User login
Nurturing Sustainability in a Growing Community Pediatric Hospital Medicine Workforce
Systematic efforts to measure and compare work hours emerged in the 19th century as laborers shifted from artisanal shops to factories, sparking debate over the appropriate length and intensity of work.1 Two centuries of unionization and regulation defined work hours for many United States employees, including graduate medical trainees, but left attending physicians largely untouched. Instead, the medical workforce has long relied on survey data to shape jobs that balance professional norms with local market demands. Leaders in young, dynamic specialties, such as pediatric hospital medicine (PHM), particularly require such data to recruit and retain talent.
PHM progressed swiftly from acknowledgment as a “distinct area of practice” in 1999 to a subspecialty recognition.2 Currently, at least 3,000 pediatric hospitalists3 practice in more than 800 US sites (Snow C, Personal communication regarding community PHM workforce survey). Approximately half of them work at community hospitals, where PHM groups often comprise fewer than five full-time equivalents (FTEs) and face unique challenges. Community PHM practices may assume broader responsibilities than university/children’s hospital colleagues, including advocacy for the needs of children in predominantly adult-oriented hospitals.4 Although data regarding academic PHM work demands are available,5 there is little information pertaining to community hospitalists regarding typical workloads or other characteristics of thriving practices.
In this issue of the Journal of Hospital Medicine, Alvarez et al. present the findings of structured interviews with 70 community PHM group leaders.6 Each participant answered 12 questions about their group, addressing the definition of a full-time workload and hours, the design of backup systems, and the respondent’s perception of the program’s sustainability. The sample is robust, with the caveats that it disproportionately represents the Midwest and West (34.3% each) and more than half of the groups were employed by an academic institution. The authors found a median work expectation per FTE of 1,882 hours/year and 21 weekends per year, although they noted significant variability in employers’ demands and services provided. The majority of hospitalist groups lacked census caps, formal backup systems, or processes to expand coverage during busy seasons. Among the site leaders, 63% perceived their program as sustainable, but no program design or employer characteristic was clearly associated with this perception.
The importance of this study derives from aggregating data about the largest cross section of community PHM groups yet reported. For many PHM group leaders, this will offer a new point of reference for key practice characteristics. Furthermore, the authors should be commended for attempting to distinguish how program sustainability manifests in community PHM, where hospitalists shoulder longer patient care hours and many of them sustain academic endeavors. It is concerning that more than a third of leaders do not perceive their program as sustainable, but the implications for the field are unclear. Perhaps part of this uncertainty arises from the terminology, as sustainability lacks a technical or a consensus definition and the authors purposefully did not define the term for the respondents. While many respondents probably worried about physician burnout, others might have channeled fears about group finances or competition with adult service lines for beds. In addition, leaders’ fears about sustainability may not exactly represent the concerns of front-line employees.
Sustainable work environments are complex constructs with several inputs. For example, supportive leaders, efficient delivery systems, optimized EHRs, competitive pay, and confidence about service line stability might all mitigate higher workloads. Ultimately, this complexity underscores an important caution about all workplace surveys in medicine; ie, average values can inform practice design, but hospitalists and administrators should always consider the local context. Blindly applying medians as benchmarks and ignoring the myriad other contributors to sustainable practice risk disrupting successful PHM programs. In other words, surveys describe how the world is, not how it should be. The spectrum of academic work and norms permeating community PHM groups instead call for a nuanced approach.
How does the field build upon this useful paper? First, the Society of Hospital Medicine (SHM) should engage PHM leaders to increase participation in regular remeasurement, a critical endeavor for this dynamic field. SHM’s State of Hospital Medicine Report queries about a wider variety of practice characteristics, but it has a smaller sample size that must grow to fill this void.7 As the work of repeated surveys transitions from academic inquiry to professional society service, SHM’s Practice Analysis Committee can meet the needs of PHM through relevant questions and efforts to foster adequate participation. Second, all practice leaders should follow the ballooning bodies of literature about burnout and healthcare value. Just as labor leaders had discovered in the industrial revolution, sustainable careers require not only measuring work hours but also advocating for safe, meaningful, and engaging work conditions. By continuously creating value for patients, families, and hospitals, we can strengthen our claim to the resources needed to optimize the work environment.
Disclosure
Andrew White is Chair of the Society of Hospital Medicine’s Practice Analysis Committee, an unpaid position. Dr. Marek serves on the American Academy of Pediatrics Section on Hospital Medicine Executive Committee which is a voluntary, unpaid, elected position.
1. Whaples R. Hours of Work in U.S. History. EH Net Encyclopedia. 2001. http://eh.net/encyclopedia/hours-of-work-in-u-s-history/. Accessed June 25, 2019.
2. Pediatric Hospital Medicine Certification. The American Board of Pediatrics.
https://www.abp.org/content/pediatric-hospital-medicine-certification.
Accessed 28 February, 2018.
3. Harbuck SM, Follmer AD, Dill MJ, Erikson C. Estimating the number and characteristics
of hospitalist physicians in the United States and their possible workforce
implications. Association of Medical Colleges. 2012. www.aamc.org/download/
300620/data/aibvol12_no3-hospitalist.pdf. Accessed June 25, 2019.
4. Roberts KB, Brown J, Quinonez RA, Percelay JM. Institutions and individuals:
what makes a hospitalist “academic”? Hosp Pediatr. 2014;4(5);326-327.
https://doi.org/10.1542/hpeds.2014-00.
5. Fromme HB, Chen CO, Fine BR, Gosdin C, Shaughnessy EE. Pediatric hospitalist
workload and sustainability in university-based programs: results from a
national interview-based survey. J Hosp Med. 2018;13(10):702-705. https://doi.
org/10.12788/jhm.2977.
6. Alvarez, F, McDaniel CE, Birnie K, et al. Community pediatric hospitalist
workload: results from a national survey. J Hosp Med. 2019; 14(11):682-685. https://
doi.org/10.12788/jhm.3263.
7. 2018 State of Hospital Medicine Report. Society of Hospital Medicine: Philadelphia,
Pennsylvania; 2019. https://www.hospitalmedicine.org/practice-management/
shms-state-of-hospital-medicine/. Accessed July 27, 2019.
Systematic efforts to measure and compare work hours emerged in the 19th century as laborers shifted from artisanal shops to factories, sparking debate over the appropriate length and intensity of work.1 Two centuries of unionization and regulation defined work hours for many United States employees, including graduate medical trainees, but left attending physicians largely untouched. Instead, the medical workforce has long relied on survey data to shape jobs that balance professional norms with local market demands. Leaders in young, dynamic specialties, such as pediatric hospital medicine (PHM), particularly require such data to recruit and retain talent.
PHM progressed swiftly from acknowledgment as a “distinct area of practice” in 1999 to a subspecialty recognition.2 Currently, at least 3,000 pediatric hospitalists3 practice in more than 800 US sites (Snow C, Personal communication regarding community PHM workforce survey). Approximately half of them work at community hospitals, where PHM groups often comprise fewer than five full-time equivalents (FTEs) and face unique challenges. Community PHM practices may assume broader responsibilities than university/children’s hospital colleagues, including advocacy for the needs of children in predominantly adult-oriented hospitals.4 Although data regarding academic PHM work demands are available,5 there is little information pertaining to community hospitalists regarding typical workloads or other characteristics of thriving practices.
In this issue of the Journal of Hospital Medicine, Alvarez et al. present the findings of structured interviews with 70 community PHM group leaders.6 Each participant answered 12 questions about their group, addressing the definition of a full-time workload and hours, the design of backup systems, and the respondent’s perception of the program’s sustainability. The sample is robust, with the caveats that it disproportionately represents the Midwest and West (34.3% each) and more than half of the groups were employed by an academic institution. The authors found a median work expectation per FTE of 1,882 hours/year and 21 weekends per year, although they noted significant variability in employers’ demands and services provided. The majority of hospitalist groups lacked census caps, formal backup systems, or processes to expand coverage during busy seasons. Among the site leaders, 63% perceived their program as sustainable, but no program design or employer characteristic was clearly associated with this perception.
The importance of this study derives from aggregating data about the largest cross section of community PHM groups yet reported. For many PHM group leaders, this will offer a new point of reference for key practice characteristics. Furthermore, the authors should be commended for attempting to distinguish how program sustainability manifests in community PHM, where hospitalists shoulder longer patient care hours and many of them sustain academic endeavors. It is concerning that more than a third of leaders do not perceive their program as sustainable, but the implications for the field are unclear. Perhaps part of this uncertainty arises from the terminology, as sustainability lacks a technical or a consensus definition and the authors purposefully did not define the term for the respondents. While many respondents probably worried about physician burnout, others might have channeled fears about group finances or competition with adult service lines for beds. In addition, leaders’ fears about sustainability may not exactly represent the concerns of front-line employees.
Sustainable work environments are complex constructs with several inputs. For example, supportive leaders, efficient delivery systems, optimized EHRs, competitive pay, and confidence about service line stability might all mitigate higher workloads. Ultimately, this complexity underscores an important caution about all workplace surveys in medicine; ie, average values can inform practice design, but hospitalists and administrators should always consider the local context. Blindly applying medians as benchmarks and ignoring the myriad other contributors to sustainable practice risk disrupting successful PHM programs. In other words, surveys describe how the world is, not how it should be. The spectrum of academic work and norms permeating community PHM groups instead call for a nuanced approach.
How does the field build upon this useful paper? First, the Society of Hospital Medicine (SHM) should engage PHM leaders to increase participation in regular remeasurement, a critical endeavor for this dynamic field. SHM’s State of Hospital Medicine Report queries about a wider variety of practice characteristics, but it has a smaller sample size that must grow to fill this void.7 As the work of repeated surveys transitions from academic inquiry to professional society service, SHM’s Practice Analysis Committee can meet the needs of PHM through relevant questions and efforts to foster adequate participation. Second, all practice leaders should follow the ballooning bodies of literature about burnout and healthcare value. Just as labor leaders had discovered in the industrial revolution, sustainable careers require not only measuring work hours but also advocating for safe, meaningful, and engaging work conditions. By continuously creating value for patients, families, and hospitals, we can strengthen our claim to the resources needed to optimize the work environment.
Disclosure
Andrew White is Chair of the Society of Hospital Medicine’s Practice Analysis Committee, an unpaid position. Dr. Marek serves on the American Academy of Pediatrics Section on Hospital Medicine Executive Committee which is a voluntary, unpaid, elected position.
Systematic efforts to measure and compare work hours emerged in the 19th century as laborers shifted from artisanal shops to factories, sparking debate over the appropriate length and intensity of work.1 Two centuries of unionization and regulation defined work hours for many United States employees, including graduate medical trainees, but left attending physicians largely untouched. Instead, the medical workforce has long relied on survey data to shape jobs that balance professional norms with local market demands. Leaders in young, dynamic specialties, such as pediatric hospital medicine (PHM), particularly require such data to recruit and retain talent.
PHM progressed swiftly from acknowledgment as a “distinct area of practice” in 1999 to a subspecialty recognition.2 Currently, at least 3,000 pediatric hospitalists3 practice in more than 800 US sites (Snow C, Personal communication regarding community PHM workforce survey). Approximately half of them work at community hospitals, where PHM groups often comprise fewer than five full-time equivalents (FTEs) and face unique challenges. Community PHM practices may assume broader responsibilities than university/children’s hospital colleagues, including advocacy for the needs of children in predominantly adult-oriented hospitals.4 Although data regarding academic PHM work demands are available,5 there is little information pertaining to community hospitalists regarding typical workloads or other characteristics of thriving practices.
In this issue of the Journal of Hospital Medicine, Alvarez et al. present the findings of structured interviews with 70 community PHM group leaders.6 Each participant answered 12 questions about their group, addressing the definition of a full-time workload and hours, the design of backup systems, and the respondent’s perception of the program’s sustainability. The sample is robust, with the caveats that it disproportionately represents the Midwest and West (34.3% each) and more than half of the groups were employed by an academic institution. The authors found a median work expectation per FTE of 1,882 hours/year and 21 weekends per year, although they noted significant variability in employers’ demands and services provided. The majority of hospitalist groups lacked census caps, formal backup systems, or processes to expand coverage during busy seasons. Among the site leaders, 63% perceived their program as sustainable, but no program design or employer characteristic was clearly associated with this perception.
The importance of this study derives from aggregating data about the largest cross section of community PHM groups yet reported. For many PHM group leaders, this will offer a new point of reference for key practice characteristics. Furthermore, the authors should be commended for attempting to distinguish how program sustainability manifests in community PHM, where hospitalists shoulder longer patient care hours and many of them sustain academic endeavors. It is concerning that more than a third of leaders do not perceive their program as sustainable, but the implications for the field are unclear. Perhaps part of this uncertainty arises from the terminology, as sustainability lacks a technical or a consensus definition and the authors purposefully did not define the term for the respondents. While many respondents probably worried about physician burnout, others might have channeled fears about group finances or competition with adult service lines for beds. In addition, leaders’ fears about sustainability may not exactly represent the concerns of front-line employees.
Sustainable work environments are complex constructs with several inputs. For example, supportive leaders, efficient delivery systems, optimized EHRs, competitive pay, and confidence about service line stability might all mitigate higher workloads. Ultimately, this complexity underscores an important caution about all workplace surveys in medicine; ie, average values can inform practice design, but hospitalists and administrators should always consider the local context. Blindly applying medians as benchmarks and ignoring the myriad other contributors to sustainable practice risk disrupting successful PHM programs. In other words, surveys describe how the world is, not how it should be. The spectrum of academic work and norms permeating community PHM groups instead call for a nuanced approach.
How does the field build upon this useful paper? First, the Society of Hospital Medicine (SHM) should engage PHM leaders to increase participation in regular remeasurement, a critical endeavor for this dynamic field. SHM’s State of Hospital Medicine Report queries about a wider variety of practice characteristics, but it has a smaller sample size that must grow to fill this void.7 As the work of repeated surveys transitions from academic inquiry to professional society service, SHM’s Practice Analysis Committee can meet the needs of PHM through relevant questions and efforts to foster adequate participation. Second, all practice leaders should follow the ballooning bodies of literature about burnout and healthcare value. Just as labor leaders had discovered in the industrial revolution, sustainable careers require not only measuring work hours but also advocating for safe, meaningful, and engaging work conditions. By continuously creating value for patients, families, and hospitals, we can strengthen our claim to the resources needed to optimize the work environment.
Disclosure
Andrew White is Chair of the Society of Hospital Medicine’s Practice Analysis Committee, an unpaid position. Dr. Marek serves on the American Academy of Pediatrics Section on Hospital Medicine Executive Committee which is a voluntary, unpaid, elected position.
1. Whaples R. Hours of Work in U.S. History. EH Net Encyclopedia. 2001. http://eh.net/encyclopedia/hours-of-work-in-u-s-history/. Accessed June 25, 2019.
2. Pediatric Hospital Medicine Certification. The American Board of Pediatrics.
https://www.abp.org/content/pediatric-hospital-medicine-certification.
Accessed 28 February, 2018.
3. Harbuck SM, Follmer AD, Dill MJ, Erikson C. Estimating the number and characteristics
of hospitalist physicians in the United States and their possible workforce
implications. Association of Medical Colleges. 2012. www.aamc.org/download/
300620/data/aibvol12_no3-hospitalist.pdf. Accessed June 25, 2019.
4. Roberts KB, Brown J, Quinonez RA, Percelay JM. Institutions and individuals:
what makes a hospitalist “academic”? Hosp Pediatr. 2014;4(5);326-327.
https://doi.org/10.1542/hpeds.2014-00.
5. Fromme HB, Chen CO, Fine BR, Gosdin C, Shaughnessy EE. Pediatric hospitalist
workload and sustainability in university-based programs: results from a
national interview-based survey. J Hosp Med. 2018;13(10):702-705. https://doi.
org/10.12788/jhm.2977.
6. Alvarez, F, McDaniel CE, Birnie K, et al. Community pediatric hospitalist
workload: results from a national survey. J Hosp Med. 2019; 14(11):682-685. https://
doi.org/10.12788/jhm.3263.
7. 2018 State of Hospital Medicine Report. Society of Hospital Medicine: Philadelphia,
Pennsylvania; 2019. https://www.hospitalmedicine.org/practice-management/
shms-state-of-hospital-medicine/. Accessed July 27, 2019.
1. Whaples R. Hours of Work in U.S. History. EH Net Encyclopedia. 2001. http://eh.net/encyclopedia/hours-of-work-in-u-s-history/. Accessed June 25, 2019.
2. Pediatric Hospital Medicine Certification. The American Board of Pediatrics.
https://www.abp.org/content/pediatric-hospital-medicine-certification.
Accessed 28 February, 2018.
3. Harbuck SM, Follmer AD, Dill MJ, Erikson C. Estimating the number and characteristics
of hospitalist physicians in the United States and their possible workforce
implications. Association of Medical Colleges. 2012. www.aamc.org/download/
300620/data/aibvol12_no3-hospitalist.pdf. Accessed June 25, 2019.
4. Roberts KB, Brown J, Quinonez RA, Percelay JM. Institutions and individuals:
what makes a hospitalist “academic”? Hosp Pediatr. 2014;4(5);326-327.
https://doi.org/10.1542/hpeds.2014-00.
5. Fromme HB, Chen CO, Fine BR, Gosdin C, Shaughnessy EE. Pediatric hospitalist
workload and sustainability in university-based programs: results from a
national interview-based survey. J Hosp Med. 2018;13(10):702-705. https://doi.
org/10.12788/jhm.2977.
6. Alvarez, F, McDaniel CE, Birnie K, et al. Community pediatric hospitalist
workload: results from a national survey. J Hosp Med. 2019; 14(11):682-685. https://
doi.org/10.12788/jhm.3263.
7. 2018 State of Hospital Medicine Report. Society of Hospital Medicine: Philadelphia,
Pennsylvania; 2019. https://www.hospitalmedicine.org/practice-management/
shms-state-of-hospital-medicine/. Accessed July 27, 2019.
© 2019 Society of Hospital Medicine
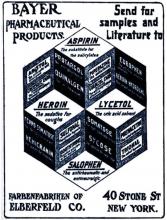
Aspirin: 4,000 years and still learning
Aspirin (acetylsalicylic acid) and its progenitors are valuable medications with a history spanning at least 4 millennia. An enormous number of patients take aspirin for a variety of reasons, and managing their therapy around the time of surgery can be challenging, as Drs. Prabhakaran and Whinney discuss in this issue.1 Even after 4,000 years, we are still learning about these remarkable drugs.
LEARNING WHAT SALICYLATES ARE
LEARNING (AND IGNORING) WHAT ASPIRIN CAN DO
In the 1940s, a general practitioner in California named Lawrence Craven recognized that many of his post-tonsillectomy patients had to be hospitalized for bleeding after he started recommending they use aspirin-containing chewing gum for pain relief.4 Under the then-debated hypothesis that myocardial infarction (MI) involves thrombosis, he recommended that adult men should take aspirin daily. He believed that women had lower rates of MI because they were more likely to take aspirin, something that men did not view as a “masculine” thing to do.
In a series of letters in journals such as the Mississippi Valley Medical Journal,5 Craven reported his observations of very low rates of MI and no strokes in aspirin users. Given the nonrigorous nature of his research and the obscure journals in which he published, his findings languished for many years. Ironically, he died of an MI in 1957.
LEARNING HOW ASPIRIN WORKS (AND A FEW OTHER THINGS)
The history of aspirin research illustrates how the fields of hemostasis and inflammation are now linked.
In the late 1960s, Weiss et al6 reported that aspirin rapidly and irreversibly inhibits platelet aggregation. In parallel, using biological assays in work that eventually led to the Nobel Prize, Vane7 discovered that inflammation involves the de novo synthesis of prostaglandins and that aspirin directly inhibits this synthesis. Further work connecting these lines of investigation led us to understand that platelet aggregation is enhanced by the prostaglandin derivative thromboxane A2, produced by cyclooxygenase-1, and that aspirin irreversibly inhibits this enzyme by acetylation.
LEARNING WHEN TO USE ASPIRIN
After decades of research ranging from the Physicians’ Health Study to well-named trials such as ARRIVE, ASCEND, and ASPREE, we now know that taking daily low doses of aspirin for primary prevention can reduce the risk of cardiovascular events and may reduce the risk of colorectal cancer—but at the cost of an increased risk of bleeding.8
Which patients will gain the most benefit and incur the least risk is still debated. What is certain, however, is that aspirin has an important role in acute coronary syndromes, secondary prevention of MI and stroke, and prevention of thrombosis after coronary stent placement. In the perioperative setting, we are learning that aspirin may benefit patients with myocardial injury after noncardiac surgery, a recently described clinical entity associated with surprisingly high mortality rates.9,10
LEARNING WHEN NOT TO USE ASPIRIN
The perioperative period is a dangerous time—surgical stress, hypercoagulability, inflammation, pain, and hemodynamic changes predispose to plaque rupture and supply-demand imbalance. It is therefore logical to hope aspirin would provide protection for at-risk patients in this context.
Unfortunately, results from the second Perioperative Ischemic Evaluation trial have dampened enthusiasm.11 Aspirin has now joined clonidine and beta-blockers on the list of interventions that probably do not reduce perioperative cardiovascular mortality rates. Other than protecting against stent thrombosis, aspirin’s main perioperative effect is to increase bleeding. Consequently, some surgical procedures mandate withdrawal of aspirin.
WHAT WE STILL NEED TO LEARN
Over the years, we have learned the broad outlines of using aspirin to prevent and treat cardiovascular disease, to relieve pain and inflammation (its original purpose), and to prevent stent thrombosis.
