User login
Breast Cancer Chemoprevention: Hit It Harder
ESTES PARK, COLO. – Primary care physicians appear to have dropped the ball when it comes to primary chemoprevention of breast cancer, studies suggest.
Chemoprevention is enormously underutilized. An estimated 2 million American premenopausal women are candidates for primary chemoprevention of breast cancer with tamoxifen, an agent shown to reduce their risk by 50%. Yet only 4% of them are on this safe and generally well-tolerated estrogen receptor antagonist, Dr. Jennifer R. Diamond said at an update in internal medicine sponsored by the University of Colorado at Denver.
Moreover, when she informally polled her audience at the outset of her talk, 93% indicated via electronic clicker that they were not comfortable with chemoprevention for breast cancer and didn’t commonly use it in appropriately selected patients in their practice.
"The most common side effect I see with tamoxifen for primary chemoprevention is hot flashes. But many young women will do fine. They don’t have any problems. And the opportunity to reduce the risk of breast cancer by 50% in these young women makes this an option I think you really need to be offering to young women" who are at increased risk for breast cancer, said Dr. Diamond, a medical oncologist at the university.
Nearly 230,000 American women will receive a new diagnosis of breast cancer in 2012. More than 39,000 women will die this year from the malignancy.
Secondary chemoprevention is most effective for women who have been diagnosed with lobular carcinoma in situ. The recommendation to embark on secondary chemoprevention usually comes from the patient’s medical oncologist.
In contrast, most candidates for primary chemoprevention have never seen a medical oncologist. Thus, primary chemoprevention falls within the bailiwick of primary care physicians. The latest guidelines from the National Comprehensive Cancer Network identify appropriate candidates for primary chemoprevention as women who have a first-degree relative with breast or ovarian cancer; a history of thoracic irradiation; mutations predisposing to breast cancer; or a 5-year risk of breast cancer of at least 1.7% according to the breast cancer risk assessment tool (the Gail model).
A 5-year risk of 1.7% or greater is not a high bar. It equates on the Gail model to being 65 years old without additional risk factors. "You’ll find that many of your patients are candidates," Dr. Diamond predicted.
Two options are available for primary chemoprevention; the determining factor as to which is best in a given high-risk individual is menopausal status. Premenopausal women can benefit from 5 years of oral tamoxifen at 20 mg/day. In postmenopausal women, however, exemestane (Aromasin), an aromatase inhibitor, is the safer, better choice, even though the drug’s use in chemoprevention is, for now, off label, she continued.
The oft-cited figure of a 50% reduction in breast cancer risk conferred by tamoxifen comes from the landmark randomized, placebo-controlled NSABP (National Surgical Adjuvant Breast and Bowel Project) P-1 trial (J. Natl. Cancer Inst. 1998;90:1371-88). The protective effect continued after treatment ended. The number needed to treat at 20 mg/day for 5 years in order to prevent one additional case of breast cancer was calculated at 95 in 5 years and 56 in 10 years. Women younger than age 50 years experienced no excess risk of serious adverse events.
"The risks of venous thromboembolism and endometrial cancer are what we all worry about with tamoxifen, but they’re actually incredibly uncommon" in women younger than age 50, she said. "I don’t recommend that you use tamoxifen in your postmenopausal women; that’s where you get into trouble with endometrial cancer and thromboembolic events. I believe that you can safely use tamoxifen in premenopausal women without a significantly increased risk of thromboembolic events. I equate the risk to that of birth control pills."
Raloxifene joins tamoxifen as the only other proved drug with Food and Drug Administration approval for primary breast cancer chemoprevention. The NSABP STAR (Study of Tamoxifen and Raloxifene) trial showed that the two medications are equivalent for prevention of invasive breast cancer, but that raloxifene is less effective in preventing ductal carcinoma in situ (JAMA 2006;295:2727-41). For this reason, Dr. Diamond and her colleagues don’t use it.
For postmenopausal women who are candidates for primary chemoprevention, Dr. Diamond said that she turns to exemestane on the basis of the National Cancer Institute of Canada CTG MAP-3 trial, which showed a 65% reduction in the annual incidence of breast cancer with 5 years of the aromatase inhibitor, compared with placebo. (N. Engl. J. Med. 2011;364:2381-91).
The number needed to treat with exemestane at 25 mg/day for 5 years in order to prevent one invasive breast cancer was 94 in 3 years and 26 in 5 years.
"I would argue that this is a really low NNT, and a lot of patients in your practice probably would fall into the category of qualifying for the MAP-3 study," Dr. Diamond said.
There were no serious risks associated with exemestane in MAP-3. Hot flashes and other menopausal symptoms were more common than with placebo, yet reassuringly there was no difference between the exemestane and control groups on quality of life measures.
Bone mineral density decreased over time in the exemestane group; however, patients on the aromatase inhibitor had no increased risk of fractures. Dr. Diamond advised monitoring bone density in exemestane-treated women, and if it drops significantly, consider prescribing denosumab as a subcutaneous injection once every 6 months. Denosumab is already FDA approved to increase bone mass in patients on adjuvant aromatase inhibitor therapy for breast cancer.
Dr. Diamond reported having no financial conflicts.
ESTES PARK, COLO. – Primary care physicians appear to have dropped the ball when it comes to primary chemoprevention of breast cancer, studies suggest.
Chemoprevention is enormously underutilized. An estimated 2 million American premenopausal women are candidates for primary chemoprevention of breast cancer with tamoxifen, an agent shown to reduce their risk by 50%. Yet only 4% of them are on this safe and generally well-tolerated estrogen receptor antagonist, Dr. Jennifer R. Diamond said at an update in internal medicine sponsored by the University of Colorado at Denver.
Moreover, when she informally polled her audience at the outset of her talk, 93% indicated via electronic clicker that they were not comfortable with chemoprevention for breast cancer and didn’t commonly use it in appropriately selected patients in their practice.
"The most common side effect I see with tamoxifen for primary chemoprevention is hot flashes. But many young women will do fine. They don’t have any problems. And the opportunity to reduce the risk of breast cancer by 50% in these young women makes this an option I think you really need to be offering to young women" who are at increased risk for breast cancer, said Dr. Diamond, a medical oncologist at the university.
Nearly 230,000 American women will receive a new diagnosis of breast cancer in 2012. More than 39,000 women will die this year from the malignancy.
Secondary chemoprevention is most effective for women who have been diagnosed with lobular carcinoma in situ. The recommendation to embark on secondary chemoprevention usually comes from the patient’s medical oncologist.
In contrast, most candidates for primary chemoprevention have never seen a medical oncologist. Thus, primary chemoprevention falls within the bailiwick of primary care physicians. The latest guidelines from the National Comprehensive Cancer Network identify appropriate candidates for primary chemoprevention as women who have a first-degree relative with breast or ovarian cancer; a history of thoracic irradiation; mutations predisposing to breast cancer; or a 5-year risk of breast cancer of at least 1.7% according to the breast cancer risk assessment tool (the Gail model).
A 5-year risk of 1.7% or greater is not a high bar. It equates on the Gail model to being 65 years old without additional risk factors. "You’ll find that many of your patients are candidates," Dr. Diamond predicted.
Two options are available for primary chemoprevention; the determining factor as to which is best in a given high-risk individual is menopausal status. Premenopausal women can benefit from 5 years of oral tamoxifen at 20 mg/day. In postmenopausal women, however, exemestane (Aromasin), an aromatase inhibitor, is the safer, better choice, even though the drug’s use in chemoprevention is, for now, off label, she continued.
The oft-cited figure of a 50% reduction in breast cancer risk conferred by tamoxifen comes from the landmark randomized, placebo-controlled NSABP (National Surgical Adjuvant Breast and Bowel Project) P-1 trial (J. Natl. Cancer Inst. 1998;90:1371-88). The protective effect continued after treatment ended. The number needed to treat at 20 mg/day for 5 years in order to prevent one additional case of breast cancer was calculated at 95 in 5 years and 56 in 10 years. Women younger than age 50 years experienced no excess risk of serious adverse events.
"The risks of venous thromboembolism and endometrial cancer are what we all worry about with tamoxifen, but they’re actually incredibly uncommon" in women younger than age 50, she said. "I don’t recommend that you use tamoxifen in your postmenopausal women; that’s where you get into trouble with endometrial cancer and thromboembolic events. I believe that you can safely use tamoxifen in premenopausal women without a significantly increased risk of thromboembolic events. I equate the risk to that of birth control pills."
Raloxifene joins tamoxifen as the only other proved drug with Food and Drug Administration approval for primary breast cancer chemoprevention. The NSABP STAR (Study of Tamoxifen and Raloxifene) trial showed that the two medications are equivalent for prevention of invasive breast cancer, but that raloxifene is less effective in preventing ductal carcinoma in situ (JAMA 2006;295:2727-41). For this reason, Dr. Diamond and her colleagues don’t use it.
For postmenopausal women who are candidates for primary chemoprevention, Dr. Diamond said that she turns to exemestane on the basis of the National Cancer Institute of Canada CTG MAP-3 trial, which showed a 65% reduction in the annual incidence of breast cancer with 5 years of the aromatase inhibitor, compared with placebo. (N. Engl. J. Med. 2011;364:2381-91).
The number needed to treat with exemestane at 25 mg/day for 5 years in order to prevent one invasive breast cancer was 94 in 3 years and 26 in 5 years.
"I would argue that this is a really low NNT, and a lot of patients in your practice probably would fall into the category of qualifying for the MAP-3 study," Dr. Diamond said.
There were no serious risks associated with exemestane in MAP-3. Hot flashes and other menopausal symptoms were more common than with placebo, yet reassuringly there was no difference between the exemestane and control groups on quality of life measures.
Bone mineral density decreased over time in the exemestane group; however, patients on the aromatase inhibitor had no increased risk of fractures. Dr. Diamond advised monitoring bone density in exemestane-treated women, and if it drops significantly, consider prescribing denosumab as a subcutaneous injection once every 6 months. Denosumab is already FDA approved to increase bone mass in patients on adjuvant aromatase inhibitor therapy for breast cancer.
Dr. Diamond reported having no financial conflicts.
ESTES PARK, COLO. – Primary care physicians appear to have dropped the ball when it comes to primary chemoprevention of breast cancer, studies suggest.
Chemoprevention is enormously underutilized. An estimated 2 million American premenopausal women are candidates for primary chemoprevention of breast cancer with tamoxifen, an agent shown to reduce their risk by 50%. Yet only 4% of them are on this safe and generally well-tolerated estrogen receptor antagonist, Dr. Jennifer R. Diamond said at an update in internal medicine sponsored by the University of Colorado at Denver.
Moreover, when she informally polled her audience at the outset of her talk, 93% indicated via electronic clicker that they were not comfortable with chemoprevention for breast cancer and didn’t commonly use it in appropriately selected patients in their practice.
"The most common side effect I see with tamoxifen for primary chemoprevention is hot flashes. But many young women will do fine. They don’t have any problems. And the opportunity to reduce the risk of breast cancer by 50% in these young women makes this an option I think you really need to be offering to young women" who are at increased risk for breast cancer, said Dr. Diamond, a medical oncologist at the university.
Nearly 230,000 American women will receive a new diagnosis of breast cancer in 2012. More than 39,000 women will die this year from the malignancy.
Secondary chemoprevention is most effective for women who have been diagnosed with lobular carcinoma in situ. The recommendation to embark on secondary chemoprevention usually comes from the patient’s medical oncologist.
In contrast, most candidates for primary chemoprevention have never seen a medical oncologist. Thus, primary chemoprevention falls within the bailiwick of primary care physicians. The latest guidelines from the National Comprehensive Cancer Network identify appropriate candidates for primary chemoprevention as women who have a first-degree relative with breast or ovarian cancer; a history of thoracic irradiation; mutations predisposing to breast cancer; or a 5-year risk of breast cancer of at least 1.7% according to the breast cancer risk assessment tool (the Gail model).
A 5-year risk of 1.7% or greater is not a high bar. It equates on the Gail model to being 65 years old without additional risk factors. "You’ll find that many of your patients are candidates," Dr. Diamond predicted.
Two options are available for primary chemoprevention; the determining factor as to which is best in a given high-risk individual is menopausal status. Premenopausal women can benefit from 5 years of oral tamoxifen at 20 mg/day. In postmenopausal women, however, exemestane (Aromasin), an aromatase inhibitor, is the safer, better choice, even though the drug’s use in chemoprevention is, for now, off label, she continued.
The oft-cited figure of a 50% reduction in breast cancer risk conferred by tamoxifen comes from the landmark randomized, placebo-controlled NSABP (National Surgical Adjuvant Breast and Bowel Project) P-1 trial (J. Natl. Cancer Inst. 1998;90:1371-88). The protective effect continued after treatment ended. The number needed to treat at 20 mg/day for 5 years in order to prevent one additional case of breast cancer was calculated at 95 in 5 years and 56 in 10 years. Women younger than age 50 years experienced no excess risk of serious adverse events.
"The risks of venous thromboembolism and endometrial cancer are what we all worry about with tamoxifen, but they’re actually incredibly uncommon" in women younger than age 50, she said. "I don’t recommend that you use tamoxifen in your postmenopausal women; that’s where you get into trouble with endometrial cancer and thromboembolic events. I believe that you can safely use tamoxifen in premenopausal women without a significantly increased risk of thromboembolic events. I equate the risk to that of birth control pills."
Raloxifene joins tamoxifen as the only other proved drug with Food and Drug Administration approval for primary breast cancer chemoprevention. The NSABP STAR (Study of Tamoxifen and Raloxifene) trial showed that the two medications are equivalent for prevention of invasive breast cancer, but that raloxifene is less effective in preventing ductal carcinoma in situ (JAMA 2006;295:2727-41). For this reason, Dr. Diamond and her colleagues don’t use it.
For postmenopausal women who are candidates for primary chemoprevention, Dr. Diamond said that she turns to exemestane on the basis of the National Cancer Institute of Canada CTG MAP-3 trial, which showed a 65% reduction in the annual incidence of breast cancer with 5 years of the aromatase inhibitor, compared with placebo. (N. Engl. J. Med. 2011;364:2381-91).
The number needed to treat with exemestane at 25 mg/day for 5 years in order to prevent one invasive breast cancer was 94 in 3 years and 26 in 5 years.
"I would argue that this is a really low NNT, and a lot of patients in your practice probably would fall into the category of qualifying for the MAP-3 study," Dr. Diamond said.
There were no serious risks associated with exemestane in MAP-3. Hot flashes and other menopausal symptoms were more common than with placebo, yet reassuringly there was no difference between the exemestane and control groups on quality of life measures.
Bone mineral density decreased over time in the exemestane group; however, patients on the aromatase inhibitor had no increased risk of fractures. Dr. Diamond advised monitoring bone density in exemestane-treated women, and if it drops significantly, consider prescribing denosumab as a subcutaneous injection once every 6 months. Denosumab is already FDA approved to increase bone mass in patients on adjuvant aromatase inhibitor therapy for breast cancer.
Dr. Diamond reported having no financial conflicts.
EXPERT ANALYSIS FROM AN UPDATE IN INTERNAL MEDICINE SPONSORED BY THE UNIVERSITY OF COLORADO
Dense Breasts Don't Increase Risk of Breast Cancer Death
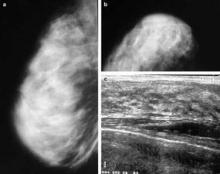
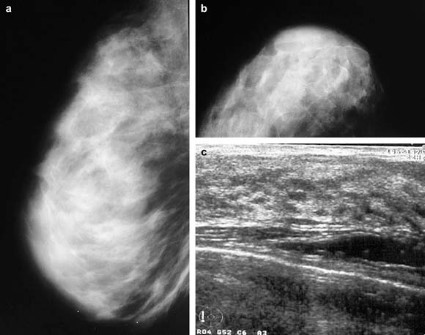
High mammographic breast density is associated with increased risk of developing breast cancer, but not with increased risk of death among those diagnosed with breast cancer, according to an analysis of data from the U.S. Breast Cancer Surveillance Consortium.
