User login
Balancing clinical and supportive care at every step of the disease continuum
It seems it was just yesterday that we did our first “mutation analysis” to help guide us in our treatment of patients with a drug that was more likely to work than not. Of course, I am referring to estrogen-receptor/progesterone receptor (ER/PR) blocking therapy, and “yesterday” actually goes all the way back to the 1970s! When tamoxifen was first given to unselected metastatic breast cancer patients, the response rate was low, but when the study population was “enriched” with breast cancer patients who were ER/ PR-positive, the response rates improved and the outcomes were more favorable. So began the era of tumor markers and enriching patient populations, and the process now referred to as mutation analysis, which is becoming more broadly applicable to other tumors as well.
Click on the PDF icon at the top of this introduction to read the full article.
It seems it was just yesterday that we did our first “mutation analysis” to help guide us in our treatment of patients with a drug that was more likely to work than not. Of course, I am referring to estrogen-receptor/progesterone receptor (ER/PR) blocking therapy, and “yesterday” actually goes all the way back to the 1970s! When tamoxifen was first given to unselected metastatic breast cancer patients, the response rate was low, but when the study population was “enriched” with breast cancer patients who were ER/ PR-positive, the response rates improved and the outcomes were more favorable. So began the era of tumor markers and enriching patient populations, and the process now referred to as mutation analysis, which is becoming more broadly applicable to other tumors as well.
Click on the PDF icon at the top of this introduction to read the full article.
It seems it was just yesterday that we did our first “mutation analysis” to help guide us in our treatment of patients with a drug that was more likely to work than not. Of course, I am referring to estrogen-receptor/progesterone receptor (ER/PR) blocking therapy, and “yesterday” actually goes all the way back to the 1970s! When tamoxifen was first given to unselected metastatic breast cancer patients, the response rate was low, but when the study population was “enriched” with breast cancer patients who were ER/ PR-positive, the response rates improved and the outcomes were more favorable. So began the era of tumor markers and enriching patient populations, and the process now referred to as mutation analysis, which is becoming more broadly applicable to other tumors as well.
Click on the PDF icon at the top of this introduction to read the full article.
Pan-AKT inhibitor shrinks tumors in patients with AKT1 mutation
BOSTON – A novel pan-AKT inhibitor was associated in a phase 1 trial with tumor shrinkage in a large proportion of patients with solid tumors bearing a mutation in AKT1.
The investigational compound, labeled AZD5363, targets the AKT1 E17K mutation, which occurs in approximately 0.5% to 4% of many different types of solid tumors. In a phase I trial, 33 of 41 assessable patients with tumors bearing the mutation had regression of tumors, reported Dr. David M. Hyman, acting director of experimental therapeutics at Memorial Sloan Kettering Cancer Center in New York.
“We believe this is the first clinical data suggesting that the AKT1 E17K mutations are targetable driver mutations in solid tumors,” he said at a briefing at the AACR/NCI/EORTC International Conference on Molecular Targets and Cancer Therapeutics.
Mutations in the PI3K/AKT/mTOR pathway are frequently found in human cancers, and dysregulation of the pathway has been shown to drive tumor growth and survival of malignant cells.
“Although this pathway is among the most commonly activated in all human cancer, it is rarely activated by somatic mutation of AKT itself,” Dr. Hyman said. “When you see AKT mutations, they are almost always of a single allele at the 17 amino acid position, which is the E17K mutation. This is a mutation that has been extensively functionally classified, and behaves as a classic driver oncogene.”
The E17K mutation occurs in approximately 4% of breast cancers, 2% of bladder cancers, 1.5% of colorectal tumors, 1% each of cervical, ovarian, and prostate cancers, and 0.5% of lung adenocarcinomas.
AZD5363 is a catalytic inhibitor of all AKT isoforms 1, 2, and 3. In preclinical studies, it has been shown to inhibit tumor cell proliferation in vitro, and tumor growth in vivo in tumor xenograft models.
Dr. Hyman and colleagues reported on early results from one part of a four-part, phase I study of AZD5363 in adults with advanced solid tumors. Part D of the ongoing study focuses on patients with tumors bearing AKT1 mutations.
At present, 45 patients with E17K mutations have been treated with the agent, including 21 with estrogen receptor (ER)-positive breast cancer, four with triple-negative breast cancer, 14 with gynecological cancers, and eight with other tumor types.
As noted, of 41 patients with sufficient data for assessment, 33 had some degree of tumor regression, and of this group 12 met RECIST (Response Evaluation Criteria in Solid Tumors) parameters for partial responses. Among patients assessable for response, 14 of 18 with ER-positive breast cancer had lesion shrinkage, and five of these patients had partial responses (3 confirmed and 2 unconfirmed).
Among patients with gynecological tumors, 9 of 11 had shrinkage of their target lesion, including 3 with confirmed partial responses. Two of these patients are still on study, with the longest follow-up at the time of data cutoff of 39.2 months
Among patients with 12 other tumor types (apocrine anal, triple-negative breast cancer, colon, lung, prostate, squamous anal, thyroid) 10 patients had demonstrated target lesion shrinkage, one had a confirmed partial response that is ongoing, and two had unconfirmed partial response, one of which is ongoing.
The investigators also used cell-free DNA (cfDNA) analysis to evaluate efficacy of AZD5363 during treatment, and found that declines in AKT1 cfDNA allele fractions were transient among non-responders, whereas declines persisting for 21 days or more correlated with both durable tumor regression and RECIST response (P = .0049).
Dr. Hyman noted that there were also preclinical signs that AZD5363 could lead to reactivation of ER signaling.
“It became a natural question to ask whether patients did better with a combination of ER-directed therapy and AKT-directed therapy,” he said.
To answer this question, the investigators offered sequential therapy to patients with ER-positive breast cancer who had previously had resistance to the ER degrader fulvestrant and who had progressed on AZD5363 monotherapy. Two patients were offered crossover to AZD5363 with fulvestrant, regardless of prior hormonal therapy.
One of the patients had disease progression while on the combination. The second patient, who had received 10 prior lines of therapy and had disease progression before starting on the combination at 120 days on treatment, had significant shrinkage of her breast lesion 6 weeks after starting on the combination, and liver lesions that had previously enhanced on imaging are no longer enhancing, and her cfDNA allele fractions have declined. She remains on the combination after more than 160 days.
“This was very convincing evidence to us of synergy between these two compounds,” he said.
Dr. Jean-Charles Soria, from the Institut Gustave Roussy, Villejuif, France, who moderated the briefing, commented that “although this [mutation] is a rare situation, in the range of 2% to 3%, it’s certainly important, because 2% to 3% of breast cancer patients is a significant number, so this drug has legs,” he said.
The question yet to be settled, however, is the true duration of response, he added.
The study is sponsored by AstraZeneca. Dr. Hyman disclosed consulting for Atara Biotherapeutics. Dr. Soria reported having no disclosures.
BOSTON – A novel pan-AKT inhibitor was associated in a phase 1 trial with tumor shrinkage in a large proportion of patients with solid tumors bearing a mutation in AKT1.
The investigational compound, labeled AZD5363, targets the AKT1 E17K mutation, which occurs in approximately 0.5% to 4% of many different types of solid tumors. In a phase I trial, 33 of 41 assessable patients with tumors bearing the mutation had regression of tumors, reported Dr. David M. Hyman, acting director of experimental therapeutics at Memorial Sloan Kettering Cancer Center in New York.
“We believe this is the first clinical data suggesting that the AKT1 E17K mutations are targetable driver mutations in solid tumors,” he said at a briefing at the AACR/NCI/EORTC International Conference on Molecular Targets and Cancer Therapeutics.
Mutations in the PI3K/AKT/mTOR pathway are frequently found in human cancers, and dysregulation of the pathway has been shown to drive tumor growth and survival of malignant cells.
“Although this pathway is among the most commonly activated in all human cancer, it is rarely activated by somatic mutation of AKT itself,” Dr. Hyman said. “When you see AKT mutations, they are almost always of a single allele at the 17 amino acid position, which is the E17K mutation. This is a mutation that has been extensively functionally classified, and behaves as a classic driver oncogene.”
The E17K mutation occurs in approximately 4% of breast cancers, 2% of bladder cancers, 1.5% of colorectal tumors, 1% each of cervical, ovarian, and prostate cancers, and 0.5% of lung adenocarcinomas.
AZD5363 is a catalytic inhibitor of all AKT isoforms 1, 2, and 3. In preclinical studies, it has been shown to inhibit tumor cell proliferation in vitro, and tumor growth in vivo in tumor xenograft models.
Dr. Hyman and colleagues reported on early results from one part of a four-part, phase I study of AZD5363 in adults with advanced solid tumors. Part D of the ongoing study focuses on patients with tumors bearing AKT1 mutations.
At present, 45 patients with E17K mutations have been treated with the agent, including 21 with estrogen receptor (ER)-positive breast cancer, four with triple-negative breast cancer, 14 with gynecological cancers, and eight with other tumor types.
As noted, of 41 patients with sufficient data for assessment, 33 had some degree of tumor regression, and of this group 12 met RECIST (Response Evaluation Criteria in Solid Tumors) parameters for partial responses. Among patients assessable for response, 14 of 18 with ER-positive breast cancer had lesion shrinkage, and five of these patients had partial responses (3 confirmed and 2 unconfirmed).
Among patients with gynecological tumors, 9 of 11 had shrinkage of their target lesion, including 3 with confirmed partial responses. Two of these patients are still on study, with the longest follow-up at the time of data cutoff of 39.2 months
Among patients with 12 other tumor types (apocrine anal, triple-negative breast cancer, colon, lung, prostate, squamous anal, thyroid) 10 patients had demonstrated target lesion shrinkage, one had a confirmed partial response that is ongoing, and two had unconfirmed partial response, one of which is ongoing.
The investigators also used cell-free DNA (cfDNA) analysis to evaluate efficacy of AZD5363 during treatment, and found that declines in AKT1 cfDNA allele fractions were transient among non-responders, whereas declines persisting for 21 days or more correlated with both durable tumor regression and RECIST response (P = .0049).
Dr. Hyman noted that there were also preclinical signs that AZD5363 could lead to reactivation of ER signaling.
“It became a natural question to ask whether patients did better with a combination of ER-directed therapy and AKT-directed therapy,” he said.
To answer this question, the investigators offered sequential therapy to patients with ER-positive breast cancer who had previously had resistance to the ER degrader fulvestrant and who had progressed on AZD5363 monotherapy. Two patients were offered crossover to AZD5363 with fulvestrant, regardless of prior hormonal therapy.
One of the patients had disease progression while on the combination. The second patient, who had received 10 prior lines of therapy and had disease progression before starting on the combination at 120 days on treatment, had significant shrinkage of her breast lesion 6 weeks after starting on the combination, and liver lesions that had previously enhanced on imaging are no longer enhancing, and her cfDNA allele fractions have declined. She remains on the combination after more than 160 days.
“This was very convincing evidence to us of synergy between these two compounds,” he said.
Dr. Jean-Charles Soria, from the Institut Gustave Roussy, Villejuif, France, who moderated the briefing, commented that “although this [mutation] is a rare situation, in the range of 2% to 3%, it’s certainly important, because 2% to 3% of breast cancer patients is a significant number, so this drug has legs,” he said.
The question yet to be settled, however, is the true duration of response, he added.
The study is sponsored by AstraZeneca. Dr. Hyman disclosed consulting for Atara Biotherapeutics. Dr. Soria reported having no disclosures.
BOSTON – A novel pan-AKT inhibitor was associated in a phase 1 trial with tumor shrinkage in a large proportion of patients with solid tumors bearing a mutation in AKT1.
The investigational compound, labeled AZD5363, targets the AKT1 E17K mutation, which occurs in approximately 0.5% to 4% of many different types of solid tumors. In a phase I trial, 33 of 41 assessable patients with tumors bearing the mutation had regression of tumors, reported Dr. David M. Hyman, acting director of experimental therapeutics at Memorial Sloan Kettering Cancer Center in New York.
“We believe this is the first clinical data suggesting that the AKT1 E17K mutations are targetable driver mutations in solid tumors,” he said at a briefing at the AACR/NCI/EORTC International Conference on Molecular Targets and Cancer Therapeutics.
Mutations in the PI3K/AKT/mTOR pathway are frequently found in human cancers, and dysregulation of the pathway has been shown to drive tumor growth and survival of malignant cells.
“Although this pathway is among the most commonly activated in all human cancer, it is rarely activated by somatic mutation of AKT itself,” Dr. Hyman said. “When you see AKT mutations, they are almost always of a single allele at the 17 amino acid position, which is the E17K mutation. This is a mutation that has been extensively functionally classified, and behaves as a classic driver oncogene.”
The E17K mutation occurs in approximately 4% of breast cancers, 2% of bladder cancers, 1.5% of colorectal tumors, 1% each of cervical, ovarian, and prostate cancers, and 0.5% of lung adenocarcinomas.
AZD5363 is a catalytic inhibitor of all AKT isoforms 1, 2, and 3. In preclinical studies, it has been shown to inhibit tumor cell proliferation in vitro, and tumor growth in vivo in tumor xenograft models.
Dr. Hyman and colleagues reported on early results from one part of a four-part, phase I study of AZD5363 in adults with advanced solid tumors. Part D of the ongoing study focuses on patients with tumors bearing AKT1 mutations.
At present, 45 patients with E17K mutations have been treated with the agent, including 21 with estrogen receptor (ER)-positive breast cancer, four with triple-negative breast cancer, 14 with gynecological cancers, and eight with other tumor types.
As noted, of 41 patients with sufficient data for assessment, 33 had some degree of tumor regression, and of this group 12 met RECIST (Response Evaluation Criteria in Solid Tumors) parameters for partial responses. Among patients assessable for response, 14 of 18 with ER-positive breast cancer had lesion shrinkage, and five of these patients had partial responses (3 confirmed and 2 unconfirmed).
Among patients with gynecological tumors, 9 of 11 had shrinkage of their target lesion, including 3 with confirmed partial responses. Two of these patients are still on study, with the longest follow-up at the time of data cutoff of 39.2 months
Among patients with 12 other tumor types (apocrine anal, triple-negative breast cancer, colon, lung, prostate, squamous anal, thyroid) 10 patients had demonstrated target lesion shrinkage, one had a confirmed partial response that is ongoing, and two had unconfirmed partial response, one of which is ongoing.
