User login
TRUST: How to build a support net for ObGyns affected by a medical error
An estimated 98,000 Americans die each year due to medical errors. This is an attention-grabbing statistic—from the year 2000.1 A recent study (published in 2016) reported that medical errors are the third leading cause of death in the United States, ranking just behind heart disease and cancer.2
As expected, much has been done to reduce medical errors and improve patient safety as a result of these publications. Quality, safety, and outcomes are paramount, as evidenced by the Institute of Health Care Improvement’s “triple aim”: reduce cost of care, improve quality of care, and improve patient outcomes.3
While these 3 aims are of paramount importance, this article seeks to portray the “quadruple aim,” with an additional focus on physician well-being. Patients and their families (first victims) are not the only ones affected by medical errors. Clinicians are, too, and these effects can be devastating. Here I offer concrete strategies to support providers involved in medical errors, including tips on developing a formal support program. First, however, I describe the devastating effects medical errors can have on providers and the signs of a second victim.
Related article:
Medical errors: Caring for the second victim (you)
The scope of the problem
In 2000, it was Dr. Albert Wu’s publication in The British Medical Journal titled “Medical Error: The Second Victim” (the doctor who makes mistakes needs help too), that first addressed this important topic.4 In his article he shared a case of another house officer who missed signs of a pericardial tamponade and was judged incompetent by peers due to his mistake.
As physicians, we do not intrinsically support colleagues who have experienced a medical error. We all have taken, with pride and commitment, our Hippocratic Oath of “do no harm,” yet we are often held to standards of perfection by society, peers, and, above all, ourselves. Have technologic wonders and precise laboratory tests supplanted the adage “doctors are only human”? Dr. Wu also points out in this landmark essay his observation and dismay at the lack of empathy, sympathy, and compassion shown by peers when medical errors occur. All of these elements are needed for the healing of those involved to take place. If they are not provided, dysfunctional coping mechanisms ensue.4
Incidence of medical errors
Despite the Institute of Medicine report from 20001 and the recent study from Johns Hopkins,2 determining the exact number of errors and incidents is not easy. Most data reporting is sparse. A prospective longitudinal study of perceived medical errors and resident distress estimated medical errors to be between 5% and 10% in hospitalized patients, but that it could be up to 50%.5 According to a 2005 study, approximately one-third of internal medicine residents report at least 1 major medical error during their 3 years of training, while 18% of multidisciplinary residents report an adverse event under their care in the previous week.6
Related article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Who is at risk of becoming a second victim?
Any and all clinicians can become a second victim, and the state can be realized at varying points in the process of an experienced medical error. The circumstances of the initial error and the severity of the effect on the patient and/or the damaged physician−patient relationship can affect whether or not there is a second victim. A second victim also can emerge as a result of peers’ or colleagues’ comments and lack of empathy or support. Certainly a lawsuit can produce a second victim.7
How often do physicians become second victims?
The prevalence of second victims has a large variation in estimates. A 2006 study estimates a prevalence of 10.4%.8 In 2010, the estimate was 30%, and a prevalence of 43.3% was reported in 2000.9,10 Regarding emotional distress within a year of a major adverse event, 30% of almost 900 providers reported these feelings.11 Other studies note 50% of health care workers reported feelings consistent with those of a second victim.7
Next: What are the symptoms of a second victim?
The signs of, and long-lasting risks for, a second victim
Second victims are at risk for several well-documented symptoms, regardless of their stage of training, including6:
- depression (in fact, they have a 3-fold risk)
- decrease in overall quality of life
- increase in burnout
- increase in feelings of distress, guilt, and shame, which may be long lasting.
Health care providers as second victims also may experience shock and hopelessness, sleep disturbance, social avoidance, intrusive thoughts and nightmares, and poor memory and concentration. Interestingly, these emotions and reactions are indistinguishable from posttraumatic stress disorder. These continued symptoms can have short- and long-term implications for physicians, patients, and the health care organization.12
Next: How to support those affected by a medical error
How to support all of those affected by a medical error
Over the past decade or so, much attention has been paid to creating safer health systems, improving outcomes and patient satisfaction, and recognizing the needs of patients and families of first victims when medical errors occur. Much less has been done to acknowledge and address the needs of struggling clinicians.
Provide nurturing discussions and sympathy
Hospital systems do have embedded processes to review outcomes and medical errors, including, among others, peer review, quality improvement, morbidity and mortality review, and root cause analysis. Unfortunately, often a “name, blame, shame game” can result from the overall process, with certain individuals or groups of individuals singled out, and only worsen the incidence and effects of the second victim. Ideally, system processes for addressing medical errors should allow for an environment more focused on nurturing discussions to prevent error and recognize all the factors contributing to an error.
Of course in any outcome or error investigation, the goal is to identify what happened, what factors contributed to the incident, and what can be done to prevent future occurrences. The concern for the family as priority is understandable, as is the desire to prevent a lawsuit. The lack of attention and sympathy to the health care provider involved contributes to the second victim.7
It is all too easy to blame, even in a Just Culture. Deficiencies in sympathy and attention can occur without a system whose culture is focused on “name, blame, shame.” A Just Culture, as defined by the Institute for Healthcare Improvement, is one in which individuals come forward with a mistake without fear of punishment. Such a culture balances the need to learn from our mistakes and the need to have disciplinary action.13
David Marx, an outcomes engineer and author of “Whack a Mole: The Price We Pay for Expecting Perfection,” touts a Just Culture as one having the following sets of beliefs:
- recognition that professionals will make mistakes
- recognition that even professionals will develop unhealthy norms
- a fierce intolerance for reckless conduct.
He strongly asserts that human error be consoled while reckless behavior be punished.14 Punishing human error is a setup for the second victim.
Read on for tips to develop a coping program
Tips for developing a coping program
In 2009, Scott and colleagues described 6 stages of a second victim. These are:
- Stage 1: Chaos and event repair
- Stage 2: Intrusive thoughts, “what if”
- Stage 3: Restoring personal identity
- Stage 4: Enduring the inquisition
- Stage 5: Obtaining emotional first aid
- Stage 6: Moving on or dropping out; surviving and/or thriving
Throughout the stages, second victims look for support and share their experience of the medical error event, as well as their personal and professional impact of the error.15
A 2007 study that examined the emotional impact of medical errors on physicians revealed some startling data. A full 82% of physicians expressed interest in counseling to help cope with their distress. And 90% felt there was inadequate support at their hospitals or health care organizations for this distress.16
Use The Joint Commission’s toolkit
Unfortunately, there are only a few well-documented second-victim support programs in the United States, despite the growing evidence of the emotional distress that second victims experience. Many hospitals do not know how to develop or implement such a support system. Recognizing this challenge, The Joint Commission developed a toolkit to assist health care organizations in developing a second-victim program. The toolkit consists of 10 modules (TABLE) designed to assist organizations not only to implement a second-victim support process but also to customize it to their specific institutional culture. This toolkit can be downloaded for free or used online. Within the first year of its availability, over 6,000 people visited the website and there were more than 700 requests for a download.17
Follow forYOU’s example
An example and well-recognized second-victim support program is the “forYOU” team at the University of Missouri. The program is free to employees, confidential, and available 24-7. Its purpose is “providing care and support to our staff,” by helping members understand the phenomenon of the second victim and quickly returning members to a satisfying professional practice.18
The “forYOU” team was created in 2007 under the direction of the University of Missouri Health Care’s Office of Clinical Effectiveness with the goals of increasing institutional awareness, providing a second victim with a “safe zone,” and allowing for the expression of emotions and reactions in a confidential setting. Team members are multidisciplinary and include physicians, nurses, respiratory therapists, social workers, and chaplains. They strive to normalize the feelings and thoughts second victims experience after a stressful outcome or event. Team members are highly trained in second-victim responses and the stages of coping. The program has established institutional actions to each of the 6 stages (FIGURE).19
Read on to learn how peer mentors are crucial to a support program
Establish TRUST
At the Carilion Clinic in Roanoke, Virginia, we too have developed a second-victim support program for all of our employees: TRUST. In the beginning stages, we quickly reaffirmed the challenges in developing such a program.
Initial challenges you will face. First, education on what a second victim is needs to be recognized. The fact that not everyone experiences second-victim emotions needs to be validated. Administrators and staff must be convinced that needing support is not a sign of weakness. And the program must ensure confidentiality and recruit mentors. These are just a few of the obstacles we faced on our path to program realization. Our journey to develop our second-victim program was approximately 5 years and required participation, affirmation, and support from all levels of the organization.
Our program name embodies its inherent purpose and goals. TRUST stands for:
- Treatment that is just. Second victims deserve the right of a presumption that their intentions were good, and should be able to depend on organizational leaders for integrity, fairness, just treatment, and shared accountability for outcomes.
- Respect. Second victims deserve respect and common decency and should not be blamed and shamed for human fallibility.
- Understanding and compassion. Second victims need compassionate help to grieve and heal.
- Supportive care. Second victims are entitled to psychological and support services that are delivered in a professional and organized way.
- Transparency and opportunity to contribute. Second victims have a right to participate in the learning gathered from the event, to share important causal information with the organization, and to be provided with an opportunity to heal by contributing to the prevention of future events.
Employ peer mentors, who serve a vital role
We have identified the need to develop a more direct and active approach to the TRUST program’s recruitment and established a subcommittee to begin this process. We began by asking leaders to nominate potential peer mentors and spoke about the program and asked for volunteers at various hospital committees. Once we had most disciplines represented, leaders were asked to take an assessment for emotional intelligence.
Other than the initial training for the TRUST program, the time requirement for participation for peer mentors is likely less than an hour per month. The dedicated time certainly is dependent on how much support the second victim is requiring, however, and varies. We encourage the peer supporters to be aware of their time constraints and establish parameters for the relationship in a direct but supportive way.
Since the inception of the TRUST Team in September 2014, we have trained 12 peer mentors, 10 of whom currently still serve in that capacity. We have 3 additional peers awaiting training. To date, The TRUST team has supported 19 clinicians/staff, including 3 ACPs, 9 nurses, 6 physicians, and 1 other (pharmacist). Of those 10, 3 are still actively receiving support so closing data have yet to be collected. Of the 16 who have been closed, 6 were referred for ongoing support and 10 were able to return to baseline with TRUST Team Supports.
Related article:
Who is liable when a surgical error occurs?
Just surviving the medical error is not the goal
Medical errors are inevitable, and the effects on providers can be devastating. It is important that physicians and institutions are aware of the signs and symptoms of a second victim as well as provide support to them. Institutions must have a just culture in which all members of the health care team can come forward with medical errors without the fear of punishment. Ideally, these institutions also have a second-victim support system that identifies those who need assistance and assist all health care clinicians not only to survive the effects of medical errors but also to thrive after receiving the necessary support.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academy Press; 2000. http://www.nap.edu/books/0309068371/html. Accessed December 18, 2016.
- Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affairs (Millwood). 2008;27(3):759−769. http://www.ihi.org/resources/Pages/Publications/TripleAimCareHealthandCost.aspx. Accessed December 18, 2016.
- Wu AW. Medical error: The second victim. The doctor who makes the mistake needs help too. BMJ . 2000;320(7237):726−727.
- West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071−1078.
- Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hetter M, Weissman JS. Residents report on adverse events and their causes. Arch Intern Med. 2005;165(22):2607−2613.
- Wu AW, Steckelberg RC. Medical error, incident investigation, and the second victim: doing better but feeling worse? BMJ Qual Saf. 2012;21(4):267−270.
- Lander LI, Connor JA, Shah RK, Kentala E, Healy, GB, Roberson DW. Otolaryngologists’ responses to errors and adverse events. Laryngoscope. 2006;116(7):1114−1120.
- Scott SD, Hirschinger LE, Cox KR. Sharing the load. Rescuing the healer after trauma. RN. 2008;71(12):38−40,42−43.
- Wolf ZR. Stress management in response to practice errors: critical events in professional practice. PA-PSRS Patient Safety Advisory. 2005;2:1−2.
- Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233−240.
- Edrees HH, Paine LA, Feroli ER, Wu AW. Health care workers as second victims of medical errors. Pol Arch Med Wewn. 2011;121(4):101−108.
- Leonard M. Organizational fairness/Just Culture. Cambridge, MA: Institute for Healthcare Improvement; 2012. http://app.ihi.org/extranetng/content/58886256-47d8-4f9c-bf7b-0afc352f013a/0efbd6cd-d0a3-4353-ad84-c86d07f499e1/4_5_Just%20Culture_ML.pdf. Accessed December 18, 2016.
- Marx D. Whack-a-Mole: The Price We Pay for Expecting Perfection. Plano, TX: By Your Side Studios; 2009.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(5):325−330.
- Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467−476.
- Pratt S, Kenney L, Scott SD, Wu AW. How to develop a second victim support program: a toolkit for health care organizations. Jt Comm J Qual Patient Saf. 2012;38(5):235−240,193.
- forYOU Team. Caring for our own. University of Missouri Health System website. http://www.muhealth.org/about/quality-of-care/office-of-clinical-effectiveness/foryou-team/. Accessed December 18, 2016.
- Second victim trajectory. Columbia, MO: University of Missouri Health System; 2009. http://www.muhealth.org/app/files/public/1390/6StagesRecovery.pdf. Accessed December 19, 2016.
An estimated 98,000 Americans die each year due to medical errors. This is an attention-grabbing statistic—from the year 2000.1 A recent study (published in 2016) reported that medical errors are the third leading cause of death in the United States, ranking just behind heart disease and cancer.2
As expected, much has been done to reduce medical errors and improve patient safety as a result of these publications. Quality, safety, and outcomes are paramount, as evidenced by the Institute of Health Care Improvement’s “triple aim”: reduce cost of care, improve quality of care, and improve patient outcomes.3
While these 3 aims are of paramount importance, this article seeks to portray the “quadruple aim,” with an additional focus on physician well-being. Patients and their families (first victims) are not the only ones affected by medical errors. Clinicians are, too, and these effects can be devastating. Here I offer concrete strategies to support providers involved in medical errors, including tips on developing a formal support program. First, however, I describe the devastating effects medical errors can have on providers and the signs of a second victim.
Related article:
Medical errors: Caring for the second victim (you)
The scope of the problem
In 2000, it was Dr. Albert Wu’s publication in The British Medical Journal titled “Medical Error: The Second Victim” (the doctor who makes mistakes needs help too), that first addressed this important topic.4 In his article he shared a case of another house officer who missed signs of a pericardial tamponade and was judged incompetent by peers due to his mistake.
As physicians, we do not intrinsically support colleagues who have experienced a medical error. We all have taken, with pride and commitment, our Hippocratic Oath of “do no harm,” yet we are often held to standards of perfection by society, peers, and, above all, ourselves. Have technologic wonders and precise laboratory tests supplanted the adage “doctors are only human”? Dr. Wu also points out in this landmark essay his observation and dismay at the lack of empathy, sympathy, and compassion shown by peers when medical errors occur. All of these elements are needed for the healing of those involved to take place. If they are not provided, dysfunctional coping mechanisms ensue.4
Incidence of medical errors
Despite the Institute of Medicine report from 20001 and the recent study from Johns Hopkins,2 determining the exact number of errors and incidents is not easy. Most data reporting is sparse. A prospective longitudinal study of perceived medical errors and resident distress estimated medical errors to be between 5% and 10% in hospitalized patients, but that it could be up to 50%.5 According to a 2005 study, approximately one-third of internal medicine residents report at least 1 major medical error during their 3 years of training, while 18% of multidisciplinary residents report an adverse event under their care in the previous week.6
Related article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Who is at risk of becoming a second victim?
