User login
Male Acne: The Importance of Gender in Acne Treatment [editorial]
Actual acne treatment lasts longer than studies suggest
MIAMI BEACH – In practice, acne patients are treated three times longer than clinical trials suggest, based on data from more than 2,000 patients at an academic medical center.
The findings have implications both for setting patients’ treatment expectations and for designing future clinical trials, said Karen Huang of Wake Forest University, Winston-Salem, N.C., said at the annual meeting of the American Academy of Dermatology.
Ms. Huang and her colleagues reviewed electronic records for patients who were treated at an academic medical practice between Jan. 1, 2009, and Nov. 15, 2012. Overall, 2,250 patients had at least one acne-related visit with a dermatologist. Of these, 57% had only one visit and 43% had multiple visits.
For patients who had multiple visits, the mean duration of treatment from the first to the last visit was approximately 9 months (0.79 years). Approximately 25% continued seeing their dermatologists for about a year, and half continued treatment for nearly 5 months (0.4 years).
Not unexpectedly, patients treated with oral medication, including isotretinoin and other oral treatments, were more likely than those treated with topical medications to have multiple visits. In addition, the number of visits by patients who received isotretinoin slowed gradually at first, then declined more rapidly over time compared with patients who received topical treatments.
Approximately 90% of individuals experience acne during their lifetimes, but the actual duration of acne episodes has not been well characterized in the literature, said Ms. Huang. The duration of treatment seen in 40 recent studies of acne treatment identified at clinicaltrials.gov was about 12 weeks, she added.
The current findings represent a lower limit on the duration of acne treatment because of a lack of data on which patients may have discontinued treatment prematurely or continued treatment elsewhere, such as with a primary care physician, she said.
The study findings may be of interest not only for clinical trial design (in that researchers might want to simulate average treatment duration), but also for physicians who want to set realistic expectations about treatment for their patients.
"It has been shown that if you help set patients’ expectations of what their treatment will be like, it may help improve adherence," she said.
Ms. Huang had no financial conflicts to disclose.
MIAMI BEACH – In practice, acne patients are treated three times longer than clinical trials suggest, based on data from more than 2,000 patients at an academic medical center.
The findings have implications both for setting patients’ treatment expectations and for designing future clinical trials, said Karen Huang of Wake Forest University, Winston-Salem, N.C., said at the annual meeting of the American Academy of Dermatology.
Ms. Huang and her colleagues reviewed electronic records for patients who were treated at an academic medical practice between Jan. 1, 2009, and Nov. 15, 2012. Overall, 2,250 patients had at least one acne-related visit with a dermatologist. Of these, 57% had only one visit and 43% had multiple visits.
For patients who had multiple visits, the mean duration of treatment from the first to the last visit was approximately 9 months (0.79 years). Approximately 25% continued seeing their dermatologists for about a year, and half continued treatment for nearly 5 months (0.4 years).
Not unexpectedly, patients treated with oral medication, including isotretinoin and other oral treatments, were more likely than those treated with topical medications to have multiple visits. In addition, the number of visits by patients who received isotretinoin slowed gradually at first, then declined more rapidly over time compared with patients who received topical treatments.
Approximately 90% of individuals experience acne during their lifetimes, but the actual duration of acne episodes has not been well characterized in the literature, said Ms. Huang. The duration of treatment seen in 40 recent studies of acne treatment identified at clinicaltrials.gov was about 12 weeks, she added.
The current findings represent a lower limit on the duration of acne treatment because of a lack of data on which patients may have discontinued treatment prematurely or continued treatment elsewhere, such as with a primary care physician, she said.
The study findings may be of interest not only for clinical trial design (in that researchers might want to simulate average treatment duration), but also for physicians who want to set realistic expectations about treatment for their patients.
"It has been shown that if you help set patients’ expectations of what their treatment will be like, it may help improve adherence," she said.
Ms. Huang had no financial conflicts to disclose.
MIAMI BEACH – In practice, acne patients are treated three times longer than clinical trials suggest, based on data from more than 2,000 patients at an academic medical center.
The findings have implications both for setting patients’ treatment expectations and for designing future clinical trials, said Karen Huang of Wake Forest University, Winston-Salem, N.C., said at the annual meeting of the American Academy of Dermatology.
Ms. Huang and her colleagues reviewed electronic records for patients who were treated at an academic medical practice between Jan. 1, 2009, and Nov. 15, 2012. Overall, 2,250 patients had at least one acne-related visit with a dermatologist. Of these, 57% had only one visit and 43% had multiple visits.
For patients who had multiple visits, the mean duration of treatment from the first to the last visit was approximately 9 months (0.79 years). Approximately 25% continued seeing their dermatologists for about a year, and half continued treatment for nearly 5 months (0.4 years).
Not unexpectedly, patients treated with oral medication, including isotretinoin and other oral treatments, were more likely than those treated with topical medications to have multiple visits. In addition, the number of visits by patients who received isotretinoin slowed gradually at first, then declined more rapidly over time compared with patients who received topical treatments.
Approximately 90% of individuals experience acne during their lifetimes, but the actual duration of acne episodes has not been well characterized in the literature, said Ms. Huang. The duration of treatment seen in 40 recent studies of acne treatment identified at clinicaltrials.gov was about 12 weeks, she added.
The current findings represent a lower limit on the duration of acne treatment because of a lack of data on which patients may have discontinued treatment prematurely or continued treatment elsewhere, such as with a primary care physician, she said.
The study findings may be of interest not only for clinical trial design (in that researchers might want to simulate average treatment duration), but also for physicians who want to set realistic expectations about treatment for their patients.
"It has been shown that if you help set patients’ expectations of what their treatment will be like, it may help improve adherence," she said.
Ms. Huang had no financial conflicts to disclose.
AT THE AAD ANNUAL MEETING
Major finding: The mean duration of acne treatment was approximately 9 months in clinical practice vs. 3 months in clinical trials.
Data source: A retrospective review of data from 2,250 patients seen at an academic practice.
Disclosures: Dr. Huang reported having no disclosures.