The investigators also used cell-free DNA (cfDNA) analysis to evaluate efficacy of AZD5363 during treatment, and found that declines in AKT1 cfDNA allele fractions were transient among non-responders, whereas declines persisting for 21 days or more correlated with both durable tumor regression and RECIST response (P = .0049).
Dr. Hyman noted that there were also preclinical signs that AZD5363 could lead to reactivation of ER signaling.
“It became a natural question to ask whether patients did better with a combination of ER-directed therapy and AKT-directed therapy,” he said.
To answer this question, the investigators offered sequential therapy to patients with ER-positive breast cancer who had previously had resistance to the ER degrader fulvestrant and who had progressed on AZD5363 monotherapy. Two patients were offered crossover to AZD5363 with fulvestrant, regardless of prior hormonal therapy.
One of the patients had disease progression while on the combination. The second patient, who had received 10 prior lines of therapy and had disease progression before starting on the combination at 120 days on treatment, had significant shrinkage of her breast lesion 6 weeks after starting on the combination, and liver lesions that had previously enhanced on imaging are no longer enhancing, and her cfDNA allele fractions have declined. She remains on the combination after more than 160 days.
“This was very convincing evidence to us of synergy between these two compounds,” he said.
Dr. Jean-Charles Soria, from the Institut Gustave Roussy, Villejuif, France, who moderated the briefing, commented that “although this [mutation] is a rare situation, in the range of 2% to 3%, it’s certainly important, because 2% to 3% of breast cancer patients is a significant number, so this drug has legs,” he said.
The question yet to be settled, however, is the true duration of response, he added.
The study is sponsored by AstraZeneca. Dr. Hyman disclosed consulting for Atara Biotherapeutics. Dr. Soria reported having no disclosures.
Key clinical point: A novel pan-AKT inhibitor shrinks tumors in patients harboring a mutation in AKT1.
Major finding: Among patients assessable for response, 33 of 41 had tumor regression on AZD5363 monotherapy.
Data source: Phase I study in 45 patients with solid tumors carrying the AKT1 E17K mutation.
Disclosures: The study is sponsored by AstraZeneca. Dr. Hyman disclosed consulting for Atara Biotherapeutics. Dr. Soria reported having no disclosures.
AHA: Candesartan protects against cardiotoxicity in breast cancer patients in PRADA
ORLANDO – Concomitant treatment with candesartan protects against the early decline in left ventricular ejection fraction associated with adjunct therapy for early breast cancer.
That was the key finding in the PRADA trial (PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy), the largest study to date looking at prevention of cardiac dysfunction in a breast cancer population.
Another important finding in PRADA was that unlike the angiotensin receptor blocker candesartan (Atacand), metoprolol, a beta blocker, didn’t prevent the early drop in LVEF commonly seen in breast cancer patients treated with anthracyclines and trastuzumab (Herceptin), even though both classes of heart medications are cornerstones of the treatment of ischemic and hypertensive cardiomyopathy, Dr. Geeta Gulati reported at the American Heart Association scientific sessions.
Although the cardiotoxicity of certain breast cancer treatments is widely recognized and has spawned the emerging field of cardio-oncology, the literature in this area is weak. Indeed, a recent meta-analysis identified only four published randomized studies evaluating the possible cardioprotective role for beta blockers and angiotensin antagonists in patients undergoing anthracycline-based chemotherapy (Postgrad Med J doi:10.1136/ postgradmedj-2015-133535). None of the studies was double-blind, all relied upon echocardiographic assessment of changes in LVEF rather than gold-standard cardiac MRI, and the study sizes were small -- just 18-45 breast cancer patients.
Most problematic of all, the studies employed a variety of different definitions of cardiotoxicity, noted Dr. Gulati of Akershus University Hospital in Lorenskog, Norway.
In contrast, PRADA was a double-blind, placebo-controlled, 2 by 2 factorial design, single-center trial, which included 120 patients with early breast cancer. Participants were randomized to candesartan at a starting dose of 8 mg and target dose of 32 mg/day, metoprolol starting at 25 mg with a target of 100 mg/day, or placebo after breast cancer surgery but before the start of anthracycline-containing chemotherapy.
The primary endpoint was change in LVEF from baseline to completion of adjuvant therapy, a period as short as 10 weeks and as long as 64 weeks depending upon whether a woman also underwent courses of trastuzumab, taxanes, and/or radiation therapy.
The overall decline in LVEF was 2.6% in the placebo group and 0.6% in the candesartan group, a significant difference. Metoprolol didn’t put a dent in the LVEF decline.
“Observational studies show early reduction in LVEF is associated with increased risk of developing heart failure later. So if a sustained, long-term effect of angiotensin inhibition can be confirmed in larger multicenter trials, preventive therapy may be indicated as standard care for breast cancer patients,” Dr. Gulati said.
Discussant Dr. Bonnie Ky of the University of Pennsylvania, Philadelphia, called PRADA an important study that moves the field of cardio-oncology forward, yet it’s also a trial that raises more questions than it answers.
PRADA certainly addresses a major problem: “The incidence of heart failure and cardiomyopathy increases over time in breast cancer patients exposed to anthracyclines and trastuzumab. Because patients are living longer because of cancer chemotherapy, their risk of dying of cardiovascular disease actually exceeds that of recurrent cancer in the long term,” she observed.
The study has three major limitations that prevent its findings being implemented in routine clinical practice at this time, Dr. Ky said. One is its relatively small size, even though it’s far bigger than any previous study. Another limitation is that this was an extremely low-cardiovascular-risk patient cohort: the baseline prevalence of diabetes was only 1.5%, fewer than 7% of patients had hypertension, and the baseline LVEF was 63%. That may be why no one developed a substantial decrement in LVEF or actual heart failure.
And since the incidence of cardiomyopathy following breast cancer therapy is known to climb over time, reaching a cumulative 12% at 6 years followup in trastuzumab-treated patients and 20% in those who receive both anthracyclines and trastuzumab (J Natl Cancer Inst. 2012 Sep 5;104(17):1293-305), the lack of extended followup time in PRADA is a significant shortcoming, she added.
The important questions raised by PRADA, Dr. Ky continued, include whether carvedilol or another beta blocker would have generated a positive result where metoprolol failed. Also, should the target population for prevention of cardiotoxicity be more narrowly focused on those at higher baseline cardiovascular risk? And bearing in mind that change in LVEF is a surrogate endpoint, what might be a more clinically meaningful and valid outcome measure? What’s the effect of carvedilol and other cardioprotective medications on cardiac biomarkers in breast cancer patients? And the most important questions of all, she said: What would be the effects of longer followup time and extended therapy?
“This study highlights for us in the field of cardio-oncology the critical need to develop a robust consensus definition of cardiotoxicity and a methodology to identify high cardiovascular risk patients,” she concluded.
PRADA was funded primarily by the University of Oslo and the Norwegian Cancer Society. Dr. Gulati reported having no financial conflicts of interest. Dr. Ky reported receiving a research grant from Pfizer and serving as a consultant to Bristol Myers Squibb.
ORLANDO – Concomitant treatment with candesartan protects against the early decline in left ventricular ejection fraction associated with adjunct therapy for early breast cancer.
That was the key finding in the PRADA trial (PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy), the largest study to date looking at prevention of cardiac dysfunction in a breast cancer population.
Another important finding in PRADA was that unlike the angiotensin receptor blocker candesartan (Atacand), metoprolol, a beta blocker, didn’t prevent the early drop in LVEF commonly seen in breast cancer patients treated with anthracyclines and trastuzumab (Herceptin), even though both classes of heart medications are cornerstones of the treatment of ischemic and hypertensive cardiomyopathy, Dr. Geeta Gulati reported at the American Heart Association scientific sessions.
Although the cardiotoxicity of certain breast cancer treatments is widely recognized and has spawned the emerging field of cardio-oncology, the literature in this area is weak. Indeed, a recent meta-analysis identified only four published randomized studies evaluating the possible cardioprotective role for beta blockers and angiotensin antagonists in patients undergoing anthracycline-based chemotherapy (Postgrad Med J doi:10.1136/ postgradmedj-2015-133535). None of the studies was double-blind, all relied upon echocardiographic assessment of changes in LVEF rather than gold-standard cardiac MRI, and the study sizes were small -- just 18-45 breast cancer patients.
Most problematic of all, the studies employed a variety of different definitions of cardiotoxicity, noted Dr. Gulati of Akershus University Hospital in Lorenskog, Norway.
In contrast, PRADA was a double-blind, placebo-controlled, 2 by 2 factorial design, single-center trial, which included 120 patients with early breast cancer. Participants were randomized to candesartan at a starting dose of 8 mg and target dose of 32 mg/day, metoprolol starting at 25 mg with a target of 100 mg/day, or placebo after breast cancer surgery but before the start of anthracycline-containing chemotherapy.
The primary endpoint was change in LVEF from baseline to completion of adjuvant therapy, a period as short as 10 weeks and as long as 64 weeks depending upon whether a woman also underwent courses of trastuzumab, taxanes, and/or radiation therapy.
The overall decline in LVEF was 2.6% in the placebo group and 0.6% in the candesartan group, a significant difference. Metoprolol didn’t put a dent in the LVEF decline.
“Observational studies show early reduction in LVEF is associated with increased risk of developing heart failure later. So if a sustained, long-term effect of angiotensin inhibition can be confirmed in larger multicenter trials, preventive therapy may be indicated as standard care for breast cancer patients,” Dr. Gulati said.
Discussant Dr. Bonnie Ky of the University of Pennsylvania, Philadelphia, called PRADA an important study that moves the field of cardio-oncology forward, yet it’s also a trial that raises more questions than it answers.
PRADA certainly addresses a major problem: “The incidence of heart failure and cardiomyopathy increases over time in breast cancer patients exposed to anthracyclines and trastuzumab. Because patients are living longer because of cancer chemotherapy, their risk of dying of cardiovascular disease actually exceeds that of recurrent cancer in the long term,” she observed.
The study has three major limitations that prevent its findings being implemented in routine clinical practice at this time, Dr. Ky said. One is its relatively small size, even though it’s far bigger than any previous study. Another limitation is that this was an extremely low-cardiovascular-risk patient cohort: the baseline prevalence of diabetes was only 1.5%, fewer than 7% of patients had hypertension, and the baseline LVEF was 63%. That may be why no one developed a substantial decrement in LVEF or actual heart failure.
And since the incidence of cardiomyopathy following breast cancer therapy is known to climb over time, reaching a cumulative 12% at 6 years followup in trastuzumab-treated patients and 20% in those who receive both anthracyclines and trastuzumab (J Natl Cancer Inst. 2012 Sep 5;104(17):1293-305), the lack of extended followup time in PRADA is a significant shortcoming, she added.
The important questions raised by PRADA, Dr. Ky continued, include whether carvedilol or another beta blocker would have generated a positive result where metoprolol failed. Also, should the target population for prevention of cardiotoxicity be more narrowly focused on those at higher baseline cardiovascular risk? And bearing in mind that change in LVEF is a surrogate endpoint, what might be a more clinically meaningful and valid outcome measure? What’s the effect of carvedilol and other cardioprotective medications on cardiac biomarkers in breast cancer patients? And the most important questions of all, she said: What would be the effects of longer followup time and extended therapy?
“This study highlights for us in the field of cardio-oncology the critical need to develop a robust consensus definition of cardiotoxicity and a methodology to identify high cardiovascular risk patients,” she concluded.
PRADA was funded primarily by the University of Oslo and the Norwegian Cancer Society. Dr. Gulati reported having no financial conflicts of interest. Dr. Ky reported receiving a research grant from Pfizer and serving as a consultant to Bristol Myers Squibb.
ORLANDO – Concomitant treatment with candesartan protects against the early decline in left ventricular ejection fraction associated with adjunct therapy for early breast cancer.
That was the key finding in the PRADA trial (PRevention of cArdiac Dysfunction during Adjuvant breast cancer therapy), the largest study to date looking at prevention of cardiac dysfunction in a breast cancer population.
Another important finding in PRADA was that unlike the angiotensin receptor blocker candesartan (Atacand), metoprolol, a beta blocker, didn’t prevent the early drop in LVEF commonly seen in breast cancer patients treated with anthracyclines and trastuzumab (Herceptin), even though both classes of heart medications are cornerstones of the treatment of ischemic and hypertensive cardiomyopathy, Dr. Geeta Gulati reported at the American Heart Association scientific sessions.
Although the cardiotoxicity of certain breast cancer treatments is widely recognized and has spawned the emerging field of cardio-oncology, the literature in this area is weak. Indeed, a recent meta-analysis identified only four published randomized studies evaluating the possible cardioprotective role for beta blockers and angiotensin antagonists in patients undergoing anthracycline-based chemotherapy (Postgrad Med J doi:10.1136/ postgradmedj-2015-133535). None of the studies was double-blind, all relied upon echocardiographic assessment of changes in LVEF rather than gold-standard cardiac MRI, and the study sizes were small -- just 18-45 breast cancer patients.
Most problematic of all, the studies employed a variety of different definitions of cardiotoxicity, noted Dr. Gulati of Akershus University Hospital in Lorenskog, Norway.
In contrast, PRADA was a double-blind, placebo-controlled, 2 by 2 factorial design, single-center trial, which included 120 patients with early breast cancer. Participants were randomized to candesartan at a starting dose of 8 mg and target dose of 32 mg/day, metoprolol starting at 25 mg with a target of 100 mg/day, or placebo after breast cancer surgery but before the start of anthracycline-containing chemotherapy.
The primary endpoint was change in LVEF from baseline to completion of adjuvant therapy, a period as short as 10 weeks and as long as 64 weeks depending upon whether a woman also underwent courses of trastuzumab, taxanes, and/or radiation therapy.
The overall decline in LVEF was 2.6% in the placebo group and 0.6% in the candesartan group, a significant difference. Metoprolol didn’t put a dent in the LVEF decline.
“Observational studies show early reduction in LVEF is associated with increased risk of developing heart failure later. So if a sustained, long-term effect of angiotensin inhibition can be confirmed in larger multicenter trials, preventive therapy may be indicated as standard care for breast cancer patients,” Dr. Gulati said.