Any and all clinicians can become a second victim, and the state can be realized at varying points in the process of an experienced medical error. The circumstances of the initial error and the severity of the effect on the patient and/or the damaged physician−patient relationship can affect whether or not there is a second victim. A second victim also can emerge as a result of peers’ or colleagues’ comments and lack of empathy or support. Certainly a lawsuit can produce a second victim.7
How often do physicians become second victims?
The prevalence of second victims has a large variation in estimates. A 2006 study estimates a prevalence of 10.4%.8 In 2010, the estimate was 30%, and a prevalence of 43.3% was reported in 2000.9,10 Regarding emotional distress within a year of a major adverse event, 30% of almost 900 providers reported these feelings.11 Other studies note 50% of health care workers reported feelings consistent with those of a second victim.7
Next: What are the symptoms of a second victim?
The signs of, and long-lasting risks for, a second victim
Second victims are at risk for several well-documented symptoms, regardless of their stage of training, including6:
- depression (in fact, they have a 3-fold risk)
- decrease in overall quality of life
- increase in burnout
- increase in feelings of distress, guilt, and shame, which may be long lasting.
Health care providers as second victims also may experience shock and hopelessness, sleep disturbance, social avoidance, intrusive thoughts and nightmares, and poor memory and concentration. Interestingly, these emotions and reactions are indistinguishable from posttraumatic stress disorder. These continued symptoms can have short- and long-term implications for physicians, patients, and the health care organization.12
Next: How to support those affected by a medical error
How to support all of those affected by a medical error
Over the past decade or so, much attention has been paid to creating safer health systems, improving outcomes and patient satisfaction, and recognizing the needs of patients and families of first victims when medical errors occur. Much less has been done to acknowledge and address the needs of struggling clinicians.
Provide nurturing discussions and sympathy
Hospital systems do have embedded processes to review outcomes and medical errors, including, among others, peer review, quality improvement, morbidity and mortality review, and root cause analysis. Unfortunately, often a “name, blame, shame game” can result from the overall process, with certain individuals or groups of individuals singled out, and only worsen the incidence and effects of the second victim. Ideally, system processes for addressing medical errors should allow for an environment more focused on nurturing discussions to prevent error and recognize all the factors contributing to an error.
Of course in any outcome or error investigation, the goal is to identify what happened, what factors contributed to the incident, and what can be done to prevent future occurrences. The concern for the family as priority is understandable, as is the desire to prevent a lawsuit. The lack of attention and sympathy to the health care provider involved contributes to the second victim.7
It is all too easy to blame, even in a Just Culture. Deficiencies in sympathy and attention can occur without a system whose culture is focused on “name, blame, shame.” A Just Culture, as defined by the Institute for Healthcare Improvement, is one in which individuals come forward with a mistake without fear of punishment. Such a culture balances the need to learn from our mistakes and the need to have disciplinary action.13
David Marx, an outcomes engineer and author of “Whack a Mole: The Price We Pay for Expecting Perfection,” touts a Just Culture as one having the following sets of beliefs:
- recognition that professionals will make mistakes
- recognition that even professionals will develop unhealthy norms
- a fierce intolerance for reckless conduct.
He strongly asserts that human error be consoled while reckless behavior be punished.14 Punishing human error is a setup for the second victim.
Read on for tips to develop a coping program
Tips for developing a coping program
In 2009, Scott and colleagues described 6 stages of a second victim. These are:
- Stage 1: Chaos and event repair
- Stage 2: Intrusive thoughts, “what if”
- Stage 3: Restoring personal identity
- Stage 4: Enduring the inquisition
- Stage 5: Obtaining emotional first aid
- Stage 6: Moving on or dropping out; surviving and/or thriving
Throughout the stages, second victims look for support and share their experience of the medical error event, as well as their personal and professional impact of the error.15
A 2007 study that examined the emotional impact of medical errors on physicians revealed some startling data. A full 82% of physicians expressed interest in counseling to help cope with their distress. And 90% felt there was inadequate support at their hospitals or health care organizations for this distress.16
Use The Joint Commission’s toolkit
Unfortunately, there are only a few well-documented second-victim support programs in the United States, despite the growing evidence of the emotional distress that second victims experience. Many hospitals do not know how to develop or implement such a support system. Recognizing this challenge, The Joint Commission developed a toolkit to assist health care organizations in developing a second-victim program. The toolkit consists of 10 modules (TABLE) designed to assist organizations not only to implement a second-victim support process but also to customize it to their specific institutional culture. This toolkit can be downloaded for free or used online. Within the first year of its availability, over 6,000 people visited the website and there were more than 700 requests for a download.17
Follow forYOU’s example
An example and well-recognized second-victim support program is the “forYOU” team at the University of Missouri. The program is free to employees, confidential, and available 24-7. Its purpose is “providing care and support to our staff,” by helping members understand the phenomenon of the second victim and quickly returning members to a satisfying professional practice.18
The “forYOU” team was created in 2007 under the direction of the University of Missouri Health Care’s Office of Clinical Effectiveness with the goals of increasing institutional awareness, providing a second victim with a “safe zone,” and allowing for the expression of emotions and reactions in a confidential setting. Team members are multidisciplinary and include physicians, nurses, respiratory therapists, social workers, and chaplains. They strive to normalize the feelings and thoughts second victims experience after a stressful outcome or event. Team members are highly trained in second-victim responses and the stages of coping. The program has established institutional actions to each of the 6 stages (FIGURE).19
Read on to learn how peer mentors are crucial to a support program
Establish TRUST
At the Carilion Clinic in Roanoke, Virginia, we too have developed a second-victim support program for all of our employees: TRUST. In the beginning stages, we quickly reaffirmed the challenges in developing such a program.
Initial challenges you will face. First, education on what a second victim is needs to be recognized. The fact that not everyone experiences second-victim emotions needs to be validated. Administrators and staff must be convinced that needing support is not a sign of weakness. And the program must ensure confidentiality and recruit mentors. These are just a few of the obstacles we faced on our path to program realization. Our journey to develop our second-victim program was approximately 5 years and required participation, affirmation, and support from all levels of the organization.
Our program name embodies its inherent purpose and goals. TRUST stands for:
- Treatment that is just. Second victims deserve the right of a presumption that their intentions were good, and should be able to depend on organizational leaders for integrity, fairness, just treatment, and shared accountability for outcomes.
- Respect. Second victims deserve respect and common decency and should not be blamed and shamed for human fallibility.
- Understanding and compassion. Second victims need compassionate help to grieve and heal.
- Supportive care. Second victims are entitled to psychological and support services that are delivered in a professional and organized way.
- Transparency and opportunity to contribute. Second victims have a right to participate in the learning gathered from the event, to share important causal information with the organization, and to be provided with an opportunity to heal by contributing to the prevention of future events.
Employ peer mentors, who serve a vital role
We have identified the need to develop a more direct and active approach to the TRUST program’s recruitment and established a subcommittee to begin this process. We began by asking leaders to nominate potential peer mentors and spoke about the program and asked for volunteers at various hospital committees. Once we had most disciplines represented, leaders were asked to take an assessment for emotional intelligence.
Other than the initial training for the TRUST program, the time requirement for participation for peer mentors is likely less than an hour per month. The dedicated time certainly is dependent on how much support the second victim is requiring, however, and varies. We encourage the peer supporters to be aware of their time constraints and establish parameters for the relationship in a direct but supportive way.
Since the inception of the TRUST Team in September 2014, we have trained 12 peer mentors, 10 of whom currently still serve in that capacity. We have 3 additional peers awaiting training. To date, The TRUST team has supported 19 clinicians/staff, including 3 ACPs, 9 nurses, 6 physicians, and 1 other (pharmacist). Of those 10, 3 are still actively receiving support so closing data have yet to be collected. Of the 16 who have been closed, 6 were referred for ongoing support and 10 were able to return to baseline with TRUST Team Supports.
Related article:
Who is liable when a surgical error occurs?
Just surviving the medical error is not the goal
Medical errors are inevitable, and the effects on providers can be devastating. It is important that physicians and institutions are aware of the signs and symptoms of a second victim as well as provide support to them. Institutions must have a just culture in which all members of the health care team can come forward with medical errors without the fear of punishment. Ideally, these institutions also have a second-victim support system that identifies those who need assistance and assist all health care clinicians not only to survive the effects of medical errors but also to thrive after receiving the necessary support.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
An estimated 98,000 Americans die each year due to medical errors. This is an attention-grabbing statistic—from the year 2000.1 A recent study (published in 2016) reported that medical errors are the third leading cause of death in the United States, ranking just behind heart disease and cancer.2
As expected, much has been done to reduce medical errors and improve patient safety as a result of these publications. Quality, safety, and outcomes are paramount, as evidenced by the Institute of Health Care Improvement’s “triple aim”: reduce cost of care, improve quality of care, and improve patient outcomes.3
While these 3 aims are of paramount importance, this article seeks to portray the “quadruple aim,” with an additional focus on physician well-being. Patients and their families (first victims) are not the only ones affected by medical errors. Clinicians are, too, and these effects can be devastating. Here I offer concrete strategies to support providers involved in medical errors, including tips on developing a formal support program. First, however, I describe the devastating effects medical errors can have on providers and the signs of a second victim.
Related article:
Medical errors: Caring for the second victim (you)
The scope of the problem
In 2000, it was Dr. Albert Wu’s publication in The British Medical Journal titled “Medical Error: The Second Victim” (the doctor who makes mistakes needs help too), that first addressed this important topic.4 In his article he shared a case of another house officer who missed signs of a pericardial tamponade and was judged incompetent by peers due to his mistake.
As physicians, we do not intrinsically support colleagues who have experienced a medical error. We all have taken, with pride and commitment, our Hippocratic Oath of “do no harm,” yet we are often held to standards of perfection by society, peers, and, above all, ourselves. Have technologic wonders and precise laboratory tests supplanted the adage “doctors are only human”? Dr. Wu also points out in this landmark essay his observation and dismay at the lack of empathy, sympathy, and compassion shown by peers when medical errors occur. All of these elements are needed for the healing of those involved to take place. If they are not provided, dysfunctional coping mechanisms ensue.4
Incidence of medical errors
Despite the Institute of Medicine report from 20001 and the recent study from Johns Hopkins,2 determining the exact number of errors and incidents is not easy. Most data reporting is sparse. A prospective longitudinal study of perceived medical errors and resident distress estimated medical errors to be between 5% and 10% in hospitalized patients, but that it could be up to 50%.5 According to a 2005 study, approximately one-third of internal medicine residents report at least 1 major medical error during their 3 years of training, while 18% of multidisciplinary residents report an adverse event under their care in the previous week.6
Related article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
Who is at risk of becoming a second victim?
Any and all clinicians can become a second victim, and the state can be realized at varying points in the process of an experienced medical error. The circumstances of the initial error and the severity of the effect on the patient and/or the damaged physician−patient relationship can affect whether or not there is a second victim. A second victim also can emerge as a result of peers’ or colleagues’ comments and lack of empathy or support. Certainly a lawsuit can produce a second victim.7
How often do physicians become second victims?
The prevalence of second victims has a large variation in estimates. A 2006 study estimates a prevalence of 10.4%.8 In 2010, the estimate was 30%, and a prevalence of 43.3% was reported in 2000.9,10 Regarding emotional distress within a year of a major adverse event, 30% of almost 900 providers reported these feelings.11 Other studies note 50% of health care workers reported feelings consistent with those of a second victim.7
Next: What are the symptoms of a second victim?
The signs of, and long-lasting risks for, a second victim
Second victims are at risk for several well-documented symptoms, regardless of their stage of training, including6:
- depression (in fact, they have a 3-fold risk)
- decrease in overall quality of life
- increase in burnout
- increase in feelings of distress, guilt, and shame, which may be long lasting.
Health care providers as second victims also may experience shock and hopelessness, sleep disturbance, social avoidance, intrusive thoughts and nightmares, and poor memory and concentration. Interestingly, these emotions and reactions are indistinguishable from posttraumatic stress disorder. These continued symptoms can have short- and long-term implications for physicians, patients, and the health care organization.12
Next: How to support those affected by a medical error
How to support all of those affected by a medical error
Over the past decade or so, much attention has been paid to creating safer health systems, improving outcomes and patient satisfaction, and recognizing the needs of patients and families of first victims when medical errors occur. Much less has been done to acknowledge and address the needs of struggling clinicians.
Provide nurturing discussions and sympathy
Hospital systems do have embedded processes to review outcomes and medical errors, including, among others, peer review, quality improvement, morbidity and mortality review, and root cause analysis. Unfortunately, often a “name, blame, shame game” can result from the overall process, with certain individuals or groups of individuals singled out, and only worsen the incidence and effects of the second victim. Ideally, system processes for addressing medical errors should allow for an environment more focused on nurturing discussions to prevent error and recognize all the factors contributing to an error.
Of course in any outcome or error investigation, the goal is to identify what happened, what factors contributed to the incident, and what can be done to prevent future occurrences. The concern for the family as priority is understandable, as is the desire to prevent a lawsuit. The lack of attention and sympathy to the health care provider involved contributes to the second victim.7
It is all too easy to blame, even in a Just Culture. Deficiencies in sympathy and attention can occur without a system whose culture is focused on “name, blame, shame.” A Just Culture, as defined by the Institute for Healthcare Improvement, is one in which individuals come forward with a mistake without fear of punishment. Such a culture balances the need to learn from our mistakes and the need to have disciplinary action.13
David Marx, an outcomes engineer and author of “Whack a Mole: The Price We Pay for Expecting Perfection,” touts a Just Culture as one having the following sets of beliefs:
- recognition that professionals will make mistakes
- recognition that even professionals will develop unhealthy norms
- a fierce intolerance for reckless conduct.
He strongly asserts that human error be consoled while reckless behavior be punished.14 Punishing human error is a setup for the second victim.
Read on for tips to develop a coping program
Tips for developing a coping program
In 2009, Scott and colleagues described 6 stages of a second victim. These are:
- Stage 1: Chaos and event repair
- Stage 2: Intrusive thoughts, “what if”
- Stage 3: Restoring personal identity
- Stage 4: Enduring the inquisition
- Stage 5: Obtaining emotional first aid
- Stage 6: Moving on or dropping out; surviving and/or thriving
Throughout the stages, second victims look for support and share their experience of the medical error event, as well as their personal and professional impact of the error.15
A 2007 study that examined the emotional impact of medical errors on physicians revealed some startling data. A full 82% of physicians expressed interest in counseling to help cope with their distress. And 90% felt there was inadequate support at their hospitals or health care organizations for this distress.16
Use The Joint Commission’s toolkit
Unfortunately, there are only a few well-documented second-victim support programs in the United States, despite the growing evidence of the emotional distress that second victims experience. Many hospitals do not know how to develop or implement such a support system. Recognizing this challenge, The Joint Commission developed a toolkit to assist health care organizations in developing a second-victim program. The toolkit consists of 10 modules (TABLE) designed to assist organizations not only to implement a second-victim support process but also to customize it to their specific institutional culture. This toolkit can be downloaded for free or used online. Within the first year of its availability, over 6,000 people visited the website and there were more than 700 requests for a download.17
Follow forYOU’s example
An example and well-recognized second-victim support program is the “forYOU” team at the University of Missouri. The program is free to employees, confidential, and available 24-7. Its purpose is “providing care and support to our staff,” by helping members understand the phenomenon of the second victim and quickly returning members to a satisfying professional practice.18
The “forYOU” team was created in 2007 under the direction of the University of Missouri Health Care’s Office of Clinical Effectiveness with the goals of increasing institutional awareness, providing a second victim with a “safe zone,” and allowing for the expression of emotions and reactions in a confidential setting. Team members are multidisciplinary and include physicians, nurses, respiratory therapists, social workers, and chaplains. They strive to normalize the feelings and thoughts second victims experience after a stressful outcome or event. Team members are highly trained in second-victim responses and the stages of coping. The program has established institutional actions to each of the 6 stages (FIGURE).19
Read on to learn how peer mentors are crucial to a support program
Establish TRUST
At the Carilion Clinic in Roanoke, Virginia, we too have developed a second-victim support program for all of our employees: TRUST. In the beginning stages, we quickly reaffirmed the challenges in developing such a program.
