User login
Methodologic Progress Note: Opportunistic Sampling for Pharmacology Studies in Hospitalized Children
Challenges in conducting and completing studies of drugs in vulnerable populations, such as hospitalized children, include weak study designs and lack of sufficient sample sizes to achieve adequate power.1 Limitations in the amount of blood that can be safely drawn in children and low parental consent rates due to concerns for anemia or pain, if venipuncture is required, lead to an insufficient number of patients enrolled in traditional clinical studies.2 Thus, sample size targets are often not met. Recognizing the limited pediatric data for many drugs routinely prescribed off-label in children, the Food and Drug Administration implemented the Best Pharmaceuticals Children Act and the Pediatric Research Equity Act (PREA) in 2003; these legislative acts require clinical studies to assess the safety and efficacy of new drugs in children.1 While studies conducted under these acts have provided important information for the clinical care of children, only one-third of mandatory pediatric postmarketing studies of the 114 new drugs and new indications subject to PREA requirements between 2007 and 2014 had been completed within seven years.3
Despite the challenges in conducting studies of drugs in children, robust pediatric data must be generated in children, especially in those with medical complexity or with chronic medical diseases and who have significant risk of experiencing adverse drug events. Data in adults cannot simply be extrapolated to children. In addition, studies from healthy children may not apply to hospitalized pediatric patients because of significant physiologic changes that occur in children who are ill enough to be hospitalized. Opportunistic sampling can provide robust drug disposition data and overcome some of the challenges encountered by traditional drug studies. In this Methodologic Progress Note, we describe the utility of opportunistic sampling as a research tool for hospitalists, in partnership with clinical pharmacologists, to study drug pharmacokinetics (PK) in hospitalized children.
OPPORTUNISTIC SAMPLING DEFINED
Opportunistic sampling relies on the use of blood samples that are ordered for clinical purposes, and its use is endorsed by the Pediatric Trials Network.2,5 Opportunistic sampling approaches have two types: sparse sampling and scavenged or remnant sampling. In sparse opportunistic sampling, additional blood is obtained at the same time clinical samples are ordered, avoiding the need for additional punctures.5 This approach requires bedside personnel to obtain additional blood that is sent to the research team for further processing. Scavenged sampling relies on leftover residual blood from clinical samples.2,5 After the clinical laboratory performs the laboratory test ordered by the clinical team, the research team can scavenge residual blood for measurement of drug concentrations. When drug concentrations are measured from multiple patients, clinical pharmacologists can perform population PK modeling to characterize the pharmacokinetics of the drug and its variability within the population level.
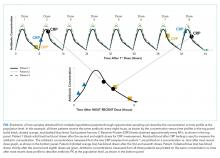
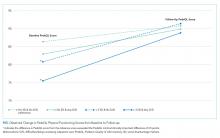
The Figure shows how scavenged samples from hypothetical patients could be used to generate a PK curve. In this example, three patients are admitted for osteomyelitis and treated with the same antibiotic administered every eight hours, as shown by the theoretical concentration versus time profiles in the top panel. To determine the effectiveness of treatment and timing of transition to enteral antibiotics, the clinical team orders C-reactive protein (CRP) approximately every 48 hours for each patient. Each patient has his/her first dose of antibiotic at a different time of day depending on the time of admission or surgical drainage. Therefore, the timing of the blood draw with respect to the most recent antibiotic dose varies between patients even if blood draws are ordered at the same time for all patients (ie, 4
Opportunistic sampling has advantages over traditional intensive PK studies that often require multiple blood draws (typically >8-10) within one dosing interval to adequately describe the phases of absorption, distribution, metabolism, and elimination. The number of vascular punctures can be painful if blood cannot be drawn from existing vascular access, and the large amount of blood (sometimes >1 mL/sample) required for these studies can be impractical, burdensome, and even dangerous in young children and neonates. Scavenged sampling reduces the risk of anemia because no additional blood is drawn beyond what is obtained for clinical purposes, and it does not disrupt nursing workflow or add to nursing workload. Approval to use scavenged blood requires approval from the institutional review board. At some institutions, the consent to treat form on admission may address the use of scavenged samples and therefore allow for waiver of consent. In addition, the consent process may occur retroactively after samples are collected. These methods lead to increased enrollment.
Limitations in this approach are that drugs may degrade over time in whole blood or processed samples. Therefore, the process by which the clinical laboratory stores the residual blood after clinical tests must be understood, and the stability of the drug or metabolite of interest in blood or plasma over time must be ensured. In addition, residual blood may not be present after a clinical test, and recording times of the drug administration and lab draws may be inaccurate.2,5
APPLICATIONS OF OPPORTUNISTIC SAMPLING IN CLINICAL PHARMACOLOGY RESEARCH
/section>Opportunistic sampling has been successfully used to study a variety of drugs in different pediatric populations but has been primarily used in neonates. The multicenter Pharmacokinetics of Understudied Drugs Administered to Children per Standard of Care trial has utilized this approach to evaluate the PK of over 30 drugs.5 Several antimicrobials have been studied through opportunistic sampling, including those frequently used in pediatric hospital medicine, such as ampicillin6 and clindamycin.7
This sampling approach may be most beneficial in studying select patients. Obese patients, who are often excluded in pediatric drug trials, have been previously included in opportunistic drug studies.8 The utility of opportunistic sampling to study antimicrobials, morphine and cardiac drugs has been demonstrated in neonates, both preterm and term, in whom additional blood draws can be challenging because of low total blood volume and limited vascular access.6,7,9-12
Although the frequency of blood draws from patients admitted to pediatric hospital medicine services is generally lower than that for patients on other subspecialty services, such as critical care, we can capitalize on the high volume of patients with common diagnoses (eg, pneumonia, skin, and soft tissue infections) who are admitted to hospital medicine. Using opportunistic sampling, we can study the PK of drugs frequently used in hospital medicine, such as antibiotics, antiepileptic drugs, steroids, and pain medications. In addition, we can measure drug concentrations to study the effects of route administration, oral versus enteric tube versus intravenous, to guide not only the dosing but also the timing of transition to enteral medications. Finally, we can study drugs that are commonly used in adult and pediatric patient populations cared for by hospitalists but who are often excluded from clinical drug trials, such as patients with medical complexity, patients with medical devices (eg, nervous system shunts and tracheostomies), patients taking concomitant medications, or patients on extracorporeal devices such as dialysis, to validate drug regimens.
CONCLUSION
Generating robust pediatric clinical pharmacology data has many inherent challenges because of the vulnerability of children. However, their vulnerability requires that medications be studied thoroughly in children to ensure their safety and effectiveness. Opportunistic sampling allows for rigorous studies to be conducted with adequate sample sizes while minimizing the risk of pain, anemia, and other adverse events related to clinical drug trials. Pediatric hospitalists should consider this approach to advance their knowledge of commonly used drugs that have not been adequately studied in hospitalized children and can expand the use of opportunistic sampling to study other aspects of disease, such as diagnostic or prognostic biomarkers.
1. Field MJ, Boat TF, eds. Safe and Effective Medicines for Children: Pediatric Studies Conducted Under the Best Pharmaceuticals for Children Act and the Pediatric Research Equity Act. Washington, DC, USA: National Academies Press; 2012.
2. Laughon MM, Benjamin DK, Jr., Capparelli EV, et al. Innovative clinical trial design for pediatric therapeutics. Expert Rev Clin Pharmacol. 2011;4(5):643-652. https://doi.org/10.1586/ecp.11.43.
3. Hwang TJ, Orenstein L, Kesselheim AS, Bourgeois FT. Completion rate and reporting of mandatory pediatric postmarketing studies under the US Pediatric Research Equity Act. JAMA Pediatr. 2018;173(1):68-74. https://doi.org/10.1001/jamapediatrics.2018.3416.
4. Rieder M. Adverse drug reactions in children: pediatric pharmacy and drug safety. J Pediatr Pharmacol Ther. 2019;24(1):4-9. https://doi.org/10.5863/1551-6776-24.1.4.
5. Balevic SJ, Cohen-Wolkowiez M. Innovative study designs optimizing clinical pharmacology research in infants and children. J Clin Pharmacol. 2018;58(10):S58-S72. https://doi.org/10.1002/jcph.1053.
6. Tremoulet A, Le J, Poindexter B, et al. Characterization of the population pharmacokinetics of ampicillin in neonates using an opportunistic study design. Antimicrob Agents Chemother. 2014;58(6):3013-3020. https://doi.org/10.1128/AAC.02374-13.
7. Gonzalez D, Melloni C, Yogev R, et al. Use of opportunistic clinical data and a population pharmacokinetic model to support dosing of clindamycin for premature infants to adolescents. Clin Pharmacol Ther. 2014;96(4):429-437. https://doi.org/10.1038/clpt.2014.134.
8. Smith MJ, Gonzalez D, Goldman JL, et al. Pharmacokinetics of clindamycin in obese and nonobese children. Antimicrob Agents Chemother. 2017;61(4). https://doi.org/10.1128/AAC.02014-16.
9. Leroux S, Turner MA, Guellec CB, et al. Pharmacokinetic studies in neonates: The utility of an opportunistic sampling design. Clin Pharmacokinet. 2015;54(12):1273-1285. https://doi.org/10.1007/s40262-015-0291-1.
10. Dallefeld SH, Atz AM, Yogev R, et al. A pharmacokinetic model for amiodarone in infants developed from an opportunistic sampling trial and published literature data. J Pharmacokinet Pharmacodyn. 2018;45(3):419-430. https://doi.org/10.1007/s10928-018-9576-y.
11. Thakkar N, Gonzalez D, Cohen-Wolkowiez M, et al. An opportunistic study evaluating pharmacokinetics of sildenafil for the treatment of pulmonary hypertension in infants. J Perinatol. 2016;36(9):744-747. https://doi.org/10.1038/jp.2016.79.
12. Euteneuer JC, Mizuno T, Fukuda T, Zhao J, Setchell KD, Vinks AA. Large variability in morphine concentrations in critically ill neonates receiving standard of care postoperative pain-management. Clin Pharmacol Ther. 2018;103:S45-S45.
Challenges in conducting and completing studies of drugs in vulnerable populations, such as hospitalized children, include weak study designs and lack of sufficient sample sizes to achieve adequate power.1 Limitations in the amount of blood that can be safely drawn in children and low parental consent rates due to concerns for anemia or pain, if venipuncture is required, lead to an insufficient number of patients enrolled in traditional clinical studies.2 Thus, sample size targets are often not met. Recognizing the limited pediatric data for many drugs routinely prescribed off-label in children, the Food and Drug Administration implemented the Best Pharmaceuticals Children Act and the Pediatric Research Equity Act (PREA) in 2003; these legislative acts require clinical studies to assess the safety and efficacy of new drugs in children.1 While studies conducted under these acts have provided important information for the clinical care of children, only one-third of mandatory pediatric postmarketing studies of the 114 new drugs and new indications subject to PREA requirements between 2007 and 2014 had been completed within seven years.3
Despite the challenges in conducting studies of drugs in children, robust pediatric data must be generated in children, especially in those with medical complexity or with chronic medical diseases and who have significant risk of experiencing adverse drug events. Data in adults cannot simply be extrapolated to children. In addition, studies from healthy children may not apply to hospitalized pediatric patients because of significant physiologic changes that occur in children who are ill enough to be hospitalized. Opportunistic sampling can provide robust drug disposition data and overcome some of the challenges encountered by traditional drug studies. In this Methodologic Progress Note, we describe the utility of opportunistic sampling as a research tool for hospitalists, in partnership with clinical pharmacologists, to study drug pharmacokinetics (PK) in hospitalized children.
OPPORTUNISTIC SAMPLING DEFINED
Opportunistic sampling relies on the use of blood samples that are ordered for clinical purposes, and its use is endorsed by the Pediatric Trials Network.2,5 Opportunistic sampling approaches have two types: sparse sampling and scavenged or remnant sampling. In sparse opportunistic sampling, additional blood is obtained at the same time clinical samples are ordered, avoiding the need for additional punctures.5 This approach requires bedside personnel to obtain additional blood that is sent to the research team for further processing. Scavenged sampling relies on leftover residual blood from clinical samples.2,5 After the clinical laboratory performs the laboratory test ordered by the clinical team, the research team can scavenge residual blood for measurement of drug concentrations. When drug concentrations are measured from multiple patients, clinical pharmacologists can perform population PK modeling to characterize the pharmacokinetics of the drug and its variability within the population level.
The Figure shows how scavenged samples from hypothetical patients could be used to generate a PK curve. In this example, three patients are admitted for osteomyelitis and treated with the same antibiotic administered every eight hours, as shown by the theoretical concentration versus time profiles in the top panel. To determine the effectiveness of treatment and timing of transition to enteral antibiotics, the clinical team orders C-reactive protein (CRP) approximately every 48 hours for each patient. Each patient has his/her first dose of antibiotic at a different time of day depending on the time of admission or surgical drainage. Therefore, the timing of the blood draw with respect to the most recent antibiotic dose varies between patients even if blood draws are ordered at the same time for all patients (ie, 4
Opportunistic sampling has advantages over traditional intensive PK studies that often require multiple blood draws (typically >8-10) within one dosing interval to adequately describe the phases of absorption, distribution, metabolism, and elimination. The number of vascular punctures can be painful if blood cannot be drawn from existing vascular access, and the large amount of blood (sometimes >1 mL/sample) required for these studies can be impractical, burdensome, and even dangerous in young children and neonates. Scavenged sampling reduces the risk of anemia because no additional blood is drawn beyond what is obtained for clinical purposes, and it does not disrupt nursing workflow or add to nursing workload. Approval to use scavenged blood requires approval from the institutional review board. At some institutions, the consent to treat form on admission may address the use of scavenged samples and therefore allow for waiver of consent. In addition, the consent process may occur retroactively after samples are collected. These methods lead to increased enrollment.
Limitations in this approach are that drugs may degrade over time in whole blood or processed samples. Therefore, the process by which the clinical laboratory stores the residual blood after clinical tests must be understood, and the stability of the drug or metabolite of interest in blood or plasma over time must be ensured. In addition, residual blood may not be present after a clinical test, and recording times of the drug administration and lab draws may be inaccurate.2,5
APPLICATIONS OF OPPORTUNISTIC SAMPLING IN CLINICAL PHARMACOLOGY RESEARCH
/section>Opportunistic sampling has been successfully used to study a variety of drugs in different pediatric populations but has been primarily used in neonates. The multicenter Pharmacokinetics of Understudied Drugs Administered to Children per Standard of Care trial has utilized this approach to evaluate the PK of over 30 drugs.5 Several antimicrobials have been studied through opportunistic sampling, including those frequently used in pediatric hospital medicine, such as ampicillin6 and clindamycin.7
This sampling approach may be most beneficial in studying select patients. Obese patients, who are often excluded in pediatric drug trials, have been previously included in opportunistic drug studies.8 The utility of opportunistic sampling to study antimicrobials, morphine and cardiac drugs has been demonstrated in neonates, both preterm and term, in whom additional blood draws can be challenging because of low total blood volume and limited vascular access.6,7,9-12
Although the frequency of blood draws from patients admitted to pediatric hospital medicine services is generally lower than that for patients on other subspecialty services, such as critical care, we can capitalize on the high volume of patients with common diagnoses (eg, pneumonia, skin, and soft tissue infections) who are admitted to hospital medicine. Using opportunistic sampling, we can study the PK of drugs frequently used in hospital medicine, such as antibiotics, antiepileptic drugs, steroids, and pain medications. In addition, we can measure drug concentrations to study the effects of route administration, oral versus enteric tube versus intravenous, to guide not only the dosing but also the timing of transition to enteral medications. Finally, we can study drugs that are commonly used in adult and pediatric patient populations cared for by hospitalists but who are often excluded from clinical drug trials, such as patients with medical complexity, patients with medical devices (eg, nervous system shunts and tracheostomies), patients taking concomitant medications, or patients on extracorporeal devices such as dialysis, to validate drug regimens.
CONCLUSION
Generating robust pediatric clinical pharmacology data has many inherent challenges because of the vulnerability of children. However, their vulnerability requires that medications be studied thoroughly in children to ensure their safety and effectiveness. Opportunistic sampling allows for rigorous studies to be conducted with adequate sample sizes while minimizing the risk of pain, anemia, and other adverse events related to clinical drug trials. Pediatric hospitalists should consider this approach to advance their knowledge of commonly used drugs that have not been adequately studied in hospitalized children and can expand the use of opportunistic sampling to study other aspects of disease, such as diagnostic or prognostic biomarkers.
Challenges in conducting and completing studies of drugs in vulnerable populations, such as hospitalized children, include weak study designs and lack of sufficient sample sizes to achieve adequate power.1 Limitations in the amount of blood that can be safely drawn in children and low parental consent rates due to concerns for anemia or pain, if venipuncture is required, lead to an insufficient number of patients enrolled in traditional clinical studies.2 Thus, sample size targets are often not met. Recognizing the limited pediatric data for many drugs routinely prescribed off-label in children, the Food and Drug Administration implemented the Best Pharmaceuticals Children Act and the Pediatric Research Equity Act (PREA) in 2003; these legislative acts require clinical studies to assess the safety and efficacy of new drugs in children.1 While studies conducted under these acts have provided important information for the clinical care of children, only one-third of mandatory pediatric postmarketing studies of the 114 new drugs and new indications subject to PREA requirements between 2007 and 2014 had been completed within seven years.3
Despite the challenges in conducting studies of drugs in children, robust pediatric data must be generated in children, especially in those with medical complexity or with chronic medical diseases and who have significant risk of experiencing adverse drug events. Data in adults cannot simply be extrapolated to children. In addition, studies from healthy children may not apply to hospitalized pediatric patients because of significant physiologic changes that occur in children who are ill enough to be hospitalized. Opportunistic sampling can provide robust drug disposition data and overcome some of the challenges encountered by traditional drug studies. In this Methodologic Progress Note, we describe the utility of opportunistic sampling as a research tool for hospitalists, in partnership with clinical pharmacologists, to study drug pharmacokinetics (PK) in hospitalized children.
OPPORTUNISTIC SAMPLING DEFINED
Opportunistic sampling relies on the use of blood samples that are ordered for clinical purposes, and its use is endorsed by the Pediatric Trials Network.2,5 Opportunistic sampling approaches have two types: sparse sampling and scavenged or remnant sampling. In sparse opportunistic sampling, additional blood is obtained at the same time clinical samples are ordered, avoiding the need for additional punctures.5 This approach requires bedside personnel to obtain additional blood that is sent to the research team for further processing. Scavenged sampling relies on leftover residual blood from clinical samples.2,5 After the clinical laboratory performs the laboratory test ordered by the clinical team, the research team can scavenge residual blood for measurement of drug concentrations. When drug concentrations are measured from multiple patients, clinical pharmacologists can perform population PK modeling to characterize the pharmacokinetics of the drug and its variability within the population level.
The Figure shows how scavenged samples from hypothetical patients could be used to generate a PK curve. In this example, three patients are admitted for osteomyelitis and treated with the same antibiotic administered every eight hours, as shown by the theoretical concentration versus time profiles in the top panel. To determine the effectiveness of treatment and timing of transition to enteral antibiotics, the clinical team orders C-reactive protein (CRP) approximately every 48 hours for each patient. Each patient has his/her first dose of antibiotic at a different time of day depending on the time of admission or surgical drainage. Therefore, the timing of the blood draw with respect to the most recent antibiotic dose varies between patients even if blood draws are ordered at the same time for all patients (ie, 4
Opportunistic sampling has advantages over traditional intensive PK studies that often require multiple blood draws (typically >8-10) within one dosing interval to adequately describe the phases of absorption, distribution, metabolism, and elimination. The number of vascular punctures can be painful if blood cannot be drawn from existing vascular access, and the large amount of blood (sometimes >1 mL/sample) required for these studies can be impractical, burdensome, and even dangerous in young children and neonates. Scavenged sampling reduces the risk of anemia because no additional blood is drawn beyond what is obtained for clinical purposes, and it does not disrupt nursing workflow or add to nursing workload. Approval to use scavenged blood requires approval from the institutional review board. At some institutions, the consent to treat form on admission may address the use of scavenged samples and therefore allow for waiver of consent. In addition, the consent process may occur retroactively after samples are collected. These methods lead to increased enrollment.
Limitations in this approach are that drugs may degrade over time in whole blood or processed samples. Therefore, the process by which the clinical laboratory stores the residual blood after clinical tests must be understood, and the stability of the drug or metabolite of interest in blood or plasma over time must be ensured. In addition, residual blood may not be present after a clinical test, and recording times of the drug administration and lab draws may be inaccurate.2,5
APPLICATIONS OF OPPORTUNISTIC SAMPLING IN CLINICAL PHARMACOLOGY RESEARCH
/section>Opportunistic sampling has been successfully used to study a variety of drugs in different pediatric populations but has been primarily used in neonates. The multicenter Pharmacokinetics of Understudied Drugs Administered to Children per Standard of Care trial has utilized this approach to evaluate the PK of over 30 drugs.5 Several antimicrobials have been studied through opportunistic sampling, including those frequently used in pediatric hospital medicine, such as ampicillin6 and clindamycin.7
This sampling approach may be most beneficial in studying select patients. Obese patients, who are often excluded in pediatric drug trials, have been previously included in opportunistic drug studies.8 The utility of opportunistic sampling to study antimicrobials, morphine and cardiac drugs has been demonstrated in neonates, both preterm and term, in whom additional blood draws can be challenging because of low total blood volume and limited vascular access.6,7,9-12
Although the frequency of blood draws from patients admitted to pediatric hospital medicine services is generally lower than that for patients on other subspecialty services, such as critical care, we can capitalize on the high volume of patients with common diagnoses (eg, pneumonia, skin, and soft tissue infections) who are admitted to hospital medicine. Using opportunistic sampling, we can study the PK of drugs frequently used in hospital medicine, such as antibiotics, antiepileptic drugs, steroids, and pain medications. In addition, we can measure drug concentrations to study the effects of route administration, oral versus enteric tube versus intravenous, to guide not only the dosing but also the timing of transition to enteral medications. Finally, we can study drugs that are commonly used in adult and pediatric patient populations cared for by hospitalists but who are often excluded from clinical drug trials, such as patients with medical complexity, patients with medical devices (eg, nervous system shunts and tracheostomies), patients taking concomitant medications, or patients on extracorporeal devices such as dialysis, to validate drug regimens.
CONCLUSION
Generating robust pediatric clinical pharmacology data has many inherent challenges because of the vulnerability of children. However, their vulnerability requires that medications be studied thoroughly in children to ensure their safety and effectiveness. Opportunistic sampling allows for rigorous studies to be conducted with adequate sample sizes while minimizing the risk of pain, anemia, and other adverse events related to clinical drug trials. Pediatric hospitalists should consider this approach to advance their knowledge of commonly used drugs that have not been adequately studied in hospitalized children and can expand the use of opportunistic sampling to study other aspects of disease, such as diagnostic or prognostic biomarkers.
1. Field MJ, Boat TF, eds. Safe and Effective Medicines for Children: Pediatric Studies Conducted Under the Best Pharmaceuticals for Children Act and the Pediatric Research Equity Act. Washington, DC, USA: National Academies Press; 2012.
2. Laughon MM, Benjamin DK, Jr., Capparelli EV, et al. Innovative clinical trial design for pediatric therapeutics. Expert Rev Clin Pharmacol. 2011;4(5):643-652. https://doi.org/10.1586/ecp.11.43.
3. Hwang TJ, Orenstein L, Kesselheim AS, Bourgeois FT. Completion rate and reporting of mandatory pediatric postmarketing studies under the US Pediatric Research Equity Act. JAMA Pediatr. 2018;173(1):68-74. https://doi.org/10.1001/jamapediatrics.2018.3416.
4. Rieder M. Adverse drug reactions in children: pediatric pharmacy and drug safety. J Pediatr Pharmacol Ther. 2019;24(1):4-9. https://doi.org/10.5863/1551-6776-24.1.4.
5. Balevic SJ, Cohen-Wolkowiez M. Innovative study designs optimizing clinical pharmacology research in infants and children. J Clin Pharmacol. 2018;58(10):S58-S72. https://doi.org/10.1002/jcph.1053.
6. Tremoulet A, Le J, Poindexter B, et al. Characterization of the population pharmacokinetics of ampicillin in neonates using an opportunistic study design. Antimicrob Agents Chemother. 2014;58(6):3013-3020. https://doi.org/10.1128/AAC.02374-13.
7. Gonzalez D, Melloni C, Yogev R, et al. Use of opportunistic clinical data and a population pharmacokinetic model to support dosing of clindamycin for premature infants to adolescents. Clin Pharmacol Ther. 2014;96(4):429-437. https://doi.org/10.1038/clpt.2014.134.
8. Smith MJ, Gonzalez D, Goldman JL, et al. Pharmacokinetics of clindamycin in obese and nonobese children. Antimicrob Agents Chemother. 2017;61(4). https://doi.org/10.1128/AAC.02014-16.
9. Leroux S, Turner MA, Guellec CB, et al. Pharmacokinetic studies in neonates: The utility of an opportunistic sampling design. Clin Pharmacokinet. 2015;54(12):1273-1285. https://doi.org/10.1007/s40262-015-0291-1.
10. Dallefeld SH, Atz AM, Yogev R, et al. A pharmacokinetic model for amiodarone in infants developed from an opportunistic sampling trial and published literature data. J Pharmacokinet Pharmacodyn. 2018;45(3):419-430. https://doi.org/10.1007/s10928-018-9576-y.
11. Thakkar N, Gonzalez D, Cohen-Wolkowiez M, et al. An opportunistic study evaluating pharmacokinetics of sildenafil for the treatment of pulmonary hypertension in infants. J Perinatol. 2016;36(9):744-747. https://doi.org/10.1038/jp.2016.79.
12. Euteneuer JC, Mizuno T, Fukuda T, Zhao J, Setchell KD, Vinks AA. Large variability in morphine concentrations in critically ill neonates receiving standard of care postoperative pain-management. Clin Pharmacol Ther. 2018;103:S45-S45.
1. Field MJ, Boat TF, eds. Safe and Effective Medicines for Children: Pediatric Studies Conducted Under the Best Pharmaceuticals for Children Act and the Pediatric Research Equity Act. Washington, DC, USA: National Academies Press; 2012.
2. Laughon MM, Benjamin DK, Jr., Capparelli EV, et al. Innovative clinical trial design for pediatric therapeutics. Expert Rev Clin Pharmacol. 2011;4(5):643-652. https://doi.org/10.1586/ecp.11.43.
3. Hwang TJ, Orenstein L, Kesselheim AS, Bourgeois FT. Completion rate and reporting of mandatory pediatric postmarketing studies under the US Pediatric Research Equity Act. JAMA Pediatr. 2018;173(1):68-74. https://doi.org/10.1001/jamapediatrics.2018.3416.
4. Rieder M. Adverse drug reactions in children: pediatric pharmacy and drug safety. J Pediatr Pharmacol Ther. 2019;24(1):4-9. https://doi.org/10.5863/1551-6776-24.1.4.
5. Balevic SJ, Cohen-Wolkowiez M. Innovative study designs optimizing clinical pharmacology research in infants and children. J Clin Pharmacol. 2018;58(10):S58-S72. https://doi.org/10.1002/jcph.1053.
6. Tremoulet A, Le J, Poindexter B, et al. Characterization of the population pharmacokinetics of ampicillin in neonates using an opportunistic study design. Antimicrob Agents Chemother. 2014;58(6):3013-3020. https://doi.org/10.1128/AAC.02374-13.
7. Gonzalez D, Melloni C, Yogev R, et al. Use of opportunistic clinical data and a population pharmacokinetic model to support dosing of clindamycin for premature infants to adolescents. Clin Pharmacol Ther. 2014;96(4):429-437. https://doi.org/10.1038/clpt.2014.134.
8. Smith MJ, Gonzalez D, Goldman JL, et al. Pharmacokinetics of clindamycin in obese and nonobese children. Antimicrob Agents Chemother. 2017;61(4). https://doi.org/10.1128/AAC.02014-16.
9. Leroux S, Turner MA, Guellec CB, et al. Pharmacokinetic studies in neonates: The utility of an opportunistic sampling design. Clin Pharmacokinet. 2015;54(12):1273-1285. https://doi.org/10.1007/s40262-015-0291-1.
10. Dallefeld SH, Atz AM, Yogev R, et al. A pharmacokinetic model for amiodarone in infants developed from an opportunistic sampling trial and published literature data. J Pharmacokinet Pharmacodyn. 2018;45(3):419-430. https://doi.org/10.1007/s10928-018-9576-y.
11. Thakkar N, Gonzalez D, Cohen-Wolkowiez M, et al. An opportunistic study evaluating pharmacokinetics of sildenafil for the treatment of pulmonary hypertension in infants. J Perinatol. 2016;36(9):744-747. https://doi.org/10.1038/jp.2016.79.
12. Euteneuer JC, Mizuno T, Fukuda T, Zhao J, Setchell KD, Vinks AA. Large variability in morphine concentrations in critically ill neonates receiving standard of care postoperative pain-management. Clin Pharmacol Ther. 2018;103:S45-S45.
© 2021 Society of Hospital Medicine
The Future of Pediatric Hospital Medicine: Challenges and Opportunities
Pediatric hospital medicine (PHM) is in the midst of an exciting period of growth. In 2016, the American Board of Medical Specialties approved the petition for PHM to become the newest pediatric subspecialty, taking PHM on a divergent path from the Focused Practice in Hospital Medicine designation established for adult hospitalists. Establishment as a subspecialty has allowed PHM to define the unique skills and qualifications that hospitalists bring to patients and the healthcare system. These skills and qualifications are delineated in the PHM core competencies and national fellowship curriculum.1,2 In order to realize the vision of PHM to improve care for hospitalized children described by Roberts et al.,3 concerted efforts are needed to train and retain a workforce that is equipped with the skills to catalyze improvements in inpatient pediatric care. We discuss challenges and opportunities facing PHM in workforce development, sustainability of clinical work models, and interhospital collaboration.
FELLOWSHIP TRAINING AND THE PHM PIPELINE
The development of PHM as a subspecialty was driven by a number of factors.4 The acuity of hospitalized children has increased significantly, with a population comprised of more children with complex chronic conditions and/or technology dependence, serious complications of acute conditions, and acute mental health problems. At the same time, the medical and behavioral conditions seen by outpatient general pediatricians have become more complex and time intensive, with these practitioners less likely to work in inpatient settings. Hospitalist care has positive impacts on healthcare efficiency and value, and both parents and primary care pediatricians report high levels of satisfaction with the healthcare delivered by PHM services.4
A national count of the number of pediatric hospitalists is currently lacking. Conservative estimates suggest that at least 3,000 pediatric hospitalists currently practice in the United States.5 These hospitalists have highly varied scopes of practice and work across diverse settings—more diverse, perhaps, than any other pediatric subspecialty. Although difficult to quantify, we estimate that approximately one-third of pediatric hospitalists in the US work in community hospitals and the remainder practice at children’s hospitals.6 Many of the needs of hospitalized children differ across these settings, and the roles and challenges faced by hospitalists in these settings correspondingly differ. Community hospitalists frequently take active roles in newborn care and emergency department consultation, often without the support of other pediatric subspecialties.7 In contrast, hospitalists working at children’s hospitals more frequently care for highly complex patients, often collaborate across multiple specialties and assume nonclinical roles in quality improvement (QI), research, and medical education.
Residents graduating in July 2019 were the last cohort of residents eligible to pursue PHM subspecialty certification via the practice pathway. Accordingly, future residency graduates interested in PHM subspecialty certification will need to complete a PHM fellowship at an accredited program in the US or Canada. Since 2008, PHM fellowship directors have met yearly to collaborate and share best practices,8 developing the two-year fellowship curriculum that forms the basis for the American Board of Pediatrics training pathway.2 The curriculum allows significant flexibility to meet diverse needs, including tailored content for fellows planning to practice in community settings, fellows planning research careers, medicine-pediatrics hospitalist careers, and those desiring increased training in QI, medical education, or leadership/administration.2 In the spring of 2019, Pediatric Research in Inpatient Settings (PRIS) leadership, directors of existing PHM fellowship programs, and national academic society representatives met to develop a fellows’ research curriculum, training resources, and guidelines around scholarship expectations.9 This collaboration aims to accelerate the growth of high-quality clinical training and scholarship to benefit hospitalized children across many different settings.
Such collaboration is essential to address an emerging workforce challenge in PHM. Although the number of PHM fellowship positions is expected to grow in the coming years, there is currently a shortage relative to the anticipated demand. With approximately 2,800 US pediatric residents graduating annually and data indicating that 7% of graduating residents enter and remain in PHM for at least five years,10,11 almost 200 fellowship spots may be needed each year. As of November 2019, 77 fellowship positions were available for residents graduating in 2020,12 which is less than half of the potential demand. To address this mismatch, the PHM Fellowship Directors’ Council has led an annual training for new and potential fellowship directors, and 18 new programs are under development.13 However, this growth may be inadequate to meet the needs of the field. The extent to which limited PHM fellowship positions will adversely affect the pipeline of pediatricians pursuing PHM is unknown.
Efforts to support institutions in creating and expanding fellowship programs will be needed to address the potential shortage of fellowship positions. Continued guidance from the PHM Fellowship Directors’ Council in the many aspects of fellowship program development (eg, curriculum design, assessment) will be crucial in this endeavor. Furthermore, given that fellowships must support fellows to conduct scholarly work and demonstrate evidence of robust faculty scholarly activities to attain accreditation, an essential area of focus is faculty development. Considering barriers such as lack of time, mentorship, and resources, some divisions interested in starting a fellowship may find it challenging to achieve these standards.14 However, hospitalists are often engaged in areas such as QI and medical education, and there is potential to turn ongoing work into meaningful scholarship with appropriate guidance. Many of our supporting organizations (eg, Academic Pediatric Association, American Academy of Pediatrics, and Society of Hospital Medicine) provide training programs for faculty in areas such as educational scholarship, research, and QI; however, more may be needed. Leaders of PHM programs will need to be mindful and creative in accessing local, regional, and national resources to invest in faculty development.
CLINICAL WORK MODELS AND SUSTAINABILITY
As a group, pediatric hospitalists report high levels of satisfaction with their jobs.11 Despite this finding, there are a number of threats to the sustainability of current work models, some of which are unique to pediatrics given the overall lower patient volumes and greater seasonal variation compared with adult hospital medicine. Both university and community-based hospitalist programs report high weekend, overnight, and in-house clinical effort.7,15 Recent studies reported that a significant proportion of PHM program leaders (50% of division directors at university-affiliated programs and 37% of community program leaders) perceive their program to be unsustainable.7,15 Among university-affiliated programs, a higher burden of weekend work as well as university employment were associated with perceived unsustainability, while no specific program or employer characteristic was associated with this perception in community programs.
These findings indicate that efforts are needed to address PHM program sustainability and that different work models and interventions may be needed for university-based and community PHM programs. Wide variability exists in the ways that programs address overall clinical burden, with strategies including census caps, seasonal expansion of coverage, and formal back-up systems.7,15 Additional potential solutions may include differential weighting or financial incentives for nights and weekends, support for nonclinical work, loan repayment programs, and competitive salaries.11 In addition, structuring clinical and nonclinical roles to facilitate career development and advancement may enhance career longevity.15 Lessons learned from pediatric emergency medicine (PEM), which developed as a field a few decades ahead of PHM, may predict future challenges. A 2015 survey of PEM faculty found that despite a 15% decrease in weekly work hours over a 15-year period, a substantial number of PEM faculty report concerns about burnout, with 40% reporting a plan to decrease their clinical workload and 13% planning to leave the field within five years.16 Like PEM, the field of PHM may benefit from the development of best practice guidelines to improve well-being and career longevity.17
INTERHOSPITAL COLLABORATION
The culture of collaboration within PHM places the field in a solid position to address both workforce challenges and barriers to high-quality care for hospitalized children. There are several hospital-based learning networks actively working to strengthen our knowledge base and improve healthcare quality. The PRIS network (www.prisnetwork.org) aims to improve healthcare for children through multihospital studies, boasting 114 sites in the US and Canada. Numerous collaborative projects have linked hospitalists across programs to tackle problems ranging from handoff communication18 to eliminating monitor overuse.19 The Value in Inpatient Pediatrics network has similarly leveraged collaborations across multiple children’s and community hospitals to improve transitions of care20 and care for common conditions such as bronchiolitis, febrile infants, and asthma.21 These networks serve as models of effective collaboration between children’s hospitals and community hospitals, more of which is needed to increase research and QI initiatives in community hospitals, where the majority of US children receive their hospital-based care.6,22
With the rapid growth of scholarly networks in research, QI, and education, PHM has a solid infrastructure on which to base continued development as a subspeciality. Building on this infrastructure will be essential in order to address current challenges in workforce development, fellowship training, and program sustainability. Ultimately, achieving a strong, stable, and skilled workforce will enable PHM to fulfill its promise of improving the care of children across the diversity of settings where they receive their hospital-based care.
Disclosures
Dr. Leyenaar provides consultative services to the American Board of Pediatrics Foundation, which is not associated with this manuscript. Drs. Wang and Shaughnessy have no disclosures
1. Stucky ER, Maniscalco J, Ottolini MC, et al. The Pediatric Hospital Medicine Core Competencies Supplement: a framework for curriculum development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(S2):1-114. https://doi.org/10.1002/jhm.776.
2. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1). https://doi.org/10.1542/peds.2017-0698.
3. Roberts KB, Fisher ER, Rauch DA. A history of pediatric hospital medicine in the United States, 1996-2019. J Hosp Med. 2019.
4. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-1823.
5. American Board of Medical Specialities. American Board of Medical Specialities application for a new subspecialty certificate: Pediatric hospital medicine. http://www.abms.org/media/114649/abpeds-application-for-pediatric-hospital-medicine.pdf. Accessed November 6, 2019.
6. Leyenaar JK, Ralston SL, Shieh MS, et al. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624.
7. Alvarez F, McDaniel CE, Birnie K, et al. Community pediatric hospitalist workload: results from a national survey. J Hosp Med. 2019;14(10):682-685. https://doi.org/10.12788/jhm.3263.
8. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: A survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571.
9. Pediatric Hospital Medicine Fellowship Research Training Development. https://projectreporter.nih.gov/project_info_description.cfm?aid=9593276&icde=47889643. Accessed December 10, 2019.
10. Leyenaar JK, Frintner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018;18(2):200-207. https://doi.org/10.1016/j.acap.2017.05.001.
11. House S, Frintner MP, Leyenaar JK. Factors influencing career longevity in pediatric hospital medicine. Hosp Pediatr. 2019;9(12):983-988. https://doi.org/10.1542/hpeds.2019-0151.
12. PHM Fellowship Programs. http://phmfellows.org/phm-programs/. Accessed November 6, 2019.
13. Rassbach C [Personal communication]; 2019.
14. Bekmezian A, Teufel RJ, 2nd, Wilson KM. Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38-44. https://doi.org/10.1542/hpeds.2011-0006.
15. Fromme HB, Chen CO, Fine BR, Gosdin C, Shaughnessy EE. Pediatric hospitalist workload and sustainability in university-based programs: Results from a national interview-based survey. J Hosp Med. 2018;13(10):702-705. https://doi.org/10.12788/jhm.2977.
16. Gorelick MH, Schremmer R, Ruch-Ross H, Radabaugh C, Selbst S. Current workforce characteristics and burnout in pediatric emergency medicine. Acad Emerg Med. 2016;23(1):48-54. https://doi.org/10.1111/acem.12845.
17. American College of Emergency Physicians. Policy Statement: Emergency Physician Shift Work; June 2017.
18. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812. https://doi.org/10.1056/NEJMsa1405556.
19. Rasooly IR, Beidas RS, Wolk CB, et al. Measuring overuse of continuous pulse oximetry in bronchiolitis and developing strategies for large-scale deimplementation: Study protocol for a feasibility trial. Pilot Feasibility Stud. 2019;5:68. https://doi.org/10.1186/s40814-019-0453-2.
20. Coghlin DT, Leyenaar JK, Shen M, et al. Pediatric discharge content: a multisite assessment of physician preferences and experiences. Hosp Pediatr. 2014;4(1):9-15. https://doi.org/10.1542/hpeds.2013-0022.
21. Value in inpatient pediatrics (VIP) Network. 2019. https://www.aap.org/en-us/professional-resources/quality-improvement/Pages/Value-in-Inpatient-Pediatrics.aspx. Accessed October 13, 2019.
22. McDaniel CE, Jennings R, Schroeder AR, et al. Aligning inpatient pediatric research with settings of care: A call to action. Pediatrics. 2019;143(5). https://doi.org/10.1542/peds.2018-2648.
Pediatric hospital medicine (PHM) is in the midst of an exciting period of growth. In 2016, the American Board of Medical Specialties approved the petition for PHM to become the newest pediatric subspecialty, taking PHM on a divergent path from the Focused Practice in Hospital Medicine designation established for adult hospitalists. Establishment as a subspecialty has allowed PHM to define the unique skills and qualifications that hospitalists bring to patients and the healthcare system. These skills and qualifications are delineated in the PHM core competencies and national fellowship curriculum.1,2 In order to realize the vision of PHM to improve care for hospitalized children described by Roberts et al.,3 concerted efforts are needed to train and retain a workforce that is equipped with the skills to catalyze improvements in inpatient pediatric care. We discuss challenges and opportunities facing PHM in workforce development, sustainability of clinical work models, and interhospital collaboration.
FELLOWSHIP TRAINING AND THE PHM PIPELINE
The development of PHM as a subspecialty was driven by a number of factors.4 The acuity of hospitalized children has increased significantly, with a population comprised of more children with complex chronic conditions and/or technology dependence, serious complications of acute conditions, and acute mental health problems. At the same time, the medical and behavioral conditions seen by outpatient general pediatricians have become more complex and time intensive, with these practitioners less likely to work in inpatient settings. Hospitalist care has positive impacts on healthcare efficiency and value, and both parents and primary care pediatricians report high levels of satisfaction with the healthcare delivered by PHM services.4
A national count of the number of pediatric hospitalists is currently lacking. Conservative estimates suggest that at least 3,000 pediatric hospitalists currently practice in the United States.5 These hospitalists have highly varied scopes of practice and work across diverse settings—more diverse, perhaps, than any other pediatric subspecialty. Although difficult to quantify, we estimate that approximately one-third of pediatric hospitalists in the US work in community hospitals and the remainder practice at children’s hospitals.6 Many of the needs of hospitalized children differ across these settings, and the roles and challenges faced by hospitalists in these settings correspondingly differ. Community hospitalists frequently take active roles in newborn care and emergency department consultation, often without the support of other pediatric subspecialties.7 In contrast, hospitalists working at children’s hospitals more frequently care for highly complex patients, often collaborate across multiple specialties and assume nonclinical roles in quality improvement (QI), research, and medical education.
Residents graduating in July 2019 were the last cohort of residents eligible to pursue PHM subspecialty certification via the practice pathway. Accordingly, future residency graduates interested in PHM subspecialty certification will need to complete a PHM fellowship at an accredited program in the US or Canada. Since 2008, PHM fellowship directors have met yearly to collaborate and share best practices,8 developing the two-year fellowship curriculum that forms the basis for the American Board of Pediatrics training pathway.2 The curriculum allows significant flexibility to meet diverse needs, including tailored content for fellows planning to practice in community settings, fellows planning research careers, medicine-pediatrics hospitalist careers, and those desiring increased training in QI, medical education, or leadership/administration.2 In the spring of 2019, Pediatric Research in Inpatient Settings (PRIS) leadership, directors of existing PHM fellowship programs, and national academic society representatives met to develop a fellows’ research curriculum, training resources, and guidelines around scholarship expectations.9 This collaboration aims to accelerate the growth of high-quality clinical training and scholarship to benefit hospitalized children across many different settings.
Such collaboration is essential to address an emerging workforce challenge in PHM. Although the number of PHM fellowship positions is expected to grow in the coming years, there is currently a shortage relative to the anticipated demand. With approximately 2,800 US pediatric residents graduating annually and data indicating that 7% of graduating residents enter and remain in PHM for at least five years,10,11 almost 200 fellowship spots may be needed each year. As of November 2019, 77 fellowship positions were available for residents graduating in 2020,12 which is less than half of the potential demand. To address this mismatch, the PHM Fellowship Directors’ Council has led an annual training for new and potential fellowship directors, and 18 new programs are under development.13 However, this growth may be inadequate to meet the needs of the field. The extent to which limited PHM fellowship positions will adversely affect the pipeline of pediatricians pursuing PHM is unknown.
Efforts to support institutions in creating and expanding fellowship programs will be needed to address the potential shortage of fellowship positions. Continued guidance from the PHM Fellowship Directors’ Council in the many aspects of fellowship program development (eg, curriculum design, assessment) will be crucial in this endeavor. Furthermore, given that fellowships must support fellows to conduct scholarly work and demonstrate evidence of robust faculty scholarly activities to attain accreditation, an essential area of focus is faculty development. Considering barriers such as lack of time, mentorship, and resources, some divisions interested in starting a fellowship may find it challenging to achieve these standards.14 However, hospitalists are often engaged in areas such as QI and medical education, and there is potential to turn ongoing work into meaningful scholarship with appropriate guidance. Many of our supporting organizations (eg, Academic Pediatric Association, American Academy of Pediatrics, and Society of Hospital Medicine) provide training programs for faculty in areas such as educational scholarship, research, and QI; however, more may be needed. Leaders of PHM programs will need to be mindful and creative in accessing local, regional, and national resources to invest in faculty development.
CLINICAL WORK MODELS AND SUSTAINABILITY
As a group, pediatric hospitalists report high levels of satisfaction with their jobs.11 Despite this finding, there are a number of threats to the sustainability of current work models, some of which are unique to pediatrics given the overall lower patient volumes and greater seasonal variation compared with adult hospital medicine. Both university and community-based hospitalist programs report high weekend, overnight, and in-house clinical effort.7,15 Recent studies reported that a significant proportion of PHM program leaders (50% of division directors at university-affiliated programs and 37% of community program leaders) perceive their program to be unsustainable.7,15 Among university-affiliated programs, a higher burden of weekend work as well as university employment were associated with perceived unsustainability, while no specific program or employer characteristic was associated with this perception in community programs.
These findings indicate that efforts are needed to address PHM program sustainability and that different work models and interventions may be needed for university-based and community PHM programs. Wide variability exists in the ways that programs address overall clinical burden, with strategies including census caps, seasonal expansion of coverage, and formal back-up systems.7,15 Additional potential solutions may include differential weighting or financial incentives for nights and weekends, support for nonclinical work, loan repayment programs, and competitive salaries.11 In addition, structuring clinical and nonclinical roles to facilitate career development and advancement may enhance career longevity.15 Lessons learned from pediatric emergency medicine (PEM), which developed as a field a few decades ahead of PHM, may predict future challenges. A 2015 survey of PEM faculty found that despite a 15% decrease in weekly work hours over a 15-year period, a substantial number of PEM faculty report concerns about burnout, with 40% reporting a plan to decrease their clinical workload and 13% planning to leave the field within five years.16 Like PEM, the field of PHM may benefit from the development of best practice guidelines to improve well-being and career longevity.17
INTERHOSPITAL COLLABORATION
The culture of collaboration within PHM places the field in a solid position to address both workforce challenges and barriers to high-quality care for hospitalized children. There are several hospital-based learning networks actively working to strengthen our knowledge base and improve healthcare quality. The PRIS network (www.prisnetwork.org) aims to improve healthcare for children through multihospital studies, boasting 114 sites in the US and Canada. Numerous collaborative projects have linked hospitalists across programs to tackle problems ranging from handoff communication18 to eliminating monitor overuse.19 The Value in Inpatient Pediatrics network has similarly leveraged collaborations across multiple children’s and community hospitals to improve transitions of care20 and care for common conditions such as bronchiolitis, febrile infants, and asthma.21 These networks serve as models of effective collaboration between children’s hospitals and community hospitals, more of which is needed to increase research and QI initiatives in community hospitals, where the majority of US children receive their hospital-based care.6,22
With the rapid growth of scholarly networks in research, QI, and education, PHM has a solid infrastructure on which to base continued development as a subspeciality. Building on this infrastructure will be essential in order to address current challenges in workforce development, fellowship training, and program sustainability. Ultimately, achieving a strong, stable, and skilled workforce will enable PHM to fulfill its promise of improving the care of children across the diversity of settings where they receive their hospital-based care.
Disclosures
Dr. Leyenaar provides consultative services to the American Board of Pediatrics Foundation, which is not associated with this manuscript. Drs. Wang and Shaughnessy have no disclosures
Pediatric hospital medicine (PHM) is in the midst of an exciting period of growth. In 2016, the American Board of Medical Specialties approved the petition for PHM to become the newest pediatric subspecialty, taking PHM on a divergent path from the Focused Practice in Hospital Medicine designation established for adult hospitalists. Establishment as a subspecialty has allowed PHM to define the unique skills and qualifications that hospitalists bring to patients and the healthcare system. These skills and qualifications are delineated in the PHM core competencies and national fellowship curriculum.1,2 In order to realize the vision of PHM to improve care for hospitalized children described by Roberts et al.,3 concerted efforts are needed to train and retain a workforce that is equipped with the skills to catalyze improvements in inpatient pediatric care. We discuss challenges and opportunities facing PHM in workforce development, sustainability of clinical work models, and interhospital collaboration.
FELLOWSHIP TRAINING AND THE PHM PIPELINE
The development of PHM as a subspecialty was driven by a number of factors.4 The acuity of hospitalized children has increased significantly, with a population comprised of more children with complex chronic conditions and/or technology dependence, serious complications of acute conditions, and acute mental health problems. At the same time, the medical and behavioral conditions seen by outpatient general pediatricians have become more complex and time intensive, with these practitioners less likely to work in inpatient settings. Hospitalist care has positive impacts on healthcare efficiency and value, and both parents and primary care pediatricians report high levels of satisfaction with the healthcare delivered by PHM services.4
A national count of the number of pediatric hospitalists is currently lacking. Conservative estimates suggest that at least 3,000 pediatric hospitalists currently practice in the United States.5 These hospitalists have highly varied scopes of practice and work across diverse settings—more diverse, perhaps, than any other pediatric subspecialty. Although difficult to quantify, we estimate that approximately one-third of pediatric hospitalists in the US work in community hospitals and the remainder practice at children’s hospitals.6 Many of the needs of hospitalized children differ across these settings, and the roles and challenges faced by hospitalists in these settings correspondingly differ. Community hospitalists frequently take active roles in newborn care and emergency department consultation, often without the support of other pediatric subspecialties.7 In contrast, hospitalists working at children’s hospitals more frequently care for highly complex patients, often collaborate across multiple specialties and assume nonclinical roles in quality improvement (QI), research, and medical education.
Residents graduating in July 2019 were the last cohort of residents eligible to pursue PHM subspecialty certification via the practice pathway. Accordingly, future residency graduates interested in PHM subspecialty certification will need to complete a PHM fellowship at an accredited program in the US or Canada. Since 2008, PHM fellowship directors have met yearly to collaborate and share best practices,8 developing the two-year fellowship curriculum that forms the basis for the American Board of Pediatrics training pathway.2 The curriculum allows significant flexibility to meet diverse needs, including tailored content for fellows planning to practice in community settings, fellows planning research careers, medicine-pediatrics hospitalist careers, and those desiring increased training in QI, medical education, or leadership/administration.2 In the spring of 2019, Pediatric Research in Inpatient Settings (PRIS) leadership, directors of existing PHM fellowship programs, and national academic society representatives met to develop a fellows’ research curriculum, training resources, and guidelines around scholarship expectations.9 This collaboration aims to accelerate the growth of high-quality clinical training and scholarship to benefit hospitalized children across many different settings.
Such collaboration is essential to address an emerging workforce challenge in PHM. Although the number of PHM fellowship positions is expected to grow in the coming years, there is currently a shortage relative to the anticipated demand. With approximately 2,800 US pediatric residents graduating annually and data indicating that 7% of graduating residents enter and remain in PHM for at least five years,10,11 almost 200 fellowship spots may be needed each year. As of November 2019, 77 fellowship positions were available for residents graduating in 2020,12 which is less than half of the potential demand. To address this mismatch, the PHM Fellowship Directors’ Council has led an annual training for new and potential fellowship directors, and 18 new programs are under development.13 However, this growth may be inadequate to meet the needs of the field. The extent to which limited PHM fellowship positions will adversely affect the pipeline of pediatricians pursuing PHM is unknown.
Efforts to support institutions in creating and expanding fellowship programs will be needed to address the potential shortage of fellowship positions. Continued guidance from the PHM Fellowship Directors’ Council in the many aspects of fellowship program development (eg, curriculum design, assessment) will be crucial in this endeavor. Furthermore, given that fellowships must support fellows to conduct scholarly work and demonstrate evidence of robust faculty scholarly activities to attain accreditation, an essential area of focus is faculty development. Considering barriers such as lack of time, mentorship, and resources, some divisions interested in starting a fellowship may find it challenging to achieve these standards.14 However, hospitalists are often engaged in areas such as QI and medical education, and there is potential to turn ongoing work into meaningful scholarship with appropriate guidance. Many of our supporting organizations (eg, Academic Pediatric Association, American Academy of Pediatrics, and Society of Hospital Medicine) provide training programs for faculty in areas such as educational scholarship, research, and QI; however, more may be needed. Leaders of PHM programs will need to be mindful and creative in accessing local, regional, and national resources to invest in faculty development.
CLINICAL WORK MODELS AND SUSTAINABILITY
As a group, pediatric hospitalists report high levels of satisfaction with their jobs.11 Despite this finding, there are a number of threats to the sustainability of current work models, some of which are unique to pediatrics given the overall lower patient volumes and greater seasonal variation compared with adult hospital medicine. Both university and community-based hospitalist programs report high weekend, overnight, and in-house clinical effort.7,15 Recent studies reported that a significant proportion of PHM program leaders (50% of division directors at university-affiliated programs and 37% of community program leaders) perceive their program to be unsustainable.7,15 Among university-affiliated programs, a higher burden of weekend work as well as university employment were associated with perceived unsustainability, while no specific program or employer characteristic was associated with this perception in community programs.
