User login
Reducing Opioid Use for Chronic Pain
The VA Opioid Safety Initiative (OSI), launched last October in Minneapolis, Minnesota, to give veterans nonopioid options for pain management, is already having an impact. Eight OSI sites in Minnesota have reduced high-dose opioid use by more than 50%, the VA says.
The initiative’s pain management plan is multifaceted, including patient and provider education, testing and tapering programs, and alternative therapies, such as acupuncture and behavior therapy. It emphasizes close patient monitoring with frequent feedback.
The OSI is “an example of [Veteran Health Administration’s] personalized, proactive, and patient-centered approach to health care,” says VA Under Secretary for Health Dr. Robert Petzel. “We are delivering health care with the patient’s long-term personal health goals at the forefront.”
The VA offers a variety of supports, such as Pain Coach, a pain management mobile application for patients; Veterans’ Health Library, which includes a Patient/Family Management Toolkit; and resources for pain management on My HealtheVet. Each VA facility employs Interdisciplinary Pain Medicine Specialty Teams and Consult Services, Facility Pain Committees, and other professionals to help achieve the OSI goals.
The VA Opioid Safety Initiative (OSI), launched last October in Minneapolis, Minnesota, to give veterans nonopioid options for pain management, is already having an impact. Eight OSI sites in Minnesota have reduced high-dose opioid use by more than 50%, the VA says.
The initiative’s pain management plan is multifaceted, including patient and provider education, testing and tapering programs, and alternative therapies, such as acupuncture and behavior therapy. It emphasizes close patient monitoring with frequent feedback.
The OSI is “an example of [Veteran Health Administration’s] personalized, proactive, and patient-centered approach to health care,” says VA Under Secretary for Health Dr. Robert Petzel. “We are delivering health care with the patient’s long-term personal health goals at the forefront.”
The VA offers a variety of supports, such as Pain Coach, a pain management mobile application for patients; Veterans’ Health Library, which includes a Patient/Family Management Toolkit; and resources for pain management on My HealtheVet. Each VA facility employs Interdisciplinary Pain Medicine Specialty Teams and Consult Services, Facility Pain Committees, and other professionals to help achieve the OSI goals.
The VA Opioid Safety Initiative (OSI), launched last October in Minneapolis, Minnesota, to give veterans nonopioid options for pain management, is already having an impact. Eight OSI sites in Minnesota have reduced high-dose opioid use by more than 50%, the VA says.
The initiative’s pain management plan is multifaceted, including patient and provider education, testing and tapering programs, and alternative therapies, such as acupuncture and behavior therapy. It emphasizes close patient monitoring with frequent feedback.
The OSI is “an example of [Veteran Health Administration’s] personalized, proactive, and patient-centered approach to health care,” says VA Under Secretary for Health Dr. Robert Petzel. “We are delivering health care with the patient’s long-term personal health goals at the forefront.”
The VA offers a variety of supports, such as Pain Coach, a pain management mobile application for patients; Veterans’ Health Library, which includes a Patient/Family Management Toolkit; and resources for pain management on My HealtheVet. Each VA facility employs Interdisciplinary Pain Medicine Specialty Teams and Consult Services, Facility Pain Committees, and other professionals to help achieve the OSI goals.
Expanding Patients’ Rights
The HHS has taken steps to make it easier for patients to get access to laboratory test results. “The right to access personal health information is a cornerstone of the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule,” said HHS Secretary Kathleen Sebelius. “Information like lab results can empower patients to track their health progress, make decisions with their health care professionals, and adhere to important treatment plans.”
The final rule, announced in February 2014, changes the Clinical Laboratory Improvement Amendments (CLIA) of 1988 to allow laboratories to give a patient or person designated by the patient access to the laboratory reports. Previously, under CLIA regulations, a laboratory could only release completed test reports directly to a patient if (1) the ordering provider expressly authorized the lab to do so at the time the test was ordered; or (2) state law expressly allowed for it.
The HIPAA Privacy Rule also included an exception to a patient’s right of access for CLIA-certified or CLIA-exempt laboratories that were prohibited by law from providing such access. In the 26 states that lacked laws authorizing direct disclosure of test reports to patients and in the 13 states that expressly prohibited such access, patients did not have direct access to their test reports through CLIA laboratories. The new changes to the rule eliminate those exceptions.
Under the revised rule, patients, their designees, and their personal representatives can see or be given a copy of the patient’s protected health information, including an electronic copy, with limited exceptions. The patient or representative may have to put the request in writing and pay for copying, mailing, or electronic media on which the information is provided, such as a CD or flash drive. In most cases, the information must be provided to the patient within 30days of requesting it. The final rule is available for review at http://federalregister.gov.
The HHS has taken steps to make it easier for patients to get access to laboratory test results. “The right to access personal health information is a cornerstone of the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule,” said HHS Secretary Kathleen Sebelius. “Information like lab results can empower patients to track their health progress, make decisions with their health care professionals, and adhere to important treatment plans.”
The final rule, announced in February 2014, changes the Clinical Laboratory Improvement Amendments (CLIA) of 1988 to allow laboratories to give a patient or person designated by the patient access to the laboratory reports. Previously, under CLIA regulations, a laboratory could only release completed test reports directly to a patient if (1) the ordering provider expressly authorized the lab to do so at the time the test was ordered; or (2) state law expressly allowed for it.
The HIPAA Privacy Rule also included an exception to a patient’s right of access for CLIA-certified or CLIA-exempt laboratories that were prohibited by law from providing such access. In the 26 states that lacked laws authorizing direct disclosure of test reports to patients and in the 13 states that expressly prohibited such access, patients did not have direct access to their test reports through CLIA laboratories. The new changes to the rule eliminate those exceptions.
