User login
Residents' ECG Interpretation Skills
Decreased efficiency at the beginning of residency training likely results in preventable harm for patients, a phenomenon known as the July Effect.[1, 2] Postgraduate year (PGY)1 residents enter training with a variety of clinical skills and experiences, and concerns exist regarding their preparation to enter graduate medical education (GME).[3] Electrocardiogram (ECG) interpretation is a core clinical skill that residents must have on the first day of training to manage patients, recognize emergencies, and develop evidence‐based and cost‐effective treatment plans. We assessed incoming PGY‐1 residents' ability to interpret common ECG findings as part of a rigorous boot camp experience.[4]
METHODS
This was an institutional review board‐approved pre‐post study of 81 new PGY‐1 residents' ECG interpretation skills. Subjects represented all trainees from internal medicine (n=47), emergency medicine (n=13), anesthesiology (n=11), and general surgery (n=10), who entered GME at Northwestern University in June 2013. Residents completed a pretest, followed by a 60‐minute interactive small group tutorial and a post‐test. Program faculty and expert cardiologists selected 10 common ECG findings for the study, many representing medical emergencies requiring immediate treatment. The diagnoses were: normal sinus rhythm, hyperkalemia, right bundle branch block (RBBB), left bundle branch block (LBBB), complete heart block, lateral wall myocardial infarction (MI), anterior wall MI, atrial fibrillation, ventricular paced rhythm, and ventricular tachycardia (VT). ECGs were selected from an online reference set (
RESULTS
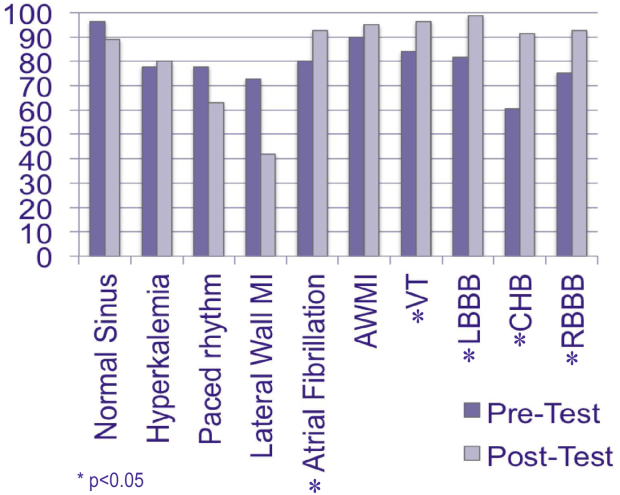
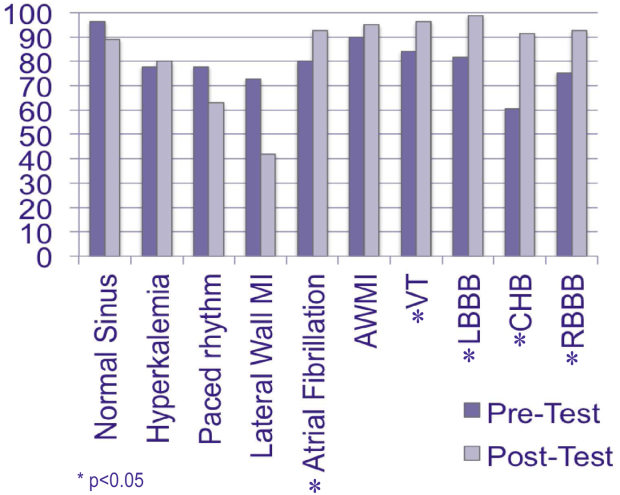
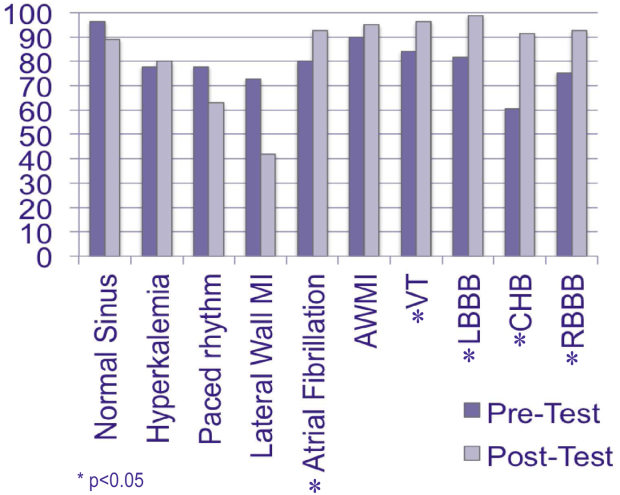
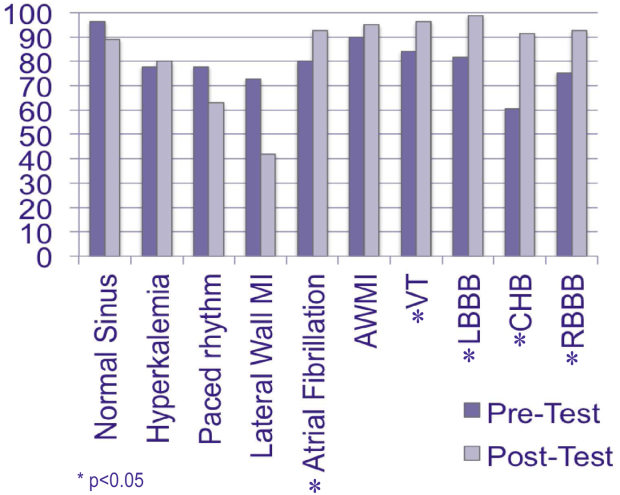
All 81 residents completed the study. The mean age was 27 years, and 56% were male. Eighty (99%) graduated from a US medical school. The mean United States Medical Licensing Examination scores were step 1: 243.8 (14.4) and step 2: 251.8 (13.6). Twenty‐six (32%) completed a cardiology rotation in medical school. Before the pretest, residents self‐assessed their ECG interpretation skills as a mean of 61.8 (standard deviation 17.2) using a scale of 0 (not confident) to 100 (very confident). Pretest results ranged from 60.5% correct (complete heart block) to 96.3% correct (normal sinus rhythm). Eighteen residents (22%) did not recognize hyperkalemia, 20 (25%) were unable to identify RBBB, and 15 (18%) LBBB. Twenty‐two (27%) could not discern a lateral wall MI, and 8 residents (10%) missed an anterior wall MI. Sixteen (20%) could not diagnose atrial fibrillation, 18 (22%) could not identify a ventricular paced rhythm, and 13 (16%) did not recognize VT. Mean post‐test scores improved significantly for 5 cases (P<0.05), but did not rise significantly for normal sinus rhythm, lateral wall MI, anterior wall MI, hyperkalemia, and ventricular paced rhythm 1.
DISCUSSION
PGY‐1 residents from multiple specialties were not confident regarding their ability to interpret ECGs and could not reliably identify 10 basic findings. This is despite graduating almost exclusively from US medical schools and performing at high levels on standardized tests. Although boot camp improved recognition of important ECG findings, including VT and bundle branch blocks, identification of emergent diagnoses such as lateral/anterior MI and hyperkalemia require additional training and close supervision during patient care. This study provides further evidence that the preparation of PGY‐1 residents to enter GME is lacking. Recent calls for inclusion of cost‐consciousness and stewardship of resources as a seventh competency for residents[5] are challenging, because incoming trainees do not uniformly possess the basic clinical skills needed to make these judgments.[3, 4] If residents cannot reliably interpret ECGs, it is not possible to determine cost‐effective testing strategies for patients with cardiac conditions. Based on the result of this study and others,[3, 4] we believe medical schools should agree upon specific graduation requirements to ensure all students have mastered core competencies and are prepared to enter GME.
Acknowledgments
Disclosure: Nothing to report.
- , . The July effect: fertile ground for systems improvement. Ann Intern Med. 2011;155(5):331–332.
- , , , , , . July effect: impact of the academic year‐end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
- , , , . Assessing residents' competencies at baseline: identifying the gaps. Acad Med. 2004;79(6):564–570.
- , , , et al. Making July safer: simulation‐based mastery learning during intern boot camp. Acad Med. 2013;88(2):233–239.
- . Providing high‐value, cost‐conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388.
Decreased efficiency at the beginning of residency training likely results in preventable harm for patients, a phenomenon known as the July Effect.[1, 2] Postgraduate year (PGY)1 residents enter training with a variety of clinical skills and experiences, and concerns exist regarding their preparation to enter graduate medical education (GME).[3] Electrocardiogram (ECG) interpretation is a core clinical skill that residents must have on the first day of training to manage patients, recognize emergencies, and develop evidence‐based and cost‐effective treatment plans. We assessed incoming PGY‐1 residents' ability to interpret common ECG findings as part of a rigorous boot camp experience.[4]
METHODS
This was an institutional review board‐approved pre‐post study of 81 new PGY‐1 residents' ECG interpretation skills. Subjects represented all trainees from internal medicine (n=47), emergency medicine (n=13), anesthesiology (n=11), and general surgery (n=10), who entered GME at Northwestern University in June 2013. Residents completed a pretest, followed by a 60‐minute interactive small group tutorial and a post‐test. Program faculty and expert cardiologists selected 10 common ECG findings for the study, many representing medical emergencies requiring immediate treatment. The diagnoses were: normal sinus rhythm, hyperkalemia, right bundle branch block (RBBB), left bundle branch block (LBBB), complete heart block, lateral wall myocardial infarction (MI), anterior wall MI, atrial fibrillation, ventricular paced rhythm, and ventricular tachycardia (VT). ECGs were selected from an online reference set (
RESULTS
All 81 residents completed the study. The mean age was 27 years, and 56% were male. Eighty (99%) graduated from a US medical school. The mean United States Medical Licensing Examination scores were step 1: 243.8 (14.4) and step 2: 251.8 (13.6). Twenty‐six (32%) completed a cardiology rotation in medical school. Before the pretest, residents self‐assessed their ECG interpretation skills as a mean of 61.8 (standard deviation 17.2) using a scale of 0 (not confident) to 100 (very confident). Pretest results ranged from 60.5% correct (complete heart block) to 96.3% correct (normal sinus rhythm). Eighteen residents (22%) did not recognize hyperkalemia, 20 (25%) were unable to identify RBBB, and 15 (18%) LBBB. Twenty‐two (27%) could not discern a lateral wall MI, and 8 residents (10%) missed an anterior wall MI. Sixteen (20%) could not diagnose atrial fibrillation, 18 (22%) could not identify a ventricular paced rhythm, and 13 (16%) did not recognize VT. Mean post‐test scores improved significantly for 5 cases (P<0.05), but did not rise significantly for normal sinus rhythm, lateral wall MI, anterior wall MI, hyperkalemia, and ventricular paced rhythm 1.
DISCUSSION
PGY‐1 residents from multiple specialties were not confident regarding their ability to interpret ECGs and could not reliably identify 10 basic findings. This is despite graduating almost exclusively from US medical schools and performing at high levels on standardized tests. Although boot camp improved recognition of important ECG findings, including VT and bundle branch blocks, identification of emergent diagnoses such as lateral/anterior MI and hyperkalemia require additional training and close supervision during patient care. This study provides further evidence that the preparation of PGY‐1 residents to enter GME is lacking. Recent calls for inclusion of cost‐consciousness and stewardship of resources as a seventh competency for residents[5] are challenging, because incoming trainees do not uniformly possess the basic clinical skills needed to make these judgments.[3, 4] If residents cannot reliably interpret ECGs, it is not possible to determine cost‐effective testing strategies for patients with cardiac conditions. Based on the result of this study and others,[3, 4] we believe medical schools should agree upon specific graduation requirements to ensure all students have mastered core competencies and are prepared to enter GME.
Acknowledgments
Disclosure: Nothing to report.
Decreased efficiency at the beginning of residency training likely results in preventable harm for patients, a phenomenon known as the July Effect.[1, 2] Postgraduate year (PGY)1 residents enter training with a variety of clinical skills and experiences, and concerns exist regarding their preparation to enter graduate medical education (GME).[3] Electrocardiogram (ECG) interpretation is a core clinical skill that residents must have on the first day of training to manage patients, recognize emergencies, and develop evidence‐based and cost‐effective treatment plans. We assessed incoming PGY‐1 residents' ability to interpret common ECG findings as part of a rigorous boot camp experience.[4]
METHODS
This was an institutional review board‐approved pre‐post study of 81 new PGY‐1 residents' ECG interpretation skills. Subjects represented all trainees from internal medicine (n=47), emergency medicine (n=13), anesthesiology (n=11), and general surgery (n=10), who entered GME at Northwestern University in June 2013. Residents completed a pretest, followed by a 60‐minute interactive small group tutorial and a post‐test. Program faculty and expert cardiologists selected 10 common ECG findings for the study, many representing medical emergencies requiring immediate treatment. The diagnoses were: normal sinus rhythm, hyperkalemia, right bundle branch block (RBBB), left bundle branch block (LBBB), complete heart block, lateral wall myocardial infarction (MI), anterior wall MI, atrial fibrillation, ventricular paced rhythm, and ventricular tachycardia (VT). ECGs were selected from an online reference set (
RESULTS
All 81 residents completed the study. The mean age was 27 years, and 56% were male. Eighty (99%) graduated from a US medical school. The mean United States Medical Licensing Examination scores were step 1: 243.8 (14.4) and step 2: 251.8 (13.6). Twenty‐six (32%) completed a cardiology rotation in medical school. Before the pretest, residents self‐assessed their ECG interpretation skills as a mean of 61.8 (standard deviation 17.2) using a scale of 0 (not confident) to 100 (very confident). Pretest results ranged from 60.5% correct (complete heart block) to 96.3% correct (normal sinus rhythm). Eighteen residents (22%) did not recognize hyperkalemia, 20 (25%) were unable to identify RBBB, and 15 (18%) LBBB. Twenty‐two (27%) could not discern a lateral wall MI, and 8 residents (10%) missed an anterior wall MI. Sixteen (20%) could not diagnose atrial fibrillation, 18 (22%) could not identify a ventricular paced rhythm, and 13 (16%) did not recognize VT. Mean post‐test scores improved significantly for 5 cases (P<0.05), but did not rise significantly for normal sinus rhythm, lateral wall MI, anterior wall MI, hyperkalemia, and ventricular paced rhythm 1.