Discussant Dr. Bonnie Ky of the University of Pennsylvania, Philadelphia, called PRADA an important study that moves the field of cardio-oncology forward, yet it’s also a trial that raises more questions than it answers.
PRADA certainly addresses a major problem: “The incidence of heart failure and cardiomyopathy increases over time in breast cancer patients exposed to anthracyclines and trastuzumab. Because patients are living longer because of cancer chemotherapy, their risk of dying of cardiovascular disease actually exceeds that of recurrent cancer in the long term,” she observed.
The study has three major limitations that prevent its findings being implemented in routine clinical practice at this time, Dr. Ky said. One is its relatively small size, even though it’s far bigger than any previous study. Another limitation is that this was an extremely low-cardiovascular-risk patient cohort: the baseline prevalence of diabetes was only 1.5%, fewer than 7% of patients had hypertension, and the baseline LVEF was 63%. That may be why no one developed a substantial decrement in LVEF or actual heart failure.
And since the incidence of cardiomyopathy following breast cancer therapy is known to climb over time, reaching a cumulative 12% at 6 years followup in trastuzumab-treated patients and 20% in those who receive both anthracyclines and trastuzumab (J Natl Cancer Inst. 2012 Sep 5;104(17):1293-305), the lack of extended followup time in PRADA is a significant shortcoming, she added.
The important questions raised by PRADA, Dr. Ky continued, include whether carvedilol or another beta blocker would have generated a positive result where metoprolol failed. Also, should the target population for prevention of cardiotoxicity be more narrowly focused on those at higher baseline cardiovascular risk? And bearing in mind that change in LVEF is a surrogate endpoint, what might be a more clinically meaningful and valid outcome measure? What’s the effect of carvedilol and other cardioprotective medications on cardiac biomarkers in breast cancer patients? And the most important questions of all, she said: What would be the effects of longer followup time and extended therapy?
“This study highlights for us in the field of cardio-oncology the critical need to develop a robust consensus definition of cardiotoxicity and a methodology to identify high cardiovascular risk patients,” she concluded.
PRADA was funded primarily by the University of Oslo and the Norwegian Cancer Society. Dr. Gulati reported having no financial conflicts of interest. Dr. Ky reported receiving a research grant from Pfizer and serving as a consultant to Bristol Myers Squibb.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Inroads are being made in the growing problem of breast cancer treatment-associated cardiomyopathy.
Major finding: The average 2.6% decline from baseline in breast cancer patients during adjuvant therapy with anthracyclines with or without trastuzumab was negated by concomitant candesartan but not by metoprolol.
Data source: The PRADA trial was a randomized, double-blind, placebo-controlled, 2 by 2 factorial design study involving 120 patients undergoing adjuvant therapy for early breast cancer.
Disclosures: The primary sponsors of the study were the University of Oslo and the Norwegian Cancer Society. Additional support was provided by Abbott Diagnostic and AstraZeneca. The presenter reported no financial conflicts of interest.
Decision model shows prophylactic double mastectomy more costly to patients
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Unilateral mastectomy costs less and provides better quality of life than contralateral prophylactic mastectomy in younger women with sporadic breast cancer.
Major finding: Unilateral mastectomy with routine surveillance cost on average $5,583 less than prophylactic contralateral mastectomy.
Data source: Cost-effectiveness analysis of contralateral prophylactic mastectomy.
Disclosures: The authors and Dr. Boughey reported no conflicts of interest.
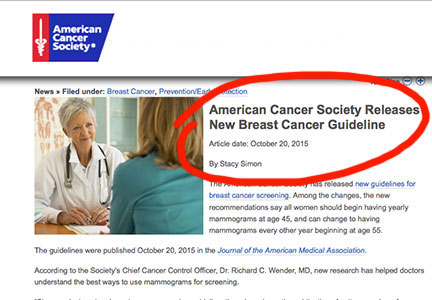
ACOG plans consensus conference on uniform guidelines for breast cancer screening
The Susan G. Komen Foundation estimates that 84% of breast cancers are found through mammography.1 Clearly, the value of mammography is proven. But controversy and confusion abound on how much mammography, and beginning at what age, is best for women.
Currently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and the American College of Obstetricians and Gynecologists (ACOG) all have differing recommendations about mammography and about the importance of clinical breast examinations. These inconsistencies largely are due to different interpretations of the same data, not the data itself, and tend to center on how harm is defined and measured. Importantly, these differences can wreak havoc on our patients’ confidence in our counsel and decision making, and can complicate women’s access to screening. Under the Affordable Care Act, women are guaranteed coverage of annual mammograms, but new USPSTF recommendations, due out soon, may undermine that guarantee.
On October 20, ACOG responded to the ACS’ new recommendations on breast cancer screening by emphasizing our continued advice that women should begin annual mammography screening at age 40, along with a clinical breast exam.2
Consensus conference plansIn an effort to address widespread confusion among patients, health care professionals, and payers, ACOG is convening a consensus conference in January 2016, with the goal of arriving at a consistent set of guidelines that can be agreed to, implemented clinically across the country, and hopefully adopted by insurers, as well. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail and to consider the available data in the broader context of patient care.
Without doubt, guidelines and recommendations will need to evolve as new evidence emerges, but our hope is that scientific and medical organizations can look at the same evidence and speak with one voice on what is best for women’s health. Our patients would benefit from that alone.
ACOG’s recommendations, summarized
- Clinical breast examination every year for women aged 19 and older.
- Screening mammography every year for women aged 40 and older.
- Breast self-awareness has the potential to detect palpable breast cancer and can be recommended.2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Susan G. Komen Web site. Accuracy of mammograms. http://ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Updated June 26, 2015. Accessed October 30, 2015.
- ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. American College of Obstetricians and Gynecologists Web site. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 30, 2015.
The Susan G. Komen Foundation estimates that 84% of breast cancers are found through mammography.1 Clearly, the value of mammography is proven. But controversy and confusion abound on how much mammography, and beginning at what age, is best for women.
Currently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and the American College of Obstetricians and Gynecologists (ACOG) all have differing recommendations about mammography and about the importance of clinical breast examinations. These inconsistencies largely are due to different interpretations of the same data, not the data itself, and tend to center on how harm is defined and measured. Importantly, these differences can wreak havoc on our patients’ confidence in our counsel and decision making, and can complicate women’s access to screening. Under the Affordable Care Act, women are guaranteed coverage of annual mammograms, but new USPSTF recommendations, due out soon, may undermine that guarantee.
On October 20, ACOG responded to the ACS’ new recommendations on breast cancer screening by emphasizing our continued advice that women should begin annual mammography screening at age 40, along with a clinical breast exam.2
Consensus conference plansIn an effort to address widespread confusion among patients, health care professionals, and payers, ACOG is convening a consensus conference in January 2016, with the goal of arriving at a consistent set of guidelines that can be agreed to, implemented clinically across the country, and hopefully adopted by insurers, as well. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail and to consider the available data in the broader context of patient care.
Without doubt, guidelines and recommendations will need to evolve as new evidence emerges, but our hope is that scientific and medical organizations can look at the same evidence and speak with one voice on what is best for women’s health. Our patients would benefit from that alone.
ACOG’s recommendations, summarized
- Clinical breast examination every year for women aged 19 and older.
- Screening mammography every year for women aged 40 and older.
- Breast self-awareness has the potential to detect palpable breast cancer and can be recommended.2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The Susan G. Komen Foundation estimates that 84% of breast cancers are found through mammography.1 Clearly, the value of mammography is proven. But controversy and confusion abound on how much mammography, and beginning at what age, is best for women.
Currently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), and the American College of Obstetricians and Gynecologists (ACOG) all have differing recommendations about mammography and about the importance of clinical breast examinations. These inconsistencies largely are due to different interpretations of the same data, not the data itself, and tend to center on how harm is defined and measured. Importantly, these differences can wreak havoc on our patients’ confidence in our counsel and decision making, and can complicate women’s access to screening. Under the Affordable Care Act, women are guaranteed coverage of annual mammograms, but new USPSTF recommendations, due out soon, may undermine that guarantee.
On October 20, ACOG responded to the ACS’ new recommendations on breast cancer screening by emphasizing our continued advice that women should begin annual mammography screening at age 40, along with a clinical breast exam.2
Consensus conference plansIn an effort to address widespread confusion among patients, health care professionals, and payers, ACOG is convening a consensus conference in January 2016, with the goal of arriving at a consistent set of guidelines that can be agreed to, implemented clinically across the country, and hopefully adopted by insurers, as well. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail and to consider the available data in the broader context of patient care.
Without doubt, guidelines and recommendations will need to evolve as new evidence emerges, but our hope is that scientific and medical organizations can look at the same evidence and speak with one voice on what is best for women’s health. Our patients would benefit from that alone.
ACOG’s recommendations, summarized
- Clinical breast examination every year for women aged 19 and older.
- Screening mammography every year for women aged 40 and older.
- Breast self-awareness has the potential to detect palpable breast cancer and can be recommended.2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Susan G. Komen Web site. Accuracy of mammograms. http://ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Updated June 26, 2015. Accessed October 30, 2015.
- ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. American College of Obstetricians and Gynecologists Web site. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 30, 2015.
- Susan G. Komen Web site. Accuracy of mammograms. http://ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Updated June 26, 2015. Accessed October 30, 2015.
- ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. American College of Obstetricians and Gynecologists Web site. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 30, 2015.
Adjuvant Systemic Therapy for Early-Stage Breast Cancer
Over the past 20 years, substantial progress has been achieved in our understanding of breast cancer and in breast cancer treatment, with mortality from breast cancer declining by more than 25% over this time. This progress has been characterized by a greater understanding of the molecular biology of breast cancer, rational drug design, development of agents with specific cellular targets and pathways, development of better prognostic and predictive multigene assays, and marked improvements in supportive care.
To read the full article in PDF:
Over the past 20 years, substantial progress has been achieved in our understanding of breast cancer and in breast cancer treatment, with mortality from breast cancer declining by more than 25% over this time. This progress has been characterized by a greater understanding of the molecular biology of breast cancer, rational drug design, development of agents with specific cellular targets and pathways, development of better prognostic and predictive multigene assays, and marked improvements in supportive care.
To read the full article in PDF:
Over the past 20 years, substantial progress has been achieved in our understanding of breast cancer and in breast cancer treatment, with mortality from breast cancer declining by more than 25% over this time. This progress has been characterized by a greater understanding of the molecular biology of breast cancer, rational drug design, development of agents with specific cellular targets and pathways, development of better prognostic and predictive multigene assays, and marked improvements in supportive care.
To read the full article in PDF:
How to individualize cancer risk reduction after a diagnosis of DCIS
A recent study reported in JAMA Oncology evaluated 10-year and 20-year breast cancer–specific mortality following diagnosis and treatment of ductal carcinoma in situ (DCIS) using the Surveillance, Epidemiology, and End Results (SEER) registries.1 The study included cases of pure DCIS (without lobular carcinoma in situ or microinvasion) diagnosed from 1988 to 2011 among women younger than age 70. It evaluated variables including age, race, income, type of surgery, radiation, subsequent diagnoses of invasive primary breast cancer, and, when applicable, cause of death.
Overall mortality rate was 3.3%
Mean follow-up was 7.5 years, with a 20-year breast cancer–specific mortality rate of 3.3% overall. Mortality was higher among young women diagnosed before the age of 35 years (7.8% vs 3.2%), and among black women (7.0% vs 3.0% for white women). The risk of dying from breast cancer was 18 times higher for women who developed subsequent ipsilateral invasive breast cancer. Mortality also was related to adverse DCIS characteristics such as grade, size, comedo-necrosis, and lack of an estrogen receptor.
Among patients who underwent lumpectomy, the addition of radiation reduced the risk of subsequent ipsilateral invasive breast cancer at 10 years (2.5% vs 4.9%; P<.001). However, radiation did not improve the 10-year rate of breast cancer mortality (0.8% for women who had lumpectomy with radiation, 0.9% for women who had lumpectomy alone, and 1.3% for women with unilateral mastectomy).
The prevention of ipsilateral invasive recurrence with radiation did not reduce mortality rates, as more than 50% of the women who died of breast cancer did not have an ipsilateral invasive recurrence prior to their death.
How these findings fit
into the larger picture
The findings of this landmark study confirm earlier reports, which showed that radiation after lumpectomy can reduce local recurrence but does not improve survival.2
Likewise, mastectomy, when compared with lumpectomy, offers no survival benefit and does not represent appropriate therapy for most women with small, unifocal DCIS.3
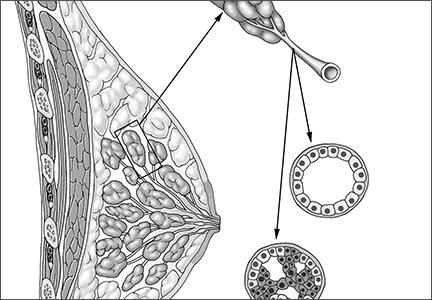
DCIS itself is not a life-threatening condition and has been described as a precursor lesion that, over 10 to 40 years, can lead to the development of invasive disease (FIGURE).4,5 High-grade DCIS tends to lead to high-grade invasive ductal carcinoma, and low-grade DCIS may develop into low-grade invasive disease.6
The increasing prevalence of screening mammography means that more small in situ lesions are being identified in US women. Unlike colonoscopy, which can prevent colon cancer by removing colon polyps, mammography with subsequent surgical treatment of DCIS has not reduced the incidence of invasive breast cancer.7This finding leads us to question whether all DCIS should be considered a precursor lesion. This well publicized study is generating controversy regarding overdiagnosis and overtreatment of DCIS.
Limitations of this study
The majority of patients in the SEER registry underwent surgical treatment of DCIS with or without radiation and had a survival rate of more than 97%. Because there was no untreated control group, this study does not allow us to draw any inferences on the role of expectant management of DCIS.
Although it is often declined by patients, tamoxifen reduces the risk of ipsilateral and contralateral invasive and in situ breast cancer. Regrettably, information on the use of adjuvant hormonal therapy after an initial diagnosis of DCIS was not included in this analysis.
Why did death from invasive
cancer sometimes follow a
diagnosis of DCIS?
