User login
ICD-10 delay: Proceed with caution, experts advise
When it comes to ICD-10 readiness, invest in low-cost, high-impact steps that will benefit the October 2015 switch to new code set, but will also improve the general health of the medical practice.
Now that implementation of ICD-10 has been delayed a full year, "I’d avoid spending too much money at this stage," said Robert Tennant, senior policy advisor at the Medical Group Management Association (MGMA).
Practical steps include checking claims already paid under ICD-9 to see whether the documentation was sufficient to assign an ICD-10 code. In the case of a sprained wrist, for example, make sure the documentation includes whether the injury was to the left or right wrist, Mr. Tennant said.
Consider dual coding – coding the same claims in both ICD-9 and ICD-10 – for some most commonly used codes, Mr. Tennant advised. If you "go through the clinical documentation improvement exercises, you will produce a better quality medical record and that can help the practice in a number of ways even if ICD-10 never goes forward."
Other low-cost, high-impact steps include reaching out to clearinghouses to request reports on the practice’s top diagnosis codes, the top pended or rejected claims, and the most frequently used unspecified codes.
"That should really focus the practice in on those claims that are the most problematic," he said.
One tough decision is when to upgrade software. Upgrade too early and the practice could lose money if there’s another delay. Wait too long and the practice risks being unprepared for the compliance date, Mr. Tennant said.
He advised finding out when the vendor will be ready with upgrades and how long it will take them to install the software and provide training. Use that to build an implementation timeline.
"It’s such a tightrope that practices have to walk," Mr. Tennant said.
Dallas-based pediatrician Joseph Schneider has been helping physicians prepare for ICD-10 in his role as chair of the Texas Medical Association’s Practice Management Services Council. The association’s official policy is that the move to ICD-10 should be scrapped, but the group is urging physicians and hospitals to prepare anyway.
Dr. Schneider said smaller practices should check in with payers, vendors, and clearinghouses now, but save significant investments and training for next year.
"If you’re in a small physician practice, probably doing not very much between now and December might be a pretty good strategy," he said. "From January forward, you have to start your engines and get everything ready."
But larger practices and health systems don’t have the luxury of waiting, he said.
Dr. George Abraham, who is part of a six-physician practice in Worcester, Mass., was ready for ICD-10 to take effect this year. His practice spent more than $25,000 preparing for the scheduled switch and had done some initial testing of systems when the delay was announced.
Now the practice faces an additional expenditure on upgrades and refresher courses for coders and physicians.
"After everything, poof, it’s gone in a puff of smoke because everything came to a standstill when ICD-10 got suspended for a year," said Dr. Abraham, governor of the Massachusetts chapter of the American College of Physicians. "It will be déjà vu all over again come summer of next year. We’ll be doing the same thing in preparation for ICD-10 being rolled out in October 2015."
Most health plans won’t begin end-to-end testing of claims until next year, Dr. Abraham said, and that’s worrisome because it may not provide enough time to work out potential glitches.
"A delay in claims being processed is our biggest anxiety," he said. "A delay in payments will lead to a severe cash flow crunch."
Waiting on the CMS for ICD-10 details
Few details have emerged from the Centers for Medicare & Medicaid Services since Congress delayed the implementation of the ICD-10 coding system earlier this year.
As part of Protecting Access to Medicare Act of 2014 (H.R. 4302), Congress delayed implementation of ICD-10 for at least a year. In May, CMS officials announced that the new compliance date would be Oct. 1, 2015, and that physicians and hospitals must continue to use ICD-9 through Sept. 30, 2015.
The agency said it would release an interim final rule in the "near future" with additional details about the compliance date.
Since then, the CMS canceled the end-to-end system testing that had been scheduled for July. The testing will be held sometime in 2015 instead, according to the agency.
But the CMS did report on results of acknowledgement testing conducted with Medicare fee-for-service contractors in March. During the test, providers, suppliers, billing companies, and clearinghouses sent more than 127,000 claims with ICD-10 codes to the Medicare fee-for-service claims system. They received an electronic acknowledgement if their claims were accepted. The exercise did not test whether the claims test had sufficient documentation to be paid by Medicare.
Overall, the CMS accepted 89% of the test claims, below the normal average Medicare claims acceptance rates of 95% to 98%.
Negative testing – the purposeful submission of error-filled claims to force a rejection – could be one reason for the lower acceptance rate, according to Niall Brennan, acting director of the CMS Offices of Enterprise Management.
While physicians and other providers can submit claims for acknowledgement testing anytime up to the implementation date, Mr. Brennan recommended waiting until after Oct. 6, 2014, when Medicare updates its systems.
Physicians should contact their local Medicare Administrative Contractor for information on acknowledgement testing, according to the CMS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
When it comes to ICD-10 readiness, invest in low-cost, high-impact steps that will benefit the October 2015 switch to new code set, but will also improve the general health of the medical practice.
Now that implementation of ICD-10 has been delayed a full year, "I’d avoid spending too much money at this stage," said Robert Tennant, senior policy advisor at the Medical Group Management Association (MGMA).
Practical steps include checking claims already paid under ICD-9 to see whether the documentation was sufficient to assign an ICD-10 code. In the case of a sprained wrist, for example, make sure the documentation includes whether the injury was to the left or right wrist, Mr. Tennant said.
Consider dual coding – coding the same claims in both ICD-9 and ICD-10 – for some most commonly used codes, Mr. Tennant advised. If you "go through the clinical documentation improvement exercises, you will produce a better quality medical record and that can help the practice in a number of ways even if ICD-10 never goes forward."
Other low-cost, high-impact steps include reaching out to clearinghouses to request reports on the practice’s top diagnosis codes, the top pended or rejected claims, and the most frequently used unspecified codes.
"That should really focus the practice in on those claims that are the most problematic," he said.
One tough decision is when to upgrade software. Upgrade too early and the practice could lose money if there’s another delay. Wait too long and the practice risks being unprepared for the compliance date, Mr. Tennant said.
He advised finding out when the vendor will be ready with upgrades and how long it will take them to install the software and provide training. Use that to build an implementation timeline.
"It’s such a tightrope that practices have to walk," Mr. Tennant said.
Dallas-based pediatrician Joseph Schneider has been helping physicians prepare for ICD-10 in his role as chair of the Texas Medical Association’s Practice Management Services Council. The association’s official policy is that the move to ICD-10 should be scrapped, but the group is urging physicians and hospitals to prepare anyway.
Dr. Schneider said smaller practices should check in with payers, vendors, and clearinghouses now, but save significant investments and training for next year.
"If you’re in a small physician practice, probably doing not very much between now and December might be a pretty good strategy," he said. "From January forward, you have to start your engines and get everything ready."
But larger practices and health systems don’t have the luxury of waiting, he said.
Dr. George Abraham, who is part of a six-physician practice in Worcester, Mass., was ready for ICD-10 to take effect this year. His practice spent more than $25,000 preparing for the scheduled switch and had done some initial testing of systems when the delay was announced.
Now the practice faces an additional expenditure on upgrades and refresher courses for coders and physicians.
"After everything, poof, it’s gone in a puff of smoke because everything came to a standstill when ICD-10 got suspended for a year," said Dr. Abraham, governor of the Massachusetts chapter of the American College of Physicians. "It will be déjà vu all over again come summer of next year. We’ll be doing the same thing in preparation for ICD-10 being rolled out in October 2015."
Most health plans won’t begin end-to-end testing of claims until next year, Dr. Abraham said, and that’s worrisome because it may not provide enough time to work out potential glitches.
"A delay in claims being processed is our biggest anxiety," he said. "A delay in payments will lead to a severe cash flow crunch."
Waiting on the CMS for ICD-10 details
Few details have emerged from the Centers for Medicare & Medicaid Services since Congress delayed the implementation of the ICD-10 coding system earlier this year.
As part of Protecting Access to Medicare Act of 2014 (H.R. 4302), Congress delayed implementation of ICD-10 for at least a year. In May, CMS officials announced that the new compliance date would be Oct. 1, 2015, and that physicians and hospitals must continue to use ICD-9 through Sept. 30, 2015.