DISCUSSION
PGY‐1 residents from multiple specialties were not confident regarding their ability to interpret ECGs and could not reliably identify 10 basic findings. This is despite graduating almost exclusively from US medical schools and performing at high levels on standardized tests. Although boot camp improved recognition of important ECG findings, including VT and bundle branch blocks, identification of emergent diagnoses such as lateral/anterior MI and hyperkalemia require additional training and close supervision during patient care. This study provides further evidence that the preparation of PGY‐1 residents to enter GME is lacking. Recent calls for inclusion of cost‐consciousness and stewardship of resources as a seventh competency for residents[5] are challenging, because incoming trainees do not uniformly possess the basic clinical skills needed to make these judgments.[3, 4] If residents cannot reliably interpret ECGs, it is not possible to determine cost‐effective testing strategies for patients with cardiac conditions. Based on the result of this study and others,[3, 4] we believe medical schools should agree upon specific graduation requirements to ensure all students have mastered core competencies and are prepared to enter GME.
Acknowledgments
Disclosure: Nothing to report.
- , . The July effect: fertile ground for systems improvement. Ann Intern Med. 2011;155(5):331–332.
- , , , , , . July effect: impact of the academic year‐end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
- , , , . Assessing residents' competencies at baseline: identifying the gaps. Acad Med. 2004;79(6):564–570.
- , , , et al. Making July safer: simulation‐based mastery learning during intern boot camp. Acad Med. 2013;88(2):233–239.
- . Providing high‐value, cost‐conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388.
- , . The July effect: fertile ground for systems improvement. Ann Intern Med. 2011;155(5):331–332.
- , , , , , . July effect: impact of the academic year‐end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309–315.
- , , , . Assessing residents' competencies at baseline: identifying the gaps. Acad Med. 2004;79(6):564–570.
- , , , et al. Making July safer: simulation‐based mastery learning during intern boot camp. Acad Med. 2013;88(2):233–239.
- . Providing high‐value, cost‐conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386–388.
Mentoring at a Community Hospital
The literature focusing on physician mentoring is limited principally to programs at academic medical centers.[1, 2, 3, 4, 5] Traditionally, physicians at academic medical centers who are engaged in research have one or more such advisors. However, many clinical faculties are not engaged in research. Further, little has been written about mentoring initiatives among physicians in full‐time clinical practice.[6] Such initiatives have been suggested as one way of reducing physician stress and improving professional satisfaction, issues of great concern among practicing physicians, particularly hospitalists and primary care physicians.[7]
A mentoring program was initiated at the Western Connecticut Health Network (WCHN) in January 2012. WCHN is a healthcare system comprised of the Danbury and New Milford Hospitals, with 371 licensed beds and a network of salaried primary care and specialty physicians. At Danbury, residency programs are in place in all specialties, and medical students from the University of Vermont rotate through the major clinical specialties.
This article describes the mentoring program at WCHN and gives a preliminary assessment of its value based on a survey of the participants after the first year of the program.
PROGRAM DESCRIPTION
Although the mentoring program was offered to all physicians of the WCHN, the principal groups of interest were the salaried primary care physicians (n=46) and the hospitalists (n=24). The program is a formal system of mentorship and career support, whose goal is to maximize the potential and career satisfaction of each member of the medical staff.
Eight senior physicians from the Departments of Medicine and Surgery served as mentors in their free time. They were selected based on their high regard as members of the medical staff who reflected the attributes of satisfactory mentorsgood listeners who are supportive, nonjudgmental, practical, and enthusiastic.[8] They received informal training through meetings with the program consultant (corresponding author) who had previously established mentoring programs at Massachusetts General Hospital, Boston, Massachusetts and the University of Rochester Medical Center, Rochester, New York.
Mentees were principally hospitalists and primary care physicians in full‐time clinical practice. Practice experiences varied from 2 or 3 to 20 years or more. All hospitalists and some primary care physicians were engaged in teaching residents and/or medical students. Mentees were asked to complete a 1‐page form indicating their goals for the coming year, what issues they would like to discuss with a mentor, and which mentor they wish to meet with. The sessions were scheduled during free time of both mentor and mentee, held in a quiet setting, were confidential, and lasted an hour or more. At the end of each session, mentee and mentor agreed on what was discussed and what next steps each had responsibility for. The mentor subsequently wrote up a summary of the meeting and reviewed it with the mentee for accuracy. Ongoing contacts were in person, phone, or e‐mail initiated either by the mentor or the mentee. Examples of next steps included helping a mentee obtain further training, observe and comment on the mentee's teaching skills, sponsor the mentee for advancement to fellowship in his/her specialty society, or assist the mentee in the preparation of an article for publication. Frequency of meetings varied from a single session on a self‐limited issue to multiple sessions throughout the year.
At the end of the first year of the program, the participants were surveyed by e‐mail about their perceptions of the program. The survey was a structured instrument asking them to indicate what the principal issue or issues were that led them to seek a mentor, whether they felt the mentoring program had been helpful, if so in what way, and if not why not.
SURVEY RESULTS
Twenty‐seven of the 39 participants responded to the survey (69%). Hospitalists were the most likely to participate in the mentoring program (18 of 24) and to respond to the survey. Career planning (52%), balance among personal and professional life (43%), and leadership development (38%) were the most common reasons given for meeting with a mentor. Twenty percent of mentees had no agenda. They simply wanted to talk. Fifteen percent had a specific project in mind about which they needed advice and counsel. All but one survey respondent felt the mentoring program met their expectations by setting goals (62%), planning next steps in their career (60%), gaining new insights (52%), completing a long‐deferred goal (30%), reducing stress (19%), and improving self‐confidence (19%).
Without exception, mentees indicated that their mentors met the criteria used to define a good mentor.[8]
DISCUSSION
One marker of the program's success is that all but 1 of the respondents felt the mentoring sessions met their expectations. Planning next career steps was a principle interest among the hospitalist group. This is not surprising given that many hospitalists are recent graduates of training programs, and their long‐term career plans may not be well defined. The mentoring program helped 3 hospitalists obtain fellowship training. About 1 in 5 mentees indicated that a reduction in stress was an outcome of their mentoring sessions. Recent studies of physician burnout have shown that physicians of first contact are at greatest risk of burnout.[9] Two‐thirds of the physicians participating in the mentoring program fell into this category. In a recent survey of physicians from all specialties across the country, mentoring was suggested as 1 of a number of strategies that organizations could provide to reduce stress and burnout.[7]
Important lessons learned over the first year of the program were that (1) mentees should have protected time to participate; (2) mentor and mentee should be in touch no less often than every 3 to 6 months, even if there is not an ongoing issue they are working on; and (3) substantive improvements in the program resulted from frequent (eg, every 2 months) meetings of the mentors.
In conclusion, although the survey sample in our study was small, the findings suggest directions and strategies for similar hospitals and health systems. Health systems that seek to improve the professional satisfaction of their physicians should be interested in this description of the physician mentoring program at the WCHN and its perceived value by the participants.
Disclosures
Disclosures: Dr. Griner received a consulting fee from the Western Connecticut Health System for his role in developing the mentoring program and participating in the writing of the article. The authors report no conflicts of interest.
- . . . . Support‐challenge‐vision: a model for faculty mentoring. Med Teach. 1998;20:595–597.
- , , , . A descriptive cross‐sectional study of formal mentoring for faculty. Fam Med. 1996;28:434–438.
- Advisor, teacher, role model, friend: on being a mentor to students in science and engineering. Washington, DC: National Academy Press; 1997. Available at: http://www.nap.edu/readingroom/books/mentor. Accessed 5/13/2013.
- , , , . Helping medical school faculty realize their dreams: an innovative, collaborative, mentoring program. Acad Med. 2002;77:377–384.
- , , , . A needs assessment of medical school faculty: caring for the caretakers. J Contin Educ Health Prof. 2003;23:21–29.
- , . Personal and rofessional learning plans—an evaluation of mentoring in general practice. Educ Gen Pract. 1998;9:261–263.
- . Burnout in health care providers. Integr Med. 2013;12:22–24.
- , , . Defining the ideal qualities of mentorship. Am J Med. 2011;124:453–458.
- , , , et al. Burnout and satisfaction with work‐life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385.
The literature focusing on physician mentoring is limited principally to programs at academic medical centers.[1, 2, 3, 4, 5] Traditionally, physicians at academic medical centers who are engaged in research have one or more such advisors. However, many clinical faculties are not engaged in research. Further, little has been written about mentoring initiatives among physicians in full‐time clinical practice.[6] Such initiatives have been suggested as one way of reducing physician stress and improving professional satisfaction, issues of great concern among practicing physicians, particularly hospitalists and primary care physicians.[7]
A mentoring program was initiated at the Western Connecticut Health Network (WCHN) in January 2012. WCHN is a healthcare system comprised of the Danbury and New Milford Hospitals, with 371 licensed beds and a network of salaried primary care and specialty physicians. At Danbury, residency programs are in place in all specialties, and medical students from the University of Vermont rotate through the major clinical specialties.
This article describes the mentoring program at WCHN and gives a preliminary assessment of its value based on a survey of the participants after the first year of the program.
PROGRAM DESCRIPTION
Although the mentoring program was offered to all physicians of the WCHN, the principal groups of interest were the salaried primary care physicians (n=46) and the hospitalists (n=24). The program is a formal system of mentorship and career support, whose goal is to maximize the potential and career satisfaction of each member of the medical staff.
Eight senior physicians from the Departments of Medicine and Surgery served as mentors in their free time. They were selected based on their high regard as members of the medical staff who reflected the attributes of satisfactory mentorsgood listeners who are supportive, nonjudgmental, practical, and enthusiastic.[8] They received informal training through meetings with the program consultant (corresponding author) who had previously established mentoring programs at Massachusetts General Hospital, Boston, Massachusetts and the University of Rochester Medical Center, Rochester, New York.
Mentees were principally hospitalists and primary care physicians in full‐time clinical practice. Practice experiences varied from 2 or 3 to 20 years or more. All hospitalists and some primary care physicians were engaged in teaching residents and/or medical students. Mentees were asked to complete a 1‐page form indicating their goals for the coming year, what issues they would like to discuss with a mentor, and which mentor they wish to meet with. The sessions were scheduled during free time of both mentor and mentee, held in a quiet setting, were confidential, and lasted an hour or more. At the end of each session, mentee and mentor agreed on what was discussed and what next steps each had responsibility for. The mentor subsequently wrote up a summary of the meeting and reviewed it with the mentee for accuracy. Ongoing contacts were in person, phone, or e‐mail initiated either by the mentor or the mentee. Examples of next steps included helping a mentee obtain further training, observe and comment on the mentee's teaching skills, sponsor the mentee for advancement to fellowship in his/her specialty society, or assist the mentee in the preparation of an article for publication. Frequency of meetings varied from a single session on a self‐limited issue to multiple sessions throughout the year.
At the end of the first year of the program, the participants were surveyed by e‐mail about their perceptions of the program. The survey was a structured instrument asking them to indicate what the principal issue or issues were that led them to seek a mentor, whether they felt the mentoring program had been helpful, if so in what way, and if not why not.
SURVEY RESULTS
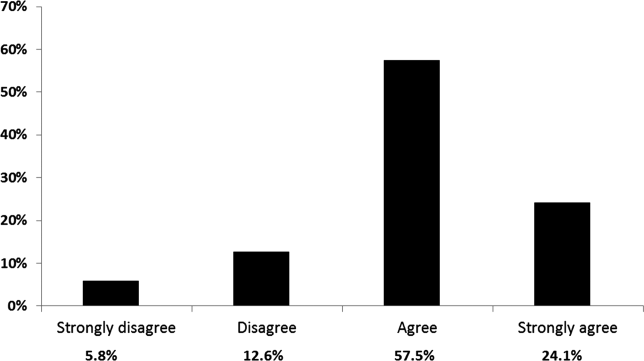
Twenty‐seven of the 39 participants responded to the survey (69%). Hospitalists were the most likely to participate in the mentoring program (18 of 24) and to respond to the survey. Career planning (52%), balance among personal and professional life (43%), and leadership development (38%) were the most common reasons given for meeting with a mentor. Twenty percent of mentees had no agenda. They simply wanted to talk. Fifteen percent had a specific project in mind about which they needed advice and counsel. All but one survey respondent felt the mentoring program met their expectations by setting goals (62%), planning next steps in their career (60%), gaining new insights (52%), completing a long‐deferred goal (30%), reducing stress (19%), and improving self‐confidence (19%).