Cosmetic Corner: Dermatologists Weigh in on OTC Acne Preparations
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top OTC acne preparations. Consideration must be given to:
- Acne Free Oil-Free Acne Cleanser
Valeant Consumer Products, a division of Valeant Pharmaceuticals North America
Recommended by Adam Friedman, MD, New York, New York
Clear Pore Cleanser/Mask
Neutrogena Corporation
Recommended by Adam Friedman, MD, New York, New York, and Marian Northington, MD, Birmingham, Alabama
"I combine Acne Free Oil-Free Acne Cleanser with benzoyl peroxide 3.7% or Neutrogena Clear Pore Cleanser/Mask with benzoyl peroxide 3.5% with subsequent application of clindamycin lotion, which limits the associated irritation often experienced with leave-on benzoyl peroxide products or combination products containing benzoyl peroxide while limiting bacterial resistance to the topical clindamycin and providing an antiacne impact. Of note, a wash-off product with benzoyl peroxide also limits the risk for clothing and towel bleaching often seen with leave-on products."—Adam Friedman, MD
- EndZit Products
Abbe Laboratories, Inc
Recommended by Deborah S. Sarnoff, MD, New York, New York
- Glytone Acne Treatment Line
Pierre Fabre Dermo-Cosmetique
Recommended by Marta I. Rendon, MD, Boca Raton, Florida
- PanOxyl 10% Acne Foaming Wash
Stiefel, a GSK company
Recommended by Gary Goldenberg, MD, New York, New York
- St. Ives Apricot Face Wash Blemish & Blackhead Control
Unilever
"This is an exfoliating 2% salicylic acid facial scrub, which is great to add into one's acne treatment. It can be used once or twice a week as a gentle keratolytic, helping to prevent comedone formation."—Anthony M. Rossi, MD, New York, New York
Cutis invites readers to send us their recommendations. Body moisturizers, face washes, and antiwrinkle treatments will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to msteiger@frontlinemedcom.com.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top OTC acne preparations. Consideration must be given to:
- Acne Free Oil-Free Acne Cleanser
Valeant Consumer Products, a division of Valeant Pharmaceuticals North America
Recommended by Adam Friedman, MD, New York, New York
Clear Pore Cleanser/Mask
Neutrogena Corporation
Recommended by Adam Friedman, MD, New York, New York, and Marian Northington, MD, Birmingham, Alabama
"I combine Acne Free Oil-Free Acne Cleanser with benzoyl peroxide 3.7% or Neutrogena Clear Pore Cleanser/Mask with benzoyl peroxide 3.5% with subsequent application of clindamycin lotion, which limits the associated irritation often experienced with leave-on benzoyl peroxide products or combination products containing benzoyl peroxide while limiting bacterial resistance to the topical clindamycin and providing an antiacne impact. Of note, a wash-off product with benzoyl peroxide also limits the risk for clothing and towel bleaching often seen with leave-on products."—Adam Friedman, MD
- EndZit Products
Abbe Laboratories, Inc
Recommended by Deborah S. Sarnoff, MD, New York, New York
- Glytone Acne Treatment Line
Pierre Fabre Dermo-Cosmetique
Recommended by Marta I. Rendon, MD, Boca Raton, Florida
- PanOxyl 10% Acne Foaming Wash
Stiefel, a GSK company
Recommended by Gary Goldenberg, MD, New York, New York
- St. Ives Apricot Face Wash Blemish & Blackhead Control
Unilever
"This is an exfoliating 2% salicylic acid facial scrub, which is great to add into one's acne treatment. It can be used once or twice a week as a gentle keratolytic, helping to prevent comedone formation."—Anthony M. Rossi, MD, New York, New York
Cutis invites readers to send us their recommendations. Body moisturizers, face washes, and antiwrinkle treatments will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to msteiger@frontlinemedcom.com.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top OTC acne preparations. Consideration must be given to:
- Acne Free Oil-Free Acne Cleanser
Valeant Consumer Products, a division of Valeant Pharmaceuticals North America
Recommended by Adam Friedman, MD, New York, New York
Clear Pore Cleanser/Mask
Neutrogena Corporation
Recommended by Adam Friedman, MD, New York, New York, and Marian Northington, MD, Birmingham, Alabama
"I combine Acne Free Oil-Free Acne Cleanser with benzoyl peroxide 3.7% or Neutrogena Clear Pore Cleanser/Mask with benzoyl peroxide 3.5% with subsequent application of clindamycin lotion, which limits the associated irritation often experienced with leave-on benzoyl peroxide products or combination products containing benzoyl peroxide while limiting bacterial resistance to the topical clindamycin and providing an antiacne impact. Of note, a wash-off product with benzoyl peroxide also limits the risk for clothing and towel bleaching often seen with leave-on products."—Adam Friedman, MD
- EndZit Products
Abbe Laboratories, Inc
Recommended by Deborah S. Sarnoff, MD, New York, New York
- Glytone Acne Treatment Line
Pierre Fabre Dermo-Cosmetique
Recommended by Marta I. Rendon, MD, Boca Raton, Florida
- PanOxyl 10% Acne Foaming Wash
Stiefel, a GSK company
Recommended by Gary Goldenberg, MD, New York, New York
- St. Ives Apricot Face Wash Blemish & Blackhead Control
Unilever
"This is an exfoliating 2% salicylic acid facial scrub, which is great to add into one's acne treatment. It can be used once or twice a week as a gentle keratolytic, helping to prevent comedone formation."—Anthony M. Rossi, MD, New York, New York
Cutis invites readers to send us their recommendations. Body moisturizers, face washes, and antiwrinkle treatments will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to msteiger@frontlinemedcom.com.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Efficacy and Tolerability of Fixed-Combination Acne Treatment in Adolescents
Triple-combination for severe acne avoids isotretinoin
MAUI, HAWAII – Combination therapy for severe acne, with a trio of familiar, well tolerated agents, knocked down the skin disease severity in a phase IV study such that 80% of patients deemed candidates for isotretinoin at baseline no longer qualified for the powerful oral retinoid 12 weeks later, Dr. Guy F. Webster reported at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
These data provide welcome news for patients who can’t take isotretinoin or don’t want to, as well as for the many physicians reluctant to prescribe the drug because of the considerable regulatory hassles and potentially serious side effects, including teratogenicity.
The treatment regimen in this open-label multicenter study consisted of an oral antibiotic, a topical antibiotic/retinoid agent, and benzoyl peroxide. More specifically, the 97 study participants aged 12-29 years, all with grade 3-4 moderate to severe facial acne by Investigator’s Global Assessment (IGA), were placed on once-daily minocycline HCL extended release at about 1 mg/kg, clindamycin phosphate 1.2%/tretinoin 0.025% gel, and 6% benzoyl peroxide foaming cloths. Patients were evaluated at weeks 0, 2, 4, 8, and 12.