The agency said it would release an interim final rule in the "near future" with additional details about the compliance date.
Since then, the CMS canceled the end-to-end system testing that had been scheduled for July. The testing will be held sometime in 2015 instead, according to the agency.
But the CMS did report on results of acknowledgement testing conducted with Medicare fee-for-service contractors in March. During the test, providers, suppliers, billing companies, and clearinghouses sent more than 127,000 claims with ICD-10 codes to the Medicare fee-for-service claims system. They received an electronic acknowledgement if their claims were accepted. The exercise did not test whether the claims test had sufficient documentation to be paid by Medicare.
Overall, the CMS accepted 89% of the test claims, below the normal average Medicare claims acceptance rates of 95% to 98%.
Negative testing – the purposeful submission of error-filled claims to force a rejection – could be one reason for the lower acceptance rate, according to Niall Brennan, acting director of the CMS Offices of Enterprise Management.
While physicians and other providers can submit claims for acknowledgement testing anytime up to the implementation date, Mr. Brennan recommended waiting until after Oct. 6, 2014, when Medicare updates its systems.
Physicians should contact their local Medicare Administrative Contractor for information on acknowledgement testing, according to the CMS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
When it comes to ICD-10 readiness, invest in low-cost, high-impact steps that will benefit the October 2015 switch to new code set, but will also improve the general health of the medical practice.
Now that implementation of ICD-10 has been delayed a full year, "I’d avoid spending too much money at this stage," said Robert Tennant, senior policy advisor at the Medical Group Management Association (MGMA).
Practical steps include checking claims already paid under ICD-9 to see whether the documentation was sufficient to assign an ICD-10 code. In the case of a sprained wrist, for example, make sure the documentation includes whether the injury was to the left or right wrist, Mr. Tennant said.
Consider dual coding – coding the same claims in both ICD-9 and ICD-10 – for some most commonly used codes, Mr. Tennant advised. If you "go through the clinical documentation improvement exercises, you will produce a better quality medical record and that can help the practice in a number of ways even if ICD-10 never goes forward."
Other low-cost, high-impact steps include reaching out to clearinghouses to request reports on the practice’s top diagnosis codes, the top pended or rejected claims, and the most frequently used unspecified codes.
"That should really focus the practice in on those claims that are the most problematic," he said.
One tough decision is when to upgrade software. Upgrade too early and the practice could lose money if there’s another delay. Wait too long and the practice risks being unprepared for the compliance date, Mr. Tennant said.
He advised finding out when the vendor will be ready with upgrades and how long it will take them to install the software and provide training. Use that to build an implementation timeline.
"It’s such a tightrope that practices have to walk," Mr. Tennant said.
Dallas-based pediatrician Joseph Schneider has been helping physicians prepare for ICD-10 in his role as chair of the Texas Medical Association’s Practice Management Services Council. The association’s official policy is that the move to ICD-10 should be scrapped, but the group is urging physicians and hospitals to prepare anyway.
Dr. Schneider said smaller practices should check in with payers, vendors, and clearinghouses now, but save significant investments and training for next year.
"If you’re in a small physician practice, probably doing not very much between now and December might be a pretty good strategy," he said. "From January forward, you have to start your engines and get everything ready."
But larger practices and health systems don’t have the luxury of waiting, he said.
Dr. George Abraham, who is part of a six-physician practice in Worcester, Mass., was ready for ICD-10 to take effect this year. His practice spent more than $25,000 preparing for the scheduled switch and had done some initial testing of systems when the delay was announced.
Now the practice faces an additional expenditure on upgrades and refresher courses for coders and physicians.
"After everything, poof, it’s gone in a puff of smoke because everything came to a standstill when ICD-10 got suspended for a year," said Dr. Abraham, governor of the Massachusetts chapter of the American College of Physicians. "It will be déjà vu all over again come summer of next year. We’ll be doing the same thing in preparation for ICD-10 being rolled out in October 2015."
Most health plans won’t begin end-to-end testing of claims until next year, Dr. Abraham said, and that’s worrisome because it may not provide enough time to work out potential glitches.
"A delay in claims being processed is our biggest anxiety," he said. "A delay in payments will lead to a severe cash flow crunch."
Waiting on the CMS for ICD-10 details
Few details have emerged from the Centers for Medicare & Medicaid Services since Congress delayed the implementation of the ICD-10 coding system earlier this year.
As part of Protecting Access to Medicare Act of 2014 (H.R. 4302), Congress delayed implementation of ICD-10 for at least a year. In May, CMS officials announced that the new compliance date would be Oct. 1, 2015, and that physicians and hospitals must continue to use ICD-9 through Sept. 30, 2015.
The agency said it would release an interim final rule in the "near future" with additional details about the compliance date.
Since then, the CMS canceled the end-to-end system testing that had been scheduled for July. The testing will be held sometime in 2015 instead, according to the agency.
But the CMS did report on results of acknowledgement testing conducted with Medicare fee-for-service contractors in March. During the test, providers, suppliers, billing companies, and clearinghouses sent more than 127,000 claims with ICD-10 codes to the Medicare fee-for-service claims system. They received an electronic acknowledgement if their claims were accepted. The exercise did not test whether the claims test had sufficient documentation to be paid by Medicare.
Overall, the CMS accepted 89% of the test claims, below the normal average Medicare claims acceptance rates of 95% to 98%.
Negative testing – the purposeful submission of error-filled claims to force a rejection – could be one reason for the lower acceptance rate, according to Niall Brennan, acting director of the CMS Offices of Enterprise Management.
While physicians and other providers can submit claims for acknowledgement testing anytime up to the implementation date, Mr. Brennan recommended waiting until after Oct. 6, 2014, when Medicare updates its systems.
Physicians should contact their local Medicare Administrative Contractor for information on acknowledgement testing, according to the CMS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
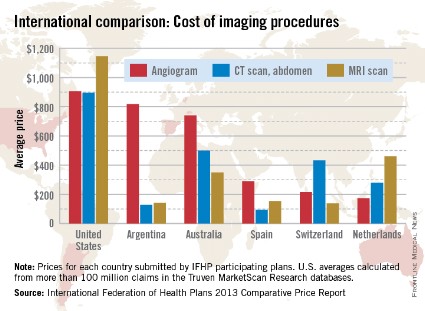
Imaging procedure costs higher in the United States
When it comes to diagnostic imaging, the average costs of angiograms, abdominal CTs, and MRIs are higher in the United States than in other industrialized countries, according to the International Federation of Health Plans’ 2013 Comparative Price Report.
The average cost of an angiogram in the United States last year was $907, about 11% higher than Argentina’s $818, which was the second-highest of the six countries included in all three IFHP comparisons. The lowest cost among the six countries was in the Netherlands, at $174.
For an abdominal CT scan, the average cost in the United States was $896 in 2013, compared with $500 in Australia. Spain had the lowest cost, with an average of $94, the IFHP reported. In the United States, the average price for an MRI in 2013 was $1,145, with the Netherlands second at $461 and Switzerland lowest at $138.
New Zealand, which was not included in the angiogram analysis and therefore left out of the graph below, was actually the second most-expensive country in which to get a CT scan ($731) and an MRI ($1,005).
The IFHP is composed of more than 100 member companies in 25 countries. For the survey, the price for each country was submitted by participating member plans. Some prices are drawn from the public sector, and some are from the private sector. U.S. averages are calculated from more than 100 million claims in the Truven MarketScan Research databases.
When it comes to diagnostic imaging, the average costs of angiograms, abdominal CTs, and MRIs are higher in the United States than in other industrialized countries, according to the International Federation of Health Plans’ 2013 Comparative Price Report.
The average cost of an angiogram in the United States last year was $907, about 11% higher than Argentina’s $818, which was the second-highest of the six countries included in all three IFHP comparisons. The lowest cost among the six countries was in the Netherlands, at $174.