Initial challenges you will face. First, education on what a second victim is needs to be recognized. The fact that not everyone experiences second-victim emotions needs to be validated. Administrators and staff must be convinced that needing support is not a sign of weakness. And the program must ensure confidentiality and recruit mentors. These are just a few of the obstacles we faced on our path to program realization. Our journey to develop our second-victim program was approximately 5 years and required participation, affirmation, and support from all levels of the organization.
Our program name embodies its inherent purpose and goals. TRUST stands for:
- Treatment that is just. Second victims deserve the right of a presumption that their intentions were good, and should be able to depend on organizational leaders for integrity, fairness, just treatment, and shared accountability for outcomes.
- Respect. Second victims deserve respect and common decency and should not be blamed and shamed for human fallibility.
- Understanding and compassion. Second victims need compassionate help to grieve and heal.
- Supportive care. Second victims are entitled to psychological and support services that are delivered in a professional and organized way.
- Transparency and opportunity to contribute. Second victims have a right to participate in the learning gathered from the event, to share important causal information with the organization, and to be provided with an opportunity to heal by contributing to the prevention of future events.
Employ peer mentors, who serve a vital role
We have identified the need to develop a more direct and active approach to the TRUST program’s recruitment and established a subcommittee to begin this process. We began by asking leaders to nominate potential peer mentors and spoke about the program and asked for volunteers at various hospital committees. Once we had most disciplines represented, leaders were asked to take an assessment for emotional intelligence.
Other than the initial training for the TRUST program, the time requirement for participation for peer mentors is likely less than an hour per month. The dedicated time certainly is dependent on how much support the second victim is requiring, however, and varies. We encourage the peer supporters to be aware of their time constraints and establish parameters for the relationship in a direct but supportive way.
Since the inception of the TRUST Team in September 2014, we have trained 12 peer mentors, 10 of whom currently still serve in that capacity. We have 3 additional peers awaiting training. To date, The TRUST team has supported 19 clinicians/staff, including 3 ACPs, 9 nurses, 6 physicians, and 1 other (pharmacist). Of those 10, 3 are still actively receiving support so closing data have yet to be collected. Of the 16 who have been closed, 6 were referred for ongoing support and 10 were able to return to baseline with TRUST Team Supports.
Related article:
Who is liable when a surgical error occurs?
Just surviving the medical error is not the goal
Medical errors are inevitable, and the effects on providers can be devastating. It is important that physicians and institutions are aware of the signs and symptoms of a second victim as well as provide support to them. Institutions must have a just culture in which all members of the health care team can come forward with medical errors without the fear of punishment. Ideally, these institutions also have a second-victim support system that identifies those who need assistance and assist all health care clinicians not only to survive the effects of medical errors but also to thrive after receiving the necessary support.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academy Press; 2000. http://www.nap.edu/books/0309068371/html. Accessed December 18, 2016.
- Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affairs (Millwood). 2008;27(3):759−769. http://www.ihi.org/resources/Pages/Publications/TripleAimCareHealthandCost.aspx. Accessed December 18, 2016.
- Wu AW. Medical error: The second victim. The doctor who makes the mistake needs help too. BMJ . 2000;320(7237):726−727.
- West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071−1078.
- Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hetter M, Weissman JS. Residents report on adverse events and their causes. Arch Intern Med. 2005;165(22):2607−2613.
- Wu AW, Steckelberg RC. Medical error, incident investigation, and the second victim: doing better but feeling worse? BMJ Qual Saf. 2012;21(4):267−270.
- Lander LI, Connor JA, Shah RK, Kentala E, Healy, GB, Roberson DW. Otolaryngologists’ responses to errors and adverse events. Laryngoscope. 2006;116(7):1114−1120.
- Scott SD, Hirschinger LE, Cox KR. Sharing the load. Rescuing the healer after trauma. RN. 2008;71(12):38−40,42−43.
- Wolf ZR. Stress management in response to practice errors: critical events in professional practice. PA-PSRS Patient Safety Advisory. 2005;2:1−2.
- Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233−240.
- Edrees HH, Paine LA, Feroli ER, Wu AW. Health care workers as second victims of medical errors. Pol Arch Med Wewn. 2011;121(4):101−108.
- Leonard M. Organizational fairness/Just Culture. Cambridge, MA: Institute for Healthcare Improvement; 2012. http://app.ihi.org/extranetng/content/58886256-47d8-4f9c-bf7b-0afc352f013a/0efbd6cd-d0a3-4353-ad84-c86d07f499e1/4_5_Just%20Culture_ML.pdf. Accessed December 18, 2016.
- Marx D. Whack-a-Mole: The Price We Pay for Expecting Perfection. Plano, TX: By Your Side Studios; 2009.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(5):325−330.
- Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467−476.
- Pratt S, Kenney L, Scott SD, Wu AW. How to develop a second victim support program: a toolkit for health care organizations. Jt Comm J Qual Patient Saf. 2012;38(5):235−240,193.
- forYOU Team. Caring for our own. University of Missouri Health System website. http://www.muhealth.org/about/quality-of-care/office-of-clinical-effectiveness/foryou-team/. Accessed December 18, 2016.
- Second victim trajectory. Columbia, MO: University of Missouri Health System; 2009. http://www.muhealth.org/app/files/public/1390/6StagesRecovery.pdf. Accessed December 19, 2016.
- To err is human: Building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, eds. Washington, DC: National Academy Press; 2000. http://www.nap.edu/books/0309068371/html. Accessed December 18, 2016.
- Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affairs (Millwood). 2008;27(3):759−769. http://www.ihi.org/resources/Pages/Publications/TripleAimCareHealthandCost.aspx. Accessed December 18, 2016.
- Wu AW. Medical error: The second victim. The doctor who makes the mistake needs help too. BMJ . 2000;320(7237):726−727.
- West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071−1078.
- Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hetter M, Weissman JS. Residents report on adverse events and their causes. Arch Intern Med. 2005;165(22):2607−2613.
- Wu AW, Steckelberg RC. Medical error, incident investigation, and the second victim: doing better but feeling worse? BMJ Qual Saf. 2012;21(4):267−270.
- Lander LI, Connor JA, Shah RK, Kentala E, Healy, GB, Roberson DW. Otolaryngologists’ responses to errors and adverse events. Laryngoscope. 2006;116(7):1114−1120.
- Scott SD, Hirschinger LE, Cox KR. Sharing the load. Rescuing the healer after trauma. RN. 2008;71(12):38−40,42−43.
- Wolf ZR. Stress management in response to practice errors: critical events in professional practice. PA-PSRS Patient Safety Advisory. 2005;2:1−2.
- Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36(5):233−240.
- Edrees HH, Paine LA, Feroli ER, Wu AW. Health care workers as second victims of medical errors. Pol Arch Med Wewn. 2011;121(4):101−108.
- Leonard M. Organizational fairness/Just Culture. Cambridge, MA: Institute for Healthcare Improvement; 2012. http://app.ihi.org/extranetng/content/58886256-47d8-4f9c-bf7b-0afc352f013a/0efbd6cd-d0a3-4353-ad84-c86d07f499e1/4_5_Just%20Culture_ML.pdf. Accessed December 18, 2016.
- Marx D. Whack-a-Mole: The Price We Pay for Expecting Perfection. Plano, TX: By Your Side Studios; 2009.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009;18(5):325−330.
- Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467−476.
- Pratt S, Kenney L, Scott SD, Wu AW. How to develop a second victim support program: a toolkit for health care organizations. Jt Comm J Qual Patient Saf. 2012;38(5):235−240,193.
- forYOU Team. Caring for our own. University of Missouri Health System website. http://www.muhealth.org/about/quality-of-care/office-of-clinical-effectiveness/foryou-team/. Accessed December 18, 2016.
- Second victim trajectory. Columbia, MO: University of Missouri Health System; 2009. http://www.muhealth.org/app/files/public/1390/6StagesRecovery.pdf. Accessed December 19, 2016.
Embrace change as a hospitalist leader
We work in complex environments and in a flawed and rapidly changing health care system. Caregivers, patients, and communities will be led through this complexity by those who embrace change. Last October, I had the privilege of attending and facilitating the SHM Leadership Academy in Orlando, which allowed me the opportunity to meet a group of people who embrace change, including the benefits and challenges that often accompany it.
SHM board member Jeff Glasheen, MD, SFHM, taught one of the first lessons at Leadership Academy, focusing on the importance of meaningful, difficult change. With comparisons to companies that have embraced change, like Apple, and some that have not, like Sears, Jeff summed up how complacency with “good” and a reluctance to tackle the difficulty of change keeps organizations – and people – from becoming great.
“Good is the enemy of great,” Jeff preached.
He largely focused on hospitalists leading organizational change, but the concepts can apply to personal change, too. He explained that “people generally want things to be different, but they don’t want to change.”
Leaders in training
Ten emerging hospitalist leaders sat at my table, soaking in the message. Several of them, like me 8 years ago, had the responsibilities of leadership unexpectedly thrust upon them. Some carried with them the heavy expectations of their colleagues or hospital administration (or both) that by being elevated into a role such as medical director, they would abruptly be able to make improvements in patient care and hospital operations. They had accepted the challenge to change – to move out of purely clinical roles and take on new ones in leadership despite having little or no experience. Doing so, they gingerly but willingly were following in the footsteps of leaders before them, growing their skills, improving their hospitals, and laying a path for future leaders to follow.
A few weeks prior, I had taken a new leadership position myself. The Cleveland Clinic recently acquired a hospital and health system in Akron, Ohio, about 40 miles away from the city. I assumed the role of president of this acquisition, embracing the complex challenge of leading the process of integrating two health systems. After 3 years overseeing a different hospital in the health system, I finally felt I had developed the people, processes, and culture that I had been striving to build. But like the young leaders at Leadership Academy, I had the opportunity to change, grow, develop, take on new risk, and become a stronger leader in this new role. A significant part of the experience of the Leadership Academy involves table exercises. For the first few exercises, the group was quiet, uncertain, tentative. I was struck both by how early these individuals were in their development and by how so much of what is happening today in hospitals and health care is dependent upon the development and success of individuals like these who are enthusiastic and talented but young and overwhelmed.
I believe that successful hospitalists are, through experience, training, and nature, rapid assimilators into their environments. By the third day, the dynamic at my table had gone from tentative and uncertain to much more confident and assertive. To experience this transformation in person at SHM’s Leadership Academy, we welcome you to Scottsdale, Ariz., later this year. Learn more about the program at www.shmleadershipacademy.org.
At Leadership Academy and beyond, I implore hospitalists to look for opportunities to change during this time of New Year’s resolutions and to take the opposite posture and want to change – change how we think, act, and respond; change our roles to take on new, uncomfortable responsibilities; and change how we view change itself.
We will be better for it both personally and professionally, and we will stand out as role models for our colleagues, coworkers, and hospitalists who follow in our footsteps.
Dr. Harte is a practicing hospitalist, president of the Society of Hospital Medicine, and president of Hillcrest Hospital in Mayfield Heights, Ohio, part of the Cleveland Clinic Health System. He is associate professor of medicine at the Cleveland Clinic, Lerner College of Medicine in Cleveland.
We work in complex environments and in a flawed and rapidly changing health care system. Caregivers, patients, and communities will be led through this complexity by those who embrace change. Last October, I had the privilege of attending and facilitating the SHM Leadership Academy in Orlando, which allowed me the opportunity to meet a group of people who embrace change, including the benefits and challenges that often accompany it.
SHM board member Jeff Glasheen, MD, SFHM, taught one of the first lessons at Leadership Academy, focusing on the importance of meaningful, difficult change. With comparisons to companies that have embraced change, like Apple, and some that have not, like Sears, Jeff summed up how complacency with “good” and a reluctance to tackle the difficulty of change keeps organizations – and people – from becoming great.
“Good is the enemy of great,” Jeff preached.
He largely focused on hospitalists leading organizational change, but the concepts can apply to personal change, too. He explained that “people generally want things to be different, but they don’t want to change.”
Leaders in training
Ten emerging hospitalist leaders sat at my table, soaking in the message. Several of them, like me 8 years ago, had the responsibilities of leadership unexpectedly thrust upon them. Some carried with them the heavy expectations of their colleagues or hospital administration (or both) that by being elevated into a role such as medical director, they would abruptly be able to make improvements in patient care and hospital operations. They had accepted the challenge to change – to move out of purely clinical roles and take on new ones in leadership despite having little or no experience. Doing so, they gingerly but willingly were following in the footsteps of leaders before them, growing their skills, improving their hospitals, and laying a path for future leaders to follow.
A few weeks prior, I had taken a new leadership position myself. The Cleveland Clinic recently acquired a hospital and health system in Akron, Ohio, about 40 miles away from the city. I assumed the role of president of this acquisition, embracing the complex challenge of leading the process of integrating two health systems. After 3 years overseeing a different hospital in the health system, I finally felt I had developed the people, processes, and culture that I had been striving to build. But like the young leaders at Leadership Academy, I had the opportunity to change, grow, develop, take on new risk, and become a stronger leader in this new role. A significant part of the experience of the Leadership Academy involves table exercises. For the first few exercises, the group was quiet, uncertain, tentative. I was struck both by how early these individuals were in their development and by how so much of what is happening today in hospitals and health care is dependent upon the development and success of individuals like these who are enthusiastic and talented but young and overwhelmed.
I believe that successful hospitalists are, through experience, training, and nature, rapid assimilators into their environments. By the third day, the dynamic at my table had gone from tentative and uncertain to much more confident and assertive. To experience this transformation in person at SHM’s Leadership Academy, we welcome you to Scottsdale, Ariz., later this year. Learn more about the program at www.shmleadershipacademy.org.
At Leadership Academy and beyond, I implore hospitalists to look for opportunities to change during this time of New Year’s resolutions and to take the opposite posture and want to change – change how we think, act, and respond; change our roles to take on new, uncomfortable responsibilities; and change how we view change itself.
We will be better for it both personally and professionally, and we will stand out as role models for our colleagues, coworkers, and hospitalists who follow in our footsteps.
Dr. Harte is a practicing hospitalist, president of the Society of Hospital Medicine, and president of Hillcrest Hospital in Mayfield Heights, Ohio, part of the Cleveland Clinic Health System. He is associate professor of medicine at the Cleveland Clinic, Lerner College of Medicine in Cleveland.
We work in complex environments and in a flawed and rapidly changing health care system. Caregivers, patients, and communities will be led through this complexity by those who embrace change. Last October, I had the privilege of attending and facilitating the SHM Leadership Academy in Orlando, which allowed me the opportunity to meet a group of people who embrace change, including the benefits and challenges that often accompany it.
SHM board member Jeff Glasheen, MD, SFHM, taught one of the first lessons at Leadership Academy, focusing on the importance of meaningful, difficult change. With comparisons to companies that have embraced change, like Apple, and some that have not, like Sears, Jeff summed up how complacency with “good” and a reluctance to tackle the difficulty of change keeps organizations – and people – from becoming great.
“Good is the enemy of great,” Jeff preached.
He largely focused on hospitalists leading organizational change, but the concepts can apply to personal change, too. He explained that “people generally want things to be different, but they don’t want to change.”
