User login
FDA approves midostaurin for adult patients with FLT3+ AML
The Food and Drug Administration has approved midostaurin for the treatment of FLT3 mutation–positive acute myeloid leukemia (FLT3+ AML) in adult patients in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation.
Approval was based on results from a randomized, double-blind, placebo-controlled trial of 717 patients with previously untreated FLT3+ AML. The hazard ratio for overall survival in patients receiving midostaurin, compared with a placebo, was 0.77 (P = .016). A companion diagnostic tool, the LeukoStrat CDx FLT3 Mutation Assay manufactured by Invivoscribe Technologies, was also approved.
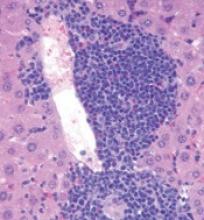
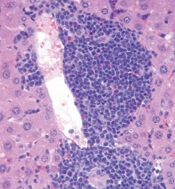
Midostaurin was also approved for the treatment of aggressive systemic mastocytosis, SM with associated hematological neoplasm, or mast cell leukemia. This indication approval was based on a single-arm, open-label study of midostaurin 100 mg, taken orally twice daily. Complete plus incomplete remission rates were 38% for ASM and 16% for SM with associated hematological neoplasm. Common adverse events included nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, fever, headache, and dyspnea.
The recommended dose of midostaurin in AML is 50 mg twice daily with food on days 8 to 21 of each cycle of induction and consolidation chemotherapy followed by 50 mg with food as a single agent for up to 12 months. The recommended dose for the treatment of adults with aggressive SM, SM with associated hematological neoplasm, or mast cell leukemia is 100 mg twice daily with food, the FDA said.
Midostaurin will be marketed as Rydapt by Novartis Pharmaceuticals.
The Food and Drug Administration has approved midostaurin for the treatment of FLT3 mutation–positive acute myeloid leukemia (FLT3+ AML) in adult patients in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation.
Approval was based on results from a randomized, double-blind, placebo-controlled trial of 717 patients with previously untreated FLT3+ AML. The hazard ratio for overall survival in patients receiving midostaurin, compared with a placebo, was 0.77 (P = .016). A companion diagnostic tool, the LeukoStrat CDx FLT3 Mutation Assay manufactured by Invivoscribe Technologies, was also approved.
Midostaurin was also approved for the treatment of aggressive systemic mastocytosis, SM with associated hematological neoplasm, or mast cell leukemia. This indication approval was based on a single-arm, open-label study of midostaurin 100 mg, taken orally twice daily. Complete plus incomplete remission rates were 38% for ASM and 16% for SM with associated hematological neoplasm. Common adverse events included nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, fever, headache, and dyspnea.
The recommended dose of midostaurin in AML is 50 mg twice daily with food on days 8 to 21 of each cycle of induction and consolidation chemotherapy followed by 50 mg with food as a single agent for up to 12 months. The recommended dose for the treatment of adults with aggressive SM, SM with associated hematological neoplasm, or mast cell leukemia is 100 mg twice daily with food, the FDA said.
Midostaurin will be marketed as Rydapt by Novartis Pharmaceuticals.
The Food and Drug Administration has approved midostaurin for the treatment of FLT3 mutation–positive acute myeloid leukemia (FLT3+ AML) in adult patients in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation.
Approval was based on results from a randomized, double-blind, placebo-controlled trial of 717 patients with previously untreated FLT3+ AML. The hazard ratio for overall survival in patients receiving midostaurin, compared with a placebo, was 0.77 (P = .016). A companion diagnostic tool, the LeukoStrat CDx FLT3 Mutation Assay manufactured by Invivoscribe Technologies, was also approved.
Midostaurin was also approved for the treatment of aggressive systemic mastocytosis, SM with associated hematological neoplasm, or mast cell leukemia. This indication approval was based on a single-arm, open-label study of midostaurin 100 mg, taken orally twice daily. Complete plus incomplete remission rates were 38% for ASM and 16% for SM with associated hematological neoplasm. Common adverse events included nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, fever, headache, and dyspnea.
The recommended dose of midostaurin in AML is 50 mg twice daily with food on days 8 to 21 of each cycle of induction and consolidation chemotherapy followed by 50 mg with food as a single agent for up to 12 months. The recommended dose for the treatment of adults with aggressive SM, SM with associated hematological neoplasm, or mast cell leukemia is 100 mg twice daily with food, the FDA said.
Midostaurin will be marketed as Rydapt by Novartis Pharmaceuticals.
Role of TET2 in hematologic malignancies
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
Extended maraviroc helps prevent graft-versus-host disease
ORLANDO – The use of the CCR5 antagonist maraviroc for 90 days is safe and effective for graft-versus-host disease (GVHD) prophylaxis in patients undergoing allogeneic stem cell transplantation, according to findings from a phase II study.
An earlier study showed that CCR5 blockade using maraviroc for 33 days was associated with a low incidence of acute GVHD, as well as with absence of early liver and gut GVHD – although delayed severe cases of visceral GVHD still occurred.
The current study was performed because the prior findings raised concerns that brief blockade was insufficient for preventing GVHD over a longer period of time. The new findings show that an extended course may indeed provide additional benefits, Ran Reshef, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In 37 high-risk patients who received allogeneic stem cell transplantation from unrelated donors using fludarabine/busulfan (Flu/Bu2) conditioning followed by peripheral blood stem cells, maraviroc was given at a dose of 300 mg twice daily, in addition to standard tacrolimus and methotrexate.
The 180-day rates of grade 2-4 and grade 3-4 acute GVHD (the primary endpoint of the study) in these patients were 27% and 5%, respectively. These rates were very similar to the 24% and 6% rates seen in the first study at 6 months after 30 days of maraviroc treatment, said Dr. Reshef of Columbia University Medical Center, New York.
The earlier results were “driven not so much by a reduction in the rates of skin GVHD, but by low rates of visceral GVHD of the gut and the liver – with a striking absence of gut and liver GVHD in the first 100 days,” he said.
Dr. Reshef also noted that the current study had a less favorable donor mix, as no matched related donors were included because of the earlier study’s very low rates of GVHD – with or without maraviroc – in those with related donors, who composed a third of donors.
Long-term follow-up of results from the earlier study, with comparison of a large contemporary control cohort, showed that “there is in fact an impact ... on grade 2-4 and grade 3-4 [GVHD], although the number of events is small, and the study was not powered enough to reach statistical significance,” Dr. Reshef said. The rates of chronic GVHD did not differ between the study subjects and contemporary controls, he noted.
At 100 days in the current study, there were no cases of liver GVHD, two cases of mild upper-GI GVHD, and one case of severe gut GVHD. At 1 year, the disease relapse rate was “fairly reasonable” at 30%, nonrelapse mortality was 12% with only one case of death from GVHD, and the incidence of chronic GVHD was 8%, which was significantly lower than in the prior study, he said.
The low rate of chronic GVHD led to a GVHD/relapse-free survival (GRFS) rate of 49%.
“To put this in context, the [Center for International Blood & Marrow Transplant Research] data for reduced-intensity transplants ... have shown 25% for acute myeloid leukemia and 12% for myelodysplastic syndrome,” he said. “So, we feel that these are by far improved numbers, compared with this benchmark.”
To determine which patients develop GVHD despite chemotaxis blockade and why, Dr. Reshef and his colleagues developed a pharmacodynamic assay to assess the activity of maraviroc in fresh blood samples. They found that those with insufficient CCR5 blockade on day 0 were those with higher incidence of severe acute GVHD, nonrelapse mortality, GRFS, and overall survival.
The investigators performed pharmacokinetic analysis using combined data from both trials to improve understanding of why some patients have insufficient CCR5 blockade. This showed significant variability in day 0 trough of maraviroc among patients (median of 65 ng/mL, range 12-316 ng/mL); levels above the median were associated with a significantly lower incidence of acute grade 2-4 GVHD and a trend toward improved GRFS.
These studies of maraviroc, which was originally developed for the treatment of HIV infection, were done to test the belief that blocking lymphocyte migration might prevent GVHD without interfering with graft-versus-tumor activity. Based on the earlier findings, Dr. Reshef and his colleagues hypothesized that treatment up to day 90 would decrease the rate to less than 30%, from a historical rate of 52%.
Patients in the study were high risk by virtue of age (median, 64 years), HLA matching (matched unrelated, 84%; mismatched unrelated, 16%), and comorbidities (comorbidity index greater than 2 in 49%). Underlying diseases were acute leukemia (78%), myelodysplastic syndrome (16%), and myeloproliferative neoplasm and cutaneous T-cell lymphomas (3% each).
