User login
FDA grants drug orphan designation for PNH
The US Food and Drug Administration (FDA) has granted orphan drug designation to RA101495 for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
RA101495 is a synthetic, macrocyclic peptide being developed by Ra Pharmaceuticals.
The peptide binds complement component 5 (C5) with sub-nanomolar affinity and allosterically inhibits its cleavage into C5a and C5b upon activation of the classical, alternative, or lectin pathways.
By binding to a region of C5 corresponding to C5b, RA101495 also disrupts the interaction between C5b and C6 and prevents assembly of the membrane attack complex.
In phase 1 studies, dosing of RA101495 was well tolerated in healthy volunteers and demonstrated sustained and near complete suppression of hemolysis and complement activity.
The phase 1 results were presented at the 21st Congress of the European Hematology Association in June 2016 (abstracts LB2249 and P632).
RA101495 is currently under investigation in a phase 2 trial of patients with PNH.
“There is an urgent need for new treatment options for patients suffering from PNH,” said Doug Treco, PhD, president and chief executive officer of Ra Pharmaceuticals.
“The current standard of care requires biweekly intravenous infusions, a dosing regimen that imposes a severe burden on patients, providers, and caregivers. We have designed RA101495 for once-daily, subcutaneous self-administration, an approach which has the potential to ease this burden, improve convenience, and provide much-needed dosing flexibility.”
“We are encouraged by our initial phase 2 data in PNH patients, which showed near-complete inhibition of hemolysis and a favorable safety and tolerability profile. We look forward to advancing our PNH program and providing additional data updates around year-end.”
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to RA101495 for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
RA101495 is a synthetic, macrocyclic peptide being developed by Ra Pharmaceuticals.
The peptide binds complement component 5 (C5) with sub-nanomolar affinity and allosterically inhibits its cleavage into C5a and C5b upon activation of the classical, alternative, or lectin pathways.
By binding to a region of C5 corresponding to C5b, RA101495 also disrupts the interaction between C5b and C6 and prevents assembly of the membrane attack complex.
In phase 1 studies, dosing of RA101495 was well tolerated in healthy volunteers and demonstrated sustained and near complete suppression of hemolysis and complement activity.
The phase 1 results were presented at the 21st Congress of the European Hematology Association in June 2016 (abstracts LB2249 and P632).
RA101495 is currently under investigation in a phase 2 trial of patients with PNH.
“There is an urgent need for new treatment options for patients suffering from PNH,” said Doug Treco, PhD, president and chief executive officer of Ra Pharmaceuticals.
“The current standard of care requires biweekly intravenous infusions, a dosing regimen that imposes a severe burden on patients, providers, and caregivers. We have designed RA101495 for once-daily, subcutaneous self-administration, an approach which has the potential to ease this burden, improve convenience, and provide much-needed dosing flexibility.”
“We are encouraged by our initial phase 2 data in PNH patients, which showed near-complete inhibition of hemolysis and a favorable safety and tolerability profile. We look forward to advancing our PNH program and providing additional data updates around year-end.”
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to RA101495 for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
RA101495 is a synthetic, macrocyclic peptide being developed by Ra Pharmaceuticals.
The peptide binds complement component 5 (C5) with sub-nanomolar affinity and allosterically inhibits its cleavage into C5a and C5b upon activation of the classical, alternative, or lectin pathways.
By binding to a region of C5 corresponding to C5b, RA101495 also disrupts the interaction between C5b and C6 and prevents assembly of the membrane attack complex.
In phase 1 studies, dosing of RA101495 was well tolerated in healthy volunteers and demonstrated sustained and near complete suppression of hemolysis and complement activity.
The phase 1 results were presented at the 21st Congress of the European Hematology Association in June 2016 (abstracts LB2249 and P632).
RA101495 is currently under investigation in a phase 2 trial of patients with PNH.
“There is an urgent need for new treatment options for patients suffering from PNH,” said Doug Treco, PhD, president and chief executive officer of Ra Pharmaceuticals.
“The current standard of care requires biweekly intravenous infusions, a dosing regimen that imposes a severe burden on patients, providers, and caregivers. We have designed RA101495 for once-daily, subcutaneous self-administration, an approach which has the potential to ease this burden, improve convenience, and provide much-needed dosing flexibility.”
“We are encouraged by our initial phase 2 data in PNH patients, which showed near-complete inhibition of hemolysis and a favorable safety and tolerability profile. We look forward to advancing our PNH program and providing additional data updates around year-end.”
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Clinical Endpoints in PTCL: The Road Less Traveled



Release Date: August 1, 2017
Expiration Date: July 31, 2018
Note: This activity is no longer available for credit.
Agenda
Developing New Strategic Goals in PTCL (duration 27:00)
Andrei R. Shustov, MD
University of Washington School of Medicine
Fred Hutchinson Cancer Research Center
Seattle, WA, USA
PTCL as a Rare Disease: A Case of Overall Survival (duration 19:00)
Owen A. O’Connor, MD, PhD
Columbia University Medical Center
The New York Presbyterian Hospital
New York, NY, USA
Why Might Response Rates Differ Between the East and West? (duration 17:00)
Kensei Tobinai, MD, PhD
National Cancer Center Hospital
Tokyo, Japan
Provided by:

Original activity supported by an educational grant from:
Spectrum Pharmaceuticals
Learning Objectives
At the end of the activity, participants should be able to:
- Explain why progression-free survival is important when treating patients with PTCL
- Determine when overall survival is possible
- Describe the challenges of using matched control analysis in PTCL clinical trials
- Discuss why different response rates to therapy for PTCL may be seen in Asian patients versus North American or European patients and define the possible contributing factors
Target Audience
Hematologists, oncologists, and other clinicians and scientists with an interest in T-cell lymphoma
Statement of Need
This activity explores clinical endpoints in PTCL, the importance of choosing the appropriate ones and the possibility of achieving them. Global and regional differences in PTCL are also explored as they relate to response rates. The presentations highlight the challenges physicians face in treating PTCL patients and recent developments are discussed to help practitioners evaluate the utility of these endpoints in choosing appropriate treatments to improve outcomes in their patients with PTCL.
FACULTY
Faculty
Andrei R. Shustov, MD
Disclosures: Consulting fee: Celgene; BMS
Owen O’Connor, MD, PhD
Disclosures: Consulting fees: Mundipharma; Celgene; Contracted Research: Mundipharma; Spectrum; Celgene; Seattle Genetics; TG Therapeutics; ADCT; Trillium
Kensei Tobinai, MD, PhD
Disclosures: Honoraria: Eisai; HUYA Bioscience International; Janssen; Mundipharma; Takeda; Zenyaku Kogyo; Contracted research: Abbvie; Celgene; Chugai Pharma; Eisai; GlaxoSmithKline; Janssen; Kyowa Hakko Kirin; Mundipharma; Ono Pharmaceutical; SERVIER; Takeda
Permissions
Andrei Shustov presentation
- Slide 7: PTCL Prognosis Is Indicative of Diverse Biology
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 8: PTCL: Global Epidemiology
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 9: PTCL: USA Epidemiology (top half)
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 9: PTCL: USA Epidemiology (bottom half)
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slide 10: PTCL Prognosis: Histology x Race (USA)
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slide 12: PTCL Prognosis: Clinical Features (top right side)
- Reprinted with permission. © 2013 American Society of Clinical Oncology. All rights reserved.
- Slide 14: PTCL Prognosis: Molecular Classifiers (left side)
- Republished with permission of the American Society of Hematology, from Parilla Castellar ER, et al. Blood 2014;124:1473-1480
- Slide 14: PTCL Prognosis: Molecular Classifiers (right side)
- Republished with permission of the American Society of Hematology, from Iqbal J, et al. Blood 2014;123:2915-2923
- Slide 17: US Epidemiology of PTCL
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slides 18-19: Romidepsin in Relapsed/Refractory PTCL
- Reprinted with permission. © 2012 American Society of Clinical Oncology. All rights reserved.
- Slides 20-22, 25: Romidepsin in Elderly Patients
- Shustov A, et al. Romidepsin is effective and well tolerated in older patients with peripheral T-cell lymphoma: analysis of two phase II trials. Leuk Lymphoma 2017 [Epub ahead of print]. Reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com
- Slides 27-28: Belinostat in Relapsed/Refractory PTCL
- Reprinted with permission. © 2015 American Society of Clinical Oncology. All rights reserved.