Leaders in training
Ten emerging hospitalist leaders sat at my table, soaking in the message. Several of them, like me 8 years ago, had the responsibilities of leadership unexpectedly thrust upon them. Some carried with them the heavy expectations of their colleagues or hospital administration (or both) that by being elevated into a role such as medical director, they would abruptly be able to make improvements in patient care and hospital operations. They had accepted the challenge to change – to move out of purely clinical roles and take on new ones in leadership despite having little or no experience. Doing so, they gingerly but willingly were following in the footsteps of leaders before them, growing their skills, improving their hospitals, and laying a path for future leaders to follow.
A few weeks prior, I had taken a new leadership position myself. The Cleveland Clinic recently acquired a hospital and health system in Akron, Ohio, about 40 miles away from the city. I assumed the role of president of this acquisition, embracing the complex challenge of leading the process of integrating two health systems. After 3 years overseeing a different hospital in the health system, I finally felt I had developed the people, processes, and culture that I had been striving to build. But like the young leaders at Leadership Academy, I had the opportunity to change, grow, develop, take on new risk, and become a stronger leader in this new role. A significant part of the experience of the Leadership Academy involves table exercises. For the first few exercises, the group was quiet, uncertain, tentative. I was struck both by how early these individuals were in their development and by how so much of what is happening today in hospitals and health care is dependent upon the development and success of individuals like these who are enthusiastic and talented but young and overwhelmed.
I believe that successful hospitalists are, through experience, training, and nature, rapid assimilators into their environments. By the third day, the dynamic at my table had gone from tentative and uncertain to much more confident and assertive. To experience this transformation in person at SHM’s Leadership Academy, we welcome you to Scottsdale, Ariz., later this year. Learn more about the program at www.shmleadershipacademy.org.
At Leadership Academy and beyond, I implore hospitalists to look for opportunities to change during this time of New Year’s resolutions and to take the opposite posture and want to change – change how we think, act, and respond; change our roles to take on new, uncomfortable responsibilities; and change how we view change itself.
We will be better for it both personally and professionally, and we will stand out as role models for our colleagues, coworkers, and hospitalists who follow in our footsteps.
Dr. Harte is a practicing hospitalist, president of the Society of Hospital Medicine, and president of Hillcrest Hospital in Mayfield Heights, Ohio, part of the Cleveland Clinic Health System. He is associate professor of medicine at the Cleveland Clinic, Lerner College of Medicine in Cleveland.
Effective hospitalist roles for NPs, PAs
I’m often asked about effective roles for nurse practitioners (NPs) and physician assistants (PAs), collectively known as advanced practice clinicians (APCs). My first response is always the same: They have much to contribute and can be effective members of hospitalist groups. Most hospital medicine groups (HMGs) should think about having them in their staffing mix if they don’t already.
Yet despite all that NPs/PAs can offer, my experience is that many (even most) hospitalist groups fail to develop roles that optimize their APCs’ skills.
An October 2016 study in the Journal of Clinical Outcomes Management adds additional data to help think about this issue. You may have seen the study mentioned in several news articles and blogs. Most summarized the study along the lines of “using high levels of PA staffing results in lower hospital costs per case.” Framing it this way is awfully misleading, so I’ll go a little deeper here.
Study context
The study, “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” is a retrospective analysis of performance measures from two hospitalist groups at Anne Arundel Medical Center (AAMC) in Annapolis, Md.1 One HMG is employed by the hospital. The other, called MDICS, is a private company that contracts with AAMC as well as approximately 13 other hospitals and 40 rehabilitation facilities. Tim Capstack, MD, is the AAMC medical director for MDICS and lead author of the study (representing a potential conflict of interest acknowledged in the article). Barry Meisenberg, MD, is a coauthor, a hospitalist in the AAMC-employed group, and chair for quality improvement and health care systems research at AAMC.
Tim told me by phone that both groups have practiced at AAMC for more than 10 years and enjoy a collegial relationship. Both groups employ PAs and pair them with a single physician in a dyad arrangement each day. Tim’s MDICS group, the “expanded PA” group, staffs each day shift with three physicians and three PAs, compared with the nine physicians and two PAs in the hospital-employed “conventional” group. The MDICS PAs are responsible for more patients each day than their conventional-group counterparts and, during the January 2012 to July 2013 study period, averaged 14.2 patients versus 8.3, respectively.
Over the course of the study, PAs in the expanded PA group saw and billed 36% of patient visits independently, compared with 5.9% for the conventional group.
Notable study findings
I think the main value of this study is in showing that the expanded PA group had rates of readmission, inpatient mortality, length of stay, and consultant use that weren’t statistically different from the conventional group.
The workloads and years of experience of doctors and PAs in each group were similar. And while there were some differences in the patients each group cared for, they seem unlikely to have a significant influence on outcomes. Clearly, there are many unmeasured variables (e.g., culture, morale, and leadership) in each group that could have influenced the outcomes, so this one study at one hospital doesn’t provide a definitive answer about appropriate APC staffing levels. However, it didn’t uncover big differences in the measured outcomes.
And this study did show that higher levels of PA staffing were associated with lower hospital charges per case. Although the difference was a modest 3%, it was statistically significant (P less than .001). I’m skeptical there is causation here; this more likely is just correlation.
It would be great to see a larger study of this.
Information applications
So does this study support the idea that HMGs can or should increase APC staffing and workload significantly to realize lower hospital cost per case and not harm patient outcomes? Not so fast!
This study only compared two hospitalist groups at one hospital. It’s probably not very generalizable.
And as described in the paper, and stressed by Tim talking with me by phone, the outcomes of their expanded PA model likely have a lot to do with their very careful recruiting and screening of experienced PAs before hiring them, not to mention a lengthy and deliberate on-boarding process (summarized in the article) to support their ability to perform well. Groups that are not as thoughtful and deliberate in how they hire and position APCs to contribute to the practice may not perform as well.
Why study only PAs? What about NPs? Tim told me that his group is agnostic regarding the training background of the APCs they hire; he suspects an identical study with NPs rather than PAs in each hospitalist group would probably yield very similar results. I see this the same way. Although there are differences in background and training between NPs and PAs, I think personal traits like years of experience in various health care settings and the ability to work efficiently are more important than training background.
A practical approach
Any group who thinks this study is evidence that adding more APCs and having them manage a higher number of patients relatively independently will go well in any setting is mistaken. But it does offer a story of one place where, with careful planning and execution, it went OK.
In my view, the real take-home message is to think carefully to ensure any APCs in your group have professionally satisfying roles that position them to contribute effectively. While common, I think configuring APCs and physicians as rounding dyads often ends up underperforming and not working out well because of inefficiency. When well executed, as is apparently the case in this study, it can be fine. But my experience is that positioning APCs to assume primary responsibility for some clinical activities, such as covering the observation unit or serving as an evening admitter/cross-cover provider (all with appropriate physician collaboration and backup), more reliably turns out well.
Reference
Capstack TM, Seguija C, Vollono LM, Moser JD, Meisenberg BR, Michtalik HJ. A comparison of conventional and expanded physician assistant hospitalist staffing models at a community hospital. J Clin Outcomes Manag. 2016;23(10):455-61.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
I’m often asked about effective roles for nurse practitioners (NPs) and physician assistants (PAs), collectively known as advanced practice clinicians (APCs). My first response is always the same: They have much to contribute and can be effective members of hospitalist groups. Most hospital medicine groups (HMGs) should think about having them in their staffing mix if they don’t already.
Yet despite all that NPs/PAs can offer, my experience is that many (even most) hospitalist groups fail to develop roles that optimize their APCs’ skills.
An October 2016 study in the Journal of Clinical Outcomes Management adds additional data to help think about this issue. You may have seen the study mentioned in several news articles and blogs. Most summarized the study along the lines of “using high levels of PA staffing results in lower hospital costs per case.” Framing it this way is awfully misleading, so I’ll go a little deeper here.
Study context
The study, “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” is a retrospective analysis of performance measures from two hospitalist groups at Anne Arundel Medical Center (AAMC) in Annapolis, Md.1 One HMG is employed by the hospital. The other, called MDICS, is a private company that contracts with AAMC as well as approximately 13 other hospitals and 40 rehabilitation facilities. Tim Capstack, MD, is the AAMC medical director for MDICS and lead author of the study (representing a potential conflict of interest acknowledged in the article). Barry Meisenberg, MD, is a coauthor, a hospitalist in the AAMC-employed group, and chair for quality improvement and health care systems research at AAMC.
Tim told me by phone that both groups have practiced at AAMC for more than 10 years and enjoy a collegial relationship. Both groups employ PAs and pair them with a single physician in a dyad arrangement each day. Tim’s MDICS group, the “expanded PA” group, staffs each day shift with three physicians and three PAs, compared with the nine physicians and two PAs in the hospital-employed “conventional” group. The MDICS PAs are responsible for more patients each day than their conventional-group counterparts and, during the January 2012 to July 2013 study period, averaged 14.2 patients versus 8.3, respectively.
Over the course of the study, PAs in the expanded PA group saw and billed 36% of patient visits independently, compared with 5.9% for the conventional group.
Notable study findings
I think the main value of this study is in showing that the expanded PA group had rates of readmission, inpatient mortality, length of stay, and consultant use that weren’t statistically different from the conventional group.
The workloads and years of experience of doctors and PAs in each group were similar. And while there were some differences in the patients each group cared for, they seem unlikely to have a significant influence on outcomes. Clearly, there are many unmeasured variables (e.g., culture, morale, and leadership) in each group that could have influenced the outcomes, so this one study at one hospital doesn’t provide a definitive answer about appropriate APC staffing levels. However, it didn’t uncover big differences in the measured outcomes.
And this study did show that higher levels of PA staffing were associated with lower hospital charges per case. Although the difference was a modest 3%, it was statistically significant (P less than .001). I’m skeptical there is causation here; this more likely is just correlation.
It would be great to see a larger study of this.
Information applications
So does this study support the idea that HMGs can or should increase APC staffing and workload significantly to realize lower hospital cost per case and not harm patient outcomes? Not so fast!
This study only compared two hospitalist groups at one hospital. It’s probably not very generalizable.
And as described in the paper, and stressed by Tim talking with me by phone, the outcomes of their expanded PA model likely have a lot to do with their very careful recruiting and screening of experienced PAs before hiring them, not to mention a lengthy and deliberate on-boarding process (summarized in the article) to support their ability to perform well. Groups that are not as thoughtful and deliberate in how they hire and position APCs to contribute to the practice may not perform as well.
Why study only PAs? What about NPs? Tim told me that his group is agnostic regarding the training background of the APCs they hire; he suspects an identical study with NPs rather than PAs in each hospitalist group would probably yield very similar results. I see this the same way. Although there are differences in background and training between NPs and PAs, I think personal traits like years of experience in various health care settings and the ability to work efficiently are more important than training background.
A practical approach
Any group who thinks this study is evidence that adding more APCs and having them manage a higher number of patients relatively independently will go well in any setting is mistaken. But it does offer a story of one place where, with careful planning and execution, it went OK.
In my view, the real take-home message is to think carefully to ensure any APCs in your group have professionally satisfying roles that position them to contribute effectively. While common, I think configuring APCs and physicians as rounding dyads often ends up underperforming and not working out well because of inefficiency. When well executed, as is apparently the case in this study, it can be fine. But my experience is that positioning APCs to assume primary responsibility for some clinical activities, such as covering the observation unit or serving as an evening admitter/cross-cover provider (all with appropriate physician collaboration and backup), more reliably turns out well.
Reference
Capstack TM, Seguija C, Vollono LM, Moser JD, Meisenberg BR, Michtalik HJ. A comparison of conventional and expanded physician assistant hospitalist staffing models at a community hospital. J Clin Outcomes Manag. 2016;23(10):455-61.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
I’m often asked about effective roles for nurse practitioners (NPs) and physician assistants (PAs), collectively known as advanced practice clinicians (APCs). My first response is always the same: They have much to contribute and can be effective members of hospitalist groups. Most hospital medicine groups (HMGs) should think about having them in their staffing mix if they don’t already.
Yet despite all that NPs/PAs can offer, my experience is that many (even most) hospitalist groups fail to develop roles that optimize their APCs’ skills.
An October 2016 study in the Journal of Clinical Outcomes Management adds additional data to help think about this issue. You may have seen the study mentioned in several news articles and blogs. Most summarized the study along the lines of “using high levels of PA staffing results in lower hospital costs per case.” Framing it this way is awfully misleading, so I’ll go a little deeper here.
Study context
The study, “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” is a retrospective analysis of performance measures from two hospitalist groups at Anne Arundel Medical Center (AAMC) in Annapolis, Md.1 One HMG is employed by the hospital. The other, called MDICS, is a private company that contracts with AAMC as well as approximately 13 other hospitals and 40 rehabilitation facilities. Tim Capstack, MD, is the AAMC medical director for MDICS and lead author of the study (representing a potential conflict of interest acknowledged in the article). Barry Meisenberg, MD, is a coauthor, a hospitalist in the AAMC-employed group, and chair for quality improvement and health care systems research at AAMC.
Tim told me by phone that both groups have practiced at AAMC for more than 10 years and enjoy a collegial relationship. Both groups employ PAs and pair them with a single physician in a dyad arrangement each day. Tim’s MDICS group, the “expanded PA” group, staffs each day shift with three physicians and three PAs, compared with the nine physicians and two PAs in the hospital-employed “conventional” group. The MDICS PAs are responsible for more patients each day than their conventional-group counterparts and, during the January 2012 to July 2013 study period, averaged 14.2 patients versus 8.3, respectively.
Over the course of the study, PAs in the expanded PA group saw and billed 36% of patient visits independently, compared with 5.9% for the conventional group.
Notable study findings
I think the main value of this study is in showing that the expanded PA group had rates of readmission, inpatient mortality, length of stay, and consultant use that weren’t statistically different from the conventional group.
The workloads and years of experience of doctors and PAs in each group were similar. And while there were some differences in the patients each group cared for, they seem unlikely to have a significant influence on outcomes. Clearly, there are many unmeasured variables (e.g., culture, morale, and leadership) in each group that could have influenced the outcomes, so this one study at one hospital doesn’t provide a definitive answer about appropriate APC staffing levels. However, it didn’t uncover big differences in the measured outcomes.
And this study did show that higher levels of PA staffing were associated with lower hospital charges per case. Although the difference was a modest 3%, it was statistically significant (P less than .001). I’m skeptical there is causation here; this more likely is just correlation.
It would be great to see a larger study of this.
Information applications
So does this study support the idea that HMGs can or should increase APC staffing and workload significantly to realize lower hospital cost per case and not harm patient outcomes? Not so fast!
This study only compared two hospitalist groups at one hospital. It’s probably not very generalizable.
And as described in the paper, and stressed by Tim talking with me by phone, the outcomes of their expanded PA model likely have a lot to do with their very careful recruiting and screening of experienced PAs before hiring them, not to mention a lengthy and deliberate on-boarding process (summarized in the article) to support their ability to perform well. Groups that are not as thoughtful and deliberate in how they hire and position APCs to contribute to the practice may not perform as well.
Why study only PAs? What about NPs? Tim told me that his group is agnostic regarding the training background of the APCs they hire; he suspects an identical study with NPs rather than PAs in each hospitalist group would probably yield very similar results. I see this the same way. Although there are differences in background and training between NPs and PAs, I think personal traits like years of experience in various health care settings and the ability to work efficiently are more important than training background.
A practical approach
Any group who thinks this study is evidence that adding more APCs and having them manage a higher number of patients relatively independently will go well in any setting is mistaken. But it does offer a story of one place where, with careful planning and execution, it went OK.
In my view, the real take-home message is to think carefully to ensure any APCs in your group have professionally satisfying roles that position them to contribute effectively. While common, I think configuring APCs and physicians as rounding dyads often ends up underperforming and not working out well because of inefficiency. When well executed, as is apparently the case in this study, it can be fine. But my experience is that positioning APCs to assume primary responsibility for some clinical activities, such as covering the observation unit or serving as an evening admitter/cross-cover provider (all with appropriate physician collaboration and backup), more reliably turns out well.
