User login
Many Commission on Care Recommendations Receive Support
Even with the clock ticking on the current election year, President Barak Obama and Congress appear ready to begin implementing at least some of the Commission on Care recommendations. In Senate and House of Representatives committee meetings over the past 2 weeks, a consensus has emerged to implement most of the Commission’s 18 recommendations. Still, most action is expected to take place after the November election, which will change who is in the White House and also could affect leadership within the VA as well as the House and Senate veteran oversight committees.
Currently 22% of veteran appointments are in community settings and the VA has already seen 5 million appointments through the Veterans Choice Program. Still, as VA Secretary Robert A. McDonald told the Senate committee on Wednesday, just 5,000 veterans are using community care only, which McDonald argued was evidence of veterans' strong desire to continue receiving VA care. The Veterans Choice Program is currently scheduled to expire August 7, 2017.
“I strongly support the Commission's principle that creating a high-performing, integrated health care system that encompasses both VA and private care is critical to serving the needs of veterans,” President Obama said in a letter to the House Committee on Veterans Affairs. “It is critical that we preserve and continue to improve the VA health care system and ensure that VA has the ability to serve veterans.” The President also emphasized the importance of preserving the high quality of VA care, noting, “VA also provides unique, highly specialized care for many medical conditions, such as spinal cord and traumatic brain injuries, which are simply not available to the same extent outside of VA.”
“In our view that VHA must change, and change profoundly, because veterans deserve a better organized, high-performing health care system,” Nancy Schlichting, Commission on Care chairperson told the House committee. “Certainly, some elements of such a high-performing system are already in place. VA has high-quality clinical staff, and this integrated health care system is marked by good care-coordination. VHA today, however, relies significantly on community providers to augment the care it provides directly, although those community partners are not part of a cohesive system.”
According to Schlichting, fixing access issues “cannot be achieved by ‘tweaking’ existing programs or mounting a complex new delivery framework on a weak infrastructure platform.” Instead, the Commission recommended the creation of integrated systems approach to the VA that would re-engineer VA’s fundamental internal systems, both in terms of how it delivers health care as well as the technology it uses.
Veteran service organizations weighed in with cautious approval of many of the Commission’s recommendations, especially those that improved oversight, governance, and access to care, but cautioned against privatizing the VA.
“After two years of spirited and passionate debate about the future of veterans health care, we envision a clear path forward that builds on the strengths of the existing VA system, while expanding access by seamlessly integrating the best of community care to ensure no veteran must travel too far or wait too long for care,” Joy J. Ilem, national legislative director of Disabled American Veterans wrote in a letter submitted to the House committee. “Congress and VA must now begin the steps to finalize plans and move forward with the evolution of veterans health care.”
Despite the emerging consensus, a number of voices expressed concern about the impact of the Commission on Care’s proposals changes. A group of unions and professional organizations that represent VA employees (Association of VA Psychologist Leaders, Association of VA Social Workers, Nurses Organization of Veterans Affairs, Veterans Affairs Physician Assistant Association, American Federation of Government Employees, National Federation of Federal Employees, National Association of Government Employees, National Nurses United, the American Psychological Association, and National Association of Social Workers) expressed its concerns in a letter submitted to the House panel. “As organizations comprised of and representing health care practitioners, researchers, educators, administrators and personnel devoted to serving veterans, we have serious reservations about the report’s major recommendation to replace the current VHA with a new entity, to be known as the VHA Care System.” The letter argues that the proposed VHA Care System “disassembles one of the most effective, innovative features of current VHA care—the Primary Care/Mental Health Integration approach.”
In his Senate testimony, Secretary McDonald also expressed concern with the potential cost of some of the Commission on Care proposals. Currently the VA is spending $13.5 billion in community care. According to McDonald, the VA would need $17 billion to make the upgrades it outlined in its October Plan to Consolidate Community Care, but he warned “the Commission on Care plan would be much more expensive than that.” More importantly, McDonald insisted, the VA should retain primary responsibility for the care of veterans. "We believe the VA needs to be the care coordinator," he insisted.
Another concern echoed by many of the commenters was the proposal to create an oversight board to provide governance, set long-term strategy, and direct and oversee reform. According to its critics, the proposal not only would undermine the authority of VA leadership, but could reduce congressional oversight as well. “NOVA strongly opposes giving an outside board—made up of civilian health care executives who may have never set foot into a VA facility—the authority to make decisions about the care and services provided America’s veterans,” argued Sharon Johnson, MSN, RN, president of the Nurses Organization of Veteran Affairs.
Mark Takata (D-Calif.) the ranking minority member of the House committee also expressed concern that the changes could impact VA clinicians’ access to high quality research, and clinician training. “The Commission on Care recommendations might in fact weaken the VA health care system,” Takata argued. “Proposals to funnels funding to private contractors and for profit care will take desperately needed resources away from our veterans and should be immediately rejected.... We cannot view expanded choice or the private sector as the panacea for solving the challenges the VA faces.”
Even with the clock ticking on the current election year, President Barak Obama and Congress appear ready to begin implementing at least some of the Commission on Care recommendations. In Senate and House of Representatives committee meetings over the past 2 weeks, a consensus has emerged to implement most of the Commission’s 18 recommendations. Still, most action is expected to take place after the November election, which will change who is in the White House and also could affect leadership within the VA as well as the House and Senate veteran oversight committees.
Currently 22% of veteran appointments are in community settings and the VA has already seen 5 million appointments through the Veterans Choice Program. Still, as VA Secretary Robert A. McDonald told the Senate committee on Wednesday, just 5,000 veterans are using community care only, which McDonald argued was evidence of veterans' strong desire to continue receiving VA care. The Veterans Choice Program is currently scheduled to expire August 7, 2017.
“I strongly support the Commission's principle that creating a high-performing, integrated health care system that encompasses both VA and private care is critical to serving the needs of veterans,” President Obama said in a letter to the House Committee on Veterans Affairs. “It is critical that we preserve and continue to improve the VA health care system and ensure that VA has the ability to serve veterans.” The President also emphasized the importance of preserving the high quality of VA care, noting, “VA also provides unique, highly specialized care for many medical conditions, such as spinal cord and traumatic brain injuries, which are simply not available to the same extent outside of VA.”
“In our view that VHA must change, and change profoundly, because veterans deserve a better organized, high-performing health care system,” Nancy Schlichting, Commission on Care chairperson told the House committee. “Certainly, some elements of such a high-performing system are already in place. VA has high-quality clinical staff, and this integrated health care system is marked by good care-coordination. VHA today, however, relies significantly on community providers to augment the care it provides directly, although those community partners are not part of a cohesive system.”
According to Schlichting, fixing access issues “cannot be achieved by ‘tweaking’ existing programs or mounting a complex new delivery framework on a weak infrastructure platform.” Instead, the Commission recommended the creation of integrated systems approach to the VA that would re-engineer VA’s fundamental internal systems, both in terms of how it delivers health care as well as the technology it uses.
Veteran service organizations weighed in with cautious approval of many of the Commission’s recommendations, especially those that improved oversight, governance, and access to care, but cautioned against privatizing the VA.
“After two years of spirited and passionate debate about the future of veterans health care, we envision a clear path forward that builds on the strengths of the existing VA system, while expanding access by seamlessly integrating the best of community care to ensure no veteran must travel too far or wait too long for care,” Joy J. Ilem, national legislative director of Disabled American Veterans wrote in a letter submitted to the House committee. “Congress and VA must now begin the steps to finalize plans and move forward with the evolution of veterans health care.”
Despite the emerging consensus, a number of voices expressed concern about the impact of the Commission on Care’s proposals changes. A group of unions and professional organizations that represent VA employees (Association of VA Psychologist Leaders, Association of VA Social Workers, Nurses Organization of Veterans Affairs, Veterans Affairs Physician Assistant Association, American Federation of Government Employees, National Federation of Federal Employees, National Association of Government Employees, National Nurses United, the American Psychological Association, and National Association of Social Workers) expressed its concerns in a letter submitted to the House panel. “As organizations comprised of and representing health care practitioners, researchers, educators, administrators and personnel devoted to serving veterans, we have serious reservations about the report’s major recommendation to replace the current VHA with a new entity, to be known as the VHA Care System.” The letter argues that the proposed VHA Care System “disassembles one of the most effective, innovative features of current VHA care—the Primary Care/Mental Health Integration approach.”
In his Senate testimony, Secretary McDonald also expressed concern with the potential cost of some of the Commission on Care proposals. Currently the VA is spending $13.5 billion in community care. According to McDonald, the VA would need $17 billion to make the upgrades it outlined in its October Plan to Consolidate Community Care, but he warned “the Commission on Care plan would be much more expensive than that.” More importantly, McDonald insisted, the VA should retain primary responsibility for the care of veterans. "We believe the VA needs to be the care coordinator," he insisted.
Another concern echoed by many of the commenters was the proposal to create an oversight board to provide governance, set long-term strategy, and direct and oversee reform. According to its critics, the proposal not only would undermine the authority of VA leadership, but could reduce congressional oversight as well. “NOVA strongly opposes giving an outside board—made up of civilian health care executives who may have never set foot into a VA facility—the authority to make decisions about the care and services provided America’s veterans,” argued Sharon Johnson, MSN, RN, president of the Nurses Organization of Veteran Affairs.
Mark Takata (D-Calif.) the ranking minority member of the House committee also expressed concern that the changes could impact VA clinicians’ access to high quality research, and clinician training. “The Commission on Care recommendations might in fact weaken the VA health care system,” Takata argued. “Proposals to funnels funding to private contractors and for profit care will take desperately needed resources away from our veterans and should be immediately rejected.... We cannot view expanded choice or the private sector as the panacea for solving the challenges the VA faces.”
Even with the clock ticking on the current election year, President Barak Obama and Congress appear ready to begin implementing at least some of the Commission on Care recommendations. In Senate and House of Representatives committee meetings over the past 2 weeks, a consensus has emerged to implement most of the Commission’s 18 recommendations. Still, most action is expected to take place after the November election, which will change who is in the White House and also could affect leadership within the VA as well as the House and Senate veteran oversight committees.
Currently 22% of veteran appointments are in community settings and the VA has already seen 5 million appointments through the Veterans Choice Program. Still, as VA Secretary Robert A. McDonald told the Senate committee on Wednesday, just 5,000 veterans are using community care only, which McDonald argued was evidence of veterans' strong desire to continue receiving VA care. The Veterans Choice Program is currently scheduled to expire August 7, 2017.