Without exception, mentees indicated that their mentors met the criteria used to define a good mentor.[8]
DISCUSSION
One marker of the program's success is that all but 1 of the respondents felt the mentoring sessions met their expectations. Planning next career steps was a principle interest among the hospitalist group. This is not surprising given that many hospitalists are recent graduates of training programs, and their long‐term career plans may not be well defined. The mentoring program helped 3 hospitalists obtain fellowship training. About 1 in 5 mentees indicated that a reduction in stress was an outcome of their mentoring sessions. Recent studies of physician burnout have shown that physicians of first contact are at greatest risk of burnout.[9] Two‐thirds of the physicians participating in the mentoring program fell into this category. In a recent survey of physicians from all specialties across the country, mentoring was suggested as 1 of a number of strategies that organizations could provide to reduce stress and burnout.[7]
Important lessons learned over the first year of the program were that (1) mentees should have protected time to participate; (2) mentor and mentee should be in touch no less often than every 3 to 6 months, even if there is not an ongoing issue they are working on; and (3) substantive improvements in the program resulted from frequent (eg, every 2 months) meetings of the mentors.
In conclusion, although the survey sample in our study was small, the findings suggest directions and strategies for similar hospitals and health systems. Health systems that seek to improve the professional satisfaction of their physicians should be interested in this description of the physician mentoring program at the WCHN and its perceived value by the participants.
Disclosures
Disclosures: Dr. Griner received a consulting fee from the Western Connecticut Health System for his role in developing the mentoring program and participating in the writing of the article. The authors report no conflicts of interest.
The literature focusing on physician mentoring is limited principally to programs at academic medical centers.[1, 2, 3, 4, 5] Traditionally, physicians at academic medical centers who are engaged in research have one or more such advisors. However, many clinical faculties are not engaged in research. Further, little has been written about mentoring initiatives among physicians in full‐time clinical practice.[6] Such initiatives have been suggested as one way of reducing physician stress and improving professional satisfaction, issues of great concern among practicing physicians, particularly hospitalists and primary care physicians.[7]
A mentoring program was initiated at the Western Connecticut Health Network (WCHN) in January 2012. WCHN is a healthcare system comprised of the Danbury and New Milford Hospitals, with 371 licensed beds and a network of salaried primary care and specialty physicians. At Danbury, residency programs are in place in all specialties, and medical students from the University of Vermont rotate through the major clinical specialties.
This article describes the mentoring program at WCHN and gives a preliminary assessment of its value based on a survey of the participants after the first year of the program.
PROGRAM DESCRIPTION
Although the mentoring program was offered to all physicians of the WCHN, the principal groups of interest were the salaried primary care physicians (n=46) and the hospitalists (n=24). The program is a formal system of mentorship and career support, whose goal is to maximize the potential and career satisfaction of each member of the medical staff.
Eight senior physicians from the Departments of Medicine and Surgery served as mentors in their free time. They were selected based on their high regard as members of the medical staff who reflected the attributes of satisfactory mentorsgood listeners who are supportive, nonjudgmental, practical, and enthusiastic.[8] They received informal training through meetings with the program consultant (corresponding author) who had previously established mentoring programs at Massachusetts General Hospital, Boston, Massachusetts and the University of Rochester Medical Center, Rochester, New York.
Mentees were principally hospitalists and primary care physicians in full‐time clinical practice. Practice experiences varied from 2 or 3 to 20 years or more. All hospitalists and some primary care physicians were engaged in teaching residents and/or medical students. Mentees were asked to complete a 1‐page form indicating their goals for the coming year, what issues they would like to discuss with a mentor, and which mentor they wish to meet with. The sessions were scheduled during free time of both mentor and mentee, held in a quiet setting, were confidential, and lasted an hour or more. At the end of each session, mentee and mentor agreed on what was discussed and what next steps each had responsibility for. The mentor subsequently wrote up a summary of the meeting and reviewed it with the mentee for accuracy. Ongoing contacts were in person, phone, or e‐mail initiated either by the mentor or the mentee. Examples of next steps included helping a mentee obtain further training, observe and comment on the mentee's teaching skills, sponsor the mentee for advancement to fellowship in his/her specialty society, or assist the mentee in the preparation of an article for publication. Frequency of meetings varied from a single session on a self‐limited issue to multiple sessions throughout the year.
At the end of the first year of the program, the participants were surveyed by e‐mail about their perceptions of the program. The survey was a structured instrument asking them to indicate what the principal issue or issues were that led them to seek a mentor, whether they felt the mentoring program had been helpful, if so in what way, and if not why not.
SURVEY RESULTS
Twenty‐seven of the 39 participants responded to the survey (69%). Hospitalists were the most likely to participate in the mentoring program (18 of 24) and to respond to the survey. Career planning (52%), balance among personal and professional life (43%), and leadership development (38%) were the most common reasons given for meeting with a mentor. Twenty percent of mentees had no agenda. They simply wanted to talk. Fifteen percent had a specific project in mind about which they needed advice and counsel. All but one survey respondent felt the mentoring program met their expectations by setting goals (62%), planning next steps in their career (60%), gaining new insights (52%), completing a long‐deferred goal (30%), reducing stress (19%), and improving self‐confidence (19%).
Without exception, mentees indicated that their mentors met the criteria used to define a good mentor.[8]
DISCUSSION
One marker of the program's success is that all but 1 of the respondents felt the mentoring sessions met their expectations. Planning next career steps was a principle interest among the hospitalist group. This is not surprising given that many hospitalists are recent graduates of training programs, and their long‐term career plans may not be well defined. The mentoring program helped 3 hospitalists obtain fellowship training. About 1 in 5 mentees indicated that a reduction in stress was an outcome of their mentoring sessions. Recent studies of physician burnout have shown that physicians of first contact are at greatest risk of burnout.[9] Two‐thirds of the physicians participating in the mentoring program fell into this category. In a recent survey of physicians from all specialties across the country, mentoring was suggested as 1 of a number of strategies that organizations could provide to reduce stress and burnout.[7]
Important lessons learned over the first year of the program were that (1) mentees should have protected time to participate; (2) mentor and mentee should be in touch no less often than every 3 to 6 months, even if there is not an ongoing issue they are working on; and (3) substantive improvements in the program resulted from frequent (eg, every 2 months) meetings of the mentors.
In conclusion, although the survey sample in our study was small, the findings suggest directions and strategies for similar hospitals and health systems. Health systems that seek to improve the professional satisfaction of their physicians should be interested in this description of the physician mentoring program at the WCHN and its perceived value by the participants.
Disclosures
Disclosures: Dr. Griner received a consulting fee from the Western Connecticut Health System for his role in developing the mentoring program and participating in the writing of the article. The authors report no conflicts of interest.
- . . . . Support‐challenge‐vision: a model for faculty mentoring. Med Teach. 1998;20:595–597.
- , , , . A descriptive cross‐sectional study of formal mentoring for faculty. Fam Med. 1996;28:434–438.
- Advisor, teacher, role model, friend: on being a mentor to students in science and engineering. Washington, DC: National Academy Press; 1997. Available at: http://www.nap.edu/readingroom/books/mentor. Accessed 5/13/2013.
- , , , . Helping medical school faculty realize their dreams: an innovative, collaborative, mentoring program. Acad Med. 2002;77:377–384.
- , , , . A needs assessment of medical school faculty: caring for the caretakers. J Contin Educ Health Prof. 2003;23:21–29.
- , . Personal and rofessional learning plans—an evaluation of mentoring in general practice. Educ Gen Pract. 1998;9:261–263.
- . Burnout in health care providers. Integr Med. 2013;12:22–24.
- , , . Defining the ideal qualities of mentorship. Am J Med. 2011;124:453–458.
- , , , et al. Burnout and satisfaction with work‐life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385.
- . . . . Support‐challenge‐vision: a model for faculty mentoring. Med Teach. 1998;20:595–597.
- , , , . A descriptive cross‐sectional study of formal mentoring for faculty. Fam Med. 1996;28:434–438.
- Advisor, teacher, role model, friend: on being a mentor to students in science and engineering. Washington, DC: National Academy Press; 1997. Available at: http://www.nap.edu/readingroom/books/mentor. Accessed 5/13/2013.
- , , , . Helping medical school faculty realize their dreams: an innovative, collaborative, mentoring program. Acad Med. 2002;77:377–384.
- , , , . A needs assessment of medical school faculty: caring for the caretakers. J Contin Educ Health Prof. 2003;23:21–29.
- , . Personal and rofessional learning plans—an evaluation of mentoring in general practice. Educ Gen Pract. 1998;9:261–263.
- . Burnout in health care providers. Integr Med. 2013;12:22–24.
- , , . Defining the ideal qualities of mentorship. Am J Med. 2011;124:453–458.
- , , , et al. Burnout and satisfaction with work‐life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385.
Predicting Safe Physician Workloads
Attending physician workload may be compromising patient safety and quality of care. Recent studies show hospitalists, intensivists, and surgeons report that excessive attending physician workload has a negative impact on patient care.[1, 2, 3] Because physician teams and hospitals differ in composition, function, and setting, it is difficult to directly compare one service to another within or between institutions. Identifying physician, team, and hospital characteristics associated with clinicians' impressions of unsafe workload provides physician leaders, hospital administrators, and policymakers with potential risk factors and specific targets for interventions.[4] In this study, we use a national survey of hospitalists to identify the physician, team, and hospital factors associated with physician report of an unsafe workload.
METHODS
We electronically surveyed 890 self‐identified hospitalists enrolled in
RESULTS
Of the 890 physicians contacted, 506 (57%) responded. Full characteristics of respondents are reported elsewhere.[1] Forty percent of physicians (n=202) indicated that their typical inpatient census exceeded safe levels at least monthly. A descriptive comparison of the lower and higher reporters of unsafe levels is provided (Table 1). Higher frequency of reporting an unsafe census was associated with higher percentages of clinical (P=0.004) and inpatient responsibilities (P<0.001) and more time seeing patients without midlevel or housestaff assistance (P=0.001) (Table 1). On the other hand, lower reported unsafe census was associated with more years in practice (P=0.02), greater percentage of personal time (P=0.02), and the presence of any system for census control (patient caps, fixed bed capacity, staffing augmentation plans) (P=0.007) (Table 1). Fixed census caps decreased the odds of reporting an unsafe census by 34% and was the only statistically significant workload control mechanism (odds ratio: 0.66; 95% confidence interval: 0.43‐0.99; P=0.04). There was no association between reported unsafe census and physician age (P=0.42), practice area (P=0.63), organization type (P=0.98), or compensation (salary [P=0.23], bonus [P=0.61], or total [P=0.54]).
| Characteristic | Report of Unsafe Workloada | Univariate Odds Ratio (95% CI) | Reported Effect on Unsafe Workload Frequency | |
|---|---|---|---|---|
| Lower | Higher | |||
| ||||
| Percentage of total work hours devoted to patient care, median [IQR] | 95 [80100] | 100 [90100] | 1.13b (1.041.23)c | Increased |
| Percentage of clinical care that is inpatient, median [IQR] | 75 [5085] | 80 [7090] | 1.21b (1.131.34)d | |
| Percentage of clinical work performed with no assistance from housestaff or midlevels, median [IQR] | 80 [25100] | 90 [50100] | 1.08b (1.031.14)c | |
| Years in practice, median [IQR] | 6 [311] | 5 [310] | 0.85e (0.750.98)f | Decreased |
| Percentage of workday allotted for personal time, median [IQR] | 5 [07] | 3 [05] | 0.50b (0.380.92)f | |
| Systems for increased patient volume, No. (%) | ||||
| Fixed census cap | 87 (30) | 45 (22) | 0.66 (0.430.99)f | |
| Fixed bed capacity | 36 (13) | 24 (12) | 0.94 (0.541.63) | |
| Staffing augmentation | 88 (31) | 58 (29) | 0.91 (0.611.35) | |
| Any system | 217 (76) | 130 (64) | 0.58 (0.390.86)g | |
| Primary practice area of hospital medicine, No. (%) | ||||
| Adult | 211 (73) | 173 (86) | 1 | Equivocal |
| Pediatric | 7 (2) | 1 (0.5) | 0.24 (0.032.10) | |
| Combined, adult and pediatric | 5 (2) | 3 (1) | 0.73 (0.173.10) | |
| Primary role, No. (%) | ||||
| Clinical | 242 (83) | 186 (92) | 1 | |
| Research | 5 (2) | 4 (2) | 1.04 (0.283.93) | |
| Administrative | 14 (5) | 6 (3) | 0.56 (0.211.48) | |
| Physician age, median [IQR], y | 36 [3242] | 37 [3342] | 0.96e (0.861.07) | |
| Compensation, median [IQR], thousands of dollars | ||||
| Salary only | 180 [130200] | 180 [150200] | 0.97h (0.981.05) | |
| Incentive pay only | 10 [025] | 10 [020] | 0.99h (0.941.04) | |
| Total | 190 [140220] | 196 [165220] | 0.99h (0.981.03) | |
| Practice area, No. (%) | ||||
| Urban | 128 (45) | 98 (49) | 1 | |
| Suburban | 126 (44) | 81 (41) | 0.84 (0.571.23) | |
| Rural | 33 (11) | 21 (10) | 0.83 (0.451.53) | |
| Practice location, No. (%) | ||||
| Academic | 82 (29) | 54 (27) | 1 | |
| Community | 153 (53) | 110 (55) | 1.09 (0.721.66) | |
| Veterans hospital | 7 (2) | 4 (2) | 0.87 (0.243.10) | |
| Group | 32 (11) | 25 (13) | 1.19 (0.632.21) | |
| Physician group size, median [IQR] | 12 [620] | 12 [822] | 0.99i (0.981.03) | |
| Localization of patients, No. (%) | ||||
| Multiple units | 179 (61) | 124 (61) | 1 | |
| Single or adjacent unit(s) | 87 (30) | 58 (29) | 0.96 (0.641.44) | |
| Multiple hospitals | 25 (9) | 20 (10) | 1.15 (0.612.17) | |
DISCUSSION
This is the first study to our knowledge to describe factors associated with provider reports of unsafe workload and identifies potential targets for intervention. By identifying modifiable factors affecting workload, such as different team structures with housestaff or midlevels, it may be possible to improve workload, efficiency, and perhaps safety.[5, 6] Less experience, decreased housestaff or midlevel assistance, higher percentages of inpatient and clinical responsibilities, and lack of systems for census control were strongly associated with reports of unsafe workload.