Reference
Capstack TM, Seguija C, Vollono LM, Moser JD, Meisenberg BR, Michtalik HJ. A comparison of conventional and expanded physician assistant hospitalist staffing models at a community hospital. J Clin Outcomes Manag. 2016;23(10):455-61.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
What can administrators and ObGyns do together to reduce physician burnout?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Related content on burnout:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Related content on burnout:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Related content on burnout:
Keeping up with New Payment Models
While in medical school, I learned about what was then called GRID (gay-related immune deficiency) and we now know as HIV/AIDS. I thought this condition would become so central to practice in nearly any specialty that I decided to try to keep up with all of the literature on it. It wasn’t yet in textbooks, so I thought it would be very important to keep up with all the new research studies and review articles about it.
I kept in my apartment a growing file of articles photocopied and torn out of journals. But I had badly misjudged the enormity of the task, and within a few years, there were far too many articles for me to read or keep up with in any fashion. Before long, HIV medicine became its own specialty, and while it has always been something I, like any hospitalist, need to know something about, I’ve left it to others to be the real HIV experts.
I was naive to have embarked on the quest. What seemed manageable at first became overwhelming very quickly. The same could be said for trying to keep up with new payment models.
New Professional Fee Reimbursement Models
For decades, most physicians could understand the general concept of how their professional activities generated revenue. But it’s gotten a lot more complicated lately.
The growing prevalence of capitation and other managed-care reimbursement models in the ’80s and ’90s might have been when reimbursement complexity began to increase significantly. But while nearly every doctor in the country heard about managed care, for many, it was something happening elsewhere that never made its way to them.
But for hospitalists, I think the arrival of the Physician Quality Reporting System (PQRS, originally Physician Quality Reporting Initiative, or PQRI) marks the swerve in reimbursement complexity. Some years ago I wrote in these pages about the importance of hospitalists understanding PQRS and described key features of the program.
Like HIV/AIDS medicine literature, the breadth and complexity of reimbursement programs from the Centers for Medicare & Medicaid Services (and other payors) seem to have grown logarithmically since PQRS. The still relatively new bundled payment and MACRA-related models are far more complicated than PQRS. And they change often. Calendar milestones come and go with changes in relevant metrics and performance thresholds, etc. Even the terminology changes frequently. Did you know, for example, that under MIPSi “Advancing Care Information” is essentially a new name for EHR Meaningful Use?
Bundled payments and MACRA are only a small portion of new models implemented over the last few years. There are many others, and dedicated effort is required just to keep track of whether each model influences only physicians (and other providers), only hospitals, or both.
Clinicians’ Responsibility for Keeping Up
My thinking about most hospitalists, or doctors in any specialty, keeping up with all of these models has evolved the same way it did with HIV/AIDS. I think it’s pretty clear that it’s folly to expect most clinicians to know more than the broad outlines of these programs.
Payment models are important. Someone needs to know them in detail, but clinicians should reserve brain cells for clinical knowledge base and focus only on the big picture of payment models. Think how well you’ve done learning and keeping up with CPT coding, observation versus inpatient status determinations, and clinical documentation. You probably still aren’t an expert at these things, so is it wise to set about becoming an expert in new payment models?
Instead, most hospitalists should rely on others to keep up with the precise details of these programs. Most commonly that will mean our employer will appoint or hire one or more people, or engage an outside party, to do this.
Don’t Feel Guilty
It’s common to leave a presentation or doctor’s lounge conversation on payment models feeling like you need to study up on the details of this or that payment model since good performance under that model will be important for your paycheck and to remain a viable “player.” And speakers sometimes intentionally or unintentionally enhance your anxiety about this. Maybe they love to show off what they know, and it’s easy for them to think only about their topic and not keep in mind all of the other stuff you need to know.
It’s terrific if someone in your practice is particularly interested in payment models and chooses to stay on top of them. Just make sure that doesn’t come at the expense of keeping up with changes in clinical practice. Most groups won’t have such a person and should rely on others, including SHM, without feeling the smallest bit of guilt.
SHM is advocating on behalf of hospitalists and working diligently to distill the impact MACRA and its various alternative payment frameworks will have on hospital medicine. With webinars, Q&As, and additional online and print resources, SHM will continue to provide digestible updates for hospitalists and their practices.
The End of Small-Group Physician Practice?
While the intent of these programs is to encourage and reward improvements in clinical practice, keeping up with and managing them is a tax that takes resources away from clinical practice. This is an especially difficult burden for small private practices and may prove to be a significant factor in nearly extinguishing them. There are relatively few small private hospitalist groups,ii but all of them should carefully consider how they will keep up with new reimbursement models.
While in medical school, I learned about what was then called GRID (gay-related immune deficiency) and we now know as HIV/AIDS. I thought this condition would become so central to practice in nearly any specialty that I decided to try to keep up with all of the literature on it. It wasn’t yet in textbooks, so I thought it would be very important to keep up with all the new research studies and review articles about it.
I kept in my apartment a growing file of articles photocopied and torn out of journals. But I had badly misjudged the enormity of the task, and within a few years, there were far too many articles for me to read or keep up with in any fashion. Before long, HIV medicine became its own specialty, and while it has always been something I, like any hospitalist, need to know something about, I’ve left it to others to be the real HIV experts.
I was naive to have embarked on the quest. What seemed manageable at first became overwhelming very quickly. The same could be said for trying to keep up with new payment models.
New Professional Fee Reimbursement Models
For decades, most physicians could understand the general concept of how their professional activities generated revenue. But it’s gotten a lot more complicated lately.
The growing prevalence of capitation and other managed-care reimbursement models in the ’80s and ’90s might have been when reimbursement complexity began to increase significantly. But while nearly every doctor in the country heard about managed care, for many, it was something happening elsewhere that never made its way to them.
But for hospitalists, I think the arrival of the Physician Quality Reporting System (PQRS, originally Physician Quality Reporting Initiative, or PQRI) marks the swerve in reimbursement complexity. Some years ago I wrote in these pages about the importance of hospitalists understanding PQRS and described key features of the program.
Like HIV/AIDS medicine literature, the breadth and complexity of reimbursement programs from the Centers for Medicare & Medicaid Services (and other payors) seem to have grown logarithmically since PQRS. The still relatively new bundled payment and MACRA-related models are far more complicated than PQRS. And they change often. Calendar milestones come and go with changes in relevant metrics and performance thresholds, etc. Even the terminology changes frequently. Did you know, for example, that under MIPSi “Advancing Care Information” is essentially a new name for EHR Meaningful Use?
Bundled payments and MACRA are only a small portion of new models implemented over the last few years. There are many others, and dedicated effort is required just to keep track of whether each model influences only physicians (and other providers), only hospitals, or both.
Clinicians’ Responsibility for Keeping Up
My thinking about most hospitalists, or doctors in any specialty, keeping up with all of these models has evolved the same way it did with HIV/AIDS. I think it’s pretty clear that it’s folly to expect most clinicians to know more than the broad outlines of these programs.
Payment models are important. Someone needs to know them in detail, but clinicians should reserve brain cells for clinical knowledge base and focus only on the big picture of payment models. Think how well you’ve done learning and keeping up with CPT coding, observation versus inpatient status determinations, and clinical documentation. You probably still aren’t an expert at these things, so is it wise to set about becoming an expert in new payment models?
Instead, most hospitalists should rely on others to keep up with the precise details of these programs. Most commonly that will mean our employer will appoint or hire one or more people, or engage an outside party, to do this.
Don’t Feel Guilty
It’s common to leave a presentation or doctor’s lounge conversation on payment models feeling like you need to study up on the details of this or that payment model since good performance under that model will be important for your paycheck and to remain a viable “player.” And speakers sometimes intentionally or unintentionally enhance your anxiety about this. Maybe they love to show off what they know, and it’s easy for them to think only about their topic and not keep in mind all of the other stuff you need to know.
It’s terrific if someone in your practice is particularly interested in payment models and chooses to stay on top of them. Just make sure that doesn’t come at the expense of keeping up with changes in clinical practice. Most groups won’t have such a person and should rely on others, including SHM, without feeling the smallest bit of guilt.
SHM is advocating on behalf of hospitalists and working diligently to distill the impact MACRA and its various alternative payment frameworks will have on hospital medicine. With webinars, Q&As, and additional online and print resources, SHM will continue to provide digestible updates for hospitalists and their practices.
The End of Small-Group Physician Practice?
While the intent of these programs is to encourage and reward improvements in clinical practice, keeping up with and managing them is a tax that takes resources away from clinical practice. This is an especially difficult burden for small private practices and may prove to be a significant factor in nearly extinguishing them. There are relatively few small private hospitalist groups,ii but all of them should carefully consider how they will keep up with new reimbursement models.
While in medical school, I learned about what was then called GRID (gay-related immune deficiency) and we now know as HIV/AIDS. I thought this condition would become so central to practice in nearly any specialty that I decided to try to keep up with all of the literature on it. It wasn’t yet in textbooks, so I thought it would be very important to keep up with all the new research studies and review articles about it.
I kept in my apartment a growing file of articles photocopied and torn out of journals. But I had badly misjudged the enormity of the task, and within a few years, there were far too many articles for me to read or keep up with in any fashion. Before long, HIV medicine became its own specialty, and while it has always been something I, like any hospitalist, need to know something about, I’ve left it to others to be the real HIV experts.
I was naive to have embarked on the quest. What seemed manageable at first became overwhelming very quickly. The same could be said for trying to keep up with new payment models.
New Professional Fee Reimbursement Models
For decades, most physicians could understand the general concept of how their professional activities generated revenue. But it’s gotten a lot more complicated lately.
The growing prevalence of capitation and other managed-care reimbursement models in the ’80s and ’90s might have been when reimbursement complexity began to increase significantly. But while nearly every doctor in the country heard about managed care, for many, it was something happening elsewhere that never made its way to them.
But for hospitalists, I think the arrival of the Physician Quality Reporting System (PQRS, originally Physician Quality Reporting Initiative, or PQRI) marks the swerve in reimbursement complexity. Some years ago I wrote in these pages about the importance of hospitalists understanding PQRS and described key features of the program.
Like HIV/AIDS medicine literature, the breadth and complexity of reimbursement programs from the Centers for Medicare & Medicaid Services (and other payors) seem to have grown logarithmically since PQRS. The still relatively new bundled payment and MACRA-related models are far more complicated than PQRS. And they change often. Calendar milestones come and go with changes in relevant metrics and performance thresholds, etc. Even the terminology changes frequently. Did you know, for example, that under MIPSi “Advancing Care Information” is essentially a new name for EHR Meaningful Use?
Bundled payments and MACRA are only a small portion of new models implemented over the last few years. There are many others, and dedicated effort is required just to keep track of whether each model influences only physicians (and other providers), only hospitals, or both.
Clinicians’ Responsibility for Keeping Up
My thinking about most hospitalists, or doctors in any specialty, keeping up with all of these models has evolved the same way it did with HIV/AIDS. I think it’s pretty clear that it’s folly to expect most clinicians to know more than the broad outlines of these programs.
Payment models are important. Someone needs to know them in detail, but clinicians should reserve brain cells for clinical knowledge base and focus only on the big picture of payment models. Think how well you’ve done learning and keeping up with CPT coding, observation versus inpatient status determinations, and clinical documentation. You probably still aren’t an expert at these things, so is it wise to set about becoming an expert in new payment models?
Instead, most hospitalists should rely on others to keep up with the precise details of these programs. Most commonly that will mean our employer will appoint or hire one or more people, or engage an outside party, to do this.
Don’t Feel Guilty
It’s common to leave a presentation or doctor’s lounge conversation on payment models feeling like you need to study up on the details of this or that payment model since good performance under that model will be important for your paycheck and to remain a viable “player.” And speakers sometimes intentionally or unintentionally enhance your anxiety about this. Maybe they love to show off what they know, and it’s easy for them to think only about their topic and not keep in mind all of the other stuff you need to know.
It’s terrific if someone in your practice is particularly interested in payment models and chooses to stay on top of them. Just make sure that doesn’t come at the expense of keeping up with changes in clinical practice. Most groups won’t have such a person and should rely on others, including SHM, without feeling the smallest bit of guilt.
SHM is advocating on behalf of hospitalists and working diligently to distill the impact MACRA and its various alternative payment frameworks will have on hospital medicine. With webinars, Q&As, and additional online and print resources, SHM will continue to provide digestible updates for hospitalists and their practices.
The End of Small-Group Physician Practice?
While the intent of these programs is to encourage and reward improvements in clinical practice, keeping up with and managing them is a tax that takes resources away from clinical practice. This is an especially difficult burden for small private practices and may prove to be a significant factor in nearly extinguishing them. There are relatively few small private hospitalist groups,ii but all of them should carefully consider how they will keep up with new reimbursement models.
Benefit of self-administered vaginal lidocaine gel in IUD placement
Fear of potential pain caused by insertion of an intrauterine device (IUD) prevents some women from using this highly effective and safe contraceptive method. Recently, investigators conducted a randomized, placebo-controlled trial to assess whether vaginal lidocaine gel administered shortly before IUD placement was associated with a decrease from baseline in patient-reported pain scores.1
In this blinded trial, Rapkinand colleagues randomly assigned nulliparous women presenting for IUD placement (either the copper T380A IUD or the 52-mg levonorgestrel-releasing IUD) at faculty and resident clinics at a US urban academic center to place 4 mL of 2% lidocaine gel or placebo gel vaginally (using an applicator) 5 to 15 minutes prior to IUD placement.1 A 100-mm visual analog scale (VAS) was used to assess pain at each step of the procedure, including at baseline (before speculum insertion), after speculum placement, tenaculum placement, uterine sound, IUD insertion, and 5 minutes after speculum removal.
Among the 58 evaluable participants, the mean age was 23 years in the lidocaine group and 24 years in the placebo group; more than 80% of the women were white.
The study’s primary outcome was change in pain experience from baseline to IUD insertion. Pain was measured on a VAS from 0 mm (no pain) to 100 mm (worst pain in my life). Secondary outcomes included patient acceptability of gel self-insertion, physician-reported ease of IUD insertion, and need for pain medication for up to 7 days after IUD insertion.
Related article:
Liletta gets a new inserter: Steps for successful placement
What the investigators found
The mean change in pain scores with IUD placement was 61 mm for the lidocaine group and 69 mm for the placebo group (P = .06). Thus, no difference in the primary outcome was found between the 2 groups. However, women who received the lidocaine gel treatment experiencedsignificantly less pain with tenaculum placement than those who received placebo gel (32 mm vs 56 mm; P = .02), and they were substantially less likely to require cervical dilation (3.3% vs 34.5%; P = .002), an often painful procedure.
Related article:
Does the injection of ketorolac prior to IUD placement reduce pain?
Patient acceptability and satisfaction. Five minutes after the IUD placement procedure, approximately two-thirds of women in both groups indicated that they experienced an acceptable level of discomfort, and more than three-quarters indicated that they were satisfied with the placement procedure. Fully 67% of the lidocaine group and 68% of the placebo group indicated definitely or probably yes when asked if the level of discomfort they experienced was acceptable, with 27% and 21%, respectively, responding as neutral. When asked if getting the IUD was worth the level of discomfort experienced, 73% of the lidocaine group and 82% of the placebo group responded “yes,” while 23% and 18%, respectively, were unsure.
Pearls for practice
As this study showed, self-administered lidocaine vaginal gel did not alter the primary outcome (pain with IUD placement), but the reduced need for cervical dilation is a promising finding and warrants additional study.