At week 2, 44% of subjects already had at least a 1-grade improvement in IGA; by week 12, 89% did. Moreover, 56% of patients had at least a 2-grade improvement in IGA.
At least a 1-grade improvement on the Global Aesthetic Improvement Scale was documented in 83% of subjects at week 2 and 96% at week 12.
"With this therapy, you can get patients with really bad acne from bad to really mild without resorting to big-time drugs," observed Dr. Webster, professor of dermatology and internal medicine at Thomas Jefferson University, Philadelphia.
Week 12 mean facial inflammatory lesion counts fell by 62%, and noninflammatory lesion counts decreased by 49% from baselines of 33 and 44 lesions, respectively.
At baseline, 69 patients were judged by three blinded assessors of clinical photos to have acne sufficiently severe for them to be candidates for isotretinoin therapy. By week 12, this number had dwindled to 14 patients. In other words, 80% of patients were no longer deemed to be candidates for isotretinoin.
Eight patients experienced treatment-related adverse events consisting of transient mild to moderate irritation and/or redness, burning, stinging, and dry skin.
The results of this Phase-4 study are consistent with studies of other multidrug regimens for acne, albeit mostly conducted in less severely affected patients.
"The general paradigm is that mixed therapies are useful because other than isotretinoin and maybe spironolactone, no one drug is strong enough to stop acne effectively. If you just hit the [Propionibacterium acnes] hard, you can’t get it down to where there’s no P. acnes. If you blunt the immune response, you’re still just blunting it, not turning it off. And if you’re addressing the plug in the follicle, it’s not a complete or rapid response," the dermatologist explained.
In clinical practice, Dr. Webster said he typically stops the oral antibiotic cold at about 12 weeks to avoid pigmentary changes and other side effects of long-term antibiotic therapy. At least 75% of patients can maintain their gains with topical therapy alone.
Compliance is often an issue with combination therapy. Patients need to understand that if they don’t use all of the medications consistently from day 1 they won’t get better.
"It’s tough with kids because kids expect to get better overnight. They see it on the Proactiv commercials and wonder why in the world they’re not better in 2 days," the dermatologist observed.
In this phase IV study, however, patient compliance was consistently excellent, perhaps because of the high disease severity. The treatment compliance rate was 91% at week 2 and 86% at week 12.
Dr. Webster is a consultant for several pharmaceutical companies, including Valeant, whose subsidiary Medicis sponsored the phase IV study.
SDEF and this news organization are owned by the same parent company.
*This story was updated March 1, 2013.
MAUI, HAWAII – Combination therapy for severe acne, with a trio of familiar, well tolerated agents, knocked down the skin disease severity in a phase IV study such that 80% of patients deemed candidates for isotretinoin at baseline no longer qualified for the powerful oral retinoid 12 weeks later, Dr. Guy F. Webster reported at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
These data provide welcome news for patients who can’t take isotretinoin or don’t want to, as well as for the many physicians reluctant to prescribe the drug because of the considerable regulatory hassles and potentially serious side effects, including teratogenicity.
The treatment regimen in this open-label multicenter study consisted of an oral antibiotic, a topical antibiotic/retinoid agent, and benzoyl peroxide. More specifically, the 97 study participants aged 12-29 years, all with grade 3-4 moderate to severe facial acne by Investigator’s Global Assessment (IGA), were placed on once-daily minocycline HCL extended release at about 1 mg/kg, clindamycin phosphate 1.2%/tretinoin 0.025% gel, and 6% benzoyl peroxide foaming cloths. Patients were evaluated at weeks 0, 2, 4, 8, and 12.
At week 2, 44% of subjects already had at least a 1-grade improvement in IGA; by week 12, 89% did. Moreover, 56% of patients had at least a 2-grade improvement in IGA.
At least a 1-grade improvement on the Global Aesthetic Improvement Scale was documented in 83% of subjects at week 2 and 96% at week 12.
"With this therapy, you can get patients with really bad acne from bad to really mild without resorting to big-time drugs," observed Dr. Webster, professor of dermatology and internal medicine at Thomas Jefferson University, Philadelphia.
Week 12 mean facial inflammatory lesion counts fell by 62%, and noninflammatory lesion counts decreased by 49% from baselines of 33 and 44 lesions, respectively.
At baseline, 69 patients were judged by three blinded assessors of clinical photos to have acne sufficiently severe for them to be candidates for isotretinoin therapy. By week 12, this number had dwindled to 14 patients. In other words, 80% of patients were no longer deemed to be candidates for isotretinoin.
Eight patients experienced treatment-related adverse events consisting of transient mild to moderate irritation and/or redness, burning, stinging, and dry skin.
The results of this Phase-4 study are consistent with studies of other multidrug regimens for acne, albeit mostly conducted in less severely affected patients.
"The general paradigm is that mixed therapies are useful because other than isotretinoin and maybe spironolactone, no one drug is strong enough to stop acne effectively. If you just hit the [Propionibacterium acnes] hard, you can’t get it down to where there’s no P. acnes. If you blunt the immune response, you’re still just blunting it, not turning it off. And if you’re addressing the plug in the follicle, it’s not a complete or rapid response," the dermatologist explained.
In clinical practice, Dr. Webster said he typically stops the oral antibiotic cold at about 12 weeks to avoid pigmentary changes and other side effects of long-term antibiotic therapy. At least 75% of patients can maintain their gains with topical therapy alone.
Compliance is often an issue with combination therapy. Patients need to understand that if they don’t use all of the medications consistently from day 1 they won’t get better.
"It’s tough with kids because kids expect to get better overnight. They see it on the Proactiv commercials and wonder why in the world they’re not better in 2 days," the dermatologist observed.
In this phase IV study, however, patient compliance was consistently excellent, perhaps because of the high disease severity. The treatment compliance rate was 91% at week 2 and 86% at week 12.
Dr. Webster is a consultant for several pharmaceutical companies, including Valeant, whose subsidiary Medicis sponsored the phase IV study.
SDEF and this news organization are owned by the same parent company.
*This story was updated March 1, 2013.
MAUI, HAWAII – Combination therapy for severe acne, with a trio of familiar, well tolerated agents, knocked down the skin disease severity in a phase IV study such that 80% of patients deemed candidates for isotretinoin at baseline no longer qualified for the powerful oral retinoid 12 weeks later, Dr. Guy F. Webster reported at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
These data provide welcome news for patients who can’t take isotretinoin or don’t want to, as well as for the many physicians reluctant to prescribe the drug because of the considerable regulatory hassles and potentially serious side effects, including teratogenicity.