Several factors could have contributed to the 3% mortality rate from invasive breast cancer among women in this large study of DCIS. For one, it is challenging for pathologists to perform comprehensive tissue sampling of mastectomy specimens—or even large lumpectomy specimens. Accordingly, occult microinvasive disease could be missed.8,9 As a result, occult invasive disease could go untreated, which could have contributed to the breast cancer mortality observed in this study.
Recommendations for practice
How can we better predict the behavior of DCIS and tailor treatment based on the biological behavior of each patient’s disease?
Individualize therapy. The likelihood of local invasive breast cancer recurrence should be estimated for each patient based on the size and grade of her disease. Furthermore, genetic profiling of DCIS has been developed with the Oncotype DX test (Genomic Health) multigene assay. This test can be performed on pathology specimens and has been shown to estimate the risk of in situ and invasive in-breast recurrence in patients who have undergone margin-negative lumpectomy for DCIS and who prefer to avoid radiation but are willing to take tamoxifen.10
Counsel precisely and accurately. Beyond such testing, we should focus on what is important to our patients in explaining the diagnosis:
- Our patients want to know that they are going to survive. Explain that DCIS is not a life-threatening cancer but a significant risk factor and is fully treatable with a long-term survival rate of 97%.
- Do not omit surgery. Follow-up surgical excision is still recommended after a core needle biopsy diagnosis of DCIS, as there is a 25% risk of finding invasive disease upon surgical excision.11,12 In our opinion, surgical excision represents the standard of care for DCIS, as some lesions may harbor invasive breast cancer.
- Explain the pros and cons of radiation to the patient once surgical excision has confirmed the diagnosis of pure DCIS. If the patient’s goal is to avoid any recurrence, then radiation can be useful and is particularly appropriate for women with high-grade, large, and estrogen-receptor–negative DCIS. However, patients in this setting need to recognize that radiation will not improve their already excellent rate of survival. For many patients, any recurrence, whether it’s DCIS or invasive disease, can be a devastating emotional event. But even in patients who experience a recurrence, early detection and treatment portend a very good outcome.
- Be aware of the fear of chemotherapy. Avoiding chemotherapy is a paramount (and understandable) desire for many women diagnosed with breast cancer. Women who choose radiation reduce their likelihood of invasive recurrence and potentially avoid the need for chemotherapy in the future.
- Know when mastectomy is indicated. Multicentric extensive DCIS is still an indication for mastectomy. The safety of avoiding mastectomy in this setting needs to be assessed by randomized trials. It may be safe for some women with DCIS, such as elderly patients with low-grade lesions, to undergo lumpectomy to rule out underlying invasive disease and be treated with endocrine therapy and observation, with or without radiation therapy. The issue of multiple re-excisions for close margins is also being re-evaluated.
Informed and shared
decision making is key
DCIS is an increasingly common and usually non–life-threatening condition. Radical surgery such as bilateral mastectomy for small unifocal DCIS is excessive and will not improve a patient’s outcome. As a prominent breast surgeon has written:
We must balance the small risk of breast cancer recurrence after lumpectomy for DCIS with patients’ quality of life concerns. This goal is best accomplished by using an informed and shared decision-making strategy to help our patients make sound decisions regarding DCIS.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Narod SA, Iqbal J, Giannakeas V, et al. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol. 2015;1(7):888–896.
- Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–488.
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–1241.
- Page D, Rogers L, Schuyler P, et al. The natural history of ductal carcinoma in situ of the breast. In: Silverstein MJ, Recht A, Lagios M, eds. Ductal Carcinoma in Situ of the Breast. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:17–21.
- Sanders M, Schuyler P, Dupont W, Page D. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer. 2005;103(12):2481–2484.
- Burstein HJ, Plyak K, Wong JS, et al. Ductal carcinoma in situ of the breast. N Engl J Med. 2004;350(14):1430–1441.
- Lin C, Moore D, DeMichelle A, et al. The majority of locally advanced breast cancers are interval cancer [Abstract 1503]. J Clin Oncol. 2009;27.
- Lagios M, Westdahl P, Margolin F, Rose M. Duct carcinoma in situ: relationship of extend of noninvasive disease to the frequency of occult invasion, multicentricity, lymph node metastases, and short-term treatment failures. Cancer. 1982;50(7):1309–1314.
- Schuh M, Nemoto T, Penetrante R, et al. Intraductal carcinoma: analysis of presentation, pathologic findings, and outcome of disease. Arch Surg. 1986;121(11):1303–1307.
- Solin LJ, Gray R, Baehner FL, et al. A multigene expression assay to predict local recurrence risk for ductal carcinoma in situ of the breast. J Natl Cancer Inst. 2013;105(10):701–710.
- Bruening W, Schoelles K, Treadwell J, et al. Comparative effectiveness of core needle and open surgical biopsy for the diagnosis of breast lesions. Rockville, MD: Prepared by ECRI Institute for the Agency for Healthcare Research and Quality under contract No. 290-02-0019; Comparative Effectiveness Review; September 2008.
- Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260(1):119–128.
- Morrow M, Winograd JM, Freer PE, et al. Case records of the Massachusetts General Hospital. Case 8-2013: a 48-year-old woman with carcinoma in situ of the breast. N Engl J Med. 2013;368(11):1046–1053.
A recent study reported in JAMA Oncology evaluated 10-year and 20-year breast cancer–specific mortality following diagnosis and treatment of ductal carcinoma in situ (DCIS) using the Surveillance, Epidemiology, and End Results (SEER) registries.1 The study included cases of pure DCIS (without lobular carcinoma in situ or microinvasion) diagnosed from 1988 to 2011 among women younger than age 70. It evaluated variables including age, race, income, type of surgery, radiation, subsequent diagnoses of invasive primary breast cancer, and, when applicable, cause of death.
Overall mortality rate was 3.3%
Mean follow-up was 7.5 years, with a 20-year breast cancer–specific mortality rate of 3.3% overall. Mortality was higher among young women diagnosed before the age of 35 years (7.8% vs 3.2%), and among black women (7.0% vs 3.0% for white women). The risk of dying from breast cancer was 18 times higher for women who developed subsequent ipsilateral invasive breast cancer. Mortality also was related to adverse DCIS characteristics such as grade, size, comedo-necrosis, and lack of an estrogen receptor.
Among patients who underwent lumpectomy, the addition of radiation reduced the risk of subsequent ipsilateral invasive breast cancer at 10 years (2.5% vs 4.9%; P<.001). However, radiation did not improve the 10-year rate of breast cancer mortality (0.8% for women who had lumpectomy with radiation, 0.9% for women who had lumpectomy alone, and 1.3% for women with unilateral mastectomy).
The prevention of ipsilateral invasive recurrence with radiation did not reduce mortality rates, as more than 50% of the women who died of breast cancer did not have an ipsilateral invasive recurrence prior to their death.
How these findings fit
into the larger picture
The findings of this landmark study confirm earlier reports, which showed that radiation after lumpectomy can reduce local recurrence but does not improve survival.2
Likewise, mastectomy, when compared with lumpectomy, offers no survival benefit and does not represent appropriate therapy for most women with small, unifocal DCIS.3
DCIS itself is not a life-threatening condition and has been described as a precursor lesion that, over 10 to 40 years, can lead to the development of invasive disease (FIGURE).4,5 High-grade DCIS tends to lead to high-grade invasive ductal carcinoma, and low-grade DCIS may develop into low-grade invasive disease.6
The increasing prevalence of screening mammography means that more small in situ lesions are being identified in US women. Unlike colonoscopy, which can prevent colon cancer by removing colon polyps, mammography with subsequent surgical treatment of DCIS has not reduced the incidence of invasive breast cancer.7This finding leads us to question whether all DCIS should be considered a precursor lesion. This well publicized study is generating controversy regarding overdiagnosis and overtreatment of DCIS.
Limitations of this study
The majority of patients in the SEER registry underwent surgical treatment of DCIS with or without radiation and had a survival rate of more than 97%. Because there was no untreated control group, this study does not allow us to draw any inferences on the role of expectant management of DCIS.
Although it is often declined by patients, tamoxifen reduces the risk of ipsilateral and contralateral invasive and in situ breast cancer. Regrettably, information on the use of adjuvant hormonal therapy after an initial diagnosis of DCIS was not included in this analysis.
Why did death from invasive
cancer sometimes follow a
diagnosis of DCIS?
Several factors could have contributed to the 3% mortality rate from invasive breast cancer among women in this large study of DCIS. For one, it is challenging for pathologists to perform comprehensive tissue sampling of mastectomy specimens—or even large lumpectomy specimens. Accordingly, occult microinvasive disease could be missed.8,9 As a result, occult invasive disease could go untreated, which could have contributed to the breast cancer mortality observed in this study.
Recommendations for practice
How can we better predict the behavior of DCIS and tailor treatment based on the biological behavior of each patient’s disease?
Individualize therapy. The likelihood of local invasive breast cancer recurrence should be estimated for each patient based on the size and grade of her disease. Furthermore, genetic profiling of DCIS has been developed with the Oncotype DX test (Genomic Health) multigene assay. This test can be performed on pathology specimens and has been shown to estimate the risk of in situ and invasive in-breast recurrence in patients who have undergone margin-negative lumpectomy for DCIS and who prefer to avoid radiation but are willing to take tamoxifen.10
Counsel precisely and accurately. Beyond such testing, we should focus on what is important to our patients in explaining the diagnosis:
- Our patients want to know that they are going to survive. Explain that DCIS is not a life-threatening cancer but a significant risk factor and is fully treatable with a long-term survival rate of 97%.
- Do not omit surgery. Follow-up surgical excision is still recommended after a core needle biopsy diagnosis of DCIS, as there is a 25% risk of finding invasive disease upon surgical excision.11,12 In our opinion, surgical excision represents the standard of care for DCIS, as some lesions may harbor invasive breast cancer.
- Explain the pros and cons of radiation to the patient once surgical excision has confirmed the diagnosis of pure DCIS. If the patient’s goal is to avoid any recurrence, then radiation can be useful and is particularly appropriate for women with high-grade, large, and estrogen-receptor–negative DCIS. However, patients in this setting need to recognize that radiation will not improve their already excellent rate of survival. For many patients, any recurrence, whether it’s DCIS or invasive disease, can be a devastating emotional event. But even in patients who experience a recurrence, early detection and treatment portend a very good outcome.
- Be aware of the fear of chemotherapy. Avoiding chemotherapy is a paramount (and understandable) desire for many women diagnosed with breast cancer. Women who choose radiation reduce their likelihood of invasive recurrence and potentially avoid the need for chemotherapy in the future.
- Know when mastectomy is indicated. Multicentric extensive DCIS is still an indication for mastectomy. The safety of avoiding mastectomy in this setting needs to be assessed by randomized trials. It may be safe for some women with DCIS, such as elderly patients with low-grade lesions, to undergo lumpectomy to rule out underlying invasive disease and be treated with endocrine therapy and observation, with or without radiation therapy. The issue of multiple re-excisions for close margins is also being re-evaluated.
Informed and shared
decision making is key
DCIS is an increasingly common and usually non–life-threatening condition. Radical surgery such as bilateral mastectomy for small unifocal DCIS is excessive and will not improve a patient’s outcome. As a prominent breast surgeon has written:
We must balance the small risk of breast cancer recurrence after lumpectomy for DCIS with patients’ quality of life concerns. This goal is best accomplished by using an informed and shared decision-making strategy to help our patients make sound decisions regarding DCIS.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
A recent study reported in JAMA Oncology evaluated 10-year and 20-year breast cancer–specific mortality following diagnosis and treatment of ductal carcinoma in situ (DCIS) using the Surveillance, Epidemiology, and End Results (SEER) registries.1 The study included cases of pure DCIS (without lobular carcinoma in situ or microinvasion) diagnosed from 1988 to 2011 among women younger than age 70. It evaluated variables including age, race, income, type of surgery, radiation, subsequent diagnoses of invasive primary breast cancer, and, when applicable, cause of death.
Overall mortality rate was 3.3%
Mean follow-up was 7.5 years, with a 20-year breast cancer–specific mortality rate of 3.3% overall. Mortality was higher among young women diagnosed before the age of 35 years (7.8% vs 3.2%), and among black women (7.0% vs 3.0% for white women). The risk of dying from breast cancer was 18 times higher for women who developed subsequent ipsilateral invasive breast cancer. Mortality also was related to adverse DCIS characteristics such as grade, size, comedo-necrosis, and lack of an estrogen receptor.
Among patients who underwent lumpectomy, the addition of radiation reduced the risk of subsequent ipsilateral invasive breast cancer at 10 years (2.5% vs 4.9%; P<.001). However, radiation did not improve the 10-year rate of breast cancer mortality (0.8% for women who had lumpectomy with radiation, 0.9% for women who had lumpectomy alone, and 1.3% for women with unilateral mastectomy).
The prevention of ipsilateral invasive recurrence with radiation did not reduce mortality rates, as more than 50% of the women who died of breast cancer did not have an ipsilateral invasive recurrence prior to their death.
How these findings fit
into the larger picture
The findings of this landmark study confirm earlier reports, which showed that radiation after lumpectomy can reduce local recurrence but does not improve survival.2
Likewise, mastectomy, when compared with lumpectomy, offers no survival benefit and does not represent appropriate therapy for most women with small, unifocal DCIS.3
DCIS itself is not a life-threatening condition and has been described as a precursor lesion that, over 10 to 40 years, can lead to the development of invasive disease (FIGURE).4,5 High-grade DCIS tends to lead to high-grade invasive ductal carcinoma, and low-grade DCIS may develop into low-grade invasive disease.6
The increasing prevalence of screening mammography means that more small in situ lesions are being identified in US women. Unlike colonoscopy, which can prevent colon cancer by removing colon polyps, mammography with subsequent surgical treatment of DCIS has not reduced the incidence of invasive breast cancer.7This finding leads us to question whether all DCIS should be considered a precursor lesion. This well publicized study is generating controversy regarding overdiagnosis and overtreatment of DCIS.
Limitations of this study
The majority of patients in the SEER registry underwent surgical treatment of DCIS with or without radiation and had a survival rate of more than 97%. Because there was no untreated control group, this study does not allow us to draw any inferences on the role of expectant management of DCIS.
Although it is often declined by patients, tamoxifen reduces the risk of ipsilateral and contralateral invasive and in situ breast cancer. Regrettably, information on the use of adjuvant hormonal therapy after an initial diagnosis of DCIS was not included in this analysis.