However, many details remain to be filled in. We need to better define groups who should and should not take aspirin for primary prevention. We also need to understand aspirin’s role in cancer chemoprevention, to find better ways to mitigate its undesirable effects, and to study its role in treating myocardial injury after noncardiac surgery.
Finally, we need to determine which (if any) patients without coronary stents will benefit from continuing their aspirin perioperatively or even initiating aspirin therapy preoperatively.
Will humanity still be using salicylates 4,000 years from now? Probably not. But what we have learned and will continue to learn from this remarkable group of medications will certainly inform new and better therapies in the years to come.
- Prabhakaran A, Whinney C. Should we stop aspirin before noncardiac surgery? Cleve Clin J Med 2019; 86(8):518–521. doi:10.3949/ccjm.86a.19036
- Jeffreys D. Aspirin: The Remarkable Story of a Wonder Drug. New York: Bloomsbury; 2008.
- Mann CC, Plummer ML. The Aspirin Wars: Money, Medicine, and 100 Years of Rampant Competition. New York: Alfred A. Knopf; 1991.
- Miner J, Hoffhines A. The discovery of aspirin's antithrombotic effects. Tex Heart Inst J 2007; 34(2):179–186. pmid:17622365
- Craven LL. Prevention of coronary and cerebral thrombosis. Miss Valley Med J 1956; 78(5):213–215. pmid:13358612
- Weiss HJ, Aledort LM, Kochwa S. The effect of salicylates on the hemostatic properties of platelets in man. J Clin Invest 1968; 47(9):2169–2180. doi:10.1172/JCI105903
- Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol 1971; 231(25):232–235. pmid:5284360
- US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 150(6):396–404. pmid:19293072
- Botto F, Alonso-Coello P, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 2014; 120(3):564–578. doi:10.1097/ALN.0000000000000113
- George R, Menon VP, Edathadathil F, et al. Myocardial injury after noncardiac surgery—incidence and predictors from a prospective observational cohort study at an Indian tertiary care centre. Medicine (Baltimore) 2018; 97(19):e0402. doi:10.1097/MD.0000000000010402
- Devereaux PJ, Mrkobrada M, Sessler DI, et al; POISE-2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med 2014; 370(16):1494–1503. doi:10.1056/NEJMoa1401105
Aspirin (acetylsalicylic acid) and its progenitors are valuable medications with a history spanning at least 4 millennia. An enormous number of patients take aspirin for a variety of reasons, and managing their therapy around the time of surgery can be challenging, as Drs. Prabhakaran and Whinney discuss in this issue.1 Even after 4,000 years, we are still learning about these remarkable drugs.
LEARNING WHAT SALICYLATES ARE
LEARNING (AND IGNORING) WHAT ASPIRIN CAN DO
In the 1940s, a general practitioner in California named Lawrence Craven recognized that many of his post-tonsillectomy patients had to be hospitalized for bleeding after he started recommending they use aspirin-containing chewing gum for pain relief.4 Under the then-debated hypothesis that myocardial infarction (MI) involves thrombosis, he recommended that adult men should take aspirin daily. He believed that women had lower rates of MI because they were more likely to take aspirin, something that men did not view as a “masculine” thing to do.
In a series of letters in journals such as the Mississippi Valley Medical Journal,5 Craven reported his observations of very low rates of MI and no strokes in aspirin users. Given the nonrigorous nature of his research and the obscure journals in which he published, his findings languished for many years. Ironically, he died of an MI in 1957.
LEARNING HOW ASPIRIN WORKS (AND A FEW OTHER THINGS)
The history of aspirin research illustrates how the fields of hemostasis and inflammation are now linked.
In the late 1960s, Weiss et al6 reported that aspirin rapidly and irreversibly inhibits platelet aggregation. In parallel, using biological assays in work that eventually led to the Nobel Prize, Vane7 discovered that inflammation involves the de novo synthesis of prostaglandins and that aspirin directly inhibits this synthesis. Further work connecting these lines of investigation led us to understand that platelet aggregation is enhanced by the prostaglandin derivative thromboxane A2, produced by cyclooxygenase-1, and that aspirin irreversibly inhibits this enzyme by acetylation.
LEARNING WHEN TO USE ASPIRIN
After decades of research ranging from the Physicians’ Health Study to well-named trials such as ARRIVE, ASCEND, and ASPREE, we now know that taking daily low doses of aspirin for primary prevention can reduce the risk of cardiovascular events and may reduce the risk of colorectal cancer—but at the cost of an increased risk of bleeding.8
Which patients will gain the most benefit and incur the least risk is still debated. What is certain, however, is that aspirin has an important role in acute coronary syndromes, secondary prevention of MI and stroke, and prevention of thrombosis after coronary stent placement. In the perioperative setting, we are learning that aspirin may benefit patients with myocardial injury after noncardiac surgery, a recently described clinical entity associated with surprisingly high mortality rates.9,10
LEARNING WHEN NOT TO USE ASPIRIN
The perioperative period is a dangerous time—surgical stress, hypercoagulability, inflammation, pain, and hemodynamic changes predispose to plaque rupture and supply-demand imbalance. It is therefore logical to hope aspirin would provide protection for at-risk patients in this context.
Unfortunately, results from the second Perioperative Ischemic Evaluation trial have dampened enthusiasm.11 Aspirin has now joined clonidine and beta-blockers on the list of interventions that probably do not reduce perioperative cardiovascular mortality rates. Other than protecting against stent thrombosis, aspirin’s main perioperative effect is to increase bleeding. Consequently, some surgical procedures mandate withdrawal of aspirin.
WHAT WE STILL NEED TO LEARN
Over the years, we have learned the broad outlines of using aspirin to prevent and treat cardiovascular disease, to relieve pain and inflammation (its original purpose), and to prevent stent thrombosis.
However, many details remain to be filled in. We need to better define groups who should and should not take aspirin for primary prevention. We also need to understand aspirin’s role in cancer chemoprevention, to find better ways to mitigate its undesirable effects, and to study its role in treating myocardial injury after noncardiac surgery.
Finally, we need to determine which (if any) patients without coronary stents will benefit from continuing their aspirin perioperatively or even initiating aspirin therapy preoperatively.
Will humanity still be using salicylates 4,000 years from now? Probably not. But what we have learned and will continue to learn from this remarkable group of medications will certainly inform new and better therapies in the years to come.
Aspirin (acetylsalicylic acid) and its progenitors are valuable medications with a history spanning at least 4 millennia. An enormous number of patients take aspirin for a variety of reasons, and managing their therapy around the time of surgery can be challenging, as Drs. Prabhakaran and Whinney discuss in this issue.1 Even after 4,000 years, we are still learning about these remarkable drugs.
LEARNING WHAT SALICYLATES ARE
LEARNING (AND IGNORING) WHAT ASPIRIN CAN DO
In the 1940s, a general practitioner in California named Lawrence Craven recognized that many of his post-tonsillectomy patients had to be hospitalized for bleeding after he started recommending they use aspirin-containing chewing gum for pain relief.4 Under the then-debated hypothesis that myocardial infarction (MI) involves thrombosis, he recommended that adult men should take aspirin daily. He believed that women had lower rates of MI because they were more likely to take aspirin, something that men did not view as a “masculine” thing to do.
In a series of letters in journals such as the Mississippi Valley Medical Journal,5 Craven reported his observations of very low rates of MI and no strokes in aspirin users. Given the nonrigorous nature of his research and the obscure journals in which he published, his findings languished for many years. Ironically, he died of an MI in 1957.
LEARNING HOW ASPIRIN WORKS (AND A FEW OTHER THINGS)
The history of aspirin research illustrates how the fields of hemostasis and inflammation are now linked.
In the late 1960s, Weiss et al6 reported that aspirin rapidly and irreversibly inhibits platelet aggregation. In parallel, using biological assays in work that eventually led to the Nobel Prize, Vane7 discovered that inflammation involves the de novo synthesis of prostaglandins and that aspirin directly inhibits this synthesis. Further work connecting these lines of investigation led us to understand that platelet aggregation is enhanced by the prostaglandin derivative thromboxane A2, produced by cyclooxygenase-1, and that aspirin irreversibly inhibits this enzyme by acetylation.
LEARNING WHEN TO USE ASPIRIN
After decades of research ranging from the Physicians’ Health Study to well-named trials such as ARRIVE, ASCEND, and ASPREE, we now know that taking daily low doses of aspirin for primary prevention can reduce the risk of cardiovascular events and may reduce the risk of colorectal cancer—but at the cost of an increased risk of bleeding.8
Which patients will gain the most benefit and incur the least risk is still debated. What is certain, however, is that aspirin has an important role in acute coronary syndromes, secondary prevention of MI and stroke, and prevention of thrombosis after coronary stent placement. In the perioperative setting, we are learning that aspirin may benefit patients with myocardial injury after noncardiac surgery, a recently described clinical entity associated with surprisingly high mortality rates.9,10
LEARNING WHEN NOT TO USE ASPIRIN
The perioperative period is a dangerous time—surgical stress, hypercoagulability, inflammation, pain, and hemodynamic changes predispose to plaque rupture and supply-demand imbalance. It is therefore logical to hope aspirin would provide protection for at-risk patients in this context.
Unfortunately, results from the second Perioperative Ischemic Evaluation trial have dampened enthusiasm.11 Aspirin has now joined clonidine and beta-blockers on the list of interventions that probably do not reduce perioperative cardiovascular mortality rates. Other than protecting against stent thrombosis, aspirin’s main perioperative effect is to increase bleeding. Consequently, some surgical procedures mandate withdrawal of aspirin.
WHAT WE STILL NEED TO LEARN
Over the years, we have learned the broad outlines of using aspirin to prevent and treat cardiovascular disease, to relieve pain and inflammation (its original purpose), and to prevent stent thrombosis.
However, many details remain to be filled in. We need to better define groups who should and should not take aspirin for primary prevention. We also need to understand aspirin’s role in cancer chemoprevention, to find better ways to mitigate its undesirable effects, and to study its role in treating myocardial injury after noncardiac surgery.
Finally, we need to determine which (if any) patients without coronary stents will benefit from continuing their aspirin perioperatively or even initiating aspirin therapy preoperatively.
Will humanity still be using salicylates 4,000 years from now? Probably not. But what we have learned and will continue to learn from this remarkable group of medications will certainly inform new and better therapies in the years to come.
- Prabhakaran A, Whinney C. Should we stop aspirin before noncardiac surgery? Cleve Clin J Med 2019; 86(8):518–521. doi:10.3949/ccjm.86a.19036
- Jeffreys D. Aspirin: The Remarkable Story of a Wonder Drug. New York: Bloomsbury; 2008.
- Mann CC, Plummer ML. The Aspirin Wars: Money, Medicine, and 100 Years of Rampant Competition. New York: Alfred A. Knopf; 1991.
- Miner J, Hoffhines A. The discovery of aspirin's antithrombotic effects. Tex Heart Inst J 2007; 34(2):179–186. pmid:17622365
- Craven LL. Prevention of coronary and cerebral thrombosis. Miss Valley Med J 1956; 78(5):213–215. pmid:13358612
- Weiss HJ, Aledort LM, Kochwa S. The effect of salicylates on the hemostatic properties of platelets in man. J Clin Invest 1968; 47(9):2169–2180. doi:10.1172/JCI105903
- Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol 1971; 231(25):232–235. pmid:5284360
- US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 150(6):396–404. pmid:19293072
- Botto F, Alonso-Coello P, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 2014; 120(3):564–578. doi:10.1097/ALN.0000000000000113
- George R, Menon VP, Edathadathil F, et al. Myocardial injury after noncardiac surgery—incidence and predictors from a prospective observational cohort study at an Indian tertiary care centre. Medicine (Baltimore) 2018; 97(19):e0402. doi:10.1097/MD.0000000000010402
- Devereaux PJ, Mrkobrada M, Sessler DI, et al; POISE-2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med 2014; 370(16):1494–1503. doi:10.1056/NEJMoa1401105
- Prabhakaran A, Whinney C. Should we stop aspirin before noncardiac surgery? Cleve Clin J Med 2019; 86(8):518–521. doi:10.3949/ccjm.86a.19036
- Jeffreys D. Aspirin: The Remarkable Story of a Wonder Drug. New York: Bloomsbury; 2008.
- Mann CC, Plummer ML. The Aspirin Wars: Money, Medicine, and 100 Years of Rampant Competition. New York: Alfred A. Knopf; 1991.
- Miner J, Hoffhines A. The discovery of aspirin's antithrombotic effects. Tex Heart Inst J 2007; 34(2):179–186. pmid:17622365
- Craven LL. Prevention of coronary and cerebral thrombosis. Miss Valley Med J 1956; 78(5):213–215. pmid:13358612
- Weiss HJ, Aledort LM, Kochwa S. The effect of salicylates on the hemostatic properties of platelets in man. J Clin Invest 1968; 47(9):2169–2180. doi:10.1172/JCI105903
- Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol 1971; 231(25):232–235. pmid:5284360
- US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 150(6):396–404. pmid:19293072
- Botto F, Alonso-Coello P, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 2014; 120(3):564–578. doi:10.1097/ALN.0000000000000113
- George R, Menon VP, Edathadathil F, et al. Myocardial injury after noncardiac surgery—incidence and predictors from a prospective observational cohort study at an Indian tertiary care centre. Medicine (Baltimore) 2018; 97(19):e0402. doi:10.1097/MD.0000000000010402
- Devereaux PJ, Mrkobrada M, Sessler DI, et al; POISE-2 Investigators. Aspirin in patients undergoing noncardiac surgery. N Engl J Med 2014; 370(16):1494–1503. doi:10.1056/NEJMoa1401105
Running in place: The uncertain future of primary care internal medicine
“My dear, here we must run as fast as we can, just to stay in place. And if you wish to go anywhere you must run twice as fast as that.”
—Lewis Carroll
Alice’s Adventures in Wonderland
The future of primary care internal medicine physicians is uncertain. According to a 2018 survey of internal medicine residents conducted by the American College of Physicians, only 11% were considering primary care as a career path.1 In 1998, that number was 54%.2
Possible reasons are many:
- Lower pay compared with subspecialists in a pay system that rewards procedural competency over mental effort
- Work schedules less flexible than in other specialties (eg, hospital medicine practitioners may have 1 week on and 1 week off)
- Perceived lack of respect
- Increasing regulatory and record-keeping burdens
- Tyranny of 15- to 20-minute appointments (irrespective of patient complexity)
- Scope-of-practice concerns as other providers seek primary care equivalency status (eg, pharmacists, walk-in clinics, advanced practice providers, telemedicine providers).
The result is a projected shortage of primary care physicians of 21,100 to 55,200 by 2030, according to a 2019 report by the Association of American Medical Colleges,3 despite an expected growth in advanced practice providers in primary care such as nurse practitioners and physician assistants.
A practical result of this shortage will be even less patient access to primary care physicians. A 2017 national survey found that the average wait time for a new patient-physician appointment has already increased by 30% since 2014.4 The wait time to see a primary care physician varied between 29 days in major metropolitan areas (up 50% from 2014) and 56 days in mid-sized markets. The longest waits by market size were 109 days for new patients in Boston, MA, and 122 days for those living in Albany, NY.
What are the implications?
In this issue, Pravia and Diaz5 make the case that primary care providers must adapt their practices to meet the needs of younger generations by increasing their use of technology. We agree that telemedicine, wearable medical devices, and enhanced patient communication through the electronic medical record (EMR) are here to stay and should be embraced.
However, we have seen the challenges of adopting technologic advances without first making an adjustment to the volume-driven patient schedule. For such advances to be successfully integrated into a clinical practice, it is vital to be cognizant of the current challenges encountered in primary care internal medicine.
UNIQUE BURDENS ON PRIMARY CARE
In addition to the stress of addressing multiple complex medical problems within a short time, evaluating multiple medical problems often leads to increases in results to review, forms to complete, and calls to patients. Even treatment plans initiated by specialists are often deferred to primary care providers for dosing adjustments, follow-up laboratory testing, and monitoring.
Moreover, patients often seek a second opinion from their primary care provider regarding care provided by subspecialists, as they consider their primary care provider to be the doctor who knows them best. And though it can be personally gratifying to be considered a trusted partner in the patient’s care, these requests often result in additional phone calls to the office or another thing to address within a complex visit.
A large in-box can be daunting in the setting of increased EMR demands. Whether you have difficulty putting in basic orders or are an advanced user, each upgrade can make you feel like you’re using the EMR for the first time. This is a problem for all specialties, but in primary care, one is addressing a large spectrum of concerns, so there is less opportunity to use standardized templates that can help buffer the problem.
A study of primary care providers found that nearly 75% of each patient visit was spent on activities other than face-to-face patient care, including working with the EMR.6 Similarly, a study using in-office observations and after-hours diaries found that physicians from various specialties spend 2 hours on administrative duties for each hour that they see patients in the office, followed by an additional 1 to 2 hours of work after clinic, mostly devoted to the EMR.7
Clinicians using scribes to help with record-keeping duties often need to see more patients to compensate for the cost. Adding 2 to 3 patients to a daily schedule usually means adding more medical conditions to manage, with an exponential increase in testing and in-box burden.
The additional burden this coverage creates in primary care is often not well understood by those in other specialties.
GUIDELINE CONFUSION AND THE DEATH OF THE ANNUAL PREVENTIVE VISIT
Another burden unique to primary care providers is the nearly continuous publication of guidelines that are often confusing and discrepant. Because many high-impact guidelines represent expert consensus or evidence from specialist perspectives, they may not fit the primary care model or values: eg, primary care guidelines tend to place more emphasis on harms associated with screening.
Screening for breast and prostate cancers is a prime example. Both require shared decision-making based on patient preferences and values.8,9 Detailed discussions about preventive screening can be difficult to achieve within the context of a medical visit owing to time limitations, especially if other medical conditions being addressed are equally controversial, such as blood pressure target goals. A decade ago, one could easily declare, “It’s time for your annual PSA test,” and move on to other concerns. Given the changing evidence, an informed patient is now likely to question whether this test should be done, how often it should be done, and whether a prostate examination should also be included.
The push toward population health has raised questions about the value of a preventive wellness visit, especially in healthy patients.10,11 Arguments against the annual physical do not account for the value of these visits, which provide the opportunity to have time-intensive shared decision-making conversations and build a trusting patient-physician relationship. The value of the annual physical is not simply to do examinations for which there is limited evidence; it is a time for us to get to know our patients, to update their preventive needs (and the medical record), and to discuss which screening tests they may safely forgo to avoid unnecessary false-positives, leading to excess cost and harm.
This trusting relationship, developed over years, is likely to save both the patient and the healthcare system significant money. For example, it enables us to reassure patients that an antibiotic is not needed for their upper respiratory infection, to encourage them to try a dietary change before proceeding with computed tomography for their abdominal pain, or to discourage them from inappropriately aggressive screening tests that may result in overtesting or overdiagnosis.
Unfortunately, it is nearly impossible to accurately quantify these substantial benefits to the healthcare system and patients. And there is a real potential that recommendations against the annual physical may eventually affect future reimbursement, which would add to the time pressures of an already overburdened primary care workforce.
DO PRIMARY CARE PHYSICIANS MAKE A DIFFERENCE?
As medicine and technology evolve, patients have more ways to access care. However, the Internet also provides patients with access to more conflicting information than ever before, making it even more important for clinicians, as trusted partners in their patients’ health, to help patients navigate the waters of information and misinformation.
Studies have shown that having a primary care physician is associated with a longer life span, higher likelihood of reporting good health, and similar clinical outcomes for common conditions such as diabetes and hypertension when compared with subspecialty care, but at a lower cost and with less resource utilization.12,13 In a study published in 2019, Basu et al12 found that for every 10 additional primary care physicians per 100,000 population, there was an associated 51.5-day increase in life expectancy, compared with a 19.2-day increase for specialists. Cost savings also occur. Similarly, a review by the American College of Physicians13 found that each additional primary care physician per 10,000 population in a US state increased the state’s health quality ranking by more than 10 spots and reduced their overall spending per Medicare beneficiary. In contrast, an increase of 1 specialist per 10,000 population was linked to a 9-spot decrease in health-quality ranking and an increase in spending.
WHY CHOOSE PRIMARY CARE?
As medical students, we fell in love with internal medicine because of the complexity and intellectual challenges of working through a diagnostic dilemma. There is a certain excitement in not knowing what type of patients will show up that day.
Primary care’s focus on continuity and developing long-standing relationships with patients and their families is largely unmatched in the subspecialty field. It is satisfying to have a general knowledge of the human body, and the central vantage point with which to weigh different subspecialty recommendations. We feel such sentiments are common to those interested in primary care, but sadly, we believe these are not enough to sustain the future of primary care internal medicine.
IS THE FUTURE BRIGHT OR BLEAK?
Primary care internists must resist the call to “run twice as fast.” Instead, we need to look for ways where our unique skill sets can benefit the health of our nation while attracting students to internal medicine primary care. The following are potential areas for moving forward.
The aging of America
The US Census Bureau projects that by the year 2035, older adults will outnumber children for the first time in US history, and by the year 2060, nearly 25% of the US population will be 65 or older.14 The rise of the geriatric patient and the need for comprehensive care will create a continued demand for primary care internists. There certainly aren’t enough geriatricians to meet this need, and primary care internists are well trained to fill this gap.
The rise of the team approach
As we are learning, complex disease management benefits from a team approach. The rise of new models of care delivery such as accountable care organizations and patient-centered medical homes echo this reality. The day of a single provider “doing it all” is fading.