Low breast density is associated with an increased risk of breast cancer death, however, in women who are obese or who have large or high-grade tumors, Gretchen L. Gierach, Ph.D., of the National Cancer Institute and her colleagues reported.
Specifically, the elevated risk was apparent for obese women (body mass index 30 kg/m2 or greater) with "almost entirely fatty breasts." This association was not apparent in overweight or lean women.
"One explanation for the increased risks associated with low density among some subgroups is that breasts with a higher percentage of fat may contribute to a tumor microenvironment that facilitates cancer growth and progression," the investigators suggested.
The findings were published Aug. 20 online in the Journal of the National Cancer Institute.
Prior studies have demonstrated that elevated mammographic breast density is among the strongest risk factors for nonfamilial breast cancer. High breast density is also associated with breast cancer risk factors including nulliparity, a positive family history of breast cancer, and menopausal hormone therapy use, but studies have consistently demonstrated that "compared with low density, high density confers relative risks of four- to fivefold for breast cancer, independent of these and other factors," the investigators said.
The association between breast density and death among those diagnosed with breast cancer has remained unclear, however. To assess this relationship, they analyzed data from the U.S. Breast Cancer Surveillance Consortium (BCSC) – a National Cancer Institute–sponsored population-based registry of breast imaging facilities.
"The BCSC offers several advantages for studying these associations relative to other studies, including the prospective follow-up of a large number of breast cancer patients with detailed information regarding potential confounding factors, including BMI, as well as on screening history, tumor characteristics, and treatment," the investigators noted.
The analysis was restricted to women aged 30 years and older at the time of diagnosis with primary incident invasive breast carcinoma. Breast cancer pathology and vital status data were obtained through the Surveillance, Epidemiology, and End Results (SEER) program and by linkage to state cancer registries and/or pathology databases. Breast density data were collected according to the American College of Radiology’s Breast Imaging Reporting and Data System, or BI-RADS, which rates density in categories from 1 (almost entirely fat) to 4 (extremely dense).
The study population comprised 9,232 women diagnosed with primary invasive breast cancer between 1996 and 2005 and followed for a mean of 6.6 years (60,759 person-years) as part of the consortium. Of these 1,795 died, including 889 who died from their breast cancer.
After adjustment for site, age at diagnosis, year of diagnosis, American Joint Committee on Cancer stage, BMI, mode of detection, treatment, and income, no significant association was found between BI-RADS 4 density and death from breast cancer (hazard ratio, 0.92) or death from all causes (HR, 0.83), compared with BI-RADS 2 (scattered fibroglandular densities).
Women with BI-RADS 1 density had an elevated risk for breast cancer death (HR, 1.36), and that risk was further increased among those with tumors of at least 2.0 cm (HR, 1.55), and those with high-grade tumors (HR, 1.45), the investigators reported (J. Natl. Cancer Inst. 2012 Aug. 20 [doi: 10.1093/jnci/djs327]).
BMI was found to modify the relationship between breast density and risk of breast cancer death (P for interaction = .007). The investigators reported a hazard ratio of 2.02 in obese women with "almost entirely fatty" breasts, and noted that it remained apparent even if morbidly obese women with BMI greater than 40 were excluded.
Although the study is limited by "moderate interobserver reliability" with respect to BI-RADS density assessment, and by the fact that that detailed, cumulative information on treatment, comorbidities, and changes in weight after diagnosis was limited, the findings raise additional questions about possible interactions between breast density, other patient characteristics, and subsequent treatment, the investigators said.
"It is reassuring that elevated breast density, a prevalent and strong breast cancer risk factor, was not associated with risk of breast cancer death or death from any cause in this large, prospective study," they said.
"However, we identified subsets of women with breast cancer for whom low density was associated with adverse prognoses, highlighting the possibility of integrating breast density with epidemiological data and other measurements to understand mechanisms of breast carcinogenesis and to identify women who are likely to develop aggressive cancers, which might be preventable or detectable through specific interventions," they said.
The findings underscore the need for improved understanding of the biological characteristics of, and the relationships between breast tissue components responsible for inter-individual variations in breast density, they added.
This study was supported by the Intramural Research Program of the National Institutes of Health, the National Cancer Institute (NCI), and the NCI-funded BCSC.
High mammographic breast density is associated with increased risk of developing breast cancer, but not with increased risk of death among those diagnosed with breast cancer, according to an analysis of data from the U.S. Breast Cancer Surveillance Consortium.
Low breast density is associated with an increased risk of breast cancer death, however, in women who are obese or who have large or high-grade tumors, Gretchen L. Gierach, Ph.D., of the National Cancer Institute and her colleagues reported.
Specifically, the elevated risk was apparent for obese women (body mass index 30 kg/m2 or greater) with "almost entirely fatty breasts." This association was not apparent in overweight or lean women.
"One explanation for the increased risks associated with low density among some subgroups is that breasts with a higher percentage of fat may contribute to a tumor microenvironment that facilitates cancer growth and progression," the investigators suggested.
The findings were published Aug. 20 online in the Journal of the National Cancer Institute.
Prior studies have demonstrated that elevated mammographic breast density is among the strongest risk factors for nonfamilial breast cancer. High breast density is also associated with breast cancer risk factors including nulliparity, a positive family history of breast cancer, and menopausal hormone therapy use, but studies have consistently demonstrated that "compared with low density, high density confers relative risks of four- to fivefold for breast cancer, independent of these and other factors," the investigators said.
The association between breast density and death among those diagnosed with breast cancer has remained unclear, however. To assess this relationship, they analyzed data from the U.S. Breast Cancer Surveillance Consortium (BCSC) – a National Cancer Institute–sponsored population-based registry of breast imaging facilities.
"The BCSC offers several advantages for studying these associations relative to other studies, including the prospective follow-up of a large number of breast cancer patients with detailed information regarding potential confounding factors, including BMI, as well as on screening history, tumor characteristics, and treatment," the investigators noted.
The analysis was restricted to women aged 30 years and older at the time of diagnosis with primary incident invasive breast carcinoma. Breast cancer pathology and vital status data were obtained through the Surveillance, Epidemiology, and End Results (SEER) program and by linkage to state cancer registries and/or pathology databases. Breast density data were collected according to the American College of Radiology’s Breast Imaging Reporting and Data System, or BI-RADS, which rates density in categories from 1 (almost entirely fat) to 4 (extremely dense).
The study population comprised 9,232 women diagnosed with primary invasive breast cancer between 1996 and 2005 and followed for a mean of 6.6 years (60,759 person-years) as part of the consortium. Of these 1,795 died, including 889 who died from their breast cancer.
After adjustment for site, age at diagnosis, year of diagnosis, American Joint Committee on Cancer stage, BMI, mode of detection, treatment, and income, no significant association was found between BI-RADS 4 density and death from breast cancer (hazard ratio, 0.92) or death from all causes (HR, 0.83), compared with BI-RADS 2 (scattered fibroglandular densities).
Women with BI-RADS 1 density had an elevated risk for breast cancer death (HR, 1.36), and that risk was further increased among those with tumors of at least 2.0 cm (HR, 1.55), and those with high-grade tumors (HR, 1.45), the investigators reported (J. Natl. Cancer Inst. 2012 Aug. 20 [doi: 10.1093/jnci/djs327]).
BMI was found to modify the relationship between breast density and risk of breast cancer death (P for interaction = .007). The investigators reported a hazard ratio of 2.02 in obese women with "almost entirely fatty" breasts, and noted that it remained apparent even if morbidly obese women with BMI greater than 40 were excluded.
Although the study is limited by "moderate interobserver reliability" with respect to BI-RADS density assessment, and by the fact that that detailed, cumulative information on treatment, comorbidities, and changes in weight after diagnosis was limited, the findings raise additional questions about possible interactions between breast density, other patient characteristics, and subsequent treatment, the investigators said.
"It is reassuring that elevated breast density, a prevalent and strong breast cancer risk factor, was not associated with risk of breast cancer death or death from any cause in this large, prospective study," they said.
"However, we identified subsets of women with breast cancer for whom low density was associated with adverse prognoses, highlighting the possibility of integrating breast density with epidemiological data and other measurements to understand mechanisms of breast carcinogenesis and to identify women who are likely to develop aggressive cancers, which might be preventable or detectable through specific interventions," they said.
The findings underscore the need for improved understanding of the biological characteristics of, and the relationships between breast tissue components responsible for inter-individual variations in breast density, they added.
This study was supported by the Intramural Research Program of the National Institutes of Health, the National Cancer Institute (NCI), and the NCI-funded BCSC.
High mammographic breast density is associated with increased risk of developing breast cancer, but not with increased risk of death among those diagnosed with breast cancer, according to an analysis of data from the U.S. Breast Cancer Surveillance Consortium.
Low breast density is associated with an increased risk of breast cancer death, however, in women who are obese or who have large or high-grade tumors, Gretchen L. Gierach, Ph.D., of the National Cancer Institute and her colleagues reported.
Specifically, the elevated risk was apparent for obese women (body mass index 30 kg/m2 or greater) with "almost entirely fatty breasts." This association was not apparent in overweight or lean women.
"One explanation for the increased risks associated with low density among some subgroups is that breasts with a higher percentage of fat may contribute to a tumor microenvironment that facilitates cancer growth and progression," the investigators suggested.
The findings were published Aug. 20 online in the Journal of the National Cancer Institute.
Prior studies have demonstrated that elevated mammographic breast density is among the strongest risk factors for nonfamilial breast cancer. High breast density is also associated with breast cancer risk factors including nulliparity, a positive family history of breast cancer, and menopausal hormone therapy use, but studies have consistently demonstrated that "compared with low density, high density confers relative risks of four- to fivefold for breast cancer, independent of these and other factors," the investigators said.
The association between breast density and death among those diagnosed with breast cancer has remained unclear, however. To assess this relationship, they analyzed data from the U.S. Breast Cancer Surveillance Consortium (BCSC) – a National Cancer Institute–sponsored population-based registry of breast imaging facilities.
"The BCSC offers several advantages for studying these associations relative to other studies, including the prospective follow-up of a large number of breast cancer patients with detailed information regarding potential confounding factors, including BMI, as well as on screening history, tumor characteristics, and treatment," the investigators noted.
The analysis was restricted to women aged 30 years and older at the time of diagnosis with primary incident invasive breast carcinoma. Breast cancer pathology and vital status data were obtained through the Surveillance, Epidemiology, and End Results (SEER) program and by linkage to state cancer registries and/or pathology databases. Breast density data were collected according to the American College of Radiology’s Breast Imaging Reporting and Data System, or BI-RADS, which rates density in categories from 1 (almost entirely fat) to 4 (extremely dense).
The study population comprised 9,232 women diagnosed with primary invasive breast cancer between 1996 and 2005 and followed for a mean of 6.6 years (60,759 person-years) as part of the consortium. Of these 1,795 died, including 889 who died from their breast cancer.
After adjustment for site, age at diagnosis, year of diagnosis, American Joint Committee on Cancer stage, BMI, mode of detection, treatment, and income, no significant association was found between BI-RADS 4 density and death from breast cancer (hazard ratio, 0.92) or death from all causes (HR, 0.83), compared with BI-RADS 2 (scattered fibroglandular densities).
Women with BI-RADS 1 density had an elevated risk for breast cancer death (HR, 1.36), and that risk was further increased among those with tumors of at least 2.0 cm (HR, 1.55), and those with high-grade tumors (HR, 1.45), the investigators reported (J. Natl. Cancer Inst. 2012 Aug. 20 [doi: 10.1093/jnci/djs327]).
BMI was found to modify the relationship between breast density and risk of breast cancer death (P for interaction = .007). The investigators reported a hazard ratio of 2.02 in obese women with "almost entirely fatty" breasts, and noted that it remained apparent even if morbidly obese women with BMI greater than 40 were excluded.
Although the study is limited by "moderate interobserver reliability" with respect to BI-RADS density assessment, and by the fact that that detailed, cumulative information on treatment, comorbidities, and changes in weight after diagnosis was limited, the findings raise additional questions about possible interactions between breast density, other patient characteristics, and subsequent treatment, the investigators said.
"It is reassuring that elevated breast density, a prevalent and strong breast cancer risk factor, was not associated with risk of breast cancer death or death from any cause in this large, prospective study," they said.
"However, we identified subsets of women with breast cancer for whom low density was associated with adverse prognoses, highlighting the possibility of integrating breast density with epidemiological data and other measurements to understand mechanisms of breast carcinogenesis and to identify women who are likely to develop aggressive cancers, which might be preventable or detectable through specific interventions," they said.
The findings underscore the need for improved understanding of the biological characteristics of, and the relationships between breast tissue components responsible for inter-individual variations in breast density, they added.
This study was supported by the Intramural Research Program of the National Institutes of Health, the National Cancer Institute (NCI), and the NCI-funded BCSC.
FROM THE JOURNAL OF THE NATIONAL CANCER INSTITUTE
Prior Thoracic Radiotherapy Warrants Annual Breast MRI
ESTES PARK, COLO. – Primary care physicians are uniquely positioned to help their younger adult female patients who have a history of thoracic radiation therapy for lymphoma by arranging for them to begin undergoing annual screening breast MRI, Dr. Jennifer R. Diamond said.
"That mantle cell radiation includes the upper inner quadrants of both breasts; those patients are at extremely high risk for developing breast cancer," explained Dr. Diamond, a medical oncologist at the University of Colorado, Aurora. "Many times, they’re no longer being followed by their oncologist, and it’s up to their primary care physician to pull the trigger and order the test."
Many patients likely wouldn’t know that they should do breast cancer screening at such an early age, she added, because breast cancer wasn’t an anticipated outcome back when they had their radiotherapy.
National Comprehensive Cancer Network guidelines call for annual breast MRI and mammography along with clinical breast exams every 6-12 months, beginning 8-10 years after thoracic radiotherapy or at age 25 years, whichever occurs later. Dr. Diamond typically has patients stagger the two imaging modalities 6 months apart.
Both annual breast MRI and mammography are necessary. Screening MRI is far more sensitive than mammography alone in high-risk women, and it leads to cancer diagnosis at an earlier stage. However, MRI can miss ductal carcinoma in situ that would be evident as abnormal calcifications on screening mammography, she continued.
Annual breast MRI, in addition to mammography, is also indicated for women at high breast cancer risk as defined by a lifetime estimated risk in excess of 20%, or because they possess a BRCA 1 or 2 mutation, according to the NCCN. Dr. Diamond recommended BRCAPRO as a very useful tool for estimating the lifetime risk of breast cancer in women with no previous breast cancer.
In response to an audience question, she said she’s had no problem in getting insurers to pay for annual breast MRI to supplement annual mammography, so long as she clearly documents in her note that the patient has a greater than 20% lifetime estimated risk of breast cancer.
"They won’t cover it even a week earlier than annually, though," Dr. Diamond added.
She is a big fan of breast tomosynthesis, also known as three-dimensional mammography. The Food and Drug Administration–licensed technology produces a 3-D view of the breast tissue in addition to the standard two-dimensional images, all obtained in one compression with only about 2 seconds of additional compression time. Studies have shown that this tool substantially reduces patient recall rates for nondefinitive mammograms, Dr. Diamond said.
"It allows the mammographer to scroll through the breast, looking up and down sort of like with a CT scan, but without the same radiation exposure," she explained. "It’s a really great new technology, and I think most mammography centers will increasingly turn to it."