Having any system in place to address increased patient volumes reduced the odds of reporting an unsafe workload. However, only fixed patient census caps were statistically significant. A system that incorporates fixed service or admitting caps may provide greater control on workload but may also result in back‐ups and delays in the emergency room. Similarly, fixed caps may require overflow of patients to less experienced or willing services or increase the number of handoffs, which may adversely affect the quality of patient care. Use of separate admitting teams has the potential to increase efficiency, but is also subject to fluctuations in patient volume and increases the number of handoffs. Each institution should use a multidisciplinary systems approach to address patient throughput and enforce manageable workload such as through the creation of patient flow teams.[7]
Limitations of the study include the relatively small sample of hospitalists and self‐reporting of safety. Because of the diverse characteristics and structures of the individual programs, even if a predictor variable was not missing, if a particular value for that predictor occurred very infrequently, it generated very wide effect estimates. This limited our ability to effectively explore potential confounders and interactions. To our knowledge, this study is the first to explore potential predictors of unsafe attending physician workload. Large national surveys of physicians with greater statistical power can expand upon this initial work and further explore the association between, and interaction of, workload factors and varying perceptions of providers.[4] The most important limitation of this work is that we relied on self‐reporting to define a safe census. We do not have any measured clinical outcomes that can serve to validate the self‐reported impressions. We recognize, however, that adverse events in healthcare require multiple weaknesses to align, and typically, multiple barriers exist to prevent such events. This often makes it difficult to show direct causal links. Additionally, self‐reporting of safety may also be subject to recall bias, because adverse patient outcomes are often particularly memorable. However, high‐reliability organizations recognize the importance of front‐line provider input, such as on the sensitivity of operations (working conditions) and by deferring to expertise (insights and recommendations from providers most knowledgeable of conditions, regardless of seniority).[8]
We acknowledge that several workload factors, such as hospital setting, may not be readily modifiable. However, we also report factors that can be intervened upon, such as assistance[5, 6] or geographic localization of patients.[9, 10] An understanding of both modifiable and fixed factors in healthcare delivery is essential for improving patient care.
This study has significant research implications. It suggests that team structure and physician experience may be used to improve workload safety. Also, particularly if these self‐reported findings are verified using clinical outcomes, providing hospitalists with greater staffing assistance and systems responsive to census fluctuations may improve the safety, quality, and flow of patient care. Future research may identify the association of physician, team, and hospital factors with outcomes and objectively assess targeted interventions to improve both the efficiency and quality of care.
Acknowledgments
The authors thank the Johns Hopkins Clinical Research Network Hospitalists, General Internal Medicine Research in Progress Physicians, and Hospitalist Directors for the Maryland/District of Columbia region for sharing their models of care and comments on the survey content. They also thank Michael Paskavitz, BA (Editor‐in‐Chief) and Brian Driscoll, BA (Managing Editor) from Quantia Communications for all of their technical assistance in administering the survey.
Disclosures: Drs. Michtalik and Brotman had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Michtalik, Pronovost, Brotman. Analysis, interpretation of data: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Drafting of the manuscript: Michtalik, Brotman. Critical revision of the manuscript for important intellectual content: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Dr. Brotman has received compensation from Quantia Communications, not exceeding $10,000 annually, for developing educational content. Dr. Michtalik was supported by NIH grant T32 HP10025‐17‐00 and NIH/Johns Hopkins Institute for Clinical and Translational Research KL2 Award 5KL2RR025006. The Johns Hopkins Hospitalist Scholars Fund provided funding for survey implementation and data acquisition by Quantia Communications. The funders had no role in the design, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–972.
- , , , . Perceived effects of attending physician workload in academic medical intensive care units: a national survey of training program directors. Crit Care Med. 2012;40(2):400–405.
- , , , , . Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026–1028.
- , , , et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist‐physician assistant model vs a traditional resident‐based model. J Hosp Med. 2011;6(3):122–130.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , . Improving patient flow and reducing emergency department crowding: a guide for hospitals. AHRQ publication no. 11(12)−0094. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , , et al. Becoming a high reliability organization: operational advice for hospital leaders. AHRQ publication no. 08–0022. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
Attending physician workload may be compromising patient safety and quality of care. Recent studies show hospitalists, intensivists, and surgeons report that excessive attending physician workload has a negative impact on patient care.[1, 2, 3] Because physician teams and hospitals differ in composition, function, and setting, it is difficult to directly compare one service to another within or between institutions. Identifying physician, team, and hospital characteristics associated with clinicians' impressions of unsafe workload provides physician leaders, hospital administrators, and policymakers with potential risk factors and specific targets for interventions.[4] In this study, we use a national survey of hospitalists to identify the physician, team, and hospital factors associated with physician report of an unsafe workload.
METHODS
We electronically surveyed 890 self‐identified hospitalists enrolled in
RESULTS
Of the 890 physicians contacted, 506 (57%) responded. Full characteristics of respondents are reported elsewhere.[1] Forty percent of physicians (n=202) indicated that their typical inpatient census exceeded safe levels at least monthly. A descriptive comparison of the lower and higher reporters of unsafe levels is provided (Table 1). Higher frequency of reporting an unsafe census was associated with higher percentages of clinical (P=0.004) and inpatient responsibilities (P<0.001) and more time seeing patients without midlevel or housestaff assistance (P=0.001) (Table 1). On the other hand, lower reported unsafe census was associated with more years in practice (P=0.02), greater percentage of personal time (P=0.02), and the presence of any system for census control (patient caps, fixed bed capacity, staffing augmentation plans) (P=0.007) (Table 1). Fixed census caps decreased the odds of reporting an unsafe census by 34% and was the only statistically significant workload control mechanism (odds ratio: 0.66; 95% confidence interval: 0.43‐0.99; P=0.04). There was no association between reported unsafe census and physician age (P=0.42), practice area (P=0.63), organization type (P=0.98), or compensation (salary [P=0.23], bonus [P=0.61], or total [P=0.54]).
| Characteristic | Report of Unsafe Workloada | Univariate Odds Ratio (95% CI) | Reported Effect on Unsafe Workload Frequency | |
|---|---|---|---|---|
| Lower | Higher | |||
| ||||
| Percentage of total work hours devoted to patient care, median [IQR] | 95 [80100] | 100 [90100] | 1.13b (1.041.23)c | Increased |
| Percentage of clinical care that is inpatient, median [IQR] | 75 [5085] | 80 [7090] | 1.21b (1.131.34)d | |
| Percentage of clinical work performed with no assistance from housestaff or midlevels, median [IQR] | 80 [25100] | 90 [50100] | 1.08b (1.031.14)c | |
| Years in practice, median [IQR] | 6 [311] | 5 [310] | 0.85e (0.750.98)f | Decreased |
| Percentage of workday allotted for personal time, median [IQR] | 5 [07] | 3 [05] | 0.50b (0.380.92)f | |
| Systems for increased patient volume, No. (%) | ||||
| Fixed census cap | 87 (30) | 45 (22) | 0.66 (0.430.99)f | |
| Fixed bed capacity | 36 (13) | 24 (12) | 0.94 (0.541.63) | |
| Staffing augmentation | 88 (31) | 58 (29) | 0.91 (0.611.35) | |
| Any system | 217 (76) | 130 (64) | 0.58 (0.390.86)g | |
| Primary practice area of hospital medicine, No. (%) | ||||
| Adult | 211 (73) | 173 (86) | 1 | Equivocal |
| Pediatric | 7 (2) | 1 (0.5) | 0.24 (0.032.10) | |
| Combined, adult and pediatric | 5 (2) | 3 (1) | 0.73 (0.173.10) | |
| Primary role, No. (%) | ||||
| Clinical | 242 (83) | 186 (92) | 1 | |
| Research | 5 (2) | 4 (2) | 1.04 (0.283.93) | |
| Administrative | 14 (5) | 6 (3) | 0.56 (0.211.48) | |
| Physician age, median [IQR], y | 36 [3242] | 37 [3342] | 0.96e (0.861.07) | |
| Compensation, median [IQR], thousands of dollars | ||||
| Salary only | 180 [130200] | 180 [150200] | 0.97h (0.981.05) | |
| Incentive pay only | 10 [025] | 10 [020] | 0.99h (0.941.04) | |
| Total | 190 [140220] | 196 [165220] | 0.99h (0.981.03) | |
| Practice area, No. (%) | ||||
| Urban | 128 (45) | 98 (49) | 1 | |
| Suburban | 126 (44) | 81 (41) | 0.84 (0.571.23) | |
| Rural | 33 (11) | 21 (10) | 0.83 (0.451.53) | |
| Practice location, No. (%) | ||||
| Academic | 82 (29) | 54 (27) | 1 | |
| Community | 153 (53) | 110 (55) | 1.09 (0.721.66) | |
| Veterans hospital | 7 (2) | 4 (2) | 0.87 (0.243.10) | |
| Group | 32 (11) | 25 (13) | 1.19 (0.632.21) | |
| Physician group size, median [IQR] | 12 [620] | 12 [822] | 0.99i (0.981.03) | |
| Localization of patients, No. (%) | ||||
| Multiple units | 179 (61) | 124 (61) | 1 | |
| Single or adjacent unit(s) | 87 (30) | 58 (29) | 0.96 (0.641.44) | |
| Multiple hospitals | 25 (9) | 20 (10) | 1.15 (0.612.17) | |
DISCUSSION
This is the first study to our knowledge to describe factors associated with provider reports of unsafe workload and identifies potential targets for intervention. By identifying modifiable factors affecting workload, such as different team structures with housestaff or midlevels, it may be possible to improve workload, efficiency, and perhaps safety.[5, 6] Less experience, decreased housestaff or midlevel assistance, higher percentages of inpatient and clinical responsibilities, and lack of systems for census control were strongly associated with reports of unsafe workload.
Having any system in place to address increased patient volumes reduced the odds of reporting an unsafe workload. However, only fixed patient census caps were statistically significant. A system that incorporates fixed service or admitting caps may provide greater control on workload but may also result in back‐ups and delays in the emergency room. Similarly, fixed caps may require overflow of patients to less experienced or willing services or increase the number of handoffs, which may adversely affect the quality of patient care. Use of separate admitting teams has the potential to increase efficiency, but is also subject to fluctuations in patient volume and increases the number of handoffs. Each institution should use a multidisciplinary systems approach to address patient throughput and enforce manageable workload such as through the creation of patient flow teams.[7]
Limitations of the study include the relatively small sample of hospitalists and self‐reporting of safety. Because of the diverse characteristics and structures of the individual programs, even if a predictor variable was not missing, if a particular value for that predictor occurred very infrequently, it generated very wide effect estimates. This limited our ability to effectively explore potential confounders and interactions. To our knowledge, this study is the first to explore potential predictors of unsafe attending physician workload. Large national surveys of physicians with greater statistical power can expand upon this initial work and further explore the association between, and interaction of, workload factors and varying perceptions of providers.[4] The most important limitation of this work is that we relied on self‐reporting to define a safe census. We do not have any measured clinical outcomes that can serve to validate the self‐reported impressions. We recognize, however, that adverse events in healthcare require multiple weaknesses to align, and typically, multiple barriers exist to prevent such events. This often makes it difficult to show direct causal links. Additionally, self‐reporting of safety may also be subject to recall bias, because adverse patient outcomes are often particularly memorable. However, high‐reliability organizations recognize the importance of front‐line provider input, such as on the sensitivity of operations (working conditions) and by deferring to expertise (insights and recommendations from providers most knowledgeable of conditions, regardless of seniority).[8]
We acknowledge that several workload factors, such as hospital setting, may not be readily modifiable. However, we also report factors that can be intervened upon, such as assistance[5, 6] or geographic localization of patients.[9, 10] An understanding of both modifiable and fixed factors in healthcare delivery is essential for improving patient care.