Kensei Tobinai presentation
- Slide 7: Overall Survival of ATL Pts in JCOG 9801
- Reprinted with permission. © 2007 American Society of Clinical Oncology. All rights reserved.
Disclaimer
The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Hemedicus, the supporter, or Frontline Medical Communications. This material is prepared based upon a review of multiple sources of information, but it is not exhaustive of the subject matter. Therefore, healthcare professionals and other individuals should review and consider other publications and materials on the subject matter before relying solely upon the information contained within this educational activity.



Release Date: August 1, 2017
Expiration Date: July 31, 2018
Note: This activity is no longer available for credit.
Agenda
Developing New Strategic Goals in PTCL (duration 27:00)
Andrei R. Shustov, MD
University of Washington School of Medicine
Fred Hutchinson Cancer Research Center
Seattle, WA, USA
PTCL as a Rare Disease: A Case of Overall Survival (duration 19:00)
Owen A. O’Connor, MD, PhD
Columbia University Medical Center
The New York Presbyterian Hospital
New York, NY, USA
Why Might Response Rates Differ Between the East and West? (duration 17:00)
Kensei Tobinai, MD, PhD
National Cancer Center Hospital
Tokyo, Japan
Provided by:

Original activity supported by an educational grant from:
Spectrum Pharmaceuticals
Learning Objectives
At the end of the activity, participants should be able to:
- Explain why progression-free survival is important when treating patients with PTCL
- Determine when overall survival is possible
- Describe the challenges of using matched control analysis in PTCL clinical trials
- Discuss why different response rates to therapy for PTCL may be seen in Asian patients versus North American or European patients and define the possible contributing factors
Target Audience
Hematologists, oncologists, and other clinicians and scientists with an interest in T-cell lymphoma
Statement of Need
This activity explores clinical endpoints in PTCL, the importance of choosing the appropriate ones and the possibility of achieving them. Global and regional differences in PTCL are also explored as they relate to response rates. The presentations highlight the challenges physicians face in treating PTCL patients and recent developments are discussed to help practitioners evaluate the utility of these endpoints in choosing appropriate treatments to improve outcomes in their patients with PTCL.
FACULTY
Faculty
Andrei R. Shustov, MD
Disclosures: Consulting fee: Celgene; BMS
Owen O’Connor, MD, PhD
Disclosures: Consulting fees: Mundipharma; Celgene; Contracted Research: Mundipharma; Spectrum; Celgene; Seattle Genetics; TG Therapeutics; ADCT; Trillium
Kensei Tobinai, MD, PhD
Disclosures: Honoraria: Eisai; HUYA Bioscience International; Janssen; Mundipharma; Takeda; Zenyaku Kogyo; Contracted research: Abbvie; Celgene; Chugai Pharma; Eisai; GlaxoSmithKline; Janssen; Kyowa Hakko Kirin; Mundipharma; Ono Pharmaceutical; SERVIER; Takeda
Permissions
Andrei Shustov presentation
- Slide 7: PTCL Prognosis Is Indicative of Diverse Biology
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 8: PTCL: Global Epidemiology
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 9: PTCL: USA Epidemiology (top half)
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 9: PTCL: USA Epidemiology (bottom half)
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slide 10: PTCL Prognosis: Histology x Race (USA)
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slide 12: PTCL Prognosis: Clinical Features (top right side)
- Reprinted with permission. © 2013 American Society of Clinical Oncology. All rights reserved.
- Slide 14: PTCL Prognosis: Molecular Classifiers (left side)
- Republished with permission of the American Society of Hematology, from Parilla Castellar ER, et al. Blood 2014;124:1473-1480
- Slide 14: PTCL Prognosis: Molecular Classifiers (right side)
- Republished with permission of the American Society of Hematology, from Iqbal J, et al. Blood 2014;123:2915-2923
- Slide 17: US Epidemiology of PTCL
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slides 18-19: Romidepsin in Relapsed/Refractory PTCL
- Reprinted with permission. © 2012 American Society of Clinical Oncology. All rights reserved.
- Slides 20-22, 25: Romidepsin in Elderly Patients
- Shustov A, et al. Romidepsin is effective and well tolerated in older patients with peripheral T-cell lymphoma: analysis of two phase II trials. Leuk Lymphoma 2017 [Epub ahead of print]. Reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com
- Slides 27-28: Belinostat in Relapsed/Refractory PTCL
- Reprinted with permission. © 2015 American Society of Clinical Oncology. All rights reserved.
Kensei Tobinai presentation
- Slide 7: Overall Survival of ATL Pts in JCOG 9801
- Reprinted with permission. © 2007 American Society of Clinical Oncology. All rights reserved.
Disclaimer
The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Hemedicus, the supporter, or Frontline Medical Communications. This material is prepared based upon a review of multiple sources of information, but it is not exhaustive of the subject matter. Therefore, healthcare professionals and other individuals should review and consider other publications and materials on the subject matter before relying solely upon the information contained within this educational activity.



Release Date: August 1, 2017
Expiration Date: July 31, 2018
Note: This activity is no longer available for credit.
Agenda
Developing New Strategic Goals in PTCL (duration 27:00)
Andrei R. Shustov, MD
University of Washington School of Medicine
Fred Hutchinson Cancer Research Center
Seattle, WA, USA
PTCL as a Rare Disease: A Case of Overall Survival (duration 19:00)
Owen A. O’Connor, MD, PhD
Columbia University Medical Center
The New York Presbyterian Hospital
New York, NY, USA
Why Might Response Rates Differ Between the East and West? (duration 17:00)
Kensei Tobinai, MD, PhD
National Cancer Center Hospital
Tokyo, Japan
Provided by:

Original activity supported by an educational grant from:
Spectrum Pharmaceuticals
Learning Objectives
At the end of the activity, participants should be able to:
- Explain why progression-free survival is important when treating patients with PTCL
- Determine when overall survival is possible
- Describe the challenges of using matched control analysis in PTCL clinical trials
- Discuss why different response rates to therapy for PTCL may be seen in Asian patients versus North American or European patients and define the possible contributing factors
Target Audience
Hematologists, oncologists, and other clinicians and scientists with an interest in T-cell lymphoma
Statement of Need
This activity explores clinical endpoints in PTCL, the importance of choosing the appropriate ones and the possibility of achieving them. Global and regional differences in PTCL are also explored as they relate to response rates. The presentations highlight the challenges physicians face in treating PTCL patients and recent developments are discussed to help practitioners evaluate the utility of these endpoints in choosing appropriate treatments to improve outcomes in their patients with PTCL.
FACULTY
Faculty
Andrei R. Shustov, MD
Disclosures: Consulting fee: Celgene; BMS
Owen O’Connor, MD, PhD
Disclosures: Consulting fees: Mundipharma; Celgene; Contracted Research: Mundipharma; Spectrum; Celgene; Seattle Genetics; TG Therapeutics; ADCT; Trillium
Kensei Tobinai, MD, PhD
Disclosures: Honoraria: Eisai; HUYA Bioscience International; Janssen; Mundipharma; Takeda; Zenyaku Kogyo; Contracted research: Abbvie; Celgene; Chugai Pharma; Eisai; GlaxoSmithKline; Janssen; Kyowa Hakko Kirin; Mundipharma; Ono Pharmaceutical; SERVIER; Takeda
Permissions
Andrei Shustov presentation
- Slide 7: PTCL Prognosis Is Indicative of Diverse Biology
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 8: PTCL: Global Epidemiology
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 9: PTCL: USA Epidemiology (top half)
- Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.
- Slide 9: PTCL: USA Epidemiology (bottom half)
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slide 10: PTCL Prognosis: Histology x Race (USA)
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slide 12: PTCL Prognosis: Clinical Features (top right side)
- Reprinted with permission. © 2013 American Society of Clinical Oncology. All rights reserved.
- Slide 14: PTCL Prognosis: Molecular Classifiers (left side)
- Republished with permission of the American Society of Hematology, from Parilla Castellar ER, et al. Blood 2014;124:1473-1480
- Slide 14: PTCL Prognosis: Molecular Classifiers (right side)
- Republished with permission of the American Society of Hematology, from Iqbal J, et al. Blood 2014;123:2915-2923
- Slide 17: US Epidemiology of PTCL
- Reprinted with permission. © 2016 American Society of Clinical Oncology. All rights reserved.