At a median follow-up of 21 months, the 3-month course of maraviroc was well tolerated. Eight patients did not complete treatment because of disease relapse (five patients), skin reaction (one patient), early infection-related death (one patient), or poor tolerance of oral drugs (one patient). Neutrophil, platelet, and T-cell engraftment were similar to historical controls, and rates of infections were also similar, Dr Reshef noted.
“To conclude, an extended course of maraviroc up to day 90 is feasible and safe in the majority of patients,” he said. “This study confirms the effect of CCR5 blockade on visceral GVHD. I’m still awaiting a randomized study to confirm that further.
“A long course of maraviroc does not necessarily affect the rates of acute GVHD, but may help reduce chronic GVHD and improve GRFS,” Dr. Reshef said. “We should look further into the pharmacodynamic and pharmacokinetic variables.”
Dr. Reshef reported receiving research funding from Pfizer.
ORLANDO – The use of the CCR5 antagonist maraviroc for 90 days is safe and effective for graft-versus-host disease (GVHD) prophylaxis in patients undergoing allogeneic stem cell transplantation, according to findings from a phase II study.
An earlier study showed that CCR5 blockade using maraviroc for 33 days was associated with a low incidence of acute GVHD, as well as with absence of early liver and gut GVHD – although delayed severe cases of visceral GVHD still occurred.
The current study was performed because the prior findings raised concerns that brief blockade was insufficient for preventing GVHD over a longer period of time. The new findings show that an extended course may indeed provide additional benefits, Ran Reshef, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In 37 high-risk patients who received allogeneic stem cell transplantation from unrelated donors using fludarabine/busulfan (Flu/Bu2) conditioning followed by peripheral blood stem cells, maraviroc was given at a dose of 300 mg twice daily, in addition to standard tacrolimus and methotrexate.
The 180-day rates of grade 2-4 and grade 3-4 acute GVHD (the primary endpoint of the study) in these patients were 27% and 5%, respectively. These rates were very similar to the 24% and 6% rates seen in the first study at 6 months after 30 days of maraviroc treatment, said Dr. Reshef of Columbia University Medical Center, New York.
The earlier results were “driven not so much by a reduction in the rates of skin GVHD, but by low rates of visceral GVHD of the gut and the liver – with a striking absence of gut and liver GVHD in the first 100 days,” he said.
Dr. Reshef also noted that the current study had a less favorable donor mix, as no matched related donors were included because of the earlier study’s very low rates of GVHD – with or without maraviroc – in those with related donors, who composed a third of donors.
Long-term follow-up of results from the earlier study, with comparison of a large contemporary control cohort, showed that “there is in fact an impact ... on grade 2-4 and grade 3-4 [GVHD], although the number of events is small, and the study was not powered enough to reach statistical significance,” Dr. Reshef said. The rates of chronic GVHD did not differ between the study subjects and contemporary controls, he noted.
At 100 days in the current study, there were no cases of liver GVHD, two cases of mild upper-GI GVHD, and one case of severe gut GVHD. At 1 year, the disease relapse rate was “fairly reasonable” at 30%, nonrelapse mortality was 12% with only one case of death from GVHD, and the incidence of chronic GVHD was 8%, which was significantly lower than in the prior study, he said.
The low rate of chronic GVHD led to a GVHD/relapse-free survival (GRFS) rate of 49%.
“To put this in context, the [Center for International Blood & Marrow Transplant Research] data for reduced-intensity transplants ... have shown 25% for acute myeloid leukemia and 12% for myelodysplastic syndrome,” he said. “So, we feel that these are by far improved numbers, compared with this benchmark.”
To determine which patients develop GVHD despite chemotaxis blockade and why, Dr. Reshef and his colleagues developed a pharmacodynamic assay to assess the activity of maraviroc in fresh blood samples. They found that those with insufficient CCR5 blockade on day 0 were those with higher incidence of severe acute GVHD, nonrelapse mortality, GRFS, and overall survival.
The investigators performed pharmacokinetic analysis using combined data from both trials to improve understanding of why some patients have insufficient CCR5 blockade. This showed significant variability in day 0 trough of maraviroc among patients (median of 65 ng/mL, range 12-316 ng/mL); levels above the median were associated with a significantly lower incidence of acute grade 2-4 GVHD and a trend toward improved GRFS.
These studies of maraviroc, which was originally developed for the treatment of HIV infection, were done to test the belief that blocking lymphocyte migration might prevent GVHD without interfering with graft-versus-tumor activity. Based on the earlier findings, Dr. Reshef and his colleagues hypothesized that treatment up to day 90 would decrease the rate to less than 30%, from a historical rate of 52%.
Patients in the study were high risk by virtue of age (median, 64 years), HLA matching (matched unrelated, 84%; mismatched unrelated, 16%), and comorbidities (comorbidity index greater than 2 in 49%). Underlying diseases were acute leukemia (78%), myelodysplastic syndrome (16%), and myeloproliferative neoplasm and cutaneous T-cell lymphomas (3% each).
At a median follow-up of 21 months, the 3-month course of maraviroc was well tolerated. Eight patients did not complete treatment because of disease relapse (five patients), skin reaction (one patient), early infection-related death (one patient), or poor tolerance of oral drugs (one patient). Neutrophil, platelet, and T-cell engraftment were similar to historical controls, and rates of infections were also similar, Dr Reshef noted.
“To conclude, an extended course of maraviroc up to day 90 is feasible and safe in the majority of patients,” he said. “This study confirms the effect of CCR5 blockade on visceral GVHD. I’m still awaiting a randomized study to confirm that further.
“A long course of maraviroc does not necessarily affect the rates of acute GVHD, but may help reduce chronic GVHD and improve GRFS,” Dr. Reshef said. “We should look further into the pharmacodynamic and pharmacokinetic variables.”
Dr. Reshef reported receiving research funding from Pfizer.
ORLANDO – The use of the CCR5 antagonist maraviroc for 90 days is safe and effective for graft-versus-host disease (GVHD) prophylaxis in patients undergoing allogeneic stem cell transplantation, according to findings from a phase II study.
An earlier study showed that CCR5 blockade using maraviroc for 33 days was associated with a low incidence of acute GVHD, as well as with absence of early liver and gut GVHD – although delayed severe cases of visceral GVHD still occurred.
The current study was performed because the prior findings raised concerns that brief blockade was insufficient for preventing GVHD over a longer period of time. The new findings show that an extended course may indeed provide additional benefits, Ran Reshef, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
In 37 high-risk patients who received allogeneic stem cell transplantation from unrelated donors using fludarabine/busulfan (Flu/Bu2) conditioning followed by peripheral blood stem cells, maraviroc was given at a dose of 300 mg twice daily, in addition to standard tacrolimus and methotrexate.
The 180-day rates of grade 2-4 and grade 3-4 acute GVHD (the primary endpoint of the study) in these patients were 27% and 5%, respectively. These rates were very similar to the 24% and 6% rates seen in the first study at 6 months after 30 days of maraviroc treatment, said Dr. Reshef of Columbia University Medical Center, New York.
The earlier results were “driven not so much by a reduction in the rates of skin GVHD, but by low rates of visceral GVHD of the gut and the liver – with a striking absence of gut and liver GVHD in the first 100 days,” he said.
Dr. Reshef also noted that the current study had a less favorable donor mix, as no matched related donors were included because of the earlier study’s very low rates of GVHD – with or without maraviroc – in those with related donors, who composed a third of donors.
Long-term follow-up of results from the earlier study, with comparison of a large contemporary control cohort, showed that “there is in fact an impact ... on grade 2-4 and grade 3-4 [GVHD], although the number of events is small, and the study was not powered enough to reach statistical significance,” Dr. Reshef said. The rates of chronic GVHD did not differ between the study subjects and contemporary controls, he noted.
At 100 days in the current study, there were no cases of liver GVHD, two cases of mild upper-GI GVHD, and one case of severe gut GVHD. At 1 year, the disease relapse rate was “fairly reasonable” at 30%, nonrelapse mortality was 12% with only one case of death from GVHD, and the incidence of chronic GVHD was 8%, which was significantly lower than in the prior study, he said.
The low rate of chronic GVHD led to a GVHD/relapse-free survival (GRFS) rate of 49%.
“To put this in context, the [Center for International Blood & Marrow Transplant Research] data for reduced-intensity transplants ... have shown 25% for acute myeloid leukemia and 12% for myelodysplastic syndrome,” he said. “So, we feel that these are by far improved numbers, compared with this benchmark.”
To determine which patients develop GVHD despite chemotaxis blockade and why, Dr. Reshef and his colleagues developed a pharmacodynamic assay to assess the activity of maraviroc in fresh blood samples. They found that those with insufficient CCR5 blockade on day 0 were those with higher incidence of severe acute GVHD, nonrelapse mortality, GRFS, and overall survival.