This study has significant research implications. It suggests that team structure and physician experience may be used to improve workload safety. Also, particularly if these self‐reported findings are verified using clinical outcomes, providing hospitalists with greater staffing assistance and systems responsive to census fluctuations may improve the safety, quality, and flow of patient care. Future research may identify the association of physician, team, and hospital factors with outcomes and objectively assess targeted interventions to improve both the efficiency and quality of care.
Acknowledgments
The authors thank the Johns Hopkins Clinical Research Network Hospitalists, General Internal Medicine Research in Progress Physicians, and Hospitalist Directors for the Maryland/District of Columbia region for sharing their models of care and comments on the survey content. They also thank Michael Paskavitz, BA (Editor‐in‐Chief) and Brian Driscoll, BA (Managing Editor) from Quantia Communications for all of their technical assistance in administering the survey.
Disclosures: Drs. Michtalik and Brotman had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Michtalik, Pronovost, Brotman. Analysis, interpretation of data: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Drafting of the manuscript: Michtalik, Brotman. Critical revision of the manuscript for important intellectual content: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Dr. Brotman has received compensation from Quantia Communications, not exceeding $10,000 annually, for developing educational content. Dr. Michtalik was supported by NIH grant T32 HP10025‐17‐00 and NIH/Johns Hopkins Institute for Clinical and Translational Research KL2 Award 5KL2RR025006. The Johns Hopkins Hospitalist Scholars Fund provided funding for survey implementation and data acquisition by Quantia Communications. The funders had no role in the design, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
Attending physician workload may be compromising patient safety and quality of care. Recent studies show hospitalists, intensivists, and surgeons report that excessive attending physician workload has a negative impact on patient care.[1, 2, 3] Because physician teams and hospitals differ in composition, function, and setting, it is difficult to directly compare one service to another within or between institutions. Identifying physician, team, and hospital characteristics associated with clinicians' impressions of unsafe workload provides physician leaders, hospital administrators, and policymakers with potential risk factors and specific targets for interventions.[4] In this study, we use a national survey of hospitalists to identify the physician, team, and hospital factors associated with physician report of an unsafe workload.
METHODS
We electronically surveyed 890 self‐identified hospitalists enrolled in
RESULTS
Of the 890 physicians contacted, 506 (57%) responded. Full characteristics of respondents are reported elsewhere.[1] Forty percent of physicians (n=202) indicated that their typical inpatient census exceeded safe levels at least monthly. A descriptive comparison of the lower and higher reporters of unsafe levels is provided (Table 1). Higher frequency of reporting an unsafe census was associated with higher percentages of clinical (P=0.004) and inpatient responsibilities (P<0.001) and more time seeing patients without midlevel or housestaff assistance (P=0.001) (Table 1). On the other hand, lower reported unsafe census was associated with more years in practice (P=0.02), greater percentage of personal time (P=0.02), and the presence of any system for census control (patient caps, fixed bed capacity, staffing augmentation plans) (P=0.007) (Table 1). Fixed census caps decreased the odds of reporting an unsafe census by 34% and was the only statistically significant workload control mechanism (odds ratio: 0.66; 95% confidence interval: 0.43‐0.99; P=0.04). There was no association between reported unsafe census and physician age (P=0.42), practice area (P=0.63), organization type (P=0.98), or compensation (salary [P=0.23], bonus [P=0.61], or total [P=0.54]).
| Characteristic | Report of Unsafe Workloada | Univariate Odds Ratio (95% CI) | Reported Effect on Unsafe Workload Frequency | |
|---|---|---|---|---|
| Lower | Higher | |||
| ||||
| Percentage of total work hours devoted to patient care, median [IQR] | 95 [80100] | 100 [90100] | 1.13b (1.041.23)c | Increased |
| Percentage of clinical care that is inpatient, median [IQR] | 75 [5085] | 80 [7090] | 1.21b (1.131.34)d | |
| Percentage of clinical work performed with no assistance from housestaff or midlevels, median [IQR] | 80 [25100] | 90 [50100] | 1.08b (1.031.14)c | |
| Years in practice, median [IQR] | 6 [311] | 5 [310] | 0.85e (0.750.98)f | Decreased |
| Percentage of workday allotted for personal time, median [IQR] | 5 [07] | 3 [05] | 0.50b (0.380.92)f | |
| Systems for increased patient volume, No. (%) | ||||
| Fixed census cap | 87 (30) | 45 (22) | 0.66 (0.430.99)f | |
| Fixed bed capacity | 36 (13) | 24 (12) | 0.94 (0.541.63) | |
| Staffing augmentation | 88 (31) | 58 (29) | 0.91 (0.611.35) | |
| Any system | 217 (76) | 130 (64) | 0.58 (0.390.86)g | |
| Primary practice area of hospital medicine, No. (%) | ||||
| Adult | 211 (73) | 173 (86) | 1 | Equivocal |
| Pediatric | 7 (2) | 1 (0.5) | 0.24 (0.032.10) | |
| Combined, adult and pediatric | 5 (2) | 3 (1) | 0.73 (0.173.10) | |
| Primary role, No. (%) | ||||
| Clinical | 242 (83) | 186 (92) | 1 | |
| Research | 5 (2) | 4 (2) | 1.04 (0.283.93) | |
| Administrative | 14 (5) | 6 (3) | 0.56 (0.211.48) | |
| Physician age, median [IQR], y | 36 [3242] | 37 [3342] | 0.96e (0.861.07) | |
| Compensation, median [IQR], thousands of dollars | ||||
| Salary only | 180 [130200] | 180 [150200] | 0.97h (0.981.05) | |
| Incentive pay only | 10 [025] | 10 [020] | 0.99h (0.941.04) | |
| Total | 190 [140220] | 196 [165220] | 0.99h (0.981.03) | |
| Practice area, No. (%) | ||||
| Urban | 128 (45) | 98 (49) | 1 | |
| Suburban | 126 (44) | 81 (41) | 0.84 (0.571.23) | |
| Rural | 33 (11) | 21 (10) | 0.83 (0.451.53) | |
| Practice location, No. (%) | ||||
| Academic | 82 (29) | 54 (27) | 1 | |
| Community | 153 (53) | 110 (55) | 1.09 (0.721.66) | |
| Veterans hospital | 7 (2) | 4 (2) | 0.87 (0.243.10) | |
| Group | 32 (11) | 25 (13) | 1.19 (0.632.21) | |
| Physician group size, median [IQR] | 12 [620] | 12 [822] | 0.99i (0.981.03) | |
| Localization of patients, No. (%) | ||||
| Multiple units | 179 (61) | 124 (61) | 1 | |
| Single or adjacent unit(s) | 87 (30) | 58 (29) | 0.96 (0.641.44) | |
| Multiple hospitals | 25 (9) | 20 (10) | 1.15 (0.612.17) | |
DISCUSSION
This is the first study to our knowledge to describe factors associated with provider reports of unsafe workload and identifies potential targets for intervention. By identifying modifiable factors affecting workload, such as different team structures with housestaff or midlevels, it may be possible to improve workload, efficiency, and perhaps safety.[5, 6] Less experience, decreased housestaff or midlevel assistance, higher percentages of inpatient and clinical responsibilities, and lack of systems for census control were strongly associated with reports of unsafe workload.
Having any system in place to address increased patient volumes reduced the odds of reporting an unsafe workload. However, only fixed patient census caps were statistically significant. A system that incorporates fixed service or admitting caps may provide greater control on workload but may also result in back‐ups and delays in the emergency room. Similarly, fixed caps may require overflow of patients to less experienced or willing services or increase the number of handoffs, which may adversely affect the quality of patient care. Use of separate admitting teams has the potential to increase efficiency, but is also subject to fluctuations in patient volume and increases the number of handoffs. Each institution should use a multidisciplinary systems approach to address patient throughput and enforce manageable workload such as through the creation of patient flow teams.[7]
Limitations of the study include the relatively small sample of hospitalists and self‐reporting of safety. Because of the diverse characteristics and structures of the individual programs, even if a predictor variable was not missing, if a particular value for that predictor occurred very infrequently, it generated very wide effect estimates. This limited our ability to effectively explore potential confounders and interactions. To our knowledge, this study is the first to explore potential predictors of unsafe attending physician workload. Large national surveys of physicians with greater statistical power can expand upon this initial work and further explore the association between, and interaction of, workload factors and varying perceptions of providers.[4] The most important limitation of this work is that we relied on self‐reporting to define a safe census. We do not have any measured clinical outcomes that can serve to validate the self‐reported impressions. We recognize, however, that adverse events in healthcare require multiple weaknesses to align, and typically, multiple barriers exist to prevent such events. This often makes it difficult to show direct causal links. Additionally, self‐reporting of safety may also be subject to recall bias, because adverse patient outcomes are often particularly memorable. However, high‐reliability organizations recognize the importance of front‐line provider input, such as on the sensitivity of operations (working conditions) and by deferring to expertise (insights and recommendations from providers most knowledgeable of conditions, regardless of seniority).[8]
We acknowledge that several workload factors, such as hospital setting, may not be readily modifiable. However, we also report factors that can be intervened upon, such as assistance[5, 6] or geographic localization of patients.[9, 10] An understanding of both modifiable and fixed factors in healthcare delivery is essential for improving patient care.
This study has significant research implications. It suggests that team structure and physician experience may be used to improve workload safety. Also, particularly if these self‐reported findings are verified using clinical outcomes, providing hospitalists with greater staffing assistance and systems responsive to census fluctuations may improve the safety, quality, and flow of patient care. Future research may identify the association of physician, team, and hospital factors with outcomes and objectively assess targeted interventions to improve both the efficiency and quality of care.
Acknowledgments
The authors thank the Johns Hopkins Clinical Research Network Hospitalists, General Internal Medicine Research in Progress Physicians, and Hospitalist Directors for the Maryland/District of Columbia region for sharing their models of care and comments on the survey content. They also thank Michael Paskavitz, BA (Editor‐in‐Chief) and Brian Driscoll, BA (Managing Editor) from Quantia Communications for all of their technical assistance in administering the survey.
Disclosures: Drs. Michtalik and Brotman had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Michtalik, Pronovost, Brotman. Analysis, interpretation of data: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Drafting of the manuscript: Michtalik, Brotman. Critical revision of the manuscript for important intellectual content: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Dr. Brotman has received compensation from Quantia Communications, not exceeding $10,000 annually, for developing educational content. Dr. Michtalik was supported by NIH grant T32 HP10025‐17‐00 and NIH/Johns Hopkins Institute for Clinical and Translational Research KL2 Award 5KL2RR025006. The Johns Hopkins Hospitalist Scholars Fund provided funding for survey implementation and data acquisition by Quantia Communications. The funders had no role in the design, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–972.
- , , , . Perceived effects of attending physician workload in academic medical intensive care units: a national survey of training program directors. Crit Care Med. 2012;40(2):400–405.
- , , , , . Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026–1028.
- , , , et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist‐physician assistant model vs a traditional resident‐based model. J Hosp Med. 2011;6(3):122–130.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , . Improving patient flow and reducing emergency department crowding: a guide for hospitals. AHRQ publication no. 11(12)−0094. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , , et al. Becoming a high reliability organization: operational advice for hospital leaders. AHRQ publication no. 08–0022. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–972.
- , , , . Perceived effects of attending physician workload in academic medical intensive care units: a national survey of training program directors. Crit Care Med. 2012;40(2):400–405.
- , , , , . Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026–1028.
- , , , et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist‐physician assistant model vs a traditional resident‐based model. J Hosp Med. 2011;6(3):122–130.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , . Improving patient flow and reducing emergency department crowding: a guide for hospitals. AHRQ publication no. 11(12)−0094. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , , et al. Becoming a high reliability organization: operational advice for hospital leaders. AHRQ publication no. 08–0022. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
Ethnic Differences in Hospice Enrollment
Studies have documented the persisting lower rates of hospice enrollment among ethnic minority groups.[1, 2] Given the positive outcomes related to hospice enrollment,[3] investigating interventions that may reduce these disparities is critical.
Inpatient palliative care (IPC) programs were developed to improve pain and symptom management, provide patients with holistic and comprehensive prognosis and treatment options, and help patient and families clarify goals of care.[4] Although significant evidence of IPC program effectiveness in improving patient outcomes exists,[5] studies have not examined the ability of IPC programs to diminish ethnic disparities in access to hospice. We conducted a retrospective cohort study to determine if ethnic differences in hospice enrollment are experienced among patients following receipt of IPC consultation.
METHODS
A retrospective study was conducted in a nonprofit health maintenance organization medical center. The sample included seriously ill patients aged 65 years and over who received an IPC consultation and survived to hospital discharge. Data were collected from IPC databases, IPC consultation checklist (which included recording of code status discussion), and electronic medical records. The IPC team recorded discharge disposition including discharge to hospice care, home‐based palliative care (a standard program similar to hospice but offered for patients with an estimated prognosis of 1 year or less and without the caveat of foregoing curative care),[6] home with home healthcare, nursing facility, and home with standard outpatient care. Ethnicity was collected via patient report.