Dr. Diamond reported having no financial conflicts.
ESTES PARK, COLO. – Primary care physicians are uniquely positioned to help their younger adult female patients who have a history of thoracic radiation therapy for lymphoma by arranging for them to begin undergoing annual screening breast MRI, Dr. Jennifer R. Diamond said.
"That mantle cell radiation includes the upper inner quadrants of both breasts; those patients are at extremely high risk for developing breast cancer," explained Dr. Diamond, a medical oncologist at the University of Colorado, Aurora. "Many times, they’re no longer being followed by their oncologist, and it’s up to their primary care physician to pull the trigger and order the test."
Many patients likely wouldn’t know that they should do breast cancer screening at such an early age, she added, because breast cancer wasn’t an anticipated outcome back when they had their radiotherapy.
National Comprehensive Cancer Network guidelines call for annual breast MRI and mammography along with clinical breast exams every 6-12 months, beginning 8-10 years after thoracic radiotherapy or at age 25 years, whichever occurs later. Dr. Diamond typically has patients stagger the two imaging modalities 6 months apart.
Both annual breast MRI and mammography are necessary. Screening MRI is far more sensitive than mammography alone in high-risk women, and it leads to cancer diagnosis at an earlier stage. However, MRI can miss ductal carcinoma in situ that would be evident as abnormal calcifications on screening mammography, she continued.
Annual breast MRI, in addition to mammography, is also indicated for women at high breast cancer risk as defined by a lifetime estimated risk in excess of 20%, or because they possess a BRCA 1 or 2 mutation, according to the NCCN. Dr. Diamond recommended BRCAPRO as a very useful tool for estimating the lifetime risk of breast cancer in women with no previous breast cancer.
In response to an audience question, she said she’s had no problem in getting insurers to pay for annual breast MRI to supplement annual mammography, so long as she clearly documents in her note that the patient has a greater than 20% lifetime estimated risk of breast cancer.
"They won’t cover it even a week earlier than annually, though," Dr. Diamond added.
She is a big fan of breast tomosynthesis, also known as three-dimensional mammography. The Food and Drug Administration–licensed technology produces a 3-D view of the breast tissue in addition to the standard two-dimensional images, all obtained in one compression with only about 2 seconds of additional compression time. Studies have shown that this tool substantially reduces patient recall rates for nondefinitive mammograms, Dr. Diamond said.
"It allows the mammographer to scroll through the breast, looking up and down sort of like with a CT scan, but without the same radiation exposure," she explained. "It’s a really great new technology, and I think most mammography centers will increasingly turn to it."
Dr. Diamond reported having no financial conflicts.
ESTES PARK, COLO. – Primary care physicians are uniquely positioned to help their younger adult female patients who have a history of thoracic radiation therapy for lymphoma by arranging for them to begin undergoing annual screening breast MRI, Dr. Jennifer R. Diamond said.
"That mantle cell radiation includes the upper inner quadrants of both breasts; those patients are at extremely high risk for developing breast cancer," explained Dr. Diamond, a medical oncologist at the University of Colorado, Aurora. "Many times, they’re no longer being followed by their oncologist, and it’s up to their primary care physician to pull the trigger and order the test."
Many patients likely wouldn’t know that they should do breast cancer screening at such an early age, she added, because breast cancer wasn’t an anticipated outcome back when they had their radiotherapy.
National Comprehensive Cancer Network guidelines call for annual breast MRI and mammography along with clinical breast exams every 6-12 months, beginning 8-10 years after thoracic radiotherapy or at age 25 years, whichever occurs later. Dr. Diamond typically has patients stagger the two imaging modalities 6 months apart.
Both annual breast MRI and mammography are necessary. Screening MRI is far more sensitive than mammography alone in high-risk women, and it leads to cancer diagnosis at an earlier stage. However, MRI can miss ductal carcinoma in situ that would be evident as abnormal calcifications on screening mammography, she continued.
Annual breast MRI, in addition to mammography, is also indicated for women at high breast cancer risk as defined by a lifetime estimated risk in excess of 20%, or because they possess a BRCA 1 or 2 mutation, according to the NCCN. Dr. Diamond recommended BRCAPRO as a very useful tool for estimating the lifetime risk of breast cancer in women with no previous breast cancer.
In response to an audience question, she said she’s had no problem in getting insurers to pay for annual breast MRI to supplement annual mammography, so long as she clearly documents in her note that the patient has a greater than 20% lifetime estimated risk of breast cancer.
"They won’t cover it even a week earlier than annually, though," Dr. Diamond added.
She is a big fan of breast tomosynthesis, also known as three-dimensional mammography. The Food and Drug Administration–licensed technology produces a 3-D view of the breast tissue in addition to the standard two-dimensional images, all obtained in one compression with only about 2 seconds of additional compression time. Studies have shown that this tool substantially reduces patient recall rates for nondefinitive mammograms, Dr. Diamond said.
"It allows the mammographer to scroll through the breast, looking up and down sort of like with a CT scan, but without the same radiation exposure," she explained. "It’s a really great new technology, and I think most mammography centers will increasingly turn to it."
Dr. Diamond reported having no financial conflicts.
EXPERT ANALYSIS FROM AN UPDATE IN INTERNAL MEDICINE SPONSORED BY THE UNIVERSITY OF COLORADO
Experimental Drug Improves Muscle Strength in Cancer
HOUSTON – An experimental drug significantly improved physical function in men with cancer-related muscle wasting, compared with placebo – and more so in the men with low testosterone levels – in a secondary analysis of a randomized, double-blind, phase II clinical trial.
In all, 60% of the 93 men for whom baseline testosterone levels were available had hypogonadism when the patients were randomized to treatment with daily placebo or 1 mg or 3 mg of enobosarm for 16 weeks. Before treatment, the eugonadal males showed significantly better physical function, as measured by stair-climb power, compared with the hypogonadal patients (174 W vs. 147 W). Lower testosterone levels correlated with lower physical function.
Enobosarm significantly improved physical function (a secondary end point in the trial) with an average 17% increase in stair-climb power in hypogonadal men, and a 12% increase in power in eugonadal men, compared with baseline, Dr. Adrian Dobs and her associates reported at the annual meeting of the Endocrine Society.
Among men on placebo, stair-climb power increased by about 10% in hypogonadal men and by roughly 1% in eugonadal men, compared with baseline, but the changes were not statistically significant, said Dr. Dobs, professor of medicine and oncology at Johns Hopkins University, Baltimore.
Adverse events included fatigue in 21% of both treatment groups, anemia in 19% of those on enobosarm and 15% in those on placebo, nausea in 18% on enobosarm and 14% on placebo, diarrhea in 16% on enobosarm and 14% on placebo, vomiting in 12% of each treatment group, weight decrease in 12% on enobosarm and 10% on placebo, and constipation in 14% on enobosarm and 4% on placebo.
The investigators defined hypogonadism as a testosterone level below 300 ng/dL.
Enobosarm is a nonsteroidal SARM (selective androgen receptor modulator) that produces anabolic effects in bone and muscle without causing the prostate effects in men or hair growth in women that is seen with steroids.
The analysis used data from a larger trial in 159 people with cancer (65% of whom were men) who had lost at least 2% (and an average of 8%) of their weight in the previous 6 months. The men were older than 45 years of age, the women were postmenopausal, and each had a body mass index less than 35 mg/kg2.
The multicenter study as a whole met its primary end point of increasing lean body mass (muscle) and its secondary end point of improving physical function, Dr. Dobs said in an interview. Those results were reported on the website of the company that is developing the drug, GTx Inc., and at previous medical meetings, according to an interview in the Los Angeles Times.
Dr. Dobs did not report results for lean body mass in the current analysis based on gonadal status.
Cancer diagnoses included colorectal cancer, non–small cell lung cancer, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and breast cancer. Patients participated in the study prior to or between courses of chemotherapy. Rates of hypogonadism were similar for each type of cancer. Patients with hypogonadism were less likely to complete the study than were eugonadal men.
Patients with cancer develop cachexia (muscle wasting) because of reduced anabolic activity, increased catabolic activity, or both, accounting for a progressive catabolic state. Up to 50% of patients with lung cancer show severe cachexia at the time of diagnosis, and the muscle wasting increases throughout the course of the malignancy, Dr. Dobs said.
Two phase III clinical trials are underway to study effects of 3 mg/day of enobosarm for the prevention and treatment of muscle wasting in patients with non–small cell lung cancer.
GTx Inc., the company that is developing enobosarm, funded the current study. Dr. Dobs reported having no other financial disclosures.
HOUSTON – An experimental drug significantly improved physical function in men with cancer-related muscle wasting, compared with placebo – and more so in the men with low testosterone levels – in a secondary analysis of a randomized, double-blind, phase II clinical trial.
In all, 60% of the 93 men for whom baseline testosterone levels were available had hypogonadism when the patients were randomized to treatment with daily placebo or 1 mg or 3 mg of enobosarm for 16 weeks. Before treatment, the eugonadal males showed significantly better physical function, as measured by stair-climb power, compared with the hypogonadal patients (174 W vs. 147 W). Lower testosterone levels correlated with lower physical function.
Enobosarm significantly improved physical function (a secondary end point in the trial) with an average 17% increase in stair-climb power in hypogonadal men, and a 12% increase in power in eugonadal men, compared with baseline, Dr. Adrian Dobs and her associates reported at the annual meeting of the Endocrine Society.
Among men on placebo, stair-climb power increased by about 10% in hypogonadal men and by roughly 1% in eugonadal men, compared with baseline, but the changes were not statistically significant, said Dr. Dobs, professor of medicine and oncology at Johns Hopkins University, Baltimore.
Adverse events included fatigue in 21% of both treatment groups, anemia in 19% of those on enobosarm and 15% in those on placebo, nausea in 18% on enobosarm and 14% on placebo, diarrhea in 16% on enobosarm and 14% on placebo, vomiting in 12% of each treatment group, weight decrease in 12% on enobosarm and 10% on placebo, and constipation in 14% on enobosarm and 4% on placebo.
The investigators defined hypogonadism as a testosterone level below 300 ng/dL.
Enobosarm is a nonsteroidal SARM (selective androgen receptor modulator) that produces anabolic effects in bone and muscle without causing the prostate effects in men or hair growth in women that is seen with steroids.
The analysis used data from a larger trial in 159 people with cancer (65% of whom were men) who had lost at least 2% (and an average of 8%) of their weight in the previous 6 months. The men were older than 45 years of age, the women were postmenopausal, and each had a body mass index less than 35 mg/kg2.
The multicenter study as a whole met its primary end point of increasing lean body mass (muscle) and its secondary end point of improving physical function, Dr. Dobs said in an interview. Those results were reported on the website of the company that is developing the drug, GTx Inc., and at previous medical meetings, according to an interview in the Los Angeles Times.
Dr. Dobs did not report results for lean body mass in the current analysis based on gonadal status.
Cancer diagnoses included colorectal cancer, non–small cell lung cancer, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and breast cancer. Patients participated in the study prior to or between courses of chemotherapy. Rates of hypogonadism were similar for each type of cancer. Patients with hypogonadism were less likely to complete the study than were eugonadal men.
Patients with cancer develop cachexia (muscle wasting) because of reduced anabolic activity, increased catabolic activity, or both, accounting for a progressive catabolic state. Up to 50% of patients with lung cancer show severe cachexia at the time of diagnosis, and the muscle wasting increases throughout the course of the malignancy, Dr. Dobs said.
Two phase III clinical trials are underway to study effects of 3 mg/day of enobosarm for the prevention and treatment of muscle wasting in patients with non–small cell lung cancer.
GTx Inc., the company that is developing enobosarm, funded the current study. Dr. Dobs reported having no other financial disclosures.
HOUSTON – An experimental drug significantly improved physical function in men with cancer-related muscle wasting, compared with placebo – and more so in the men with low testosterone levels – in a secondary analysis of a randomized, double-blind, phase II clinical trial.
In all, 60% of the 93 men for whom baseline testosterone levels were available had hypogonadism when the patients were randomized to treatment with daily placebo or 1 mg or 3 mg of enobosarm for 16 weeks. Before treatment, the eugonadal males showed significantly better physical function, as measured by stair-climb power, compared with the hypogonadal patients (174 W vs. 147 W). Lower testosterone levels correlated with lower physical function.
Enobosarm significantly improved physical function (a secondary end point in the trial) with an average 17% increase in stair-climb power in hypogonadal men, and a 12% increase in power in eugonadal men, compared with baseline, Dr. Adrian Dobs and her associates reported at the annual meeting of the Endocrine Society.
Among men on placebo, stair-climb power increased by about 10% in hypogonadal men and by roughly 1% in eugonadal men, compared with baseline, but the changes were not statistically significant, said Dr. Dobs, professor of medicine and oncology at Johns Hopkins University, Baltimore.
Adverse events included fatigue in 21% of both treatment groups, anemia in 19% of those on enobosarm and 15% in those on placebo, nausea in 18% on enobosarm and 14% on placebo, diarrhea in 16% on enobosarm and 14% on placebo, vomiting in 12% of each treatment group, weight decrease in 12% on enobosarm and 10% on placebo, and constipation in 14% on enobosarm and 4% on placebo.
The investigators defined hypogonadism as a testosterone level below 300 ng/dL.
Enobosarm is a nonsteroidal SARM (selective androgen receptor modulator) that produces anabolic effects in bone and muscle without causing the prostate effects in men or hair growth in women that is seen with steroids.
The analysis used data from a larger trial in 159 people with cancer (65% of whom were men) who had lost at least 2% (and an average of 8%) of their weight in the previous 6 months. The men were older than 45 years of age, the women were postmenopausal, and each had a body mass index less than 35 mg/kg2.
The multicenter study as a whole met its primary end point of increasing lean body mass (muscle) and its secondary end point of improving physical function, Dr. Dobs said in an interview. Those results were reported on the website of the company that is developing the drug, GTx Inc., and at previous medical meetings, according to an interview in the Los Angeles Times.
Dr. Dobs did not report results for lean body mass in the current analysis based on gonadal status.
Cancer diagnoses included colorectal cancer, non–small cell lung cancer, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and breast cancer. Patients participated in the study prior to or between courses of chemotherapy. Rates of hypogonadism were similar for each type of cancer. Patients with hypogonadism were less likely to complete the study than were eugonadal men.
Patients with cancer develop cachexia (muscle wasting) because of reduced anabolic activity, increased catabolic activity, or both, accounting for a progressive catabolic state. Up to 50% of patients with lung cancer show severe cachexia at the time of diagnosis, and the muscle wasting increases throughout the course of the malignancy, Dr. Dobs said.
Two phase III clinical trials are underway to study effects of 3 mg/day of enobosarm for the prevention and treatment of muscle wasting in patients with non–small cell lung cancer.
GTx Inc., the company that is developing enobosarm, funded the current study. Dr. Dobs reported having no other financial disclosures.
AT THE ANNUAL MEETING OF THE ENDOCRINE SOCIETY
Major Finding: The experimental drug enobosarm significantly improved physical function on a stair-climb test by 17% in hypogonadal men with cancer and by 12% in eugonadal men with cancer, compared with nonsignificant improvements in men on placebo.
Data Source: Data are from an analysis of data on a secondary end point (physical function) in 93 men from a randomized, double-blind, multicenter trial in 159 cancer patients.
Disclosures: GTx, the company that is developing enobosarm, funded the study. Dr. Dobs reported having no other financial disclosures.
Ovarian Cortex Autografts in Cancer Survivors Yield Live Births
SANTA BARBARA, CALIF. – Ovarian cortex orthotransplantation has resulted in the live births of at least 21 babies to cancer survivors in Europe, where the technique was pioneered and is being refined, Dr. Antonio Pellicer reported at a meeting on in vitro fertilization and embryo transfer.