The investigators performed pharmacokinetic analysis using combined data from both trials to improve understanding of why some patients have insufficient CCR5 blockade. This showed significant variability in day 0 trough of maraviroc among patients (median of 65 ng/mL, range 12-316 ng/mL); levels above the median were associated with a significantly lower incidence of acute grade 2-4 GVHD and a trend toward improved GRFS.
These studies of maraviroc, which was originally developed for the treatment of HIV infection, were done to test the belief that blocking lymphocyte migration might prevent GVHD without interfering with graft-versus-tumor activity. Based on the earlier findings, Dr. Reshef and his colleagues hypothesized that treatment up to day 90 would decrease the rate to less than 30%, from a historical rate of 52%.
Patients in the study were high risk by virtue of age (median, 64 years), HLA matching (matched unrelated, 84%; mismatched unrelated, 16%), and comorbidities (comorbidity index greater than 2 in 49%). Underlying diseases were acute leukemia (78%), myelodysplastic syndrome (16%), and myeloproliferative neoplasm and cutaneous T-cell lymphomas (3% each).
At a median follow-up of 21 months, the 3-month course of maraviroc was well tolerated. Eight patients did not complete treatment because of disease relapse (five patients), skin reaction (one patient), early infection-related death (one patient), or poor tolerance of oral drugs (one patient). Neutrophil, platelet, and T-cell engraftment were similar to historical controls, and rates of infections were also similar, Dr Reshef noted.
“To conclude, an extended course of maraviroc up to day 90 is feasible and safe in the majority of patients,” he said. “This study confirms the effect of CCR5 blockade on visceral GVHD. I’m still awaiting a randomized study to confirm that further.
“A long course of maraviroc does not necessarily affect the rates of acute GVHD, but may help reduce chronic GVHD and improve GRFS,” Dr. Reshef said. “We should look further into the pharmacodynamic and pharmacokinetic variables.”
Dr. Reshef reported receiving research funding from Pfizer.
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: The 180-day rates of grade 2-4 and grade 3-4 acute GVHD were 27% and 5%, respectively.
Data source: A phase II study of 37 patients.
Disclosures: Dr. Reshef reported receiving research funding from Pfizer.
Second cancers take greater toll on younger patients
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Pegylated interferon alfa-2a induces durable responses in MPNs
Pegylated interferon alfa-2a can induce durable hematologic and molecular responses in patients with advanced essential thrombocythemia and polycythemia vera, according to a post hoc analysis of data from a prospective, open-label, phase II trial.
Of 83 patients treated with pegylated interferon alfa-2a, 66 (80%) experienced hematological response, and of 55 of the 83 who were positive for the JAK2 Val617 mutation and who were evaluable for a molecular response, 35 (64%) experienced molecular response. The median response durations were 66 months and 53 months, respectively, wrote Lucia Masarova, MD, and her colleagues at MD Anderson Cancer Center, Houston.
Of the 66 hematological responders, 26 (39%) maintained some response during a median follow-up of 83 months. Among the 40 who lost their response, 19 had dose reductions or had the drug withheld because of intolerance or toxicity, 1 developed concurrent diffuse large B-cell lymphoma, and 20 progressed despite treatment with the highest tolerable dose of pegylated interferon alfa-2a. Of note, 7 (28%) of 25 patients who were treated for at least 46 months (median of 77 months) sustained their hematologic response for a median of 6 months after discontinuation of therapy, the investigators said (Lancet Haematol. 2017 Apr;4:e165-75).
Of the 35 molecular responders, 25 (71%) maintained some response during follow-up. Of the nine evaluable patients who did not maintain response (the 10th patient was taken off the study because of concurrent non-Hodgkin lymphoma) four lost response at a median of 2 years after the drug was withheld, and five lost response while on therapy. Three maintained their complete molecular remission – for 18, 55, and 79 months – after discontinuation of therapy.
“Only one patient who achieved a complete molecular remission has relapsed after stopping therapy for 16 months (complete molecular remission duration, 66 months). The other 9 of 10 patients had durable remissions (median duration 69 months),” the investigators wrote, noting that among the 20 patients with a partial molecular remission, 5 (25%) sustained best partial remission, 7 (28%) are in minor molecular remission, 8 (32%) lost their response, and 3 of 5 (60%) with minor molecular remission sustained that remission.
The study comprised adults over age 18 years who were diagnosed with essential thrombocythemia (40 patients) or polycythemia vera (43) and were enrolled during May 2005 to October 2009. Of the 83 patients, 52 (63%) had received some form of therapy prior to enrollment, including 14 who were treated with standard interferon alfa-2a and 1 who was treated with pegylated interferon alfa-2a. The initial starting dose of pegylated interferon alfa-2a used in the study was 450 mcg delivered subcutaneously once each week, but the dose was decreased in a stepwise manner to a final starting dose of 90 mcg per week due to toxicity; starting doses include 450 mcg in 3 patients, 360 mcg in 3 patients, 270 mcg in 19 patients, 180 mcg in 26 patients, and 90 mcg in 32 patients). Treatment continued as long as clinical benefit continued, and hematological responses were assessed every 3-6 months.
Treatment-related toxicities decreased over time, but five patients had treatment-limiting grade 3 or 4 toxicities after 60 months on therapy; overall 18 patients (22%) discontinued treatment due to toxicity.
The therapeutic approach to essential thrombocythemia and polycythemia vera has mainly focused on control of blood counts and reduction of the risk of thrombosis. Those at high risk for thrombosis generally undergo cytoreductive therapy with hydroxyurea. Recombinant interferon alfa is an alternative to hydroxyurea “given its biological, anti-proliferative, immunomodulating, and anticlonal effects,” the investigators explained.
“However, the widespread use of this biological drug has been limited by high rates of discontinuation due to side effects. Pegylated forms of interferon have a better pharmacological profile than short-acting interferons: they require less frequent injection, lower immunogenicity, and possibly fewer toxic effects,” they said.
Although pegylated interferon-alfa 2a has shown promise in several trials, most had short follow-up. The nearly 7 years of follow-up in the current trial is almost twice as long as in those prior studies.
During the current study, including follow-up, eight major vascular thromboembolic events occurred. One was associated with heart catheterization, one with elective chest surgery, and one with an angiogram. The remaining five occurred with no discernible cause after a median of 38 months of therapy for an incidence of 1.22 unprovoked vascular thromboembolic events per 100 person-years, and three of those were in patients with complete hematologic response. Two of the five patients were under age 60 years and had no history of thrombosis. Another patient had a serious unprovoked cerebrovascular hemorrhage after 3 years on therapy and while in complete hematological response.
In addition, 7 of the 83 patients in the study had disease progression on therapy; 6 progressed to myelofibrosis, and 1 developed acute myeloid leukemia. The median time to transformation in these patients was 40 months.
At the time of publication, 32 patient remained in the study and 24 were receiving treatment. Nineteen were in hematologic response at last follow-up, and most (75%) were on a dose of 90 mcg or less per week.
In addition to showing that some patients achieve durable responses on pegylated interferon alfa-2a, this study provided five important observations, the investigators said: 1) Patients might continue to derive clinical benefit from pegylated interferon alfa-2a even after losing response. 2) Only complete molecular remissions are durable, and some cases can be sustained after therapy discontinuation. 3) Clinical activity of pegylated interferon alfa-2a is not correlated with JAK2 mutation status. 4) Toxic effects unrelated to dose may develop and can be treatment-limiting, even after a long exposure to the drug. 5) Disease-related vascular complications or progression to myelofibrosis can still occur in patients on therapy.
“Our findings suggest that pegylated interferon alfa-2a is a viable treatment option, especially for young patients who want to avoid prolonged cytotoxic therapy. Lower doses minimize side effects while retaining efficacy,” they wrote, suggesting – based on these and other results – a starting dose of 45 mcg weekly to limit adverse events and maximize response.
They also noted that treated patients with a history of autoimmune disease and those with mood disorder should be monitored closely for side effects.
Future studies on pegylated interferon afla-2a alone or in combination with novel immunomodulatory drugs are needed to identify patients who would benefit most from treatment, and additional objective response criteria, such as measurement of spleen size, bone marrow histology, and quality of life should be used to better assess clinical benefit, they said.
The National Cancer Institute funded the study. The authors reported having no disclosures.
The finding by Masarova et al. that interferon alfa induces durable responses that persist even after stopping treatment in a relatively large proportion of patients contradicts the main issues raised against use of interferon alfa in this setting, Jean-Jacques Kiladjian, MD, said in an editorial.
