User login
Inflammatory Responses to a Common Food Additive May Depend On the Microbiome
Inflammatory responses to the food additive carboxymethylcellulose (CMC) may depend on the unique characteristics of an individual’s microbiome, according to recent research.
These findings suggest that CMC, which is commonly used as a thickener and emulsifier to improve texture and shelf life of food, could potentially trigger chronic inflammation in genetically prone individuals, although more work is needed to pinpoint the exact microbiota involved, reported lead author Noëmie Daniel, PhD, of the French National Institute of Health and Medical Research (INSERM), Paris, and colleagues.“Preclinical work has shown that [CMC] consumption detrimentally impacts the intestinal microbiota in a way that promotes chronic inflammation,” the investigators wrote in a research letter in Cellular and Molecular Gastroenterology and Hepatology.
They published the results of a randomized, double-blind controlled trial that showed that the seven individuals exposed to a CMC-supplemented diet had “significant alterations in microbiota composition and metabolome” compared with the nine control subjects.
Yet responses to CMC varied widely. In the treatment group, some participants were relatively insensitive to CMC, while two participants had “stark alterations” in their microbiome.
“Such CMC sensitivity was not associated with overt signs of intestinal inflammation but nonetheless might mark proneness to chronic inflammation, compelling us to better understand mechanisms that mediate CMC sensitivity,” the investigators wrote.
To learn more, Dr. Daniel and colleagues conducted the present study, which involved a series of analyses and experiments.
They first compared inflammatory bowel disease-associated mutations and basal gene expression between CMC-sensitive and CMC-insensitive individuals from their previous trial. Neither were associated with CMC sensitivity, they found.
Evaluating microbiota was a more fruitful approach. Microbiome multivariable association with linear models analysis revealed 11 amplicon sequence variants (ASVs) that differed between groups.
“This algorithm did not detect differences between randomly selected subjects, arguing that ASVs that are associated with CMC sensitivity were not false discoveries but rather had marked, and perhaps contributed to, CMC sensitivity status,” the investigators wrote.
Next, they transplanted pre-CMC fecal samples from 2 CMC-sensitive and 2 CMC-insensitive individuals into germ-free, colitis-prone, interleukin 10-/- mice. Exposing these mice to CMC led to distinct changes in microbiota that was not clearly associated with the sensitivity status of the donor. However, mice that received transplants from CMC-sensitive individuals demonstrated increased microbiota-derived proinflammatory markers, increased microbiota encroachment, and “stark” intestinal inflammation after CMC consumption, suggesting that these responses were somehow mediated by the microbiome.
“These [results] indicate a role for basal microbiotas in influencing CMC impact on this cardinal feature of intestinal inflammation and suspected driver of chronic diseases,” the investigators wrote.
“Our findings suggest that the microbiota participate in the extent to which an individual harbors proneness to CMC-induced inflammatory diseases,” they added. “Accordingly, CMC consumption may be one trigger of chronic inflammation in genetically prone individuals colonized with a given microbial ecosystem.”
Research on a larger number of participants appears needed to substantiate their observations and determine the exact microbiota contributor(s) driving CMC sensitivity, the researchers concluded.
The investigators disclosed no conflicts of interest. Funding support came from a starting grant from the European Research Council under the European Union’s Horizon 2020 research and innovation program, a Chaire d’Excellence from IdEx Université de Paris, an award from the Fondation de l’Avenir, ANR grants EMULBIONT and DREAM, and the national program Microbiote from INSERM (B.C.). Supported also came from National Institutes of Health grants, the Penn Center for Nutritional Science and Medicine, and the Max Planck Society.
The consumption of highly processed foods, enriched with food additives, is associated with an increased risk of developing inflammatory bowel disease (IBD). Alteration of the intestinal barrier and microbiota encroachment on epithelial cells is thought to be one of the mechanisms leading to inappropriate mucosal immune activation in response to food additive intake. However, we still do not know why some exposed individuals develop IBD while others do not. The findings of Daniel and colleagues suggest that proinflammatory sensitivity to the food additive carboxymethylcellulose (CMC) is primarily dependent on the composition of the gut microbiota, and that this sensitivity can be, at least partially, transferable, using fecal microbiota transfers in a mouse model of IBD. In particular, they identified 11 taxa of the host basal microbiota associated with the development of intestinal inflammation in response to CMC.