Unlike the freezing of oocytes or embryos to preserve potential fertility, which requires ovarian stimulation, the ovarian cortex can be harvested from a cancer patient without delay, permitting immediate initiation of chemotherapy and/or radiation therapy. The tissue is cryopreserved until the patient is in remission.
If cancer treatment results in premature ovarian failure and the patient wishes to become pregnant, her autologous ovarian cortex can then be reintroduced.
Ovarian function generally resumes within 3-4 months, said Dr. Pellicer, professor of obstetrics and gynecology and dean of the medical school at the University of Valencia (Spain). Follicle stimulating hormone rates do not reach normal levels, but are sufficient in many cases for resumption of menses and pregnancy, either naturally or through assisted reproductive techniques.
The technique is currently believed to be safe for breast cancer patients and those with Hodgkin’s and non-Hodgkin’s lymphoma, based on histologic and immunologic evaluations of harvested ovarian tissue, Dr. Pellicer said at the meeting, which was sponsored by the University of California, Los Angeles.
It is considered unsafe for patients with leukemia, as metastatic cells might well circulate through the bloodstream to the ovaries. Because of its highly metastatic potential, Ewing’s sarcoma is also considered a contraindication for the procedure, according to Dr. Pellicer.
The technique offers hope, potentially, for prepubertal girls and adolescents with other types of cancer, as well as adult cancer patients, although much remains unknown about the viability and usefulness of the treatment, explained Dr. Pellicer.
At the Valencia Program of Fertility Preservation, more than 600 cancer patients from across Spain have undergone removal of the ovarian cortex around the time of diagnosis, said Dr. Pellicer.
He reported on results in 583 of those patients who were treated since 2005, 55% of whom had been diagnosed with breast cancer.
Regular menses and fertility were restored in some patients who received ovarian autografts, said Dr. Pellicer. In all, 16 pregnancies and 3 live births have occurred, some following in vitro fertilization and some following natural conception.
Those results, along with published studies from programs in France, Germany, Denmark, Belgium, and other countries, indicate that at least 21 and perhaps 23 or more live births have resulted from the technique.
The problem, as Dr. Pellicer sees it, is a lack of cohesive follow-up or evidence that would put those births into perspective.
"We don’t know the number of failed attempts," he said. "There are no registries. There are no real data. Are we doing something which is really helpful? Or are the unsuccessful cases more [typical] than the successful cases?"
"This is a concern to me," he said.
Responding to a question from an audience member, Dr. Pellicer acknowledged that the removal of one ovarian cortex prior to cancer treatment might diminish fertility potential rather than enhance it, because some cancer patients conceive naturally following remission.
Dr. Pellicer reported that he had no relevant financial relationships to disclose.
SANTA BARBARA, CALIF. – Ovarian cortex orthotransplantation has resulted in the live births of at least 21 babies to cancer survivors in Europe, where the technique was pioneered and is being refined, Dr. Antonio Pellicer reported at a meeting on in vitro fertilization and embryo transfer.
Unlike the freezing of oocytes or embryos to preserve potential fertility, which requires ovarian stimulation, the ovarian cortex can be harvested from a cancer patient without delay, permitting immediate initiation of chemotherapy and/or radiation therapy. The tissue is cryopreserved until the patient is in remission.
If cancer treatment results in premature ovarian failure and the patient wishes to become pregnant, her autologous ovarian cortex can then be reintroduced.
Ovarian function generally resumes within 3-4 months, said Dr. Pellicer, professor of obstetrics and gynecology and dean of the medical school at the University of Valencia (Spain). Follicle stimulating hormone rates do not reach normal levels, but are sufficient in many cases for resumption of menses and pregnancy, either naturally or through assisted reproductive techniques.
The technique is currently believed to be safe for breast cancer patients and those with Hodgkin’s and non-Hodgkin’s lymphoma, based on histologic and immunologic evaluations of harvested ovarian tissue, Dr. Pellicer said at the meeting, which was sponsored by the University of California, Los Angeles.
It is considered unsafe for patients with leukemia, as metastatic cells might well circulate through the bloodstream to the ovaries. Because of its highly metastatic potential, Ewing’s sarcoma is also considered a contraindication for the procedure, according to Dr. Pellicer.
The technique offers hope, potentially, for prepubertal girls and adolescents with other types of cancer, as well as adult cancer patients, although much remains unknown about the viability and usefulness of the treatment, explained Dr. Pellicer.
At the Valencia Program of Fertility Preservation, more than 600 cancer patients from across Spain have undergone removal of the ovarian cortex around the time of diagnosis, said Dr. Pellicer.
He reported on results in 583 of those patients who were treated since 2005, 55% of whom had been diagnosed with breast cancer.
Regular menses and fertility were restored in some patients who received ovarian autografts, said Dr. Pellicer. In all, 16 pregnancies and 3 live births have occurred, some following in vitro fertilization and some following natural conception.
Those results, along with published studies from programs in France, Germany, Denmark, Belgium, and other countries, indicate that at least 21 and perhaps 23 or more live births have resulted from the technique.
The problem, as Dr. Pellicer sees it, is a lack of cohesive follow-up or evidence that would put those births into perspective.
"We don’t know the number of failed attempts," he said. "There are no registries. There are no real data. Are we doing something which is really helpful? Or are the unsuccessful cases more [typical] than the successful cases?"
"This is a concern to me," he said.
Responding to a question from an audience member, Dr. Pellicer acknowledged that the removal of one ovarian cortex prior to cancer treatment might diminish fertility potential rather than enhance it, because some cancer patients conceive naturally following remission.
Dr. Pellicer reported that he had no relevant financial relationships to disclose.
SANTA BARBARA, CALIF. – Ovarian cortex orthotransplantation has resulted in the live births of at least 21 babies to cancer survivors in Europe, where the technique was pioneered and is being refined, Dr. Antonio Pellicer reported at a meeting on in vitro fertilization and embryo transfer.
Unlike the freezing of oocytes or embryos to preserve potential fertility, which requires ovarian stimulation, the ovarian cortex can be harvested from a cancer patient without delay, permitting immediate initiation of chemotherapy and/or radiation therapy. The tissue is cryopreserved until the patient is in remission.
If cancer treatment results in premature ovarian failure and the patient wishes to become pregnant, her autologous ovarian cortex can then be reintroduced.
Ovarian function generally resumes within 3-4 months, said Dr. Pellicer, professor of obstetrics and gynecology and dean of the medical school at the University of Valencia (Spain). Follicle stimulating hormone rates do not reach normal levels, but are sufficient in many cases for resumption of menses and pregnancy, either naturally or through assisted reproductive techniques.
The technique is currently believed to be safe for breast cancer patients and those with Hodgkin’s and non-Hodgkin’s lymphoma, based on histologic and immunologic evaluations of harvested ovarian tissue, Dr. Pellicer said at the meeting, which was sponsored by the University of California, Los Angeles.
It is considered unsafe for patients with leukemia, as metastatic cells might well circulate through the bloodstream to the ovaries. Because of its highly metastatic potential, Ewing’s sarcoma is also considered a contraindication for the procedure, according to Dr. Pellicer.
The technique offers hope, potentially, for prepubertal girls and adolescents with other types of cancer, as well as adult cancer patients, although much remains unknown about the viability and usefulness of the treatment, explained Dr. Pellicer.
At the Valencia Program of Fertility Preservation, more than 600 cancer patients from across Spain have undergone removal of the ovarian cortex around the time of diagnosis, said Dr. Pellicer.
He reported on results in 583 of those patients who were treated since 2005, 55% of whom had been diagnosed with breast cancer.
Regular menses and fertility were restored in some patients who received ovarian autografts, said Dr. Pellicer. In all, 16 pregnancies and 3 live births have occurred, some following in vitro fertilization and some following natural conception.
Those results, along with published studies from programs in France, Germany, Denmark, Belgium, and other countries, indicate that at least 21 and perhaps 23 or more live births have resulted from the technique.
The problem, as Dr. Pellicer sees it, is a lack of cohesive follow-up or evidence that would put those births into perspective.
"We don’t know the number of failed attempts," he said. "There are no registries. There are no real data. Are we doing something which is really helpful? Or are the unsuccessful cases more [typical] than the successful cases?"
"This is a concern to me," he said.
Responding to a question from an audience member, Dr. Pellicer acknowledged that the removal of one ovarian cortex prior to cancer treatment might diminish fertility potential rather than enhance it, because some cancer patients conceive naturally following remission.
Dr. Pellicer reported that he had no relevant financial relationships to disclose.
AT A MEETING ON IN VITRO FERTILIZATION AND EMBRYO TRANSFER
Major Finding: Sixteen pregnancies and three live births have occurred, some following in vitro fertilization and some following natural conception.
Data Source: This was a study of 583 patients who received ovarian autografts since 2005, 55% of whom had been diagnosed with breast cancer.
Disclosures: Dr. Pellicer reported that he had no relevant financial relationships to disclose.
Breast Cancer During Pregnancy Can Be Treated as in Nonpregnant Women
It appears that breast cancer diagnosed during pregnancy can be treated much the same as breast cancer diagnosed in nonpregnant women without substantially raising the risks to mother or child, according to a study published online August 16 in the Lancet Oncology .
This conclusion, from an observational study involving 447 European women included in registries of cancers diagnosed during pregnancy, must still be validated in other studies. But until then, the current evidence indicates that pregnancy outcomes are not significantly different between women who receive breast cancer chemotherapy during the second or third trimesters and those who wait until after delivery to start treatment, said Dr. Sibylle Loibl of the German Breast Group, Neu-Isenburg, Germany, and her associates.
In this study, infants exposed to their mothers’ breast cancer chemotherapy while in utero had slightly lower birth weights and slightly more complications than those not exposed to chemotherapy, but these differences were not clinically significant.
Breast cancer diagnosed during pregnancy is rare, estimated to occur in less than 1% of breast cancers in Europe. But its incidence is increasing in high-income countries due to the trend of women delaying childbirth until they are older, when breast cancer is more prevalent.
The German Breast Group established its Breast Cancer During Pregnancy registry in 2003 and expanded it to include cases in the Netherlands, the United Kingdom, Poland, Italy, and the Czech Republic in 2009. In the same time period, Belgium also established a registry of all cancers diagnosed during pregnancy. Dr. Loibl and her colleagues assessed outcomes in 447 cases from these registries in which women were diagnosed as having early (413 patients) or metastatic (34 patients) breast cancer while pregnant (Lancet Oncol. 2012 Aug. 15 [doi:10.1016/S1470-2045(12)70261-9]).
The median gestational age at diagnosis was 24 weeks (range, 5-40 weeks), and the median age of the women was 33 years (range, 22-51 years).
Data on chemotherapy were available for 368 women. Of these, 197 received chemotherapy while pregnant and 171 received it after delivery.
Overall, 1,187 cycles of chemotherapy were given, and 63% of these were given during pregnancy. The women received a median of four cycles (range, one to eight cycles) during pregnancy.
A total of 90% of those treated during pregnancy received an anthracyline; 8% received a combination of cyclophosphamide, methotrexate, and fluorouracil; and 7% received a taxane. None of the women received trastuzumab, endocrine therapy, or radiotherapy during pregnancy.
Women with early breast cancer who opted for chemotherapy during pregnancy tended to have more advanced disease, with more unfavorable tumor stage and nodal status, than did those who chose to begin chemotherapy after delivery. After the data were adjusted to account for this difference, the researchers found no significant difference between the two groups in disease-free or overall survival.
The estimated 3-year disease-free survival was 70.2% in women with early disease who underwent chemotherapy while pregnant and 74.3% in those who waited until after delivery. Similarly, the estimated overall 3-year survival was 84.9% in women with early breast cancer who underwent chemotherapy while pregnant and 87.4% in those who delayed chemotherapy until after delivery.
The estimated 5-year disease-free survival was 61.1% in women who had chemotherapy while pregnant and 64.4% in those who waited, and the estimated 5-year overall survival was 77% and 82.4%, respectively.
Data were available for 373 newborns, of whom 203 had been exposed to chemotherapy in utero and 170 had not.
Birth weight was slightly lower in the exposed than in the nonexposed infants, but this difference was judged to be "clinically irrelevant" because it didn’t affect the health of the babies, Dr. Loibl and her associates said.
Moreover, there were no significant differences between the two groups in major birth defects, infant height, Apgar scores, hemoglobin concentration, leukocyte counts, thrombocyte counts, or alopecia. And there was no significant difference in the proportion of infants discharged with their mothers (34% vs. 41%).
Adverse events occurred more often when chemotherapy was received during pregnancy (15%) than when it was delayed (4%). However, this difference was attributed to the higher rates of preterm labor and premature rupture of the membrane among exposed pregnancies. "Most complications were reported in babies who were delivered prematurely, regardless of exposure to chemotherapy," the investigators said.
The data were not adequate to determine why women who received chemotherapy had a higher rate of preterm delivery. Both physical stress and psychological stress may have played a role, and it is possible that women who received chemotherapy were more prone to infections that may have triggered labor.
In addition, the cytotoxic agents themselves may have hastened labor through some as yet unknown mechanism. However, the rate of preeclampsia was similar between the two groups, so oxidative stress, which is known to be induced by cytoxic agents, was not responsible.
Further study of the data being collected in the registries of cancers diagnosed during pregnancy will likely shed light on these issues. Dr. Loibl and her colleagues are now performing a matched-pair analysis to assess whether the prognosis of breast cancer in nonpregnant women differs from that in pregnant women when the latter are treated according to current guidelines.
This study was supported by BANSS Foundation, University Hospital Frankfurt, the German Breast Group, Research Foundation-Flanders, Clinical Research Fund-UZ Gasthuisberg, and the Belgian Cancer Plan. No financial conflicts of interest were reported.
Future studies should address not just the toxic effects of chemotherapy during pregnancy but also the pharmacokinetics of cytotoxic agents in pregnant women, because the physiologic changes of pregnancy can greatly affect drug disposition, said Dr. Olivier Mir and Dr. Paul Berveiller.
"Whether doses should be increased in this population is uncertain because such increases could result in severe thrombocytopenia, neutropenia, and infection, with potentially devastating consequences for both mother and baby," they noted.
More research also is needed to determine whether the slightly increased fetal risks identified by Dr. Loibl and her colleagues could be minimized with better drug selection and dosing, they added.
Dr. Mir and Dr. Berveiller are in the Cancer Associated With Pregnancy Network, Paris. Dr. Mir is also in the department of medical oncology at Hôpital Cochin at the Université René Descartes, Paris. Dr. Mir reported ties to Roche, Pfizer, and Servier. These remarks were taken from their editorial comment accompanying Dr. Loibl’s report (Lancet Oncol. 2012 Aug. 15 [doi:10.1016/S1470-2045(12)70331-5]).
Future studies should address not just the toxic effects of chemotherapy during pregnancy but also the pharmacokinetics of cytotoxic agents in pregnant women, because the physiologic changes of pregnancy can greatly affect drug disposition, said Dr. Olivier Mir and Dr. Paul Berveiller.
"Whether doses should be increased in this population is uncertain because such increases could result in severe thrombocytopenia, neutropenia, and infection, with potentially devastating consequences for both mother and baby," they noted.
More research also is needed to determine whether the slightly increased fetal risks identified by Dr. Loibl and her colleagues could be minimized with better drug selection and dosing, they added.
Dr. Mir and Dr. Berveiller are in the Cancer Associated With Pregnancy Network, Paris. Dr. Mir is also in the department of medical oncology at Hôpital Cochin at the Université René Descartes, Paris. Dr. Mir reported ties to Roche, Pfizer, and Servier. These remarks were taken from their editorial comment accompanying Dr. Loibl’s report (Lancet Oncol. 2012 Aug. 15 [doi:10.1016/S1470-2045(12)70331-5]).