2 and t tests were conducted to compare those admitted to hospice with those who were not. We used logistic regression to determine the effects of ethnicity on enrollment in hospice, adjusting for demographics and clinical factors. We conducted analysis using IBM SPSS 19 (IBM, Armonk, NY).
FINDINGS
From 2007 to 2009, 408 patients received IPC consults and were subsequently discharged from the hospital. Forty‐four had missing data on ethnicity or discharge disposition, leaving 364 in the analytic sample. The mean age was 80.1 years (standard deviation [SD]=8.2), and 48.9% were female. The sample was diverse; 42.6% were white, 25.5% Latino, 23.1% black, and 8.8% of other ethnic background. Primary diagnosis included cancer (33.8%), congestive heart failure (CHF) (17.4%), coronary artery disease (12.6%), dementia (12.4%), chronic obstructive pulmonary disease (6%), cerebral vascular accident (CVA) (5.2%), and other conditions (13.6%). More than half (57.7%) were discharged to hospice, 15.4% to home‐based palliative care,[6] 14.6% to a nursing facility, 8.2% to home with usual outpatient care, and 4.1% to home with home healthcare. Code status was discussed by the IPC team among 81% of the patients, with no difference between ethnic groups.
Those discharged to hospice were older (80.8, SD=8.4 vs 79.1, SD=7.8), more likely to have cancer (71.5%) or CVA (79.5%) and less likely to have end stage renal disease (28.6%) or CHF (39%), and more likely to have had a code discussion (85.8%). There were no differences between hospice users and nonusers in gender, marital status, ethnicity, and number of chronic conditions (Table 1).
| Variable | All, N=364 | Hospice Users, n=210 | Nonhospice Users, n=154 | P Value |
|---|---|---|---|---|
| ||||
| Age, y, mean (SD) | 80.1 (8.2) | 80.8 (8.4) | 79.1 (7.8) | 0.049 |
| Gender (female), % | 48.9 | 56.2 | 43.8 | 0.568 |
| Ethnicity, % | 0.702 | |||
| White | 42.6 | 43.3 | 41.6 | |
| Latino | 25.5 | 27.1 | 23.4 | |
| African American | 23.1 | 21.4 | 25.3 | |
| Other | 8.8 | 8.1 | 9.7 | |
| Marital status, % | 0.809 | |||
| Married | 45.6 | 43.8 | 48.1 | |
| Widowed | 36.0 | 38.1 | 33.1 | |
| Divorced | 7.7 | 7.6 | 7.8 | |
| Other | 7.7 | 7.6 | 7.8 | |
| Missing | 3.0 | 2.9 | 3.2 | |
| Diagnosis, % | <0.001 | |||
| Cancer | 33.8 | 42.1 | 22.9 | |
| CHF | 16.2 | 11.0 | 23.5 | |
| CAD | 12.6 | 12.4 | 13.1 | |
| Dementia | 12.4 | 12.4 | 12.4 | |
| COPD | 6.0 | 5.3 | 7.2 | |
| CVA | 5.2 | 7.2 | 2.6 | |
| Other | 13.6 | 9.6 | 18.3 | |
| Number of chronic conditions, mean (SD) | 1.0 | 1.7 (0.8) | 1.7 (0.9) | 0.949 |
| Code status discussed, % | 81.1 | 87.0 | 72.8 | 0.001 |
Significant differences between hospice users and nonusers were controlled in a regression adjusting for age, gender, marital status, and number of chronic conditions. Compared to whites, no significant differences in hospice use were found for blacks (odds ratio [OR]: 0.67; 95% confidence interval [CI]: 0.37‐1.21), Latinos (OR: 1.24; 95% CI: 0.68‐2.25), or other ethnic groups (OR: 0.78; 95% CI: 0.34‐1.56). Compared with other diagnoses, those with cancer (OR: 3.66; 95% CI: 1.77‐7.59) and older patients (OR: 1.05; 95% CI: 1.01‐1.08) were significantly more likely to receive hospice care following IPC consult. Those discussing code status were twice as likely to be discharged to hospice (OR: 2.14; 95% CI: 1.20‐3.79).
DISCUSSION
This study found similar rates of hospice enrollment following IPC consult among Latinos, blacks, and other ethnic groups as compared with whites. Others found comparable rates of advance directive completion between whites and African Americans following IPC consultation,[7]and that IPC intensity resulting in a plan of care was highly associated with receipt of hospice care.[8] Likewise, our study found that discussion of code status, another marker of intensity, was positively associated with hospice use.
Our findings among patients receiving IPC consultation contrast with previous studies examining ethnic variation in hospice use among general samples of decedents. A study of California dual eligibles found that blacks were 26% and Asians 34% less likely than whites to use hospice. Others have found similar results among patients with CHF and lung cancer.[9, 10]
Misconceptions and lack of awareness, knowledge, and trust in healthcare providers serve as barriers to hospice care for minorities.[11, 12] IPC consultations may overcome these barriers by discussing goals of care including discussing the condition, eliciting patient/family understanding of the condition, and presenting options for code status.
This study employed a single‐cohort design without a comparison group. It was conducted within a health maintenance organization with strong hospice and palliative care programs and may not represent other settings. Nevertheless, this study provides promise for IPC consultation to increase equitable access to hospice care among minority groups. Further studies are needed to confirm the preliminary findings reported here.
Disclosures: Supported in part by a career development award from the National Palliative Care Research Center and by a grant from the Archstone Foundation. Evie Vesper and Dr. Rebecca Goldstein were employees of the healthcare organization at the time of the study. Susan Enguidanos received compensation for project evaluation during the original study. The sponsors had no role in the design, implementation, or analysis of the study. The authors report no conflicts of interest.
- , , . Ethnic variation in site of death among Medicaid/Medicare dually eligible older adults. J Am Geriatr Soc. 2005;53(8):1411–1416.
- . Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008;11(5):763–768.
- . The Medicare hospice benefit: 15 years of success. J Palliat Med. 1998;1(2):139–146.
- . Palliative care in hospitals. J Hosp Med. 2006;1(1):21–28.
- , , , et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190.
- , , , et al. Increased satisfaction with care and lower costs: results of a randomized trial of in‐home palliative care. J Am Geriatr Soc. 2007;55(7):993–1000.
- , , , et al. Ethnicity, race, and advance directives in an inpatient palliative care consultation service. Palliat Support Care. 2012;6(1):1–7.
- , , . Hospice referrals and code status: outcomes of inpatient palliative care consultations among Asian Americans and Pacific Islanders with cancer. J Pain Symptom Manage. 2011;42(4):557–564.
- , , , , . Racial differences in hospice use and patterns of care after enrollment in hospice among Medicare beneficiaries with heart failure. Am Heart J. 2012;163(6):987–993.
- , , , et al. Racial disparities in length of stay in hospice care by tumor stage in a large elderly cohort with non‐small cell lung cancer. Palliat Med. 2012;26(1):61–71.
- , , , , . Knowledge, attitudes and beliefs about end‐of‐life care among inner‐city African Americans and Latino/Hispanic Americans. J Palliat Med. 2004;7(2):247–256.
- , , . Does caregiver knowledge matter for hospice enrollment and beyond? Pilot study of minority hospice patients. Am J Hospice Palliat Med. 2009;26(3):165–171.
Studies have documented the persisting lower rates of hospice enrollment among ethnic minority groups.[1, 2] Given the positive outcomes related to hospice enrollment,[3] investigating interventions that may reduce these disparities is critical.
Inpatient palliative care (IPC) programs were developed to improve pain and symptom management, provide patients with holistic and comprehensive prognosis and treatment options, and help patient and families clarify goals of care.[4] Although significant evidence of IPC program effectiveness in improving patient outcomes exists,[5] studies have not examined the ability of IPC programs to diminish ethnic disparities in access to hospice. We conducted a retrospective cohort study to determine if ethnic differences in hospice enrollment are experienced among patients following receipt of IPC consultation.
METHODS
A retrospective study was conducted in a nonprofit health maintenance organization medical center. The sample included seriously ill patients aged 65 years and over who received an IPC consultation and survived to hospital discharge. Data were collected from IPC databases, IPC consultation checklist (which included recording of code status discussion), and electronic medical records. The IPC team recorded discharge disposition including discharge to hospice care, home‐based palliative care (a standard program similar to hospice but offered for patients with an estimated prognosis of 1 year or less and without the caveat of foregoing curative care),[6] home with home healthcare, nursing facility, and home with standard outpatient care. Ethnicity was collected via patient report.
2 and t tests were conducted to compare those admitted to hospice with those who were not. We used logistic regression to determine the effects of ethnicity on enrollment in hospice, adjusting for demographics and clinical factors. We conducted analysis using IBM SPSS 19 (IBM, Armonk, NY).
FINDINGS
From 2007 to 2009, 408 patients received IPC consults and were subsequently discharged from the hospital. Forty‐four had missing data on ethnicity or discharge disposition, leaving 364 in the analytic sample. The mean age was 80.1 years (standard deviation [SD]=8.2), and 48.9% were female. The sample was diverse; 42.6% were white, 25.5% Latino, 23.1% black, and 8.8% of other ethnic background. Primary diagnosis included cancer (33.8%), congestive heart failure (CHF) (17.4%), coronary artery disease (12.6%), dementia (12.4%), chronic obstructive pulmonary disease (6%), cerebral vascular accident (CVA) (5.2%), and other conditions (13.6%). More than half (57.7%) were discharged to hospice, 15.4% to home‐based palliative care,[6] 14.6% to a nursing facility, 8.2% to home with usual outpatient care, and 4.1% to home with home healthcare. Code status was discussed by the IPC team among 81% of the patients, with no difference between ethnic groups.
Those discharged to hospice were older (80.8, SD=8.4 vs 79.1, SD=7.8), more likely to have cancer (71.5%) or CVA (79.5%) and less likely to have end stage renal disease (28.6%) or CHF (39%), and more likely to have had a code discussion (85.8%). There were no differences between hospice users and nonusers in gender, marital status, ethnicity, and number of chronic conditions (Table 1).
| Variable | All, N=364 | Hospice Users, n=210 | Nonhospice Users, n=154 | P Value |
|---|---|---|---|---|
| ||||
| Age, y, mean (SD) | 80.1 (8.2) | 80.8 (8.4) | 79.1 (7.8) | 0.049 |
| Gender (female), % | 48.9 | 56.2 | 43.8 | 0.568 |
| Ethnicity, % | 0.702 | |||
| White | 42.6 | 43.3 | 41.6 | |
| Latino | 25.5 | 27.1 | 23.4 | |
| African American | 23.1 | 21.4 | 25.3 | |
| Other | 8.8 | 8.1 | 9.7 | |
| Marital status, % | 0.809 | |||
| Married | 45.6 | 43.8 | 48.1 | |
| Widowed | 36.0 | 38.1 | 33.1 | |
| Divorced | 7.7 | 7.6 | 7.8 | |
| Other | 7.7 | 7.6 | 7.8 | |
| Missing | 3.0 | 2.9 | 3.2 | |
| Diagnosis, % | <0.001 | |||
| Cancer | 33.8 | 42.1 | 22.9 | |
| CHF | 16.2 | 11.0 | 23.5 | |
| CAD | 12.6 | 12.4 | 13.1 | |
| Dementia | 12.4 | 12.4 | 12.4 | |
| COPD | 6.0 | 5.3 | 7.2 | |
| CVA | 5.2 | 7.2 | 2.6 | |
| Other | 13.6 | 9.6 | 18.3 | |
| Number of chronic conditions, mean (SD) | 1.0 | 1.7 (0.8) | 1.7 (0.9) | 0.949 |
| Code status discussed, % | 81.1 | 87.0 | 72.8 | 0.001 |
Significant differences between hospice users and nonusers were controlled in a regression adjusting for age, gender, marital status, and number of chronic conditions. Compared to whites, no significant differences in hospice use were found for blacks (odds ratio [OR]: 0.67; 95% confidence interval [CI]: 0.37‐1.21), Latinos (OR: 1.24; 95% CI: 0.68‐2.25), or other ethnic groups (OR: 0.78; 95% CI: 0.34‐1.56). Compared with other diagnoses, those with cancer (OR: 3.66; 95% CI: 1.77‐7.59) and older patients (OR: 1.05; 95% CI: 1.01‐1.08) were significantly more likely to receive hospice care following IPC consult. Those discussing code status were twice as likely to be discharged to hospice (OR: 2.14; 95% CI: 1.20‐3.79).
DISCUSSION
This study found similar rates of hospice enrollment following IPC consult among Latinos, blacks, and other ethnic groups as compared with whites. Others found comparable rates of advance directive completion between whites and African Americans following IPC consultation,[7]and that IPC intensity resulting in a plan of care was highly associated with receipt of hospice care.[8] Likewise, our study found that discussion of code status, another marker of intensity, was positively associated with hospice use.