For an abdominal CT scan, the average cost in the United States was $896 in 2013, compared with $500 in Australia. Spain had the lowest cost, with an average of $94, the IFHP reported. In the United States, the average price for an MRI in 2013 was $1,145, with the Netherlands second at $461 and Switzerland lowest at $138.
New Zealand, which was not included in the angiogram analysis and therefore left out of the graph below, was actually the second most-expensive country in which to get a CT scan ($731) and an MRI ($1,005).
The IFHP is composed of more than 100 member companies in 25 countries. For the survey, the price for each country was submitted by participating member plans. Some prices are drawn from the public sector, and some are from the private sector. U.S. averages are calculated from more than 100 million claims in the Truven MarketScan Research databases.
When it comes to diagnostic imaging, the average costs of angiograms, abdominal CTs, and MRIs are higher in the United States than in other industrialized countries, according to the International Federation of Health Plans’ 2013 Comparative Price Report.
The average cost of an angiogram in the United States last year was $907, about 11% higher than Argentina’s $818, which was the second-highest of the six countries included in all three IFHP comparisons. The lowest cost among the six countries was in the Netherlands, at $174.
For an abdominal CT scan, the average cost in the United States was $896 in 2013, compared with $500 in Australia. Spain had the lowest cost, with an average of $94, the IFHP reported. In the United States, the average price for an MRI in 2013 was $1,145, with the Netherlands second at $461 and Switzerland lowest at $138.
New Zealand, which was not included in the angiogram analysis and therefore left out of the graph below, was actually the second most-expensive country in which to get a CT scan ($731) and an MRI ($1,005).
The IFHP is composed of more than 100 member companies in 25 countries. For the survey, the price for each country was submitted by participating member plans. Some prices are drawn from the public sector, and some are from the private sector. U.S. averages are calculated from more than 100 million claims in the Truven MarketScan Research databases.
Stopping Obesity in Its Infancy
The IHS Baby-Friendly Hospital Initiative just added another hospital to its roster. In February 2014, Whiteriver Indian Hospital in Arizona became the seventh facility to adopt a policy of encouraging and supporting breastfeeding.
The initiative is part of the wide-ranging effort to improve the health of Native Americans. According to the IHS Clinical Reporting System, more than 80% of American Indian and Alaska Native (AIAN) adults aged 20 to 74 years are overweight or obese, and about half of AIAN children and youth are not at a healthy weight. More important, 45% of children aged 2 to 5 years are overweight or obese. It’s a very specific issue: An analysis of the Centers for Disease Control and Prevention data found that between 2003 and 2008, the rate of obesity remained stable among low-income, preschool-aged children participating in federally funded health and nutrition programs—all except AIAN children.
Noting that the risk for obesity begins as early as the perinatal period, the IHS encourages clinicians in Indian Country to support policies and practices that foster breastfeeding as the exclusive feeding choice for infants in the first 6 months of life. Studies have shown a positive association between breastfeeding and lower rates of overweight among children; the protective effect seems to last well into older childhood. Breastfeeding reduces a baby’s risk of obesity by about one-third and significantly reduces the risk of type 2 diabetes for both mother and infant. Thus, the IHS initiative encourages clinicians in Indian Country who serve new mothers to familiarize themselves with the benefits of breastfeeding, problems that may arise for breastfeeding mothers, and challenges for health facilities in implementing breastfeeding policies. The website http://www.ihs.gov/babyfriendly offers a toolkit on providing education on breastfeeding.
To be designated as a Baby-Friendly facility, the facility must follow 10 steps created by the World Health Organization and UNICEF (the United Nations Children’s Fund) and endorsed by major maternal and child health authorities in the U.S. For example, the hospital or birthing facility must have a written breastfeeding policy, train staff in the skills needed to implement the policy, inform all pregnant women about the benefits of breastfeeding, and practice rooming-in (allowing mothers and infants to remain together 24 hours a day). Research has shown women are 6 times more likely to breastfeed when delivered in hospitals that practice 6 or 7 of the steps than are women in hospitals that practice none or 1 of the steps.
The IHS is working toward the Baby-Friendly designation for 14 of its obstetric facilities and encouraging tribal obstetric facilities to adopt the initiative as well.
The IHS Baby-Friendly Hospital Initiative just added another hospital to its roster. In February 2014, Whiteriver Indian Hospital in Arizona became the seventh facility to adopt a policy of encouraging and supporting breastfeeding.
The initiative is part of the wide-ranging effort to improve the health of Native Americans. According to the IHS Clinical Reporting System, more than 80% of American Indian and Alaska Native (AIAN) adults aged 20 to 74 years are overweight or obese, and about half of AIAN children and youth are not at a healthy weight. More important, 45% of children aged 2 to 5 years are overweight or obese. It’s a very specific issue: An analysis of the Centers for Disease Control and Prevention data found that between 2003 and 2008, the rate of obesity remained stable among low-income, preschool-aged children participating in federally funded health and nutrition programs—all except AIAN children.
Noting that the risk for obesity begins as early as the perinatal period, the IHS encourages clinicians in Indian Country to support policies and practices that foster breastfeeding as the exclusive feeding choice for infants in the first 6 months of life. Studies have shown a positive association between breastfeeding and lower rates of overweight among children; the protective effect seems to last well into older childhood. Breastfeeding reduces a baby’s risk of obesity by about one-third and significantly reduces the risk of type 2 diabetes for both mother and infant. Thus, the IHS initiative encourages clinicians in Indian Country who serve new mothers to familiarize themselves with the benefits of breastfeeding, problems that may arise for breastfeeding mothers, and challenges for health facilities in implementing breastfeeding policies. The website http://www.ihs.gov/babyfriendly offers a toolkit on providing education on breastfeeding.
To be designated as a Baby-Friendly facility, the facility must follow 10 steps created by the World Health Organization and UNICEF (the United Nations Children’s Fund) and endorsed by major maternal and child health authorities in the U.S. For example, the hospital or birthing facility must have a written breastfeeding policy, train staff in the skills needed to implement the policy, inform all pregnant women about the benefits of breastfeeding, and practice rooming-in (allowing mothers and infants to remain together 24 hours a day). Research has shown women are 6 times more likely to breastfeed when delivered in hospitals that practice 6 or 7 of the steps than are women in hospitals that practice none or 1 of the steps.
The IHS is working toward the Baby-Friendly designation for 14 of its obstetric facilities and encouraging tribal obstetric facilities to adopt the initiative as well.
The IHS Baby-Friendly Hospital Initiative just added another hospital to its roster. In February 2014, Whiteriver Indian Hospital in Arizona became the seventh facility to adopt a policy of encouraging and supporting breastfeeding.
The initiative is part of the wide-ranging effort to improve the health of Native Americans. According to the IHS Clinical Reporting System, more than 80% of American Indian and Alaska Native (AIAN) adults aged 20 to 74 years are overweight or obese, and about half of AIAN children and youth are not at a healthy weight. More important, 45% of children aged 2 to 5 years are overweight or obese. It’s a very specific issue: An analysis of the Centers for Disease Control and Prevention data found that between 2003 and 2008, the rate of obesity remained stable among low-income, preschool-aged children participating in federally funded health and nutrition programs—all except AIAN children.
Noting that the risk for obesity begins as early as the perinatal period, the IHS encourages clinicians in Indian Country to support policies and practices that foster breastfeeding as the exclusive feeding choice for infants in the first 6 months of life. Studies have shown a positive association between breastfeeding and lower rates of overweight among children; the protective effect seems to last well into older childhood. Breastfeeding reduces a baby’s risk of obesity by about one-third and significantly reduces the risk of type 2 diabetes for both mother and infant. Thus, the IHS initiative encourages clinicians in Indian Country who serve new mothers to familiarize themselves with the benefits of breastfeeding, problems that may arise for breastfeeding mothers, and challenges for health facilities in implementing breastfeeding policies. The website http://www.ihs.gov/babyfriendly offers a toolkit on providing education on breastfeeding.