The treatment regimen in this open-label multicenter study consisted of an oral antibiotic, a topical antibiotic/retinoid agent, and benzoyl peroxide. More specifically, the 97 study participants aged 12-29 years, all with grade 3-4 moderate to severe facial acne by Investigator’s Global Assessment (IGA), were placed on once-daily minocycline HCL extended release at about 1 mg/kg, clindamycin phosphate 1.2%/tretinoin 0.025% gel, and 6% benzoyl peroxide foaming cloths. Patients were evaluated at weeks 0, 2, 4, 8, and 12.
At week 2, 44% of subjects already had at least a 1-grade improvement in IGA; by week 12, 89% did. Moreover, 56% of patients had at least a 2-grade improvement in IGA.
At least a 1-grade improvement on the Global Aesthetic Improvement Scale was documented in 83% of subjects at week 2 and 96% at week 12.
"With this therapy, you can get patients with really bad acne from bad to really mild without resorting to big-time drugs," observed Dr. Webster, professor of dermatology and internal medicine at Thomas Jefferson University, Philadelphia.
Week 12 mean facial inflammatory lesion counts fell by 62%, and noninflammatory lesion counts decreased by 49% from baselines of 33 and 44 lesions, respectively.
At baseline, 69 patients were judged by three blinded assessors of clinical photos to have acne sufficiently severe for them to be candidates for isotretinoin therapy. By week 12, this number had dwindled to 14 patients. In other words, 80% of patients were no longer deemed to be candidates for isotretinoin.
Eight patients experienced treatment-related adverse events consisting of transient mild to moderate irritation and/or redness, burning, stinging, and dry skin.
The results of this Phase-4 study are consistent with studies of other multidrug regimens for acne, albeit mostly conducted in less severely affected patients.
"The general paradigm is that mixed therapies are useful because other than isotretinoin and maybe spironolactone, no one drug is strong enough to stop acne effectively. If you just hit the [Propionibacterium acnes] hard, you can’t get it down to where there’s no P. acnes. If you blunt the immune response, you’re still just blunting it, not turning it off. And if you’re addressing the plug in the follicle, it’s not a complete or rapid response," the dermatologist explained.
In clinical practice, Dr. Webster said he typically stops the oral antibiotic cold at about 12 weeks to avoid pigmentary changes and other side effects of long-term antibiotic therapy. At least 75% of patients can maintain their gains with topical therapy alone.
Compliance is often an issue with combination therapy. Patients need to understand that if they don’t use all of the medications consistently from day 1 they won’t get better.
"It’s tough with kids because kids expect to get better overnight. They see it on the Proactiv commercials and wonder why in the world they’re not better in 2 days," the dermatologist observed.
In this phase IV study, however, patient compliance was consistently excellent, perhaps because of the high disease severity. The treatment compliance rate was 91% at week 2 and 86% at week 12.
Dr. Webster is a consultant for several pharmaceutical companies, including Valeant, whose subsidiary Medicis sponsored the phase IV study.
SDEF and this news organization are owned by the same parent company.
*This story was updated March 1, 2013.
AT THE HAWAII DERMATOLOGY SEMINAR SPONSORED BY SKIN DISEASE EDUCATION FOUNDATION (SDEF)
Major Finding: Eighty percent of patients with acne sufficiently severe that blinded evaluators judged them to be candidates for isotretinoin at baseline no longer qualified for the potent oral retinoid after 12 weeks on triple therapy with an oral antibiotic, benzoyl peroxide, and a topical antibiotic/retinoid.
Data Source: An open-label, multicenter, phase IV study involving 97 patients with moderate to severe acne.
Disclosures: The study was sponsored by Medicis. The presenter is a consultant to the company.
The puzzling relationship between diet and acne
The relationship between acne and diet has been an ongoing debate. There are no meta-analyses, randomized controlled clinical studies, or well-designed scientific trials that follow evidence-based guidelines to elucidate a cause-effect relationship. However, for decades anecdotal evidence has shown that acne and insulin resistance, such as that seen in patients with polycystic ovarian syndrome (PCOS), are highly linked. Now the literature points to the growing relationship between nutrition and the prevalence of acne, especially to glycemic index and the consumption of dairy.
Glycemic index is a ranking system based on the quality and quantity of consumed carbohydrates and its ability to raise blood sugar levels. Foods with high glycemic indices such as potatoes, bread, chips, and pasta, require more insulin to maintain blood glucose levels within the normal range. High-glycemic diets that are prevalent in the United States not only lead to insulin resistance, diabetes, obesity, and heart disease but also to acne.
Several studies have looked at the glycemic load, insulin sensitivity, and hormonal mediators correlating to acne (Am. J. Clin. Nutr. 2007; 86:107-15; J. Dermatol. Sci. 2008;50:41-52). Foods with a high-glycemic index may contribute to acne by elevating serum insulin concentrations (which can stimulate sebocyte proliferation and sebum production), suppress sex hormone-binding globulin (SHBG) concentrations, and raise androgen concentrations. On the contrary, low-glycemic-index foods increase SHBG and reduce androgen levels; this is of great importance because higher SHBG levels are associated with lower acne severity. Consumption of fat and carbohydrates increases sebum production and affects sebum composition, ultimately encouraging acne production (Br. J. Dermatol. 1967;79:119-21).
A new study by Anna Di Landro et al. published in the December 2012 found a link between acne and the consumption of milk, particularly in those drinking skim milk and more than three servings of milk per week (J. Am. Acad. Dermatol. 2012;67:1129-35).
Dr. Di Landro et al. also found that the consumption of fish had a protective effect on acne. This interesting finding points to the larger issue of acne developing in ethnic populations that immigrate to the United States. Population studies have shown that non-Western diets have a reduced incidence of acne. Western diets are deficient in long-chain omega-3 fatty acids. The ratio of omega-6 to omega-3 fatty acids in our Western diet is 10:1 to 20:1, vs. 3:1 to 2:1 in a non-Western diet. Omega-6 fatty acids in increased concentrations induce proinflammatory mediators and have been associated with the development of inflammatory acne. Western diets with high consumption of seafood have high levels of omega-3 fatty acids and have shown to decrease inflammatory mediators in the skin (Arch. Dermatol. 2003;139:941-2).