Why did death from invasive
cancer sometimes follow a
diagnosis of DCIS?
Several factors could have contributed to the 3% mortality rate from invasive breast cancer among women in this large study of DCIS. For one, it is challenging for pathologists to perform comprehensive tissue sampling of mastectomy specimens—or even large lumpectomy specimens. Accordingly, occult microinvasive disease could be missed.8,9 As a result, occult invasive disease could go untreated, which could have contributed to the breast cancer mortality observed in this study.
Recommendations for practice
How can we better predict the behavior of DCIS and tailor treatment based on the biological behavior of each patient’s disease?
Individualize therapy. The likelihood of local invasive breast cancer recurrence should be estimated for each patient based on the size and grade of her disease. Furthermore, genetic profiling of DCIS has been developed with the Oncotype DX test (Genomic Health) multigene assay. This test can be performed on pathology specimens and has been shown to estimate the risk of in situ and invasive in-breast recurrence in patients who have undergone margin-negative lumpectomy for DCIS and who prefer to avoid radiation but are willing to take tamoxifen.10
Counsel precisely and accurately. Beyond such testing, we should focus on what is important to our patients in explaining the diagnosis:
- Our patients want to know that they are going to survive. Explain that DCIS is not a life-threatening cancer but a significant risk factor and is fully treatable with a long-term survival rate of 97%.
- Do not omit surgery. Follow-up surgical excision is still recommended after a core needle biopsy diagnosis of DCIS, as there is a 25% risk of finding invasive disease upon surgical excision.11,12 In our opinion, surgical excision represents the standard of care for DCIS, as some lesions may harbor invasive breast cancer.
- Explain the pros and cons of radiation to the patient once surgical excision has confirmed the diagnosis of pure DCIS. If the patient’s goal is to avoid any recurrence, then radiation can be useful and is particularly appropriate for women with high-grade, large, and estrogen-receptor–negative DCIS. However, patients in this setting need to recognize that radiation will not improve their already excellent rate of survival. For many patients, any recurrence, whether it’s DCIS or invasive disease, can be a devastating emotional event. But even in patients who experience a recurrence, early detection and treatment portend a very good outcome.
- Be aware of the fear of chemotherapy. Avoiding chemotherapy is a paramount (and understandable) desire for many women diagnosed with breast cancer. Women who choose radiation reduce their likelihood of invasive recurrence and potentially avoid the need for chemotherapy in the future.
- Know when mastectomy is indicated. Multicentric extensive DCIS is still an indication for mastectomy. The safety of avoiding mastectomy in this setting needs to be assessed by randomized trials. It may be safe for some women with DCIS, such as elderly patients with low-grade lesions, to undergo lumpectomy to rule out underlying invasive disease and be treated with endocrine therapy and observation, with or without radiation therapy. The issue of multiple re-excisions for close margins is also being re-evaluated.
Informed and shared
decision making is key
DCIS is an increasingly common and usually non–life-threatening condition. Radical surgery such as bilateral mastectomy for small unifocal DCIS is excessive and will not improve a patient’s outcome. As a prominent breast surgeon has written:
We must balance the small risk of breast cancer recurrence after lumpectomy for DCIS with patients’ quality of life concerns. This goal is best accomplished by using an informed and shared decision-making strategy to help our patients make sound decisions regarding DCIS.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Narod SA, Iqbal J, Giannakeas V, et al. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol. 2015;1(7):888–896.
- Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–488.
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–1241.
- Page D, Rogers L, Schuyler P, et al. The natural history of ductal carcinoma in situ of the breast. In: Silverstein MJ, Recht A, Lagios M, eds. Ductal Carcinoma in Situ of the Breast. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:17–21.
- Sanders M, Schuyler P, Dupont W, Page D. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer. 2005;103(12):2481–2484.
- Burstein HJ, Plyak K, Wong JS, et al. Ductal carcinoma in situ of the breast. N Engl J Med. 2004;350(14):1430–1441.
- Lin C, Moore D, DeMichelle A, et al. The majority of locally advanced breast cancers are interval cancer [Abstract 1503]. J Clin Oncol. 2009;27.
- Lagios M, Westdahl P, Margolin F, Rose M. Duct carcinoma in situ: relationship of extend of noninvasive disease to the frequency of occult invasion, multicentricity, lymph node metastases, and short-term treatment failures. Cancer. 1982;50(7):1309–1314.
- Schuh M, Nemoto T, Penetrante R, et al. Intraductal carcinoma: analysis of presentation, pathologic findings, and outcome of disease. Arch Surg. 1986;121(11):1303–1307.
- Solin LJ, Gray R, Baehner FL, et al. A multigene expression assay to predict local recurrence risk for ductal carcinoma in situ of the breast. J Natl Cancer Inst. 2013;105(10):701–710.
- Bruening W, Schoelles K, Treadwell J, et al. Comparative effectiveness of core needle and open surgical biopsy for the diagnosis of breast lesions. Rockville, MD: Prepared by ECRI Institute for the Agency for Healthcare Research and Quality under contract No. 290-02-0019; Comparative Effectiveness Review; September 2008.
- Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260(1):119–128.
- Morrow M, Winograd JM, Freer PE, et al. Case records of the Massachusetts General Hospital. Case 8-2013: a 48-year-old woman with carcinoma in situ of the breast. N Engl J Med. 2013;368(11):1046–1053.
- Narod SA, Iqbal J, Giannakeas V, et al. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol. 2015;1(7):888–896.
- Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–488.
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–1241.
- Page D, Rogers L, Schuyler P, et al. The natural history of ductal carcinoma in situ of the breast. In: Silverstein MJ, Recht A, Lagios M, eds. Ductal Carcinoma in Situ of the Breast. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:17–21.
- Sanders M, Schuyler P, Dupont W, Page D. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer. 2005;103(12):2481–2484.
- Burstein HJ, Plyak K, Wong JS, et al. Ductal carcinoma in situ of the breast. N Engl J Med. 2004;350(14):1430–1441.
- Lin C, Moore D, DeMichelle A, et al. The majority of locally advanced breast cancers are interval cancer [Abstract 1503]. J Clin Oncol. 2009;27.
- Lagios M, Westdahl P, Margolin F, Rose M. Duct carcinoma in situ: relationship of extend of noninvasive disease to the frequency of occult invasion, multicentricity, lymph node metastases, and short-term treatment failures. Cancer. 1982;50(7):1309–1314.
- Schuh M, Nemoto T, Penetrante R, et al. Intraductal carcinoma: analysis of presentation, pathologic findings, and outcome of disease. Arch Surg. 1986;121(11):1303–1307.
- Solin LJ, Gray R, Baehner FL, et al. A multigene expression assay to predict local recurrence risk for ductal carcinoma in situ of the breast. J Natl Cancer Inst. 2013;105(10):701–710.
- Bruening W, Schoelles K, Treadwell J, et al. Comparative effectiveness of core needle and open surgical biopsy for the diagnosis of breast lesions. Rockville, MD: Prepared by ECRI Institute for the Agency for Healthcare Research and Quality under contract No. 290-02-0019; Comparative Effectiveness Review; September 2008.
- Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260(1):119–128.
- Morrow M, Winograd JM, Freer PE, et al. Case records of the Massachusetts General Hospital. Case 8-2013: a 48-year-old woman with carcinoma in situ of the breast. N Engl J Med. 2013;368(11):1046–1053.
In this Article
- What is DCIS?
- Why did some deaths occur after diagnosis of DCIS?
- Why did some deaths occur after diagnosis of DCIS?
Partial breast irradiation valid option to prevent local recurrence
SAN ANTONIO – Accelerated partial breast irradiation (APBI) using an interstitial multicatheter brachytherapy method is as effective as whole breast irradiation (WBI) at preventing local disease recurrence 5 years after surgery for early breast cancer, according to the long-term results of a large European randomized phase III trial.
The cumulative incidence of local recurrence was 1.44% in the women who received ABPI and 0.92% in the women who received conventional WBI followed by a further boost of radiation to the tumor-bed in the GEC-ESTRO (Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology) trial. The 0.52% difference between the two types of radiation therapy was not statistically significant and was within the 3% margin set for noninferiority.
Results of the trial also showed similarly high, and not statistically different, 5-year disease-free (95.03% vs. 94.4%) and overall survival (97.3% vs. 95.5%) for APBI and WBI.
“This is the first phase III study proving noninferiority of APBI in comparison to whole breast irradiation for selected early stage breast cancer patients,” said Dr. Vratislav Strnad of University Hospital Erlangen, Germany, during a press briefing at the annual meeting of the American Society for Radiation Oncology.
Dr. Strnad added, “Based on our results, APBI using multicatheter brachytherapy can be considered as a valid alternative treatment option after breast conserving surgery.” It could be offered to all women with early-stage, low-risk breast cancer patients in routine clinical practice, he observed.
More evidence is needed before APBI can be considered a new standard, said U.K. commentators in an editorial to accompany the published findings (Lancet. 2015 Oct 19. doi: 10.1016/S0140-6736[15]00471-7).
“This trial presents maturing data and further evidence is required from the 14,000 patients in five, as yet unreported, APBI phase III trials,” saidDr. Charlotte Coles of Cambridge (England) University NHS Foundation Trust and Dr. John Yarnold of the Royal Marsden Hospital NHS Foundation Trust in London in the editorial (Lancet. 2015 Oct 19. doi: 10.1016/S0140-6736[15]00518-8).
Continued follow-up for at least 10 years is planned, “which is essential in view of the linear rate of recurrence for lower risk patients and the ongoing effect of radiotherapy after 5 years of treatment,” Dr. Coles and Dr. Yarnold add.
One of the main reasons for APBI is to reduce the number and duration of treatment from weeks to days and thereby radiation exposure that may result in toxicity. The editorialists noted, however, that recent studies have shown it is possible to give WBI over 3 rather than 5 weeks, and the FAST-Forward trial in the United Kingdom, is looking to see if 1 week is possible.
In the current trial, APBI was delivered at a total dose of 30-32 Gy given in seven to eight fractions over 4-5 days to 633 women, and WBI was given at a total dose of 50 Gy in 25-28 fractions over a 5-week period with a 10 Gy boost to the tumor bed given in five fractions to 551 women.
The median age of the women in the trial was 62 years and 39% had stage I and 51% had stage II cancer. The remainder had stage III or unknown stage disease. The majority of patients had invasive carcinoma (95%), and in 86%, the primary tumor was 2 cm or smaller in size.
“The efficacy of partial breast irradiation is the same as whole breast radiation but is more gentle,” Dr. Strnad observed in an interview.
There fewer grade 2-3 adverse events involving the skin (3.2% vs. 5.7%; P = .08) at 5 years’ follow-up with APBI than with WBI. There was no significant difference between the two radiation modalities in grade 2-3 adverse effects involving the subcutaneous tissue (7.6% vs. 6.3%; P = .053) or grade 3 fibrosis (0% vs. 0.2%; P = .46). No grade 4 late side effects were reported.
“I think the take-home message is that we have two alternatives for radiation therapy after breast-conserving surgery,” Dr. Strnad said. “Everybody should know these data and decide on the most appropriate therapy.”
SAN ANTONIO – Accelerated partial breast irradiation (APBI) using an interstitial multicatheter brachytherapy method is as effective as whole breast irradiation (WBI) at preventing local disease recurrence 5 years after surgery for early breast cancer, according to the long-term results of a large European randomized phase III trial.
The cumulative incidence of local recurrence was 1.44% in the women who received ABPI and 0.92% in the women who received conventional WBI followed by a further boost of radiation to the tumor-bed in the GEC-ESTRO (Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology) trial. The 0.52% difference between the two types of radiation therapy was not statistically significant and was within the 3% margin set for noninferiority.
Results of the trial also showed similarly high, and not statistically different, 5-year disease-free (95.03% vs. 94.4%) and overall survival (97.3% vs. 95.5%) for APBI and WBI.
“This is the first phase III study proving noninferiority of APBI in comparison to whole breast irradiation for selected early stage breast cancer patients,” said Dr. Vratislav Strnad of University Hospital Erlangen, Germany, during a press briefing at the annual meeting of the American Society for Radiation Oncology.
Dr. Strnad added, “Based on our results, APBI using multicatheter brachytherapy can be considered as a valid alternative treatment option after breast conserving surgery.” It could be offered to all women with early-stage, low-risk breast cancer patients in routine clinical practice, he observed.
More evidence is needed before APBI can be considered a new standard, said U.K. commentators in an editorial to accompany the published findings (Lancet. 2015 Oct 19. doi: 10.1016/S0140-6736[15]00471-7).
“This trial presents maturing data and further evidence is required from the 14,000 patients in five, as yet unreported, APBI phase III trials,” saidDr. Charlotte Coles of Cambridge (England) University NHS Foundation Trust and Dr. John Yarnold of the Royal Marsden Hospital NHS Foundation Trust in London in the editorial (Lancet. 2015 Oct 19. doi: 10.1016/S0140-6736[15]00518-8).
Continued follow-up for at least 10 years is planned, “which is essential in view of the linear rate of recurrence for lower risk patients and the ongoing effect of radiotherapy after 5 years of treatment,” Dr. Coles and Dr. Yarnold add.
One of the main reasons for APBI is to reduce the number and duration of treatment from weeks to days and thereby radiation exposure that may result in toxicity. The editorialists noted, however, that recent studies have shown it is possible to give WBI over 3 rather than 5 weeks, and the FAST-Forward trial in the United Kingdom, is looking to see if 1 week is possible.
In the current trial, APBI was delivered at a total dose of 30-32 Gy given in seven to eight fractions over 4-5 days to 633 women, and WBI was given at a total dose of 50 Gy in 25-28 fractions over a 5-week period with a 10 Gy boost to the tumor bed given in five fractions to 551 women.
The median age of the women in the trial was 62 years and 39% had stage I and 51% had stage II cancer. The remainder had stage III or unknown stage disease. The majority of patients had invasive carcinoma (95%), and in 86%, the primary tumor was 2 cm or smaller in size.
“The efficacy of partial breast irradiation is the same as whole breast radiation but is more gentle,” Dr. Strnad observed in an interview.