Finally, this study also illustrates the relevance of systematically assessing the impact of food additives and emulsifiers on the gut microbiota and intestinal physiology in order to evaluate their safety using translational approaches similar to those applied by Daniel and colleagues.
Nicolas Benech, MD, PhD is an assistant professor at the Lyon 1 University and Gastroenterology department, Hôpital de la Croix-Rousse, Hospices Civils de Lyon, Lyon, France, the director of the Lyon Fecal Microbiota transplantation Center, and cofounder of the Lyon GEM Microbiota Study Group. He has no conflicts.
The consumption of highly processed foods, enriched with food additives, is associated with an increased risk of developing inflammatory bowel disease (IBD). Alteration of the intestinal barrier and microbiota encroachment on epithelial cells is thought to be one of the mechanisms leading to inappropriate mucosal immune activation in response to food additive intake. However, we still do not know why some exposed individuals develop IBD while others do not. The findings of Daniel and colleagues suggest that proinflammatory sensitivity to the food additive carboxymethylcellulose (CMC) is primarily dependent on the composition of the gut microbiota, and that this sensitivity can be, at least partially, transferable, using fecal microbiota transfers in a mouse model of IBD. In particular, they identified 11 taxa of the host basal microbiota associated with the development of intestinal inflammation in response to CMC.
Finally, this study also illustrates the relevance of systematically assessing the impact of food additives and emulsifiers on the gut microbiota and intestinal physiology in order to evaluate their safety using translational approaches similar to those applied by Daniel and colleagues.
Nicolas Benech, MD, PhD is an assistant professor at the Lyon 1 University and Gastroenterology department, Hôpital de la Croix-Rousse, Hospices Civils de Lyon, Lyon, France, the director of the Lyon Fecal Microbiota transplantation Center, and cofounder of the Lyon GEM Microbiota Study Group. He has no conflicts.
The consumption of highly processed foods, enriched with food additives, is associated with an increased risk of developing inflammatory bowel disease (IBD). Alteration of the intestinal barrier and microbiota encroachment on epithelial cells is thought to be one of the mechanisms leading to inappropriate mucosal immune activation in response to food additive intake. However, we still do not know why some exposed individuals develop IBD while others do not. The findings of Daniel and colleagues suggest that proinflammatory sensitivity to the food additive carboxymethylcellulose (CMC) is primarily dependent on the composition of the gut microbiota, and that this sensitivity can be, at least partially, transferable, using fecal microbiota transfers in a mouse model of IBD. In particular, they identified 11 taxa of the host basal microbiota associated with the development of intestinal inflammation in response to CMC.
Finally, this study also illustrates the relevance of systematically assessing the impact of food additives and emulsifiers on the gut microbiota and intestinal physiology in order to evaluate their safety using translational approaches similar to those applied by Daniel and colleagues.
Nicolas Benech, MD, PhD is an assistant professor at the Lyon 1 University and Gastroenterology department, Hôpital de la Croix-Rousse, Hospices Civils de Lyon, Lyon, France, the director of the Lyon Fecal Microbiota transplantation Center, and cofounder of the Lyon GEM Microbiota Study Group. He has no conflicts.
Inflammatory responses to the food additive carboxymethylcellulose (CMC) may depend on the unique characteristics of an individual’s microbiome, according to recent research.
These findings suggest that CMC, which is commonly used as a thickener and emulsifier to improve texture and shelf life of food, could potentially trigger chronic inflammation in genetically prone individuals, although more work is needed to pinpoint the exact microbiota involved, reported lead author Noëmie Daniel, PhD, of the French National Institute of Health and Medical Research (INSERM), Paris, and colleagues.“Preclinical work has shown that [CMC] consumption detrimentally impacts the intestinal microbiota in a way that promotes chronic inflammation,” the investigators wrote in a research letter in Cellular and Molecular Gastroenterology and Hepatology.