In my clinic, the ethnic populations that immigrate to the United States often develop acne to a greater extent than they had in their native countries. Although factors including stress, hormonal differences in foods, and pollution can be confounding factors, we must not ignore the Western diet that these populations adapt to is higher in refined sugars and carbohydrates and lower in vegetables and lean protein. Every acne patient in my clinic is asked to complete a nutritional questionnaire discussing the intake of fast food, carbohydrates, juice, sodas, and processed sugar. We have noticed that acne improves clinically and is more responsive to traditional acne medications when patients reduce their consumption of processed sugars and dairy and increase their intake of lean protein. Similarly, our PCOS patients who are treated with medications such as metformin, which improves the body’s ability to regulate blood glucose levels, have improvements in their acne. So, is acne a marker for early insulin resistance?
The underlying etiology of acne is multifactorial, although now we can appreciate diet as one of the causative factors. Although there is no direct correlation between obesity or insulin resistance and the prevalence of acne, a low glycemic index diet in combination with topical and systemic acne medications can be a powerful method of treating acne. Nutritional counseling is an adjunct educational service we should provide to our patients in addition to skin care advice and medical treatments for acne.
No single food directly causes acne, but a balanced diet can alter its severity. Encouraging our patients to eat a variety of fruits and vegetables, lean protein, and healthy fats can prevent the inflammation seen with acne and also can protect against cardiovascular disease, type II diabetes, and even obesity.
It is unfortunate that the medical education system in the United States has no formal nutrition education. Nearly every field of medicine including internal medicine, cardiology, endocrinology, allergy, pediatrics, obstetrics and gynecology, surgery, and not the least, dermatology, is influenced in some realm by nutrition. As the population diversifies, so will the importance of dietary guidance. We need to educate ourselves and our residents-in-training to better appreciate the symbiotic relationship between diet and skin health and to provide this guidance to our patients.
Dr. Talakoub is in private practice in McLean, Va.
Do you have questions about treating patients with dark skin? If so, send them to sknews@elsevier.com.
The relationship between acne and diet has been an ongoing debate. There are no meta-analyses, randomized controlled clinical studies, or well-designed scientific trials that follow evidence-based guidelines to elucidate a cause-effect relationship. However, for decades anecdotal evidence has shown that acne and insulin resistance, such as that seen in patients with polycystic ovarian syndrome (PCOS), are highly linked. Now the literature points to the growing relationship between nutrition and the prevalence of acne, especially to glycemic index and the consumption of dairy.
Glycemic index is a ranking system based on the quality and quantity of consumed carbohydrates and its ability to raise blood sugar levels. Foods with high glycemic indices such as potatoes, bread, chips, and pasta, require more insulin to maintain blood glucose levels within the normal range. High-glycemic diets that are prevalent in the United States not only lead to insulin resistance, diabetes, obesity, and heart disease but also to acne.
Several studies have looked at the glycemic load, insulin sensitivity, and hormonal mediators correlating to acne (Am. J. Clin. Nutr. 2007; 86:107-15; J. Dermatol. Sci. 2008;50:41-52). Foods with a high-glycemic index may contribute to acne by elevating serum insulin concentrations (which can stimulate sebocyte proliferation and sebum production), suppress sex hormone-binding globulin (SHBG) concentrations, and raise androgen concentrations. On the contrary, low-glycemic-index foods increase SHBG and reduce androgen levels; this is of great importance because higher SHBG levels are associated with lower acne severity. Consumption of fat and carbohydrates increases sebum production and affects sebum composition, ultimately encouraging acne production (Br. J. Dermatol. 1967;79:119-21).
A new study by Anna Di Landro et al. published in the December 2012 found a link between acne and the consumption of milk, particularly in those drinking skim milk and more than three servings of milk per week (J. Am. Acad. Dermatol. 2012;67:1129-35).
Dr. Di Landro et al. also found that the consumption of fish had a protective effect on acne. This interesting finding points to the larger issue of acne developing in ethnic populations that immigrate to the United States. Population studies have shown that non-Western diets have a reduced incidence of acne. Western diets are deficient in long-chain omega-3 fatty acids. The ratio of omega-6 to omega-3 fatty acids in our Western diet is 10:1 to 20:1, vs. 3:1 to 2:1 in a non-Western diet. Omega-6 fatty acids in increased concentrations induce proinflammatory mediators and have been associated with the development of inflammatory acne. Western diets with high consumption of seafood have high levels of omega-3 fatty acids and have shown to decrease inflammatory mediators in the skin (Arch. Dermatol. 2003;139:941-2).
In my clinic, the ethnic populations that immigrate to the United States often develop acne to a greater extent than they had in their native countries. Although factors including stress, hormonal differences in foods, and pollution can be confounding factors, we must not ignore the Western diet that these populations adapt to is higher in refined sugars and carbohydrates and lower in vegetables and lean protein. Every acne patient in my clinic is asked to complete a nutritional questionnaire discussing the intake of fast food, carbohydrates, juice, sodas, and processed sugar. We have noticed that acne improves clinically and is more responsive to traditional acne medications when patients reduce their consumption of processed sugars and dairy and increase their intake of lean protein. Similarly, our PCOS patients who are treated with medications such as metformin, which improves the body’s ability to regulate blood glucose levels, have improvements in their acne. So, is acne a marker for early insulin resistance?
The underlying etiology of acne is multifactorial, although now we can appreciate diet as one of the causative factors. Although there is no direct correlation between obesity or insulin resistance and the prevalence of acne, a low glycemic index diet in combination with topical and systemic acne medications can be a powerful method of treating acne. Nutritional counseling is an adjunct educational service we should provide to our patients in addition to skin care advice and medical treatments for acne.
No single food directly causes acne, but a balanced diet can alter its severity. Encouraging our patients to eat a variety of fruits and vegetables, lean protein, and healthy fats can prevent the inflammation seen with acne and also can protect against cardiovascular disease, type II diabetes, and even obesity.
It is unfortunate that the medical education system in the United States has no formal nutrition education. Nearly every field of medicine including internal medicine, cardiology, endocrinology, allergy, pediatrics, obstetrics and gynecology, surgery, and not the least, dermatology, is influenced in some realm by nutrition. As the population diversifies, so will the importance of dietary guidance. We need to educate ourselves and our residents-in-training to better appreciate the symbiotic relationship between diet and skin health and to provide this guidance to our patients.