For example, despite concerns about side effects and an inability of patients to tolerate interferon alfa, the findings confirm that it can control myeloproliferative neoplasms at reduced doses, with toxicity similar to that reported with hydroxyurea and, importantly, with no new safety issues noted, he said.
Further, the findings underscore the value of achieving a molecular response, which is a subject of debate.
“In particular, patients who achieved complete molecular response derived the longest clinical benefit and none of them had disease progression,” he wrote (Lancet Haematol. 2017 Apr;4:e150-1).
While the investigators did not note a clear decrease in the expected incidence of transformation to myelofibrosis or acute leukemia among study participants, they did “underline the limitations of this study for accurate estimation of these events,” and two ongoing studies comparing interferon alfa and hydroxyurea in much larger cohorts (the Proud-PV and MPD-RC 112 studies) should provide stronger evidence regarding the leukemogenic potential of the therapies, he said.
Dr. Kiladjian is with Assistance Publique–Hopitaux de Paris and Centre d’Investigations Cliniques, Hopital Saint-Louis, Université Paris Diderot, France. He reported receiving institutional research grants from Novartis and AOP Orphan, and serving as an advisory board member for Novartis, AOP Orphan, and Shire.
The finding by Masarova et al. that interferon alfa induces durable responses that persist even after stopping treatment in a relatively large proportion of patients contradicts the main issues raised against use of interferon alfa in this setting, Jean-Jacques Kiladjian, MD, said in an editorial.
For example, despite concerns about side effects and an inability of patients to tolerate interferon alfa, the findings confirm that it can control myeloproliferative neoplasms at reduced doses, with toxicity similar to that reported with hydroxyurea and, importantly, with no new safety issues noted, he said.
Further, the findings underscore the value of achieving a molecular response, which is a subject of debate.
“In particular, patients who achieved complete molecular response derived the longest clinical benefit and none of them had disease progression,” he wrote (Lancet Haematol. 2017 Apr;4:e150-1).
While the investigators did not note a clear decrease in the expected incidence of transformation to myelofibrosis or acute leukemia among study participants, they did “underline the limitations of this study for accurate estimation of these events,” and two ongoing studies comparing interferon alfa and hydroxyurea in much larger cohorts (the Proud-PV and MPD-RC 112 studies) should provide stronger evidence regarding the leukemogenic potential of the therapies, he said.
Dr. Kiladjian is with Assistance Publique–Hopitaux de Paris and Centre d’Investigations Cliniques, Hopital Saint-Louis, Université Paris Diderot, France. He reported receiving institutional research grants from Novartis and AOP Orphan, and serving as an advisory board member for Novartis, AOP Orphan, and Shire.
The finding by Masarova et al. that interferon alfa induces durable responses that persist even after stopping treatment in a relatively large proportion of patients contradicts the main issues raised against use of interferon alfa in this setting, Jean-Jacques Kiladjian, MD, said in an editorial.
For example, despite concerns about side effects and an inability of patients to tolerate interferon alfa, the findings confirm that it can control myeloproliferative neoplasms at reduced doses, with toxicity similar to that reported with hydroxyurea and, importantly, with no new safety issues noted, he said.
Further, the findings underscore the value of achieving a molecular response, which is a subject of debate.
“In particular, patients who achieved complete molecular response derived the longest clinical benefit and none of them had disease progression,” he wrote (Lancet Haematol. 2017 Apr;4:e150-1).
While the investigators did not note a clear decrease in the expected incidence of transformation to myelofibrosis or acute leukemia among study participants, they did “underline the limitations of this study for accurate estimation of these events,” and two ongoing studies comparing interferon alfa and hydroxyurea in much larger cohorts (the Proud-PV and MPD-RC 112 studies) should provide stronger evidence regarding the leukemogenic potential of the therapies, he said.
Dr. Kiladjian is with Assistance Publique–Hopitaux de Paris and Centre d’Investigations Cliniques, Hopital Saint-Louis, Université Paris Diderot, France. He reported receiving institutional research grants from Novartis and AOP Orphan, and serving as an advisory board member for Novartis, AOP Orphan, and Shire.
Pegylated interferon alfa-2a can induce durable hematologic and molecular responses in patients with advanced essential thrombocythemia and polycythemia vera, according to a post hoc analysis of data from a prospective, open-label, phase II trial.
Of 83 patients treated with pegylated interferon alfa-2a, 66 (80%) experienced hematological response, and of 55 of the 83 who were positive for the JAK2 Val617 mutation and who were evaluable for a molecular response, 35 (64%) experienced molecular response. The median response durations were 66 months and 53 months, respectively, wrote Lucia Masarova, MD, and her colleagues at MD Anderson Cancer Center, Houston.
Of the 66 hematological responders, 26 (39%) maintained some response during a median follow-up of 83 months. Among the 40 who lost their response, 19 had dose reductions or had the drug withheld because of intolerance or toxicity, 1 developed concurrent diffuse large B-cell lymphoma, and 20 progressed despite treatment with the highest tolerable dose of pegylated interferon alfa-2a. Of note, 7 (28%) of 25 patients who were treated for at least 46 months (median of 77 months) sustained their hematologic response for a median of 6 months after discontinuation of therapy, the investigators said (Lancet Haematol. 2017 Apr;4:e165-75).
Of the 35 molecular responders, 25 (71%) maintained some response during follow-up. Of the nine evaluable patients who did not maintain response (the 10th patient was taken off the study because of concurrent non-Hodgkin lymphoma) four lost response at a median of 2 years after the drug was withheld, and five lost response while on therapy. Three maintained their complete molecular remission – for 18, 55, and 79 months – after discontinuation of therapy.
“Only one patient who achieved a complete molecular remission has relapsed after stopping therapy for 16 months (complete molecular remission duration, 66 months). The other 9 of 10 patients had durable remissions (median duration 69 months),” the investigators wrote, noting that among the 20 patients with a partial molecular remission, 5 (25%) sustained best partial remission, 7 (28%) are in minor molecular remission, 8 (32%) lost their response, and 3 of 5 (60%) with minor molecular remission sustained that remission.
The study comprised adults over age 18 years who were diagnosed with essential thrombocythemia (40 patients) or polycythemia vera (43) and were enrolled during May 2005 to October 2009. Of the 83 patients, 52 (63%) had received some form of therapy prior to enrollment, including 14 who were treated with standard interferon alfa-2a and 1 who was treated with pegylated interferon alfa-2a. The initial starting dose of pegylated interferon alfa-2a used in the study was 450 mcg delivered subcutaneously once each week, but the dose was decreased in a stepwise manner to a final starting dose of 90 mcg per week due to toxicity; starting doses include 450 mcg in 3 patients, 360 mcg in 3 patients, 270 mcg in 19 patients, 180 mcg in 26 patients, and 90 mcg in 32 patients). Treatment continued as long as clinical benefit continued, and hematological responses were assessed every 3-6 months.
Treatment-related toxicities decreased over time, but five patients had treatment-limiting grade 3 or 4 toxicities after 60 months on therapy; overall 18 patients (22%) discontinued treatment due to toxicity.
The therapeutic approach to essential thrombocythemia and polycythemia vera has mainly focused on control of blood counts and reduction of the risk of thrombosis. Those at high risk for thrombosis generally undergo cytoreductive therapy with hydroxyurea. Recombinant interferon alfa is an alternative to hydroxyurea “given its biological, anti-proliferative, immunomodulating, and anticlonal effects,” the investigators explained.
“However, the widespread use of this biological drug has been limited by high rates of discontinuation due to side effects. Pegylated forms of interferon have a better pharmacological profile than short-acting interferons: they require less frequent injection, lower immunogenicity, and possibly fewer toxic effects,” they said.
Although pegylated interferon-alfa 2a has shown promise in several trials, most had short follow-up. The nearly 7 years of follow-up in the current trial is almost twice as long as in those prior studies.
During the current study, including follow-up, eight major vascular thromboembolic events occurred. One was associated with heart catheterization, one with elective chest surgery, and one with an angiogram. The remaining five occurred with no discernible cause after a median of 38 months of therapy for an incidence of 1.22 unprovoked vascular thromboembolic events per 100 person-years, and three of those were in patients with complete hematologic response. Two of the five patients were under age 60 years and had no history of thrombosis. Another patient had a serious unprovoked cerebrovascular hemorrhage after 3 years on therapy and while in complete hematological response.
In addition, 7 of the 83 patients in the study had disease progression on therapy; 6 progressed to myelofibrosis, and 1 developed acute myeloid leukemia. The median time to transformation in these patients was 40 months.
At the time of publication, 32 patient remained in the study and 24 were receiving treatment. Nineteen were in hematologic response at last follow-up, and most (75%) were on a dose of 90 mcg or less per week.