The focus on population health in these models has given rise to multidisciplinary teams—including physicians, nurses, advanced practice providers, social workers, and pharmacists—whose function is to help manage and improve the physical, mental, and social care of patients, often in a capitated payment system. The primary care internist can play a key role in leading these teams, and such partnerships may help lessen reliance on the current primary care hustle of 15- to 20-minute visits. In such models, it is possible that the internist will need to see each patient only once or twice a year, in a longer appointment slot, instead of 4 to 6 times per year in rushed visits. The hope is that this will encourage the relationship-building that is so important in primary care and reduce the time and volume scheduling burdens seen in the current fee-for-service system.
Technology and advanced diagnostics
The joy of digging into a diagnostic dilemma has been a hallmark of internal medicine. The rise of technology should enable primary care internists to increase their diagnostic capabilities in the office without an overreliance on subspecialists.
Examples of technology that may benefit primary care are artificial intelligence with real-time diagnostic support, precision medicine, and office-based point-of-care ultrasonography.15–17 By increasing the diagnostic power of an office-based visit, we hope that the prestige factor of primary care medicine will increase as internists incorporate such advances into their clinics—not to mention the joy of making an appropriate diagnosis in real time.
Reimbursement and the value of time
Time is a valuable commodity for primary care internists. Unfortunately, there seems to be less of it in today’s practice. Gone are the days when we could go to the doctors’ dining room to decompress, chat, and break bread with colleagues. Today, we are more likely to be found in front of our computers over lunch answering patients’ messages. Time is also a key reason that physicians express frustration with issues such as prior authorizations for medications. These tasks routinely take time away from what is valuable—the care of our patients.
The rise of innovative practice models such as direct primary care and concierge medicine can be seen as a market response to the frustrations of increasing regulatory complexity, billing hassles, and lack of time. However, some have cautioned that such models have the potential to worsen healthcare disparities because patients pay out of pocket for some or all of their care in these practices.18
Interestingly, the Centers for Medicare and Medicaid Services recently unveiled new voluntary payment models for primary care that go into effect in 2020. These models may allow for increased practice innovation. The 2 proposed options are Primary Care First (designed for small primary care practices) and Direct Contracting (aimed at larger practices). These models are designed to provide a predictable up-front payment stream (a set payment per beneficiary) to the primary care practice. Hopefully, these options will move primary care away from the current fee-for-service, multiple-patient-visit model.
The primary care model allows practices to “assume financial risk in exchange for reduced administrative burden and performance-based payments” and “introduces new, higher payments for practices that care for complex, chronically ill patients.”19 It is too soon to know the effectiveness of such models, but any reimbursement innovation should be met with cautious optimism.
In addition, the Centers for Medicare and Medicaid Services has recently moved to reduce requirements for documentation. For example, one can fully bill with a medical student note without needing to repeat visit notes.20,21 Such changes should decrease the time needed to document the EMR and free up more time to care for patients.
A CALL TO ACTION
The national shortage of primary care providers points to the fact that this is a difficult career, and one that remains undervalued. One step we need to take is to protect the time we have with patients. It is doubtful that seeing a greater number of sicker patients each day, in addition to the responsibilities of proactive population-based care (“panel management”), will attract younger generations of physicians to fill this void, no matter what technology we adopt.
Keys to facilitating this change include understanding the value of primary care physicians, decreasing the burden of documentation, facilitating team-care options to support them, and expanding diagnostic tools available to use within primary care. If we don’t demand change, who will be there to take care of us when we grow old?
- American College of Physicians. Internal Medicine In-Training Examination® 2018 Residents Survey: Report of Findings, unpublished data. [Summary and analysis of residents' answers to questions about training] Philadelphia: American College of Physicians; 2019.
- American College of Physicians. Internal Medicine In-Training Examination® 1998 Residents Survey: Report of Findings, unpublished data. [Summary and analysis of residents' answers to questions about training] Philadelphia: American College of Physicians; 1999.
- Association of American Medical Colleges. New findings confirm predictions on physician shortage. news.aamc.org/press-releases/article/2019-workforce-projections-update. Accessed July 3, 2019.
- Merritt Hawkins Associates. 2017 Survey of physician appointment wait times and Medicare and Medicaid acceptance rates. www.merritthawkins.com/news-and-insights/thought-leadership/survey/survey-of-physician-appointment-wait-times. Accessed July 3, 2019.
- Pravia CI, Diaz YM. Primary care: practice meets technology. Cleve Clin J Med 2019; 86(8):525–528. doi:10.3949/ccjm.86a.18122
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A time-motion study of primary care physicians’ work in the electronic health record era. Fam Med 2018; 50(2):91–99. doi:10.22454/FamMed.2018.184803
- Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165(11):753–760. doi:10.7326/M16-0961
- O'Callaghan ME, Kichenadasse G, Vatandoust S, Moretti K. Informed decision making about prostate cancer screening. Ann Intern Med 2015; 162(6):457. doi:10.7326/L15-5063
- Batur P, Walsh J. Annual mammography starting at age 40: More talk, less action? Cleve Clin J Med 2015; 82(5):272–275. doi:10.3949/ccjm.82a.14156
- Mehrotra A, Prochazka A. Improving value in health care—against the annual physical. N Engl J Med 2015; 373(16):1485–1487. doi:10.1056/NEJMp1507485
- Krogsboll LT, Jorgensen KJ, Gotzsche PC. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev 2019; 1:CD009009. doi:10.1002/14651858.CD009009.pub3
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med 2019; 179(4):506–514. doi:10.1001/jamainternmed.2018.7624
- American College of Physicians. How is a shortage of primary care physicians affecting the quality and cost of medical care? www.acponline.org/acp_policy/policies/primary_care_shortage_affecting_hc_2008.pdf. Accessed July 3, 2019.
- Vespa, J, Armstrong D, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. www.census.gov/content/dam/Census/library/publications/2018/demo/P25_1144.pdf. Accessed July 3, 2019.
- Lin S, Mahoney M, Sinsky C. Ten ways artificial intelligence will transform primary care. J Gen Intern Med 2019. doi:10.1007/s11606-019-05035-1. Epub ahead of print.
- Feero WG. Is “precision medicine” ready to use in primary care practice? Yes: It offers patients more individualized ways of managing their health. Am Fam Physician 2017; 96(12):767–768. pmid:29431374
- Bornemann P, Jayasekera N, Bergman K, Ramos M, Gerhart J. Point-of-care ultrasound: coming soon to primary care? J Fam Pract 2018; 67(2):70–80. pmid:29400896
- Doherty R; Medical Practice and Quality Committee of the American College of Physicians. Assessing the patient care implications of “concierge” and other direct patient contracting practices: a policy position paper from the American College of Physicians. Ann Intern Med 2015; 163(12):949–952. doi:10.7326/M15-0366
- Centers for Medicare and Medicaid Services. Primary care first model options. innovation.cms.gov/initiatives/primary-care-first-model-options. Accessed July 29, 2019.
- Centers for Medicare and Medicaid Services. Final Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2019. www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year. Accessed July 3, 2019.
- Centers for Medicare and Medicaid Services. E/M Service Documentation Provided By Students. www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM10412.pdf. Accessed July 3, 2019.
“My dear, here we must run as fast as we can, just to stay in place. And if you wish to go anywhere you must run twice as fast as that.”
—Lewis Carroll
Alice’s Adventures in Wonderland
The future of primary care internal medicine physicians is uncertain. According to a 2018 survey of internal medicine residents conducted by the American College of Physicians, only 11% were considering primary care as a career path.1 In 1998, that number was 54%.2
Possible reasons are many:
- Lower pay compared with subspecialists in a pay system that rewards procedural competency over mental effort
- Work schedules less flexible than in other specialties (eg, hospital medicine practitioners may have 1 week on and 1 week off)
- Perceived lack of respect
- Increasing regulatory and record-keeping burdens
- Tyranny of 15- to 20-minute appointments (irrespective of patient complexity)
- Scope-of-practice concerns as other providers seek primary care equivalency status (eg, pharmacists, walk-in clinics, advanced practice providers, telemedicine providers).
The result is a projected shortage of primary care physicians of 21,100 to 55,200 by 2030, according to a 2019 report by the Association of American Medical Colleges,3 despite an expected growth in advanced practice providers in primary care such as nurse practitioners and physician assistants.
A practical result of this shortage will be even less patient access to primary care physicians. A 2017 national survey found that the average wait time for a new patient-physician appointment has already increased by 30% since 2014.4 The wait time to see a primary care physician varied between 29 days in major metropolitan areas (up 50% from 2014) and 56 days in mid-sized markets. The longest waits by market size were 109 days for new patients in Boston, MA, and 122 days for those living in Albany, NY.
What are the implications?
In this issue, Pravia and Diaz5 make the case that primary care providers must adapt their practices to meet the needs of younger generations by increasing their use of technology. We agree that telemedicine, wearable medical devices, and enhanced patient communication through the electronic medical record (EMR) are here to stay and should be embraced.
However, we have seen the challenges of adopting technologic advances without first making an adjustment to the volume-driven patient schedule. For such advances to be successfully integrated into a clinical practice, it is vital to be cognizant of the current challenges encountered in primary care internal medicine.
UNIQUE BURDENS ON PRIMARY CARE
In addition to the stress of addressing multiple complex medical problems within a short time, evaluating multiple medical problems often leads to increases in results to review, forms to complete, and calls to patients. Even treatment plans initiated by specialists are often deferred to primary care providers for dosing adjustments, follow-up laboratory testing, and monitoring.
Moreover, patients often seek a second opinion from their primary care provider regarding care provided by subspecialists, as they consider their primary care provider to be the doctor who knows them best. And though it can be personally gratifying to be considered a trusted partner in the patient’s care, these requests often result in additional phone calls to the office or another thing to address within a complex visit.
A large in-box can be daunting in the setting of increased EMR demands. Whether you have difficulty putting in basic orders or are an advanced user, each upgrade can make you feel like you’re using the EMR for the first time. This is a problem for all specialties, but in primary care, one is addressing a large spectrum of concerns, so there is less opportunity to use standardized templates that can help buffer the problem.
A study of primary care providers found that nearly 75% of each patient visit was spent on activities other than face-to-face patient care, including working with the EMR.6 Similarly, a study using in-office observations and after-hours diaries found that physicians from various specialties spend 2 hours on administrative duties for each hour that they see patients in the office, followed by an additional 1 to 2 hours of work after clinic, mostly devoted to the EMR.7
Clinicians using scribes to help with record-keeping duties often need to see more patients to compensate for the cost. Adding 2 to 3 patients to a daily schedule usually means adding more medical conditions to manage, with an exponential increase in testing and in-box burden.
The additional burden this coverage creates in primary care is often not well understood by those in other specialties.
GUIDELINE CONFUSION AND THE DEATH OF THE ANNUAL PREVENTIVE VISIT
Another burden unique to primary care providers is the nearly continuous publication of guidelines that are often confusing and discrepant. Because many high-impact guidelines represent expert consensus or evidence from specialist perspectives, they may not fit the primary care model or values: eg, primary care guidelines tend to place more emphasis on harms associated with screening.
Screening for breast and prostate cancers is a prime example. Both require shared decision-making based on patient preferences and values.8,9 Detailed discussions about preventive screening can be difficult to achieve within the context of a medical visit owing to time limitations, especially if other medical conditions being addressed are equally controversial, such as blood pressure target goals. A decade ago, one could easily declare, “It’s time for your annual PSA test,” and move on to other concerns. Given the changing evidence, an informed patient is now likely to question whether this test should be done, how often it should be done, and whether a prostate examination should also be included.
The push toward population health has raised questions about the value of a preventive wellness visit, especially in healthy patients.10,11 Arguments against the annual physical do not account for the value of these visits, which provide the opportunity to have time-intensive shared decision-making conversations and build a trusting patient-physician relationship. The value of the annual physical is not simply to do examinations for which there is limited evidence; it is a time for us to get to know our patients, to update their preventive needs (and the medical record), and to discuss which screening tests they may safely forgo to avoid unnecessary false-positives, leading to excess cost and harm.
This trusting relationship, developed over years, is likely to save both the patient and the healthcare system significant money. For example, it enables us to reassure patients that an antibiotic is not needed for their upper respiratory infection, to encourage them to try a dietary change before proceeding with computed tomography for their abdominal pain, or to discourage them from inappropriately aggressive screening tests that may result in overtesting or overdiagnosis.
Unfortunately, it is nearly impossible to accurately quantify these substantial benefits to the healthcare system and patients. And there is a real potential that recommendations against the annual physical may eventually affect future reimbursement, which would add to the time pressures of an already overburdened primary care workforce.
DO PRIMARY CARE PHYSICIANS MAKE A DIFFERENCE?
As medicine and technology evolve, patients have more ways to access care. However, the Internet also provides patients with access to more conflicting information than ever before, making it even more important for clinicians, as trusted partners in their patients’ health, to help patients navigate the waters of information and misinformation.
Studies have shown that having a primary care physician is associated with a longer life span, higher likelihood of reporting good health, and similar clinical outcomes for common conditions such as diabetes and hypertension when compared with subspecialty care, but at a lower cost and with less resource utilization.12,13 In a study published in 2019, Basu et al12 found that for every 10 additional primary care physicians per 100,000 population, there was an associated 51.5-day increase in life expectancy, compared with a 19.2-day increase for specialists. Cost savings also occur. Similarly, a review by the American College of Physicians13 found that each additional primary care physician per 10,000 population in a US state increased the state’s health quality ranking by more than 10 spots and reduced their overall spending per Medicare beneficiary. In contrast, an increase of 1 specialist per 10,000 population was linked to a 9-spot decrease in health-quality ranking and an increase in spending.
WHY CHOOSE PRIMARY CARE?
As medical students, we fell in love with internal medicine because of the complexity and intellectual challenges of working through a diagnostic dilemma. There is a certain excitement in not knowing what type of patients will show up that day.
Primary care’s focus on continuity and developing long-standing relationships with patients and their families is largely unmatched in the subspecialty field. It is satisfying to have a general knowledge of the human body, and the central vantage point with which to weigh different subspecialty recommendations. We feel such sentiments are common to those interested in primary care, but sadly, we believe these are not enough to sustain the future of primary care internal medicine.
IS THE FUTURE BRIGHT OR BLEAK?
Primary care internists must resist the call to “run twice as fast.” Instead, we need to look for ways where our unique skill sets can benefit the health of our nation while attracting students to internal medicine primary care. The following are potential areas for moving forward.
The aging of America
The US Census Bureau projects that by the year 2035, older adults will outnumber children for the first time in US history, and by the year 2060, nearly 25% of the US population will be 65 or older.14 The rise of the geriatric patient and the need for comprehensive care will create a continued demand for primary care internists. There certainly aren’t enough geriatricians to meet this need, and primary care internists are well trained to fill this gap.
The rise of the team approach
As we are learning, complex disease management benefits from a team approach. The rise of new models of care delivery such as accountable care organizations and patient-centered medical homes echo this reality. The day of a single provider “doing it all” is fading.
The focus on population health in these models has given rise to multidisciplinary teams—including physicians, nurses, advanced practice providers, social workers, and pharmacists—whose function is to help manage and improve the physical, mental, and social care of patients, often in a capitated payment system. The primary care internist can play a key role in leading these teams, and such partnerships may help lessen reliance on the current primary care hustle of 15- to 20-minute visits. In such models, it is possible that the internist will need to see each patient only once or twice a year, in a longer appointment slot, instead of 4 to 6 times per year in rushed visits. The hope is that this will encourage the relationship-building that is so important in primary care and reduce the time and volume scheduling burdens seen in the current fee-for-service system.
Technology and advanced diagnostics
The joy of digging into a diagnostic dilemma has been a hallmark of internal medicine. The rise of technology should enable primary care internists to increase their diagnostic capabilities in the office without an overreliance on subspecialists.
Examples of technology that may benefit primary care are artificial intelligence with real-time diagnostic support, precision medicine, and office-based point-of-care ultrasonography.15–17 By increasing the diagnostic power of an office-based visit, we hope that the prestige factor of primary care medicine will increase as internists incorporate such advances into their clinics—not to mention the joy of making an appropriate diagnosis in real time.
Reimbursement and the value of time
Time is a valuable commodity for primary care internists. Unfortunately, there seems to be less of it in today’s practice. Gone are the days when we could go to the doctors’ dining room to decompress, chat, and break bread with colleagues. Today, we are more likely to be found in front of our computers over lunch answering patients’ messages. Time is also a key reason that physicians express frustration with issues such as prior authorizations for medications. These tasks routinely take time away from what is valuable—the care of our patients.
The rise of innovative practice models such as direct primary care and concierge medicine can be seen as a market response to the frustrations of increasing regulatory complexity, billing hassles, and lack of time. However, some have cautioned that such models have the potential to worsen healthcare disparities because patients pay out of pocket for some or all of their care in these practices.18
Interestingly, the Centers for Medicare and Medicaid Services recently unveiled new voluntary payment models for primary care that go into effect in 2020. These models may allow for increased practice innovation. The 2 proposed options are Primary Care First (designed for small primary care practices) and Direct Contracting (aimed at larger practices). These models are designed to provide a predictable up-front payment stream (a set payment per beneficiary) to the primary care practice. Hopefully, these options will move primary care away from the current fee-for-service, multiple-patient-visit model.
The primary care model allows practices to “assume financial risk in exchange for reduced administrative burden and performance-based payments” and “introduces new, higher payments for practices that care for complex, chronically ill patients.”19 It is too soon to know the effectiveness of such models, but any reimbursement innovation should be met with cautious optimism.
In addition, the Centers for Medicare and Medicaid Services has recently moved to reduce requirements for documentation. For example, one can fully bill with a medical student note without needing to repeat visit notes.20,21 Such changes should decrease the time needed to document the EMR and free up more time to care for patients.
A CALL TO ACTION
The national shortage of primary care providers points to the fact that this is a difficult career, and one that remains undervalued. One step we need to take is to protect the time we have with patients. It is doubtful that seeing a greater number of sicker patients each day, in addition to the responsibilities of proactive population-based care (“panel management”), will attract younger generations of physicians to fill this void, no matter what technology we adopt.
Keys to facilitating this change include understanding the value of primary care physicians, decreasing the burden of documentation, facilitating team-care options to support them, and expanding diagnostic tools available to use within primary care. If we don’t demand change, who will be there to take care of us when we grow old?
“My dear, here we must run as fast as we can, just to stay in place. And if you wish to go anywhere you must run twice as fast as that.”
—Lewis Carroll
Alice’s Adventures in Wonderland
The future of primary care internal medicine physicians is uncertain. According to a 2018 survey of internal medicine residents conducted by the American College of Physicians, only 11% were considering primary care as a career path.1 In 1998, that number was 54%.2
Possible reasons are many:
- Lower pay compared with subspecialists in a pay system that rewards procedural competency over mental effort
- Work schedules less flexible than in other specialties (eg, hospital medicine practitioners may have 1 week on and 1 week off)
- Perceived lack of respect
- Increasing regulatory and record-keeping burdens
- Tyranny of 15- to 20-minute appointments (irrespective of patient complexity)
- Scope-of-practice concerns as other providers seek primary care equivalency status (eg, pharmacists, walk-in clinics, advanced practice providers, telemedicine providers).
The result is a projected shortage of primary care physicians of 21,100 to 55,200 by 2030, according to a 2019 report by the Association of American Medical Colleges,3 despite an expected growth in advanced practice providers in primary care such as nurse practitioners and physician assistants.
A practical result of this shortage will be even less patient access to primary care physicians. A 2017 national survey found that the average wait time for a new patient-physician appointment has already increased by 30% since 2014.4 The wait time to see a primary care physician varied between 29 days in major metropolitan areas (up 50% from 2014) and 56 days in mid-sized markets. The longest waits by market size were 109 days for new patients in Boston, MA, and 122 days for those living in Albany, NY.
What are the implications?
In this issue, Pravia and Diaz5 make the case that primary care providers must adapt their practices to meet the needs of younger generations by increasing their use of technology. We agree that telemedicine, wearable medical devices, and enhanced patient communication through the electronic medical record (EMR) are here to stay and should be embraced.
However, we have seen the challenges of adopting technologic advances without first making an adjustment to the volume-driven patient schedule. For such advances to be successfully integrated into a clinical practice, it is vital to be cognizant of the current challenges encountered in primary care internal medicine.
UNIQUE BURDENS ON PRIMARY CARE
In addition to the stress of addressing multiple complex medical problems within a short time, evaluating multiple medical problems often leads to increases in results to review, forms to complete, and calls to patients. Even treatment plans initiated by specialists are often deferred to primary care providers for dosing adjustments, follow-up laboratory testing, and monitoring.
Moreover, patients often seek a second opinion from their primary care provider regarding care provided by subspecialists, as they consider their primary care provider to be the doctor who knows them best. And though it can be personally gratifying to be considered a trusted partner in the patient’s care, these requests often result in additional phone calls to the office or another thing to address within a complex visit.
A large in-box can be daunting in the setting of increased EMR demands. Whether you have difficulty putting in basic orders or are an advanced user, each upgrade can make you feel like you’re using the EMR for the first time. This is a problem for all specialties, but in primary care, one is addressing a large spectrum of concerns, so there is less opportunity to use standardized templates that can help buffer the problem.
A study of primary care providers found that nearly 75% of each patient visit was spent on activities other than face-to-face patient care, including working with the EMR.6 Similarly, a study using in-office observations and after-hours diaries found that physicians from various specialties spend 2 hours on administrative duties for each hour that they see patients in the office, followed by an additional 1 to 2 hours of work after clinic, mostly devoted to the EMR.7
Clinicians using scribes to help with record-keeping duties often need to see more patients to compensate for the cost. Adding 2 to 3 patients to a daily schedule usually means adding more medical conditions to manage, with an exponential increase in testing and in-box burden.
The additional burden this coverage creates in primary care is often not well understood by those in other specialties.