Dr. Talakoub is in private practice in McLean, Va.
Do you have questions about treating patients with dark skin? If so, send them to sknews@elsevier.com.
The relationship between acne and diet has been an ongoing debate. There are no meta-analyses, randomized controlled clinical studies, or well-designed scientific trials that follow evidence-based guidelines to elucidate a cause-effect relationship. However, for decades anecdotal evidence has shown that acne and insulin resistance, such as that seen in patients with polycystic ovarian syndrome (PCOS), are highly linked. Now the literature points to the growing relationship between nutrition and the prevalence of acne, especially to glycemic index and the consumption of dairy.
Glycemic index is a ranking system based on the quality and quantity of consumed carbohydrates and its ability to raise blood sugar levels. Foods with high glycemic indices such as potatoes, bread, chips, and pasta, require more insulin to maintain blood glucose levels within the normal range. High-glycemic diets that are prevalent in the United States not only lead to insulin resistance, diabetes, obesity, and heart disease but also to acne.
Several studies have looked at the glycemic load, insulin sensitivity, and hormonal mediators correlating to acne (Am. J. Clin. Nutr. 2007; 86:107-15; J. Dermatol. Sci. 2008;50:41-52). Foods with a high-glycemic index may contribute to acne by elevating serum insulin concentrations (which can stimulate sebocyte proliferation and sebum production), suppress sex hormone-binding globulin (SHBG) concentrations, and raise androgen concentrations. On the contrary, low-glycemic-index foods increase SHBG and reduce androgen levels; this is of great importance because higher SHBG levels are associated with lower acne severity. Consumption of fat and carbohydrates increases sebum production and affects sebum composition, ultimately encouraging acne production (Br. J. Dermatol. 1967;79:119-21).
A new study by Anna Di Landro et al. published in the December 2012 found a link between acne and the consumption of milk, particularly in those drinking skim milk and more than three servings of milk per week (J. Am. Acad. Dermatol. 2012;67:1129-35).
Dr. Di Landro et al. also found that the consumption of fish had a protective effect on acne. This interesting finding points to the larger issue of acne developing in ethnic populations that immigrate to the United States. Population studies have shown that non-Western diets have a reduced incidence of acne. Western diets are deficient in long-chain omega-3 fatty acids. The ratio of omega-6 to omega-3 fatty acids in our Western diet is 10:1 to 20:1, vs. 3:1 to 2:1 in a non-Western diet. Omega-6 fatty acids in increased concentrations induce proinflammatory mediators and have been associated with the development of inflammatory acne. Western diets with high consumption of seafood have high levels of omega-3 fatty acids and have shown to decrease inflammatory mediators in the skin (Arch. Dermatol. 2003;139:941-2).
In my clinic, the ethnic populations that immigrate to the United States often develop acne to a greater extent than they had in their native countries. Although factors including stress, hormonal differences in foods, and pollution can be confounding factors, we must not ignore the Western diet that these populations adapt to is higher in refined sugars and carbohydrates and lower in vegetables and lean protein. Every acne patient in my clinic is asked to complete a nutritional questionnaire discussing the intake of fast food, carbohydrates, juice, sodas, and processed sugar. We have noticed that acne improves clinically and is more responsive to traditional acne medications when patients reduce their consumption of processed sugars and dairy and increase their intake of lean protein. Similarly, our PCOS patients who are treated with medications such as metformin, which improves the body’s ability to regulate blood glucose levels, have improvements in their acne. So, is acne a marker for early insulin resistance?
The underlying etiology of acne is multifactorial, although now we can appreciate diet as one of the causative factors. Although there is no direct correlation between obesity or insulin resistance and the prevalence of acne, a low glycemic index diet in combination with topical and systemic acne medications can be a powerful method of treating acne. Nutritional counseling is an adjunct educational service we should provide to our patients in addition to skin care advice and medical treatments for acne.
No single food directly causes acne, but a balanced diet can alter its severity. Encouraging our patients to eat a variety of fruits and vegetables, lean protein, and healthy fats can prevent the inflammation seen with acne and also can protect against cardiovascular disease, type II diabetes, and even obesity.
It is unfortunate that the medical education system in the United States has no formal nutrition education. Nearly every field of medicine including internal medicine, cardiology, endocrinology, allergy, pediatrics, obstetrics and gynecology, surgery, and not the least, dermatology, is influenced in some realm by nutrition. As the population diversifies, so will the importance of dietary guidance. We need to educate ourselves and our residents-in-training to better appreciate the symbiotic relationship between diet and skin health and to provide this guidance to our patients.
Dr. Talakoub is in private practice in McLean, Va.
Do you have questions about treating patients with dark skin? If so, send them to sknews@elsevier.com.
Clindamycin Phosphate 1.2%–Benzoyl Peroxide (5% or 2.5%) Plus Tazarotene Cream 0.1% for the Treatment of Acne
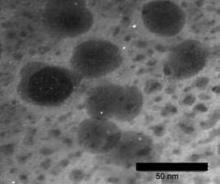
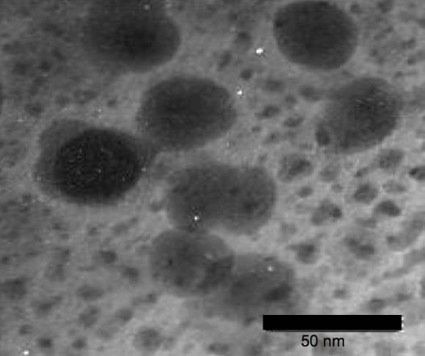
Nanoparticles take aim at acne
Nanotechnology stands to make a big difference in the way acne is treated.
A 0.1% concentration of benzoyl peroxide encapsulated in chitosan-alginate nanoparticles showed more antimicrobial activity against acne bacteria than typical benzoyl peroxide or the nanoparticles alone in a recently published in vitro study (J. Invest. Dermatol. 2012 Nov. 29 [doi:10.1038/jid.2012.399]).
Chitosan-alginate has both antimicrobial and anti-inflammatory impact on Propionibacterium acnes, wrote Dr. Adam Friedman of Albert Einstein College of Medicine, New York, and his colleagues. The nanoparticle structure preserves the antimicrobial and immunological properties of chitosan while alginate lends stability.