To be designated as a Baby-Friendly facility, the facility must follow 10 steps created by the World Health Organization and UNICEF (the United Nations Children’s Fund) and endorsed by major maternal and child health authorities in the U.S. For example, the hospital or birthing facility must have a written breastfeeding policy, train staff in the skills needed to implement the policy, inform all pregnant women about the benefits of breastfeeding, and practice rooming-in (allowing mothers and infants to remain together 24 hours a day). Research has shown women are 6 times more likely to breastfeed when delivered in hospitals that practice 6 or 7 of the steps than are women in hospitals that practice none or 1 of the steps.
The IHS is working toward the Baby-Friendly designation for 14 of its obstetric facilities and encouraging tribal obstetric facilities to adopt the initiative as well.
Redesigned Health ID Cards
The VA is replacing the Veteran Identification Card (VIC) with the newly designed Veteran Health Identification Card (VHIC). “VA is committed to providing high-quality health care while ensuring the personal security of veterans,” said Secretary of Veterans Affairs Eric K. Shinseki in a February 20, 2014, press release. The new card, which has additional safety features, is an “important step forward” in protecting veterans from identity theft and other personal crimes, he said.
Similar to a typical health insurance card, the VHIC displays the veteran’s Member ID number, a new unique identifier, Plan ID number, and the emblem of the veteran’s latest branch of service. No personally identifiable information is contained on the magnetic strip or barcode, the VA says. New features that make the card easier to use include the addition of “VA” in Braille, to help visually impaired veterans, and the printing of VA phone numbers and emergency care instructions on the cards.
The phased rollout began in February 2014, first offering the card to newly enrolled and other veterans who have not been issued a VIC, then automatically mailing new cards to current VIC cardholders, beginning in April. While a VHIC is not required to receive VA health care, all enrolled veterans are encouraged to get one. VA recommends veterans safeguard their old VIC as they would a credit card, and cut up or shred the card once it is replaced.
Veterans can get more information about the VHIC by visiting their VA medical facility enrollment coordinator, logging on to http://www.va.gov/healthbenefits/vhic, or calling (877) 222-VETS (8387).
The VA is replacing the Veteran Identification Card (VIC) with the newly designed Veteran Health Identification Card (VHIC). “VA is committed to providing high-quality health care while ensuring the personal security of veterans,” said Secretary of Veterans Affairs Eric K. Shinseki in a February 20, 2014, press release. The new card, which has additional safety features, is an “important step forward” in protecting veterans from identity theft and other personal crimes, he said.
Similar to a typical health insurance card, the VHIC displays the veteran’s Member ID number, a new unique identifier, Plan ID number, and the emblem of the veteran’s latest branch of service. No personally identifiable information is contained on the magnetic strip or barcode, the VA says. New features that make the card easier to use include the addition of “VA” in Braille, to help visually impaired veterans, and the printing of VA phone numbers and emergency care instructions on the cards.
The phased rollout began in February 2014, first offering the card to newly enrolled and other veterans who have not been issued a VIC, then automatically mailing new cards to current VIC cardholders, beginning in April. While a VHIC is not required to receive VA health care, all enrolled veterans are encouraged to get one. VA recommends veterans safeguard their old VIC as they would a credit card, and cut up or shred the card once it is replaced.
Veterans can get more information about the VHIC by visiting their VA medical facility enrollment coordinator, logging on to http://www.va.gov/healthbenefits/vhic, or calling (877) 222-VETS (8387).
The VA is replacing the Veteran Identification Card (VIC) with the newly designed Veteran Health Identification Card (VHIC). “VA is committed to providing high-quality health care while ensuring the personal security of veterans,” said Secretary of Veterans Affairs Eric K. Shinseki in a February 20, 2014, press release. The new card, which has additional safety features, is an “important step forward” in protecting veterans from identity theft and other personal crimes, he said.
Similar to a typical health insurance card, the VHIC displays the veteran’s Member ID number, a new unique identifier, Plan ID number, and the emblem of the veteran’s latest branch of service. No personally identifiable information is contained on the magnetic strip or barcode, the VA says. New features that make the card easier to use include the addition of “VA” in Braille, to help visually impaired veterans, and the printing of VA phone numbers and emergency care instructions on the cards.
The phased rollout began in February 2014, first offering the card to newly enrolled and other veterans who have not been issued a VIC, then automatically mailing new cards to current VIC cardholders, beginning in April. While a VHIC is not required to receive VA health care, all enrolled veterans are encouraged to get one. VA recommends veterans safeguard their old VIC as they would a credit card, and cut up or shred the card once it is replaced.
Veterans can get more information about the VHIC by visiting their VA medical facility enrollment coordinator, logging on to http://www.va.gov/healthbenefits/vhic, or calling (877) 222-VETS (8387).
Attorneys: Doctors' first steps after lawsuit filing vital
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more beneficial resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
 |
| Dr. James A. L. Mathers, Jr. |
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
 |
| Dr. James A. L. Mathers, Jr. |
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
 |
| Dr. James A. L. Mathers, Jr. |
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more beneficial resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more beneficial resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
Pharmacy Wins Popular Vote
Another year, another thumbs-up for the VA Consolidated Mail Outpatient Pharmacy (CMOP). This is the fourth year in a row the service has received the highest customer satisfaction score in the J.D. Power independent survey of U.S. public and private mail-order pharmacies. The VA scored 871 out of 1,000 possible points—the highest score among participating mail-order pharmacies.
More than 13,500 pharmacy customers who filled a new prescription or refilled a prescription during the 3 months before the study period responded to the 2013 U.S. Pharmacy Study survey, rating cost competitiveness, delivery, ordering process, and customer service.
The VA takes part in the annual survey as a way to check itself against industry leaders and to ensure VA health care meets the highest standards. “The fact that we are rated higher than our private-sector counterparts is due in part to our unique partnership with our patients and medical centers,” explained VA Under Secretary for Health Dr. Robert Petzel in a press release. “In addition to the convenience of mail-order service, veterans also have a pharmacist available to meet with them face to face.”
In February 2014, 5 months after the J.D. Power survey results were announced, Kenneth Siehr, director of the CMOP program, had an idea to use technology to help make the pharmacy even more efficient—allowing veterans to track the status of their mail-order prescriptions via the MyHealtheVet web portal. That idea won him the 2013 Securing Americans Value Efficiency (SAVE) award from President Obama.
Another year, another thumbs-up for the VA Consolidated Mail Outpatient Pharmacy (CMOP). This is the fourth year in a row the service has received the highest customer satisfaction score in the J.D. Power independent survey of U.S. public and private mail-order pharmacies. The VA scored 871 out of 1,000 possible points—the highest score among participating mail-order pharmacies.
More than 13,500 pharmacy customers who filled a new prescription or refilled a prescription during the 3 months before the study period responded to the 2013 U.S. Pharmacy Study survey, rating cost competitiveness, delivery, ordering process, and customer service.
The VA takes part in the annual survey as a way to check itself against industry leaders and to ensure VA health care meets the highest standards. “The fact that we are rated higher than our private-sector counterparts is due in part to our unique partnership with our patients and medical centers,” explained VA Under Secretary for Health Dr. Robert Petzel in a press release. “In addition to the convenience of mail-order service, veterans also have a pharmacist available to meet with them face to face.”
In February 2014, 5 months after the J.D. Power survey results were announced, Kenneth Siehr, director of the CMOP program, had an idea to use technology to help make the pharmacy even more efficient—allowing veterans to track the status of their mail-order prescriptions via the MyHealtheVet web portal. That idea won him the 2013 Securing Americans Value Efficiency (SAVE) award from President Obama.
Another year, another thumbs-up for the VA Consolidated Mail Outpatient Pharmacy (CMOP). This is the fourth year in a row the service has received the highest customer satisfaction score in the J.D. Power independent survey of U.S. public and private mail-order pharmacies. The VA scored 871 out of 1,000 possible points—the highest score among participating mail-order pharmacies.
More than 13,500 pharmacy customers who filled a new prescription or refilled a prescription during the 3 months before the study period responded to the 2013 U.S. Pharmacy Study survey, rating cost competitiveness, delivery, ordering process, and customer service.