“I strongly support the Commission's principle that creating a high-performing, integrated health care system that encompasses both VA and private care is critical to serving the needs of veterans,” President Obama said in a letter to the House Committee on Veterans Affairs. “It is critical that we preserve and continue to improve the VA health care system and ensure that VA has the ability to serve veterans.” The President also emphasized the importance of preserving the high quality of VA care, noting, “VA also provides unique, highly specialized care for many medical conditions, such as spinal cord and traumatic brain injuries, which are simply not available to the same extent outside of VA.”
“In our view that VHA must change, and change profoundly, because veterans deserve a better organized, high-performing health care system,” Nancy Schlichting, Commission on Care chairperson told the House committee. “Certainly, some elements of such a high-performing system are already in place. VA has high-quality clinical staff, and this integrated health care system is marked by good care-coordination. VHA today, however, relies significantly on community providers to augment the care it provides directly, although those community partners are not part of a cohesive system.”
According to Schlichting, fixing access issues “cannot be achieved by ‘tweaking’ existing programs or mounting a complex new delivery framework on a weak infrastructure platform.” Instead, the Commission recommended the creation of integrated systems approach to the VA that would re-engineer VA’s fundamental internal systems, both in terms of how it delivers health care as well as the technology it uses.
Veteran service organizations weighed in with cautious approval of many of the Commission’s recommendations, especially those that improved oversight, governance, and access to care, but cautioned against privatizing the VA.
“After two years of spirited and passionate debate about the future of veterans health care, we envision a clear path forward that builds on the strengths of the existing VA system, while expanding access by seamlessly integrating the best of community care to ensure no veteran must travel too far or wait too long for care,” Joy J. Ilem, national legislative director of Disabled American Veterans wrote in a letter submitted to the House committee. “Congress and VA must now begin the steps to finalize plans and move forward with the evolution of veterans health care.”
Despite the emerging consensus, a number of voices expressed concern about the impact of the Commission on Care’s proposals changes. A group of unions and professional organizations that represent VA employees (Association of VA Psychologist Leaders, Association of VA Social Workers, Nurses Organization of Veterans Affairs, Veterans Affairs Physician Assistant Association, American Federation of Government Employees, National Federation of Federal Employees, National Association of Government Employees, National Nurses United, the American Psychological Association, and National Association of Social Workers) expressed its concerns in a letter submitted to the House panel. “As organizations comprised of and representing health care practitioners, researchers, educators, administrators and personnel devoted to serving veterans, we have serious reservations about the report’s major recommendation to replace the current VHA with a new entity, to be known as the VHA Care System.” The letter argues that the proposed VHA Care System “disassembles one of the most effective, innovative features of current VHA care—the Primary Care/Mental Health Integration approach.”
In his Senate testimony, Secretary McDonald also expressed concern with the potential cost of some of the Commission on Care proposals. Currently the VA is spending $13.5 billion in community care. According to McDonald, the VA would need $17 billion to make the upgrades it outlined in its October Plan to Consolidate Community Care, but he warned “the Commission on Care plan would be much more expensive than that.” More importantly, McDonald insisted, the VA should retain primary responsibility for the care of veterans. "We believe the VA needs to be the care coordinator," he insisted.
Another concern echoed by many of the commenters was the proposal to create an oversight board to provide governance, set long-term strategy, and direct and oversee reform. According to its critics, the proposal not only would undermine the authority of VA leadership, but could reduce congressional oversight as well. “NOVA strongly opposes giving an outside board—made up of civilian health care executives who may have never set foot into a VA facility—the authority to make decisions about the care and services provided America’s veterans,” argued Sharon Johnson, MSN, RN, president of the Nurses Organization of Veteran Affairs.
Mark Takata (D-Calif.) the ranking minority member of the House committee also expressed concern that the changes could impact VA clinicians’ access to high quality research, and clinician training. “The Commission on Care recommendations might in fact weaken the VA health care system,” Takata argued. “Proposals to funnels funding to private contractors and for profit care will take desperately needed resources away from our veterans and should be immediately rejected.... We cannot view expanded choice or the private sector as the panacea for solving the challenges the VA faces.”
Laboring in the Shadow of the Media: Care and Perceptions of Care in the VA
Just over 2 years ago, I finished a psychiatry residency at the Mayo Clinic, turned down an offer to stay on staff, and topped it off by taking a position at the VA. Not one of my brighter moments—or so one of my friends thought. “Are you off your rocker? Don’t you know that the VA is terrible? Why would you go work there?” he jabbed incredulously. I cringed, knowing that I had passed up an opportunity to stay in arguably the best hospital system in the nation, possibly the world, to work at what some (maybe even a lot) view as a corpulent and recalcitrant bastion of ineptitude bound by the dictates of a fickle Congress.
In the wake of the Phoenix wait-time scandal (and no, it’s not like Disneyland), the suicide by self-immolation of Charles Richard Ingram III outside a VA facility in New Jersey, the new data on veteran suicide showing progress but continued significant concern, and the ongoing VA privatization discussion, the prevailing discourse about the VA is largely negative.1,2 And in a high-voltage election cycle where public outrage can serve as an efficient tool to garner support, the VA risks getting pummeled.
Add to this the shocking research that shows nearly half of VA psychiatrists are considering leaving the VA within the next 2 years, and it’s clear that dissatisfaction within and outside the VA is high.3 This does not bode well for veterans at a time when suicide and mental health care needs are so critically important. But while the bureaucracy of the VA is often the focus of negative press, it also filters down and unfortunately has the potential to directly affect VA practitioners and veterans. When we lose sight of what the VA does well, we risk being caught up in a vortex of negativity and a profound sense of inadequacy and helplessness. More attention to what is already being done well can help us as a nation more realistically chart a path forward rather than being fueled by negative rhetoric and rage.
Despite the challenges, the VA is currently succeeding in a number of areas that deserve recognition:
Medical school and resident education and collaboration with VA. In 2014, > 41,000 medical residents and nearly 23,000 medical students had some or all of their training in a VA setting. More than 95% of allopathic medical schools and nearly 90% of osteopathic medical schools had affiliation agreements with the VA in 2014.4 Suffice it to say, if the educational endeavors of the VA were curtailed, there would be an unholy scramble to provide well-trained physicians for our nation. (This does not include the dentists, psychologists, pharmacists, social workers, nurses, and other health care professionals whose training involves the VA in some capacity.) In addition, the VA often provides loan repayment assistance, which is very important given that many young professionals carry substantial school debt after completing training.
Mental health and primary care integration. Medical care overall is changing, and there is an increasing shift away from volume-based, fee-for-service care to integrated, team-based models. The VA is one of several successful leaders at a time when most U.S. health care providers are being scrutinized for their use of health care dollars and overall national health outcomes.5 In addition to primary care integration, the VA uses home-based primary care and mental health intensive case management teams for vulnerable veterans, adding flexibility, continuity, and access for many.
Overall excellent mental health care. A recent study by Watkins and colleagues found that when comparing quality measures for medication evaluation and management for schizophrenia, bipolar disorder, posttraumatic stress disorder, depression, and substance use disorders, “In every case, VA performance was superior to that of the private sector by more than 30%.”6 This is not an aberration and not limited to mental health care. It is a consistent finding about which books have been written.7 However, the availability of evidence-based care may not be consistent across all VA facilities nationally, depending on demand and staffing.
Despite the rumors, VA has high customer satisfaction. According to the American Customer Satisfaction Index, the VA has consistently performed well in measures of customer satisfaction compared with those of the private sector health care providers.8 Let’s not ignore what veterans have actually said and continue to say about their care.
Once in, you’re in! I recently missed an initial appointment with a private sector pediatrician for one of my sons. I was tersely invited to find another doctor. This seemed scandalous since I have become accustomed in my role as a VA physician to reaching out, sometimes incessantly, to patients who do not come in for either a new or follow-up appointment. Yes, I call my patients; personally, directly, and often. In many clinics, patients receive reminder letters about upcoming appointments and then phone calls and sometimes letters when appointments are missed. My colleagues and I have jokingly referred to this practice as “benign stalking.”
Further, if a veteran is dissatisfied with care, there is a process to review and make adjustments if necessary, including transfer to a different doctor. Additionally, and sometimes alarmingly, veterans are not “fired” (and actually can’t be) for bad behavior (including direct threats to VA staff). Time, place, and manner of care can be tailored based on assessed risk, and VA police may be involved, but veterans continue to get care. I can assure you that if I made a threat to one of my doctors in private practice, I would very quickly be searching for a new doctor and answering some tough questions from law enforcement. Unlike many patients in private care, veterans have consistent access via phone (though admittedly not always user-friendly), walk-in appointments, after-hours availability in some locations, and secure messaging.
Electronic medical record and telehealth initiatives. The VA Computerized Patient Record System, has been around for some time and provides an excellent (although not perfect) system for documenting patient care. Each VA is linked to other VAs across the nation so patients don’t have to reinvent their story when they move and can actually get down to the business of being treated. Prior interventions, hospitalizations, medication trials, diagnostic impressions, imaging, lab work, etc, are all available at the touch of a button! And the VA’s telehealth initiative is all about access.
Veteran suicide prevention and opioid prescribing. Suicide is disproportionately high among veterans in the U.S. Recent data show that in 2014, an average of 20 veterans died by suicide per day.1 This accounted for 18% of all U.S. adult suicide deaths, even though veterans represent only 8.5% of the population. And while these recent statistics represent some improvement over prior research, prevention and care coordination remain major priorities in the VA. Veterans have access to same-day care (at least in Boise, Idaho) and a 24-hour crisis line that gives feedback to the patient’s local VA and can help coordinate follow-up care. The VA has specialized suicide prevention coordinators who attend to the needs of patients assessed to be at high risk for suicide and also disseminate training to providers in a variety of disciplines. All of this as the VA moves to ensure that suicide prevention remains a priority across disciplines and treatment sites.
Additionally, the VA is directly addressing the nationwide crisis of overprescription of opioids, beginning with education for both patients and staff and systemic encouragement of responsible prescribing via the national Opioid Safety Initiative and increased emphasis on providing at-risk veterans with naloxone kits.9
Research. VA research endeavors are wide ranging. The VA has been involved in pioneering clinical research in a substantial way since at least the 1920s and has contributed to important innovations in treatment, ranging from prosthetics to imaging, neuromodulation to medication intervention for a broad array of pathology.10
Drawing in professionals who want to work with veterans. The reason that many health care providers work at the VA is the veterans themselves. Veterans by and large represent a segment of our population who have demonstrated dedication, commitment to a shared goal, and the willingness to sacrifice their health or their lives for a greater good. The veteran identity and sacrifice has drawn many of us to want to serve them. My father’s and cousin’s service are truly inspirational on a personal level. I am not alone in this.