GUIDELINE CONFUSION AND THE DEATH OF THE ANNUAL PREVENTIVE VISIT
Another burden unique to primary care providers is the nearly continuous publication of guidelines that are often confusing and discrepant. Because many high-impact guidelines represent expert consensus or evidence from specialist perspectives, they may not fit the primary care model or values: eg, primary care guidelines tend to place more emphasis on harms associated with screening.
Screening for breast and prostate cancers is a prime example. Both require shared decision-making based on patient preferences and values.8,9 Detailed discussions about preventive screening can be difficult to achieve within the context of a medical visit owing to time limitations, especially if other medical conditions being addressed are equally controversial, such as blood pressure target goals. A decade ago, one could easily declare, “It’s time for your annual PSA test,” and move on to other concerns. Given the changing evidence, an informed patient is now likely to question whether this test should be done, how often it should be done, and whether a prostate examination should also be included.
The push toward population health has raised questions about the value of a preventive wellness visit, especially in healthy patients.10,11 Arguments against the annual physical do not account for the value of these visits, which provide the opportunity to have time-intensive shared decision-making conversations and build a trusting patient-physician relationship. The value of the annual physical is not simply to do examinations for which there is limited evidence; it is a time for us to get to know our patients, to update their preventive needs (and the medical record), and to discuss which screening tests they may safely forgo to avoid unnecessary false-positives, leading to excess cost and harm.
This trusting relationship, developed over years, is likely to save both the patient and the healthcare system significant money. For example, it enables us to reassure patients that an antibiotic is not needed for their upper respiratory infection, to encourage them to try a dietary change before proceeding with computed tomography for their abdominal pain, or to discourage them from inappropriately aggressive screening tests that may result in overtesting or overdiagnosis.
Unfortunately, it is nearly impossible to accurately quantify these substantial benefits to the healthcare system and patients. And there is a real potential that recommendations against the annual physical may eventually affect future reimbursement, which would add to the time pressures of an already overburdened primary care workforce.
DO PRIMARY CARE PHYSICIANS MAKE A DIFFERENCE?
As medicine and technology evolve, patients have more ways to access care. However, the Internet also provides patients with access to more conflicting information than ever before, making it even more important for clinicians, as trusted partners in their patients’ health, to help patients navigate the waters of information and misinformation.
Studies have shown that having a primary care physician is associated with a longer life span, higher likelihood of reporting good health, and similar clinical outcomes for common conditions such as diabetes and hypertension when compared with subspecialty care, but at a lower cost and with less resource utilization.12,13 In a study published in 2019, Basu et al12 found that for every 10 additional primary care physicians per 100,000 population, there was an associated 51.5-day increase in life expectancy, compared with a 19.2-day increase for specialists. Cost savings also occur. Similarly, a review by the American College of Physicians13 found that each additional primary care physician per 10,000 population in a US state increased the state’s health quality ranking by more than 10 spots and reduced their overall spending per Medicare beneficiary. In contrast, an increase of 1 specialist per 10,000 population was linked to a 9-spot decrease in health-quality ranking and an increase in spending.
WHY CHOOSE PRIMARY CARE?
As medical students, we fell in love with internal medicine because of the complexity and intellectual challenges of working through a diagnostic dilemma. There is a certain excitement in not knowing what type of patients will show up that day.
Primary care’s focus on continuity and developing long-standing relationships with patients and their families is largely unmatched in the subspecialty field. It is satisfying to have a general knowledge of the human body, and the central vantage point with which to weigh different subspecialty recommendations. We feel such sentiments are common to those interested in primary care, but sadly, we believe these are not enough to sustain the future of primary care internal medicine.
IS THE FUTURE BRIGHT OR BLEAK?
Primary care internists must resist the call to “run twice as fast.” Instead, we need to look for ways where our unique skill sets can benefit the health of our nation while attracting students to internal medicine primary care. The following are potential areas for moving forward.
The aging of America
The US Census Bureau projects that by the year 2035, older adults will outnumber children for the first time in US history, and by the year 2060, nearly 25% of the US population will be 65 or older.14 The rise of the geriatric patient and the need for comprehensive care will create a continued demand for primary care internists. There certainly aren’t enough geriatricians to meet this need, and primary care internists are well trained to fill this gap.
The rise of the team approach
As we are learning, complex disease management benefits from a team approach. The rise of new models of care delivery such as accountable care organizations and patient-centered medical homes echo this reality. The day of a single provider “doing it all” is fading.
The focus on population health in these models has given rise to multidisciplinary teams—including physicians, nurses, advanced practice providers, social workers, and pharmacists—whose function is to help manage and improve the physical, mental, and social care of patients, often in a capitated payment system. The primary care internist can play a key role in leading these teams, and such partnerships may help lessen reliance on the current primary care hustle of 15- to 20-minute visits. In such models, it is possible that the internist will need to see each patient only once or twice a year, in a longer appointment slot, instead of 4 to 6 times per year in rushed visits. The hope is that this will encourage the relationship-building that is so important in primary care and reduce the time and volume scheduling burdens seen in the current fee-for-service system.
Technology and advanced diagnostics
The joy of digging into a diagnostic dilemma has been a hallmark of internal medicine. The rise of technology should enable primary care internists to increase their diagnostic capabilities in the office without an overreliance on subspecialists.
Examples of technology that may benefit primary care are artificial intelligence with real-time diagnostic support, precision medicine, and office-based point-of-care ultrasonography.15–17 By increasing the diagnostic power of an office-based visit, we hope that the prestige factor of primary care medicine will increase as internists incorporate such advances into their clinics—not to mention the joy of making an appropriate diagnosis in real time.
Reimbursement and the value of time
Time is a valuable commodity for primary care internists. Unfortunately, there seems to be less of it in today’s practice. Gone are the days when we could go to the doctors’ dining room to decompress, chat, and break bread with colleagues. Today, we are more likely to be found in front of our computers over lunch answering patients’ messages. Time is also a key reason that physicians express frustration with issues such as prior authorizations for medications. These tasks routinely take time away from what is valuable—the care of our patients.
The rise of innovative practice models such as direct primary care and concierge medicine can be seen as a market response to the frustrations of increasing regulatory complexity, billing hassles, and lack of time. However, some have cautioned that such models have the potential to worsen healthcare disparities because patients pay out of pocket for some or all of their care in these practices.18
Interestingly, the Centers for Medicare and Medicaid Services recently unveiled new voluntary payment models for primary care that go into effect in 2020. These models may allow for increased practice innovation. The 2 proposed options are Primary Care First (designed for small primary care practices) and Direct Contracting (aimed at larger practices). These models are designed to provide a predictable up-front payment stream (a set payment per beneficiary) to the primary care practice. Hopefully, these options will move primary care away from the current fee-for-service, multiple-patient-visit model.
The primary care model allows practices to “assume financial risk in exchange for reduced administrative burden and performance-based payments” and “introduces new, higher payments for practices that care for complex, chronically ill patients.”19 It is too soon to know the effectiveness of such models, but any reimbursement innovation should be met with cautious optimism.
In addition, the Centers for Medicare and Medicaid Services has recently moved to reduce requirements for documentation. For example, one can fully bill with a medical student note without needing to repeat visit notes.20,21 Such changes should decrease the time needed to document the EMR and free up more time to care for patients.
A CALL TO ACTION
The national shortage of primary care providers points to the fact that this is a difficult career, and one that remains undervalued. One step we need to take is to protect the time we have with patients. It is doubtful that seeing a greater number of sicker patients each day, in addition to the responsibilities of proactive population-based care (“panel management”), will attract younger generations of physicians to fill this void, no matter what technology we adopt.
Keys to facilitating this change include understanding the value of primary care physicians, decreasing the burden of documentation, facilitating team-care options to support them, and expanding diagnostic tools available to use within primary care. If we don’t demand change, who will be there to take care of us when we grow old?
- American College of Physicians. Internal Medicine In-Training Examination® 2018 Residents Survey: Report of Findings, unpublished data. [Summary and analysis of residents' answers to questions about training] Philadelphia: American College of Physicians; 2019.
- American College of Physicians. Internal Medicine In-Training Examination® 1998 Residents Survey: Report of Findings, unpublished data. [Summary and analysis of residents' answers to questions about training] Philadelphia: American College of Physicians; 1999.
- Association of American Medical Colleges. New findings confirm predictions on physician shortage. news.aamc.org/press-releases/article/2019-workforce-projections-update. Accessed July 3, 2019.
- Merritt Hawkins Associates. 2017 Survey of physician appointment wait times and Medicare and Medicaid acceptance rates. www.merritthawkins.com/news-and-insights/thought-leadership/survey/survey-of-physician-appointment-wait-times. Accessed July 3, 2019.
- Pravia CI, Diaz YM. Primary care: practice meets technology. Cleve Clin J Med 2019; 86(8):525–528. doi:10.3949/ccjm.86a.18122
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A time-motion study of primary care physicians’ work in the electronic health record era. Fam Med 2018; 50(2):91–99. doi:10.22454/FamMed.2018.184803
- Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165(11):753–760. doi:10.7326/M16-0961
- O'Callaghan ME, Kichenadasse G, Vatandoust S, Moretti K. Informed decision making about prostate cancer screening. Ann Intern Med 2015; 162(6):457. doi:10.7326/L15-5063
- Batur P, Walsh J. Annual mammography starting at age 40: More talk, less action? Cleve Clin J Med 2015; 82(5):272–275. doi:10.3949/ccjm.82a.14156
- Mehrotra A, Prochazka A. Improving value in health care—against the annual physical. N Engl J Med 2015; 373(16):1485–1487. doi:10.1056/NEJMp1507485
- Krogsboll LT, Jorgensen KJ, Gotzsche PC. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev 2019; 1:CD009009. doi:10.1002/14651858.CD009009.pub3
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med 2019; 179(4):506–514. doi:10.1001/jamainternmed.2018.7624
- American College of Physicians. How is a shortage of primary care physicians affecting the quality and cost of medical care? www.acponline.org/acp_policy/policies/primary_care_shortage_affecting_hc_2008.pdf. Accessed July 3, 2019.
- Vespa, J, Armstrong D, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. www.census.gov/content/dam/Census/library/publications/2018/demo/P25_1144.pdf. Accessed July 3, 2019.
- Lin S, Mahoney M, Sinsky C. Ten ways artificial intelligence will transform primary care. J Gen Intern Med 2019. doi:10.1007/s11606-019-05035-1. Epub ahead of print.
- Feero WG. Is “precision medicine” ready to use in primary care practice? Yes: It offers patients more individualized ways of managing their health. Am Fam Physician 2017; 96(12):767–768. pmid:29431374
- Bornemann P, Jayasekera N, Bergman K, Ramos M, Gerhart J. Point-of-care ultrasound: coming soon to primary care? J Fam Pract 2018; 67(2):70–80. pmid:29400896
- Doherty R; Medical Practice and Quality Committee of the American College of Physicians. Assessing the patient care implications of “concierge” and other direct patient contracting practices: a policy position paper from the American College of Physicians. Ann Intern Med 2015; 163(12):949–952. doi:10.7326/M15-0366
- Centers for Medicare and Medicaid Services. Primary care first model options. innovation.cms.gov/initiatives/primary-care-first-model-options. Accessed July 29, 2019.
- Centers for Medicare and Medicaid Services. Final Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2019. www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year. Accessed July 3, 2019.
- Centers for Medicare and Medicaid Services. E/M Service Documentation Provided By Students. www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM10412.pdf. Accessed July 3, 2019.
- American College of Physicians. Internal Medicine In-Training Examination® 2018 Residents Survey: Report of Findings, unpublished data. [Summary and analysis of residents' answers to questions about training] Philadelphia: American College of Physicians; 2019.
- American College of Physicians. Internal Medicine In-Training Examination® 1998 Residents Survey: Report of Findings, unpublished data. [Summary and analysis of residents' answers to questions about training] Philadelphia: American College of Physicians; 1999.
- Association of American Medical Colleges. New findings confirm predictions on physician shortage. news.aamc.org/press-releases/article/2019-workforce-projections-update. Accessed July 3, 2019.
- Merritt Hawkins Associates. 2017 Survey of physician appointment wait times and Medicare and Medicaid acceptance rates. www.merritthawkins.com/news-and-insights/thought-leadership/survey/survey-of-physician-appointment-wait-times. Accessed July 3, 2019.
- Pravia CI, Diaz YM. Primary care: practice meets technology. Cleve Clin J Med 2019; 86(8):525–528. doi:10.3949/ccjm.86a.18122
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A time-motion study of primary care physicians’ work in the electronic health record era. Fam Med 2018; 50(2):91–99. doi:10.22454/FamMed.2018.184803
- Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165(11):753–760. doi:10.7326/M16-0961
- O'Callaghan ME, Kichenadasse G, Vatandoust S, Moretti K. Informed decision making about prostate cancer screening. Ann Intern Med 2015; 162(6):457. doi:10.7326/L15-5063
- Batur P, Walsh J. Annual mammography starting at age 40: More talk, less action? Cleve Clin J Med 2015; 82(5):272–275. doi:10.3949/ccjm.82a.14156
- Mehrotra A, Prochazka A. Improving value in health care—against the annual physical. N Engl J Med 2015; 373(16):1485–1487. doi:10.1056/NEJMp1507485
- Krogsboll LT, Jorgensen KJ, Gotzsche PC. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev 2019; 1:CD009009. doi:10.1002/14651858.CD009009.pub3
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med 2019; 179(4):506–514. doi:10.1001/jamainternmed.2018.7624
- American College of Physicians. How is a shortage of primary care physicians affecting the quality and cost of medical care? www.acponline.org/acp_policy/policies/primary_care_shortage_affecting_hc_2008.pdf. Accessed July 3, 2019.
- Vespa, J, Armstrong D, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. www.census.gov/content/dam/Census/library/publications/2018/demo/P25_1144.pdf. Accessed July 3, 2019.
- Lin S, Mahoney M, Sinsky C. Ten ways artificial intelligence will transform primary care. J Gen Intern Med 2019. doi:10.1007/s11606-019-05035-1. Epub ahead of print.
- Feero WG. Is “precision medicine” ready to use in primary care practice? Yes: It offers patients more individualized ways of managing their health. Am Fam Physician 2017; 96(12):767–768. pmid:29431374
- Bornemann P, Jayasekera N, Bergman K, Ramos M, Gerhart J. Point-of-care ultrasound: coming soon to primary care? J Fam Pract 2018; 67(2):70–80. pmid:29400896
- Doherty R; Medical Practice and Quality Committee of the American College of Physicians. Assessing the patient care implications of “concierge” and other direct patient contracting practices: a policy position paper from the American College of Physicians. Ann Intern Med 2015; 163(12):949–952. doi:10.7326/M15-0366
- Centers for Medicare and Medicaid Services. Primary care first model options. innovation.cms.gov/initiatives/primary-care-first-model-options. Accessed July 29, 2019.
- Centers for Medicare and Medicaid Services. Final Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2019. www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year. Accessed July 3, 2019.
- Centers for Medicare and Medicaid Services. E/M Service Documentation Provided By Students. www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM10412.pdf. Accessed July 3, 2019.
Where have all the children gone? Intentional communities for adults with autism
Autism spectrum disorder (ASD) is a neurodevelopmental condition typically diagnosed early in life: the median age at diagnosis is 52 months.1 Because research demonstrates the benefits of early intervention,2 when we think about people with ASD, we generally think about children and adolescents.
However, autism spans the entirety of one’s life. This means that children with ASD will grow to be adults with ASD. The US Centers for Disease Control and Prevention estimated that 1 in 59 children were diagnosed with ASD during the surveillance year 2014,1 which was nearly double the prevalence from just 8 years earlier,3 and a 15% increase since 2012.4 As these children grow up, this translates to an ever-growing number of adults with autism.
UNMET NEEDS
Healthcare, housing, and intellectual and developmental disability services for adults with ASD currently fall well short of meeting the needs of this exploding population. If solutions are to be realized, innovative approaches must be employed.
Swetlik et al,5 in this issue of the Journal, offer valuable insights into the challenges that practitioners and their adult patients with ASD encounter as a result of seismic shifts in diagnostic criteria, increasing prevalence, and changes to healthcare financial coverage. They also review behavioral and pharmacologic treatments, reproductive health, and caregiver fatigue and discuss the role of the physician and other healthcare practitioners who are likely to have only limited exposure to adult patients with ASD. These wide-ranging considerations speak to the complexity of the healthcare needs of this population.
Swetlik et al also underscore that transition planning is essential for primary care, psychiatry, behavioral health services, continuing education, skill development, and appropriate prevocational training for adolescents with ASD, and yet it is often underutilized or unavailable. There is a dearth of experienced practitioners across these disciplines to serve adults with ASD. The complexity of navigating bureaucratic processes to secure funding (typically Medicaid) supports the necessity of planning early to achieve desired outcomes for each young adult. Additionally, the number of Medicaid waivers that fund many supportive services are limited.
GROWING UP IS HARD; START PLANNING EARLY
Swetlik et al describe the stress these circumstances create for people with ASD and their families. Entering adulthood is a complicated process, fraught with emotional overtones that must include medical care, work considerations, legal and financial arrangements, and, for many, the search for an appropriate residential environment. Planning for these transitions should begin years before adulthood if the process is to work smoothly and effectively.
A transition involving a shift away from a team of familiar pediatric healthcare providers to unfamiliar adult practitioners can be distressing for any adolescent with a chronic condition. For those with ASD, who may have diminished socialization and communication skills, the transition can be especially challenging and must be handled with care.
This transition pales in comparison with the disruptive force of a permanent move out of the family home. Over the next 10 years, 500,000 youths in the United States will age out of school-based ASD services,6 and a great many of them will be put on long waiting lists for residential placement.7
For young adults with ASD, particularly those with complex needs, establishing an advantageous long-term living arrangement may mean the difference between a healthy, self-directed launch into a new phase of life, or a consequential misstep that exacerbates or worsens symptoms and creates new stressors for the young adult and his or her family. It is especially important that arrangements be made before an aging guardian starts to experience declining health.
Thoughtful and deliberate preplanning helps to reduce stress and prevent emergency placements, and promotes long-term quality of life for people with ASD.
OUT OF THE INSTITUTION, INTO THE COMMUNITY
For many years, the prevailing model for the provision of long-term care services for individuals with intellectual and developmental disabilities was institutional care. Large facilities, often located in expansive, self-contained campuses, provided around-the-clock care. Residents slept, ate, worked, and were expected to receive social and emotional fulfillment at the facility.
For some, this was an acceptable model. For many, it was not, but there were few available alternatives. At its best, this model provided a safe environment for its residents, but it did not facilitate achieving an integrated, self-directed life experience. At its worst, neglect and abuse were rampant.
Numerous legislative acts, court decisions, and advocacy efforts drove the deinstitutionalization movement for individuals with intellectual and developmental disabilities between the early 1960s and today. The 1999 case of Olmstead v LC8 was among the most significant. In this landmark case, in accordance with the 1990 Americans With Disabilities Act, the US Supreme Court ruled that people with disabilities have the right to receive state-funded services and support in the community rather than in institutions, as long as several criteria are met:
- Community supports are appropriate
- The individual desires to live in the community
- The accommodations to facilitate that arrangement are considered to be reasonable.
In the 20 years since the Olmstead decision, residential services for adults have shifted at an accelerated rate away from institutions toward smaller, community-based settings.9,10 Community models include but are not limited to:
- Group homes that serve individuals with intellectual and developmental disabilities and provide 24-hour support
- Apartments or homes where individuals live and receive intermittent, less-intensive support
- Adult foster care.
DSM-5: AUTISM IS HETEROGENEOUS
In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5),11 ASD is characterized by persistent deficits in social interaction and social communication, which begin in early development and are observed in conjunction with restricted, repetitive behaviors, interests, or activities.
DSM-5 provides more than 20 examples of how these criteria might be met. Further, DSM-5 encourages clinicians to select diagnostic specifiers to address overall symptom severity, cognitive abilities, and associated medical conditions.
ONE RESIDENTIAL MODEL DOES NOT FIT ALL
The complex matrix of potential symptom manifestations in people with ASD clearly indicates the need for numerous distinctive residential models for adults with ASD.
One person with severe symptoms of ASD may require one-to-one staffing and proactive preparatory support in order to safely leave the house for a desired social experience. The person may be unable to read, to independently access public transportation, to cope with deviations in expected routine, to initiate conversation, or to remain calm if distressed. This person would benefit from a residential model that allows for a high staffing ratio, access to appropriate transportation, sophisticated autism-informed supports, and the availability of social experiences that are easily accessed—in other words, a very controlled environment.
Another person, with less severe symptoms and fewer behavioral challenges, who possesses a driver’s license and holds a job, may struggle with isolation and loneliness resulting from social inhibitions and skill deficits. This person’s support needs would differ, with emphasis placed on maintaining the appropriate social context rather than on providing a high level of individualized behavioral support.
The shift away from a one-size-fits-all institutional model for long-term care has benefited many individuals with intellectual and developmental disabilities who have experienced opportunities for community integration.
Still, for many adults with ASD, particularly those with complex needs and complex behavior profiles, the widespread conceptual shift to new and different models that assume that all people with intellectual and developmental disabilities will benefit from smaller, scattered-site settings is ill-fitting. It is erroneous to believe that for all adults with ASD, regardless of the complexity of their symptoms, living within a broader community of neurotypically developing neighbors breeds a richer sense of inclusion and connectivity.
FINDING CARE CAN BE DAUNTING
Families of adults with severe symptoms of ASD who seek placement in more traditional community residential models often find it difficult to find capable healthcare providers to serve them. Such settings are ill-equipped to deal with significantly challenging behaviors such as physical aggression, self-injury, property destruction, and elopement (wandering). These supported housing models lack the necessary staffing resources.