These findings indicate that efforts are needed to address PHM program sustainability and that different work models and interventions may be needed for university-based and community PHM programs. Wide variability exists in the ways that programs address overall clinical burden, with strategies including census caps, seasonal expansion of coverage, and formal back-up systems.7,15 Additional potential solutions may include differential weighting or financial incentives for nights and weekends, support for nonclinical work, loan repayment programs, and competitive salaries.11 In addition, structuring clinical and nonclinical roles to facilitate career development and advancement may enhance career longevity.15 Lessons learned from pediatric emergency medicine (PEM), which developed as a field a few decades ahead of PHM, may predict future challenges. A 2015 survey of PEM faculty found that despite a 15% decrease in weekly work hours over a 15-year period, a substantial number of PEM faculty report concerns about burnout, with 40% reporting a plan to decrease their clinical workload and 13% planning to leave the field within five years.16 Like PEM, the field of PHM may benefit from the development of best practice guidelines to improve well-being and career longevity.17
INTERHOSPITAL COLLABORATION
The culture of collaboration within PHM places the field in a solid position to address both workforce challenges and barriers to high-quality care for hospitalized children. There are several hospital-based learning networks actively working to strengthen our knowledge base and improve healthcare quality. The PRIS network (www.prisnetwork.org) aims to improve healthcare for children through multihospital studies, boasting 114 sites in the US and Canada. Numerous collaborative projects have linked hospitalists across programs to tackle problems ranging from handoff communication18 to eliminating monitor overuse.19 The Value in Inpatient Pediatrics network has similarly leveraged collaborations across multiple children’s and community hospitals to improve transitions of care20 and care for common conditions such as bronchiolitis, febrile infants, and asthma.21 These networks serve as models of effective collaboration between children’s hospitals and community hospitals, more of which is needed to increase research and QI initiatives in community hospitals, where the majority of US children receive their hospital-based care.6,22
With the rapid growth of scholarly networks in research, QI, and education, PHM has a solid infrastructure on which to base continued development as a subspeciality. Building on this infrastructure will be essential in order to address current challenges in workforce development, fellowship training, and program sustainability. Ultimately, achieving a strong, stable, and skilled workforce will enable PHM to fulfill its promise of improving the care of children across the diversity of settings where they receive their hospital-based care.
Disclosures
Dr. Leyenaar provides consultative services to the American Board of Pediatrics Foundation, which is not associated with this manuscript. Drs. Wang and Shaughnessy have no disclosures
1. Stucky ER, Maniscalco J, Ottolini MC, et al. The Pediatric Hospital Medicine Core Competencies Supplement: a framework for curriculum development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(S2):1-114. https://doi.org/10.1002/jhm.776.
2. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1). https://doi.org/10.1542/peds.2017-0698.
3. Roberts KB, Fisher ER, Rauch DA. A history of pediatric hospital medicine in the United States, 1996-2019. J Hosp Med. 2019.
4. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-1823.
5. American Board of Medical Specialities. American Board of Medical Specialities application for a new subspecialty certificate: Pediatric hospital medicine. http://www.abms.org/media/114649/abpeds-application-for-pediatric-hospital-medicine.pdf. Accessed November 6, 2019.
6. Leyenaar JK, Ralston SL, Shieh MS, et al. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624.
7. Alvarez F, McDaniel CE, Birnie K, et al. Community pediatric hospitalist workload: results from a national survey. J Hosp Med. 2019;14(10):682-685. https://doi.org/10.12788/jhm.3263.
8. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: A survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571.
9. Pediatric Hospital Medicine Fellowship Research Training Development. https://projectreporter.nih.gov/project_info_description.cfm?aid=9593276&icde=47889643. Accessed December 10, 2019.
10. Leyenaar JK, Frintner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018;18(2):200-207. https://doi.org/10.1016/j.acap.2017.05.001.
11. House S, Frintner MP, Leyenaar JK. Factors influencing career longevity in pediatric hospital medicine. Hosp Pediatr. 2019;9(12):983-988. https://doi.org/10.1542/hpeds.2019-0151.
12. PHM Fellowship Programs. http://phmfellows.org/phm-programs/. Accessed November 6, 2019.
13. Rassbach C [Personal communication]; 2019.
14. Bekmezian A, Teufel RJ, 2nd, Wilson KM. Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38-44. https://doi.org/10.1542/hpeds.2011-0006.
15. Fromme HB, Chen CO, Fine BR, Gosdin C, Shaughnessy EE. Pediatric hospitalist workload and sustainability in university-based programs: Results from a national interview-based survey. J Hosp Med. 2018;13(10):702-705. https://doi.org/10.12788/jhm.2977.
16. Gorelick MH, Schremmer R, Ruch-Ross H, Radabaugh C, Selbst S. Current workforce characteristics and burnout in pediatric emergency medicine. Acad Emerg Med. 2016;23(1):48-54. https://doi.org/10.1111/acem.12845.
17. American College of Emergency Physicians. Policy Statement: Emergency Physician Shift Work; June 2017.
18. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812. https://doi.org/10.1056/NEJMsa1405556.
19. Rasooly IR, Beidas RS, Wolk CB, et al. Measuring overuse of continuous pulse oximetry in bronchiolitis and developing strategies for large-scale deimplementation: Study protocol for a feasibility trial. Pilot Feasibility Stud. 2019;5:68. https://doi.org/10.1186/s40814-019-0453-2.
20. Coghlin DT, Leyenaar JK, Shen M, et al. Pediatric discharge content: a multisite assessment of physician preferences and experiences. Hosp Pediatr. 2014;4(1):9-15. https://doi.org/10.1542/hpeds.2013-0022.
21. Value in inpatient pediatrics (VIP) Network. 2019. https://www.aap.org/en-us/professional-resources/quality-improvement/Pages/Value-in-Inpatient-Pediatrics.aspx. Accessed October 13, 2019.
22. McDaniel CE, Jennings R, Schroeder AR, et al. Aligning inpatient pediatric research with settings of care: A call to action. Pediatrics. 2019;143(5). https://doi.org/10.1542/peds.2018-2648.
1. Stucky ER, Maniscalco J, Ottolini MC, et al. The Pediatric Hospital Medicine Core Competencies Supplement: a framework for curriculum development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(S2):1-114. https://doi.org/10.1002/jhm.776.
2. Jerardi KE, Fisher E, Rassbach C, et al. Development of a curricular framework for pediatric hospital medicine fellowships. Pediatrics. 2017;140(1). https://doi.org/10.1542/peds.2017-0698.
3. Roberts KB, Fisher ER, Rauch DA. A history of pediatric hospital medicine in the United States, 1996-2019. J Hosp Med. 2019.
4. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-1823.
5. American Board of Medical Specialities. American Board of Medical Specialities application for a new subspecialty certificate: Pediatric hospital medicine. http://www.abms.org/media/114649/abpeds-application-for-pediatric-hospital-medicine.pdf. Accessed November 6, 2019.
6. Leyenaar JK, Ralston SL, Shieh MS, et al. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624.
7. Alvarez F, McDaniel CE, Birnie K, et al. Community pediatric hospitalist workload: results from a national survey. J Hosp Med. 2019;14(10):682-685. https://doi.org/10.12788/jhm.3263.
8. Shah NH, Rhim HJ, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: A survey of program directors. J Hosp Med. 2016;11(5):324-328. https://doi.org/10.1002/jhm.2571.
9. Pediatric Hospital Medicine Fellowship Research Training Development. https://projectreporter.nih.gov/project_info_description.cfm?aid=9593276&icde=47889643. Accessed December 10, 2019.
10. Leyenaar JK, Frintner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018;18(2):200-207. https://doi.org/10.1016/j.acap.2017.05.001.
11. House S, Frintner MP, Leyenaar JK. Factors influencing career longevity in pediatric hospital medicine. Hosp Pediatr. 2019;9(12):983-988. https://doi.org/10.1542/hpeds.2019-0151.
12. PHM Fellowship Programs. http://phmfellows.org/phm-programs/. Accessed November 6, 2019.
13. Rassbach C [Personal communication]; 2019.
14. Bekmezian A, Teufel RJ, 2nd, Wilson KM. Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38-44. https://doi.org/10.1542/hpeds.2011-0006.
15. Fromme HB, Chen CO, Fine BR, Gosdin C, Shaughnessy EE. Pediatric hospitalist workload and sustainability in university-based programs: Results from a national interview-based survey. J Hosp Med. 2018;13(10):702-705. https://doi.org/10.12788/jhm.2977.
16. Gorelick MH, Schremmer R, Ruch-Ross H, Radabaugh C, Selbst S. Current workforce characteristics and burnout in pediatric emergency medicine. Acad Emerg Med. 2016;23(1):48-54. https://doi.org/10.1111/acem.12845.
17. American College of Emergency Physicians. Policy Statement: Emergency Physician Shift Work; June 2017.
18. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812. https://doi.org/10.1056/NEJMsa1405556.
19. Rasooly IR, Beidas RS, Wolk CB, et al. Measuring overuse of continuous pulse oximetry in bronchiolitis and developing strategies for large-scale deimplementation: Study protocol for a feasibility trial. Pilot Feasibility Stud. 2019;5:68. https://doi.org/10.1186/s40814-019-0453-2.
20. Coghlin DT, Leyenaar JK, Shen M, et al. Pediatric discharge content: a multisite assessment of physician preferences and experiences. Hosp Pediatr. 2014;4(1):9-15. https://doi.org/10.1542/hpeds.2013-0022.
21. Value in inpatient pediatrics (VIP) Network. 2019. https://www.aap.org/en-us/professional-resources/quality-improvement/Pages/Value-in-Inpatient-Pediatrics.aspx. Accessed October 13, 2019.
22. McDaniel CE, Jennings R, Schroeder AR, et al. Aligning inpatient pediatric research with settings of care: A call to action. Pediatrics. 2019;143(5). https://doi.org/10.1542/peds.2018-2648.
© 2020 Society of Hospital Medicine
Facilitated Peer Mentoring: Filling a Critical Gap in Academic Hospital Medicine
Traditional mentorship models may not be adequate for academic hospitalists. The traditional dyadic mentorship model, in which a senior principal investigator and research mentee collaborate for career advancement, is well suited for basic science or clinical research. In contrast, areas of academic hospital medicine such as quality improvement, medical education, hospital operations, point-of-care ultrasound, and clinical expertise may be less suited to this traditional mentoring model. In addition, experienced mentors are limited and those available are often overcommitted or have inadequate time due to responsibilities with other leadership roles. Senior mentors may also be limited because of our specialty’s focus on clinical practice rather than longitudinal research or projects.9 There are other limitations of traditional mentorship that are applicable to all fields of academic medicine, including disparate goals, expectations, levels of commitment, and the inherent power differential between the mentor and mentee.10
In this perspective, we discuss our experience with implementing an alternative and complementary mentorship strategy called facilitated peer mentorship with junior faculty hospitalists in the Division of General Internal Medicine at New York–Presbyterian/Weill Cornell Medical Center.
In facilitated peer mentoring programs, faculty typically work collaboratively in groups of three to five with other faculty who are of similar rank, and a faculty member of a higher academic rank works with the group in meeting their scholarly goals.11 The role of the facilitator is to ensure a safe and respectful learning environment, foster peer collaboration, and redirect the group to draw upon their own experiences. Each junior faculty member serves as both a mentor and mentee for each other with bidirectional feedback, guidance, and support in a group setting. This model emphasizes collaboration, peer networking, empowerment, and the development of personal awareness.10 A number of academic medical centers have used peer mentoring as a response to the challenges encountered in the traditional dyad model.12 To our knowledge, the only published example of a peer mentoring model in academic hospital medicine is in the form of a research-in-progress conference.13 While this example addresses peer-mentored research, there is a gap in other areas of academic hospital medicine with mentoring needs—most of all in personal development and career satisfaction.
We piloted a 12-month facilitated peer mentoring program for new hospitalists. The goal of the program was for junior faculty hospitalists to develop a better understanding of their own identity and core values that would enable them to more confidently navigate career choices, enhance their work vitality and career satisfaction, and develop their potential for leadership roles in academic hospital medicine. Each year, a cohort of four to five incoming hospitalists from different backgrounds, interests, and experience were grouped with a more experienced colleague at an associate professor rank who expressed interest and was selected by our section chief to lead the program. The program was required for new hospitalists and consisted of six 90-minute sessions every two months. The attendance rate was 100% and was ensured by scheduling all sessions at the beginning of the academic year with dates agreed upon by all participants. An e-mail reminder was sent one week prior to each session. Each session had assigned readings and an agenda for discussions (see Table for details).
Our evaluation of the program after two years with two separate cohorts included qualitative feedback through an anonymous survey for participants; in addition, qualitative feedback was collected in a one-hour, in-person discussion and reflection with each cohort. We learned several lessons from the feedback we received from program participants. First, our impression was that the career experience of the junior faculty member had a significant impact on the perceived value of group meetings. For those who entered the hospitalist workforce immediately upon completing their terminal training in internal medicine, the exercise of considering different career versions of themselves had added value in promoting thinking outside-the-box for career opportunities within hospital medicine. Academic hospitalists and general internists more broadly, tend to have broad interests that fuel their passions but may also make it more difficult to define long-term goals. One junior faculty member paired her life interests in global medical education with building an international collaboration with other academic hospitalist programs; another faculty member gained confidence and expanded her network of collaborators by designing a research pilot study on hospitalist-initiated end-of-life discussions. In both cases, the junior faculty identified the facilitated peer mentoring program as a strong influence in finding these opportunities. Peer mentoring at the time of entry into the field of hospital medicine, when many have undefined career goals, can be helpful for navigating this issue at the start of a career. On the other hand, those who had already worked as a hospitalist for one or two years and joined the program found less value in career planning exercises.
Second, junior faculty differed in their desire for scope and depth of the curriculum. Some preferred more frequent sessions with more premeeting readings and self-assessments in fewer topics that were covered more longitudinally. A proposed example of a longitudinal topic was defining and refining existing mentoring relationships. Others found it useful to cover more ground with a potpourri of themes; they wanted to cover different knowledge, skills, and attitudes considered important for personal growth and career development, such as negotiation, leading teams, and managing conflict. We recommend the goals of the peer group be defined collaboratively at the beginning of new groups to respond to the needs of the group.
Third, junior faculty varied in how they viewed the goal of the program on a spectrum ranging from social support to mentorship. On one end of the spectrum, the program provided a safe venue for colleagues to convene periodically to discuss work challenges; this group found the support from peers to be helpful. On the other end, some found value in the coaching and mentoring from peers and the experienced facilitator that guided personal growth and career development.
Our pilot program has several limitations. This is a single-center program with a relatively small number of participants; thus, our experience may be unique to our institution and not representative of all academic hospital medicine programs. We also did not obtain any quantitative metrics of evaluation—mixed methods should be used in the future for more rigorous program evaluation. Finally, our peer mentoring model may not cover all domains of mentoring such as sponsorship for career advancement, provision of resources, and promotion of scholarship, though we mentioned an anecdote of scholarship that resulted from networking and redefining of goals that were facilitated through this program. Scholarship is certainly an important feature of academic medicine—other peer mentoring programs may consider forming groups based on research interests to address this gap. A tailored curriculum toward research and scholarship may garner more interest and benefit from participants interested in advancement of scholarship activities.
Overall, the field of hospital medicine is growing rapidly with junior faculty who need effective mentorship. Facilitated peer mentorship among small groups of junior faculty is a feasible and pragmatic mentorship model that can complement more traditional mentorship models. We discovered wide-ranging and contrasting experiences in our program, which suggests that peer mentorship is not a one-size-fits-all approach. However, facilitated peer mentorship can be a highly adaptable and alternative approach to mentorship for diverse groups of hospitalists, including general internal medicine, pediatrics, and other sub
1. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836.
2. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5.
3. Cumbler E, Rendón P, Yirdaw E, et al. Keys to career success: resources and barriers identified by early career academic hospitalists. J Gen Intern Med. 2018;33(5):588-589. https://doi.org/10.1007/s11606-018-4336-7.
4. Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103-1115. https://doi.org/10.1001/jama.296.9.1103.
5. Pololi LH, Evans AT, Civian JT, et al. Faculty vitality-surviving the challenges facing academic health centers: a national survey of medical faculty. Acad Med. 2015;90(7):930-936. https://doi.org/10.1097/ACM.0000000000000674.
6. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. https://doi.org/10.12788/jhm.2854.
7. Wachter RM. The state of hospital medicine in 2008. Med Clin North Am. 2008;92(2):265-273, vii. https://doi.org/10.1016/j.mcna.2007.10.008.
8. Wiese J, Centor R. The need for mentors in the odyssey of the academic hospitalist. J Hosp Med. 2011;6(1):1-2.
9. Rogers JC, Holloway RL, Miller SM. Academic mentoring and family medicine’s research productivity. Fam Med. 1990;22(3):186-190.
10. Pololi L, Knight S. Mentoring faculty in academic medicine. A new paradigm? J Gen Intern Med. 2005;20(9):866-870.
11. Varkey P, Jatoi A, Williams A, et al. The positive impact of a facilitated peer mentoring program on academic skills of women faculty. BMC Med Educ. 2012;12:14. https://doi.org/10.1186/1472-6920-12-14.
12. Pololi LH, Evans AT. Group peer mentoring: an answer to the faculty mentoring problem? A successful program at a large academic department of medicine. J Contin Educ Health Prof. 2015;35(3):192-200. https://doi.org/10.1002/chp.21296.
13. Abougergi MS, Wright SM, Landis R, Howell EE. Research in progress conference for hospitalists provides valuable peer mentoring. J Hosp Med. 2011;6(1):43-46. https://doi.org/10.1002/jhm.865.
Traditional mentorship models may not be adequate for academic hospitalists. The traditional dyadic mentorship model, in which a senior principal investigator and research mentee collaborate for career advancement, is well suited for basic science or clinical research. In contrast, areas of academic hospital medicine such as quality improvement, medical education, hospital operations, point-of-care ultrasound, and clinical expertise may be less suited to this traditional mentoring model. In addition, experienced mentors are limited and those available are often overcommitted or have inadequate time due to responsibilities with other leadership roles. Senior mentors may also be limited because of our specialty’s focus on clinical practice rather than longitudinal research or projects.9 There are other limitations of traditional mentorship that are applicable to all fields of academic medicine, including disparate goals, expectations, levels of commitment, and the inherent power differential between the mentor and mentee.10
In this perspective, we discuss our experience with implementing an alternative and complementary mentorship strategy called facilitated peer mentorship with junior faculty hospitalists in the Division of General Internal Medicine at New York–Presbyterian/Weill Cornell Medical Center.
In facilitated peer mentoring programs, faculty typically work collaboratively in groups of three to five with other faculty who are of similar rank, and a faculty member of a higher academic rank works with the group in meeting their scholarly goals.11 The role of the facilitator is to ensure a safe and respectful learning environment, foster peer collaboration, and redirect the group to draw upon their own experiences. Each junior faculty member serves as both a mentor and mentee for each other with bidirectional feedback, guidance, and support in a group setting. This model emphasizes collaboration, peer networking, empowerment, and the development of personal awareness.10 A number of academic medical centers have used peer mentoring as a response to the challenges encountered in the traditional dyad model.12 To our knowledge, the only published example of a peer mentoring model in academic hospital medicine is in the form of a research-in-progress conference.13 While this example addresses peer-mentored research, there is a gap in other areas of academic hospital medicine with mentoring needs—most of all in personal development and career satisfaction.
We piloted a 12-month facilitated peer mentoring program for new hospitalists. The goal of the program was for junior faculty hospitalists to develop a better understanding of their own identity and core values that would enable them to more confidently navigate career choices, enhance their work vitality and career satisfaction, and develop their potential for leadership roles in academic hospital medicine. Each year, a cohort of four to five incoming hospitalists from different backgrounds, interests, and experience were grouped with a more experienced colleague at an associate professor rank who expressed interest and was selected by our section chief to lead the program. The program was required for new hospitalists and consisted of six 90-minute sessions every two months. The attendance rate was 100% and was ensured by scheduling all sessions at the beginning of the academic year with dates agreed upon by all participants. An e-mail reminder was sent one week prior to each session. Each session had assigned readings and an agenda for discussions (see Table for details).
Our evaluation of the program after two years with two separate cohorts included qualitative feedback through an anonymous survey for participants; in addition, qualitative feedback was collected in a one-hour, in-person discussion and reflection with each cohort. We learned several lessons from the feedback we received from program participants. First, our impression was that the career experience of the junior faculty member had a significant impact on the perceived value of group meetings. For those who entered the hospitalist workforce immediately upon completing their terminal training in internal medicine, the exercise of considering different career versions of themselves had added value in promoting thinking outside-the-box for career opportunities within hospital medicine. Academic hospitalists and general internists more broadly, tend to have broad interests that fuel their passions but may also make it more difficult to define long-term goals. One junior faculty member paired her life interests in global medical education with building an international collaboration with other academic hospitalist programs; another faculty member gained confidence and expanded her network of collaborators by designing a research pilot study on hospitalist-initiated end-of-life discussions. In both cases, the junior faculty identified the facilitated peer mentoring program as a strong influence in finding these opportunities. Peer mentoring at the time of entry into the field of hospital medicine, when many have undefined career goals, can be helpful for navigating this issue at the start of a career. On the other hand, those who had already worked as a hospitalist for one or two years and joined the program found less value in career planning exercises.
Second, junior faculty differed in their desire for scope and depth of the curriculum. Some preferred more frequent sessions with more premeeting readings and self-assessments in fewer topics that were covered more longitudinally. A proposed example of a longitudinal topic was defining and refining existing mentoring relationships. Others found it useful to cover more ground with a potpourri of themes; they wanted to cover different knowledge, skills, and attitudes considered important for personal growth and career development, such as negotiation, leading teams, and managing conflict. We recommend the goals of the peer group be defined collaboratively at the beginning of new groups to respond to the needs of the group.
Third, junior faculty varied in how they viewed the goal of the program on a spectrum ranging from social support to mentorship. On one end of the spectrum, the program provided a safe venue for colleagues to convene periodically to discuss work challenges; this group found the support from peers to be helpful. On the other end, some found value in the coaching and mentoring from peers and the experienced facilitator that guided personal growth and career development.
Our pilot program has several limitations. This is a single-center program with a relatively small number of participants; thus, our experience may be unique to our institution and not representative of all academic hospital medicine programs. We also did not obtain any quantitative metrics of evaluation—mixed methods should be used in the future for more rigorous program evaluation. Finally, our peer mentoring model may not cover all domains of mentoring such as sponsorship for career advancement, provision of resources, and promotion of scholarship, though we mentioned an anecdote of scholarship that resulted from networking and redefining of goals that were facilitated through this program. Scholarship is certainly an important feature of academic medicine—other peer mentoring programs may consider forming groups based on research interests to address this gap. A tailored curriculum toward research and scholarship may garner more interest and benefit from participants interested in advancement of scholarship activities.
Overall, the field of hospital medicine is growing rapidly with junior faculty who need effective mentorship. Facilitated peer mentorship among small groups of junior faculty is a feasible and pragmatic mentorship model that can complement more traditional mentorship models. We discovered wide-ranging and contrasting experiences in our program, which suggests that peer mentorship is not a one-size-fits-all approach. However, facilitated peer mentorship can be a highly adaptable and alternative approach to mentorship for diverse groups of hospitalists, including general internal medicine, pediatrics, and other sub
Traditional mentorship models may not be adequate for academic hospitalists. The traditional dyadic mentorship model, in which a senior principal investigator and research mentee collaborate for career advancement, is well suited for basic science or clinical research. In contrast, areas of academic hospital medicine such as quality improvement, medical education, hospital operations, point-of-care ultrasound, and clinical expertise may be less suited to this traditional mentoring model. In addition, experienced mentors are limited and those available are often overcommitted or have inadequate time due to responsibilities with other leadership roles. Senior mentors may also be limited because of our specialty’s focus on clinical practice rather than longitudinal research or projects.9 There are other limitations of traditional mentorship that are applicable to all fields of academic medicine, including disparate goals, expectations, levels of commitment, and the inherent power differential between the mentor and mentee.10
In this perspective, we discuss our experience with implementing an alternative and complementary mentorship strategy called facilitated peer mentorship with junior faculty hospitalists in the Division of General Internal Medicine at New York–Presbyterian/Weill Cornell Medical Center.
In facilitated peer mentoring programs, faculty typically work collaboratively in groups of three to five with other faculty who are of similar rank, and a faculty member of a higher academic rank works with the group in meeting their scholarly goals.11 The role of the facilitator is to ensure a safe and respectful learning environment, foster peer collaboration, and redirect the group to draw upon their own experiences. Each junior faculty member serves as both a mentor and mentee for each other with bidirectional feedback, guidance, and support in a group setting. This model emphasizes collaboration, peer networking, empowerment, and the development of personal awareness.10 A number of academic medical centers have used peer mentoring as a response to the challenges encountered in the traditional dyad model.12 To our knowledge, the only published example of a peer mentoring model in academic hospital medicine is in the form of a research-in-progress conference.13 While this example addresses peer-mentored research, there is a gap in other areas of academic hospital medicine with mentoring needs—most of all in personal development and career satisfaction.
We piloted a 12-month facilitated peer mentoring program for new hospitalists. The goal of the program was for junior faculty hospitalists to develop a better understanding of their own identity and core values that would enable them to more confidently navigate career choices, enhance their work vitality and career satisfaction, and develop their potential for leadership roles in academic hospital medicine. Each year, a cohort of four to five incoming hospitalists from different backgrounds, interests, and experience were grouped with a more experienced colleague at an associate professor rank who expressed interest and was selected by our section chief to lead the program. The program was required for new hospitalists and consisted of six 90-minute sessions every two months. The attendance rate was 100% and was ensured by scheduling all sessions at the beginning of the academic year with dates agreed upon by all participants. An e-mail reminder was sent one week prior to each session. Each session had assigned readings and an agenda for discussions (see Table for details).
Our evaluation of the program after two years with two separate cohorts included qualitative feedback through an anonymous survey for participants; in addition, qualitative feedback was collected in a one-hour, in-person discussion and reflection with each cohort. We learned several lessons from the feedback we received from program participants. First, our impression was that the career experience of the junior faculty member had a significant impact on the perceived value of group meetings. For those who entered the hospitalist workforce immediately upon completing their terminal training in internal medicine, the exercise of considering different career versions of themselves had added value in promoting thinking outside-the-box for career opportunities within hospital medicine. Academic hospitalists and general internists more broadly, tend to have broad interests that fuel their passions but may also make it more difficult to define long-term goals. One junior faculty member paired her life interests in global medical education with building an international collaboration with other academic hospitalist programs; another faculty member gained confidence and expanded her network of collaborators by designing a research pilot study on hospitalist-initiated end-of-life discussions. In both cases, the junior faculty identified the facilitated peer mentoring program as a strong influence in finding these opportunities. Peer mentoring at the time of entry into the field of hospital medicine, when many have undefined career goals, can be helpful for navigating this issue at the start of a career. On the other hand, those who had already worked as a hospitalist for one or two years and joined the program found less value in career planning exercises.
Second, junior faculty differed in their desire for scope and depth of the curriculum. Some preferred more frequent sessions with more premeeting readings and self-assessments in fewer topics that were covered more longitudinally. A proposed example of a longitudinal topic was defining and refining existing mentoring relationships. Others found it useful to cover more ground with a potpourri of themes; they wanted to cover different knowledge, skills, and attitudes considered important for personal growth and career development, such as negotiation, leading teams, and managing conflict. We recommend the goals of the peer group be defined collaboratively at the beginning of new groups to respond to the needs of the group.
Third, junior faculty varied in how they viewed the goal of the program on a spectrum ranging from social support to mentorship. On one end of the spectrum, the program provided a safe venue for colleagues to convene periodically to discuss work challenges; this group found the support from peers to be helpful. On the other end, some found value in the coaching and mentoring from peers and the experienced facilitator that guided personal growth and career development.
Our pilot program has several limitations. This is a single-center program with a relatively small number of participants; thus, our experience may be unique to our institution and not representative of all academic hospital medicine programs. We also did not obtain any quantitative metrics of evaluation—mixed methods should be used in the future for more rigorous program evaluation. Finally, our peer mentoring model may not cover all domains of mentoring such as sponsorship for career advancement, provision of resources, and promotion of scholarship, though we mentioned an anecdote of scholarship that resulted from networking and redefining of goals that were facilitated through this program. Scholarship is certainly an important feature of academic medicine—other peer mentoring programs may consider forming groups based on research interests to address this gap. A tailored curriculum toward research and scholarship may garner more interest and benefit from participants interested in advancement of scholarship activities.
Overall, the field of hospital medicine is growing rapidly with junior faculty who need effective mentorship. Facilitated peer mentorship among small groups of junior faculty is a feasible and pragmatic mentorship model that can complement more traditional mentorship models. We discovered wide-ranging and contrasting experiences in our program, which suggests that peer mentorship is not a one-size-fits-all approach. However, facilitated peer mentorship can be a highly adaptable and alternative approach to mentorship for diverse groups of hospitalists, including general internal medicine, pediatrics, and other sub
1. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836.
2. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5.
3. Cumbler E, Rendón P, Yirdaw E, et al. Keys to career success: resources and barriers identified by early career academic hospitalists. J Gen Intern Med. 2018;33(5):588-589. https://doi.org/10.1007/s11606-018-4336-7.
4. Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103-1115. https://doi.org/10.1001/jama.296.9.1103.
5. Pololi LH, Evans AT, Civian JT, et al. Faculty vitality-surviving the challenges facing academic health centers: a national survey of medical faculty. Acad Med. 2015;90(7):930-936. https://doi.org/10.1097/ACM.0000000000000674.
6. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. https://doi.org/10.12788/jhm.2854.
7. Wachter RM. The state of hospital medicine in 2008. Med Clin North Am. 2008;92(2):265-273, vii. https://doi.org/10.1016/j.mcna.2007.10.008.
8. Wiese J, Centor R. The need for mentors in the odyssey of the academic hospitalist. J Hosp Med. 2011;6(1):1-2.
9. Rogers JC, Holloway RL, Miller SM. Academic mentoring and family medicine’s research productivity. Fam Med. 1990;22(3):186-190.
10. Pololi L, Knight S. Mentoring faculty in academic medicine. A new paradigm? J Gen Intern Med. 2005;20(9):866-870.
11. Varkey P, Jatoi A, Williams A, et al. The positive impact of a facilitated peer mentoring program on academic skills of women faculty. BMC Med Educ. 2012;12:14. https://doi.org/10.1186/1472-6920-12-14.
12. Pololi LH, Evans AT. Group peer mentoring: an answer to the faculty mentoring problem? A successful program at a large academic department of medicine. J Contin Educ Health Prof. 2015;35(3):192-200. https://doi.org/10.1002/chp.21296.
13. Abougergi MS, Wright SM, Landis R, Howell EE. Research in progress conference for hospitalists provides valuable peer mentoring. J Hosp Med. 2011;6(1):43-46. https://doi.org/10.1002/jhm.865.
1. Harrison R, Hunter AJ, Sharpe B, Auerbach AD. Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5-9. https://doi.org/10.1002/jhm.836.
2. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5.
3. Cumbler E, Rendón P, Yirdaw E, et al. Keys to career success: resources and barriers identified by early career academic hospitalists. J Gen Intern Med. 2018;33(5):588-589. https://doi.org/10.1007/s11606-018-4336-7.
4. Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103-1115. https://doi.org/10.1001/jama.296.9.1103.
5. Pololi LH, Evans AT, Civian JT, et al. Faculty vitality-surviving the challenges facing academic health centers: a national survey of medical faculty. Acad Med. 2015;90(7):930-936. https://doi.org/10.1097/ACM.0000000000000674.
6. Nagarur A, O’Neill RM, Lawton D, Greenwald JL. Supporting faculty development in hospital medicine: design and implementation of a personalized structured mentoring program. J Hosp Med. 2018;13(2):96-99. https://doi.org/10.12788/jhm.2854.
7. Wachter RM. The state of hospital medicine in 2008. Med Clin North Am. 2008;92(2):265-273, vii. https://doi.org/10.1016/j.mcna.2007.10.008.
8. Wiese J, Centor R. The need for mentors in the odyssey of the academic hospitalist. J Hosp Med. 2011;6(1):1-2.
9. Rogers JC, Holloway RL, Miller SM. Academic mentoring and family medicine’s research productivity. Fam Med. 1990;22(3):186-190.
10. Pololi L, Knight S. Mentoring faculty in academic medicine. A new paradigm? J Gen Intern Med. 2005;20(9):866-870.
11. Varkey P, Jatoi A, Williams A, et al. The positive impact of a facilitated peer mentoring program on academic skills of women faculty. BMC Med Educ. 2012;12:14. https://doi.org/10.1186/1472-6920-12-14.
12. Pololi LH, Evans AT. Group peer mentoring: an answer to the faculty mentoring problem? A successful program at a large academic department of medicine. J Contin Educ Health Prof. 2015;35(3):192-200. https://doi.org/10.1002/chp.21296.
13. Abougergi MS, Wright SM, Landis R, Howell EE. Research in progress conference for hospitalists provides valuable peer mentoring. J Hosp Med. 2011;6(1):43-46. https://doi.org/10.1002/jhm.865.
© 2020 Society of Hospital Medicine
Academic Hospital Medicine 2.0: If You Aren’t Teaching Residents, Are You Still Academic?
“How much teaching time will I get in my first year on faculty?” Leaders at academic hospitalist programs know to expect this question from almost every applicant. We also know that we will be graded on our response; the more resident-covered service time, the better. For some applicants, this question is a key litmus test. Some prospective faculty choose to pursue academic hospital medicine because of their own experiences on the wards during residency. They recall the excitement of leading a team of interns and students under the wing of a seasoned attending, replete with chalk talks, clinical pearls, and inspired learners. Teaching time is more quantifiable than mentorship quality and academic opportunity, more important than salary and patient load for some, and more familiar than relative value unit expectations.
Over the past two decades, academic hospitalist programs have steadily grown,1 but their teaching footprints have not.2,3 Although historically some academic hospitalists spent almost 100% of their clinical time on teaching services, work hour rules and diversification of resident clinical time toward outpatient and subspecialty activities have decreased the amount of general medicine ward time for residents.2 In addition, as academic medical centers broadened their clinical networks, inpatient volumes exceeded the capacity of teaching services. Finally, several large academic medical centers and healthcare networks are acquiring or building additional hospitals, increasing the number of medical beds that are staffed by hospitalists without residents.4
In our experience, as academic healthcare systems continue to grow and hospital medicine programs rapidly expand to meet clinical needs, the percentage of clinical time spent on a traditional ward teaching service continues to decrease. In several academic hospitalist programs, the majority of faculty effort is now devoted to direct care,5 with limited resident-covered ward time spread across a larger group of faculty. The 2018 State of Hospital Medicine Report suggests that our experience is not unique with academic programs caring for adults reporting that 31% of clinical work was on traditional ward teaching services, 16% on direct care services with intermittent learners, and 53% on nonteaching services.5
This current state of affairs raises a number of questions as follows:
- How can hospitalist program leaders take advantage of existing resident teaching opportunities?
- How should those teaching opportunities be allocated?
- What nontraditional teaching venues exist in academic medicine?
- How can faculty develop their teaching skills in an environment with limited traditional ward teaching time.
We believe that these changes require us to redefine what it means to be an academic hospitalist, both for existing faculty and for prospective faculty whose views of academic hospital medicine may have been shaped by role models seen only in their clinical teaching role.
MAXIMIZING RESIDENT TEACHING OPPORTUNITIES
Is reduced teaching time the new normal or will the pendulum swing back toward more resident teaching time for academic hospitalists? The former is likely the case. None of the current trends in medical education point to an expansion of residents in the inpatient setting. Although there may be some opportunities to assume general medicine attending time is currently covered by primary care physicians and subspecialists, in several programs, hospitalists already cover the overwhelming majority of general medicine teaching services.
Although there may be occasional opportunities for academic hospitalist programs to develop new teaching roles with residents or fellows (for example, by expanding to community sites with residency programs or to subspecialty teaching services, or by creating hospital medicine fellowships and resident or student electives), the reality is that we as hospitalists will need to adapt to direct care as the plurality of our work.
ALLOCATING TEACHING TIME
How should we allocate traditional teaching time among our faculty? Since it is a coveted—but relatively scarce—resource, teaching time should be allocated thoughtfully. Based on our collective experience, academic hospitalist groups have taken a variety of approaches to this challenge, including forming separate clinical groups at the same institution (a teaching faculty group and a nonteaching group),6 requiring all hospitalists to do some amount of direct care to facilitate distribution of teaching time or having merit or seniority-based teaching time allocation (based on teaching evaluations, formal teaching roles such as program director status, or years on faculty).
Each approach to assigning teaching time has its challenges. Hospitalist leaders must manage these issues through transparency about the selection process for teaching rotations and open discussion of teaching evaluations with faculty. It is also critical that the recruitment process set appropriate expectations for faculty candidates. Highlighting academic opportunities outside of teaching residents, including leadership roles, quality improvement work, and research, may encourage applicants and current hospitalists to explore more varied career trajectories. Hospitalists focusing on these other paths may elect to have less teaching time, freeing up opportunities for dedicated clinician educators.
BEYOND TRADITIONAL RESIDENT TEACHING TEAMS
What other ward-based teaching opportunities might be available for academic hospitalists who do not have the opportunity to attend on traditional resident teaching teams? As supervisory requirements for residents have been strengthened, expansion of teaching into the evening and overnight hours to supervise new admissions to the teaching services has been one approach to augment teaching footprints.7,8
In addition, nontraditional teaching teams such as attending/intern teams (without a supervising resident) or attending/subintern (fourth-year medical student) teams have been developed at some institutions.9 Although allowing for additional exposure to learners, these models require a more hands-on approach than traditional teaching teams, particularly at the start of the academic year. Finally, as hospitalist teams have grown to include advanced practice providers (APPs), some programs have established formal teaching programs to address professional development needs of these healthcare professionals.10,11
DEVELOPING HOSPITALIST EDUCATORS
How do we help junior faculty who have the potential to be talented educators succeed in teaching when they have limited opportunities to engage with residents on clinical services? One approach is to encourage hospitalists to participate in resident didactic sessions such as “morning report” and noon conference. Another approach is to focus on teaching other learners. For example, several academic medical centers provide opportunities for hospitalists to engage in student teaching, either on the wards or via classroom instruction. In addition, as mentioned previously, APPs who are new to hospital medicine are an engaged audience and represent an opportunity for hospitalist educators to utilize and hone their teaching skills. Finally, organizing lectures for nursing colleagues is another way for the faculty to practice “chalk talks” and develop teaching portfolios.
Hospitalists can also leverage their expertise to build systems in which academic hospitalists are teaching each other, creating a culture of continuous learning. These activities may include case conferences, morbidity and mortality conferences, journal clubs, clinical topic updates developed by and for hospitalists, simulation exercises, and other group learning sessions. Giving hospitalists the opportunity to teach each other allows for professional growth that is not dependent on the presence of traditional learners.
REDEFINING ACADEMIC HOSPITALISTS
Philosophically, a key question is “What makes ‘academic’ academic?” Traditionally, academic hospitalist positions were synonymous with resident teaching or, for a small number of academic hospitalists, significant funded research. In an era where teaching residents may no longer be part of the job description for many hospitalists at academic medical centers, what distinguishes these positions from 100% clinical positions and what are the implications for academic hospital medicine?
Although data regarding why hospitalists seek “nonteaching” positions at academic medical centers are lacking, we believe that these jobs remain popular due to opportunities that are perceived to be unique to academic medical centers. These include more flexible scheduling (academic programs may be less likely to have seven-on/seven-off schedules), exposure to research and cutting-edge technology, opportunities to care for tertiary and quaternary care patients, collaboration with academic peers and experts in the field, and interaction with a range of learners, including medical, pharmacy, advanced practitioner, and other students.
Understanding the motivation of candidates who apply for academic hospital medicine positions—aside from supervising/teaching residents—will be an important goal for academic hospitalist leaders to ensure future success in staffing growing programs and creating sustainable academic hospitalist careers. As resident teaching time decreases, implementing robust faculty or professional development programs to address the broader interests and needs of academic hospitalist faculty will be increasingly important. Sehgal et al. described one such program for faculty development,12 and a more recent paper outlines a faculty development program focused on quality improvement and patient safety.13 These types of programs provide opportunities for academic hospitalists to engage in academic pursuits that are independent of residency programs.
CONCLUSION
Therefore, what do we tell the eager faculty applicant? First, we should not hide from the honest answer, ie, new faculty may not get as much resident teaching time as they would like or expect. Although we want hospitalists to maintain integral involvement in residency training programs, we also want to build a culture of clinical excellence, scholarship, and continuous learning that is not dependent on directly teaching residents. We should highlight the unique opportunities of academic hospital medicine, including teaching other learners, caring for tertiary/quaternary care patients, working with colleagues who are leaders in their field, and engaging in research and quality improvement work. By capitalizing on these opportunities, we can actively redefine what makes “academic” academic and ensure that we sustain academic hospital medicine as a desirable and rewarding career.
Disclosures
The authors have nothing to disclose.
1. Wachter RM, Goldman L. Zero to 50,000-the 20th anniversary of the hospitalist. N Engl J Med 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
2. Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392-393. https://doi.org/10.1111/j.1525-1497.2004.42002.x.
3. Flanders SA, Saint S, McMahon LF, Howell JD. Where should hospitalists sit within the academic medical center? J Gen Intern Med. 2008;23(8):1269-1272. https://doi.org/10.1007/s11606-008-0682-1.
4. 5 Hospital projects announced this year worth $1B or more. ASC Communications, 2019. https://www.beckershospitalreview.com/facilities-management/5-hospital-projects-announced-this-year-worth-1b-or-more.html. Accessed August 24, 2019.
5. White A, Anders J, Anoff DL, Creamer J, Flores LA. Table 3.45 Distribution of work in academic hmgs. Philadelphia, PA: Society of Hospital Medicine; 201 8.
6. Hunt D, Burger A, Harrison R, Southern W, Boonyasai RT, Leykum L. Hospitalist staffing: To split or not to split? SGIM Forum 2013;36:6.
7. Farnan JM, Burger A, Boonyasai RT, et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521-523. https://doi.org/10.1002/jhm.1961.
8. Sani SN, Wistar E, Le L, Chia D, Haber LA. Shining a light on overnight education: Hospitalist and resident impressions of the current state, barriers, and methods for improvement. Cureus 2018;10:e2939. https://doi.org/10.7759/cureus.2939.
9. O’Leary KJ, Chadha V, Fleming VM, Martin GJ, Baker DW. Medical subinternship: student experience on a resident uncovered hospitalist service. Teach Learn Med. 2008;20(1):18-21. https://doi.org/10.1080/10401330701797974.
10. Klimpl D, Franco T, Tackett S, et al. The current state of advanced practice provider fellowships in hospital medicine: A survey of program directors. J Hosp Med. 2019;14(7):401-406. https://doi.org/10.12788/jhm.3191.
11. Lackner C, Eid S, Panek T, Kisuule F. An advanced practice provider clinical fellowship as a pipeline to staffing a hospitalist program. J Hosp Med. 2019;14(6):336-339. https://doi.org/10.12788/jhm.3183.
12. Sehgal NL, Sharpe BA, Auerbach AA et al. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845.
13. van Schaik SM, Chang A, Fogh S, et al. Jumpstarting faculty development in quality improvement and patient safety education: A team-based approach. Acad Med. 2019.
“How much teaching time will I get in my first year on faculty?” Leaders at academic hospitalist programs know to expect this question from almost every applicant. We also know that we will be graded on our response; the more resident-covered service time, the better. For some applicants, this question is a key litmus test. Some prospective faculty choose to pursue academic hospital medicine because of their own experiences on the wards during residency. They recall the excitement of leading a team of interns and students under the wing of a seasoned attending, replete with chalk talks, clinical pearls, and inspired learners. Teaching time is more quantifiable than mentorship quality and academic opportunity, more important than salary and patient load for some, and more familiar than relative value unit expectations.
Over the past two decades, academic hospitalist programs have steadily grown,1 but their teaching footprints have not.2,3 Although historically some academic hospitalists spent almost 100% of their clinical time on teaching services, work hour rules and diversification of resident clinical time toward outpatient and subspecialty activities have decreased the amount of general medicine ward time for residents.2 In addition, as academic medical centers broadened their clinical networks, inpatient volumes exceeded the capacity of teaching services. Finally, several large academic medical centers and healthcare networks are acquiring or building additional hospitals, increasing the number of medical beds that are staffed by hospitalists without residents.4
In our experience, as academic healthcare systems continue to grow and hospital medicine programs rapidly expand to meet clinical needs, the percentage of clinical time spent on a traditional ward teaching service continues to decrease. In several academic hospitalist programs, the majority of faculty effort is now devoted to direct care,5 with limited resident-covered ward time spread across a larger group of faculty. The 2018 State of Hospital Medicine Report suggests that our experience is not unique with academic programs caring for adults reporting that 31% of clinical work was on traditional ward teaching services, 16% on direct care services with intermittent learners, and 53% on nonteaching services.5
This current state of affairs raises a number of questions as follows:
- How can hospitalist program leaders take advantage of existing resident teaching opportunities?
- How should those teaching opportunities be allocated?
- What nontraditional teaching venues exist in academic medicine?
- How can faculty develop their teaching skills in an environment with limited traditional ward teaching time.
We believe that these changes require us to redefine what it means to be an academic hospitalist, both for existing faculty and for prospective faculty whose views of academic hospital medicine may have been shaped by role models seen only in their clinical teaching role.
MAXIMIZING RESIDENT TEACHING OPPORTUNITIES
Is reduced teaching time the new normal or will the pendulum swing back toward more resident teaching time for academic hospitalists? The former is likely the case. None of the current trends in medical education point to an expansion of residents in the inpatient setting. Although there may be some opportunities to assume general medicine attending time is currently covered by primary care physicians and subspecialists, in several programs, hospitalists already cover the overwhelming majority of general medicine teaching services.
Although there may be occasional opportunities for academic hospitalist programs to develop new teaching roles with residents or fellows (for example, by expanding to community sites with residency programs or to subspecialty teaching services, or by creating hospital medicine fellowships and resident or student electives), the reality is that we as hospitalists will need to adapt to direct care as the plurality of our work.
ALLOCATING TEACHING TIME
How should we allocate traditional teaching time among our faculty? Since it is a coveted—but relatively scarce—resource, teaching time should be allocated thoughtfully. Based on our collective experience, academic hospitalist groups have taken a variety of approaches to this challenge, including forming separate clinical groups at the same institution (a teaching faculty group and a nonteaching group),6 requiring all hospitalists to do some amount of direct care to facilitate distribution of teaching time or having merit or seniority-based teaching time allocation (based on teaching evaluations, formal teaching roles such as program director status, or years on faculty).
Each approach to assigning teaching time has its challenges. Hospitalist leaders must manage these issues through transparency about the selection process for teaching rotations and open discussion of teaching evaluations with faculty. It is also critical that the recruitment process set appropriate expectations for faculty candidates. Highlighting academic opportunities outside of teaching residents, including leadership roles, quality improvement work, and research, may encourage applicants and current hospitalists to explore more varied career trajectories. Hospitalists focusing on these other paths may elect to have less teaching time, freeing up opportunities for dedicated clinician educators.
BEYOND TRADITIONAL RESIDENT TEACHING TEAMS
What other ward-based teaching opportunities might be available for academic hospitalists who do not have the opportunity to attend on traditional resident teaching teams? As supervisory requirements for residents have been strengthened, expansion of teaching into the evening and overnight hours to supervise new admissions to the teaching services has been one approach to augment teaching footprints.7,8
In addition, nontraditional teaching teams such as attending/intern teams (without a supervising resident) or attending/subintern (fourth-year medical student) teams have been developed at some institutions.9 Although allowing for additional exposure to learners, these models require a more hands-on approach than traditional teaching teams, particularly at the start of the academic year. Finally, as hospitalist teams have grown to include advanced practice providers (APPs), some programs have established formal teaching programs to address professional development needs of these healthcare professionals.10,11
DEVELOPING HOSPITALIST EDUCATORS
How do we help junior faculty who have the potential to be talented educators succeed in teaching when they have limited opportunities to engage with residents on clinical services? One approach is to encourage hospitalists to participate in resident didactic sessions such as “morning report” and noon conference. Another approach is to focus on teaching other learners. For example, several academic medical centers provide opportunities for hospitalists to engage in student teaching, either on the wards or via classroom instruction. In addition, as mentioned previously, APPs who are new to hospital medicine are an engaged audience and represent an opportunity for hospitalist educators to utilize and hone their teaching skills. Finally, organizing lectures for nursing colleagues is another way for the faculty to practice “chalk talks” and develop teaching portfolios.
Hospitalists can also leverage their expertise to build systems in which academic hospitalists are teaching each other, creating a culture of continuous learning. These activities may include case conferences, morbidity and mortality conferences, journal clubs, clinical topic updates developed by and for hospitalists, simulation exercises, and other group learning sessions. Giving hospitalists the opportunity to teach each other allows for professional growth that is not dependent on the presence of traditional learners.
REDEFINING ACADEMIC HOSPITALISTS
Philosophically, a key question is “What makes ‘academic’ academic?” Traditionally, academic hospitalist positions were synonymous with resident teaching or, for a small number of academic hospitalists, significant funded research. In an era where teaching residents may no longer be part of the job description for many hospitalists at academic medical centers, what distinguishes these positions from 100% clinical positions and what are the implications for academic hospital medicine?
Although data regarding why hospitalists seek “nonteaching” positions at academic medical centers are lacking, we believe that these jobs remain popular due to opportunities that are perceived to be unique to academic medical centers. These include more flexible scheduling (academic programs may be less likely to have seven-on/seven-off schedules), exposure to research and cutting-edge technology, opportunities to care for tertiary and quaternary care patients, collaboration with academic peers and experts in the field, and interaction with a range of learners, including medical, pharmacy, advanced practitioner, and other students.
Understanding the motivation of candidates who apply for academic hospital medicine positions—aside from supervising/teaching residents—will be an important goal for academic hospitalist leaders to ensure future success in staffing growing programs and creating sustainable academic hospitalist careers. As resident teaching time decreases, implementing robust faculty or professional development programs to address the broader interests and needs of academic hospitalist faculty will be increasingly important. Sehgal et al. described one such program for faculty development,12 and a more recent paper outlines a faculty development program focused on quality improvement and patient safety.13 These types of programs provide opportunities for academic hospitalists to engage in academic pursuits that are independent of residency programs.
CONCLUSION
Therefore, what do we tell the eager faculty applicant? First, we should not hide from the honest answer, ie, new faculty may not get as much resident teaching time as they would like or expect. Although we want hospitalists to maintain integral involvement in residency training programs, we also want to build a culture of clinical excellence, scholarship, and continuous learning that is not dependent on directly teaching residents. We should highlight the unique opportunities of academic hospital medicine, including teaching other learners, caring for tertiary/quaternary care patients, working with colleagues who are leaders in their field, and engaging in research and quality improvement work. By capitalizing on these opportunities, we can actively redefine what makes “academic” academic and ensure that we sustain academic hospital medicine as a desirable and rewarding career.
Disclosures
The authors have nothing to disclose.
“How much teaching time will I get in my first year on faculty?” Leaders at academic hospitalist programs know to expect this question from almost every applicant. We also know that we will be graded on our response; the more resident-covered service time, the better. For some applicants, this question is a key litmus test. Some prospective faculty choose to pursue academic hospital medicine because of their own experiences on the wards during residency. They recall the excitement of leading a team of interns and students under the wing of a seasoned attending, replete with chalk talks, clinical pearls, and inspired learners. Teaching time is more quantifiable than mentorship quality and academic opportunity, more important than salary and patient load for some, and more familiar than relative value unit expectations.
Over the past two decades, academic hospitalist programs have steadily grown,1 but their teaching footprints have not.2,3 Although historically some academic hospitalists spent almost 100% of their clinical time on teaching services, work hour rules and diversification of resident clinical time toward outpatient and subspecialty activities have decreased the amount of general medicine ward time for residents.2 In addition, as academic medical centers broadened their clinical networks, inpatient volumes exceeded the capacity of teaching services. Finally, several large academic medical centers and healthcare networks are acquiring or building additional hospitals, increasing the number of medical beds that are staffed by hospitalists without residents.4
In our experience, as academic healthcare systems continue to grow and hospital medicine programs rapidly expand to meet clinical needs, the percentage of clinical time spent on a traditional ward teaching service continues to decrease. In several academic hospitalist programs, the majority of faculty effort is now devoted to direct care,5 with limited resident-covered ward time spread across a larger group of faculty. The 2018 State of Hospital Medicine Report suggests that our experience is not unique with academic programs caring for adults reporting that 31% of clinical work was on traditional ward teaching services, 16% on direct care services with intermittent learners, and 53% on nonteaching services.5
This current state of affairs raises a number of questions as follows:
- How can hospitalist program leaders take advantage of existing resident teaching opportunities?
- How should those teaching opportunities be allocated?
- What nontraditional teaching venues exist in academic medicine?
- How can faculty develop their teaching skills in an environment with limited traditional ward teaching time.
We believe that these changes require us to redefine what it means to be an academic hospitalist, both for existing faculty and for prospective faculty whose views of academic hospital medicine may have been shaped by role models seen only in their clinical teaching role.
MAXIMIZING RESIDENT TEACHING OPPORTUNITIES
Is reduced teaching time the new normal or will the pendulum swing back toward more resident teaching time for academic hospitalists? The former is likely the case. None of the current trends in medical education point to an expansion of residents in the inpatient setting. Although there may be some opportunities to assume general medicine attending time is currently covered by primary care physicians and subspecialists, in several programs, hospitalists already cover the overwhelming majority of general medicine teaching services.
Although there may be occasional opportunities for academic hospitalist programs to develop new teaching roles with residents or fellows (for example, by expanding to community sites with residency programs or to subspecialty teaching services, or by creating hospital medicine fellowships and resident or student electives), the reality is that we as hospitalists will need to adapt to direct care as the plurality of our work.
ALLOCATING TEACHING TIME
How should we allocate traditional teaching time among our faculty? Since it is a coveted—but relatively scarce—resource, teaching time should be allocated thoughtfully. Based on our collective experience, academic hospitalist groups have taken a variety of approaches to this challenge, including forming separate clinical groups at the same institution (a teaching faculty group and a nonteaching group),6 requiring all hospitalists to do some amount of direct care to facilitate distribution of teaching time or having merit or seniority-based teaching time allocation (based on teaching evaluations, formal teaching roles such as program director status, or years on faculty).
Each approach to assigning teaching time has its challenges. Hospitalist leaders must manage these issues through transparency about the selection process for teaching rotations and open discussion of teaching evaluations with faculty. It is also critical that the recruitment process set appropriate expectations for faculty candidates. Highlighting academic opportunities outside of teaching residents, including leadership roles, quality improvement work, and research, may encourage applicants and current hospitalists to explore more varied career trajectories. Hospitalists focusing on these other paths may elect to have less teaching time, freeing up opportunities for dedicated clinician educators.