I recently had a veteran in my office who, once seated, pulled his chair closer to mine than I ordinarily prefer. He then gave me a penetrating stare, moved well within the comfort zone of even the closest of close-talkers, and began to scream about the wrongs he had heard about in the VA system. When he finished screaming (and once the other clinicians in the building realized that I wasn’t being physically attacked), he freely acknowledged that he had never actually experienced any of the VA shortcomings personally but, nonetheless, learned how reprehensible the VA is through the media. Our veterans deserve the best care that we as a nation can provide, and they also deserve to know the truth about the quality of VA care. But too often the negative media attention does not tell the whole story that directly impacts the well-being of our veterans.
I sit on the disruptive behavior committee at the Boise VAMC and see firsthand the stress that our veterans and staff are under. We review reports of veterans who disrupt the environment, sometimes by direct threats to shoot or in some way physically harm those taking care of them. Some of this is over pain medications or other specific health care issues. Some is due to frustration in trying to navigate an increasingly complex and nonintuitive system as the VA scrambles to implement congressional directives that sometimes clash with what is clinically appropriate and evidence-based. Some of the disruptive behavior, however, is fueled by the negative national discourse against the political establishment and its nearest representative—in this case, the VA. And again, this is often fueled, in my opinion, by incomplete media coverage.
The VA has problems. It would be delusional to argue otherwise. It is rightly open to public scrutiny as a tax-funded governmental agency, and lives are literally at stake as we grapple nationally with how best to deliver on Lincoln’s promise to “care for those who have borne the battle.”
As I reflect on my friend’s skepticism at my taking a VA position, I can answer that yes, the VA needs work. It has some major issues. But I no longer feel the need to cringe, because I now know firsthand the kind of care that is being delivered (at least to the veterans in Boise).
Wherever you stand on the quality of VA care, the movement to privatize, or the politicizing inevitable during an election year, to indiscriminately excoriate the VA is to risk marginalizing the superlative care that many currently receive by the thousands of physicians and other health care providers and administrators throughout the VA. Our veterans are a national treasure that deserve excellent care and real solutions to the problems that exist in the VA, not overwhelming negative rhetoric.
1. U.S. Department of Veterans Affairs, Office of Suicide Prevention. Suicide Among Veterans and Other Americans 2001-2014. http://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Published August 3, 2016. Accessed August 10, 2016.
2. Longman P, Gordon S. A conversation about the commission on care and the future of the VA. Washington Monthly. http://washingtonmonthly.com/2016/07/14/a-conversation-about-the-commission-on-care-and-the-future-of-the-va/. Published July 14, 2016. Accessed August 4, 2016.
3. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the Veterans Health Administration. Burnout Research. 2015;2(4):108-114.
4. U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and dental education program. http://www.va.gov/oaa/GME_default.asp. Updated December 9, 2015. Accessed August 4, 2016.
5. Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906.
6. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396.
7. Longman P. Best Care Anywhere: Why VA Health Care Would Work Better for Everyone. 3rd ed. San Francisco, CA: Berrett-Koehler; 2012.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. American customer satisfaction index 2013 customer satisfaction outpatient survey. http://www.va.gov/health/docs/VA2013OutpatientACSI.pdf. Published March 2014. Accessed August 10, 2016.
9. U.S. Department of Veterans Affairs. VHA pain management, Opioid Safety Initiative (OSI). http://www.va.gov/PAINMANAGEMENT/Opioid_Safety_Initiative_OSI.asp. Updated June 17, 2015. Accessed August 4, 2016.
10. U.S. Department of Veterans Affairs. Office of Research and Development. http://www.research.va.gov. Updated July 21, 2016. Accessed August 4, 2016.
Just over 2 years ago, I finished a psychiatry residency at the Mayo Clinic, turned down an offer to stay on staff, and topped it off by taking a position at the VA. Not one of my brighter moments—or so one of my friends thought. “Are you off your rocker? Don’t you know that the VA is terrible? Why would you go work there?” he jabbed incredulously. I cringed, knowing that I had passed up an opportunity to stay in arguably the best hospital system in the nation, possibly the world, to work at what some (maybe even a lot) view as a corpulent and recalcitrant bastion of ineptitude bound by the dictates of a fickle Congress.
In the wake of the Phoenix wait-time scandal (and no, it’s not like Disneyland), the suicide by self-immolation of Charles Richard Ingram III outside a VA facility in New Jersey, the new data on veteran suicide showing progress but continued significant concern, and the ongoing VA privatization discussion, the prevailing discourse about the VA is largely negative.1,2 And in a high-voltage election cycle where public outrage can serve as an efficient tool to garner support, the VA risks getting pummeled.
Add to this the shocking research that shows nearly half of VA psychiatrists are considering leaving the VA within the next 2 years, and it’s clear that dissatisfaction within and outside the VA is high.3 This does not bode well for veterans at a time when suicide and mental health care needs are so critically important. But while the bureaucracy of the VA is often the focus of negative press, it also filters down and unfortunately has the potential to directly affect VA practitioners and veterans. When we lose sight of what the VA does well, we risk being caught up in a vortex of negativity and a profound sense of inadequacy and helplessness. More attention to what is already being done well can help us as a nation more realistically chart a path forward rather than being fueled by negative rhetoric and rage.
Despite the challenges, the VA is currently succeeding in a number of areas that deserve recognition:
Medical school and resident education and collaboration with VA. In 2014, > 41,000 medical residents and nearly 23,000 medical students had some or all of their training in a VA setting. More than 95% of allopathic medical schools and nearly 90% of osteopathic medical schools had affiliation agreements with the VA in 2014.4 Suffice it to say, if the educational endeavors of the VA were curtailed, there would be an unholy scramble to provide well-trained physicians for our nation. (This does not include the dentists, psychologists, pharmacists, social workers, nurses, and other health care professionals whose training involves the VA in some capacity.) In addition, the VA often provides loan repayment assistance, which is very important given that many young professionals carry substantial school debt after completing training.
Mental health and primary care integration. Medical care overall is changing, and there is an increasing shift away from volume-based, fee-for-service care to integrated, team-based models. The VA is one of several successful leaders at a time when most U.S. health care providers are being scrutinized for their use of health care dollars and overall national health outcomes.5 In addition to primary care integration, the VA uses home-based primary care and mental health intensive case management teams for vulnerable veterans, adding flexibility, continuity, and access for many.
Overall excellent mental health care. A recent study by Watkins and colleagues found that when comparing quality measures for medication evaluation and management for schizophrenia, bipolar disorder, posttraumatic stress disorder, depression, and substance use disorders, “In every case, VA performance was superior to that of the private sector by more than 30%.”6 This is not an aberration and not limited to mental health care. It is a consistent finding about which books have been written.7 However, the availability of evidence-based care may not be consistent across all VA facilities nationally, depending on demand and staffing.
Despite the rumors, VA has high customer satisfaction. According to the American Customer Satisfaction Index, the VA has consistently performed well in measures of customer satisfaction compared with those of the private sector health care providers.8 Let’s not ignore what veterans have actually said and continue to say about their care.
Once in, you’re in! I recently missed an initial appointment with a private sector pediatrician for one of my sons. I was tersely invited to find another doctor. This seemed scandalous since I have become accustomed in my role as a VA physician to reaching out, sometimes incessantly, to patients who do not come in for either a new or follow-up appointment. Yes, I call my patients; personally, directly, and often. In many clinics, patients receive reminder letters about upcoming appointments and then phone calls and sometimes letters when appointments are missed. My colleagues and I have jokingly referred to this practice as “benign stalking.”
Further, if a veteran is dissatisfied with care, there is a process to review and make adjustments if necessary, including transfer to a different doctor. Additionally, and sometimes alarmingly, veterans are not “fired” (and actually can’t be) for bad behavior (including direct threats to VA staff). Time, place, and manner of care can be tailored based on assessed risk, and VA police may be involved, but veterans continue to get care. I can assure you that if I made a threat to one of my doctors in private practice, I would very quickly be searching for a new doctor and answering some tough questions from law enforcement. Unlike many patients in private care, veterans have consistent access via phone (though admittedly not always user-friendly), walk-in appointments, after-hours availability in some locations, and secure messaging.
Electronic medical record and telehealth initiatives. The VA Computerized Patient Record System, has been around for some time and provides an excellent (although not perfect) system for documenting patient care. Each VA is linked to other VAs across the nation so patients don’t have to reinvent their story when they move and can actually get down to the business of being treated. Prior interventions, hospitalizations, medication trials, diagnostic impressions, imaging, lab work, etc, are all available at the touch of a button! And the VA’s telehealth initiative is all about access.
Veteran suicide prevention and opioid prescribing. Suicide is disproportionately high among veterans in the U.S. Recent data show that in 2014, an average of 20 veterans died by suicide per day.1 This accounted for 18% of all U.S. adult suicide deaths, even though veterans represent only 8.5% of the population. And while these recent statistics represent some improvement over prior research, prevention and care coordination remain major priorities in the VA. Veterans have access to same-day care (at least in Boise, Idaho) and a 24-hour crisis line that gives feedback to the patient’s local VA and can help coordinate follow-up care. The VA has specialized suicide prevention coordinators who attend to the needs of patients assessed to be at high risk for suicide and also disseminate training to providers in a variety of disciplines. All of this as the VA moves to ensure that suicide prevention remains a priority across disciplines and treatment sites.
Additionally, the VA is directly addressing the nationwide crisis of overprescription of opioids, beginning with education for both patients and staff and systemic encouragement of responsible prescribing via the national Opioid Safety Initiative and increased emphasis on providing at-risk veterans with naloxone kits.9
Research. VA research endeavors are wide ranging. The VA has been involved in pioneering clinical research in a substantial way since at least the 1920s and has contributed to important innovations in treatment, ranging from prosthetics to imaging, neuromodulation to medication intervention for a broad array of pathology.10
Drawing in professionals who want to work with veterans. The reason that many health care providers work at the VA is the veterans themselves. Veterans by and large represent a segment of our population who have demonstrated dedication, commitment to a shared goal, and the willingness to sacrifice their health or their lives for a greater good. The veteran identity and sacrifice has drawn many of us to want to serve them. My father’s and cousin’s service are truly inspirational on a personal level. I am not alone in this.