In addition to showing that some patients achieve durable responses on pegylated interferon alfa-2a, this study provided five important observations, the investigators said: 1) Patients might continue to derive clinical benefit from pegylated interferon alfa-2a even after losing response. 2) Only complete molecular remissions are durable, and some cases can be sustained after therapy discontinuation. 3) Clinical activity of pegylated interferon alfa-2a is not correlated with JAK2 mutation status. 4) Toxic effects unrelated to dose may develop and can be treatment-limiting, even after a long exposure to the drug. 5) Disease-related vascular complications or progression to myelofibrosis can still occur in patients on therapy.
“Our findings suggest that pegylated interferon alfa-2a is a viable treatment option, especially for young patients who want to avoid prolonged cytotoxic therapy. Lower doses minimize side effects while retaining efficacy,” they wrote, suggesting – based on these and other results – a starting dose of 45 mcg weekly to limit adverse events and maximize response.
They also noted that treated patients with a history of autoimmune disease and those with mood disorder should be monitored closely for side effects.
Future studies on pegylated interferon afla-2a alone or in combination with novel immunomodulatory drugs are needed to identify patients who would benefit most from treatment, and additional objective response criteria, such as measurement of spleen size, bone marrow histology, and quality of life should be used to better assess clinical benefit, they said.
The National Cancer Institute funded the study. The authors reported having no disclosures.
Pegylated interferon alfa-2a can induce durable hematologic and molecular responses in patients with advanced essential thrombocythemia and polycythemia vera, according to a post hoc analysis of data from a prospective, open-label, phase II trial.
Of 83 patients treated with pegylated interferon alfa-2a, 66 (80%) experienced hematological response, and of 55 of the 83 who were positive for the JAK2 Val617 mutation and who were evaluable for a molecular response, 35 (64%) experienced molecular response. The median response durations were 66 months and 53 months, respectively, wrote Lucia Masarova, MD, and her colleagues at MD Anderson Cancer Center, Houston.
Of the 66 hematological responders, 26 (39%) maintained some response during a median follow-up of 83 months. Among the 40 who lost their response, 19 had dose reductions or had the drug withheld because of intolerance or toxicity, 1 developed concurrent diffuse large B-cell lymphoma, and 20 progressed despite treatment with the highest tolerable dose of pegylated interferon alfa-2a. Of note, 7 (28%) of 25 patients who were treated for at least 46 months (median of 77 months) sustained their hematologic response for a median of 6 months after discontinuation of therapy, the investigators said (Lancet Haematol. 2017 Apr;4:e165-75).
Of the 35 molecular responders, 25 (71%) maintained some response during follow-up. Of the nine evaluable patients who did not maintain response (the 10th patient was taken off the study because of concurrent non-Hodgkin lymphoma) four lost response at a median of 2 years after the drug was withheld, and five lost response while on therapy. Three maintained their complete molecular remission – for 18, 55, and 79 months – after discontinuation of therapy.
“Only one patient who achieved a complete molecular remission has relapsed after stopping therapy for 16 months (complete molecular remission duration, 66 months). The other 9 of 10 patients had durable remissions (median duration 69 months),” the investigators wrote, noting that among the 20 patients with a partial molecular remission, 5 (25%) sustained best partial remission, 7 (28%) are in minor molecular remission, 8 (32%) lost their response, and 3 of 5 (60%) with minor molecular remission sustained that remission.
The study comprised adults over age 18 years who were diagnosed with essential thrombocythemia (40 patients) or polycythemia vera (43) and were enrolled during May 2005 to October 2009. Of the 83 patients, 52 (63%) had received some form of therapy prior to enrollment, including 14 who were treated with standard interferon alfa-2a and 1 who was treated with pegylated interferon alfa-2a. The initial starting dose of pegylated interferon alfa-2a used in the study was 450 mcg delivered subcutaneously once each week, but the dose was decreased in a stepwise manner to a final starting dose of 90 mcg per week due to toxicity; starting doses include 450 mcg in 3 patients, 360 mcg in 3 patients, 270 mcg in 19 patients, 180 mcg in 26 patients, and 90 mcg in 32 patients). Treatment continued as long as clinical benefit continued, and hematological responses were assessed every 3-6 months.
Treatment-related toxicities decreased over time, but five patients had treatment-limiting grade 3 or 4 toxicities after 60 months on therapy; overall 18 patients (22%) discontinued treatment due to toxicity.
The therapeutic approach to essential thrombocythemia and polycythemia vera has mainly focused on control of blood counts and reduction of the risk of thrombosis. Those at high risk for thrombosis generally undergo cytoreductive therapy with hydroxyurea. Recombinant interferon alfa is an alternative to hydroxyurea “given its biological, anti-proliferative, immunomodulating, and anticlonal effects,” the investigators explained.
“However, the widespread use of this biological drug has been limited by high rates of discontinuation due to side effects. Pegylated forms of interferon have a better pharmacological profile than short-acting interferons: they require less frequent injection, lower immunogenicity, and possibly fewer toxic effects,” they said.
Although pegylated interferon-alfa 2a has shown promise in several trials, most had short follow-up. The nearly 7 years of follow-up in the current trial is almost twice as long as in those prior studies.
During the current study, including follow-up, eight major vascular thromboembolic events occurred. One was associated with heart catheterization, one with elective chest surgery, and one with an angiogram. The remaining five occurred with no discernible cause after a median of 38 months of therapy for an incidence of 1.22 unprovoked vascular thromboembolic events per 100 person-years, and three of those were in patients with complete hematologic response. Two of the five patients were under age 60 years and had no history of thrombosis. Another patient had a serious unprovoked cerebrovascular hemorrhage after 3 years on therapy and while in complete hematological response.
In addition, 7 of the 83 patients in the study had disease progression on therapy; 6 progressed to myelofibrosis, and 1 developed acute myeloid leukemia. The median time to transformation in these patients was 40 months.
At the time of publication, 32 patient remained in the study and 24 were receiving treatment. Nineteen were in hematologic response at last follow-up, and most (75%) were on a dose of 90 mcg or less per week.
In addition to showing that some patients achieve durable responses on pegylated interferon alfa-2a, this study provided five important observations, the investigators said: 1) Patients might continue to derive clinical benefit from pegylated interferon alfa-2a even after losing response. 2) Only complete molecular remissions are durable, and some cases can be sustained after therapy discontinuation. 3) Clinical activity of pegylated interferon alfa-2a is not correlated with JAK2 mutation status. 4) Toxic effects unrelated to dose may develop and can be treatment-limiting, even after a long exposure to the drug. 5) Disease-related vascular complications or progression to myelofibrosis can still occur in patients on therapy.
“Our findings suggest that pegylated interferon alfa-2a is a viable treatment option, especially for young patients who want to avoid prolonged cytotoxic therapy. Lower doses minimize side effects while retaining efficacy,” they wrote, suggesting – based on these and other results – a starting dose of 45 mcg weekly to limit adverse events and maximize response.
They also noted that treated patients with a history of autoimmune disease and those with mood disorder should be monitored closely for side effects.
Future studies on pegylated interferon afla-2a alone or in combination with novel immunomodulatory drugs are needed to identify patients who would benefit most from treatment, and additional objective response criteria, such as measurement of spleen size, bone marrow histology, and quality of life should be used to better assess clinical benefit, they said.
The National Cancer Institute funded the study. The authors reported having no disclosures.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: Eighty percent of patients experienced hematological response and 64% experienced molecular response. The median response durations were 66 months and 53 months, respectively.
Data source: A post hoc analysis of data from an open-label, phase II study of 83 patients.
Disclosures: The National Cancer Institute funded the study. The authors reported having no disclosures.
Study correlates genetic mutations with AML subgroups
A large study of adults with acute myeloid leukemia (AML) correlates cancer-related genetic mutations with subtypes of AML defined by the presence of specific cytogenetic abnormalities.
Researchers combined the cytogenetic abnormalities that define each of 34 AML subgroups with the mutation status of 80 cancer-related genes to produce an “oncoprint,” a tabular summary of the mutations associated with each cytogenetic group.
This allowed the researchers to identify genetic differences among the 34 subgroups and unexpected associations between the AML subsets and specific genetic mutations as well as gene functional groups.
The researchers believe their findings, published in Leukemia, might help guide mutation testing and treatment decisions in the future.
The study involved 1603 newly diagnosed adult AML patients who were treated on Cancer and Leukemia Group B/Alliance for Clinical Trials in Oncology trials in multiple centers across the US. Most patients (n=1080) were under age 60.
The researchers classified the patients into 34 karyotype subgroups within 5 major cytogenetic groups—cytogenetically normal (CN) AML, complex karyotype (CK) AML, core-binding factor (CBF) AML, AML with balanced translocations or inversions other than those associated with CBF-AML, and AML with unbalanced chromosomal abnormalities detected in non-complex karyotypes.
