are novel entrants in the cleansing realm, particularly for individuals with acne. In fact, sodium hypochlorite is formulated to be mild enough for daily use while still sufficiently effective for acne-prone skin.
CLEANSER CHOICE BY SKIN ISSUE
Acne
Recommending the right cleanser for acne-prone skin first depends on whether the patient has oily or dry skin. Individuals with dry skin and acne cannot tolerate drying acne medications. Choosing the correct cleanser and moisturizer can help acne patients be more compliant with the acne treatment plan because of fewer side effects. Dry skin acne types often need two different cleansers. For the morning cleanser, AHA cleansers such as glycolic acid are effective at managing dry. acne-prone skin because glycolic acid has a relatively low pH. P. acnes is less likely to grow on skin with a lower pH.
Hydroxy acids help prevent clogged pores and exfoliate dead skin, which helps prevent acne comedones. Glycolic acid also serves as a humectant ingredient. Creamy cleansers should be used once daily, preferably at night for patients who use makeup since these products are effective at makeup removal. Foaming cleansers should never be used on dry, acne-prone skin. Individuals with the acne subtype of sensitive skin should avoid using scrubs, loofahs, and other forms of mechanical exfoliation.
Patients with oily skin and acne are easier to treat than are dry types because they can better tolerate acne medications. I recommend a salicylic acid cleanser in the morning to unclog pores. The anti-inflammatory properties of salicylic acid help prevent the formation of papules and pustules that characterize acne. Twice-daily use of salicylic acid by patients with oily skin and acne may feel too drying when combined with acne medications such as a retinoid and benzoyl peroxide. If this is the case, a foaming cleanser can be used in the evening to remove dirt, makeup, sunscreen, and debris that can clog pores and exacerbate acne.
Rosacea
Most dry skin type rosacea patients flush red when they wash their face, even if they only use water. The friction alone is enough to cause them to react. Rosacea patients can skip the morning cleanse to help reduce this skin irritation and flushing. Instead they should apply their a.m. anti-redness products followed by a sunscreen appropriate for their skin type. In the evening, a soothing, nonfoaming cleanser with anti-inflammatory ingredients is the best choice to remove makeup, sunscreen, and any built-up dirt or bacteria from the skin’s surface. This should be followed by an anti-redness product that targets the inflammation caused by rosacea.
Anti-inflammatory ingredients that can be found in soothing cleansers and moisturizers for rosacea prone skin include argan oil, green tea, feverfew, chamomile, licorice extract, and aloe.
Patients with very oily skin who have rosacea need to cleanse twice daily to remove excess oil to prevent comedones and acne lesions. A foaming cleanser that contains anti-inflammatory ingredients such as green tea, feverfew, licorice extract, aloe, niacinamide, green tea, and salicylic acid are a good choice for oily rosacea prone skin types.
All rosacea patients should be counseled to avoid mechanical exfoliation, including cleansing scrubs, chemical exfoliants, and abrasive loofahs or cloths.
Eczema
Patients with eczema should choose the same nonfoaming cleansers recommended for dry skin. For patients with frequent skin infections, hypochlorite and silver are beneficial ingredients found in cleansers to help decrease skin bacteria and prevent infections. Foaming cleansers should never be used in eczema prone types.
Conclusion
Cleansers play an important role in skin care because they affect the skin barrier, pH of the skin, presence of bacteria, condition of the pores, and penetration of the post cleanser–applied ingredients. Knowing which cleansing product to use based on a patient’s skin type is critical to recommending the proper ingredients so that patients can achieve and maintain healthy skin.
Table 1. Ingredients used in foaming cleansers
Acyl glycinates
Acylglutamates
Alkyl acyl isethionates
Alkyl carboxylates
Alkyl ether sulfates
Alkyl ethoxy sulfates
Alkyl phosphates
Alkyl sulfates
Alkyl sulfonates
Alkyl sulfosuccinates
Alkyl taurates
Reference
Cleansing is one of the most important steps in any skin care routine, but the surfeit of products on the market can lead to patients selecting an inappropriate cleanser for their skin type. This can engender various adverse cutaneous effects, including xerosis, flaking, acne, and flare-ups of chronic skin conditions such as eczema and rosacea. For example, acne medications are better tolerated when the proper cleanser is used. Cleanser choice is particularly important for individuals with dry skin who have an impaired barrier and those with sensitive skin who are susceptible to inflammation. The following discussion focuses on the factors that practitioners should address with patients when recommending cleansing products to help them maximize their outcomes and maintain clear, healthy-looking skin.
TYPES OF CLEANSERS
Foaming agents
Anionic surface acting agents (surfactants or detergents) produce foam and display the greatest cleansing potency. (Table 1). Because these detergents remove lipids from the skin’s surface and protective bilayer membrane barrier, they should only be used only by individuals with increased sebum production. Ingredients in this category injure the skin barrier and make the skin more susceptible to irritant reactions.1 For example, the widely used compound sodium lauryl sulfate (SLS), which strips lipids from the skin, irritates the skin to such an extent that it is used in research labs to hinder the skin barrier to test “barrier repair products.” The “sulfate- free” trend originates from the irritation caused by SLS. The barrier disruption caused by SLS can be used to intentionally damage the skin barrier to allow increased penetration of chemical peeling products and other therapeutic agents. An alternative to SLS is sodium laureth sulfate (or sodium lauryl ether sulfate, also known as SLES), which exhibits foaming attributes but is less likely than SLS to cause irritation. We often use a foaming cleanser in our practice prior to injectable procedures to ensure that makeup and debris are removed from the skin, and to decrease the time needed for topical lidocaine to penetrate into the skin. If you adopt this strategy, you should follow the injectable procedure with a barrier repair moisturizer.
Nonfoaming agents
These agents were developed through efforts to reduce detergent irritancy. This class of cleansers includes superfatted soaps, combination bars (“combars”), syndet bars (composed of synthetic surfactants) and compounds that deposit lipids on the skin, such as creams, lotions and oils. Cream, milk, cold creams, and oil cleansers fall into this category. These products usually have a neutral pH, and include ingredients such as alkyl glyceryl, ether sulfonate, alpha olefin sulfonates, betaines, sulfosuccinates, sodium cocoyl monoglyceride sulfate, and sodium cocoyl isethionate. Organic nonfoaming agents are also available, and may include saponins, a large family of structurally related compounds derived from plant, and sucrose laurate. Nonfoaming cleansers are most appropriate for dry skin types. Oily skin types often report that they “do not feel clean” when they use these cleansers.
Hydroxy acid cleansers
Alpha hydroxy acids (AHAs) are well suited for use by individuals with dry skin because hydroxy acids act as humectants (water-soluble materials with high water absorption capabilities). These hydrophilic cleansers provide exfoliation, and are appropriate for individuals with dry skin and acne because their low pH contributes to an inhospitable microbiome for Propionibacterium acnes, making it harder for the bacteria to thrive. Importantly, the exfoliating activity imparted by hydroxy acids sets the stage for better penetration into the stratum corneum by ingredients applied subsequent to the cleanser. Alpha hydroxy acid cleansers do not dry out the skin the way that salicylic acid cleansers do because their hydrophilic nature makes them unable to penetrate through sebum.
Salicylic acid (SA) cleansers are a member of the aspirin family and therefore confer anti-inflammatory properties. Salicylic acid is lipophilic and can penetrate through the sebum derived lipids into pores. They are the most effective cleansers to unclog pores. Therefore, SA cleansers are ideal for use by individuals with oily, sensitive skin prone to acne, seborrheic dermatitis, or rosacea. The exfoliation yielded by salicylic acid also enhances skin barrier penetration by ingredients applied after its use and is well tolerated by individuals with oily skin. Dry skin types, especially those on retinoids and benzoyl peroxide, will not tolerate SA as well as they will AHA cleansers.