Further, publicly available funding options for stand-alone group homes do not typically allow for intensive supervision and management from professionals with expertise in autism. Without specialists who can implement autism-specific best-practice methods for assessment, service planning, staff training, data collection, and the provision of visual and technological supports for residents, it is difficult to achieve desired outcomes. For example, patients can find it challenging to visit physicians’ offices for preventive and urgent care. Lacking a caregiver who is familiar with the adult patient with ASD and who can help express his or her concerns to healthcare providers, efficient evaluation of any potentially serious medical issue is a daunting task.
INTENTIONAL COMMUNITIES
A residential model that is gaining popularity across the United States among families and individuals affected by ASD is the intentional community.
Although forms and functions may vary, intentional communities are planned residential developments that promote social cohesion and strive to meet the shared needs of its members. Intentional communities for adults with ASD are designed to meet their social, communication, sensory, and behavioral needs. Every detail from the selection of land, to the construction of housing, the selected staffing model, the daily structure, and the considerations for transportation and amenities are all informed by the specific needs of individuals with autism. Safety, integration, self-direction, independence, and social connectivity are common goals.
Successful intentional communities designed for people with intellectual and developmental disabilities often have facilities devoted to recreation, continuing education, socialization, and supportive services. Staff members who work within these communities are highly trained in the unique needs of people with these disorders. Intentional communities aspire to embody the individualized, integrated community-living approach that the Olmstead decision called for, while simultaneously offering the resource-rich, safe, and supportive experience that a campus atmosphere can offer.
Almost all recently developed models allow for residents to live among neurotypical peers and have easy access to the broader community. Communities range in size from several condominiums on a cul-de-sac to expansive developments with more than a hundred homes.
The allure of an ASD-informed intentional community that provides for the social, vocational, health, and safety needs of its residents is similar to that which leads large numbers of aging, neurotypically developing individuals to seek out retirement communities. Nationally recognized models of intentional communities include First Place (Phoenix, AZ), Sweetwater Spectrum (Sonoma, CA), Cape Cod Village (Orleans, MA), and Bittersweet Farms in Ohio.
First Place is a 55-unit apartment complex near downtown Phoenix that identifies as “community-connected” and “transit-oriented.” Although there are some individuals in the complex who do not have ASD, the development was created for those who do. The goal is to enhance the quality of life for residents through the provision of housing, jobs, social opportunities, and a supportive community.
Sweetwater Spectrum is located blocks from the Sonoma downtown plaza, on just under 3 acres of land. It includes several 4-bedroom homes, a community center with a kitchen, exercise studio, media room, and library, an expansive organic garden, and an outdoor pool.
The Autism Housing Network lists more than 75 intentional communities on its resource page. There are many exciting models in development. For example, Monarch Center for Autism in Cleveland, OH, is planning to develop an innovative intentional community. It will include mixed supported living options for adults across the autism spectrum, separate housing options for parents and family members, on-site social and recreational opportunities, green space, and retail stores intended to serve members of the surrounding community and provide employment and socialization opportunities for its residents.
Casa Familia in South Florida will soon begin constructing a large intentional community that will include innovative housing options, classrooms, social areas, an auditorium, walkways, bike paths, pools, and social enterprises.
It is critical that these ASD intentional communities continue to emerge to meet the long-term needs of the rapidly growing and aging ASD population.
THE TIME TO ACT IS NOW
Swetlik et al synthesize important, contemporary research on adult ASD healthcare considerations, pursuant to informing the many decisions that physicians and other healthcare professionals must make to address the diverse needs of this population. Their article advocates for further research and highlights the crisis surrounding the scarcity of practitioners specializing in adult ASD.
As for current healthcare providers, parents, care coordinators, and other stakeholders who are tasked with transition planning for individuals with ASD, particularly those with severe symptoms, the time to act is now, especially in creating new intentional community models.
Most adult healthcare providers have not been routinely charged with the responsibility, nor do they have the available time and resources to meet the social and communication needs of these patients. But when faced with an ever-expanding group of patients who demonstrate inadequate social and communication skills, the healthcare system must not turn a blind eye.
The symptoms of autism do not magically resolve when a child reaches adulthood. The medical community must partner with society at large to offer transitional solutions, including intentional communities, to the rapidly growing number of adults with ASD. Current demand outweighs supply, but if we work together, we can create innovative and highly effective solutions. After all, children with autism do not disappear. They grow into adults with autism.
- Baio J, Wiggins L, Christensen DL, et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2014. MMWR Surveill Summ 2018; 67(No. SS-6):1–23. doi:10.15585/mmwr.ss6706a1
- Remington B, Hastings RP, Kovshoff H, et al. Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 2007; 112(6):418-438. doi:10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators; Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2006. (Erratum in MMWR Surveill Summ 2010; 59[30]:956.) MMWR Surveill Summ 2009; 58(10):1–20. pmid:20023608
- Christensen DL, Baio J, Van Naarden Braun K, et al; Centers for Disease Control and Prevention (CDC). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Surveill Summ 2016; 65(3):1–23. doi:10.15585/mmwr.ss6503a1
- Swetlik C, Earp SE, Franco KN. Adults with autism spectrum disorder: updated considerations for healthcare providers. Cleve Clin J Med 2019; 86(8):543–553. doi:10.3949/ccjm.86a.18100
- Roux AM, Shattuck PT, Rast JE, Rava JA, Anderson KA. National Autism Indicators Report: Transition into Young Adulthood. Philadelphia, PA: Life Course Outcomes Research Program, A.J. Drexel Autism Institute, Drexel University, 2015.
- Gerhardt P. The Current State of Services for Adults with Autism. Organization for Autism Research, 2009. www.afaa-us.org/storage/documents/OAR_NYCA_survey_Current_State_of_Services_for_Adults_with_Autism.pdf. Accessed July 3, 2019.
- US Supreme Court. Olmstead v LC, US 527, 581 (1998).
- Braddock DL, Hemp RE, Tanis ES, Wu J, Haffer L. The State of the States in Intellectual and Developmental Disabilities, 11th edition. Washington D.C.: American Association on Intellectual and Developmental Disabilities, 2017.
- Larson SA, Eschenbacher HJ, Anderson LL, et al. In-home and residential long-term supports and services for persons with intellectual or developmental disabilities: status and trends through 2016. Minneapolis: University of Minnesota, Research and Training Center on Community Living, Institute on Community Integration, 2018. doi:10.13140/RG.2.2.11726.10567
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, D.C: American Psychiatric Association; 2013.
Autism spectrum disorder (ASD) is a neurodevelopmental condition typically diagnosed early in life: the median age at diagnosis is 52 months.1 Because research demonstrates the benefits of early intervention,2 when we think about people with ASD, we generally think about children and adolescents.
However, autism spans the entirety of one’s life. This means that children with ASD will grow to be adults with ASD. The US Centers for Disease Control and Prevention estimated that 1 in 59 children were diagnosed with ASD during the surveillance year 2014,1 which was nearly double the prevalence from just 8 years earlier,3 and a 15% increase since 2012.4 As these children grow up, this translates to an ever-growing number of adults with autism.
UNMET NEEDS
Healthcare, housing, and intellectual and developmental disability services for adults with ASD currently fall well short of meeting the needs of this exploding population. If solutions are to be realized, innovative approaches must be employed.
Swetlik et al,5 in this issue of the Journal, offer valuable insights into the challenges that practitioners and their adult patients with ASD encounter as a result of seismic shifts in diagnostic criteria, increasing prevalence, and changes to healthcare financial coverage. They also review behavioral and pharmacologic treatments, reproductive health, and caregiver fatigue and discuss the role of the physician and other healthcare practitioners who are likely to have only limited exposure to adult patients with ASD. These wide-ranging considerations speak to the complexity of the healthcare needs of this population.
Swetlik et al also underscore that transition planning is essential for primary care, psychiatry, behavioral health services, continuing education, skill development, and appropriate prevocational training for adolescents with ASD, and yet it is often underutilized or unavailable. There is a dearth of experienced practitioners across these disciplines to serve adults with ASD. The complexity of navigating bureaucratic processes to secure funding (typically Medicaid) supports the necessity of planning early to achieve desired outcomes for each young adult. Additionally, the number of Medicaid waivers that fund many supportive services are limited.
GROWING UP IS HARD; START PLANNING EARLY
Swetlik et al describe the stress these circumstances create for people with ASD and their families. Entering adulthood is a complicated process, fraught with emotional overtones that must include medical care, work considerations, legal and financial arrangements, and, for many, the search for an appropriate residential environment. Planning for these transitions should begin years before adulthood if the process is to work smoothly and effectively.
A transition involving a shift away from a team of familiar pediatric healthcare providers to unfamiliar adult practitioners can be distressing for any adolescent with a chronic condition. For those with ASD, who may have diminished socialization and communication skills, the transition can be especially challenging and must be handled with care.
This transition pales in comparison with the disruptive force of a permanent move out of the family home. Over the next 10 years, 500,000 youths in the United States will age out of school-based ASD services,6 and a great many of them will be put on long waiting lists for residential placement.7
For young adults with ASD, particularly those with complex needs, establishing an advantageous long-term living arrangement may mean the difference between a healthy, self-directed launch into a new phase of life, or a consequential misstep that exacerbates or worsens symptoms and creates new stressors for the young adult and his or her family. It is especially important that arrangements be made before an aging guardian starts to experience declining health.
Thoughtful and deliberate preplanning helps to reduce stress and prevent emergency placements, and promotes long-term quality of life for people with ASD.
OUT OF THE INSTITUTION, INTO THE COMMUNITY
For many years, the prevailing model for the provision of long-term care services for individuals with intellectual and developmental disabilities was institutional care. Large facilities, often located in expansive, self-contained campuses, provided around-the-clock care. Residents slept, ate, worked, and were expected to receive social and emotional fulfillment at the facility.
For some, this was an acceptable model. For many, it was not, but there were few available alternatives. At its best, this model provided a safe environment for its residents, but it did not facilitate achieving an integrated, self-directed life experience. At its worst, neglect and abuse were rampant.
Numerous legislative acts, court decisions, and advocacy efforts drove the deinstitutionalization movement for individuals with intellectual and developmental disabilities between the early 1960s and today. The 1999 case of Olmstead v LC8 was among the most significant. In this landmark case, in accordance with the 1990 Americans With Disabilities Act, the US Supreme Court ruled that people with disabilities have the right to receive state-funded services and support in the community rather than in institutions, as long as several criteria are met:
- Community supports are appropriate
- The individual desires to live in the community
- The accommodations to facilitate that arrangement are considered to be reasonable.
In the 20 years since the Olmstead decision, residential services for adults have shifted at an accelerated rate away from institutions toward smaller, community-based settings.9,10 Community models include but are not limited to:
- Group homes that serve individuals with intellectual and developmental disabilities and provide 24-hour support
- Apartments or homes where individuals live and receive intermittent, less-intensive support
- Adult foster care.
DSM-5: AUTISM IS HETEROGENEOUS
In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5),11 ASD is characterized by persistent deficits in social interaction and social communication, which begin in early development and are observed in conjunction with restricted, repetitive behaviors, interests, or activities.
DSM-5 provides more than 20 examples of how these criteria might be met. Further, DSM-5 encourages clinicians to select diagnostic specifiers to address overall symptom severity, cognitive abilities, and associated medical conditions.
ONE RESIDENTIAL MODEL DOES NOT FIT ALL
The complex matrix of potential symptom manifestations in people with ASD clearly indicates the need for numerous distinctive residential models for adults with ASD.
One person with severe symptoms of ASD may require one-to-one staffing and proactive preparatory support in order to safely leave the house for a desired social experience. The person may be unable to read, to independently access public transportation, to cope with deviations in expected routine, to initiate conversation, or to remain calm if distressed. This person would benefit from a residential model that allows for a high staffing ratio, access to appropriate transportation, sophisticated autism-informed supports, and the availability of social experiences that are easily accessed—in other words, a very controlled environment.
Another person, with less severe symptoms and fewer behavioral challenges, who possesses a driver’s license and holds a job, may struggle with isolation and loneliness resulting from social inhibitions and skill deficits. This person’s support needs would differ, with emphasis placed on maintaining the appropriate social context rather than on providing a high level of individualized behavioral support.
The shift away from a one-size-fits-all institutional model for long-term care has benefited many individuals with intellectual and developmental disabilities who have experienced opportunities for community integration.
Still, for many adults with ASD, particularly those with complex needs and complex behavior profiles, the widespread conceptual shift to new and different models that assume that all people with intellectual and developmental disabilities will benefit from smaller, scattered-site settings is ill-fitting. It is erroneous to believe that for all adults with ASD, regardless of the complexity of their symptoms, living within a broader community of neurotypically developing neighbors breeds a richer sense of inclusion and connectivity.
FINDING CARE CAN BE DAUNTING
Families of adults with severe symptoms of ASD who seek placement in more traditional community residential models often find it difficult to find capable healthcare providers to serve them. Such settings are ill-equipped to deal with significantly challenging behaviors such as physical aggression, self-injury, property destruction, and elopement (wandering). These supported housing models lack the necessary staffing resources.
Further, publicly available funding options for stand-alone group homes do not typically allow for intensive supervision and management from professionals with expertise in autism. Without specialists who can implement autism-specific best-practice methods for assessment, service planning, staff training, data collection, and the provision of visual and technological supports for residents, it is difficult to achieve desired outcomes. For example, patients can find it challenging to visit physicians’ offices for preventive and urgent care. Lacking a caregiver who is familiar with the adult patient with ASD and who can help express his or her concerns to healthcare providers, efficient evaluation of any potentially serious medical issue is a daunting task.
INTENTIONAL COMMUNITIES
A residential model that is gaining popularity across the United States among families and individuals affected by ASD is the intentional community.
Although forms and functions may vary, intentional communities are planned residential developments that promote social cohesion and strive to meet the shared needs of its members. Intentional communities for adults with ASD are designed to meet their social, communication, sensory, and behavioral needs. Every detail from the selection of land, to the construction of housing, the selected staffing model, the daily structure, and the considerations for transportation and amenities are all informed by the specific needs of individuals with autism. Safety, integration, self-direction, independence, and social connectivity are common goals.
Successful intentional communities designed for people with intellectual and developmental disabilities often have facilities devoted to recreation, continuing education, socialization, and supportive services. Staff members who work within these communities are highly trained in the unique needs of people with these disorders. Intentional communities aspire to embody the individualized, integrated community-living approach that the Olmstead decision called for, while simultaneously offering the resource-rich, safe, and supportive experience that a campus atmosphere can offer.
Almost all recently developed models allow for residents to live among neurotypical peers and have easy access to the broader community. Communities range in size from several condominiums on a cul-de-sac to expansive developments with more than a hundred homes.
The allure of an ASD-informed intentional community that provides for the social, vocational, health, and safety needs of its residents is similar to that which leads large numbers of aging, neurotypically developing individuals to seek out retirement communities. Nationally recognized models of intentional communities include First Place (Phoenix, AZ), Sweetwater Spectrum (Sonoma, CA), Cape Cod Village (Orleans, MA), and Bittersweet Farms in Ohio.
First Place is a 55-unit apartment complex near downtown Phoenix that identifies as “community-connected” and “transit-oriented.” Although there are some individuals in the complex who do not have ASD, the development was created for those who do. The goal is to enhance the quality of life for residents through the provision of housing, jobs, social opportunities, and a supportive community.
Sweetwater Spectrum is located blocks from the Sonoma downtown plaza, on just under 3 acres of land. It includes several 4-bedroom homes, a community center with a kitchen, exercise studio, media room, and library, an expansive organic garden, and an outdoor pool.
The Autism Housing Network lists more than 75 intentional communities on its resource page. There are many exciting models in development. For example, Monarch Center for Autism in Cleveland, OH, is planning to develop an innovative intentional community. It will include mixed supported living options for adults across the autism spectrum, separate housing options for parents and family members, on-site social and recreational opportunities, green space, and retail stores intended to serve members of the surrounding community and provide employment and socialization opportunities for its residents.
Casa Familia in South Florida will soon begin constructing a large intentional community that will include innovative housing options, classrooms, social areas, an auditorium, walkways, bike paths, pools, and social enterprises.
It is critical that these ASD intentional communities continue to emerge to meet the long-term needs of the rapidly growing and aging ASD population.
THE TIME TO ACT IS NOW
Swetlik et al synthesize important, contemporary research on adult ASD healthcare considerations, pursuant to informing the many decisions that physicians and other healthcare professionals must make to address the diverse needs of this population. Their article advocates for further research and highlights the crisis surrounding the scarcity of practitioners specializing in adult ASD.
As for current healthcare providers, parents, care coordinators, and other stakeholders who are tasked with transition planning for individuals with ASD, particularly those with severe symptoms, the time to act is now, especially in creating new intentional community models.
Most adult healthcare providers have not been routinely charged with the responsibility, nor do they have the available time and resources to meet the social and communication needs of these patients. But when faced with an ever-expanding group of patients who demonstrate inadequate social and communication skills, the healthcare system must not turn a blind eye.
The symptoms of autism do not magically resolve when a child reaches adulthood. The medical community must partner with society at large to offer transitional solutions, including intentional communities, to the rapidly growing number of adults with ASD. Current demand outweighs supply, but if we work together, we can create innovative and highly effective solutions. After all, children with autism do not disappear. They grow into adults with autism.
Autism spectrum disorder (ASD) is a neurodevelopmental condition typically diagnosed early in life: the median age at diagnosis is 52 months.1 Because research demonstrates the benefits of early intervention,2 when we think about people with ASD, we generally think about children and adolescents.
However, autism spans the entirety of one’s life. This means that children with ASD will grow to be adults with ASD. The US Centers for Disease Control and Prevention estimated that 1 in 59 children were diagnosed with ASD during the surveillance year 2014,1 which was nearly double the prevalence from just 8 years earlier,3 and a 15% increase since 2012.4 As these children grow up, this translates to an ever-growing number of adults with autism.
UNMET NEEDS
Healthcare, housing, and intellectual and developmental disability services for adults with ASD currently fall well short of meeting the needs of this exploding population. If solutions are to be realized, innovative approaches must be employed.
Swetlik et al,5 in this issue of the Journal, offer valuable insights into the challenges that practitioners and their adult patients with ASD encounter as a result of seismic shifts in diagnostic criteria, increasing prevalence, and changes to healthcare financial coverage. They also review behavioral and pharmacologic treatments, reproductive health, and caregiver fatigue and discuss the role of the physician and other healthcare practitioners who are likely to have only limited exposure to adult patients with ASD. These wide-ranging considerations speak to the complexity of the healthcare needs of this population.
Swetlik et al also underscore that transition planning is essential for primary care, psychiatry, behavioral health services, continuing education, skill development, and appropriate prevocational training for adolescents with ASD, and yet it is often underutilized or unavailable. There is a dearth of experienced practitioners across these disciplines to serve adults with ASD. The complexity of navigating bureaucratic processes to secure funding (typically Medicaid) supports the necessity of planning early to achieve desired outcomes for each young adult. Additionally, the number of Medicaid waivers that fund many supportive services are limited.
GROWING UP IS HARD; START PLANNING EARLY
Swetlik et al describe the stress these circumstances create for people with ASD and their families. Entering adulthood is a complicated process, fraught with emotional overtones that must include medical care, work considerations, legal and financial arrangements, and, for many, the search for an appropriate residential environment. Planning for these transitions should begin years before adulthood if the process is to work smoothly and effectively.
A transition involving a shift away from a team of familiar pediatric healthcare providers to unfamiliar adult practitioners can be distressing for any adolescent with a chronic condition. For those with ASD, who may have diminished socialization and communication skills, the transition can be especially challenging and must be handled with care.
This transition pales in comparison with the disruptive force of a permanent move out of the family home. Over the next 10 years, 500,000 youths in the United States will age out of school-based ASD services,6 and a great many of them will be put on long waiting lists for residential placement.7
For young adults with ASD, particularly those with complex needs, establishing an advantageous long-term living arrangement may mean the difference between a healthy, self-directed launch into a new phase of life, or a consequential misstep that exacerbates or worsens symptoms and creates new stressors for the young adult and his or her family. It is especially important that arrangements be made before an aging guardian starts to experience declining health.
Thoughtful and deliberate preplanning helps to reduce stress and prevent emergency placements, and promotes long-term quality of life for people with ASD.
OUT OF THE INSTITUTION, INTO THE COMMUNITY
For many years, the prevailing model for the provision of long-term care services for individuals with intellectual and developmental disabilities was institutional care. Large facilities, often located in expansive, self-contained campuses, provided around-the-clock care. Residents slept, ate, worked, and were expected to receive social and emotional fulfillment at the facility.
For some, this was an acceptable model. For many, it was not, but there were few available alternatives. At its best, this model provided a safe environment for its residents, but it did not facilitate achieving an integrated, self-directed life experience. At its worst, neglect and abuse were rampant.
Numerous legislative acts, court decisions, and advocacy efforts drove the deinstitutionalization movement for individuals with intellectual and developmental disabilities between the early 1960s and today. The 1999 case of Olmstead v LC8 was among the most significant. In this landmark case, in accordance with the 1990 Americans With Disabilities Act, the US Supreme Court ruled that people with disabilities have the right to receive state-funded services and support in the community rather than in institutions, as long as several criteria are met:
- Community supports are appropriate
- The individual desires to live in the community
- The accommodations to facilitate that arrangement are considered to be reasonable.
In the 20 years since the Olmstead decision, residential services for adults have shifted at an accelerated rate away from institutions toward smaller, community-based settings.9,10 Community models include but are not limited to:
- Group homes that serve individuals with intellectual and developmental disabilities and provide 24-hour support
- Apartments or homes where individuals live and receive intermittent, less-intensive support
- Adult foster care.