I recently had a veteran in my office who, once seated, pulled his chair closer to mine than I ordinarily prefer. He then gave me a penetrating stare, moved well within the comfort zone of even the closest of close-talkers, and began to scream about the wrongs he had heard about in the VA system. When he finished screaming (and once the other clinicians in the building realized that I wasn’t being physically attacked), he freely acknowledged that he had never actually experienced any of the VA shortcomings personally but, nonetheless, learned how reprehensible the VA is through the media. Our veterans deserve the best care that we as a nation can provide, and they also deserve to know the truth about the quality of VA care. But too often the negative media attention does not tell the whole story that directly impacts the well-being of our veterans.
I sit on the disruptive behavior committee at the Boise VAMC and see firsthand the stress that our veterans and staff are under. We review reports of veterans who disrupt the environment, sometimes by direct threats to shoot or in some way physically harm those taking care of them. Some of this is over pain medications or other specific health care issues. Some is due to frustration in trying to navigate an increasingly complex and nonintuitive system as the VA scrambles to implement congressional directives that sometimes clash with what is clinically appropriate and evidence-based. Some of the disruptive behavior, however, is fueled by the negative national discourse against the political establishment and its nearest representative—in this case, the VA. And again, this is often fueled, in my opinion, by incomplete media coverage.
The VA has problems. It would be delusional to argue otherwise. It is rightly open to public scrutiny as a tax-funded governmental agency, and lives are literally at stake as we grapple nationally with how best to deliver on Lincoln’s promise to “care for those who have borne the battle.”
As I reflect on my friend’s skepticism at my taking a VA position, I can answer that yes, the VA needs work. It has some major issues. But I no longer feel the need to cringe, because I now know firsthand the kind of care that is being delivered (at least to the veterans in Boise).
Wherever you stand on the quality of VA care, the movement to privatize, or the politicizing inevitable during an election year, to indiscriminately excoriate the VA is to risk marginalizing the superlative care that many currently receive by the thousands of physicians and other health care providers and administrators throughout the VA. Our veterans are a national treasure that deserve excellent care and real solutions to the problems that exist in the VA, not overwhelming negative rhetoric.
Just over 2 years ago, I finished a psychiatry residency at the Mayo Clinic, turned down an offer to stay on staff, and topped it off by taking a position at the VA. Not one of my brighter moments—or so one of my friends thought. “Are you off your rocker? Don’t you know that the VA is terrible? Why would you go work there?” he jabbed incredulously. I cringed, knowing that I had passed up an opportunity to stay in arguably the best hospital system in the nation, possibly the world, to work at what some (maybe even a lot) view as a corpulent and recalcitrant bastion of ineptitude bound by the dictates of a fickle Congress.
In the wake of the Phoenix wait-time scandal (and no, it’s not like Disneyland), the suicide by self-immolation of Charles Richard Ingram III outside a VA facility in New Jersey, the new data on veteran suicide showing progress but continued significant concern, and the ongoing VA privatization discussion, the prevailing discourse about the VA is largely negative.1,2 And in a high-voltage election cycle where public outrage can serve as an efficient tool to garner support, the VA risks getting pummeled.
Add to this the shocking research that shows nearly half of VA psychiatrists are considering leaving the VA within the next 2 years, and it’s clear that dissatisfaction within and outside the VA is high.3 This does not bode well for veterans at a time when suicide and mental health care needs are so critically important. But while the bureaucracy of the VA is often the focus of negative press, it also filters down and unfortunately has the potential to directly affect VA practitioners and veterans. When we lose sight of what the VA does well, we risk being caught up in a vortex of negativity and a profound sense of inadequacy and helplessness. More attention to what is already being done well can help us as a nation more realistically chart a path forward rather than being fueled by negative rhetoric and rage.
Despite the challenges, the VA is currently succeeding in a number of areas that deserve recognition:
Medical school and resident education and collaboration with VA. In 2014, > 41,000 medical residents and nearly 23,000 medical students had some or all of their training in a VA setting. More than 95% of allopathic medical schools and nearly 90% of osteopathic medical schools had affiliation agreements with the VA in 2014.4 Suffice it to say, if the educational endeavors of the VA were curtailed, there would be an unholy scramble to provide well-trained physicians for our nation. (This does not include the dentists, psychologists, pharmacists, social workers, nurses, and other health care professionals whose training involves the VA in some capacity.) In addition, the VA often provides loan repayment assistance, which is very important given that many young professionals carry substantial school debt after completing training.
Mental health and primary care integration. Medical care overall is changing, and there is an increasing shift away from volume-based, fee-for-service care to integrated, team-based models. The VA is one of several successful leaders at a time when most U.S. health care providers are being scrutinized for their use of health care dollars and overall national health outcomes.5 In addition to primary care integration, the VA uses home-based primary care and mental health intensive case management teams for vulnerable veterans, adding flexibility, continuity, and access for many.
Overall excellent mental health care. A recent study by Watkins and colleagues found that when comparing quality measures for medication evaluation and management for schizophrenia, bipolar disorder, posttraumatic stress disorder, depression, and substance use disorders, “In every case, VA performance was superior to that of the private sector by more than 30%.”6 This is not an aberration and not limited to mental health care. It is a consistent finding about which books have been written.7 However, the availability of evidence-based care may not be consistent across all VA facilities nationally, depending on demand and staffing.
Despite the rumors, VA has high customer satisfaction. According to the American Customer Satisfaction Index, the VA has consistently performed well in measures of customer satisfaction compared with those of the private sector health care providers.8 Let’s not ignore what veterans have actually said and continue to say about their care.
Once in, you’re in! I recently missed an initial appointment with a private sector pediatrician for one of my sons. I was tersely invited to find another doctor. This seemed scandalous since I have become accustomed in my role as a VA physician to reaching out, sometimes incessantly, to patients who do not come in for either a new or follow-up appointment. Yes, I call my patients; personally, directly, and often. In many clinics, patients receive reminder letters about upcoming appointments and then phone calls and sometimes letters when appointments are missed. My colleagues and I have jokingly referred to this practice as “benign stalking.”
Further, if a veteran is dissatisfied with care, there is a process to review and make adjustments if necessary, including transfer to a different doctor. Additionally, and sometimes alarmingly, veterans are not “fired” (and actually can’t be) for bad behavior (including direct threats to VA staff). Time, place, and manner of care can be tailored based on assessed risk, and VA police may be involved, but veterans continue to get care. I can assure you that if I made a threat to one of my doctors in private practice, I would very quickly be searching for a new doctor and answering some tough questions from law enforcement. Unlike many patients in private care, veterans have consistent access via phone (though admittedly not always user-friendly), walk-in appointments, after-hours availability in some locations, and secure messaging.
Electronic medical record and telehealth initiatives. The VA Computerized Patient Record System, has been around for some time and provides an excellent (although not perfect) system for documenting patient care. Each VA is linked to other VAs across the nation so patients don’t have to reinvent their story when they move and can actually get down to the business of being treated. Prior interventions, hospitalizations, medication trials, diagnostic impressions, imaging, lab work, etc, are all available at the touch of a button! And the VA’s telehealth initiative is all about access.
Veteran suicide prevention and opioid prescribing. Suicide is disproportionately high among veterans in the U.S. Recent data show that in 2014, an average of 20 veterans died by suicide per day.1 This accounted for 18% of all U.S. adult suicide deaths, even though veterans represent only 8.5% of the population. And while these recent statistics represent some improvement over prior research, prevention and care coordination remain major priorities in the VA. Veterans have access to same-day care (at least in Boise, Idaho) and a 24-hour crisis line that gives feedback to the patient’s local VA and can help coordinate follow-up care. The VA has specialized suicide prevention coordinators who attend to the needs of patients assessed to be at high risk for suicide and also disseminate training to providers in a variety of disciplines. All of this as the VA moves to ensure that suicide prevention remains a priority across disciplines and treatment sites.
Additionally, the VA is directly addressing the nationwide crisis of overprescription of opioids, beginning with education for both patients and staff and systemic encouragement of responsible prescribing via the national Opioid Safety Initiative and increased emphasis on providing at-risk veterans with naloxone kits.9
Research. VA research endeavors are wide ranging. The VA has been involved in pioneering clinical research in a substantial way since at least the 1920s and has contributed to important innovations in treatment, ranging from prosthetics to imaging, neuromodulation to medication intervention for a broad array of pathology.10
Drawing in professionals who want to work with veterans. The reason that many health care providers work at the VA is the veterans themselves. Veterans by and large represent a segment of our population who have demonstrated dedication, commitment to a shared goal, and the willingness to sacrifice their health or their lives for a greater good. The veteran identity and sacrifice has drawn many of us to want to serve them. My father’s and cousin’s service are truly inspirational on a personal level. I am not alone in this.
I recently had a veteran in my office who, once seated, pulled his chair closer to mine than I ordinarily prefer. He then gave me a penetrating stare, moved well within the comfort zone of even the closest of close-talkers, and began to scream about the wrongs he had heard about in the VA system. When he finished screaming (and once the other clinicians in the building realized that I wasn’t being physically attacked), he freely acknowledged that he had never actually experienced any of the VA shortcomings personally but, nonetheless, learned how reprehensible the VA is through the media. Our veterans deserve the best care that we as a nation can provide, and they also deserve to know the truth about the quality of VA care. But too often the negative media attention does not tell the whole story that directly impacts the well-being of our veterans.
I sit on the disruptive behavior committee at the Boise VAMC and see firsthand the stress that our veterans and staff are under. We review reports of veterans who disrupt the environment, sometimes by direct threats to shoot or in some way physically harm those taking care of them. Some of this is over pain medications or other specific health care issues. Some is due to frustration in trying to navigate an increasingly complex and nonintuitive system as the VA scrambles to implement congressional directives that sometimes clash with what is clinically appropriate and evidence-based. Some of the disruptive behavior, however, is fueled by the negative national discourse against the political establishment and its nearest representative—in this case, the VA. And again, this is often fueled, in my opinion, by incomplete media coverage.
The VA has problems. It would be delusional to argue otherwise. It is rightly open to public scrutiny as a tax-funded governmental agency, and lives are literally at stake as we grapple nationally with how best to deliver on Lincoln’s promise to “care for those who have borne the battle.”