There fewer grade 2-3 adverse events involving the skin (3.2% vs. 5.7%; P = .08) at 5 years’ follow-up with APBI than with WBI. There was no significant difference between the two radiation modalities in grade 2-3 adverse effects involving the subcutaneous tissue (7.6% vs. 6.3%; P = .053) or grade 3 fibrosis (0% vs. 0.2%; P = .46). No grade 4 late side effects were reported.
“I think the take-home message is that we have two alternatives for radiation therapy after breast-conserving surgery,” Dr. Strnad said. “Everybody should know these data and decide on the most appropriate therapy.”
SAN ANTONIO – Accelerated partial breast irradiation (APBI) using an interstitial multicatheter brachytherapy method is as effective as whole breast irradiation (WBI) at preventing local disease recurrence 5 years after surgery for early breast cancer, according to the long-term results of a large European randomized phase III trial.
The cumulative incidence of local recurrence was 1.44% in the women who received ABPI and 0.92% in the women who received conventional WBI followed by a further boost of radiation to the tumor-bed in the GEC-ESTRO (Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology) trial. The 0.52% difference between the two types of radiation therapy was not statistically significant and was within the 3% margin set for noninferiority.
Results of the trial also showed similarly high, and not statistically different, 5-year disease-free (95.03% vs. 94.4%) and overall survival (97.3% vs. 95.5%) for APBI and WBI.
“This is the first phase III study proving noninferiority of APBI in comparison to whole breast irradiation for selected early stage breast cancer patients,” said Dr. Vratislav Strnad of University Hospital Erlangen, Germany, during a press briefing at the annual meeting of the American Society for Radiation Oncology.
Dr. Strnad added, “Based on our results, APBI using multicatheter brachytherapy can be considered as a valid alternative treatment option after breast conserving surgery.” It could be offered to all women with early-stage, low-risk breast cancer patients in routine clinical practice, he observed.
More evidence is needed before APBI can be considered a new standard, said U.K. commentators in an editorial to accompany the published findings (Lancet. 2015 Oct 19. doi: 10.1016/S0140-6736[15]00471-7).
“This trial presents maturing data and further evidence is required from the 14,000 patients in five, as yet unreported, APBI phase III trials,” saidDr. Charlotte Coles of Cambridge (England) University NHS Foundation Trust and Dr. John Yarnold of the Royal Marsden Hospital NHS Foundation Trust in London in the editorial (Lancet. 2015 Oct 19. doi: 10.1016/S0140-6736[15]00518-8).
Continued follow-up for at least 10 years is planned, “which is essential in view of the linear rate of recurrence for lower risk patients and the ongoing effect of radiotherapy after 5 years of treatment,” Dr. Coles and Dr. Yarnold add.
One of the main reasons for APBI is to reduce the number and duration of treatment from weeks to days and thereby radiation exposure that may result in toxicity. The editorialists noted, however, that recent studies have shown it is possible to give WBI over 3 rather than 5 weeks, and the FAST-Forward trial in the United Kingdom, is looking to see if 1 week is possible.
In the current trial, APBI was delivered at a total dose of 30-32 Gy given in seven to eight fractions over 4-5 days to 633 women, and WBI was given at a total dose of 50 Gy in 25-28 fractions over a 5-week period with a 10 Gy boost to the tumor bed given in five fractions to 551 women.
The median age of the women in the trial was 62 years and 39% had stage I and 51% had stage II cancer. The remainder had stage III or unknown stage disease. The majority of patients had invasive carcinoma (95%), and in 86%, the primary tumor was 2 cm or smaller in size.
“The efficacy of partial breast irradiation is the same as whole breast radiation but is more gentle,” Dr. Strnad observed in an interview.
There fewer grade 2-3 adverse events involving the skin (3.2% vs. 5.7%; P = .08) at 5 years’ follow-up with APBI than with WBI. There was no significant difference between the two radiation modalities in grade 2-3 adverse effects involving the subcutaneous tissue (7.6% vs. 6.3%; P = .053) or grade 3 fibrosis (0% vs. 0.2%; P = .46). No grade 4 late side effects were reported.
“I think the take-home message is that we have two alternatives for radiation therapy after breast-conserving surgery,” Dr. Strnad said. “Everybody should know these data and decide on the most appropriate therapy.”
AT THE ASTRO ANNUAL MEETING
Key clinical point:Accelerated partial breast irradiation (APBI) was as effective as whole breast irradiation (WBI) plus a boost in preventing local recurrence at 5 years in early breast cancer.
Major finding: 5-year local recurrence rates were 1.44% for ABPI and 0.92% for WBI, with the 0.52% difference within the pre-specified 3% noninferiority margin.
Data source: Phase III randomized, noninferiority trial involving 1,184 women with early breast cancer treated 2004 and 2009 in 16 European hospitals and medical centers.
Disclosures: The study was funded by German Cancer Aid. Dr. Strnad has received a grant from German Cancer Aid and consultation fees from Nucletron Operations BV that were not related to the study.
Gene mutations had little impact on everolimus benefit in advanced breast cancer
Genetic alterations affecting phosphoinositide 3-kinase (PI3K) and fibroblast growth factor receptor (FGFR), and associated pathways, only minimally affected the efficacy of everolimus in patients with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (EGFR-) advanced breast cancer.
To determine whether everolimus yielded greater treatment benefits in tumors dependent on a hyperactive PI3K/mTOR pathway, progression-free survival (PFS) in the presence and absence of mutated PIK3CA (catalytic subunit of PI3K) was examined. Median PFS was longer for all patients with wild-type PIK3CA (catalytic subunit of PI3K); everolimus was associated with a slightly greater reduction in risk than placebo: the hazard ratio was 0.37 (95% CI, 0.25 to 0.55) for wild-type PIK3CA and 0.51 (95% CI, 0.34 to 0.77) for mutated. The everolimus benefit was greater in patients with exon-9 mutations (HR, 0.26; 95% CI, 0.12 to 0.54) than exon-20 mutations (HR, 0.56; 95% CI, 0.31 to 1.00).
The lack of an appreciable effect of activating mutations on everolimus benefit, “highlighted the oversimplification of both the hypothesis and the analytic method of pooling all genetic alterations in this frequently mutated gene or hyperactive pathway,” wrote Dr. Gabriel N. Hortobagyi, professor of medicine, University of Texas MD Anderson Cancer Center, Houston, and his colleagues (J Clin Oncol. 2015 Oct. 26. doi:10.1200/JCO.2014.60.1971).
The data showed that PIK3CA exon-9 mutations were associated with more benefit than were exon-20 mutations, pointing to the importance of clinically evaluating mutations in terms of their specific functional effects, the investigators said.
Similar to observations with the PI3K pathway, genetic alterations in FGFR and cell-cycle control genes had minimal effect on PFS gains with everolimus.
The study also used NextGen sequencing to derive a contrast-induced nephropathy scoring system to assess the influence of chromosomal instability on everolimus benefit. Patients with low chromosomal instability (below the 75th percentile) derived a median PFS gain of 5.5 months with everolimus, compared with 1.5 months for patients with high chromosomal instability (above the 75th percentile). The effect of chromosomal instability on PFS was evident only in the everolimus arm, suggesting that tumors with lower chromosomal instability may derive greater benefit from the addition of everolimus.
Using data acquired from a medium-size cancer panel to measure chromosomal instability expands the utility of the NextGen sequencing data increasingly collected in oncology practice, Dr. Hortobagyi and his associates wrote.
Genetic alterations affecting phosphoinositide 3-kinase (PI3K) and fibroblast growth factor receptor (FGFR), and associated pathways, only minimally affected the efficacy of everolimus in patients with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (EGFR-) advanced breast cancer.
To determine whether everolimus yielded greater treatment benefits in tumors dependent on a hyperactive PI3K/mTOR pathway, progression-free survival (PFS) in the presence and absence of mutated PIK3CA (catalytic subunit of PI3K) was examined. Median PFS was longer for all patients with wild-type PIK3CA (catalytic subunit of PI3K); everolimus was associated with a slightly greater reduction in risk than placebo: the hazard ratio was 0.37 (95% CI, 0.25 to 0.55) for wild-type PIK3CA and 0.51 (95% CI, 0.34 to 0.77) for mutated. The everolimus benefit was greater in patients with exon-9 mutations (HR, 0.26; 95% CI, 0.12 to 0.54) than exon-20 mutations (HR, 0.56; 95% CI, 0.31 to 1.00).
The lack of an appreciable effect of activating mutations on everolimus benefit, “highlighted the oversimplification of both the hypothesis and the analytic method of pooling all genetic alterations in this frequently mutated gene or hyperactive pathway,” wrote Dr. Gabriel N. Hortobagyi, professor of medicine, University of Texas MD Anderson Cancer Center, Houston, and his colleagues (J Clin Oncol. 2015 Oct. 26. doi:10.1200/JCO.2014.60.1971).
The data showed that PIK3CA exon-9 mutations were associated with more benefit than were exon-20 mutations, pointing to the importance of clinically evaluating mutations in terms of their specific functional effects, the investigators said.
Similar to observations with the PI3K pathway, genetic alterations in FGFR and cell-cycle control genes had minimal effect on PFS gains with everolimus.
The study also used NextGen sequencing to derive a contrast-induced nephropathy scoring system to assess the influence of chromosomal instability on everolimus benefit. Patients with low chromosomal instability (below the 75th percentile) derived a median PFS gain of 5.5 months with everolimus, compared with 1.5 months for patients with high chromosomal instability (above the 75th percentile). The effect of chromosomal instability on PFS was evident only in the everolimus arm, suggesting that tumors with lower chromosomal instability may derive greater benefit from the addition of everolimus.
Using data acquired from a medium-size cancer panel to measure chromosomal instability expands the utility of the NextGen sequencing data increasingly collected in oncology practice, Dr. Hortobagyi and his associates wrote.
Genetic alterations affecting phosphoinositide 3-kinase (PI3K) and fibroblast growth factor receptor (FGFR), and associated pathways, only minimally affected the efficacy of everolimus in patients with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (EGFR-) advanced breast cancer.
To determine whether everolimus yielded greater treatment benefits in tumors dependent on a hyperactive PI3K/mTOR pathway, progression-free survival (PFS) in the presence and absence of mutated PIK3CA (catalytic subunit of PI3K) was examined. Median PFS was longer for all patients with wild-type PIK3CA (catalytic subunit of PI3K); everolimus was associated with a slightly greater reduction in risk than placebo: the hazard ratio was 0.37 (95% CI, 0.25 to 0.55) for wild-type PIK3CA and 0.51 (95% CI, 0.34 to 0.77) for mutated. The everolimus benefit was greater in patients with exon-9 mutations (HR, 0.26; 95% CI, 0.12 to 0.54) than exon-20 mutations (HR, 0.56; 95% CI, 0.31 to 1.00).
The lack of an appreciable effect of activating mutations on everolimus benefit, “highlighted the oversimplification of both the hypothesis and the analytic method of pooling all genetic alterations in this frequently mutated gene or hyperactive pathway,” wrote Dr. Gabriel N. Hortobagyi, professor of medicine, University of Texas MD Anderson Cancer Center, Houston, and his colleagues (J Clin Oncol. 2015 Oct. 26. doi:10.1200/JCO.2014.60.1971).
The data showed that PIK3CA exon-9 mutations were associated with more benefit than were exon-20 mutations, pointing to the importance of clinically evaluating mutations in terms of their specific functional effects, the investigators said.
Similar to observations with the PI3K pathway, genetic alterations in FGFR and cell-cycle control genes had minimal effect on PFS gains with everolimus.
The study also used NextGen sequencing to derive a contrast-induced nephropathy scoring system to assess the influence of chromosomal instability on everolimus benefit. Patients with low chromosomal instability (below the 75th percentile) derived a median PFS gain of 5.5 months with everolimus, compared with 1.5 months for patients with high chromosomal instability (above the 75th percentile). The effect of chromosomal instability on PFS was evident only in the everolimus arm, suggesting that tumors with lower chromosomal instability may derive greater benefit from the addition of everolimus.
Using data acquired from a medium-size cancer panel to measure chromosomal instability expands the utility of the NextGen sequencing data increasingly collected in oncology practice, Dr. Hortobagyi and his associates wrote.
Key clinical point: Mutations in genes involved in the PI3K/mTOR pathway, FGFR signaling, and cell cycle regulation had little impact on everolimus benefit in hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (EGFR-) advanced breast cancer.
Major finding: For patients treated with either everolimus or placebo, median PFS was longer if they carried wild-type PIK3CA. For patients treated with everolimus, hazard ratios for wild-type vs. mutated PIK3CA were 0.37 (95% CI, 0.25 to 0.55) and 0.51 (95% CI, 0.34 to 0.77), respectively.
Data source: The BOLERO-2 trial included 724 patients with HR+, HER2- advanced breast cancer; samples from 302 (42%) were evaluated with NextGen sequencing.
Disclosures: Dr. Hortobagyi reported consulting or advisory roles with Pfizer, Antigen Express, Novartis, Galena, Genentech, and Amgen. Several of his coauthors reported having ties to industry sources.
What you should know about the latest change in mammography screening guidelines
When the American Cancer Society (ACS) updated its guidelines for screening mammography earlier this week,1 the effect was that of a stone being tossed into a tranquil pond, generating ripples in all directions.
The new guidelines focus on women at average risk for breast cancer (TABLE 1) and were updated for the first time since 2003, based on new evidence, a new emphasis on eliminating as many screening harms as possible, and a goal of “supporting the interplay among values, preferences, informed decision making, and recommendations.”1 Earlier ACS guidelines recommended annual screening starting at age 40.
TABLE 1 What constitutes “average risk” of breast cancer?
|
The new guidelines are graded according to the strength of the rec ommendation as being either “strong” or “qualified.” The ACS defines a “strong” recommendation as one that most individuals should follow. “Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator,” the guidelines note.1
A “qualified” recommendation indicates that “Clinicians should acknowledge that different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her or his values and preferences.”1
The recommendations are:
- Regular screening mammography should start at age 45 years (strong recommendation)
- Screening should be annual in women aged 45 to 54 years (qualified recommendation)
- Screening should shift to biennial intervals at age 55, unless the patient prefers to continue screening annually (qualified recommendation)
- Women who desire to initiate annual screening between the ages of 40 and 44 years should be accommodated (qualified recommendation)
- Screening mammography should continue as long as the woman is in good health and has a life expectancy of at least 10 years (qualified recommendation)
- Clinical breast examination (CBE) is not recommended at any age (qualified recommendation).1
ACOG weighs in
Shortly after publication of the new ACS guidelines, the American College of Obstetricians and Gynecologists (ACOG) issued a formal statement in response2:
Response of the USPSTF
The US Preventive Services Task Force (USPSTF) also issued a statement in response to the new ACS guidelines:
The USPSTF currently recommends biennial screening beginning at age 50.