Tip. Interestingly, the placebo-treated women experienced pain intensity with cervical tenaculum placement similar to that associated with IUD placement. This finding illuminates the fact that IUD placement is not the only action that can produce pain. For this reason, I use a finer, single-tooth tenaculum designed for use with sonohysterograms (Goldstein Grasp Cervical Stabilizer).2 This instrument appears to cause less pain and bleeding than conventional tenacula.
Related article:
How to identify and localize IUDs on ultrasound
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Rapkin RB, Achilles SL, Schwarz B, et al. Self-administered lidocaine gel for intrauterine device insertion in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2016;128(3):621–628.
- Goldstein Grasp Cervical Stabilzer. CooperSurgical, Inc. website. http://www.coopersurgical.com/Products/Detail/Goldstein-Grasp-Cervical-Stabilizer. Accessed November 16, 2016.
Fear of potential pain caused by insertion of an intrauterine device (IUD) prevents some women from using this highly effective and safe contraceptive method. Recently, investigators conducted a randomized, placebo-controlled trial to assess whether vaginal lidocaine gel administered shortly before IUD placement was associated with a decrease from baseline in patient-reported pain scores.1
In this blinded trial, Rapkinand colleagues randomly assigned nulliparous women presenting for IUD placement (either the copper T380A IUD or the 52-mg levonorgestrel-releasing IUD) at faculty and resident clinics at a US urban academic center to place 4 mL of 2% lidocaine gel or placebo gel vaginally (using an applicator) 5 to 15 minutes prior to IUD placement.1 A 100-mm visual analog scale (VAS) was used to assess pain at each step of the procedure, including at baseline (before speculum insertion), after speculum placement, tenaculum placement, uterine sound, IUD insertion, and 5 minutes after speculum removal.
Among the 58 evaluable participants, the mean age was 23 years in the lidocaine group and 24 years in the placebo group; more than 80% of the women were white.
The study’s primary outcome was change in pain experience from baseline to IUD insertion. Pain was measured on a VAS from 0 mm (no pain) to 100 mm (worst pain in my life). Secondary outcomes included patient acceptability of gel self-insertion, physician-reported ease of IUD insertion, and need for pain medication for up to 7 days after IUD insertion.
Related article:
Liletta gets a new inserter: Steps for successful placement
What the investigators found
The mean change in pain scores with IUD placement was 61 mm for the lidocaine group and 69 mm for the placebo group (P = .06). Thus, no difference in the primary outcome was found between the 2 groups. However, women who received the lidocaine gel treatment experiencedsignificantly less pain with tenaculum placement than those who received placebo gel (32 mm vs 56 mm; P = .02), and they were substantially less likely to require cervical dilation (3.3% vs 34.5%; P = .002), an often painful procedure.
Related article:
Does the injection of ketorolac prior to IUD placement reduce pain?
Patient acceptability and satisfaction. Five minutes after the IUD placement procedure, approximately two-thirds of women in both groups indicated that they experienced an acceptable level of discomfort, and more than three-quarters indicated that they were satisfied with the placement procedure. Fully 67% of the lidocaine group and 68% of the placebo group indicated definitely or probably yes when asked if the level of discomfort they experienced was acceptable, with 27% and 21%, respectively, responding as neutral. When asked if getting the IUD was worth the level of discomfort experienced, 73% of the lidocaine group and 82% of the placebo group responded “yes,” while 23% and 18%, respectively, were unsure.
Pearls for practice
As this study showed, self-administered lidocaine vaginal gel did not alter the primary outcome (pain with IUD placement), but the reduced need for cervical dilation is a promising finding and warrants additional study.
Tip. Interestingly, the placebo-treated women experienced pain intensity with cervical tenaculum placement similar to that associated with IUD placement. This finding illuminates the fact that IUD placement is not the only action that can produce pain. For this reason, I use a finer, single-tooth tenaculum designed for use with sonohysterograms (Goldstein Grasp Cervical Stabilizer).2 This instrument appears to cause less pain and bleeding than conventional tenacula.
Related article:
How to identify and localize IUDs on ultrasound
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Fear of potential pain caused by insertion of an intrauterine device (IUD) prevents some women from using this highly effective and safe contraceptive method. Recently, investigators conducted a randomized, placebo-controlled trial to assess whether vaginal lidocaine gel administered shortly before IUD placement was associated with a decrease from baseline in patient-reported pain scores.1
In this blinded trial, Rapkinand colleagues randomly assigned nulliparous women presenting for IUD placement (either the copper T380A IUD or the 52-mg levonorgestrel-releasing IUD) at faculty and resident clinics at a US urban academic center to place 4 mL of 2% lidocaine gel or placebo gel vaginally (using an applicator) 5 to 15 minutes prior to IUD placement.1 A 100-mm visual analog scale (VAS) was used to assess pain at each step of the procedure, including at baseline (before speculum insertion), after speculum placement, tenaculum placement, uterine sound, IUD insertion, and 5 minutes after speculum removal.
Among the 58 evaluable participants, the mean age was 23 years in the lidocaine group and 24 years in the placebo group; more than 80% of the women were white.
The study’s primary outcome was change in pain experience from baseline to IUD insertion. Pain was measured on a VAS from 0 mm (no pain) to 100 mm (worst pain in my life). Secondary outcomes included patient acceptability of gel self-insertion, physician-reported ease of IUD insertion, and need for pain medication for up to 7 days after IUD insertion.
Related article:
Liletta gets a new inserter: Steps for successful placement
What the investigators found
The mean change in pain scores with IUD placement was 61 mm for the lidocaine group and 69 mm for the placebo group (P = .06). Thus, no difference in the primary outcome was found between the 2 groups. However, women who received the lidocaine gel treatment experiencedsignificantly less pain with tenaculum placement than those who received placebo gel (32 mm vs 56 mm; P = .02), and they were substantially less likely to require cervical dilation (3.3% vs 34.5%; P = .002), an often painful procedure.
Related article:
Does the injection of ketorolac prior to IUD placement reduce pain?
Patient acceptability and satisfaction. Five minutes after the IUD placement procedure, approximately two-thirds of women in both groups indicated that they experienced an acceptable level of discomfort, and more than three-quarters indicated that they were satisfied with the placement procedure. Fully 67% of the lidocaine group and 68% of the placebo group indicated definitely or probably yes when asked if the level of discomfort they experienced was acceptable, with 27% and 21%, respectively, responding as neutral. When asked if getting the IUD was worth the level of discomfort experienced, 73% of the lidocaine group and 82% of the placebo group responded “yes,” while 23% and 18%, respectively, were unsure.
Pearls for practice
As this study showed, self-administered lidocaine vaginal gel did not alter the primary outcome (pain with IUD placement), but the reduced need for cervical dilation is a promising finding and warrants additional study.
Tip. Interestingly, the placebo-treated women experienced pain intensity with cervical tenaculum placement similar to that associated with IUD placement. This finding illuminates the fact that IUD placement is not the only action that can produce pain. For this reason, I use a finer, single-tooth tenaculum designed for use with sonohysterograms (Goldstein Grasp Cervical Stabilizer).2 This instrument appears to cause less pain and bleeding than conventional tenacula.
Related article:
How to identify and localize IUDs on ultrasound
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Rapkin RB, Achilles SL, Schwarz B, et al. Self-administered lidocaine gel for intrauterine device insertion in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2016;128(3):621–628.
- Goldstein Grasp Cervical Stabilzer. CooperSurgical, Inc. website. http://www.coopersurgical.com/Products/Detail/Goldstein-Grasp-Cervical-Stabilizer. Accessed November 16, 2016.
- Rapkin RB, Achilles SL, Schwarz B, et al. Self-administered lidocaine gel for intrauterine device insertion in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2016;128(3):621–628.
- Goldstein Grasp Cervical Stabilzer. CooperSurgical, Inc. website. http://www.coopersurgical.com/Products/Detail/Goldstein-Grasp-Cervical-Stabilizer. Accessed November 16, 2016.
In this article
What are the modern cardiovascular risk indicators and how should ObGyns be using them in their practice?
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
- Visit NAMS
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
- Visit NAMS
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
- Visit NAMS
Top 3 things I learned at the NAMS 2016 annual meeting
- Visit NAMS
- Visit NAMS
- Visit NAMS
Liletta gets a new inserter: Steps for successful placement
A new single-handed inserter (SHI) for placement of Liletta has been introduced and is currently available (FIGURE 1). Liletta is a levonorgestrel 52-mg intrauterine system (IUS) that is currently approved for 3 years of use as a contraceptive in the United States. The same product in Europe, known as Levosert, is approved for both contraception and the treatment of heavy menstrual bleeding. Liletta, as a branded contraceptive, is being studied through a large Phase 3 clinical trial called ACCESS IUS, which will continue to evaluate the contraceptive efficacy of Liletta for at least 7 years of use.1 A recent publication from the study showed that the levonorgestrel release rates from Liletta are almost identical to the rates reported for the other levonorgestrel 52-mg IUS on the market (Mirena) through 5 years and supports the continued study of the IUS for at least 7 years.2
Related article:
Benefit of self-administered vaginal lidocaine gel in IUD placement
The initial marketing and distribution of Liletta used a two-handed inserter that allowed for successful placement but required multiple steps. The SHI will make loading and placement of Liletta easier for all clinicians. Features of the new SHI include:
- A double-slider mechanism in which the first slider moves into the second slider during IUS placement, providing a tactile sense for the user during the insertion process
- The ability to reload the inserter if needed before placement
- A firm but bendable tube (that is 2 cm longer than other IUS inserters on the market). This length can be helpful for obese patients or postprocedure placements.
- Depth markings to 12 cm on both sides of the insertion tube.
Related article:
2016 Update on contraception
Liletta is an important and unique product in the US market. For most public sector providers and clinics, Liletta costs only $50, significantly less than other long-acting reversible contraceptives. The price of the IUS is only one aspect of its overall cost, however, as women still need to pay for any office visit or insertion fees. Liletta is unique in its pricing. Sales of Liletta in the private sector support the low price in the public sector. As a health care community, even if we do not directly care for women in public-sector settings, we all can help poor women access affordable, effective contraception. For providers, Liletta is a highly effective and lower-cost alternative to currently available hormonal IUS products.
How to insert Liletta
Insertion can be performed using a no-touch technique. The loading and placement technique outlined below should occur after speculum and tenaculum placement, sounding of the uterus, and vaginal preparation as would be performed for any intrauterine contraceptive insertion. Never force the uterine sound or insertion tube through the cervix; if necessary, stop and dilate the cervical canal. The steps below are the main points for successful Liletta placement; see the full product label for more details.3
Related article:
In which clinical situations can the use of the 52-mg levonorgestrel-releasing IUD (Mirena) and the TCu380A copper-IUD (ParaGard) be extended?
The key steps to remember are firm-gentle-firm
- Load the device. While pushing forward firmly on the blue slider (with the number 1), load Liletta by pulling down evenly on the threads. The IUS should be laid on a flat surface in the sterile tray to keep the arms parallel to the floor while pulling on the threads. Once loaded, the threads can be pulled up or down to be locked in the cleft. The tip of the IUS will form a hemispheric dome at the top of the insertion tube.
- Adjust the flange to the measured uterine depth based on sounding using the notch in the tray.
- Place inserter into the cervix. Apply gentle traction on the tenaculum to align the cervical canal and uterine cavity. While still holding firm forward pressure on the blue slider, place the tube through the cervical canal until the flange is approximately 1.5 to 2 cm from the cervix. (FIGURE 2.) Gently slide the blue slider downward until it is flush with the green slider (with the number 2; FIGURE 3). This step will allow the IUS arms to open in the lower uterine segment; wait 10 to 15 seconds for the arms to fully unfold. By sliding gently, you will feel when to stop moving the slider.
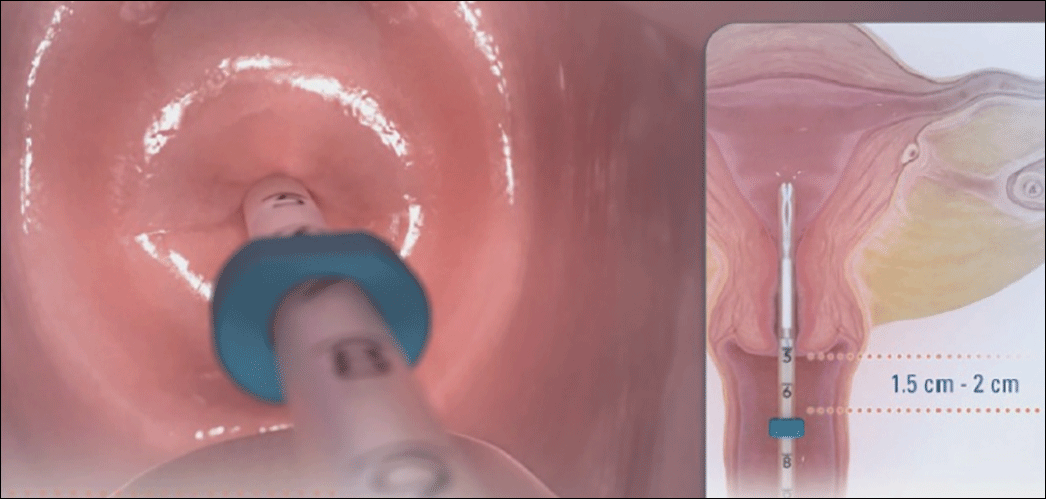 Image copyright Medicines360.
Image copyright Medicines360.Figure 2. Placing the inserter through the cervix 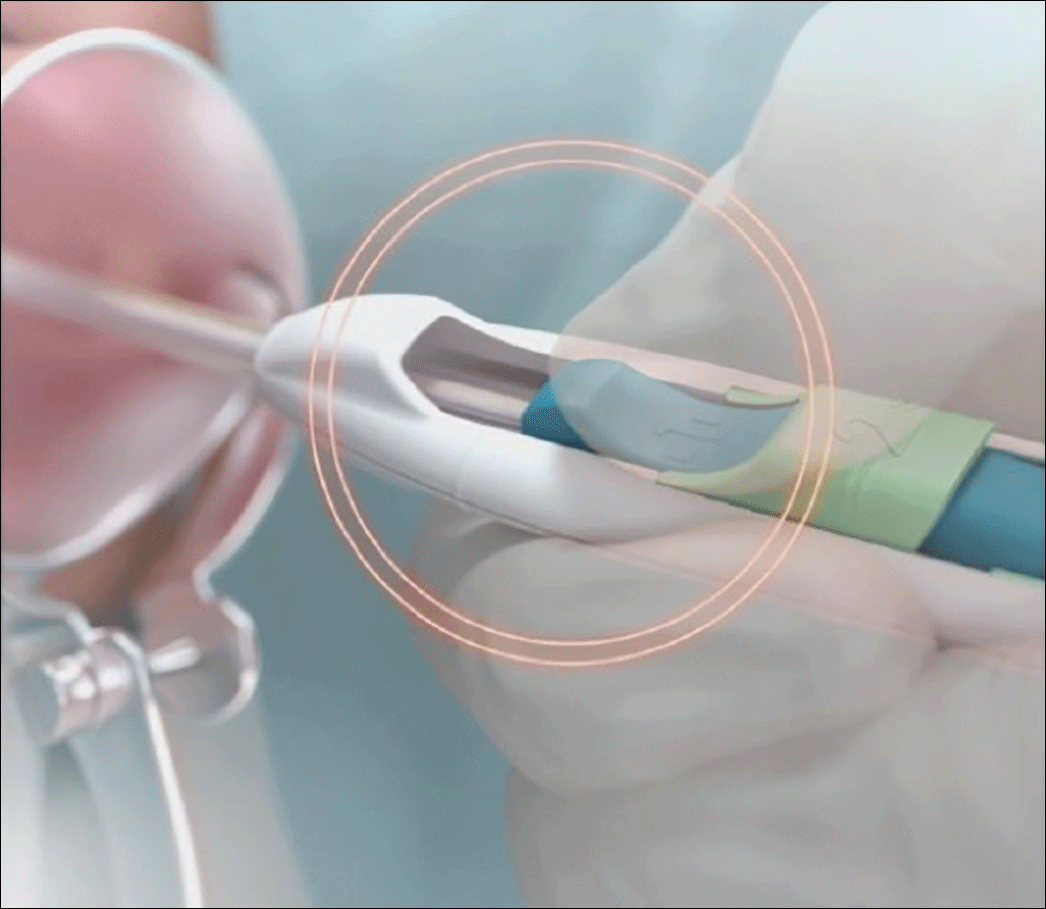 Image copyright Medicines360.