Benzoyl peroxide is, of course, already a first-line therapy for acne, but encapsulating benzoyl peroxide in the nanoparticles stands to reduce the irritating side effects common with topical benzoyl peroxide use, the researchers noted. Less irritation could greatly improve patient compliance.
In the study, scanning electron microscopy and transmission electron microscopy showed "severe disruption, destruction, and ‘peeling’ of the cell wall," the researchers wrote. "These images suggest that the cell damage is due to an osmotic disturbance" created by the encapsulated benzoyl peroxide.
Nanoparticle encapsulation "provides previously undescribed therapeutic opportunities, including delivery of multidrug regimens to combat resistant microbes and inflammatory disease states," the researchers said.
Nanotechnology stands to make a big difference in the way acne is treated.
A 0.1% concentration of benzoyl peroxide encapsulated in chitosan-alginate nanoparticles showed more antimicrobial activity against acne bacteria than typical benzoyl peroxide or the nanoparticles alone in a recently published in vitro study (J. Invest. Dermatol. 2012 Nov. 29 [doi:10.1038/jid.2012.399]).
Chitosan-alginate has both antimicrobial and anti-inflammatory impact on Propionibacterium acnes, wrote Dr. Adam Friedman of Albert Einstein College of Medicine, New York, and his colleagues. The nanoparticle structure preserves the antimicrobial and immunological properties of chitosan while alginate lends stability.
Benzoyl peroxide is, of course, already a first-line therapy for acne, but encapsulating benzoyl peroxide in the nanoparticles stands to reduce the irritating side effects common with topical benzoyl peroxide use, the researchers noted. Less irritation could greatly improve patient compliance.
In the study, scanning electron microscopy and transmission electron microscopy showed "severe disruption, destruction, and ‘peeling’ of the cell wall," the researchers wrote. "These images suggest that the cell damage is due to an osmotic disturbance" created by the encapsulated benzoyl peroxide.
Nanoparticle encapsulation "provides previously undescribed therapeutic opportunities, including delivery of multidrug regimens to combat resistant microbes and inflammatory disease states," the researchers said.
Nanotechnology stands to make a big difference in the way acne is treated.
A 0.1% concentration of benzoyl peroxide encapsulated in chitosan-alginate nanoparticles showed more antimicrobial activity against acne bacteria than typical benzoyl peroxide or the nanoparticles alone in a recently published in vitro study (J. Invest. Dermatol. 2012 Nov. 29 [doi:10.1038/jid.2012.399]).
Chitosan-alginate has both antimicrobial and anti-inflammatory impact on Propionibacterium acnes, wrote Dr. Adam Friedman of Albert Einstein College of Medicine, New York, and his colleagues. The nanoparticle structure preserves the antimicrobial and immunological properties of chitosan while alginate lends stability.
Benzoyl peroxide is, of course, already a first-line therapy for acne, but encapsulating benzoyl peroxide in the nanoparticles stands to reduce the irritating side effects common with topical benzoyl peroxide use, the researchers noted. Less irritation could greatly improve patient compliance.
In the study, scanning electron microscopy and transmission electron microscopy showed "severe disruption, destruction, and ‘peeling’ of the cell wall," the researchers wrote. "These images suggest that the cell damage is due to an osmotic disturbance" created by the encapsulated benzoyl peroxide.
Nanoparticle encapsulation "provides previously undescribed therapeutic opportunities, including delivery of multidrug regimens to combat resistant microbes and inflammatory disease states," the researchers said.
New-Generation Radiofrequency Technology
Acne 101: Educate Patients Before Topical Therapy
LAS VEGAS – Acne patients need to know it’s a bad idea to spot-treat comedones with topical retinoids, according to Dr. Linda F. Stein Gold.
"We have to educate our patients that if they spot treat, they’re going to have acne indefinitely until their body decides it’s done having acne," she said. "You have to educate them that they have to treat the entire acne-prone area and [keep treating it] to maintain remission. Their skin may look clear, but they are not cured."
Topical retinoids remain the gold standard for acne treatment. They clear and prevent comedones, help clindamycin and other antibiotics penetrate the skin, and calm inflammation, which is probably the initial step in acne’s development, noted Dr. Stein Gold, director of dermatology research at Henry Ford Hospital, Detroit.
Microsphere and micronized tretinoin gel formulations are less irritating than generic topical tretinoin, and they’re less apt to be deactivated by benzoyl peroxide and ultraviolet light, she said at SDEF Las Vegas Dermatology Seminar.
One of the newer topicals combines benzoyl peroxide and a retinoid stable in its presence, adapalene. One study found about a 70% reduction in lesions after 4 months of use (J. Drugs Dermatol. 2007;6:899-905). With that topical combination and other acne treatments, patients should be told that it may take a while to see maximal improvements, she said.
With any retinoid treatment, patients should also expect flare-ups of redness, irritation, and dryness in the first 2 weeks. "If I’m concerned about irritation, I’ll ask them to go every other night for the first 2 weeks until they adjust to the medication, and then titrate up to every night," Dr. Stein Gold noted. "I also have them use a moisturizer and general cleanser." But she tells them not to use facial scrubs, because scrubbing does "more harm than good."
Benzoil peroxide also remains important, either alone or in combination, because Propionibacterium acnes bacteria do not develop resistance to it, and it helps prevent resistance when used with antibiotics.
"You get a nice reduction both in inflammatory and noninflammatory lesions with benzoil peroxide," she said, but patients should be warned about possible skin bleaching.
The concentration of benzoyl peroxide isn’t that important, Dr. Stein Gold explained. "We know that 2.5% and 10% gels have fairly similar efficacy," she added (Int. J. Dermatol. 1986;25:664-7).
Benzoil peroxide gels are known to work well, although foams and cleansers are available for patients who find them too irritating. Cleansers appear most effective at reducing P. acnes on the face, as long as patients wait 20 seconds before rinsing. One study found foams effective on the back when massaged into dry skin for 20 seconds and patients waited 2 minutes before showering (J. Drugs Dermatol. 2012;11:830-3).
Whatever the treatment, Dr. Stein Gold noted, "stress compliance. My first question is, ‘Did you get a chance to fill your medicine?’ and then, ‘How many times do you think you got a chance to use it?’ "
She cautioned physicians to "have no expectations" – that way, patients won’t be afraid to admit that they only used it once or twice. Whatever their usage, "you say, ‘Great. Good for you. Keep on going.’ "
In addition, "the simpler you make the regimen, the more likely it is your patients are going to" stick with it, Dr. Stein Gold explained.