BEYOND TRADITIONAL RESIDENT TEACHING TEAMS
What other ward-based teaching opportunities might be available for academic hospitalists who do not have the opportunity to attend on traditional resident teaching teams? As supervisory requirements for residents have been strengthened, expansion of teaching into the evening and overnight hours to supervise new admissions to the teaching services has been one approach to augment teaching footprints.7,8
In addition, nontraditional teaching teams such as attending/intern teams (without a supervising resident) or attending/subintern (fourth-year medical student) teams have been developed at some institutions.9 Although allowing for additional exposure to learners, these models require a more hands-on approach than traditional teaching teams, particularly at the start of the academic year. Finally, as hospitalist teams have grown to include advanced practice providers (APPs), some programs have established formal teaching programs to address professional development needs of these healthcare professionals.10,11
DEVELOPING HOSPITALIST EDUCATORS
How do we help junior faculty who have the potential to be talented educators succeed in teaching when they have limited opportunities to engage with residents on clinical services? One approach is to encourage hospitalists to participate in resident didactic sessions such as “morning report” and noon conference. Another approach is to focus on teaching other learners. For example, several academic medical centers provide opportunities for hospitalists to engage in student teaching, either on the wards or via classroom instruction. In addition, as mentioned previously, APPs who are new to hospital medicine are an engaged audience and represent an opportunity for hospitalist educators to utilize and hone their teaching skills. Finally, organizing lectures for nursing colleagues is another way for the faculty to practice “chalk talks” and develop teaching portfolios.
Hospitalists can also leverage their expertise to build systems in which academic hospitalists are teaching each other, creating a culture of continuous learning. These activities may include case conferences, morbidity and mortality conferences, journal clubs, clinical topic updates developed by and for hospitalists, simulation exercises, and other group learning sessions. Giving hospitalists the opportunity to teach each other allows for professional growth that is not dependent on the presence of traditional learners.
REDEFINING ACADEMIC HOSPITALISTS
Philosophically, a key question is “What makes ‘academic’ academic?” Traditionally, academic hospitalist positions were synonymous with resident teaching or, for a small number of academic hospitalists, significant funded research. In an era where teaching residents may no longer be part of the job description for many hospitalists at academic medical centers, what distinguishes these positions from 100% clinical positions and what are the implications for academic hospital medicine?
Although data regarding why hospitalists seek “nonteaching” positions at academic medical centers are lacking, we believe that these jobs remain popular due to opportunities that are perceived to be unique to academic medical centers. These include more flexible scheduling (academic programs may be less likely to have seven-on/seven-off schedules), exposure to research and cutting-edge technology, opportunities to care for tertiary and quaternary care patients, collaboration with academic peers and experts in the field, and interaction with a range of learners, including medical, pharmacy, advanced practitioner, and other students.
Understanding the motivation of candidates who apply for academic hospital medicine positions—aside from supervising/teaching residents—will be an important goal for academic hospitalist leaders to ensure future success in staffing growing programs and creating sustainable academic hospitalist careers. As resident teaching time decreases, implementing robust faculty or professional development programs to address the broader interests and needs of academic hospitalist faculty will be increasingly important. Sehgal et al. described one such program for faculty development,12 and a more recent paper outlines a faculty development program focused on quality improvement and patient safety.13 These types of programs provide opportunities for academic hospitalists to engage in academic pursuits that are independent of residency programs.
CONCLUSION
Therefore, what do we tell the eager faculty applicant? First, we should not hide from the honest answer, ie, new faculty may not get as much resident teaching time as they would like or expect. Although we want hospitalists to maintain integral involvement in residency training programs, we also want to build a culture of clinical excellence, scholarship, and continuous learning that is not dependent on directly teaching residents. We should highlight the unique opportunities of academic hospital medicine, including teaching other learners, caring for tertiary/quaternary care patients, working with colleagues who are leaders in their field, and engaging in research and quality improvement work. By capitalizing on these opportunities, we can actively redefine what makes “academic” academic and ensure that we sustain academic hospital medicine as a desirable and rewarding career.
Disclosures
The authors have nothing to disclose.
1. Wachter RM, Goldman L. Zero to 50,000-the 20th anniversary of the hospitalist. N Engl J Med 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
2. Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392-393. https://doi.org/10.1111/j.1525-1497.2004.42002.x.
3. Flanders SA, Saint S, McMahon LF, Howell JD. Where should hospitalists sit within the academic medical center? J Gen Intern Med. 2008;23(8):1269-1272. https://doi.org/10.1007/s11606-008-0682-1.
4. 5 Hospital projects announced this year worth $1B or more. ASC Communications, 2019. https://www.beckershospitalreview.com/facilities-management/5-hospital-projects-announced-this-year-worth-1b-or-more.html. Accessed August 24, 2019.
5. White A, Anders J, Anoff DL, Creamer J, Flores LA. Table 3.45 Distribution of work in academic hmgs. Philadelphia, PA: Society of Hospital Medicine; 201 8.
6. Hunt D, Burger A, Harrison R, Southern W, Boonyasai RT, Leykum L. Hospitalist staffing: To split or not to split? SGIM Forum 2013;36:6.
7. Farnan JM, Burger A, Boonyasai RT, et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521-523. https://doi.org/10.1002/jhm.1961.
8. Sani SN, Wistar E, Le L, Chia D, Haber LA. Shining a light on overnight education: Hospitalist and resident impressions of the current state, barriers, and methods for improvement. Cureus 2018;10:e2939. https://doi.org/10.7759/cureus.2939.
9. O’Leary KJ, Chadha V, Fleming VM, Martin GJ, Baker DW. Medical subinternship: student experience on a resident uncovered hospitalist service. Teach Learn Med. 2008;20(1):18-21. https://doi.org/10.1080/10401330701797974.
10. Klimpl D, Franco T, Tackett S, et al. The current state of advanced practice provider fellowships in hospital medicine: A survey of program directors. J Hosp Med. 2019;14(7):401-406. https://doi.org/10.12788/jhm.3191.
11. Lackner C, Eid S, Panek T, Kisuule F. An advanced practice provider clinical fellowship as a pipeline to staffing a hospitalist program. J Hosp Med. 2019;14(6):336-339. https://doi.org/10.12788/jhm.3183.
12. Sehgal NL, Sharpe BA, Auerbach AA et al. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845.
13. van Schaik SM, Chang A, Fogh S, et al. Jumpstarting faculty development in quality improvement and patient safety education: A team-based approach. Acad Med. 2019.
1. Wachter RM, Goldman L. Zero to 50,000-the 20th anniversary of the hospitalist. N Engl J Med 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
2. Saint S, Flanders SA. Hospitalists in teaching hospitals: opportunities but not without danger. J Gen Intern Med. 2004;19(4):392-393. https://doi.org/10.1111/j.1525-1497.2004.42002.x.
3. Flanders SA, Saint S, McMahon LF, Howell JD. Where should hospitalists sit within the academic medical center? J Gen Intern Med. 2008;23(8):1269-1272. https://doi.org/10.1007/s11606-008-0682-1.
4. 5 Hospital projects announced this year worth $1B or more. ASC Communications, 2019. https://www.beckershospitalreview.com/facilities-management/5-hospital-projects-announced-this-year-worth-1b-or-more.html. Accessed August 24, 2019.
5. White A, Anders J, Anoff DL, Creamer J, Flores LA. Table 3.45 Distribution of work in academic hmgs. Philadelphia, PA: Society of Hospital Medicine; 201 8.
6. Hunt D, Burger A, Harrison R, Southern W, Boonyasai RT, Leykum L. Hospitalist staffing: To split or not to split? SGIM Forum 2013;36:6.
7. Farnan JM, Burger A, Boonyasai RT, et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521-523. https://doi.org/10.1002/jhm.1961.
8. Sani SN, Wistar E, Le L, Chia D, Haber LA. Shining a light on overnight education: Hospitalist and resident impressions of the current state, barriers, and methods for improvement. Cureus 2018;10:e2939. https://doi.org/10.7759/cureus.2939.
9. O’Leary KJ, Chadha V, Fleming VM, Martin GJ, Baker DW. Medical subinternship: student experience on a resident uncovered hospitalist service. Teach Learn Med. 2008;20(1):18-21. https://doi.org/10.1080/10401330701797974.
10. Klimpl D, Franco T, Tackett S, et al. The current state of advanced practice provider fellowships in hospital medicine: A survey of program directors. J Hosp Med. 2019;14(7):401-406. https://doi.org/10.12788/jhm.3191.
11. Lackner C, Eid S, Panek T, Kisuule F. An advanced practice provider clinical fellowship as a pipeline to staffing a hospitalist program. J Hosp Med. 2019;14(6):336-339. https://doi.org/10.12788/jhm.3183.
12. Sehgal NL, Sharpe BA, Auerbach AA et al. Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161-166. https://doi.org/10.1002/jhm.845.
13. van Schaik SM, Chang A, Fogh S, et al. Jumpstarting faculty development in quality improvement and patient safety education: A team-based approach. Acad Med. 2019.
© 2020 Society of Hospital Medicine
Integrated Fragility Hip Fracture Program: A Model for High Quality Care
Hip fractures are a significant cause of morbidity and mortality among elderly patients. Patients with fragility hip fractures often carry multiple comorbid diagnoses with a significant risk of perioperative complications. After hip fracture, 30-day mortality has been reported as 3.3% to 17.2% with one-year mortality as high as 50%.1
Multidisciplinary care,2-5 surgery within 24 hours (h),6-12 use of regional peripheral nerve blocks,13-16 restrictive blood transfusion strategies,17,18 tranexamic acid (TXA) use,19 pharmacologic deep venous thrombosis (DVT) prophylaxis,20 surgical site infection prevention protocols,21 early mobilization,22 and nutritional optimization23-25 have been individually shown to improve outcomes in hip fracture patients.
Our program sought to define, standardize, and implement evidence-based best practices to improve clinical care and outcomes of patients with hip fractures. We convened a Center for Musculoskeletal Care (CMC) Hip Fracture Oversight Group that included surgeons and advanced practice providers from Orthopedics; physicians from Internal Medicine Hospitalist, Geriatrics, Emergency Medicine, and Anesthesia; and representatives from rehabilitation services, nursing, care management, pharmacy, and performance improvement. With clinical input from all involved services, we developed evidence-based protocols to standardize the care of patients with fragility hip fractures from the time of the patient’s evaluation in the emergency room to discharge and outpatient rehabilitation. The program was operationalized in February 2016.
This project was considered by the Yale University institutional review board (IRB) to be a quality improvement and, therefore, exempted from IRB approval.
MATERIALS AND METHODS
Yale-New Haven Hospital is composed of two main campuses. The York Street Campus (YSC) is the Level 1 Trauma Center. The St. Raphael’s Campus (SRC) houses the CMC nursing units for elective lower extremity arthroplasty and spine procedures. Prior to 2016, patients with hip fractures were cared for equally at both Yale-New Haven Hospital campuses. Patients were admitted to both medical and surgical services with no standardization of hip fracture care processes. Surgeons were assigned based on availability. Frequently, patients were added on to the operating room (OR) schedule and did not undergo surgery until off-hours and after a prolonged waiting period.
Medical comanagement of patients with fragility hip fractures at our institution predated the start of our CMC Integrated Fragility Hip Fracture Program (IFHFP). Comanagement was instituted in 2012 at YSC and in 2014 at SRC but without standardized protocols. The IFHFP began in February 2016 with the centralization of all patients with fragility hip fractures to the SRC at Yale-New Haven Hospital. Emergency medical services directed patients with suspected hip fractures to the designated campus. A dedicated hip fracture OR was allocated daily with a hip fracture surgeon assigned by a shared community and faculty surgeon call schedule. Patients were encouraged but not required to accept care from the on-call hip fracture surgical attending. Anesthesia was notified of the arrival of a patient with a hip fracture in the emergency department, and if the patient consented and qualified, a single-shot femoral nerve block was performed. Patients were screened for nasal staphylococcal colonization and treated with povidone-iodine nasal decolonization, chlorhexidine wash, and antibiotics determined by staphylococcal status and type of surgical procedure planned. Preoperative and postoperative order sets were implemented that dictated the care processes as outlined in Table 1. Surgeons determined the choice of operative intervention as per usual; this included internal fixation and partial or total hip replacement. Detailed medical and surgical protocols are included in Appendix A.
Since the initiation of the IFHFP on February 1, 2016, the program has continued to advance with our experience. We used the year preceding the start of the program as our baseline year (January 1, 2015, through December 31, 2015). The following years, 2016 and 2017, were a transition time during which our protocols were implemented. The intervention year was defined as January 1, 2018, through December 31, 2018. The outcomes during the intervention year were compared with the baseline year. It is important to note that our program has been in continuous evolution, including during the intervention year, with protocols created and refined as we gain experience.
Outcomes include 30-day mortality, transfusions, adverse effects of drugs, venous thromboembolic complications, sepsis, myocardial infarction, mechanical surgical fixation complications, length of stay, 30-day readmission rate, unexpected return to the OR, and time to operative intervention. Definitions of the outcome variables are reviewed in Appendix B.
RESULTS
There were 275 consecutive patients with hip fractures admitted to SRC in the baseline year (January 1, 2015 to December 31, 2015) and 434 patients with hip fractures admitted in the intervention year (January 1, 2018, to December 31, 2018) after consolidation of the program to the single Yale-New Haven Campus and implementation of standardized care processes. Patient demographic data including age, sex, ethnicity, body mass index, and American Society of Anesthesiologists physical status classification were evaluated for the baseline year and intervention year and reported in Table 2. There were no differences in the demographics of patients between baseline and intervention years.
From baseline year to intervention year, 30-day mortality, transfusion, adverse effects of drugs, length of stay, unexpected return to OR, and time to OR were all significantly reduced. Mortality within 30 days decreased from 8.0% to 2.8%. The results are displayed in Table 3. No significant difference was seen in the incidence of venous thromboembolism, sepsis, myocardial infarctions, readmission at 30 days, or mechanical surgical fixation complications.
The Figure shows the 30-day IFHFP mortality rate as reported on a monthly basis starting on January 1 of the baseline year, 2015, and continuing through December 31 of the intervention year, 2018. The process interventions are mapped according to the date of initiation. The median mortality rate (including all data from January 1, 2015, to December 31, 2018) is demonstrated as the dotted line. From May 2018 to December 2018, each monthly mortality rate was recorded below the four-year median, a visual demonstration of the statistical significance seen in our mortality reduction from 8.0% in the baseline year to 2.8% in the intervention year.
DISCUSSION
Patients with fragility hip fractures are a medically complex and vulnerable population. The goal of the CMC IFHFP was to standardize the care of these high-risk patients in an effort to reduce time to the OR, perioperative medical complications, time spent in the hospital, and ultimately mortality.
The barriers to implementing coordinated, multidisciplinary care are significant. In our case, we had a fragmented care model with fragility hip fracture patients cared for at two campuses, on different nursing units, with both community and faculty surgeons providing operative care, and with no predesignated primary team. We structured our program for equal sharing of call between community and faculty surgeons. However, there was distrust among the physician groups: Primary care physicians were concerned that their referral lines with orthopedic surgical colleagues would be fractured by the new shared call. Surgeons doubted that patients would be distributed equally among community and faculty practices. Hospitalists feared that comanagement would mean surgeons abdicating responsibility for care. Surgeons worried that routine medical involvement would delay surgery and prolong the length of stay with excessive testing. In order to achieve consensus, address concerns, and allay fears, we engaged the primary care and surgeon leadership for their support at the onset of the program and held monthly large group meetings and many smaller sessions to advance objectives. We meticulously tracked data and frequently reported out to the involved groups.
As it is well established that operative intervention on a hip fracture is best completed within 24 h to optimize a patient’s clinical outcomes, critical interventions were the designation of a hip fracture OR starting midday and expectation that surgery be performed the day after admission for medically cleared patients. Surgeons were able to book elective cases or outpatient clinic time in the morning. The morning hours prior to surgery allowed time for any final medical optimization, preoperative nursing care, and family discussions. Most surgeries were then completed by the primary OR staff during standard operating hours. Patients were out of the postanesthesia care unit and settled back on the orthopedic nursing unit in the early evening without a prolonged period of nil per os, bed rest, or sleep interruption.
While our protocol expected surgery the day after admission for medically cleared patients, we used surgery within 24 h as a simple metric to compare baseline with intervention outcomes. With our hip fracture OR block time beginning midday, the majority of our medically cleared hip fracture patients would receive surgical treatment within 24 h of admission. Our data show a significant improvement in timeliness of surgical intervention from 41.8% of patients to the OR within 24 h in 2015 to 55% in 2018. In 2017, we conducted an interval four-month audit involving a detailed chart review of all patients for whom surgery was delayed beyond 24 h from hospital admission. Chart review identified anticoagulation as the primary reason for surgical delay. Of patients who were eligible for surgery (medically stabilized and not therapeutically anticoagulated), 90% underwent surgery within 24 h during this four-month period in 2017. This compares to an overall rate of surgery within 24 h of 57% during the calendar year 2017. We did not perform a subgroup analysis of outcomes in patients with time to OR of 24-36 h. From this study, we are therefore unable to draw any conclusion regarding time to surgery and mortality.
Our dedicated OR hip fracture block time was changed from 7:30
Transfusion rate reduction from 46.6% to 28.1% was achieved primarily by the implementation and strict enforcement of a policy to avoid transfusing asymptomatic patients with hemoglobin >7.0 g/dL. In addition, we recommended TXA using standard perioperative arthroplasty dosing of 1 g intravenously (IV) at the time of incision followed by 1 g IV 3 h later in the postanaesthesia care unit. However, adherence to TXA recommendations was poor. A year-long audit (February 2017 to February 2018) demonstrated that only 29% of patients undergoing hip fracture surgery received the recommended TXA. After the conclusion of the study period of this review, we revised our TXA protocol to include an infusion at the time of admission and subsequent perioperative doses. The expanded TXA protocol (with clear exclusion criteria) has been “hard-wired” into our electronic perioperative order sets. We are tracking TXA compliance on a weekly basis. We anticipate that earlier TXA administration and improved compliance will further reduce transfusion rates.
We reduced the adverse effects of medications with two initiatives: First, dedicated hip fracture order sets with medications selected and dosed specifically for the geriatric population were launched at the onset of the IFHFP in 2016. Second, in coordination with our regional anesthesia team, patients who met criteria underwent a single-shot femoral nerve block upon diagnosis of the hip fracture. Patients reported up to 24 h of nonnarcotic pain relief with the femoral nerve block.
Prior to the introduction of the IFHFP, surgeons determined DVT prophylaxis based on their personal preference. Many of our surgeons were concerned that standardizing DVT prophylaxis to enoxaparin would increase the risk of surgical site bleeding, hematoma, infection, and reoperation. With data tracking and periodic reporting, we were able to reassure our surgeons: We demonstrated a reduction in the rate of patients unexpectedly requiring a return to the OR from 5.1% in 2015 to 0% in 2018.
We did not find a significant difference in mechanical complications due to surgical fixation during the index admission. Most mechanical complications do not present within the index admission and, therefore, would not be identified by this metric. Furthermore, in this phase of the program, we did not seek to change or standardize intraoperative surgical processes outside of surgical site infection prevention measures. Surgical technical quality and variation among surgeons is an area of ongoing evaluation within our program. We have begun a surgical quality review process with an expert review of postoperative radiography, beginning with fixation of nondisplaced femoral neck fractures, feedback to surgeons, and tracking of mechanical complications beyond the index admission. The surgical quality outcomes will be presented in a future manuscript.
Anticoagulation use is common in patients with hip fractures because of the high prevalence of comorbid conditions such as atrial fibrillation and venous thromboembolic disease. Direct oral anticoagulants (DOACs) are now commonly used in place of the vitamin K antagonist, warfarin. Our inability to efficiently reverse the DOACs compounded by surgeon unfamiliarity with these agents led to extreme caution in the timing of OR, with most patients delayed a full 48 h from the last dose of their prescribed DOAC. After recognizing the impact of anticoagulation on the timing of surgery, we convened a multidisciplinary group to determine rational guidelines for the timing of surgery in patients on chronic anticoagulation based on the bleeding risk of the planned operative procedure. These guidelines were instituted in December 2018, so their impact is not reflected in this review.
Our results showing a reduction in length of stay and mortality cannot be explained by any one intervention. We propose that the standardization of all processes and protocols, the establishment of clear expectations among all the medical and nursing personnel, and the shorter time spent waiting for surgery all contributed to the length of stay reduction. Likewise, the decrease in time to OR, reduction in time spent in the hospital, fewer transfusions, adverse effects of medication, and surgical complications requiring a return to the OR have all likely contributed to the significant reduction in mortality. The efforts of the orthopedic nursing team certainly contributed: The CMC nurses led the efforts to standardize surgical site infection bundle care, reduce indwelling bladder catheter use, and together with physical therapy, mobilize patients out of bed for meals postoperatively. The strong focus on teamwork, data tracking, feedback and accountability, and the desire for continued improvement may have been the strongest drivers in this program’s success.
Our results showed a nonsignificant increase in 30-day readmission from 9.1% to 12.5%. One limitation of this study is that we did not track specific readmission diagnoses to better understand trends in diagnoses or indications for hospital readmission. Going forward, we are reviewing readmissions to better understand opportunities to improve our inpatient processes and transitions of care.
This an evolving project. We have expanded our use of TXA in an effort to further reduce transfusion rates. We have adjusted our protocols for patients admitted on DOACs and warfarin to allow more rapid surgical intervention. We have initiated a surgical quality review process in which surgical fixation is reviewed with timely feedback to the operating surgeon. We are working closely with the skilled nursing facilities to extend our rehabilitation and nursing care protocols beyond the acute care setting. We are measuring patient engagement with a brief discharge survey specific to the CMC IFHFP. We continue to seek feedback from our referring primary care physicians to improve communication at times of care transition.
One of the limitations of a quality improvement project such as this one is the inability to identify the effect of each individual intervention. We can conclude that the totality of the multidisciplinary project reduced mortality in our hip fracture population, but we cannot report the relative effect of each process change. Another center seeking to replicate this success cannot determine from this research how to prioritize their resources to achieve a similar outcome.
How we care for the fragility hip fracture patient after hospital discharge is critical and unaddressed in this current study. A limitation of our current program is the lack of consistent postdischarge bone health management—which we are working to address. Also related to postdischarge management, we have partnered with a network of preferred skilled nursing facilities to standardize the care and decrease the length of stay. These data will be published separately.
We understand that our experience at the CMC is unique and specific to our care environment. This is a single site study and may not be generalizable to other centers. Nonetheless, the principles of multidisciplinary care, evidence-based protocol development, technological integration of protocols through order sets, and data tracking with feedback and accountability are the essential elements of our success that can be generalized to other institutions.
CONCLUSIONS
The CMC at Yale School of Medicine and Yale-New Haven Hospital IFHFP provides a model for implementing well-documented evidence-based interventions to standardize the care of patients with fragility hip fractures. The IFHFP yielded reduced mortality, length of stay, blood transfusion utilization, adverse effects of medications, unexpected return to the OR, and time to the OR.
Acknowledgments
The authors thank the work of the Center for Musculoskeletal Care Hip Fracture Oversight Group, program surgeons, and community primary care leaders: Olukemi Akande, MD, Mark Altman, MD, Diren Arsoy, MD, John Aversa, MD, Michael Connair, MD, Leo Cooney, MD, Kenneth Donohue, MD, David Gibson, MD, Gail Haesche, RN, MS, ACM-RN, Carol Just, MSN, NEA-BC, RN, Patricia Kenyon, RN, ACM, Francis Lee MD, Michael Leslie, MD, Michael Lucchini, MD, Christopher Lynch, MD, Rowland Mayor, MD, Tara Messina, PT, Lorraine Novella, RN, Paul Oliver, PA-C, Vivek Parwani, MD, Joseph Quaranta, MD, Lee Rubin, MD, Derek Shia, MD, Jeff Sumner, MD, John Tarutis, Arya Varthi, MD, Anuruddha Walaliyadda, MD, Daniel Wiznia, MD, Shirvinda Wijesekera, MD, Joseph Wu, MD, Brad Yoo, MD, and James Yue, MD.
1. Abrahamsen B, van Staa T, Ariely M, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiologic review. Osteoporos Int. 2009;20(10):1633-1650. https://doi.org/10.1007/s00198-009-0920-3.
2. DellaRocca GJ, Moylan KC, Crist BD, Volgas DA, Stannard JP, Mehr DR. Comanagement of geriatric patients with hip fractures: a retrospective, controlled cohort study. Geriatr Orthop Surg Rehabil. 2013;4(1):10-15. https://doi.org/10.1177/2151458513495238.
3. Wang Y, Tang J, Zhou F, Yang L, Wu J. Comprehensive geriatric care reduces acute perioperative delirium in elderly patients with hip fractures: a meta-analysis. Medicine. 2017; 96(26): e7361. https://doi.org/10.1097/MD.0000000000007361.
4. Liu VX, Rosas E, Hwang J, et al. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017;152(7):e171032. https://doi.org/10.1001/jamasurg.2017.1032.
5. Taraldsen K, Sletvold O, Thingstad P, et al. Physical behavior and function early after hip fracture surgery in patients receiving geriatric care or orthopedic care—a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69(3):338-345. https://doi.org/10.1093/gerona/glt097.
6. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson Jl. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702-709. https://doi.org/10.1016/s0002-9343(02)01119-1.
7. Hamlet WP, Lieberman JR, Freedman EL, Dorey FJ, Fletcher A, Johnson EE. Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop. 1997;26(9):621-627.
8. Hoenig H, Rubenstein LV, Sloane R, Honer R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157(5):513-520.
9. Orosz GM, Magaziner J, Hannan El, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743. https://doi.org/10.1001/jama.291.14.1738.
10. Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004:124(5):334-340. https://doi.org/10.1007/s00402-004-0662-9.
11. Doruk H, Mas MR, Yidiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179-185.https://doi.org/10.1016/j.archger.2004.03.004.
12. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-729. https://doi.org/10.1016/j.injury.2012.08.025.
13. Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;5: CD001159. https://doi.org/10.1002/14651858.CD001159.pub2.
14. Morrison RS, Dickman E, Hwang U, et al. Regional nerve blocks improve pain and functional outcomes in hip fracture: a randomized controlled trial. J Am Geriatr Soc. 2016;64(12):2433-2439. https://doi.org/10.1111/jgs.14386.
15. Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency deparment patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584-591. https://doi.org/10.1111/acem.12154.
16. Dickman E, Pushkar I, Likourezos A, et al. Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. Am J Emerg Med. 2016;34(3):586-589. https://doi.org/10.1016/j.ajem.2015.12.016.
17. Carson JL, Terrin MI, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453-2462. https://doi.org/10.1056/NEJMoa1012452.
18. Garcia-Alvarez F, Al-Ghanem R, García-Alvarez I, López-Baisson A, Bernal M. Risk factors for postoperative infections in patients with hip fracture treated by means of Thompson arthoplasty. Arch Gerontol Geriatr. 2010; 50(1):51-55. https://doi.org/10.1016/j.archger.2009.01.009.
19. Farrow LS, Smith TO, Ashcroft GP, Myint PK. A systematic review of tranexamic acid in hip fracture surgery. Br J Clin Pharmacol. 2016;82(6):1458-1470. https://doi.org/10.1111/bcp.13079.
20. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e278S-e325S. https://doi.org/10.1378/chest.11-2404.
21. Gillespie WJ, Walenkamp G. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev. 2010;(3):CD000244. https://doi.org/10.1002/14651858.CD000244.pub2.
22. Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG. Time to ambulation after hip fracture surgery: relation to hospitalization outcomes. J Gerontol A Biol Sci Med Sci. 2003;58(11):1042-1045. https://doi.org/10.1093/gerona/58.11.m1042.
23. Foster MR, Heppenstall RB, Friedenberg ZB, Hozack WJ. A prospective assessment of nutritional status and complications in patients with fractures of the hip. J Orthop Trauma. 1990;4(1):49-57. https://doi.org/10.1097/00005131-199003000-00009.
24. Bell JJ, Pulle RC, Crouch AM, Kuys SS, Ferrier RL, Whitehouse SL. Impact of malnutrition on 12-month mortality following acute hip fracture. ANZ J Surg. 2016;86(3):157-161. https://doi.org/10.1111/ans.13429.
25. Avenell A, Handoll HH. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. 2010;(1):CD001880. https://doi.org/10.1002/14651858.CD001880.pub5.
Hip fractures are a significant cause of morbidity and mortality among elderly patients. Patients with fragility hip fractures often carry multiple comorbid diagnoses with a significant risk of perioperative complications. After hip fracture, 30-day mortality has been reported as 3.3% to 17.2% with one-year mortality as high as 50%.1
Multidisciplinary care,2-5 surgery within 24 hours (h),6-12 use of regional peripheral nerve blocks,13-16 restrictive blood transfusion strategies,17,18 tranexamic acid (TXA) use,19 pharmacologic deep venous thrombosis (DVT) prophylaxis,20 surgical site infection prevention protocols,21 early mobilization,22 and nutritional optimization23-25 have been individually shown to improve outcomes in hip fracture patients.
Our program sought to define, standardize, and implement evidence-based best practices to improve clinical care and outcomes of patients with hip fractures. We convened a Center for Musculoskeletal Care (CMC) Hip Fracture Oversight Group that included surgeons and advanced practice providers from Orthopedics; physicians from Internal Medicine Hospitalist, Geriatrics, Emergency Medicine, and Anesthesia; and representatives from rehabilitation services, nursing, care management, pharmacy, and performance improvement. With clinical input from all involved services, we developed evidence-based protocols to standardize the care of patients with fragility hip fractures from the time of the patient’s evaluation in the emergency room to discharge and outpatient rehabilitation. The program was operationalized in February 2016.
This project was considered by the Yale University institutional review board (IRB) to be a quality improvement and, therefore, exempted from IRB approval.
MATERIALS AND METHODS
Yale-New Haven Hospital is composed of two main campuses. The York Street Campus (YSC) is the Level 1 Trauma Center. The St. Raphael’s Campus (SRC) houses the CMC nursing units for elective lower extremity arthroplasty and spine procedures. Prior to 2016, patients with hip fractures were cared for equally at both Yale-New Haven Hospital campuses. Patients were admitted to both medical and surgical services with no standardization of hip fracture care processes. Surgeons were assigned based on availability. Frequently, patients were added on to the operating room (OR) schedule and did not undergo surgery until off-hours and after a prolonged waiting period.
Medical comanagement of patients with fragility hip fractures at our institution predated the start of our CMC Integrated Fragility Hip Fracture Program (IFHFP). Comanagement was instituted in 2012 at YSC and in 2014 at SRC but without standardized protocols. The IFHFP began in February 2016 with the centralization of all patients with fragility hip fractures to the SRC at Yale-New Haven Hospital. Emergency medical services directed patients with suspected hip fractures to the designated campus. A dedicated hip fracture OR was allocated daily with a hip fracture surgeon assigned by a shared community and faculty surgeon call schedule. Patients were encouraged but not required to accept care from the on-call hip fracture surgical attending. Anesthesia was notified of the arrival of a patient with a hip fracture in the emergency department, and if the patient consented and qualified, a single-shot femoral nerve block was performed. Patients were screened for nasal staphylococcal colonization and treated with povidone-iodine nasal decolonization, chlorhexidine wash, and antibiotics determined by staphylococcal status and type of surgical procedure planned. Preoperative and postoperative order sets were implemented that dictated the care processes as outlined in Table 1. Surgeons determined the choice of operative intervention as per usual; this included internal fixation and partial or total hip replacement. Detailed medical and surgical protocols are included in Appendix A.
Since the initiation of the IFHFP on February 1, 2016, the program has continued to advance with our experience. We used the year preceding the start of the program as our baseline year (January 1, 2015, through December 31, 2015). The following years, 2016 and 2017, were a transition time during which our protocols were implemented. The intervention year was defined as January 1, 2018, through December 31, 2018. The outcomes during the intervention year were compared with the baseline year. It is important to note that our program has been in continuous evolution, including during the intervention year, with protocols created and refined as we gain experience.
Outcomes include 30-day mortality, transfusions, adverse effects of drugs, venous thromboembolic complications, sepsis, myocardial infarction, mechanical surgical fixation complications, length of stay, 30-day readmission rate, unexpected return to the OR, and time to operative intervention. Definitions of the outcome variables are reviewed in Appendix B.
RESULTS
There were 275 consecutive patients with hip fractures admitted to SRC in the baseline year (January 1, 2015 to December 31, 2015) and 434 patients with hip fractures admitted in the intervention year (January 1, 2018, to December 31, 2018) after consolidation of the program to the single Yale-New Haven Campus and implementation of standardized care processes. Patient demographic data including age, sex, ethnicity, body mass index, and American Society of Anesthesiologists physical status classification were evaluated for the baseline year and intervention year and reported in Table 2. There were no differences in the demographics of patients between baseline and intervention years.
From baseline year to intervention year, 30-day mortality, transfusion, adverse effects of drugs, length of stay, unexpected return to OR, and time to OR were all significantly reduced. Mortality within 30 days decreased from 8.0% to 2.8%. The results are displayed in Table 3. No significant difference was seen in the incidence of venous thromboembolism, sepsis, myocardial infarctions, readmission at 30 days, or mechanical surgical fixation complications.
The Figure shows the 30-day IFHFP mortality rate as reported on a monthly basis starting on January 1 of the baseline year, 2015, and continuing through December 31 of the intervention year, 2018. The process interventions are mapped according to the date of initiation. The median mortality rate (including all data from January 1, 2015, to December 31, 2018) is demonstrated as the dotted line. From May 2018 to December 2018, each monthly mortality rate was recorded below the four-year median, a visual demonstration of the statistical significance seen in our mortality reduction from 8.0% in the baseline year to 2.8% in the intervention year.
DISCUSSION
Patients with fragility hip fractures are a medically complex and vulnerable population. The goal of the CMC IFHFP was to standardize the care of these high-risk patients in an effort to reduce time to the OR, perioperative medical complications, time spent in the hospital, and ultimately mortality.
The barriers to implementing coordinated, multidisciplinary care are significant. In our case, we had a fragmented care model with fragility hip fracture patients cared for at two campuses, on different nursing units, with both community and faculty surgeons providing operative care, and with no predesignated primary team. We structured our program for equal sharing of call between community and faculty surgeons. However, there was distrust among the physician groups: Primary care physicians were concerned that their referral lines with orthopedic surgical colleagues would be fractured by the new shared call. Surgeons doubted that patients would be distributed equally among community and faculty practices. Hospitalists feared that comanagement would mean surgeons abdicating responsibility for care. Surgeons worried that routine medical involvement would delay surgery and prolong the length of stay with excessive testing. In order to achieve consensus, address concerns, and allay fears, we engaged the primary care and surgeon leadership for their support at the onset of the program and held monthly large group meetings and many smaller sessions to advance objectives. We meticulously tracked data and frequently reported out to the involved groups.
As it is well established that operative intervention on a hip fracture is best completed within 24 h to optimize a patient’s clinical outcomes, critical interventions were the designation of a hip fracture OR starting midday and expectation that surgery be performed the day after admission for medically cleared patients. Surgeons were able to book elective cases or outpatient clinic time in the morning. The morning hours prior to surgery allowed time for any final medical optimization, preoperative nursing care, and family discussions. Most surgeries were then completed by the primary OR staff during standard operating hours. Patients were out of the postanesthesia care unit and settled back on the orthopedic nursing unit in the early evening without a prolonged period of nil per os, bed rest, or sleep interruption.
While our protocol expected surgery the day after admission for medically cleared patients, we used surgery within 24 h as a simple metric to compare baseline with intervention outcomes. With our hip fracture OR block time beginning midday, the majority of our medically cleared hip fracture patients would receive surgical treatment within 24 h of admission. Our data show a significant improvement in timeliness of surgical intervention from 41.8% of patients to the OR within 24 h in 2015 to 55% in 2018. In 2017, we conducted an interval four-month audit involving a detailed chart review of all patients for whom surgery was delayed beyond 24 h from hospital admission. Chart review identified anticoagulation as the primary reason for surgical delay. Of patients who were eligible for surgery (medically stabilized and not therapeutically anticoagulated), 90% underwent surgery within 24 h during this four-month period in 2017. This compares to an overall rate of surgery within 24 h of 57% during the calendar year 2017. We did not perform a subgroup analysis of outcomes in patients with time to OR of 24-36 h. From this study, we are therefore unable to draw any conclusion regarding time to surgery and mortality.
Our dedicated OR hip fracture block time was changed from 7:30
Transfusion rate reduction from 46.6% to 28.1% was achieved primarily by the implementation and strict enforcement of a policy to avoid transfusing asymptomatic patients with hemoglobin >7.0 g/dL. In addition, we recommended TXA using standard perioperative arthroplasty dosing of 1 g intravenously (IV) at the time of incision followed by 1 g IV 3 h later in the postanaesthesia care unit. However, adherence to TXA recommendations was poor. A year-long audit (February 2017 to February 2018) demonstrated that only 29% of patients undergoing hip fracture surgery received the recommended TXA. After the conclusion of the study period of this review, we revised our TXA protocol to include an infusion at the time of admission and subsequent perioperative doses. The expanded TXA protocol (with clear exclusion criteria) has been “hard-wired” into our electronic perioperative order sets. We are tracking TXA compliance on a weekly basis. We anticipate that earlier TXA administration and improved compliance will further reduce transfusion rates.
We reduced the adverse effects of medications with two initiatives: First, dedicated hip fracture order sets with medications selected and dosed specifically for the geriatric population were launched at the onset of the IFHFP in 2016. Second, in coordination with our regional anesthesia team, patients who met criteria underwent a single-shot femoral nerve block upon diagnosis of the hip fracture. Patients reported up to 24 h of nonnarcotic pain relief with the femoral nerve block.
Prior to the introduction of the IFHFP, surgeons determined DVT prophylaxis based on their personal preference. Many of our surgeons were concerned that standardizing DVT prophylaxis to enoxaparin would increase the risk of surgical site bleeding, hematoma, infection, and reoperation. With data tracking and periodic reporting, we were able to reassure our surgeons: We demonstrated a reduction in the rate of patients unexpectedly requiring a return to the OR from 5.1% in 2015 to 0% in 2018.
We did not find a significant difference in mechanical complications due to surgical fixation during the index admission. Most mechanical complications do not present within the index admission and, therefore, would not be identified by this metric. Furthermore, in this phase of the program, we did not seek to change or standardize intraoperative surgical processes outside of surgical site infection prevention measures. Surgical technical quality and variation among surgeons is an area of ongoing evaluation within our program. We have begun a surgical quality review process with an expert review of postoperative radiography, beginning with fixation of nondisplaced femoral neck fractures, feedback to surgeons, and tracking of mechanical complications beyond the index admission. The surgical quality outcomes will be presented in a future manuscript.
Anticoagulation use is common in patients with hip fractures because of the high prevalence of comorbid conditions such as atrial fibrillation and venous thromboembolic disease. Direct oral anticoagulants (DOACs) are now commonly used in place of the vitamin K antagonist, warfarin. Our inability to efficiently reverse the DOACs compounded by surgeon unfamiliarity with these agents led to extreme caution in the timing of OR, with most patients delayed a full 48 h from the last dose of their prescribed DOAC. After recognizing the impact of anticoagulation on the timing of surgery, we convened a multidisciplinary group to determine rational guidelines for the timing of surgery in patients on chronic anticoagulation based on the bleeding risk of the planned operative procedure. These guidelines were instituted in December 2018, so their impact is not reflected in this review.
Our results showing a reduction in length of stay and mortality cannot be explained by any one intervention. We propose that the standardization of all processes and protocols, the establishment of clear expectations among all the medical and nursing personnel, and the shorter time spent waiting for surgery all contributed to the length of stay reduction. Likewise, the decrease in time to OR, reduction in time spent in the hospital, fewer transfusions, adverse effects of medication, and surgical complications requiring a return to the OR have all likely contributed to the significant reduction in mortality. The efforts of the orthopedic nursing team certainly contributed: The CMC nurses led the efforts to standardize surgical site infection bundle care, reduce indwelling bladder catheter use, and together with physical therapy, mobilize patients out of bed for meals postoperatively. The strong focus on teamwork, data tracking, feedback and accountability, and the desire for continued improvement may have been the strongest drivers in this program’s success.
Our results showed a nonsignificant increase in 30-day readmission from 9.1% to 12.5%. One limitation of this study is that we did not track specific readmission diagnoses to better understand trends in diagnoses or indications for hospital readmission. Going forward, we are reviewing readmissions to better understand opportunities to improve our inpatient processes and transitions of care.
This an evolving project. We have expanded our use of TXA in an effort to further reduce transfusion rates. We have adjusted our protocols for patients admitted on DOACs and warfarin to allow more rapid surgical intervention. We have initiated a surgical quality review process in which surgical fixation is reviewed with timely feedback to the operating surgeon. We are working closely with the skilled nursing facilities to extend our rehabilitation and nursing care protocols beyond the acute care setting. We are measuring patient engagement with a brief discharge survey specific to the CMC IFHFP. We continue to seek feedback from our referring primary care physicians to improve communication at times of care transition.
One of the limitations of a quality improvement project such as this one is the inability to identify the effect of each individual intervention. We can conclude that the totality of the multidisciplinary project reduced mortality in our hip fracture population, but we cannot report the relative effect of each process change. Another center seeking to replicate this success cannot determine from this research how to prioritize their resources to achieve a similar outcome.
How we care for the fragility hip fracture patient after hospital discharge is critical and unaddressed in this current study. A limitation of our current program is the lack of consistent postdischarge bone health management—which we are working to address. Also related to postdischarge management, we have partnered with a network of preferred skilled nursing facilities to standardize the care and decrease the length of stay. These data will be published separately.
We understand that our experience at the CMC is unique and specific to our care environment. This is a single site study and may not be generalizable to other centers. Nonetheless, the principles of multidisciplinary care, evidence-based protocol development, technological integration of protocols through order sets, and data tracking with feedback and accountability are the essential elements of our success that can be generalized to other institutions.
CONCLUSIONS
The CMC at Yale School of Medicine and Yale-New Haven Hospital IFHFP provides a model for implementing well-documented evidence-based interventions to standardize the care of patients with fragility hip fractures. The IFHFP yielded reduced mortality, length of stay, blood transfusion utilization, adverse effects of medications, unexpected return to the OR, and time to the OR.
Acknowledgments
The authors thank the work of the Center for Musculoskeletal Care Hip Fracture Oversight Group, program surgeons, and community primary care leaders: Olukemi Akande, MD, Mark Altman, MD, Diren Arsoy, MD, John Aversa, MD, Michael Connair, MD, Leo Cooney, MD, Kenneth Donohue, MD, David Gibson, MD, Gail Haesche, RN, MS, ACM-RN, Carol Just, MSN, NEA-BC, RN, Patricia Kenyon, RN, ACM, Francis Lee MD, Michael Leslie, MD, Michael Lucchini, MD, Christopher Lynch, MD, Rowland Mayor, MD, Tara Messina, PT, Lorraine Novella, RN, Paul Oliver, PA-C, Vivek Parwani, MD, Joseph Quaranta, MD, Lee Rubin, MD, Derek Shia, MD, Jeff Sumner, MD, John Tarutis, Arya Varthi, MD, Anuruddha Walaliyadda, MD, Daniel Wiznia, MD, Shirvinda Wijesekera, MD, Joseph Wu, MD, Brad Yoo, MD, and James Yue, MD.
Hip fractures are a significant cause of morbidity and mortality among elderly patients. Patients with fragility hip fractures often carry multiple comorbid diagnoses with a significant risk of perioperative complications. After hip fracture, 30-day mortality has been reported as 3.3% to 17.2% with one-year mortality as high as 50%.1
Multidisciplinary care,2-5 surgery within 24 hours (h),6-12 use of regional peripheral nerve blocks,13-16 restrictive blood transfusion strategies,17,18 tranexamic acid (TXA) use,19 pharmacologic deep venous thrombosis (DVT) prophylaxis,20 surgical site infection prevention protocols,21 early mobilization,22 and nutritional optimization23-25 have been individually shown to improve outcomes in hip fracture patients.
Our program sought to define, standardize, and implement evidence-based best practices to improve clinical care and outcomes of patients with hip fractures. We convened a Center for Musculoskeletal Care (CMC) Hip Fracture Oversight Group that included surgeons and advanced practice providers from Orthopedics; physicians from Internal Medicine Hospitalist, Geriatrics, Emergency Medicine, and Anesthesia; and representatives from rehabilitation services, nursing, care management, pharmacy, and performance improvement. With clinical input from all involved services, we developed evidence-based protocols to standardize the care of patients with fragility hip fractures from the time of the patient’s evaluation in the emergency room to discharge and outpatient rehabilitation. The program was operationalized in February 2016.
This project was considered by the Yale University institutional review board (IRB) to be a quality improvement and, therefore, exempted from IRB approval.
MATERIALS AND METHODS
Yale-New Haven Hospital is composed of two main campuses. The York Street Campus (YSC) is the Level 1 Trauma Center. The St. Raphael’s Campus (SRC) houses the CMC nursing units for elective lower extremity arthroplasty and spine procedures. Prior to 2016, patients with hip fractures were cared for equally at both Yale-New Haven Hospital campuses. Patients were admitted to both medical and surgical services with no standardization of hip fracture care processes. Surgeons were assigned based on availability. Frequently, patients were added on to the operating room (OR) schedule and did not undergo surgery until off-hours and after a prolonged waiting period.
Medical comanagement of patients with fragility hip fractures at our institution predated the start of our CMC Integrated Fragility Hip Fracture Program (IFHFP). Comanagement was instituted in 2012 at YSC and in 2014 at SRC but without standardized protocols. The IFHFP began in February 2016 with the centralization of all patients with fragility hip fractures to the SRC at Yale-New Haven Hospital. Emergency medical services directed patients with suspected hip fractures to the designated campus. A dedicated hip fracture OR was allocated daily with a hip fracture surgeon assigned by a shared community and faculty surgeon call schedule. Patients were encouraged but not required to accept care from the on-call hip fracture surgical attending. Anesthesia was notified of the arrival of a patient with a hip fracture in the emergency department, and if the patient consented and qualified, a single-shot femoral nerve block was performed. Patients were screened for nasal staphylococcal colonization and treated with povidone-iodine nasal decolonization, chlorhexidine wash, and antibiotics determined by staphylococcal status and type of surgical procedure planned. Preoperative and postoperative order sets were implemented that dictated the care processes as outlined in Table 1. Surgeons determined the choice of operative intervention as per usual; this included internal fixation and partial or total hip replacement. Detailed medical and surgical protocols are included in Appendix A.
Since the initiation of the IFHFP on February 1, 2016, the program has continued to advance with our experience. We used the year preceding the start of the program as our baseline year (January 1, 2015, through December 31, 2015). The following years, 2016 and 2017, were a transition time during which our protocols were implemented. The intervention year was defined as January 1, 2018, through December 31, 2018. The outcomes during the intervention year were compared with the baseline year. It is important to note that our program has been in continuous evolution, including during the intervention year, with protocols created and refined as we gain experience.
Outcomes include 30-day mortality, transfusions, adverse effects of drugs, venous thromboembolic complications, sepsis, myocardial infarction, mechanical surgical fixation complications, length of stay, 30-day readmission rate, unexpected return to the OR, and time to operative intervention. Definitions of the outcome variables are reviewed in Appendix B.
RESULTS
There were 275 consecutive patients with hip fractures admitted to SRC in the baseline year (January 1, 2015 to December 31, 2015) and 434 patients with hip fractures admitted in the intervention year (January 1, 2018, to December 31, 2018) after consolidation of the program to the single Yale-New Haven Campus and implementation of standardized care processes. Patient demographic data including age, sex, ethnicity, body mass index, and American Society of Anesthesiologists physical status classification were evaluated for the baseline year and intervention year and reported in Table 2. There were no differences in the demographics of patients between baseline and intervention years.
From baseline year to intervention year, 30-day mortality, transfusion, adverse effects of drugs, length of stay, unexpected return to OR, and time to OR were all significantly reduced. Mortality within 30 days decreased from 8.0% to 2.8%. The results are displayed in Table 3. No significant difference was seen in the incidence of venous thromboembolism, sepsis, myocardial infarctions, readmission at 30 days, or mechanical surgical fixation complications.
The Figure shows the 30-day IFHFP mortality rate as reported on a monthly basis starting on January 1 of the baseline year, 2015, and continuing through December 31 of the intervention year, 2018. The process interventions are mapped according to the date of initiation. The median mortality rate (including all data from January 1, 2015, to December 31, 2018) is demonstrated as the dotted line. From May 2018 to December 2018, each monthly mortality rate was recorded below the four-year median, a visual demonstration of the statistical significance seen in our mortality reduction from 8.0% in the baseline year to 2.8% in the intervention year.
DISCUSSION
Patients with fragility hip fractures are a medically complex and vulnerable population. The goal of the CMC IFHFP was to standardize the care of these high-risk patients in an effort to reduce time to the OR, perioperative medical complications, time spent in the hospital, and ultimately mortality.
The barriers to implementing coordinated, multidisciplinary care are significant. In our case, we had a fragmented care model with fragility hip fracture patients cared for at two campuses, on different nursing units, with both community and faculty surgeons providing operative care, and with no predesignated primary team. We structured our program for equal sharing of call between community and faculty surgeons. However, there was distrust among the physician groups: Primary care physicians were concerned that their referral lines with orthopedic surgical colleagues would be fractured by the new shared call. Surgeons doubted that patients would be distributed equally among community and faculty practices. Hospitalists feared that comanagement would mean surgeons abdicating responsibility for care. Surgeons worried that routine medical involvement would delay surgery and prolong the length of stay with excessive testing. In order to achieve consensus, address concerns, and allay fears, we engaged the primary care and surgeon leadership for their support at the onset of the program and held monthly large group meetings and many smaller sessions to advance objectives. We meticulously tracked data and frequently reported out to the involved groups.
As it is well established that operative intervention on a hip fracture is best completed within 24 h to optimize a patient’s clinical outcomes, critical interventions were the designation of a hip fracture OR starting midday and expectation that surgery be performed the day after admission for medically cleared patients. Surgeons were able to book elective cases or outpatient clinic time in the morning. The morning hours prior to surgery allowed time for any final medical optimization, preoperative nursing care, and family discussions. Most surgeries were then completed by the primary OR staff during standard operating hours. Patients were out of the postanesthesia care unit and settled back on the orthopedic nursing unit in the early evening without a prolonged period of nil per os, bed rest, or sleep interruption.
While our protocol expected surgery the day after admission for medically cleared patients, we used surgery within 24 h as a simple metric to compare baseline with intervention outcomes. With our hip fracture OR block time beginning midday, the majority of our medically cleared hip fracture patients would receive surgical treatment within 24 h of admission. Our data show a significant improvement in timeliness of surgical intervention from 41.8% of patients to the OR within 24 h in 2015 to 55% in 2018. In 2017, we conducted an interval four-month audit involving a detailed chart review of all patients for whom surgery was delayed beyond 24 h from hospital admission. Chart review identified anticoagulation as the primary reason for surgical delay. Of patients who were eligible for surgery (medically stabilized and not therapeutically anticoagulated), 90% underwent surgery within 24 h during this four-month period in 2017. This compares to an overall rate of surgery within 24 h of 57% during the calendar year 2017. We did not perform a subgroup analysis of outcomes in patients with time to OR of 24-36 h. From this study, we are therefore unable to draw any conclusion regarding time to surgery and mortality.
Our dedicated OR hip fracture block time was changed from 7:30
Transfusion rate reduction from 46.6% to 28.1% was achieved primarily by the implementation and strict enforcement of a policy to avoid transfusing asymptomatic patients with hemoglobin >7.0 g/dL. In addition, we recommended TXA using standard perioperative arthroplasty dosing of 1 g intravenously (IV) at the time of incision followed by 1 g IV 3 h later in the postanaesthesia care unit. However, adherence to TXA recommendations was poor. A year-long audit (February 2017 to February 2018) demonstrated that only 29% of patients undergoing hip fracture surgery received the recommended TXA. After the conclusion of the study period of this review, we revised our TXA protocol to include an infusion at the time of admission and subsequent perioperative doses. The expanded TXA protocol (with clear exclusion criteria) has been “hard-wired” into our electronic perioperative order sets. We are tracking TXA compliance on a weekly basis. We anticipate that earlier TXA administration and improved compliance will further reduce transfusion rates.
We reduced the adverse effects of medications with two initiatives: First, dedicated hip fracture order sets with medications selected and dosed specifically for the geriatric population were launched at the onset of the IFHFP in 2016. Second, in coordination with our regional anesthesia team, patients who met criteria underwent a single-shot femoral nerve block upon diagnosis of the hip fracture. Patients reported up to 24 h of nonnarcotic pain relief with the femoral nerve block.
Prior to the introduction of the IFHFP, surgeons determined DVT prophylaxis based on their personal preference. Many of our surgeons were concerned that standardizing DVT prophylaxis to enoxaparin would increase the risk of surgical site bleeding, hematoma, infection, and reoperation. With data tracking and periodic reporting, we were able to reassure our surgeons: We demonstrated a reduction in the rate of patients unexpectedly requiring a return to the OR from 5.1% in 2015 to 0% in 2018.
We did not find a significant difference in mechanical complications due to surgical fixation during the index admission. Most mechanical complications do not present within the index admission and, therefore, would not be identified by this metric. Furthermore, in this phase of the program, we did not seek to change or standardize intraoperative surgical processes outside of surgical site infection prevention measures. Surgical technical quality and variation among surgeons is an area of ongoing evaluation within our program. We have begun a surgical quality review process with an expert review of postoperative radiography, beginning with fixation of nondisplaced femoral neck fractures, feedback to surgeons, and tracking of mechanical complications beyond the index admission. The surgical quality outcomes will be presented in a future manuscript.
Anticoagulation use is common in patients with hip fractures because of the high prevalence of comorbid conditions such as atrial fibrillation and venous thromboembolic disease. Direct oral anticoagulants (DOACs) are now commonly used in place of the vitamin K antagonist, warfarin. Our inability to efficiently reverse the DOACs compounded by surgeon unfamiliarity with these agents led to extreme caution in the timing of OR, with most patients delayed a full 48 h from the last dose of their prescribed DOAC. After recognizing the impact of anticoagulation on the timing of surgery, we convened a multidisciplinary group to determine rational guidelines for the timing of surgery in patients on chronic anticoagulation based on the bleeding risk of the planned operative procedure. These guidelines were instituted in December 2018, so their impact is not reflected in this review.
Our results showing a reduction in length of stay and mortality cannot be explained by any one intervention. We propose that the standardization of all processes and protocols, the establishment of clear expectations among all the medical and nursing personnel, and the shorter time spent waiting for surgery all contributed to the length of stay reduction. Likewise, the decrease in time to OR, reduction in time spent in the hospital, fewer transfusions, adverse effects of medication, and surgical complications requiring a return to the OR have all likely contributed to the significant reduction in mortality. The efforts of the orthopedic nursing team certainly contributed: The CMC nurses led the efforts to standardize surgical site infection bundle care, reduce indwelling bladder catheter use, and together with physical therapy, mobilize patients out of bed for meals postoperatively. The strong focus on teamwork, data tracking, feedback and accountability, and the desire for continued improvement may have been the strongest drivers in this program’s success.