Future studies should address not just the toxic effects of chemotherapy during pregnancy but also the pharmacokinetics of cytotoxic agents in pregnant women, because the physiologic changes of pregnancy can greatly affect drug disposition, said Dr. Olivier Mir and Dr. Paul Berveiller.
"Whether doses should be increased in this population is uncertain because such increases could result in severe thrombocytopenia, neutropenia, and infection, with potentially devastating consequences for both mother and baby," they noted.
More research also is needed to determine whether the slightly increased fetal risks identified by Dr. Loibl and her colleagues could be minimized with better drug selection and dosing, they added.
Dr. Mir and Dr. Berveiller are in the Cancer Associated With Pregnancy Network, Paris. Dr. Mir is also in the department of medical oncology at Hôpital Cochin at the Université René Descartes, Paris. Dr. Mir reported ties to Roche, Pfizer, and Servier. These remarks were taken from their editorial comment accompanying Dr. Loibl’s report (Lancet Oncol. 2012 Aug. 15 [doi:10.1016/S1470-2045(12)70331-5]).
It appears that breast cancer diagnosed during pregnancy can be treated much the same as breast cancer diagnosed in nonpregnant women without substantially raising the risks to mother or child, according to a study published online August 16 in the Lancet Oncology .
This conclusion, from an observational study involving 447 European women included in registries of cancers diagnosed during pregnancy, must still be validated in other studies. But until then, the current evidence indicates that pregnancy outcomes are not significantly different between women who receive breast cancer chemotherapy during the second or third trimesters and those who wait until after delivery to start treatment, said Dr. Sibylle Loibl of the German Breast Group, Neu-Isenburg, Germany, and her associates.
In this study, infants exposed to their mothers’ breast cancer chemotherapy while in utero had slightly lower birth weights and slightly more complications than those not exposed to chemotherapy, but these differences were not clinically significant.
Breast cancer diagnosed during pregnancy is rare, estimated to occur in less than 1% of breast cancers in Europe. But its incidence is increasing in high-income countries due to the trend of women delaying childbirth until they are older, when breast cancer is more prevalent.
The German Breast Group established its Breast Cancer During Pregnancy registry in 2003 and expanded it to include cases in the Netherlands, the United Kingdom, Poland, Italy, and the Czech Republic in 2009. In the same time period, Belgium also established a registry of all cancers diagnosed during pregnancy. Dr. Loibl and her colleagues assessed outcomes in 447 cases from these registries in which women were diagnosed as having early (413 patients) or metastatic (34 patients) breast cancer while pregnant (Lancet Oncol. 2012 Aug. 15 [doi:10.1016/S1470-2045(12)70261-9]).
The median gestational age at diagnosis was 24 weeks (range, 5-40 weeks), and the median age of the women was 33 years (range, 22-51 years).
Data on chemotherapy were available for 368 women. Of these, 197 received chemotherapy while pregnant and 171 received it after delivery.
Overall, 1,187 cycles of chemotherapy were given, and 63% of these were given during pregnancy. The women received a median of four cycles (range, one to eight cycles) during pregnancy.
A total of 90% of those treated during pregnancy received an anthracyline; 8% received a combination of cyclophosphamide, methotrexate, and fluorouracil; and 7% received a taxane. None of the women received trastuzumab, endocrine therapy, or radiotherapy during pregnancy.
Women with early breast cancer who opted for chemotherapy during pregnancy tended to have more advanced disease, with more unfavorable tumor stage and nodal status, than did those who chose to begin chemotherapy after delivery. After the data were adjusted to account for this difference, the researchers found no significant difference between the two groups in disease-free or overall survival.
The estimated 3-year disease-free survival was 70.2% in women with early disease who underwent chemotherapy while pregnant and 74.3% in those who waited until after delivery. Similarly, the estimated overall 3-year survival was 84.9% in women with early breast cancer who underwent chemotherapy while pregnant and 87.4% in those who delayed chemotherapy until after delivery.
The estimated 5-year disease-free survival was 61.1% in women who had chemotherapy while pregnant and 64.4% in those who waited, and the estimated 5-year overall survival was 77% and 82.4%, respectively.
Data were available for 373 newborns, of whom 203 had been exposed to chemotherapy in utero and 170 had not.
Birth weight was slightly lower in the exposed than in the nonexposed infants, but this difference was judged to be "clinically irrelevant" because it didn’t affect the health of the babies, Dr. Loibl and her associates said.
Moreover, there were no significant differences between the two groups in major birth defects, infant height, Apgar scores, hemoglobin concentration, leukocyte counts, thrombocyte counts, or alopecia. And there was no significant difference in the proportion of infants discharged with their mothers (34% vs. 41%).
Adverse events occurred more often when chemotherapy was received during pregnancy (15%) than when it was delayed (4%). However, this difference was attributed to the higher rates of preterm labor and premature rupture of the membrane among exposed pregnancies. "Most complications were reported in babies who were delivered prematurely, regardless of exposure to chemotherapy," the investigators said.
The data were not adequate to determine why women who received chemotherapy had a higher rate of preterm delivery. Both physical stress and psychological stress may have played a role, and it is possible that women who received chemotherapy were more prone to infections that may have triggered labor.
In addition, the cytotoxic agents themselves may have hastened labor through some as yet unknown mechanism. However, the rate of preeclampsia was similar between the two groups, so oxidative stress, which is known to be induced by cytoxic agents, was not responsible.
Further study of the data being collected in the registries of cancers diagnosed during pregnancy will likely shed light on these issues. Dr. Loibl and her colleagues are now performing a matched-pair analysis to assess whether the prognosis of breast cancer in nonpregnant women differs from that in pregnant women when the latter are treated according to current guidelines.
This study was supported by BANSS Foundation, University Hospital Frankfurt, the German Breast Group, Research Foundation-Flanders, Clinical Research Fund-UZ Gasthuisberg, and the Belgian Cancer Plan. No financial conflicts of interest were reported.
It appears that breast cancer diagnosed during pregnancy can be treated much the same as breast cancer diagnosed in nonpregnant women without substantially raising the risks to mother or child, according to a study published online August 16 in the Lancet Oncology .
This conclusion, from an observational study involving 447 European women included in registries of cancers diagnosed during pregnancy, must still be validated in other studies. But until then, the current evidence indicates that pregnancy outcomes are not significantly different between women who receive breast cancer chemotherapy during the second or third trimesters and those who wait until after delivery to start treatment, said Dr. Sibylle Loibl of the German Breast Group, Neu-Isenburg, Germany, and her associates.
In this study, infants exposed to their mothers’ breast cancer chemotherapy while in utero had slightly lower birth weights and slightly more complications than those not exposed to chemotherapy, but these differences were not clinically significant.
Breast cancer diagnosed during pregnancy is rare, estimated to occur in less than 1% of breast cancers in Europe. But its incidence is increasing in high-income countries due to the trend of women delaying childbirth until they are older, when breast cancer is more prevalent.
The German Breast Group established its Breast Cancer During Pregnancy registry in 2003 and expanded it to include cases in the Netherlands, the United Kingdom, Poland, Italy, and the Czech Republic in 2009. In the same time period, Belgium also established a registry of all cancers diagnosed during pregnancy. Dr. Loibl and her colleagues assessed outcomes in 447 cases from these registries in which women were diagnosed as having early (413 patients) or metastatic (34 patients) breast cancer while pregnant (Lancet Oncol. 2012 Aug. 15 [doi:10.1016/S1470-2045(12)70261-9]).
The median gestational age at diagnosis was 24 weeks (range, 5-40 weeks), and the median age of the women was 33 years (range, 22-51 years).
Data on chemotherapy were available for 368 women. Of these, 197 received chemotherapy while pregnant and 171 received it after delivery.
Overall, 1,187 cycles of chemotherapy were given, and 63% of these were given during pregnancy. The women received a median of four cycles (range, one to eight cycles) during pregnancy.
A total of 90% of those treated during pregnancy received an anthracyline; 8% received a combination of cyclophosphamide, methotrexate, and fluorouracil; and 7% received a taxane. None of the women received trastuzumab, endocrine therapy, or radiotherapy during pregnancy.
Women with early breast cancer who opted for chemotherapy during pregnancy tended to have more advanced disease, with more unfavorable tumor stage and nodal status, than did those who chose to begin chemotherapy after delivery. After the data were adjusted to account for this difference, the researchers found no significant difference between the two groups in disease-free or overall survival.
The estimated 3-year disease-free survival was 70.2% in women with early disease who underwent chemotherapy while pregnant and 74.3% in those who waited until after delivery. Similarly, the estimated overall 3-year survival was 84.9% in women with early breast cancer who underwent chemotherapy while pregnant and 87.4% in those who delayed chemotherapy until after delivery.
The estimated 5-year disease-free survival was 61.1% in women who had chemotherapy while pregnant and 64.4% in those who waited, and the estimated 5-year overall survival was 77% and 82.4%, respectively.
Data were available for 373 newborns, of whom 203 had been exposed to chemotherapy in utero and 170 had not.
Birth weight was slightly lower in the exposed than in the nonexposed infants, but this difference was judged to be "clinically irrelevant" because it didn’t affect the health of the babies, Dr. Loibl and her associates said.
Moreover, there were no significant differences between the two groups in major birth defects, infant height, Apgar scores, hemoglobin concentration, leukocyte counts, thrombocyte counts, or alopecia. And there was no significant difference in the proportion of infants discharged with their mothers (34% vs. 41%).
Adverse events occurred more often when chemotherapy was received during pregnancy (15%) than when it was delayed (4%). However, this difference was attributed to the higher rates of preterm labor and premature rupture of the membrane among exposed pregnancies. "Most complications were reported in babies who were delivered prematurely, regardless of exposure to chemotherapy," the investigators said.
The data were not adequate to determine why women who received chemotherapy had a higher rate of preterm delivery. Both physical stress and psychological stress may have played a role, and it is possible that women who received chemotherapy were more prone to infections that may have triggered labor.
In addition, the cytotoxic agents themselves may have hastened labor through some as yet unknown mechanism. However, the rate of preeclampsia was similar between the two groups, so oxidative stress, which is known to be induced by cytoxic agents, was not responsible.
Further study of the data being collected in the registries of cancers diagnosed during pregnancy will likely shed light on these issues. Dr. Loibl and her colleagues are now performing a matched-pair analysis to assess whether the prognosis of breast cancer in nonpregnant women differs from that in pregnant women when the latter are treated according to current guidelines.
This study was supported by BANSS Foundation, University Hospital Frankfurt, the German Breast Group, Research Foundation-Flanders, Clinical Research Fund-UZ Gasthuisberg, and the Belgian Cancer Plan. No financial conflicts of interest were reported.
FROM THE LANCET ONCOLOGY
Major Finding: Rates of low birth weight and adverse events were slightly higher when women underwent breast cancer chemotherapy while pregnant than when they delayed chemotherapy until after delivery, but the small differences were deemed clinically irrelevant.
Data Source: An observational study of pregnancy outcomes in European women diagnosed as having breast cancer during pregnancy, of whom 197 received chemotherapy while pregnant and 171 delayed chemotherapy until after delivery.
Disclosures: This study was supported by BANSS Foundation, University Hospital Frankfurt, the German Breast Group, Research Foundation-Flanders, Clinical Research Fund-UZ Gasthuisberg, and the Belgian Cancer Plan. No financial conflicts of interest were reported.
Romidepsin-Decitabine Duo Battles Breast and Kidney Cancers
Two blood cancer drugs, romidepsin and decitabine, may form a partnership that can treat specific types of breast and kidney cancers, based on data from a stem cell study published online in Molecular Cancer Therapeutics.
Each drug is approved by the Food and Drug Administration to treat hematologic cancer, but this study uniquely combined romidepsin (Istodax) and decitabine (Dacogen) to activate a tumor suppressor gene that is inactive in triple-negative breast cancer and clear cell renal cell carcinoma.
Activating the gene known as secreted frizzled-related protein 1 (sFRP1) killed kidney and breast cancer cells in multiple cell lines tested, but only when the drugs were used in tandem (Mol. Cancer Ther. July 23, 2012 [doi:10.1158/1535-7163.MCT-11-0873]).
Ultimately, clinicians may be able to target treatment of triple-negative breast cancer and clear cell renal cell carcinoma by identifying which patients have tumors in which sFRP1 is inactivated, the researchers noted. "We predict that there are a number of drug targetable genes that are re-expressed after combinatorial treatment that possess antitumor activity," they said.
"We now have the basis for a clinical trial aimed at providing effective therapy for two drug-resistant cancers and perhaps many more tumor types in the future," senior author John A. Copland, Ph.D., of the Mayo Clinic in Jacksonville, Florida, added in a statement issued July 31 by the Mayo Clinic.
The researchers had no financial conflicts to disclose. The study was funded in part by grants from several organizations, including the National Cancer Institute; Kidney Cancer Research at Mayo Clinic, Florida; and the Breast Cancer Research Foundation.
Two blood cancer drugs, romidepsin and decitabine, may form a partnership that can treat specific types of breast and kidney cancers, based on data from a stem cell study published online in Molecular Cancer Therapeutics.
Each drug is approved by the Food and Drug Administration to treat hematologic cancer, but this study uniquely combined romidepsin (Istodax) and decitabine (Dacogen) to activate a tumor suppressor gene that is inactive in triple-negative breast cancer and clear cell renal cell carcinoma.
Activating the gene known as secreted frizzled-related protein 1 (sFRP1) killed kidney and breast cancer cells in multiple cell lines tested, but only when the drugs were used in tandem (Mol. Cancer Ther. July 23, 2012 [doi:10.1158/1535-7163.MCT-11-0873]).
Ultimately, clinicians may be able to target treatment of triple-negative breast cancer and clear cell renal cell carcinoma by identifying which patients have tumors in which sFRP1 is inactivated, the researchers noted. "We predict that there are a number of drug targetable genes that are re-expressed after combinatorial treatment that possess antitumor activity," they said.
"We now have the basis for a clinical trial aimed at providing effective therapy for two drug-resistant cancers and perhaps many more tumor types in the future," senior author John A. Copland, Ph.D., of the Mayo Clinic in Jacksonville, Florida, added in a statement issued July 31 by the Mayo Clinic.
The researchers had no financial conflicts to disclose. The study was funded in part by grants from several organizations, including the National Cancer Institute; Kidney Cancer Research at Mayo Clinic, Florida; and the Breast Cancer Research Foundation.
Two blood cancer drugs, romidepsin and decitabine, may form a partnership that can treat specific types of breast and kidney cancers, based on data from a stem cell study published online in Molecular Cancer Therapeutics.
Each drug is approved by the Food and Drug Administration to treat hematologic cancer, but this study uniquely combined romidepsin (Istodax) and decitabine (Dacogen) to activate a tumor suppressor gene that is inactive in triple-negative breast cancer and clear cell renal cell carcinoma.
Activating the gene known as secreted frizzled-related protein 1 (sFRP1) killed kidney and breast cancer cells in multiple cell lines tested, but only when the drugs were used in tandem (Mol. Cancer Ther. July 23, 2012 [doi:10.1158/1535-7163.MCT-11-0873]).
Ultimately, clinicians may be able to target treatment of triple-negative breast cancer and clear cell renal cell carcinoma by identifying which patients have tumors in which sFRP1 is inactivated, the researchers noted. "We predict that there are a number of drug targetable genes that are re-expressed after combinatorial treatment that possess antitumor activity," they said.