The VA takes part in the annual survey as a way to check itself against industry leaders and to ensure VA health care meets the highest standards. “The fact that we are rated higher than our private-sector counterparts is due in part to our unique partnership with our patients and medical centers,” explained VA Under Secretary for Health Dr. Robert Petzel in a press release. “In addition to the convenience of mail-order service, veterans also have a pharmacist available to meet with them face to face.”
In February 2014, 5 months after the J.D. Power survey results were announced, Kenneth Siehr, director of the CMOP program, had an idea to use technology to help make the pharmacy even more efficient—allowing veterans to track the status of their mail-order prescriptions via the MyHealtheVet web portal. That idea won him the 2013 Securing Americans Value Efficiency (SAVE) award from President Obama.
Patient Connectivity During Power Outages
Power outages can be devastating for people who rely on portable ventilators and other electricity-dependent durable medical equipment (DME). But thanks to innovative solutions from winners of a contest sponsored by the HHS Office of the Assistant Secretary for Preparedness and Response, emergencies won’t have to become life-or-death situations.
The first-prize team, Leo Angelo Gumpas and Xadean Ahmasi, created an integrated, Internet-based system that automatically monitors and transmits essential data from DME to caregivers and responders to provide actionable information in support of emergency planning and response operations.
Second-place winner Stan Barrack created an integrated set of tools that could use inexpensive technology, such as a cellular phone application, to securely share critical information on the status of DMEs with existing data centers where specific patient information is stored.
Third place went to An-Hu-Li and David-Li, whose idea for a cost-effective wireless DME status reporter is based on two-way radio technology. Their device would securely transmit vital information between a patient’s DME unit and authorized users, such as caregivers and first responders, operating on the same radio frequency.
Power outages can be devastating for people who rely on portable ventilators and other electricity-dependent durable medical equipment (DME). But thanks to innovative solutions from winners of a contest sponsored by the HHS Office of the Assistant Secretary for Preparedness and Response, emergencies won’t have to become life-or-death situations.
The first-prize team, Leo Angelo Gumpas and Xadean Ahmasi, created an integrated, Internet-based system that automatically monitors and transmits essential data from DME to caregivers and responders to provide actionable information in support of emergency planning and response operations.
Second-place winner Stan Barrack created an integrated set of tools that could use inexpensive technology, such as a cellular phone application, to securely share critical information on the status of DMEs with existing data centers where specific patient information is stored.
Third place went to An-Hu-Li and David-Li, whose idea for a cost-effective wireless DME status reporter is based on two-way radio technology. Their device would securely transmit vital information between a patient’s DME unit and authorized users, such as caregivers and first responders, operating on the same radio frequency.
Power outages can be devastating for people who rely on portable ventilators and other electricity-dependent durable medical equipment (DME). But thanks to innovative solutions from winners of a contest sponsored by the HHS Office of the Assistant Secretary for Preparedness and Response, emergencies won’t have to become life-or-death situations.
The first-prize team, Leo Angelo Gumpas and Xadean Ahmasi, created an integrated, Internet-based system that automatically monitors and transmits essential data from DME to caregivers and responders to provide actionable information in support of emergency planning and response operations.
Second-place winner Stan Barrack created an integrated set of tools that could use inexpensive technology, such as a cellular phone application, to securely share critical information on the status of DMEs with existing data centers where specific patient information is stored.
Third place went to An-Hu-Li and David-Li, whose idea for a cost-effective wireless DME status reporter is based on two-way radio technology. Their device would securely transmit vital information between a patient’s DME unit and authorized users, such as caregivers and first responders, operating on the same radio frequency.
Patient satisfaction not always linked to hospital safety, effectiveness
BOSTON – Hospital size and operative volume were significantly associated with satisfaction among general surgery patients in an analysis of 171 U.S. hospitals.
Surprisingly, all other safety and effectiveness measures, with the exception of low hospital mortality index, did not reliably reflect patient satisfaction, "indicating that the system plays perhaps a bigger role than anything else we can do," Dr. Gregory D. Kennedy said at the annual meeting of the American Surgical Association.
Moreover, a clean room and well-controlled pain were the best predictors of high patient satisfaction.
If it’s "the quality of the hotel, not the quality of the surgeon that drives patient satisfaction," and given that this is tied to reimbursement, what should the message be to hospital CEOs? asked discussant Dr. John J. Ricotta, chief of surgery at MedStar Washington (D.C.) Hospital Center.
Dr. Kennedy said the message he takes to the C-suite is that patient satisfaction cannot be a surrogate marker for safety and effectiveness or the only measure of quality because, in doing the right thing, surgeons often make patients unhappy. As a colorectal surgeon, he said he has unhappy patients every day, and remarked that he sometimes feels like a used car salesman where the only thing that he worries about is whether the patient is having a good experience when they drive off the lot, not whether it’s a safe, reliable car.
Dr. Kennedy, vice chair of quality at the University of Wisconsin School of Medicine, Madison, suggested that future quality measures also may need to make the distinction between satisfied and engaged, well-informed patients because a disengaged patient can be highly satisfied, while a highly engaged patient may not.
For the current study, the investigators examined federal Hospital Consumer Assessment Healthcare Providers and Systems (HCAHPS) survey results from 171 hospitals in the University Health System Consortium database from 2011 to 2012. Patients can check one of four boxes for each question on the 27-item survey, with high satisfaction defined as median responses above the 75th percentile on the top box score. This cutoff was used because the Centers for Medicare & Medicaid Services, which developed the HCAHPS, uses only the top box score, Dr. Kennedy explained.
The median hospital size was 421 beds (range, 25-1,280 beds), the median operative volume was 6,341 cases (range, 192-24,258 cases), and the mortality index was 0.83 (range, 0-2.61).
In all, 62% of high-volume hospitals, defined as those with an operative volume above the median, achieved high patient satisfaction, compared with 38% of low-volume hospitals (P less than .001). Similar results were seen for operative volume, he said.
Other system measures such as number of ICU cases and Surgical Care Improvement Project (SCIP) compliance were not associated with high HCAHPS scores.
Among patient safety indicators, only low mortality index was associated with high satisfaction (P less than .001), while complications, early mortality, and overall mortality were not.
Interestingly, hospitals with a higher number of Patient Safety Indicator cases – those involving accidental puncture, laceration, and venous thromboembolism – had higher rates of patient satisfaction, "suggesting that unsafe care is perhaps correlated with high satisfaction," Dr. Kennedy said.
Discussant Dr. Fabrizio Michelassi, chair of surgery at Weill Cornell Medical College and surgeon-in-chief, New York–Presbyterian Hospital/Weill Cornell Medical Center, in New York City, questioned whether "unsafe care gives more options for physicians to show their compassionate side," and said the overall findings are not that surprising to practicing surgeons, who frequently hear patient complaints, despite having performed a quality operation.
Dr. Kennedy said a recent paper from the Cleveland Clinic (Dis. Colon Rectum. 2013;56:219-25) suggests that Patient Safety Indicator cases are really a reflection of surgical complexity and not unsafe care at all.
Finally, other discussants criticized the study for failing to tie satisfaction to patient outcomes; for failing to control for factors influencing patient satisfaction such as age, sex, or social status; and for not looking at geographic differences or nursing-to-staff ratios.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
Dr. Kennedy reported no conflicting interests.
BOSTON – Hospital size and operative volume were significantly associated with satisfaction among general surgery patients in an analysis of 171 U.S. hospitals.
Surprisingly, all other safety and effectiveness measures, with the exception of low hospital mortality index, did not reliably reflect patient satisfaction, "indicating that the system plays perhaps a bigger role than anything else we can do," Dr. Gregory D. Kennedy said at the annual meeting of the American Surgical Association.
Moreover, a clean room and well-controlled pain were the best predictors of high patient satisfaction.
If it’s "the quality of the hotel, not the quality of the surgeon that drives patient satisfaction," and given that this is tied to reimbursement, what should the message be to hospital CEOs? asked discussant Dr. John J. Ricotta, chief of surgery at MedStar Washington (D.C.) Hospital Center.