Under the revised rule, patients, their designees, and their personal representatives can see or be given a copy of the patient’s protected health information, including an electronic copy, with limited exceptions. The patient or representative may have to put the request in writing and pay for copying, mailing, or electronic media on which the information is provided, such as a CD or flash drive. In most cases, the information must be provided to the patient within 30days of requesting it. The final rule is available for review at http://federalregister.gov.
The HHS has taken steps to make it easier for patients to get access to laboratory test results. “The right to access personal health information is a cornerstone of the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule,” said HHS Secretary Kathleen Sebelius. “Information like lab results can empower patients to track their health progress, make decisions with their health care professionals, and adhere to important treatment plans.”
The final rule, announced in February 2014, changes the Clinical Laboratory Improvement Amendments (CLIA) of 1988 to allow laboratories to give a patient or person designated by the patient access to the laboratory reports. Previously, under CLIA regulations, a laboratory could only release completed test reports directly to a patient if (1) the ordering provider expressly authorized the lab to do so at the time the test was ordered; or (2) state law expressly allowed for it.
The HIPAA Privacy Rule also included an exception to a patient’s right of access for CLIA-certified or CLIA-exempt laboratories that were prohibited by law from providing such access. In the 26 states that lacked laws authorizing direct disclosure of test reports to patients and in the 13 states that expressly prohibited such access, patients did not have direct access to their test reports through CLIA laboratories. The new changes to the rule eliminate those exceptions.
Under the revised rule, patients, their designees, and their personal representatives can see or be given a copy of the patient’s protected health information, including an electronic copy, with limited exceptions. The patient or representative may have to put the request in writing and pay for copying, mailing, or electronic media on which the information is provided, such as a CD or flash drive. In most cases, the information must be provided to the patient within 30days of requesting it. The final rule is available for review at http://federalregister.gov.
New law averts SGR cut, delays ICD-10's debut
On April 1, President Obama officially halted the 24% Medicare physician pay cut when he signed into law a bill that provides a 12-month pay patch.
The legislation (H.R. 4302) replaces the scheduled fee cut with a 0.5% pay increase through the end of 2014. It then freezes payment levels for the first three months of 2015, giving Congress another year to figure out if it can pass legislation to permanently repeal Medicare's Sustainable Growth Rate (SGR) formula.
The biggest policy change is the one-year delay of the implementation of the ICD-10 coding sets, which had been scheduled to go into effect on Oct. 1, 2014. Under the recently passed law, the Department of Health & Human Services is barred from implementing the new coding sets until at least Oct. 1, 2015.
The delay was greeted with relief from most physician groups, which had already warned the government that many physicians, especially those in small practices, weren't ready to make the switch. But a coalition that includes health information technology companies, health plans, and the American Hospital Association decried the delay. The industry has already invested time and money in the switch, and a delay will cause only disruption, according to the Coalition for ICD-10.
The SGR legislation also further delays the full implementation of the two-midnight rule governing when Medicare patients should be admitted to the hospital versus placed under observation. Enforcement of the controversial policy by Recovery Audit Contractors (RACs) had already been delayed until Oct. 1, 2014. Under H.R. 4302, most postpayment claim audits by RACs are now delayed until March 31, 2015. However, RACs are allowed to perform audits in cases where there is evidence of systematic gaming, fraud, abuse, or delays in delivering care, according to the legislation.
The bill also includes a provision to target more aggressively potentially misvalued codes. For instance, it directs HHS to examine codes that
- have experienced the fastest growth
- have undergone substantial changes in practice expenses
- describe new technologies
- account for the majority of spending under the Physician Fee Schedule
- have high-cost supplies.
The bill sets a target for reducing misvalued services from 2017 through 2020 (0.5% of the estimated amount of the Fee Schedule spending). If the target is met, the savings are redistributed to other services in the Fee Schedule. However, if the target is not meet, payments are reduced. Cuts of 20% or more in a year will be phased in over a 2-year period, according to the legislation.
While primary care groups have been urging the government to shift payments toward cognitive services and away from procedural work for years, they said the bill's misvalued code provision is likely bad news for physicians.
The problem, said Norman E. Vinn, D.O., president of the American Osteopathic Association, is that it doesn't just redirect payments from one area to another but instead appears to cut payments to physicians across the board. "We agree with the goal, but not the method," said Dr. Reid Blackwelder, president of the American Academy of Family Physicians.
But physicians praised the bill's increased funding for mental health services. The bill funds a 2-year pilot project aimed at improving community mental health services and a grant program for assisted outpatient treatment for people with serious mental illness.
In the pilot project, which will include eight states, community behavior health clinics will certify that they have met certain standards, including offering 24-hour crisis management; screening assessments and diagnosis services; and outpatient mental health and substance abuse services. In exchange, they can qualify for higher federal matching funds through Medicaid.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
On April 1, President Obama officially halted the 24% Medicare physician pay cut when he signed into law a bill that provides a 12-month pay patch.
The legislation (H.R. 4302) replaces the scheduled fee cut with a 0.5% pay increase through the end of 2014. It then freezes payment levels for the first three months of 2015, giving Congress another year to figure out if it can pass legislation to permanently repeal Medicare's Sustainable Growth Rate (SGR) formula.