Image copyright Medicines360.Figure 3. Merging the blue and green sliders together to release the IUS arms - Advance the inserter. While holding traction on the tenaculum, advance the inserter to the fundus. You will feel slight resistance when the IUS is at the fundus and the flange should be flush against the cervix.
- Firmly slide both sliders together downward until a click is heard (FIGURE 4). A green indicator will be visible at the bottom of the handle to show that the threads have been ejected from the cleft.
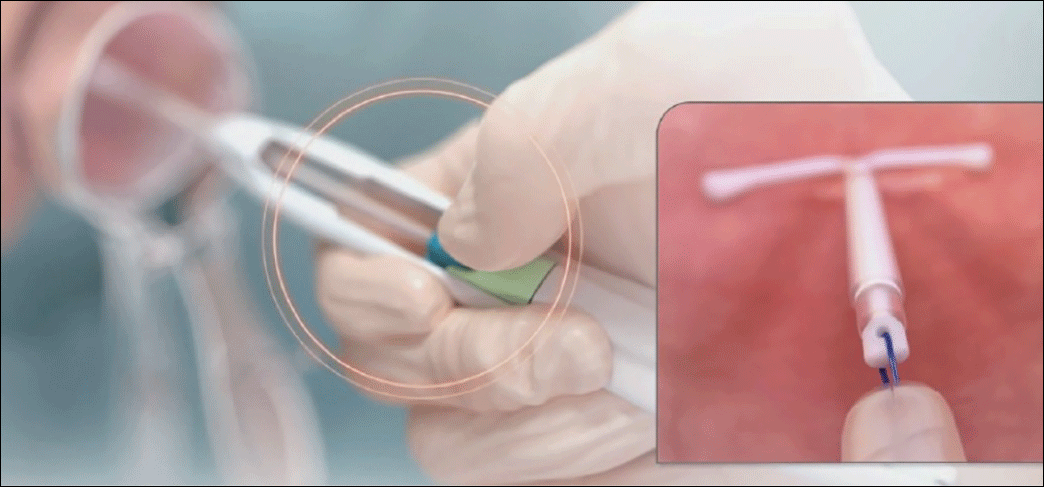 Image copyright Medicines360.
Image copyright Medicines360.Figure 4. Moving the blue and green sliders downward together to release the IUS - Withdraw the inserter from the uterus and cut the threads with blunt tipped scissors approximately 3 cm from the cervical os.
Technique video
Allergan and Medicines360 offer a video demonstrating proper Liletta insertion technique at www.lilettahcp.com. The video includes proper loading of the inserter as well as correct uterine depth measurement and release of Liletta from the inserter. Clinicians are reminded to use aseptic technique during the entire insertion procedure.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Eisenberg DL, Schreiber CA, Turok DK, Teal SB, Westhoff CL, Creinin MD. Three year efficacy and safety of a new 52-mg levonorgestrel-releasing intrauterine system. Contraception. 2015;92(1):10-16.
- Creinin MD, Jansen R, Starr R, Gobburu J, Gopalakrishnan M, Olariu A. Levonorgestrel release rates over 5 years with the Liletta® 52 mg intrauterine system. Contraception. 2016;94(4):353-356.
- Liletta [package insert]. Irvine, California: Allergan USA, Inc., and San Francisco, California: Medicines360; 2016.
A new single-handed inserter (SHI) for placement of Liletta has been introduced and is currently available (FIGURE 1). Liletta is a levonorgestrel 52-mg intrauterine system (IUS) that is currently approved for 3 years of use as a contraceptive in the United States. The same product in Europe, known as Levosert, is approved for both contraception and the treatment of heavy menstrual bleeding. Liletta, as a branded contraceptive, is being studied through a large Phase 3 clinical trial called ACCESS IUS, which will continue to evaluate the contraceptive efficacy of Liletta for at least 7 years of use.1 A recent publication from the study showed that the levonorgestrel release rates from Liletta are almost identical to the rates reported for the other levonorgestrel 52-mg IUS on the market (Mirena) through 5 years and supports the continued study of the IUS for at least 7 years.2
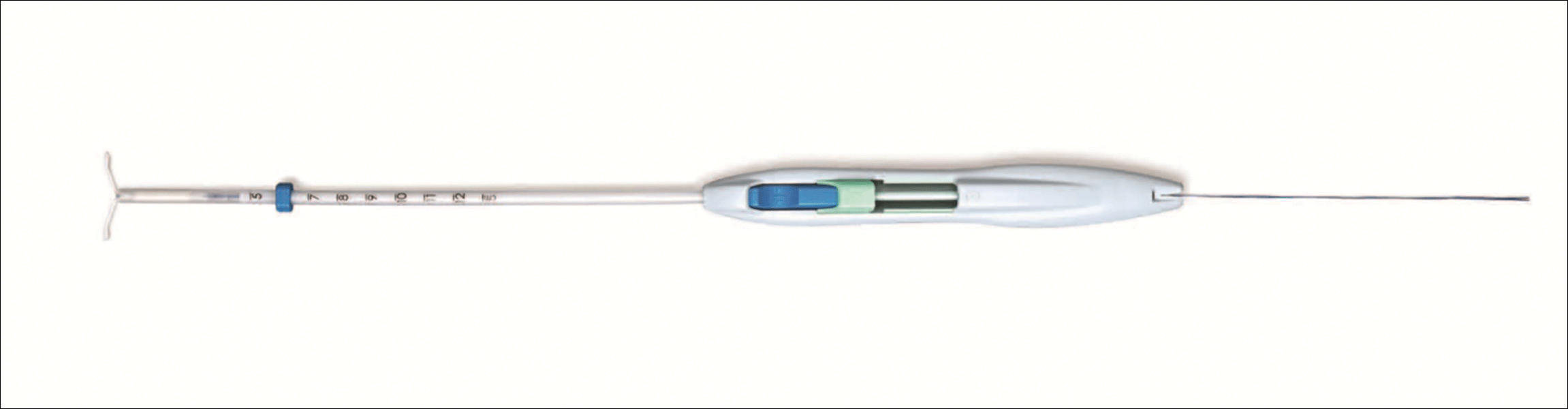
Related article:
Benefit of self-administered vaginal lidocaine gel in IUD placement
The initial marketing and distribution of Liletta used a two-handed inserter that allowed for successful placement but required multiple steps. The SHI will make loading and placement of Liletta easier for all clinicians. Features of the new SHI include:
- A double-slider mechanism in which the first slider moves into the second slider during IUS placement, providing a tactile sense for the user during the insertion process
- The ability to reload the inserter if needed before placement
- A firm but bendable tube (that is 2 cm longer than other IUS inserters on the market). This length can be helpful for obese patients or postprocedure placements.
- Depth markings to 12 cm on both sides of the insertion tube.
Related article:
2016 Update on contraception
Liletta is an important and unique product in the US market. For most public sector providers and clinics, Liletta costs only $50, significantly less than other long-acting reversible contraceptives. The price of the IUS is only one aspect of its overall cost, however, as women still need to pay for any office visit or insertion fees. Liletta is unique in its pricing. Sales of Liletta in the private sector support the low price in the public sector. As a health care community, even if we do not directly care for women in public-sector settings, we all can help poor women access affordable, effective contraception. For providers, Liletta is a highly effective and lower-cost alternative to currently available hormonal IUS products.
How to insert Liletta
Insertion can be performed using a no-touch technique. The loading and placement technique outlined below should occur after speculum and tenaculum placement, sounding of the uterus, and vaginal preparation as would be performed for any intrauterine contraceptive insertion. Never force the uterine sound or insertion tube through the cervix; if necessary, stop and dilate the cervical canal. The steps below are the main points for successful Liletta placement; see the full product label for more details.3
Related article:
In which clinical situations can the use of the 52-mg levonorgestrel-releasing IUD (Mirena) and the TCu380A copper-IUD (ParaGard) be extended?
The key steps to remember are firm-gentle-firm
- Load the device. While pushing forward firmly on the blue slider (with the number 1), load Liletta by pulling down evenly on the threads. The IUS should be laid on a flat surface in the sterile tray to keep the arms parallel to the floor while pulling on the threads. Once loaded, the threads can be pulled up or down to be locked in the cleft. The tip of the IUS will form a hemispheric dome at the top of the insertion tube.
- Adjust the flange to the measured uterine depth based on sounding using the notch in the tray.
- Place inserter into the cervix. Apply gentle traction on the tenaculum to align the cervical canal and uterine cavity. While still holding firm forward pressure on the blue slider, place the tube through the cervical canal until the flange is approximately 1.5 to 2 cm from the cervix. (FIGURE 2.) Gently slide the blue slider downward until it is flush with the green slider (with the number 2; FIGURE 3). This step will allow the IUS arms to open in the lower uterine segment; wait 10 to 15 seconds for the arms to fully unfold. By sliding gently, you will feel when to stop moving the slider.
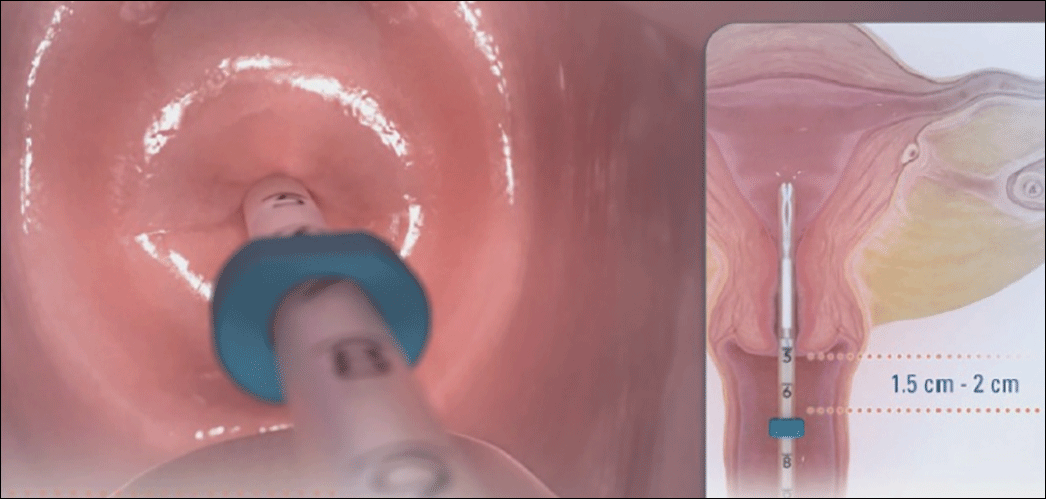 Image copyright Medicines360.
Image copyright Medicines360.Figure 2. Placing the inserter through the cervix 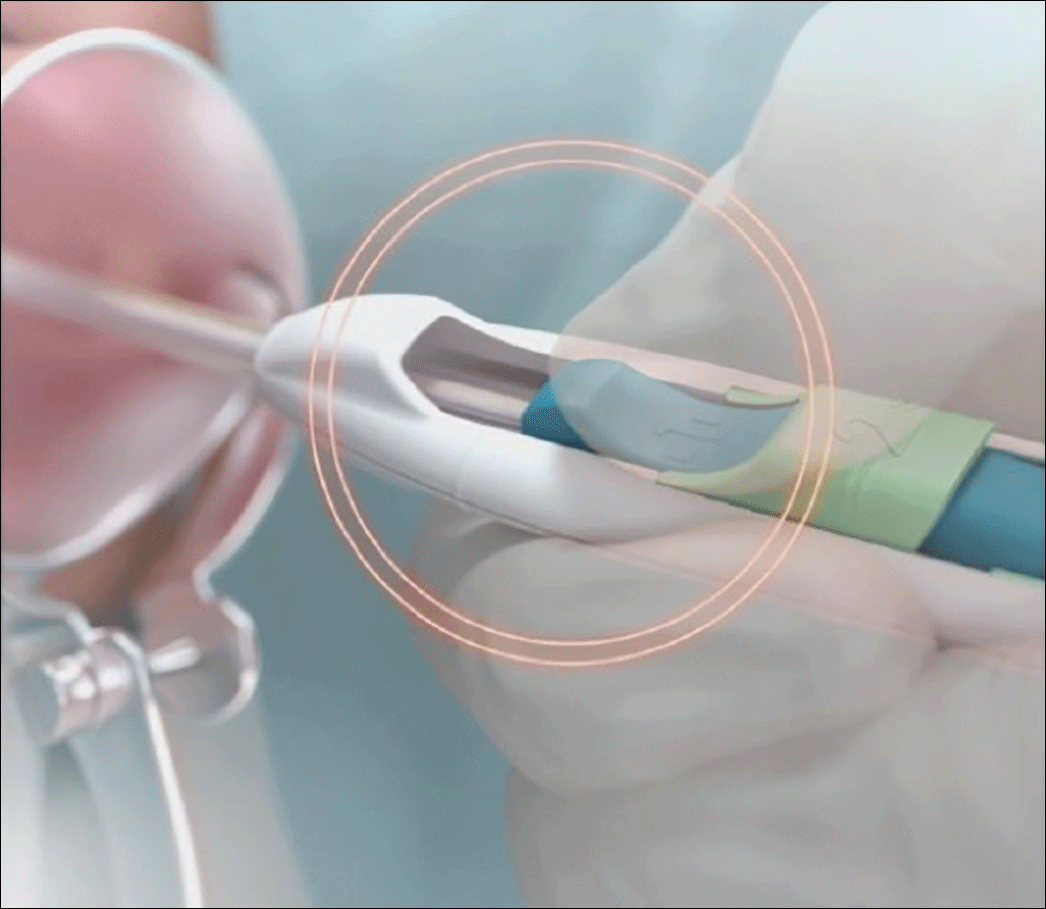 Image copyright Medicines360.
Image copyright Medicines360.Figure 3. Merging the blue and green sliders together to release the IUS arms - Advance the inserter. While holding traction on the tenaculum, advance the inserter to the fundus. You will feel slight resistance when the IUS is at the fundus and the flange should be flush against the cervix.
- Firmly slide both sliders together downward until a click is heard (FIGURE 4). A green indicator will be visible at the bottom of the handle to show that the threads have been ejected from the cleft.