DSM-5: AUTISM IS HETEROGENEOUS
In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5),11 ASD is characterized by persistent deficits in social interaction and social communication, which begin in early development and are observed in conjunction with restricted, repetitive behaviors, interests, or activities.
DSM-5 provides more than 20 examples of how these criteria might be met. Further, DSM-5 encourages clinicians to select diagnostic specifiers to address overall symptom severity, cognitive abilities, and associated medical conditions.
ONE RESIDENTIAL MODEL DOES NOT FIT ALL
The complex matrix of potential symptom manifestations in people with ASD clearly indicates the need for numerous distinctive residential models for adults with ASD.
One person with severe symptoms of ASD may require one-to-one staffing and proactive preparatory support in order to safely leave the house for a desired social experience. The person may be unable to read, to independently access public transportation, to cope with deviations in expected routine, to initiate conversation, or to remain calm if distressed. This person would benefit from a residential model that allows for a high staffing ratio, access to appropriate transportation, sophisticated autism-informed supports, and the availability of social experiences that are easily accessed—in other words, a very controlled environment.
Another person, with less severe symptoms and fewer behavioral challenges, who possesses a driver’s license and holds a job, may struggle with isolation and loneliness resulting from social inhibitions and skill deficits. This person’s support needs would differ, with emphasis placed on maintaining the appropriate social context rather than on providing a high level of individualized behavioral support.
The shift away from a one-size-fits-all institutional model for long-term care has benefited many individuals with intellectual and developmental disabilities who have experienced opportunities for community integration.
Still, for many adults with ASD, particularly those with complex needs and complex behavior profiles, the widespread conceptual shift to new and different models that assume that all people with intellectual and developmental disabilities will benefit from smaller, scattered-site settings is ill-fitting. It is erroneous to believe that for all adults with ASD, regardless of the complexity of their symptoms, living within a broader community of neurotypically developing neighbors breeds a richer sense of inclusion and connectivity.
FINDING CARE CAN BE DAUNTING
Families of adults with severe symptoms of ASD who seek placement in more traditional community residential models often find it difficult to find capable healthcare providers to serve them. Such settings are ill-equipped to deal with significantly challenging behaviors such as physical aggression, self-injury, property destruction, and elopement (wandering). These supported housing models lack the necessary staffing resources.
Further, publicly available funding options for stand-alone group homes do not typically allow for intensive supervision and management from professionals with expertise in autism. Without specialists who can implement autism-specific best-practice methods for assessment, service planning, staff training, data collection, and the provision of visual and technological supports for residents, it is difficult to achieve desired outcomes. For example, patients can find it challenging to visit physicians’ offices for preventive and urgent care. Lacking a caregiver who is familiar with the adult patient with ASD and who can help express his or her concerns to healthcare providers, efficient evaluation of any potentially serious medical issue is a daunting task.
INTENTIONAL COMMUNITIES
A residential model that is gaining popularity across the United States among families and individuals affected by ASD is the intentional community.
Although forms and functions may vary, intentional communities are planned residential developments that promote social cohesion and strive to meet the shared needs of its members. Intentional communities for adults with ASD are designed to meet their social, communication, sensory, and behavioral needs. Every detail from the selection of land, to the construction of housing, the selected staffing model, the daily structure, and the considerations for transportation and amenities are all informed by the specific needs of individuals with autism. Safety, integration, self-direction, independence, and social connectivity are common goals.
Successful intentional communities designed for people with intellectual and developmental disabilities often have facilities devoted to recreation, continuing education, socialization, and supportive services. Staff members who work within these communities are highly trained in the unique needs of people with these disorders. Intentional communities aspire to embody the individualized, integrated community-living approach that the Olmstead decision called for, while simultaneously offering the resource-rich, safe, and supportive experience that a campus atmosphere can offer.
Almost all recently developed models allow for residents to live among neurotypical peers and have easy access to the broader community. Communities range in size from several condominiums on a cul-de-sac to expansive developments with more than a hundred homes.
The allure of an ASD-informed intentional community that provides for the social, vocational, health, and safety needs of its residents is similar to that which leads large numbers of aging, neurotypically developing individuals to seek out retirement communities. Nationally recognized models of intentional communities include First Place (Phoenix, AZ), Sweetwater Spectrum (Sonoma, CA), Cape Cod Village (Orleans, MA), and Bittersweet Farms in Ohio.
First Place is a 55-unit apartment complex near downtown Phoenix that identifies as “community-connected” and “transit-oriented.” Although there are some individuals in the complex who do not have ASD, the development was created for those who do. The goal is to enhance the quality of life for residents through the provision of housing, jobs, social opportunities, and a supportive community.
Sweetwater Spectrum is located blocks from the Sonoma downtown plaza, on just under 3 acres of land. It includes several 4-bedroom homes, a community center with a kitchen, exercise studio, media room, and library, an expansive organic garden, and an outdoor pool.
The Autism Housing Network lists more than 75 intentional communities on its resource page. There are many exciting models in development. For example, Monarch Center for Autism in Cleveland, OH, is planning to develop an innovative intentional community. It will include mixed supported living options for adults across the autism spectrum, separate housing options for parents and family members, on-site social and recreational opportunities, green space, and retail stores intended to serve members of the surrounding community and provide employment and socialization opportunities for its residents.
Casa Familia in South Florida will soon begin constructing a large intentional community that will include innovative housing options, classrooms, social areas, an auditorium, walkways, bike paths, pools, and social enterprises.
It is critical that these ASD intentional communities continue to emerge to meet the long-term needs of the rapidly growing and aging ASD population.
THE TIME TO ACT IS NOW
Swetlik et al synthesize important, contemporary research on adult ASD healthcare considerations, pursuant to informing the many decisions that physicians and other healthcare professionals must make to address the diverse needs of this population. Their article advocates for further research and highlights the crisis surrounding the scarcity of practitioners specializing in adult ASD.
As for current healthcare providers, parents, care coordinators, and other stakeholders who are tasked with transition planning for individuals with ASD, particularly those with severe symptoms, the time to act is now, especially in creating new intentional community models.
Most adult healthcare providers have not been routinely charged with the responsibility, nor do they have the available time and resources to meet the social and communication needs of these patients. But when faced with an ever-expanding group of patients who demonstrate inadequate social and communication skills, the healthcare system must not turn a blind eye.
The symptoms of autism do not magically resolve when a child reaches adulthood. The medical community must partner with society at large to offer transitional solutions, including intentional communities, to the rapidly growing number of adults with ASD. Current demand outweighs supply, but if we work together, we can create innovative and highly effective solutions. After all, children with autism do not disappear. They grow into adults with autism.
- Baio J, Wiggins L, Christensen DL, et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2014. MMWR Surveill Summ 2018; 67(No. SS-6):1–23. doi:10.15585/mmwr.ss6706a1
- Remington B, Hastings RP, Kovshoff H, et al. Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 2007; 112(6):418-438. doi:10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators; Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2006. (Erratum in MMWR Surveill Summ 2010; 59[30]:956.) MMWR Surveill Summ 2009; 58(10):1–20. pmid:20023608
- Christensen DL, Baio J, Van Naarden Braun K, et al; Centers for Disease Control and Prevention (CDC). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Surveill Summ 2016; 65(3):1–23. doi:10.15585/mmwr.ss6503a1
- Swetlik C, Earp SE, Franco KN. Adults with autism spectrum disorder: updated considerations for healthcare providers. Cleve Clin J Med 2019; 86(8):543–553. doi:10.3949/ccjm.86a.18100
- Roux AM, Shattuck PT, Rast JE, Rava JA, Anderson KA. National Autism Indicators Report: Transition into Young Adulthood. Philadelphia, PA: Life Course Outcomes Research Program, A.J. Drexel Autism Institute, Drexel University, 2015.
- Gerhardt P. The Current State of Services for Adults with Autism. Organization for Autism Research, 2009. www.afaa-us.org/storage/documents/OAR_NYCA_survey_Current_State_of_Services_for_Adults_with_Autism.pdf. Accessed July 3, 2019.
- US Supreme Court. Olmstead v LC, US 527, 581 (1998).
- Braddock DL, Hemp RE, Tanis ES, Wu J, Haffer L. The State of the States in Intellectual and Developmental Disabilities, 11th edition. Washington D.C.: American Association on Intellectual and Developmental Disabilities, 2017.
- Larson SA, Eschenbacher HJ, Anderson LL, et al. In-home and residential long-term supports and services for persons with intellectual or developmental disabilities: status and trends through 2016. Minneapolis: University of Minnesota, Research and Training Center on Community Living, Institute on Community Integration, 2018. doi:10.13140/RG.2.2.11726.10567
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, D.C: American Psychiatric Association; 2013.
- Baio J, Wiggins L, Christensen DL, et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2014. MMWR Surveill Summ 2018; 67(No. SS-6):1–23. doi:10.15585/mmwr.ss6706a1
- Remington B, Hastings RP, Kovshoff H, et al. Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 2007; 112(6):418-438. doi:10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators; Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2006. (Erratum in MMWR Surveill Summ 2010; 59[30]:956.) MMWR Surveill Summ 2009; 58(10):1–20. pmid:20023608
- Christensen DL, Baio J, Van Naarden Braun K, et al; Centers for Disease Control and Prevention (CDC). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Surveill Summ 2016; 65(3):1–23. doi:10.15585/mmwr.ss6503a1
- Swetlik C, Earp SE, Franco KN. Adults with autism spectrum disorder: updated considerations for healthcare providers. Cleve Clin J Med 2019; 86(8):543–553. doi:10.3949/ccjm.86a.18100
- Roux AM, Shattuck PT, Rast JE, Rava JA, Anderson KA. National Autism Indicators Report: Transition into Young Adulthood. Philadelphia, PA: Life Course Outcomes Research Program, A.J. Drexel Autism Institute, Drexel University, 2015.
- Gerhardt P. The Current State of Services for Adults with Autism. Organization for Autism Research, 2009. www.afaa-us.org/storage/documents/OAR_NYCA_survey_Current_State_of_Services_for_Adults_with_Autism.pdf. Accessed July 3, 2019.
- US Supreme Court. Olmstead v LC, US 527, 581 (1998).
- Braddock DL, Hemp RE, Tanis ES, Wu J, Haffer L. The State of the States in Intellectual and Developmental Disabilities, 11th edition. Washington D.C.: American Association on Intellectual and Developmental Disabilities, 2017.
- Larson SA, Eschenbacher HJ, Anderson LL, et al. In-home and residential long-term supports and services for persons with intellectual or developmental disabilities: status and trends through 2016. Minneapolis: University of Minnesota, Research and Training Center on Community Living, Institute on Community Integration, 2018. doi:10.13140/RG.2.2.11726.10567
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, D.C: American Psychiatric Association; 2013.
Interhospital Transfers for Quality Assessment of Healthcare Systems
With the increasing percentage of our gross national product being allotted to healthcare and concerns about the care received by patients, the number of measures to assess the quality and efficiency of care delivered by healthcare professionals has increased. The paper by Mueller et al.1 adds to our understanding of an important yet relatively understudied group of patients: those that require transfer from one inpatient facility to another. In general, these patients are sicker and exhibit poor outcomes, especially with time-sensitive management conditions, such as cerebrovascular accidents, or conditions where the transfer itself may cause harm to the patient, such as the case of an infant born prematurely. However, transferring patients with less time-dependent conditions may not be associated with such negative results.1 The uniqueness of interhospital transfers is attributed to their ability to provide insights into the care practices of other actors within the healthcare system, namely, the transferring hospital and the larger healthcare system, and to describe how the care quality may change in hospitals during periods of stress, such as during overcrowding or high patient acuity.
As described by Mueller et al. the care and outcomes of patients transferred to a hospital may provide information regarding the key aspects of care at the receiving hospital; these aspects include the capability for triage of potentially high-acuity patients and the management of such patients during periods of crowding and organizational stress. These measures of efficiency have rarely been studied in relation to the care provided to patients and their ultimate outcomes. The most studied efficiency measure is hospital crowding, which has been shown in numerous studies to be associated with lower efficiency as measured by the length of stay, lower quality of care, and higher mortality.2-3 This report by Mueller et al. is one of the first papers to highlight how other aspects of the care delivery system, including the triage practices and the response of a hospital system to stress, may influence care outcomes. The limitation of other studies in exploring the relationship between the measures of efficiency and quality of care, as noted by a systematic review of healthcare efficiency measures by Hussey et al.4 emphasizes the need to understand the drivers of low quality of care and to determine the specific times at which such care may be compromised by other factors, such as patient volumes.
Although interhospital transfers may offer certain insights into the efficiency of care delivered at the hospitals receiving these patients, they are generally rare and centered on a few quaternary hospitals within a region.3 In addition, the Mueller paper reveals that not all these transfers have high disease acuity, particularly for cardiac patients. Whether claims-based approaches to risk adjustment would sufficiently differentiate the reasons for the transfer/failure to transfer of patients is unclear and thus may be affected by the selection bias. With these issues, the outcome of transferred patients may be only of limited value when assessing the care quality of hospitals that generally receive transferred patients from other medical institutions within a given geographic area.5
Interhospital transfers may provide insights into the care of patients at the hospitals which transfer out such patients, focusing on the appropriateness of transfers, how these hospitals operate when such a sick patient arrives at that hospital, and the outcomes of patients with conditions that may require transfer. A few studies have explored the preventable transfer, particularly for trauma patients, where a preventable transfer was defined as a transfer that was was not admitted to the receiving hospital and did not receive any procedures or testing. Although not readily defined for numerous conditions, such a measure would provide insights into how hospitals decide whether a patient requires care at a higher-level hospital and assessing the processes needed to optimize this decision-making process, including where the patient ultimately is transferred. In a study of patients with acute myocardial infarction, 36.8% of cases that required transfer were not directed to hospitals with the best outcomes as measured by 30-day risk-adjusted mortality rates within a given geographic region.6 Such decisions would contribute to the potential worse outcomes observed in patients requiring interhospital transfer.
Finally, transfers provide insights into the functioning of the larger healthcare system. The measures assessing the functioning of the healthcare system are rare. In theory, interhospital transfers meet the goals of a functioning regional healthcare system by matching the patients to facilities with the suitable capabilities to manage the patient’s given type of illness or injury. Such a system, however, requires collaboration between hospitals who otherwise compete for patients. The literature suggests that such collaboration is widely variable and dependent on patient factors, such as the types of conditions and their insurance status,7 and the costs required by hospitals to add the services needed to care for increasingly ill patients. In addition, the growth of so-called narrow insurance networks, which limit the number of hospitals an insurance company will include on their preferred network, may place barriers on the appropriate location of such transfers based on the quality of the receiving hospital.8
The paper by Mueller et al. adds to the literature the unique aspects of the care needed by the patients requiring interhospital transfer. Unlike most other measures of care quality and efficiency, interhospital transfers potentially offer knowledge about the quality of the larger healthcare system, assessing the appropriateness and ultimate outcomes not only of patients who are transferred but similarly sick patients who could have potentially benefited from a transfer and how the actors within the system may respond to periods of high patient load and stress. By understanding the drivers of the appropriateness of where patients receive care, we can gain insights into the mechanisms needed to fulfill the goals of a functional regionalized healthcare system.
Disclosures
The author has no financial or other relevant conflicts of interest to disclose.
1. Mueller SK, Fiskio J, Schnipper J. Interhospital transfer: transfer processes and patient outcomes. J Hosp Med. 2019;(8):486-491. https://doi.org/10.12788/jhm.3192.
2. Lorch SA, Millman AM, Zhang X, Even-Shoshan O, Silber JH. Impact of admission-day crowding on the length of stay of pediatric hospitalizations. Pediatrics. 2008;121(4):e718-e730. https://doi.org/10.1542/peds.2007-1280.
3. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605-611.e6. https://doi.org/10.1016/j.annemergmed.2012.10.026
4. Hussey PS, de Vries H, Romley J, et al. A systematic review of health care efficiency measures. Health Serv Res. 2009;44(3):784-805. https://doi.org/10.1111/j.1475-6773.2008.00942.x.
5. Lorch SA. National quality measures in perinatal medicine. Clin Perinatol. 2017;44(3):485-509. https://doi.org/10.1016/j.clp.2017.05.001
6. Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes. 2010;3(5):468-475. https://doi.org/10.1161/CIRCOUTCOMES.110.957993.
7. Green A, Showstack J, Rennie D, Goldman L. The relationship of insurance status, hospital ownership, and teaching status with interhospital transfers in California in 2000. Acad Med. 2005;80(8):774-779. https://doi.org/10.1097/00001888-200508000-00015
8. Colvin JD, Hall M, Thurm C, et al. Hypothetical network adequacy schemes for children fail to ensure patients’ access to in-network children’s hospital. Health Aff (Millwood). 2018;37(6):873-880. https://doi.org/10.1377/hlthaff.2017.1339.
With the increasing percentage of our gross national product being allotted to healthcare and concerns about the care received by patients, the number of measures to assess the quality and efficiency of care delivered by healthcare professionals has increased. The paper by Mueller et al.1 adds to our understanding of an important yet relatively understudied group of patients: those that require transfer from one inpatient facility to another. In general, these patients are sicker and exhibit poor outcomes, especially with time-sensitive management conditions, such as cerebrovascular accidents, or conditions where the transfer itself may cause harm to the patient, such as the case of an infant born prematurely. However, transferring patients with less time-dependent conditions may not be associated with such negative results.1 The uniqueness of interhospital transfers is attributed to their ability to provide insights into the care practices of other actors within the healthcare system, namely, the transferring hospital and the larger healthcare system, and to describe how the care quality may change in hospitals during periods of stress, such as during overcrowding or high patient acuity.
As described by Mueller et al. the care and outcomes of patients transferred to a hospital may provide information regarding the key aspects of care at the receiving hospital; these aspects include the capability for triage of potentially high-acuity patients and the management of such patients during periods of crowding and organizational stress. These measures of efficiency have rarely been studied in relation to the care provided to patients and their ultimate outcomes. The most studied efficiency measure is hospital crowding, which has been shown in numerous studies to be associated with lower efficiency as measured by the length of stay, lower quality of care, and higher mortality.2-3 This report by Mueller et al. is one of the first papers to highlight how other aspects of the care delivery system, including the triage practices and the response of a hospital system to stress, may influence care outcomes. The limitation of other studies in exploring the relationship between the measures of efficiency and quality of care, as noted by a systematic review of healthcare efficiency measures by Hussey et al.4 emphasizes the need to understand the drivers of low quality of care and to determine the specific times at which such care may be compromised by other factors, such as patient volumes.
Although interhospital transfers may offer certain insights into the efficiency of care delivered at the hospitals receiving these patients, they are generally rare and centered on a few quaternary hospitals within a region.3 In addition, the Mueller paper reveals that not all these transfers have high disease acuity, particularly for cardiac patients. Whether claims-based approaches to risk adjustment would sufficiently differentiate the reasons for the transfer/failure to transfer of patients is unclear and thus may be affected by the selection bias. With these issues, the outcome of transferred patients may be only of limited value when assessing the care quality of hospitals that generally receive transferred patients from other medical institutions within a given geographic area.5
Interhospital transfers may provide insights into the care of patients at the hospitals which transfer out such patients, focusing on the appropriateness of transfers, how these hospitals operate when such a sick patient arrives at that hospital, and the outcomes of patients with conditions that may require transfer. A few studies have explored the preventable transfer, particularly for trauma patients, where a preventable transfer was defined as a transfer that was was not admitted to the receiving hospital and did not receive any procedures or testing. Although not readily defined for numerous conditions, such a measure would provide insights into how hospitals decide whether a patient requires care at a higher-level hospital and assessing the processes needed to optimize this decision-making process, including where the patient ultimately is transferred. In a study of patients with acute myocardial infarction, 36.8% of cases that required transfer were not directed to hospitals with the best outcomes as measured by 30-day risk-adjusted mortality rates within a given geographic region.6 Such decisions would contribute to the potential worse outcomes observed in patients requiring interhospital transfer.
Finally, transfers provide insights into the functioning of the larger healthcare system. The measures assessing the functioning of the healthcare system are rare. In theory, interhospital transfers meet the goals of a functioning regional healthcare system by matching the patients to facilities with the suitable capabilities to manage the patient’s given type of illness or injury. Such a system, however, requires collaboration between hospitals who otherwise compete for patients. The literature suggests that such collaboration is widely variable and dependent on patient factors, such as the types of conditions and their insurance status,7 and the costs required by hospitals to add the services needed to care for increasingly ill patients. In addition, the growth of so-called narrow insurance networks, which limit the number of hospitals an insurance company will include on their preferred network, may place barriers on the appropriate location of such transfers based on the quality of the receiving hospital.8
The paper by Mueller et al. adds to the literature the unique aspects of the care needed by the patients requiring interhospital transfer. Unlike most other measures of care quality and efficiency, interhospital transfers potentially offer knowledge about the quality of the larger healthcare system, assessing the appropriateness and ultimate outcomes not only of patients who are transferred but similarly sick patients who could have potentially benefited from a transfer and how the actors within the system may respond to periods of high patient load and stress. By understanding the drivers of the appropriateness of where patients receive care, we can gain insights into the mechanisms needed to fulfill the goals of a functional regionalized healthcare system.
Disclosures
The author has no financial or other relevant conflicts of interest to disclose.
With the increasing percentage of our gross national product being allotted to healthcare and concerns about the care received by patients, the number of measures to assess the quality and efficiency of care delivered by healthcare professionals has increased. The paper by Mueller et al.1 adds to our understanding of an important yet relatively understudied group of patients: those that require transfer from one inpatient facility to another. In general, these patients are sicker and exhibit poor outcomes, especially with time-sensitive management conditions, such as cerebrovascular accidents, or conditions where the transfer itself may cause harm to the patient, such as the case of an infant born prematurely. However, transferring patients with less time-dependent conditions may not be associated with such negative results.1 The uniqueness of interhospital transfers is attributed to their ability to provide insights into the care practices of other actors within the healthcare system, namely, the transferring hospital and the larger healthcare system, and to describe how the care quality may change in hospitals during periods of stress, such as during overcrowding or high patient acuity.