- Slides 18-19: Romidepsin in Relapsed/Refractory PTCL
- Reprinted with permission. © 2012 American Society of Clinical Oncology. All rights reserved.
- Slides 20-22, 25: Romidepsin in Elderly Patients
- Shustov A, et al. Romidepsin is effective and well tolerated in older patients with peripheral T-cell lymphoma: analysis of two phase II trials. Leuk Lymphoma 2017 [Epub ahead of print]. Reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com
- Slides 27-28: Belinostat in Relapsed/Refractory PTCL
- Reprinted with permission. © 2015 American Society of Clinical Oncology. All rights reserved.
Kensei Tobinai presentation
- Slide 7: Overall Survival of ATL Pts in JCOG 9801
- Reprinted with permission. © 2007 American Society of Clinical Oncology. All rights reserved.
Disclaimer
The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Hemedicus, the supporter, or Frontline Medical Communications. This material is prepared based upon a review of multiple sources of information, but it is not exhaustive of the subject matter. Therefore, healthcare professionals and other individuals should review and consider other publications and materials on the subject matter before relying solely upon the information contained within this educational activity.
Thalassemia case provides insight into history of malaria
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
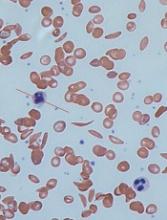
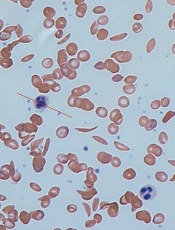
Models provide new understanding of sickle cell disease
Computer models have revealed new details of what happens inside a red blood cell affected by sickle cell disease (SCD), according to research published in Biophysical Journal.
In patients with SCD, mutated hemoglobin can polymerize, assembling into long fibers that push against the membranes of red blood cells and force them out of shape.
“The goal of our work is to model both how these sickle hemoglobin fibers form as well as the mechanical properties of those fibers,” said study author Lu Lu, a PhD student at Brown University in Providence, Rhode Island.
“There had been separate models for each of these things individually developed by us, but this brings those together into one comprehensive model.”
The model uses detailed biomechanical data on how sickle hemoglobin molecules behave and bind with each other to simulate the assembly of a polymer fiber.
Prior to this work, the problem had been that, as the fiber grows, so does the amount of data the model must crunch. Modeling an entire polymer fiber at a cellular scale using the details of each molecule was simply too computationally expensive.
“Even the world’s fastest supercomputers wouldn’t be able to handle it,” said study author George Karniadakis, PhD, of Brown University.
“There’s just too much happening and no way to capture it all computationally. That’s what we were able to overcome with this work.”
The researchers’ solution was to apply what they call a mesoscopic adaptive resolution scheme (MARS).
The MARS model calculates the detailed dynamics of each individual hemoglobin molecule only at the end of polymer fibers, where new molecules are being recruited into the fiber.
Once 4 layers of a fiber have been established, the model automatically dials back the resolution at which it represents that section. The model retains the important information about how the fiber behaves mechanically but glosses over the fine details of each constituent molecule.
“By eliminating the fine details where we don’t need them, we develop a model that can simulate this whole process and its effects on a red blood cell,” Dr Karniadakis said.
Using the new MARS simulations, the researchers were able to show how different configurations of growing polymer fibers are able to produce cells with different shapes.
“We are able to produce a polymerization profile for each of the cell types associated with the disease,” Dr Karniadakis said. “Now, the goal is to use these models to look for ways of preventing the disease onset.”
Using these new models, Dr Karniadakis and his colleagues can run simulations that include fetal hemoglobin. Those simulations could be used to confirm the theory that fetal hemoglobin disrupts polymerization, as well as determine how much fetal hemoglobin is necessary.
That could help in establishing better dosage guidelines for hydroxyurea or in developing new and more effective drugs for SCD, according to the researchers.
“The models give us a way to do preliminary testing on new approaches to stopping this disease,” Dr Karniadakis said. “Now that we can simulate the entire polymerization process, we think the models will be much more useful.” ![]()
Computer models have revealed new details of what happens inside a red blood cell affected by sickle cell disease (SCD), according to research published in Biophysical Journal.
In patients with SCD, mutated hemoglobin can polymerize, assembling into long fibers that push against the membranes of red blood cells and force them out of shape.
“The goal of our work is to model both how these sickle hemoglobin fibers form as well as the mechanical properties of those fibers,” said study author Lu Lu, a PhD student at Brown University in Providence, Rhode Island.
“There had been separate models for each of these things individually developed by us, but this brings those together into one comprehensive model.”
The model uses detailed biomechanical data on how sickle hemoglobin molecules behave and bind with each other to simulate the assembly of a polymer fiber.
Prior to this work, the problem had been that, as the fiber grows, so does the amount of data the model must crunch. Modeling an entire polymer fiber at a cellular scale using the details of each molecule was simply too computationally expensive.
“Even the world’s fastest supercomputers wouldn’t be able to handle it,” said study author George Karniadakis, PhD, of Brown University.
“There’s just too much happening and no way to capture it all computationally. That’s what we were able to overcome with this work.”
The researchers’ solution was to apply what they call a mesoscopic adaptive resolution scheme (MARS).
The MARS model calculates the detailed dynamics of each individual hemoglobin molecule only at the end of polymer fibers, where new molecules are being recruited into the fiber.
Once 4 layers of a fiber have been established, the model automatically dials back the resolution at which it represents that section. The model retains the important information about how the fiber behaves mechanically but glosses over the fine details of each constituent molecule.
“By eliminating the fine details where we don’t need them, we develop a model that can simulate this whole process and its effects on a red blood cell,” Dr Karniadakis said.
Using the new MARS simulations, the researchers were able to show how different configurations of growing polymer fibers are able to produce cells with different shapes.
“We are able to produce a polymerization profile for each of the cell types associated with the disease,” Dr Karniadakis said. “Now, the goal is to use these models to look for ways of preventing the disease onset.”
Using these new models, Dr Karniadakis and his colleagues can run simulations that include fetal hemoglobin. Those simulations could be used to confirm the theory that fetal hemoglobin disrupts polymerization, as well as determine how much fetal hemoglobin is necessary.
That could help in establishing better dosage guidelines for hydroxyurea or in developing new and more effective drugs for SCD, according to the researchers.
“The models give us a way to do preliminary testing on new approaches to stopping this disease,” Dr Karniadakis said. “Now that we can simulate the entire polymerization process, we think the models will be much more useful.” ![]()
Computer models have revealed new details of what happens inside a red blood cell affected by sickle cell disease (SCD), according to research published in Biophysical Journal.
In patients with SCD, mutated hemoglobin can polymerize, assembling into long fibers that push against the membranes of red blood cells and force them out of shape.
“The goal of our work is to model both how these sickle hemoglobin fibers form as well as the mechanical properties of those fibers,” said study author Lu Lu, a PhD student at Brown University in Providence, Rhode Island.
“There had been separate models for each of these things individually developed by us, but this brings those together into one comprehensive model.”
The model uses detailed biomechanical data on how sickle hemoglobin molecules behave and bind with each other to simulate the assembly of a polymer fiber.
Prior to this work, the problem had been that, as the fiber grows, so does the amount of data the model must crunch. Modeling an entire polymer fiber at a cellular scale using the details of each molecule was simply too computationally expensive.
“Even the world’s fastest supercomputers wouldn’t be able to handle it,” said study author George Karniadakis, PhD, of Brown University.
“There’s just too much happening and no way to capture it all computationally. That’s what we were able to overcome with this work.”
The researchers’ solution was to apply what they call a mesoscopic adaptive resolution scheme (MARS).
The MARS model calculates the detailed dynamics of each individual hemoglobin molecule only at the end of polymer fibers, where new molecules are being recruited into the fiber.
Once 4 layers of a fiber have been established, the model automatically dials back the resolution at which it represents that section. The model retains the important information about how the fiber behaves mechanically but glosses over the fine details of each constituent molecule.
“By eliminating the fine details where we don’t need them, we develop a model that can simulate this whole process and its effects on a red blood cell,” Dr Karniadakis said.
Using the new MARS simulations, the researchers were able to show how different configurations of growing polymer fibers are able to produce cells with different shapes.
“We are able to produce a polymerization profile for each of the cell types associated with the disease,” Dr Karniadakis said. “Now, the goal is to use these models to look for ways of preventing the disease onset.”