The biggest policy change is the one-year delay of the implementation of the ICD-10 coding sets, which had been scheduled to go into effect on Oct. 1, 2014. Under the recently passed law, the Department of Health & Human Services is barred from implementing the new coding sets until at least Oct. 1, 2015.
The delay was greeted with relief from most physician groups, which had already warned the government that many physicians, especially those in small practices, weren't ready to make the switch. But a coalition that includes health information technology companies, health plans, and the American Hospital Association decried the delay. The industry has already invested time and money in the switch, and a delay will cause only disruption, according to the Coalition for ICD-10.
The SGR legislation also further delays the full implementation of the two-midnight rule governing when Medicare patients should be admitted to the hospital versus placed under observation. Enforcement of the controversial policy by Recovery Audit Contractors (RACs) had already been delayed until Oct. 1, 2014. Under H.R. 4302, most postpayment claim audits by RACs are now delayed until March 31, 2015. However, RACs are allowed to perform audits in cases where there is evidence of systematic gaming, fraud, abuse, or delays in delivering care, according to the legislation.
The bill also includes a provision to target more aggressively potentially misvalued codes. For instance, it directs HHS to examine codes that
- have experienced the fastest growth
- have undergone substantial changes in practice expenses
- describe new technologies
- account for the majority of spending under the Physician Fee Schedule
- have high-cost supplies.
The bill sets a target for reducing misvalued services from 2017 through 2020 (0.5% of the estimated amount of the Fee Schedule spending). If the target is met, the savings are redistributed to other services in the Fee Schedule. However, if the target is not meet, payments are reduced. Cuts of 20% or more in a year will be phased in over a 2-year period, according to the legislation.
While primary care groups have been urging the government to shift payments toward cognitive services and away from procedural work for years, they said the bill's misvalued code provision is likely bad news for physicians.
The problem, said Norman E. Vinn, D.O., president of the American Osteopathic Association, is that it doesn't just redirect payments from one area to another but instead appears to cut payments to physicians across the board. "We agree with the goal, but not the method," said Dr. Reid Blackwelder, president of the American Academy of Family Physicians.
But physicians praised the bill's increased funding for mental health services. The bill funds a 2-year pilot project aimed at improving community mental health services and a grant program for assisted outpatient treatment for people with serious mental illness.
In the pilot project, which will include eight states, community behavior health clinics will certify that they have met certain standards, including offering 24-hour crisis management; screening assessments and diagnosis services; and outpatient mental health and substance abuse services. In exchange, they can qualify for higher federal matching funds through Medicaid.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
On April 1, President Obama officially halted the 24% Medicare physician pay cut when he signed into law a bill that provides a 12-month pay patch.
The legislation (H.R. 4302) replaces the scheduled fee cut with a 0.5% pay increase through the end of 2014. It then freezes payment levels for the first three months of 2015, giving Congress another year to figure out if it can pass legislation to permanently repeal Medicare's Sustainable Growth Rate (SGR) formula.
The biggest policy change is the one-year delay of the implementation of the ICD-10 coding sets, which had been scheduled to go into effect on Oct. 1, 2014. Under the recently passed law, the Department of Health & Human Services is barred from implementing the new coding sets until at least Oct. 1, 2015.
The delay was greeted with relief from most physician groups, which had already warned the government that many physicians, especially those in small practices, weren't ready to make the switch. But a coalition that includes health information technology companies, health plans, and the American Hospital Association decried the delay. The industry has already invested time and money in the switch, and a delay will cause only disruption, according to the Coalition for ICD-10.
The SGR legislation also further delays the full implementation of the two-midnight rule governing when Medicare patients should be admitted to the hospital versus placed under observation. Enforcement of the controversial policy by Recovery Audit Contractors (RACs) had already been delayed until Oct. 1, 2014. Under H.R. 4302, most postpayment claim audits by RACs are now delayed until March 31, 2015. However, RACs are allowed to perform audits in cases where there is evidence of systematic gaming, fraud, abuse, or delays in delivering care, according to the legislation.
The bill also includes a provision to target more aggressively potentially misvalued codes. For instance, it directs HHS to examine codes that
- have experienced the fastest growth
- have undergone substantial changes in practice expenses
- describe new technologies
- account for the majority of spending under the Physician Fee Schedule
- have high-cost supplies.
The bill sets a target for reducing misvalued services from 2017 through 2020 (0.5% of the estimated amount of the Fee Schedule spending). If the target is met, the savings are redistributed to other services in the Fee Schedule. However, if the target is not meet, payments are reduced. Cuts of 20% or more in a year will be phased in over a 2-year period, according to the legislation.
While primary care groups have been urging the government to shift payments toward cognitive services and away from procedural work for years, they said the bill's misvalued code provision is likely bad news for physicians.
The problem, said Norman E. Vinn, D.O., president of the American Osteopathic Association, is that it doesn't just redirect payments from one area to another but instead appears to cut payments to physicians across the board. "We agree with the goal, but not the method," said Dr. Reid Blackwelder, president of the American Academy of Family Physicians.
But physicians praised the bill's increased funding for mental health services. The bill funds a 2-year pilot project aimed at improving community mental health services and a grant program for assisted outpatient treatment for people with serious mental illness.
In the pilot project, which will include eight states, community behavior health clinics will certify that they have met certain standards, including offering 24-hour crisis management; screening assessments and diagnosis services; and outpatient mental health and substance abuse services. In exchange, they can qualify for higher federal matching funds through Medicaid.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Vaccine Agencies Consolidate for More Effectiveness
In response to the shift in focus of the Military Health System (MHS) from treating disease to preventing it, the Military Vaccine Agency (MILVAX) and Vaccine Healthcare Centers Network (VHCN) have joined to become 1 agency. As a single agency, MILVAX-VHCN says it will be better able to do more of what the 2 agencies have done separately in the past: provide expert consultation, educate and train, enhance safety surveillance and research, and implement communication activities. Regional support operations at more than a dozen sites have also been combined to reduce gaps and redundancies, the MHS said in a January 2, 2014, press release.