Dr. Kennedy said the message he takes to the C-suite is that patient satisfaction cannot be a surrogate marker for safety and effectiveness or the only measure of quality because, in doing the right thing, surgeons often make patients unhappy. As a colorectal surgeon, he said he has unhappy patients every day, and remarked that he sometimes feels like a used car salesman where the only thing that he worries about is whether the patient is having a good experience when they drive off the lot, not whether it’s a safe, reliable car.
Dr. Kennedy, vice chair of quality at the University of Wisconsin School of Medicine, Madison, suggested that future quality measures also may need to make the distinction between satisfied and engaged, well-informed patients because a disengaged patient can be highly satisfied, while a highly engaged patient may not.
For the current study, the investigators examined federal Hospital Consumer Assessment Healthcare Providers and Systems (HCAHPS) survey results from 171 hospitals in the University Health System Consortium database from 2011 to 2012. Patients can check one of four boxes for each question on the 27-item survey, with high satisfaction defined as median responses above the 75th percentile on the top box score. This cutoff was used because the Centers for Medicare & Medicaid Services, which developed the HCAHPS, uses only the top box score, Dr. Kennedy explained.
The median hospital size was 421 beds (range, 25-1,280 beds), the median operative volume was 6,341 cases (range, 192-24,258 cases), and the mortality index was 0.83 (range, 0-2.61).
In all, 62% of high-volume hospitals, defined as those with an operative volume above the median, achieved high patient satisfaction, compared with 38% of low-volume hospitals (P less than .001). Similar results were seen for operative volume, he said.
Other system measures such as number of ICU cases and Surgical Care Improvement Project (SCIP) compliance were not associated with high HCAHPS scores.
Among patient safety indicators, only low mortality index was associated with high satisfaction (P less than .001), while complications, early mortality, and overall mortality were not.
Interestingly, hospitals with a higher number of Patient Safety Indicator cases – those involving accidental puncture, laceration, and venous thromboembolism – had higher rates of patient satisfaction, "suggesting that unsafe care is perhaps correlated with high satisfaction," Dr. Kennedy said.
Discussant Dr. Fabrizio Michelassi, chair of surgery at Weill Cornell Medical College and surgeon-in-chief, New York–Presbyterian Hospital/Weill Cornell Medical Center, in New York City, questioned whether "unsafe care gives more options for physicians to show their compassionate side," and said the overall findings are not that surprising to practicing surgeons, who frequently hear patient complaints, despite having performed a quality operation.
Dr. Kennedy said a recent paper from the Cleveland Clinic (Dis. Colon Rectum. 2013;56:219-25) suggests that Patient Safety Indicator cases are really a reflection of surgical complexity and not unsafe care at all.
Finally, other discussants criticized the study for failing to tie satisfaction to patient outcomes; for failing to control for factors influencing patient satisfaction such as age, sex, or social status; and for not looking at geographic differences or nursing-to-staff ratios.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
Dr. Kennedy reported no conflicting interests.
BOSTON – Hospital size and operative volume were significantly associated with satisfaction among general surgery patients in an analysis of 171 U.S. hospitals.
Surprisingly, all other safety and effectiveness measures, with the exception of low hospital mortality index, did not reliably reflect patient satisfaction, "indicating that the system plays perhaps a bigger role than anything else we can do," Dr. Gregory D. Kennedy said at the annual meeting of the American Surgical Association.
Moreover, a clean room and well-controlled pain were the best predictors of high patient satisfaction.
If it’s "the quality of the hotel, not the quality of the surgeon that drives patient satisfaction," and given that this is tied to reimbursement, what should the message be to hospital CEOs? asked discussant Dr. John J. Ricotta, chief of surgery at MedStar Washington (D.C.) Hospital Center.
Dr. Kennedy said the message he takes to the C-suite is that patient satisfaction cannot be a surrogate marker for safety and effectiveness or the only measure of quality because, in doing the right thing, surgeons often make patients unhappy. As a colorectal surgeon, he said he has unhappy patients every day, and remarked that he sometimes feels like a used car salesman where the only thing that he worries about is whether the patient is having a good experience when they drive off the lot, not whether it’s a safe, reliable car.
Dr. Kennedy, vice chair of quality at the University of Wisconsin School of Medicine, Madison, suggested that future quality measures also may need to make the distinction between satisfied and engaged, well-informed patients because a disengaged patient can be highly satisfied, while a highly engaged patient may not.
For the current study, the investigators examined federal Hospital Consumer Assessment Healthcare Providers and Systems (HCAHPS) survey results from 171 hospitals in the University Health System Consortium database from 2011 to 2012. Patients can check one of four boxes for each question on the 27-item survey, with high satisfaction defined as median responses above the 75th percentile on the top box score. This cutoff was used because the Centers for Medicare & Medicaid Services, which developed the HCAHPS, uses only the top box score, Dr. Kennedy explained.
The median hospital size was 421 beds (range, 25-1,280 beds), the median operative volume was 6,341 cases (range, 192-24,258 cases), and the mortality index was 0.83 (range, 0-2.61).
In all, 62% of high-volume hospitals, defined as those with an operative volume above the median, achieved high patient satisfaction, compared with 38% of low-volume hospitals (P less than .001). Similar results were seen for operative volume, he said.
Other system measures such as number of ICU cases and Surgical Care Improvement Project (SCIP) compliance were not associated with high HCAHPS scores.
Among patient safety indicators, only low mortality index was associated with high satisfaction (P less than .001), while complications, early mortality, and overall mortality were not.
Interestingly, hospitals with a higher number of Patient Safety Indicator cases – those involving accidental puncture, laceration, and venous thromboembolism – had higher rates of patient satisfaction, "suggesting that unsafe care is perhaps correlated with high satisfaction," Dr. Kennedy said.
Discussant Dr. Fabrizio Michelassi, chair of surgery at Weill Cornell Medical College and surgeon-in-chief, New York–Presbyterian Hospital/Weill Cornell Medical Center, in New York City, questioned whether "unsafe care gives more options for physicians to show their compassionate side," and said the overall findings are not that surprising to practicing surgeons, who frequently hear patient complaints, despite having performed a quality operation.
Dr. Kennedy said a recent paper from the Cleveland Clinic (Dis. Colon Rectum. 2013;56:219-25) suggests that Patient Safety Indicator cases are really a reflection of surgical complexity and not unsafe care at all.
Finally, other discussants criticized the study for failing to tie satisfaction to patient outcomes; for failing to control for factors influencing patient satisfaction such as age, sex, or social status; and for not looking at geographic differences or nursing-to-staff ratios.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
Dr. Kennedy reported no conflicting interests.
AT ASA 2014
Major finding: In the sample, 62% of high-volume hospitals achieved high patient satisfaction, vs. 38% of low-volume hospitals. Other system measures such as number of ICU cases and Surgical Care Improvement Project (compliance were not associated with high HCAHPS scores.
Data source: A retrospective analysis of HCAHPS surveys at 171 U.S. hospitals.
Disclosures: Dr. Kennedy reported no conflicting interests.
Accelerated Process for Housing Loan
The VA offers Specially Adapted Housing (SAH) grants to disabled veterans so they can build or modify their homes to meet their personal needs. Now, veterans and active-duty military personnel who have service-connected amyotrophic lateral sclerosis (ALS) have a faster track to getting an SAH grant. The VA has changed the rules of eligibility for the grants, which pay up to a maximum of $67,555 toward the costs of building, buying, or adapting a home.
Veterans with service-connected ALS no longer have to file multiple claims for increased benefits as their condition progresses. Many veterans and service members have service-connected ALS, but their symptoms are not yet severe enough to affect their mobility to the degree required for the grant. Before the SAH regulatory change, they couldn’t begin the process of modifying their homes to keep pace with an often rapidly progressive disease.
The VA estimates the change will save about 12 months in the automatic process of an SAH grant. “This change will make it easier for some of our most severely impaired veterans to receive speedy assistance adapting their homes to their unique needs,” said Secretary of Veterans Affairs Eric K. Shinseki in a March 19, 2014, press release.