Using these new models, Dr Karniadakis and his colleagues can run simulations that include fetal hemoglobin. Those simulations could be used to confirm the theory that fetal hemoglobin disrupts polymerization, as well as determine how much fetal hemoglobin is necessary.
That could help in establishing better dosage guidelines for hydroxyurea or in developing new and more effective drugs for SCD, according to the researchers.
“The models give us a way to do preliminary testing on new approaches to stopping this disease,” Dr Karniadakis said. “Now that we can simulate the entire polymerization process, we think the models will be much more useful.” ![]()
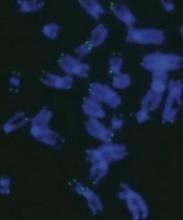
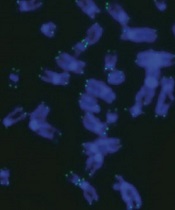
CRISPR sheds light on dyskeratosis congenita
Gene editing has revealed how dyskeratosis congenita (DC) impairs the formation of blood cells, according to research published in Stem Cell Reports.
The discovery has opened up new lines of investigation into how to treat DC, which is characterized by shortened telomeres.
“Lengthening telomeres seems like a logical way to help these patients, but it could possibly come with its own set of problems,” said study author Luis F.Z. Batista, PhD, of the Washington University School of Medicine in St. Louis, Missouri.
“We would worry about encouraging cancer formation, for example, as high levels of the protein that lengthens telomeres—telomerase—are commonly found with cancer. But if we could find a way to block the signaling pathways that short telomeres activate—that specifically lead to the problems in blood cell formation—it could allow these patients to continue making blood cells.”
With this in mind, Dr Batista and his colleagues used CRISPR to edit into human embryonic stem cells a pair of mutations associated with DC— DKC1_A353V and TERT_P704S. These cells reproduced the telomere-shortening defect seen in patients with DC.
With this model, the researchers showed how the telomere defect leads to the gradual loss of blood cell formation and how blocking the downstream effects of the defect can reverse this loss, leading to normal production of blood cells.
Blocking this signaling pathway did not lengthen telomeres or stop their shortening, but it allowed the manufacturing of different types of blood cells to continue.
The researchers also made a discovery that provides a distinction regarding the detrimental effect of short telomeres during early development. The team found the defect did not hinder primitive hematopoiesis, but it did impair definitive hematopoiesis.
“This was tremendously interesting from a developmental biology perspective as well as from a disease modeling perspective,” said study author Christopher M. Sturgeon, PhD, of the Washington University School of Medicine. “We now have a platform to really dig deeper into understanding the mechanisms behind some forms of bone marrow failure.”
The researchers implicated high levels of the protein p53 as one of the signals that leads to the drop in definitive hematopoiesis.
“P53 is thought of as a guardian of the genome,” Dr Batista noted. “Mutations that disable p53 are associated with different types of cancer. Because of this, we would not consider directly trying to block p53 in these patients.”
“But what this study provides is proof-of-concept that this pathway is involved in this response. So we now are looking for ways to block the pathway further downstream without necessarily blocking p53 directly.”
Drs Batista and Sturgeon recently received a grant from the Department of Defense to investigate the pathway. The pair believes the strategy used in this study could be relevant for other bone marrow failure syndromes as well, such as Fanconi anemia and aplastic anemia. ![]()
Gene editing has revealed how dyskeratosis congenita (DC) impairs the formation of blood cells, according to research published in Stem Cell Reports.
The discovery has opened up new lines of investigation into how to treat DC, which is characterized by shortened telomeres.
“Lengthening telomeres seems like a logical way to help these patients, but it could possibly come with its own set of problems,” said study author Luis F.Z. Batista, PhD, of the Washington University School of Medicine in St. Louis, Missouri.
“We would worry about encouraging cancer formation, for example, as high levels of the protein that lengthens telomeres—telomerase—are commonly found with cancer. But if we could find a way to block the signaling pathways that short telomeres activate—that specifically lead to the problems in blood cell formation—it could allow these patients to continue making blood cells.”
With this in mind, Dr Batista and his colleagues used CRISPR to edit into human embryonic stem cells a pair of mutations associated with DC— DKC1_A353V and TERT_P704S. These cells reproduced the telomere-shortening defect seen in patients with DC.
With this model, the researchers showed how the telomere defect leads to the gradual loss of blood cell formation and how blocking the downstream effects of the defect can reverse this loss, leading to normal production of blood cells.
Blocking this signaling pathway did not lengthen telomeres or stop their shortening, but it allowed the manufacturing of different types of blood cells to continue.
The researchers also made a discovery that provides a distinction regarding the detrimental effect of short telomeres during early development. The team found the defect did not hinder primitive hematopoiesis, but it did impair definitive hematopoiesis.
“This was tremendously interesting from a developmental biology perspective as well as from a disease modeling perspective,” said study author Christopher M. Sturgeon, PhD, of the Washington University School of Medicine. “We now have a platform to really dig deeper into understanding the mechanisms behind some forms of bone marrow failure.”
The researchers implicated high levels of the protein p53 as one of the signals that leads to the drop in definitive hematopoiesis.
“P53 is thought of as a guardian of the genome,” Dr Batista noted. “Mutations that disable p53 are associated with different types of cancer. Because of this, we would not consider directly trying to block p53 in these patients.”
“But what this study provides is proof-of-concept that this pathway is involved in this response. So we now are looking for ways to block the pathway further downstream without necessarily blocking p53 directly.”
Drs Batista and Sturgeon recently received a grant from the Department of Defense to investigate the pathway. The pair believes the strategy used in this study could be relevant for other bone marrow failure syndromes as well, such as Fanconi anemia and aplastic anemia. ![]()
Gene editing has revealed how dyskeratosis congenita (DC) impairs the formation of blood cells, according to research published in Stem Cell Reports.
The discovery has opened up new lines of investigation into how to treat DC, which is characterized by shortened telomeres.
“Lengthening telomeres seems like a logical way to help these patients, but it could possibly come with its own set of problems,” said study author Luis F.Z. Batista, PhD, of the Washington University School of Medicine in St. Louis, Missouri.
“We would worry about encouraging cancer formation, for example, as high levels of the protein that lengthens telomeres—telomerase—are commonly found with cancer. But if we could find a way to block the signaling pathways that short telomeres activate—that specifically lead to the problems in blood cell formation—it could allow these patients to continue making blood cells.”
With this in mind, Dr Batista and his colleagues used CRISPR to edit into human embryonic stem cells a pair of mutations associated with DC— DKC1_A353V and TERT_P704S. These cells reproduced the telomere-shortening defect seen in patients with DC.
With this model, the researchers showed how the telomere defect leads to the gradual loss of blood cell formation and how blocking the downstream effects of the defect can reverse this loss, leading to normal production of blood cells.
Blocking this signaling pathway did not lengthen telomeres or stop their shortening, but it allowed the manufacturing of different types of blood cells to continue.
The researchers also made a discovery that provides a distinction regarding the detrimental effect of short telomeres during early development. The team found the defect did not hinder primitive hematopoiesis, but it did impair definitive hematopoiesis.
“This was tremendously interesting from a developmental biology perspective as well as from a disease modeling perspective,” said study author Christopher M. Sturgeon, PhD, of the Washington University School of Medicine. “We now have a platform to really dig deeper into understanding the mechanisms behind some forms of bone marrow failure.”
The researchers implicated high levels of the protein p53 as one of the signals that leads to the drop in definitive hematopoiesis.
“P53 is thought of as a guardian of the genome,” Dr Batista noted. “Mutations that disable p53 are associated with different types of cancer. Because of this, we would not consider directly trying to block p53 in these patients.”
“But what this study provides is proof-of-concept that this pathway is involved in this response. So we now are looking for ways to block the pathway further downstream without necessarily blocking p53 directly.”
Drs Batista and Sturgeon recently received a grant from the Department of Defense to investigate the pathway. The pair believes the strategy used in this study could be relevant for other bone marrow failure syndromes as well, such as Fanconi anemia and aplastic anemia. ![]()
Product granted fast track designation for aTTP
The US Food and Drug Administration (FDA) has granted fast track designation to caplacizumab, an anti-von Willebrand factor (vWF) nanobody being developed for the treatment of acquired thrombotic thrombocytopenic purpura (aTTP).
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the new drug application or biologics license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
About caplacizumab
Caplacizumab is a bivalent anti-vWF nanobody being developed by Ablynx. Caplacizumab works by blocking the interaction of ultra-large vWF multimers with platelets, having an immediate effect on platelet aggregation and the ensuing formation and accumulation of the micro-clots that cause the severe thrombocytopenia, tissue ischemia, and organ dysfunction that occurs in patients with aTTP.
Researchers evaluated the efficacy and safety of caplacizumab, given with standard care for aTTP, in the phase 2 TITAN trial.
The trial enrolled 75 patients with aTTP. They all received the standard of care—daily plasma exchange and immunosuppressive therapy. Thirty-six patients were randomized to receive caplacizumab as well, and 39 were randomized to placebo.
The study’s primary endpoint was time to response (platelet count normalization). Patients in the caplacizumab arm had a 39% reduction in the median time to response compared to patients in the placebo arm (P=0.005).
The rate of confirmed response was 86.1% (n=31) in the caplacizumab arm and 71.8% (n=28) in the placebo arm.
There were more relapses in the caplacizumab arm than the placebo arm—8 (22.2%) and 0, respectively. Relapse was defined as a TTP event occurring more than 30 days after the end of daily plasma exchange.
There were fewer exacerbations in the caplacizumab arm than the placebo arm—3 (8.3%) and 11 (28.2%), respectively. Exacerbation was defined as recurrent thrombocytopenia within 30 days of the end of daily plasma exchange that required re-initiation of daily exchange.
The rate of adverse events thought to be related to the study drug was 17% in the caplacizumab arm and 11% in the placebo arm. The rate of events that were possibly related was 54% and 8%, respectively.
A lower proportion of subjects in the caplacizumab arm experienced one or more major thromboembolic events or died, compared to the placebo arm—11.4% and 43.2%, respectively.
In addition, fewer caplacizumab-treated patients were refractory to treatment—5.7% vs 21.6%.
There were 2 deaths in the placebo arm, and both of those patients were refractory to treatment. There were no deaths reported in the caplacizumab arm.
Now, researchers are evaluating caplacizumab in the phase 3 HERCULES trial (NCT02553317). Results from this study are anticipated in the second half of 2017 are expected to support a planned biologics license application filing in the US in 2018. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to caplacizumab, an anti-von Willebrand factor (vWF) nanobody being developed for the treatment of acquired thrombotic thrombocytopenic purpura (aTTP).
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the new drug application or biologics license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
About caplacizumab
Caplacizumab is a bivalent anti-vWF nanobody being developed by Ablynx. Caplacizumab works by blocking the interaction of ultra-large vWF multimers with platelets, having an immediate effect on platelet aggregation and the ensuing formation and accumulation of the micro-clots that cause the severe thrombocytopenia, tissue ischemia, and organ dysfunction that occurs in patients with aTTP.
Researchers evaluated the efficacy and safety of caplacizumab, given with standard care for aTTP, in the phase 2 TITAN trial.
The trial enrolled 75 patients with aTTP. They all received the standard of care—daily plasma exchange and immunosuppressive therapy. Thirty-six patients were randomized to receive caplacizumab as well, and 39 were randomized to placebo.
The study’s primary endpoint was time to response (platelet count normalization). Patients in the caplacizumab arm had a 39% reduction in the median time to response compared to patients in the placebo arm (P=0.005).
The rate of confirmed response was 86.1% (n=31) in the caplacizumab arm and 71.8% (n=28) in the placebo arm.
There were more relapses in the caplacizumab arm than the placebo arm—8 (22.2%) and 0, respectively. Relapse was defined as a TTP event occurring more than 30 days after the end of daily plasma exchange.
There were fewer exacerbations in the caplacizumab arm than the placebo arm—3 (8.3%) and 11 (28.2%), respectively. Exacerbation was defined as recurrent thrombocytopenia within 30 days of the end of daily plasma exchange that required re-initiation of daily exchange.
The rate of adverse events thought to be related to the study drug was 17% in the caplacizumab arm and 11% in the placebo arm. The rate of events that were possibly related was 54% and 8%, respectively.
A lower proportion of subjects in the caplacizumab arm experienced one or more major thromboembolic events or died, compared to the placebo arm—11.4% and 43.2%, respectively.
In addition, fewer caplacizumab-treated patients were refractory to treatment—5.7% vs 21.6%.
There were 2 deaths in the placebo arm, and both of those patients were refractory to treatment. There were no deaths reported in the caplacizumab arm.
Now, researchers are evaluating caplacizumab in the phase 3 HERCULES trial (NCT02553317). Results from this study are anticipated in the second half of 2017 are expected to support a planned biologics license application filing in the US in 2018. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to caplacizumab, an anti-von Willebrand factor (vWF) nanobody being developed for the treatment of acquired thrombotic thrombocytopenic purpura (aTTP).
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the new drug application or biologics license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
About caplacizumab
Caplacizumab is a bivalent anti-vWF nanobody being developed by Ablynx. Caplacizumab works by blocking the interaction of ultra-large vWF multimers with platelets, having an immediate effect on platelet aggregation and the ensuing formation and accumulation of the micro-clots that cause the severe thrombocytopenia, tissue ischemia, and organ dysfunction that occurs in patients with aTTP.
Researchers evaluated the efficacy and safety of caplacizumab, given with standard care for aTTP, in the phase 2 TITAN trial.
The trial enrolled 75 patients with aTTP. They all received the standard of care—daily plasma exchange and immunosuppressive therapy. Thirty-six patients were randomized to receive caplacizumab as well, and 39 were randomized to placebo.
The study’s primary endpoint was time to response (platelet count normalization). Patients in the caplacizumab arm had a 39% reduction in the median time to response compared to patients in the placebo arm (P=0.005).
The rate of confirmed response was 86.1% (n=31) in the caplacizumab arm and 71.8% (n=28) in the placebo arm.
There were more relapses in the caplacizumab arm than the placebo arm—8 (22.2%) and 0, respectively. Relapse was defined as a TTP event occurring more than 30 days after the end of daily plasma exchange.
There were fewer exacerbations in the caplacizumab arm than the placebo arm—3 (8.3%) and 11 (28.2%), respectively. Exacerbation was defined as recurrent thrombocytopenia within 30 days of the end of daily plasma exchange that required re-initiation of daily exchange.
The rate of adverse events thought to be related to the study drug was 17% in the caplacizumab arm and 11% in the placebo arm. The rate of events that were possibly related was 54% and 8%, respectively.
A lower proportion of subjects in the caplacizumab arm experienced one or more major thromboembolic events or died, compared to the placebo arm—11.4% and 43.2%, respectively.
In addition, fewer caplacizumab-treated patients were refractory to treatment—5.7% vs 21.6%.
There were 2 deaths in the placebo arm, and both of those patients were refractory to treatment. There were no deaths reported in the caplacizumab arm.
Now, researchers are evaluating caplacizumab in the phase 3 HERCULES trial (NCT02553317). Results from this study are anticipated in the second half of 2017 are expected to support a planned biologics license application filing in the US in 2018. ![]()
Predicting response to treatment in AML, MDS
Researchers say they have determined which patients will respond to treatment with SY-1425, a retinoic acid receptor alpha (RARα) agonist.
The team discovered a subset of patients with acute myeloid leukemia (AML) who had a super-enhancer associated with the RARA gene, which is predictive of response to SY-1425.
The researchers also identified a subset of patients with myelodysplastic syndromes (MDS) who had high expression of the RARA gene.
And experiments showed that RARA-high MDS had a similar response to SY-1425 as that seen in AML driven by the RARA super-enhancer.
Ravindra Majeti MD, PhD, of Stanford University School of Medicine in California, and colleagues reported these findings in Cancer Discovery. Employees of Syros Pharmaceuticals, the company developing SY-1425, were also involved in this research.
In collaboration with the Majeti lab, Syros used its gene control platform to analyze 66 AML patients’ tumor samples. In this way, the researchers identified 6 distinct patient subsets based on super-enhancer profiles, including 1 enriched for a super-enhancer associated with the RARA gene.
The team found that super-enhancer profiles were strongly associated with survival outcomes, often independent of known genetic mutations in AML.
The RARA super-enhancer was associated with high expression of the RARA gene, which codes for a transcription factor targeted by SY-1425.
The RARA super-enhancer was predictive of response to SY-1425. In AML cells with high RARA expression, SY-1425 reduced proliferation and promoted differentiation.
Moreover, SY-1425 decreased tumor burden and prolonged survival in patient-derived xenograft models of AML with high RARA expression. However, there was no effect on AML cells or models with low RARA expression.
The researchers said SY-1425 induced profound transcriptional changes promoting cell differentiation in AML cells with high RARA expression, but the drug produced little to no transcriptional changes in AML cells with low RARA expression.
DHRS3 was the most strongly and rapidly induced gene in response to treatment with SY-1425. This led to the identification of DHRS3 induction as an early indicator of whether SY-1425 is affecting the targeted biology in defined subsets of AML and MDS patients. It is therefore used as a pharmacodynamic marker in the ongoing phase 2 trial of SY-1425.
In this trial, researchers are assessing the safety and efficacy of SY-1425 as a single agent in 4 AML and MDS patient populations, as well as testing SY-1425 in combination with azacitidine in newly diagnosed AML patients who are not suitable candidates for standard chemotherapy. ![]()
Researchers say they have determined which patients will respond to treatment with SY-1425, a retinoic acid receptor alpha (RARα) agonist.
The team discovered a subset of patients with acute myeloid leukemia (AML) who had a super-enhancer associated with the RARA gene, which is predictive of response to SY-1425.
The researchers also identified a subset of patients with myelodysplastic syndromes (MDS) who had high expression of the RARA gene.
And experiments showed that RARA-high MDS had a similar response to SY-1425 as that seen in AML driven by the RARA super-enhancer.
Ravindra Majeti MD, PhD, of Stanford University School of Medicine in California, and colleagues reported these findings in Cancer Discovery. Employees of Syros Pharmaceuticals, the company developing SY-1425, were also involved in this research.
In collaboration with the Majeti lab, Syros used its gene control platform to analyze 66 AML patients’ tumor samples. In this way, the researchers identified 6 distinct patient subsets based on super-enhancer profiles, including 1 enriched for a super-enhancer associated with the RARA gene.
The team found that super-enhancer profiles were strongly associated with survival outcomes, often independent of known genetic mutations in AML.
The RARA super-enhancer was associated with high expression of the RARA gene, which codes for a transcription factor targeted by SY-1425.
The RARA super-enhancer was predictive of response to SY-1425. In AML cells with high RARA expression, SY-1425 reduced proliferation and promoted differentiation.
Moreover, SY-1425 decreased tumor burden and prolonged survival in patient-derived xenograft models of AML with high RARA expression. However, there was no effect on AML cells or models with low RARA expression.
The researchers said SY-1425 induced profound transcriptional changes promoting cell differentiation in AML cells with high RARA expression, but the drug produced little to no transcriptional changes in AML cells with low RARA expression.
DHRS3 was the most strongly and rapidly induced gene in response to treatment with SY-1425. This led to the identification of DHRS3 induction as an early indicator of whether SY-1425 is affecting the targeted biology in defined subsets of AML and MDS patients. It is therefore used as a pharmacodynamic marker in the ongoing phase 2 trial of SY-1425.
In this trial, researchers are assessing the safety and efficacy of SY-1425 as a single agent in 4 AML and MDS patient populations, as well as testing SY-1425 in combination with azacitidine in newly diagnosed AML patients who are not suitable candidates for standard chemotherapy. ![]()
Researchers say they have determined which patients will respond to treatment with SY-1425, a retinoic acid receptor alpha (RARα) agonist.
The team discovered a subset of patients with acute myeloid leukemia (AML) who had a super-enhancer associated with the RARA gene, which is predictive of response to SY-1425.
The researchers also identified a subset of patients with myelodysplastic syndromes (MDS) who had high expression of the RARA gene.
And experiments showed that RARA-high MDS had a similar response to SY-1425 as that seen in AML driven by the RARA super-enhancer.
Ravindra Majeti MD, PhD, of Stanford University School of Medicine in California, and colleagues reported these findings in Cancer Discovery. Employees of Syros Pharmaceuticals, the company developing SY-1425, were also involved in this research.
In collaboration with the Majeti lab, Syros used its gene control platform to analyze 66 AML patients’ tumor samples. In this way, the researchers identified 6 distinct patient subsets based on super-enhancer profiles, including 1 enriched for a super-enhancer associated with the RARA gene.
The team found that super-enhancer profiles were strongly associated with survival outcomes, often independent of known genetic mutations in AML.
The RARA super-enhancer was associated with high expression of the RARA gene, which codes for a transcription factor targeted by SY-1425.
The RARA super-enhancer was predictive of response to SY-1425. In AML cells with high RARA expression, SY-1425 reduced proliferation and promoted differentiation.
Moreover, SY-1425 decreased tumor burden and prolonged survival in patient-derived xenograft models of AML with high RARA expression. However, there was no effect on AML cells or models with low RARA expression.
The researchers said SY-1425 induced profound transcriptional changes promoting cell differentiation in AML cells with high RARA expression, but the drug produced little to no transcriptional changes in AML cells with low RARA expression.
DHRS3 was the most strongly and rapidly induced gene in response to treatment with SY-1425. This led to the identification of DHRS3 induction as an early indicator of whether SY-1425 is affecting the targeted biology in defined subsets of AML and MDS patients. It is therefore used as a pharmacodynamic marker in the ongoing phase 2 trial of SY-1425.
In this trial, researchers are assessing the safety and efficacy of SY-1425 as a single agent in 4 AML and MDS patient populations, as well as testing SY-1425 in combination with azacitidine in newly diagnosed AML patients who are not suitable candidates for standard chemotherapy. ![]()
Tests reveal risk of passing on SCD, other diseases
Quest Diagnostics has announced the US launch of QHerit™, a genetic screening service that helps people of multiple ethnicities identify their risk of passing on heritable disorders to their offspring.
The QHerit Pan-Ethnic Expanded Carrier Screen is a panel of tests for the 22 heritable diseases cited in new screening guidelines from the American College of Gynecology (ACOG).
Among the diseases are alpha-thalassemia, Fanconi anemia, and beta-hemoglobinopathies, including sickle cell disease (SCD).
Traditionally, genetic carrier screening has been used for at-risk populations based on specific ancestry assumptions and focused on only a few likely disorders with higher prevalence associated with that ethnicity.
In its new guidelines, ACOG recommends offering pan-ethnic, expanded carrier, and ethnic-specific screening for all women considering pregnancy. The guidelines also state that the partner of a woman who tests positive may be a candidate for screening.
QHerit screens women and men for clinically relevant variants of genes for disorders that could have potentially devastating consequences, result in early death, or create a need for significant early intervention.
The disorders covered by QHerit include:
| Disease | Race/ethnicity | |||
| Alpha-thalassemia | Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Beta-
hemoglobinopathies (including SCD) |
Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Bloom syndrome | Ashkenazi Jewish descent (AJ) | |||
| Canavan disease | AJ and non-AJ | |||
| Cystic fibrosis | African American, AJ, Asian American, Hispanic American, non-Hispanic Caucasian | |||
| Dihydrolipoamide
dehydrogenase deficiency |
AJ | |||
| Familial dysautonomia | AJ | |||
| Familial hyperinsulinism | AJ | |||
| Fanconi anemia Type C | AJ | |||
| Fragile X syndrome | Females | |||
| Gaucher disease | AJ | |||
| Glycogen storage
disease Type Ia |
AJ, Caucasian | |||
| Joubert syndrome 2 | AJ | |||
| Maple syrup urine
disease |
AJ | |||
| Mucolipidosis Type IV | AJ | |||
| Nemaline myopathy | AJ | |||
| Niemann-Pick
disease Types A & B |
AJ | |||
| Spinal muscular
atrophy |
African American, AJ, Asian, Caucasian, Hispanic | |||
| Tay-Sachs disease | AJ, French Canadian, general population | |||
| Usher syndrome,
Type IF |
AJ | |||
| Usher syndrome,
Type IIIA |
AJ | |||
| Walker-Warburg
syndrome |
AJ | |||
QHerit is now available for order by US physicians. For more information, visit www.QHerit.com. ![]()
Quest Diagnostics has announced the US launch of QHerit™, a genetic screening service that helps people of multiple ethnicities identify their risk of passing on heritable disorders to their offspring.