The move will have significance for more than 9 million beneficiaries worldwide, the MHS notes. Dr. Limone Collins, deputy director of clinical services, said the expansion will allow for a better use of resources, including doctors, nurses, and other health care personnel. Lt. Col. Jorge Carrillo, acting director of the MILVAX-VHCN, said the integration “also allows for an expanded and dedicated staff to focus on research and enhancing scientific understanding of vaccine safety and effectiveness.”
In response to the shift in focus of the Military Health System (MHS) from treating disease to preventing it, the Military Vaccine Agency (MILVAX) and Vaccine Healthcare Centers Network (VHCN) have joined to become 1 agency. As a single agency, MILVAX-VHCN says it will be better able to do more of what the 2 agencies have done separately in the past: provide expert consultation, educate and train, enhance safety surveillance and research, and implement communication activities. Regional support operations at more than a dozen sites have also been combined to reduce gaps and redundancies, the MHS said in a January 2, 2014, press release.
The move will have significance for more than 9 million beneficiaries worldwide, the MHS notes. Dr. Limone Collins, deputy director of clinical services, said the expansion will allow for a better use of resources, including doctors, nurses, and other health care personnel. Lt. Col. Jorge Carrillo, acting director of the MILVAX-VHCN, said the integration “also allows for an expanded and dedicated staff to focus on research and enhancing scientific understanding of vaccine safety and effectiveness.”
In response to the shift in focus of the Military Health System (MHS) from treating disease to preventing it, the Military Vaccine Agency (MILVAX) and Vaccine Healthcare Centers Network (VHCN) have joined to become 1 agency. As a single agency, MILVAX-VHCN says it will be better able to do more of what the 2 agencies have done separately in the past: provide expert consultation, educate and train, enhance safety surveillance and research, and implement communication activities. Regional support operations at more than a dozen sites have also been combined to reduce gaps and redundancies, the MHS said in a January 2, 2014, press release.
The move will have significance for more than 9 million beneficiaries worldwide, the MHS notes. Dr. Limone Collins, deputy director of clinical services, said the expansion will allow for a better use of resources, including doctors, nurses, and other health care personnel. Lt. Col. Jorge Carrillo, acting director of the MILVAX-VHCN, said the integration “also allows for an expanded and dedicated staff to focus on research and enhancing scientific understanding of vaccine safety and effectiveness.”
Getting Along With Electronic Technology—Safely
Not sure about the safety of electronic health information technology (IT)? To help health care practitioners get more comfortable with electronic health records (EHRs) and other products, the HHS is providing evidence-based Safety Assurance Factors for EHR Resilience (SAFER) Guides.
The guides “combine the latest applied knowledge of health IT safety with practical tools that will help providers…effectively assess and optimize the safety and safe use of EHR technology within their organizations,” said Jacob Reider, MD, chief medical officer at the HHS Office of the National Coordinator for Health Information Technology (ONC).
Developed by leading health IT safety and informatics researchers, the SAFER guides are based on the latest available evidence, expert opinion, stakeholder engagement, and field work. They complement existing health IT safety tools and research developed by the Agency for Healthcare Research and Quality and ONC.
Each guide contains self-assessment checklists, practice worksheets, and recommended practices. They address such topics as high-priority practices, patient identification, and reviewing and following up on test results. The guides are available as downloadable PDFs and as interactive Web-based tools at http://www.HealthIT.gov/saferguide.
Not sure about the safety of electronic health information technology (IT)? To help health care practitioners get more comfortable with electronic health records (EHRs) and other products, the HHS is providing evidence-based Safety Assurance Factors for EHR Resilience (SAFER) Guides.
The guides “combine the latest applied knowledge of health IT safety with practical tools that will help providers…effectively assess and optimize the safety and safe use of EHR technology within their organizations,” said Jacob Reider, MD, chief medical officer at the HHS Office of the National Coordinator for Health Information Technology (ONC).
Developed by leading health IT safety and informatics researchers, the SAFER guides are based on the latest available evidence, expert opinion, stakeholder engagement, and field work. They complement existing health IT safety tools and research developed by the Agency for Healthcare Research and Quality and ONC.
Each guide contains self-assessment checklists, practice worksheets, and recommended practices. They address such topics as high-priority practices, patient identification, and reviewing and following up on test results. The guides are available as downloadable PDFs and as interactive Web-based tools at http://www.HealthIT.gov/saferguide.
Not sure about the safety of electronic health information technology (IT)? To help health care practitioners get more comfortable with electronic health records (EHRs) and other products, the HHS is providing evidence-based Safety Assurance Factors for EHR Resilience (SAFER) Guides.
The guides “combine the latest applied knowledge of health IT safety with practical tools that will help providers…effectively assess and optimize the safety and safe use of EHR technology within their organizations,” said Jacob Reider, MD, chief medical officer at the HHS Office of the National Coordinator for Health Information Technology (ONC).
Developed by leading health IT safety and informatics researchers, the SAFER guides are based on the latest available evidence, expert opinion, stakeholder engagement, and field work. They complement existing health IT safety tools and research developed by the Agency for Healthcare Research and Quality and ONC.