As I reflect on my friend’s skepticism at my taking a VA position, I can answer that yes, the VA needs work. It has some major issues. But I no longer feel the need to cringe, because I now know firsthand the kind of care that is being delivered (at least to the veterans in Boise).
Wherever you stand on the quality of VA care, the movement to privatize, or the politicizing inevitable during an election year, to indiscriminately excoriate the VA is to risk marginalizing the superlative care that many currently receive by the thousands of physicians and other health care providers and administrators throughout the VA. Our veterans are a national treasure that deserve excellent care and real solutions to the problems that exist in the VA, not overwhelming negative rhetoric.
1. U.S. Department of Veterans Affairs, Office of Suicide Prevention. Suicide Among Veterans and Other Americans 2001-2014. http://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Published August 3, 2016. Accessed August 10, 2016.
2. Longman P, Gordon S. A conversation about the commission on care and the future of the VA. Washington Monthly. http://washingtonmonthly.com/2016/07/14/a-conversation-about-the-commission-on-care-and-the-future-of-the-va/. Published July 14, 2016. Accessed August 4, 2016.
3. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the Veterans Health Administration. Burnout Research. 2015;2(4):108-114.
4. U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and dental education program. http://www.va.gov/oaa/GME_default.asp. Updated December 9, 2015. Accessed August 4, 2016.
5. Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906.
6. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396.
7. Longman P. Best Care Anywhere: Why VA Health Care Would Work Better for Everyone. 3rd ed. San Francisco, CA: Berrett-Koehler; 2012.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. American customer satisfaction index 2013 customer satisfaction outpatient survey. http://www.va.gov/health/docs/VA2013OutpatientACSI.pdf. Published March 2014. Accessed August 10, 2016.
9. U.S. Department of Veterans Affairs. VHA pain management, Opioid Safety Initiative (OSI). http://www.va.gov/PAINMANAGEMENT/Opioid_Safety_Initiative_OSI.asp. Updated June 17, 2015. Accessed August 4, 2016.
10. U.S. Department of Veterans Affairs. Office of Research and Development. http://www.research.va.gov. Updated July 21, 2016. Accessed August 4, 2016.
1. U.S. Department of Veterans Affairs, Office of Suicide Prevention. Suicide Among Veterans and Other Americans 2001-2014. http://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Published August 3, 2016. Accessed August 10, 2016.
2. Longman P, Gordon S. A conversation about the commission on care and the future of the VA. Washington Monthly. http://washingtonmonthly.com/2016/07/14/a-conversation-about-the-commission-on-care-and-the-future-of-the-va/. Published July 14, 2016. Accessed August 4, 2016.
3. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the Veterans Health Administration. Burnout Research. 2015;2(4):108-114.
4. U.S. Department of Veterans Affairs, Office of Academic Affiliations. Medical and dental education program. http://www.va.gov/oaa/GME_default.asp. Updated December 9, 2015. Accessed August 4, 2016.
5. Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906.
6. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396.
7. Longman P. Best Care Anywhere: Why VA Health Care Would Work Better for Everyone. 3rd ed. San Francisco, CA: Berrett-Koehler; 2012.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. American customer satisfaction index 2013 customer satisfaction outpatient survey. http://www.va.gov/health/docs/VA2013OutpatientACSI.pdf. Published March 2014. Accessed August 10, 2016.
9. U.S. Department of Veterans Affairs. VHA pain management, Opioid Safety Initiative (OSI). http://www.va.gov/PAINMANAGEMENT/Opioid_Safety_Initiative_OSI.asp. Updated June 17, 2015. Accessed August 4, 2016.
10. U.S. Department of Veterans Affairs. Office of Research and Development. http://www.research.va.gov. Updated July 21, 2016. Accessed August 4, 2016.
NIH Launches Study for New Zika Vaccine
An early-stage study to evaluate the safety and efficacy of an experimental Zika vaccine in humans is being launched by the National Institute of Allergy and Infectious Diseases (NIAID). “Results in animal testing have been very encouraging,” said NIAID Director Anthony Fauci, MD. “Although it will take some time before a vaccine against Zika is commercially available, the launch of this study is an important step forward.”
The NIAID scientists developed the investigational vaccine earlier this year. The approach is similar to that taken for another NIAID investigational vaccine developed for West Nile virus, which was found to be safe and effective in a phase 1 clinical trial. The vaccine includes a plasmid (small piece of DNA) engineered to contain genes that code for proteins of the Zika virus. The body reads the genes and makes Zika virus proteins, which cause an immune response. The DNA vaccines do not contain infectious material and cannot cause a vaccinated person to become infected with Zika.
The phase 1 clinical trial (VRC 319) will involve 4 groups of 20 people. The participants will be vaccinated at the first visit, and then half will receive another vaccination 8 weeks or 12 weeks later. The remaining participants will receive 2 additional vaccines, 1 group at week 4 and week 8; the other group, at week 4 and week 20. Participants will be followed for 44 weeks.
The study will be conducted at the NIH Clinical Center in Bethesda, the Center for Vaccine Development at the University of Maryland, and Emory University, Atlanta. Initial safety and immunogenicity data from the trial are expected by January 2017. In early 2017, If the results are favorable, NIAID plans a phase 2 trial in Zika-endemic countries.
An early-stage study to evaluate the safety and efficacy of an experimental Zika vaccine in humans is being launched by the National Institute of Allergy and Infectious Diseases (NIAID). “Results in animal testing have been very encouraging,” said NIAID Director Anthony Fauci, MD. “Although it will take some time before a vaccine against Zika is commercially available, the launch of this study is an important step forward.”
The NIAID scientists developed the investigational vaccine earlier this year. The approach is similar to that taken for another NIAID investigational vaccine developed for West Nile virus, which was found to be safe and effective in a phase 1 clinical trial. The vaccine includes a plasmid (small piece of DNA) engineered to contain genes that code for proteins of the Zika virus. The body reads the genes and makes Zika virus proteins, which cause an immune response. The DNA vaccines do not contain infectious material and cannot cause a vaccinated person to become infected with Zika.
The phase 1 clinical trial (VRC 319) will involve 4 groups of 20 people. The participants will be vaccinated at the first visit, and then half will receive another vaccination 8 weeks or 12 weeks later. The remaining participants will receive 2 additional vaccines, 1 group at week 4 and week 8; the other group, at week 4 and week 20. Participants will be followed for 44 weeks.
The study will be conducted at the NIH Clinical Center in Bethesda, the Center for Vaccine Development at the University of Maryland, and Emory University, Atlanta. Initial safety and immunogenicity data from the trial are expected by January 2017. In early 2017, If the results are favorable, NIAID plans a phase 2 trial in Zika-endemic countries.
An early-stage study to evaluate the safety and efficacy of an experimental Zika vaccine in humans is being launched by the National Institute of Allergy and Infectious Diseases (NIAID). “Results in animal testing have been very encouraging,” said NIAID Director Anthony Fauci, MD. “Although it will take some time before a vaccine against Zika is commercially available, the launch of this study is an important step forward.”
The NIAID scientists developed the investigational vaccine earlier this year. The approach is similar to that taken for another NIAID investigational vaccine developed for West Nile virus, which was found to be safe and effective in a phase 1 clinical trial. The vaccine includes a plasmid (small piece of DNA) engineered to contain genes that code for proteins of the Zika virus. The body reads the genes and makes Zika virus proteins, which cause an immune response. The DNA vaccines do not contain infectious material and cannot cause a vaccinated person to become infected with Zika.
The phase 1 clinical trial (VRC 319) will involve 4 groups of 20 people. The participants will be vaccinated at the first visit, and then half will receive another vaccination 8 weeks or 12 weeks later. The remaining participants will receive 2 additional vaccines, 1 group at week 4 and week 8; the other group, at week 4 and week 20. Participants will be followed for 44 weeks.
The study will be conducted at the NIH Clinical Center in Bethesda, the Center for Vaccine Development at the University of Maryland, and Emory University, Atlanta. Initial safety and immunogenicity data from the trial are expected by January 2017. In early 2017, If the results are favorable, NIAID plans a phase 2 trial in Zika-endemic countries.
Massive Gap in HIV Screening
Between 2009 and 2012, white men aged 15 to 39 years made an average of 1.6 visits to doctor’s offices each year. But in 99% of those visits, the men did not get an HIV test—even though in 2012, about 15% of men living with HIV had undiagnosed HIV infection. Those percentages were worse than the findings for blacks and Hispanics, although those were not much better: Only 2.7% of black men and 1.4% of Hispanic men were tested, and they were less likely to visit the doctor’s office.
To identify opportunities for HIV diagnosis in young men, CDC researchers analyzed data from the 2009-2012 National Ambulatory Medical Care Survey (NAMCS) and U.S. census data.
Although the number of men visiting health care offices was up from 59% in 2010 and 63% in 2011, to 75% in 2014, it seems that the group aged 20 to 29 years is getting the most attention. HIV testing was lowest among men aged 15 to 19 and 35 to 39 years.
Why is screening still so rare? The researchers suggest that providers may not know about national testing recommendations, believe that their patients are not at risk, or believe that HIV testing is the responsibility of other health care professionals in other settings.
The CDC report says interventions to make HIV testing routine, such as opt-out testing, might help increase coverage among young men who might not otherwise seek it.
Between 2009 and 2012, white men aged 15 to 39 years made an average of 1.6 visits to doctor’s offices each year. But in 99% of those visits, the men did not get an HIV test—even though in 2012, about 15% of men living with HIV had undiagnosed HIV infection. Those percentages were worse than the findings for blacks and Hispanics, although those were not much better: Only 2.7% of black men and 1.4% of Hispanic men were tested, and they were less likely to visit the doctor’s office.
To identify opportunities for HIV diagnosis in young men, CDC researchers analyzed data from the 2009-2012 National Ambulatory Medical Care Survey (NAMCS) and U.S. census data.
Although the number of men visiting health care offices was up from 59% in 2010 and 63% in 2011, to 75% in 2014, it seems that the group aged 20 to 29 years is getting the most attention. HIV testing was lowest among men aged 15 to 19 and 35 to 39 years.
Why is screening still so rare? The researchers suggest that providers may not know about national testing recommendations, believe that their patients are not at risk, or believe that HIV testing is the responsibility of other health care professionals in other settings.
The CDC report says interventions to make HIV testing routine, such as opt-out testing, might help increase coverage among young men who might not otherwise seek it.