A leader in breast health cites pros and cons of ACS recommendations
Mark Pearlman, MD, professor of obstetrics and gynecology at the University of Michigan health system, is a nationally recognized expert on breast cancer screening. He sits on the National Comprehensive Cancer Network (NCCN) breast cancer screening and diagnosis group, helped author ACOG guidelines on mammography screening, and serves as a Contributing Editor to OBG Management.
“I believe the overall ACS mammography benefit evidence synthesis is reasonable and is in keeping with both NCCN and ACOG’s current recommendations. NCCN and ACOG mammography screening recommendations have both valued lives saved more highly than the ‘harms’ such as recalls and needle biopsies,” Dr. Pearlman says.
“If one combines ACS ‘strong’ and ‘qualified’ recommendations, ACS recommendations are similar to current ACOG and NCCN recommendations for mammography,” he adds.
Dr. Pearlman finds 7 areas of agreement between NCCN/ACOG and ACS recommendations, using both strong and qualified recommendations:
- “They reaffirm that screening from age 40 to 69 years is associated with a reduction in breast cancer deaths.
- They support annual screening for women in their 40s [although the ACS’ ‘strong’ recommendation is that regular screening begin at age 45 instead of 40].
- They support screening for women 70 and older who are in good health (10-year life expectancy).
- They support the finding that annual screening yields a larger mortality reduction than biennial screening.
- They confirm much uncertainty about the “over-diagnosis/overtreatment” issue.
- They endorse insurance coverage at all ages and intervals of screening (not just USPSTF ‘A’ or ‘B’ recommendations).
- They involve the patient in informed decision making.”
Where the ACS and ACOG/NCCN disagree is over the issue of the physical exam (abandoning CBE in average-risk women).
In regard to this last item, Dr. Pearlman says, “The ACS made a qualified recommendation against clinical breast exam. There is no high-level data to support such a marked change in practice. For example, when recommendations against breast self-examinations (BSE) were made, there were randomized controlled trials (RCTs) showing a lack of benefit and significant harms with BSE. With RCT-level data, it made sense to make a recommendation against the long-taught practice of SBE in average-risk women. That was not the case here. In fact, there are small amounts of data showing benefits of clinical breast exam.”
“One of my biggest concerns is not just the recommendation against CBE,” says Dr. Pearlman, “but that this may lead many women to interpret [this statement] as if they do not need to see their health care provider anymore. As you may recall, the American College of Physicians (ACP) recommended against annual pelvic examinations in asymptomatic patients. The ACS recommendation statement—taken together with the ACP statement—basically suggests that average-risk women don’t ever need to see a provider for a pelvic or breast examination except every 5 years for a Pap smear. That thinking does not recognize the importance of the clinical encounter (not just the CBE or pelvic exam), which is the opportunity to perform risk assessment and provide risk-reduction recommendations and healthy lifestyle recommendations.”
Radiologists resist new recommendations
Although the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) agree with the ACS that mammography screening saves lives and should be available to women aged 40 and older, the 2 imaging organizations continue to recommend that annual screening begin at age 40. Their rationale: The latest ACS breast cancer screening guidelines, and earlier data used by the USPSTF to create its recommendations, both note that starting annual mammography at age 40 “saves the most lives.”
Where the organizations differ from the ACR is summed up by a formal statement on the ACR Web site: “The ACR and SBI strongly encourage women to obtain the maximum lifesaving benefits from mammography by continuing to get annual screening.”4
When OBG Management touched base with radiologist Barbara Monsees, MD, professor of radiology and Evens Professor of Women’s Health at Washington University Medical Center in St. Louis, Missouri, she expressed dismay at early news reports on the ACS guidelines.
“I’m dismayed that the headlines don’t seem to correlate with what the ACS actually recommended. The ACS did not state that women should wait until age 45 to begin screening. I believe the ACS was going for a more nuanced approach, but since that’s a bit complicated, I think that reporters have misconstrued what was intended,” Dr. Monsees says.
“The ACS guideline says that women between 40 and 44 years should have the opportunity to begin annual screening,” she says, noting that this recommendation was graded as “qualified.”
“The ACS states that a qualified recommendation indicates that ‘there is clear evidence of benefit of screening, but less certainty about the balance of benefits and harms, or about patients’ values and preferences, which could lead to different decisions about screening.’” The guideline also articulates the view “that the meaning of a qualified recommendation for patients is that the ‘majority of individuals in this situation would want the suggested course of action, but many would not.’ Therefore, I find it mind-boggling that this has been interpreted to mean that women should not begin screening until age 45.”1
“It is my opinion that it is clear that if women want to achieve the most lifesaving benefit from screening, they should adhere to a schedule of yearly mammograms beginning at age 40,” says Dr. Monsees. However, she also agrees with the ACS notation that clinicians should acknowledge that “different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her values and preferences.”1
The word from an expert ObGyn
“By changing its guidance to begin screening at age 45 instead of 40, and in recommending biennial rather than annual screens in women 55 years of age and older, the updated ACS guidance will reduce harms (overdiagnosis and unnecessary additional imaging and biopsies) and moves closer to USPSTF guidance,” says Andrew M. Kaunitz, MD. He is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He also serves on the OBG Management Board of Editors.
“As one editorialist points out, the ACS recommendation that women begin screening at age 45 years is based on observational comparisons of screened and unscreened cohorts—a type of analysis which the USPSTF does not consider due to concerns regarding bias,” notes Dr. Kaunitz.5
“The ACS recommendation for annual screening in women aged 45 to 54 is largely based on the findings of a report showing that, for premenopausal (but not postmenopausal) women, tumor stage was higher and size larger for screen-detected lesions among women undergoing biennial screens."6
As for the recommendation against screening CBE, Dr. Kaunitz considers that “a dramatic change from prior guidance. It is based on the absence of data finding benefits with CBE (alone or with screening mammography). Furthermore, the updated ACS guidance does not change its 2003 guidance, which does not support routine performance of or instruction regarding SBE.”
“These updated ACS guidelines should result in more women starting screening mammograms later in life, and they endorse biennial screening for many women, meaning that patients following ACS guidance will have fewer lifetime screens than with earlier recommendations,” says Dr. Kaunitz.
“Another plus is that performing fewer breast examinations during well-woman visits will allow us more time to assess family history and other risk factors for breast cancer, and to discuss screening recommendations.”
The bottom line
What is one to make of the many viewpoints on screening? For now, it probably is best to adhere to either the new ACS guidelines or current ACOG guidelines (TABLE 2), says OBG Management Editor in Chief Robert L. Barbieri, MD. He is chief of the Department of Obstetrics and Gynecology at Brigham and Women’s Hospital in Boston, and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School.
TABLE 2 What are ACOG’s current recommendations?
|
ACOG recommends screening mammography every year for women starting at age 40. ACOG also states that “breast self-awareness has the potential to detect palpable breast cancer and can be recommended”; it also recommends CBE every year for women aged 19 or older.
These recommendations may change early next year, after ACOG convenes a consensus conference on the subject. The aim: “To develop a consistent set of uniform guidelines for breast cancer screening that can be implemented nationwide. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail.”2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- American College of Obstetricians and Gynecologists. ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 20, 2015.
- US Preventive Services Task Force. Email communication, USPSTF Newsroom, October 20, 2015.
- American College of Radiology. News Release: ACR and SBI Continue to Recommend Regular Mammography Starting at Age 40. http://www.acr.org/About-Us/Media-Center/Press-Releases/2015-Press-Releases/20151020-ACR-SBI-Recommend-Mammography-at-Age-40. Published October 20, 2015. Accessed October 21, 2015.
- Kerlikowske K. Progress toward consensus on breast cancer screening guidelines and reducing screening harms [published online ahead of print October 20, 2015]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6466.
- Miglioretti DL, Zhu W, Kerlikowske K, et al; Breast Cancer Surveillance Consortium. Breast tumor prognostic characteristics and biennial vs annual mammography, age, and menopausal status [published online ahead of print October 20, 2015]. JAMA. doi:10.1001/jamaoncol.2015.3084.
When the American Cancer Society (ACS) updated its guidelines for screening mammography earlier this week,1 the effect was that of a stone being tossed into a tranquil pond, generating ripples in all directions.
The new guidelines focus on women at average risk for breast cancer (TABLE 1) and were updated for the first time since 2003, based on new evidence, a new emphasis on eliminating as many screening harms as possible, and a goal of “supporting the interplay among values, preferences, informed decision making, and recommendations.”1 Earlier ACS guidelines recommended annual screening starting at age 40.
TABLE 1 What constitutes “average risk” of breast cancer?
|
The new guidelines are graded according to the strength of the rec ommendation as being either “strong” or “qualified.” The ACS defines a “strong” recommendation as one that most individuals should follow. “Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator,” the guidelines note.1
A “qualified” recommendation indicates that “Clinicians should acknowledge that different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her or his values and preferences.”1
The recommendations are:
- Regular screening mammography should start at age 45 years (strong recommendation)
- Screening should be annual in women aged 45 to 54 years (qualified recommendation)
- Screening should shift to biennial intervals at age 55, unless the patient prefers to continue screening annually (qualified recommendation)
- Women who desire to initiate annual screening between the ages of 40 and 44 years should be accommodated (qualified recommendation)
- Screening mammography should continue as long as the woman is in good health and has a life expectancy of at least 10 years (qualified recommendation)
- Clinical breast examination (CBE) is not recommended at any age (qualified recommendation).1
ACOG weighs in
Shortly after publication of the new ACS guidelines, the American College of Obstetricians and Gynecologists (ACOG) issued a formal statement in response2:
Response of the USPSTF
The US Preventive Services Task Force (USPSTF) also issued a statement in response to the new ACS guidelines:
The USPSTF currently recommends biennial screening beginning at age 50.
A leader in breast health cites pros and cons of ACS recommendations
Mark Pearlman, MD, professor of obstetrics and gynecology at the University of Michigan health system, is a nationally recognized expert on breast cancer screening. He sits on the National Comprehensive Cancer Network (NCCN) breast cancer screening and diagnosis group, helped author ACOG guidelines on mammography screening, and serves as a Contributing Editor to OBG Management.
“I believe the overall ACS mammography benefit evidence synthesis is reasonable and is in keeping with both NCCN and ACOG’s current recommendations. NCCN and ACOG mammography screening recommendations have both valued lives saved more highly than the ‘harms’ such as recalls and needle biopsies,” Dr. Pearlman says.
“If one combines ACS ‘strong’ and ‘qualified’ recommendations, ACS recommendations are similar to current ACOG and NCCN recommendations for mammography,” he adds.
Dr. Pearlman finds 7 areas of agreement between NCCN/ACOG and ACS recommendations, using both strong and qualified recommendations:
- “They reaffirm that screening from age 40 to 69 years is associated with a reduction in breast cancer deaths.
- They support annual screening for women in their 40s [although the ACS’ ‘strong’ recommendation is that regular screening begin at age 45 instead of 40].
- They support screening for women 70 and older who are in good health (10-year life expectancy).
- They support the finding that annual screening yields a larger mortality reduction than biennial screening.
- They confirm much uncertainty about the “over-diagnosis/overtreatment” issue.
- They endorse insurance coverage at all ages and intervals of screening (not just USPSTF ‘A’ or ‘B’ recommendations).
- They involve the patient in informed decision making.”
Where the ACS and ACOG/NCCN disagree is over the issue of the physical exam (abandoning CBE in average-risk women).
In regard to this last item, Dr. Pearlman says, “The ACS made a qualified recommendation against clinical breast exam. There is no high-level data to support such a marked change in practice. For example, when recommendations against breast self-examinations (BSE) were made, there were randomized controlled trials (RCTs) showing a lack of benefit and significant harms with BSE. With RCT-level data, it made sense to make a recommendation against the long-taught practice of SBE in average-risk women. That was not the case here. In fact, there are small amounts of data showing benefits of clinical breast exam.”
“One of my biggest concerns is not just the recommendation against CBE,” says Dr. Pearlman, “but that this may lead many women to interpret [this statement] as if they do not need to see their health care provider anymore. As you may recall, the American College of Physicians (ACP) recommended against annual pelvic examinations in asymptomatic patients. The ACS recommendation statement—taken together with the ACP statement—basically suggests that average-risk women don’t ever need to see a provider for a pelvic or breast examination except every 5 years for a Pap smear. That thinking does not recognize the importance of the clinical encounter (not just the CBE or pelvic exam), which is the opportunity to perform risk assessment and provide risk-reduction recommendations and healthy lifestyle recommendations.”
Radiologists resist new recommendations
Although the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) agree with the ACS that mammography screening saves lives and should be available to women aged 40 and older, the 2 imaging organizations continue to recommend that annual screening begin at age 40. Their rationale: The latest ACS breast cancer screening guidelines, and earlier data used by the USPSTF to create its recommendations, both note that starting annual mammography at age 40 “saves the most lives.”
Where the organizations differ from the ACR is summed up by a formal statement on the ACR Web site: “The ACR and SBI strongly encourage women to obtain the maximum lifesaving benefits from mammography by continuing to get annual screening.”4
When OBG Management touched base with radiologist Barbara Monsees, MD, professor of radiology and Evens Professor of Women’s Health at Washington University Medical Center in St. Louis, Missouri, she expressed dismay at early news reports on the ACS guidelines.
“I’m dismayed that the headlines don’t seem to correlate with what the ACS actually recommended. The ACS did not state that women should wait until age 45 to begin screening. I believe the ACS was going for a more nuanced approach, but since that’s a bit complicated, I think that reporters have misconstrued what was intended,” Dr. Monsees says.
“The ACS guideline says that women between 40 and 44 years should have the opportunity to begin annual screening,” she says, noting that this recommendation was graded as “qualified.”