Dr. Stein Gold is a consultant or researcher for Galderma, Leo, Medicis, Novartis, and Stiefel. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Acne patients need to know it’s a bad idea to spot-treat comedones with topical retinoids, according to Dr. Linda F. Stein Gold.
"We have to educate our patients that if they spot treat, they’re going to have acne indefinitely until their body decides it’s done having acne," she said. "You have to educate them that they have to treat the entire acne-prone area and [keep treating it] to maintain remission. Their skin may look clear, but they are not cured."
Topical retinoids remain the gold standard for acne treatment. They clear and prevent comedones, help clindamycin and other antibiotics penetrate the skin, and calm inflammation, which is probably the initial step in acne’s development, noted Dr. Stein Gold, director of dermatology research at Henry Ford Hospital, Detroit.
Microsphere and micronized tretinoin gel formulations are less irritating than generic topical tretinoin, and they’re less apt to be deactivated by benzoyl peroxide and ultraviolet light, she said at SDEF Las Vegas Dermatology Seminar.
One of the newer topicals combines benzoyl peroxide and a retinoid stable in its presence, adapalene. One study found about a 70% reduction in lesions after 4 months of use (J. Drugs Dermatol. 2007;6:899-905). With that topical combination and other acne treatments, patients should be told that it may take a while to see maximal improvements, she said.
With any retinoid treatment, patients should also expect flare-ups of redness, irritation, and dryness in the first 2 weeks. "If I’m concerned about irritation, I’ll ask them to go every other night for the first 2 weeks until they adjust to the medication, and then titrate up to every night," Dr. Stein Gold noted. "I also have them use a moisturizer and general cleanser." But she tells them not to use facial scrubs, because scrubbing does "more harm than good."
Benzoil peroxide also remains important, either alone or in combination, because Propionibacterium acnes bacteria do not develop resistance to it, and it helps prevent resistance when used with antibiotics.
"You get a nice reduction both in inflammatory and noninflammatory lesions with benzoil peroxide," she said, but patients should be warned about possible skin bleaching.
The concentration of benzoyl peroxide isn’t that important, Dr. Stein Gold explained. "We know that 2.5% and 10% gels have fairly similar efficacy," she added (Int. J. Dermatol. 1986;25:664-7).
Benzoil peroxide gels are known to work well, although foams and cleansers are available for patients who find them too irritating. Cleansers appear most effective at reducing P. acnes on the face, as long as patients wait 20 seconds before rinsing. One study found foams effective on the back when massaged into dry skin for 20 seconds and patients waited 2 minutes before showering (J. Drugs Dermatol. 2012;11:830-3).
Whatever the treatment, Dr. Stein Gold noted, "stress compliance. My first question is, ‘Did you get a chance to fill your medicine?’ and then, ‘How many times do you think you got a chance to use it?’ "
She cautioned physicians to "have no expectations" – that way, patients won’t be afraid to admit that they only used it once or twice. Whatever their usage, "you say, ‘Great. Good for you. Keep on going.’ "
In addition, "the simpler you make the regimen, the more likely it is your patients are going to" stick with it, Dr. Stein Gold explained.
Dr. Stein Gold is a consultant or researcher for Galderma, Leo, Medicis, Novartis, and Stiefel. SDEF and this news organization are owned by Frontline Medical Communications.
LAS VEGAS – Acne patients need to know it’s a bad idea to spot-treat comedones with topical retinoids, according to Dr. Linda F. Stein Gold.
"We have to educate our patients that if they spot treat, they’re going to have acne indefinitely until their body decides it’s done having acne," she said. "You have to educate them that they have to treat the entire acne-prone area and [keep treating it] to maintain remission. Their skin may look clear, but they are not cured."
Topical retinoids remain the gold standard for acne treatment. They clear and prevent comedones, help clindamycin and other antibiotics penetrate the skin, and calm inflammation, which is probably the initial step in acne’s development, noted Dr. Stein Gold, director of dermatology research at Henry Ford Hospital, Detroit.
Microsphere and micronized tretinoin gel formulations are less irritating than generic topical tretinoin, and they’re less apt to be deactivated by benzoyl peroxide and ultraviolet light, she said at SDEF Las Vegas Dermatology Seminar.
One of the newer topicals combines benzoyl peroxide and a retinoid stable in its presence, adapalene. One study found about a 70% reduction in lesions after 4 months of use (J. Drugs Dermatol. 2007;6:899-905). With that topical combination and other acne treatments, patients should be told that it may take a while to see maximal improvements, she said.
With any retinoid treatment, patients should also expect flare-ups of redness, irritation, and dryness in the first 2 weeks. "If I’m concerned about irritation, I’ll ask them to go every other night for the first 2 weeks until they adjust to the medication, and then titrate up to every night," Dr. Stein Gold noted. "I also have them use a moisturizer and general cleanser." But she tells them not to use facial scrubs, because scrubbing does "more harm than good."
Benzoil peroxide also remains important, either alone or in combination, because Propionibacterium acnes bacteria do not develop resistance to it, and it helps prevent resistance when used with antibiotics.
"You get a nice reduction both in inflammatory and noninflammatory lesions with benzoil peroxide," she said, but patients should be warned about possible skin bleaching.
The concentration of benzoyl peroxide isn’t that important, Dr. Stein Gold explained. "We know that 2.5% and 10% gels have fairly similar efficacy," she added (Int. J. Dermatol. 1986;25:664-7).
Benzoil peroxide gels are known to work well, although foams and cleansers are available for patients who find them too irritating. Cleansers appear most effective at reducing P. acnes on the face, as long as patients wait 20 seconds before rinsing. One study found foams effective on the back when massaged into dry skin for 20 seconds and patients waited 2 minutes before showering (J. Drugs Dermatol. 2012;11:830-3).
Whatever the treatment, Dr. Stein Gold noted, "stress compliance. My first question is, ‘Did you get a chance to fill your medicine?’ and then, ‘How many times do you think you got a chance to use it?’ "
She cautioned physicians to "have no expectations" – that way, patients won’t be afraid to admit that they only used it once or twice. Whatever their usage, "you say, ‘Great. Good for you. Keep on going.’ "
In addition, "the simpler you make the regimen, the more likely it is your patients are going to" stick with it, Dr. Stein Gold explained.
Dr. Stein Gold is a consultant or researcher for Galderma, Leo, Medicis, Novartis, and Stiefel. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR