User login
Managing menopausal symptoms after risk-reducing salpingo-oophorectomy
Compared to the general population, women with mutations in the BRCA1 or BRCA2 genes have a significantly higher lifetime risk of ovarian and breast cancers (Science. 2003 Oct 24;302[5645]:643-6). Since the occurrence of ovarian and breast cancer in BRCA carriers is often prior to menopause, and because we have no screening test to detect early stage ovarian cancer, risk-reducing salpingo-oophorectomy has been recommended around age 40.
It has been shown that risk-reducing salpingo-oophorectomy significantly reduces ovarian cancer risk by 85%-95% in BRCA-affected women. Also, this surgery can reduce breast cancer risk by 53%-68% (N Engl J Med. 2002 May 23;346[21]:1609-15). The 2008 Practice Bulletin from the American College of Obstetricians and Gynecologists recommends that risk-reducing salpingo-oophorectomy should be performed in women with BRCA1 or BRCA2 mutations after the completion of childbearing or age 40 (Obstet Gynecol. 2008 Jan;111[1]:231-41).
Health implications
Nearly 60% of women who have a BRCA1 or BRCA2 mutation will elect to undergo risk-reducing salpingo-oophorectomy between the ages of 35 and 40 years (Open Med. 2007 Aug 13;1[2]:e92-8). As such, surgical menopause can result in hot flashes, vaginal dryness, sexual dysfunction, sleep disturbances, and cognitive changes, which may significantly impact a woman’s quality of life. In addition, increased risk of cardiovascular disease and osteoporosis following bilateral salpingo-oophorectomy may have a significant impact on a woman’s health.
Since these women undergo surgical menopause as opposed to natural menopause, they have an abrupt loss in hormones, and due to their younger age at the time of surgery, they may also have a longer exposure period to the detrimental effects of hypoestrogenism.
Symptom management
Various treatment options exist for relief of menopausal symptoms, including nonhormonal therapies and hormone replacement therapies (HT).
Nonhormonal therapies include serotonin receptor inhibitors (venlafaxine and paroxetine) and alpha-2 adrenergic agonists (clonidine), which are most appropriate for the treatment of vasomotor symptoms. Unfortunately, these options have proved to be as effective as HT. Also, women should be adequately counseled regarding the various side effects of these nonhormonal medications. Alternative approaches such as phytoestrogens are unproven and are still undergoing investigation. As such, HT remains the standard for treatment of menopausal symptoms, and many trials have confirmed that HT can effectively treat menopausal symptoms following risk-reducing salpingo-oophorectomy.
This then raises the question of safety regarding use of HT in this patient population; especially the possibility of increased risk of breast cancer. Interestingly, only 10%-25% of BRCA1 carriers will have estrogen receptor–positive breast cancer, while 65%-79% of BRCA2-associated breast cancers will be positive for the receptor (Clin Cancer Res. 2004 Mar 15;10[6]:2029-34).
Unfortunately, we do not have adequate trials or studies with sufficient long-term follow-up to validate whether HT increases the risk of breast cancer or recurrence. However, the PROSE Study Group did report on a prospective cohort of 462 women with BRCA1 or BRCA2 mutations. In this study, HT did not alter the reduction in breast cancer risk from risk-reducing salpingo-oophorectomy (J Clin Oncol. 2005 Nov 1;23[31]:7804-10). In addition to a paucity of data regarding systemic HT, there is little data in the BRCA-positive population to confirm the safety of local vaginal estrogen for treatment of vaginal atrophy (J Clin Oncol. 2004 Mar 15;22[6]:1045-54).
Understanding the options
Use of HT in women with BRCA1 and BRCA2 mutations requires further investigation. There should be shared decision making between the patient and provider when counseling on the management of menopausal symptoms following risk-reducing salpingo-oophorectomy. Most importantly, women should understand the options of nonhormonal therapies and their specific side effects. They should also understand the lack of significant data regarding use of systemic HT, and that if use is elected, there may be an increased risk of breast cancer.
Women who do elect to use systemic HT following risk-reducing salpingo-oophorectomy have options that can help reduce the risk of HT-associated breast cancer, including a shorter duration of systemic HT or concurrent hysterectomy to allow for estrogen-only HT, which has a decreased risk of breast cancer compared with combined therapies that include progestins. These women may also be considering prophylactic mastectomy, which would change the concerns regarding HT and an increased risk of breast cancer.
Increased awareness of these options among physicians and patients alike can help to decrease unsatisfactory symptoms and improve quality of life in women undergoing risk-reducing salpingo-oophorectomy.
Dr. Staley is a resident physician in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at obnews@frontlinemedcom.com.
Compared to the general population, women with mutations in the BRCA1 or BRCA2 genes have a significantly higher lifetime risk of ovarian and breast cancers (Science. 2003 Oct 24;302[5645]:643-6). Since the occurrence of ovarian and breast cancer in BRCA carriers is often prior to menopause, and because we have no screening test to detect early stage ovarian cancer, risk-reducing salpingo-oophorectomy has been recommended around age 40.
It has been shown that risk-reducing salpingo-oophorectomy significantly reduces ovarian cancer risk by 85%-95% in BRCA-affected women. Also, this surgery can reduce breast cancer risk by 53%-68% (N Engl J Med. 2002 May 23;346[21]:1609-15). The 2008 Practice Bulletin from the American College of Obstetricians and Gynecologists recommends that risk-reducing salpingo-oophorectomy should be performed in women with BRCA1 or BRCA2 mutations after the completion of childbearing or age 40 (Obstet Gynecol. 2008 Jan;111[1]:231-41).
Health implications
Nearly 60% of women who have a BRCA1 or BRCA2 mutation will elect to undergo risk-reducing salpingo-oophorectomy between the ages of 35 and 40 years (Open Med. 2007 Aug 13;1[2]:e92-8). As such, surgical menopause can result in hot flashes, vaginal dryness, sexual dysfunction, sleep disturbances, and cognitive changes, which may significantly impact a woman’s quality of life. In addition, increased risk of cardiovascular disease and osteoporosis following bilateral salpingo-oophorectomy may have a significant impact on a woman’s health.
Since these women undergo surgical menopause as opposed to natural menopause, they have an abrupt loss in hormones, and due to their younger age at the time of surgery, they may also have a longer exposure period to the detrimental effects of hypoestrogenism.
Symptom management
Various treatment options exist for relief of menopausal symptoms, including nonhormonal therapies and hormone replacement therapies (HT).
Nonhormonal therapies include serotonin receptor inhibitors (venlafaxine and paroxetine) and alpha-2 adrenergic agonists (clonidine), which are most appropriate for the treatment of vasomotor symptoms. Unfortunately, these options have proved to be as effective as HT. Also, women should be adequately counseled regarding the various side effects of these nonhormonal medications. Alternative approaches such as phytoestrogens are unproven and are still undergoing investigation. As such, HT remains the standard for treatment of menopausal symptoms, and many trials have confirmed that HT can effectively treat menopausal symptoms following risk-reducing salpingo-oophorectomy.
This then raises the question of safety regarding use of HT in this patient population; especially the possibility of increased risk of breast cancer. Interestingly, only 10%-25% of BRCA1 carriers will have estrogen receptor–positive breast cancer, while 65%-79% of BRCA2-associated breast cancers will be positive for the receptor (Clin Cancer Res. 2004 Mar 15;10[6]:2029-34).
Unfortunately, we do not have adequate trials or studies with sufficient long-term follow-up to validate whether HT increases the risk of breast cancer or recurrence. However, the PROSE Study Group did report on a prospective cohort of 462 women with BRCA1 or BRCA2 mutations. In this study, HT did not alter the reduction in breast cancer risk from risk-reducing salpingo-oophorectomy (J Clin Oncol. 2005 Nov 1;23[31]:7804-10). In addition to a paucity of data regarding systemic HT, there is little data in the BRCA-positive population to confirm the safety of local vaginal estrogen for treatment of vaginal atrophy (J Clin Oncol. 2004 Mar 15;22[6]:1045-54).
Understanding the options
Use of HT in women with BRCA1 and BRCA2 mutations requires further investigation. There should be shared decision making between the patient and provider when counseling on the management of menopausal symptoms following risk-reducing salpingo-oophorectomy. Most importantly, women should understand the options of nonhormonal therapies and their specific side effects. They should also understand the lack of significant data regarding use of systemic HT, and that if use is elected, there may be an increased risk of breast cancer.
Women who do elect to use systemic HT following risk-reducing salpingo-oophorectomy have options that can help reduce the risk of HT-associated breast cancer, including a shorter duration of systemic HT or concurrent hysterectomy to allow for estrogen-only HT, which has a decreased risk of breast cancer compared with combined therapies that include progestins. These women may also be considering prophylactic mastectomy, which would change the concerns regarding HT and an increased risk of breast cancer.
Increased awareness of these options among physicians and patients alike can help to decrease unsatisfactory symptoms and improve quality of life in women undergoing risk-reducing salpingo-oophorectomy.
Dr. Staley is a resident physician in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at obnews@frontlinemedcom.com.
Compared to the general population, women with mutations in the BRCA1 or BRCA2 genes have a significantly higher lifetime risk of ovarian and breast cancers (Science. 2003 Oct 24;302[5645]:643-6). Since the occurrence of ovarian and breast cancer in BRCA carriers is often prior to menopause, and because we have no screening test to detect early stage ovarian cancer, risk-reducing salpingo-oophorectomy has been recommended around age 40.
It has been shown that risk-reducing salpingo-oophorectomy significantly reduces ovarian cancer risk by 85%-95% in BRCA-affected women. Also, this surgery can reduce breast cancer risk by 53%-68% (N Engl J Med. 2002 May 23;346[21]:1609-15). The 2008 Practice Bulletin from the American College of Obstetricians and Gynecologists recommends that risk-reducing salpingo-oophorectomy should be performed in women with BRCA1 or BRCA2 mutations after the completion of childbearing or age 40 (Obstet Gynecol. 2008 Jan;111[1]:231-41).
Health implications
Nearly 60% of women who have a BRCA1 or BRCA2 mutation will elect to undergo risk-reducing salpingo-oophorectomy between the ages of 35 and 40 years (Open Med. 2007 Aug 13;1[2]:e92-8). As such, surgical menopause can result in hot flashes, vaginal dryness, sexual dysfunction, sleep disturbances, and cognitive changes, which may significantly impact a woman’s quality of life. In addition, increased risk of cardiovascular disease and osteoporosis following bilateral salpingo-oophorectomy may have a significant impact on a woman’s health.
Since these women undergo surgical menopause as opposed to natural menopause, they have an abrupt loss in hormones, and due to their younger age at the time of surgery, they may also have a longer exposure period to the detrimental effects of hypoestrogenism.
Symptom management
Various treatment options exist for relief of menopausal symptoms, including nonhormonal therapies and hormone replacement therapies (HT).
Nonhormonal therapies include serotonin receptor inhibitors (venlafaxine and paroxetine) and alpha-2 adrenergic agonists (clonidine), which are most appropriate for the treatment of vasomotor symptoms. Unfortunately, these options have proved to be as effective as HT. Also, women should be adequately counseled regarding the various side effects of these nonhormonal medications. Alternative approaches such as phytoestrogens are unproven and are still undergoing investigation. As such, HT remains the standard for treatment of menopausal symptoms, and many trials have confirmed that HT can effectively treat menopausal symptoms following risk-reducing salpingo-oophorectomy.
This then raises the question of safety regarding use of HT in this patient population; especially the possibility of increased risk of breast cancer. Interestingly, only 10%-25% of BRCA1 carriers will have estrogen receptor–positive breast cancer, while 65%-79% of BRCA2-associated breast cancers will be positive for the receptor (Clin Cancer Res. 2004 Mar 15;10[6]:2029-34).
Unfortunately, we do not have adequate trials or studies with sufficient long-term follow-up to validate whether HT increases the risk of breast cancer or recurrence. However, the PROSE Study Group did report on a prospective cohort of 462 women with BRCA1 or BRCA2 mutations. In this study, HT did not alter the reduction in breast cancer risk from risk-reducing salpingo-oophorectomy (J Clin Oncol. 2005 Nov 1;23[31]:7804-10). In addition to a paucity of data regarding systemic HT, there is little data in the BRCA-positive population to confirm the safety of local vaginal estrogen for treatment of vaginal atrophy (J Clin Oncol. 2004 Mar 15;22[6]:1045-54).
Understanding the options
Use of HT in women with BRCA1 and BRCA2 mutations requires further investigation. There should be shared decision making between the patient and provider when counseling on the management of menopausal symptoms following risk-reducing salpingo-oophorectomy. Most importantly, women should understand the options of nonhormonal therapies and their specific side effects. They should also understand the lack of significant data regarding use of systemic HT, and that if use is elected, there may be an increased risk of breast cancer.
Women who do elect to use systemic HT following risk-reducing salpingo-oophorectomy have options that can help reduce the risk of HT-associated breast cancer, including a shorter duration of systemic HT or concurrent hysterectomy to allow for estrogen-only HT, which has a decreased risk of breast cancer compared with combined therapies that include progestins. These women may also be considering prophylactic mastectomy, which would change the concerns regarding HT and an increased risk of breast cancer.
Increased awareness of these options among physicians and patients alike can help to decrease unsatisfactory symptoms and improve quality of life in women undergoing risk-reducing salpingo-oophorectomy.
Dr. Staley is a resident physician in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at obnews@frontlinemedcom.com.
DenseBreast-info.org: What this resource can offer you, and your patients
Read the article Get smart about dense breasts by Wendie Berg, MD, PhD, JoAnn Pushkin, and Cindy Henke-Sarmento (October 2015)
Read the article Get smart about dense breasts by Wendie Berg, MD, PhD, JoAnn Pushkin, and Cindy Henke-Sarmento (October 2015)
Read the article Get smart about dense breasts by Wendie Berg, MD, PhD, JoAnn Pushkin, and Cindy Henke-Sarmento (October 2015)
Access DenseBreast-info.org
Will New American Cancer Society Mammography Policy Change VHA Practice?
The new American Cancer Society (ACS) policy for mammography screening now recommends annual mammograms from age 45 until age 54, suggesting a less aggressive approach to screening than in the 2003 guidelines. The recommendation is for asymptomatic women at average risk of developing breast cancer.
Related: How Much Is Too Much Cancer Screening?
“These recommendations are made with the intent of maximizing reductions in breast cancer mortality and years of life saved while being attentive to the need to minimize harms associated with screening,” said Dr. Kevin C. Oeffinger, chairman of the breast cancer guideline panel.
Related: Advances in Targeted Therapy for Breast Cancer
The guideline, developed by a panel of outside experts, was published October 20, 2015, in The Journal of the American Medical Association.
Other important recommendation changes include:
- ŸWomen aged 45 to 54 years should receive annual screening mammography and at age 55 women should transition to biennial screening.
- ŸWomen should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer.
- ŸClinical breast examination is no longer recommended at any age.
- ŸThe panel noted that the recommendations are an effort to avoid false positive findings, which can take an emotional toll.
The current VHA recommendations state:
- Mammography is not recommended for women aged 13 to 39 years.
- Women aged 40 to 49 years should talk with their health care providers about screening.
- ŸMammograms are recommended every 2 years for women aged 50 to 74 years.
- ŸWomen aged > 75 years should talk with their health care providers.
According to Anita Aggarwal, DO, PhD, president of the Association of VA Hematology and Oncology (AVAHO), the VHA recommendations leave a lot of wiggle room; every year starting at age 40 is still acceptable practice at the VA.
Related: Breast Cancer Research Group Aims to Improve Veteran Survival Rates
“Keep in mind that recommendations are just recommendations,” Dr. Aggarwal told Federal Practitioner. “One size may not fit all. I believe we should use our sound judgment based on valid research to recommend what is best for the patient. Based on my literature search, annual screening starting at 40 saves the most lives via early detection.”
The new American Cancer Society (ACS) policy for mammography screening now recommends annual mammograms from age 45 until age 54, suggesting a less aggressive approach to screening than in the 2003 guidelines. The recommendation is for asymptomatic women at average risk of developing breast cancer.
Related: How Much Is Too Much Cancer Screening?
“These recommendations are made with the intent of maximizing reductions in breast cancer mortality and years of life saved while being attentive to the need to minimize harms associated with screening,” said Dr. Kevin C. Oeffinger, chairman of the breast cancer guideline panel.
Related: Advances in Targeted Therapy for Breast Cancer
The guideline, developed by a panel of outside experts, was published October 20, 2015, in The Journal of the American Medical Association.
Other important recommendation changes include:
- ŸWomen aged 45 to 54 years should receive annual screening mammography and at age 55 women should transition to biennial screening.
- ŸWomen should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer.
- ŸClinical breast examination is no longer recommended at any age.
- ŸThe panel noted that the recommendations are an effort to avoid false positive findings, which can take an emotional toll.
The current VHA recommendations state:
- Mammography is not recommended for women aged 13 to 39 years.
- Women aged 40 to 49 years should talk with their health care providers about screening.
- ŸMammograms are recommended every 2 years for women aged 50 to 74 years.
- ŸWomen aged > 75 years should talk with their health care providers.
According to Anita Aggarwal, DO, PhD, president of the Association of VA Hematology and Oncology (AVAHO), the VHA recommendations leave a lot of wiggle room; every year starting at age 40 is still acceptable practice at the VA.
Related: Breast Cancer Research Group Aims to Improve Veteran Survival Rates
“Keep in mind that recommendations are just recommendations,” Dr. Aggarwal told Federal Practitioner. “One size may not fit all. I believe we should use our sound judgment based on valid research to recommend what is best for the patient. Based on my literature search, annual screening starting at 40 saves the most lives via early detection.”
The new American Cancer Society (ACS) policy for mammography screening now recommends annual mammograms from age 45 until age 54, suggesting a less aggressive approach to screening than in the 2003 guidelines. The recommendation is for asymptomatic women at average risk of developing breast cancer.
Related: How Much Is Too Much Cancer Screening?
“These recommendations are made with the intent of maximizing reductions in breast cancer mortality and years of life saved while being attentive to the need to minimize harms associated with screening,” said Dr. Kevin C. Oeffinger, chairman of the breast cancer guideline panel.
Related: Advances in Targeted Therapy for Breast Cancer
The guideline, developed by a panel of outside experts, was published October 20, 2015, in The Journal of the American Medical Association.
Other important recommendation changes include:
- ŸWomen aged 45 to 54 years should receive annual screening mammography and at age 55 women should transition to biennial screening.
- ŸWomen should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer.
- ŸClinical breast examination is no longer recommended at any age.
- ŸThe panel noted that the recommendations are an effort to avoid false positive findings, which can take an emotional toll.
The current VHA recommendations state:
- Mammography is not recommended for women aged 13 to 39 years.
- Women aged 40 to 49 years should talk with their health care providers about screening.
- ŸMammograms are recommended every 2 years for women aged 50 to 74 years.
- ŸWomen aged > 75 years should talk with their health care providers.
According to Anita Aggarwal, DO, PhD, president of the Association of VA Hematology and Oncology (AVAHO), the VHA recommendations leave a lot of wiggle room; every year starting at age 40 is still acceptable practice at the VA.
Related: Breast Cancer Research Group Aims to Improve Veteran Survival Rates
“Keep in mind that recommendations are just recommendations,” Dr. Aggarwal told Federal Practitioner. “One size may not fit all. I believe we should use our sound judgment based on valid research to recommend what is best for the patient. Based on my literature search, annual screening starting at 40 saves the most lives via early detection.”
Study finds no link between thyroid autoimmunity, breast cancer outcomes
LAKE BUENA VISTA, FLA. – In contrast with at least two prior small studies, thyroid peroxidase autoantibodies were not associated with breast cancer outcomes in a large cohort of patients.
Stored serum samples from 1,974 patients with lymph node–positive or high-risk lymph node–negative breast cancer who were enrolled in the TACT (Taxotere as Adjuvant Chemotherapy for Early Breast Cancer) trial were tested, and investigators assessed the prognostic significance of thyroid peroxidase autoantibodies (TPOAb) and thyroid function for disease-free survival (DFS), overall survival (OS), and time to recurrence (TTR).
At a median follow-up of 97.5 months, investigators found no evidence of a difference in outcomes, either on univariate or multivariable analysis, for any of those outcomes based on free thyroxine (FT4) or thyroid-stimulating hormone (TSH) levels alone or in combination as hypo- or hyperthyroidism, Dr. Ilaria Muller, of Cardiff (England) University reported at the International Thyroid Congress.
For example, the unadjusted hazard ratios for DFS, OS, and TTR based on TPOAb-positive vs. TPOAb-negative status were 0.97, 0.86, and 0.97, respectively, Dr. Muller said.
An explorative multivariable analysis of the impact of TPOab status and thyroid function on breast cancer DFS, OS, and TTR also showed no evidence of a difference (HR, 1 and 0.97 for TPOAb-negative and TPOAb-positive status; HR, 1 and 1.27 for euthyroid and hypothyroid status), Dr. Muller said.
Similarly, no evidence of a difference in outcomes was seen based on an explorative analysis of TPOAb status in clinical subgroups based on age, nodal status, tumor grade, tumor size, type of surgery, estrogen receptor (ER)-positive status, human epidermal growth factor receptor 2 (HER2)-positive status, and molecular subgroup, she noted.
Serum samples used in the study were from patients who had undergone breast cancer surgery a mean of 15.5 months prior and were mainly taken during/after adjuvant treatments for breast cancer. All had received chemotherapy: 88.4% received radiotherapy, 98.7% of ER-positive patients received hormonal therapy, and trastuzumab was given in 11.8% of HER2-positive patients.
About a fifth (20.6%) of patients were TPOAb-positive, 89.16% were euthyroid, 4.86% were hypothyroid, and 5.97% were hyperthyroid.
The TPOAb-positive and -negative patients were largely comparable, except the TPOAb-positive women were slightly older.
A sensitivity analysis performed in 123 patients with blood taken after surgery but before any adjuvant therapy for breast cancer also showed no evidence of TPOAb prognostic ability, Dr. Muller said.
Despite an ongoing debate aabout a possible association between breast cancer and thyroid autoimmunity, findings have been conflicting. Two small studies correlated TPOAb positivity with improved breast cancer outcomes, but a third did not confirm the findings.
“As a possible explanation, we hypothesized an immune response to shared thyroid/breast antigens. We recently reported that TPO is expressed in breast cancer tissue,” Dr. Muller wrote.
However, the findings of the current study – the largest retrospective study to date investigating the prognostic role of TPOAb in breast cancer – suggest that TPOAb and thyroid function are not prognostic markers in breast cancer.
“Effects of chemotherapy and/or radiotherapy for breast cancer are currently under debate. Tamoxifen exerts an antithyroid effect. However, confounding due to breast cancer adjuvant treatment is unlikely to alter significantly any results, as suggested by our sensitivity analysis performed on 123 patients,” she said at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association , European Thyroid Association, and Latin American Thyroid Society.
This study was supported by a Tenovus Innovation Grant from Tenovus Cancer Care. TACT was funded by Cancer Research UK. Dr. Muller reported having no disclosures.
LAKE BUENA VISTA, FLA. – In contrast with at least two prior small studies, thyroid peroxidase autoantibodies were not associated with breast cancer outcomes in a large cohort of patients.
Stored serum samples from 1,974 patients with lymph node–positive or high-risk lymph node–negative breast cancer who were enrolled in the TACT (Taxotere as Adjuvant Chemotherapy for Early Breast Cancer) trial were tested, and investigators assessed the prognostic significance of thyroid peroxidase autoantibodies (TPOAb) and thyroid function for disease-free survival (DFS), overall survival (OS), and time to recurrence (TTR).
At a median follow-up of 97.5 months, investigators found no evidence of a difference in outcomes, either on univariate or multivariable analysis, for any of those outcomes based on free thyroxine (FT4) or thyroid-stimulating hormone (TSH) levels alone or in combination as hypo- or hyperthyroidism, Dr. Ilaria Muller, of Cardiff (England) University reported at the International Thyroid Congress.
For example, the unadjusted hazard ratios for DFS, OS, and TTR based on TPOAb-positive vs. TPOAb-negative status were 0.97, 0.86, and 0.97, respectively, Dr. Muller said.
An explorative multivariable analysis of the impact of TPOab status and thyroid function on breast cancer DFS, OS, and TTR also showed no evidence of a difference (HR, 1 and 0.97 for TPOAb-negative and TPOAb-positive status; HR, 1 and 1.27 for euthyroid and hypothyroid status), Dr. Muller said.
Similarly, no evidence of a difference in outcomes was seen based on an explorative analysis of TPOAb status in clinical subgroups based on age, nodal status, tumor grade, tumor size, type of surgery, estrogen receptor (ER)-positive status, human epidermal growth factor receptor 2 (HER2)-positive status, and molecular subgroup, she noted.
Serum samples used in the study were from patients who had undergone breast cancer surgery a mean of 15.5 months prior and were mainly taken during/after adjuvant treatments for breast cancer. All had received chemotherapy: 88.4% received radiotherapy, 98.7% of ER-positive patients received hormonal therapy, and trastuzumab was given in 11.8% of HER2-positive patients.
About a fifth (20.6%) of patients were TPOAb-positive, 89.16% were euthyroid, 4.86% were hypothyroid, and 5.97% were hyperthyroid.
The TPOAb-positive and -negative patients were largely comparable, except the TPOAb-positive women were slightly older.
A sensitivity analysis performed in 123 patients with blood taken after surgery but before any adjuvant therapy for breast cancer also showed no evidence of TPOAb prognostic ability, Dr. Muller said.
Despite an ongoing debate aabout a possible association between breast cancer and thyroid autoimmunity, findings have been conflicting. Two small studies correlated TPOAb positivity with improved breast cancer outcomes, but a third did not confirm the findings.
“As a possible explanation, we hypothesized an immune response to shared thyroid/breast antigens. We recently reported that TPO is expressed in breast cancer tissue,” Dr. Muller wrote.
However, the findings of the current study – the largest retrospective study to date investigating the prognostic role of TPOAb in breast cancer – suggest that TPOAb and thyroid function are not prognostic markers in breast cancer.
“Effects of chemotherapy and/or radiotherapy for breast cancer are currently under debate. Tamoxifen exerts an antithyroid effect. However, confounding due to breast cancer adjuvant treatment is unlikely to alter significantly any results, as suggested by our sensitivity analysis performed on 123 patients,” she said at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association , European Thyroid Association, and Latin American Thyroid Society.
This study was supported by a Tenovus Innovation Grant from Tenovus Cancer Care. TACT was funded by Cancer Research UK. Dr. Muller reported having no disclosures.
LAKE BUENA VISTA, FLA. – In contrast with at least two prior small studies, thyroid peroxidase autoantibodies were not associated with breast cancer outcomes in a large cohort of patients.
Stored serum samples from 1,974 patients with lymph node–positive or high-risk lymph node–negative breast cancer who were enrolled in the TACT (Taxotere as Adjuvant Chemotherapy for Early Breast Cancer) trial were tested, and investigators assessed the prognostic significance of thyroid peroxidase autoantibodies (TPOAb) and thyroid function for disease-free survival (DFS), overall survival (OS), and time to recurrence (TTR).
At a median follow-up of 97.5 months, investigators found no evidence of a difference in outcomes, either on univariate or multivariable analysis, for any of those outcomes based on free thyroxine (FT4) or thyroid-stimulating hormone (TSH) levels alone or in combination as hypo- or hyperthyroidism, Dr. Ilaria Muller, of Cardiff (England) University reported at the International Thyroid Congress.
For example, the unadjusted hazard ratios for DFS, OS, and TTR based on TPOAb-positive vs. TPOAb-negative status were 0.97, 0.86, and 0.97, respectively, Dr. Muller said.
An explorative multivariable analysis of the impact of TPOab status and thyroid function on breast cancer DFS, OS, and TTR also showed no evidence of a difference (HR, 1 and 0.97 for TPOAb-negative and TPOAb-positive status; HR, 1 and 1.27 for euthyroid and hypothyroid status), Dr. Muller said.
Similarly, no evidence of a difference in outcomes was seen based on an explorative analysis of TPOAb status in clinical subgroups based on age, nodal status, tumor grade, tumor size, type of surgery, estrogen receptor (ER)-positive status, human epidermal growth factor receptor 2 (HER2)-positive status, and molecular subgroup, she noted.
Serum samples used in the study were from patients who had undergone breast cancer surgery a mean of 15.5 months prior and were mainly taken during/after adjuvant treatments for breast cancer. All had received chemotherapy: 88.4% received radiotherapy, 98.7% of ER-positive patients received hormonal therapy, and trastuzumab was given in 11.8% of HER2-positive patients.
About a fifth (20.6%) of patients were TPOAb-positive, 89.16% were euthyroid, 4.86% were hypothyroid, and 5.97% were hyperthyroid.
The TPOAb-positive and -negative patients were largely comparable, except the TPOAb-positive women were slightly older.
A sensitivity analysis performed in 123 patients with blood taken after surgery but before any adjuvant therapy for breast cancer also showed no evidence of TPOAb prognostic ability, Dr. Muller said.
Despite an ongoing debate aabout a possible association between breast cancer and thyroid autoimmunity, findings have been conflicting. Two small studies correlated TPOAb positivity with improved breast cancer outcomes, but a third did not confirm the findings.
“As a possible explanation, we hypothesized an immune response to shared thyroid/breast antigens. We recently reported that TPO is expressed in breast cancer tissue,” Dr. Muller wrote.
However, the findings of the current study – the largest retrospective study to date investigating the prognostic role of TPOAb in breast cancer – suggest that TPOAb and thyroid function are not prognostic markers in breast cancer.
“Effects of chemotherapy and/or radiotherapy for breast cancer are currently under debate. Tamoxifen exerts an antithyroid effect. However, confounding due to breast cancer adjuvant treatment is unlikely to alter significantly any results, as suggested by our sensitivity analysis performed on 123 patients,” she said at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association , European Thyroid Association, and Latin American Thyroid Society.
This study was supported by a Tenovus Innovation Grant from Tenovus Cancer Care. TACT was funded by Cancer Research UK. Dr. Muller reported having no disclosures.
At ITC 2015
Key clinical point: In contrast with at least two prior small studies, thyroid peroxidase autoantibodies were not associated with breast cancer outcomes in a large cohort of patients.
Major finding: An explorative multivariable analysis showed no impact of TPOab status and thyroid function on breast cancer DFS, OS, and TTR (hazard ratios, 1.00 and 0.97 for TPOAb-negative and TPOAb-positive status, and 1.00 and 1.27 for euthyroid and hypothyroid status).
Data source: An analysis of serum samples from 1,974 TACT trial participants.
Disclosures: This study was supported by a Tenovus Innovation Grant from Tenovus Cancer Care. TACT was funded by Cancer Research UK. Dr. Muller reported having no disclosures.
American Cancer Society recommends annual mammography starting at age 45
For asymptomatic women at average risk of breast cancer, the American Cancer Society recommends annual mammograms from age 45 until age 54, with a transition to biennial screening mammography starting at age 55, according to new guidelines published Oct. 20.
This is the first time the American Cancer Society (ACS) has updated its breast cancer screening guidelines since 2003. The new version makes several changes, including shifting the start of annual mammography from age 40 to 45 years, and increasing the suggested screening interval for postmenopausal women (JAMA. 2015;314[15]:1599-1614. doi:10.1001/jama.2015.12783).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For the first time, the guidelines address the question of when to stop routine mammography, recommending a halt to routine screening for women with a life expectancy under 10 years. The ACS guidelines also recommend against clinical breast examinations at any age.
These changes bring the ACS guidelines more into line with recommendations from the U.S. Preventive Services Task Force, Dr. Nancy L. Keating and Dr. Lydia E. Pace, both of Brigham and Women’s Hospital, Boston, wrote in an editorial accompanying the report.
The two organizations are now in agreement on most recommendations and emphasize that breast cancer screening decisions should be individualized to reflect a woman’s values and preferences, not just her underlying risk. Both sets of recommendations also give greater consideration to the potential harms of mammography: overdiagnosis and overtreatment of indolent breast cancers, as well as false-positive results, additional imaging studies, and unnecessary biopsies.
The ACS updated the guideline after noting that new evidence had accumulated from long-term follow-up of both randomized controlled trials and population-based screening programs. The guideline development group, which included four clinicians, two biostatisticians, two epidemiologists, an economist, and two patient representatives, based its revised recommendations on an independent systemic evidence review of the breast cancer screening literature conducted by the Duke University Evidence Synthesis Group, as well as an analysis screening interval and outcomes from the Breast Cancer Surveillance Consortium.
For asymptomatic women at average risk of developing breast cancer, the ACS guideline makes the following recommendations:
Begin routine annual screening mammography at age 45 years (rather than age 40). Assessing the burden of breast cancer by 5-year rather than 10-year age categories demonstrated that the risk/benefit profiles of women aged 40-44 years differed markedly from those of older women and no longer warranted a recommendation to begin screening at age 40, wrote Dr. Kevin C. Oeffinger of Memorial Sloan Kettering Cancer Center, New York, and his associates in the ACS Guideline Development Group.
However, the ACS encourages clinicians to discuss breast cancer screening with patients “around the age of 40 years.” Women who want to begin annual screening mammography before age 45, based on a clear consideration of the trade-offs, should be given that choice, they wrote.
“Some women will value the potential early detection benefit and will be willing to accept the risk of additional testing,” Dr. Oeffinger and his associates wrote. “Other women will choose to defer beginning screening, based on the relatively lower risk of breast cancer.”
Women aged 45-54 years should receive annual screening mammography and at age 55 women should transition to biennial screening. The relative benefits of annual screening decline after menopause and as women age, and the majority of women are postmenopausal at age 55. At the same time, the relative harms of annual screening increase at this age, because the chance of false-positive results rises as the number of screenings rises. However, women who prefer to continue annual screening after age 55 should be given that opportunity, according to the ACS guidelines.
Women should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer. Breast cancer incidence continues to increase with age until the age of 75-79 years, and mammography’s sensitivity and specificity improve with increasing age, so screening mammography in this age group will likely reduce breast cancer deaths. However, the authors noted that recent studies have raised concerns that older women with serious, or even terminal disorders, are still subjected to mammograms even though it will not increase their life expectancy or improve their quality of life.
“Health and life expectancy, not simply age, must be considered in screening decisions,” Dr. Oeffinger and his associates wrote.
Clinical breast examination is no longer recommended at any age. Historically, the ACS had advised periodic clinical breast exams for women younger than 40 and annual exams for women 40 and older. But there is no evidence that these exams, whether they are performed alone or in conjunction with mammography, enhance the detection of breast cancer, according to the guidelines.
Given that clinical breast exams are somewhat time consuming, “clinicians should use this time instead for ascertaining family history and counseling women regarding the importance of being alert to breast changes and the potential benefits, limitations, and harms of screening mammography,” the authors wrote.
“This new recommendation should not be interpreted to discount the potential value of clinical breast exams in low-resource settings where mammography screening may not be feasible,” they added.
In the accompanying editorial, Dr. Keating and Dr. Pace called this recommendation “a marked deviation from prior ACS guidelines and a stronger statement than that of the USPSTF,” which states only that the evidence is insufficient to recommend for or against clinical breast exams.
They noted that the majority of women who are diagnosed as having breast cancer “will do well regardless of whether their cancer was found by mammography.”
According to the most recent data, approximately 85% of women in their 40s and 50s who die of breast cancer would have died regardless of mammography screening. And even that 15% relative benefit translates to a very small absolute benefit: only 5 of 10,000 women in their 40s and 10 of 10,000 women in their 50s are likely to have a breast cancer death prevented by regular mammography, Dr. Keating and Dr. Pace wrote (JAMA 2015;314[15]:1569-71).
“It is important to remember and emphasize with average-risk women older than 40 years that there is no single right answer to the question ‘Should I have a mammogram?’ ” they wrote.
The American Cancer Society and the National Cancer Institute sponsored this work. Dr. Oeffinger reported having no relevant financial disclosures, and his associates reported ties to numerous industry sources.
After a little over a decade, the American Cancer Society has published guidelines for screening for the average-risk population. These guidelines provide some flexibility on the initiation of screening mammograms but strongly recommend starting at age 45. As this is an average-risk population, and the rate below this age is low and the rate of false positives is increased (due to dense breast tissue), this recommendation is based on good logic.
The question of frequency of screening is a little more challenging. The authors provide sound rationale for biennial screening after the age of 55. Unfortunately, patients are often hesitant to “skip a year” and this may be harder to enforce. Secondly, practitioners are often slow to adopt new practices as noted by changes in Pap test guidelines. Though this is a reasonable recommendation, it will take some education for patients to understand and will likely be less followed, at least in the beginning.
The final question of when to stop screening is fantastic. As mostly left-brain thinkers, we are often set on an actual age, completely disregarding the health of the patient. As the life expectancy of women in the United States is nearing 80 and many are surviving beyond that age with a high functioning status, consideration of this factor will allow for screening in women who can undergo management (if required) with favorable outcomes. Though practice changes take some time, it is likely that these recommendations will reduce unnecessary costs without impacting outcomes.
Given the substantial reduction in overall mortality, breast cancer screening is an integral part of women’s health. Providers in obstetrics and gynecology are often the primary source of education and the ordering team for breast cancer screening. Thus, it is critical for us to stay current on the recommendations for screening as well as the identification of high-risk women, allowing for well-informed decisions regarding individualized screening.
Dr. Ritu Salani is associate professor in gynecologic oncology at The Ohio State University, Columbus. Dr. Monica Hagan Vetter is a third-year resident in ob.gyn. at The Ohio State University. They reported having no financial disclosures.
After a little over a decade, the American Cancer Society has published guidelines for screening for the average-risk population. These guidelines provide some flexibility on the initiation of screening mammograms but strongly recommend starting at age 45. As this is an average-risk population, and the rate below this age is low and the rate of false positives is increased (due to dense breast tissue), this recommendation is based on good logic.
The question of frequency of screening is a little more challenging. The authors provide sound rationale for biennial screening after the age of 55. Unfortunately, patients are often hesitant to “skip a year” and this may be harder to enforce. Secondly, practitioners are often slow to adopt new practices as noted by changes in Pap test guidelines. Though this is a reasonable recommendation, it will take some education for patients to understand and will likely be less followed, at least in the beginning.
The final question of when to stop screening is fantastic. As mostly left-brain thinkers, we are often set on an actual age, completely disregarding the health of the patient. As the life expectancy of women in the United States is nearing 80 and many are surviving beyond that age with a high functioning status, consideration of this factor will allow for screening in women who can undergo management (if required) with favorable outcomes. Though practice changes take some time, it is likely that these recommendations will reduce unnecessary costs without impacting outcomes.
Given the substantial reduction in overall mortality, breast cancer screening is an integral part of women’s health. Providers in obstetrics and gynecology are often the primary source of education and the ordering team for breast cancer screening. Thus, it is critical for us to stay current on the recommendations for screening as well as the identification of high-risk women, allowing for well-informed decisions regarding individualized screening.
Dr. Ritu Salani is associate professor in gynecologic oncology at The Ohio State University, Columbus. Dr. Monica Hagan Vetter is a third-year resident in ob.gyn. at The Ohio State University. They reported having no financial disclosures.
After a little over a decade, the American Cancer Society has published guidelines for screening for the average-risk population. These guidelines provide some flexibility on the initiation of screening mammograms but strongly recommend starting at age 45. As this is an average-risk population, and the rate below this age is low and the rate of false positives is increased (due to dense breast tissue), this recommendation is based on good logic.
The question of frequency of screening is a little more challenging. The authors provide sound rationale for biennial screening after the age of 55. Unfortunately, patients are often hesitant to “skip a year” and this may be harder to enforce. Secondly, practitioners are often slow to adopt new practices as noted by changes in Pap test guidelines. Though this is a reasonable recommendation, it will take some education for patients to understand and will likely be less followed, at least in the beginning.
The final question of when to stop screening is fantastic. As mostly left-brain thinkers, we are often set on an actual age, completely disregarding the health of the patient. As the life expectancy of women in the United States is nearing 80 and many are surviving beyond that age with a high functioning status, consideration of this factor will allow for screening in women who can undergo management (if required) with favorable outcomes. Though practice changes take some time, it is likely that these recommendations will reduce unnecessary costs without impacting outcomes.
Given the substantial reduction in overall mortality, breast cancer screening is an integral part of women’s health. Providers in obstetrics and gynecology are often the primary source of education and the ordering team for breast cancer screening. Thus, it is critical for us to stay current on the recommendations for screening as well as the identification of high-risk women, allowing for well-informed decisions regarding individualized screening.
Dr. Ritu Salani is associate professor in gynecologic oncology at The Ohio State University, Columbus. Dr. Monica Hagan Vetter is a third-year resident in ob.gyn. at The Ohio State University. They reported having no financial disclosures.
For asymptomatic women at average risk of breast cancer, the American Cancer Society recommends annual mammograms from age 45 until age 54, with a transition to biennial screening mammography starting at age 55, according to new guidelines published Oct. 20.
This is the first time the American Cancer Society (ACS) has updated its breast cancer screening guidelines since 2003. The new version makes several changes, including shifting the start of annual mammography from age 40 to 45 years, and increasing the suggested screening interval for postmenopausal women (JAMA. 2015;314[15]:1599-1614. doi:10.1001/jama.2015.12783).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For the first time, the guidelines address the question of when to stop routine mammography, recommending a halt to routine screening for women with a life expectancy under 10 years. The ACS guidelines also recommend against clinical breast examinations at any age.
These changes bring the ACS guidelines more into line with recommendations from the U.S. Preventive Services Task Force, Dr. Nancy L. Keating and Dr. Lydia E. Pace, both of Brigham and Women’s Hospital, Boston, wrote in an editorial accompanying the report.
The two organizations are now in agreement on most recommendations and emphasize that breast cancer screening decisions should be individualized to reflect a woman’s values and preferences, not just her underlying risk. Both sets of recommendations also give greater consideration to the potential harms of mammography: overdiagnosis and overtreatment of indolent breast cancers, as well as false-positive results, additional imaging studies, and unnecessary biopsies.
The ACS updated the guideline after noting that new evidence had accumulated from long-term follow-up of both randomized controlled trials and population-based screening programs. The guideline development group, which included four clinicians, two biostatisticians, two epidemiologists, an economist, and two patient representatives, based its revised recommendations on an independent systemic evidence review of the breast cancer screening literature conducted by the Duke University Evidence Synthesis Group, as well as an analysis screening interval and outcomes from the Breast Cancer Surveillance Consortium.
For asymptomatic women at average risk of developing breast cancer, the ACS guideline makes the following recommendations:
Begin routine annual screening mammography at age 45 years (rather than age 40). Assessing the burden of breast cancer by 5-year rather than 10-year age categories demonstrated that the risk/benefit profiles of women aged 40-44 years differed markedly from those of older women and no longer warranted a recommendation to begin screening at age 40, wrote Dr. Kevin C. Oeffinger of Memorial Sloan Kettering Cancer Center, New York, and his associates in the ACS Guideline Development Group.
However, the ACS encourages clinicians to discuss breast cancer screening with patients “around the age of 40 years.” Women who want to begin annual screening mammography before age 45, based on a clear consideration of the trade-offs, should be given that choice, they wrote.
“Some women will value the potential early detection benefit and will be willing to accept the risk of additional testing,” Dr. Oeffinger and his associates wrote. “Other women will choose to defer beginning screening, based on the relatively lower risk of breast cancer.”
Women aged 45-54 years should receive annual screening mammography and at age 55 women should transition to biennial screening. The relative benefits of annual screening decline after menopause and as women age, and the majority of women are postmenopausal at age 55. At the same time, the relative harms of annual screening increase at this age, because the chance of false-positive results rises as the number of screenings rises. However, women who prefer to continue annual screening after age 55 should be given that opportunity, according to the ACS guidelines.
Women should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer. Breast cancer incidence continues to increase with age until the age of 75-79 years, and mammography’s sensitivity and specificity improve with increasing age, so screening mammography in this age group will likely reduce breast cancer deaths. However, the authors noted that recent studies have raised concerns that older women with serious, or even terminal disorders, are still subjected to mammograms even though it will not increase their life expectancy or improve their quality of life.
“Health and life expectancy, not simply age, must be considered in screening decisions,” Dr. Oeffinger and his associates wrote.
Clinical breast examination is no longer recommended at any age. Historically, the ACS had advised periodic clinical breast exams for women younger than 40 and annual exams for women 40 and older. But there is no evidence that these exams, whether they are performed alone or in conjunction with mammography, enhance the detection of breast cancer, according to the guidelines.
Given that clinical breast exams are somewhat time consuming, “clinicians should use this time instead for ascertaining family history and counseling women regarding the importance of being alert to breast changes and the potential benefits, limitations, and harms of screening mammography,” the authors wrote.
“This new recommendation should not be interpreted to discount the potential value of clinical breast exams in low-resource settings where mammography screening may not be feasible,” they added.
In the accompanying editorial, Dr. Keating and Dr. Pace called this recommendation “a marked deviation from prior ACS guidelines and a stronger statement than that of the USPSTF,” which states only that the evidence is insufficient to recommend for or against clinical breast exams.
They noted that the majority of women who are diagnosed as having breast cancer “will do well regardless of whether their cancer was found by mammography.”
According to the most recent data, approximately 85% of women in their 40s and 50s who die of breast cancer would have died regardless of mammography screening. And even that 15% relative benefit translates to a very small absolute benefit: only 5 of 10,000 women in their 40s and 10 of 10,000 women in their 50s are likely to have a breast cancer death prevented by regular mammography, Dr. Keating and Dr. Pace wrote (JAMA 2015;314[15]:1569-71).
“It is important to remember and emphasize with average-risk women older than 40 years that there is no single right answer to the question ‘Should I have a mammogram?’ ” they wrote.
The American Cancer Society and the National Cancer Institute sponsored this work. Dr. Oeffinger reported having no relevant financial disclosures, and his associates reported ties to numerous industry sources.
For asymptomatic women at average risk of breast cancer, the American Cancer Society recommends annual mammograms from age 45 until age 54, with a transition to biennial screening mammography starting at age 55, according to new guidelines published Oct. 20.
This is the first time the American Cancer Society (ACS) has updated its breast cancer screening guidelines since 2003. The new version makes several changes, including shifting the start of annual mammography from age 40 to 45 years, and increasing the suggested screening interval for postmenopausal women (JAMA. 2015;314[15]:1599-1614. doi:10.1001/jama.2015.12783).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For the first time, the guidelines address the question of when to stop routine mammography, recommending a halt to routine screening for women with a life expectancy under 10 years. The ACS guidelines also recommend against clinical breast examinations at any age.
These changes bring the ACS guidelines more into line with recommendations from the U.S. Preventive Services Task Force, Dr. Nancy L. Keating and Dr. Lydia E. Pace, both of Brigham and Women’s Hospital, Boston, wrote in an editorial accompanying the report.
The two organizations are now in agreement on most recommendations and emphasize that breast cancer screening decisions should be individualized to reflect a woman’s values and preferences, not just her underlying risk. Both sets of recommendations also give greater consideration to the potential harms of mammography: overdiagnosis and overtreatment of indolent breast cancers, as well as false-positive results, additional imaging studies, and unnecessary biopsies.
The ACS updated the guideline after noting that new evidence had accumulated from long-term follow-up of both randomized controlled trials and population-based screening programs. The guideline development group, which included four clinicians, two biostatisticians, two epidemiologists, an economist, and two patient representatives, based its revised recommendations on an independent systemic evidence review of the breast cancer screening literature conducted by the Duke University Evidence Synthesis Group, as well as an analysis screening interval and outcomes from the Breast Cancer Surveillance Consortium.
For asymptomatic women at average risk of developing breast cancer, the ACS guideline makes the following recommendations:
Begin routine annual screening mammography at age 45 years (rather than age 40). Assessing the burden of breast cancer by 5-year rather than 10-year age categories demonstrated that the risk/benefit profiles of women aged 40-44 years differed markedly from those of older women and no longer warranted a recommendation to begin screening at age 40, wrote Dr. Kevin C. Oeffinger of Memorial Sloan Kettering Cancer Center, New York, and his associates in the ACS Guideline Development Group.
However, the ACS encourages clinicians to discuss breast cancer screening with patients “around the age of 40 years.” Women who want to begin annual screening mammography before age 45, based on a clear consideration of the trade-offs, should be given that choice, they wrote.
“Some women will value the potential early detection benefit and will be willing to accept the risk of additional testing,” Dr. Oeffinger and his associates wrote. “Other women will choose to defer beginning screening, based on the relatively lower risk of breast cancer.”
Women aged 45-54 years should receive annual screening mammography and at age 55 women should transition to biennial screening. The relative benefits of annual screening decline after menopause and as women age, and the majority of women are postmenopausal at age 55. At the same time, the relative harms of annual screening increase at this age, because the chance of false-positive results rises as the number of screenings rises. However, women who prefer to continue annual screening after age 55 should be given that opportunity, according to the ACS guidelines.
Women should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer. Breast cancer incidence continues to increase with age until the age of 75-79 years, and mammography’s sensitivity and specificity improve with increasing age, so screening mammography in this age group will likely reduce breast cancer deaths. However, the authors noted that recent studies have raised concerns that older women with serious, or even terminal disorders, are still subjected to mammograms even though it will not increase their life expectancy or improve their quality of life.
“Health and life expectancy, not simply age, must be considered in screening decisions,” Dr. Oeffinger and his associates wrote.
Clinical breast examination is no longer recommended at any age. Historically, the ACS had advised periodic clinical breast exams for women younger than 40 and annual exams for women 40 and older. But there is no evidence that these exams, whether they are performed alone or in conjunction with mammography, enhance the detection of breast cancer, according to the guidelines.
Given that clinical breast exams are somewhat time consuming, “clinicians should use this time instead for ascertaining family history and counseling women regarding the importance of being alert to breast changes and the potential benefits, limitations, and harms of screening mammography,” the authors wrote.
“This new recommendation should not be interpreted to discount the potential value of clinical breast exams in low-resource settings where mammography screening may not be feasible,” they added.
In the accompanying editorial, Dr. Keating and Dr. Pace called this recommendation “a marked deviation from prior ACS guidelines and a stronger statement than that of the USPSTF,” which states only that the evidence is insufficient to recommend for or against clinical breast exams.
They noted that the majority of women who are diagnosed as having breast cancer “will do well regardless of whether their cancer was found by mammography.”
According to the most recent data, approximately 85% of women in their 40s and 50s who die of breast cancer would have died regardless of mammography screening. And even that 15% relative benefit translates to a very small absolute benefit: only 5 of 10,000 women in their 40s and 10 of 10,000 women in their 50s are likely to have a breast cancer death prevented by regular mammography, Dr. Keating and Dr. Pace wrote (JAMA 2015;314[15]:1569-71).
“It is important to remember and emphasize with average-risk women older than 40 years that there is no single right answer to the question ‘Should I have a mammogram?’ ” they wrote.
The American Cancer Society and the National Cancer Institute sponsored this work. Dr. Oeffinger reported having no relevant financial disclosures, and his associates reported ties to numerous industry sources.
FROM JAMA
Key clinical point: The American Cancer Society recommends annual mammograms for average-risk, asymptomatic women aged 45-54 years.
Major finding: The risk/benefit profiles of women aged 40-44 years differed markedly from those of older women and no longer warranted a recommendation to begin annual mammographic screening at age 40.
Data source: An update of the 2003 ACS guideline on breast cancer screening for women at average risk, based on a review of current evidence and an analysis of registry data for 15,440 women diagnosed during a 15-year period.
Disclosures: The American Cancer Society and the National Cancer Institute sponsored this work. Dr. Oeffinger reported having no relevant financial disclosures, and his associates reported ties to numerous industry sources.
Menopause status could guide breast cancer screening interval
Among postmenopausal women, breast cancers diagnosed following biennial mammography intervals are no more “unfavorable” than those diagnosed following annual intervals, according to a report published online Oct. 20 in JAMA Oncology.
“When considering recommendations regarding screening intervals, the potential benefit of diagnosing cancers at an earlier stage must be weighed against the increased potential for harms associated with more frequent screening, such as false-positive recalls and biopsies, which are 1.5 to 2 times higher in annual vs. biennial screeners,” wrote Diana L. Miglioretti, Ph.D., of the University of California, Davis, and her associates in the Breast Cancer Surveillance Consortium (BCSC).
The optimal frequency of mammographic screening remains controversial. The American Cancer Society commissioned the BCSC to analyze the most recent information on this issue as part of its effort to update the ACS guideline for breast cancer screening for women at average risk.
BCSC registries collect patient and clinical data from community radiology facilities across the country. For this analysis, Dr. Miglioretti and her colleagues focused on 15,440 women aged 40-85 years in these registries who were diagnosed as having breast cancer from 1996 to 2012. A total of 12,070 of the women underwent annual mammographic screening and 3,370 underwent biennial mammographic screening.
Among premenopausal women, those diagnosed after biennial mammograms were more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (relative risk, 1.11). In contrast, among postmenopausal women, those diagnosed after biennial mammograms were not more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (RR, 1.03), the investigators wrote (JAMA Oncol. 2015 Oct 20. doi: 10.1001/jamaoncology.2015.3084).
In an editorial accompanying this report, Dr. Wendy Y. Chen of Brigham and Women’s Hospital, Dana Farber Cancer Institute, and Harvard Medical School, all in Boston, wrote, “Although the authors do not endorse annual or biennial screening, they imply that biennial screening would be acceptable for postmenopausal women but inferior for premenopausal women.”
Most developed countries outside the United States – including the United Kingdom, Canada, and Australia – recommend screening every 2 or 3 years, Dr. Chen noted (JAMA Oncol. 2015 Oct 20 doi: 10.1001/jamaoncology.2015.3286).
This study and others clearly show that, with less frequent mammography, breast cancers will be larger and have a slightly more advanced stage when they are discovered, Dr. Chen wrote. But with a better understanding of tumor biology and improvements in targeted therapy, the best approach may not be simply trying to identify a smaller tumor, she added.
“Efforts should be focused on a better understanding of how screening interacts with tumor biology with a better understanding of the types of interval cancers and sojourn times and how these characteristics differ by age and/or menopausal status,” Dr. Chen wrote.
This study was supported by the American Cancer Society and the National Cancer Institute. Dr. Miglioretti reported having no relevant financial disclosures. One of the investigators reported being an unpaid advisor on General Electric Health Care’s breast medical advisory board.
Among postmenopausal women, breast cancers diagnosed following biennial mammography intervals are no more “unfavorable” than those diagnosed following annual intervals, according to a report published online Oct. 20 in JAMA Oncology.
“When considering recommendations regarding screening intervals, the potential benefit of diagnosing cancers at an earlier stage must be weighed against the increased potential for harms associated with more frequent screening, such as false-positive recalls and biopsies, which are 1.5 to 2 times higher in annual vs. biennial screeners,” wrote Diana L. Miglioretti, Ph.D., of the University of California, Davis, and her associates in the Breast Cancer Surveillance Consortium (BCSC).
The optimal frequency of mammographic screening remains controversial. The American Cancer Society commissioned the BCSC to analyze the most recent information on this issue as part of its effort to update the ACS guideline for breast cancer screening for women at average risk.
BCSC registries collect patient and clinical data from community radiology facilities across the country. For this analysis, Dr. Miglioretti and her colleagues focused on 15,440 women aged 40-85 years in these registries who were diagnosed as having breast cancer from 1996 to 2012. A total of 12,070 of the women underwent annual mammographic screening and 3,370 underwent biennial mammographic screening.
Among premenopausal women, those diagnosed after biennial mammograms were more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (relative risk, 1.11). In contrast, among postmenopausal women, those diagnosed after biennial mammograms were not more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (RR, 1.03), the investigators wrote (JAMA Oncol. 2015 Oct 20. doi: 10.1001/jamaoncology.2015.3084).
In an editorial accompanying this report, Dr. Wendy Y. Chen of Brigham and Women’s Hospital, Dana Farber Cancer Institute, and Harvard Medical School, all in Boston, wrote, “Although the authors do not endorse annual or biennial screening, they imply that biennial screening would be acceptable for postmenopausal women but inferior for premenopausal women.”
Most developed countries outside the United States – including the United Kingdom, Canada, and Australia – recommend screening every 2 or 3 years, Dr. Chen noted (JAMA Oncol. 2015 Oct 20 doi: 10.1001/jamaoncology.2015.3286).
This study and others clearly show that, with less frequent mammography, breast cancers will be larger and have a slightly more advanced stage when they are discovered, Dr. Chen wrote. But with a better understanding of tumor biology and improvements in targeted therapy, the best approach may not be simply trying to identify a smaller tumor, she added.
“Efforts should be focused on a better understanding of how screening interacts with tumor biology with a better understanding of the types of interval cancers and sojourn times and how these characteristics differ by age and/or menopausal status,” Dr. Chen wrote.
This study was supported by the American Cancer Society and the National Cancer Institute. Dr. Miglioretti reported having no relevant financial disclosures. One of the investigators reported being an unpaid advisor on General Electric Health Care’s breast medical advisory board.
Among postmenopausal women, breast cancers diagnosed following biennial mammography intervals are no more “unfavorable” than those diagnosed following annual intervals, according to a report published online Oct. 20 in JAMA Oncology.
“When considering recommendations regarding screening intervals, the potential benefit of diagnosing cancers at an earlier stage must be weighed against the increased potential for harms associated with more frequent screening, such as false-positive recalls and biopsies, which are 1.5 to 2 times higher in annual vs. biennial screeners,” wrote Diana L. Miglioretti, Ph.D., of the University of California, Davis, and her associates in the Breast Cancer Surveillance Consortium (BCSC).
The optimal frequency of mammographic screening remains controversial. The American Cancer Society commissioned the BCSC to analyze the most recent information on this issue as part of its effort to update the ACS guideline for breast cancer screening for women at average risk.
BCSC registries collect patient and clinical data from community radiology facilities across the country. For this analysis, Dr. Miglioretti and her colleagues focused on 15,440 women aged 40-85 years in these registries who were diagnosed as having breast cancer from 1996 to 2012. A total of 12,070 of the women underwent annual mammographic screening and 3,370 underwent biennial mammographic screening.
Among premenopausal women, those diagnosed after biennial mammograms were more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (relative risk, 1.11). In contrast, among postmenopausal women, those diagnosed after biennial mammograms were not more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (RR, 1.03), the investigators wrote (JAMA Oncol. 2015 Oct 20. doi: 10.1001/jamaoncology.2015.3084).
In an editorial accompanying this report, Dr. Wendy Y. Chen of Brigham and Women’s Hospital, Dana Farber Cancer Institute, and Harvard Medical School, all in Boston, wrote, “Although the authors do not endorse annual or biennial screening, they imply that biennial screening would be acceptable for postmenopausal women but inferior for premenopausal women.”
Most developed countries outside the United States – including the United Kingdom, Canada, and Australia – recommend screening every 2 or 3 years, Dr. Chen noted (JAMA Oncol. 2015 Oct 20 doi: 10.1001/jamaoncology.2015.3286).
This study and others clearly show that, with less frequent mammography, breast cancers will be larger and have a slightly more advanced stage when they are discovered, Dr. Chen wrote. But with a better understanding of tumor biology and improvements in targeted therapy, the best approach may not be simply trying to identify a smaller tumor, she added.
“Efforts should be focused on a better understanding of how screening interacts with tumor biology with a better understanding of the types of interval cancers and sojourn times and how these characteristics differ by age and/or menopausal status,” Dr. Chen wrote.
This study was supported by the American Cancer Society and the National Cancer Institute. Dr. Miglioretti reported having no relevant financial disclosures. One of the investigators reported being an unpaid advisor on General Electric Health Care’s breast medical advisory board.
FROM JAMA ONCOLOGY
Key clinical point: After menopause, breast cancers diagnosed after 2-year mammography intervals are no more unfavorable than those arising after 1-year intervals.
Major finding: Among postmenopausal women, those diagnosed after biennial mammograms were not more likely to have tumors with unfavorable prognostic characteristics than were those diagnosed after annual mammograms (relative risk, 1.03).
Data source: A prospective cohort study involving 15,440 women diagnosed with breast cancer from 1996 to 2012.
Disclosures: This study was supported by the American Cancer Society and the National Cancer Institute. Dr. Miglioretti reported having no relevant financial disclosures. One of the investigators reported being an unpaid advisor on General Electric Health Care’s breast medical advisory board.
Why I will continue to perform clinical breast exams
When practice guidelines differ from each other, it is up to individual providers to make the choice that is best for their patients, and we once again find ourselves in this position – this time, regarding mammography recommendations.
Specifically, the American Cancer Society (ACS) is now recommending annual mammograms beginning at 45 years, with biennial screening available after 55 years. ACS also does not recommend clinical breast examinations.
Meanwhile, the American College of Obstetricians and Gynecologists (ACOG) stands by its previous recommendations for screening to begin at age 40 years and be conducted every 1-2 years and then annually after age 50. Moreover, ACOG continues to encourage clinical breast exams every year for women over age 19.
That these two respected organizations diverge in their recommendations may be confusing, but it reflects the fact that medical information is constantly evolving and that different groups may weigh evidence in different ways.
So, what is a gynecologist to do?
Increasingly, ob.gyns. are our patients’ primary well woman–care provider. It is incumbent on us to give the women we treat the screening and counseling that they need to live healthy lives and to make sure that part of the shared decision-making includes not just practice guidelines, but also our own clinical experiences.
In my practice, I have always included clinical breast exams in my patients’ visits. Without question, the moments that I have spent performing this relatively noninvasive service have paid dividends, as I have found enough evidence of abnormal tissue that I have recommended mammograms to women who would not have yet received them routinely. Those who ultimately received cancer diagnoses were able to receive treatment early, improving their survival.
Similarly, I have seen patients younger than 45 years – women with no apparent elevated risk – benefit from annual mammograms. We know that early diagnosis is key to beating breast cancer, and for these women, starting mammography screening at age 45 would have delayed their life-saving interventions.
I am sure that countless women are celebrating the new ACS guidelines, as they anticipate avoiding the discomfort associated with mammograms. But as I reflect on my patients’ experiences, I plan to continue providing clinical exams and recommending regular mammograms. In fact, I have worked with patient advocates through my hospital’s Breast Health Ambassador Program to mitigate women’s fears about mammograms and to encourage them to regular testing.
There is a one in eight chance that a woman will be diagnosed with breast cancer in her lifetime. We cannot let these women down by postponing their chance at early detection.
Dr. Rabin is professor of obstetrics and gynecology at Hofstra University in Hempstead, N.Y., and co-chief of the division of ambulatory care and women’s health prenatal care assistance program in the North Shore-LIJ Health System. She has been a practicing ob.gyn. and urogynecologist for more than 30 years. She reported having no relevant financial disclosures.
When practice guidelines differ from each other, it is up to individual providers to make the choice that is best for their patients, and we once again find ourselves in this position – this time, regarding mammography recommendations.
Specifically, the American Cancer Society (ACS) is now recommending annual mammograms beginning at 45 years, with biennial screening available after 55 years. ACS also does not recommend clinical breast examinations.
Meanwhile, the American College of Obstetricians and Gynecologists (ACOG) stands by its previous recommendations for screening to begin at age 40 years and be conducted every 1-2 years and then annually after age 50. Moreover, ACOG continues to encourage clinical breast exams every year for women over age 19.
That these two respected organizations diverge in their recommendations may be confusing, but it reflects the fact that medical information is constantly evolving and that different groups may weigh evidence in different ways.
So, what is a gynecologist to do?
Increasingly, ob.gyns. are our patients’ primary well woman–care provider. It is incumbent on us to give the women we treat the screening and counseling that they need to live healthy lives and to make sure that part of the shared decision-making includes not just practice guidelines, but also our own clinical experiences.
In my practice, I have always included clinical breast exams in my patients’ visits. Without question, the moments that I have spent performing this relatively noninvasive service have paid dividends, as I have found enough evidence of abnormal tissue that I have recommended mammograms to women who would not have yet received them routinely. Those who ultimately received cancer diagnoses were able to receive treatment early, improving their survival.
Similarly, I have seen patients younger than 45 years – women with no apparent elevated risk – benefit from annual mammograms. We know that early diagnosis is key to beating breast cancer, and for these women, starting mammography screening at age 45 would have delayed their life-saving interventions.
I am sure that countless women are celebrating the new ACS guidelines, as they anticipate avoiding the discomfort associated with mammograms. But as I reflect on my patients’ experiences, I plan to continue providing clinical exams and recommending regular mammograms. In fact, I have worked with patient advocates through my hospital’s Breast Health Ambassador Program to mitigate women’s fears about mammograms and to encourage them to regular testing.
There is a one in eight chance that a woman will be diagnosed with breast cancer in her lifetime. We cannot let these women down by postponing their chance at early detection.
Dr. Rabin is professor of obstetrics and gynecology at Hofstra University in Hempstead, N.Y., and co-chief of the division of ambulatory care and women’s health prenatal care assistance program in the North Shore-LIJ Health System. She has been a practicing ob.gyn. and urogynecologist for more than 30 years. She reported having no relevant financial disclosures.
When practice guidelines differ from each other, it is up to individual providers to make the choice that is best for their patients, and we once again find ourselves in this position – this time, regarding mammography recommendations.
Specifically, the American Cancer Society (ACS) is now recommending annual mammograms beginning at 45 years, with biennial screening available after 55 years. ACS also does not recommend clinical breast examinations.
Meanwhile, the American College of Obstetricians and Gynecologists (ACOG) stands by its previous recommendations for screening to begin at age 40 years and be conducted every 1-2 years and then annually after age 50. Moreover, ACOG continues to encourage clinical breast exams every year for women over age 19.
That these two respected organizations diverge in their recommendations may be confusing, but it reflects the fact that medical information is constantly evolving and that different groups may weigh evidence in different ways.
So, what is a gynecologist to do?
Increasingly, ob.gyns. are our patients’ primary well woman–care provider. It is incumbent on us to give the women we treat the screening and counseling that they need to live healthy lives and to make sure that part of the shared decision-making includes not just practice guidelines, but also our own clinical experiences.
In my practice, I have always included clinical breast exams in my patients’ visits. Without question, the moments that I have spent performing this relatively noninvasive service have paid dividends, as I have found enough evidence of abnormal tissue that I have recommended mammograms to women who would not have yet received them routinely. Those who ultimately received cancer diagnoses were able to receive treatment early, improving their survival.
Similarly, I have seen patients younger than 45 years – women with no apparent elevated risk – benefit from annual mammograms. We know that early diagnosis is key to beating breast cancer, and for these women, starting mammography screening at age 45 would have delayed their life-saving interventions.
I am sure that countless women are celebrating the new ACS guidelines, as they anticipate avoiding the discomfort associated with mammograms. But as I reflect on my patients’ experiences, I plan to continue providing clinical exams and recommending regular mammograms. In fact, I have worked with patient advocates through my hospital’s Breast Health Ambassador Program to mitigate women’s fears about mammograms and to encourage them to regular testing.
There is a one in eight chance that a woman will be diagnosed with breast cancer in her lifetime. We cannot let these women down by postponing their chance at early detection.
Dr. Rabin is professor of obstetrics and gynecology at Hofstra University in Hempstead, N.Y., and co-chief of the division of ambulatory care and women’s health prenatal care assistance program in the North Shore-LIJ Health System. She has been a practicing ob.gyn. and urogynecologist for more than 30 years. She reported having no relevant financial disclosures.
Prolonged zoledronic acid-induced hypocalcemia in hypercalcemia of malignancy
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Delayed diagnosis tops breast cancer malpractice claims
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
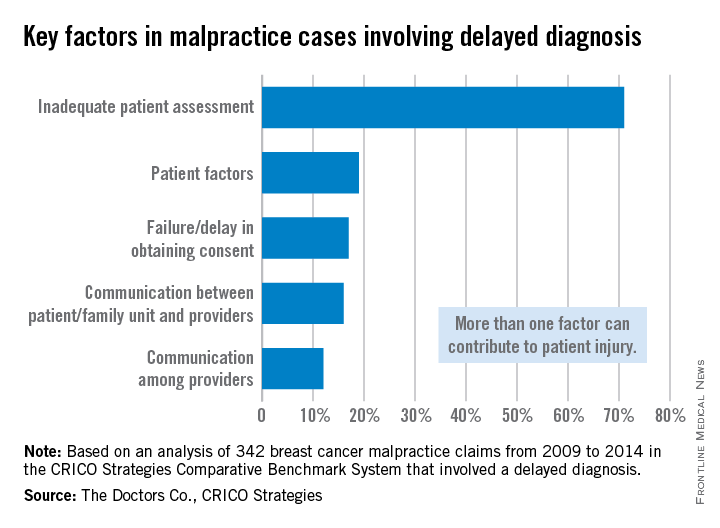
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
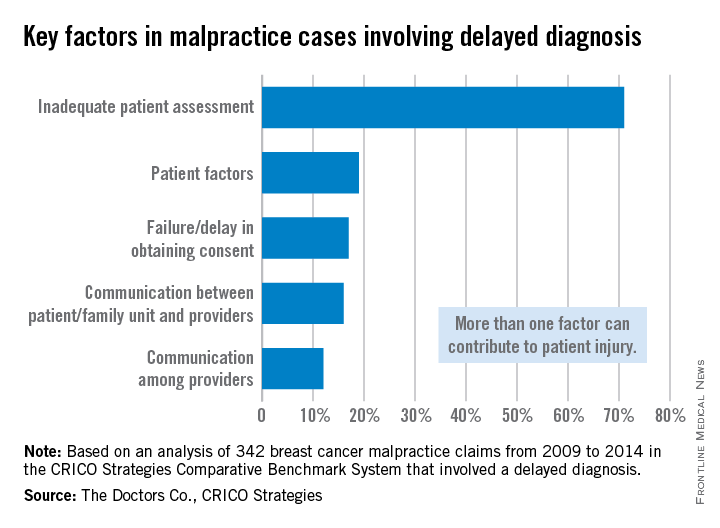
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
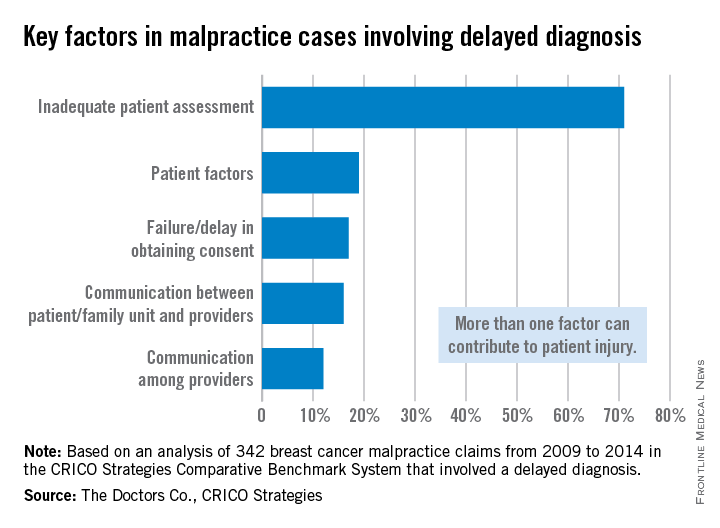
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med