Each guide contains self-assessment checklists, practice worksheets, and recommended practices. They address such topics as high-priority practices, patient identification, and reviewing and following up on test results. The guides are available as downloadable PDFs and as interactive Web-based tools at http://www.HealthIT.gov/saferguide.
Inpatient safety efforts yield mixed results
Adverse events decreased over the last decade for Medicare inpatients with acute myocardial infarction or heart failure but barely changed for those with pneumonia or conditions requiring surgery, according to an analysis of a Medicare database.
The improvements likely translated to 81,000 fewer adverse events for patients with acute MI (AMI) and heart failure (HF) from 2010 to 2011 alone, according to the study published Jan. 22 in the New England Journal of Medicine.
"Although this suggests that national efforts focused on patient safety have made some inroads, the lack of reductions across the board is disappointing," Yun Wang, Ph.D., of the Harvard School of Public Health, Boston, and his colleagues wrote.
The researchers examined whether hospitalized patients are any better off in light of the current focus on patient safety, including the launch of initiatives such as the American College of Surgeons’ National Surgical Quality Improvement Program and the federal government’s Surgical Infection Prevention Project.
They used three composite outcomes measures: the rate of occurrence for adverse events for which patients were at risk (for instance, only patients receiving warfarin were at risk for warfarin-related events); the proportion of patients with one or more adverse events; and the number of adverse events per 1,000 hospitalizations. They analyzed data on 61,523 patients who were discharged from 4,372 hospitals; the data were extracted from the Medicare Patient Safety Monitoring System database (N. Engl. J. Med. 2014:370;341-51).
The 61,523 patients included 11,399 with AMI, 15,374 with HF, 18,269 with pneumonia, and 16,481 with conditions requiring surgery. Postsurgical patients largely were being treated for joint replacement procedures and other osteoarthritis-related conditions, femur fracture, colon cancer, post-AMI procedures, or other forms of chronic ischemic heart disease.
From 2005-2006 to 2010-2011, AMI and HF patients saw a 1.3 percentage point decline in the rate of adverse events, from 5% to 3.7%. The proportion who had one or more such events decreased from 26% to 19%. The number of adverse events per 1,000 hospitalizations declined from 402 to 262 for AMI patients and from 235 to 167 for HF patients.
Infection-related and drug-related adverse events declined significantly in heart attack and HF patients. There was also a substantial improvement in postprocedure events in HF patients.
Postsurgical patients experienced slight increases in all three outcomes measures, in particular, increases in infection-related and postprocedural events such as venous thromboembolism, and cardiac and catheter-related events. The number of events per 1,000 hospitalizations for pneumonia patients increased insignificantly from 216 to 223. For postsurgical patients, the number of events increased insignificantly from 352/1,000 to 368/1,000.
Patients who had adverse events had significantly longer hospital stays and were at higher risk for death. As the number of adverse events increased, so did the risk of death.
The authors noted that declines in events for AMI and HF patients might be a reflection of the numerous efforts and initiatives to improve care in those two conditions.
But they also found that concerted efforts to improve safety did not necessarily work. There was an increase in pressure ulcers in postsurgical patients, and no decline in ventilator-associated pneumonia in most patients, even though there have been initiatives focused on those conditions.
"Our finding of an increased adverse-event rate among surgical patients indicates a continuing challenge and identifies an important target for patient-safety initiatives," the researchers said.
The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Several researchers were associated with Qualidigm, a consultancy that administers the Medicare database. No other relevant conflicts of interest were disclosed.
On Twitter @aliciaault
Adverse events decreased over the last decade for Medicare inpatients with acute myocardial infarction or heart failure but barely changed for those with pneumonia or conditions requiring surgery, according to an analysis of a Medicare database.
The improvements likely translated to 81,000 fewer adverse events for patients with acute MI (AMI) and heart failure (HF) from 2010 to 2011 alone, according to the study published Jan. 22 in the New England Journal of Medicine.
"Although this suggests that national efforts focused on patient safety have made some inroads, the lack of reductions across the board is disappointing," Yun Wang, Ph.D., of the Harvard School of Public Health, Boston, and his colleagues wrote.
The researchers examined whether hospitalized patients are any better off in light of the current focus on patient safety, including the launch of initiatives such as the American College of Surgeons’ National Surgical Quality Improvement Program and the federal government’s Surgical Infection Prevention Project.
They used three composite outcomes measures: the rate of occurrence for adverse events for which patients were at risk (for instance, only patients receiving warfarin were at risk for warfarin-related events); the proportion of patients with one or more adverse events; and the number of adverse events per 1,000 hospitalizations. They analyzed data on 61,523 patients who were discharged from 4,372 hospitals; the data were extracted from the Medicare Patient Safety Monitoring System database (N. Engl. J. Med. 2014:370;341-51).
The 61,523 patients included 11,399 with AMI, 15,374 with HF, 18,269 with pneumonia, and 16,481 with conditions requiring surgery. Postsurgical patients largely were being treated for joint replacement procedures and other osteoarthritis-related conditions, femur fracture, colon cancer, post-AMI procedures, or other forms of chronic ischemic heart disease.
From 2005-2006 to 2010-2011, AMI and HF patients saw a 1.3 percentage point decline in the rate of adverse events, from 5% to 3.7%. The proportion who had one or more such events decreased from 26% to 19%. The number of adverse events per 1,000 hospitalizations declined from 402 to 262 for AMI patients and from 235 to 167 for HF patients.
Infection-related and drug-related adverse events declined significantly in heart attack and HF patients. There was also a substantial improvement in postprocedure events in HF patients.