Our results showed a nonsignificant increase in 30-day readmission from 9.1% to 12.5%. One limitation of this study is that we did not track specific readmission diagnoses to better understand trends in diagnoses or indications for hospital readmission. Going forward, we are reviewing readmissions to better understand opportunities to improve our inpatient processes and transitions of care.
This an evolving project. We have expanded our use of TXA in an effort to further reduce transfusion rates. We have adjusted our protocols for patients admitted on DOACs and warfarin to allow more rapid surgical intervention. We have initiated a surgical quality review process in which surgical fixation is reviewed with timely feedback to the operating surgeon. We are working closely with the skilled nursing facilities to extend our rehabilitation and nursing care protocols beyond the acute care setting. We are measuring patient engagement with a brief discharge survey specific to the CMC IFHFP. We continue to seek feedback from our referring primary care physicians to improve communication at times of care transition.
One of the limitations of a quality improvement project such as this one is the inability to identify the effect of each individual intervention. We can conclude that the totality of the multidisciplinary project reduced mortality in our hip fracture population, but we cannot report the relative effect of each process change. Another center seeking to replicate this success cannot determine from this research how to prioritize their resources to achieve a similar outcome.
How we care for the fragility hip fracture patient after hospital discharge is critical and unaddressed in this current study. A limitation of our current program is the lack of consistent postdischarge bone health management—which we are working to address. Also related to postdischarge management, we have partnered with a network of preferred skilled nursing facilities to standardize the care and decrease the length of stay. These data will be published separately.
We understand that our experience at the CMC is unique and specific to our care environment. This is a single site study and may not be generalizable to other centers. Nonetheless, the principles of multidisciplinary care, evidence-based protocol development, technological integration of protocols through order sets, and data tracking with feedback and accountability are the essential elements of our success that can be generalized to other institutions.
CONCLUSIONS
The CMC at Yale School of Medicine and Yale-New Haven Hospital IFHFP provides a model for implementing well-documented evidence-based interventions to standardize the care of patients with fragility hip fractures. The IFHFP yielded reduced mortality, length of stay, blood transfusion utilization, adverse effects of medications, unexpected return to the OR, and time to the OR.
Acknowledgments
The authors thank the work of the Center for Musculoskeletal Care Hip Fracture Oversight Group, program surgeons, and community primary care leaders: Olukemi Akande, MD, Mark Altman, MD, Diren Arsoy, MD, John Aversa, MD, Michael Connair, MD, Leo Cooney, MD, Kenneth Donohue, MD, David Gibson, MD, Gail Haesche, RN, MS, ACM-RN, Carol Just, MSN, NEA-BC, RN, Patricia Kenyon, RN, ACM, Francis Lee MD, Michael Leslie, MD, Michael Lucchini, MD, Christopher Lynch, MD, Rowland Mayor, MD, Tara Messina, PT, Lorraine Novella, RN, Paul Oliver, PA-C, Vivek Parwani, MD, Joseph Quaranta, MD, Lee Rubin, MD, Derek Shia, MD, Jeff Sumner, MD, John Tarutis, Arya Varthi, MD, Anuruddha Walaliyadda, MD, Daniel Wiznia, MD, Shirvinda Wijesekera, MD, Joseph Wu, MD, Brad Yoo, MD, and James Yue, MD.
1. Abrahamsen B, van Staa T, Ariely M, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiologic review. Osteoporos Int. 2009;20(10):1633-1650. https://doi.org/10.1007/s00198-009-0920-3.
2. DellaRocca GJ, Moylan KC, Crist BD, Volgas DA, Stannard JP, Mehr DR. Comanagement of geriatric patients with hip fractures: a retrospective, controlled cohort study. Geriatr Orthop Surg Rehabil. 2013;4(1):10-15. https://doi.org/10.1177/2151458513495238.
3. Wang Y, Tang J, Zhou F, Yang L, Wu J. Comprehensive geriatric care reduces acute perioperative delirium in elderly patients with hip fractures: a meta-analysis. Medicine. 2017; 96(26): e7361. https://doi.org/10.1097/MD.0000000000007361.
4. Liu VX, Rosas E, Hwang J, et al. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017;152(7):e171032. https://doi.org/10.1001/jamasurg.2017.1032.
5. Taraldsen K, Sletvold O, Thingstad P, et al. Physical behavior and function early after hip fracture surgery in patients receiving geriatric care or orthopedic care—a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69(3):338-345. https://doi.org/10.1093/gerona/glt097.
6. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson Jl. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702-709. https://doi.org/10.1016/s0002-9343(02)01119-1.
7. Hamlet WP, Lieberman JR, Freedman EL, Dorey FJ, Fletcher A, Johnson EE. Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop. 1997;26(9):621-627.
8. Hoenig H, Rubenstein LV, Sloane R, Honer R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157(5):513-520.
9. Orosz GM, Magaziner J, Hannan El, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743. https://doi.org/10.1001/jama.291.14.1738.
10. Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004:124(5):334-340. https://doi.org/10.1007/s00402-004-0662-9.
11. Doruk H, Mas MR, Yidiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179-185.https://doi.org/10.1016/j.archger.2004.03.004.
12. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-729. https://doi.org/10.1016/j.injury.2012.08.025.
13. Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;5: CD001159. https://doi.org/10.1002/14651858.CD001159.pub2.
14. Morrison RS, Dickman E, Hwang U, et al. Regional nerve blocks improve pain and functional outcomes in hip fracture: a randomized controlled trial. J Am Geriatr Soc. 2016;64(12):2433-2439. https://doi.org/10.1111/jgs.14386.
15. Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency deparment patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584-591. https://doi.org/10.1111/acem.12154.
16. Dickman E, Pushkar I, Likourezos A, et al. Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. Am J Emerg Med. 2016;34(3):586-589. https://doi.org/10.1016/j.ajem.2015.12.016.
17. Carson JL, Terrin MI, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453-2462. https://doi.org/10.1056/NEJMoa1012452.
18. Garcia-Alvarez F, Al-Ghanem R, García-Alvarez I, López-Baisson A, Bernal M. Risk factors for postoperative infections in patients with hip fracture treated by means of Thompson arthoplasty. Arch Gerontol Geriatr. 2010; 50(1):51-55. https://doi.org/10.1016/j.archger.2009.01.009.
19. Farrow LS, Smith TO, Ashcroft GP, Myint PK. A systematic review of tranexamic acid in hip fracture surgery. Br J Clin Pharmacol. 2016;82(6):1458-1470. https://doi.org/10.1111/bcp.13079.
20. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e278S-e325S. https://doi.org/10.1378/chest.11-2404.
21. Gillespie WJ, Walenkamp G. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev. 2010;(3):CD000244. https://doi.org/10.1002/14651858.CD000244.pub2.
22. Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG. Time to ambulation after hip fracture surgery: relation to hospitalization outcomes. J Gerontol A Biol Sci Med Sci. 2003;58(11):1042-1045. https://doi.org/10.1093/gerona/58.11.m1042.
23. Foster MR, Heppenstall RB, Friedenberg ZB, Hozack WJ. A prospective assessment of nutritional status and complications in patients with fractures of the hip. J Orthop Trauma. 1990;4(1):49-57. https://doi.org/10.1097/00005131-199003000-00009.
24. Bell JJ, Pulle RC, Crouch AM, Kuys SS, Ferrier RL, Whitehouse SL. Impact of malnutrition on 12-month mortality following acute hip fracture. ANZ J Surg. 2016;86(3):157-161. https://doi.org/10.1111/ans.13429.
25. Avenell A, Handoll HH. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. 2010;(1):CD001880. https://doi.org/10.1002/14651858.CD001880.pub5.
1. Abrahamsen B, van Staa T, Ariely M, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiologic review. Osteoporos Int. 2009;20(10):1633-1650. https://doi.org/10.1007/s00198-009-0920-3.
2. DellaRocca GJ, Moylan KC, Crist BD, Volgas DA, Stannard JP, Mehr DR. Comanagement of geriatric patients with hip fractures: a retrospective, controlled cohort study. Geriatr Orthop Surg Rehabil. 2013;4(1):10-15. https://doi.org/10.1177/2151458513495238.
3. Wang Y, Tang J, Zhou F, Yang L, Wu J. Comprehensive geriatric care reduces acute perioperative delirium in elderly patients with hip fractures: a meta-analysis. Medicine. 2017; 96(26): e7361. https://doi.org/10.1097/MD.0000000000007361.
4. Liu VX, Rosas E, Hwang J, et al. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017;152(7):e171032. https://doi.org/10.1001/jamasurg.2017.1032.
5. Taraldsen K, Sletvold O, Thingstad P, et al. Physical behavior and function early after hip fracture surgery in patients receiving geriatric care or orthopedic care—a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69(3):338-345. https://doi.org/10.1093/gerona/glt097.
6. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson Jl. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702-709. https://doi.org/10.1016/s0002-9343(02)01119-1.
7. Hamlet WP, Lieberman JR, Freedman EL, Dorey FJ, Fletcher A, Johnson EE. Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop. 1997;26(9):621-627.
8. Hoenig H, Rubenstein LV, Sloane R, Honer R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157(5):513-520.
9. Orosz GM, Magaziner J, Hannan El, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743. https://doi.org/10.1001/jama.291.14.1738.
10. Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004:124(5):334-340. https://doi.org/10.1007/s00402-004-0662-9.
11. Doruk H, Mas MR, Yidiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179-185.https://doi.org/10.1016/j.archger.2004.03.004.
12. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-729. https://doi.org/10.1016/j.injury.2012.08.025.
13. Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;5: CD001159. https://doi.org/10.1002/14651858.CD001159.pub2.
14. Morrison RS, Dickman E, Hwang U, et al. Regional nerve blocks improve pain and functional outcomes in hip fracture: a randomized controlled trial. J Am Geriatr Soc. 2016;64(12):2433-2439. https://doi.org/10.1111/jgs.14386.
15. Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency deparment patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584-591. https://doi.org/10.1111/acem.12154.
16. Dickman E, Pushkar I, Likourezos A, et al. Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. Am J Emerg Med. 2016;34(3):586-589. https://doi.org/10.1016/j.ajem.2015.12.016.
17. Carson JL, Terrin MI, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453-2462. https://doi.org/10.1056/NEJMoa1012452.
18. Garcia-Alvarez F, Al-Ghanem R, García-Alvarez I, López-Baisson A, Bernal M. Risk factors for postoperative infections in patients with hip fracture treated by means of Thompson arthoplasty. Arch Gerontol Geriatr. 2010; 50(1):51-55. https://doi.org/10.1016/j.archger.2009.01.009.
19. Farrow LS, Smith TO, Ashcroft GP, Myint PK. A systematic review of tranexamic acid in hip fracture surgery. Br J Clin Pharmacol. 2016;82(6):1458-1470. https://doi.org/10.1111/bcp.13079.
20. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e278S-e325S. https://doi.org/10.1378/chest.11-2404.
21. Gillespie WJ, Walenkamp G. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev. 2010;(3):CD000244. https://doi.org/10.1002/14651858.CD000244.pub2.
22. Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG. Time to ambulation after hip fracture surgery: relation to hospitalization outcomes. J Gerontol A Biol Sci Med Sci. 2003;58(11):1042-1045. https://doi.org/10.1093/gerona/58.11.m1042.
23. Foster MR, Heppenstall RB, Friedenberg ZB, Hozack WJ. A prospective assessment of nutritional status and complications in patients with fractures of the hip. J Orthop Trauma. 1990;4(1):49-57. https://doi.org/10.1097/00005131-199003000-00009.
24. Bell JJ, Pulle RC, Crouch AM, Kuys SS, Ferrier RL, Whitehouse SL. Impact of malnutrition on 12-month mortality following acute hip fracture. ANZ J Surg. 2016;86(3):157-161. https://doi.org/10.1111/ans.13429.
25. Avenell A, Handoll HH. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. 2010;(1):CD001880. https://doi.org/10.1002/14651858.CD001880.pub5.
© 2020 Society of Hospital Medicine
Social Disadvantage, Access to Care, and Disparities in Physical Functioning Among Children Hospitalized with Respiratory Illness
Examining disparities in health-related quality of life (HRQoL) outcomes in children provides a unique patient-centered perspective on pediatric health services equity.1,2 Prior studies have demonstrated the relationship between minority race, low socioeconomic status, and lower maternal education with poorer HRQoL outcomes in children.3-6 Some studies have also shown a dose-response relationship between social disadvantage markers and poorer child health status.7,8 Furthermore, the associations between social disadvantage and poor access to care,9-11 and between poor access to care and lower HRQoL, are also well established.12-14
Examining HRQoL before and after hospitalization can further our understanding of how disparities in HRQoL may change once children engage with the medical system for an acute illness.15 Children requiring hospitalization constitute a useful population for examination of this question as they represent a group of children with variable social disadvantage markers and access to outpatient care.16 Although interventions to address social determinants of health for patients with social disadvantages have been associated with within-group improvements in HRQoL, none have assessed changes in disparities as an outcome.17 Furthermore, many of these studies were conducted in the outpatient setting,18,19 whereas hospitalization provides an additional point of care to address the social determinants of health for vulnerable families.20 Even for short hospitalizations, the 24/7 nature of hospital care provides the opportunity for frequent interactions with clinicians, nurses, and support staff to clarify illness-related questions, discuss other health concerns and unmet needs, and connect with social services or community resources. These opportunities may be particularly important for families with a higher number of social disadvantage markers and even more beneficial to those with difficulty accessing needed care from their primary medical home.
In this study, we focused on children with common respiratory illnesses (asthma, bronchiolitis, and pneumonia), which constitute the majority of childhood hospitalizations.21 Additionally, we only focused on the child’s physical functioning component of HRQoL because this component is most likely to improve after hospitalization for children with an acute respiratory illness.22 A prior study examining HRQoL before and after hospitalization demonstrated that most children return to and/or surpass their baseline physical functioning by 1 month after hospital discharge.23
Our primary objective was to examine associations between several markers of social disadvantage, access to care, and child physical functioning before and after hospitalization for acute respiratory illness. Second, we aimed to understand if access to care (defined as perceived difficulty/delays getting care) acts as an independent predictor of improvement in physical functioning from baseline to follow-up and/or if it modifies the relationship between social disadvantage and improvement in physical functioning (Appendix Figure).
METHODS
Study Design and Population
This study was nested within a multicenter, prospective cohort study of children who were hospitalized for asthma, bronchiolitis, or pneumonia between July 2014 and June 2016 at one of five children’s hospitals in the Pediatric Research in Inpatient Settings Network.24
We approached families for study participation within 72 hours of admission to the hospital using a standard protocol. Patients and their caregivers were eligible to participate in the study if the patient was 2 weeks to 16 years old and if the primary caregiver’s preferred language for medical communication was either English or Spanish. Patients with chronic medical conditions (except asthma), with moderate to severe developmental delay, with a history of prematurity <32 weeks, or who received care in the intensive care unit were excluded. Patients could only participate in the study once.
The study team set out to enroll an even number of patients across all three conditions. If a patient’s discharge diagnosis differed from their admission diagnosis (eg, from bronchiolitis to pneumonia), discharge diagnosis was used for condition group assignment. If the discharge diagnosis was not one of these three respiratory conditions, we excluded the patient from further analysis.
Data Collection
We collected data using two surveys. The first survey was administered within 72 hours of admission. This survey asked questions related to (1) caregiver-reported markers of social disadvantage, (2) caregiver perceptions of access to care, and (3) caregiver- and patient-reported assessments of physical functioning. The second survey was administered within 2 to 8 weeks after the patient’s discharge and included a second assessment of physical functioning.
Social Disadvantage
Patients were considered to have a marker of social disadvantage if their caregiver reported (1) being of non-White race and/or Hispanic ethnicity, (2) primarily speaking a language other than English at home and not speaking English very well (ie, limited English proficiency), (3) attaining at most a high school or equivalent degree, or (4) having a =/<$30,000 annual household income.
Access to Care
We used the following survey item from the 2009-2010 National Survey of Children with Special Health Care Needs25 to measure caregiver perceptions of access to care: “In the last six months, did you have any difficulties or delays getting care for your child because there were waiting lists, backlogs, or other problems getting an appointment?” We narrowed the original assessment time frame from 12 months to 6 months to provide a more proximal assessment of access in relation to the hospitalization.
Child Physical Functioning
We assessed child physical functioning using the physical functioning domain of the Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales and PedsQL Infant Scales, which have been validated for use in the inpatient setting.22 Caregivers completed one of these scales based on their child’s age. Assenting patients 8 to 16 years old completed the self-report PedsQL 4.0 Generic Core Scales instrument. When completing the first PedsQL survey, caregivers and patients reflected on the previous month before their child (or they) became ill to obtain a baseline physical functioning assessment.23 When completing the second PedsQL survey, caregivers and patients reflected on the past 7 days to obtain a follow-up assessment.
All study procedures were approved by the Western Institutional Review Board (IRB) or the participating hospitals’ IRB.
Statistical Analysis
Patients with no missing data for all four social disadvantage markers were categorized based on the number of markers they reported: none, one, two, or three or more markers. We combined patients with three and four social disadvantage markers into one group to maximize power for the analyses. We dichotomized the access to care variable and coded response options as “no difficulty/delays accessing care” if the caregiver chose “Never” and “any difficulty/delays accessing care” if they chose “Sometimes/Usually/Always.”
For each patient–caregiver dyad, PedsQL items were scored using a standard method in which higher scores reflected better functioning.22 A single set of PedsQL scores was used for each patient–caregiver dyad. We used self-reported patient scores if the patient completed the PedsQL instrument; otherwise, we used proxy-reported caregiver scores. Intraclass correlations between child self-report and parent proxy-report demonstrate moderate to good agreement above age 8 years.26 We computed a change in the physical functioning score by subtracting the baseline score from the follow-up score. The minimal clinically important difference (MCID) for the PedsQL instrument is 4.5 points, which we used to identify clinically meaningful differences.13
Analysis of variance models were constructed to test for differences in mean baseline and follow-up PedsQL scores (dependent variable) between the following independent variables: (1) social disadvantage groups and (2) those who reported having any difficulty/delays accessing care compared with those who did not. Only patient–caregiver dyads with both baseline and follow-up assessments were included in these analyses. Mixed-effects linear regression models were constructed to identify clinically meaningful differences in PedsQL scores between groups (MCID =/> 4.5) with adjustment for patient age, gender, respiratory condition, days between surveys, and hospital site as fixed effects. Site-specific random effects were included to account for within-hospital clustering. A similarly adjusted mixed-effects linear regression model was constructed to examine whether having any difficulty/delays accessing care modified the association between social disadvantage and PedsQL change scores (eg, an improvement from baseline to follow-up).
Because 17% of respondents had missing data for at least one social disadvantage marker, sensitivity analyses were conducted using multiple imputation to account for missing social disadvantage markers using chained equations.27 Sensitivity analyses were also conducted to adjust for severity of illness using vital sign data within the first 24 hours, which could only be validly captured on patients with asthma within our dataset. By restricting this latter analysis to patients with asthma, we were able to examine the relationships of interest in a population with chronic disease.
RESULTS
The study sample included 1,860 patients, of which 1,325 had both baseline and follow-up PedsQL data (71%). Descriptive statistics were similar between those who completed the baseline and follow-up surveys (Table 1).
Twenty-two percent of patients had >/=3 social disadvantages and 30% of caregivers reported having any difficulty/delays accessing care. The mean follow-up PedsQL score was higher than the baseline score (90.4 vs 82.5; Table 1).
Social Disadvantage Markers and PedsQL Scores
The number of social disadvantage markers was inversely related to mean baseline PedsQL scores, but there was no difference in mean follow-up PedsQL scores between social disadvantage groups (Table 2). In adjusted analyses, the mean baseline PedsQL score was −6.1 points (95% CI: −8.7, −3.5) lower for patients with >/= 3 social disadvantage markers compared with patients with no social disadvantage markers, which exceeded the scale’s MCID.
Difficulty/Delays Accessing Care and PedsQL Scores
Having any difficulty/delays accessing care was significantly associated with lower baseline and follow-up PedsQL scores (Table 2). In adjusted analyses, the difference in baseline scores was 5.2 points (95% CI: −7.2, −3.2), which exceedes the scale’s MCID.
Interaction Between Social Disadvantage Markers, Difficulty/Delays Accessing Care, and Change in PedsQL Scores from Baseline to Follow-Up
While having =/>2 social disadvantage markers and difficulty/delays accessing care were each positively associated with changes in PedsQL scores from baseline to follow-up (Table 3), only patients with =/> 3 social disadvantage markers exceeded the PedsQL MCID. In stratified analyses, patients with a combination of social disadvantage makers and difficulties/delays accessing care had lower baseline PedsQL scores and greater change in PedsQL scores from baseline to follow-up compared with those without difficulties/delays accessing care (Figure). However, having any difficulty/delays accessing care did not significantly modify the relationship between social disadvantage and change in PedsQL scores, as none of the interaction terms were significant (Table 3, Model 3).
Sensitivity Analysis
Baseline, follow-up, and change in PedsQL scores were similar to our main analysis after performing multiple imputation for missing social disadvantage markers (Supplemental Table 1). Findings were also similar for patients with a diagnosis of asthma only; however, changes in PedsQL scores were greater in magnitude (Appendix Table 2).
DISCUSSION
This study examined the relationship between social disadvantage and child physical functioning before and after hospitalization for acute respiratory illness. Study findings indicated that patients with higher numbers of social disadvantage markers reported lower PedsQL scores before hospitalization; however, differences in PedsQL scores were not apparent after hospitalization. Patients who experienced difficulty/delays accessing care also reported lower PedsQL scores at baseline. This difference was still significant but did not exceed the PedsQL MCID threshold after hospitalization. Difficulty/delays accessing care appeared to be an additional social disadvantage marker; however, it did not modify the relationship between social disadvantage and improvement in physical functioning.
The study findings at baseline are consistent with prior studies demonstrating a negative association between social disadvantage markers and HRQoL and a cumulative effect based on the number of social disadvantages.3,4,7,8 This study adds to the existing literature by examining how this relationship changes after hospitalization. As evidenced by the lack of association between social disadvantage markers and follow-up PedsQL scores, our findings suggest that receipt of inpatient care improved perceptions of physical functioning to a greater extent for patients with more social disadvantage markers (especially patients with =/> 3 social disadvantage markers). There are several potential reasons for these findings.
One possibility is that caregivers and/or patients with more social disadvantage markers are more influenced by context when assessing physical functioning. This could lead to an underestimation of functioning when asked to recall baseline physical functioning at the time of acute illness and overestimation of functioning after recovery from an illness. This possibility is consistent with a form of response bias, extreme response tendencies, in which lower socioeconomic subgroups tend to choose the more extreme response options of a scale.28 In the absence of longitudinal assessments of HRQoL across the care continuum over time, disentangling whether these differences are due to response bias or representative of true changes in physical functioning remains challenging.
Given that disparities in physical functioning at baseline were consistent with prior evidence, another possibility is that hospitalization provided an opportunity to address gaps in access and quality that may have existed for patients with social disadvantage in the community setting. The 24/7 nature of hospital care, usually from a multidisciplinary team of providers, lends itself to opportunities to receive intensive education related to the current illness or to address other health concerns that parents or providers identify during a hospital stay. For example, consistent and repetitive asthma education may be more beneficial to patients and families with more social disadvantage markers. The fact that the association between social disadvantage markers and change in physical functioning scores were greater for patients with asthma supports this reasoning. Hospital care may also provide an opportunity to address other unmet medical needs or psychosocial needs by providing efficient access to subspecialists, social workers, or interpreters. Further research is needed to elucidate whether families received additional services in the hospital setting that were not available to them prior to hospitalization, such as consistent interpreter use, social work engagement, and subspecialty/community referrals. Further studies should also determine whether the provision of equitable medical and social support services is associated with improvements in HRQoL disparities. Additionally, studies should examine whether physical functioning improvements following hospitalization return to baseline levels after a longer period of time and, if so, how we might sustain these reductions in HRQoL disparities. Such studies may identify tangible targets and interventions to reduce disparities in HRQoL for these children.
This study highlights the importance of assessing for difficulty/delays accessing care in addition to social disadvantage markers, as this was also a significant predictor of lower child physical functioning. Differences in PedsQL scores between those who reported any versus no difficulty/delays accessing care were more pronounced at baseline compared with follow-up. A possible reason for these findings is that receiving hospital care may have addressed some access to care issues that were present in the outpatient setting, which resulted in improved perceptions of physical functioning. For example, hospital care may mitigate access to care barriers such as limited after-hours clinic appointments, language barriers, and lack of insurance, thus providing some patients with an alternative pathway to address their health concerns. Alternatively, hospital staff may assist families in scheduling follow-up appointments with the patient’s primary medical home after discharge, which potentially reduced some access to care barriers. The question is whether these disparities will widen once again after a longer follow-up period if families continue facing barriers to accessing needed care in the outpatient setting.
The results of the effect modification analysis demonstrated that the association between social disadvantage and change in PedsQL scores from baseline to follow-up was not significantly different based on a child’s ability to access care. In our stratified analysis, difficulty/delays accessing care added to baseline disparities at each social disadvantage level but did not alter how perceptions of physical functioning change over time. Therefore, physical functioning improvements may rely more heavily on the type of care received within the hospital setting as opposed to accessing care in the first place. However, future studies should examine whether access to high-quality care instead of simply measuring difficulty/delays in accessing care would lead to different results. Access to a comprehensive medical home may be a better measure to assess for effect modification because it measures features beyond access to care, such as continuity, comprehensiveness, communication, and coordination of outpatient care.29-31
If additional studies find evidence that the nature of hospital care, an intensive 24/7 care setting, differentially benefits patients with higher social disadvantage markers (particularly those with =/> 3 markers and chronic illness), this would support the need for systematic screening for social disadvantages or difficulty/delays accessing care in the inpatient setting. Systematic screening could help ensure all patients who may benefit from additional services, such as intensive, culturally tailored education or connections to food, housing, or financial services, will in fact receive them, which may lead to sustained reductions in health disparities.20 Further research into pairing validated screening tools with proven interventions is needed.32
This study has additional limitations aside from those noted above. First, we did not reassess perceived or actual access to care after hospitalization, which may have allowed for analyses to examine access to care as a mediator between social disadvantage and lower child physical functioning. Second, this study included only English- and Spanish-speaking patients and families. Patients with less commonly spoken languages may experience more difficulty accessing or navigating the health system, which may further impact access to care and HRQoL. Third, we had a considerable amount of missing social disadvantage marker data (mainly income); however, our sensitivity analyses did not result in significantly different or clinically meaningful differences in our findings. Insurance status is more feasible to obtain from administrative data and could serve as a proxy for income or as an additional social disadvantage marker in future studies. Finally, we could calculate illness severity only for patients with asthma based on the available data; therefore, we could not adequately control for illness severity across all conditions.
CONCLUSIONS
Social disadvantage was associated with lower child physical functioning before hospitalization, but differences were not apparent after hospitalization for children with acute respiratory illness. Caregiver-perceived difficulty/delays accessing care was found to be an additional predictor of lower physical functioning at baseline but did not significantly alter the association between social disadvantage and improvement in physical functioning over time. Further studies are needed to understand how hospital care may differentially impact child physical functioning for patients with higher social disadvantage makers in order to sustain improvements in HRQoL disparities.
Acknowledgments
The authors thank the following individuals of the Pediatric Respiratory Illness Measurement System (PRIMES) study team for their contributions to this work: Karen M. Wilson, New York, New York; Ricardo A. Quinonez, Houston, Texas; Joyee G. Vachani, Houston, Texas; and Amy Tyler, Aurora, Colorado. We would also like to thank the Pediatric Research in Inpatient Settings Network for facilitating this work.
1. Szilagyi PG, Schor EL. The health of children. Health Serv Res. 1998;33(4 Pt 2):1001-1039.
2. Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005;3(1):34. https://doi.org/10.1186/1477-7525-3-34.
3. von Rueden U, Gosch A, Rajmil L, Bisegger C, Ravens-Sieberer U. Socioeconomic determinants of health related quality of life in childhood and adolescence: results from a European study. J Epidemiol Community Health. 2006;60(2):130-135. https://doi.org/10.1136/jech.2005.039792.
4. Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137(3):642-650. https://doi.org/10.1378/chest.09-0345.
5. Flores G, Tomany-Korman SC, Corey CR, Freeman HE, Shapiro MF. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2):e286-98. https://doi.org/10.1542/peds.2007-1243.
6. Fedele DA, Molzon ES, Eddington AR, Hullmann SE, Mullins LL, Gillaspy SG. Perceived barriers to care in a pediatric medical home: the moderating role of caregiver minority status. Clin Pediatr (Phila). 2014;53(4):351-355. https://doi.org/10.1177/0009922813507994.
7. Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337-344. https://doi.org/10.1542/peds.2007-0447.
8. Bauman LJ, Silver EJ, Stein REK. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321-1328. https://doi.org/10.1542/peds.2005-1647.
9. Andrulis DP. Moving beyond the status quo in reducing racial and ethnic disparities in children’s health. Public Health Rep. 2005;120(4):370-377. https://doi.org/10.1177/003335490512000403.
10. Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: has anything changed over the years? Int J Equity Health. 2013;12:10. https://doi.org/10.1186/1475-9276-12-10.
11. Seid M, Stevens GD, Varni JW. Parents’ perceptions of pediatric primary care quality: effects of race/ethnicity, language, and access. Health Serv Res. 2003;38(4):1009-1031. https://doi.org/10.1111/1475-6773.00160.
12. Seid M, Varni JW, Cummings L, Schonlau M. The impact of realized access to care on health-related quality of life: a two-year prospective cohort study of children in the California State Children’s Health Insurance Program. J Pediatr. 2006;149(3):354-361. https://doi.org/10.1016/j.jpeds.2006.04.024.
13. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329-341. https://doi.xorg/10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2.
14. Simon AE, Chan KS, Forrest CB. Assessment of children’s health-related quality of life in the united states with a multidimensional index. Pediatrics. 2008;121(1):e118-e126. https://doi.org/10.1542/peds.2007-0480.
15. Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: what can a clinician do? Pediatrics. 2015;136(5):961-968. https://doi.org/10.1542/peds.2014-4126.
16. Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524-529. https://doi.org/10.1542/peds.107.3.524.
17. Lion KC, Raphael JL. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135(2):354-361. https://doi.org/10.1542/peds.2014-2982.
18. Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14:S8-S17. https://doi.org/10.1097/01.PHH.0000338382.36695.42.
19. Beck AF, Cohen AJ, Colvin JD, et al. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84(1):10-21. https://doi.org/10.1038/s41390-018-0012-1.
20. Shah AN, Simmons J, Beck AF. Adding a vital sign: considering the utility of place-based measures in health care settings. Hosp Pediatr. 2018;8(2):112-114. https://doi.org/10.1542/hpeds.2017-0219.
21. Leyenaar JK, Ralston SL, Shieh M-S, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624.
22. Desai AD, Zhou C, Stanford S, Haaland W, Varni JW, Mangione-Smith RM. Validity and responsiveness of the pediatric quality of life inventory (PedsQL) 4.0 generic core scales in the pediatric inpatient setting. JAMA Pediatr. 2014;168(12):1114-1121. https://doi.org/10.1001/jamapediatrics.2014.1600.
23. Rabbitts JA, Palermo TM, Zhou C, Mangione-Smith R. Pain and health-related quality of life after pediatric inpatient surgery. J Pain. 2015;16(12):1334-1341. https://doi.org/10.1016/j.jpain.2015.09.005.
24. Mangione-Smith R, Zhou C, Williams DJ, et al. Pediatric respiratory illness measurement system (PRIMES) scores and outcomes. Pediatrics. 2019;144(2):e20190242. https://doi.org/10.1542/peds.2019-0242.
25. Child and Adolescent Health Measurement Initiative. National survey of children with special health care needs (NS-CSHCN), 2009-2010. Available at: http://childhealthdata.org/learn/NS-CSHCN/topics_questions. Accessed on September 20, 2018.
26. Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:1. https://doi.org/10.1186/1477-7525-5-1.
27. Buuren S van, Groothuis-Oudshoorn K. Mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. https://doi.org/10.18637/jss.v045.i03.
28. Elliott MN, Haviland AM, Kanouse DE, Hambarsoomian K, Hays RD. Adjusting for subgroup differences in extreme response tendency in ratings of health care: impact on disparity estimates. Heal Serv Res. 2009;44(2 Pt 1):542-561. https://doi.org/10.1111/j.1475-6773.2008.00922.x.
29. Stevens GD, Vane C, Cousineau MR. Association of experiences of medical home quality with health-related quality of life and school engagement among Latino children in low-income families. Health Serv Res. 2011;46(6pt1):1822-1842. https://doi.org/10.1111/j.1475-6773.2011.01292.x.
30. Long WE, Bauchner H, Sege RD, Cabral HJ, Garg A. The value of the medical home for children without special health care needs. Pediatrics. 2012;129(1):87-98. https://doi.org/10.1542/peds.2011-1739.
31. Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604-611. https://doi.org/10.1542/peds.2009-3555.
32. Sokol R, Austin A, Chandler C, et al. Screening children for social determinants of health: a systematic review. Pediatrics. 2019;144(4):e20191622. https://doi.org/10.1542/peds.2019-1622.
Examining disparities in health-related quality of life (HRQoL) outcomes in children provides a unique patient-centered perspective on pediatric health services equity.1,2 Prior studies have demonstrated the relationship between minority race, low socioeconomic status, and lower maternal education with poorer HRQoL outcomes in children.3-6 Some studies have also shown a dose-response relationship between social disadvantage markers and poorer child health status.7,8 Furthermore, the associations between social disadvantage and poor access to care,9-11 and between poor access to care and lower HRQoL, are also well established.12-14
Examining HRQoL before and after hospitalization can further our understanding of how disparities in HRQoL may change once children engage with the medical system for an acute illness.15 Children requiring hospitalization constitute a useful population for examination of this question as they represent a group of children with variable social disadvantage markers and access to outpatient care.16 Although interventions to address social determinants of health for patients with social disadvantages have been associated with within-group improvements in HRQoL, none have assessed changes in disparities as an outcome.17 Furthermore, many of these studies were conducted in the outpatient setting,18,19 whereas hospitalization provides an additional point of care to address the social determinants of health for vulnerable families.20 Even for short hospitalizations, the 24/7 nature of hospital care provides the opportunity for frequent interactions with clinicians, nurses, and support staff to clarify illness-related questions, discuss other health concerns and unmet needs, and connect with social services or community resources. These opportunities may be particularly important for families with a higher number of social disadvantage markers and even more beneficial to those with difficulty accessing needed care from their primary medical home.
In this study, we focused on children with common respiratory illnesses (asthma, bronchiolitis, and pneumonia), which constitute the majority of childhood hospitalizations.21 Additionally, we only focused on the child’s physical functioning component of HRQoL because this component is most likely to improve after hospitalization for children with an acute respiratory illness.22 A prior study examining HRQoL before and after hospitalization demonstrated that most children return to and/or surpass their baseline physical functioning by 1 month after hospital discharge.23
Our primary objective was to examine associations between several markers of social disadvantage, access to care, and child physical functioning before and after hospitalization for acute respiratory illness. Second, we aimed to understand if access to care (defined as perceived difficulty/delays getting care) acts as an independent predictor of improvement in physical functioning from baseline to follow-up and/or if it modifies the relationship between social disadvantage and improvement in physical functioning (Appendix Figure).
METHODS
Study Design and Population
This study was nested within a multicenter, prospective cohort study of children who were hospitalized for asthma, bronchiolitis, or pneumonia between July 2014 and June 2016 at one of five children’s hospitals in the Pediatric Research in Inpatient Settings Network.24
We approached families for study participation within 72 hours of admission to the hospital using a standard protocol. Patients and their caregivers were eligible to participate in the study if the patient was 2 weeks to 16 years old and if the primary caregiver’s preferred language for medical communication was either English or Spanish. Patients with chronic medical conditions (except asthma), with moderate to severe developmental delay, with a history of prematurity <32 weeks, or who received care in the intensive care unit were excluded. Patients could only participate in the study once.
The study team set out to enroll an even number of patients across all three conditions. If a patient’s discharge diagnosis differed from their admission diagnosis (eg, from bronchiolitis to pneumonia), discharge diagnosis was used for condition group assignment. If the discharge diagnosis was not one of these three respiratory conditions, we excluded the patient from further analysis.
Data Collection
We collected data using two surveys. The first survey was administered within 72 hours of admission. This survey asked questions related to (1) caregiver-reported markers of social disadvantage, (2) caregiver perceptions of access to care, and (3) caregiver- and patient-reported assessments of physical functioning. The second survey was administered within 2 to 8 weeks after the patient’s discharge and included a second assessment of physical functioning.
Social Disadvantage
Patients were considered to have a marker of social disadvantage if their caregiver reported (1) being of non-White race and/or Hispanic ethnicity, (2) primarily speaking a language other than English at home and not speaking English very well (ie, limited English proficiency), (3) attaining at most a high school or equivalent degree, or (4) having a =/<$30,000 annual household income.
Access to Care
We used the following survey item from the 2009-2010 National Survey of Children with Special Health Care Needs25 to measure caregiver perceptions of access to care: “In the last six months, did you have any difficulties or delays getting care for your child because there were waiting lists, backlogs, or other problems getting an appointment?” We narrowed the original assessment time frame from 12 months to 6 months to provide a more proximal assessment of access in relation to the hospitalization.
Child Physical Functioning
We assessed child physical functioning using the physical functioning domain of the Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales and PedsQL Infant Scales, which have been validated for use in the inpatient setting.22 Caregivers completed one of these scales based on their child’s age. Assenting patients 8 to 16 years old completed the self-report PedsQL 4.0 Generic Core Scales instrument. When completing the first PedsQL survey, caregivers and patients reflected on the previous month before their child (or they) became ill to obtain a baseline physical functioning assessment.23 When completing the second PedsQL survey, caregivers and patients reflected on the past 7 days to obtain a follow-up assessment.
All study procedures were approved by the Western Institutional Review Board (IRB) or the participating hospitals’ IRB.
Statistical Analysis
Patients with no missing data for all four social disadvantage markers were categorized based on the number of markers they reported: none, one, two, or three or more markers. We combined patients with three and four social disadvantage markers into one group to maximize power for the analyses. We dichotomized the access to care variable and coded response options as “no difficulty/delays accessing care” if the caregiver chose “Never” and “any difficulty/delays accessing care” if they chose “Sometimes/Usually/Always.”
For each patient–caregiver dyad, PedsQL items were scored using a standard method in which higher scores reflected better functioning.22 A single set of PedsQL scores was used for each patient–caregiver dyad. We used self-reported patient scores if the patient completed the PedsQL instrument; otherwise, we used proxy-reported caregiver scores. Intraclass correlations between child self-report and parent proxy-report demonstrate moderate to good agreement above age 8 years.26 We computed a change in the physical functioning score by subtracting the baseline score from the follow-up score. The minimal clinically important difference (MCID) for the PedsQL instrument is 4.5 points, which we used to identify clinically meaningful differences.13
Analysis of variance models were constructed to test for differences in mean baseline and follow-up PedsQL scores (dependent variable) between the following independent variables: (1) social disadvantage groups and (2) those who reported having any difficulty/delays accessing care compared with those who did not. Only patient–caregiver dyads with both baseline and follow-up assessments were included in these analyses. Mixed-effects linear regression models were constructed to identify clinically meaningful differences in PedsQL scores between groups (MCID =/> 4.5) with adjustment for patient age, gender, respiratory condition, days between surveys, and hospital site as fixed effects. Site-specific random effects were included to account for within-hospital clustering. A similarly adjusted mixed-effects linear regression model was constructed to examine whether having any difficulty/delays accessing care modified the association between social disadvantage and PedsQL change scores (eg, an improvement from baseline to follow-up).
Because 17% of respondents had missing data for at least one social disadvantage marker, sensitivity analyses were conducted using multiple imputation to account for missing social disadvantage markers using chained equations.27 Sensitivity analyses were also conducted to adjust for severity of illness using vital sign data within the first 24 hours, which could only be validly captured on patients with asthma within our dataset. By restricting this latter analysis to patients with asthma, we were able to examine the relationships of interest in a population with chronic disease.
RESULTS
The study sample included 1,860 patients, of which 1,325 had both baseline and follow-up PedsQL data (71%). Descriptive statistics were similar between those who completed the baseline and follow-up surveys (Table 1).
Twenty-two percent of patients had >/=3 social disadvantages and 30% of caregivers reported having any difficulty/delays accessing care. The mean follow-up PedsQL score was higher than the baseline score (90.4 vs 82.5; Table 1).
Social Disadvantage Markers and PedsQL Scores
The number of social disadvantage markers was inversely related to mean baseline PedsQL scores, but there was no difference in mean follow-up PedsQL scores between social disadvantage groups (Table 2). In adjusted analyses, the mean baseline PedsQL score was −6.1 points (95% CI: −8.7, −3.5) lower for patients with >/= 3 social disadvantage markers compared with patients with no social disadvantage markers, which exceeded the scale’s MCID.
Difficulty/Delays Accessing Care and PedsQL Scores
Having any difficulty/delays accessing care was significantly associated with lower baseline and follow-up PedsQL scores (Table 2). In adjusted analyses, the difference in baseline scores was 5.2 points (95% CI: −7.2, −3.2), which exceedes the scale’s MCID.
Interaction Between Social Disadvantage Markers, Difficulty/Delays Accessing Care, and Change in PedsQL Scores from Baseline to Follow-Up
While having =/>2 social disadvantage markers and difficulty/delays accessing care were each positively associated with changes in PedsQL scores from baseline to follow-up (Table 3), only patients with =/> 3 social disadvantage markers exceeded the PedsQL MCID. In stratified analyses, patients with a combination of social disadvantage makers and difficulties/delays accessing care had lower baseline PedsQL scores and greater change in PedsQL scores from baseline to follow-up compared with those without difficulties/delays accessing care (Figure). However, having any difficulty/delays accessing care did not significantly modify the relationship between social disadvantage and change in PedsQL scores, as none of the interaction terms were significant (Table 3, Model 3).
Sensitivity Analysis
Baseline, follow-up, and change in PedsQL scores were similar to our main analysis after performing multiple imputation for missing social disadvantage markers (Supplemental Table 1). Findings were also similar for patients with a diagnosis of asthma only; however, changes in PedsQL scores were greater in magnitude (Appendix Table 2).
DISCUSSION
This study examined the relationship between social disadvantage and child physical functioning before and after hospitalization for acute respiratory illness. Study findings indicated that patients with higher numbers of social disadvantage markers reported lower PedsQL scores before hospitalization; however, differences in PedsQL scores were not apparent after hospitalization. Patients who experienced difficulty/delays accessing care also reported lower PedsQL scores at baseline. This difference was still significant but did not exceed the PedsQL MCID threshold after hospitalization. Difficulty/delays accessing care appeared to be an additional social disadvantage marker; however, it did not modify the relationship between social disadvantage and improvement in physical functioning.
The study findings at baseline are consistent with prior studies demonstrating a negative association between social disadvantage markers and HRQoL and a cumulative effect based on the number of social disadvantages.3,4,7,8 This study adds to the existing literature by examining how this relationship changes after hospitalization. As evidenced by the lack of association between social disadvantage markers and follow-up PedsQL scores, our findings suggest that receipt of inpatient care improved perceptions of physical functioning to a greater extent for patients with more social disadvantage markers (especially patients with =/> 3 social disadvantage markers). There are several potential reasons for these findings.
One possibility is that caregivers and/or patients with more social disadvantage markers are more influenced by context when assessing physical functioning. This could lead to an underestimation of functioning when asked to recall baseline physical functioning at the time of acute illness and overestimation of functioning after recovery from an illness. This possibility is consistent with a form of response bias, extreme response tendencies, in which lower socioeconomic subgroups tend to choose the more extreme response options of a scale.28 In the absence of longitudinal assessments of HRQoL across the care continuum over time, disentangling whether these differences are due to response bias or representative of true changes in physical functioning remains challenging.
Given that disparities in physical functioning at baseline were consistent with prior evidence, another possibility is that hospitalization provided an opportunity to address gaps in access and quality that may have existed for patients with social disadvantage in the community setting. The 24/7 nature of hospital care, usually from a multidisciplinary team of providers, lends itself to opportunities to receive intensive education related to the current illness or to address other health concerns that parents or providers identify during a hospital stay. For example, consistent and repetitive asthma education may be more beneficial to patients and families with more social disadvantage markers. The fact that the association between social disadvantage markers and change in physical functioning scores were greater for patients with asthma supports this reasoning. Hospital care may also provide an opportunity to address other unmet medical needs or psychosocial needs by providing efficient access to subspecialists, social workers, or interpreters. Further research is needed to elucidate whether families received additional services in the hospital setting that were not available to them prior to hospitalization, such as consistent interpreter use, social work engagement, and subspecialty/community referrals. Further studies should also determine whether the provision of equitable medical and social support services is associated with improvements in HRQoL disparities. Additionally, studies should examine whether physical functioning improvements following hospitalization return to baseline levels after a longer period of time and, if so, how we might sustain these reductions in HRQoL disparities. Such studies may identify tangible targets and interventions to reduce disparities in HRQoL for these children.
This study highlights the importance of assessing for difficulty/delays accessing care in addition to social disadvantage markers, as this was also a significant predictor of lower child physical functioning. Differences in PedsQL scores between those who reported any versus no difficulty/delays accessing care were more pronounced at baseline compared with follow-up. A possible reason for these findings is that receiving hospital care may have addressed some access to care issues that were present in the outpatient setting, which resulted in improved perceptions of physical functioning. For example, hospital care may mitigate access to care barriers such as limited after-hours clinic appointments, language barriers, and lack of insurance, thus providing some patients with an alternative pathway to address their health concerns. Alternatively, hospital staff may assist families in scheduling follow-up appointments with the patient’s primary medical home after discharge, which potentially reduced some access to care barriers. The question is whether these disparities will widen once again after a longer follow-up period if families continue facing barriers to accessing needed care in the outpatient setting.
The results of the effect modification analysis demonstrated that the association between social disadvantage and change in PedsQL scores from baseline to follow-up was not significantly different based on a child’s ability to access care. In our stratified analysis, difficulty/delays accessing care added to baseline disparities at each social disadvantage level but did not alter how perceptions of physical functioning change over time. Therefore, physical functioning improvements may rely more heavily on the type of care received within the hospital setting as opposed to accessing care in the first place. However, future studies should examine whether access to high-quality care instead of simply measuring difficulty/delays in accessing care would lead to different results. Access to a comprehensive medical home may be a better measure to assess for effect modification because it measures features beyond access to care, such as continuity, comprehensiveness, communication, and coordination of outpatient care.29-31
If additional studies find evidence that the nature of hospital care, an intensive 24/7 care setting, differentially benefits patients with higher social disadvantage markers (particularly those with =/> 3 markers and chronic illness), this would support the need for systematic screening for social disadvantages or difficulty/delays accessing care in the inpatient setting. Systematic screening could help ensure all patients who may benefit from additional services, such as intensive, culturally tailored education or connections to food, housing, or financial services, will in fact receive them, which may lead to sustained reductions in health disparities.20 Further research into pairing validated screening tools with proven interventions is needed.32
This study has additional limitations aside from those noted above. First, we did not reassess perceived or actual access to care after hospitalization, which may have allowed for analyses to examine access to care as a mediator between social disadvantage and lower child physical functioning. Second, this study included only English- and Spanish-speaking patients and families. Patients with less commonly spoken languages may experience more difficulty accessing or navigating the health system, which may further impact access to care and HRQoL. Third, we had a considerable amount of missing social disadvantage marker data (mainly income); however, our sensitivity analyses did not result in significantly different or clinically meaningful differences in our findings. Insurance status is more feasible to obtain from administrative data and could serve as a proxy for income or as an additional social disadvantage marker in future studies. Finally, we could calculate illness severity only for patients with asthma based on the available data; therefore, we could not adequately control for illness severity across all conditions.
CONCLUSIONS
Social disadvantage was associated with lower child physical functioning before hospitalization, but differences were not apparent after hospitalization for children with acute respiratory illness. Caregiver-perceived difficulty/delays accessing care was found to be an additional predictor of lower physical functioning at baseline but did not significantly alter the association between social disadvantage and improvement in physical functioning over time. Further studies are needed to understand how hospital care may differentially impact child physical functioning for patients with higher social disadvantage makers in order to sustain improvements in HRQoL disparities.
Acknowledgments
The authors thank the following individuals of the Pediatric Respiratory Illness Measurement System (PRIMES) study team for their contributions to this work: Karen M. Wilson, New York, New York; Ricardo A. Quinonez, Houston, Texas; Joyee G. Vachani, Houston, Texas; and Amy Tyler, Aurora, Colorado. We would also like to thank the Pediatric Research in Inpatient Settings Network for facilitating this work.
Examining disparities in health-related quality of life (HRQoL) outcomes in children provides a unique patient-centered perspective on pediatric health services equity.1,2 Prior studies have demonstrated the relationship between minority race, low socioeconomic status, and lower maternal education with poorer HRQoL outcomes in children.3-6 Some studies have also shown a dose-response relationship between social disadvantage markers and poorer child health status.7,8 Furthermore, the associations between social disadvantage and poor access to care,9-11 and between poor access to care and lower HRQoL, are also well established.12-14
Examining HRQoL before and after hospitalization can further our understanding of how disparities in HRQoL may change once children engage with the medical system for an acute illness.15 Children requiring hospitalization constitute a useful population for examination of this question as they represent a group of children with variable social disadvantage markers and access to outpatient care.16 Although interventions to address social determinants of health for patients with social disadvantages have been associated with within-group improvements in HRQoL, none have assessed changes in disparities as an outcome.17 Furthermore, many of these studies were conducted in the outpatient setting,18,19 whereas hospitalization provides an additional point of care to address the social determinants of health for vulnerable families.20 Even for short hospitalizations, the 24/7 nature of hospital care provides the opportunity for frequent interactions with clinicians, nurses, and support staff to clarify illness-related questions, discuss other health concerns and unmet needs, and connect with social services or community resources. These opportunities may be particularly important for families with a higher number of social disadvantage markers and even more beneficial to those with difficulty accessing needed care from their primary medical home.
In this study, we focused on children with common respiratory illnesses (asthma, bronchiolitis, and pneumonia), which constitute the majority of childhood hospitalizations.21 Additionally, we only focused on the child’s physical functioning component of HRQoL because this component is most likely to improve after hospitalization for children with an acute respiratory illness.22 A prior study examining HRQoL before and after hospitalization demonstrated that most children return to and/or surpass their baseline physical functioning by 1 month after hospital discharge.23
Our primary objective was to examine associations between several markers of social disadvantage, access to care, and child physical functioning before and after hospitalization for acute respiratory illness. Second, we aimed to understand if access to care (defined as perceived difficulty/delays getting care) acts as an independent predictor of improvement in physical functioning from baseline to follow-up and/or if it modifies the relationship between social disadvantage and improvement in physical functioning (Appendix Figure).
METHODS
Study Design and Population
This study was nested within a multicenter, prospective cohort study of children who were hospitalized for asthma, bronchiolitis, or pneumonia between July 2014 and June 2016 at one of five children’s hospitals in the Pediatric Research in Inpatient Settings Network.24
We approached families for study participation within 72 hours of admission to the hospital using a standard protocol. Patients and their caregivers were eligible to participate in the study if the patient was 2 weeks to 16 years old and if the primary caregiver’s preferred language for medical communication was either English or Spanish. Patients with chronic medical conditions (except asthma), with moderate to severe developmental delay, with a history of prematurity <32 weeks, or who received care in the intensive care unit were excluded. Patients could only participate in the study once.
The study team set out to enroll an even number of patients across all three conditions. If a patient’s discharge diagnosis differed from their admission diagnosis (eg, from bronchiolitis to pneumonia), discharge diagnosis was used for condition group assignment. If the discharge diagnosis was not one of these three respiratory conditions, we excluded the patient from further analysis.
Data Collection
We collected data using two surveys. The first survey was administered within 72 hours of admission. This survey asked questions related to (1) caregiver-reported markers of social disadvantage, (2) caregiver perceptions of access to care, and (3) caregiver- and patient-reported assessments of physical functioning. The second survey was administered within 2 to 8 weeks after the patient’s discharge and included a second assessment of physical functioning.
Social Disadvantage
Patients were considered to have a marker of social disadvantage if their caregiver reported (1) being of non-White race and/or Hispanic ethnicity, (2) primarily speaking a language other than English at home and not speaking English very well (ie, limited English proficiency), (3) attaining at most a high school or equivalent degree, or (4) having a =/<$30,000 annual household income.
Access to Care
We used the following survey item from the 2009-2010 National Survey of Children with Special Health Care Needs25 to measure caregiver perceptions of access to care: “In the last six months, did you have any difficulties or delays getting care for your child because there were waiting lists, backlogs, or other problems getting an appointment?” We narrowed the original assessment time frame from 12 months to 6 months to provide a more proximal assessment of access in relation to the hospitalization.
Child Physical Functioning
We assessed child physical functioning using the physical functioning domain of the Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales and PedsQL Infant Scales, which have been validated for use in the inpatient setting.22 Caregivers completed one of these scales based on their child’s age. Assenting patients 8 to 16 years old completed the self-report PedsQL 4.0 Generic Core Scales instrument. When completing the first PedsQL survey, caregivers and patients reflected on the previous month before their child (or they) became ill to obtain a baseline physical functioning assessment.23 When completing the second PedsQL survey, caregivers and patients reflected on the past 7 days to obtain a follow-up assessment.
All study procedures were approved by the Western Institutional Review Board (IRB) or the participating hospitals’ IRB.
Statistical Analysis
Patients with no missing data for all four social disadvantage markers were categorized based on the number of markers they reported: none, one, two, or three or more markers. We combined patients with three and four social disadvantage markers into one group to maximize power for the analyses. We dichotomized the access to care variable and coded response options as “no difficulty/delays accessing care” if the caregiver chose “Never” and “any difficulty/delays accessing care” if they chose “Sometimes/Usually/Always.”
For each patient–caregiver dyad, PedsQL items were scored using a standard method in which higher scores reflected better functioning.22 A single set of PedsQL scores was used for each patient–caregiver dyad. We used self-reported patient scores if the patient completed the PedsQL instrument; otherwise, we used proxy-reported caregiver scores. Intraclass correlations between child self-report and parent proxy-report demonstrate moderate to good agreement above age 8 years.26 We computed a change in the physical functioning score by subtracting the baseline score from the follow-up score. The minimal clinically important difference (MCID) for the PedsQL instrument is 4.5 points, which we used to identify clinically meaningful differences.13
Analysis of variance models were constructed to test for differences in mean baseline and follow-up PedsQL scores (dependent variable) between the following independent variables: (1) social disadvantage groups and (2) those who reported having any difficulty/delays accessing care compared with those who did not. Only patient–caregiver dyads with both baseline and follow-up assessments were included in these analyses. Mixed-effects linear regression models were constructed to identify clinically meaningful differences in PedsQL scores between groups (MCID =/> 4.5) with adjustment for patient age, gender, respiratory condition, days between surveys, and hospital site as fixed effects. Site-specific random effects were included to account for within-hospital clustering. A similarly adjusted mixed-effects linear regression model was constructed to examine whether having any difficulty/delays accessing care modified the association between social disadvantage and PedsQL change scores (eg, an improvement from baseline to follow-up).