"We now have the basis for a clinical trial aimed at providing effective therapy for two drug-resistant cancers and perhaps many more tumor types in the future," senior author John A. Copland, Ph.D., of the Mayo Clinic in Jacksonville, Florida, added in a statement issued July 31 by the Mayo Clinic.
The researchers had no financial conflicts to disclose. The study was funded in part by grants from several organizations, including the National Cancer Institute; Kidney Cancer Research at Mayo Clinic, Florida; and the Breast Cancer Research Foundation.
FROM MOLECULAR CANCER THERAPEUTICS
Faster Injectable Trastuzumab Matches Intravenous in Response Rates
A subcutaneous injectable form of trastuzumab achieved pharmacokinetic and clinical outcomes that equaled those of intravenous infusion for women with HER2-positive breast cancers in a randomized open-label phase III study.
The international HannaH trial found no significant differences in presurgical serum trough levels at any time during the six-cycle neoadjuvant treatment. At the end of the year-long study, 45% of the subcutaneous group and 41% of the intravenous group had a pathological complete response (pCR).
The subcutaneous form of trastuzumab (Herceptin) takes 5 minutes to administer; patients can self-administer the drug at home. The infusion takes 90 minutes and must be done in the clinic.
If clinical results are equivalent, the injection could become an attractive alternative to intravenous treatment, Dr. Gustavo Ismael of the Hospital Amaral Carvalho, Jaú, Brazil, and his coauthors proposed in the Aug. 9 online issue of the Lancet Oncology (2012 [doi.org/10.1016/S1470-2045(12)70329-7]).*
"The shortened duration of administration with subcutaneous trastuzumab ... suggests the potential for substantial time saving for patients, physicians, and nursing staff," the investigators wrote.
Susan Willson, a spokesperson for Genentech, said the company is looking at the HannaH data, as well as that of other studies, to determine whether the subcutaneous form of trastuzumab will be put forth to the Food and Drug Administration.
Earlier this year, Roche, Genetech’s parent company, submitted a line extension application for subcutaneous trastuzumab to the European Medicines Association. The requested indication is the treatment of HER-2-positive breast cancer.
Trastuzumab Given with Neoadjuvant Chemo
The HannaH (enHANced treatment with NeoAdjuvant Herceptin) trial randomized 596 women with HER-2 positive breast cancer to six cycles of neoadjuvant chemotherapy with either the injections or intravenous infusions; both were administered once every 3 weeks.
The injection was a fixed dose of 600 mg trastuzumab with recombinant hyaluronidase PH-20 delivered to the thigh by study nurses. The enzyme temporarily degrades interstitial hyaluronan, expanding the space to accommodate the volume of the injection.
Women in the subcutaneous group did not take a loading dose of the medication. Those in the intravenous group received an 8 mg/kg loading dose followed by a 6 mg/kg maintenance dose. The follow-up period was 24 months or until disease recurrence
The chemotherapy regimen for both groups consisted of four 3-week cycles of docetaxel (Taxotere) followed by four cycles of fluorouracil and cyclophosphamide. After surgery, all patients continued their trastuzumab regimen for 1 year.
Median patient age was 50 years. About 50% were positive for estrogen receptor tumors. More than half had operable cancer; more than a third had locally advanced cancer; and about 6% had inflammatory breast cancer. Median follow-up in both groups was a little more than 1 year.
The pharmacokinetic profile was similar between the two forms of trastuzumab. After the first cycle, the mean trough serum level was similar between the injectable and intravenous forms (32.7 mcg/mL vs. 34.5 mcg/mL). The levels were also similar before the third cycle (45 and 48 mcg/mL). Almost all patients (98%) reached the therapeutic level of more than 20 micrograms/ml by cycle 8.
The mean presurgical trough level of the subcutaneous form was 58 mcg/mL; for the intravenous form, the mean level was 79 mcg/mL.
Similar Efficacy and Toxicity
The efficacy analysis included 523 patients and showed noninferiority of subcutaneous trastuzumab to intravenous trastuzumab. A pathological complete response occurred in 45% of the subcutaneous group and in 41% of the intravenous group in a per-protocol analysis. An intent-to-treat analysis showed similar numbers, with a complete pathological response in 42% of the subcutaneous group an 37% of the intravenous group.
Overall responses rates, including complete and partial responses, were comparable. Event-free and overall survival data were not yet mature, and have yet to be reported.
The rate of adverse events was similar between the subcutaneous and intravenous groups: alopecia (63% each), nausea (49% each), neutropenia (44% subcutaneous vs. 46% intravenous), diarrhea (34% subcutaneous vs. 37% intravenous), asthenia (25% each), and fatigue (23% subcutaneous vs. 26% intravenous).
The same proportion of patients in each group experienced at least one serious adverse event (52%). The most common were neutropenia, leucopenia, and febrile neutropenia.
Four adverse events lead to death – one in the subcutaneous group and three in the intravenous group during neoadjuvant treatment. These included a fatal acute pneumonia in an obese 66-year-old with pulmonary fibrosis in the subcutaneous group. In the intravenous group, the deaths were a myocardial infarction in an obese patient with a history of hypertension; a sudden death in an overweight patient who with hypertension and diabetes; fatal septic shock in a patient who developed febrile neutropenia. The septic shock and cardiac deaths were attributed to the treatment, the investigators said.
The proportion of grade 3 adverse events was similar in both groups, but the relative percentage of those classified as serious adverse events was 7.7% for the intravenous group and 18% for the subcutaneous group. "A similar finding was made for grade 2 adverse events, of which 0.5% was classed as serous ... in the intravenous group versus 1.5% in the subcutaneous group," they wrote. The investigators could not find an explanation for the imbalance in reporting of serious adverse events, but suggested that they may have been more conservative in assessing the subcutaneous arm of the trial.
Two patients in the subcutaneous group had mild congestive heart failure; both were obese with a history of hypertension. Six patients in the intravenous group and seven in the subcutaneous group had a significant decrease in left ventricular ejection fraction.
Antitrastuzumab antibodies developed in 10 patients in the intravenous group and 20 in the subcutaneous group, but these did not affect serum trough levels.
F. Hoffman-LaRoche funded the study Dr. Ismael disclosed that he has received honoraria from the company. His co-investigators also reported several financial relationships, including travels grants, speakers fees, research support, and employment.
Click here to hear Dr. Ismael discuss the trial in a podcast at the Lancet Oncology website.
*Correction, 08/13/12: This sentence was corrected to state that injectable trastuzumab could become an alternative to intravenous treatment. Weekly treatment was not specified.
A rapid, subcutaneous delivery of trastuzumab could come with several big advantages, Dr. Jose Perez-Garcia and Dr. Javier Cortes wrote in an accompanying editorial (Lancet Onc. 2012 Aug. 9 [doi.org/10.1016/S1470-2045(12)70367-4]).
"First, the ability to deliver the drug in about 5 minutes without the need to secure intravenous access makes subcutaneous treatment more convenient," wrote Dr. Perez-Garcia and Dr. Cortes of Vall d’Hebron Institute of Oncology, Barcelona. "Second, in addition to time savings, once the drug can be administered at home, patients will be able to continue their lives with less hospital dependence, which is an important psychological aspect."
The study didn’t address which drug delivery method patients preferred, or how an at-home subcutaneous administration might affect their quality of life. But another randomized study, PrefHer, aims to explore that, they wrote. PrefHer will evaluate patients' preference and healthcare satisfaction with subcutaneous vs. intravenous trastuzumab.
They also noted that the HannaH study could set a precedent for rapid approval of neoadjuvant drugs based on the pathological complete response (pCR) – but that pCR as an end point has not yet been fully vetted. "This approach appears to have at least two major limitations. First, we do not know what improvement in pCR would be necessary to translate into disease-free survival or overall survival benefit. Second, we also do not know what proportion of patients achieving a pCR would be needed to establish noninferiority between two drugs or between two methods of administering the same drug."
Finally, they wrote. "Third, the method of categorizing long-term adverse effects might be insufficient because many adverse events might appear after pCR, so if pCR is enough for regulatory purposes, the consequences of these long-term events might not be taken into account."
Dr. Perez-Garcia is an oncologist in the breast cancer program at Vall d’Hebron Institute of Oncology, Barcelona. He had no financial disclosures. Dr. Cortes, of the same institution, disclosed relationships with Roche and other companies.
A rapid, subcutaneous delivery of trastuzumab could come with several big advantages, Dr. Jose Perez-Garcia and Dr. Javier Cortes wrote in an accompanying editorial (Lancet Onc. 2012 Aug. 9 [doi.org/10.1016/S1470-2045(12)70367-4]).
"First, the ability to deliver the drug in about 5 minutes without the need to secure intravenous access makes subcutaneous treatment more convenient," wrote Dr. Perez-Garcia and Dr. Cortes of Vall d’Hebron Institute of Oncology, Barcelona. "Second, in addition to time savings, once the drug can be administered at home, patients will be able to continue their lives with less hospital dependence, which is an important psychological aspect."
The study didn’t address which drug delivery method patients preferred, or how an at-home subcutaneous administration might affect their quality of life. But another randomized study, PrefHer, aims to explore that, they wrote. PrefHer will evaluate patients' preference and healthcare satisfaction with subcutaneous vs. intravenous trastuzumab.
They also noted that the HannaH study could set a precedent for rapid approval of neoadjuvant drugs based on the pathological complete response (pCR) – but that pCR as an end point has not yet been fully vetted. "This approach appears to have at least two major limitations. First, we do not know what improvement in pCR would be necessary to translate into disease-free survival or overall survival benefit. Second, we also do not know what proportion of patients achieving a pCR would be needed to establish noninferiority between two drugs or between two methods of administering the same drug."
Finally, they wrote. "Third, the method of categorizing long-term adverse effects might be insufficient because many adverse events might appear after pCR, so if pCR is enough for regulatory purposes, the consequences of these long-term events might not be taken into account."
Dr. Perez-Garcia is an oncologist in the breast cancer program at Vall d’Hebron Institute of Oncology, Barcelona. He had no financial disclosures. Dr. Cortes, of the same institution, disclosed relationships with Roche and other companies.
A rapid, subcutaneous delivery of trastuzumab could come with several big advantages, Dr. Jose Perez-Garcia and Dr. Javier Cortes wrote in an accompanying editorial (Lancet Onc. 2012 Aug. 9 [doi.org/10.1016/S1470-2045(12)70367-4]).
"First, the ability to deliver the drug in about 5 minutes without the need to secure intravenous access makes subcutaneous treatment more convenient," wrote Dr. Perez-Garcia and Dr. Cortes of Vall d’Hebron Institute of Oncology, Barcelona. "Second, in addition to time savings, once the drug can be administered at home, patients will be able to continue their lives with less hospital dependence, which is an important psychological aspect."
The study didn’t address which drug delivery method patients preferred, or how an at-home subcutaneous administration might affect their quality of life. But another randomized study, PrefHer, aims to explore that, they wrote. PrefHer will evaluate patients' preference and healthcare satisfaction with subcutaneous vs. intravenous trastuzumab.
They also noted that the HannaH study could set a precedent for rapid approval of neoadjuvant drugs based on the pathological complete response (pCR) – but that pCR as an end point has not yet been fully vetted. "This approach appears to have at least two major limitations. First, we do not know what improvement in pCR would be necessary to translate into disease-free survival or overall survival benefit. Second, we also do not know what proportion of patients achieving a pCR would be needed to establish noninferiority between two drugs or between two methods of administering the same drug."
Finally, they wrote. "Third, the method of categorizing long-term adverse effects might be insufficient because many adverse events might appear after pCR, so if pCR is enough for regulatory purposes, the consequences of these long-term events might not be taken into account."
Dr. Perez-Garcia is an oncologist in the breast cancer program at Vall d’Hebron Institute of Oncology, Barcelona. He had no financial disclosures. Dr. Cortes, of the same institution, disclosed relationships with Roche and other companies.
A subcutaneous injectable form of trastuzumab achieved pharmacokinetic and clinical outcomes that equaled those of intravenous infusion for women with HER2-positive breast cancers in a randomized open-label phase III study.
The international HannaH trial found no significant differences in presurgical serum trough levels at any time during the six-cycle neoadjuvant treatment. At the end of the year-long study, 45% of the subcutaneous group and 41% of the intravenous group had a pathological complete response (pCR).
The subcutaneous form of trastuzumab (Herceptin) takes 5 minutes to administer; patients can self-administer the drug at home. The infusion takes 90 minutes and must be done in the clinic.
If clinical results are equivalent, the injection could become an attractive alternative to intravenous treatment, Dr. Gustavo Ismael of the Hospital Amaral Carvalho, Jaú, Brazil, and his coauthors proposed in the Aug. 9 online issue of the Lancet Oncology (2012 [doi.org/10.1016/S1470-2045(12)70329-7]).*
"The shortened duration of administration with subcutaneous trastuzumab ... suggests the potential for substantial time saving for patients, physicians, and nursing staff," the investigators wrote.
Susan Willson, a spokesperson for Genentech, said the company is looking at the HannaH data, as well as that of other studies, to determine whether the subcutaneous form of trastuzumab will be put forth to the Food and Drug Administration.
Earlier this year, Roche, Genetech’s parent company, submitted a line extension application for subcutaneous trastuzumab to the European Medicines Association. The requested indication is the treatment of HER-2-positive breast cancer.
Trastuzumab Given with Neoadjuvant Chemo
The HannaH (enHANced treatment with NeoAdjuvant Herceptin) trial randomized 596 women with HER-2 positive breast cancer to six cycles of neoadjuvant chemotherapy with either the injections or intravenous infusions; both were administered once every 3 weeks.
The injection was a fixed dose of 600 mg trastuzumab with recombinant hyaluronidase PH-20 delivered to the thigh by study nurses. The enzyme temporarily degrades interstitial hyaluronan, expanding the space to accommodate the volume of the injection.
Women in the subcutaneous group did not take a loading dose of the medication. Those in the intravenous group received an 8 mg/kg loading dose followed by a 6 mg/kg maintenance dose. The follow-up period was 24 months or until disease recurrence
The chemotherapy regimen for both groups consisted of four 3-week cycles of docetaxel (Taxotere) followed by four cycles of fluorouracil and cyclophosphamide. After surgery, all patients continued their trastuzumab regimen for 1 year.
Median patient age was 50 years. About 50% were positive for estrogen receptor tumors. More than half had operable cancer; more than a third had locally advanced cancer; and about 6% had inflammatory breast cancer. Median follow-up in both groups was a little more than 1 year.
The pharmacokinetic profile was similar between the two forms of trastuzumab. After the first cycle, the mean trough serum level was similar between the injectable and intravenous forms (32.7 mcg/mL vs. 34.5 mcg/mL). The levels were also similar before the third cycle (45 and 48 mcg/mL). Almost all patients (98%) reached the therapeutic level of more than 20 micrograms/ml by cycle 8.
The mean presurgical trough level of the subcutaneous form was 58 mcg/mL; for the intravenous form, the mean level was 79 mcg/mL.
Similar Efficacy and Toxicity
The efficacy analysis included 523 patients and showed noninferiority of subcutaneous trastuzumab to intravenous trastuzumab. A pathological complete response occurred in 45% of the subcutaneous group and in 41% of the intravenous group in a per-protocol analysis. An intent-to-treat analysis showed similar numbers, with a complete pathological response in 42% of the subcutaneous group an 37% of the intravenous group.
Overall responses rates, including complete and partial responses, were comparable. Event-free and overall survival data were not yet mature, and have yet to be reported.
The rate of adverse events was similar between the subcutaneous and intravenous groups: alopecia (63% each), nausea (49% each), neutropenia (44% subcutaneous vs. 46% intravenous), diarrhea (34% subcutaneous vs. 37% intravenous), asthenia (25% each), and fatigue (23% subcutaneous vs. 26% intravenous).