“The ACS states that a qualified recommendation indicates that ‘there is clear evidence of benefit of screening, but less certainty about the balance of benefits and harms, or about patients’ values and preferences, which could lead to different decisions about screening.’” The guideline also articulates the view “that the meaning of a qualified recommendation for patients is that the ‘majority of individuals in this situation would want the suggested course of action, but many would not.’ Therefore, I find it mind-boggling that this has been interpreted to mean that women should not begin screening until age 45.”1
“It is my opinion that it is clear that if women want to achieve the most lifesaving benefit from screening, they should adhere to a schedule of yearly mammograms beginning at age 40,” says Dr. Monsees. However, she also agrees with the ACS notation that clinicians should acknowledge that “different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her values and preferences.”1
The word from an expert ObGyn
“By changing its guidance to begin screening at age 45 instead of 40, and in recommending biennial rather than annual screens in women 55 years of age and older, the updated ACS guidance will reduce harms (overdiagnosis and unnecessary additional imaging and biopsies) and moves closer to USPSTF guidance,” says Andrew M. Kaunitz, MD. He is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He also serves on the OBG Management Board of Editors.
“As one editorialist points out, the ACS recommendation that women begin screening at age 45 years is based on observational comparisons of screened and unscreened cohorts—a type of analysis which the USPSTF does not consider due to concerns regarding bias,” notes Dr. Kaunitz.5
“The ACS recommendation for annual screening in women aged 45 to 54 is largely based on the findings of a report showing that, for premenopausal (but not postmenopausal) women, tumor stage was higher and size larger for screen-detected lesions among women undergoing biennial screens."6
As for the recommendation against screening CBE, Dr. Kaunitz considers that “a dramatic change from prior guidance. It is based on the absence of data finding benefits with CBE (alone or with screening mammography). Furthermore, the updated ACS guidance does not change its 2003 guidance, which does not support routine performance of or instruction regarding SBE.”
“These updated ACS guidelines should result in more women starting screening mammograms later in life, and they endorse biennial screening for many women, meaning that patients following ACS guidance will have fewer lifetime screens than with earlier recommendations,” says Dr. Kaunitz.
“Another plus is that performing fewer breast examinations during well-woman visits will allow us more time to assess family history and other risk factors for breast cancer, and to discuss screening recommendations.”
The bottom line
What is one to make of the many viewpoints on screening? For now, it probably is best to adhere to either the new ACS guidelines or current ACOG guidelines (TABLE 2), says OBG Management Editor in Chief Robert L. Barbieri, MD. He is chief of the Department of Obstetrics and Gynecology at Brigham and Women’s Hospital in Boston, and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School.
TABLE 2 What are ACOG’s current recommendations?
|
ACOG recommends screening mammography every year for women starting at age 40. ACOG also states that “breast self-awareness has the potential to detect palpable breast cancer and can be recommended”; it also recommends CBE every year for women aged 19 or older.
These recommendations may change early next year, after ACOG convenes a consensus conference on the subject. The aim: “To develop a consistent set of uniform guidelines for breast cancer screening that can be implemented nationwide. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail.”2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
When the American Cancer Society (ACS) updated its guidelines for screening mammography earlier this week,1 the effect was that of a stone being tossed into a tranquil pond, generating ripples in all directions.
The new guidelines focus on women at average risk for breast cancer (TABLE 1) and were updated for the first time since 2003, based on new evidence, a new emphasis on eliminating as many screening harms as possible, and a goal of “supporting the interplay among values, preferences, informed decision making, and recommendations.”1 Earlier ACS guidelines recommended annual screening starting at age 40.
TABLE 1 What constitutes “average risk” of breast cancer?
|
The new guidelines are graded according to the strength of the rec ommendation as being either “strong” or “qualified.” The ACS defines a “strong” recommendation as one that most individuals should follow. “Adherence to this recommendation according to the guideline could be used as a quality criterion or performance indicator,” the guidelines note.1
A “qualified” recommendation indicates that “Clinicians should acknowledge that different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her or his values and preferences.”1
The recommendations are:
- Regular screening mammography should start at age 45 years (strong recommendation)
- Screening should be annual in women aged 45 to 54 years (qualified recommendation)
- Screening should shift to biennial intervals at age 55, unless the patient prefers to continue screening annually (qualified recommendation)
- Women who desire to initiate annual screening between the ages of 40 and 44 years should be accommodated (qualified recommendation)
- Screening mammography should continue as long as the woman is in good health and has a life expectancy of at least 10 years (qualified recommendation)
- Clinical breast examination (CBE) is not recommended at any age (qualified recommendation).1
ACOG weighs in
Shortly after publication of the new ACS guidelines, the American College of Obstetricians and Gynecologists (ACOG) issued a formal statement in response2:
Response of the USPSTF
The US Preventive Services Task Force (USPSTF) also issued a statement in response to the new ACS guidelines:
The USPSTF currently recommends biennial screening beginning at age 50.
A leader in breast health cites pros and cons of ACS recommendations
Mark Pearlman, MD, professor of obstetrics and gynecology at the University of Michigan health system, is a nationally recognized expert on breast cancer screening. He sits on the National Comprehensive Cancer Network (NCCN) breast cancer screening and diagnosis group, helped author ACOG guidelines on mammography screening, and serves as a Contributing Editor to OBG Management.
“I believe the overall ACS mammography benefit evidence synthesis is reasonable and is in keeping with both NCCN and ACOG’s current recommendations. NCCN and ACOG mammography screening recommendations have both valued lives saved more highly than the ‘harms’ such as recalls and needle biopsies,” Dr. Pearlman says.
“If one combines ACS ‘strong’ and ‘qualified’ recommendations, ACS recommendations are similar to current ACOG and NCCN recommendations for mammography,” he adds.
Dr. Pearlman finds 7 areas of agreement between NCCN/ACOG and ACS recommendations, using both strong and qualified recommendations:
- “They reaffirm that screening from age 40 to 69 years is associated with a reduction in breast cancer deaths.
- They support annual screening for women in their 40s [although the ACS’ ‘strong’ recommendation is that regular screening begin at age 45 instead of 40].
- They support screening for women 70 and older who are in good health (10-year life expectancy).
- They support the finding that annual screening yields a larger mortality reduction than biennial screening.
- They confirm much uncertainty about the “over-diagnosis/overtreatment” issue.
- They endorse insurance coverage at all ages and intervals of screening (not just USPSTF ‘A’ or ‘B’ recommendations).
- They involve the patient in informed decision making.”
Where the ACS and ACOG/NCCN disagree is over the issue of the physical exam (abandoning CBE in average-risk women).
In regard to this last item, Dr. Pearlman says, “The ACS made a qualified recommendation against clinical breast exam. There is no high-level data to support such a marked change in practice. For example, when recommendations against breast self-examinations (BSE) were made, there were randomized controlled trials (RCTs) showing a lack of benefit and significant harms with BSE. With RCT-level data, it made sense to make a recommendation against the long-taught practice of SBE in average-risk women. That was not the case here. In fact, there are small amounts of data showing benefits of clinical breast exam.”
“One of my biggest concerns is not just the recommendation against CBE,” says Dr. Pearlman, “but that this may lead many women to interpret [this statement] as if they do not need to see their health care provider anymore. As you may recall, the American College of Physicians (ACP) recommended against annual pelvic examinations in asymptomatic patients. The ACS recommendation statement—taken together with the ACP statement—basically suggests that average-risk women don’t ever need to see a provider for a pelvic or breast examination except every 5 years for a Pap smear. That thinking does not recognize the importance of the clinical encounter (not just the CBE or pelvic exam), which is the opportunity to perform risk assessment and provide risk-reduction recommendations and healthy lifestyle recommendations.”
Radiologists resist new recommendations
Although the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) agree with the ACS that mammography screening saves lives and should be available to women aged 40 and older, the 2 imaging organizations continue to recommend that annual screening begin at age 40. Their rationale: The latest ACS breast cancer screening guidelines, and earlier data used by the USPSTF to create its recommendations, both note that starting annual mammography at age 40 “saves the most lives.”
Where the organizations differ from the ACR is summed up by a formal statement on the ACR Web site: “The ACR and SBI strongly encourage women to obtain the maximum lifesaving benefits from mammography by continuing to get annual screening.”4
When OBG Management touched base with radiologist Barbara Monsees, MD, professor of radiology and Evens Professor of Women’s Health at Washington University Medical Center in St. Louis, Missouri, she expressed dismay at early news reports on the ACS guidelines.
“I’m dismayed that the headlines don’t seem to correlate with what the ACS actually recommended. The ACS did not state that women should wait until age 45 to begin screening. I believe the ACS was going for a more nuanced approach, but since that’s a bit complicated, I think that reporters have misconstrued what was intended,” Dr. Monsees says.
“The ACS guideline says that women between 40 and 44 years should have the opportunity to begin annual screening,” she says, noting that this recommendation was graded as “qualified.”
“The ACS states that a qualified recommendation indicates that ‘there is clear evidence of benefit of screening, but less certainty about the balance of benefits and harms, or about patients’ values and preferences, which could lead to different decisions about screening.’” The guideline also articulates the view “that the meaning of a qualified recommendation for patients is that the ‘majority of individuals in this situation would want the suggested course of action, but many would not.’ Therefore, I find it mind-boggling that this has been interpreted to mean that women should not begin screening until age 45.”1
“It is my opinion that it is clear that if women want to achieve the most lifesaving benefit from screening, they should adhere to a schedule of yearly mammograms beginning at age 40,” says Dr. Monsees. However, she also agrees with the ACS notation that clinicians should acknowledge that “different choices will be appropriate for different patients and that clinicians must help each patient arrive at a management decision consistent with her values and preferences.”1
The word from an expert ObGyn
“By changing its guidance to begin screening at age 45 instead of 40, and in recommending biennial rather than annual screens in women 55 years of age and older, the updated ACS guidance will reduce harms (overdiagnosis and unnecessary additional imaging and biopsies) and moves closer to USPSTF guidance,” says Andrew M. Kaunitz, MD. He is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, at the University of Florida College of Medicine–Jacksonville. He also serves on the OBG Management Board of Editors.
“As one editorialist points out, the ACS recommendation that women begin screening at age 45 years is based on observational comparisons of screened and unscreened cohorts—a type of analysis which the USPSTF does not consider due to concerns regarding bias,” notes Dr. Kaunitz.5
“The ACS recommendation for annual screening in women aged 45 to 54 is largely based on the findings of a report showing that, for premenopausal (but not postmenopausal) women, tumor stage was higher and size larger for screen-detected lesions among women undergoing biennial screens."6
As for the recommendation against screening CBE, Dr. Kaunitz considers that “a dramatic change from prior guidance. It is based on the absence of data finding benefits with CBE (alone or with screening mammography). Furthermore, the updated ACS guidance does not change its 2003 guidance, which does not support routine performance of or instruction regarding SBE.”
“These updated ACS guidelines should result in more women starting screening mammograms later in life, and they endorse biennial screening for many women, meaning that patients following ACS guidance will have fewer lifetime screens than with earlier recommendations,” says Dr. Kaunitz.
“Another plus is that performing fewer breast examinations during well-woman visits will allow us more time to assess family history and other risk factors for breast cancer, and to discuss screening recommendations.”
The bottom line
What is one to make of the many viewpoints on screening? For now, it probably is best to adhere to either the new ACS guidelines or current ACOG guidelines (TABLE 2), says OBG Management Editor in Chief Robert L. Barbieri, MD. He is chief of the Department of Obstetrics and Gynecology at Brigham and Women’s Hospital in Boston, and Kate Macy Ladd Professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School.
TABLE 2 What are ACOG’s current recommendations?
|
ACOG recommends screening mammography every year for women starting at age 40. ACOG also states that “breast self-awareness has the potential to detect palpable breast cancer and can be recommended”; it also recommends CBE every year for women aged 19 or older.
These recommendations may change early next year, after ACOG convenes a consensus conference on the subject. The aim: “To develop a consistent set of uniform guidelines for breast cancer screening that can be implemented nationwide. Major organizations and providers of women’s health care, including ACS, will gather to evaluate and interpret the data in greater detail.”2
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- American College of Obstetricians and Gynecologists. ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 20, 2015.
- US Preventive Services Task Force. Email communication, USPSTF Newsroom, October 20, 2015.
- American College of Radiology. News Release: ACR and SBI Continue to Recommend Regular Mammography Starting at Age 40. http://www.acr.org/About-Us/Media-Center/Press-Releases/2015-Press-Releases/20151020-ACR-SBI-Recommend-Mammography-at-Age-40. Published October 20, 2015. Accessed October 21, 2015.
- Kerlikowske K. Progress toward consensus on breast cancer screening guidelines and reducing screening harms [published online ahead of print October 20, 2015]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6466.
- Miglioretti DL, Zhu W, Kerlikowske K, et al; Breast Cancer Surveillance Consortium. Breast tumor prognostic characteristics and biennial vs annual mammography, age, and menopausal status [published online ahead of print October 20, 2015]. JAMA. doi:10.1001/jamaoncol.2015.3084.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk. 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- American College of Obstetricians and Gynecologists. ACOG Statement on Revised American Cancer Society Recommendations on Breast Cancer Screening. http://www.acog.org/About-ACOG/News-Room/Statements/2015/ACOG-Statement-on-Recommendations-on-Breast-Cancer-Screening. Published October 20, 2015. Accessed October 20, 2015.
- US Preventive Services Task Force. Email communication, USPSTF Newsroom, October 20, 2015.
- American College of Radiology. News Release: ACR and SBI Continue to Recommend Regular Mammography Starting at Age 40. http://www.acr.org/About-Us/Media-Center/Press-Releases/2015-Press-Releases/20151020-ACR-SBI-Recommend-Mammography-at-Age-40. Published October 20, 2015. Accessed October 21, 2015.
- Kerlikowske K. Progress toward consensus on breast cancer screening guidelines and reducing screening harms [published online ahead of print October 20, 2015]. JAMA Intern Med. doi:10.1001/jamainternmed.2015.6466.
- Miglioretti DL, Zhu W, Kerlikowske K, et al; Breast Cancer Surveillance Consortium. Breast tumor prognostic characteristics and biennial vs annual mammography, age, and menopausal status [published online ahead of print October 20, 2015]. JAMA. doi:10.1001/jamaoncol.2015.3084.