In 2008, the VA established a “presumption of service connection” for ALS for any veteran who develops the disease at any time after separation from service, making them eligible for monthly VA disability compensation benefits. The VA amended its disability rating scale in January 2012 to assign a 100% disability evaluation for any veteran who has service-connected ALS.
For more information, visit http://www.benefits.va.gov/homeloans or call (800) 827-3702.
The VA offers Specially Adapted Housing (SAH) grants to disabled veterans so they can build or modify their homes to meet their personal needs. Now, veterans and active-duty military personnel who have service-connected amyotrophic lateral sclerosis (ALS) have a faster track to getting an SAH grant. The VA has changed the rules of eligibility for the grants, which pay up to a maximum of $67,555 toward the costs of building, buying, or adapting a home.
Veterans with service-connected ALS no longer have to file multiple claims for increased benefits as their condition progresses. Many veterans and service members have service-connected ALS, but their symptoms are not yet severe enough to affect their mobility to the degree required for the grant. Before the SAH regulatory change, they couldn’t begin the process of modifying their homes to keep pace with an often rapidly progressive disease.
The VA estimates the change will save about 12 months in the automatic process of an SAH grant. “This change will make it easier for some of our most severely impaired veterans to receive speedy assistance adapting their homes to their unique needs,” said Secretary of Veterans Affairs Eric K. Shinseki in a March 19, 2014, press release.
In 2008, the VA established a “presumption of service connection” for ALS for any veteran who develops the disease at any time after separation from service, making them eligible for monthly VA disability compensation benefits. The VA amended its disability rating scale in January 2012 to assign a 100% disability evaluation for any veteran who has service-connected ALS.
For more information, visit http://www.benefits.va.gov/homeloans or call (800) 827-3702.
The VA offers Specially Adapted Housing (SAH) grants to disabled veterans so they can build or modify their homes to meet their personal needs. Now, veterans and active-duty military personnel who have service-connected amyotrophic lateral sclerosis (ALS) have a faster track to getting an SAH grant. The VA has changed the rules of eligibility for the grants, which pay up to a maximum of $67,555 toward the costs of building, buying, or adapting a home.
Veterans with service-connected ALS no longer have to file multiple claims for increased benefits as their condition progresses. Many veterans and service members have service-connected ALS, but their symptoms are not yet severe enough to affect their mobility to the degree required for the grant. Before the SAH regulatory change, they couldn’t begin the process of modifying their homes to keep pace with an often rapidly progressive disease.
The VA estimates the change will save about 12 months in the automatic process of an SAH grant. “This change will make it easier for some of our most severely impaired veterans to receive speedy assistance adapting their homes to their unique needs,” said Secretary of Veterans Affairs Eric K. Shinseki in a March 19, 2014, press release.
In 2008, the VA established a “presumption of service connection” for ALS for any veteran who develops the disease at any time after separation from service, making them eligible for monthly VA disability compensation benefits. The VA amended its disability rating scale in January 2012 to assign a 100% disability evaluation for any veteran who has service-connected ALS.
For more information, visit http://www.benefits.va.gov/homeloans or call (800) 827-3702.
Bill to Clarify Three-Midnight Rule for Medicare Patients Gains Support from Congress, Hospitalists
In 2010, my office received a call from a Norwich, Conn., family whose 89-year-old father had fallen and broken his hip. After he was treated in the local hospital for four days, his doctor prescribed follow-on skilled nursing facility (SNF) care. Upon his arrival at the nursing home, his family was informed that they would have to pay more than $10,000 up front to cover the cost of his care: Because he had never been admitted to the hospital as an inpatient, Medicare would not cover the prescribed rehabilitative care that he needed to return home safely.
I know that hospitalists are already far too familiar with stories like this. Together, we can work to make sure it doesn’t happen again.
Support Is Growing
For me, that family’s story was a call for action. Shortly after speaking with the family, I introduced the Improving Access to Medicare Coverage Act (H.R. 1179). The bill is simple: It would restore the three-day hospital stay standard for SNF coverage, whether the stay is coded as inpatient under Part A or outpatient observation under Part B. Two Congresses later, support for the proposal is growing. In the 113th Congress, the bill has 137 bipartisan cosponsors, an indication of how widespread this problem is for Medicare beneficiaries.
The outdated Medicare law on skilled nursing care coverage is creating financial and healthcare dilemmas for families across the country. Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing. Patients are suffering, and healthcare providers are caught in the middle.
In fact, the Office of the Inspector General at the Department of Health and Human Services released a report last fall that showed that Medicare beneficiaries in 2012 had more than 600,000 hospital stays that lasted three nights, yet none were admitted as inpatients. Even though these beneficiaries likely received the same care inpatients received, their observation status designation disqualified them from Medicare coverage of the SNF benefit. For their families, prescribed follow-on SNF care would have an out-of-pocket cost averaging more than $10,000. For seniors on fixed incomes, that is a devastating financial penalty for a service that should be covered by their health plans.

—Rep. Joe Courtney
Administrative Oversight
There are many reasons for the growth in observation status treatments, but a primary driver is increasing scrutiny of admitting practices by recovery audit contractors (RACs). The consequences of RAC review processes have created difficult situations for hospitals, because admitting decisions are reviewable for three years, and hospitals can be hit with claw-back penalties for payments on behalf of patients RACs determine were incorrectly admitted. To prevent costly penalties and protracted appeals of individual cases, many hospitals feel an understandable amount of pressure to err on the side of treating patients under outpatient observation status covered under Part B.
The original intent of the three-day inpatient stay requirement was to serve as a tangible measure of medical necessity of SNF care. And, when the three-day inpatient stay prerequisite was written into law, long-term hospital observation stays were nonexistent. This intent has been lost in a changing system of hospital oversight under RACs and admitting practices.
The impact on patients and families is tragic.
Ann Sheehy, MD, MS, FHM, a hospitalist speaking on behalf of the Society of Hospital Medicine on a recent conference call I hosted, detailed the scenes she sees every day with her own patients. She described how doctors, knowing that a patient lacks the means to pay for rehabilitative care out of pocket and the support system to recover safely at home, sometimes keep the patient in the hospital longer, at a higher cost to Medicare. In other cases, Dr. Sheehy noted that patients end up back in the hospital soon after being discharged, having foregone expensive SNF care and subsequently suffered preventable injuries and illnesses. Both of these outcomes are bad for patients—and bad for Medicare expenditures.
Three-Day Fix
While the problem of observation status treatment is complex, the solution is simple.
As observation status becomes more ingrained in the healthcare lexicon, a legislative fix to restore the three-day hospital stay standard is needed now more than ever. Three days in the hospital—whether as an inpatient or under outpatient observation—should count for three days in the hospital when Medicare determines eligibility for SNF coverage.
My bill, H.R. 1179, is the most direct solution to rectify the flaw that leaves hundreds of thousands of beneficiaries wondering how their stay in the hospital does not “count” and scrambling to figure out how to pay for care—or foregoing it entirely. The strong support in the advocacy community for this legislation—especially from SHM—and the sway of outside groups cannot be overstated. In Washington’s current climate, the only thing that moves bipartisan issues forward is outside pressure.
Together, I hope hospitalists and members of Congress will reach the critical mass needed to pass this legislation and ensure that Medicare beneficiaries are covered for medically necessary care.
Joseph “Joe” Courtney is the U.S. Representative for Connecticut’s second congressional district, serving since 2007. The district includes most of the eastern third of the state, including Norwich and New London.
In 2010, my office received a call from a Norwich, Conn., family whose 89-year-old father had fallen and broken his hip. After he was treated in the local hospital for four days, his doctor prescribed follow-on skilled nursing facility (SNF) care. Upon his arrival at the nursing home, his family was informed that they would have to pay more than $10,000 up front to cover the cost of his care: Because he had never been admitted to the hospital as an inpatient, Medicare would not cover the prescribed rehabilitative care that he needed to return home safely.
I know that hospitalists are already far too familiar with stories like this. Together, we can work to make sure it doesn’t happen again.