The same proportion of patients in each group experienced at least one serious adverse event (52%). The most common were neutropenia, leucopenia, and febrile neutropenia.
Four adverse events lead to death – one in the subcutaneous group and three in the intravenous group during neoadjuvant treatment. These included a fatal acute pneumonia in an obese 66-year-old with pulmonary fibrosis in the subcutaneous group. In the intravenous group, the deaths were a myocardial infarction in an obese patient with a history of hypertension; a sudden death in an overweight patient who with hypertension and diabetes; fatal septic shock in a patient who developed febrile neutropenia. The septic shock and cardiac deaths were attributed to the treatment, the investigators said.
The proportion of grade 3 adverse events was similar in both groups, but the relative percentage of those classified as serious adverse events was 7.7% for the intravenous group and 18% for the subcutaneous group. "A similar finding was made for grade 2 adverse events, of which 0.5% was classed as serous ... in the intravenous group versus 1.5% in the subcutaneous group," they wrote. The investigators could not find an explanation for the imbalance in reporting of serious adverse events, but suggested that they may have been more conservative in assessing the subcutaneous arm of the trial.
Two patients in the subcutaneous group had mild congestive heart failure; both were obese with a history of hypertension. Six patients in the intravenous group and seven in the subcutaneous group had a significant decrease in left ventricular ejection fraction.
Antitrastuzumab antibodies developed in 10 patients in the intravenous group and 20 in the subcutaneous group, but these did not affect serum trough levels.
F. Hoffman-LaRoche funded the study Dr. Ismael disclosed that he has received honoraria from the company. His co-investigators also reported several financial relationships, including travels grants, speakers fees, research support, and employment.
Click here to hear Dr. Ismael discuss the trial in a podcast at the Lancet Oncology website.
*Correction, 08/13/12: This sentence was corrected to state that injectable trastuzumab could become an alternative to intravenous treatment. Weekly treatment was not specified.
A subcutaneous injectable form of trastuzumab achieved pharmacokinetic and clinical outcomes that equaled those of intravenous infusion for women with HER2-positive breast cancers in a randomized open-label phase III study.
The international HannaH trial found no significant differences in presurgical serum trough levels at any time during the six-cycle neoadjuvant treatment. At the end of the year-long study, 45% of the subcutaneous group and 41% of the intravenous group had a pathological complete response (pCR).
The subcutaneous form of trastuzumab (Herceptin) takes 5 minutes to administer; patients can self-administer the drug at home. The infusion takes 90 minutes and must be done in the clinic.
If clinical results are equivalent, the injection could become an attractive alternative to intravenous treatment, Dr. Gustavo Ismael of the Hospital Amaral Carvalho, Jaú, Brazil, and his coauthors proposed in the Aug. 9 online issue of the Lancet Oncology (2012 [doi.org/10.1016/S1470-2045(12)70329-7]).*
"The shortened duration of administration with subcutaneous trastuzumab ... suggests the potential for substantial time saving for patients, physicians, and nursing staff," the investigators wrote.
Susan Willson, a spokesperson for Genentech, said the company is looking at the HannaH data, as well as that of other studies, to determine whether the subcutaneous form of trastuzumab will be put forth to the Food and Drug Administration.
Earlier this year, Roche, Genetech’s parent company, submitted a line extension application for subcutaneous trastuzumab to the European Medicines Association. The requested indication is the treatment of HER-2-positive breast cancer.
Trastuzumab Given with Neoadjuvant Chemo
The HannaH (enHANced treatment with NeoAdjuvant Herceptin) trial randomized 596 women with HER-2 positive breast cancer to six cycles of neoadjuvant chemotherapy with either the injections or intravenous infusions; both were administered once every 3 weeks.
The injection was a fixed dose of 600 mg trastuzumab with recombinant hyaluronidase PH-20 delivered to the thigh by study nurses. The enzyme temporarily degrades interstitial hyaluronan, expanding the space to accommodate the volume of the injection.
Women in the subcutaneous group did not take a loading dose of the medication. Those in the intravenous group received an 8 mg/kg loading dose followed by a 6 mg/kg maintenance dose. The follow-up period was 24 months or until disease recurrence
The chemotherapy regimen for both groups consisted of four 3-week cycles of docetaxel (Taxotere) followed by four cycles of fluorouracil and cyclophosphamide. After surgery, all patients continued their trastuzumab regimen for 1 year.
Median patient age was 50 years. About 50% were positive for estrogen receptor tumors. More than half had operable cancer; more than a third had locally advanced cancer; and about 6% had inflammatory breast cancer. Median follow-up in both groups was a little more than 1 year.
The pharmacokinetic profile was similar between the two forms of trastuzumab. After the first cycle, the mean trough serum level was similar between the injectable and intravenous forms (32.7 mcg/mL vs. 34.5 mcg/mL). The levels were also similar before the third cycle (45 and 48 mcg/mL). Almost all patients (98%) reached the therapeutic level of more than 20 micrograms/ml by cycle 8.
The mean presurgical trough level of the subcutaneous form was 58 mcg/mL; for the intravenous form, the mean level was 79 mcg/mL.
Similar Efficacy and Toxicity
The efficacy analysis included 523 patients and showed noninferiority of subcutaneous trastuzumab to intravenous trastuzumab. A pathological complete response occurred in 45% of the subcutaneous group and in 41% of the intravenous group in a per-protocol analysis. An intent-to-treat analysis showed similar numbers, with a complete pathological response in 42% of the subcutaneous group an 37% of the intravenous group.
Overall responses rates, including complete and partial responses, were comparable. Event-free and overall survival data were not yet mature, and have yet to be reported.
The rate of adverse events was similar between the subcutaneous and intravenous groups: alopecia (63% each), nausea (49% each), neutropenia (44% subcutaneous vs. 46% intravenous), diarrhea (34% subcutaneous vs. 37% intravenous), asthenia (25% each), and fatigue (23% subcutaneous vs. 26% intravenous).
The same proportion of patients in each group experienced at least one serious adverse event (52%). The most common were neutropenia, leucopenia, and febrile neutropenia.
Four adverse events lead to death – one in the subcutaneous group and three in the intravenous group during neoadjuvant treatment. These included a fatal acute pneumonia in an obese 66-year-old with pulmonary fibrosis in the subcutaneous group. In the intravenous group, the deaths were a myocardial infarction in an obese patient with a history of hypertension; a sudden death in an overweight patient who with hypertension and diabetes; fatal septic shock in a patient who developed febrile neutropenia. The septic shock and cardiac deaths were attributed to the treatment, the investigators said.
The proportion of grade 3 adverse events was similar in both groups, but the relative percentage of those classified as serious adverse events was 7.7% for the intravenous group and 18% for the subcutaneous group. "A similar finding was made for grade 2 adverse events, of which 0.5% was classed as serous ... in the intravenous group versus 1.5% in the subcutaneous group," they wrote. The investigators could not find an explanation for the imbalance in reporting of serious adverse events, but suggested that they may have been more conservative in assessing the subcutaneous arm of the trial.
Two patients in the subcutaneous group had mild congestive heart failure; both were obese with a history of hypertension. Six patients in the intravenous group and seven in the subcutaneous group had a significant decrease in left ventricular ejection fraction.
Antitrastuzumab antibodies developed in 10 patients in the intravenous group and 20 in the subcutaneous group, but these did not affect serum trough levels.
F. Hoffman-LaRoche funded the study Dr. Ismael disclosed that he has received honoraria from the company. His co-investigators also reported several financial relationships, including travels grants, speakers fees, research support, and employment.
Click here to hear Dr. Ismael discuss the trial in a podcast at the Lancet Oncology website.
*Correction, 08/13/12: This sentence was corrected to state that injectable trastuzumab could become an alternative to intravenous treatment. Weekly treatment was not specified.
FROM LANCET ONCOLOGY
Major Finding: A pathologic complete response occurred in 45% of those who used a subcutaneous injectable trastuzumab and 41% of those who underwent the traditional intravenous treatment.
Data Source: HannaH was an open-label, randomized study of 596 women with HER2-positive breast cancer.
Disclosures: F. Hoffman-LaRoche funded the study Dr. Ismael disclosed that he has received honoraria from the company. His co-investigators also reported financial relationships, including travels grants, speakers’ fees, research support, and employment.
Pregnancy-Related Cancers: Rise Is Largely Unrelated to Delayed Childbearing
MINNEAPOLIS – Pregnancy-associated cancers are increasing, although the phenomenon of delayed childbirth is only partially responsible, researchers suggest.
From 1994 to 2008, the crude incidence of pregnancy-associated cancer increased from 112 to 192 per 100,000 pregnancies (P less than .001) in an analysis of 787,907 Australian women.
During the same period, the number of Australian mothers aged 35 years or more nearly doubled from 13% to 24%, including an increase from 2% to 4% of mothers over age 40, Christine L. Roberts, Ph.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
After the cancer rate was standardized to the age of the 1994 population, however, only 14% of the increase in cancer was explained by increasing maternal age, said Dr. Roberts of the University of Sydney, New South Wales, Australia.
"Improved diagnostic techniques, detection, and interracial health services likely contribute to the unexplained portion," she said. "The increasing incidence of cancer confirmed a clinical impression that obstetricians were seeing women with cancer more frequently, although of course it remains uncommon."
The growing number of women postponing childbearing has raised concerns that the incidence of pregnancy-associated cancer would rise. The incidence is generally reported to be about 1 in 1,000 pregnancies, but estimates based largely on cancer reports have been imprecise, Dr. Roberts said.
The investigators obtained cancer and maternal information from linked cancer registry, birth, and hospital records for 1.31 million pregnancies and 1.33 million infants among 781,907 women in Australia.
During the study period, 1,798 women had a new cancer diagnosis: 499 during pregnancy and 1,299 within 12 months of delivery. This equates to 137.3 cancers per 100,000 pregnancies, Dr. Roberts said.
There were 42 cancer deaths, or 3.2 deaths per 100,000 pregnancies.
The highest proportion of cancers (14.5%) was diagnosed in the first 2 months post partum, lending support to the rationale that women and physicians may incorrectly attribute cancer-related symptoms to the physiologic changes of pregnancy and may be reluctant to use radiographs or invasive procedures during pregnancy, she observed.
The cancers were predominantly melanoma (599) or breast cancer (377), followed by thyroid/endocrine (228) and lymphohematopoietic (151) cancers.
Melanoma was twice as likely to be observed in pregnant women as in women of similar reproductive age (observed to expected ratio, 2.2), according to the authors, led by Dr. Yuen Yi (Cathy) Lee of the New South Wales Ministry of Health in North Sydney, Australia.
In prior studies, breast and thyroid cancer were the most common pregnancy-related cancers in California in the 1990s (Am. J. Obstet. Gynecol. 2003;189:1128-35), whereas more recently, melanoma and cervical cancer were the most common cancers during pregnancy in Norway (J. Clin. Oncol. 2009;27:45-51), Dr. Roberts noted.
In logistic regression analysis adjusted for age, country of birth, socioeconomic status, rural residence, parity, plurality, previous cancer, and assisted reproductive technology, significant risk factors for a pregnancy-associated cancer were previous cancer diagnosis (adjusted odds ratio, 3.8), multiple pregnancy (OR, 1.5), age 30-34 years (OR, 2.1), age 35-39 years (OR, 3.0), and age 40 years or older (OR, 3.6).
Women with a cancer diagnosis had a significantly higher risk of thromboembolic events (OR, 10.2), sepsis (OR, 4.3), and life-threatening maternal morbidity (OR, 6.9) after adjustment for maternal age, socioeconomic status, plurality, parity, previous preterm birth, diabetes, and hypertension.
A novel finding was that cancer during pregnancy also was associated with large-for-gestational age infants (OR, 1.5), said Dr. Roberts, who pointed out that large-for-gestational age is also a risk factor for pediatric cancer.
"Elevated levels of maternal hormone angiogenic factors during pregnancy may influence both infant size and tumor growth," she speculated.
Dr. Roberts said there is an Australian national policy on cervical screening recommending that Pap smears be offered to every woman presenting for antenatal care who has not had cervical screening within the past 2 years; however, this was introduced in 2008 at the end of the study period. "We are not aware of other policies for screening during pregnancy," she added.
Full details of the study are expected to be published in the coming weeks (BJOG 2012 [doi: 10.111/j.1471-0528.2012.03475.x]).
The authors report no conflicts of interest.
postponing childbearing, pregnancy-associated cancer,
MINNEAPOLIS – Pregnancy-associated cancers are increasing, although the phenomenon of delayed childbirth is only partially responsible, researchers suggest.
From 1994 to 2008, the crude incidence of pregnancy-associated cancer increased from 112 to 192 per 100,000 pregnancies (P less than .001) in an analysis of 787,907 Australian women.
During the same period, the number of Australian mothers aged 35 years or more nearly doubled from 13% to 24%, including an increase from 2% to 4% of mothers over age 40, Christine L. Roberts, Ph.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
After the cancer rate was standardized to the age of the 1994 population, however, only 14% of the increase in cancer was explained by increasing maternal age, said Dr. Roberts of the University of Sydney, New South Wales, Australia.
"Improved diagnostic techniques, detection, and interracial health services likely contribute to the unexplained portion," she said. "The increasing incidence of cancer confirmed a clinical impression that obstetricians were seeing women with cancer more frequently, although of course it remains uncommon."
The growing number of women postponing childbearing has raised concerns that the incidence of pregnancy-associated cancer would rise. The incidence is generally reported to be about 1 in 1,000 pregnancies, but estimates based largely on cancer reports have been imprecise, Dr. Roberts said.
The investigators obtained cancer and maternal information from linked cancer registry, birth, and hospital records for 1.31 million pregnancies and 1.33 million infants among 781,907 women in Australia.
During the study period, 1,798 women had a new cancer diagnosis: 499 during pregnancy and 1,299 within 12 months of delivery. This equates to 137.3 cancers per 100,000 pregnancies, Dr. Roberts said.
There were 42 cancer deaths, or 3.2 deaths per 100,000 pregnancies.
The highest proportion of cancers (14.5%) was diagnosed in the first 2 months post partum, lending support to the rationale that women and physicians may incorrectly attribute cancer-related symptoms to the physiologic changes of pregnancy and may be reluctant to use radiographs or invasive procedures during pregnancy, she observed.
The cancers were predominantly melanoma (599) or breast cancer (377), followed by thyroid/endocrine (228) and lymphohematopoietic (151) cancers.
Melanoma was twice as likely to be observed in pregnant women as in women of similar reproductive age (observed to expected ratio, 2.2), according to the authors, led by Dr. Yuen Yi (Cathy) Lee of the New South Wales Ministry of Health in North Sydney, Australia.
In prior studies, breast and thyroid cancer were the most common pregnancy-related cancers in California in the 1990s (Am. J. Obstet. Gynecol. 2003;189:1128-35), whereas more recently, melanoma and cervical cancer were the most common cancers during pregnancy in Norway (J. Clin. Oncol. 2009;27:45-51), Dr. Roberts noted.
In logistic regression analysis adjusted for age, country of birth, socioeconomic status, rural residence, parity, plurality, previous cancer, and assisted reproductive technology, significant risk factors for a pregnancy-associated cancer were previous cancer diagnosis (adjusted odds ratio, 3.8), multiple pregnancy (OR, 1.5), age 30-34 years (OR, 2.1), age 35-39 years (OR, 3.0), and age 40 years or older (OR, 3.6).
Women with a cancer diagnosis had a significantly higher risk of thromboembolic events (OR, 10.2), sepsis (OR, 4.3), and life-threatening maternal morbidity (OR, 6.9) after adjustment for maternal age, socioeconomic status, plurality, parity, previous preterm birth, diabetes, and hypertension.