Postsurgical patients experienced slight increases in all three outcomes measures, in particular, increases in infection-related and postprocedural events such as venous thromboembolism, and cardiac and catheter-related events. The number of events per 1,000 hospitalizations for pneumonia patients increased insignificantly from 216 to 223. For postsurgical patients, the number of events increased insignificantly from 352/1,000 to 368/1,000.
Patients who had adverse events had significantly longer hospital stays and were at higher risk for death. As the number of adverse events increased, so did the risk of death.
The authors noted that declines in events for AMI and HF patients might be a reflection of the numerous efforts and initiatives to improve care in those two conditions.
But they also found that concerted efforts to improve safety did not necessarily work. There was an increase in pressure ulcers in postsurgical patients, and no decline in ventilator-associated pneumonia in most patients, even though there have been initiatives focused on those conditions.
"Our finding of an increased adverse-event rate among surgical patients indicates a continuing challenge and identifies an important target for patient-safety initiatives," the researchers said.
The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Several researchers were associated with Qualidigm, a consultancy that administers the Medicare database. No other relevant conflicts of interest were disclosed.
On Twitter @aliciaault
Adverse events decreased over the last decade for Medicare inpatients with acute myocardial infarction or heart failure but barely changed for those with pneumonia or conditions requiring surgery, according to an analysis of a Medicare database.
The improvements likely translated to 81,000 fewer adverse events for patients with acute MI (AMI) and heart failure (HF) from 2010 to 2011 alone, according to the study published Jan. 22 in the New England Journal of Medicine.
"Although this suggests that national efforts focused on patient safety have made some inroads, the lack of reductions across the board is disappointing," Yun Wang, Ph.D., of the Harvard School of Public Health, Boston, and his colleagues wrote.
The researchers examined whether hospitalized patients are any better off in light of the current focus on patient safety, including the launch of initiatives such as the American College of Surgeons’ National Surgical Quality Improvement Program and the federal government’s Surgical Infection Prevention Project.
They used three composite outcomes measures: the rate of occurrence for adverse events for which patients were at risk (for instance, only patients receiving warfarin were at risk for warfarin-related events); the proportion of patients with one or more adverse events; and the number of adverse events per 1,000 hospitalizations. They analyzed data on 61,523 patients who were discharged from 4,372 hospitals; the data were extracted from the Medicare Patient Safety Monitoring System database (N. Engl. J. Med. 2014:370;341-51).
The 61,523 patients included 11,399 with AMI, 15,374 with HF, 18,269 with pneumonia, and 16,481 with conditions requiring surgery. Postsurgical patients largely were being treated for joint replacement procedures and other osteoarthritis-related conditions, femur fracture, colon cancer, post-AMI procedures, or other forms of chronic ischemic heart disease.
From 2005-2006 to 2010-2011, AMI and HF patients saw a 1.3 percentage point decline in the rate of adverse events, from 5% to 3.7%. The proportion who had one or more such events decreased from 26% to 19%. The number of adverse events per 1,000 hospitalizations declined from 402 to 262 for AMI patients and from 235 to 167 for HF patients.
Infection-related and drug-related adverse events declined significantly in heart attack and HF patients. There was also a substantial improvement in postprocedure events in HF patients.
Postsurgical patients experienced slight increases in all three outcomes measures, in particular, increases in infection-related and postprocedural events such as venous thromboembolism, and cardiac and catheter-related events. The number of events per 1,000 hospitalizations for pneumonia patients increased insignificantly from 216 to 223. For postsurgical patients, the number of events increased insignificantly from 352/1,000 to 368/1,000.
Patients who had adverse events had significantly longer hospital stays and were at higher risk for death. As the number of adverse events increased, so did the risk of death.
The authors noted that declines in events for AMI and HF patients might be a reflection of the numerous efforts and initiatives to improve care in those two conditions.
But they also found that concerted efforts to improve safety did not necessarily work. There was an increase in pressure ulcers in postsurgical patients, and no decline in ventilator-associated pneumonia in most patients, even though there have been initiatives focused on those conditions.
"Our finding of an increased adverse-event rate among surgical patients indicates a continuing challenge and identifies an important target for patient-safety initiatives," the researchers said.
The study was supported by the Agency for Healthcare Research and Quality as well as academic and federal grants. Several researchers were associated with Qualidigm, a consultancy that administers the Medicare database. No other relevant conflicts of interest were disclosed.
On Twitter @aliciaault
Physician Compare site adds quality scores
Physician Compare, Medicare's online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations. The site displays how a group of physicians performed on five quality indicators related to management of diabetes and heart disease. The website will display the ratings using stars, as well as the percentage score.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare & Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares the CMS's strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, the CMS is posting quality data from 66 group practices and 141 ACOs. The data are reported at the group practice and ACO level. The quality measures include:
- Controlling hemoglobin A1c in patients with diabetes.
- Controlling blood pressure in patients with diabetes.
- Prescribing aspirin to patients with diabetes and heart disease.
- Reporting the number of diabetic patients who do not use tobacco.
- Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
Physician Compare, Medicare's online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations. The site displays how a group of physicians performed on five quality indicators related to management of diabetes and heart disease. The website will display the ratings using stars, as well as the percentage score.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare & Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares the CMS's strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, the CMS is posting quality data from 66 group practices and 141 ACOs. The data are reported at the group practice and ACO level. The quality measures include:
- Controlling hemoglobin A1c in patients with diabetes.
- Controlling blood pressure in patients with diabetes.
- Prescribing aspirin to patients with diabetes and heart disease.