Our findings among patients receiving IPC consultation contrast with previous studies examining ethnic variation in hospice use among general samples of decedents. A study of California dual eligibles found that blacks were 26% and Asians 34% less likely than whites to use hospice. Others have found similar results among patients with CHF and lung cancer.[9, 10]
Misconceptions and lack of awareness, knowledge, and trust in healthcare providers serve as barriers to hospice care for minorities.[11, 12] IPC consultations may overcome these barriers by discussing goals of care including discussing the condition, eliciting patient/family understanding of the condition, and presenting options for code status.
This study employed a single‐cohort design without a comparison group. It was conducted within a health maintenance organization with strong hospice and palliative care programs and may not represent other settings. Nevertheless, this study provides promise for IPC consultation to increase equitable access to hospice care among minority groups. Further studies are needed to confirm the preliminary findings reported here.
Disclosures: Supported in part by a career development award from the National Palliative Care Research Center and by a grant from the Archstone Foundation. Evie Vesper and Dr. Rebecca Goldstein were employees of the healthcare organization at the time of the study. Susan Enguidanos received compensation for project evaluation during the original study. The sponsors had no role in the design, implementation, or analysis of the study. The authors report no conflicts of interest.
Studies have documented the persisting lower rates of hospice enrollment among ethnic minority groups.[1, 2] Given the positive outcomes related to hospice enrollment,[3] investigating interventions that may reduce these disparities is critical.
Inpatient palliative care (IPC) programs were developed to improve pain and symptom management, provide patients with holistic and comprehensive prognosis and treatment options, and help patient and families clarify goals of care.[4] Although significant evidence of IPC program effectiveness in improving patient outcomes exists,[5] studies have not examined the ability of IPC programs to diminish ethnic disparities in access to hospice. We conducted a retrospective cohort study to determine if ethnic differences in hospice enrollment are experienced among patients following receipt of IPC consultation.
METHODS
A retrospective study was conducted in a nonprofit health maintenance organization medical center. The sample included seriously ill patients aged 65 years and over who received an IPC consultation and survived to hospital discharge. Data were collected from IPC databases, IPC consultation checklist (which included recording of code status discussion), and electronic medical records. The IPC team recorded discharge disposition including discharge to hospice care, home‐based palliative care (a standard program similar to hospice but offered for patients with an estimated prognosis of 1 year or less and without the caveat of foregoing curative care),[6] home with home healthcare, nursing facility, and home with standard outpatient care. Ethnicity was collected via patient report.
2 and t tests were conducted to compare those admitted to hospice with those who were not. We used logistic regression to determine the effects of ethnicity on enrollment in hospice, adjusting for demographics and clinical factors. We conducted analysis using IBM SPSS 19 (IBM, Armonk, NY).
FINDINGS
From 2007 to 2009, 408 patients received IPC consults and were subsequently discharged from the hospital. Forty‐four had missing data on ethnicity or discharge disposition, leaving 364 in the analytic sample. The mean age was 80.1 years (standard deviation [SD]=8.2), and 48.9% were female. The sample was diverse; 42.6% were white, 25.5% Latino, 23.1% black, and 8.8% of other ethnic background. Primary diagnosis included cancer (33.8%), congestive heart failure (CHF) (17.4%), coronary artery disease (12.6%), dementia (12.4%), chronic obstructive pulmonary disease (6%), cerebral vascular accident (CVA) (5.2%), and other conditions (13.6%). More than half (57.7%) were discharged to hospice, 15.4% to home‐based palliative care,[6] 14.6% to a nursing facility, 8.2% to home with usual outpatient care, and 4.1% to home with home healthcare. Code status was discussed by the IPC team among 81% of the patients, with no difference between ethnic groups.
Those discharged to hospice were older (80.8, SD=8.4 vs 79.1, SD=7.8), more likely to have cancer (71.5%) or CVA (79.5%) and less likely to have end stage renal disease (28.6%) or CHF (39%), and more likely to have had a code discussion (85.8%). There were no differences between hospice users and nonusers in gender, marital status, ethnicity, and number of chronic conditions (Table 1).
| Variable | All, N=364 | Hospice Users, n=210 | Nonhospice Users, n=154 | P Value |
|---|---|---|---|---|
| ||||
| Age, y, mean (SD) | 80.1 (8.2) | 80.8 (8.4) | 79.1 (7.8) | 0.049 |
| Gender (female), % | 48.9 | 56.2 | 43.8 | 0.568 |
| Ethnicity, % | 0.702 | |||
| White | 42.6 | 43.3 | 41.6 | |
| Latino | 25.5 | 27.1 | 23.4 | |
| African American | 23.1 | 21.4 | 25.3 | |
| Other | 8.8 | 8.1 | 9.7 | |
| Marital status, % | 0.809 | |||
| Married | 45.6 | 43.8 | 48.1 | |
| Widowed | 36.0 | 38.1 | 33.1 | |
| Divorced | 7.7 | 7.6 | 7.8 | |
| Other | 7.7 | 7.6 | 7.8 | |
| Missing | 3.0 | 2.9 | 3.2 | |
| Diagnosis, % | <0.001 | |||
| Cancer | 33.8 | 42.1 | 22.9 | |
| CHF | 16.2 | 11.0 | 23.5 | |
| CAD | 12.6 | 12.4 | 13.1 | |
| Dementia | 12.4 | 12.4 | 12.4 | |
| COPD | 6.0 | 5.3 | 7.2 | |
| CVA | 5.2 | 7.2 | 2.6 | |
| Other | 13.6 | 9.6 | 18.3 | |
| Number of chronic conditions, mean (SD) | 1.0 | 1.7 (0.8) | 1.7 (0.9) | 0.949 |
| Code status discussed, % | 81.1 | 87.0 | 72.8 | 0.001 |
Significant differences between hospice users and nonusers were controlled in a regression adjusting for age, gender, marital status, and number of chronic conditions. Compared to whites, no significant differences in hospice use were found for blacks (odds ratio [OR]: 0.67; 95% confidence interval [CI]: 0.37‐1.21), Latinos (OR: 1.24; 95% CI: 0.68‐2.25), or other ethnic groups (OR: 0.78; 95% CI: 0.34‐1.56). Compared with other diagnoses, those with cancer (OR: 3.66; 95% CI: 1.77‐7.59) and older patients (OR: 1.05; 95% CI: 1.01‐1.08) were significantly more likely to receive hospice care following IPC consult. Those discussing code status were twice as likely to be discharged to hospice (OR: 2.14; 95% CI: 1.20‐3.79).
DISCUSSION
This study found similar rates of hospice enrollment following IPC consult among Latinos, blacks, and other ethnic groups as compared with whites. Others found comparable rates of advance directive completion between whites and African Americans following IPC consultation,[7]and that IPC intensity resulting in a plan of care was highly associated with receipt of hospice care.[8] Likewise, our study found that discussion of code status, another marker of intensity, was positively associated with hospice use.
Our findings among patients receiving IPC consultation contrast with previous studies examining ethnic variation in hospice use among general samples of decedents. A study of California dual eligibles found that blacks were 26% and Asians 34% less likely than whites to use hospice. Others have found similar results among patients with CHF and lung cancer.[9, 10]
Misconceptions and lack of awareness, knowledge, and trust in healthcare providers serve as barriers to hospice care for minorities.[11, 12] IPC consultations may overcome these barriers by discussing goals of care including discussing the condition, eliciting patient/family understanding of the condition, and presenting options for code status.
This study employed a single‐cohort design without a comparison group. It was conducted within a health maintenance organization with strong hospice and palliative care programs and may not represent other settings. Nevertheless, this study provides promise for IPC consultation to increase equitable access to hospice care among minority groups. Further studies are needed to confirm the preliminary findings reported here.
Disclosures: Supported in part by a career development award from the National Palliative Care Research Center and by a grant from the Archstone Foundation. Evie Vesper and Dr. Rebecca Goldstein were employees of the healthcare organization at the time of the study. Susan Enguidanos received compensation for project evaluation during the original study. The sponsors had no role in the design, implementation, or analysis of the study. The authors report no conflicts of interest.
- , , . Ethnic variation in site of death among Medicaid/Medicare dually eligible older adults. J Am Geriatr Soc. 2005;53(8):1411–1416.
- . Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008;11(5):763–768.
- . The Medicare hospice benefit: 15 years of success. J Palliat Med. 1998;1(2):139–146.
- . Palliative care in hospitals. J Hosp Med. 2006;1(1):21–28.
- , , , et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190.
- , , , et al. Increased satisfaction with care and lower costs: results of a randomized trial of in‐home palliative care. J Am Geriatr Soc. 2007;55(7):993–1000.
- , , , et al. Ethnicity, race, and advance directives in an inpatient palliative care consultation service. Palliat Support Care. 2012;6(1):1–7.
- , , . Hospice referrals and code status: outcomes of inpatient palliative care consultations among Asian Americans and Pacific Islanders with cancer. J Pain Symptom Manage. 2011;42(4):557–564.
- , , , , . Racial differences in hospice use and patterns of care after enrollment in hospice among Medicare beneficiaries with heart failure. Am Heart J. 2012;163(6):987–993.
- , , , et al. Racial disparities in length of stay in hospice care by tumor stage in a large elderly cohort with non‐small cell lung cancer. Palliat Med. 2012;26(1):61–71.
- , , , , . Knowledge, attitudes and beliefs about end‐of‐life care among inner‐city African Americans and Latino/Hispanic Americans. J Palliat Med. 2004;7(2):247–256.
- , , . Does caregiver knowledge matter for hospice enrollment and beyond? Pilot study of minority hospice patients. Am J Hospice Palliat Med. 2009;26(3):165–171.
- , , . Ethnic variation in site of death among Medicaid/Medicare dually eligible older adults. J Am Geriatr Soc. 2005;53(8):1411–1416.
- . Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008;11(5):763–768.
- . The Medicare hospice benefit: 15 years of success. J Palliat Med. 1998;1(2):139–146.
- . Palliative care in hospitals. J Hosp Med. 2006;1(1):21–28.
- , , , et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190.
- , , , et al. Increased satisfaction with care and lower costs: results of a randomized trial of in‐home palliative care. J Am Geriatr Soc. 2007;55(7):993–1000.
- , , , et al. Ethnicity, race, and advance directives in an inpatient palliative care consultation service. Palliat Support Care. 2012;6(1):1–7.
- , , . Hospice referrals and code status: outcomes of inpatient palliative care consultations among Asian Americans and Pacific Islanders with cancer. J Pain Symptom Manage. 2011;42(4):557–564.
- , , , , . Racial differences in hospice use and patterns of care after enrollment in hospice among Medicare beneficiaries with heart failure. Am Heart J. 2012;163(6):987–993.
- , , , et al. Racial disparities in length of stay in hospice care by tumor stage in a large elderly cohort with non‐small cell lung cancer. Palliat Med. 2012;26(1):61–71.
- , , , , . Knowledge, attitudes and beliefs about end‐of‐life care among inner‐city African Americans and Latino/Hispanic Americans. J Palliat Med. 2004;7(2):247–256.
- , , . Does caregiver knowledge matter for hospice enrollment and beyond? Pilot study of minority hospice patients. Am J Hospice Palliat Med. 2009;26(3):165–171.
Smartphone Policy for Attending Rounds
Despite the many benefits of smartphones for physicians, there are also potential downsides to utilizing these devices in the patient care setting. Prior research at our hospital found that smartphone use during inpatient attending rounds can distract faculty and residents, and nearly 80% of attendings favored the institution of codes of conduct governing appropriate use of smartphones during rounds.[1] Based on these findings, a policy regulating faculty and resident smartphone use was instituted in February 2012 in the Departments of Medicine and Pediatrics at our hospital.[1]
Although our faculty's enthusiasm for the smartphone policy was clear, residents' attitudes toward this new regulation were unknown. Born in the 1980s, today's residents are members of the millennial generation, who seamlessly integrate technology into their lives.[2, 3, 4, 5] Millennials generally do not perceive their multitasking with technology to be rude or distracting.[2] Having grown up with the Internet, they employ digital tools as an inherent sixth sense,[3] and view their use of technology as the defining characteristic of their generation.[5]
Housestaff feedback was instrumental in shaping the specifics of the smartphone policy.[1] However, given the primacy of technology in the life of the millennial, it is plausible that residents would resent restrictions on their smartphone use. Such resentment could limit a policy's effectiveness, as well as negatively impact resident morale. With increasing discussion about the need to manage personal electronic device use in the patient care setting,[2, 6, 7, 8] we sought to assess residents' attitudes toward our hospital's smartphone policy.
METHODS
A brief survey instrument was designed to increase housestaff awareness of and evaluate their attitudes toward the smartphone policy. In November 2012, the anonymous survey was administered via SurveyMonkey (
The survey provided a summary of the policy: The smartphone code of conduct policy was instituted to minimize distraction during attending rounds. The policy applies to all team members, including faculty, and essentially states that at the start of attending rounds, all phones must be silenced or turned off. These devices are to be used during rounds only for patient care or for urgent personal/family concerns. Any use must be made explicit to the person leading rounds. Residents also received a copy of the complete policy as an attachment to the request email. A copy of this policy is available as an appendix to Katz‐Sidlow et al.[1]
The survey requested information regarding departmental affiliation, and asked whether the resident had prior awareness of the smartphone policy. Residents' attitudes were evaluated by asking for their level of agreement with the following statement: It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds. This statement was graded on a 4‐point frequency scale (strongly disagree, disagree, agree, or strongly agree). Residents' attitudes were further explored in a follow‐up question: Which statement most closely expresses your feelings? Three options were offered: (1) There should be no guidelines as to how team members should use smartphones during inpatient attending rounds. Every person should decide for him/herself how and when to use the phone during rounds. (2) I agree that a smartphone code of conduct for attending rounds is a good idea, but I suggest modifying the current policy (please use the text box below to explain). (3) I agree with the current smartphone code of conduct policy for attending rounds. A text box was provided for comments.