As described by Mueller et al. the care and outcomes of patients transferred to a hospital may provide information regarding the key aspects of care at the receiving hospital; these aspects include the capability for triage of potentially high-acuity patients and the management of such patients during periods of crowding and organizational stress. These measures of efficiency have rarely been studied in relation to the care provided to patients and their ultimate outcomes. The most studied efficiency measure is hospital crowding, which has been shown in numerous studies to be associated with lower efficiency as measured by the length of stay, lower quality of care, and higher mortality.2-3 This report by Mueller et al. is one of the first papers to highlight how other aspects of the care delivery system, including the triage practices and the response of a hospital system to stress, may influence care outcomes. The limitation of other studies in exploring the relationship between the measures of efficiency and quality of care, as noted by a systematic review of healthcare efficiency measures by Hussey et al.4 emphasizes the need to understand the drivers of low quality of care and to determine the specific times at which such care may be compromised by other factors, such as patient volumes.
Although interhospital transfers may offer certain insights into the efficiency of care delivered at the hospitals receiving these patients, they are generally rare and centered on a few quaternary hospitals within a region.3 In addition, the Mueller paper reveals that not all these transfers have high disease acuity, particularly for cardiac patients. Whether claims-based approaches to risk adjustment would sufficiently differentiate the reasons for the transfer/failure to transfer of patients is unclear and thus may be affected by the selection bias. With these issues, the outcome of transferred patients may be only of limited value when assessing the care quality of hospitals that generally receive transferred patients from other medical institutions within a given geographic area.5
Interhospital transfers may provide insights into the care of patients at the hospitals which transfer out such patients, focusing on the appropriateness of transfers, how these hospitals operate when such a sick patient arrives at that hospital, and the outcomes of patients with conditions that may require transfer. A few studies have explored the preventable transfer, particularly for trauma patients, where a preventable transfer was defined as a transfer that was was not admitted to the receiving hospital and did not receive any procedures or testing. Although not readily defined for numerous conditions, such a measure would provide insights into how hospitals decide whether a patient requires care at a higher-level hospital and assessing the processes needed to optimize this decision-making process, including where the patient ultimately is transferred. In a study of patients with acute myocardial infarction, 36.8% of cases that required transfer were not directed to hospitals with the best outcomes as measured by 30-day risk-adjusted mortality rates within a given geographic region.6 Such decisions would contribute to the potential worse outcomes observed in patients requiring interhospital transfer.
Finally, transfers provide insights into the functioning of the larger healthcare system. The measures assessing the functioning of the healthcare system are rare. In theory, interhospital transfers meet the goals of a functioning regional healthcare system by matching the patients to facilities with the suitable capabilities to manage the patient’s given type of illness or injury. Such a system, however, requires collaboration between hospitals who otherwise compete for patients. The literature suggests that such collaboration is widely variable and dependent on patient factors, such as the types of conditions and their insurance status,7 and the costs required by hospitals to add the services needed to care for increasingly ill patients. In addition, the growth of so-called narrow insurance networks, which limit the number of hospitals an insurance company will include on their preferred network, may place barriers on the appropriate location of such transfers based on the quality of the receiving hospital.8
The paper by Mueller et al. adds to the literature the unique aspects of the care needed by the patients requiring interhospital transfer. Unlike most other measures of care quality and efficiency, interhospital transfers potentially offer knowledge about the quality of the larger healthcare system, assessing the appropriateness and ultimate outcomes not only of patients who are transferred but similarly sick patients who could have potentially benefited from a transfer and how the actors within the system may respond to periods of high patient load and stress. By understanding the drivers of the appropriateness of where patients receive care, we can gain insights into the mechanisms needed to fulfill the goals of a functional regionalized healthcare system.
Disclosures
The author has no financial or other relevant conflicts of interest to disclose.
1. Mueller SK, Fiskio J, Schnipper J. Interhospital transfer: transfer processes and patient outcomes. J Hosp Med. 2019;(8):486-491. https://doi.org/10.12788/jhm.3192.
2. Lorch SA, Millman AM, Zhang X, Even-Shoshan O, Silber JH. Impact of admission-day crowding on the length of stay of pediatric hospitalizations. Pediatrics. 2008;121(4):e718-e730. https://doi.org/10.1542/peds.2007-1280.
3. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605-611.e6. https://doi.org/10.1016/j.annemergmed.2012.10.026
4. Hussey PS, de Vries H, Romley J, et al. A systematic review of health care efficiency measures. Health Serv Res. 2009;44(3):784-805. https://doi.org/10.1111/j.1475-6773.2008.00942.x.
5. Lorch SA. National quality measures in perinatal medicine. Clin Perinatol. 2017;44(3):485-509. https://doi.org/10.1016/j.clp.2017.05.001
6. Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes. 2010;3(5):468-475. https://doi.org/10.1161/CIRCOUTCOMES.110.957993.
7. Green A, Showstack J, Rennie D, Goldman L. The relationship of insurance status, hospital ownership, and teaching status with interhospital transfers in California in 2000. Acad Med. 2005;80(8):774-779. https://doi.org/10.1097/00001888-200508000-00015
8. Colvin JD, Hall M, Thurm C, et al. Hypothetical network adequacy schemes for children fail to ensure patients’ access to in-network children’s hospital. Health Aff (Millwood). 2018;37(6):873-880. https://doi.org/10.1377/hlthaff.2017.1339.
1. Mueller SK, Fiskio J, Schnipper J. Interhospital transfer: transfer processes and patient outcomes. J Hosp Med. 2019;(8):486-491. https://doi.org/10.12788/jhm.3192.
2. Lorch SA, Millman AM, Zhang X, Even-Shoshan O, Silber JH. Impact of admission-day crowding on the length of stay of pediatric hospitalizations. Pediatrics. 2008;121(4):e718-e730. https://doi.org/10.1542/peds.2007-1280.
3. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605-611.e6. https://doi.org/10.1016/j.annemergmed.2012.10.026
4. Hussey PS, de Vries H, Romley J, et al. A systematic review of health care efficiency measures. Health Serv Res. 2009;44(3):784-805. https://doi.org/10.1111/j.1475-6773.2008.00942.x.
5. Lorch SA. National quality measures in perinatal medicine. Clin Perinatol. 2017;44(3):485-509. https://doi.org/10.1016/j.clp.2017.05.001
6. Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes. 2010;3(5):468-475. https://doi.org/10.1161/CIRCOUTCOMES.110.957993.
7. Green A, Showstack J, Rennie D, Goldman L. The relationship of insurance status, hospital ownership, and teaching status with interhospital transfers in California in 2000. Acad Med. 2005;80(8):774-779. https://doi.org/10.1097/00001888-200508000-00015
8. Colvin JD, Hall M, Thurm C, et al. Hypothetical network adequacy schemes for children fail to ensure patients’ access to in-network children’s hospital. Health Aff (Millwood). 2018;37(6):873-880. https://doi.org/10.1377/hlthaff.2017.1339.
© 2019 Society of Hospital Medicine
Quantity, Quality, or Neither–Measuring the Effectiveness of Rounds
Medicine has a rich history of attending-led rounds, with some iteration of this ritual occurring as far back as the 1600s.1 In the early 1900s, the concept of “bedside rounds” was popularized by William Osler, who widely espoused their importance as a clinical and educational tool. Despite our best intentions, however, rounds today may be little reminiscent of the rounds of Osler’s day. Recent investigations into the characteristics of rounds have specifically revealed a “shift in the format from the beside to conference rooms and hallways.”2 Most of our practices for rounding in the modern era are built on tradition and belief rather than evidence. The ecosystem of modern hospital care is dramatically different than that of Osler’s day, and fundamental questions about the format, content, stakeholders, and processes of rounds remain. Perhaps the greatest and most needed change in rounding in recent years is the shift of rounds from a physician-centric activity to an activity that values the modern interprofessional hospital team. Ultimately, the very definition of “rounds” and the purpose they are meant to serve in the context of a dynamic and complicated hospital ecosystem has become increasingly complex and thus, difficult to assess and improve.
In this month’s Journal of Hospital Medicine, Sang et al.3 address this complexity by returning to basics and utilizing a novel approach to precisely measure the frequency and duration of a necessary (albeit insufficient) condition for interdisciplinary bedside rounding to occur: colocation of physician, nurse, and patient. Ultimately, their results provide a springboard to ask more complex and meaningful questions. Why, despite a recent culture shift prioritizing a return to bedside, is substantive physician and nurse colocation so persistently difficult to attain? How can we study outcomes of interdisciplinary bedside rounds if we cannot reliably facilitate their occurrence? What does “effective” rounding even mean? That is, what variables would be both meaningful and sensitive to changes in rounds?
After centuries of rounding, the medical community would be presumed to have perfected this art; however, we are instead left with more questions than answers. Prior research efforts have demonstrated the shifting of rounds away from the bedside, with bedside rounds occurring only 10%-40% of the time based on bias-prone survey data.2,4 Interestingly, a study by Huang et al., designed specifically to increase implementation of interdisciplinary bedside rounds, showed a frequency of only 64%.5 These studies are focused primarily on parameters such as patient and nursing satisfaction and did not include other important outcomes such as length of stay, readmission rates, diagnostic quality, patient engagement, or mortality.2,4,6
In Sang et al.,3 the authors utilized a real-time locator system, namely, radiofrequency identification, to precisely track the physical workflow of both attending hospitalists and bedside nurses and then subsequently used the data obtained to measure the frequency and duration of colocation at the patient bedside. The authors defined a physician “rounding event” as the physician’s presence in a single bed patient room for at least 10 seconds. The study revealed that colocation of physician and nurse (for at least 10 seconds) occurred in only 30% of all physician rounding events recorded. The duration of a physician rounding event was 5.68 minutes without nurse colocation and 9.56 minutes if a nurse was present. No difference in the frequency of physician-nurse overlap was observed between weekdays and weekends. Interestingly and not surprisingly, patient rooms located farther from the nursing station had a decreased likelihood of physician-nurse overlap.
A greater understanding of the medical community’s inability to reliably implement interdisciplinary bedside rounding may be found by examining the ecosystem of inpatient medicine. Physicians and nurses function in an environment with increasingly complex patients, more stringent (and non- evidence-based) documentation requirements, the physical decoupling of patients and their clinical information, and, as Sang et al.3 illuminate, complex geographical ward structures. As the rapidity with which patients are diagnosed and treated continues to escalate, physicians and nurses are also asked to attempt to squeeze an Oslerian-type rounding system into an ecosystem that is in overdrive. That the puzzle pieces do not fit should not be a surprise.
There is a risk that systems may implement interventions to “check the box” for interdisciplinary bedside rounding instead of seeking to change outcomes. How much time is time enough together at the bedside? Sang et al., among others, ponder whether a rounding duration of just under 10 minutes is enough.3,6 However, Rothberg et al. demonstrated that increased duration of communication alone is not necessarily associated with increased patient satisfaction or nurse–physician agreement on plan of care,7 suggesting that colocation and communication are necessary but not sufficient for true interdisciplinary patient care. The discordance between communication and understanding can potentially be explained by the varying agendas of the members of the interdisciplinary team during the same interaction.8
Ultimately, the future of interdisciplinary bedside rounding, and rounding in general, remains uncertain. Potential areas for improvement and further study include patient regionalization,3,5 tools to align agendas among stakeholders,8 integrating recommendations for interdisciplinary communication,9 and utilizing a common definition and taxonomy for study design.10 These interventions may improve future study designs and outcomes. However, these interventions are small tweaks in a complex ecosystem, and the return on these interventions may eventually reach an asymptote. Perhaps the concept of rounding as we know it is broken beyond repair, and a more radical approach is needed: either the creation of a completely innovative shared mental model of acute care that acknowledges the complex environment of inpatient medicine, or a complete restructuring of the ecosystem itself. Nonetheless, the findings of Sang et al.3 with respect to the ongoing difficulty of implementing interdisciplinary bedside rounding elucidate the need for innovation in study design and rounding implementation strategies; they also prompt us to ask—and answer—the complicated questions related to this integral component of our practice.
Disclosures
The authors have nothing to disclose.
1. Linfors EW, Neelon FA. The case for bedside rounds. N Engl J Med. 1980;303(21):1230-1233. https://doi.org/10.1056/NEJM198011203032110.
2. Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era. JAMA Intern Med. 2013;173(12):1084. https://doi.org/10.1001/jamainternmed.2013.6041.
3. Sang AX, Tisdale RL, Nielson D, et al. How much time are physicians and nurses spending together at the patient bedside? J Hosp Med. 2019;14(8):468-473. https://doi.org/10.12788/jhm.3204.
4. O’leary KJ, Killarney A, Hansen LO, et al. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual Saf. https://doi.org/10.1136/bmjqs-2015-005035.
5. Huang KTL, Minahan J, Brita-Rossi P, et al. All together now: impact of a regionalization and bedside rounding initiative on the efficiency and inclusiveness of clinical rounds OR. J Hosp Med. 2017;12(3):150-156. https://doi.org/10.12788/jhm.2696.
6. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
7. Rothberg MB, Steele JR, Wheeler J, Arora A, Priya A, Lindenauer PK. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27(2):185-189. https://doi.org/10.1007/s11606-011-1857-8.
8. Holton R, Patel R, Eggebrecht M, et al. Rounding on rounds. Am J Med Qual. 2015;30(5):493-493. https://doi.org/10.1177/1062860615596388.
9. Kassutto S , Seam N, Carlos WG, et al. Twelve tips for conducting successful interprofessional teaching rounds [published online ahead of print February 1, 2019]. Med Teach. https://doi.org/10.1080/0142159X.2018.1545086.
10. Bhamidipati VS, Elliott DJ, Justice EM, Belleh E, Sonnad SS, Robinson EJ. Structure and outcomes of interdisciplinary rounds in hospitalized medicine patients: a systematic review and suggested taxonomy. J Hosp Med. 2016;11(7):513-523. https://doi.org/10.1002/jhm.2575.
Medicine has a rich history of attending-led rounds, with some iteration of this ritual occurring as far back as the 1600s.1 In the early 1900s, the concept of “bedside rounds” was popularized by William Osler, who widely espoused their importance as a clinical and educational tool. Despite our best intentions, however, rounds today may be little reminiscent of the rounds of Osler’s day. Recent investigations into the characteristics of rounds have specifically revealed a “shift in the format from the beside to conference rooms and hallways.”2 Most of our practices for rounding in the modern era are built on tradition and belief rather than evidence. The ecosystem of modern hospital care is dramatically different than that of Osler’s day, and fundamental questions about the format, content, stakeholders, and processes of rounds remain. Perhaps the greatest and most needed change in rounding in recent years is the shift of rounds from a physician-centric activity to an activity that values the modern interprofessional hospital team. Ultimately, the very definition of “rounds” and the purpose they are meant to serve in the context of a dynamic and complicated hospital ecosystem has become increasingly complex and thus, difficult to assess and improve.
In this month’s Journal of Hospital Medicine, Sang et al.3 address this complexity by returning to basics and utilizing a novel approach to precisely measure the frequency and duration of a necessary (albeit insufficient) condition for interdisciplinary bedside rounding to occur: colocation of physician, nurse, and patient. Ultimately, their results provide a springboard to ask more complex and meaningful questions. Why, despite a recent culture shift prioritizing a return to bedside, is substantive physician and nurse colocation so persistently difficult to attain? How can we study outcomes of interdisciplinary bedside rounds if we cannot reliably facilitate their occurrence? What does “effective” rounding even mean? That is, what variables would be both meaningful and sensitive to changes in rounds?
After centuries of rounding, the medical community would be presumed to have perfected this art; however, we are instead left with more questions than answers. Prior research efforts have demonstrated the shifting of rounds away from the bedside, with bedside rounds occurring only 10%-40% of the time based on bias-prone survey data.2,4 Interestingly, a study by Huang et al., designed specifically to increase implementation of interdisciplinary bedside rounds, showed a frequency of only 64%.5 These studies are focused primarily on parameters such as patient and nursing satisfaction and did not include other important outcomes such as length of stay, readmission rates, diagnostic quality, patient engagement, or mortality.2,4,6
In Sang et al.,3 the authors utilized a real-time locator system, namely, radiofrequency identification, to precisely track the physical workflow of both attending hospitalists and bedside nurses and then subsequently used the data obtained to measure the frequency and duration of colocation at the patient bedside. The authors defined a physician “rounding event” as the physician’s presence in a single bed patient room for at least 10 seconds. The study revealed that colocation of physician and nurse (for at least 10 seconds) occurred in only 30% of all physician rounding events recorded. The duration of a physician rounding event was 5.68 minutes without nurse colocation and 9.56 minutes if a nurse was present. No difference in the frequency of physician-nurse overlap was observed between weekdays and weekends. Interestingly and not surprisingly, patient rooms located farther from the nursing station had a decreased likelihood of physician-nurse overlap.
A greater understanding of the medical community’s inability to reliably implement interdisciplinary bedside rounding may be found by examining the ecosystem of inpatient medicine. Physicians and nurses function in an environment with increasingly complex patients, more stringent (and non- evidence-based) documentation requirements, the physical decoupling of patients and their clinical information, and, as Sang et al.3 illuminate, complex geographical ward structures. As the rapidity with which patients are diagnosed and treated continues to escalate, physicians and nurses are also asked to attempt to squeeze an Oslerian-type rounding system into an ecosystem that is in overdrive. That the puzzle pieces do not fit should not be a surprise.
There is a risk that systems may implement interventions to “check the box” for interdisciplinary bedside rounding instead of seeking to change outcomes. How much time is time enough together at the bedside? Sang et al., among others, ponder whether a rounding duration of just under 10 minutes is enough.3,6 However, Rothberg et al. demonstrated that increased duration of communication alone is not necessarily associated with increased patient satisfaction or nurse–physician agreement on plan of care,7 suggesting that colocation and communication are necessary but not sufficient for true interdisciplinary patient care. The discordance between communication and understanding can potentially be explained by the varying agendas of the members of the interdisciplinary team during the same interaction.8
Ultimately, the future of interdisciplinary bedside rounding, and rounding in general, remains uncertain. Potential areas for improvement and further study include patient regionalization,3,5 tools to align agendas among stakeholders,8 integrating recommendations for interdisciplinary communication,9 and utilizing a common definition and taxonomy for study design.10 These interventions may improve future study designs and outcomes. However, these interventions are small tweaks in a complex ecosystem, and the return on these interventions may eventually reach an asymptote. Perhaps the concept of rounding as we know it is broken beyond repair, and a more radical approach is needed: either the creation of a completely innovative shared mental model of acute care that acknowledges the complex environment of inpatient medicine, or a complete restructuring of the ecosystem itself. Nonetheless, the findings of Sang et al.3 with respect to the ongoing difficulty of implementing interdisciplinary bedside rounding elucidate the need for innovation in study design and rounding implementation strategies; they also prompt us to ask—and answer—the complicated questions related to this integral component of our practice.
Disclosures
The authors have nothing to disclose.
Medicine has a rich history of attending-led rounds, with some iteration of this ritual occurring as far back as the 1600s.1 In the early 1900s, the concept of “bedside rounds” was popularized by William Osler, who widely espoused their importance as a clinical and educational tool. Despite our best intentions, however, rounds today may be little reminiscent of the rounds of Osler’s day. Recent investigations into the characteristics of rounds have specifically revealed a “shift in the format from the beside to conference rooms and hallways.”2 Most of our practices for rounding in the modern era are built on tradition and belief rather than evidence. The ecosystem of modern hospital care is dramatically different than that of Osler’s day, and fundamental questions about the format, content, stakeholders, and processes of rounds remain. Perhaps the greatest and most needed change in rounding in recent years is the shift of rounds from a physician-centric activity to an activity that values the modern interprofessional hospital team. Ultimately, the very definition of “rounds” and the purpose they are meant to serve in the context of a dynamic and complicated hospital ecosystem has become increasingly complex and thus, difficult to assess and improve.
In this month’s Journal of Hospital Medicine, Sang et al.3 address this complexity by returning to basics and utilizing a novel approach to precisely measure the frequency and duration of a necessary (albeit insufficient) condition for interdisciplinary bedside rounding to occur: colocation of physician, nurse, and patient. Ultimately, their results provide a springboard to ask more complex and meaningful questions. Why, despite a recent culture shift prioritizing a return to bedside, is substantive physician and nurse colocation so persistently difficult to attain? How can we study outcomes of interdisciplinary bedside rounds if we cannot reliably facilitate their occurrence? What does “effective” rounding even mean? That is, what variables would be both meaningful and sensitive to changes in rounds?
After centuries of rounding, the medical community would be presumed to have perfected this art; however, we are instead left with more questions than answers. Prior research efforts have demonstrated the shifting of rounds away from the bedside, with bedside rounds occurring only 10%-40% of the time based on bias-prone survey data.2,4 Interestingly, a study by Huang et al., designed specifically to increase implementation of interdisciplinary bedside rounds, showed a frequency of only 64%.5 These studies are focused primarily on parameters such as patient and nursing satisfaction and did not include other important outcomes such as length of stay, readmission rates, diagnostic quality, patient engagement, or mortality.2,4,6
In Sang et al.,3 the authors utilized a real-time locator system, namely, radiofrequency identification, to precisely track the physical workflow of both attending hospitalists and bedside nurses and then subsequently used the data obtained to measure the frequency and duration of colocation at the patient bedside. The authors defined a physician “rounding event” as the physician’s presence in a single bed patient room for at least 10 seconds. The study revealed that colocation of physician and nurse (for at least 10 seconds) occurred in only 30% of all physician rounding events recorded. The duration of a physician rounding event was 5.68 minutes without nurse colocation and 9.56 minutes if a nurse was present. No difference in the frequency of physician-nurse overlap was observed between weekdays and weekends. Interestingly and not surprisingly, patient rooms located farther from the nursing station had a decreased likelihood of physician-nurse overlap.