Because 17% of respondents had missing data for at least one social disadvantage marker, sensitivity analyses were conducted using multiple imputation to account for missing social disadvantage markers using chained equations.27 Sensitivity analyses were also conducted to adjust for severity of illness using vital sign data within the first 24 hours, which could only be validly captured on patients with asthma within our dataset. By restricting this latter analysis to patients with asthma, we were able to examine the relationships of interest in a population with chronic disease.
RESULTS
The study sample included 1,860 patients, of which 1,325 had both baseline and follow-up PedsQL data (71%). Descriptive statistics were similar between those who completed the baseline and follow-up surveys (Table 1).
Twenty-two percent of patients had >/=3 social disadvantages and 30% of caregivers reported having any difficulty/delays accessing care. The mean follow-up PedsQL score was higher than the baseline score (90.4 vs 82.5; Table 1).
Social Disadvantage Markers and PedsQL Scores
The number of social disadvantage markers was inversely related to mean baseline PedsQL scores, but there was no difference in mean follow-up PedsQL scores between social disadvantage groups (Table 2). In adjusted analyses, the mean baseline PedsQL score was −6.1 points (95% CI: −8.7, −3.5) lower for patients with >/= 3 social disadvantage markers compared with patients with no social disadvantage markers, which exceeded the scale’s MCID.
Difficulty/Delays Accessing Care and PedsQL Scores
Having any difficulty/delays accessing care was significantly associated with lower baseline and follow-up PedsQL scores (Table 2). In adjusted analyses, the difference in baseline scores was 5.2 points (95% CI: −7.2, −3.2), which exceedes the scale’s MCID.
Interaction Between Social Disadvantage Markers, Difficulty/Delays Accessing Care, and Change in PedsQL Scores from Baseline to Follow-Up
While having =/>2 social disadvantage markers and difficulty/delays accessing care were each positively associated with changes in PedsQL scores from baseline to follow-up (Table 3), only patients with =/> 3 social disadvantage markers exceeded the PedsQL MCID. In stratified analyses, patients with a combination of social disadvantage makers and difficulties/delays accessing care had lower baseline PedsQL scores and greater change in PedsQL scores from baseline to follow-up compared with those without difficulties/delays accessing care (Figure). However, having any difficulty/delays accessing care did not significantly modify the relationship between social disadvantage and change in PedsQL scores, as none of the interaction terms were significant (Table 3, Model 3).
Sensitivity Analysis
Baseline, follow-up, and change in PedsQL scores were similar to our main analysis after performing multiple imputation for missing social disadvantage markers (Supplemental Table 1). Findings were also similar for patients with a diagnosis of asthma only; however, changes in PedsQL scores were greater in magnitude (Appendix Table 2).
DISCUSSION
This study examined the relationship between social disadvantage and child physical functioning before and after hospitalization for acute respiratory illness. Study findings indicated that patients with higher numbers of social disadvantage markers reported lower PedsQL scores before hospitalization; however, differences in PedsQL scores were not apparent after hospitalization. Patients who experienced difficulty/delays accessing care also reported lower PedsQL scores at baseline. This difference was still significant but did not exceed the PedsQL MCID threshold after hospitalization. Difficulty/delays accessing care appeared to be an additional social disadvantage marker; however, it did not modify the relationship between social disadvantage and improvement in physical functioning.
The study findings at baseline are consistent with prior studies demonstrating a negative association between social disadvantage markers and HRQoL and a cumulative effect based on the number of social disadvantages.3,4,7,8 This study adds to the existing literature by examining how this relationship changes after hospitalization. As evidenced by the lack of association between social disadvantage markers and follow-up PedsQL scores, our findings suggest that receipt of inpatient care improved perceptions of physical functioning to a greater extent for patients with more social disadvantage markers (especially patients with =/> 3 social disadvantage markers). There are several potential reasons for these findings.
One possibility is that caregivers and/or patients with more social disadvantage markers are more influenced by context when assessing physical functioning. This could lead to an underestimation of functioning when asked to recall baseline physical functioning at the time of acute illness and overestimation of functioning after recovery from an illness. This possibility is consistent with a form of response bias, extreme response tendencies, in which lower socioeconomic subgroups tend to choose the more extreme response options of a scale.28 In the absence of longitudinal assessments of HRQoL across the care continuum over time, disentangling whether these differences are due to response bias or representative of true changes in physical functioning remains challenging.
Given that disparities in physical functioning at baseline were consistent with prior evidence, another possibility is that hospitalization provided an opportunity to address gaps in access and quality that may have existed for patients with social disadvantage in the community setting. The 24/7 nature of hospital care, usually from a multidisciplinary team of providers, lends itself to opportunities to receive intensive education related to the current illness or to address other health concerns that parents or providers identify during a hospital stay. For example, consistent and repetitive asthma education may be more beneficial to patients and families with more social disadvantage markers. The fact that the association between social disadvantage markers and change in physical functioning scores were greater for patients with asthma supports this reasoning. Hospital care may also provide an opportunity to address other unmet medical needs or psychosocial needs by providing efficient access to subspecialists, social workers, or interpreters. Further research is needed to elucidate whether families received additional services in the hospital setting that were not available to them prior to hospitalization, such as consistent interpreter use, social work engagement, and subspecialty/community referrals. Further studies should also determine whether the provision of equitable medical and social support services is associated with improvements in HRQoL disparities. Additionally, studies should examine whether physical functioning improvements following hospitalization return to baseline levels after a longer period of time and, if so, how we might sustain these reductions in HRQoL disparities. Such studies may identify tangible targets and interventions to reduce disparities in HRQoL for these children.
This study highlights the importance of assessing for difficulty/delays accessing care in addition to social disadvantage markers, as this was also a significant predictor of lower child physical functioning. Differences in PedsQL scores between those who reported any versus no difficulty/delays accessing care were more pronounced at baseline compared with follow-up. A possible reason for these findings is that receiving hospital care may have addressed some access to care issues that were present in the outpatient setting, which resulted in improved perceptions of physical functioning. For example, hospital care may mitigate access to care barriers such as limited after-hours clinic appointments, language barriers, and lack of insurance, thus providing some patients with an alternative pathway to address their health concerns. Alternatively, hospital staff may assist families in scheduling follow-up appointments with the patient’s primary medical home after discharge, which potentially reduced some access to care barriers. The question is whether these disparities will widen once again after a longer follow-up period if families continue facing barriers to accessing needed care in the outpatient setting.
The results of the effect modification analysis demonstrated that the association between social disadvantage and change in PedsQL scores from baseline to follow-up was not significantly different based on a child’s ability to access care. In our stratified analysis, difficulty/delays accessing care added to baseline disparities at each social disadvantage level but did not alter how perceptions of physical functioning change over time. Therefore, physical functioning improvements may rely more heavily on the type of care received within the hospital setting as opposed to accessing care in the first place. However, future studies should examine whether access to high-quality care instead of simply measuring difficulty/delays in accessing care would lead to different results. Access to a comprehensive medical home may be a better measure to assess for effect modification because it measures features beyond access to care, such as continuity, comprehensiveness, communication, and coordination of outpatient care.29-31
If additional studies find evidence that the nature of hospital care, an intensive 24/7 care setting, differentially benefits patients with higher social disadvantage markers (particularly those with =/> 3 markers and chronic illness), this would support the need for systematic screening for social disadvantages or difficulty/delays accessing care in the inpatient setting. Systematic screening could help ensure all patients who may benefit from additional services, such as intensive, culturally tailored education or connections to food, housing, or financial services, will in fact receive them, which may lead to sustained reductions in health disparities.20 Further research into pairing validated screening tools with proven interventions is needed.32
This study has additional limitations aside from those noted above. First, we did not reassess perceived or actual access to care after hospitalization, which may have allowed for analyses to examine access to care as a mediator between social disadvantage and lower child physical functioning. Second, this study included only English- and Spanish-speaking patients and families. Patients with less commonly spoken languages may experience more difficulty accessing or navigating the health system, which may further impact access to care and HRQoL. Third, we had a considerable amount of missing social disadvantage marker data (mainly income); however, our sensitivity analyses did not result in significantly different or clinically meaningful differences in our findings. Insurance status is more feasible to obtain from administrative data and could serve as a proxy for income or as an additional social disadvantage marker in future studies. Finally, we could calculate illness severity only for patients with asthma based on the available data; therefore, we could not adequately control for illness severity across all conditions.
CONCLUSIONS
Social disadvantage was associated with lower child physical functioning before hospitalization, but differences were not apparent after hospitalization for children with acute respiratory illness. Caregiver-perceived difficulty/delays accessing care was found to be an additional predictor of lower physical functioning at baseline but did not significantly alter the association between social disadvantage and improvement in physical functioning over time. Further studies are needed to understand how hospital care may differentially impact child physical functioning for patients with higher social disadvantage makers in order to sustain improvements in HRQoL disparities.
Acknowledgments
The authors thank the following individuals of the Pediatric Respiratory Illness Measurement System (PRIMES) study team for their contributions to this work: Karen M. Wilson, New York, New York; Ricardo A. Quinonez, Houston, Texas; Joyee G. Vachani, Houston, Texas; and Amy Tyler, Aurora, Colorado. We would also like to thank the Pediatric Research in Inpatient Settings Network for facilitating this work.
1. Szilagyi PG, Schor EL. The health of children. Health Serv Res. 1998;33(4 Pt 2):1001-1039.
2. Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005;3(1):34. https://doi.org/10.1186/1477-7525-3-34.
3. von Rueden U, Gosch A, Rajmil L, Bisegger C, Ravens-Sieberer U. Socioeconomic determinants of health related quality of life in childhood and adolescence: results from a European study. J Epidemiol Community Health. 2006;60(2):130-135. https://doi.org/10.1136/jech.2005.039792.
4. Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137(3):642-650. https://doi.org/10.1378/chest.09-0345.
5. Flores G, Tomany-Korman SC, Corey CR, Freeman HE, Shapiro MF. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2):e286-98. https://doi.org/10.1542/peds.2007-1243.
6. Fedele DA, Molzon ES, Eddington AR, Hullmann SE, Mullins LL, Gillaspy SG. Perceived barriers to care in a pediatric medical home: the moderating role of caregiver minority status. Clin Pediatr (Phila). 2014;53(4):351-355. https://doi.org/10.1177/0009922813507994.
7. Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337-344. https://doi.org/10.1542/peds.2007-0447.
8. Bauman LJ, Silver EJ, Stein REK. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321-1328. https://doi.org/10.1542/peds.2005-1647.
9. Andrulis DP. Moving beyond the status quo in reducing racial and ethnic disparities in children’s health. Public Health Rep. 2005;120(4):370-377. https://doi.org/10.1177/003335490512000403.
10. Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: has anything changed over the years? Int J Equity Health. 2013;12:10. https://doi.org/10.1186/1475-9276-12-10.
11. Seid M, Stevens GD, Varni JW. Parents’ perceptions of pediatric primary care quality: effects of race/ethnicity, language, and access. Health Serv Res. 2003;38(4):1009-1031. https://doi.org/10.1111/1475-6773.00160.
12. Seid M, Varni JW, Cummings L, Schonlau M. The impact of realized access to care on health-related quality of life: a two-year prospective cohort study of children in the California State Children’s Health Insurance Program. J Pediatr. 2006;149(3):354-361. https://doi.org/10.1016/j.jpeds.2006.04.024.
13. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329-341. https://doi.xorg/10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2.
14. Simon AE, Chan KS, Forrest CB. Assessment of children’s health-related quality of life in the united states with a multidimensional index. Pediatrics. 2008;121(1):e118-e126. https://doi.org/10.1542/peds.2007-0480.
15. Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: what can a clinician do? Pediatrics. 2015;136(5):961-968. https://doi.org/10.1542/peds.2014-4126.
16. Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524-529. https://doi.org/10.1542/peds.107.3.524.
17. Lion KC, Raphael JL. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135(2):354-361. https://doi.org/10.1542/peds.2014-2982.
18. Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14:S8-S17. https://doi.org/10.1097/01.PHH.0000338382.36695.42.
19. Beck AF, Cohen AJ, Colvin JD, et al. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84(1):10-21. https://doi.org/10.1038/s41390-018-0012-1.
20. Shah AN, Simmons J, Beck AF. Adding a vital sign: considering the utility of place-based measures in health care settings. Hosp Pediatr. 2018;8(2):112-114. https://doi.org/10.1542/hpeds.2017-0219.
21. Leyenaar JK, Ralston SL, Shieh M-S, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624.
22. Desai AD, Zhou C, Stanford S, Haaland W, Varni JW, Mangione-Smith RM. Validity and responsiveness of the pediatric quality of life inventory (PedsQL) 4.0 generic core scales in the pediatric inpatient setting. JAMA Pediatr. 2014;168(12):1114-1121. https://doi.org/10.1001/jamapediatrics.2014.1600.
23. Rabbitts JA, Palermo TM, Zhou C, Mangione-Smith R. Pain and health-related quality of life after pediatric inpatient surgery. J Pain. 2015;16(12):1334-1341. https://doi.org/10.1016/j.jpain.2015.09.005.
24. Mangione-Smith R, Zhou C, Williams DJ, et al. Pediatric respiratory illness measurement system (PRIMES) scores and outcomes. Pediatrics. 2019;144(2):e20190242. https://doi.org/10.1542/peds.2019-0242.
25. Child and Adolescent Health Measurement Initiative. National survey of children with special health care needs (NS-CSHCN), 2009-2010. Available at: http://childhealthdata.org/learn/NS-CSHCN/topics_questions. Accessed on September 20, 2018.
26. Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:1. https://doi.org/10.1186/1477-7525-5-1.
27. Buuren S van, Groothuis-Oudshoorn K. Mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. https://doi.org/10.18637/jss.v045.i03.
28. Elliott MN, Haviland AM, Kanouse DE, Hambarsoomian K, Hays RD. Adjusting for subgroup differences in extreme response tendency in ratings of health care: impact on disparity estimates. Heal Serv Res. 2009;44(2 Pt 1):542-561. https://doi.org/10.1111/j.1475-6773.2008.00922.x.
29. Stevens GD, Vane C, Cousineau MR. Association of experiences of medical home quality with health-related quality of life and school engagement among Latino children in low-income families. Health Serv Res. 2011;46(6pt1):1822-1842. https://doi.org/10.1111/j.1475-6773.2011.01292.x.
30. Long WE, Bauchner H, Sege RD, Cabral HJ, Garg A. The value of the medical home for children without special health care needs. Pediatrics. 2012;129(1):87-98. https://doi.org/10.1542/peds.2011-1739.
31. Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604-611. https://doi.org/10.1542/peds.2009-3555.
32. Sokol R, Austin A, Chandler C, et al. Screening children for social determinants of health: a systematic review. Pediatrics. 2019;144(4):e20191622. https://doi.org/10.1542/peds.2019-1622.
1. Szilagyi PG, Schor EL. The health of children. Health Serv Res. 1998;33(4 Pt 2):1001-1039.
2. Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005;3(1):34. https://doi.org/10.1186/1477-7525-3-34.
3. von Rueden U, Gosch A, Rajmil L, Bisegger C, Ravens-Sieberer U. Socioeconomic determinants of health related quality of life in childhood and adolescence: results from a European study. J Epidemiol Community Health. 2006;60(2):130-135. https://doi.org/10.1136/jech.2005.039792.
4. Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137(3):642-650. https://doi.org/10.1378/chest.09-0345.
5. Flores G, Tomany-Korman SC, Corey CR, Freeman HE, Shapiro MF. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2):e286-98. https://doi.org/10.1542/peds.2007-1243.
6. Fedele DA, Molzon ES, Eddington AR, Hullmann SE, Mullins LL, Gillaspy SG. Perceived barriers to care in a pediatric medical home: the moderating role of caregiver minority status. Clin Pediatr (Phila). 2014;53(4):351-355. https://doi.org/10.1177/0009922813507994.
7. Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337-344. https://doi.org/10.1542/peds.2007-0447.
8. Bauman LJ, Silver EJ, Stein REK. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321-1328. https://doi.org/10.1542/peds.2005-1647.
9. Andrulis DP. Moving beyond the status quo in reducing racial and ethnic disparities in children’s health. Public Health Rep. 2005;120(4):370-377. https://doi.org/10.1177/003335490512000403.
10. Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: has anything changed over the years? Int J Equity Health. 2013;12:10. https://doi.org/10.1186/1475-9276-12-10.
11. Seid M, Stevens GD, Varni JW. Parents’ perceptions of pediatric primary care quality: effects of race/ethnicity, language, and access. Health Serv Res. 2003;38(4):1009-1031. https://doi.org/10.1111/1475-6773.00160.
12. Seid M, Varni JW, Cummings L, Schonlau M. The impact of realized access to care on health-related quality of life: a two-year prospective cohort study of children in the California State Children’s Health Insurance Program. J Pediatr. 2006;149(3):354-361. https://doi.org/10.1016/j.jpeds.2006.04.024.
13. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329-341. https://doi.xorg/10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2.
14. Simon AE, Chan KS, Forrest CB. Assessment of children’s health-related quality of life in the united states with a multidimensional index. Pediatrics. 2008;121(1):e118-e126. https://doi.org/10.1542/peds.2007-0480.
15. Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: what can a clinician do? Pediatrics. 2015;136(5):961-968. https://doi.org/10.1542/peds.2014-4126.
16. Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524-529. https://doi.org/10.1542/peds.107.3.524.
17. Lion KC, Raphael JL. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135(2):354-361. https://doi.org/10.1542/peds.2014-2982.
18. Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14:S8-S17. https://doi.org/10.1097/01.PHH.0000338382.36695.42.
19. Beck AF, Cohen AJ, Colvin JD, et al. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84(1):10-21. https://doi.org/10.1038/s41390-018-0012-1.
20. Shah AN, Simmons J, Beck AF. Adding a vital sign: considering the utility of place-based measures in health care settings. Hosp Pediatr. 2018;8(2):112-114. https://doi.org/10.1542/hpeds.2017-0219.
21. Leyenaar JK, Ralston SL, Shieh M-S, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. https://doi.org/10.1002/jhm.2624.
22. Desai AD, Zhou C, Stanford S, Haaland W, Varni JW, Mangione-Smith RM. Validity and responsiveness of the pediatric quality of life inventory (PedsQL) 4.0 generic core scales in the pediatric inpatient setting. JAMA Pediatr. 2014;168(12):1114-1121. https://doi.org/10.1001/jamapediatrics.2014.1600.
23. Rabbitts JA, Palermo TM, Zhou C, Mangione-Smith R. Pain and health-related quality of life after pediatric inpatient surgery. J Pain. 2015;16(12):1334-1341. https://doi.org/10.1016/j.jpain.2015.09.005.
24. Mangione-Smith R, Zhou C, Williams DJ, et al. Pediatric respiratory illness measurement system (PRIMES) scores and outcomes. Pediatrics. 2019;144(2):e20190242. https://doi.org/10.1542/peds.2019-0242.
25. Child and Adolescent Health Measurement Initiative. National survey of children with special health care needs (NS-CSHCN), 2009-2010. Available at: http://childhealthdata.org/learn/NS-CSHCN/topics_questions. Accessed on September 20, 2018.
26. Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:1. https://doi.org/10.1186/1477-7525-5-1.
27. Buuren S van, Groothuis-Oudshoorn K. Mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. https://doi.org/10.18637/jss.v045.i03.
28. Elliott MN, Haviland AM, Kanouse DE, Hambarsoomian K, Hays RD. Adjusting for subgroup differences in extreme response tendency in ratings of health care: impact on disparity estimates. Heal Serv Res. 2009;44(2 Pt 1):542-561. https://doi.org/10.1111/j.1475-6773.2008.00922.x.
29. Stevens GD, Vane C, Cousineau MR. Association of experiences of medical home quality with health-related quality of life and school engagement among Latino children in low-income families. Health Serv Res. 2011;46(6pt1):1822-1842. https://doi.org/10.1111/j.1475-6773.2011.01292.x.
30. Long WE, Bauchner H, Sege RD, Cabral HJ, Garg A. The value of the medical home for children without special health care needs. Pediatrics. 2012;129(1):87-98. https://doi.org/10.1542/peds.2011-1739.
31. Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604-611. https://doi.org/10.1542/peds.2009-3555.
32. Sokol R, Austin A, Chandler C, et al. Screening children for social determinants of health: a systematic review. Pediatrics. 2019;144(4):e20191622. https://doi.org/10.1542/peds.2019-1622.
© 2020 Society of Hospital Medicine
Patient Preferences for Physician Attire: A Multicenter Study in Japan
The patient-physician relationship is critical for ensuring the delivery of high-quality healthcare. Successful patient-physician relationships arise from shared trust, knowledge, mutual respect, and effective verbal and nonverbal communication. The ways in which patients experience healthcare and their satisfaction with physicians affect a myriad of important health outcomes, such as adherence to treatment and outcomes for conditions such as hypertension and diabetes mellitus.1-5 One method for potentially enhancing patient satisfaction is through understanding how patients wish their physicians to dress6-8 and tailoring attire to match these expectations. In addition to our systematic review,9 a recent large-scale, multicenter study in the United States revealed that most patients perceive physician attire as important, but that preferences for specific types of attire are contextual.9,10 For example, elderly patients preferred physicians in formal attire and white coat, while scrubs with white coat or scrubs alone were preferred for emergency department (ED) physicians and surgeons, respectively. Moreover, regional variation regarding attire preference was also observed in the US, with preferences for more formal attire in the South and less formal in the Midwest.
Geographic variation, regarding patient preferences for physician dress, is perhaps even more relevant internationally. In particular, Japan is considered to have a highly contextualized culture that relies on nonverbal and implicit communication. However, medical professionals have no specific dress code and, thus, don many different kinds of attire. In part, this may be because it is not clear whether or how physician attire impacts patient satisfaction and perceived healthcare quality in Japan.11-13 Although previous studies in Japan have suggested that physician attire has a considerable influence on patient satisfaction, these studies either involved a single department in one hospital or a small number of respondents.14-17 Therefore, we performed a multicenter, cross-sectional study to understand patients’ preferences for physician attire in different clinical settings and in different geographic regions in Japan.
METHODS
Study Population
We conducted a cross-sectional, questionnaire-based study from 2015 to 2017, in four geographically diverse hospitals in Japan. Two of these hospitals, Tokyo Joto Hospital and Juntendo University Hospital, are located in eastern Japan whereas the others, Kurashiki Central Hospital and Akashi Medical Center, are in western Japan.
Questionnaires were printed and randomly distributed by research staff to outpatients in waiting rooms and inpatients in medical wards who were 20 years of age or older. We placed no restriction on ward site or time of questionnaire distribution. Research staff, including physicians, nurses, and medical clerks, were instructed to avoid guiding or influencing participants’ responses. Informed consent was obtained by the staff; only those who provided informed consent participated in the study. Respondents could request assistance with form completion from persons accompanying them if they had difficulties, such as physical, visual, or hearing impairments. All responses were collected anonymously. The study was approved by the ethics committees of all four hospitals.
Questionnaire
We used a modified version of the survey instrument from a prior study.10 The first section of the survey showed photographs of either a male or female physician with 7 unique forms of attire, including casual, casual with white coat, scrubs, scrubs with white coat, formal, formal with white coat, and business suit (Figure 1). Given the Japanese context of this study, the language was translated to Japanese and photographs of physicians of Japanese descent were used. Photographs were taken with attention paid to achieving constant facial expressions on the physicians as well as in other visual cues (eg, lighting, background, pose). The physician’s gender and attire in the first photograph seen by each respondent were randomized to prevent bias in ordering, priming, and anchoring; all other sections of the survey were identical.
Respondents were first asked to rate the standalone, randomized physician photograph using a 1-10 scale across five domains (ie, how knowledgeable, trustworthy, caring, and approachable the physician appeared and how comfortable the physician’s appearance made the respondent feel), with a score of 10 representing the highest rating. Respondents were subsequently given 7 photographs of the same physician wearing various forms of attire. Questions were asked regarding preference of attire in varied clinical settings (ie, primary care, ED, hospital, surgery, overall preference). To identify the influence of and respondent preferences for physician dress and white coats, a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was employed. The scale was trichotomized into “disagree” (1, 2), “neither agree nor disagree” (3), and “agree” (4, 5) for analysis. Demographic data, including age, gender, education level, nationality (Japanese or non-Japanese), and number of physicians seen in the past year were collected.
Outcomes and Sample Size Calculation
The primary outcome of attire preference was calculated as the mean composite score of the five individual rating domains (ie, knowledgeable, trustworthy, caring, approachable, and comfortable), with the highest score representing the most preferred form of attire. We also assessed variation in preferences for physician attire by respondent characteristics, such as age and gender.
Sample size estimation was based on previous survey methodology.10 The Likert scale range for identifying influence of and respondent preferences for physician dress and white coats was 1-5 (“strongly disagree” to “strongly agree”). The scale range for measuring preferences for the randomized attire photograph was 1-10. An assumption of normality was made regarding responses on the 1-10 scale. An estimated standard deviation of 2.2 was assumed, based on prior findings.10 Based on these assumptions and the inclusion of at least 816 respondents (assuming a two-sided alpha error of 0.05), we expected to have 90% capacity to detect differences for effect sizes of 0.50 on the 1-10 scale.
Statistical Analyses
Paper-based survey data were entered independently and in duplicate by the study team. Respondents were not required to answer all questions; therefore, the denominator for each question varied. Data were reported as mean and standard deviation (SD) or percentages, where appropriate. Differences in the mean composite rating scores were assessed using one-way ANOVA with the Tukey method for pairwise comparisons. Differences in proportions for categorical data were compared using the Z-test. Chi-squared tests were used for bivariate comparisons between respondent age, gender, and level of education and corresponding respondent preferences. All analyses were performed using Stata 14 MP/SE (Stata Corp., College Station, Texas, USA).
RESULTS
Characteristics of Participants
Between December 1, 2015 and October 30, 2017, a total of 2,020 surveys were completed by patients across four academic hospitals in Japan. Of those, 1,960 patients (97.0%) completed the survey in its entirety. Approximately half of the respondents were 65 years of age or older (49%), of female gender (52%), and reported receiving care in the outpatient setting (53%). Regarding use of healthcare, 91% had seen more than one physician in the year preceding the time of survey completion (Table 1).
Ratings of Physician Attire
Compared with all forms of attire depicted in the survey’s first standalone photograph, respondents rated “casual attire with white coat” the highest (Figure 2). The mean composite score for “casual attire with white coat” was 7.1 (standard deviation [SD] = 1.8), and this attire was set as the referent group. Cronbach’s alpha, for the five items included in the composite score, was 0.95. However, “formal attire with white coat” was rated almost as highly as “casual attire with white coat” with an overall mean composite score of 7.0 (SD = 1.6).
Variation in Preference for Physician Attire by Clinical Setting
Preferences for physician attire varied by clinical care setting. Most respondents preferred “casual attire with white coat” or “formal attire with white coat” in both primary care and hospital settings, with a slight preference for “casual attire with white coat.” In contrast, respondents preferred “scrubs without white coat” in the ED and surgical settings. When asked about their overall preference, respondents reported they felt their physician should wear “formal attire with white coat” (35%) or “casual attire with white coat” (30%; Table 2). When comparing the group of photographs of physicians with white coats to the group without white coats (Figure 1), respondents preferred physicians wearing white coats overall and specifically when providing care in primary care and hospital settings. However, they preferred physicians without white coats when providing care in the ED (P < .001). With respect to surgeons, there was no statistically significant difference between preference for white coats and no white coats. These results were similar for photographs of both male and female physicians.
When asked whether physician dress was important to them and if physician attire influenced their satisfaction with the care received, 61% of participants agreed that physician dress was important, and 47% agreed that physician attire influenced satisfaction (Appendix Table 1). With respect to appropriateness of physicians dressing casually over the weekend in clinical settings, 52% responded that casual wear was inappropriate, while 31% had a neutral opinion.
Participants were asked whether physicians should wear a white coat in different clinical settings. Nearly two-thirds indicated a preference for white coats in the office and hospital (65% and 64%, respectively). Responses regarding whether emergency physicians should wear white coats were nearly equally divided (Agree, 37%; Disagree, 32%; Neither Agree nor Disagree, 31%). However, “scrubs without white coat” was most preferred (56%) when patients were given photographs of various attire and asked, “Which physician would you prefer to see when visiting the ER?” Responses to the question “Physicians should always wear a white coat when seeing patients in any setting” varied equally (Agree, 32%; Disagree, 34%; Neither Agree nor Disagree, 34%).
Variation in Preference for Physician Attire by Respondent Demographics
When comparing respondents by age, those 65 years or older preferred “formal attire with white coat” more so than respondents younger than 65 years (Appendix Table 2). This finding was identified in both primary care (36% vs 31%, P < .001) and hospital settings (37% vs 30%, P < .001). Additionally, physician attire had a greater impact on older respondents’ satisfaction and experience (Appendix Table 3). For example, 67% of respondents 65 years and older agreed that physician attire was important, and 54% agreed that attire influenced satisfaction. Conversely, for respondents younger than 65 years, the proportion agreeing with these statements was lower (56% and 41%, both P < .001). When comparing older and younger respondents, those 65 years and older more often preferred physicians wearing white coats in any setting (39% vs 26%, P < .001) and specifically in their office (68% vs 61%, P = .002), the ED (40% vs 34%, P < .001), and the hospital (69% vs 60%, P < .001).
When comparing male and female respondents, male respondents more often stated that physician dress was important to them (men, 64%; women, 58%; P = .002). When comparing responses to the question “Overall, which clothes do you feel a doctor should wear?”, between the eastern and western Japanese hospitals, preferences for physician attire varied.
Variation in Expectations Between Male and Female Physicians
When comparing the ratings of male and female physicians, female physicians were rated higher in how caring (P = .005) and approachable (P < .001) they appeared. However, there were no significant differences in the ratings of the three remaining domains (ie, knowledgeable, trustworthy, and comfortable) or the composite score.
DISCUSSION
Since we employed the same methodology as previous studies conducted in the US10 and Switzerland,18 a notable strength of our approach is that comparisons among these countries can be drawn. For example, physician attire appears to hold greater importance in Japan than in the US and Switzerland. Among Japanese participants, 61% agreed that physician dress is important (US, 53%; Switzerland, 36%), and 47% agreed that physician dress influenced how satisfied they were with their care (US, 36%; Switzerland, 23%).10 This result supports the notion that nonverbal and implicit communications (such as physician dress) may carry more importance among Japanese people.11-13
Regarding preference ratings for type of dress among respondents in Japan, “casual attire with white coat” received the highest mean composite score rating, with “formal attire with white coat” rated second overall. In contrast, US respondents rated “formal attire with white coat” highest and “scrubs with white coat” second.10 Our result runs counter to our expectation in that we expected Japanese respondents to prefer formal attire, since Japan is one of the most formal cultures in the world. One potential explanation for this difference is that the casual style chosen for this study was close to the smart casual style (slightly casual). Most hospitals and clinics in Japan do not allow physicians to wear jeans or polo shirts, which were chosen as the casual attire in the previous US study.
When examining various care settings and physician types, both Japanese and US respondents were more likely to prefer physicians wearing a white coat in the office or hospital.10 However, Japanese participants preferred both “casual attire with white coat” and “formal attire with white coat” equally in primary care or hospital settings. A smaller proportion of US respondents preferred “casual attire with white coat” in primary care (11%) and hospital settings (9%), but more preferred “formal attire with white coat” for primary care (44%) and hospital physicians (39%). In the ED setting, 32% of participants in Japan and 18% in the US disagreed with the idea that physicians should wear a white coat. Among Japanese participants, “scrubs without white coat” was rated highest for emergency physicians (56%) and surgeons (47%), while US preferences were 40% and 42%, respectively.10 One potential explanation is that scrubs-based attire became popular among Japanese ED and surgical contexts as a result of cultural influence and spread from western countries.19, 20
With respect to perceptions regarding physician attire on weekends, 52% of participants considered it inappropriate for a physician to dress casually over the weekend, compared with only 30% in Switzerland and 21% in the US.11,12 Given Japan’s level of formality and the fact that most Japanese physicians continue to work over the weekend,21-23 Japanese patients tend to expect their physicians to dress in more formal attire during these times.
Previous studies in Japan have demonstrated that older patients gave low ratings to scrubs and high ratings to white coat with any attire,15,17 and this was also the case in our study. Perhaps elderly patients reflect conservative values in their preferences of physician dress. Their perceptions may be less influenced by scenes portraying physicians in popular media when compared with the perceptions of younger patients. Though a 2015 systematic review and studies in other countries revealed white coats were preferred regardless of exact dress,9,24-26 they also showed variation in preferences for physician attire. For example, patients in Saudi Arabia preferred white coat and traditional ethnic dress,25 whereas mothers of pediatric patients in Saudi Arabia preferred scrubs for their pediatricians.27 Therefore, it is recommended for internationally mobile physicians to choose their dress depending on a variety of factors including country, context, and patient age group.
Our study has limitations. First, because some physicians presented the surveys to the patients, participants may have responded differently. Second, participants may have identified photographs of the male physician model as their personal healthcare provider (one author, K.K.). To avoid this possible bias, we randomly distributed 14 different versions of physician photographs in the questionnaire. Third, although physician photographs were strictly controlled, the “formal attire and white coat” and “casual attire and white coat” photographs appeared similar, especially given that the white coats were buttoned. Also, the female physician depicted in the photographs did not have the scrub shirt tucked in, while the male physician did. These nuances may have affected participant ratings between groups. Fourth,
In conclusion, patient preferences for physician attire were examined using a multicenter survey with a large sample size and robust survey methodology, thus overcoming weaknesses of previous studies into Japanese attire. Japanese patients perceive that physician attire is important and influences satisfaction with their care, more so than patients in other countries, like the US and Switzerland. Geography, settings of care, and patient age play a role in preferences. As a result, hospitals and health systems may use these findings to inform dress code policy based on patient population and context, recognizing that the appearance of their providers affects the patient-physician relationship. Future research should focus on better understanding the various cultural and societal customs that lead to patient expectations of physician attire.
Acknowledgments
The authors thank Drs. Fumi Takemoto, Masayuki Ueno, Kazuya Sakai, Saori Kinami, and Toshio Naito for their assistance with data collection at their respective sites. Additionally, the authors thank Dr. Yoko Kanamitsu for serving as a model for photographs.
1. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. https://doi.org/ 10.1056/NEJMp1211775.
2. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
3. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39-48. https://doi.org/10.2147/PPA.S24752.
4. Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921-31. https://doi.org/10.1056/NEJMsa080411.
5. O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144-54. https://doi.org/10.1046/j.1525-1497.2002.10431.x.
6. Chung H, Lee H, Chang DS, Kim HS, Park HJ, Chae Y. Doctor’s attire influences perceived empathy in the patient-doctor relationship. Patient Educ Couns. 2012;89(3):387-391. https://doi.org/10.1016/j.pec.2012.02.017.
7. Bianchi MT. Desiderata or dogma: what the evidence reveals about physician attire. J Gen Intern Med. 2008;23(5):641-643. https://doi.org/10.1007/s11606-008-0546-8.
8. Brandt LJ. On the value of an old dress code in the new millennium. Arch Intern Med. 2003;163(11):1277-1281. https://doi.org/10.1001/archinte.163.11.1277.
9. Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature--targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578. https://doi.org/10.1136/bmjopen-2014-006578.
10. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. https://doi.org/10.1136/bmjopen-2017-021239.
11. Rowbury R. The need for more proactive communications. Low trust and changing values mean Japan can no longer fall back on its homogeneity. The Japan Times. 2017, Oct 15;Sect. Opinion. https://www.japantimes.co.jp/opinion/2017/10/15/commentary/japan-commentary/need-proactive-communications/#.Xej7lC3MzUI. Accessed December 5, 2019.
12. Shoji Nishimura ANaST. Communication Style and Cultural Features in High/Low Context Communication Cultures: A Case Study of Finland, Japan and India. Nov 22nd, 2009.
13. Smith RMRSW. The influence of high/low-context culture and power distance on choice of communication media: Students’ media choice to communicate with Professors in Japan and America. Int J Intercultural Relations. 2007;31(4):479-501.
14. Yamada Y, Takahashi O, Ohde S, Deshpande GA, Fukui T. Patients’ preferences for doctors’ attire in Japan. Intern Med. 2010;49(15):1521-1526. https://doi.org/10.2169/internalmedicine.49.3572.
15. Ikusaka M, Kamegai M, Sunaga T, et al. Patients’ attitude toward consultations by a physician without a white coat in Japan. Intern Med. 1999;38(7):533-536. https://doi.org/10.2169/internalmedicine.38.533.
16. Lefor AK, Ohnuma T, Nunomiya S, Yokota S, Makino J, Sanui M. Physician attire in the intensive care unit in Japan influences visitors’ perception of care. J Crit Care. 2018;43:288-293.
17. Kurihara H, Maeno T. Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pac Fam Med. 2014;13(1):2. https://doi.org/10.1186/1447-056X-13-2.
18. Zollinger M, Houchens N, Chopra V, et al. Understanding patient preference for physician attire in ambulatory clinics: a cross-sectional observational study. BMJ Open. 2019;9(5):e026009. https://doi.org/10.1136/bmjopen-2018-026009.
19. Chung JE. Medical Dramas and Viewer Perception of Health: Testing Cultivation Effects. Hum Commun Res. 2014;40(3):333-349.
20. Michael Pfau LJM, Kirsten Garrow. The influence of television viewing on public perceptions of physicians. J Broadcast Electron Media. 1995;39(4):441-458.
21. Suzuki S. Exhausting physicians employed in hospitals in Japan assessed by a health questionnaire [in Japanese]. Sangyo Eiseigaku Zasshi. 2017;59(4):107-118. https://doi.org/10.1539/sangyoeisei.
22. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):50. https://doi.org/10.1186/s12909-018-1171-9.
23. Saijo Y, Chiba S, Yoshioka E, et al. Effects of work burden, job strain and support on depressive symptoms and burnout among Japanese physicians. Int J Occup Med Environ Health. 2014;27(6):980-992. https://doi.org/10.2478/s13382-014-0324-2.
24. Tiang KW, Razack AH, Ng KL. The ‘auxiliary’ white coat effect in hospitals: perceptions of patients and doctors. Singapore Med J. 2017;58(10):574-575. https://doi.org/10.11622/smedj.2017023.
25. Al Amry KM, Al Farrah M, Ur Rahman S, Abdulmajeed I. Patient perceptions and preferences of physicians’ attire in Saudi primary healthcare setting. J Community Hosp Intern Med Perspect. 2018;8(6):326-330. https://doi.org/10.1080/20009666.2018.1551026.
26. Healy WL. Letter to the editor: editor’s spotlight/take 5: physicians’ attire influences patients’ perceptions in the urban outpatient orthopaedic surgery setting. Clin Orthop Relat Res. 2016;474(11):2545-2546. https://doi.org/10.1007/s11999-016-5049-z.
27. Aldrees T, Alsuhaibani R, Alqaryan S, et al. Physicians’ attire. Parents preferences in a tertiary hospital. Saudi Med J. 2017;38(4):435-439. https://doi.org/10.15537/smj.2017.4.15853.
The patient-physician relationship is critical for ensuring the delivery of high-quality healthcare. Successful patient-physician relationships arise from shared trust, knowledge, mutual respect, and effective verbal and nonverbal communication. The ways in which patients experience healthcare and their satisfaction with physicians affect a myriad of important health outcomes, such as adherence to treatment and outcomes for conditions such as hypertension and diabetes mellitus.1-5 One method for potentially enhancing patient satisfaction is through understanding how patients wish their physicians to dress6-8 and tailoring attire to match these expectations. In addition to our systematic review,9 a recent large-scale, multicenter study in the United States revealed that most patients perceive physician attire as important, but that preferences for specific types of attire are contextual.9,10 For example, elderly patients preferred physicians in formal attire and white coat, while scrubs with white coat or scrubs alone were preferred for emergency department (ED) physicians and surgeons, respectively. Moreover, regional variation regarding attire preference was also observed in the US, with preferences for more formal attire in the South and less formal in the Midwest.
Geographic variation, regarding patient preferences for physician dress, is perhaps even more relevant internationally. In particular, Japan is considered to have a highly contextualized culture that relies on nonverbal and implicit communication. However, medical professionals have no specific dress code and, thus, don many different kinds of attire. In part, this may be because it is not clear whether or how physician attire impacts patient satisfaction and perceived healthcare quality in Japan.11-13 Although previous studies in Japan have suggested that physician attire has a considerable influence on patient satisfaction, these studies either involved a single department in one hospital or a small number of respondents.14-17 Therefore, we performed a multicenter, cross-sectional study to understand patients’ preferences for physician attire in different clinical settings and in different geographic regions in Japan.
METHODS
Study Population
We conducted a cross-sectional, questionnaire-based study from 2015 to 2017, in four geographically diverse hospitals in Japan. Two of these hospitals, Tokyo Joto Hospital and Juntendo University Hospital, are located in eastern Japan whereas the others, Kurashiki Central Hospital and Akashi Medical Center, are in western Japan.
Questionnaires were printed and randomly distributed by research staff to outpatients in waiting rooms and inpatients in medical wards who were 20 years of age or older. We placed no restriction on ward site or time of questionnaire distribution. Research staff, including physicians, nurses, and medical clerks, were instructed to avoid guiding or influencing participants’ responses. Informed consent was obtained by the staff; only those who provided informed consent participated in the study. Respondents could request assistance with form completion from persons accompanying them if they had difficulties, such as physical, visual, or hearing impairments. All responses were collected anonymously. The study was approved by the ethics committees of all four hospitals.
Questionnaire
We used a modified version of the survey instrument from a prior study.10 The first section of the survey showed photographs of either a male or female physician with 7 unique forms of attire, including casual, casual with white coat, scrubs, scrubs with white coat, formal, formal with white coat, and business suit (Figure 1). Given the Japanese context of this study, the language was translated to Japanese and photographs of physicians of Japanese descent were used. Photographs were taken with attention paid to achieving constant facial expressions on the physicians as well as in other visual cues (eg, lighting, background, pose). The physician’s gender and attire in the first photograph seen by each respondent were randomized to prevent bias in ordering, priming, and anchoring; all other sections of the survey were identical.
Respondents were first asked to rate the standalone, randomized physician photograph using a 1-10 scale across five domains (ie, how knowledgeable, trustworthy, caring, and approachable the physician appeared and how comfortable the physician’s appearance made the respondent feel), with a score of 10 representing the highest rating. Respondents were subsequently given 7 photographs of the same physician wearing various forms of attire. Questions were asked regarding preference of attire in varied clinical settings (ie, primary care, ED, hospital, surgery, overall preference). To identify the influence of and respondent preferences for physician dress and white coats, a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was employed. The scale was trichotomized into “disagree” (1, 2), “neither agree nor disagree” (3), and “agree” (4, 5) for analysis. Demographic data, including age, gender, education level, nationality (Japanese or non-Japanese), and number of physicians seen in the past year were collected.
Outcomes and Sample Size Calculation
The primary outcome of attire preference was calculated as the mean composite score of the five individual rating domains (ie, knowledgeable, trustworthy, caring, approachable, and comfortable), with the highest score representing the most preferred form of attire. We also assessed variation in preferences for physician attire by respondent characteristics, such as age and gender.
Sample size estimation was based on previous survey methodology.10 The Likert scale range for identifying influence of and respondent preferences for physician dress and white coats was 1-5 (“strongly disagree” to “strongly agree”). The scale range for measuring preferences for the randomized attire photograph was 1-10. An assumption of normality was made regarding responses on the 1-10 scale. An estimated standard deviation of 2.2 was assumed, based on prior findings.10 Based on these assumptions and the inclusion of at least 816 respondents (assuming a two-sided alpha error of 0.05), we expected to have 90% capacity to detect differences for effect sizes of 0.50 on the 1-10 scale.
Statistical Analyses
Paper-based survey data were entered independently and in duplicate by the study team. Respondents were not required to answer all questions; therefore, the denominator for each question varied. Data were reported as mean and standard deviation (SD) or percentages, where appropriate. Differences in the mean composite rating scores were assessed using one-way ANOVA with the Tukey method for pairwise comparisons. Differences in proportions for categorical data were compared using the Z-test. Chi-squared tests were used for bivariate comparisons between respondent age, gender, and level of education and corresponding respondent preferences. All analyses were performed using Stata 14 MP/SE (Stata Corp., College Station, Texas, USA).
RESULTS
Characteristics of Participants
Between December 1, 2015 and October 30, 2017, a total of 2,020 surveys were completed by patients across four academic hospitals in Japan. Of those, 1,960 patients (97.0%) completed the survey in its entirety. Approximately half of the respondents were 65 years of age or older (49%), of female gender (52%), and reported receiving care in the outpatient setting (53%). Regarding use of healthcare, 91% had seen more than one physician in the year preceding the time of survey completion (Table 1).
Ratings of Physician Attire
Compared with all forms of attire depicted in the survey’s first standalone photograph, respondents rated “casual attire with white coat” the highest (Figure 2). The mean composite score for “casual attire with white coat” was 7.1 (standard deviation [SD] = 1.8), and this attire was set as the referent group. Cronbach’s alpha, for the five items included in the composite score, was 0.95. However, “formal attire with white coat” was rated almost as highly as “casual attire with white coat” with an overall mean composite score of 7.0 (SD = 1.6).
Variation in Preference for Physician Attire by Clinical Setting
Preferences for physician attire varied by clinical care setting. Most respondents preferred “casual attire with white coat” or “formal attire with white coat” in both primary care and hospital settings, with a slight preference for “casual attire with white coat.” In contrast, respondents preferred “scrubs without white coat” in the ED and surgical settings. When asked about their overall preference, respondents reported they felt their physician should wear “formal attire with white coat” (35%) or “casual attire with white coat” (30%; Table 2). When comparing the group of photographs of physicians with white coats to the group without white coats (Figure 1), respondents preferred physicians wearing white coats overall and specifically when providing care in primary care and hospital settings. However, they preferred physicians without white coats when providing care in the ED (P < .001). With respect to surgeons, there was no statistically significant difference between preference for white coats and no white coats. These results were similar for photographs of both male and female physicians.
When asked whether physician dress was important to them and if physician attire influenced their satisfaction with the care received, 61% of participants agreed that physician dress was important, and 47% agreed that physician attire influenced satisfaction (Appendix Table 1). With respect to appropriateness of physicians dressing casually over the weekend in clinical settings, 52% responded that casual wear was inappropriate, while 31% had a neutral opinion.
Participants were asked whether physicians should wear a white coat in different clinical settings. Nearly two-thirds indicated a preference for white coats in the office and hospital (65% and 64%, respectively). Responses regarding whether emergency physicians should wear white coats were nearly equally divided (Agree, 37%; Disagree, 32%; Neither Agree nor Disagree, 31%). However, “scrubs without white coat” was most preferred (56%) when patients were given photographs of various attire and asked, “Which physician would you prefer to see when visiting the ER?” Responses to the question “Physicians should always wear a white coat when seeing patients in any setting” varied equally (Agree, 32%; Disagree, 34%; Neither Agree nor Disagree, 34%).
Variation in Preference for Physician Attire by Respondent Demographics
When comparing respondents by age, those 65 years or older preferred “formal attire with white coat” more so than respondents younger than 65 years (Appendix Table 2). This finding was identified in both primary care (36% vs 31%, P < .001) and hospital settings (37% vs 30%, P < .001). Additionally, physician attire had a greater impact on older respondents’ satisfaction and experience (Appendix Table 3). For example, 67% of respondents 65 years and older agreed that physician attire was important, and 54% agreed that attire influenced satisfaction. Conversely, for respondents younger than 65 years, the proportion agreeing with these statements was lower (56% and 41%, both P < .001). When comparing older and younger respondents, those 65 years and older more often preferred physicians wearing white coats in any setting (39% vs 26%, P < .001) and specifically in their office (68% vs 61%, P = .002), the ED (40% vs 34%, P < .001), and the hospital (69% vs 60%, P < .001).
When comparing male and female respondents, male respondents more often stated that physician dress was important to them (men, 64%; women, 58%; P = .002). When comparing responses to the question “Overall, which clothes do you feel a doctor should wear?”, between the eastern and western Japanese hospitals, preferences for physician attire varied.
Variation in Expectations Between Male and Female Physicians
When comparing the ratings of male and female physicians, female physicians were rated higher in how caring (P = .005) and approachable (P < .001) they appeared. However, there were no significant differences in the ratings of the three remaining domains (ie, knowledgeable, trustworthy, and comfortable) or the composite score.
DISCUSSION
Since we employed the same methodology as previous studies conducted in the US10 and Switzerland,18 a notable strength of our approach is that comparisons among these countries can be drawn. For example, physician attire appears to hold greater importance in Japan than in the US and Switzerland. Among Japanese participants, 61% agreed that physician dress is important (US, 53%; Switzerland, 36%), and 47% agreed that physician dress influenced how satisfied they were with their care (US, 36%; Switzerland, 23%).10 This result supports the notion that nonverbal and implicit communications (such as physician dress) may carry more importance among Japanese people.11-13
Regarding preference ratings for type of dress among respondents in Japan, “casual attire with white coat” received the highest mean composite score rating, with “formal attire with white coat” rated second overall. In contrast, US respondents rated “formal attire with white coat” highest and “scrubs with white coat” second.10 Our result runs counter to our expectation in that we expected Japanese respondents to prefer formal attire, since Japan is one of the most formal cultures in the world. One potential explanation for this difference is that the casual style chosen for this study was close to the smart casual style (slightly casual). Most hospitals and clinics in Japan do not allow physicians to wear jeans or polo shirts, which were chosen as the casual attire in the previous US study.
When examining various care settings and physician types, both Japanese and US respondents were more likely to prefer physicians wearing a white coat in the office or hospital.10 However, Japanese participants preferred both “casual attire with white coat” and “formal attire with white coat” equally in primary care or hospital settings. A smaller proportion of US respondents preferred “casual attire with white coat” in primary care (11%) and hospital settings (9%), but more preferred “formal attire with white coat” for primary care (44%) and hospital physicians (39%). In the ED setting, 32% of participants in Japan and 18% in the US disagreed with the idea that physicians should wear a white coat. Among Japanese participants, “scrubs without white coat” was rated highest for emergency physicians (56%) and surgeons (47%), while US preferences were 40% and 42%, respectively.10 One potential explanation is that scrubs-based attire became popular among Japanese ED and surgical contexts as a result of cultural influence and spread from western countries.19, 20
With respect to perceptions regarding physician attire on weekends, 52% of participants considered it inappropriate for a physician to dress casually over the weekend, compared with only 30% in Switzerland and 21% in the US.11,12 Given Japan’s level of formality and the fact that most Japanese physicians continue to work over the weekend,21-23 Japanese patients tend to expect their physicians to dress in more formal attire during these times.
Previous studies in Japan have demonstrated that older patients gave low ratings to scrubs and high ratings to white coat with any attire,15,17 and this was also the case in our study. Perhaps elderly patients reflect conservative values in their preferences of physician dress. Their perceptions may be less influenced by scenes portraying physicians in popular media when compared with the perceptions of younger patients. Though a 2015 systematic review and studies in other countries revealed white coats were preferred regardless of exact dress,9,24-26 they also showed variation in preferences for physician attire. For example, patients in Saudi Arabia preferred white coat and traditional ethnic dress,25 whereas mothers of pediatric patients in Saudi Arabia preferred scrubs for their pediatricians.27 Therefore, it is recommended for internationally mobile physicians to choose their dress depending on a variety of factors including country, context, and patient age group.
Our study has limitations. First, because some physicians presented the surveys to the patients, participants may have responded differently. Second, participants may have identified photographs of the male physician model as their personal healthcare provider (one author, K.K.). To avoid this possible bias, we randomly distributed 14 different versions of physician photographs in the questionnaire. Third, although physician photographs were strictly controlled, the “formal attire and white coat” and “casual attire and white coat” photographs appeared similar, especially given that the white coats were buttoned. Also, the female physician depicted in the photographs did not have the scrub shirt tucked in, while the male physician did. These nuances may have affected participant ratings between groups. Fourth,
In conclusion, patient preferences for physician attire were examined using a multicenter survey with a large sample size and robust survey methodology, thus overcoming weaknesses of previous studies into Japanese attire. Japanese patients perceive that physician attire is important and influences satisfaction with their care, more so than patients in other countries, like the US and Switzerland. Geography, settings of care, and patient age play a role in preferences. As a result, hospitals and health systems may use these findings to inform dress code policy based on patient population and context, recognizing that the appearance of their providers affects the patient-physician relationship. Future research should focus on better understanding the various cultural and societal customs that lead to patient expectations of physician attire.
Acknowledgments
The authors thank Drs. Fumi Takemoto, Masayuki Ueno, Kazuya Sakai, Saori Kinami, and Toshio Naito for their assistance with data collection at their respective sites. Additionally, the authors thank Dr. Yoko Kanamitsu for serving as a model for photographs.
The patient-physician relationship is critical for ensuring the delivery of high-quality healthcare. Successful patient-physician relationships arise from shared trust, knowledge, mutual respect, and effective verbal and nonverbal communication. The ways in which patients experience healthcare and their satisfaction with physicians affect a myriad of important health outcomes, such as adherence to treatment and outcomes for conditions such as hypertension and diabetes mellitus.1-5 One method for potentially enhancing patient satisfaction is through understanding how patients wish their physicians to dress6-8 and tailoring attire to match these expectations. In addition to our systematic review,9 a recent large-scale, multicenter study in the United States revealed that most patients perceive physician attire as important, but that preferences for specific types of attire are contextual.9,10 For example, elderly patients preferred physicians in formal attire and white coat, while scrubs with white coat or scrubs alone were preferred for emergency department (ED) physicians and surgeons, respectively. Moreover, regional variation regarding attire preference was also observed in the US, with preferences for more formal attire in the South and less formal in the Midwest.
Geographic variation, regarding patient preferences for physician dress, is perhaps even more relevant internationally. In particular, Japan is considered to have a highly contextualized culture that relies on nonverbal and implicit communication. However, medical professionals have no specific dress code and, thus, don many different kinds of attire. In part, this may be because it is not clear whether or how physician attire impacts patient satisfaction and perceived healthcare quality in Japan.11-13 Although previous studies in Japan have suggested that physician attire has a considerable influence on patient satisfaction, these studies either involved a single department in one hospital or a small number of respondents.14-17 Therefore, we performed a multicenter, cross-sectional study to understand patients’ preferences for physician attire in different clinical settings and in different geographic regions in Japan.