Support Is Growing
For me, that family’s story was a call for action. Shortly after speaking with the family, I introduced the Improving Access to Medicare Coverage Act (H.R. 1179). The bill is simple: It would restore the three-day hospital stay standard for SNF coverage, whether the stay is coded as inpatient under Part A or outpatient observation under Part B. Two Congresses later, support for the proposal is growing. In the 113th Congress, the bill has 137 bipartisan cosponsors, an indication of how widespread this problem is for Medicare beneficiaries.
The outdated Medicare law on skilled nursing care coverage is creating financial and healthcare dilemmas for families across the country. Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing. Patients are suffering, and healthcare providers are caught in the middle.
In fact, the Office of the Inspector General at the Department of Health and Human Services released a report last fall that showed that Medicare beneficiaries in 2012 had more than 600,000 hospital stays that lasted three nights, yet none were admitted as inpatients. Even though these beneficiaries likely received the same care inpatients received, their observation status designation disqualified them from Medicare coverage of the SNF benefit. For their families, prescribed follow-on SNF care would have an out-of-pocket cost averaging more than $10,000. For seniors on fixed incomes, that is a devastating financial penalty for a service that should be covered by their health plans.

—Rep. Joe Courtney
Administrative Oversight
There are many reasons for the growth in observation status treatments, but a primary driver is increasing scrutiny of admitting practices by recovery audit contractors (RACs). The consequences of RAC review processes have created difficult situations for hospitals, because admitting decisions are reviewable for three years, and hospitals can be hit with claw-back penalties for payments on behalf of patients RACs determine were incorrectly admitted. To prevent costly penalties and protracted appeals of individual cases, many hospitals feel an understandable amount of pressure to err on the side of treating patients under outpatient observation status covered under Part B.
The original intent of the three-day inpatient stay requirement was to serve as a tangible measure of medical necessity of SNF care. And, when the three-day inpatient stay prerequisite was written into law, long-term hospital observation stays were nonexistent. This intent has been lost in a changing system of hospital oversight under RACs and admitting practices.
The impact on patients and families is tragic.
Ann Sheehy, MD, MS, FHM, a hospitalist speaking on behalf of the Society of Hospital Medicine on a recent conference call I hosted, detailed the scenes she sees every day with her own patients. She described how doctors, knowing that a patient lacks the means to pay for rehabilitative care out of pocket and the support system to recover safely at home, sometimes keep the patient in the hospital longer, at a higher cost to Medicare. In other cases, Dr. Sheehy noted that patients end up back in the hospital soon after being discharged, having foregone expensive SNF care and subsequently suffered preventable injuries and illnesses. Both of these outcomes are bad for patients—and bad for Medicare expenditures.
Three-Day Fix
While the problem of observation status treatment is complex, the solution is simple.
As observation status becomes more ingrained in the healthcare lexicon, a legislative fix to restore the three-day hospital stay standard is needed now more than ever. Three days in the hospital—whether as an inpatient or under outpatient observation—should count for three days in the hospital when Medicare determines eligibility for SNF coverage.
My bill, H.R. 1179, is the most direct solution to rectify the flaw that leaves hundreds of thousands of beneficiaries wondering how their stay in the hospital does not “count” and scrambling to figure out how to pay for care—or foregoing it entirely. The strong support in the advocacy community for this legislation—especially from SHM—and the sway of outside groups cannot be overstated. In Washington’s current climate, the only thing that moves bipartisan issues forward is outside pressure.
Together, I hope hospitalists and members of Congress will reach the critical mass needed to pass this legislation and ensure that Medicare beneficiaries are covered for medically necessary care.
Joseph “Joe” Courtney is the U.S. Representative for Connecticut’s second congressional district, serving since 2007. The district includes most of the eastern third of the state, including Norwich and New London.
In 2010, my office received a call from a Norwich, Conn., family whose 89-year-old father had fallen and broken his hip. After he was treated in the local hospital for four days, his doctor prescribed follow-on skilled nursing facility (SNF) care. Upon his arrival at the nursing home, his family was informed that they would have to pay more than $10,000 up front to cover the cost of his care: Because he had never been admitted to the hospital as an inpatient, Medicare would not cover the prescribed rehabilitative care that he needed to return home safely.
I know that hospitalists are already far too familiar with stories like this. Together, we can work to make sure it doesn’t happen again.
Support Is Growing
For me, that family’s story was a call for action. Shortly after speaking with the family, I introduced the Improving Access to Medicare Coverage Act (H.R. 1179). The bill is simple: It would restore the three-day hospital stay standard for SNF coverage, whether the stay is coded as inpatient under Part A or outpatient observation under Part B. Two Congresses later, support for the proposal is growing. In the 113th Congress, the bill has 137 bipartisan cosponsors, an indication of how widespread this problem is for Medicare beneficiaries.
The outdated Medicare law on skilled nursing care coverage is creating financial and healthcare dilemmas for families across the country. Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing. Patients are suffering, and healthcare providers are caught in the middle.
In fact, the Office of the Inspector General at the Department of Health and Human Services released a report last fall that showed that Medicare beneficiaries in 2012 had more than 600,000 hospital stays that lasted three nights, yet none were admitted as inpatients. Even though these beneficiaries likely received the same care inpatients received, their observation status designation disqualified them from Medicare coverage of the SNF benefit. For their families, prescribed follow-on SNF care would have an out-of-pocket cost averaging more than $10,000. For seniors on fixed incomes, that is a devastating financial penalty for a service that should be covered by their health plans.

—Rep. Joe Courtney
Administrative Oversight
There are many reasons for the growth in observation status treatments, but a primary driver is increasing scrutiny of admitting practices by recovery audit contractors (RACs). The consequences of RAC review processes have created difficult situations for hospitals, because admitting decisions are reviewable for three years, and hospitals can be hit with claw-back penalties for payments on behalf of patients RACs determine were incorrectly admitted. To prevent costly penalties and protracted appeals of individual cases, many hospitals feel an understandable amount of pressure to err on the side of treating patients under outpatient observation status covered under Part B.
The original intent of the three-day inpatient stay requirement was to serve as a tangible measure of medical necessity of SNF care. And, when the three-day inpatient stay prerequisite was written into law, long-term hospital observation stays were nonexistent. This intent has been lost in a changing system of hospital oversight under RACs and admitting practices.
The impact on patients and families is tragic.
Ann Sheehy, MD, MS, FHM, a hospitalist speaking on behalf of the Society of Hospital Medicine on a recent conference call I hosted, detailed the scenes she sees every day with her own patients. She described how doctors, knowing that a patient lacks the means to pay for rehabilitative care out of pocket and the support system to recover safely at home, sometimes keep the patient in the hospital longer, at a higher cost to Medicare. In other cases, Dr. Sheehy noted that patients end up back in the hospital soon after being discharged, having foregone expensive SNF care and subsequently suffered preventable injuries and illnesses. Both of these outcomes are bad for patients—and bad for Medicare expenditures.
Three-Day Fix
While the problem of observation status treatment is complex, the solution is simple.
As observation status becomes more ingrained in the healthcare lexicon, a legislative fix to restore the three-day hospital stay standard is needed now more than ever. Three days in the hospital—whether as an inpatient or under outpatient observation—should count for three days in the hospital when Medicare determines eligibility for SNF coverage.
My bill, H.R. 1179, is the most direct solution to rectify the flaw that leaves hundreds of thousands of beneficiaries wondering how their stay in the hospital does not “count” and scrambling to figure out how to pay for care—or foregoing it entirely. The strong support in the advocacy community for this legislation—especially from SHM—and the sway of outside groups cannot be overstated. In Washington’s current climate, the only thing that moves bipartisan issues forward is outside pressure.
Together, I hope hospitalists and members of Congress will reach the critical mass needed to pass this legislation and ensure that Medicare beneficiaries are covered for medically necessary care.
Joseph “Joe” Courtney is the U.S. Representative for Connecticut’s second congressional district, serving since 2007. The district includes most of the eastern third of the state, including Norwich and New London.