The team sequenced pretreatment bone marrow or peripheral blood samples from each patient to learn the mutational status of 80 cancer- and leukemia-related genes.
The mutations were assigned to 1 of 9 categories based on the gene’s biological function—for example, methylation-related, cohesin complex, chromatin remodeling, and tumor-suppressor genes.
The researchers identified 4390 mutations, with a median of 3 mutations per patient.
Overall, the most frequently mutated genes that contributed to AML in this cohort belonged to the methylation group.
The researchers observed a high incidence of mutations in methylation-related genes in patients with CN-AML, CK-AML, or unbalanced chromosomal abnormalities.
In contrast, mutations in methylation-related genes were almost absent in CBF-AML patients and were rather rare in patients with non-CBF-AML-related balanced translocations or inversions.
Mutations in spliceosome genes were frequent in patients with unbalanced chromosomal abnormalities, especially those with sole trisomy of chromosomes 4, 8, 11, 13, or 21.
“Our study summarizes cytogenetic and mutational information of 1603 AML patients in a single image,” said Ann-Kathrin Eisfeld, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“The identification of key mutational features of each subgroup may help us to better understand the pathogenesis of the different AML types and provides a wealth of information for ongoing and future research.” ![]()
A large study of adults with acute myeloid leukemia (AML) correlates cancer-related genetic mutations with subtypes of AML defined by the presence of specific cytogenetic abnormalities.
Researchers combined the cytogenetic abnormalities that define each of 34 AML subgroups with the mutation status of 80 cancer-related genes to produce an “oncoprint,” a tabular summary of the mutations associated with each cytogenetic group.
This allowed the researchers to identify genetic differences among the 34 subgroups and unexpected associations between the AML subsets and specific genetic mutations as well as gene functional groups.
The researchers believe their findings, published in Leukemia, might help guide mutation testing and treatment decisions in the future.
The study involved 1603 newly diagnosed adult AML patients who were treated on Cancer and Leukemia Group B/Alliance for Clinical Trials in Oncology trials in multiple centers across the US. Most patients (n=1080) were under age 60.
The researchers classified the patients into 34 karyotype subgroups within 5 major cytogenetic groups—cytogenetically normal (CN) AML, complex karyotype (CK) AML, core-binding factor (CBF) AML, AML with balanced translocations or inversions other than those associated with CBF-AML, and AML with unbalanced chromosomal abnormalities detected in non-complex karyotypes.
The team sequenced pretreatment bone marrow or peripheral blood samples from each patient to learn the mutational status of 80 cancer- and leukemia-related genes.
The mutations were assigned to 1 of 9 categories based on the gene’s biological function—for example, methylation-related, cohesin complex, chromatin remodeling, and tumor-suppressor genes.
The researchers identified 4390 mutations, with a median of 3 mutations per patient.
Overall, the most frequently mutated genes that contributed to AML in this cohort belonged to the methylation group.
The researchers observed a high incidence of mutations in methylation-related genes in patients with CN-AML, CK-AML, or unbalanced chromosomal abnormalities.
In contrast, mutations in methylation-related genes were almost absent in CBF-AML patients and were rather rare in patients with non-CBF-AML-related balanced translocations or inversions.
Mutations in spliceosome genes were frequent in patients with unbalanced chromosomal abnormalities, especially those with sole trisomy of chromosomes 4, 8, 11, 13, or 21.
“Our study summarizes cytogenetic and mutational information of 1603 AML patients in a single image,” said Ann-Kathrin Eisfeld, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“The identification of key mutational features of each subgroup may help us to better understand the pathogenesis of the different AML types and provides a wealth of information for ongoing and future research.” ![]()
A large study of adults with acute myeloid leukemia (AML) correlates cancer-related genetic mutations with subtypes of AML defined by the presence of specific cytogenetic abnormalities.
Researchers combined the cytogenetic abnormalities that define each of 34 AML subgroups with the mutation status of 80 cancer-related genes to produce an “oncoprint,” a tabular summary of the mutations associated with each cytogenetic group.
This allowed the researchers to identify genetic differences among the 34 subgroups and unexpected associations between the AML subsets and specific genetic mutations as well as gene functional groups.
The researchers believe their findings, published in Leukemia, might help guide mutation testing and treatment decisions in the future.
The study involved 1603 newly diagnosed adult AML patients who were treated on Cancer and Leukemia Group B/Alliance for Clinical Trials in Oncology trials in multiple centers across the US. Most patients (n=1080) were under age 60.
The researchers classified the patients into 34 karyotype subgroups within 5 major cytogenetic groups—cytogenetically normal (CN) AML, complex karyotype (CK) AML, core-binding factor (CBF) AML, AML with balanced translocations or inversions other than those associated with CBF-AML, and AML with unbalanced chromosomal abnormalities detected in non-complex karyotypes.
The team sequenced pretreatment bone marrow or peripheral blood samples from each patient to learn the mutational status of 80 cancer- and leukemia-related genes.
The mutations were assigned to 1 of 9 categories based on the gene’s biological function—for example, methylation-related, cohesin complex, chromatin remodeling, and tumor-suppressor genes.
The researchers identified 4390 mutations, with a median of 3 mutations per patient.
Overall, the most frequently mutated genes that contributed to AML in this cohort belonged to the methylation group.
The researchers observed a high incidence of mutations in methylation-related genes in patients with CN-AML, CK-AML, or unbalanced chromosomal abnormalities.
In contrast, mutations in methylation-related genes were almost absent in CBF-AML patients and were rather rare in patients with non-CBF-AML-related balanced translocations or inversions.
Mutations in spliceosome genes were frequent in patients with unbalanced chromosomal abnormalities, especially those with sole trisomy of chromosomes 4, 8, 11, 13, or 21.
“Our study summarizes cytogenetic and mutational information of 1603 AML patients in a single image,” said Ann-Kathrin Eisfeld, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“The identification of key mutational features of each subgroup may help us to better understand the pathogenesis of the different AML types and provides a wealth of information for ongoing and future research.” ![]()
TKI shows promise in preclinical study of AML
WASHINGTON, DC—Preclinical data suggest a novel tyrosine kinase inhibitor (TKI) may be an effective treatment for patients with NTRK-rearranged acute myeloid leukemia (AML).
Entrectinib is a TKI targeting tumors that harbor TRK, ROS1, or ALK fusions.
Researchers found that entrectinib inhibited cell proliferation in NTRK-rearranged AML cell lines.
In mouse models of NTRK-rearranged AML, entrectinib induced tumor regression and eliminated residual AML cells from the bone marrow.
These results were presented at the AACR Annual Meeting 2017 (abstract 5158). The research was conducted by employees of Ignyta, Inc., the company developing entrectinib.
The researchers first tested entrectinib in AML cell lines. They observed “potent” anti-proliferative activity in a pair of NTRK-fusion-positive AML cell lines, IMS-M2 and M0-91.
Entrectinib inhibited TRK signaling and induced cell-cycle arrest in these cell lines. The TKI also induced both caspase 3-dependent apoptosis and PARP cleavage in a dose- and time-dependent manner.
However, entrectinib showed minimal activity against an NTRK-fusion-negative AML cell line, Kasumi-1.
The researchers also tested entrectinib in mouse models of NTRK-fusion-driven AML.
The TKI induced tumor regression in both IMS-M2 and M0-91 models, and the drug eliminated leukemic cells in the bone marrow.
The researchers said these results provide rationale for the clinical development of entrectinib in molecularly defined hematologic malignancies.
Entrectinib is currently being studied in a phase 2 trial of solid tumor malignancies. ![]()
WASHINGTON, DC—Preclinical data suggest a novel tyrosine kinase inhibitor (TKI) may be an effective treatment for patients with NTRK-rearranged acute myeloid leukemia (AML).
Entrectinib is a TKI targeting tumors that harbor TRK, ROS1, or ALK fusions.
Researchers found that entrectinib inhibited cell proliferation in NTRK-rearranged AML cell lines.
In mouse models of NTRK-rearranged AML, entrectinib induced tumor regression and eliminated residual AML cells from the bone marrow.
These results were presented at the AACR Annual Meeting 2017 (abstract 5158). The research was conducted by employees of Ignyta, Inc., the company developing entrectinib.
The researchers first tested entrectinib in AML cell lines. They observed “potent” anti-proliferative activity in a pair of NTRK-fusion-positive AML cell lines, IMS-M2 and M0-91.
Entrectinib inhibited TRK signaling and induced cell-cycle arrest in these cell lines. The TKI also induced both caspase 3-dependent apoptosis and PARP cleavage in a dose- and time-dependent manner.