METHODS
Study Population
We conducted a cross-sectional, questionnaire-based study from 2015 to 2017, in four geographically diverse hospitals in Japan. Two of these hospitals, Tokyo Joto Hospital and Juntendo University Hospital, are located in eastern Japan whereas the others, Kurashiki Central Hospital and Akashi Medical Center, are in western Japan.
Questionnaires were printed and randomly distributed by research staff to outpatients in waiting rooms and inpatients in medical wards who were 20 years of age or older. We placed no restriction on ward site or time of questionnaire distribution. Research staff, including physicians, nurses, and medical clerks, were instructed to avoid guiding or influencing participants’ responses. Informed consent was obtained by the staff; only those who provided informed consent participated in the study. Respondents could request assistance with form completion from persons accompanying them if they had difficulties, such as physical, visual, or hearing impairments. All responses were collected anonymously. The study was approved by the ethics committees of all four hospitals.
Questionnaire
We used a modified version of the survey instrument from a prior study.10 The first section of the survey showed photographs of either a male or female physician with 7 unique forms of attire, including casual, casual with white coat, scrubs, scrubs with white coat, formal, formal with white coat, and business suit (Figure 1). Given the Japanese context of this study, the language was translated to Japanese and photographs of physicians of Japanese descent were used. Photographs were taken with attention paid to achieving constant facial expressions on the physicians as well as in other visual cues (eg, lighting, background, pose). The physician’s gender and attire in the first photograph seen by each respondent were randomized to prevent bias in ordering, priming, and anchoring; all other sections of the survey were identical.
Respondents were first asked to rate the standalone, randomized physician photograph using a 1-10 scale across five domains (ie, how knowledgeable, trustworthy, caring, and approachable the physician appeared and how comfortable the physician’s appearance made the respondent feel), with a score of 10 representing the highest rating. Respondents were subsequently given 7 photographs of the same physician wearing various forms of attire. Questions were asked regarding preference of attire in varied clinical settings (ie, primary care, ED, hospital, surgery, overall preference). To identify the influence of and respondent preferences for physician dress and white coats, a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was employed. The scale was trichotomized into “disagree” (1, 2), “neither agree nor disagree” (3), and “agree” (4, 5) for analysis. Demographic data, including age, gender, education level, nationality (Japanese or non-Japanese), and number of physicians seen in the past year were collected.
Outcomes and Sample Size Calculation
The primary outcome of attire preference was calculated as the mean composite score of the five individual rating domains (ie, knowledgeable, trustworthy, caring, approachable, and comfortable), with the highest score representing the most preferred form of attire. We also assessed variation in preferences for physician attire by respondent characteristics, such as age and gender.
Sample size estimation was based on previous survey methodology.10 The Likert scale range for identifying influence of and respondent preferences for physician dress and white coats was 1-5 (“strongly disagree” to “strongly agree”). The scale range for measuring preferences for the randomized attire photograph was 1-10. An assumption of normality was made regarding responses on the 1-10 scale. An estimated standard deviation of 2.2 was assumed, based on prior findings.10 Based on these assumptions and the inclusion of at least 816 respondents (assuming a two-sided alpha error of 0.05), we expected to have 90% capacity to detect differences for effect sizes of 0.50 on the 1-10 scale.
Statistical Analyses
Paper-based survey data were entered independently and in duplicate by the study team. Respondents were not required to answer all questions; therefore, the denominator for each question varied. Data were reported as mean and standard deviation (SD) or percentages, where appropriate. Differences in the mean composite rating scores were assessed using one-way ANOVA with the Tukey method for pairwise comparisons. Differences in proportions for categorical data were compared using the Z-test. Chi-squared tests were used for bivariate comparisons between respondent age, gender, and level of education and corresponding respondent preferences. All analyses were performed using Stata 14 MP/SE (Stata Corp., College Station, Texas, USA).
RESULTS
Characteristics of Participants
Between December 1, 2015 and October 30, 2017, a total of 2,020 surveys were completed by patients across four academic hospitals in Japan. Of those, 1,960 patients (97.0%) completed the survey in its entirety. Approximately half of the respondents were 65 years of age or older (49%), of female gender (52%), and reported receiving care in the outpatient setting (53%). Regarding use of healthcare, 91% had seen more than one physician in the year preceding the time of survey completion (Table 1).
Ratings of Physician Attire
Compared with all forms of attire depicted in the survey’s first standalone photograph, respondents rated “casual attire with white coat” the highest (Figure 2). The mean composite score for “casual attire with white coat” was 7.1 (standard deviation [SD] = 1.8), and this attire was set as the referent group. Cronbach’s alpha, for the five items included in the composite score, was 0.95. However, “formal attire with white coat” was rated almost as highly as “casual attire with white coat” with an overall mean composite score of 7.0 (SD = 1.6).
Variation in Preference for Physician Attire by Clinical Setting
Preferences for physician attire varied by clinical care setting. Most respondents preferred “casual attire with white coat” or “formal attire with white coat” in both primary care and hospital settings, with a slight preference for “casual attire with white coat.” In contrast, respondents preferred “scrubs without white coat” in the ED and surgical settings. When asked about their overall preference, respondents reported they felt their physician should wear “formal attire with white coat” (35%) or “casual attire with white coat” (30%; Table 2). When comparing the group of photographs of physicians with white coats to the group without white coats (Figure 1), respondents preferred physicians wearing white coats overall and specifically when providing care in primary care and hospital settings. However, they preferred physicians without white coats when providing care in the ED (P < .001). With respect to surgeons, there was no statistically significant difference between preference for white coats and no white coats. These results were similar for photographs of both male and female physicians.
When asked whether physician dress was important to them and if physician attire influenced their satisfaction with the care received, 61% of participants agreed that physician dress was important, and 47% agreed that physician attire influenced satisfaction (Appendix Table 1). With respect to appropriateness of physicians dressing casually over the weekend in clinical settings, 52% responded that casual wear was inappropriate, while 31% had a neutral opinion.
Participants were asked whether physicians should wear a white coat in different clinical settings. Nearly two-thirds indicated a preference for white coats in the office and hospital (65% and 64%, respectively). Responses regarding whether emergency physicians should wear white coats were nearly equally divided (Agree, 37%; Disagree, 32%; Neither Agree nor Disagree, 31%). However, “scrubs without white coat” was most preferred (56%) when patients were given photographs of various attire and asked, “Which physician would you prefer to see when visiting the ER?” Responses to the question “Physicians should always wear a white coat when seeing patients in any setting” varied equally (Agree, 32%; Disagree, 34%; Neither Agree nor Disagree, 34%).
Variation in Preference for Physician Attire by Respondent Demographics
When comparing respondents by age, those 65 years or older preferred “formal attire with white coat” more so than respondents younger than 65 years (Appendix Table 2). This finding was identified in both primary care (36% vs 31%, P < .001) and hospital settings (37% vs 30%, P < .001). Additionally, physician attire had a greater impact on older respondents’ satisfaction and experience (Appendix Table 3). For example, 67% of respondents 65 years and older agreed that physician attire was important, and 54% agreed that attire influenced satisfaction. Conversely, for respondents younger than 65 years, the proportion agreeing with these statements was lower (56% and 41%, both P < .001). When comparing older and younger respondents, those 65 years and older more often preferred physicians wearing white coats in any setting (39% vs 26%, P < .001) and specifically in their office (68% vs 61%, P = .002), the ED (40% vs 34%, P < .001), and the hospital (69% vs 60%, P < .001).
When comparing male and female respondents, male respondents more often stated that physician dress was important to them (men, 64%; women, 58%; P = .002). When comparing responses to the question “Overall, which clothes do you feel a doctor should wear?”, between the eastern and western Japanese hospitals, preferences for physician attire varied.
Variation in Expectations Between Male and Female Physicians
When comparing the ratings of male and female physicians, female physicians were rated higher in how caring (P = .005) and approachable (P < .001) they appeared. However, there were no significant differences in the ratings of the three remaining domains (ie, knowledgeable, trustworthy, and comfortable) or the composite score.
DISCUSSION
Since we employed the same methodology as previous studies conducted in the US10 and Switzerland,18 a notable strength of our approach is that comparisons among these countries can be drawn. For example, physician attire appears to hold greater importance in Japan than in the US and Switzerland. Among Japanese participants, 61% agreed that physician dress is important (US, 53%; Switzerland, 36%), and 47% agreed that physician dress influenced how satisfied they were with their care (US, 36%; Switzerland, 23%).10 This result supports the notion that nonverbal and implicit communications (such as physician dress) may carry more importance among Japanese people.11-13
Regarding preference ratings for type of dress among respondents in Japan, “casual attire with white coat” received the highest mean composite score rating, with “formal attire with white coat” rated second overall. In contrast, US respondents rated “formal attire with white coat” highest and “scrubs with white coat” second.10 Our result runs counter to our expectation in that we expected Japanese respondents to prefer formal attire, since Japan is one of the most formal cultures in the world. One potential explanation for this difference is that the casual style chosen for this study was close to the smart casual style (slightly casual). Most hospitals and clinics in Japan do not allow physicians to wear jeans or polo shirts, which were chosen as the casual attire in the previous US study.
When examining various care settings and physician types, both Japanese and US respondents were more likely to prefer physicians wearing a white coat in the office or hospital.10 However, Japanese participants preferred both “casual attire with white coat” and “formal attire with white coat” equally in primary care or hospital settings. A smaller proportion of US respondents preferred “casual attire with white coat” in primary care (11%) and hospital settings (9%), but more preferred “formal attire with white coat” for primary care (44%) and hospital physicians (39%). In the ED setting, 32% of participants in Japan and 18% in the US disagreed with the idea that physicians should wear a white coat. Among Japanese participants, “scrubs without white coat” was rated highest for emergency physicians (56%) and surgeons (47%), while US preferences were 40% and 42%, respectively.10 One potential explanation is that scrubs-based attire became popular among Japanese ED and surgical contexts as a result of cultural influence and spread from western countries.19, 20
With respect to perceptions regarding physician attire on weekends, 52% of participants considered it inappropriate for a physician to dress casually over the weekend, compared with only 30% in Switzerland and 21% in the US.11,12 Given Japan’s level of formality and the fact that most Japanese physicians continue to work over the weekend,21-23 Japanese patients tend to expect their physicians to dress in more formal attire during these times.
Previous studies in Japan have demonstrated that older patients gave low ratings to scrubs and high ratings to white coat with any attire,15,17 and this was also the case in our study. Perhaps elderly patients reflect conservative values in their preferences of physician dress. Their perceptions may be less influenced by scenes portraying physicians in popular media when compared with the perceptions of younger patients. Though a 2015 systematic review and studies in other countries revealed white coats were preferred regardless of exact dress,9,24-26 they also showed variation in preferences for physician attire. For example, patients in Saudi Arabia preferred white coat and traditional ethnic dress,25 whereas mothers of pediatric patients in Saudi Arabia preferred scrubs for their pediatricians.27 Therefore, it is recommended for internationally mobile physicians to choose their dress depending on a variety of factors including country, context, and patient age group.
Our study has limitations. First, because some physicians presented the surveys to the patients, participants may have responded differently. Second, participants may have identified photographs of the male physician model as their personal healthcare provider (one author, K.K.). To avoid this possible bias, we randomly distributed 14 different versions of physician photographs in the questionnaire. Third, although physician photographs were strictly controlled, the “formal attire and white coat” and “casual attire and white coat” photographs appeared similar, especially given that the white coats were buttoned. Also, the female physician depicted in the photographs did not have the scrub shirt tucked in, while the male physician did. These nuances may have affected participant ratings between groups. Fourth,
In conclusion, patient preferences for physician attire were examined using a multicenter survey with a large sample size and robust survey methodology, thus overcoming weaknesses of previous studies into Japanese attire. Japanese patients perceive that physician attire is important and influences satisfaction with their care, more so than patients in other countries, like the US and Switzerland. Geography, settings of care, and patient age play a role in preferences. As a result, hospitals and health systems may use these findings to inform dress code policy based on patient population and context, recognizing that the appearance of their providers affects the patient-physician relationship. Future research should focus on better understanding the various cultural and societal customs that lead to patient expectations of physician attire.
Acknowledgments
The authors thank Drs. Fumi Takemoto, Masayuki Ueno, Kazuya Sakai, Saori Kinami, and Toshio Naito for their assistance with data collection at their respective sites. Additionally, the authors thank Dr. Yoko Kanamitsu for serving as a model for photographs.
1. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. https://doi.org/ 10.1056/NEJMp1211775.
2. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
3. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39-48. https://doi.org/10.2147/PPA.S24752.
4. Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921-31. https://doi.org/10.1056/NEJMsa080411.
5. O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144-54. https://doi.org/10.1046/j.1525-1497.2002.10431.x.
6. Chung H, Lee H, Chang DS, Kim HS, Park HJ, Chae Y. Doctor’s attire influences perceived empathy in the patient-doctor relationship. Patient Educ Couns. 2012;89(3):387-391. https://doi.org/10.1016/j.pec.2012.02.017.
7. Bianchi MT. Desiderata or dogma: what the evidence reveals about physician attire. J Gen Intern Med. 2008;23(5):641-643. https://doi.org/10.1007/s11606-008-0546-8.
8. Brandt LJ. On the value of an old dress code in the new millennium. Arch Intern Med. 2003;163(11):1277-1281. https://doi.org/10.1001/archinte.163.11.1277.
9. Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature--targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578. https://doi.org/10.1136/bmjopen-2014-006578.
10. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. https://doi.org/10.1136/bmjopen-2017-021239.
11. Rowbury R. The need for more proactive communications. Low trust and changing values mean Japan can no longer fall back on its homogeneity. The Japan Times. 2017, Oct 15;Sect. Opinion. https://www.japantimes.co.jp/opinion/2017/10/15/commentary/japan-commentary/need-proactive-communications/#.Xej7lC3MzUI. Accessed December 5, 2019.
12. Shoji Nishimura ANaST. Communication Style and Cultural Features in High/Low Context Communication Cultures: A Case Study of Finland, Japan and India. Nov 22nd, 2009.
13. Smith RMRSW. The influence of high/low-context culture and power distance on choice of communication media: Students’ media choice to communicate with Professors in Japan and America. Int J Intercultural Relations. 2007;31(4):479-501.
14. Yamada Y, Takahashi O, Ohde S, Deshpande GA, Fukui T. Patients’ preferences for doctors’ attire in Japan. Intern Med. 2010;49(15):1521-1526. https://doi.org/10.2169/internalmedicine.49.3572.
15. Ikusaka M, Kamegai M, Sunaga T, et al. Patients’ attitude toward consultations by a physician without a white coat in Japan. Intern Med. 1999;38(7):533-536. https://doi.org/10.2169/internalmedicine.38.533.
16. Lefor AK, Ohnuma T, Nunomiya S, Yokota S, Makino J, Sanui M. Physician attire in the intensive care unit in Japan influences visitors’ perception of care. J Crit Care. 2018;43:288-293.
17. Kurihara H, Maeno T. Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pac Fam Med. 2014;13(1):2. https://doi.org/10.1186/1447-056X-13-2.
18. Zollinger M, Houchens N, Chopra V, et al. Understanding patient preference for physician attire in ambulatory clinics: a cross-sectional observational study. BMJ Open. 2019;9(5):e026009. https://doi.org/10.1136/bmjopen-2018-026009.
19. Chung JE. Medical Dramas and Viewer Perception of Health: Testing Cultivation Effects. Hum Commun Res. 2014;40(3):333-349.
20. Michael Pfau LJM, Kirsten Garrow. The influence of television viewing on public perceptions of physicians. J Broadcast Electron Media. 1995;39(4):441-458.
21. Suzuki S. Exhausting physicians employed in hospitals in Japan assessed by a health questionnaire [in Japanese]. Sangyo Eiseigaku Zasshi. 2017;59(4):107-118. https://doi.org/10.1539/sangyoeisei.
22. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):50. https://doi.org/10.1186/s12909-018-1171-9.
23. Saijo Y, Chiba S, Yoshioka E, et al. Effects of work burden, job strain and support on depressive symptoms and burnout among Japanese physicians. Int J Occup Med Environ Health. 2014;27(6):980-992. https://doi.org/10.2478/s13382-014-0324-2.
24. Tiang KW, Razack AH, Ng KL. The ‘auxiliary’ white coat effect in hospitals: perceptions of patients and doctors. Singapore Med J. 2017;58(10):574-575. https://doi.org/10.11622/smedj.2017023.
25. Al Amry KM, Al Farrah M, Ur Rahman S, Abdulmajeed I. Patient perceptions and preferences of physicians’ attire in Saudi primary healthcare setting. J Community Hosp Intern Med Perspect. 2018;8(6):326-330. https://doi.org/10.1080/20009666.2018.1551026.
26. Healy WL. Letter to the editor: editor’s spotlight/take 5: physicians’ attire influences patients’ perceptions in the urban outpatient orthopaedic surgery setting. Clin Orthop Relat Res. 2016;474(11):2545-2546. https://doi.org/10.1007/s11999-016-5049-z.
27. Aldrees T, Alsuhaibani R, Alqaryan S, et al. Physicians’ attire. Parents preferences in a tertiary hospital. Saudi Med J. 2017;38(4):435-439. https://doi.org/10.15537/smj.2017.4.15853.
1. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. https://doi.org/ 10.1056/NEJMp1211775.
2. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
3. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39-48. https://doi.org/10.2147/PPA.S24752.
4. Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921-31. https://doi.org/10.1056/NEJMsa080411.
5. O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144-54. https://doi.org/10.1046/j.1525-1497.2002.10431.x.
6. Chung H, Lee H, Chang DS, Kim HS, Park HJ, Chae Y. Doctor’s attire influences perceived empathy in the patient-doctor relationship. Patient Educ Couns. 2012;89(3):387-391. https://doi.org/10.1016/j.pec.2012.02.017.
7. Bianchi MT. Desiderata or dogma: what the evidence reveals about physician attire. J Gen Intern Med. 2008;23(5):641-643. https://doi.org/10.1007/s11606-008-0546-8.
8. Brandt LJ. On the value of an old dress code in the new millennium. Arch Intern Med. 2003;163(11):1277-1281. https://doi.org/10.1001/archinte.163.11.1277.
9. Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature--targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578. https://doi.org/10.1136/bmjopen-2014-006578.
10. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. https://doi.org/10.1136/bmjopen-2017-021239.
11. Rowbury R. The need for more proactive communications. Low trust and changing values mean Japan can no longer fall back on its homogeneity. The Japan Times. 2017, Oct 15;Sect. Opinion. https://www.japantimes.co.jp/opinion/2017/10/15/commentary/japan-commentary/need-proactive-communications/#.Xej7lC3MzUI. Accessed December 5, 2019.
12. Shoji Nishimura ANaST. Communication Style and Cultural Features in High/Low Context Communication Cultures: A Case Study of Finland, Japan and India. Nov 22nd, 2009.
13. Smith RMRSW. The influence of high/low-context culture and power distance on choice of communication media: Students’ media choice to communicate with Professors in Japan and America. Int J Intercultural Relations. 2007;31(4):479-501.
14. Yamada Y, Takahashi O, Ohde S, Deshpande GA, Fukui T. Patients’ preferences for doctors’ attire in Japan. Intern Med. 2010;49(15):1521-1526. https://doi.org/10.2169/internalmedicine.49.3572.
15. Ikusaka M, Kamegai M, Sunaga T, et al. Patients’ attitude toward consultations by a physician without a white coat in Japan. Intern Med. 1999;38(7):533-536. https://doi.org/10.2169/internalmedicine.38.533.
16. Lefor AK, Ohnuma T, Nunomiya S, Yokota S, Makino J, Sanui M. Physician attire in the intensive care unit in Japan influences visitors’ perception of care. J Crit Care. 2018;43:288-293.
17. Kurihara H, Maeno T. Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pac Fam Med. 2014;13(1):2. https://doi.org/10.1186/1447-056X-13-2.
18. Zollinger M, Houchens N, Chopra V, et al. Understanding patient preference for physician attire in ambulatory clinics: a cross-sectional observational study. BMJ Open. 2019;9(5):e026009. https://doi.org/10.1136/bmjopen-2018-026009.
19. Chung JE. Medical Dramas and Viewer Perception of Health: Testing Cultivation Effects. Hum Commun Res. 2014;40(3):333-349.
20. Michael Pfau LJM, Kirsten Garrow. The influence of television viewing on public perceptions of physicians. J Broadcast Electron Media. 1995;39(4):441-458.
21. Suzuki S. Exhausting physicians employed in hospitals in Japan assessed by a health questionnaire [in Japanese]. Sangyo Eiseigaku Zasshi. 2017;59(4):107-118. https://doi.org/10.1539/sangyoeisei.
22. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):50. https://doi.org/10.1186/s12909-018-1171-9.
23. Saijo Y, Chiba S, Yoshioka E, et al. Effects of work burden, job strain and support on depressive symptoms and burnout among Japanese physicians. Int J Occup Med Environ Health. 2014;27(6):980-992. https://doi.org/10.2478/s13382-014-0324-2.
24. Tiang KW, Razack AH, Ng KL. The ‘auxiliary’ white coat effect in hospitals: perceptions of patients and doctors. Singapore Med J. 2017;58(10):574-575. https://doi.org/10.11622/smedj.2017023.
25. Al Amry KM, Al Farrah M, Ur Rahman S, Abdulmajeed I. Patient perceptions and preferences of physicians’ attire in Saudi primary healthcare setting. J Community Hosp Intern Med Perspect. 2018;8(6):326-330. https://doi.org/10.1080/20009666.2018.1551026.
26. Healy WL. Letter to the editor: editor’s spotlight/take 5: physicians’ attire influences patients’ perceptions in the urban outpatient orthopaedic surgery setting. Clin Orthop Relat Res. 2016;474(11):2545-2546. https://doi.org/10.1007/s11999-016-5049-z.
27. Aldrees T, Alsuhaibani R, Alqaryan S, et al. Physicians’ attire. Parents preferences in a tertiary hospital. Saudi Med J. 2017;38(4):435-439. https://doi.org/10.15537/smj.2017.4.15853.
© 2020 Society of Hospital Medicine
Portable Ultrasound Device Usage and Learning Outcomes Among Internal Medicine Trainees: A Parallel-Group Randomized Trial
Point-of-care ultrasonography (POCUS) can transform healthcare delivery through its diagnostic and therapeutic expediency.1 POCUS has been shown to bolster diagnostic accuracy, reduce procedural complications, decrease inpatient length of stay, and improve patient satisfaction by encouraging the physician to be present at the bedside.2-8
POCUS has become widespread across a variety of clinical settings as more investigations have demonstrated its positive impact on patient care.1,9-12 This includes the use of POCUS by trainees, who are now utilizing this technology as part of their assessments of patients.13,14 However, trainees may be performing these examinations with minimal oversight, and outside of emergency medicine, there are few guidelines on how to effectively teach POCUS or measure competency.13,14 While POCUS is rapidly becoming a part of inpatient care, teaching physicians may have little experience in ultrasound or the expertise to adequately supervise trainees.14 There is a growing need to study what trainees can learn and how this knowledge is acquired.
Previous investigations have demonstrated that inexperienced users can be taught to use POCUS to identify a variety of pathological states.2,3,15-23 Most of these curricula used a single lecture series as their pedagogical vehicle, and they variably included junior medical trainees. More importantly, the investigations did not explore whether personal access to handheld ultrasound devices (HUDs) improved learning. In theory, improved access to POCUS devices increases opportunities for authentic and deliberate practice, which may be needed to improve trainee skill with POCUS beyond the classroom setting.14
This study aimed to address several ongoing gaps in knowledge related to learning POCUS. First, we hypothesized that personal HUD access would improve trainees’ POCUS-related knowledge and interpretive ability as a result of increased practice opportunities. Second, we hypothesized that trainees who receive personal access to HUDs would be more likely to perform POCUS examinations and feel more confident in their interpretations. Finally, we hypothesized that repeated exposure to POCUS-related lectures would result in greater improvements in knowledge as compared with a single lecture series.
METHODS
Participants and Setting
The 2017 intern class (n = 47) at an academic internal medicine residency program participated in the study. Control data were obtained from the 2016 intern class (historical control; n = 50) and the 2018 intern class (contemporaneous control; n = 52). The Stanford University Institutional Review Board approved this study.
Study Design
The 2017 intern class (n = 47) received POCUS didactics from June 2017 to June 2018. To evaluate if increased access to HUDs improved learning outcomes, the 2017 interns were randomized 1:1 to receive their own personal HUD that could be used for patient care and/or self-directed learning (n = 24) vs no-HUD (n = 23; Figure). Learning outcomes were assessed over the course of 1 year (see “Outcomes” below) and were compared with the 2016 and 2018 controls. The 2016 intern class had completed a year of training but had not received formalized POCUS didactics (historical control), whereas the 2018 intern class was assessed at the beginning of their year (contemporaneous control; Figure). In order to make comparisons based on intern experience, baseline data for the 2017 intern class were compared with the 2018 intern class, whereas end-of-study data for 2017 interns were compared with 2016 interns.
Outcomes
The primary outcome was the difference in assessment scores at the end of the study period between interns randomized to receive a HUD and those who were not. Secondary outcomes included differences in HUD usage rates, lecture attendance, and assessment scores. To assess whether repeated lecture exposure resulted in greater amounts of learning, this study evaluated for assessment score improvements after each lecture block. Finally, trainee attitudes toward POCUS and their confidence in their interpretative ability were measured at the beginning and end of the study period.
Curriculum Implementation
The lectures were administered as once-weekly didactics of 1-hour duration to interns rotating on the inpatient wards rotation. This rotation is 4 weeks long, and each intern will experience the rotation two to four times per year. Each lecture contained two parts: (1) 20-30 minutes of didactics via Microsoft PowerPointTM and (2) 30-40 minutes of supervised practice using HUDs on standardized patients. Four lectures were given each month: (1) introduction to POCUS and ultrasound physics, (2) thoracic/lung ultrasound, (3) echocardiography, and (4) abdominal POCUS. The lectures consisted of contrasting cases of normal/abnormal videos and clinical vignettes. These four lectures were repeated each month as new interns rotated on service. Some interns experienced the same content multiple times, which was intentional in order to assess their rates of learning over time. Lecture contents were based on previously published guidelines and expert consensus for teaching POCUS in internal medicine.13, 24-26 Content from the Accreditation Council for Graduate Medical Education (ACGME) and the American College of Emergency Physicians (ACEP) was also incorporated because these organizations had published relevant guidelines for teaching POCUS.13,26 Further development of the lectures occurred through review of previously described POCUS-relevant curricula.27-32
Handheld Ultrasound Devices
This study used the Philips LumifyTM, a United States Food and Drug Administration–approved device. Interns randomized to HUDs received their own device at the start of the rotation. It was at their discretion to use the device outside of the course. All devices were approved for patient use and were encrypted in compliance with our information security office. For privacy reasons, any saved patient images were not reviewed by the researchers. Interns were encouraged to share their findings with supervising physicians during rounds, but actual oversight was not measured. Interns not randomized to HUDs could access a single community device that was shared among all residents and fellows in the hospital. Interns reported the average number of POCUS examinations performed each week via a survey sent during the last week of the rotation.
Assessment Design and Implementation
Assessments evaluating trainee knowledge were administered before, during, and after the study period (Figure). For the 2017 cohort, assessments were also administered at the start and end of the ward month to track knowledge acquisition. Assessment contents were selected from POCUS guidelines for internal medicine and adaptation of the ACGME and ACEP guidelines.13,24,26 Additional content was obtained from major society POCUS tutorials and deidentified images collected by the study authors.13,24,33 In keeping with previously described methodology, the images were shown for approximately 12 seconds, followed by five additional seconds to allow the learner to answer the question.32 Final assessment contents were determined by the authors using the Delphi method.34 A sample assessment can be found in the Appendix Material.
Surveys
Surveys were administered alongside the assessments to the 2016-2018 intern classes. These surveys assessed trainee attitudes toward POCUS and were based on previously validated assessments.27,28,30 Attitudes were measured using 5-point Likert scales.
Statistical Analysis
For the primary outcome, we performed generalized binomial mixed-effect regressions using the survey periods, randomization group, and the interaction of the two as independent variables after adjusting for attendance and controlling of intra-intern correlations. The bivariate unadjusted analysis was performed to display the distribution of overall correctness on the assessments. Wilcoxon signed rank test was used to determine score significance for dependent score variables (R-Statistical Programming Language, Vienna, Austria).
RESULTS
Baseline Characteristics
There were 149 interns who participated in this study (Figure). Assessment/survey completion rates were as follows: 2016 control: 68.0%; 2017 preintervention: 97.9%; 2017 postintervention: 89.4%; and 2018 control: 100%. The 2017 interns reported similar amounts of prior POCUS exposure in medical school (Table 1).
Primary Outcome: Assessment Scores (HUD vs no HUD)
There were no significant differences in assessment scores at the end of the study between interns randomized to personal HUD access vs those to no-HUD access (Table 1). HUD interns reported performing POCUS assessments on patients a mean 6.8 (standard deviation [SD] 2.2) times per week vs 6.4 (SD 2.9) times per week in the no-HUD arm (P = .66). The mean lecture attendance was 75.0% and did not significantly differ between the HUD arms (Table 1).
Secondary Outcomes
Impact of Repeating Lectures
The 2017 interns demonstrated significant increases in preblock vs postblock assessment scores after first-time exposure to the lectures (median preblock score 0.61 [interquartile range (IQR), 0.53-0.70] vs postblock score 0.81 [IQR, 0.72-0.86]; P < .001; Table 2). However, intern performance on the preblock vs postblock assessments after second-time exposure to the curriculum failed to improve (median second preblock score 0.78 [IQR, 0.69-0.83] vs postblock score 0.81 [IQR, 0.64-0.89]; P = .94). Intern performance on individual domains of knowledge for each block is listed in Appendix Table 1.
Intervention Performance vs Controls
The 2016 historical control had significantly higher scores compared with the 2017 preintervention group (P < .001; Appendix Table 2). The year-long lecture series resulted in significant increases in median scores for the 2017 group (median preintervention score 0.55 [0.41-0.61] vs median postintervention score 0.84 [0.71-0.90]; P = .006; Appendix Table 1). At the end of the study, the 2017 postintervention scores were significantly higher across multiple knowledge domains compared with the 2016 historical control (Appendix Table 2).
Survey Results
Notably, the 2017 intern class at the end of the intervention did not have significantly different assessment scores for several disease-specific domains, compared with the 2016 control (Appendix Table 2). Nonetheless, the 2017 intern class reported higher levels of confidence in these same domains despite similar scores (Supplementary Figure). The HUD group seldomly cited a lack of confidence in their abilities as a barrier to performing POCUS examinations (17.6%), compared with the no-HUD group (50.0%), despite nearly identical assessment scores between the two groups (Table 1).
DISCUSSION
Previous guidelines have recommended increased HUD access for learners,13,24,35,36 but there have been few investigations that have evaluated the impact of such access on learning POCUS. One previous investigation found that hospitalists who carried HUDs were more likely to identify heart failure on bedside examination.37 In contrast, our study found no improvement in interpretative ability when randomizing interns to carry HUDs for patient care. Notably, interns did not perform more POCUS examinations when given HUDs. We offer several explanations for this finding. First, time-motion studies have demonstrated that internal medicine interns spend less than 15% of their time toward direct patient care.38 It is possible that the demands of being an intern impeded their ability to perform more POCUS examinations on their patients, regardless of HUD access. Alternatively, the interns randomized to no personal access may have used the community device more frequently as a result of the lecture series. Given the cost of HUDs, further studies are needed to assess the degree to which HUD access will improve trainee interpretive ability, especially as more training programs consider the creation of ultrasound curricula.10,11,24,39,40
This study was unique because it followed interns over a year-long course that repeated the same material to assess rates of learning with repeated exposure. Learners improved their scores after the first, but not second, block. Furthermore, the median scores were nearly identical between the first postblock assessment and second preblock assessment (0.81 vs 0.78), suggesting that knowledge was retained between blocks. Together, these findings suggest there may be limitations of traditional lectures that use standardized patient models for practice. Supplementary pedagogies, such as in-the-moment feedback with actual patients, may be needed to promote mastery.14,35
Despite no formal curriculum, the 2016 intern class (historical control) had learned POCUS to some degree based on their higher assessment scores compared with the 2017 intern class during the preintervention period. Such learning may be informal, and yet, trainees may feel confident in making clinical decisions without formalized training, accreditation, or oversight. As suggested by this study, adding regular didactics or giving trainees HUDs may not immediately solve this issue. For assessment items in which the 2017 interns did not significantly differ from the controls, they nonetheless reported higher confidence in their abilities. Similarly, interns randomized to HUDs less frequently cited a lack of confidence in their abilities, despite similar scores to the no-HUD group. Such confidence may be incongruent with their actual knowledge or ability to safely use POCUS. This phenomenon of misplaced confidence is known as the Dunning–Kruger effect, and it may be common with ultrasound learning.41 While confidence can be part of a holistic definition of competency,14 these results raise the concern that trainees may have difficulty assessing their own competency level with POCUS.35
There are several limitations to this study. It was performed at a single institution with limited sample size. It examined only intern physicians because of funding constraints, which limits the generalizability of these findings among medical trainees. Technical ability assessments (including obtaining and interpreting images) were not included. We were unable to track the timing or location of the devices’ usage, and the interns’ self-reported usage rates may be subject to recall bias. To our knowledge, there were no significant lapses in device availability/functionality. Intern physicians in the HUD arm did not receive formal feedback on personally acquired patient images, which may have limited the intervention’s impact.
In conclusion, internal medicine interns who received personal HUDs were not better at recognizing normal/abnormal findings on image assessments, and they did not report performing more POCUS examinations. Since the minority of a trainee’s time is spent toward direct patient care, offering trainees HUDs without substantial guidance may not be enough to promote mastery. Notably, trainees who received HUDs felt more confident in their abilities, despite no objective increase in their actual skill. Finally, interns who received POCUS-related lectures experienced significant benefit upon first exposure to the material, while repeated exposures did not improve performance. Future investigations should stringently track trainee POCUS usage rates with HUDs and assess whether image acquisition ability improves as a result of personal access.
1. Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749-757. https://doi.org/10.1056/NEJMra0909487.
2. Akkaya A, Yesilaras M, Aksay E, Sever M, Atilla OD. The interrater reliability of ultrasound imaging of the inferior vena cava performed by emergency residents. Am J Emerg Med. 2013;31(10):1509-1511. https://doi.org/10.1016/j.ajem.2013.07.006.
3. Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr. 2011;24(12):1319-1324. https://doi.org/10.1016/j.echo.2011.07.013.
4. Dodge KL, Lynch CA, Moore CL, Biroscak BJ, Evans LV. Use of ultrasound guidance improves central venous catheter insertion success rates among junior residents. J Ultrasound Med. 2012;31(10):1519-1526. https://doi.org/10.7863/jum.2012.31.10.1519.
5. Cavanna L, Mordenti P, Bertè R, et al. Ultrasound guidance reduces pneumothorax rate and improves safety of thoracentesis in malignant pleural effusion: Report on 445 consecutive patients with advanced cancer. World J Surg Oncol. 2014;12:139. https://doi.org/10.1186/1477-7819-12-139.
6. Testa A, Francesconi A, Giannuzzi R, Berardi S, Sbraccia P. Economic analysis of bedside ultrasonography (US) implementation in an Internal Medicine department. Intern Emerg Med. 2015;10(8):1015-1024. https://doi.org/10.1007/s11739-015-1320-7.
7. Howard ZD, Noble VE, Marill KA, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46-53. https://doi.org/10.1016/j.jemermed.2013.05.044.
8. Park YH, Jung RB, Lee YG, et al. Does the use of bedside ultrasonography reduce emergency department length of stay for patients with renal colic? A pilot study. Clin Exp Emerg Med. 2016;3(4):197-203. https://doi.org/10.15441/ceem.15.109.
9. Glomb N, D’Amico B, Rus M, Chen C. Point-of-care ultrasound in resource-limited settings. Clin Pediatr Emerg Med. 2015;16(4):256-261. https://doi.org/10.1016/j.cpem.2015.10.001.
10. Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89(12):1681-1686. https://doi.org/10.1097/ACM.0000000000000414.
11. Hall JWW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: A CERA study. Fam Med. 2015;47(9):706-711.
12. Schnobrich DJ, Gladding S, Olson APJ, Duran-Nelson A. Point-of-care ultrasound in internal medicine: A national survey of educational leadership. J Grad Med Educ. 2013;5(3):498-502. https://doi.org/10.4300/JGME-D-12-00215.1.
13. Stolz LA, Stolz U, Fields JM, et al. Emergency medicine resident assessment of the emergency ultrasound milestones and current training recommendations. Acad Emerg Med. 2017;24(3):353-361. https://doi.org/10.1111/acem.13113.
14. Kumar, A., Jensen, T., Kugler, J. Evaluation of trainee competency with point-of-care ultrasonography (POCUS): A conceptual framework and review of existing assessments. J Gen Intern Med. 2019;34(6):1025-1031. https://doi.org/10.1007/s11606-019-04945-4.
15. Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients—part ii: Cardiac ultrasonography. Crit Care Med. 2016;44(6):1206-1227. https://doi.org/10.1097/CCM.0000000000001847.
16. Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002-1006. https://doi.org/10.1016/j.amjcard.2005.05.060.
17. Ceriani E, Cogliati C. Update on bedside ultrasound diagnosis of pericardial effusion. Intern Emerg Med. 2016;11(3):477-480. https://doi.org/10.1007/s11739-015-1372-8.
18. Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: A consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23(12):1225-1230. https://doi.org/10.1016/j.echo.2010.10.005.
19. Keil-Ríos D, Terrazas-Solís H, González-Garay A, Sánchez-Ávila JF, García-Juárez I. Pocket ultrasound device as a complement to physical examination for ascites evaluation and guided paracentesis. Intern Emerg Med. 2016;11(3):461-466. https://doi.org/10.1007/s11739-016-1406-x.
20. Riddell J, Case A, Wopat R, et al. Sensitivity of emergency bedside ultrasound to detect hydronephrosis in patients with computed tomography–proven stones. West J Emerg Med. 2014;15(1):96-100. https://doi.org/10.5811/westjem.2013.9.15874.
21. Dalziel PJ, Noble VE. Bedside ultrasound and the assessment of renal colic: A review. Emerg Med J. 2013;30(1):3-8. https://doi.org/10.1136/emermed-2012-201375.
22. Whitson MR, Mayo PH. Ultrasonography in the emergency department. Crit Care. 2016;20(1):227. https://doi.org/10.1186/s13054-016-1399-x.
23. Kumar A, Liu G, Chi J, Kugler J. The role of technology in the bedside encounter. Med Clin North Am. 2018;102(3):443-451. https://doi.org/10.1016/j.mcna.2017.12.006.
24. Ma IWY, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: Consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052-1057. https://doi.org/10.1007/s11606-017-4071-5.
15. Sabath BF, Singh G. Point-of-care ultrasonography as a training milestone for internal medicine residents: The time is now. J Community Hosp Intern Med Perspect. 2016;6(5):33094. https://doi.org/10.3402/jchimp.v6.33094.
26. American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69(5):e27-e54. https://doi.org/10.1016/j.annemergmed.2016.08.457.
27. Ramsingh D, Rinehart J, Kain Z, et al. Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology. 2015;123(3):670-682. https://doi.org/10.1097/ALN.0000000000000776.
28. Keddis MT, Cullen MW, Reed DA, et al. Effectiveness of an ultrasound training module for internal medicine residents. BMC Med Educ. 2011;11:75. https://doi.org/10.1186/1472-6920-11-75.
29. Townsend NT, Kendall J, Barnett C, Robinson T. An effective curriculum for focused assessment diagnostic echocardiography: Establishing the learning curve in surgical residents. J Surg Educ. 2016;73(2):190-196. https://doi.org/10.1016/j.jsurg.2015.10.009.
30. Hoppmann RA, Rao VV, Bell F, et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J. 2015;7(1):18. https://doi.org/10.1186/s13089-015-0035-3.
31. Skalski JH, Elrashidi M, Reed DA, McDonald FS, Bhagra A. Using standardized patients to teach point-of-care ultrasound–guided physical examination skills to internal medicine residents. J Grad Med Educ. 2015;7(1):95-97. https://doi.org/10.4300/JGME-D-14-00178.1.
32. Chisholm CB, Dodge WR, Balise RR, Williams SR, Gharahbaghian L, Beraud A-S. Focused cardiac ultrasound training: How much is enough? J Emerg Med. 2013;44(4):818-822. https://doi.org/10.1016/j.jemermed.2012.07.092.
33. Schmidt GA, Schraufnagel D. Introduction to ATS seminars: Intensive care ultrasound. Ann Am Thorac Soc. 2013;10(5):538-539. https://doi.org/10.1513/AnnalsATS.201306-203ED.
34. Skaarup SH, Laursen CB, Bjerrum AS, Hilberg O. Objective and structured assessment of lung ultrasound competence. A multispecialty Delphi consensus and construct validity study. Ann Am Thorac Soc. 2017;14(4):555-560. https://doi.org/10.1513/AnnalsATS.201611-894OC.
35. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: A position statement of the Society of Hospital Medicine. J Hosp Med. 2018;13(2):117-125. https://doi.org/10.12788/jhm.2917.
36. Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part i: General ultrasonography. Crit Care Med. 2015;43(11):2479-2502. https://doi.org/10.1097/CCM.0000000000001216.
37. Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed by hospitalists: Does it improve the cardiac physical examination? Am J Med. 2009;122(1):35-41. https://doi.org/10.1016/j.amjmed.2008.07.022.
38. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty-hour flexibility trial in internal medicine. N Engl J Med. 2018;378(16):1494-1508. https://doi.org/10.1056/NEJMoa1800965.
39. Baltarowich OH, Di Salvo DN, Scoutt LM, et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014;30(1):13-19. https://doi.org/10.1097/RUQ.0000000000000066.
40. Beal EW, Sigmond BR, Sage-Silski L, Lahey S, Nguyen V, Bahner DP. Point-of-care ultrasound in general surgery residency training: A proposal for milestones in graduate medical education ultrasound. J Ultrasound Med. 2017;36(12):2577-2584. https://doi.org/10.1002/jum.14298.
41. Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77(6):1121-1134. https://doi.org/10.1037//0022-3514.77.6.1121.
Point-of-care ultrasonography (POCUS) can transform healthcare delivery through its diagnostic and therapeutic expediency.1 POCUS has been shown to bolster diagnostic accuracy, reduce procedural complications, decrease inpatient length of stay, and improve patient satisfaction by encouraging the physician to be present at the bedside.2-8
POCUS has become widespread across a variety of clinical settings as more investigations have demonstrated its positive impact on patient care.1,9-12 This includes the use of POCUS by trainees, who are now utilizing this technology as part of their assessments of patients.13,14 However, trainees may be performing these examinations with minimal oversight, and outside of emergency medicine, there are few guidelines on how to effectively teach POCUS or measure competency.13,14 While POCUS is rapidly becoming a part of inpatient care, teaching physicians may have little experience in ultrasound or the expertise to adequately supervise trainees.14 There is a growing need to study what trainees can learn and how this knowledge is acquired.
Previous investigations have demonstrated that inexperienced users can be taught to use POCUS to identify a variety of pathological states.2,3,15-23 Most of these curricula used a single lecture series as their pedagogical vehicle, and they variably included junior medical trainees. More importantly, the investigations did not explore whether personal access to handheld ultrasound devices (HUDs) improved learning. In theory, improved access to POCUS devices increases opportunities for authentic and deliberate practice, which may be needed to improve trainee skill with POCUS beyond the classroom setting.14
This study aimed to address several ongoing gaps in knowledge related to learning POCUS. First, we hypothesized that personal HUD access would improve trainees’ POCUS-related knowledge and interpretive ability as a result of increased practice opportunities. Second, we hypothesized that trainees who receive personal access to HUDs would be more likely to perform POCUS examinations and feel more confident in their interpretations. Finally, we hypothesized that repeated exposure to POCUS-related lectures would result in greater improvements in knowledge as compared with a single lecture series.
METHODS
Participants and Setting
The 2017 intern class (n = 47) at an academic internal medicine residency program participated in the study. Control data were obtained from the 2016 intern class (historical control; n = 50) and the 2018 intern class (contemporaneous control; n = 52). The Stanford University Institutional Review Board approved this study.
Study Design
The 2017 intern class (n = 47) received POCUS didactics from June 2017 to June 2018. To evaluate if increased access to HUDs improved learning outcomes, the 2017 interns were randomized 1:1 to receive their own personal HUD that could be used for patient care and/or self-directed learning (n = 24) vs no-HUD (n = 23; Figure). Learning outcomes were assessed over the course of 1 year (see “Outcomes” below) and were compared with the 2016 and 2018 controls. The 2016 intern class had completed a year of training but had not received formalized POCUS didactics (historical control), whereas the 2018 intern class was assessed at the beginning of their year (contemporaneous control; Figure). In order to make comparisons based on intern experience, baseline data for the 2017 intern class were compared with the 2018 intern class, whereas end-of-study data for 2017 interns were compared with 2016 interns.
Outcomes
The primary outcome was the difference in assessment scores at the end of the study period between interns randomized to receive a HUD and those who were not. Secondary outcomes included differences in HUD usage rates, lecture attendance, and assessment scores. To assess whether repeated lecture exposure resulted in greater amounts of learning, this study evaluated for assessment score improvements after each lecture block. Finally, trainee attitudes toward POCUS and their confidence in their interpretative ability were measured at the beginning and end of the study period.
Curriculum Implementation
The lectures were administered as once-weekly didactics of 1-hour duration to interns rotating on the inpatient wards rotation. This rotation is 4 weeks long, and each intern will experience the rotation two to four times per year. Each lecture contained two parts: (1) 20-30 minutes of didactics via Microsoft PowerPointTM and (2) 30-40 minutes of supervised practice using HUDs on standardized patients. Four lectures were given each month: (1) introduction to POCUS and ultrasound physics, (2) thoracic/lung ultrasound, (3) echocardiography, and (4) abdominal POCUS. The lectures consisted of contrasting cases of normal/abnormal videos and clinical vignettes. These four lectures were repeated each month as new interns rotated on service. Some interns experienced the same content multiple times, which was intentional in order to assess their rates of learning over time. Lecture contents were based on previously published guidelines and expert consensus for teaching POCUS in internal medicine.13, 24-26 Content from the Accreditation Council for Graduate Medical Education (ACGME) and the American College of Emergency Physicians (ACEP) was also incorporated because these organizations had published relevant guidelines for teaching POCUS.13,26 Further development of the lectures occurred through review of previously described POCUS-relevant curricula.27-32
Handheld Ultrasound Devices
This study used the Philips LumifyTM, a United States Food and Drug Administration–approved device. Interns randomized to HUDs received their own device at the start of the rotation. It was at their discretion to use the device outside of the course. All devices were approved for patient use and were encrypted in compliance with our information security office. For privacy reasons, any saved patient images were not reviewed by the researchers. Interns were encouraged to share their findings with supervising physicians during rounds, but actual oversight was not measured. Interns not randomized to HUDs could access a single community device that was shared among all residents and fellows in the hospital. Interns reported the average number of POCUS examinations performed each week via a survey sent during the last week of the rotation.
Assessment Design and Implementation
Assessments evaluating trainee knowledge were administered before, during, and after the study period (Figure). For the 2017 cohort, assessments were also administered at the start and end of the ward month to track knowledge acquisition. Assessment contents were selected from POCUS guidelines for internal medicine and adaptation of the ACGME and ACEP guidelines.13,24,26 Additional content was obtained from major society POCUS tutorials and deidentified images collected by the study authors.13,24,33 In keeping with previously described methodology, the images were shown for approximately 12 seconds, followed by five additional seconds to allow the learner to answer the question.32 Final assessment contents were determined by the authors using the Delphi method.34 A sample assessment can be found in the Appendix Material.
Surveys
Surveys were administered alongside the assessments to the 2016-2018 intern classes. These surveys assessed trainee attitudes toward POCUS and were based on previously validated assessments.27,28,30 Attitudes were measured using 5-point Likert scales.
Statistical Analysis
For the primary outcome, we performed generalized binomial mixed-effect regressions using the survey periods, randomization group, and the interaction of the two as independent variables after adjusting for attendance and controlling of intra-intern correlations. The bivariate unadjusted analysis was performed to display the distribution of overall correctness on the assessments. Wilcoxon signed rank test was used to determine score significance for dependent score variables (R-Statistical Programming Language, Vienna, Austria).
RESULTS
Baseline Characteristics
There were 149 interns who participated in this study (Figure). Assessment/survey completion rates were as follows: 2016 control: 68.0%; 2017 preintervention: 97.9%; 2017 postintervention: 89.4%; and 2018 control: 100%. The 2017 interns reported similar amounts of prior POCUS exposure in medical school (Table 1).
Primary Outcome: Assessment Scores (HUD vs no HUD)
There were no significant differences in assessment scores at the end of the study between interns randomized to personal HUD access vs those to no-HUD access (Table 1). HUD interns reported performing POCUS assessments on patients a mean 6.8 (standard deviation [SD] 2.2) times per week vs 6.4 (SD 2.9) times per week in the no-HUD arm (P = .66). The mean lecture attendance was 75.0% and did not significantly differ between the HUD arms (Table 1).
Secondary Outcomes
Impact of Repeating Lectures
The 2017 interns demonstrated significant increases in preblock vs postblock assessment scores after first-time exposure to the lectures (median preblock score 0.61 [interquartile range (IQR), 0.53-0.70] vs postblock score 0.81 [IQR, 0.72-0.86]; P < .001; Table 2). However, intern performance on the preblock vs postblock assessments after second-time exposure to the curriculum failed to improve (median second preblock score 0.78 [IQR, 0.69-0.83] vs postblock score 0.81 [IQR, 0.64-0.89]; P = .94). Intern performance on individual domains of knowledge for each block is listed in Appendix Table 1.
Intervention Performance vs Controls
The 2016 historical control had significantly higher scores compared with the 2017 preintervention group (P < .001; Appendix Table 2). The year-long lecture series resulted in significant increases in median scores for the 2017 group (median preintervention score 0.55 [0.41-0.61] vs median postintervention score 0.84 [0.71-0.90]; P = .006; Appendix Table 1). At the end of the study, the 2017 postintervention scores were significantly higher across multiple knowledge domains compared with the 2016 historical control (Appendix Table 2).
Survey Results
Notably, the 2017 intern class at the end of the intervention did not have significantly different assessment scores for several disease-specific domains, compared with the 2016 control (Appendix Table 2). Nonetheless, the 2017 intern class reported higher levels of confidence in these same domains despite similar scores (Supplementary Figure). The HUD group seldomly cited a lack of confidence in their abilities as a barrier to performing POCUS examinations (17.6%), compared with the no-HUD group (50.0%), despite nearly identical assessment scores between the two groups (Table 1).
DISCUSSION
Previous guidelines have recommended increased HUD access for learners,13,24,35,36 but there have been few investigations that have evaluated the impact of such access on learning POCUS. One previous investigation found that hospitalists who carried HUDs were more likely to identify heart failure on bedside examination.37 In contrast, our study found no improvement in interpretative ability when randomizing interns to carry HUDs for patient care. Notably, interns did not perform more POCUS examinations when given HUDs. We offer several explanations for this finding. First, time-motion studies have demonstrated that internal medicine interns spend less than 15% of their time toward direct patient care.38 It is possible that the demands of being an intern impeded their ability to perform more POCUS examinations on their patients, regardless of HUD access. Alternatively, the interns randomized to no personal access may have used the community device more frequently as a result of the lecture series. Given the cost of HUDs, further studies are needed to assess the degree to which HUD access will improve trainee interpretive ability, especially as more training programs consider the creation of ultrasound curricula.10,11,24,39,40
This study was unique because it followed interns over a year-long course that repeated the same material to assess rates of learning with repeated exposure. Learners improved their scores after the first, but not second, block. Furthermore, the median scores were nearly identical between the first postblock assessment and second preblock assessment (0.81 vs 0.78), suggesting that knowledge was retained between blocks. Together, these findings suggest there may be limitations of traditional lectures that use standardized patient models for practice. Supplementary pedagogies, such as in-the-moment feedback with actual patients, may be needed to promote mastery.14,35
Despite no formal curriculum, the 2016 intern class (historical control) had learned POCUS to some degree based on their higher assessment scores compared with the 2017 intern class during the preintervention period. Such learning may be informal, and yet, trainees may feel confident in making clinical decisions without formalized training, accreditation, or oversight. As suggested by this study, adding regular didactics or giving trainees HUDs may not immediately solve this issue. For assessment items in which the 2017 interns did not significantly differ from the controls, they nonetheless reported higher confidence in their abilities. Similarly, interns randomized to HUDs less frequently cited a lack of confidence in their abilities, despite similar scores to the no-HUD group. Such confidence may be incongruent with their actual knowledge or ability to safely use POCUS. This phenomenon of misplaced confidence is known as the Dunning–Kruger effect, and it may be common with ultrasound learning.41 While confidence can be part of a holistic definition of competency,14 these results raise the concern that trainees may have difficulty assessing their own competency level with POCUS.35
There are several limitations to this study. It was performed at a single institution with limited sample size. It examined only intern physicians because of funding constraints, which limits the generalizability of these findings among medical trainees. Technical ability assessments (including obtaining and interpreting images) were not included. We were unable to track the timing or location of the devices’ usage, and the interns’ self-reported usage rates may be subject to recall bias. To our knowledge, there were no significant lapses in device availability/functionality. Intern physicians in the HUD arm did not receive formal feedback on personally acquired patient images, which may have limited the intervention’s impact.
In conclusion, internal medicine interns who received personal HUDs were not better at recognizing normal/abnormal findings on image assessments, and they did not report performing more POCUS examinations. Since the minority of a trainee’s time is spent toward direct patient care, offering trainees HUDs without substantial guidance may not be enough to promote mastery. Notably, trainees who received HUDs felt more confident in their abilities, despite no objective increase in their actual skill. Finally, interns who received POCUS-related lectures experienced significant benefit upon first exposure to the material, while repeated exposures did not improve performance. Future investigations should stringently track trainee POCUS usage rates with HUDs and assess whether image acquisition ability improves as a result of personal access.
Point-of-care ultrasonography (POCUS) can transform healthcare delivery through its diagnostic and therapeutic expediency.1 POCUS has been shown to bolster diagnostic accuracy, reduce procedural complications, decrease inpatient length of stay, and improve patient satisfaction by encouraging the physician to be present at the bedside.2-8
POCUS has become widespread across a variety of clinical settings as more investigations have demonstrated its positive impact on patient care.1,9-12 This includes the use of POCUS by trainees, who are now utilizing this technology as part of their assessments of patients.13,14 However, trainees may be performing these examinations with minimal oversight, and outside of emergency medicine, there are few guidelines on how to effectively teach POCUS or measure competency.13,14 While POCUS is rapidly becoming a part of inpatient care, teaching physicians may have little experience in ultrasound or the expertise to adequately supervise trainees.14 There is a growing need to study what trainees can learn and how this knowledge is acquired.