Antibacterial cleansers
Antibacterial cleansers contain ingredients that reduce P. acnes and other types of bacteria on the skin. These products include benzoyl peroxide (BP), silver, hypochlorous acid, and sodium hypochlorite. Benzoyl peroxide can be highly irritating and is not well tolerated by patients with dry skin. Silver has a long history, having been used as an antibacterial agent since the times of King Herod. On the other hand, hypochlorous acid and sodium hypochlorite are novel entrants in the cleansing realm, particularly for individuals with acne. In fact, sodium hypochlorite is formulated to be mild enough for daily use while still sufficiently effective for acne-prone skin.
CLEANSER CHOICE BY SKIN ISSUE
Acne
Recommending the right cleanser for acne-prone skin first depends on whether the patient has oily or dry skin. Individuals with dry skin and acne cannot tolerate drying acne medications. Choosing the correct cleanser and moisturizer can help acne patients be more compliant with the acne treatment plan because of fewer side effects. Dry skin acne types often need two different cleansers. For the morning cleanser, AHA cleansers such as glycolic acid are effective at managing dry. acne-prone skin because glycolic acid has a relatively low pH. P. acnes is less likely to grow on skin with a lower pH.
Hydroxy acids help prevent clogged pores and exfoliate dead skin, which helps prevent acne comedones. Glycolic acid also serves as a humectant ingredient. Creamy cleansers should be used once daily, preferably at night for patients who use makeup since these products are effective at makeup removal. Foaming cleansers should never be used on dry, acne-prone skin. Individuals with the acne subtype of sensitive skin should avoid using scrubs, loofahs, and other forms of mechanical exfoliation.
Patients with oily skin and acne are easier to treat than are dry types because they can better tolerate acne medications. I recommend a salicylic acid cleanser in the morning to unclog pores. The anti-inflammatory properties of salicylic acid help prevent the formation of papules and pustules that characterize acne. Twice-daily use of salicylic acid by patients with oily skin and acne may feel too drying when combined with acne medications such as a retinoid and benzoyl peroxide. If this is the case, a foaming cleanser can be used in the evening to remove dirt, makeup, sunscreen, and debris that can clog pores and exacerbate acne.
Rosacea
Most dry skin type rosacea patients flush red when they wash their face, even if they only use water. The friction alone is enough to cause them to react. Rosacea patients can skip the morning cleanse to help reduce this skin irritation and flushing. Instead they should apply their a.m. anti-redness products followed by a sunscreen appropriate for their skin type. In the evening, a soothing, nonfoaming cleanser with anti-inflammatory ingredients is the best choice to remove makeup, sunscreen, and any built-up dirt or bacteria from the skin’s surface. This should be followed by an anti-redness product that targets the inflammation caused by rosacea.
Anti-inflammatory ingredients that can be found in soothing cleansers and moisturizers for rosacea prone skin include argan oil, green tea, feverfew, chamomile, licorice extract, and aloe.
Patients with very oily skin who have rosacea need to cleanse twice daily to remove excess oil to prevent comedones and acne lesions. A foaming cleanser that contains anti-inflammatory ingredients such as green tea, feverfew, licorice extract, aloe, niacinamide, green tea, and salicylic acid are a good choice for oily rosacea prone skin types.
All rosacea patients should be counseled to avoid mechanical exfoliation, including cleansing scrubs, chemical exfoliants, and abrasive loofahs or cloths.
Eczema
Patients with eczema should choose the same nonfoaming cleansers recommended for dry skin. For patients with frequent skin infections, hypochlorite and silver are beneficial ingredients found in cleansers to help decrease skin bacteria and prevent infections. Foaming cleansers should never be used in eczema prone types.
Conclusion
Cleansers play an important role in skin care because they affect the skin barrier, pH of the skin, presence of bacteria, condition of the pores, and penetration of the post cleanser–applied ingredients. Knowing which cleansing product to use based on a patient’s skin type is critical to recommending the proper ingredients so that patients can achieve and maintain healthy skin.
Table 1. Ingredients used in foaming cleansers
Acyl glycinates
Acylglutamates
Alkyl acyl isethionates
Alkyl carboxylates
Alkyl ether sulfates
Alkyl ethoxy sulfates
Alkyl phosphates
Alkyl sulfates
Alkyl sulfonates
Alkyl sulfosuccinates
Alkyl taurates
Reference
Expert Panel: Little support for delaying cosmetic procedures after isotretinoin
In most cases, there is little evidence to support delaying cosmetic procedures, such as laser therapy or chemical peels, in patients who have recently been treated with isotretinoin for acne, according to a consensus statement from the American Society of Dermatologic Surgery (ASDS).
An expert panel convened by the ASDS issued specific recommendations that supported safe, early initiation of cosmetic procedures in most cases. It noted that the likelihood of any potential harms from initiating cosmetic procedures after recent isotretinoin treatment is “low to very low” and that such harms have been reported only in case reports and case series.
Notable exceptions included dermabrasion and full-face ablative resurfacing; the experts recommended against having such procedures within 6 months of isotretinoin use because of potentially increased risks of adverse events in some patients.
“Potential benefits of this guideline include early access to scar treatments for many patients who are at the highest risk for scarring and, thereby, potentially improved patient quality of life,” Abigail Waldman, MD, of the department of dermatology at Brigham and Women’s Hospital, Boston, and her coauthors wrote in the consensus statement (Dermatol Surg. 2017 Oct;43[10]:1249-62). This is the first consensus statement document published by the ASDS to address this topic.
Isotretinoin was approved by the Food and Drug Administration in 1982 for treating severe and nodulocystic acne. Because of a perceived higher risk of scarring or irritation associated with isotretinoin use, standard clinical practice has been to avoid performing laser procedures, chemical peels, waxing, dermabrasion, and incisional or excisional cutaneous surgeries on patients within 6 months of their using isotretinoin, according to the authors. A warning regarding the potential for scarring with cosmetic procedures meant to smooth the skin is even included in the patient information leaflet for isotretinoin.
“This is in contradistinction to the observation that nodulocystic or severe inflammatory acne patients who have recently completed treatment with isotretinoin are among those most likely to benefit from treatment of their acne scars with modalities such as laser, dermabrasion, or chemical peels,” the experts wrote in the consensus recommendations.
Following a review of the 36 source documents, the task force concluded that, for patients currently or recently receiving isotretinoin, evidence was “insufficient” to justify delaying treatment with superficial chemical peels, vascular lasers, and nonablative modalities, such as hair removal lasers and lights. They also stated that superficial and focal dermabrasion “may also be safe when performed by a well-trained clinician” in a clinical setting.
The panel recommendations covered the following four key areas:
- Dermabrasion. Treating specific facial areas while the patient is on isotretinoin or within 6 months of discontinuation “is not associated with increased risk of scar or delay in wound healing, and there is no evidence in the literature that supports a need to delay treatment,” they wrote. In contrast, they did not recommend full-face or mechanical dermabrasion with rotary devices within the 6-month window because it may be “associated with increased risk of adverse events in selected patients.”
- Lasers and energy devices. Similarly, the panel found no evidence that would justify delaying use of vascular lasers, hair removal lasers and lights, and nonablative or ablative fractional devices among patients recently treated with isotretinoin. However, they said fully ablative treatment of the entire face or regions other than the face should “generally be avoided until 6 months after completion of isotretinoin treatment because of the likely elevated risk of avoidable adverse events.”
- Chemical peels. Patients currently on isotretinoin or who have recently discontinued it can safely undergo superficial chemical peels, according to the panel. For medium or deep chemical peels, there was “insufficient data … to preclude a recommendation in this case,” the panel wrote.
- Other surgeries. Because of the risk of dry eyes, isotretinoin should be discontinued prior to laser eye surgery. For incisional and excisional cutaneous surgery, the data on isotretinoin were insufficient to make any recommendations, the experts concluded, though they acknowledged that in some cases, the surgeries may be “medically necessary.”