Between 2009 and 2012, white men aged 15 to 39 years made an average of 1.6 visits to doctor’s offices each year. But in 99% of those visits, the men did not get an HIV test—even though in 2012, about 15% of men living with HIV had undiagnosed HIV infection. Those percentages were worse than the findings for blacks and Hispanics, although those were not much better: Only 2.7% of black men and 1.4% of Hispanic men were tested, and they were less likely to visit the doctor’s office.
To identify opportunities for HIV diagnosis in young men, CDC researchers analyzed data from the 2009-2012 National Ambulatory Medical Care Survey (NAMCS) and U.S. census data.
Although the number of men visiting health care offices was up from 59% in 2010 and 63% in 2011, to 75% in 2014, it seems that the group aged 20 to 29 years is getting the most attention. HIV testing was lowest among men aged 15 to 19 and 35 to 39 years.
Why is screening still so rare? The researchers suggest that providers may not know about national testing recommendations, believe that their patients are not at risk, or believe that HIV testing is the responsibility of other health care professionals in other settings.
The CDC report says interventions to make HIV testing routine, such as opt-out testing, might help increase coverage among young men who might not otherwise seek it.
Unraveling the Causes of Breast Cancer Disparities
Why are black women more likely to develop certain aggressive subtypes of breast cancer than are white women? Also, why are black women more likely to die of breast cancer? The National Cancer Institute (NCI) has launched a collaborative research project to pinpoint genetic factors that underlie these and other disparities.
The Breast Cancer Genetic Study in African-Ancestry Populations is the largest study to date to investigate genetic and biological factors behind black women’s risk of breast cancer. It won’t enroll new patients but instead will bring together researchers and data from a variety of venues, including the African-American Breast Cancer Consortium, the African-American Breast Cancer Epidemiology and Risk Consortium, and the NCI Cohort Consortium. Minority scientists from various institutions are playing an important role in the study, NCI says.
The researchers will share biospecimens, data, and resources of the 20,000 black women involved in 18 previous studies. The genomes of those women will be compared with those of 20,000 black women who do not have breast cancer as well as with white women who have breast cancer. The project will investigate genetic variations associated with breast cancer risk in black women and gene expression in tumor samples to identify genetic pathways.
“This effort is about making sure that all Americans—no matter their background—reap the same benefits from the promising advances of precisions medicine,” said Douglas Lowy, MD, acting director of NCI. “I’m hopeful about where this new research can take us, not only in addressing the unique breast cancer profiles of African American women, but also in learning more about the origin of cancer disparities.”
Why are black women more likely to develop certain aggressive subtypes of breast cancer than are white women? Also, why are black women more likely to die of breast cancer? The National Cancer Institute (NCI) has launched a collaborative research project to pinpoint genetic factors that underlie these and other disparities.
The Breast Cancer Genetic Study in African-Ancestry Populations is the largest study to date to investigate genetic and biological factors behind black women’s risk of breast cancer. It won’t enroll new patients but instead will bring together researchers and data from a variety of venues, including the African-American Breast Cancer Consortium, the African-American Breast Cancer Epidemiology and Risk Consortium, and the NCI Cohort Consortium. Minority scientists from various institutions are playing an important role in the study, NCI says.
The researchers will share biospecimens, data, and resources of the 20,000 black women involved in 18 previous studies. The genomes of those women will be compared with those of 20,000 black women who do not have breast cancer as well as with white women who have breast cancer. The project will investigate genetic variations associated with breast cancer risk in black women and gene expression in tumor samples to identify genetic pathways.
“This effort is about making sure that all Americans—no matter their background—reap the same benefits from the promising advances of precisions medicine,” said Douglas Lowy, MD, acting director of NCI. “I’m hopeful about where this new research can take us, not only in addressing the unique breast cancer profiles of African American women, but also in learning more about the origin of cancer disparities.”
Why are black women more likely to develop certain aggressive subtypes of breast cancer than are white women? Also, why are black women more likely to die of breast cancer? The National Cancer Institute (NCI) has launched a collaborative research project to pinpoint genetic factors that underlie these and other disparities.
The Breast Cancer Genetic Study in African-Ancestry Populations is the largest study to date to investigate genetic and biological factors behind black women’s risk of breast cancer. It won’t enroll new patients but instead will bring together researchers and data from a variety of venues, including the African-American Breast Cancer Consortium, the African-American Breast Cancer Epidemiology and Risk Consortium, and the NCI Cohort Consortium. Minority scientists from various institutions are playing an important role in the study, NCI says.
The researchers will share biospecimens, data, and resources of the 20,000 black women involved in 18 previous studies. The genomes of those women will be compared with those of 20,000 black women who do not have breast cancer as well as with white women who have breast cancer. The project will investigate genetic variations associated with breast cancer risk in black women and gene expression in tumor samples to identify genetic pathways.
“This effort is about making sure that all Americans—no matter their background—reap the same benefits from the promising advances of precisions medicine,” said Douglas Lowy, MD, acting director of NCI. “I’m hopeful about where this new research can take us, not only in addressing the unique breast cancer profiles of African American women, but also in learning more about the origin of cancer disparities.”
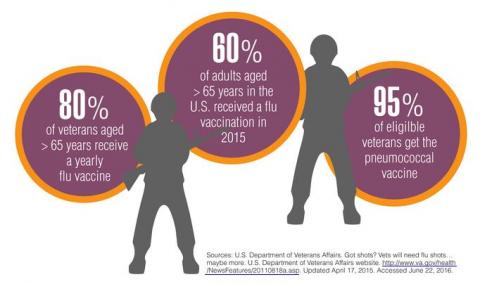
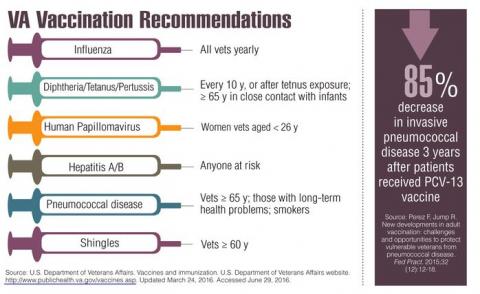
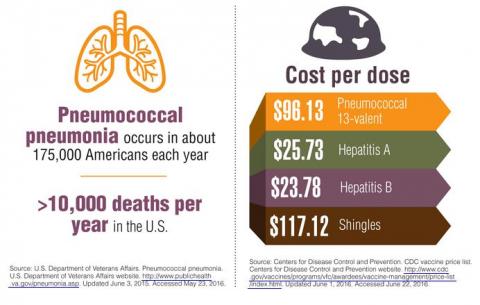
New Vaccination Data & Trends
For many diseases, prevention may be the most effective treatment plan. Vaccination is considered a safe medical procedure that not only protects those who receive the immunization, but also helps to prevent the spread of communicable diseases. Or more simply, vaccines are the most effective tool we have to prevent infectious diseases, according to the National Vaccine Program Office.
When the measles vaccine was licensed in 1962, there were more than 400,000 cases reported in the U.S. In 2012, there were just 55, according to the CDC. In fact today, a single outbreak, such as the one experienced by visitors to Disneyland in 2015 creates national headlines.
The CDC offers a tool that can help veterans determine which age-appropriate vaccinations they need to protect their health group. A short quiz, available at http://www2a.cdc.gov/nip/adultImmSched/ can help people determine which vaccinations are most crucial for them to receive. At a minimum the VA recommends that all veterans consider receiving vaccinations for influenza; pneumococcal; hepatitis A and B; measles, mumps and rubella (MMR); chickenpox (varicella); shingles (herpes zoster); tetanus, diphtheria, and pertussis vaccines. In addition, international travelers may be eligible to receive vaccinations that protect against diseases common in the countries being visited. Vaccination needs can change based on age, so the VA advises veterans to speak with their health care team about additional immunizations that might be wise to consider.
Click here to read the digital edition.
For many diseases, prevention may be the most effective treatment plan. Vaccination is considered a safe medical procedure that not only protects those who receive the immunization, but also helps to prevent the spread of communicable diseases. Or more simply, vaccines are the most effective tool we have to prevent infectious diseases, according to the National Vaccine Program Office.
When the measles vaccine was licensed in 1962, there were more than 400,000 cases reported in the U.S. In 2012, there were just 55, according to the CDC. In fact today, a single outbreak, such as the one experienced by visitors to Disneyland in 2015 creates national headlines.
The CDC offers a tool that can help veterans determine which age-appropriate vaccinations they need to protect their health group. A short quiz, available at http://www2a.cdc.gov/nip/adultImmSched/ can help people determine which vaccinations are most crucial for them to receive. At a minimum the VA recommends that all veterans consider receiving vaccinations for influenza; pneumococcal; hepatitis A and B; measles, mumps and rubella (MMR); chickenpox (varicella); shingles (herpes zoster); tetanus, diphtheria, and pertussis vaccines. In addition, international travelers may be eligible to receive vaccinations that protect against diseases common in the countries being visited. Vaccination needs can change based on age, so the VA advises veterans to speak with their health care team about additional immunizations that might be wise to consider.
Click here to read the digital edition.
For many diseases, prevention may be the most effective treatment plan. Vaccination is considered a safe medical procedure that not only protects those who receive the immunization, but also helps to prevent the spread of communicable diseases. Or more simply, vaccines are the most effective tool we have to prevent infectious diseases, according to the National Vaccine Program Office.
When the measles vaccine was licensed in 1962, there were more than 400,000 cases reported in the U.S. In 2012, there were just 55, according to the CDC. In fact today, a single outbreak, such as the one experienced by visitors to Disneyland in 2015 creates national headlines.
The CDC offers a tool that can help veterans determine which age-appropriate vaccinations they need to protect their health group. A short quiz, available at http://www2a.cdc.gov/nip/adultImmSched/ can help people determine which vaccinations are most crucial for them to receive. At a minimum the VA recommends that all veterans consider receiving vaccinations for influenza; pneumococcal; hepatitis A and B; measles, mumps and rubella (MMR); chickenpox (varicella); shingles (herpes zoster); tetanus, diphtheria, and pertussis vaccines. In addition, international travelers may be eligible to receive vaccinations that protect against diseases common in the countries being visited. Vaccination needs can change based on age, so the VA advises veterans to speak with their health care team about additional immunizations that might be wise to consider.
Click here to read the digital edition.
Veteran Suicide Rate Up 32% Since 2001
Veteran suicides increased 32% from 2001 to 2014 according to a new VA report. The report also noted that rates for adult nonveterans also increased by 23% over the same period. However, veterans still account for 18% of all suicides in the U.S.