Previous investigations have demonstrated that inexperienced users can be taught to use POCUS to identify a variety of pathological states.2,3,15-23 Most of these curricula used a single lecture series as their pedagogical vehicle, and they variably included junior medical trainees. More importantly, the investigations did not explore whether personal access to handheld ultrasound devices (HUDs) improved learning. In theory, improved access to POCUS devices increases opportunities for authentic and deliberate practice, which may be needed to improve trainee skill with POCUS beyond the classroom setting.14
This study aimed to address several ongoing gaps in knowledge related to learning POCUS. First, we hypothesized that personal HUD access would improve trainees’ POCUS-related knowledge and interpretive ability as a result of increased practice opportunities. Second, we hypothesized that trainees who receive personal access to HUDs would be more likely to perform POCUS examinations and feel more confident in their interpretations. Finally, we hypothesized that repeated exposure to POCUS-related lectures would result in greater improvements in knowledge as compared with a single lecture series.
METHODS
Participants and Setting
The 2017 intern class (n = 47) at an academic internal medicine residency program participated in the study. Control data were obtained from the 2016 intern class (historical control; n = 50) and the 2018 intern class (contemporaneous control; n = 52). The Stanford University Institutional Review Board approved this study.
Study Design
The 2017 intern class (n = 47) received POCUS didactics from June 2017 to June 2018. To evaluate if increased access to HUDs improved learning outcomes, the 2017 interns were randomized 1:1 to receive their own personal HUD that could be used for patient care and/or self-directed learning (n = 24) vs no-HUD (n = 23; Figure). Learning outcomes were assessed over the course of 1 year (see “Outcomes” below) and were compared with the 2016 and 2018 controls. The 2016 intern class had completed a year of training but had not received formalized POCUS didactics (historical control), whereas the 2018 intern class was assessed at the beginning of their year (contemporaneous control; Figure). In order to make comparisons based on intern experience, baseline data for the 2017 intern class were compared with the 2018 intern class, whereas end-of-study data for 2017 interns were compared with 2016 interns.
Outcomes
The primary outcome was the difference in assessment scores at the end of the study period between interns randomized to receive a HUD and those who were not. Secondary outcomes included differences in HUD usage rates, lecture attendance, and assessment scores. To assess whether repeated lecture exposure resulted in greater amounts of learning, this study evaluated for assessment score improvements after each lecture block. Finally, trainee attitudes toward POCUS and their confidence in their interpretative ability were measured at the beginning and end of the study period.
Curriculum Implementation
The lectures were administered as once-weekly didactics of 1-hour duration to interns rotating on the inpatient wards rotation. This rotation is 4 weeks long, and each intern will experience the rotation two to four times per year. Each lecture contained two parts: (1) 20-30 minutes of didactics via Microsoft PowerPointTM and (2) 30-40 minutes of supervised practice using HUDs on standardized patients. Four lectures were given each month: (1) introduction to POCUS and ultrasound physics, (2) thoracic/lung ultrasound, (3) echocardiography, and (4) abdominal POCUS. The lectures consisted of contrasting cases of normal/abnormal videos and clinical vignettes. These four lectures were repeated each month as new interns rotated on service. Some interns experienced the same content multiple times, which was intentional in order to assess their rates of learning over time. Lecture contents were based on previously published guidelines and expert consensus for teaching POCUS in internal medicine.13, 24-26 Content from the Accreditation Council for Graduate Medical Education (ACGME) and the American College of Emergency Physicians (ACEP) was also incorporated because these organizations had published relevant guidelines for teaching POCUS.13,26 Further development of the lectures occurred through review of previously described POCUS-relevant curricula.27-32
Handheld Ultrasound Devices
This study used the Philips LumifyTM, a United States Food and Drug Administration–approved device. Interns randomized to HUDs received their own device at the start of the rotation. It was at their discretion to use the device outside of the course. All devices were approved for patient use and were encrypted in compliance with our information security office. For privacy reasons, any saved patient images were not reviewed by the researchers. Interns were encouraged to share their findings with supervising physicians during rounds, but actual oversight was not measured. Interns not randomized to HUDs could access a single community device that was shared among all residents and fellows in the hospital. Interns reported the average number of POCUS examinations performed each week via a survey sent during the last week of the rotation.
Assessment Design and Implementation
Assessments evaluating trainee knowledge were administered before, during, and after the study period (Figure). For the 2017 cohort, assessments were also administered at the start and end of the ward month to track knowledge acquisition. Assessment contents were selected from POCUS guidelines for internal medicine and adaptation of the ACGME and ACEP guidelines.13,24,26 Additional content was obtained from major society POCUS tutorials and deidentified images collected by the study authors.13,24,33 In keeping with previously described methodology, the images were shown for approximately 12 seconds, followed by five additional seconds to allow the learner to answer the question.32 Final assessment contents were determined by the authors using the Delphi method.34 A sample assessment can be found in the Appendix Material.
Surveys
Surveys were administered alongside the assessments to the 2016-2018 intern classes. These surveys assessed trainee attitudes toward POCUS and were based on previously validated assessments.27,28,30 Attitudes were measured using 5-point Likert scales.
Statistical Analysis
For the primary outcome, we performed generalized binomial mixed-effect regressions using the survey periods, randomization group, and the interaction of the two as independent variables after adjusting for attendance and controlling of intra-intern correlations. The bivariate unadjusted analysis was performed to display the distribution of overall correctness on the assessments. Wilcoxon signed rank test was used to determine score significance for dependent score variables (R-Statistical Programming Language, Vienna, Austria).
RESULTS
Baseline Characteristics
There were 149 interns who participated in this study (Figure). Assessment/survey completion rates were as follows: 2016 control: 68.0%; 2017 preintervention: 97.9%; 2017 postintervention: 89.4%; and 2018 control: 100%. The 2017 interns reported similar amounts of prior POCUS exposure in medical school (Table 1).
Primary Outcome: Assessment Scores (HUD vs no HUD)
There were no significant differences in assessment scores at the end of the study between interns randomized to personal HUD access vs those to no-HUD access (Table 1). HUD interns reported performing POCUS assessments on patients a mean 6.8 (standard deviation [SD] 2.2) times per week vs 6.4 (SD 2.9) times per week in the no-HUD arm (P = .66). The mean lecture attendance was 75.0% and did not significantly differ between the HUD arms (Table 1).
Secondary Outcomes
Impact of Repeating Lectures
The 2017 interns demonstrated significant increases in preblock vs postblock assessment scores after first-time exposure to the lectures (median preblock score 0.61 [interquartile range (IQR), 0.53-0.70] vs postblock score 0.81 [IQR, 0.72-0.86]; P < .001; Table 2). However, intern performance on the preblock vs postblock assessments after second-time exposure to the curriculum failed to improve (median second preblock score 0.78 [IQR, 0.69-0.83] vs postblock score 0.81 [IQR, 0.64-0.89]; P = .94). Intern performance on individual domains of knowledge for each block is listed in Appendix Table 1.
Intervention Performance vs Controls
The 2016 historical control had significantly higher scores compared with the 2017 preintervention group (P < .001; Appendix Table 2). The year-long lecture series resulted in significant increases in median scores for the 2017 group (median preintervention score 0.55 [0.41-0.61] vs median postintervention score 0.84 [0.71-0.90]; P = .006; Appendix Table 1). At the end of the study, the 2017 postintervention scores were significantly higher across multiple knowledge domains compared with the 2016 historical control (Appendix Table 2).
Survey Results
Notably, the 2017 intern class at the end of the intervention did not have significantly different assessment scores for several disease-specific domains, compared with the 2016 control (Appendix Table 2). Nonetheless, the 2017 intern class reported higher levels of confidence in these same domains despite similar scores (Supplementary Figure). The HUD group seldomly cited a lack of confidence in their abilities as a barrier to performing POCUS examinations (17.6%), compared with the no-HUD group (50.0%), despite nearly identical assessment scores between the two groups (Table 1).
DISCUSSION
Previous guidelines have recommended increased HUD access for learners,13,24,35,36 but there have been few investigations that have evaluated the impact of such access on learning POCUS. One previous investigation found that hospitalists who carried HUDs were more likely to identify heart failure on bedside examination.37 In contrast, our study found no improvement in interpretative ability when randomizing interns to carry HUDs for patient care. Notably, interns did not perform more POCUS examinations when given HUDs. We offer several explanations for this finding. First, time-motion studies have demonstrated that internal medicine interns spend less than 15% of their time toward direct patient care.38 It is possible that the demands of being an intern impeded their ability to perform more POCUS examinations on their patients, regardless of HUD access. Alternatively, the interns randomized to no personal access may have used the community device more frequently as a result of the lecture series. Given the cost of HUDs, further studies are needed to assess the degree to which HUD access will improve trainee interpretive ability, especially as more training programs consider the creation of ultrasound curricula.10,11,24,39,40
This study was unique because it followed interns over a year-long course that repeated the same material to assess rates of learning with repeated exposure. Learners improved their scores after the first, but not second, block. Furthermore, the median scores were nearly identical between the first postblock assessment and second preblock assessment (0.81 vs 0.78), suggesting that knowledge was retained between blocks. Together, these findings suggest there may be limitations of traditional lectures that use standardized patient models for practice. Supplementary pedagogies, such as in-the-moment feedback with actual patients, may be needed to promote mastery.14,35
Despite no formal curriculum, the 2016 intern class (historical control) had learned POCUS to some degree based on their higher assessment scores compared with the 2017 intern class during the preintervention period. Such learning may be informal, and yet, trainees may feel confident in making clinical decisions without formalized training, accreditation, or oversight. As suggested by this study, adding regular didactics or giving trainees HUDs may not immediately solve this issue. For assessment items in which the 2017 interns did not significantly differ from the controls, they nonetheless reported higher confidence in their abilities. Similarly, interns randomized to HUDs less frequently cited a lack of confidence in their abilities, despite similar scores to the no-HUD group. Such confidence may be incongruent with their actual knowledge or ability to safely use POCUS. This phenomenon of misplaced confidence is known as the Dunning–Kruger effect, and it may be common with ultrasound learning.41 While confidence can be part of a holistic definition of competency,14 these results raise the concern that trainees may have difficulty assessing their own competency level with POCUS.35
There are several limitations to this study. It was performed at a single institution with limited sample size. It examined only intern physicians because of funding constraints, which limits the generalizability of these findings among medical trainees. Technical ability assessments (including obtaining and interpreting images) were not included. We were unable to track the timing or location of the devices’ usage, and the interns’ self-reported usage rates may be subject to recall bias. To our knowledge, there were no significant lapses in device availability/functionality. Intern physicians in the HUD arm did not receive formal feedback on personally acquired patient images, which may have limited the intervention’s impact.
In conclusion, internal medicine interns who received personal HUDs were not better at recognizing normal/abnormal findings on image assessments, and they did not report performing more POCUS examinations. Since the minority of a trainee’s time is spent toward direct patient care, offering trainees HUDs without substantial guidance may not be enough to promote mastery. Notably, trainees who received HUDs felt more confident in their abilities, despite no objective increase in their actual skill. Finally, interns who received POCUS-related lectures experienced significant benefit upon first exposure to the material, while repeated exposures did not improve performance. Future investigations should stringently track trainee POCUS usage rates with HUDs and assess whether image acquisition ability improves as a result of personal access.
1. Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749-757. https://doi.org/10.1056/NEJMra0909487.
2. Akkaya A, Yesilaras M, Aksay E, Sever M, Atilla OD. The interrater reliability of ultrasound imaging of the inferior vena cava performed by emergency residents. Am J Emerg Med. 2013;31(10):1509-1511. https://doi.org/10.1016/j.ajem.2013.07.006.
3. Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr. 2011;24(12):1319-1324. https://doi.org/10.1016/j.echo.2011.07.013.
4. Dodge KL, Lynch CA, Moore CL, Biroscak BJ, Evans LV. Use of ultrasound guidance improves central venous catheter insertion success rates among junior residents. J Ultrasound Med. 2012;31(10):1519-1526. https://doi.org/10.7863/jum.2012.31.10.1519.
5. Cavanna L, Mordenti P, Bertè R, et al. Ultrasound guidance reduces pneumothorax rate and improves safety of thoracentesis in malignant pleural effusion: Report on 445 consecutive patients with advanced cancer. World J Surg Oncol. 2014;12:139. https://doi.org/10.1186/1477-7819-12-139.
6. Testa A, Francesconi A, Giannuzzi R, Berardi S, Sbraccia P. Economic analysis of bedside ultrasonography (US) implementation in an Internal Medicine department. Intern Emerg Med. 2015;10(8):1015-1024. https://doi.org/10.1007/s11739-015-1320-7.
7. Howard ZD, Noble VE, Marill KA, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46-53. https://doi.org/10.1016/j.jemermed.2013.05.044.
8. Park YH, Jung RB, Lee YG, et al. Does the use of bedside ultrasonography reduce emergency department length of stay for patients with renal colic? A pilot study. Clin Exp Emerg Med. 2016;3(4):197-203. https://doi.org/10.15441/ceem.15.109.
9. Glomb N, D’Amico B, Rus M, Chen C. Point-of-care ultrasound in resource-limited settings. Clin Pediatr Emerg Med. 2015;16(4):256-261. https://doi.org/10.1016/j.cpem.2015.10.001.
10. Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89(12):1681-1686. https://doi.org/10.1097/ACM.0000000000000414.
11. Hall JWW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: A CERA study. Fam Med. 2015;47(9):706-711.
12. Schnobrich DJ, Gladding S, Olson APJ, Duran-Nelson A. Point-of-care ultrasound in internal medicine: A national survey of educational leadership. J Grad Med Educ. 2013;5(3):498-502. https://doi.org/10.4300/JGME-D-12-00215.1.
13. Stolz LA, Stolz U, Fields JM, et al. Emergency medicine resident assessment of the emergency ultrasound milestones and current training recommendations. Acad Emerg Med. 2017;24(3):353-361. https://doi.org/10.1111/acem.13113.
14. Kumar, A., Jensen, T., Kugler, J. Evaluation of trainee competency with point-of-care ultrasonography (POCUS): A conceptual framework and review of existing assessments. J Gen Intern Med. 2019;34(6):1025-1031. https://doi.org/10.1007/s11606-019-04945-4.
15. Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients—part ii: Cardiac ultrasonography. Crit Care Med. 2016;44(6):1206-1227. https://doi.org/10.1097/CCM.0000000000001847.
16. Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002-1006. https://doi.org/10.1016/j.amjcard.2005.05.060.
17. Ceriani E, Cogliati C. Update on bedside ultrasound diagnosis of pericardial effusion. Intern Emerg Med. 2016;11(3):477-480. https://doi.org/10.1007/s11739-015-1372-8.
18. Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: A consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23(12):1225-1230. https://doi.org/10.1016/j.echo.2010.10.005.
19. Keil-Ríos D, Terrazas-Solís H, González-Garay A, Sánchez-Ávila JF, García-Juárez I. Pocket ultrasound device as a complement to physical examination for ascites evaluation and guided paracentesis. Intern Emerg Med. 2016;11(3):461-466. https://doi.org/10.1007/s11739-016-1406-x.
20. Riddell J, Case A, Wopat R, et al. Sensitivity of emergency bedside ultrasound to detect hydronephrosis in patients with computed tomography–proven stones. West J Emerg Med. 2014;15(1):96-100. https://doi.org/10.5811/westjem.2013.9.15874.
21. Dalziel PJ, Noble VE. Bedside ultrasound and the assessment of renal colic: A review. Emerg Med J. 2013;30(1):3-8. https://doi.org/10.1136/emermed-2012-201375.
22. Whitson MR, Mayo PH. Ultrasonography in the emergency department. Crit Care. 2016;20(1):227. https://doi.org/10.1186/s13054-016-1399-x.
23. Kumar A, Liu G, Chi J, Kugler J. The role of technology in the bedside encounter. Med Clin North Am. 2018;102(3):443-451. https://doi.org/10.1016/j.mcna.2017.12.006.
24. Ma IWY, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: Consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052-1057. https://doi.org/10.1007/s11606-017-4071-5.
15. Sabath BF, Singh G. Point-of-care ultrasonography as a training milestone for internal medicine residents: The time is now. J Community Hosp Intern Med Perspect. 2016;6(5):33094. https://doi.org/10.3402/jchimp.v6.33094.
26. American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69(5):e27-e54. https://doi.org/10.1016/j.annemergmed.2016.08.457.
27. Ramsingh D, Rinehart J, Kain Z, et al. Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology. 2015;123(3):670-682. https://doi.org/10.1097/ALN.0000000000000776.
28. Keddis MT, Cullen MW, Reed DA, et al. Effectiveness of an ultrasound training module for internal medicine residents. BMC Med Educ. 2011;11:75. https://doi.org/10.1186/1472-6920-11-75.
29. Townsend NT, Kendall J, Barnett C, Robinson T. An effective curriculum for focused assessment diagnostic echocardiography: Establishing the learning curve in surgical residents. J Surg Educ. 2016;73(2):190-196. https://doi.org/10.1016/j.jsurg.2015.10.009.
30. Hoppmann RA, Rao VV, Bell F, et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J. 2015;7(1):18. https://doi.org/10.1186/s13089-015-0035-3.
31. Skalski JH, Elrashidi M, Reed DA, McDonald FS, Bhagra A. Using standardized patients to teach point-of-care ultrasound–guided physical examination skills to internal medicine residents. J Grad Med Educ. 2015;7(1):95-97. https://doi.org/10.4300/JGME-D-14-00178.1.
32. Chisholm CB, Dodge WR, Balise RR, Williams SR, Gharahbaghian L, Beraud A-S. Focused cardiac ultrasound training: How much is enough? J Emerg Med. 2013;44(4):818-822. https://doi.org/10.1016/j.jemermed.2012.07.092.
33. Schmidt GA, Schraufnagel D. Introduction to ATS seminars: Intensive care ultrasound. Ann Am Thorac Soc. 2013;10(5):538-539. https://doi.org/10.1513/AnnalsATS.201306-203ED.
34. Skaarup SH, Laursen CB, Bjerrum AS, Hilberg O. Objective and structured assessment of lung ultrasound competence. A multispecialty Delphi consensus and construct validity study. Ann Am Thorac Soc. 2017;14(4):555-560. https://doi.org/10.1513/AnnalsATS.201611-894OC.
35. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: A position statement of the Society of Hospital Medicine. J Hosp Med. 2018;13(2):117-125. https://doi.org/10.12788/jhm.2917.
36. Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part i: General ultrasonography. Crit Care Med. 2015;43(11):2479-2502. https://doi.org/10.1097/CCM.0000000000001216.
37. Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed by hospitalists: Does it improve the cardiac physical examination? Am J Med. 2009;122(1):35-41. https://doi.org/10.1016/j.amjmed.2008.07.022.
38. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty-hour flexibility trial in internal medicine. N Engl J Med. 2018;378(16):1494-1508. https://doi.org/10.1056/NEJMoa1800965.
39. Baltarowich OH, Di Salvo DN, Scoutt LM, et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014;30(1):13-19. https://doi.org/10.1097/RUQ.0000000000000066.
40. Beal EW, Sigmond BR, Sage-Silski L, Lahey S, Nguyen V, Bahner DP. Point-of-care ultrasound in general surgery residency training: A proposal for milestones in graduate medical education ultrasound. J Ultrasound Med. 2017;36(12):2577-2584. https://doi.org/10.1002/jum.14298.
41. Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77(6):1121-1134. https://doi.org/10.1037//0022-3514.77.6.1121.
1. Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749-757. https://doi.org/10.1056/NEJMra0909487.
2. Akkaya A, Yesilaras M, Aksay E, Sever M, Atilla OD. The interrater reliability of ultrasound imaging of the inferior vena cava performed by emergency residents. Am J Emerg Med. 2013;31(10):1509-1511. https://doi.org/10.1016/j.ajem.2013.07.006.
3. Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr. 2011;24(12):1319-1324. https://doi.org/10.1016/j.echo.2011.07.013.
4. Dodge KL, Lynch CA, Moore CL, Biroscak BJ, Evans LV. Use of ultrasound guidance improves central venous catheter insertion success rates among junior residents. J Ultrasound Med. 2012;31(10):1519-1526. https://doi.org/10.7863/jum.2012.31.10.1519.
5. Cavanna L, Mordenti P, Bertè R, et al. Ultrasound guidance reduces pneumothorax rate and improves safety of thoracentesis in malignant pleural effusion: Report on 445 consecutive patients with advanced cancer. World J Surg Oncol. 2014;12:139. https://doi.org/10.1186/1477-7819-12-139.
6. Testa A, Francesconi A, Giannuzzi R, Berardi S, Sbraccia P. Economic analysis of bedside ultrasonography (US) implementation in an Internal Medicine department. Intern Emerg Med. 2015;10(8):1015-1024. https://doi.org/10.1007/s11739-015-1320-7.
7. Howard ZD, Noble VE, Marill KA, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46-53. https://doi.org/10.1016/j.jemermed.2013.05.044.
8. Park YH, Jung RB, Lee YG, et al. Does the use of bedside ultrasonography reduce emergency department length of stay for patients with renal colic? A pilot study. Clin Exp Emerg Med. 2016;3(4):197-203. https://doi.org/10.15441/ceem.15.109.
9. Glomb N, D’Amico B, Rus M, Chen C. Point-of-care ultrasound in resource-limited settings. Clin Pediatr Emerg Med. 2015;16(4):256-261. https://doi.org/10.1016/j.cpem.2015.10.001.
10. Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89(12):1681-1686. https://doi.org/10.1097/ACM.0000000000000414.
11. Hall JWW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: A CERA study. Fam Med. 2015;47(9):706-711.
12. Schnobrich DJ, Gladding S, Olson APJ, Duran-Nelson A. Point-of-care ultrasound in internal medicine: A national survey of educational leadership. J Grad Med Educ. 2013;5(3):498-502. https://doi.org/10.4300/JGME-D-12-00215.1.
13. Stolz LA, Stolz U, Fields JM, et al. Emergency medicine resident assessment of the emergency ultrasound milestones and current training recommendations. Acad Emerg Med. 2017;24(3):353-361. https://doi.org/10.1111/acem.13113.
14. Kumar, A., Jensen, T., Kugler, J. Evaluation of trainee competency with point-of-care ultrasonography (POCUS): A conceptual framework and review of existing assessments. J Gen Intern Med. 2019;34(6):1025-1031. https://doi.org/10.1007/s11606-019-04945-4.
15. Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients—part ii: Cardiac ultrasonography. Crit Care Med. 2016;44(6):1206-1227. https://doi.org/10.1097/CCM.0000000000001847.
16. Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002-1006. https://doi.org/10.1016/j.amjcard.2005.05.060.
17. Ceriani E, Cogliati C. Update on bedside ultrasound diagnosis of pericardial effusion. Intern Emerg Med. 2016;11(3):477-480. https://doi.org/10.1007/s11739-015-1372-8.
18. Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: A consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23(12):1225-1230. https://doi.org/10.1016/j.echo.2010.10.005.
19. Keil-Ríos D, Terrazas-Solís H, González-Garay A, Sánchez-Ávila JF, García-Juárez I. Pocket ultrasound device as a complement to physical examination for ascites evaluation and guided paracentesis. Intern Emerg Med. 2016;11(3):461-466. https://doi.org/10.1007/s11739-016-1406-x.
20. Riddell J, Case A, Wopat R, et al. Sensitivity of emergency bedside ultrasound to detect hydronephrosis in patients with computed tomography–proven stones. West J Emerg Med. 2014;15(1):96-100. https://doi.org/10.5811/westjem.2013.9.15874.
21. Dalziel PJ, Noble VE. Bedside ultrasound and the assessment of renal colic: A review. Emerg Med J. 2013;30(1):3-8. https://doi.org/10.1136/emermed-2012-201375.
22. Whitson MR, Mayo PH. Ultrasonography in the emergency department. Crit Care. 2016;20(1):227. https://doi.org/10.1186/s13054-016-1399-x.
23. Kumar A, Liu G, Chi J, Kugler J. The role of technology in the bedside encounter. Med Clin North Am. 2018;102(3):443-451. https://doi.org/10.1016/j.mcna.2017.12.006.
24. Ma IWY, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: Consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052-1057. https://doi.org/10.1007/s11606-017-4071-5.
15. Sabath BF, Singh G. Point-of-care ultrasonography as a training milestone for internal medicine residents: The time is now. J Community Hosp Intern Med Perspect. 2016;6(5):33094. https://doi.org/10.3402/jchimp.v6.33094.
26. American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69(5):e27-e54. https://doi.org/10.1016/j.annemergmed.2016.08.457.
27. Ramsingh D, Rinehart J, Kain Z, et al. Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology. 2015;123(3):670-682. https://doi.org/10.1097/ALN.0000000000000776.
28. Keddis MT, Cullen MW, Reed DA, et al. Effectiveness of an ultrasound training module for internal medicine residents. BMC Med Educ. 2011;11:75. https://doi.org/10.1186/1472-6920-11-75.
29. Townsend NT, Kendall J, Barnett C, Robinson T. An effective curriculum for focused assessment diagnostic echocardiography: Establishing the learning curve in surgical residents. J Surg Educ. 2016;73(2):190-196. https://doi.org/10.1016/j.jsurg.2015.10.009.
30. Hoppmann RA, Rao VV, Bell F, et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J. 2015;7(1):18. https://doi.org/10.1186/s13089-015-0035-3.
31. Skalski JH, Elrashidi M, Reed DA, McDonald FS, Bhagra A. Using standardized patients to teach point-of-care ultrasound–guided physical examination skills to internal medicine residents. J Grad Med Educ. 2015;7(1):95-97. https://doi.org/10.4300/JGME-D-14-00178.1.
32. Chisholm CB, Dodge WR, Balise RR, Williams SR, Gharahbaghian L, Beraud A-S. Focused cardiac ultrasound training: How much is enough? J Emerg Med. 2013;44(4):818-822. https://doi.org/10.1016/j.jemermed.2012.07.092.
33. Schmidt GA, Schraufnagel D. Introduction to ATS seminars: Intensive care ultrasound. Ann Am Thorac Soc. 2013;10(5):538-539. https://doi.org/10.1513/AnnalsATS.201306-203ED.
34. Skaarup SH, Laursen CB, Bjerrum AS, Hilberg O. Objective and structured assessment of lung ultrasound competence. A multispecialty Delphi consensus and construct validity study. Ann Am Thorac Soc. 2017;14(4):555-560. https://doi.org/10.1513/AnnalsATS.201611-894OC.
35. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: A position statement of the Society of Hospital Medicine. J Hosp Med. 2018;13(2):117-125. https://doi.org/10.12788/jhm.2917.
36. Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part i: General ultrasonography. Crit Care Med. 2015;43(11):2479-2502. https://doi.org/10.1097/CCM.0000000000001216.
37. Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed by hospitalists: Does it improve the cardiac physical examination? Am J Med. 2009;122(1):35-41. https://doi.org/10.1016/j.amjmed.2008.07.022.
38. Desai SV, Asch DA, Bellini LM, et al. Education outcomes in a duty-hour flexibility trial in internal medicine. N Engl J Med. 2018;378(16):1494-1508. https://doi.org/10.1056/NEJMoa1800965.
39. Baltarowich OH, Di Salvo DN, Scoutt LM, et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014;30(1):13-19. https://doi.org/10.1097/RUQ.0000000000000066.
40. Beal EW, Sigmond BR, Sage-Silski L, Lahey S, Nguyen V, Bahner DP. Point-of-care ultrasound in general surgery residency training: A proposal for milestones in graduate medical education ultrasound. J Ultrasound Med. 2017;36(12):2577-2584. https://doi.org/10.1002/jum.14298.
41. Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77(6):1121-1134. https://doi.org/10.1037//0022-3514.77.6.1121.
© 2020 Society of Hospital Medicine
Things We Do for No Reason™: Card Flipping Rounds
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 32-year-old man with a history of polysubstance use disorder is hospitalized with endocarditis. The senior resident on the inpatient medical team suggests that the team “card flip” on this patient, citing a large number of patients on the team census, time constraints, and concerns that his substance use history will make bedside rounds uncomfortable.
BACKGROUND
“Rounds” is an inpatient care model in which teams of practitioners assess patients, determine care plans, and communicate with patients, families, and other healthcare professionals.1 One form of rounds is bedside rounding (BSR) through which an entire patient presentation occurs at the bedside, analogous to family-centered rounds common in pediatric inpatient care.2 This style of rounding is distinct from “walk rounding” that involves presentations occurring separately from a patient followed by a brief team bedside encounter. BSR is also different from “card flipping” or “table rounding” that involves presentations of a case separately without a team-patient encounter. The frequency of BSR at academic institutions has markedly decreased across the United States, and the time spent at the bedside is only a small fraction of rounding time.3
WHY YOU MIGHT THINK CARD FLIPPING IS HELPFUL
There are several reasons to employ strategies such as card-flipping or walk-rounding for discussing patient care away from the bedside. These BSR risks can be organized into patient harm, inefficiency, and risks to healthcare professional training.
First, BSR may result in patient harm. For example, discussing private health information in a semiprivate room may not only be uncomfortable for patients but may also violate patient privacy.4 Care teams are often large in number and rounding at the bedside can simultaneously trigger anxiety among patients, cause confusion about plans, or result in lack of clarity on the role of each provider.4 Furthermore, delivering bad news during BSR, or discussing sensitive topics such as substance use, psychiatric illness, or concerns of malingering behavior, may be difficult and uncomfortable.4,5 Additionally, some potential diagnoses, such as cancer or human immunodeficiency virus, even if unlikely, could induce panic among patients when they hear them being discussed.5 Trainees may also lose situational awareness because they focus on the agenda of bedside rounds and fail to respond to patients’ emotional needs.6
Efficiency is another reason to avoid BSR. The systemic factors of changing hospital demographics, such as short length of stay and increasing patient volumes, generate a substantial administrative burden on trainees.7 Modern trainees are also constrained by work hour restrictions, engagement with mandatory curricula, and other professional development opportunities. Furthermore, changes in a medical work environment cause trainees to rely heavily on electronic health records, which forces them to be at a computer instead of in a patient’s room.8 This confluence of factors results in substantial time pressure, and BSR is perceived as an inefficient use of time.9
The impact on education and trainee development is another concern of BSR. Rounding away from a patient ensures a safe environment for learners to interpret data and articulate clinical reasoning without the risk of embarrassment in front of a patient. This time outside a patient room also allows the team to have a shared mental model so that communication is aligned when a patient encounter does occur. Card flipping may result in improved trainee autonomy because the constant presence of attending supervision, particularly in front of patients, can risk undermining resident leadership and patient trust.9
WHY WE SHOULD RETURN TO THE BEDSIDE
The cited reasons for provider hesitancy to BSR, including possible patient harm and inefficiency, may be mostly related to individual perceptions and have recently been questioned.10,11
Several studies have suggested that bedside rounds may be better for patients’ experience over traditional walk-rounding or card-flipping models. In these studies, patients signal a preference for bedside rounds and suggest that discussing sensitive issues or concerning differential diagnoses during BSR may not be as concerning as physicians worry.11 For example, one randomized trial found that 87% of patients are untroubled by bedside discussions,12 and another trial revealed no difference between rounding models in emotional distress to patients or families.11 Patients and families also report higher levels of clarity from physicians, and they cited significantly improved levels of understanding their illness10 and test results.9 Furthermore, patients describe that physicians spend about twice as much time on their care when BSR is used.12 In many related studies, patients report a preference for BSR as a rounding strategy.2,11-13 For example, one study found that 99% of patients prefer BSR.13 Another study showed that 85% of families request to be part of bedside family-centered rounds over traditional walk rounding.2
Rounding away from a patient via card flipping or walk rounding seems more efficient, but this idea may be illusory. Although these strategies may seem faster, the lack of communication and coordination between team members and the patient may cause inefficiencies and delays in care throughout the day.14 For example, one study has demonstrated that family-centered bedside rounds are about 20% longer than walk rounding, but everyone involved, including housestaff, felt it was more efficient and saved time later in the day.2 Additionally, a study comparing BSR with walk rounding13 found no difference in time spent per patient, and another study has shown similar results in terms of family-centered rounds.15 Both studies have reported a similar amount of time spent per patient.
Physicians should return to BSR not only to improve patient experience but also to develop the clinical skills of trainees. The direct observation of trainees with patients allows high-level impactful clinical feedback and provides a basis for calibrating how much autonomy to allow.16 Trainees also indicate that teaching is more impactful during BSR than during walk rounding or card flipping, and clinical skill training during BSR is superior to a discussion in a conference room or a hallway context.2,3,15,17,18 One study has even suggested that the education of bedside rounds may help improve clinical skills in comparison with traditional models.18
The lack of BSR during medical school and residency training results in a deleterious cycle. Trainees become less proficient and less comfortable with BSR skills and therefore graduate as faculty members who are unskilled or uncomfortable insisting on BSR. As such, the cycle continues. As a result and as the traditional cornerstone of clinical training and inpatient care, BSR is recommended as standard practice by some professional organizations.19
WHAT WE SHOULD DO INSTEAD
Developing buy-in is an important first step for engaging in BSR. We recommend starting by demonstrating the value of BSR to overcome initial team or trainee hesitancy. Regardless of systems established to improve the efficiency of BSR, it is our experience that learners hesitantly engage if they do not understand the value of a given activity. We also urge attendings to demonstrate value by articulating how BSR fits in a patient-centered approach to emphasize the evidence-based positive impacts of BSR on patients.9 Beyond reviewing the benefits, faculty should set an expectation that the team will carry out BSR.9 Doing so sets an informal curriculum showing that BSR is important and sets the standard of care, which allows an inpatient team to adapt early in a rotation.
Next, faculty should ensure that BSR remains efficient.9 We believe that efficiency starts by setting expectations with patients. Patient expectations can be set by an attending or a supervising resident and should include a preview about how each encounter will progress, who will be in the room, how large the team will be, and what their role is during the encounter. Patients should be invited to be part of the discussion, offered an opportunity to opt out, and informed that questions arising from or clarifications needed following encounters can be addressed later within the day or after BSR. Nurses should be invited to actively participate during patient presentations. Each bedside encounter should be kept brief and standardized.20,21 To maximize efficiency, we also believe that roles should be delegated ahead of time and positioning in the room should be deliberate.22 Team members should know who is speaking when and in what order, who is accessing the electronic health record, and who will be examining the patient. Ideally, goals should be set ahead of time and tailored to each individual encounter. Finally, ensure everyone is on the same page by huddling briefly before each encounter to establish goals and roles and huddle afterward to debrief for learning and teamwork calibration.
In order to mitigate the learner’s anxiety about presenting in front of patients, build a partnership with the trainee, and time should be allotted to establish a safe learning environment.9 Sustain a supportive learning environment by providing positive feedback to learners in front of patients and teams. Faculty members should demonstrate how to bedside round effectively by leading initial encounters and generate momentum by selecting initial patient encounters that are most likely to succeed.23 Checklists can also be useful cognitive aids to facilitate an encounter and manage the cognitive load of learners.24 Ultimately, hesitancies can be overcome with experience.
Faculty members should ensure that bedside encounters are educationally valuable for an entire team.9 This initiative starts by preparing ahead of time, which allows the mental energy during encounters to be directly observed by learners in action.16 Preparation also allows the presentation to focus more on clinical reasoning rather than data gathering.20 Faculty members should also consider ways to foster resident autonomy and establish the role of a supervising resident as the team leader. Positioning in the room is critical22; we suggest that faculty members should position themselves near the head of the bed, out of a patient’s direct eyesight. In this way, they can observe how individual team members and the team as a whole interact with patients. The supervising resident should be at the foot of the bed, central to the team and the focal point of a patient’s view. The presenting intern or student should be seated near the head of the bed and opposite the supervising attending. Clinical teaching should also be kept short and pertinent to the patient, and questions should be phrased as “how” or “why” rather than “what” to reduce the risk of “wrong” answers in front of patients and the team.
WHEN IS CARD FLIPPING APPROPRIATE?
We believe that bedside rounds are most consistent with patient-centered inpatient care and should be considered the first-line approach. We also acknowledge that it is not always possible to bedside round on every patient on an inpatient census. For example, at an average of 13-15 minutes per patient,2,13 a census of 16 patients can take up to 4 hours to round. This timeline is not always feasible given the timing of training program didactics, interprofessional or case management rounds, and pressure for early discharges. Similar to all aspects of medicine, many approaches have been established to provide patient care, and context is important. Therefore, card flipping and walk rounding are beneficial to patients in some instances. For example, consider BSR for new, sick, or undifferentiated patients or when the history or exam findings need clarification; walk rounding or card flipping is suitable for patients with clear plans in place or when an encounter will be too disruptive to the rounding flow.21 Census size and individual patient or family concerns should dictate the style of rounding; in most situations, BSR may be equally efficient because it offers significant benefits to patients and families.
RECOMMENDATIONS
- Expectations should be set early with both trainees and patients. Patients should be informed that the team can come back later for more in-depth discussions.
- Trainees should be taught evidence-based approaches supporting the value of bedside rounds for patients.
- Faculty should consider leading initial encounters to demonstrate how to bedside round and to model behaviors.
- Positive feedback should be provided in front of patients and the team to build confidence.
- Encounters should be kept brief and efficient.
- A sufficient space for resident autonomy should be ensured through deliberate positioning, delegation of responsibilities, and huddling before and after encounters.
- Bedside rounds should be educationally worthwhile.
CONCLUSION
BSR is a traditional cornerstone of clinical training and inpatient care. Teaching at the bedside has many established benefits, such as connecting with patients and families, affording educators a valuable opportunity to assess learners and role model, and solidifying medical content by integrating teaching with clinical care. Concerns about bedside rounding may be based more on conjecture than on available evidence and can be overcome with deliberate education and proper planning. We propose several recommendations to successfully implement efficient, patient-centered, and educationally valuable bedside rounds.
For this (and most) patient(s), we recommend BSR. If this BSR is the first encounter, we suggest that the team should start with a more straightforward patient and come back to the new admission after the team has a chance to practice with other patients.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
1. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
2. Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829-832. https://doi.org/10.1542/peds.2006-2528.
3. Ngo TL, Blankenburg R, Yu CE. Teaching at the bedside: strategies for optimizing education on patient and family centered rounds. Pediatr Clin North Am. 2019;66(4):881-889. https://doi.org/10.1016/j.pcl.2019.03.012.
4. Berkwitt A, Grossman M. A Qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hosp Pediatr. 2015;5(7):357. https://doi.org/10.1542/hpeds.2014-0198.
5. Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016;8(4):523-531. https://doi.org/10.4300/JGME-D-15-00106.1.
6. Pingree EW, Freed JA, Riviello ED, et al. A tale of two rounds: managing conflict during the worst of times in family-centered rounds. Hosp Pediatr. 2019;9(7):563-565. https://doi.org/10.1542/hpeds.2019-0047.
7. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148.
8. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461.
9. Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326-334. https://doi.org/10.1097/ACM.0000000000000100.
10. Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945-949. https://doi.org/10.1097/00001888-200309000-00023.
11. Landry M-A, Lafrenaye S, Roy M-C, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275-280. https://doi.org/10.1542/peds.2007-0107.
12. Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150-1156. https://doi.org/10.1056/NEJM199704173361606.
13. Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792-798. https://doi.org/10.1007/s11606-010-1344-7.
14. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. https://doi.org/10.2147/JMDH.S72633.
15. Kelly MM, Xie A, Li Y, et al. System factors influencing the use of a family-centered rounds checklist. Pediatr Qual Saf. 2019;4(4):e196. https://doi.org/10.1097/pq9.0000000000000196.
16. Kogan JR, Hatala R, Hauer KE, Holmboe E. Guidelines: The do’s, don’ts and don’t knows of direct observation of clinical skills in medical education. Perspect Med Educ. 2017;6(5):286-305. https://doi.org/10.1007/s40037-017-0376-7.
17. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257-264. https://doi.org/10.1097/ACM.0b013e3181637f3e.
18. Heckmann JG, Bleh C, Dütsch M, Lang CJG, Neundörfer B. Does improved problem-based teaching influence students’ knowledge at the end of their neurology elective? An observational study of 40 students. J Neurol. 2003;250(12):1464-1468. https://doi.org/10.1007/s00415-003-0255-5.
19. Committee on hospital care and institute for patient and family centered care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404. https://doi.org/10.1542/peds.2011-3084.
20. Dhaliwal G, Hauer KE. The oral patient presentation in the era of night float admissions. JAMA. 2013;310(21):2247. https://doi.org/10.1001/jama.2013.282322.
21. Wiese JG. Teaching in the Hospital. Philadelphia, PA: ACP PRess; 2010. https://books.google.co.uk/books?hl=en&lr=&id=qquGWP4d2Q4C&oi=fnd&pg=PR13&dq=Wiese+J.+2010.+ACP+Teaching+Medicine+Series:+Teaching+in+the+Hospital.+Philadelphia,+PA:+ACP+Press&ots=JSRFojkBSn&sig=c33tapsL9DzV9nuFhENA6eObISA#v=onepage&q=bedside round&f=fals. Accessed November 29, 2019.
22. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit. Pediatr Qual Saf. 2019;4(3):e176. https://doi.org/10.1097/pq9.0000000000000176.
23. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med. 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189.
24. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. https://doi.org/10.1542/peds.2016-1688.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 32-year-old man with a history of polysubstance use disorder is hospitalized with endocarditis. The senior resident on the inpatient medical team suggests that the team “card flip” on this patient, citing a large number of patients on the team census, time constraints, and concerns that his substance use history will make bedside rounds uncomfortable.
BACKGROUND
“Rounds” is an inpatient care model in which teams of practitioners assess patients, determine care plans, and communicate with patients, families, and other healthcare professionals.1 One form of rounds is bedside rounding (BSR) through which an entire patient presentation occurs at the bedside, analogous to family-centered rounds common in pediatric inpatient care.2 This style of rounding is distinct from “walk rounding” that involves presentations occurring separately from a patient followed by a brief team bedside encounter. BSR is also different from “card flipping” or “table rounding” that involves presentations of a case separately without a team-patient encounter. The frequency of BSR at academic institutions has markedly decreased across the United States, and the time spent at the bedside is only a small fraction of rounding time.3
WHY YOU MIGHT THINK CARD FLIPPING IS HELPFUL
There are several reasons to employ strategies such as card-flipping or walk-rounding for discussing patient care away from the bedside. These BSR risks can be organized into patient harm, inefficiency, and risks to healthcare professional training.
First, BSR may result in patient harm. For example, discussing private health information in a semiprivate room may not only be uncomfortable for patients but may also violate patient privacy.4 Care teams are often large in number and rounding at the bedside can simultaneously trigger anxiety among patients, cause confusion about plans, or result in lack of clarity on the role of each provider.4 Furthermore, delivering bad news during BSR, or discussing sensitive topics such as substance use, psychiatric illness, or concerns of malingering behavior, may be difficult and uncomfortable.4,5 Additionally, some potential diagnoses, such as cancer or human immunodeficiency virus, even if unlikely, could induce panic among patients when they hear them being discussed.5 Trainees may also lose situational awareness because they focus on the agenda of bedside rounds and fail to respond to patients’ emotional needs.6
Efficiency is another reason to avoid BSR. The systemic factors of changing hospital demographics, such as short length of stay and increasing patient volumes, generate a substantial administrative burden on trainees.7 Modern trainees are also constrained by work hour restrictions, engagement with mandatory curricula, and other professional development opportunities. Furthermore, changes in a medical work environment cause trainees to rely heavily on electronic health records, which forces them to be at a computer instead of in a patient’s room.8 This confluence of factors results in substantial time pressure, and BSR is perceived as an inefficient use of time.9
The impact on education and trainee development is another concern of BSR. Rounding away from a patient ensures a safe environment for learners to interpret data and articulate clinical reasoning without the risk of embarrassment in front of a patient. This time outside a patient room also allows the team to have a shared mental model so that communication is aligned when a patient encounter does occur. Card flipping may result in improved trainee autonomy because the constant presence of attending supervision, particularly in front of patients, can risk undermining resident leadership and patient trust.9
WHY WE SHOULD RETURN TO THE BEDSIDE
The cited reasons for provider hesitancy to BSR, including possible patient harm and inefficiency, may be mostly related to individual perceptions and have recently been questioned.10,11
Several studies have suggested that bedside rounds may be better for patients’ experience over traditional walk-rounding or card-flipping models. In these studies, patients signal a preference for bedside rounds and suggest that discussing sensitive issues or concerning differential diagnoses during BSR may not be as concerning as physicians worry.11 For example, one randomized trial found that 87% of patients are untroubled by bedside discussions,12 and another trial revealed no difference between rounding models in emotional distress to patients or families.11 Patients and families also report higher levels of clarity from physicians, and they cited significantly improved levels of understanding their illness10 and test results.9 Furthermore, patients describe that physicians spend about twice as much time on their care when BSR is used.12 In many related studies, patients report a preference for BSR as a rounding strategy.2,11-13 For example, one study found that 99% of patients prefer BSR.13 Another study showed that 85% of families request to be part of bedside family-centered rounds over traditional walk rounding.2
Rounding away from a patient via card flipping or walk rounding seems more efficient, but this idea may be illusory. Although these strategies may seem faster, the lack of communication and coordination between team members and the patient may cause inefficiencies and delays in care throughout the day.14 For example, one study has demonstrated that family-centered bedside rounds are about 20% longer than walk rounding, but everyone involved, including housestaff, felt it was more efficient and saved time later in the day.2 Additionally, a study comparing BSR with walk rounding13 found no difference in time spent per patient, and another study has shown similar results in terms of family-centered rounds.15 Both studies have reported a similar amount of time spent per patient.
Physicians should return to BSR not only to improve patient experience but also to develop the clinical skills of trainees. The direct observation of trainees with patients allows high-level impactful clinical feedback and provides a basis for calibrating how much autonomy to allow.16 Trainees also indicate that teaching is more impactful during BSR than during walk rounding or card flipping, and clinical skill training during BSR is superior to a discussion in a conference room or a hallway context.2,3,15,17,18 One study has even suggested that the education of bedside rounds may help improve clinical skills in comparison with traditional models.18
The lack of BSR during medical school and residency training results in a deleterious cycle. Trainees become less proficient and less comfortable with BSR skills and therefore graduate as faculty members who are unskilled or uncomfortable insisting on BSR. As such, the cycle continues. As a result and as the traditional cornerstone of clinical training and inpatient care, BSR is recommended as standard practice by some professional organizations.19
WHAT WE SHOULD DO INSTEAD
Developing buy-in is an important first step for engaging in BSR. We recommend starting by demonstrating the value of BSR to overcome initial team or trainee hesitancy. Regardless of systems established to improve the efficiency of BSR, it is our experience that learners hesitantly engage if they do not understand the value of a given activity. We also urge attendings to demonstrate value by articulating how BSR fits in a patient-centered approach to emphasize the evidence-based positive impacts of BSR on patients.9 Beyond reviewing the benefits, faculty should set an expectation that the team will carry out BSR.9 Doing so sets an informal curriculum showing that BSR is important and sets the standard of care, which allows an inpatient team to adapt early in a rotation.
Next, faculty should ensure that BSR remains efficient.9 We believe that efficiency starts by setting expectations with patients. Patient expectations can be set by an attending or a supervising resident and should include a preview about how each encounter will progress, who will be in the room, how large the team will be, and what their role is during the encounter. Patients should be invited to be part of the discussion, offered an opportunity to opt out, and informed that questions arising from or clarifications needed following encounters can be addressed later within the day or after BSR. Nurses should be invited to actively participate during patient presentations. Each bedside encounter should be kept brief and standardized.20,21 To maximize efficiency, we also believe that roles should be delegated ahead of time and positioning in the room should be deliberate.22 Team members should know who is speaking when and in what order, who is accessing the electronic health record, and who will be examining the patient. Ideally, goals should be set ahead of time and tailored to each individual encounter. Finally, ensure everyone is on the same page by huddling briefly before each encounter to establish goals and roles and huddle afterward to debrief for learning and teamwork calibration.
In order to mitigate the learner’s anxiety about presenting in front of patients, build a partnership with the trainee, and time should be allotted to establish a safe learning environment.9 Sustain a supportive learning environment by providing positive feedback to learners in front of patients and teams. Faculty members should demonstrate how to bedside round effectively by leading initial encounters and generate momentum by selecting initial patient encounters that are most likely to succeed.23 Checklists can also be useful cognitive aids to facilitate an encounter and manage the cognitive load of learners.24 Ultimately, hesitancies can be overcome with experience.
Faculty members should ensure that bedside encounters are educationally valuable for an entire team.9 This initiative starts by preparing ahead of time, which allows the mental energy during encounters to be directly observed by learners in action.16 Preparation also allows the presentation to focus more on clinical reasoning rather than data gathering.20 Faculty members should also consider ways to foster resident autonomy and establish the role of a supervising resident as the team leader. Positioning in the room is critical22; we suggest that faculty members should position themselves near the head of the bed, out of a patient’s direct eyesight. In this way, they can observe how individual team members and the team as a whole interact with patients. The supervising resident should be at the foot of the bed, central to the team and the focal point of a patient’s view. The presenting intern or student should be seated near the head of the bed and opposite the supervising attending. Clinical teaching should also be kept short and pertinent to the patient, and questions should be phrased as “how” or “why” rather than “what” to reduce the risk of “wrong” answers in front of patients and the team.
WHEN IS CARD FLIPPING APPROPRIATE?
We believe that bedside rounds are most consistent with patient-centered inpatient care and should be considered the first-line approach. We also acknowledge that it is not always possible to bedside round on every patient on an inpatient census. For example, at an average of 13-15 minutes per patient,2,13 a census of 16 patients can take up to 4 hours to round. This timeline is not always feasible given the timing of training program didactics, interprofessional or case management rounds, and pressure for early discharges. Similar to all aspects of medicine, many approaches have been established to provide patient care, and context is important. Therefore, card flipping and walk rounding are beneficial to patients in some instances. For example, consider BSR for new, sick, or undifferentiated patients or when the history or exam findings need clarification; walk rounding or card flipping is suitable for patients with clear plans in place or when an encounter will be too disruptive to the rounding flow.21 Census size and individual patient or family concerns should dictate the style of rounding; in most situations, BSR may be equally efficient because it offers significant benefits to patients and families.
RECOMMENDATIONS
- Expectations should be set early with both trainees and patients. Patients should be informed that the team can come back later for more in-depth discussions.
- Trainees should be taught evidence-based approaches supporting the value of bedside rounds for patients.
- Faculty should consider leading initial encounters to demonstrate how to bedside round and to model behaviors.
- Positive feedback should be provided in front of patients and the team to build confidence.
- Encounters should be kept brief and efficient.
- A sufficient space for resident autonomy should be ensured through deliberate positioning, delegation of responsibilities, and huddling before and after encounters.
- Bedside rounds should be educationally worthwhile.
CONCLUSION
BSR is a traditional cornerstone of clinical training and inpatient care. Teaching at the bedside has many established benefits, such as connecting with patients and families, affording educators a valuable opportunity to assess learners and role model, and solidifying medical content by integrating teaching with clinical care. Concerns about bedside rounding may be based more on conjecture than on available evidence and can be overcome with deliberate education and proper planning. We propose several recommendations to successfully implement efficient, patient-centered, and educationally valuable bedside rounds.
For this (and most) patient(s), we recommend BSR. If this BSR is the first encounter, we suggest that the team should start with a more straightforward patient and come back to the new admission after the team has a chance to practice with other patients.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 32-year-old man with a history of polysubstance use disorder is hospitalized with endocarditis. The senior resident on the inpatient medical team suggests that the team “card flip” on this patient, citing a large number of patients on the team census, time constraints, and concerns that his substance use history will make bedside rounds uncomfortable.
BACKGROUND
“Rounds” is an inpatient care model in which teams of practitioners assess patients, determine care plans, and communicate with patients, families, and other healthcare professionals.1 One form of rounds is bedside rounding (BSR) through which an entire patient presentation occurs at the bedside, analogous to family-centered rounds common in pediatric inpatient care.2 This style of rounding is distinct from “walk rounding” that involves presentations occurring separately from a patient followed by a brief team bedside encounter. BSR is also different from “card flipping” or “table rounding” that involves presentations of a case separately without a team-patient encounter. The frequency of BSR at academic institutions has markedly decreased across the United States, and the time spent at the bedside is only a small fraction of rounding time.3
WHY YOU MIGHT THINK CARD FLIPPING IS HELPFUL
There are several reasons to employ strategies such as card-flipping or walk-rounding for discussing patient care away from the bedside. These BSR risks can be organized into patient harm, inefficiency, and risks to healthcare professional training.
First, BSR may result in patient harm. For example, discussing private health information in a semiprivate room may not only be uncomfortable for patients but may also violate patient privacy.4 Care teams are often large in number and rounding at the bedside can simultaneously trigger anxiety among patients, cause confusion about plans, or result in lack of clarity on the role of each provider.4 Furthermore, delivering bad news during BSR, or discussing sensitive topics such as substance use, psychiatric illness, or concerns of malingering behavior, may be difficult and uncomfortable.4,5 Additionally, some potential diagnoses, such as cancer or human immunodeficiency virus, even if unlikely, could induce panic among patients when they hear them being discussed.5 Trainees may also lose situational awareness because they focus on the agenda of bedside rounds and fail to respond to patients’ emotional needs.6
Efficiency is another reason to avoid BSR. The systemic factors of changing hospital demographics, such as short length of stay and increasing patient volumes, generate a substantial administrative burden on trainees.7 Modern trainees are also constrained by work hour restrictions, engagement with mandatory curricula, and other professional development opportunities. Furthermore, changes in a medical work environment cause trainees to rely heavily on electronic health records, which forces them to be at a computer instead of in a patient’s room.8 This confluence of factors results in substantial time pressure, and BSR is perceived as an inefficient use of time.9
The impact on education and trainee development is another concern of BSR. Rounding away from a patient ensures a safe environment for learners to interpret data and articulate clinical reasoning without the risk of embarrassment in front of a patient. This time outside a patient room also allows the team to have a shared mental model so that communication is aligned when a patient encounter does occur. Card flipping may result in improved trainee autonomy because the constant presence of attending supervision, particularly in front of patients, can risk undermining resident leadership and patient trust.9
WHY WE SHOULD RETURN TO THE BEDSIDE
The cited reasons for provider hesitancy to BSR, including possible patient harm and inefficiency, may be mostly related to individual perceptions and have recently been questioned.10,11
Several studies have suggested that bedside rounds may be better for patients’ experience over traditional walk-rounding or card-flipping models. In these studies, patients signal a preference for bedside rounds and suggest that discussing sensitive issues or concerning differential diagnoses during BSR may not be as concerning as physicians worry.11 For example, one randomized trial found that 87% of patients are untroubled by bedside discussions,12 and another trial revealed no difference between rounding models in emotional distress to patients or families.11 Patients and families also report higher levels of clarity from physicians, and they cited significantly improved levels of understanding their illness10 and test results.9 Furthermore, patients describe that physicians spend about twice as much time on their care when BSR is used.12 In many related studies, patients report a preference for BSR as a rounding strategy.2,11-13 For example, one study found that 99% of patients prefer BSR.13 Another study showed that 85% of families request to be part of bedside family-centered rounds over traditional walk rounding.2
Rounding away from a patient via card flipping or walk rounding seems more efficient, but this idea may be illusory. Although these strategies may seem faster, the lack of communication and coordination between team members and the patient may cause inefficiencies and delays in care throughout the day.14 For example, one study has demonstrated that family-centered bedside rounds are about 20% longer than walk rounding, but everyone involved, including housestaff, felt it was more efficient and saved time later in the day.2 Additionally, a study comparing BSR with walk rounding13 found no difference in time spent per patient, and another study has shown similar results in terms of family-centered rounds.15 Both studies have reported a similar amount of time spent per patient.