However, entrectinib showed minimal activity against an NTRK-fusion-negative AML cell line, Kasumi-1.
The researchers also tested entrectinib in mouse models of NTRK-fusion-driven AML.
The TKI induced tumor regression in both IMS-M2 and M0-91 models, and the drug eliminated leukemic cells in the bone marrow.
The researchers said these results provide rationale for the clinical development of entrectinib in molecularly defined hematologic malignancies.
Entrectinib is currently being studied in a phase 2 trial of solid tumor malignancies. ![]()
WASHINGTON, DC—Preclinical data suggest a novel tyrosine kinase inhibitor (TKI) may be an effective treatment for patients with NTRK-rearranged acute myeloid leukemia (AML).
Entrectinib is a TKI targeting tumors that harbor TRK, ROS1, or ALK fusions.
Researchers found that entrectinib inhibited cell proliferation in NTRK-rearranged AML cell lines.
In mouse models of NTRK-rearranged AML, entrectinib induced tumor regression and eliminated residual AML cells from the bone marrow.
These results were presented at the AACR Annual Meeting 2017 (abstract 5158). The research was conducted by employees of Ignyta, Inc., the company developing entrectinib.
The researchers first tested entrectinib in AML cell lines. They observed “potent” anti-proliferative activity in a pair of NTRK-fusion-positive AML cell lines, IMS-M2 and M0-91.
Entrectinib inhibited TRK signaling and induced cell-cycle arrest in these cell lines. The TKI also induced both caspase 3-dependent apoptosis and PARP cleavage in a dose- and time-dependent manner.
However, entrectinib showed minimal activity against an NTRK-fusion-negative AML cell line, Kasumi-1.
The researchers also tested entrectinib in mouse models of NTRK-fusion-driven AML.
The TKI induced tumor regression in both IMS-M2 and M0-91 models, and the drug eliminated leukemic cells in the bone marrow.
The researchers said these results provide rationale for the clinical development of entrectinib in molecularly defined hematologic malignancies.
Entrectinib is currently being studied in a phase 2 trial of solid tumor malignancies. ![]()
Study reveals global inequalities in childhood leukemia survival
New research has revealed global inequalities in survival rates for pediatric patients with leukemia.
Investigators analyzed data on nearly 90,000 pediatric leukemia patients treated in 53 countries.
In most countries, patients with lymphoid leukemias or acute myeloid leukemia (AML) saw an increase in 5-year survival between 1995 and 2009.
However, there were wide variations in survival between the countries.
The investigators reported these findings in The Lancet Haematology.
They evaluated data from 89,828 leukemia patients (ages 0 to 14) included in 198 cancer registries in 53 countries.
The team estimated 5-year net survival for patients with AML or lymphoid leukemias (controlling for non-leukemia-related deaths) by calendar period of diagnosis—1995–1999, 2000–2004, and 2005–2009—in each country.
For children diagnosed with lymphoid leukemias between 1995 and 1999, 5-year survival rates ranged from 10.6% (in China) to 86.8% (in Austria). For children diagnosed between 2005 and 2009, the rates ranged from 52.4% (Colombia) to 91.6% (Germany).
For AML, 5-year survival rates ranged from 4.2% (China) to 72.2% (Sweden) in patients diagnosed between 1995 and 1999. For children diagnosed between 2005 and 2009, 5-year survival rates ranged from 33.3% (Bulgaria) to 78.2% (Germany).
The investigators noted that, in some countries, survival for both groups of leukemia patients was consistently high.
In Austria, for example, 5-year survival rates for lymphoid leukemias were 86.8% in 1995-1999 and 91.1% in 2005-2009. For AML, rates were 60.1% and 72.6%, respectively.
Other countries saw substantial increases in survival over time.
In China, the 5-year survival rate for patients with lymphoid leukemias increased from 10.6% in 1995-1999 to 69.2% in 2005-2009. For patients with AML, the rate increased from 4.2% to 41.1%.
“These findings show the extent of worldwide inequalities in access to optimal healthcare for children with cancer,” said study author Audrey Bonaventure, MD, PhD, of the London School of Hygiene & Tropical Medicine in the UK.
“Providing additional resources, alongside evidence-based initiatives such as international collaborations and treatment guidelines, could improve access to efficient treatment and care for all children with leukemia. This would contribute substantially to reducing worldwide inequalities in survival.” ![]()
New research has revealed global inequalities in survival rates for pediatric patients with leukemia.
Investigators analyzed data on nearly 90,000 pediatric leukemia patients treated in 53 countries.
In most countries, patients with lymphoid leukemias or acute myeloid leukemia (AML) saw an increase in 5-year survival between 1995 and 2009.
However, there were wide variations in survival between the countries.
The investigators reported these findings in The Lancet Haematology.
They evaluated data from 89,828 leukemia patients (ages 0 to 14) included in 198 cancer registries in 53 countries.
The team estimated 5-year net survival for patients with AML or lymphoid leukemias (controlling for non-leukemia-related deaths) by calendar period of diagnosis—1995–1999, 2000–2004, and 2005–2009—in each country.
For children diagnosed with lymphoid leukemias between 1995 and 1999, 5-year survival rates ranged from 10.6% (in China) to 86.8% (in Austria). For children diagnosed between 2005 and 2009, the rates ranged from 52.4% (Colombia) to 91.6% (Germany).
For AML, 5-year survival rates ranged from 4.2% (China) to 72.2% (Sweden) in patients diagnosed between 1995 and 1999. For children diagnosed between 2005 and 2009, 5-year survival rates ranged from 33.3% (Bulgaria) to 78.2% (Germany).
The investigators noted that, in some countries, survival for both groups of leukemia patients was consistently high.
In Austria, for example, 5-year survival rates for lymphoid leukemias were 86.8% in 1995-1999 and 91.1% in 2005-2009. For AML, rates were 60.1% and 72.6%, respectively.
Other countries saw substantial increases in survival over time.
In China, the 5-year survival rate for patients with lymphoid leukemias increased from 10.6% in 1995-1999 to 69.2% in 2005-2009. For patients with AML, the rate increased from 4.2% to 41.1%.
“These findings show the extent of worldwide inequalities in access to optimal healthcare for children with cancer,” said study author Audrey Bonaventure, MD, PhD, of the London School of Hygiene & Tropical Medicine in the UK.
“Providing additional resources, alongside evidence-based initiatives such as international collaborations and treatment guidelines, could improve access to efficient treatment and care for all children with leukemia. This would contribute substantially to reducing worldwide inequalities in survival.” ![]()
New research has revealed global inequalities in survival rates for pediatric patients with leukemia.
Investigators analyzed data on nearly 90,000 pediatric leukemia patients treated in 53 countries.
In most countries, patients with lymphoid leukemias or acute myeloid leukemia (AML) saw an increase in 5-year survival between 1995 and 2009.
However, there were wide variations in survival between the countries.
The investigators reported these findings in The Lancet Haematology.
They evaluated data from 89,828 leukemia patients (ages 0 to 14) included in 198 cancer registries in 53 countries.
The team estimated 5-year net survival for patients with AML or lymphoid leukemias (controlling for non-leukemia-related deaths) by calendar period of diagnosis—1995–1999, 2000–2004, and 2005–2009—in each country.
For children diagnosed with lymphoid leukemias between 1995 and 1999, 5-year survival rates ranged from 10.6% (in China) to 86.8% (in Austria). For children diagnosed between 2005 and 2009, the rates ranged from 52.4% (Colombia) to 91.6% (Germany).
For AML, 5-year survival rates ranged from 4.2% (China) to 72.2% (Sweden) in patients diagnosed between 1995 and 1999. For children diagnosed between 2005 and 2009, 5-year survival rates ranged from 33.3% (Bulgaria) to 78.2% (Germany).
The investigators noted that, in some countries, survival for both groups of leukemia patients was consistently high.
In Austria, for example, 5-year survival rates for lymphoid leukemias were 86.8% in 1995-1999 and 91.1% in 2005-2009. For AML, rates were 60.1% and 72.6%, respectively.
Other countries saw substantial increases in survival over time.
In China, the 5-year survival rate for patients with lymphoid leukemias increased from 10.6% in 1995-1999 to 69.2% in 2005-2009. For patients with AML, the rate increased from 4.2% to 41.1%.
“These findings show the extent of worldwide inequalities in access to optimal healthcare for children with cancer,” said study author Audrey Bonaventure, MD, PhD, of the London School of Hygiene & Tropical Medicine in the UK.