The QHerit Pan-Ethnic Expanded Carrier Screen is a panel of tests for the 22 heritable diseases cited in new screening guidelines from the American College of Gynecology (ACOG).
Among the diseases are alpha-thalassemia, Fanconi anemia, and beta-hemoglobinopathies, including sickle cell disease (SCD).
Traditionally, genetic carrier screening has been used for at-risk populations based on specific ancestry assumptions and focused on only a few likely disorders with higher prevalence associated with that ethnicity.
In its new guidelines, ACOG recommends offering pan-ethnic, expanded carrier, and ethnic-specific screening for all women considering pregnancy. The guidelines also state that the partner of a woman who tests positive may be a candidate for screening.
QHerit screens women and men for clinically relevant variants of genes for disorders that could have potentially devastating consequences, result in early death, or create a need for significant early intervention.
The disorders covered by QHerit include:
| Disease | Race/ethnicity | |||
| Alpha-thalassemia | Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Beta-
hemoglobinopathies (including SCD) |
Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Bloom syndrome | Ashkenazi Jewish descent (AJ) | |||
| Canavan disease | AJ and non-AJ | |||
| Cystic fibrosis | African American, AJ, Asian American, Hispanic American, non-Hispanic Caucasian | |||
| Dihydrolipoamide
dehydrogenase deficiency |
AJ | |||
| Familial dysautonomia | AJ | |||
| Familial hyperinsulinism | AJ | |||
| Fanconi anemia Type C | AJ | |||
| Fragile X syndrome | Females | |||
| Gaucher disease | AJ | |||
| Glycogen storage
disease Type Ia |
AJ, Caucasian | |||
| Joubert syndrome 2 | AJ | |||
| Maple syrup urine
disease |
AJ | |||
| Mucolipidosis Type IV | AJ | |||
| Nemaline myopathy | AJ | |||
| Niemann-Pick
disease Types A & B |
AJ | |||
| Spinal muscular
atrophy |
African American, AJ, Asian, Caucasian, Hispanic | |||
| Tay-Sachs disease | AJ, French Canadian, general population | |||
| Usher syndrome,
Type IF |
AJ | |||
| Usher syndrome,
Type IIIA |
AJ | |||
| Walker-Warburg
syndrome |
AJ | |||
QHerit is now available for order by US physicians. For more information, visit www.QHerit.com. ![]()
Quest Diagnostics has announced the US launch of QHerit™, a genetic screening service that helps people of multiple ethnicities identify their risk of passing on heritable disorders to their offspring.
The QHerit Pan-Ethnic Expanded Carrier Screen is a panel of tests for the 22 heritable diseases cited in new screening guidelines from the American College of Gynecology (ACOG).
Among the diseases are alpha-thalassemia, Fanconi anemia, and beta-hemoglobinopathies, including sickle cell disease (SCD).
Traditionally, genetic carrier screening has been used for at-risk populations based on specific ancestry assumptions and focused on only a few likely disorders with higher prevalence associated with that ethnicity.
In its new guidelines, ACOG recommends offering pan-ethnic, expanded carrier, and ethnic-specific screening for all women considering pregnancy. The guidelines also state that the partner of a woman who tests positive may be a candidate for screening.
QHerit screens women and men for clinically relevant variants of genes for disorders that could have potentially devastating consequences, result in early death, or create a need for significant early intervention.
The disorders covered by QHerit include:
| Disease | Race/ethnicity | |||
| Alpha-thalassemia | Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Beta-
hemoglobinopathies (including SCD) |
Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Bloom syndrome | Ashkenazi Jewish descent (AJ) | |||
| Canavan disease | AJ and non-AJ | |||
| Cystic fibrosis | African American, AJ, Asian American, Hispanic American, non-Hispanic Caucasian | |||
| Dihydrolipoamide
dehydrogenase deficiency |
AJ | |||
| Familial dysautonomia | AJ | |||
| Familial hyperinsulinism | AJ | |||
| Fanconi anemia Type C | AJ | |||
| Fragile X syndrome | Females | |||
| Gaucher disease | AJ | |||
| Glycogen storage
disease Type Ia |
AJ, Caucasian | |||
| Joubert syndrome 2 | AJ | |||
| Maple syrup urine
disease |
AJ | |||
| Mucolipidosis Type IV | AJ | |||
| Nemaline myopathy | AJ | |||
| Niemann-Pick
disease Types A & B |
AJ | |||
| Spinal muscular
atrophy |
African American, AJ, Asian, Caucasian, Hispanic | |||
| Tay-Sachs disease | AJ, French Canadian, general population | |||
| Usher syndrome,
Type IF |
AJ | |||
| Usher syndrome,
Type IIIA |
AJ | |||
| Walker-Warburg
syndrome |
AJ | |||
QHerit is now available for order by US physicians. For more information, visit www.QHerit.com.
Allele-matching in cord blood transplant yields better survival
Matching down to the allele level in umbilical cord blood transplantation between unrelated donors results in greater overall survival for those with nonmalignant diseases, such as aplastic anemia, researchers found in a retrospective study published in the Lancet Haematology.
The review (Lancet Haematol. 2017 Jul;4[7]:e325-33), the largest published on the topic, indicates that clinicians should change practice from the current standard of antigen-level matching, said Mary Eapen, MD, director of the Center for International Blood and Marrow Transplant Research (CIBMTR) in Wauwatosa, Wisconsin.
“Our findings,” Dr. Eapen wrote, “support a change in clinical practice to prioritization of units on allele-level HLA matching at HLA-A, HLA-B, HLA-C, and HLA-DRB1.”
Data were pulled from cases reported to the Center for International Blood and Marrow Transplant Research or the European Group for Blood and Marrow Transplant. Researchers looked at 1,199 donor-recipient matches of cord blood transplantation for diseases, such as severe combined immunodeficiency (SCID), non-SCID primary immunodeficiency, inborn errors of metabolism, severe aplastic anemia, and Fanconi anemia. Recipients could be as old as age 16, but most were age 5 or younger.
After adjustment for factors, including cytomegalovirus serostatus, the intensity of the conditioning regimen, and the total nucleated cell dose, the 5-year overall survival was 79% for transplants that were matched at all eight alleles at HLA-A, HLA-B, HLA-C and HLA-DRB1. These results compare with 76% after transplants with one mismatch, 70% with two mismatches, 62% with three mismatches, and 49% with 4 or more mismatches.
Mortality risks were significantly higher for patients who received transplants with two (P = .018), three (P = .0001), and four or more mismatches (P less than .0001), compared with those whose transplants were fully matched. There was no difference statistically between full matches and one mismatch, but the findings suggest that the mortality risk might prove significant with a larger sample size.
Researchers cautioned that, because most patients were age 5 or younger, the results might not be generalizable to older children.
Although HLA typing is available at CIBMTR for most blood cord transplants for nonmalignant diseases, full allele matches or just one mismatch are not the norm, Dr. Eapen wrote. Researchers said that they suspect this is because of difficulties finding matches or because a high total nucleated cell count is prioritized above HLA matching. They suggest clinicians change their decision making in this regard.
Matching down to the allele level in umbilical cord blood transplantation between unrelated donors results in greater overall survival for those with nonmalignant diseases, such as aplastic anemia, researchers found in a retrospective study published in the Lancet Haematology.
The review (Lancet Haematol. 2017 Jul;4[7]:e325-33), the largest published on the topic, indicates that clinicians should change practice from the current standard of antigen-level matching, said Mary Eapen, MD, director of the Center for International Blood and Marrow Transplant Research (CIBMTR) in Wauwatosa, Wisconsin.
“Our findings,” Dr. Eapen wrote, “support a change in clinical practice to prioritization of units on allele-level HLA matching at HLA-A, HLA-B, HLA-C, and HLA-DRB1.”
Data were pulled from cases reported to the Center for International Blood and Marrow Transplant Research or the European Group for Blood and Marrow Transplant. Researchers looked at 1,199 donor-recipient matches of cord blood transplantation for diseases, such as severe combined immunodeficiency (SCID), non-SCID primary immunodeficiency, inborn errors of metabolism, severe aplastic anemia, and Fanconi anemia. Recipients could be as old as age 16, but most were age 5 or younger.
After adjustment for factors, including cytomegalovirus serostatus, the intensity of the conditioning regimen, and the total nucleated cell dose, the 5-year overall survival was 79% for transplants that were matched at all eight alleles at HLA-A, HLA-B, HLA-C and HLA-DRB1. These results compare with 76% after transplants with one mismatch, 70% with two mismatches, 62% with three mismatches, and 49% with 4 or more mismatches.