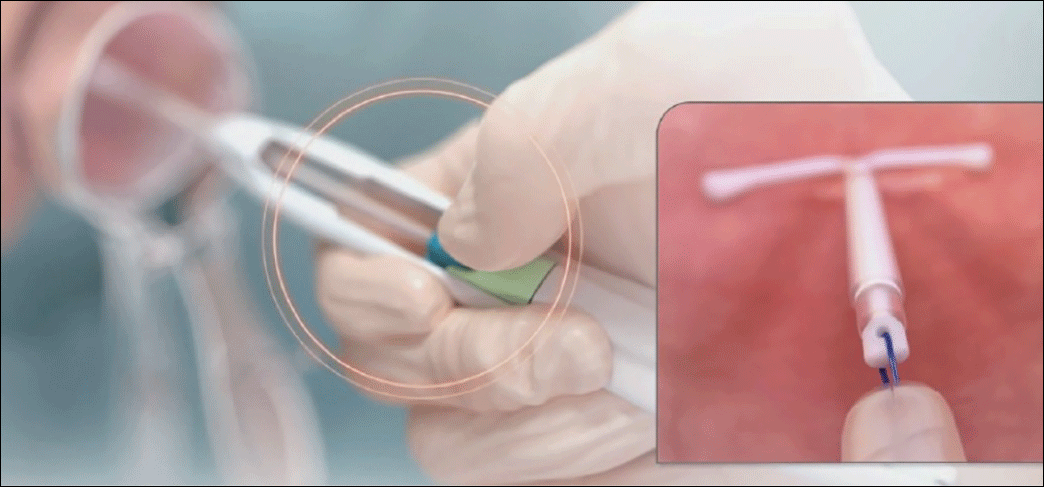 Image copyright Medicines360.
Image copyright Medicines360.Figure 4. Moving the blue and green sliders downward together to release the IUS - Withdraw the inserter from the uterus and cut the threads with blunt tipped scissors approximately 3 cm from the cervical os.
Technique video
Allergan and Medicines360 offer a video demonstrating proper Liletta insertion technique at www.lilettahcp.com. The video includes proper loading of the inserter as well as correct uterine depth measurement and release of Liletta from the inserter. Clinicians are reminded to use aseptic technique during the entire insertion procedure.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
A new single-handed inserter (SHI) for placement of Liletta has been introduced and is currently available (FIGURE 1). Liletta is a levonorgestrel 52-mg intrauterine system (IUS) that is currently approved for 3 years of use as a contraceptive in the United States. The same product in Europe, known as Levosert, is approved for both contraception and the treatment of heavy menstrual bleeding. Liletta, as a branded contraceptive, is being studied through a large Phase 3 clinical trial called ACCESS IUS, which will continue to evaluate the contraceptive efficacy of Liletta for at least 7 years of use.1 A recent publication from the study showed that the levonorgestrel release rates from Liletta are almost identical to the rates reported for the other levonorgestrel 52-mg IUS on the market (Mirena) through 5 years and supports the continued study of the IUS for at least 7 years.2
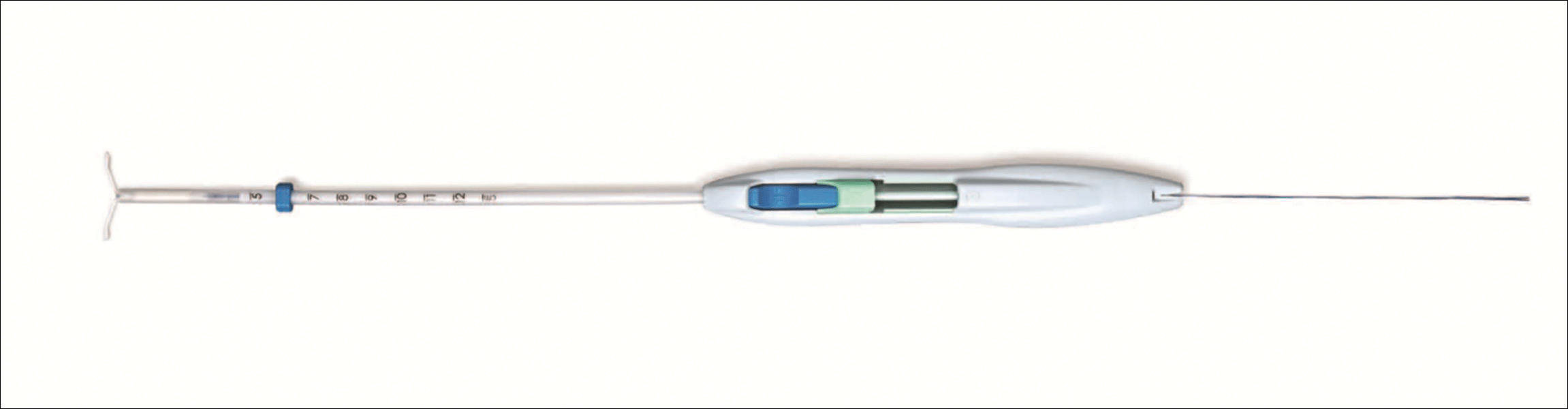
Related article:
Benefit of self-administered vaginal lidocaine gel in IUD placement
The initial marketing and distribution of Liletta used a two-handed inserter that allowed for successful placement but required multiple steps. The SHI will make loading and placement of Liletta easier for all clinicians. Features of the new SHI include:
- A double-slider mechanism in which the first slider moves into the second slider during IUS placement, providing a tactile sense for the user during the insertion process
- The ability to reload the inserter if needed before placement
- A firm but bendable tube (that is 2 cm longer than other IUS inserters on the market). This length can be helpful for obese patients or postprocedure placements.
- Depth markings to 12 cm on both sides of the insertion tube.
Related article:
2016 Update on contraception
Liletta is an important and unique product in the US market. For most public sector providers and clinics, Liletta costs only $50, significantly less than other long-acting reversible contraceptives. The price of the IUS is only one aspect of its overall cost, however, as women still need to pay for any office visit or insertion fees. Liletta is unique in its pricing. Sales of Liletta in the private sector support the low price in the public sector. As a health care community, even if we do not directly care for women in public-sector settings, we all can help poor women access affordable, effective contraception. For providers, Liletta is a highly effective and lower-cost alternative to currently available hormonal IUS products.
How to insert Liletta
Insertion can be performed using a no-touch technique. The loading and placement technique outlined below should occur after speculum and tenaculum placement, sounding of the uterus, and vaginal preparation as would be performed for any intrauterine contraceptive insertion. Never force the uterine sound or insertion tube through the cervix; if necessary, stop and dilate the cervical canal. The steps below are the main points for successful Liletta placement; see the full product label for more details.3
Related article:
In which clinical situations can the use of the 52-mg levonorgestrel-releasing IUD (Mirena) and the TCu380A copper-IUD (ParaGard) be extended?
The key steps to remember are firm-gentle-firm
- Load the device. While pushing forward firmly on the blue slider (with the number 1), load Liletta by pulling down evenly on the threads. The IUS should be laid on a flat surface in the sterile tray to keep the arms parallel to the floor while pulling on the threads. Once loaded, the threads can be pulled up or down to be locked in the cleft. The tip of the IUS will form a hemispheric dome at the top of the insertion tube.
- Adjust the flange to the measured uterine depth based on sounding using the notch in the tray.
- Place inserter into the cervix. Apply gentle traction on the tenaculum to align the cervical canal and uterine cavity. While still holding firm forward pressure on the blue slider, place the tube through the cervical canal until the flange is approximately 1.5 to 2 cm from the cervix. (FIGURE 2.) Gently slide the blue slider downward until it is flush with the green slider (with the number 2; FIGURE 3). This step will allow the IUS arms to open in the lower uterine segment; wait 10 to 15 seconds for the arms to fully unfold. By sliding gently, you will feel when to stop moving the slider.
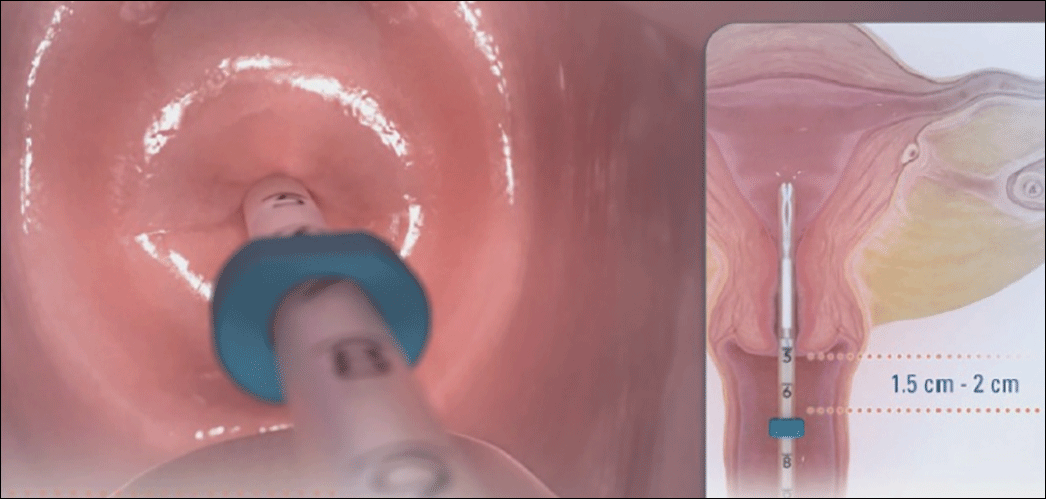 Image copyright Medicines360.
Image copyright Medicines360.Figure 2. Placing the inserter through the cervix 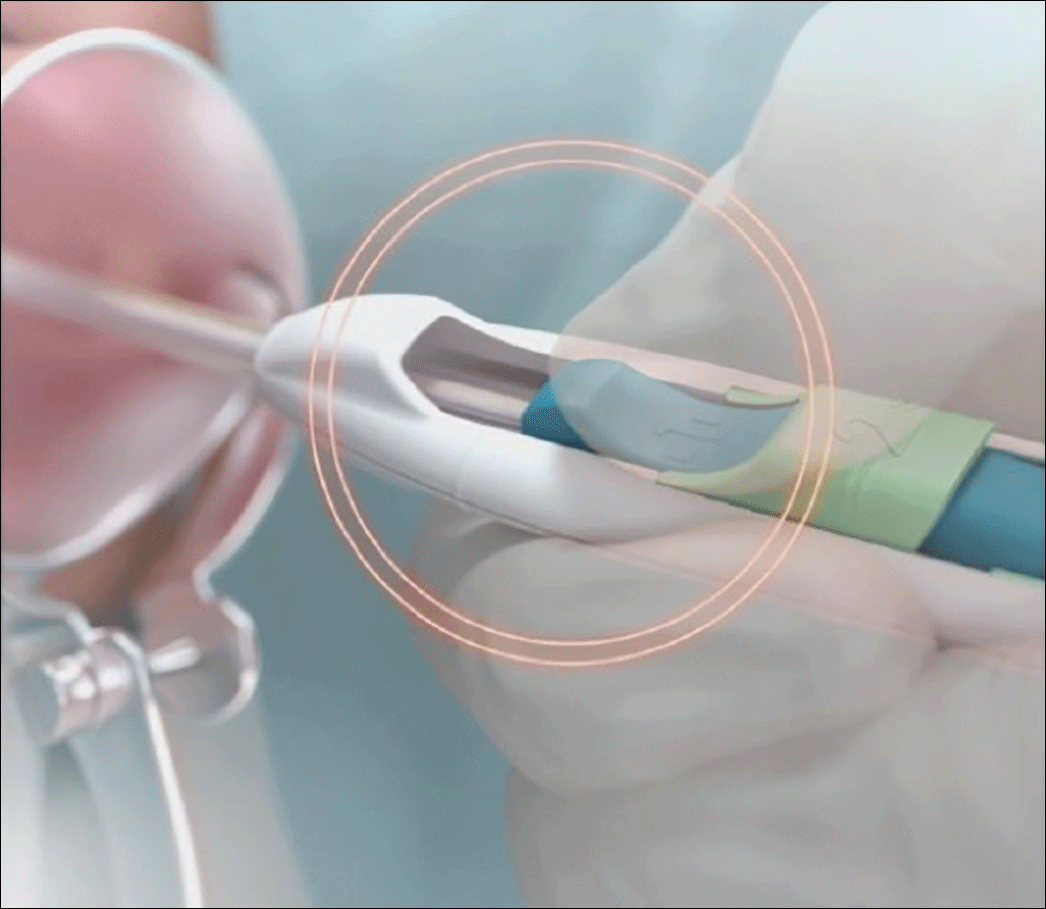 Image copyright Medicines360.
Image copyright Medicines360.Figure 3. Merging the blue and green sliders together to release the IUS arms - Advance the inserter. While holding traction on the tenaculum, advance the inserter to the fundus. You will feel slight resistance when the IUS is at the fundus and the flange should be flush against the cervix.
- Firmly slide both sliders together downward until a click is heard (FIGURE 4). A green indicator will be visible at the bottom of the handle to show that the threads have been ejected from the cleft.
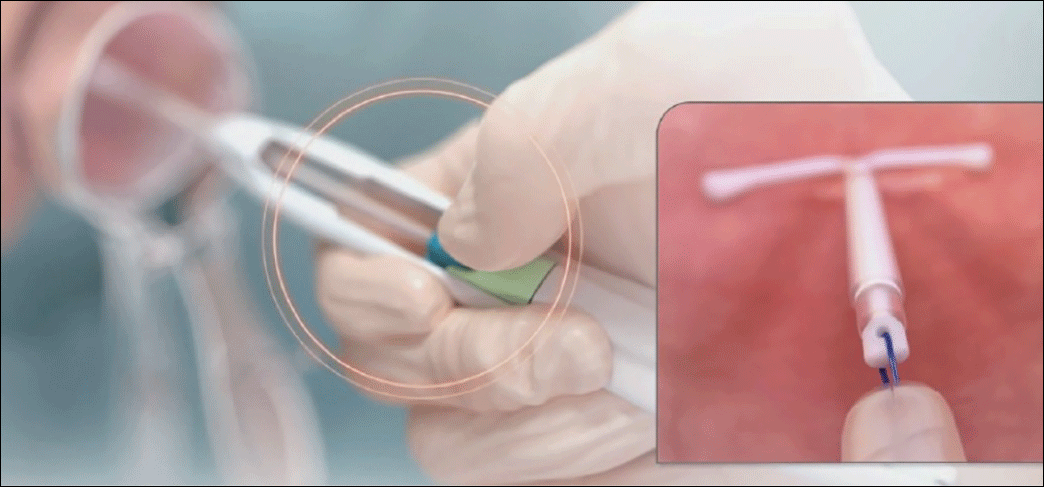 Image copyright Medicines360.
Image copyright Medicines360.Figure 4. Moving the blue and green sliders downward together to release the IUS - Withdraw the inserter from the uterus and cut the threads with blunt tipped scissors approximately 3 cm from the cervical os.
Technique video
Allergan and Medicines360 offer a video demonstrating proper Liletta insertion technique at www.lilettahcp.com. The video includes proper loading of the inserter as well as correct uterine depth measurement and release of Liletta from the inserter. Clinicians are reminded to use aseptic technique during the entire insertion procedure.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Eisenberg DL, Schreiber CA, Turok DK, Teal SB, Westhoff CL, Creinin MD. Three year efficacy and safety of a new 52-mg levonorgestrel-releasing intrauterine system. Contraception. 2015;92(1):10-16.
- Creinin MD, Jansen R, Starr R, Gobburu J, Gopalakrishnan M, Olariu A. Levonorgestrel release rates over 5 years with the Liletta® 52 mg intrauterine system. Contraception. 2016;94(4):353-356.
- Liletta [package insert]. Irvine, California: Allergan USA, Inc., and San Francisco, California: Medicines360; 2016.
- Eisenberg DL, Schreiber CA, Turok DK, Teal SB, Westhoff CL, Creinin MD. Three year efficacy and safety of a new 52-mg levonorgestrel-releasing intrauterine system. Contraception. 2015;92(1):10-16.
- Creinin MD, Jansen R, Starr R, Gobburu J, Gopalakrishnan M, Olariu A. Levonorgestrel release rates over 5 years with the Liletta® 52 mg intrauterine system. Contraception. 2016;94(4):353-356.
- Liletta [package insert]. Irvine, California: Allergan USA, Inc., and San Francisco, California: Medicines360; 2016.
In this article