The report also highlighted a number of positive developments. For example, a previous study, conducted in 2012, estimated that 22 veterans committed suicide per day. That study included information from 3 million records obtained from mortality records in 20 states or data from veterans who used VHA health services. The more recent study, which examines 55 million veteran records from every state from 1979 to 2014, found that an average of 20 veterans per day die by suicide.
“Twenty a day is not that different from 22,” said David J. Shulkin, MD, VA Under Secretary for Health, in an interview. “It is far too high.”
Preventing veteran suicide is a top priority for the VA, and the recent report showed that the VA’s efforts are making an impact. For example, the rate of suicide among veterans who use VA services increased by 8.8% from 2001 to 2014, compared with a 38.6% increase in suicide among veterans who do not use VA services. These services include mental health treatment at VA medical centers, community-based outpatient clinics, and Vet Centers offering readjustment counseling.
In addition, the Veterans Crisis Line, launched in 2007, offers immediate support to veterans experiencing suicidal thoughts. To date, staffers have answered nearly 2.4 million calls and initiated the dispatch of emergency services to callers in crisis more than 62,000 times. The VA announced that it is expanding its Veterans Crisis Line by creating a satellite site in Atlanta, Georgia, and adding 200 additional responders.
“This collaborative effort provides both updated and comprehensive data that allow us to make better informed decisions on how to prevent this national tragedy,” said Dr. Shulkin, in a statement that previewed the survey results. “We as a nation must focus on bringing the number of veteran suicides to zero.”
Veteran suicides increased 32% from 2001 to 2014 according to a new VA report. The report also noted that rates for adult nonveterans also increased by 23% over the same period. However, veterans still account for 18% of all suicides in the U.S.
The report also highlighted a number of positive developments. For example, a previous study, conducted in 2012, estimated that 22 veterans committed suicide per day. That study included information from 3 million records obtained from mortality records in 20 states or data from veterans who used VHA health services. The more recent study, which examines 55 million veteran records from every state from 1979 to 2014, found that an average of 20 veterans per day die by suicide.
“Twenty a day is not that different from 22,” said David J. Shulkin, MD, VA Under Secretary for Health, in an interview. “It is far too high.”
Preventing veteran suicide is a top priority for the VA, and the recent report showed that the VA’s efforts are making an impact. For example, the rate of suicide among veterans who use VA services increased by 8.8% from 2001 to 2014, compared with a 38.6% increase in suicide among veterans who do not use VA services. These services include mental health treatment at VA medical centers, community-based outpatient clinics, and Vet Centers offering readjustment counseling.
In addition, the Veterans Crisis Line, launched in 2007, offers immediate support to veterans experiencing suicidal thoughts. To date, staffers have answered nearly 2.4 million calls and initiated the dispatch of emergency services to callers in crisis more than 62,000 times. The VA announced that it is expanding its Veterans Crisis Line by creating a satellite site in Atlanta, Georgia, and adding 200 additional responders.
“This collaborative effort provides both updated and comprehensive data that allow us to make better informed decisions on how to prevent this national tragedy,” said Dr. Shulkin, in a statement that previewed the survey results. “We as a nation must focus on bringing the number of veteran suicides to zero.”
Veteran suicides increased 32% from 2001 to 2014 according to a new VA report. The report also noted that rates for adult nonveterans also increased by 23% over the same period. However, veterans still account for 18% of all suicides in the U.S.
The report also highlighted a number of positive developments. For example, a previous study, conducted in 2012, estimated that 22 veterans committed suicide per day. That study included information from 3 million records obtained from mortality records in 20 states or data from veterans who used VHA health services. The more recent study, which examines 55 million veteran records from every state from 1979 to 2014, found that an average of 20 veterans per day die by suicide.
“Twenty a day is not that different from 22,” said David J. Shulkin, MD, VA Under Secretary for Health, in an interview. “It is far too high.”
Preventing veteran suicide is a top priority for the VA, and the recent report showed that the VA’s efforts are making an impact. For example, the rate of suicide among veterans who use VA services increased by 8.8% from 2001 to 2014, compared with a 38.6% increase in suicide among veterans who do not use VA services. These services include mental health treatment at VA medical centers, community-based outpatient clinics, and Vet Centers offering readjustment counseling.
In addition, the Veterans Crisis Line, launched in 2007, offers immediate support to veterans experiencing suicidal thoughts. To date, staffers have answered nearly 2.4 million calls and initiated the dispatch of emergency services to callers in crisis more than 62,000 times. The VA announced that it is expanding its Veterans Crisis Line by creating a satellite site in Atlanta, Georgia, and adding 200 additional responders.
“This collaborative effort provides both updated and comprehensive data that allow us to make better informed decisions on how to prevent this national tragedy,” said Dr. Shulkin, in a statement that previewed the survey results. “We as a nation must focus on bringing the number of veteran suicides to zero.”
Veteran Homelessness Drops 47% Since 2010
In the latest Department of Housing and Urban Development annual Point-in-Time (PIT) estimate of America’s homeless population, President Barak Obama revealed that since 2010 the rate of homelessness among veterans has dropped 47%. The January count found 13,000 homeless veterans, although the count fell well short of the President’s pledge to completely eliminate homelessness by 2016. “We will not stop until every veteran who fought for America has a home in America,” President Obama told the national Disabled American Veterans (DAV) convention on August 1. “This is something we’ve got to get done.”
“The dramatic decline in veteran homelessness is the result of the Obama administration’s investments in permanent supportive housing solutions, such as HUD-VASH [Housing and Urban Development-VA Supportive Housing] and Supportive Services for Veteran Families programs, extensive community partnerships, coordinated data and outreach, and other proven strategies that put Veterans first,” said VA Secretary Robert A. McDonald in a release. According to the VA, Virginia, Connecticut and 27 cities and towns across the country have “effectively ended” veteran homelessness.
In the DAV speech, President Obama also touted a number of VA health care programs, ranging from rural telehealth initiatives to increased funding for prosthetics and access to women’s health providers at all VA clinics. Pointing out that VA funding has increased during his administration, the President noted that “We’ve made VA benefits available to more than 2 million veterans who didn’t have them before.” The President also pointed out that veterans can apply for VA health care “…from any device, including your smartphone—simple, easy, in as little as 20 minutes.”
The White House also announced that the Million Veteran Program (MVP) had reached a new milestone with 500,000 veterans enrolled. About 62% of MVP enrollees reported a current or past diagnosis of high blood pressure and about one-third reported tinnitus. Also, nearly one-third, or 32%, of veterans present with a history or current diagnosis of cancer. “We believe MVP will accelerate our understanding of disease detection, progression, prevention and treatment by combining this rich clinical, environmental and genomic data,” said VA Under Secretary for Health David J. Shulkin, MD, in a statement. “VA has a deep history of innovation and research. The MVP will allow the nation’s top researchers to perform the most cutting-edge science to treat some of the nation’s most troubling diseases.”
“What this does is it gives us a better understanding of genetics, which will allow us to improve treatments for things like traumatic brain injury and posttraumatic stress, and diabetes, and cancer,” President Obama told the DAV audience. “And that won’t just help veterans. It will help all Americans. And it’s just one more example of how our veterans keep serving our country even after they come home.”
While Acknowledging the VA’s challenges to meet the needs of veterans, President Obama was insistent that VA care was essential for veterans. “Study after study shows that in many areas, like mental health, the quality of care at the VA is often better than in private care,” he told the DAV members. “So let’s listen to our veterans, who are telling us: Don’t destroy VA health care. Fix it and make it work, but don’t break our covenant with our veterans.”
In the latest Department of Housing and Urban Development annual Point-in-Time (PIT) estimate of America’s homeless population, President Barak Obama revealed that since 2010 the rate of homelessness among veterans has dropped 47%. The January count found 13,000 homeless veterans, although the count fell well short of the President’s pledge to completely eliminate homelessness by 2016. “We will not stop until every veteran who fought for America has a home in America,” President Obama told the national Disabled American Veterans (DAV) convention on August 1. “This is something we’ve got to get done.”
“The dramatic decline in veteran homelessness is the result of the Obama administration’s investments in permanent supportive housing solutions, such as HUD-VASH [Housing and Urban Development-VA Supportive Housing] and Supportive Services for Veteran Families programs, extensive community partnerships, coordinated data and outreach, and other proven strategies that put Veterans first,” said VA Secretary Robert A. McDonald in a release. According to the VA, Virginia, Connecticut and 27 cities and towns across the country have “effectively ended” veteran homelessness.
In the DAV speech, President Obama also touted a number of VA health care programs, ranging from rural telehealth initiatives to increased funding for prosthetics and access to women’s health providers at all VA clinics. Pointing out that VA funding has increased during his administration, the President noted that “We’ve made VA benefits available to more than 2 million veterans who didn’t have them before.” The President also pointed out that veterans can apply for VA health care “…from any device, including your smartphone—simple, easy, in as little as 20 minutes.”
The White House also announced that the Million Veteran Program (MVP) had reached a new milestone with 500,000 veterans enrolled. About 62% of MVP enrollees reported a current or past diagnosis of high blood pressure and about one-third reported tinnitus. Also, nearly one-third, or 32%, of veterans present with a history or current diagnosis of cancer. “We believe MVP will accelerate our understanding of disease detection, progression, prevention and treatment by combining this rich clinical, environmental and genomic data,” said VA Under Secretary for Health David J. Shulkin, MD, in a statement. “VA has a deep history of innovation and research. The MVP will allow the nation’s top researchers to perform the most cutting-edge science to treat some of the nation’s most troubling diseases.”
“What this does is it gives us a better understanding of genetics, which will allow us to improve treatments for things like traumatic brain injury and posttraumatic stress, and diabetes, and cancer,” President Obama told the DAV audience. “And that won’t just help veterans. It will help all Americans. And it’s just one more example of how our veterans keep serving our country even after they come home.”
While Acknowledging the VA’s challenges to meet the needs of veterans, President Obama was insistent that VA care was essential for veterans. “Study after study shows that in many areas, like mental health, the quality of care at the VA is often better than in private care,” he told the DAV members. “So let’s listen to our veterans, who are telling us: Don’t destroy VA health care. Fix it and make it work, but don’t break our covenant with our veterans.”