Mortality risks were significantly higher for patients who received transplants with two (P = .018), three (P = .0001), and four or more mismatches (P less than .0001), compared with those whose transplants were fully matched. There was no difference statistically between full matches and one mismatch, but the findings suggest that the mortality risk might prove significant with a larger sample size.
Researchers cautioned that, because most patients were age 5 or younger, the results might not be generalizable to older children.
Although HLA typing is available at CIBMTR for most blood cord transplants for nonmalignant diseases, full allele matches or just one mismatch are not the norm, Dr. Eapen wrote. Researchers said that they suspect this is because of difficulties finding matches or because a high total nucleated cell count is prioritized above HLA matching. They suggest clinicians change their decision making in this regard.
Matching down to the allele level in umbilical cord blood transplantation between unrelated donors results in greater overall survival for those with nonmalignant diseases, such as aplastic anemia, researchers found in a retrospective study published in the Lancet Haematology.
The review (Lancet Haematol. 2017 Jul;4[7]:e325-33), the largest published on the topic, indicates that clinicians should change practice from the current standard of antigen-level matching, said Mary Eapen, MD, director of the Center for International Blood and Marrow Transplant Research (CIBMTR) in Wauwatosa, Wisconsin.
“Our findings,” Dr. Eapen wrote, “support a change in clinical practice to prioritization of units on allele-level HLA matching at HLA-A, HLA-B, HLA-C, and HLA-DRB1.”
Data were pulled from cases reported to the Center for International Blood and Marrow Transplant Research or the European Group for Blood and Marrow Transplant. Researchers looked at 1,199 donor-recipient matches of cord blood transplantation for diseases, such as severe combined immunodeficiency (SCID), non-SCID primary immunodeficiency, inborn errors of metabolism, severe aplastic anemia, and Fanconi anemia. Recipients could be as old as age 16, but most were age 5 or younger.
After adjustment for factors, including cytomegalovirus serostatus, the intensity of the conditioning regimen, and the total nucleated cell dose, the 5-year overall survival was 79% for transplants that were matched at all eight alleles at HLA-A, HLA-B, HLA-C and HLA-DRB1. These results compare with 76% after transplants with one mismatch, 70% with two mismatches, 62% with three mismatches, and 49% with 4 or more mismatches.
Mortality risks were significantly higher for patients who received transplants with two (P = .018), three (P = .0001), and four or more mismatches (P less than .0001), compared with those whose transplants were fully matched. There was no difference statistically between full matches and one mismatch, but the findings suggest that the mortality risk might prove significant with a larger sample size.
Researchers cautioned that, because most patients were age 5 or younger, the results might not be generalizable to older children.
Although HLA typing is available at CIBMTR for most blood cord transplants for nonmalignant diseases, full allele matches or just one mismatch are not the norm, Dr. Eapen wrote. Researchers said that they suspect this is because of difficulties finding matches or because a high total nucleated cell count is prioritized above HLA matching. They suggest clinicians change their decision making in this regard.
FROM THE LANCET HAEMATOLOGY
Key clinical point: HLA matching at the allele-level produces better survival in umbilical cord blood transplantation for nonmalignant diseases.
Major finding: Mortality risks were significantly higher for patients who received transplants with two (P = .018), three (P = .0001), and four or more mismatches (P less than .0001), compared with those whose transplants were fully matched at all eight alleles at HLA-A, HLA-B, HLA-C and HLA-DRB1.
Data source: A retrospective review of 1,199 cases reported to the Center for International Blood and Marrow Transplant Research (CIBMTR) or the European Group for Blood and Marrow Transplant (EGBMT).
Disclosures: The authors reported no conflicts of interest.
Predicting response to azacitidine in MDS
Research published in Cell Reports helps explain why some patients with myelodysplastic syndrome (MDS) do not respond to treatment with azacitidine.
The study showed that patients who were resistant to the drug had relatively quiescent hematopoietic progenitor cells (HPCs).
A smaller proportion of their HPCs were undergoing active cell-cycle progression when compared to the HPCs of patients who responded to azacitidine.
This discovery could provide the first method to identify non-responders to azacitidine early, according to study author Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
“These are early days, but this could avoid what has really been a ‘wait and see’ approach with patients that sometimes results in them receiving futile treatment for 6 months,” Dr Unnikrishnan said.
“By that stage, the patient’s disease has progressed, and there’s no alternative for them.”
Dr Unnikrishnan and his colleagues also found the HPC quiescence in non-responders was mediated by integrin α5 (ITGA5) signaling, and the cells’ hematopoietic potential improved when the team combined azacitidine treatment with an ITGA5 inhibitor.
This suggests a potential avenue for future combination therapies that would improve azacitidine responsiveness.
Lastly, the researchers made discoveries that could explain why some patients who initially respond to azacitidine eventually relapse.
“All of the pernicious mutations that we associate with MDS never disappear in these patients, even after years of treatment,” Dr Unnikrishnan said. “From a clinical perspective, blood cell production is restored in patients, but they are a ticking time bomb, waiting to relapse.”
“[Azacitidine] is not a cure, and we are starting to understand why it does what it does. We need to find better treatments than azacitidine if we want a more durable therapy for MDS, and that’s the basis for our future work.”
Research published in Cell Reports helps explain why some patients with myelodysplastic syndrome (MDS) do not respond to treatment with azacitidine.
The study showed that patients who were resistant to the drug had relatively quiescent hematopoietic progenitor cells (HPCs).
A smaller proportion of their HPCs were undergoing active cell-cycle progression when compared to the HPCs of patients who responded to azacitidine.
This discovery could provide the first method to identify non-responders to azacitidine early, according to study author Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
“These are early days, but this could avoid what has really been a ‘wait and see’ approach with patients that sometimes results in them receiving futile treatment for 6 months,” Dr Unnikrishnan said.
“By that stage, the patient’s disease has progressed, and there’s no alternative for them.”
Dr Unnikrishnan and his colleagues also found the HPC quiescence in non-responders was mediated by integrin α5 (ITGA5) signaling, and the cells’ hematopoietic potential improved when the team combined azacitidine treatment with an ITGA5 inhibitor.
This suggests a potential avenue for future combination therapies that would improve azacitidine responsiveness.
Lastly, the researchers made discoveries that could explain why some patients who initially respond to azacitidine eventually relapse.
“All of the pernicious mutations that we associate with MDS never disappear in these patients, even after years of treatment,” Dr Unnikrishnan said. “From a clinical perspective, blood cell production is restored in patients, but they are a ticking time bomb, waiting to relapse.”
“[Azacitidine] is not a cure, and we are starting to understand why it does what it does. We need to find better treatments than azacitidine if we want a more durable therapy for MDS, and that’s the basis for our future work.”
Research published in Cell Reports helps explain why some patients with myelodysplastic syndrome (MDS) do not respond to treatment with azacitidine.
The study showed that patients who were resistant to the drug had relatively quiescent hematopoietic progenitor cells (HPCs).
A smaller proportion of their HPCs were undergoing active cell-cycle progression when compared to the HPCs of patients who responded to azacitidine.
This discovery could provide the first method to identify non-responders to azacitidine early, according to study author Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
“These are early days, but this could avoid what has really been a ‘wait and see’ approach with patients that sometimes results in them receiving futile treatment for 6 months,” Dr Unnikrishnan said.
“By that stage, the patient’s disease has progressed, and there’s no alternative for them.”
Dr Unnikrishnan and his colleagues also found the HPC quiescence in non-responders was mediated by integrin α5 (ITGA5) signaling, and the cells’ hematopoietic potential improved when the team combined azacitidine treatment with an ITGA5 inhibitor.
This suggests a potential avenue for future combination therapies that would improve azacitidine responsiveness.
Lastly, the researchers made discoveries that could explain why some patients who initially respond to azacitidine eventually relapse.
“All of the pernicious mutations that we associate with MDS never disappear in these patients, even after years of treatment,” Dr Unnikrishnan said. “From a clinical perspective, blood cell production is restored in patients, but they are a ticking time bomb, waiting to relapse.”
“[Azacitidine] is not a cure, and we are starting to understand why it does what it does. We need to find better treatments than azacitidine if we want a more durable therapy for MDS, and that’s the basis for our future work.”