RESULTS
The overall response rate was 65% (93/142), representing 58% (57/98) of all Department of Medicine residents and 82% (36/44) of all Department of Pediatrics residents. Seventy‐one percent of respondents (57% Department of Medicine; 92% Department of Pediatrics) indicated a prior knowledge of the smartphone policy.
Overall, 82% of respondents agreed or strongly agreed with the statement, It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds (Figure 1). Residents' responses to the follow‐up question revealed that nearly 60% agreed with the stipulations of the current policy; another 18% believed that a policy is needed, but felt that the current code should be modified. Only one resident provided a modification suggestion, which was to expand the policy to include resident work rounds.

Responses to these 2 questions differed slightly for trainees with an awareness of the preexisting policy as compared to those without prior awareness; however, these differences were not statistically significant.
CONCLUSIONS
Despite concerns that residents would resent policies regulating their use of technology, we found that the majority of residents indicated a desire for, and acceptance of, clear guidelines regarding smartphone use during inpatient rounds. Our findings are in line with prior research suggesting that millennials appreciate a structured work environment and explicit guidance regarding workplace expectations.[2, 3, 4] To minimize distraction and support residents' professionalism, we recommend that training programs develop and implement clear expectations regarding smartphone use in the active patient care setting.
- , , , . Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–599.
- , . The challenges and opportunities of teaching “generation y.” J Grad Med Educ. 2011;3:458–461.
- , . Millennials and the world of work: an organization and management perspective. J Bus Psychol. 2010;25:211–223.
- , , . Is your residency program ready for generation y? J Surg Educ. 2010;67:108–111.
- Pew Research Center. Millennials: a portrait of generation next. Pew Research Center Web site. February 2010. Available at: http://www.pewsocialtrends.org/files/2010/10/millennials‐confident‐connected‐open‐to‐change.pdf. Accessed May 9, 2013.
- . Spotlight case. Order interrupted by text: multitasking mishap. Agency for Healthcare Research and Quality Web site. December 2011. Available at: http://webmm.ahrq.gov/case.aspx?caseID=257. Accessed May 9, 2013.
- . Training health care professionals to deal with an explosion of electronic distraction. Neurocrit Care. 2013;18:115–117.
- ECRI Institute. Top 10 health technology hazards for 2013. ECRI Institute Web site. Available at: https://www.ecri.org/Documents/Secure/Health_Devices_Top_10_Hazards_2013.pdf. Accessed May 9, 2013.
Despite the many benefits of smartphones for physicians, there are also potential downsides to utilizing these devices in the patient care setting. Prior research at our hospital found that smartphone use during inpatient attending rounds can distract faculty and residents, and nearly 80% of attendings favored the institution of codes of conduct governing appropriate use of smartphones during rounds.[1] Based on these findings, a policy regulating faculty and resident smartphone use was instituted in February 2012 in the Departments of Medicine and Pediatrics at our hospital.[1]
Although our faculty's enthusiasm for the smartphone policy was clear, residents' attitudes toward this new regulation were unknown. Born in the 1980s, today's residents are members of the millennial generation, who seamlessly integrate technology into their lives.[2, 3, 4, 5] Millennials generally do not perceive their multitasking with technology to be rude or distracting.[2] Having grown up with the Internet, they employ digital tools as an inherent sixth sense,[3] and view their use of technology as the defining characteristic of their generation.[5]
Housestaff feedback was instrumental in shaping the specifics of the smartphone policy.[1] However, given the primacy of technology in the life of the millennial, it is plausible that residents would resent restrictions on their smartphone use. Such resentment could limit a policy's effectiveness, as well as negatively impact resident morale. With increasing discussion about the need to manage personal electronic device use in the patient care setting,[2, 6, 7, 8] we sought to assess residents' attitudes toward our hospital's smartphone policy.
METHODS
A brief survey instrument was designed to increase housestaff awareness of and evaluate their attitudes toward the smartphone policy. In November 2012, the anonymous survey was administered via SurveyMonkey (
The survey provided a summary of the policy: The smartphone code of conduct policy was instituted to minimize distraction during attending rounds. The policy applies to all team members, including faculty, and essentially states that at the start of attending rounds, all phones must be silenced or turned off. These devices are to be used during rounds only for patient care or for urgent personal/family concerns. Any use must be made explicit to the person leading rounds. Residents also received a copy of the complete policy as an attachment to the request email. A copy of this policy is available as an appendix to Katz‐Sidlow et al.[1]
The survey requested information regarding departmental affiliation, and asked whether the resident had prior awareness of the smartphone policy. Residents' attitudes were evaluated by asking for their level of agreement with the following statement: It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds. This statement was graded on a 4‐point frequency scale (strongly disagree, disagree, agree, or strongly agree). Residents' attitudes were further explored in a follow‐up question: Which statement most closely expresses your feelings? Three options were offered: (1) There should be no guidelines as to how team members should use smartphones during inpatient attending rounds. Every person should decide for him/herself how and when to use the phone during rounds. (2) I agree that a smartphone code of conduct for attending rounds is a good idea, but I suggest modifying the current policy (please use the text box below to explain). (3) I agree with the current smartphone code of conduct policy for attending rounds. A text box was provided for comments.
RESULTS
The overall response rate was 65% (93/142), representing 58% (57/98) of all Department of Medicine residents and 82% (36/44) of all Department of Pediatrics residents. Seventy‐one percent of respondents (57% Department of Medicine; 92% Department of Pediatrics) indicated a prior knowledge of the smartphone policy.
Overall, 82% of respondents agreed or strongly agreed with the statement, It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds (Figure 1). Residents' responses to the follow‐up question revealed that nearly 60% agreed with the stipulations of the current policy; another 18% believed that a policy is needed, but felt that the current code should be modified. Only one resident provided a modification suggestion, which was to expand the policy to include resident work rounds.

Responses to these 2 questions differed slightly for trainees with an awareness of the preexisting policy as compared to those without prior awareness; however, these differences were not statistically significant.
CONCLUSIONS
Despite concerns that residents would resent policies regulating their use of technology, we found that the majority of residents indicated a desire for, and acceptance of, clear guidelines regarding smartphone use during inpatient rounds. Our findings are in line with prior research suggesting that millennials appreciate a structured work environment and explicit guidance regarding workplace expectations.[2, 3, 4] To minimize distraction and support residents' professionalism, we recommend that training programs develop and implement clear expectations regarding smartphone use in the active patient care setting.
Despite the many benefits of smartphones for physicians, there are also potential downsides to utilizing these devices in the patient care setting. Prior research at our hospital found that smartphone use during inpatient attending rounds can distract faculty and residents, and nearly 80% of attendings favored the institution of codes of conduct governing appropriate use of smartphones during rounds.[1] Based on these findings, a policy regulating faculty and resident smartphone use was instituted in February 2012 in the Departments of Medicine and Pediatrics at our hospital.[1]
Although our faculty's enthusiasm for the smartphone policy was clear, residents' attitudes toward this new regulation were unknown. Born in the 1980s, today's residents are members of the millennial generation, who seamlessly integrate technology into their lives.[2, 3, 4, 5] Millennials generally do not perceive their multitasking with technology to be rude or distracting.[2] Having grown up with the Internet, they employ digital tools as an inherent sixth sense,[3] and view their use of technology as the defining characteristic of their generation.[5]
Housestaff feedback was instrumental in shaping the specifics of the smartphone policy.[1] However, given the primacy of technology in the life of the millennial, it is plausible that residents would resent restrictions on their smartphone use. Such resentment could limit a policy's effectiveness, as well as negatively impact resident morale. With increasing discussion about the need to manage personal electronic device use in the patient care setting,[2, 6, 7, 8] we sought to assess residents' attitudes toward our hospital's smartphone policy.
METHODS
A brief survey instrument was designed to increase housestaff awareness of and evaluate their attitudes toward the smartphone policy. In November 2012, the anonymous survey was administered via SurveyMonkey (
The survey provided a summary of the policy: The smartphone code of conduct policy was instituted to minimize distraction during attending rounds. The policy applies to all team members, including faculty, and essentially states that at the start of attending rounds, all phones must be silenced or turned off. These devices are to be used during rounds only for patient care or for urgent personal/family concerns. Any use must be made explicit to the person leading rounds. Residents also received a copy of the complete policy as an attachment to the request email. A copy of this policy is available as an appendix to Katz‐Sidlow et al.[1]
The survey requested information regarding departmental affiliation, and asked whether the resident had prior awareness of the smartphone policy. Residents' attitudes were evaluated by asking for their level of agreement with the following statement: It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds. This statement was graded on a 4‐point frequency scale (strongly disagree, disagree, agree, or strongly agree). Residents' attitudes were further explored in a follow‐up question: Which statement most closely expresses your feelings? Three options were offered: (1) There should be no guidelines as to how team members should use smartphones during inpatient attending rounds. Every person should decide for him/herself how and when to use the phone during rounds. (2) I agree that a smartphone code of conduct for attending rounds is a good idea, but I suggest modifying the current policy (please use the text box below to explain). (3) I agree with the current smartphone code of conduct policy for attending rounds. A text box was provided for comments.
RESULTS
The overall response rate was 65% (93/142), representing 58% (57/98) of all Department of Medicine residents and 82% (36/44) of all Department of Pediatrics residents. Seventy‐one percent of respondents (57% Department of Medicine; 92% Department of Pediatrics) indicated a prior knowledge of the smartphone policy.
Overall, 82% of respondents agreed or strongly agreed with the statement, It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds (Figure 1). Residents' responses to the follow‐up question revealed that nearly 60% agreed with the stipulations of the current policy; another 18% believed that a policy is needed, but felt that the current code should be modified. Only one resident provided a modification suggestion, which was to expand the policy to include resident work rounds.

Responses to these 2 questions differed slightly for trainees with an awareness of the preexisting policy as compared to those without prior awareness; however, these differences were not statistically significant.
CONCLUSIONS
Despite concerns that residents would resent policies regulating their use of technology, we found that the majority of residents indicated a desire for, and acceptance of, clear guidelines regarding smartphone use during inpatient rounds. Our findings are in line with prior research suggesting that millennials appreciate a structured work environment and explicit guidance regarding workplace expectations.[2, 3, 4] To minimize distraction and support residents' professionalism, we recommend that training programs develop and implement clear expectations regarding smartphone use in the active patient care setting.
- , , , . Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–599.
- , . The challenges and opportunities of teaching “generation y.” J Grad Med Educ. 2011;3:458–461.
- , . Millennials and the world of work: an organization and management perspective. J Bus Psychol. 2010;25:211–223.
- , , . Is your residency program ready for generation y? J Surg Educ. 2010;67:108–111.
- Pew Research Center. Millennials: a portrait of generation next. Pew Research Center Web site. February 2010. Available at: http://www.pewsocialtrends.org/files/2010/10/millennials‐confident‐connected‐open‐to‐change.pdf. Accessed May 9, 2013.
- . Spotlight case. Order interrupted by text: multitasking mishap. Agency for Healthcare Research and Quality Web site. December 2011. Available at: http://webmm.ahrq.gov/case.aspx?caseID=257. Accessed May 9, 2013.
- . Training health care professionals to deal with an explosion of electronic distraction. Neurocrit Care. 2013;18:115–117.
- ECRI Institute. Top 10 health technology hazards for 2013. ECRI Institute Web site. Available at: https://www.ecri.org/Documents/Secure/Health_Devices_Top_10_Hazards_2013.pdf. Accessed May 9, 2013.
- , , , . Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–599.
- , . The challenges and opportunities of teaching “generation y.” J Grad Med Educ. 2011;3:458–461.
- , . Millennials and the world of work: an organization and management perspective. J Bus Psychol. 2010;25:211–223.
- , , . Is your residency program ready for generation y? J Surg Educ. 2010;67:108–111.
- Pew Research Center. Millennials: a portrait of generation next. Pew Research Center Web site. February 2010. Available at: http://www.pewsocialtrends.org/files/2010/10/millennials‐confident‐connected‐open‐to‐change.pdf. Accessed May 9, 2013.
- . Spotlight case. Order interrupted by text: multitasking mishap. Agency for Healthcare Research and Quality Web site. December 2011. Available at: http://webmm.ahrq.gov/case.aspx?caseID=257. Accessed May 9, 2013.
- . Training health care professionals to deal with an explosion of electronic distraction. Neurocrit Care. 2013;18:115–117.
- ECRI Institute. Top 10 health technology hazards for 2013. ECRI Institute Web site. Available at: https://www.ecri.org/Documents/Secure/Health_Devices_Top_10_Hazards_2013.pdf. Accessed May 9, 2013.