A greater understanding of the medical community’s inability to reliably implement interdisciplinary bedside rounding may be found by examining the ecosystem of inpatient medicine. Physicians and nurses function in an environment with increasingly complex patients, more stringent (and non- evidence-based) documentation requirements, the physical decoupling of patients and their clinical information, and, as Sang et al.3 illuminate, complex geographical ward structures. As the rapidity with which patients are diagnosed and treated continues to escalate, physicians and nurses are also asked to attempt to squeeze an Oslerian-type rounding system into an ecosystem that is in overdrive. That the puzzle pieces do not fit should not be a surprise.
There is a risk that systems may implement interventions to “check the box” for interdisciplinary bedside rounding instead of seeking to change outcomes. How much time is time enough together at the bedside? Sang et al., among others, ponder whether a rounding duration of just under 10 minutes is enough.3,6 However, Rothberg et al. demonstrated that increased duration of communication alone is not necessarily associated with increased patient satisfaction or nurse–physician agreement on plan of care,7 suggesting that colocation and communication are necessary but not sufficient for true interdisciplinary patient care. The discordance between communication and understanding can potentially be explained by the varying agendas of the members of the interdisciplinary team during the same interaction.8
Ultimately, the future of interdisciplinary bedside rounding, and rounding in general, remains uncertain. Potential areas for improvement and further study include patient regionalization,3,5 tools to align agendas among stakeholders,8 integrating recommendations for interdisciplinary communication,9 and utilizing a common definition and taxonomy for study design.10 These interventions may improve future study designs and outcomes. However, these interventions are small tweaks in a complex ecosystem, and the return on these interventions may eventually reach an asymptote. Perhaps the concept of rounding as we know it is broken beyond repair, and a more radical approach is needed: either the creation of a completely innovative shared mental model of acute care that acknowledges the complex environment of inpatient medicine, or a complete restructuring of the ecosystem itself. Nonetheless, the findings of Sang et al.3 with respect to the ongoing difficulty of implementing interdisciplinary bedside rounding elucidate the need for innovation in study design and rounding implementation strategies; they also prompt us to ask—and answer—the complicated questions related to this integral component of our practice.
Disclosures
The authors have nothing to disclose.
1. Linfors EW, Neelon FA. The case for bedside rounds. N Engl J Med. 1980;303(21):1230-1233. https://doi.org/10.1056/NEJM198011203032110.
2. Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era. JAMA Intern Med. 2013;173(12):1084. https://doi.org/10.1001/jamainternmed.2013.6041.
3. Sang AX, Tisdale RL, Nielson D, et al. How much time are physicians and nurses spending together at the patient bedside? J Hosp Med. 2019;14(8):468-473. https://doi.org/10.12788/jhm.3204.
4. O’leary KJ, Killarney A, Hansen LO, et al. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual Saf. https://doi.org/10.1136/bmjqs-2015-005035.
5. Huang KTL, Minahan J, Brita-Rossi P, et al. All together now: impact of a regionalization and bedside rounding initiative on the efficiency and inclusiveness of clinical rounds OR. J Hosp Med. 2017;12(3):150-156. https://doi.org/10.12788/jhm.2696.
6. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
7. Rothberg MB, Steele JR, Wheeler J, Arora A, Priya A, Lindenauer PK. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27(2):185-189. https://doi.org/10.1007/s11606-011-1857-8.
8. Holton R, Patel R, Eggebrecht M, et al. Rounding on rounds. Am J Med Qual. 2015;30(5):493-493. https://doi.org/10.1177/1062860615596388.
9. Kassutto S , Seam N, Carlos WG, et al. Twelve tips for conducting successful interprofessional teaching rounds [published online ahead of print February 1, 2019]. Med Teach. https://doi.org/10.1080/0142159X.2018.1545086.
10. Bhamidipati VS, Elliott DJ, Justice EM, Belleh E, Sonnad SS, Robinson EJ. Structure and outcomes of interdisciplinary rounds in hospitalized medicine patients: a systematic review and suggested taxonomy. J Hosp Med. 2016;11(7):513-523. https://doi.org/10.1002/jhm.2575.
1. Linfors EW, Neelon FA. The case for bedside rounds. N Engl J Med. 1980;303(21):1230-1233. https://doi.org/10.1056/NEJM198011203032110.
2. Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era. JAMA Intern Med. 2013;173(12):1084. https://doi.org/10.1001/jamainternmed.2013.6041.
3. Sang AX, Tisdale RL, Nielson D, et al. How much time are physicians and nurses spending together at the patient bedside? J Hosp Med. 2019;14(8):468-473. https://doi.org/10.12788/jhm.3204.
4. O’leary KJ, Killarney A, Hansen LO, et al. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual Saf. https://doi.org/10.1136/bmjqs-2015-005035.
5. Huang KTL, Minahan J, Brita-Rossi P, et al. All together now: impact of a regionalization and bedside rounding initiative on the efficiency and inclusiveness of clinical rounds OR. J Hosp Med. 2017;12(3):150-156. https://doi.org/10.12788/jhm.2696.
6. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
7. Rothberg MB, Steele JR, Wheeler J, Arora A, Priya A, Lindenauer PK. The relationship between time spent communicating and communication outcomes on a hospital medicine service. J Gen Intern Med. 2012;27(2):185-189. https://doi.org/10.1007/s11606-011-1857-8.
8. Holton R, Patel R, Eggebrecht M, et al. Rounding on rounds. Am J Med Qual. 2015;30(5):493-493. https://doi.org/10.1177/1062860615596388.
9. Kassutto S , Seam N, Carlos WG, et al. Twelve tips for conducting successful interprofessional teaching rounds [published online ahead of print February 1, 2019]. Med Teach. https://doi.org/10.1080/0142159X.2018.1545086.
10. Bhamidipati VS, Elliott DJ, Justice EM, Belleh E, Sonnad SS, Robinson EJ. Structure and outcomes of interdisciplinary rounds in hospitalized medicine patients: a systematic review and suggested taxonomy. J Hosp Med. 2016;11(7):513-523. https://doi.org/10.1002/jhm.2575.
© 2019 Society of Hospital Medicine
Waiting for Godot: The Quest to Promote Scholarship in Hospital Medicine
Twenty years into the hospitalist movement, the proven formula for developing high-quality scholarly output in a hospital medicine group remains elusive. In this issue of the Journal of Hospital Medicine, McKinney et al. describe a new model in which an academic research coach—a PhD-trained researcher with 50% protected time to assist with hospitalist scholarly activities—is utilized to support scholarship.1 Built on the premise that most hospitalist faculty do not have research training and many are embarking on their first academic project, the research coach was available to engage hospitalists at any stage of scholarship from conceptualizing an idea, to submitting one’s first IRB, to data analysis, and grant and manuscript submission. This innovation (and the financial investment required) provides an opportunity to consider how to facilitate scholarship and measure its value in hospital medicine groups.
Academic institutions are built on the premise that scholarship—and research in particular—is of equal value to clinical care and teaching; a perspective that is commonly enshrined in promotion criteria that require scholarship for career advancement. While hospitalists are competent to begin clinical practice and transfer their knowledge to others at the conclusion of their residency, most are not prepared to lead research programs or create academic products from their clinical innovations, quality improvement, or medical education work. Yet, particularly for hospitalists who choose to practice in an academic setting, the leadership of their Section, Division, or Department may naturally expect scholarship to occur, similar to other clinical disciplines. In our experience as the directors of research and faculty development in our hospital medicine group, meeting this expectation requires recognizing that faculty development and scholarship development are intertwined and there must be an investment in both.
We believe that faculty development is required—but not sufficient—for the development of high-quality scholarship. In order for hospitalists to generate new knowledge in clinical, educational, quality improvement, and research domains, they must acquire a new skill set after residency training. These skills can be gained in different formats and time frames such as dedicated hospital medicine fellowships, internal faculty development programs, external programs (eg, Academic Hospitalist Academy), and/or individual mentorship. Descriptions of internal faculty development programs have unfortunately been limited to a single institutions with uncertain generalizability.2,3 One could argue that faculty development may even be more important in hospital medicine than in clinical subspecialties given the relative youth of the field and the experience level of the entry-level faculty. Pediatric hospital medicine may be farthest along in faculty development and scholarship development after becoming a distinct subspecialty recognized by the American Board of Pediatrics and American Board of Medical Specialties; pediatric hospitalists must now complete fellowship training after residency before independent practice.4 Importantly, completion of a scholarly product that advances the field is a required component of the pediatric hospital medicine fellowship curricular framework.5 Regardless of what infrastructure a hospital medicine group chooses to build, there is a growing realization that faculty development must be firmly in place in order for scholarship to flourish.
In addition to junior faculty development, there is also a need for scholarship development to translate new skills into products of scholarship. For example, a well-published senior faculty member still may need statistical assistance and a midcareer hospitalist who leads quality improvement may struggle to write an effective manuscript to disseminate their findings. McKinney et al.’s innovation seems intended to meet this need, and the just-in-time and menu-style nature of the academic research coach resource is unique and novel. One can imagine how this approach to increasing scholarship productivity could be effective and utilized by busy junior, midcareer, and senior hospitalists alike. As the authors point out, this model attempts to mitigate the drawbacks that other models for enhancing hospitalist scholarship have faced, such as relying on physician scientists as mentors, holding works-in-progress or research seminars, or funding a consulting statistician. A well-trained scientist who meets hospitalists “where they are” is appealing when placed in the context of an effective faculty development program that enables faculty to take advantage of this resource. We hope that future evaluations of this promising innovation will include a comparison group to measure the effect of the academic research coach and demonstrate a return on the financial investment supporting the academic research coach.
Measuring return on investment requires defining the value of scholarship in hospital medicine. Some things that are easy to measure and have valence for traditional academic productivity are captured in the McKinney manuscript: the number of abstracts, papers, and grants.
Measuring the value of scholarship in hospital medicine touches very near to the core of the value proposition of hospital medicine overall as a specialty. Without high-quality scholarship that demonstrates the influence of hospitalists in improving systems, leading change, educating learners, and advocating for the needs of our patients, why continue to invest in this model? We are struck every year at the Society of Hospital Medicine national conference about how much innovation hospitalists are leading – and how little is systematically evaluated or disseminated. In Beckett’s “Waiting for Godot,” Vladimir and Estragon talk about life and wait for Godot who, of course, never arrives. Instead of patiently waiting for more scholarship to arrive, we suggest that hospital medicine leaders follow the lead of McKinney et al. and take action by investing in it.
Disclosures
The views expressed are those of the authors and not necessarily those of the Department of Veterans Affairs.
Funding
Dr. Burke is funded by a VA HSR&D Career Development Award.
1. McKinney CM, Mookherjee S, Fihn SD, Gallagher TH. An academic research coach: an innovative approach to increasing scholarly productivity in medicine. J Hosp Med. 2019;14(8):457-461. https://doi.org/10.12788/jhm.3194.
2. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845.
3. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603.
4. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: a proposed new subspecialty. Pediatrics. 2017;139(3):e20161823. https://doi.org/10.1542/peds.2016-1823.
5. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698.
6. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
Twenty years into the hospitalist movement, the proven formula for developing high-quality scholarly output in a hospital medicine group remains elusive. In this issue of the Journal of Hospital Medicine, McKinney et al. describe a new model in which an academic research coach—a PhD-trained researcher with 50% protected time to assist with hospitalist scholarly activities—is utilized to support scholarship.1 Built on the premise that most hospitalist faculty do not have research training and many are embarking on their first academic project, the research coach was available to engage hospitalists at any stage of scholarship from conceptualizing an idea, to submitting one’s first IRB, to data analysis, and grant and manuscript submission. This innovation (and the financial investment required) provides an opportunity to consider how to facilitate scholarship and measure its value in hospital medicine groups.
Academic institutions are built on the premise that scholarship—and research in particular—is of equal value to clinical care and teaching; a perspective that is commonly enshrined in promotion criteria that require scholarship for career advancement. While hospitalists are competent to begin clinical practice and transfer their knowledge to others at the conclusion of their residency, most are not prepared to lead research programs or create academic products from their clinical innovations, quality improvement, or medical education work. Yet, particularly for hospitalists who choose to practice in an academic setting, the leadership of their Section, Division, or Department may naturally expect scholarship to occur, similar to other clinical disciplines. In our experience as the directors of research and faculty development in our hospital medicine group, meeting this expectation requires recognizing that faculty development and scholarship development are intertwined and there must be an investment in both.
We believe that faculty development is required—but not sufficient—for the development of high-quality scholarship. In order for hospitalists to generate new knowledge in clinical, educational, quality improvement, and research domains, they must acquire a new skill set after residency training. These skills can be gained in different formats and time frames such as dedicated hospital medicine fellowships, internal faculty development programs, external programs (eg, Academic Hospitalist Academy), and/or individual mentorship. Descriptions of internal faculty development programs have unfortunately been limited to a single institutions with uncertain generalizability.2,3 One could argue that faculty development may even be more important in hospital medicine than in clinical subspecialties given the relative youth of the field and the experience level of the entry-level faculty. Pediatric hospital medicine may be farthest along in faculty development and scholarship development after becoming a distinct subspecialty recognized by the American Board of Pediatrics and American Board of Medical Specialties; pediatric hospitalists must now complete fellowship training after residency before independent practice.4 Importantly, completion of a scholarly product that advances the field is a required component of the pediatric hospital medicine fellowship curricular framework.5 Regardless of what infrastructure a hospital medicine group chooses to build, there is a growing realization that faculty development must be firmly in place in order for scholarship to flourish.
In addition to junior faculty development, there is also a need for scholarship development to translate new skills into products of scholarship. For example, a well-published senior faculty member still may need statistical assistance and a midcareer hospitalist who leads quality improvement may struggle to write an effective manuscript to disseminate their findings. McKinney et al.’s innovation seems intended to meet this need, and the just-in-time and menu-style nature of the academic research coach resource is unique and novel. One can imagine how this approach to increasing scholarship productivity could be effective and utilized by busy junior, midcareer, and senior hospitalists alike. As the authors point out, this model attempts to mitigate the drawbacks that other models for enhancing hospitalist scholarship have faced, such as relying on physician scientists as mentors, holding works-in-progress or research seminars, or funding a consulting statistician. A well-trained scientist who meets hospitalists “where they are” is appealing when placed in the context of an effective faculty development program that enables faculty to take advantage of this resource. We hope that future evaluations of this promising innovation will include a comparison group to measure the effect of the academic research coach and demonstrate a return on the financial investment supporting the academic research coach.
Measuring return on investment requires defining the value of scholarship in hospital medicine. Some things that are easy to measure and have valence for traditional academic productivity are captured in the McKinney manuscript: the number of abstracts, papers, and grants.
Measuring the value of scholarship in hospital medicine touches very near to the core of the value proposition of hospital medicine overall as a specialty. Without high-quality scholarship that demonstrates the influence of hospitalists in improving systems, leading change, educating learners, and advocating for the needs of our patients, why continue to invest in this model? We are struck every year at the Society of Hospital Medicine national conference about how much innovation hospitalists are leading – and how little is systematically evaluated or disseminated. In Beckett’s “Waiting for Godot,” Vladimir and Estragon talk about life and wait for Godot who, of course, never arrives. Instead of patiently waiting for more scholarship to arrive, we suggest that hospital medicine leaders follow the lead of McKinney et al. and take action by investing in it.
Disclosures
The views expressed are those of the authors and not necessarily those of the Department of Veterans Affairs.
Funding
Dr. Burke is funded by a VA HSR&D Career Development Award.
Twenty years into the hospitalist movement, the proven formula for developing high-quality scholarly output in a hospital medicine group remains elusive. In this issue of the Journal of Hospital Medicine, McKinney et al. describe a new model in which an academic research coach—a PhD-trained researcher with 50% protected time to assist with hospitalist scholarly activities—is utilized to support scholarship.1 Built on the premise that most hospitalist faculty do not have research training and many are embarking on their first academic project, the research coach was available to engage hospitalists at any stage of scholarship from conceptualizing an idea, to submitting one’s first IRB, to data analysis, and grant and manuscript submission. This innovation (and the financial investment required) provides an opportunity to consider how to facilitate scholarship and measure its value in hospital medicine groups.
Academic institutions are built on the premise that scholarship—and research in particular—is of equal value to clinical care and teaching; a perspective that is commonly enshrined in promotion criteria that require scholarship for career advancement. While hospitalists are competent to begin clinical practice and transfer their knowledge to others at the conclusion of their residency, most are not prepared to lead research programs or create academic products from their clinical innovations, quality improvement, or medical education work. Yet, particularly for hospitalists who choose to practice in an academic setting, the leadership of their Section, Division, or Department may naturally expect scholarship to occur, similar to other clinical disciplines. In our experience as the directors of research and faculty development in our hospital medicine group, meeting this expectation requires recognizing that faculty development and scholarship development are intertwined and there must be an investment in both.
We believe that faculty development is required—but not sufficient—for the development of high-quality scholarship. In order for hospitalists to generate new knowledge in clinical, educational, quality improvement, and research domains, they must acquire a new skill set after residency training. These skills can be gained in different formats and time frames such as dedicated hospital medicine fellowships, internal faculty development programs, external programs (eg, Academic Hospitalist Academy), and/or individual mentorship. Descriptions of internal faculty development programs have unfortunately been limited to a single institutions with uncertain generalizability.2,3 One could argue that faculty development may even be more important in hospital medicine than in clinical subspecialties given the relative youth of the field and the experience level of the entry-level faculty. Pediatric hospital medicine may be farthest along in faculty development and scholarship development after becoming a distinct subspecialty recognized by the American Board of Pediatrics and American Board of Medical Specialties; pediatric hospitalists must now complete fellowship training after residency before independent practice.4 Importantly, completion of a scholarly product that advances the field is a required component of the pediatric hospital medicine fellowship curricular framework.5 Regardless of what infrastructure a hospital medicine group chooses to build, there is a growing realization that faculty development must be firmly in place in order for scholarship to flourish.
In addition to junior faculty development, there is also a need for scholarship development to translate new skills into products of scholarship. For example, a well-published senior faculty member still may need statistical assistance and a midcareer hospitalist who leads quality improvement may struggle to write an effective manuscript to disseminate their findings. McKinney et al.’s innovation seems intended to meet this need, and the just-in-time and menu-style nature of the academic research coach resource is unique and novel. One can imagine how this approach to increasing scholarship productivity could be effective and utilized by busy junior, midcareer, and senior hospitalists alike. As the authors point out, this model attempts to mitigate the drawbacks that other models for enhancing hospitalist scholarship have faced, such as relying on physician scientists as mentors, holding works-in-progress or research seminars, or funding a consulting statistician. A well-trained scientist who meets hospitalists “where they are” is appealing when placed in the context of an effective faculty development program that enables faculty to take advantage of this resource. We hope that future evaluations of this promising innovation will include a comparison group to measure the effect of the academic research coach and demonstrate a return on the financial investment supporting the academic research coach.
Measuring return on investment requires defining the value of scholarship in hospital medicine. Some things that are easy to measure and have valence for traditional academic productivity are captured in the McKinney manuscript: the number of abstracts, papers, and grants.
Measuring the value of scholarship in hospital medicine touches very near to the core of the value proposition of hospital medicine overall as a specialty. Without high-quality scholarship that demonstrates the influence of hospitalists in improving systems, leading change, educating learners, and advocating for the needs of our patients, why continue to invest in this model? We are struck every year at the Society of Hospital Medicine national conference about how much innovation hospitalists are leading – and how little is systematically evaluated or disseminated. In Beckett’s “Waiting for Godot,” Vladimir and Estragon talk about life and wait for Godot who, of course, never arrives. Instead of patiently waiting for more scholarship to arrive, we suggest that hospital medicine leaders follow the lead of McKinney et al. and take action by investing in it.
Disclosures
The views expressed are those of the authors and not necessarily those of the Department of Veterans Affairs.
Funding
Dr. Burke is funded by a VA HSR&D Career Development Award.
1. McKinney CM, Mookherjee S, Fihn SD, Gallagher TH. An academic research coach: an innovative approach to increasing scholarly productivity in medicine. J Hosp Med. 2019;14(8):457-461. https://doi.org/10.12788/jhm.3194.
2. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845.
3. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603.
4. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: a proposed new subspecialty. Pediatrics. 2017;139(3):e20161823. https://doi.org/10.1542/peds.2016-1823.
5. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698.
6. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
1. McKinney CM, Mookherjee S, Fihn SD, Gallagher TH. An academic research coach: an innovative approach to increasing scholarly productivity in medicine. J Hosp Med. 2019;14(8):457-461. https://doi.org/10.12788/jhm.3194.
2. Sehgal NL, Sharpe BA, Auerbach AA, Wachter RM. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845.
3. Seymann GB, Southern W, Burger A, et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (SuCcessful HOspitaLists in academics and research) project. J Hosp Med. 2016;11(10):708-713. https://doi.org/10.1002/jhm.2603.
4. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: a proposed new subspecialty. Pediatrics. 2017;139(3):e20161823. https://doi.org/10.1542/peds.2016-1823.
5. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1):e20170698. https://doi.org/10.1542/peds.2017-0698.
6. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
© 2019 Society of Hospital Medicine