- Reporting the number of diabetic patients who do not use tobacco.
- Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
Physician Compare, Medicare's online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations. The site displays how a group of physicians performed on five quality indicators related to management of diabetes and heart disease. The website will display the ratings using stars, as well as the percentage score.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare & Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares the CMS's strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, the CMS is posting quality data from 66 group practices and 141 ACOs. The data are reported at the group practice and ACO level. The quality measures include:
- Controlling hemoglobin A1c in patients with diabetes.
- Controlling blood pressure in patients with diabetes.
- Prescribing aspirin to patients with diabetes and heart disease.
- Reporting the number of diabetic patients who do not use tobacco.
- Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
New HAI reduction targets proposed
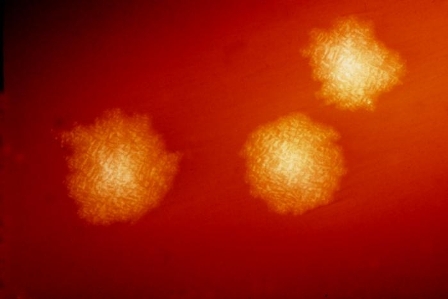
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
- Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
- Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
- Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
- Reduce facility-onset MRSA by 50% from the 2015 baseline.
- Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
- Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
- Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
- Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
- Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
- Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
- Reduce facility-onset MRSA by 50% from the 2015 baseline.
- Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
- Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
- Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
- Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
- Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
- Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
- Reduce facility-onset MRSA by 50% from the 2015 baseline.
- Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
- Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
- Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Making Community Living a Reality for More Americans
In 2009, the HHS Community Living Initiative (CLI) was launched (as part of the Affordable Care Act) to develop and implement innovative strategies to increase opportunities for Americans with disabilities and older adults to “enjoy meaningful community living.” To that end, the Centers for Medicare & Medicaid Services (CMS) recently issued a final rule that ensures that Medicaid home and community-based services (HCBS) programs provide full access to the benefits of community living. “People with disabilities and older adults have a right to live, work, and participate in the greater community. The HHS, through its Community Living Initiative, has been expanding and improving the community services necessary to make this a reality,” said HHS Secretary Kathleen Sebelius. The final rule was developed from discussions with stakeholders, states, and federal partners about the qualities of community-based settings that distinguish them from institutional settings.
The CMS says it is moving away from defining HCBS settings by “what they are not” and toward defining them by the nature and quality of individuals’ experiences. That includes establishing a more outcome-oriented definition of HCBS settings, according to the HHS.
The CLI supports inclusive, sustainable, and transparent programs. The rule specifies that service planning for participants in certain Medicaid HCBS programs must be developed through a “person-centered” process that addresses health and long-term services and support needs in a “manner that reflects individual preferences and goals.” For example, it requires that all HCBS settings are integrated into and support full access to the greater community, that the patient is allowed to choose from among setting options, and that it optimizes autonomy and independence in making life choices.
The final rule includes a transitional period for states to ensure their programs meet the HCBS settings requirements. Technical assistance will also be available for states. For more information regarding HCBS available under Medicaid, visit http://www.medicaid.gov/HCBS. For more information regarding the CLI, visit http://www.hhs.gov/od/community.
In 2009, the HHS Community Living Initiative (CLI) was launched (as part of the Affordable Care Act) to develop and implement innovative strategies to increase opportunities for Americans with disabilities and older adults to “enjoy meaningful community living.” To that end, the Centers for Medicare & Medicaid Services (CMS) recently issued a final rule that ensures that Medicaid home and community-based services (HCBS) programs provide full access to the benefits of community living. “People with disabilities and older adults have a right to live, work, and participate in the greater community. The HHS, through its Community Living Initiative, has been expanding and improving the community services necessary to make this a reality,” said HHS Secretary Kathleen Sebelius. The final rule was developed from discussions with stakeholders, states, and federal partners about the qualities of community-based settings that distinguish them from institutional settings.
The CMS says it is moving away from defining HCBS settings by “what they are not” and toward defining them by the nature and quality of individuals’ experiences. That includes establishing a more outcome-oriented definition of HCBS settings, according to the HHS.
The CLI supports inclusive, sustainable, and transparent programs. The rule specifies that service planning for participants in certain Medicaid HCBS programs must be developed through a “person-centered” process that addresses health and long-term services and support needs in a “manner that reflects individual preferences and goals.” For example, it requires that all HCBS settings are integrated into and support full access to the greater community, that the patient is allowed to choose from among setting options, and that it optimizes autonomy and independence in making life choices.
The final rule includes a transitional period for states to ensure their programs meet the HCBS settings requirements. Technical assistance will also be available for states. For more information regarding HCBS available under Medicaid, visit http://www.medicaid.gov/HCBS. For more information regarding the CLI, visit http://www.hhs.gov/od/community.
In 2009, the HHS Community Living Initiative (CLI) was launched (as part of the Affordable Care Act) to develop and implement innovative strategies to increase opportunities for Americans with disabilities and older adults to “enjoy meaningful community living.” To that end, the Centers for Medicare & Medicaid Services (CMS) recently issued a final rule that ensures that Medicaid home and community-based services (HCBS) programs provide full access to the benefits of community living. “People with disabilities and older adults have a right to live, work, and participate in the greater community. The HHS, through its Community Living Initiative, has been expanding and improving the community services necessary to make this a reality,” said HHS Secretary Kathleen Sebelius. The final rule was developed from discussions with stakeholders, states, and federal partners about the qualities of community-based settings that distinguish them from institutional settings.