A novel finding was that cancer during pregnancy also was associated with large-for-gestational age infants (OR, 1.5), said Dr. Roberts, who pointed out that large-for-gestational age is also a risk factor for pediatric cancer.
"Elevated levels of maternal hormone angiogenic factors during pregnancy may influence both infant size and tumor growth," she speculated.
Dr. Roberts said there is an Australian national policy on cervical screening recommending that Pap smears be offered to every woman presenting for antenatal care who has not had cervical screening within the past 2 years; however, this was introduced in 2008 at the end of the study period. "We are not aware of other policies for screening during pregnancy," she added.
Full details of the study are expected to be published in the coming weeks (BJOG 2012 [doi: 10.111/j.1471-0528.2012.03475.x]).
The authors report no conflicts of interest.
MINNEAPOLIS – Pregnancy-associated cancers are increasing, although the phenomenon of delayed childbirth is only partially responsible, researchers suggest.
From 1994 to 2008, the crude incidence of pregnancy-associated cancer increased from 112 to 192 per 100,000 pregnancies (P less than .001) in an analysis of 787,907 Australian women.
During the same period, the number of Australian mothers aged 35 years or more nearly doubled from 13% to 24%, including an increase from 2% to 4% of mothers over age 40, Christine L. Roberts, Ph.D., said at the annual meeting of the Society for Pediatric and Perinatal Epidemiologic Research.
After the cancer rate was standardized to the age of the 1994 population, however, only 14% of the increase in cancer was explained by increasing maternal age, said Dr. Roberts of the University of Sydney, New South Wales, Australia.
"Improved diagnostic techniques, detection, and interracial health services likely contribute to the unexplained portion," she said. "The increasing incidence of cancer confirmed a clinical impression that obstetricians were seeing women with cancer more frequently, although of course it remains uncommon."
The growing number of women postponing childbearing has raised concerns that the incidence of pregnancy-associated cancer would rise. The incidence is generally reported to be about 1 in 1,000 pregnancies, but estimates based largely on cancer reports have been imprecise, Dr. Roberts said.
The investigators obtained cancer and maternal information from linked cancer registry, birth, and hospital records for 1.31 million pregnancies and 1.33 million infants among 781,907 women in Australia.
During the study period, 1,798 women had a new cancer diagnosis: 499 during pregnancy and 1,299 within 12 months of delivery. This equates to 137.3 cancers per 100,000 pregnancies, Dr. Roberts said.
There were 42 cancer deaths, or 3.2 deaths per 100,000 pregnancies.
The highest proportion of cancers (14.5%) was diagnosed in the first 2 months post partum, lending support to the rationale that women and physicians may incorrectly attribute cancer-related symptoms to the physiologic changes of pregnancy and may be reluctant to use radiographs or invasive procedures during pregnancy, she observed.
The cancers were predominantly melanoma (599) or breast cancer (377), followed by thyroid/endocrine (228) and lymphohematopoietic (151) cancers.
Melanoma was twice as likely to be observed in pregnant women as in women of similar reproductive age (observed to expected ratio, 2.2), according to the authors, led by Dr. Yuen Yi (Cathy) Lee of the New South Wales Ministry of Health in North Sydney, Australia.
In prior studies, breast and thyroid cancer were the most common pregnancy-related cancers in California in the 1990s (Am. J. Obstet. Gynecol. 2003;189:1128-35), whereas more recently, melanoma and cervical cancer were the most common cancers during pregnancy in Norway (J. Clin. Oncol. 2009;27:45-51), Dr. Roberts noted.
In logistic regression analysis adjusted for age, country of birth, socioeconomic status, rural residence, parity, plurality, previous cancer, and assisted reproductive technology, significant risk factors for a pregnancy-associated cancer were previous cancer diagnosis (adjusted odds ratio, 3.8), multiple pregnancy (OR, 1.5), age 30-34 years (OR, 2.1), age 35-39 years (OR, 3.0), and age 40 years or older (OR, 3.6).
Women with a cancer diagnosis had a significantly higher risk of thromboembolic events (OR, 10.2), sepsis (OR, 4.3), and life-threatening maternal morbidity (OR, 6.9) after adjustment for maternal age, socioeconomic status, plurality, parity, previous preterm birth, diabetes, and hypertension.
A novel finding was that cancer during pregnancy also was associated with large-for-gestational age infants (OR, 1.5), said Dr. Roberts, who pointed out that large-for-gestational age is also a risk factor for pediatric cancer.
"Elevated levels of maternal hormone angiogenic factors during pregnancy may influence both infant size and tumor growth," she speculated.
Dr. Roberts said there is an Australian national policy on cervical screening recommending that Pap smears be offered to every woman presenting for antenatal care who has not had cervical screening within the past 2 years; however, this was introduced in 2008 at the end of the study period. "We are not aware of other policies for screening during pregnancy," she added.
Full details of the study are expected to be published in the coming weeks (BJOG 2012 [doi: 10.111/j.1471-0528.2012.03475.x]).
The authors report no conflicts of interest.
postponing childbearing, pregnancy-associated cancer,
postponing childbearing, pregnancy-associated cancer,
AT THE ANNUAL MEETING OF THE SOCIETY FOR PEDIATRIC AND PERINATAL EPIDEMIOLOGIC RESEARCH
Radiation Oncologists Say Medicare Cuts Could Shutter Practices
Radiation oncologists say they could be forced to shut their doors or consolidate their practices, if the proposed cuts to radiation therapy in the 2013 Medicare physician fee schedule are allowed to stay in place.
And this is likely to hasten a shift of services out of the community and into the hospital, according to officials at the American Society for Radiation Oncology (ASTRO), which surveyed its membership in the wake of the Centers for Medicare and Medicaid Services’ proposed rule in early July.
"Some patients will likely receive their care in radiation therapy centers at a far greater distance from their home in both hospital-based facilities and larger freestanding centers that survive these cuts," said Dr. Michael L. Steinberg, president of the ASTRO’s board of directors, in an interview.
With the closure of radiation therapy centers, physicians would seek employment in surviving freestanding or hospital-based facilities, he added,
The CMS is proposing a 15% reduction in payment for IMRT (Intensity Modulated Radiation Therapy) and SBRT (Stereotactic Body Radiation Therapy). The agency also proposed a 19% cut for community-based radiation therapy centers.
IMRT and SBRT account for about a third of Medicare spending on radiation therapy, according to a spokeswoman for the ASTRO. Medicare and Medicaid are the predominant payers for radiation therapy, which is delivered to two-thirds of the nation’s 1.5 million cancer patients annually.
The ASTRO survey, which was conducted online, received about 600 responses. (There are about 4,500 radiation oncologists in the United States.) Of the 599 who participated, almost 60% were from community practices or combined community- and hospital-based practices. The results reported were only for that 60%.
Physicians were not asked about the impact of the almost-29% overall cut in physician pay called for by Medicare’s Sustainable Growth Rate (SGR) formula.
If just the close-to-20% cut for radiation therapy centers goes into effect, 35% of practices said they would probably have to close their doors, and 64% said they would consolidate. Both actions would lead to longer wait times for treatment, said ASTRO CEO Laura Thevenot in a briefing with reporters.
The consequences may also mean that physicians will spend less time with patients – that is, with those patients who would still be able to access a radiation oncologist. Some 70% of respondents said they would limit Medicare patients if the cuts go through, and 49% said they would stop accepting Medicare patients altogether.
Radiation oncologists also said they would cut back on purchases of new technology and lay off support staff and other nonphysician employees.
"The likely end result for limited access to radiation therapy – an integral form of care used in nearly 70% of all cancer patients – would be an erosion in the gains in cure rates, quality of life, and other clinical outcomes that have been achieved in our country over the last 20 years," said Dr. Constantine A. Mantz, a radiation oncologist in Ft. Myers, Fla., during the press briefing.
Ms. Thevenot said that the CMS had used faulty information to calculate the true costs of IMRT and SBRT, and that the agency should revisit the codes for both procedures.
Added Dr. Steinberg in a statement, "ASTRO welcomes a comprehensive review of these procedure codes and supports the necessary sophistication of a process, such as provided by the [American Medical Association’s Relative Value Scale Update Committee (RUC)], to value complex medical procedures including IMRT and SBRT." He is also professor and chairman of radiation oncology at the University of California, Los Angeles.
According to Ms. Thevenot, IMRT was reviewed by AMA’s RUC in fall 2010, and SBRT was reviewed in February 2011.
The ASTRO has also enlisted the support of Congress to overturn the cuts. Representatives Joe Pitts (R-Penn.) and Frank Pallone (D-N.J.), along with Rep. Mike Rogers (R-Mich.), have been circulating a letter decrying the cuts that will eventually be sent to officials at the CMS. The organization says that a "similar bipartisan letter is being drafted in the Senate."
Radiation oncologists say they could be forced to shut their doors or consolidate their practices, if the proposed cuts to radiation therapy in the 2013 Medicare physician fee schedule are allowed to stay in place.
And this is likely to hasten a shift of services out of the community and into the hospital, according to officials at the American Society for Radiation Oncology (ASTRO), which surveyed its membership in the wake of the Centers for Medicare and Medicaid Services’ proposed rule in early July.
"Some patients will likely receive their care in radiation therapy centers at a far greater distance from their home in both hospital-based facilities and larger freestanding centers that survive these cuts," said Dr. Michael L. Steinberg, president of the ASTRO’s board of directors, in an interview.
With the closure of radiation therapy centers, physicians would seek employment in surviving freestanding or hospital-based facilities, he added,
The CMS is proposing a 15% reduction in payment for IMRT (Intensity Modulated Radiation Therapy) and SBRT (Stereotactic Body Radiation Therapy). The agency also proposed a 19% cut for community-based radiation therapy centers.
IMRT and SBRT account for about a third of Medicare spending on radiation therapy, according to a spokeswoman for the ASTRO. Medicare and Medicaid are the predominant payers for radiation therapy, which is delivered to two-thirds of the nation’s 1.5 million cancer patients annually.
The ASTRO survey, which was conducted online, received about 600 responses. (There are about 4,500 radiation oncologists in the United States.) Of the 599 who participated, almost 60% were from community practices or combined community- and hospital-based practices. The results reported were only for that 60%.
Physicians were not asked about the impact of the almost-29% overall cut in physician pay called for by Medicare’s Sustainable Growth Rate (SGR) formula.
If just the close-to-20% cut for radiation therapy centers goes into effect, 35% of practices said they would probably have to close their doors, and 64% said they would consolidate. Both actions would lead to longer wait times for treatment, said ASTRO CEO Laura Thevenot in a briefing with reporters.
The consequences may also mean that physicians will spend less time with patients – that is, with those patients who would still be able to access a radiation oncologist. Some 70% of respondents said they would limit Medicare patients if the cuts go through, and 49% said they would stop accepting Medicare patients altogether.
Radiation oncologists also said they would cut back on purchases of new technology and lay off support staff and other nonphysician employees.
"The likely end result for limited access to radiation therapy – an integral form of care used in nearly 70% of all cancer patients – would be an erosion in the gains in cure rates, quality of life, and other clinical outcomes that have been achieved in our country over the last 20 years," said Dr. Constantine A. Mantz, a radiation oncologist in Ft. Myers, Fla., during the press briefing.
Ms. Thevenot said that the CMS had used faulty information to calculate the true costs of IMRT and SBRT, and that the agency should revisit the codes for both procedures.
Added Dr. Steinberg in a statement, "ASTRO welcomes a comprehensive review of these procedure codes and supports the necessary sophistication of a process, such as provided by the [American Medical Association’s Relative Value Scale Update Committee (RUC)], to value complex medical procedures including IMRT and SBRT." He is also professor and chairman of radiation oncology at the University of California, Los Angeles.
According to Ms. Thevenot, IMRT was reviewed by AMA’s RUC in fall 2010, and SBRT was reviewed in February 2011.
The ASTRO has also enlisted the support of Congress to overturn the cuts. Representatives Joe Pitts (R-Penn.) and Frank Pallone (D-N.J.), along with Rep. Mike Rogers (R-Mich.), have been circulating a letter decrying the cuts that will eventually be sent to officials at the CMS. The organization says that a "similar bipartisan letter is being drafted in the Senate."
Radiation oncologists say they could be forced to shut their doors or consolidate their practices, if the proposed cuts to radiation therapy in the 2013 Medicare physician fee schedule are allowed to stay in place.
And this is likely to hasten a shift of services out of the community and into the hospital, according to officials at the American Society for Radiation Oncology (ASTRO), which surveyed its membership in the wake of the Centers for Medicare and Medicaid Services’ proposed rule in early July.
"Some patients will likely receive their care in radiation therapy centers at a far greater distance from their home in both hospital-based facilities and larger freestanding centers that survive these cuts," said Dr. Michael L. Steinberg, president of the ASTRO’s board of directors, in an interview.
With the closure of radiation therapy centers, physicians would seek employment in surviving freestanding or hospital-based facilities, he added,
The CMS is proposing a 15% reduction in payment for IMRT (Intensity Modulated Radiation Therapy) and SBRT (Stereotactic Body Radiation Therapy). The agency also proposed a 19% cut for community-based radiation therapy centers.
IMRT and SBRT account for about a third of Medicare spending on radiation therapy, according to a spokeswoman for the ASTRO. Medicare and Medicaid are the predominant payers for radiation therapy, which is delivered to two-thirds of the nation’s 1.5 million cancer patients annually.
The ASTRO survey, which was conducted online, received about 600 responses. (There are about 4,500 radiation oncologists in the United States.) Of the 599 who participated, almost 60% were from community practices or combined community- and hospital-based practices. The results reported were only for that 60%.
Physicians were not asked about the impact of the almost-29% overall cut in physician pay called for by Medicare’s Sustainable Growth Rate (SGR) formula.
If just the close-to-20% cut for radiation therapy centers goes into effect, 35% of practices said they would probably have to close their doors, and 64% said they would consolidate. Both actions would lead to longer wait times for treatment, said ASTRO CEO Laura Thevenot in a briefing with reporters.
The consequences may also mean that physicians will spend less time with patients – that is, with those patients who would still be able to access a radiation oncologist. Some 70% of respondents said they would limit Medicare patients if the cuts go through, and 49% said they would stop accepting Medicare patients altogether.
Radiation oncologists also said they would cut back on purchases of new technology and lay off support staff and other nonphysician employees.
"The likely end result for limited access to radiation therapy – an integral form of care used in nearly 70% of all cancer patients – would be an erosion in the gains in cure rates, quality of life, and other clinical outcomes that have been achieved in our country over the last 20 years," said Dr. Constantine A. Mantz, a radiation oncologist in Ft. Myers, Fla., during the press briefing.
Ms. Thevenot said that the CMS had used faulty information to calculate the true costs of IMRT and SBRT, and that the agency should revisit the codes for both procedures.
Added Dr. Steinberg in a statement, "ASTRO welcomes a comprehensive review of these procedure codes and supports the necessary sophistication of a process, such as provided by the [American Medical Association’s Relative Value Scale Update Committee (RUC)], to value complex medical procedures including IMRT and SBRT." He is also professor and chairman of radiation oncology at the University of California, Los Angeles.
According to Ms. Thevenot, IMRT was reviewed by AMA’s RUC in fall 2010, and SBRT was reviewed in February 2011.
The ASTRO has also enlisted the support of Congress to overturn the cuts. Representatives Joe Pitts (R-Penn.) and Frank Pallone (D-N.J.), along with Rep. Mike Rogers (R-Mich.), have been circulating a letter decrying the cuts that will eventually be sent to officials at the CMS. The organization says that a "similar bipartisan letter is being drafted in the Senate."