In the latest Department of Housing and Urban Development annual Point-in-Time (PIT) estimate of America’s homeless population, President Barak Obama revealed that since 2010 the rate of homelessness among veterans has dropped 47%. The January count found 13,000 homeless veterans, although the count fell well short of the President’s pledge to completely eliminate homelessness by 2016. “We will not stop until every veteran who fought for America has a home in America,” President Obama told the national Disabled American Veterans (DAV) convention on August 1. “This is something we’ve got to get done.”
“The dramatic decline in veteran homelessness is the result of the Obama administration’s investments in permanent supportive housing solutions, such as HUD-VASH [Housing and Urban Development-VA Supportive Housing] and Supportive Services for Veteran Families programs, extensive community partnerships, coordinated data and outreach, and other proven strategies that put Veterans first,” said VA Secretary Robert A. McDonald in a release. According to the VA, Virginia, Connecticut and 27 cities and towns across the country have “effectively ended” veteran homelessness.
In the DAV speech, President Obama also touted a number of VA health care programs, ranging from rural telehealth initiatives to increased funding for prosthetics and access to women’s health providers at all VA clinics. Pointing out that VA funding has increased during his administration, the President noted that “We’ve made VA benefits available to more than 2 million veterans who didn’t have them before.” The President also pointed out that veterans can apply for VA health care “…from any device, including your smartphone—simple, easy, in as little as 20 minutes.”
The White House also announced that the Million Veteran Program (MVP) had reached a new milestone with 500,000 veterans enrolled. About 62% of MVP enrollees reported a current or past diagnosis of high blood pressure and about one-third reported tinnitus. Also, nearly one-third, or 32%, of veterans present with a history or current diagnosis of cancer. “We believe MVP will accelerate our understanding of disease detection, progression, prevention and treatment by combining this rich clinical, environmental and genomic data,” said VA Under Secretary for Health David J. Shulkin, MD, in a statement. “VA has a deep history of innovation and research. The MVP will allow the nation’s top researchers to perform the most cutting-edge science to treat some of the nation’s most troubling diseases.”
“What this does is it gives us a better understanding of genetics, which will allow us to improve treatments for things like traumatic brain injury and posttraumatic stress, and diabetes, and cancer,” President Obama told the DAV audience. “And that won’t just help veterans. It will help all Americans. And it’s just one more example of how our veterans keep serving our country even after they come home.”
While Acknowledging the VA’s challenges to meet the needs of veterans, President Obama was insistent that VA care was essential for veterans. “Study after study shows that in many areas, like mental health, the quality of care at the VA is often better than in private care,” he told the DAV members. “So let’s listen to our veterans, who are telling us: Don’t destroy VA health care. Fix it and make it work, but don’t break our covenant with our veterans.”
McDonald to VFW—We’re Already Seeing Results
Addressing the Veterans of Foreign Wars National Convention on Tuesday, VA Secretary Robert A. McDonald insisted that the VA has made significant progress. “Not only can it be transformed, transformation is well underway—and we’re already seeing results,” he told the audience of more than 12,000 veterans.
In his speech, Secretary McDonald noted the significant change in 13 of the VA’s top 18 executive positions. Still, McDonald insisted, “We can’t fire our way to excellence….We won’t punish people based on opinions, recycled and embellished media accounts, or external pressure. It’s not in the best interest of the veterans we serve. Excellence is what we’re after.”
McDonald touted the VA’s unique approach to health care. “We have a unique lifetime relationship with our 9 million patients and a single electronic health record across the entire enterprise. Nobody else offers that,” he insisted. “Our mental health care’s integrated with primary care, with specialty care, and with psychosocial support to minimize barriers and help resolve problems early. Nobody else offers that.”
According to McDonald, “The VA is embracing what works to heal veterans. And VA care is integrated with nonmedical determinants of health and well-being that people often miss,” he told the VFW. “Under Secretary of Health Dr. David Shulkin is changing our system to proactive, holistic health care and wellness. It’s time we got beyond just reacting to disease when it happens.”
McDonald told the audience that in 2015, veterans had nearly 5 million more appointments than in 2014. Almost 57 million of these appointments were in VA-operated facilities and another 21 million in community settings. Now 97% of appointments are completed within 30 days of veterans’ preferred date, he told the audience, and 86% were completed within 7 days—22% are completed the same day.
“We are making important progress,” McDonald asserted. “But you rarely hear that in the media. You’d never know we lead in many fields of research that benefit all Americans—PTSD, traumatic brain injury, spinal cord injury, prosthetics, genetics.”
Addressing the Veterans of Foreign Wars National Convention on Tuesday, VA Secretary Robert A. McDonald insisted that the VA has made significant progress. “Not only can it be transformed, transformation is well underway—and we’re already seeing results,” he told the audience of more than 12,000 veterans.
In his speech, Secretary McDonald noted the significant change in 13 of the VA’s top 18 executive positions. Still, McDonald insisted, “We can’t fire our way to excellence….We won’t punish people based on opinions, recycled and embellished media accounts, or external pressure. It’s not in the best interest of the veterans we serve. Excellence is what we’re after.”
McDonald touted the VA’s unique approach to health care. “We have a unique lifetime relationship with our 9 million patients and a single electronic health record across the entire enterprise. Nobody else offers that,” he insisted. “Our mental health care’s integrated with primary care, with specialty care, and with psychosocial support to minimize barriers and help resolve problems early. Nobody else offers that.”
According to McDonald, “The VA is embracing what works to heal veterans. And VA care is integrated with nonmedical determinants of health and well-being that people often miss,” he told the VFW. “Under Secretary of Health Dr. David Shulkin is changing our system to proactive, holistic health care and wellness. It’s time we got beyond just reacting to disease when it happens.”
McDonald told the audience that in 2015, veterans had nearly 5 million more appointments than in 2014. Almost 57 million of these appointments were in VA-operated facilities and another 21 million in community settings. Now 97% of appointments are completed within 30 days of veterans’ preferred date, he told the audience, and 86% were completed within 7 days—22% are completed the same day.
“We are making important progress,” McDonald asserted. “But you rarely hear that in the media. You’d never know we lead in many fields of research that benefit all Americans—PTSD, traumatic brain injury, spinal cord injury, prosthetics, genetics.”
Addressing the Veterans of Foreign Wars National Convention on Tuesday, VA Secretary Robert A. McDonald insisted that the VA has made significant progress. “Not only can it be transformed, transformation is well underway—and we’re already seeing results,” he told the audience of more than 12,000 veterans.
In his speech, Secretary McDonald noted the significant change in 13 of the VA’s top 18 executive positions. Still, McDonald insisted, “We can’t fire our way to excellence….We won’t punish people based on opinions, recycled and embellished media accounts, or external pressure. It’s not in the best interest of the veterans we serve. Excellence is what we’re after.”
McDonald touted the VA’s unique approach to health care. “We have a unique lifetime relationship with our 9 million patients and a single electronic health record across the entire enterprise. Nobody else offers that,” he insisted. “Our mental health care’s integrated with primary care, with specialty care, and with psychosocial support to minimize barriers and help resolve problems early. Nobody else offers that.”
According to McDonald, “The VA is embracing what works to heal veterans. And VA care is integrated with nonmedical determinants of health and well-being that people often miss,” he told the VFW. “Under Secretary of Health Dr. David Shulkin is changing our system to proactive, holistic health care and wellness. It’s time we got beyond just reacting to disease when it happens.”
McDonald told the audience that in 2015, veterans had nearly 5 million more appointments than in 2014. Almost 57 million of these appointments were in VA-operated facilities and another 21 million in community settings. Now 97% of appointments are completed within 30 days of veterans’ preferred date, he told the audience, and 86% were completed within 7 days—22% are completed the same day.
“We are making important progress,” McDonald asserted. “But you rarely hear that in the media. You’d never know we lead in many fields of research that benefit all Americans—PTSD, traumatic brain injury, spinal cord injury, prosthetics, genetics.”
Education and Anxiety Disorders
Adults with lower than a high school education are more than twice as likely to have experienced an anxiety disorder in the past year than those with higher levels of education, according to a study by the Substance Abuse and Mental Health Services Administration.
The National Survey on Drug Use and Health’s 2008 to 2012 Mental Health Surveillance Study (MHSS) found an estimated 12.9 million adults aged ≥ 18 years had 1 or more anxiety disorders in the past year. That included 3.9 million with lower than a high school education, 3.3 million high school graduates, 2.8 million with some college, and 3 million with college education or higher.
In the past year, 12.9% of adults with lower than a high school education had anxiety disorders compared with 5% of high school graduates and 4.3% of adults with college degrees or higher levels of education.
Although the MHSS results cannot be used to determine whether anxiety stopped people from finishing high school, the research showed that having an anxiety disorder can lower the odds of finishing high school and attending college and reach past the school years into the health and well-being of later adulthood.
Adults with lower than a high school education are more than twice as likely to have experienced an anxiety disorder in the past year than those with higher levels of education, according to a study by the Substance Abuse and Mental Health Services Administration.
The National Survey on Drug Use and Health’s 2008 to 2012 Mental Health Surveillance Study (MHSS) found an estimated 12.9 million adults aged ≥ 18 years had 1 or more anxiety disorders in the past year. That included 3.9 million with lower than a high school education, 3.3 million high school graduates, 2.8 million with some college, and 3 million with college education or higher.
In the past year, 12.9% of adults with lower than a high school education had anxiety disorders compared with 5% of high school graduates and 4.3% of adults with college degrees or higher levels of education.
Although the MHSS results cannot be used to determine whether anxiety stopped people from finishing high school, the research showed that having an anxiety disorder can lower the odds of finishing high school and attending college and reach past the school years into the health and well-being of later adulthood.
Adults with lower than a high school education are more than twice as likely to have experienced an anxiety disorder in the past year than those with higher levels of education, according to a study by the Substance Abuse and Mental Health Services Administration.
The National Survey on Drug Use and Health’s 2008 to 2012 Mental Health Surveillance Study (MHSS) found an estimated 12.9 million adults aged ≥ 18 years had 1 or more anxiety disorders in the past year. That included 3.9 million with lower than a high school education, 3.3 million high school graduates, 2.8 million with some college, and 3 million with college education or higher.
In the past year, 12.9% of adults with lower than a high school education had anxiety disorders compared with 5% of high school graduates and 4.3% of adults with college degrees or higher levels of education.
Although the MHSS results cannot be used to determine whether anxiety stopped people from finishing high school, the research showed that having an anxiety disorder can lower the odds of finishing high school and attending college and reach past the school years into the health and well-being of later adulthood.