The CMS says it is moving away from defining HCBS settings by “what they are not” and toward defining them by the nature and quality of individuals’ experiences. That includes establishing a more outcome-oriented definition of HCBS settings, according to the HHS.
The CLI supports inclusive, sustainable, and transparent programs. The rule specifies that service planning for participants in certain Medicaid HCBS programs must be developed through a “person-centered” process that addresses health and long-term services and support needs in a “manner that reflects individual preferences and goals.” For example, it requires that all HCBS settings are integrated into and support full access to the greater community, that the patient is allowed to choose from among setting options, and that it optimizes autonomy and independence in making life choices.
The final rule includes a transitional period for states to ensure their programs meet the HCBS settings requirements. Technical assistance will also be available for states. For more information regarding HCBS available under Medicaid, visit http://www.medicaid.gov/HCBS. For more information regarding the CLI, visit http://www.hhs.gov/od/community.
U.S. Army Suicides Decline
Thanks in part to the U.S. Army’s Ready and Resilient Campaign (R2C), launched a year ago, fewer soldiers committed suicide in 2013, compared with 2012, said U.S. Army Deputy Chief of Staff Lt. Gen. Howard B. Bromberg: 301, vs 325 suicides in the active U.S. Army, Army National Guard, and Army Reserve.
The R2C is intended to “instill a cultural change in the Army by directly linking personal resilience to readiness.” The R2C promotes the development of a healthy mind-set and behavior through healthful lifestyles. It was designed to help integrate and synchronize multiple armed forces programs aimed at improving physical, psychological, and emotional health. R2C also includes the Comprehensive Soldier and Family Fitness Program (CSF2), which stresses strengthening of the entire family unit.
The R2C aims to reduce barriers and stigma associated with seeking help. “I am optimistic that more soldiers are seeking help and learning ways to address and cope with issues they may have,” Lt. Gen. Bromberg said in an Army News Service interview published on February 3, 2014. “I am very encouraged that we have hit a turning point where people are really talking about behavioral health. It’s OK to have problems, but it’s what you do about those problems…that is what’s really important.”
The U.S. Army has also expanded access to behavioral health services and increased pre- and postdeployment screenings to improve diagnosis and treatment. The R2C reviews programs, processes, and policies to ensure effectiveness and reduce redundancies. It also emphasizes the responsibility of people at all levels to “build and maintain resilience,” from helping commanders understand high-risk behaviors so they can intervene early, to supporting efforts to reduce hazing, bullying, and sexual assault.
Thanks in part to the U.S. Army’s Ready and Resilient Campaign (R2C), launched a year ago, fewer soldiers committed suicide in 2013, compared with 2012, said U.S. Army Deputy Chief of Staff Lt. Gen. Howard B. Bromberg: 301, vs 325 suicides in the active U.S. Army, Army National Guard, and Army Reserve.
The R2C is intended to “instill a cultural change in the Army by directly linking personal resilience to readiness.” The R2C promotes the development of a healthy mind-set and behavior through healthful lifestyles. It was designed to help integrate and synchronize multiple armed forces programs aimed at improving physical, psychological, and emotional health. R2C also includes the Comprehensive Soldier and Family Fitness Program (CSF2), which stresses strengthening of the entire family unit.
The R2C aims to reduce barriers and stigma associated with seeking help. “I am optimistic that more soldiers are seeking help and learning ways to address and cope with issues they may have,” Lt. Gen. Bromberg said in an Army News Service interview published on February 3, 2014. “I am very encouraged that we have hit a turning point where people are really talking about behavioral health. It’s OK to have problems, but it’s what you do about those problems…that is what’s really important.”
The U.S. Army has also expanded access to behavioral health services and increased pre- and postdeployment screenings to improve diagnosis and treatment. The R2C reviews programs, processes, and policies to ensure effectiveness and reduce redundancies. It also emphasizes the responsibility of people at all levels to “build and maintain resilience,” from helping commanders understand high-risk behaviors so they can intervene early, to supporting efforts to reduce hazing, bullying, and sexual assault.
Thanks in part to the U.S. Army’s Ready and Resilient Campaign (R2C), launched a year ago, fewer soldiers committed suicide in 2013, compared with 2012, said U.S. Army Deputy Chief of Staff Lt. Gen. Howard B. Bromberg: 301, vs 325 suicides in the active U.S. Army, Army National Guard, and Army Reserve.
The R2C is intended to “instill a cultural change in the Army by directly linking personal resilience to readiness.” The R2C promotes the development of a healthy mind-set and behavior through healthful lifestyles. It was designed to help integrate and synchronize multiple armed forces programs aimed at improving physical, psychological, and emotional health. R2C also includes the Comprehensive Soldier and Family Fitness Program (CSF2), which stresses strengthening of the entire family unit.
The R2C aims to reduce barriers and stigma associated with seeking help. “I am optimistic that more soldiers are seeking help and learning ways to address and cope with issues they may have,” Lt. Gen. Bromberg said in an Army News Service interview published on February 3, 2014. “I am very encouraged that we have hit a turning point where people are really talking about behavioral health. It’s OK to have problems, but it’s what you do about those problems…that is what’s really important.”
The U.S. Army has also expanded access to behavioral health services and increased pre- and postdeployment screenings to improve diagnosis and treatment. The R2C reviews programs, processes, and policies to ensure effectiveness and reduce redundancies. It also emphasizes the responsibility of people at all levels to “build and maintain resilience,” from helping commanders understand high-risk behaviors so they can intervene early, to supporting efforts to reduce hazing, bullying, and sexual assault.