Physicians should return to BSR not only to improve patient experience but also to develop the clinical skills of trainees. The direct observation of trainees with patients allows high-level impactful clinical feedback and provides a basis for calibrating how much autonomy to allow.16 Trainees also indicate that teaching is more impactful during BSR than during walk rounding or card flipping, and clinical skill training during BSR is superior to a discussion in a conference room or a hallway context.2,3,15,17,18 One study has even suggested that the education of bedside rounds may help improve clinical skills in comparison with traditional models.18
The lack of BSR during medical school and residency training results in a deleterious cycle. Trainees become less proficient and less comfortable with BSR skills and therefore graduate as faculty members who are unskilled or uncomfortable insisting on BSR. As such, the cycle continues. As a result and as the traditional cornerstone of clinical training and inpatient care, BSR is recommended as standard practice by some professional organizations.19
WHAT WE SHOULD DO INSTEAD
Developing buy-in is an important first step for engaging in BSR. We recommend starting by demonstrating the value of BSR to overcome initial team or trainee hesitancy. Regardless of systems established to improve the efficiency of BSR, it is our experience that learners hesitantly engage if they do not understand the value of a given activity. We also urge attendings to demonstrate value by articulating how BSR fits in a patient-centered approach to emphasize the evidence-based positive impacts of BSR on patients.9 Beyond reviewing the benefits, faculty should set an expectation that the team will carry out BSR.9 Doing so sets an informal curriculum showing that BSR is important and sets the standard of care, which allows an inpatient team to adapt early in a rotation.
Next, faculty should ensure that BSR remains efficient.9 We believe that efficiency starts by setting expectations with patients. Patient expectations can be set by an attending or a supervising resident and should include a preview about how each encounter will progress, who will be in the room, how large the team will be, and what their role is during the encounter. Patients should be invited to be part of the discussion, offered an opportunity to opt out, and informed that questions arising from or clarifications needed following encounters can be addressed later within the day or after BSR. Nurses should be invited to actively participate during patient presentations. Each bedside encounter should be kept brief and standardized.20,21 To maximize efficiency, we also believe that roles should be delegated ahead of time and positioning in the room should be deliberate.22 Team members should know who is speaking when and in what order, who is accessing the electronic health record, and who will be examining the patient. Ideally, goals should be set ahead of time and tailored to each individual encounter. Finally, ensure everyone is on the same page by huddling briefly before each encounter to establish goals and roles and huddle afterward to debrief for learning and teamwork calibration.
In order to mitigate the learner’s anxiety about presenting in front of patients, build a partnership with the trainee, and time should be allotted to establish a safe learning environment.9 Sustain a supportive learning environment by providing positive feedback to learners in front of patients and teams. Faculty members should demonstrate how to bedside round effectively by leading initial encounters and generate momentum by selecting initial patient encounters that are most likely to succeed.23 Checklists can also be useful cognitive aids to facilitate an encounter and manage the cognitive load of learners.24 Ultimately, hesitancies can be overcome with experience.
Faculty members should ensure that bedside encounters are educationally valuable for an entire team.9 This initiative starts by preparing ahead of time, which allows the mental energy during encounters to be directly observed by learners in action.16 Preparation also allows the presentation to focus more on clinical reasoning rather than data gathering.20 Faculty members should also consider ways to foster resident autonomy and establish the role of a supervising resident as the team leader. Positioning in the room is critical22; we suggest that faculty members should position themselves near the head of the bed, out of a patient’s direct eyesight. In this way, they can observe how individual team members and the team as a whole interact with patients. The supervising resident should be at the foot of the bed, central to the team and the focal point of a patient’s view. The presenting intern or student should be seated near the head of the bed and opposite the supervising attending. Clinical teaching should also be kept short and pertinent to the patient, and questions should be phrased as “how” or “why” rather than “what” to reduce the risk of “wrong” answers in front of patients and the team.
WHEN IS CARD FLIPPING APPROPRIATE?
We believe that bedside rounds are most consistent with patient-centered inpatient care and should be considered the first-line approach. We also acknowledge that it is not always possible to bedside round on every patient on an inpatient census. For example, at an average of 13-15 minutes per patient,2,13 a census of 16 patients can take up to 4 hours to round. This timeline is not always feasible given the timing of training program didactics, interprofessional or case management rounds, and pressure for early discharges. Similar to all aspects of medicine, many approaches have been established to provide patient care, and context is important. Therefore, card flipping and walk rounding are beneficial to patients in some instances. For example, consider BSR for new, sick, or undifferentiated patients or when the history or exam findings need clarification; walk rounding or card flipping is suitable for patients with clear plans in place or when an encounter will be too disruptive to the rounding flow.21 Census size and individual patient or family concerns should dictate the style of rounding; in most situations, BSR may be equally efficient because it offers significant benefits to patients and families.
RECOMMENDATIONS
- Expectations should be set early with both trainees and patients. Patients should be informed that the team can come back later for more in-depth discussions.
- Trainees should be taught evidence-based approaches supporting the value of bedside rounds for patients.
- Faculty should consider leading initial encounters to demonstrate how to bedside round and to model behaviors.
- Positive feedback should be provided in front of patients and the team to build confidence.
- Encounters should be kept brief and efficient.
- A sufficient space for resident autonomy should be ensured through deliberate positioning, delegation of responsibilities, and huddling before and after encounters.
- Bedside rounds should be educationally worthwhile.
CONCLUSION
BSR is a traditional cornerstone of clinical training and inpatient care. Teaching at the bedside has many established benefits, such as connecting with patients and families, affording educators a valuable opportunity to assess learners and role model, and solidifying medical content by integrating teaching with clinical care. Concerns about bedside rounding may be based more on conjecture than on available evidence and can be overcome with deliberate education and proper planning. We propose several recommendations to successfully implement efficient, patient-centered, and educationally valuable bedside rounds.
For this (and most) patient(s), we recommend BSR. If this BSR is the first encounter, we suggest that the team should start with a more straightforward patient and come back to the new admission after the team has a chance to practice with other patients.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
1. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
2. Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829-832. https://doi.org/10.1542/peds.2006-2528.
3. Ngo TL, Blankenburg R, Yu CE. Teaching at the bedside: strategies for optimizing education on patient and family centered rounds. Pediatr Clin North Am. 2019;66(4):881-889. https://doi.org/10.1016/j.pcl.2019.03.012.
4. Berkwitt A, Grossman M. A Qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hosp Pediatr. 2015;5(7):357. https://doi.org/10.1542/hpeds.2014-0198.
5. Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016;8(4):523-531. https://doi.org/10.4300/JGME-D-15-00106.1.
6. Pingree EW, Freed JA, Riviello ED, et al. A tale of two rounds: managing conflict during the worst of times in family-centered rounds. Hosp Pediatr. 2019;9(7):563-565. https://doi.org/10.1542/hpeds.2019-0047.
7. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148.
8. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461.
9. Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326-334. https://doi.org/10.1097/ACM.0000000000000100.
10. Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945-949. https://doi.org/10.1097/00001888-200309000-00023.
11. Landry M-A, Lafrenaye S, Roy M-C, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275-280. https://doi.org/10.1542/peds.2007-0107.
12. Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150-1156. https://doi.org/10.1056/NEJM199704173361606.
13. Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792-798. https://doi.org/10.1007/s11606-010-1344-7.
14. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. https://doi.org/10.2147/JMDH.S72633.
15. Kelly MM, Xie A, Li Y, et al. System factors influencing the use of a family-centered rounds checklist. Pediatr Qual Saf. 2019;4(4):e196. https://doi.org/10.1097/pq9.0000000000000196.
16. Kogan JR, Hatala R, Hauer KE, Holmboe E. Guidelines: The do’s, don’ts and don’t knows of direct observation of clinical skills in medical education. Perspect Med Educ. 2017;6(5):286-305. https://doi.org/10.1007/s40037-017-0376-7.
17. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257-264. https://doi.org/10.1097/ACM.0b013e3181637f3e.
18. Heckmann JG, Bleh C, Dütsch M, Lang CJG, Neundörfer B. Does improved problem-based teaching influence students’ knowledge at the end of their neurology elective? An observational study of 40 students. J Neurol. 2003;250(12):1464-1468. https://doi.org/10.1007/s00415-003-0255-5.
19. Committee on hospital care and institute for patient and family centered care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404. https://doi.org/10.1542/peds.2011-3084.
20. Dhaliwal G, Hauer KE. The oral patient presentation in the era of night float admissions. JAMA. 2013;310(21):2247. https://doi.org/10.1001/jama.2013.282322.
21. Wiese JG. Teaching in the Hospital. Philadelphia, PA: ACP PRess; 2010. https://books.google.co.uk/books?hl=en&lr=&id=qquGWP4d2Q4C&oi=fnd&pg=PR13&dq=Wiese+J.+2010.+ACP+Teaching+Medicine+Series:+Teaching+in+the+Hospital.+Philadelphia,+PA:+ACP+Press&ots=JSRFojkBSn&sig=c33tapsL9DzV9nuFhENA6eObISA#v=onepage&q=bedside round&f=fals. Accessed November 29, 2019.
22. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit. Pediatr Qual Saf. 2019;4(3):e176. https://doi.org/10.1097/pq9.0000000000000176.
23. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med. 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189.
24. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. https://doi.org/10.1542/peds.2016-1688.
1. Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040-1047. https://doi.org/10.1007/s11606-014-2817-x.
2. Muething SE, Kotagal UR, Schoettker PJ, del Rey JG, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119(4):829-832. https://doi.org/10.1542/peds.2006-2528.
3. Ngo TL, Blankenburg R, Yu CE. Teaching at the bedside: strategies for optimizing education on patient and family centered rounds. Pediatr Clin North Am. 2019;66(4):881-889. https://doi.org/10.1016/j.pcl.2019.03.012.
4. Berkwitt A, Grossman M. A Qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hosp Pediatr. 2015;5(7):357. https://doi.org/10.1542/hpeds.2014-0198.
5. Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016;8(4):523-531. https://doi.org/10.4300/JGME-D-15-00106.1.
6. Pingree EW, Freed JA, Riviello ED, et al. A tale of two rounds: managing conflict during the worst of times in family-centered rounds. Hosp Pediatr. 2019;9(7):563-565. https://doi.org/10.1542/hpeds.2019-0047.
7. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148.
8. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461.
9. Gonzalo JD, Heist BS, Duffy BL, et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326-334. https://doi.org/10.1097/ACM.0000000000000100.
10. Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945-949. https://doi.org/10.1097/00001888-200309000-00023.
11. Landry M-A, Lafrenaye S, Roy M-C, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275-280. https://doi.org/10.1542/peds.2007-0107.
12. Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150-1156. https://doi.org/10.1056/NEJM199704173361606.
13. Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792-798. https://doi.org/10.1007/s11606-010-1344-7.
14. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. https://doi.org/10.2147/JMDH.S72633.
15. Kelly MM, Xie A, Li Y, et al. System factors influencing the use of a family-centered rounds checklist. Pediatr Qual Saf. 2019;4(4):e196. https://doi.org/10.1097/pq9.0000000000000196.
16. Kogan JR, Hatala R, Hauer KE, Holmboe E. Guidelines: The do’s, don’ts and don’t knows of direct observation of clinical skills in medical education. Perspect Med Educ. 2017;6(5):286-305. https://doi.org/10.1007/s40037-017-0376-7.
17. Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257-264. https://doi.org/10.1097/ACM.0b013e3181637f3e.
18. Heckmann JG, Bleh C, Dütsch M, Lang CJG, Neundörfer B. Does improved problem-based teaching influence students’ knowledge at the end of their neurology elective? An observational study of 40 students. J Neurol. 2003;250(12):1464-1468. https://doi.org/10.1007/s00415-003-0255-5.
19. Committee on hospital care and institute for patient and family centered care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404. https://doi.org/10.1542/peds.2011-3084.
20. Dhaliwal G, Hauer KE. The oral patient presentation in the era of night float admissions. JAMA. 2013;310(21):2247. https://doi.org/10.1001/jama.2013.282322.
21. Wiese JG. Teaching in the Hospital. Philadelphia, PA: ACP PRess; 2010. https://books.google.co.uk/books?hl=en&lr=&id=qquGWP4d2Q4C&oi=fnd&pg=PR13&dq=Wiese+J.+2010.+ACP+Teaching+Medicine+Series:+Teaching+in+the+Hospital.+Philadelphia,+PA:+ACP+Press&ots=JSRFojkBSn&sig=c33tapsL9DzV9nuFhENA6eObISA#v=onepage&q=bedside round&f=fals. Accessed November 29, 2019.
22. Lopez M, Vaks Y, Wilson M, et al. Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit. Pediatr Qual Saf. 2019;4(3):e176. https://doi.org/10.1097/pq9.0000000000000176.
23. Benbassat J. Role modeling in medical education: the importance of a reflective imitation. Acad Med. 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189.
24. Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. https://doi.org/10.1542/peds.2016-1688.
© 2020 Society of Hospital Medicine
Things We Do for No Reason™: Routinely Prescribing Transfusion Premedication To Prevent Acute Transfusion Reactions

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 68-year-old woman with a known history of myelodysplastic syndrome is admitted for fatigue and shortness of breath on exertion. Her hemoglobin concentration decreased from 9.1 g/dL to 6.5 g/dL. Her physical examination is unremarkable except for mild tachycardia with a heart rate of 105. She is scheduled to receive her first red blood cell (RBC) transfusion. The hospitalist orders premedication with acetaminophen and/or diphenhydramine to prevent an acute transfusion reaction.
BACKGROUND
The most frequent complications of blood transfusion are allergic transfusion reactions (ATRs) and febrile nonhemolytic transfusion reactions (FNHTRs), with a combined incidence of approximately 1%-4% per transfusion.1 ATRs may range in severity from mild urticaria to life-threatening anaphylaxis. FNHTRs manifest as a fever (oral temperature greater than or equal to 38°C/100.4°F and an increase of at least 1°C/1.8°F from pretransfusion values) or chills/rigors. With approximately 17 million blood transfusions, including RBCs, plasma, platelet, and cryoprecipitate components, administered annually in the United States, often to those with severe illnesses, ATRs and FNHTRs confer a substantial public health burden. Currently, the prevalence of premedication to prevent acute transfusion reactions in the United States and Canada is variable, ranging from 1.6% in one Canadian institution to as high as 80% in one large US hospital.2,3
WHY YOU MIGHT THINK PREMEDICATION IS HELPFUL TO PREVENT TRANSFUSION REACTIONS
FNHTRs are thought to be caused by cytokines elaborated by donor leukocytes that remain in blood products and/or by recipient antibodies reacting with donor leukocytes.1 While the clinical course is self-limited, these reactions can cause patients significant distress. The rationale behind acetaminophen premedication is to blunt the febrile response.
ATRs are usually mild, but anaphylaxis (which may include respiratory compromise, hypotension, and even death) can occur. They are caused by recipient histamine release in response to exposure to donor plasma proteins.1 This provides the theoretical rationale for antihistamine (eg, diphenhydramine) premedication as a prevention strategy.
Data on pretransfusion medication originate from the mid-20th century. In 1952, Ferris et al. published results showing a significant decrease in both febrile and ATRs when blood bottles were injected with an antihistamine.4 This was followed, in 1956, by Winter and Taplin’s further demonstration that both febrile and allergic reactions were significantly reduced when patients received units of blood injected with both oral acetylsalicylic acid and an antihistamine (chlorprophenpyridamine).5 These trials notably lacked appropriate controls and blinding, and numerous transfusion practice changes have taken place during the subsequent decades.
WHY PREMEDICATION TO PREVENT TRANSFUSION REACTION IS NOT HELPFUL
In the past 20 years, three double-blind randomized controlled trials published show that premedication with a combination of acetaminophen and an antihistamine (either diphenhydramine or chlorpheniramine) does not reduce the risk of ATR and FNHTR. The first study, published in 2002, randomized 51 patients with hematological malignancies receiving prestorage-irradiated, leukocyte-reduced, single-donor apheresis platelets to premedication with either acetaminophen and diphenhydramine or placebo.6 Patients with a history of either ATR or FNHTR were included, but patients with a history of hemolytic transfusion reaction were excluded.6 The study found that premedication did not significantly lower the incidence of these transfusion reactions (15.4%) as compared with placebo (15.2%; P = .94).6
In a larger study published in 2008, Kennedy et al. randomized 315 patients with hematological malignancies receiving RBC or platelet transfusion to either pretransfusion acetaminophen and diphenhydramine or placebo.7 Patients with a documented history of an ATR or FNHTR were excluded, which may have contributed to the lower incidence compared with the aforementioned earlier clinical trial. There was no significant difference in the overall rate of transfusion reactions between the two groups (1.44 per 100 transfusions vs 1.51 per 100 transfusions, P = .433). When the rates of ATRs and FNHTRs were analyzed separately, there was no significant difference between the treatment and control groups for either reaction type (P = .899 and P = .084, respectively). There was a trend toward a reduction in FNHTRs, but the authors calculated that we would need to premedicate approximately 344 transfusions to prevent one febrile reaction.7
A more recent study published in 2018 evaluated 147 Thai children and adolescents with thalassemia receiving leukoreduced blood products.8 Researchers randomized them to either premedication with acetaminophen and chlorpheniramine or placebo.8 The incidences of FNHTR were not statistically significantly different: 6.9% in the intervention group, compared with 9.5% in the placebo group (P = .565).8 These three studies constitute the best currently available evidence and suggest that pretransfusion antihistamines and/or antipyretics are not effective.
Beyond a lack of proven benefit, the use of premedication is not without risk. Diphenhydramine, the most commonly used antihistamine for premedication, can cause cognitive impairment, sedation, and delirium.9 Such adverse effects are potentially heightened in the elderly and seriously ill populations where transfusion commonly occurs. Acetaminophen, although generally safe, can result in hepatotoxicity in patients who are fasting, regularly consume alcohol, or have underlying liver disease. Since there is both a lack of clinical benefit and potential for harm, avoid premedication.
WHAT YOU SHOULD DO INSTEAD
Rather than pretreating the patient, consider modifying the blood product selected for transfusion. Administering platelet and/or RBC components with certain modifications (a product-centered approach) is effective at reducing mild transfusion reactions.10 A well-known product-centered modification method includes prestorage leukoreduction of RBC and platelet components to remove donor leukocytes to a level <5 × 106 per unit. This intervention reduces the incidence of FNHTRs by approximately 50%.11 A recent large, national survey demonstrated 90% of institutions (2,712/3,032) use universal leukoreduction.12 This widely employed and effective prevention strategy has likely helped reduce FNHTRs nationwide, so there are now fewer to prevent.12
Irradiation is another common modification of blood components used to prevent transfusion-associated graft-vs-host-disease (TA-GVHD) for recipients with significantly compromised cellular immunity. TA-GVHD is a rare but nearly universally fatal delayed complication of transfusion. Note that irradiation does not prevent FNHTRs or ATRs.
Under the premise that platelet-related allergic reactions are the result of recipient reaction to donor plasma proteins, reducing the plasma volume administered should decrease the coadministration of allergy-inducing plasma proteins.1 Reducing plasma volume can be achieved by two means: using a platelet additive solution that replaces two-thirds of the plasma content in a platelet unit or plasma removal by centrifugation. These two strategies decrease the plasma volume from 300 mL to ~100 mL per unit transfused, which effectively reduces the incidence of platelet-associated ATRs by 50%.10 For patients with recurrent severe ATRs, blood banks can wash RBC and platelet components, virtually removing all plasma proteins from the units.13 Epinephrine should be available at the bedside for patients with a history of severe ATRs.
Volume reduction and washing do negatively affect the quality of the unit: Platelets activate during the process, and transfusions result in a 20%-30% reduction in posttransfusion platelet counts.14 In addition, product manipulation takes significant blood bank processing time and results in an open system with greater risk of bacterial contamination, leading to a significantly shortened product expiration (24 hours for washed RBCs and 4 hours for washed or volume-reduced platelets).1 Reserve volume reduction and washing for patients with a history of multiple recurrent or severe ATRs, respectively. Platelet additive solution results in a reduction in posttransfusion count but does not require additional manipulation. Platelet additive solution products may not be available at many centers but could be used selectively (similar to volume reduction) depending on availability and cost.
Avoiding unnecessary transfusions is an essential strategy to prevent ATRs and FNHTRs. Evidence-based patient blood management (PBM), now considered the standard of care, is defined as optimizing anemia and hemostasis in patients with the goal of restricting blood transfusions. Evidence supporting restrictive transfusion strategies continues to accumulate, and numerous hospital systems have implemented PBM programs resulting in a significant nationwide reduction in transfusions since 2008. An effective PBM program reduces unnecessary transfusions and subsequent transfusion reactions.
Finally, appropriate close monitoring of patients undergoing blood transfusion and after completion of a transfusion is highly important. Paying close attention to signs and symptoms can alert the transfusing team to a developing adverse reaction and should prompt immediate cessation of an ongoing transfusion, the critical first step when a transfusion reaction is suspected. Hospitalists may need to take additional actions to treat the patient (eg, antihistamines after an ATR manifests or a diuretic in the setting of transfusion-associated circulatory overload). Report suspected transfusion reactions to the transfusion service. Failing to report a suspected transfusion reaction can lead to catastrophic consequences that can even be fatal.15
RECOMMENDATIONS
- Do not prescribe an antihistamine or acetaminophen prior to transfusion.
- Reduce the risk of FNHTRs in all transfusion recipients with universal prestorage leukoreduction.
- For individuals with multiple recurrent ATRs to platelets, employ platelet additive solution or platelet volume reduction.
- Reserve washing RBC and platelet components for patients with a history of severe ATRs. Make sure epinephrine is at the patient’s bedside.
- Curb unnecessary blood transfusions to reduce avoidable transfusion reactions.
- Monitor patients undergoing transfusion closely.
CONCLUSION
In our clinical scenario, there is no indication for premedication with acetaminophen and/or an antihistamine. Routine premedication is a low-value practice. Our RBC and platelet components are leukoreduced to prevent FNHTRs (and lower the risk of human leukocyte antigen alloimmunization and cytomegalovirus transmission). For individuals with multiple recurrent ATRs to platelets, we recommend platelet additive solution–stored or volume-reduced platelet components to lower the risk of future reactions. For patients with a history of severe ATRs, some blood banks may be able to provide washed components. Make sure epinephrine is at the patient’s bedside. Avoiding unnecessary transfusion is also essential to prevent adverse events related to blood transfusion—if a transfusion does not occur, then neither will a transfusion reaction. Finally, monitor patients undergoing transfusion closely.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing TWDFNR@hospitalmedicine.org.
Disclosures
The authors have nothing to disclose.
1. Fung MK, Eder A, Spitalnik SL, Westhoff CM. American Association of Blood Banks Technical Manual. 19th Ed: Bethesda, Md: AABB; 2017.
2. Ezidiegwu CN, Lauenstein KJ, Rosales LG, Kelly KC, Henry JB. Febrile nonhemolytic transfusion reactions: management by premedication and cost implications in adult patients. Arch Pathol Lab Med. 2004;128(9):991-995. doi: 10.1043/1543-2165(2004)128<991:FNTR>2.0.CO;2.
3. Fry JL, Arnold DM, Clase CM, et al. Transfusion premedication to prevent acute transfusion reactions: a retrospective observational study to assess current practices. Transfusion. 2010;50(8):1722-1730. doi: 10.1111/j.1537-2995.2010.02636.x.
4. Ferris HE, Alpert S, Coakley CS. Prevention of allergic transfusion reactions; the prophylactic use of antihistamine in blood to prevent allergic transfusion reactions. Am Pract Dig Treat. 1952;3(3):177-183.
5. Winter CC, Taplin GV. Prevention of acute allergic and febrile reactions to blood transfusions by prophylactic use of an antihistamine plus an antipyretic. Ann Allergy. 1956;14(1):76-81.
6. Wang SE, Lara PN, Jr., Lee-Ow A, et al. Acetaminophen and diphenhydramine as premedication for platelet transfusions: a prospective randomized double-blind placebo-controlled trial. Am J Hematol. 2002;70(3):191-194. doi: 10.1002/ajh.10119.
7. Kennedy LD, Case LD, Hurd DD, Cruz JM, Pomper GJ. A prospective, randomized, double-blind controlled trial of acetaminophen and diphenhydramine pretransfusion medication versus placebo for the prevention of transfusion reactions. Transfusion. 2008;48(11):2285-2291. doi: 10.1111/j.1537-2995.2008.01858.x.
8. Rujkijyanont P, Monsereenusorn C, Manoonphol P, Traivaree C. Efficacy of oral acetaminophen and intravenous chlorpheniramine maleate versus placebo to prevent red cell transfusion reactions in children and adolescent with thalassemia: a prospective, randomized, double-blind controlled trial. Anemia. 2018;2018:9492303. doi: 10.1155/2018/9492303.
9. By the American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227-2246. doi: 10.1111/jgs.13702.
10. Pagano MB, Katchatag BL, Khoobyari S, et al. Evaluating safety and cost-effectiveness of platelets stored in additive solution (PAS-F) as a hemolysis risk mitigation strategy. Transfusion. 2019;59(4):1246-1251. doi: 10.1111/trf.15138.
11. King KE, Shirey RS, Thoman SK, Bensen-Kennedy D, Tanz WS, Ness PM. Universal leukoreduction decreases the incidence of febrile nonhemolytic transfusion reactions to RBCs. Transfusion. 2004;44(1):25-29. doi: 10.1046/j.0041-1132.2004.00609.x.
12. Weisberg SP, Staley EM, Williams LA 3rd, et al. Survey on transfusion-transmitted cytomegalovirus and cytomegalovirus disease mitigation. Arch Pathol Lab Med. 2017;141(12):1705-1711. doi: 10.5858/arpa.2016-0461-OA.
13. Tobian AA, Savage WJ, Tisch DJ, Thoman S, King KE, Ness PM. Prevention of allergic transfusion reactions to platelets and red blood cells through plasma reduction. Transfusion. 2011;51(8):1676-1683. doi: 10.1111/j.1537-2995.2010.03008.x.
14. Veeraputhiran M, Ware J, Dent J, et al. A comparison of washed and volume-reduced platelets with respect to platelet activation, aggregation, and plasma protein removal. Transfusion. 2011;51(5):1030-1036. doi: 10.1111/j.1537-2995.2010.02897.x.
15. Corean J, Al-Tigar R, Pysher T, Blaylock R, Metcalf RA. Quality improvement after multiple fatal transfusion-transmitted bacterial infections. Am J Clin Pathol. 2018;149(4):293-299. doi: 10.1111/j.1537-2995.2010.02897.x.

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 68-year-old woman with a known history of myelodysplastic syndrome is admitted for fatigue and shortness of breath on exertion. Her hemoglobin concentration decreased from 9.1 g/dL to 6.5 g/dL. Her physical examination is unremarkable except for mild tachycardia with a heart rate of 105. She is scheduled to receive her first red blood cell (RBC) transfusion. The hospitalist orders premedication with acetaminophen and/or diphenhydramine to prevent an acute transfusion reaction.
BACKGROUND
The most frequent complications of blood transfusion are allergic transfusion reactions (ATRs) and febrile nonhemolytic transfusion reactions (FNHTRs), with a combined incidence of approximately 1%-4% per transfusion.1 ATRs may range in severity from mild urticaria to life-threatening anaphylaxis. FNHTRs manifest as a fever (oral temperature greater than or equal to 38°C/100.4°F and an increase of at least 1°C/1.8°F from pretransfusion values) or chills/rigors. With approximately 17 million blood transfusions, including RBCs, plasma, platelet, and cryoprecipitate components, administered annually in the United States, often to those with severe illnesses, ATRs and FNHTRs confer a substantial public health burden. Currently, the prevalence of premedication to prevent acute transfusion reactions in the United States and Canada is variable, ranging from 1.6% in one Canadian institution to as high as 80% in one large US hospital.2,3
WHY YOU MIGHT THINK PREMEDICATION IS HELPFUL TO PREVENT TRANSFUSION REACTIONS
FNHTRs are thought to be caused by cytokines elaborated by donor leukocytes that remain in blood products and/or by recipient antibodies reacting with donor leukocytes.1 While the clinical course is self-limited, these reactions can cause patients significant distress. The rationale behind acetaminophen premedication is to blunt the febrile response.
ATRs are usually mild, but anaphylaxis (which may include respiratory compromise, hypotension, and even death) can occur. They are caused by recipient histamine release in response to exposure to donor plasma proteins.1 This provides the theoretical rationale for antihistamine (eg, diphenhydramine) premedication as a prevention strategy.
Data on pretransfusion medication originate from the mid-20th century. In 1952, Ferris et al. published results showing a significant decrease in both febrile and ATRs when blood bottles were injected with an antihistamine.4 This was followed, in 1956, by Winter and Taplin’s further demonstration that both febrile and allergic reactions were significantly reduced when patients received units of blood injected with both oral acetylsalicylic acid and an antihistamine (chlorprophenpyridamine).5 These trials notably lacked appropriate controls and blinding, and numerous transfusion practice changes have taken place during the subsequent decades.
WHY PREMEDICATION TO PREVENT TRANSFUSION REACTION IS NOT HELPFUL
In the past 20 years, three double-blind randomized controlled trials published show that premedication with a combination of acetaminophen and an antihistamine (either diphenhydramine or chlorpheniramine) does not reduce the risk of ATR and FNHTR. The first study, published in 2002, randomized 51 patients with hematological malignancies receiving prestorage-irradiated, leukocyte-reduced, single-donor apheresis platelets to premedication with either acetaminophen and diphenhydramine or placebo.6 Patients with a history of either ATR or FNHTR were included, but patients with a history of hemolytic transfusion reaction were excluded.6 The study found that premedication did not significantly lower the incidence of these transfusion reactions (15.4%) as compared with placebo (15.2%; P = .94).6
In a larger study published in 2008, Kennedy et al. randomized 315 patients with hematological malignancies receiving RBC or platelet transfusion to either pretransfusion acetaminophen and diphenhydramine or placebo.7 Patients with a documented history of an ATR or FNHTR were excluded, which may have contributed to the lower incidence compared with the aforementioned earlier clinical trial. There was no significant difference in the overall rate of transfusion reactions between the two groups (1.44 per 100 transfusions vs 1.51 per 100 transfusions, P = .433). When the rates of ATRs and FNHTRs were analyzed separately, there was no significant difference between the treatment and control groups for either reaction type (P = .899 and P = .084, respectively). There was a trend toward a reduction in FNHTRs, but the authors calculated that we would need to premedicate approximately 344 transfusions to prevent one febrile reaction.7
A more recent study published in 2018 evaluated 147 Thai children and adolescents with thalassemia receiving leukoreduced blood products.8 Researchers randomized them to either premedication with acetaminophen and chlorpheniramine or placebo.8 The incidences of FNHTR were not statistically significantly different: 6.9% in the intervention group, compared with 9.5% in the placebo group (P = .565).8 These three studies constitute the best currently available evidence and suggest that pretransfusion antihistamines and/or antipyretics are not effective.
Beyond a lack of proven benefit, the use of premedication is not without risk. Diphenhydramine, the most commonly used antihistamine for premedication, can cause cognitive impairment, sedation, and delirium.9 Such adverse effects are potentially heightened in the elderly and seriously ill populations where transfusion commonly occurs. Acetaminophen, although generally safe, can result in hepatotoxicity in patients who are fasting, regularly consume alcohol, or have underlying liver disease. Since there is both a lack of clinical benefit and potential for harm, avoid premedication.
WHAT YOU SHOULD DO INSTEAD
Rather than pretreating the patient, consider modifying the blood product selected for transfusion. Administering platelet and/or RBC components with certain modifications (a product-centered approach) is effective at reducing mild transfusion reactions.10 A well-known product-centered modification method includes prestorage leukoreduction of RBC and platelet components to remove donor leukocytes to a level <5 × 106 per unit. This intervention reduces the incidence of FNHTRs by approximately 50%.11 A recent large, national survey demonstrated 90% of institutions (2,712/3,032) use universal leukoreduction.12 This widely employed and effective prevention strategy has likely helped reduce FNHTRs nationwide, so there are now fewer to prevent.12
Irradiation is another common modification of blood components used to prevent transfusion-associated graft-vs-host-disease (TA-GVHD) for recipients with significantly compromised cellular immunity. TA-GVHD is a rare but nearly universally fatal delayed complication of transfusion. Note that irradiation does not prevent FNHTRs or ATRs.
Under the premise that platelet-related allergic reactions are the result of recipient reaction to donor plasma proteins, reducing the plasma volume administered should decrease the coadministration of allergy-inducing plasma proteins.1 Reducing plasma volume can be achieved by two means: using a platelet additive solution that replaces two-thirds of the plasma content in a platelet unit or plasma removal by centrifugation. These two strategies decrease the plasma volume from 300 mL to ~100 mL per unit transfused, which effectively reduces the incidence of platelet-associated ATRs by 50%.10 For patients with recurrent severe ATRs, blood banks can wash RBC and platelet components, virtually removing all plasma proteins from the units.13 Epinephrine should be available at the bedside for patients with a history of severe ATRs.
Volume reduction and washing do negatively affect the quality of the unit: Platelets activate during the process, and transfusions result in a 20%-30% reduction in posttransfusion platelet counts.14 In addition, product manipulation takes significant blood bank processing time and results in an open system with greater risk of bacterial contamination, leading to a significantly shortened product expiration (24 hours for washed RBCs and 4 hours for washed or volume-reduced platelets).1 Reserve volume reduction and washing for patients with a history of multiple recurrent or severe ATRs, respectively. Platelet additive solution results in a reduction in posttransfusion count but does not require additional manipulation. Platelet additive solution products may not be available at many centers but could be used selectively (similar to volume reduction) depending on availability and cost.
Avoiding unnecessary transfusions is an essential strategy to prevent ATRs and FNHTRs. Evidence-based patient blood management (PBM), now considered the standard of care, is defined as optimizing anemia and hemostasis in patients with the goal of restricting blood transfusions. Evidence supporting restrictive transfusion strategies continues to accumulate, and numerous hospital systems have implemented PBM programs resulting in a significant nationwide reduction in transfusions since 2008. An effective PBM program reduces unnecessary transfusions and subsequent transfusion reactions.
Finally, appropriate close monitoring of patients undergoing blood transfusion and after completion of a transfusion is highly important. Paying close attention to signs and symptoms can alert the transfusing team to a developing adverse reaction and should prompt immediate cessation of an ongoing transfusion, the critical first step when a transfusion reaction is suspected. Hospitalists may need to take additional actions to treat the patient (eg, antihistamines after an ATR manifests or a diuretic in the setting of transfusion-associated circulatory overload). Report suspected transfusion reactions to the transfusion service. Failing to report a suspected transfusion reaction can lead to catastrophic consequences that can even be fatal.15
RECOMMENDATIONS
- Do not prescribe an antihistamine or acetaminophen prior to transfusion.
- Reduce the risk of FNHTRs in all transfusion recipients with universal prestorage leukoreduction.
- For individuals with multiple recurrent ATRs to platelets, employ platelet additive solution or platelet volume reduction.
- Reserve washing RBC and platelet components for patients with a history of severe ATRs. Make sure epinephrine is at the patient’s bedside.
- Curb unnecessary blood transfusions to reduce avoidable transfusion reactions.
- Monitor patients undergoing transfusion closely.
CONCLUSION
In our clinical scenario, there is no indication for premedication with acetaminophen and/or an antihistamine. Routine premedication is a low-value practice. Our RBC and platelet components are leukoreduced to prevent FNHTRs (and lower the risk of human leukocyte antigen alloimmunization and cytomegalovirus transmission). For individuals with multiple recurrent ATRs to platelets, we recommend platelet additive solution–stored or volume-reduced platelet components to lower the risk of future reactions. For patients with a history of severe ATRs, some blood banks may be able to provide washed components. Make sure epinephrine is at the patient’s bedside. Avoiding unnecessary transfusion is also essential to prevent adverse events related to blood transfusion—if a transfusion does not occur, then neither will a transfusion reaction. Finally, monitor patients undergoing transfusion closely.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing TWDFNR@hospitalmedicine.org.
Disclosures
The authors have nothing to disclose.

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 68-year-old woman with a known history of myelodysplastic syndrome is admitted for fatigue and shortness of breath on exertion. Her hemoglobin concentration decreased from 9.1 g/dL to 6.5 g/dL. Her physical examination is unremarkable except for mild tachycardia with a heart rate of 105. She is scheduled to receive her first red blood cell (RBC) transfusion. The hospitalist orders premedication with acetaminophen and/or diphenhydramine to prevent an acute transfusion reaction.
BACKGROUND
The most frequent complications of blood transfusion are allergic transfusion reactions (ATRs) and febrile nonhemolytic transfusion reactions (FNHTRs), with a combined incidence of approximately 1%-4% per transfusion.1 ATRs may range in severity from mild urticaria to life-threatening anaphylaxis. FNHTRs manifest as a fever (oral temperature greater than or equal to 38°C/100.4°F and an increase of at least 1°C/1.8°F from pretransfusion values) or chills/rigors. With approximately 17 million blood transfusions, including RBCs, plasma, platelet, and cryoprecipitate components, administered annually in the United States, often to those with severe illnesses, ATRs and FNHTRs confer a substantial public health burden. Currently, the prevalence of premedication to prevent acute transfusion reactions in the United States and Canada is variable, ranging from 1.6% in one Canadian institution to as high as 80% in one large US hospital.2,3
WHY YOU MIGHT THINK PREMEDICATION IS HELPFUL TO PREVENT TRANSFUSION REACTIONS
FNHTRs are thought to be caused by cytokines elaborated by donor leukocytes that remain in blood products and/or by recipient antibodies reacting with donor leukocytes.1 While the clinical course is self-limited, these reactions can cause patients significant distress. The rationale behind acetaminophen premedication is to blunt the febrile response.
ATRs are usually mild, but anaphylaxis (which may include respiratory compromise, hypotension, and even death) can occur. They are caused by recipient histamine release in response to exposure to donor plasma proteins.1 This provides the theoretical rationale for antihistamine (eg, diphenhydramine) premedication as a prevention strategy.
Data on pretransfusion medication originate from the mid-20th century. In 1952, Ferris et al. published results showing a significant decrease in both febrile and ATRs when blood bottles were injected with an antihistamine.4 This was followed, in 1956, by Winter and Taplin’s further demonstration that both febrile and allergic reactions were significantly reduced when patients received units of blood injected with both oral acetylsalicylic acid and an antihistamine (chlorprophenpyridamine).5 These trials notably lacked appropriate controls and blinding, and numerous transfusion practice changes have taken place during the subsequent decades.
WHY PREMEDICATION TO PREVENT TRANSFUSION REACTION IS NOT HELPFUL
In the past 20 years, three double-blind randomized controlled trials published show that premedication with a combination of acetaminophen and an antihistamine (either diphenhydramine or chlorpheniramine) does not reduce the risk of ATR and FNHTR. The first study, published in 2002, randomized 51 patients with hematological malignancies receiving prestorage-irradiated, leukocyte-reduced, single-donor apheresis platelets to premedication with either acetaminophen and diphenhydramine or placebo.6 Patients with a history of either ATR or FNHTR were included, but patients with a history of hemolytic transfusion reaction were excluded.6 The study found that premedication did not significantly lower the incidence of these transfusion reactions (15.4%) as compared with placebo (15.2%; P = .94).6
In a larger study published in 2008, Kennedy et al. randomized 315 patients with hematological malignancies receiving RBC or platelet transfusion to either pretransfusion acetaminophen and diphenhydramine or placebo.7 Patients with a documented history of an ATR or FNHTR were excluded, which may have contributed to the lower incidence compared with the aforementioned earlier clinical trial. There was no significant difference in the overall rate of transfusion reactions between the two groups (1.44 per 100 transfusions vs 1.51 per 100 transfusions, P = .433). When the rates of ATRs and FNHTRs were analyzed separately, there was no significant difference between the treatment and control groups for either reaction type (P = .899 and P = .084, respectively). There was a trend toward a reduction in FNHTRs, but the authors calculated that we would need to premedicate approximately 344 transfusions to prevent one febrile reaction.7
A more recent study published in 2018 evaluated 147 Thai children and adolescents with thalassemia receiving leukoreduced blood products.8 Researchers randomized them to either premedication with acetaminophen and chlorpheniramine or placebo.8 The incidences of FNHTR were not statistically significantly different: 6.9% in the intervention group, compared with 9.5% in the placebo group (P = .565).8 These three studies constitute the best currently available evidence and suggest that pretransfusion antihistamines and/or antipyretics are not effective.
Beyond a lack of proven benefit, the use of premedication is not without risk. Diphenhydramine, the most commonly used antihistamine for premedication, can cause cognitive impairment, sedation, and delirium.9 Such adverse effects are potentially heightened in the elderly and seriously ill populations where transfusion commonly occurs. Acetaminophen, although generally safe, can result in hepatotoxicity in patients who are fasting, regularly consume alcohol, or have underlying liver disease. Since there is both a lack of clinical benefit and potential for harm, avoid premedication.
WHAT YOU SHOULD DO INSTEAD
Rather than pretreating the patient, consider modifying the blood product selected for transfusion. Administering platelet and/or RBC components with certain modifications (a product-centered approach) is effective at reducing mild transfusion reactions.10 A well-known product-centered modification method includes prestorage leukoreduction of RBC and platelet components to remove donor leukocytes to a level <5 × 106 per unit. This intervention reduces the incidence of FNHTRs by approximately 50%.11 A recent large, national survey demonstrated 90% of institutions (2,712/3,032) use universal leukoreduction.12 This widely employed and effective prevention strategy has likely helped reduce FNHTRs nationwide, so there are now fewer to prevent.12
Irradiation is another common modification of blood components used to prevent transfusion-associated graft-vs-host-disease (TA-GVHD) for recipients with significantly compromised cellular immunity. TA-GVHD is a rare but nearly universally fatal delayed complication of transfusion. Note that irradiation does not prevent FNHTRs or ATRs.
Under the premise that platelet-related allergic reactions are the result of recipient reaction to donor plasma proteins, reducing the plasma volume administered should decrease the coadministration of allergy-inducing plasma proteins.1 Reducing plasma volume can be achieved by two means: using a platelet additive solution that replaces two-thirds of the plasma content in a platelet unit or plasma removal by centrifugation. These two strategies decrease the plasma volume from 300 mL to ~100 mL per unit transfused, which effectively reduces the incidence of platelet-associated ATRs by 50%.10 For patients with recurrent severe ATRs, blood banks can wash RBC and platelet components, virtually removing all plasma proteins from the units.13 Epinephrine should be available at the bedside for patients with a history of severe ATRs.
Volume reduction and washing do negatively affect the quality of the unit: Platelets activate during the process, and transfusions result in a 20%-30% reduction in posttransfusion platelet counts.14 In addition, product manipulation takes significant blood bank processing time and results in an open system with greater risk of bacterial contamination, leading to a significantly shortened product expiration (24 hours for washed RBCs and 4 hours for washed or volume-reduced platelets).1 Reserve volume reduction and washing for patients with a history of multiple recurrent or severe ATRs, respectively. Platelet additive solution results in a reduction in posttransfusion count but does not require additional manipulation. Platelet additive solution products may not be available at many centers but could be used selectively (similar to volume reduction) depending on availability and cost.
Avoiding unnecessary transfusions is an essential strategy to prevent ATRs and FNHTRs. Evidence-based patient blood management (PBM), now considered the standard of care, is defined as optimizing anemia and hemostasis in patients with the goal of restricting blood transfusions. Evidence supporting restrictive transfusion strategies continues to accumulate, and numerous hospital systems have implemented PBM programs resulting in a significant nationwide reduction in transfusions since 2008. An effective PBM program reduces unnecessary transfusions and subsequent transfusion reactions.
Finally, appropriate close monitoring of patients undergoing blood transfusion and after completion of a transfusion is highly important. Paying close attention to signs and symptoms can alert the transfusing team to a developing adverse reaction and should prompt immediate cessation of an ongoing transfusion, the critical first step when a transfusion reaction is suspected. Hospitalists may need to take additional actions to treat the patient (eg, antihistamines after an ATR manifests or a diuretic in the setting of transfusion-associated circulatory overload). Report suspected transfusion reactions to the transfusion service. Failing to report a suspected transfusion reaction can lead to catastrophic consequences that can even be fatal.15
RECOMMENDATIONS
- Do not prescribe an antihistamine or acetaminophen prior to transfusion.
- Reduce the risk of FNHTRs in all transfusion recipients with universal prestorage leukoreduction.
- For individuals with multiple recurrent ATRs to platelets, employ platelet additive solution or platelet volume reduction.
- Reserve washing RBC and platelet components for patients with a history of severe ATRs. Make sure epinephrine is at the patient’s bedside.
- Curb unnecessary blood transfusions to reduce avoidable transfusion reactions.
- Monitor patients undergoing transfusion closely.
CONCLUSION
In our clinical scenario, there is no indication for premedication with acetaminophen and/or an antihistamine. Routine premedication is a low-value practice. Our RBC and platelet components are leukoreduced to prevent FNHTRs (and lower the risk of human leukocyte antigen alloimmunization and cytomegalovirus transmission). For individuals with multiple recurrent ATRs to platelets, we recommend platelet additive solution–stored or volume-reduced platelet components to lower the risk of future reactions. For patients with a history of severe ATRs, some blood banks may be able to provide washed components. Make sure epinephrine is at the patient’s bedside. Avoiding unnecessary transfusion is also essential to prevent adverse events related to blood transfusion—if a transfusion does not occur, then neither will a transfusion reaction. Finally, monitor patients undergoing transfusion closely.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing TWDFNR@hospitalmedicine.org.
Disclosures
The authors have nothing to disclose.
1. Fung MK, Eder A, Spitalnik SL, Westhoff CM. American Association of Blood Banks Technical Manual. 19th Ed: Bethesda, Md: AABB; 2017.
2. Ezidiegwu CN, Lauenstein KJ, Rosales LG, Kelly KC, Henry JB. Febrile nonhemolytic transfusion reactions: management by premedication and cost implications in adult patients. Arch Pathol Lab Med. 2004;128(9):991-995. doi: 10.1043/1543-2165(2004)128<991:FNTR>2.0.CO;2.
3. Fry JL, Arnold DM, Clase CM, et al. Transfusion premedication to prevent acute transfusion reactions: a retrospective observational study to assess current practices. Transfusion. 2010;50(8):1722-1730. doi: 10.1111/j.1537-2995.2010.02636.x.
4. Ferris HE, Alpert S, Coakley CS. Prevention of allergic transfusion reactions; the prophylactic use of antihistamine in blood to prevent allergic transfusion reactions. Am Pract Dig Treat. 1952;3(3):177-183.
5. Winter CC, Taplin GV. Prevention of acute allergic and febrile reactions to blood transfusions by prophylactic use of an antihistamine plus an antipyretic. Ann Allergy. 1956;14(1):76-81.
6. Wang SE, Lara PN, Jr., Lee-Ow A, et al. Acetaminophen and diphenhydramine as premedication for platelet transfusions: a prospective randomized double-blind placebo-controlled trial. Am J Hematol. 2002;70(3):191-194. doi: 10.1002/ajh.10119.
7. Kennedy LD, Case LD, Hurd DD, Cruz JM, Pomper GJ. A prospective, randomized, double-blind controlled trial of acetaminophen and diphenhydramine pretransfusion medication versus placebo for the prevention of transfusion reactions. Transfusion. 2008;48(11):2285-2291. doi: 10.1111/j.1537-2995.2008.01858.x.
8. Rujkijyanont P, Monsereenusorn C, Manoonphol P, Traivaree C. Efficacy of oral acetaminophen and intravenous chlorpheniramine maleate versus placebo to prevent red cell transfusion reactions in children and adolescent with thalassemia: a prospective, randomized, double-blind controlled trial. Anemia. 2018;2018:9492303. doi: 10.1155/2018/9492303.
9. By the American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227-2246. doi: 10.1111/jgs.13702.
10. Pagano MB, Katchatag BL, Khoobyari S, et al. Evaluating safety and cost-effectiveness of platelets stored in additive solution (PAS-F) as a hemolysis risk mitigation strategy. Transfusion. 2019;59(4):1246-1251. doi: 10.1111/trf.15138.
11. King KE, Shirey RS, Thoman SK, Bensen-Kennedy D, Tanz WS, Ness PM. Universal leukoreduction decreases the incidence of febrile nonhemolytic transfusion reactions to RBCs. Transfusion. 2004;44(1):25-29. doi: 10.1046/j.0041-1132.2004.00609.x.
12. Weisberg SP, Staley EM, Williams LA 3rd, et al. Survey on transfusion-transmitted cytomegalovirus and cytomegalovirus disease mitigation. Arch Pathol Lab Med. 2017;141(12):1705-1711. doi: 10.5858/arpa.2016-0461-OA.
13. Tobian AA, Savage WJ, Tisch DJ, Thoman S, King KE, Ness PM. Prevention of allergic transfusion reactions to platelets and red blood cells through plasma reduction. Transfusion. 2011;51(8):1676-1683. doi: 10.1111/j.1537-2995.2010.03008.x.
14. Veeraputhiran M, Ware J, Dent J, et al. A comparison of washed and volume-reduced platelets with respect to platelet activation, aggregation, and plasma protein removal. Transfusion. 2011;51(5):1030-1036. doi: 10.1111/j.1537-2995.2010.02897.x.
15. Corean J, Al-Tigar R, Pysher T, Blaylock R, Metcalf RA. Quality improvement after multiple fatal transfusion-transmitted bacterial infections. Am J Clin Pathol. 2018;149(4):293-299. doi: 10.1111/j.1537-2995.2010.02897.x.
1. Fung MK, Eder A, Spitalnik SL, Westhoff CM. American Association of Blood Banks Technical Manual. 19th Ed: Bethesda, Md: AABB; 2017.
2. Ezidiegwu CN, Lauenstein KJ, Rosales LG, Kelly KC, Henry JB. Febrile nonhemolytic transfusion reactions: management by premedication and cost implications in adult patients. Arch Pathol Lab Med. 2004;128(9):991-995. doi: 10.1043/1543-2165(2004)128<991:FNTR>2.0.CO;2.
3. Fry JL, Arnold DM, Clase CM, et al. Transfusion premedication to prevent acute transfusion reactions: a retrospective observational study to assess current practices. Transfusion. 2010;50(8):1722-1730. doi: 10.1111/j.1537-2995.2010.02636.x.
4. Ferris HE, Alpert S, Coakley CS. Prevention of allergic transfusion reactions; the prophylactic use of antihistamine in blood to prevent allergic transfusion reactions. Am Pract Dig Treat. 1952;3(3):177-183.
5. Winter CC, Taplin GV. Prevention of acute allergic and febrile reactions to blood transfusions by prophylactic use of an antihistamine plus an antipyretic. Ann Allergy. 1956;14(1):76-81.
6. Wang SE, Lara PN, Jr., Lee-Ow A, et al. Acetaminophen and diphenhydramine as premedication for platelet transfusions: a prospective randomized double-blind placebo-controlled trial. Am J Hematol. 2002;70(3):191-194. doi: 10.1002/ajh.10119.
7. Kennedy LD, Case LD, Hurd DD, Cruz JM, Pomper GJ. A prospective, randomized, double-blind controlled trial of acetaminophen and diphenhydramine pretransfusion medication versus placebo for the prevention of transfusion reactions. Transfusion. 2008;48(11):2285-2291. doi: 10.1111/j.1537-2995.2008.01858.x.
8. Rujkijyanont P, Monsereenusorn C, Manoonphol P, Traivaree C. Efficacy of oral acetaminophen and intravenous chlorpheniramine maleate versus placebo to prevent red cell transfusion reactions in children and adolescent with thalassemia: a prospective, randomized, double-blind controlled trial. Anemia. 2018;2018:9492303. doi: 10.1155/2018/9492303.
9. By the American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227-2246. doi: 10.1111/jgs.13702.
10. Pagano MB, Katchatag BL, Khoobyari S, et al. Evaluating safety and cost-effectiveness of platelets stored in additive solution (PAS-F) as a hemolysis risk mitigation strategy. Transfusion. 2019;59(4):1246-1251. doi: 10.1111/trf.15138.
11. King KE, Shirey RS, Thoman SK, Bensen-Kennedy D, Tanz WS, Ness PM. Universal leukoreduction decreases the incidence of febrile nonhemolytic transfusion reactions to RBCs. Transfusion. 2004;44(1):25-29. doi: 10.1046/j.0041-1132.2004.00609.x.
12. Weisberg SP, Staley EM, Williams LA 3rd, et al. Survey on transfusion-transmitted cytomegalovirus and cytomegalovirus disease mitigation. Arch Pathol Lab Med. 2017;141(12):1705-1711. doi: 10.5858/arpa.2016-0461-OA.
13. Tobian AA, Savage WJ, Tisch DJ, Thoman S, King KE, Ness PM. Prevention of allergic transfusion reactions to platelets and red blood cells through plasma reduction. Transfusion. 2011;51(8):1676-1683. doi: 10.1111/j.1537-2995.2010.03008.x.
14. Veeraputhiran M, Ware J, Dent J, et al. A comparison of washed and volume-reduced platelets with respect to platelet activation, aggregation, and plasma protein removal. Transfusion. 2011;51(5):1030-1036. doi: 10.1111/j.1537-2995.2010.02897.x.
15. Corean J, Al-Tigar R, Pysher T, Blaylock R, Metcalf RA. Quality improvement after multiple fatal transfusion-transmitted bacterial infections. Am J Clin Pathol. 2018;149(4):293-299. doi: 10.1111/j.1537-2995.2010.02897.x.
© 2020 Society of Hospital Medicine