“Providing additional resources, alongside evidence-based initiatives such as international collaborations and treatment guidelines, could improve access to efficient treatment and care for all children with leukemia. This would contribute substantially to reducing worldwide inequalities in survival.” ![]()
Drug receives orphan designation for AML
The US Food and Drug Administration (FDA) has granted annamycin orphan designation for the treatment of acute myeloid leukemia (AML).
Annamycin is a liposomal anthracycline under development by Moleculin Biotech, Inc.
The company said it is working with the FDA on an investigative new drug application for a phase 1/2 trial of annamycin in patients with relapsed or refractory AML.
Annamycin has already been tested in 6 clinical trials, 3 of which focused on leukemia.
Results from one of these trials, in adults with relapsed/refractory acute lymphoblastic leukemia, were published in Clinical Lymphoma, Myeloma & Leukemia in 2013.
Annamycin has been under development by several other pharmaceutical companies. Moleculin Biotech, Inc. acquired rights and development assets relating to the drug in 2015.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted annamycin orphan designation for the treatment of acute myeloid leukemia (AML).
Annamycin is a liposomal anthracycline under development by Moleculin Biotech, Inc.
The company said it is working with the FDA on an investigative new drug application for a phase 1/2 trial of annamycin in patients with relapsed or refractory AML.
Annamycin has already been tested in 6 clinical trials, 3 of which focused on leukemia.
Results from one of these trials, in adults with relapsed/refractory acute lymphoblastic leukemia, were published in Clinical Lymphoma, Myeloma & Leukemia in 2013.
Annamycin has been under development by several other pharmaceutical companies. Moleculin Biotech, Inc. acquired rights and development assets relating to the drug in 2015.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted annamycin orphan designation for the treatment of acute myeloid leukemia (AML).
Annamycin is a liposomal anthracycline under development by Moleculin Biotech, Inc.
The company said it is working with the FDA on an investigative new drug application for a phase 1/2 trial of annamycin in patients with relapsed or refractory AML.
Annamycin has already been tested in 6 clinical trials, 3 of which focused on leukemia.
Results from one of these trials, in adults with relapsed/refractory acute lymphoblastic leukemia, were published in Clinical Lymphoma, Myeloma & Leukemia in 2013.
Annamycin has been under development by several other pharmaceutical companies. Moleculin Biotech, Inc. acquired rights and development assets relating to the drug in 2015.
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved. ![]()
Protein may prevent transformation from MDS to AML
The protein p300 may prevent the transformation from myelodysplastic syndromes (MDS) to acute myeloid leukemia (AML), according to research published in Leukemia.
Researchers found that loss of p300 “markedly” increased leukemogenesis in a mouse model of MDS.
“The loss of p300 allows these defective [MDS] cells to grow and become leukemic,” said study author Stephen Nimer, MD, of Sylvester Comprehensive Cancer Center in Miami, Florida.
“This work offers us a window into AML, which we are now going to try to exploit.”
Previous research suggested that p300 and CBP (both histone lysine acetyltransferases) may be tumor suppressors. The current study indicates that, in the context of MDS, that is only true for p300.
The researchers evaluated the effects of deleting both p300 and CBP in Nup98-HoxD13 (NHD13) transgenic mice, a model of human MDS.
The team found that p300 deletion, but not CBP deletion, accelerated leukemogenesis in the mice.
“When we eliminated p300, 100% of the mice developed leukemia,” Dr Nimer said. “It indicated that, under this specific circumstance, p300 is a tumor suppressor, offering great insight into how MDS converts to leukemia. It was quite surprising that CBP plays no role at all.”
The researchers also found that deleting p300 restored the ability of NHD13-expressing hematopoietic stem and progenitor cells (HSPCs) to self-renew, and p300 deletion decreased apoptosis.
“While investigating how p300 functions in MDS cells, we found that MDS cells do not grow well in the lab,” Dr Nimer said. “However, when you eliminate p300, suddenly, the cells continue to grow.”
On the other hand, deletion of p300 did not have a significant effect on wild-type hematopoiesis.
Finally, the researchers found that p300 deletion enhanced cytokine signaling in NHD13-expressing HSPCs. They observed enhanced activation of the MAPK and JAK/STAT pathways in HSPCs isolated from NHD13 transgenic mice.
The team said more research is needed to understand exactly how p300 controls MDS cells, but these findings could ultimately help MDS patients avoid AML.
“Other than chemotherapy, right now, there’s no way to prevent MDS from developing into myeloid leukemia,” Dr Nimer said. “However, drugs are being developed that can promote p300 function and possibly prevent MDS patients from developing leukemia.” ![]()
The protein p300 may prevent the transformation from myelodysplastic syndromes (MDS) to acute myeloid leukemia (AML), according to research published in Leukemia.
Researchers found that loss of p300 “markedly” increased leukemogenesis in a mouse model of MDS.
“The loss of p300 allows these defective [MDS] cells to grow and become leukemic,” said study author Stephen Nimer, MD, of Sylvester Comprehensive Cancer Center in Miami, Florida.
“This work offers us a window into AML, which we are now going to try to exploit.”
Previous research suggested that p300 and CBP (both histone lysine acetyltransferases) may be tumor suppressors. The current study indicates that, in the context of MDS, that is only true for p300.
The researchers evaluated the effects of deleting both p300 and CBP in Nup98-HoxD13 (NHD13) transgenic mice, a model of human MDS.
The team found that p300 deletion, but not CBP deletion, accelerated leukemogenesis in the mice.
“When we eliminated p300, 100% of the mice developed leukemia,” Dr Nimer said. “It indicated that, under this specific circumstance, p300 is a tumor suppressor, offering great insight into how MDS converts to leukemia. It was quite surprising that CBP plays no role at all.”
The researchers also found that deleting p300 restored the ability of NHD13-expressing hematopoietic stem and progenitor cells (HSPCs) to self-renew, and p300 deletion decreased apoptosis.
“While investigating how p300 functions in MDS cells, we found that MDS cells do not grow well in the lab,” Dr Nimer said. “However, when you eliminate p300, suddenly, the cells continue to grow.”
On the other hand, deletion of p300 did not have a significant effect on wild-type hematopoiesis.
Finally, the researchers found that p300 deletion enhanced cytokine signaling in NHD13-expressing HSPCs. They observed enhanced activation of the MAPK and JAK/STAT pathways in HSPCs isolated from NHD13 transgenic mice.
The team said more research is needed to understand exactly how p300 controls MDS cells, but these findings could ultimately help MDS patients avoid AML.
“Other than chemotherapy, right now, there’s no way to prevent MDS from developing into myeloid leukemia,” Dr Nimer said. “However, drugs are being developed that can promote p300 function and possibly prevent MDS patients from developing leukemia.” ![]()
The protein p300 may prevent the transformation from myelodysplastic syndromes (MDS) to acute myeloid leukemia (AML), according to research published in Leukemia.
Researchers found that loss of p300 “markedly” increased leukemogenesis in a mouse model of MDS.
“The loss of p300 allows these defective [MDS] cells to grow and become leukemic,” said study author Stephen Nimer, MD, of Sylvester Comprehensive Cancer Center in Miami, Florida.
“This work offers us a window into AML, which we are now going to try to exploit.”
Previous research suggested that p300 and CBP (both histone lysine acetyltransferases) may be tumor suppressors. The current study indicates that, in the context of MDS, that is only true for p300.
The researchers evaluated the effects of deleting both p300 and CBP in Nup98-HoxD13 (NHD13) transgenic mice, a model of human MDS.
The team found that p300 deletion, but not CBP deletion, accelerated leukemogenesis in the mice.
“When we eliminated p300, 100% of the mice developed leukemia,” Dr Nimer said. “It indicated that, under this specific circumstance, p300 is a tumor suppressor, offering great insight into how MDS converts to leukemia. It was quite surprising that CBP plays no role at all.”
The researchers also found that deleting p300 restored the ability of NHD13-expressing hematopoietic stem and progenitor cells (HSPCs) to self-renew, and p300 deletion decreased apoptosis.
“While investigating how p300 functions in MDS cells, we found that MDS cells do not grow well in the lab,” Dr Nimer said. “However, when you eliminate p300, suddenly, the cells continue to grow.”
On the other hand, deletion of p300 did not have a significant effect on wild-type hematopoiesis.
Finally, the researchers found that p300 deletion enhanced cytokine signaling in NHD13-expressing HSPCs. They observed enhanced activation of the MAPK and JAK/STAT pathways in HSPCs isolated from NHD13 transgenic mice.
The team said more research is needed to understand exactly how p300 controls MDS cells, but these findings could ultimately help MDS patients avoid AML.
“Other than chemotherapy, right now, there’s no way to prevent MDS from developing into myeloid leukemia,” Dr Nimer said. “However, drugs are being developed that can promote p300 function and possibly prevent MDS patients from developing leukemia.”