Most of these recommendations were based on case series and cohort studies, the panel said, rather than higher-quality, randomized clinical trials, which are “generally impractical and not likely forthcoming in this setting.” Moreover, they cautioned that insufficient evidence to make a recommendation should not be misconstrued as a confirmation of safety or a warning about risk.
Overall, the results of the analysis suggested that “procedural interventions during or soon after isotretinoin treatment can safely and effectively address acne scarring and similar disorders, thus providing relief to patients without the need for protracted waiting,” the authors wrote.
In August, another expert panel’s recommendations were published, which concluded that skin procedures, including superficial chemical peels, laser hair removal, minor cutaneous surgery, manual dermabrasion, and fractional ablative and fractional nonablative laser procedures, can be performed safely on patients who have recently been or are currently being treated with isotretinoin (JAMA Dermatol. 2017 Aug 1;153[8]:802-9).
The authors of the ASDS statement reported no relevant financial conflicts.
In most cases, there is little evidence to support delaying cosmetic procedures, such as laser therapy or chemical peels, in patients who have recently been treated with isotretinoin for acne, according to a consensus statement from the American Society of Dermatologic Surgery (ASDS).
An expert panel convened by the ASDS issued specific recommendations that supported safe, early initiation of cosmetic procedures in most cases. It noted that the likelihood of any potential harms from initiating cosmetic procedures after recent isotretinoin treatment is “low to very low” and that such harms have been reported only in case reports and case series.
Notable exceptions included dermabrasion and full-face ablative resurfacing; the experts recommended against having such procedures within 6 months of isotretinoin use because of potentially increased risks of adverse events in some patients.
“Potential benefits of this guideline include early access to scar treatments for many patients who are at the highest risk for scarring and, thereby, potentially improved patient quality of life,” Abigail Waldman, MD, of the department of dermatology at Brigham and Women’s Hospital, Boston, and her coauthors wrote in the consensus statement (Dermatol Surg. 2017 Oct;43[10]:1249-62). This is the first consensus statement document published by the ASDS to address this topic.
Isotretinoin was approved by the Food and Drug Administration in 1982 for treating severe and nodulocystic acne. Because of a perceived higher risk of scarring or irritation associated with isotretinoin use, standard clinical practice has been to avoid performing laser procedures, chemical peels, waxing, dermabrasion, and incisional or excisional cutaneous surgeries on patients within 6 months of their using isotretinoin, according to the authors. A warning regarding the potential for scarring with cosmetic procedures meant to smooth the skin is even included in the patient information leaflet for isotretinoin.
“This is in contradistinction to the observation that nodulocystic or severe inflammatory acne patients who have recently completed treatment with isotretinoin are among those most likely to benefit from treatment of their acne scars with modalities such as laser, dermabrasion, or chemical peels,” the experts wrote in the consensus recommendations.
Following a review of the 36 source documents, the task force concluded that, for patients currently or recently receiving isotretinoin, evidence was “insufficient” to justify delaying treatment with superficial chemical peels, vascular lasers, and nonablative modalities, such as hair removal lasers and lights. They also stated that superficial and focal dermabrasion “may also be safe when performed by a well-trained clinician” in a clinical setting.
The panel recommendations covered the following four key areas:
- Dermabrasion. Treating specific facial areas while the patient is on isotretinoin or within 6 months of discontinuation “is not associated with increased risk of scar or delay in wound healing, and there is no evidence in the literature that supports a need to delay treatment,” they wrote. In contrast, they did not recommend full-face or mechanical dermabrasion with rotary devices within the 6-month window because it may be “associated with increased risk of adverse events in selected patients.”
- Lasers and energy devices. Similarly, the panel found no evidence that would justify delaying use of vascular lasers, hair removal lasers and lights, and nonablative or ablative fractional devices among patients recently treated with isotretinoin. However, they said fully ablative treatment of the entire face or regions other than the face should “generally be avoided until 6 months after completion of isotretinoin treatment because of the likely elevated risk of avoidable adverse events.”
- Chemical peels. Patients currently on isotretinoin or who have recently discontinued it can safely undergo superficial chemical peels, according to the panel. For medium or deep chemical peels, there was “insufficient data … to preclude a recommendation in this case,” the panel wrote.
- Other surgeries. Because of the risk of dry eyes, isotretinoin should be discontinued prior to laser eye surgery. For incisional and excisional cutaneous surgery, the data on isotretinoin were insufficient to make any recommendations, the experts concluded, though they acknowledged that in some cases, the surgeries may be “medically necessary.”
Most of these recommendations were based on case series and cohort studies, the panel said, rather than higher-quality, randomized clinical trials, which are “generally impractical and not likely forthcoming in this setting.” Moreover, they cautioned that insufficient evidence to make a recommendation should not be misconstrued as a confirmation of safety or a warning about risk.
Overall, the results of the analysis suggested that “procedural interventions during or soon after isotretinoin treatment can safely and effectively address acne scarring and similar disorders, thus providing relief to patients without the need for protracted waiting,” the authors wrote.
In August, another expert panel’s recommendations were published, which concluded that skin procedures, including superficial chemical peels, laser hair removal, minor cutaneous surgery, manual dermabrasion, and fractional ablative and fractional nonablative laser procedures, can be performed safely on patients who have recently been or are currently being treated with isotretinoin (JAMA Dermatol. 2017 Aug 1;153[8]:802-9).
The authors of the ASDS statement reported no relevant financial conflicts.
In most cases, there is little evidence to support delaying cosmetic procedures, such as laser therapy or chemical peels, in patients who have recently been treated with isotretinoin for acne, according to a consensus statement from the American Society of Dermatologic Surgery (ASDS).
An expert panel convened by the ASDS issued specific recommendations that supported safe, early initiation of cosmetic procedures in most cases. It noted that the likelihood of any potential harms from initiating cosmetic procedures after recent isotretinoin treatment is “low to very low” and that such harms have been reported only in case reports and case series.
Notable exceptions included dermabrasion and full-face ablative resurfacing; the experts recommended against having such procedures within 6 months of isotretinoin use because of potentially increased risks of adverse events in some patients.
“Potential benefits of this guideline include early access to scar treatments for many patients who are at the highest risk for scarring and, thereby, potentially improved patient quality of life,” Abigail Waldman, MD, of the department of dermatology at Brigham and Women’s Hospital, Boston, and her coauthors wrote in the consensus statement (Dermatol Surg. 2017 Oct;43[10]:1249-62). This is the first consensus statement document published by the ASDS to address this topic.
Isotretinoin was approved by the Food and Drug Administration in 1982 for treating severe and nodulocystic acne. Because of a perceived higher risk of scarring or irritation associated with isotretinoin use, standard clinical practice has been to avoid performing laser procedures, chemical peels, waxing, dermabrasion, and incisional or excisional cutaneous surgeries on patients within 6 months of their using isotretinoin, according to the authors. A warning regarding the potential for scarring with cosmetic procedures meant to smooth the skin is even included in the patient information leaflet for isotretinoin.
“This is in contradistinction to the observation that nodulocystic or severe inflammatory acne patients who have recently completed treatment with isotretinoin are among those most likely to benefit from treatment of their acne scars with modalities such as laser, dermabrasion, or chemical peels,” the experts wrote in the consensus recommendations.
Following a review of the 36 source documents, the task force concluded that, for patients currently or recently receiving isotretinoin, evidence was “insufficient” to justify delaying treatment with superficial chemical peels, vascular lasers, and nonablative modalities, such as hair removal lasers and lights. They also stated that superficial and focal dermabrasion “may also be safe when performed by a well-trained clinician” in a clinical setting.
The panel recommendations covered the following four key areas:
- Dermabrasion. Treating specific facial areas while the patient is on isotretinoin or within 6 months of discontinuation “is not associated with increased risk of scar or delay in wound healing, and there is no evidence in the literature that supports a need to delay treatment,” they wrote. In contrast, they did not recommend full-face or mechanical dermabrasion with rotary devices within the 6-month window because it may be “associated with increased risk of adverse events in selected patients.”
- Lasers and energy devices. Similarly, the panel found no evidence that would justify delaying use of vascular lasers, hair removal lasers and lights, and nonablative or ablative fractional devices among patients recently treated with isotretinoin. However, they said fully ablative treatment of the entire face or regions other than the face should “generally be avoided until 6 months after completion of isotretinoin treatment because of the likely elevated risk of avoidable adverse events.”
- Chemical peels. Patients currently on isotretinoin or who have recently discontinued it can safely undergo superficial chemical peels, according to the panel. For medium or deep chemical peels, there was “insufficient data … to preclude a recommendation in this case,” the panel wrote.
- Other surgeries. Because of the risk of dry eyes, isotretinoin should be discontinued prior to laser eye surgery. For incisional and excisional cutaneous surgery, the data on isotretinoin were insufficient to make any recommendations, the experts concluded, though they acknowledged that in some cases, the surgeries may be “medically necessary.”
Most of these recommendations were based on case series and cohort studies, the panel said, rather than higher-quality, randomized clinical trials, which are “generally impractical and not likely forthcoming in this setting.” Moreover, they cautioned that insufficient evidence to make a recommendation should not be misconstrued as a confirmation of safety or a warning about risk.
Overall, the results of the analysis suggested that “procedural interventions during or soon after isotretinoin treatment can safely and effectively address acne scarring and similar disorders, thus providing relief to patients without the need for protracted waiting,” the authors wrote.
In August, another expert panel’s recommendations were published, which concluded that skin procedures, including superficial chemical peels, laser hair removal, minor cutaneous surgery, manual dermabrasion, and fractional ablative and fractional nonablative laser procedures, can be performed safely on patients who have recently been or are currently being treated with isotretinoin (JAMA Dermatol. 2017 Aug 1;153[8]:802-9).
The authors of the ASDS statement reported no relevant financial conflicts.
FROM DERMATOLOGIC SURGERY
Key clinical point: Contrary to current recommendations,
Major finding: Experts convened by the American Society of Dermatologic Surgery found that, in most cases, the likelihood of potential harms of initiating cosmetic procedures after recent isotretinoin use is “low to very low,” and those that did occur were reported only in case reports and case series rather than in higher-quality clinical trials.
Data source: A consensus review of 36 source documents obtained by a literature review, the results of which were then validated by peer review.
Disclosures: The authors reported no relevant financial conflicts.
Benefits of topical product evaluated in patients undergoing laser treatment
The use of a combination product applied to treated areas before and after laser treatment of the face or decollete appeared to improve healing, compared with standard care, in a split-face study of 10 patients undergoing fractional CO2 laser treatment of the face and decollete.
The results were presented in a poster at the Summit in Aesthetic Medicine held by Global Academy for Medical Education. The product, manufactured by Alastin Skincare, is a topical formulation designed for use before and after laser therapy.
Before and after treatment, patients in the trial were given the topical treatment on one side of their faces or decollete and a standard treatment on the other, according to the poster.
Based on the blinded investigator ratings, the sides treated with the new product scored higher on day 4 for lentigines (P = .009), texture (P = .043), and Global Skin Quality (P = .051), according to Deanne Robinson, MD, director of the body sculpting center at the Connecticut Dermatology Group and the author of the study.
In addition, patients said they were more satisfied with the side treated with the product in terms of looking better and feeling better on that side (P = .05).
Dr. Robinson reported no financial conflicts. Global Academy and this news organization are owned the same company.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
The use of a combination product applied to treated areas before and after laser treatment of the face or decollete appeared to improve healing, compared with standard care, in a split-face study of 10 patients undergoing fractional CO2 laser treatment of the face and decollete.
The results were presented in a poster at the Summit in Aesthetic Medicine held by Global Academy for Medical Education. The product, manufactured by Alastin Skincare, is a topical formulation designed for use before and after laser therapy.
Before and after treatment, patients in the trial were given the topical treatment on one side of their faces or decollete and a standard treatment on the other, according to the poster.
Based on the blinded investigator ratings, the sides treated with the new product scored higher on day 4 for lentigines (P = .009), texture (P = .043), and Global Skin Quality (P = .051), according to Deanne Robinson, MD, director of the body sculpting center at the Connecticut Dermatology Group and the author of the study.
In addition, patients said they were more satisfied with the side treated with the product in terms of looking better and feeling better on that side (P = .05).
Dr. Robinson reported no financial conflicts. Global Academy and this news organization are owned the same company.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
The use of a combination product applied to treated areas before and after laser treatment of the face or decollete appeared to improve healing, compared with standard care, in a split-face study of 10 patients undergoing fractional CO2 laser treatment of the face and decollete.
The results were presented in a poster at the Summit in Aesthetic Medicine held by Global Academy for Medical Education. The product, manufactured by Alastin Skincare, is a topical formulation designed for use before and after laser therapy.
Before and after treatment, patients in the trial were given the topical treatment on one side of their faces or decollete and a standard treatment on the other, according to the poster.
Based on the blinded investigator ratings, the sides treated with the new product scored higher on day 4 for lentigines (P = .009), texture (P = .043), and Global Skin Quality (P = .051), according to Deanne Robinson, MD, director of the body sculpting center at the Connecticut Dermatology Group and the author of the study.
In addition, patients said they were more satisfied with the side treated with the product in terms of looking better and feeling better on that side (P = .05).
Dr. Robinson reported no financial conflicts. Global Academy and this news organization are owned the same company.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
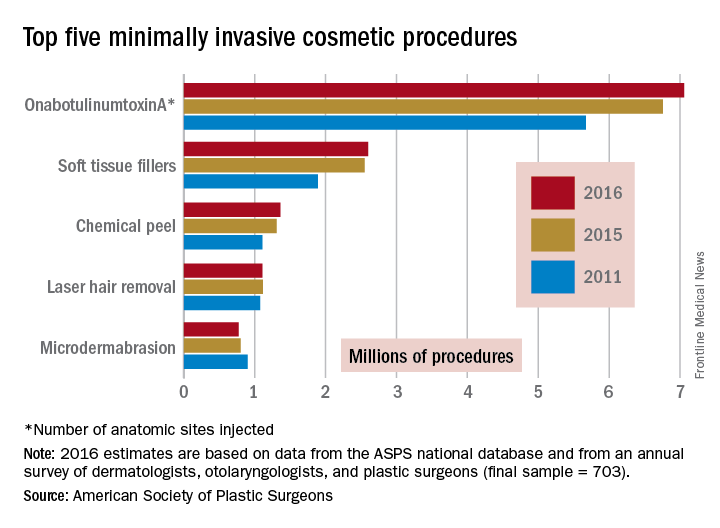
Minimally invasive cosmetic procedures more popular than ever
The total number of minimally invasive cosmetic procedures topped 15 million for the first time in 2016, with onabotulinumtoxinA injections leading the way, according to the American Society of Plastic Surgeons.
An estimated 15.4 million minimally invasive cosmetic procedures were performed last year, with onabotulinumtoxinA making up over 45% – approximately 7.1 million anatomic sites injected – of that total, ASPS data show.
Next in popularity was injection of soft tissue fillers, with just over 2.6 million procedures – almost 17% of the procedures performed in 2016 – followed by chemical peels with almost 1.4 million procedures, laser hair removal with 1.1 million procedures, and microdermabrasion at 775,000, the ASPS reported.
The total number of minimally invasive procedures was up 3% from the 14.96 million performed in 2015, while onabotulinumtoxinA was up 4%, soft tissue fillers were up 2%, chemical peels were up 4%, laser hair removal was down 1%, and microdermabrasion was down 3%. Larger changes were seen among some less common procedures: injection lipolysis was up 18% (55,660 procedures in 2016), fat injection was up 13% (79,208 procedures in 2016), and acellular dermal matrix procedures were down 18% (7,809 in 2016), according to the ASPS Tracking Operations and Outcomes for Plastic Surgeons database and an annual survey of board-certified dermatologists, otolaryngologists, and plastic surgeons (final sample = 703).
The total number of minimally invasive cosmetic procedures topped 15 million for the first time in 2016, with onabotulinumtoxinA injections leading the way, according to the American Society of Plastic Surgeons.
An estimated 15.4 million minimally invasive cosmetic procedures were performed last year, with onabotulinumtoxinA making up over 45% – approximately 7.1 million anatomic sites injected – of that total, ASPS data show.
Next in popularity was injection of soft tissue fillers, with just over 2.6 million procedures – almost 17% of the procedures performed in 2016 – followed by chemical peels with almost 1.4 million procedures, laser hair removal with 1.1 million procedures, and microdermabrasion at 775,000, the ASPS reported.
The total number of minimally invasive procedures was up 3% from the 14.96 million performed in 2015, while onabotulinumtoxinA was up 4%, soft tissue fillers were up 2%, chemical peels were up 4%, laser hair removal was down 1%, and microdermabrasion was down 3%. Larger changes were seen among some less common procedures: injection lipolysis was up 18% (55,660 procedures in 2016), fat injection was up 13% (79,208 procedures in 2016), and acellular dermal matrix procedures were down 18% (7,809 in 2016), according to the ASPS Tracking Operations and Outcomes for Plastic Surgeons database and an annual survey of board-certified dermatologists, otolaryngologists, and plastic surgeons (final sample = 703).
The total number of minimally invasive cosmetic procedures topped 15 million for the first time in 2016, with onabotulinumtoxinA injections leading the way, according to the American Society of Plastic Surgeons.
An estimated 15.4 million minimally invasive cosmetic procedures were performed last year, with onabotulinumtoxinA making up over 45% – approximately 7.1 million anatomic sites injected – of that total, ASPS data show.
Next in popularity was injection of soft tissue fillers, with just over 2.6 million procedures – almost 17% of the procedures performed in 2016 – followed by chemical peels with almost 1.4 million procedures, laser hair removal with 1.1 million procedures, and microdermabrasion at 775,000, the ASPS reported.
The total number of minimally invasive procedures was up 3% from the 14.96 million performed in 2015, while onabotulinumtoxinA was up 4%, soft tissue fillers were up 2%, chemical peels were up 4%, laser hair removal was down 1%, and microdermabrasion was down 3%. Larger changes were seen among some less common procedures: injection lipolysis was up 18% (55,660 procedures in 2016), fat injection was up 13% (79,208 procedures in 2016), and acellular dermal matrix procedures were down 18% (7,809 in 2016), according to the ASPS Tracking Operations and Outcomes for Plastic Surgeons database and an annual survey of board-certified dermatologists, otolaryngologists, and plastic surgeons (final sample = 703).
VIDEO: Picowave laser uses are expanding beyond tattoo removal
ORLANDO – The applications for picowavelength lasers are expanding, with emerging data on their uses for cosmetic indications other than tattoo removal, according to Anne Chapas, MD, who is in private practice in New York.
First introduced and cleared by the Food and Drug Administration for tattoo removal, “picowave devices ... are now being studied in multiple different cosmetic conditions, including their use in acne scars, fine lines and wrinkles, and melasma,” Dr. Chapas said in a video interview at the annual meeting of the American Academy of Dermatology.
The No. 1 thing dermatologists need to know is that these types of lasers are delivering energy extremely quickly,” at 1,000 times faster than nanosecond lasers, she said. Another difference between the two is that “the laser tissue interaction between the two types of devices is completely different.”
In the interview, she highlighted other important points about picowave lasers, including less downtime after treatment.
At the meeting, Dr. Chapas spoke during a session entitled “the Science Behind New Devices in Dermatology.”
Her disclosures include serving as a consultant and investigator for Syneron and Candela.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The applications for picowavelength lasers are expanding, with emerging data on their uses for cosmetic indications other than tattoo removal, according to Anne Chapas, MD, who is in private practice in New York.
First introduced and cleared by the Food and Drug Administration for tattoo removal, “picowave devices ... are now being studied in multiple different cosmetic conditions, including their use in acne scars, fine lines and wrinkles, and melasma,” Dr. Chapas said in a video interview at the annual meeting of the American Academy of Dermatology.
The No. 1 thing dermatologists need to know is that these types of lasers are delivering energy extremely quickly,” at 1,000 times faster than nanosecond lasers, she said. Another difference between the two is that “the laser tissue interaction between the two types of devices is completely different.”
In the interview, she highlighted other important points about picowave lasers, including less downtime after treatment.
At the meeting, Dr. Chapas spoke during a session entitled “the Science Behind New Devices in Dermatology.”
Her disclosures include serving as a consultant and investigator for Syneron and Candela.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – The applications for picowavelength lasers are expanding, with emerging data on their uses for cosmetic indications other than tattoo removal, according to Anne Chapas, MD, who is in private practice in New York.
First introduced and cleared by the Food and Drug Administration for tattoo removal, “picowave devices ... are now being studied in multiple different cosmetic conditions, including their use in acne scars, fine lines and wrinkles, and melasma,” Dr. Chapas said in a video interview at the annual meeting of the American Academy of Dermatology.
The No. 1 thing dermatologists need to know is that these types of lasers are delivering energy extremely quickly,” at 1,000 times faster than nanosecond lasers, she said. Another difference between the two is that “the laser tissue interaction between the two types of devices is completely different.”
In the interview, she highlighted other important points about picowave lasers, including less downtime after treatment.
At the meeting, Dr. Chapas spoke during a session entitled “the Science Behind New Devices in Dermatology.”
Her disclosures include serving as a consultant and investigator for Syneron and Candela.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT AAD 17
Lasers for Latino skin – A balance of gentleness and strength
ORLANDO – With its unique tendency to develop postinflammatory hyperpigmentation (PIH), Latino skin needs a gentle touch from powerful lasers, according to Eduardo Weiss, MD.
“It’s often best to use a lower power, even though you trade off some efficacy for safety,” said Dr. Weiss, a dermatologist in Miami. “In general, it’s better to go with less aggressive treatment and more sessions, than to risk getting too aggressive and having a bad outcome.”
Dr. Weiss stressed that there are no “one size fits all” recommendations about laser treatment in typical Latino skin, because there’s no such thing as typical Latino skin. The group comprises all Fitzpatrick phototypes. But, in general, he said, the darker the skin, the greater the chance of an acute laser-induced burn, postinflammatory hyperpigmentation, and scarring.
Although general skin tone can provide a good first guess about the potential for hyperreaction to lasers, Dr. Weiss bolsters his judgments with a very simple – but effective – screen: palmar and digital crease pigmentation. First suggested by Hector G. Leal-Silva, MD, of the Institute of Dermatology and Cosmetic Surgery, Monterrey, Mexico, the screen divides patients into four groups, depending on the concentration of pigment present in palmar creases. A score of 0 means no pigment is visible, and the risk of PIH is negligible; a score of 3 means the creases are highly pigmented, and that the risk of PIH is very high.
But, with some adjustments in delivery – including using longer wavelengths and pulse duration, lower fluence and density, and smaller spot sizes – lasers can be used safely and effectively in these at-risk patients, Dr. Weiss said.
Safe treatment starts with pretreatment. It’s best to avoid laser procedures during the summer, when skin is at its darkest. Dr. Weiss also recommends a 6-week regimen aimed at lightening the area to be treated. This can include:
- Sun avoidance and the regular use of a high SPF sunscreen.
- Hydroquinone 4%-8%.
- A “Miami peel,” which is a modified Jessner’s peel with kojic acid and hydroquinone.
- Kligman’s formula of hydroquinone, tretinoin, and a corticosteroid.
- Heliocare, an oral extract of the Polypodium leucotomos fern.
About a month before the procedure, he performs a test spot with the intended laser and its planned settings, in the preauricular area. Any PIH will be obvious within 2-4 weeks. He also carefully screens patients or any photosensitizing condition, like lupus or herpes simplex, or a history of any photosensitizing drugs, such as tetracycline.
Dr. Weiss made specific suggestions for laser treatment of some common Latino skin issues:
Pigmented lesions
The high density of epidermal melanin in Fitzpatrick types IV-VI acts as a competitive chromophore against hemoglobin and oxyhemoglobin. This makes it quite challenging to treat vascular lesions such as port wine stains and telangiectasias, he said. The pulsed dye laser is a good choice, with wavelengths of 585-590 nm especially effective. “The longer 595-nm wavelength allows for a slightly deeper penetration,” Dr. Weiss said. “However, the absorption coefficient of oxyhemoglobin is three times higher at 585 nm than [at] 590 nm.”
Longer pulses are generally safer in dark-skinned patients, he noted. “It will be much less effective than the 585, but for darker-skinned patients, we must sacrifice a little efficacy for safety.”
For rosacea and telangiectasias, Dr. Weiss suggests a 515-nm intense pulsed light with pulse duration of 12-15/ms for these lesions, or pigmentation, he also uses 540 nm or 500-600 nm with pulse duration of 12-15/ms.
Melasma, a very common condition in dark-skinned Latinos, is also “one of the most difficult and frustrating conditions to manage,” he pointed out. He turns to a laser only when the case is resistant to more conservative treatment, which typically includes Kligman’s formula, sunscreen, light peels, and azelaic or kojic acid.
“Lasers are still controversial and, in my opinion, a last resort for melasma. I wouldn’t start unless everything else fails. I reserve them for the deep nonresponding melasmas.”
The Q-switched Nd:YAG is the most widely used for melasma. The fluence used is less than 5 J/cm2, with a 6-mm spot size and a frequency of 10 Hz. The number of treatment sessions varies from 5 to 10 at 1-week intervals, Dr. Weiss said. “Keep in mind that rebound hyperpigmentation could be due to the multiple subthreshold exposures that can stimulate melanogenesis in some areas.”
Skin rejuvenation
Ablative lasers – long the gold standard for skin rejuvenation in those with light skin – can be problematic for darker-skinned patients, Dr. Weiss said.
“These lasers, like the CO2 and Erbium:YAG, can cause several unwanted side effects in Latino skin.” These can include hyperpigmentation, which occurs in 50% of Fitzpatrick III or higher phototypes; erythema that can last for months; and delayed-onset hypopigmentation.
“I think better options for our darker-skinned patients are nonablative infrared, microneedling, and radiofrequency devices,” Dr. Weiss said. “There are, however, newer microablative resurfacing lasers. Fractional CO2, fractional Erbium, and the 2,790-nm yttrium scandium gallium garnet, offer a safer modality with which to treat skin types IV and above. Compared with the older-generation resurfacing lasers, the microablative lasers minimize the amount and duration of erythema and edema, which can last just 3-4 days.”
Dr. Weiss had no relevant financial disclosures.
ORLANDO – With its unique tendency to develop postinflammatory hyperpigmentation (PIH), Latino skin needs a gentle touch from powerful lasers, according to Eduardo Weiss, MD.
“It’s often best to use a lower power, even though you trade off some efficacy for safety,” said Dr. Weiss, a dermatologist in Miami. “In general, it’s better to go with less aggressive treatment and more sessions, than to risk getting too aggressive and having a bad outcome.”
Dr. Weiss stressed that there are no “one size fits all” recommendations about laser treatment in typical Latino skin, because there’s no such thing as typical Latino skin. The group comprises all Fitzpatrick phototypes. But, in general, he said, the darker the skin, the greater the chance of an acute laser-induced burn, postinflammatory hyperpigmentation, and scarring.
Although general skin tone can provide a good first guess about the potential for hyperreaction to lasers, Dr. Weiss bolsters his judgments with a very simple – but effective – screen: palmar and digital crease pigmentation. First suggested by Hector G. Leal-Silva, MD, of the Institute of Dermatology and Cosmetic Surgery, Monterrey, Mexico, the screen divides patients into four groups, depending on the concentration of pigment present in palmar creases. A score of 0 means no pigment is visible, and the risk of PIH is negligible; a score of 3 means the creases are highly pigmented, and that the risk of PIH is very high.
But, with some adjustments in delivery – including using longer wavelengths and pulse duration, lower fluence and density, and smaller spot sizes – lasers can be used safely and effectively in these at-risk patients, Dr. Weiss said.
Safe treatment starts with pretreatment. It’s best to avoid laser procedures during the summer, when skin is at its darkest. Dr. Weiss also recommends a 6-week regimen aimed at lightening the area to be treated. This can include:
- Sun avoidance and the regular use of a high SPF sunscreen.
- Hydroquinone 4%-8%.
- A “Miami peel,” which is a modified Jessner’s peel with kojic acid and hydroquinone.
- Kligman’s formula of hydroquinone, tretinoin, and a corticosteroid.
- Heliocare, an oral extract of the Polypodium leucotomos fern.
About a month before the procedure, he performs a test spot with the intended laser and its planned settings, in the preauricular area. Any PIH will be obvious within 2-4 weeks. He also carefully screens patients or any photosensitizing condition, like lupus or herpes simplex, or a history of any photosensitizing drugs, such as tetracycline.
Dr. Weiss made specific suggestions for laser treatment of some common Latino skin issues:
Pigmented lesions
The high density of epidermal melanin in Fitzpatrick types IV-VI acts as a competitive chromophore against hemoglobin and oxyhemoglobin. This makes it quite challenging to treat vascular lesions such as port wine stains and telangiectasias, he said. The pulsed dye laser is a good choice, with wavelengths of 585-590 nm especially effective. “The longer 595-nm wavelength allows for a slightly deeper penetration,” Dr. Weiss said. “However, the absorption coefficient of oxyhemoglobin is three times higher at 585 nm than [at] 590 nm.”
Longer pulses are generally safer in dark-skinned patients, he noted. “It will be much less effective than the 585, but for darker-skinned patients, we must sacrifice a little efficacy for safety.”
For rosacea and telangiectasias, Dr. Weiss suggests a 515-nm intense pulsed light with pulse duration of 12-15/ms for these lesions, or pigmentation, he also uses 540 nm or 500-600 nm with pulse duration of 12-15/ms.
Melasma, a very common condition in dark-skinned Latinos, is also “one of the most difficult and frustrating conditions to manage,” he pointed out. He turns to a laser only when the case is resistant to more conservative treatment, which typically includes Kligman’s formula, sunscreen, light peels, and azelaic or kojic acid.
“Lasers are still controversial and, in my opinion, a last resort for melasma. I wouldn’t start unless everything else fails. I reserve them for the deep nonresponding melasmas.”
The Q-switched Nd:YAG is the most widely used for melasma. The fluence used is less than 5 J/cm2, with a 6-mm spot size and a frequency of 10 Hz. The number of treatment sessions varies from 5 to 10 at 1-week intervals, Dr. Weiss said. “Keep in mind that rebound hyperpigmentation could be due to the multiple subthreshold exposures that can stimulate melanogenesis in some areas.”
Skin rejuvenation
Ablative lasers – long the gold standard for skin rejuvenation in those with light skin – can be problematic for darker-skinned patients, Dr. Weiss said.
“These lasers, like the CO2 and Erbium:YAG, can cause several unwanted side effects in Latino skin.” These can include hyperpigmentation, which occurs in 50% of Fitzpatrick III or higher phototypes; erythema that can last for months; and delayed-onset hypopigmentation.
“I think better options for our darker-skinned patients are nonablative infrared, microneedling, and radiofrequency devices,” Dr. Weiss said. “There are, however, newer microablative resurfacing lasers. Fractional CO2, fractional Erbium, and the 2,790-nm yttrium scandium gallium garnet, offer a safer modality with which to treat skin types IV and above. Compared with the older-generation resurfacing lasers, the microablative lasers minimize the amount and duration of erythema and edema, which can last just 3-4 days.”
Dr. Weiss had no relevant financial disclosures.
ORLANDO – With its unique tendency to develop postinflammatory hyperpigmentation (PIH), Latino skin needs a gentle touch from powerful lasers, according to Eduardo Weiss, MD.
“It’s often best to use a lower power, even though you trade off some efficacy for safety,” said Dr. Weiss, a dermatologist in Miami. “In general, it’s better to go with less aggressive treatment and more sessions, than to risk getting too aggressive and having a bad outcome.”
Dr. Weiss stressed that there are no “one size fits all” recommendations about laser treatment in typical Latino skin, because there’s no such thing as typical Latino skin. The group comprises all Fitzpatrick phototypes. But, in general, he said, the darker the skin, the greater the chance of an acute laser-induced burn, postinflammatory hyperpigmentation, and scarring.
Although general skin tone can provide a good first guess about the potential for hyperreaction to lasers, Dr. Weiss bolsters his judgments with a very simple – but effective – screen: palmar and digital crease pigmentation. First suggested by Hector G. Leal-Silva, MD, of the Institute of Dermatology and Cosmetic Surgery, Monterrey, Mexico, the screen divides patients into four groups, depending on the concentration of pigment present in palmar creases. A score of 0 means no pigment is visible, and the risk of PIH is negligible; a score of 3 means the creases are highly pigmented, and that the risk of PIH is very high.
But, with some adjustments in delivery – including using longer wavelengths and pulse duration, lower fluence and density, and smaller spot sizes – lasers can be used safely and effectively in these at-risk patients, Dr. Weiss said.
Safe treatment starts with pretreatment. It’s best to avoid laser procedures during the summer, when skin is at its darkest. Dr. Weiss also recommends a 6-week regimen aimed at lightening the area to be treated. This can include:
- Sun avoidance and the regular use of a high SPF sunscreen.
- Hydroquinone 4%-8%.
- A “Miami peel,” which is a modified Jessner’s peel with kojic acid and hydroquinone.
- Kligman’s formula of hydroquinone, tretinoin, and a corticosteroid.
- Heliocare, an oral extract of the Polypodium leucotomos fern.
About a month before the procedure, he performs a test spot with the intended laser and its planned settings, in the preauricular area. Any PIH will be obvious within 2-4 weeks. He also carefully screens patients or any photosensitizing condition, like lupus or herpes simplex, or a history of any photosensitizing drugs, such as tetracycline.
Dr. Weiss made specific suggestions for laser treatment of some common Latino skin issues:
Pigmented lesions
The high density of epidermal melanin in Fitzpatrick types IV-VI acts as a competitive chromophore against hemoglobin and oxyhemoglobin. This makes it quite challenging to treat vascular lesions such as port wine stains and telangiectasias, he said. The pulsed dye laser is a good choice, with wavelengths of 585-590 nm especially effective. “The longer 595-nm wavelength allows for a slightly deeper penetration,” Dr. Weiss said. “However, the absorption coefficient of oxyhemoglobin is three times higher at 585 nm than [at] 590 nm.”
Longer pulses are generally safer in dark-skinned patients, he noted. “It will be much less effective than the 585, but for darker-skinned patients, we must sacrifice a little efficacy for safety.”
For rosacea and telangiectasias, Dr. Weiss suggests a 515-nm intense pulsed light with pulse duration of 12-15/ms for these lesions, or pigmentation, he also uses 540 nm or 500-600 nm with pulse duration of 12-15/ms.
Melasma, a very common condition in dark-skinned Latinos, is also “one of the most difficult and frustrating conditions to manage,” he pointed out. He turns to a laser only when the case is resistant to more conservative treatment, which typically includes Kligman’s formula, sunscreen, light peels, and azelaic or kojic acid.
“Lasers are still controversial and, in my opinion, a last resort for melasma. I wouldn’t start unless everything else fails. I reserve them for the deep nonresponding melasmas.”
The Q-switched Nd:YAG is the most widely used for melasma. The fluence used is less than 5 J/cm2, with a 6-mm spot size and a frequency of 10 Hz. The number of treatment sessions varies from 5 to 10 at 1-week intervals, Dr. Weiss said. “Keep in mind that rebound hyperpigmentation could be due to the multiple subthreshold exposures that can stimulate melanogenesis in some areas.”
Skin rejuvenation
Ablative lasers – long the gold standard for skin rejuvenation in those with light skin – can be problematic for darker-skinned patients, Dr. Weiss said.
“These lasers, like the CO2 and Erbium:YAG, can cause several unwanted side effects in Latino skin.” These can include hyperpigmentation, which occurs in 50% of Fitzpatrick III or higher phototypes; erythema that can last for months; and delayed-onset hypopigmentation.
“I think better options for our darker-skinned patients are nonablative infrared, microneedling, and radiofrequency devices,” Dr. Weiss said. “There are, however, newer microablative resurfacing lasers. Fractional CO2, fractional Erbium, and the 2,790-nm yttrium scandium gallium garnet, offer a safer modality with which to treat skin types IV and above. Compared with the older-generation resurfacing lasers, the microablative lasers minimize the amount and duration of erythema and edema, which can last just 3-4 days.”
Dr. Weiss had no relevant financial disclosures.
EXPERT ANALYSIS FROM AAD 17
VIDEO: Advances in noninvasive fat reduction include permanent effects
WAILEA, HAWAII – In the past few years, there have been “exciting” advances in noninvasive techniques to permanently remove fat, according to Suzanne Kilmer, MD, of the department of dermatology, University of California, Davis.
There are devices now available to reduce fat “in a permanent way that’s not injurious, it’s not uncomfortable – patients love it,” Dr. Kilmer said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Currently, the three noninvasive modalities she considers most effective for reducing fat are cryolipolysis, the 1,060-nm laser, and focused pulsed ultrasound. In the interview, she discussed the ways these treatments work and their safety.
With all three, “the fat that goes away stays away,” said Dr. Kilmer, who is director of the Laser and Skin Surgery Center of Northern California, Sacramento. Treatment results in release of fat, which is “cleared like it is as if you ate a cheeseburger,” she added. Interestingly, she said, trials that have looked at whether the fat reduction is accompanied by weight loss have found that, in most cases, the patient’s weight remains stable.
Dr. Kilmer’s disclosures included serving as a consultant and/or researcher for Allergan, Cutera, Cynosure, Cytrellis, Kythera, Lumenis, Merz, Miramar, Sebacia, Sienna Labs, Solta, Zeltiq, and Zift.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – In the past few years, there have been “exciting” advances in noninvasive techniques to permanently remove fat, according to Suzanne Kilmer, MD, of the department of dermatology, University of California, Davis.
There are devices now available to reduce fat “in a permanent way that’s not injurious, it’s not uncomfortable – patients love it,” Dr. Kilmer said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Currently, the three noninvasive modalities she considers most effective for reducing fat are cryolipolysis, the 1,060-nm laser, and focused pulsed ultrasound. In the interview, she discussed the ways these treatments work and their safety.
With all three, “the fat that goes away stays away,” said Dr. Kilmer, who is director of the Laser and Skin Surgery Center of Northern California, Sacramento. Treatment results in release of fat, which is “cleared like it is as if you ate a cheeseburger,” she added. Interestingly, she said, trials that have looked at whether the fat reduction is accompanied by weight loss have found that, in most cases, the patient’s weight remains stable.
Dr. Kilmer’s disclosures included serving as a consultant and/or researcher for Allergan, Cutera, Cynosure, Cytrellis, Kythera, Lumenis, Merz, Miramar, Sebacia, Sienna Labs, Solta, Zeltiq, and Zift.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WAILEA, HAWAII – In the past few years, there have been “exciting” advances in noninvasive techniques to permanently remove fat, according to Suzanne Kilmer, MD, of the department of dermatology, University of California, Davis.
There are devices now available to reduce fat “in a permanent way that’s not injurious, it’s not uncomfortable – patients love it,” Dr. Kilmer said in a video interview at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Currently, the three noninvasive modalities she considers most effective for reducing fat are cryolipolysis, the 1,060-nm laser, and focused pulsed ultrasound. In the interview, she discussed the ways these treatments work and their safety.
With all three, “the fat that goes away stays away,” said Dr. Kilmer, who is director of the Laser and Skin Surgery Center of Northern California, Sacramento. Treatment results in release of fat, which is “cleared like it is as if you ate a cheeseburger,” she added. Interestingly, she said, trials that have looked at whether the fat reduction is accompanied by weight loss have found that, in most cases, the patient’s weight remains stable.
Dr. Kilmer’s disclosures included serving as a consultant and/or researcher for Allergan, Cutera, Cynosure, Cytrellis, Kythera, Lumenis, Merz, Miramar, Sebacia, Sienna Labs, Solta, Zeltiq, and Zift.
SDEF and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Consider plumes from laser hair removal a biohazard
The plume of burning hair occurring during laser hair removal should be considered a biohazard, reported Gary S. Chuang, MD, of Harvard Medical School, Boston and his coauthors.
Use of smoke evacuators, good ventilation, and respiratory protection are warranted, especially for health care workers exposed to the plume for extended periods, they said.
While the laser was treating the hair, the particle counters recorded a eightfold increase in ultrafine-particle concentrations, compared with ambient room baseline; this occurred even with a smoke evacuator within 5 cm of the procedure site. When a smoke evacuator was turned off for 30 seconds, the increase was 26-fold, Dr. Chuang and his associates reported.
Read more at JAMA Dermatology (2016;152[12]:1320-6).
The plume of burning hair occurring during laser hair removal should be considered a biohazard, reported Gary S. Chuang, MD, of Harvard Medical School, Boston and his coauthors.
Use of smoke evacuators, good ventilation, and respiratory protection are warranted, especially for health care workers exposed to the plume for extended periods, they said.
While the laser was treating the hair, the particle counters recorded a eightfold increase in ultrafine-particle concentrations, compared with ambient room baseline; this occurred even with a smoke evacuator within 5 cm of the procedure site. When a smoke evacuator was turned off for 30 seconds, the increase was 26-fold, Dr. Chuang and his associates reported.
Read more at JAMA Dermatology (2016;152[12]:1320-6).
The plume of burning hair occurring during laser hair removal should be considered a biohazard, reported Gary S. Chuang, MD, of Harvard Medical School, Boston and his coauthors.
Use of smoke evacuators, good ventilation, and respiratory protection are warranted, especially for health care workers exposed to the plume for extended periods, they said.
While the laser was treating the hair, the particle counters recorded a eightfold increase in ultrafine-particle concentrations, compared with ambient room baseline; this occurred even with a smoke evacuator within 5 cm of the procedure site. When a smoke evacuator was turned off for 30 seconds, the increase was 26-fold, Dr. Chuang and his associates reported.
Read more at JAMA Dermatology (2016;152[12]:1320-6).
FROM JAMA DERMATOLOGY
Picosecond alexandrite laser with lens modification effective for wrinkles
reported Robert A. Weiss, MD, of the MD Laser and Vein Institute, Baltimore, and his associates.
In a prospective, blinded study of perioral and periocular wrinkles in 40 healthy women (average age 58 years) who were nonsmokers, a 6-mm spot size diffractive lens array delivered a fluence of 0.71 J/cm2 at each focal point using 10-Hz pulse repetition at a pulse duration of 750 picoseconds. During each treatment, four passes of the 755-nm alexandrite laser (Picosure) for a total of 5,000 pulses were delivered. At 6 months follow-up, the mean Fitzpatrick wrinkle score had improved to 3.47 from the baseline average of 5.48 (P less than .05), with an overall average change in score of 1.97. Adverse events were mild, and all resolved, most within 24 hours (Lasers Surg Med. 2017 Jan;49[1]:40-44).
At 1 and 6 months, physician satisfaction ratings were 97.4% and 89.5% (extremely satisfied or satisfied), respectively. At 1 month, 42.1% of the patients were extremely satisfied, and 47.4% were satisfied. At 6 months, 42.1% were extremely likely to recommend the treatment, and 44.7% were likely to recommend the treatment.
The picosecond 755-nm alexandrite laser has been reported to be effective for tattoo removal, compared with the nanosecond domain lasers, they noted.
Dr. Weiss and a coauthor are consultants, researchers, and speakers for Cynosure, manufacturer of PicoSure. The other authors had no financial disclosures.
reported Robert A. Weiss, MD, of the MD Laser and Vein Institute, Baltimore, and his associates.
In a prospective, blinded study of perioral and periocular wrinkles in 40 healthy women (average age 58 years) who were nonsmokers, a 6-mm spot size diffractive lens array delivered a fluence of 0.71 J/cm2 at each focal point using 10-Hz pulse repetition at a pulse duration of 750 picoseconds. During each treatment, four passes of the 755-nm alexandrite laser (Picosure) for a total of 5,000 pulses were delivered. At 6 months follow-up, the mean Fitzpatrick wrinkle score had improved to 3.47 from the baseline average of 5.48 (P less than .05), with an overall average change in score of 1.97. Adverse events were mild, and all resolved, most within 24 hours (Lasers Surg Med. 2017 Jan;49[1]:40-44).
At 1 and 6 months, physician satisfaction ratings were 97.4% and 89.5% (extremely satisfied or satisfied), respectively. At 1 month, 42.1% of the patients were extremely satisfied, and 47.4% were satisfied. At 6 months, 42.1% were extremely likely to recommend the treatment, and 44.7% were likely to recommend the treatment.
The picosecond 755-nm alexandrite laser has been reported to be effective for tattoo removal, compared with the nanosecond domain lasers, they noted.
Dr. Weiss and a coauthor are consultants, researchers, and speakers for Cynosure, manufacturer of PicoSure. The other authors had no financial disclosures.
reported Robert A. Weiss, MD, of the MD Laser and Vein Institute, Baltimore, and his associates.
In a prospective, blinded study of perioral and periocular wrinkles in 40 healthy women (average age 58 years) who were nonsmokers, a 6-mm spot size diffractive lens array delivered a fluence of 0.71 J/cm2 at each focal point using 10-Hz pulse repetition at a pulse duration of 750 picoseconds. During each treatment, four passes of the 755-nm alexandrite laser (Picosure) for a total of 5,000 pulses were delivered. At 6 months follow-up, the mean Fitzpatrick wrinkle score had improved to 3.47 from the baseline average of 5.48 (P less than .05), with an overall average change in score of 1.97. Adverse events were mild, and all resolved, most within 24 hours (Lasers Surg Med. 2017 Jan;49[1]:40-44).
At 1 and 6 months, physician satisfaction ratings were 97.4% and 89.5% (extremely satisfied or satisfied), respectively. At 1 month, 42.1% of the patients were extremely satisfied, and 47.4% were satisfied. At 6 months, 42.1% were extremely likely to recommend the treatment, and 44.7% were likely to recommend the treatment.
The picosecond 755-nm alexandrite laser has been reported to be effective for tattoo removal, compared with the nanosecond domain lasers, they noted.
Dr. Weiss and a coauthor are consultants, researchers, and speakers for Cynosure, manufacturer of PicoSure. The other authors had no financial disclosures.
FROM LASERS IN SURGERY AND MEDICINE