They published the results of a randomized, double-blind controlled trial that showed that the seven individuals exposed to a CMC-supplemented diet had “significant alterations in microbiota composition and metabolome” compared with the nine control subjects.
Yet responses to CMC varied widely. In the treatment group, some participants were relatively insensitive to CMC, while two participants had “stark alterations” in their microbiome.
“Such CMC sensitivity was not associated with overt signs of intestinal inflammation but nonetheless might mark proneness to chronic inflammation, compelling us to better understand mechanisms that mediate CMC sensitivity,” the investigators wrote.
To learn more, Dr. Daniel and colleagues conducted the present study, which involved a series of analyses and experiments.
They first compared inflammatory bowel disease-associated mutations and basal gene expression between CMC-sensitive and CMC-insensitive individuals from their previous trial. Neither were associated with CMC sensitivity, they found.
Evaluating microbiota was a more fruitful approach. Microbiome multivariable association with linear models analysis revealed 11 amplicon sequence variants (ASVs) that differed between groups.
“This algorithm did not detect differences between randomly selected subjects, arguing that ASVs that are associated with CMC sensitivity were not false discoveries but rather had marked, and perhaps contributed to, CMC sensitivity status,” the investigators wrote.
Next, they transplanted pre-CMC fecal samples from 2 CMC-sensitive and 2 CMC-insensitive individuals into germ-free, colitis-prone, interleukin 10-/- mice. Exposing these mice to CMC led to distinct changes in microbiota that was not clearly associated with the sensitivity status of the donor. However, mice that received transplants from CMC-sensitive individuals demonstrated increased microbiota-derived proinflammatory markers, increased microbiota encroachment, and “stark” intestinal inflammation after CMC consumption, suggesting that these responses were somehow mediated by the microbiome.
“These [results] indicate a role for basal microbiotas in influencing CMC impact on this cardinal feature of intestinal inflammation and suspected driver of chronic diseases,” the investigators wrote.
“Our findings suggest that the microbiota participate in the extent to which an individual harbors proneness to CMC-induced inflammatory diseases,” they added. “Accordingly, CMC consumption may be one trigger of chronic inflammation in genetically prone individuals colonized with a given microbial ecosystem.”
Research on a larger number of participants appears needed to substantiate their observations and determine the exact microbiota contributor(s) driving CMC sensitivity, the researchers concluded.
The investigators disclosed no conflicts of interest. Funding support came from a starting grant from the European Research Council under the European Union’s Horizon 2020 research and innovation program, a Chaire d’Excellence from IdEx Université de Paris, an award from the Fondation de l’Avenir, ANR grants EMULBIONT and DREAM, and the national program Microbiote from INSERM (B.C.). Supported also came from National Institutes of Health grants, the Penn Center for Nutritional Science and Medicine, and the Max Planck Society.
Inflammatory responses to the food additive carboxymethylcellulose (CMC) may depend on the unique characteristics of an individual’s microbiome, according to recent research.
These findings suggest that CMC, which is commonly used as a thickener and emulsifier to improve texture and shelf life of food, could potentially trigger chronic inflammation in genetically prone individuals, although more work is needed to pinpoint the exact microbiota involved, reported lead author Noëmie Daniel, PhD, of the French National Institute of Health and Medical Research (INSERM), Paris, and colleagues.“Preclinical work has shown that [CMC] consumption detrimentally impacts the intestinal microbiota in a way that promotes chronic inflammation,” the investigators wrote in a research letter in Cellular and Molecular Gastroenterology and Hepatology.
They published the results of a randomized, double-blind controlled trial that showed that the seven individuals exposed to a CMC-supplemented diet had “significant alterations in microbiota composition and metabolome” compared with the nine control subjects.
Yet responses to CMC varied widely. In the treatment group, some participants were relatively insensitive to CMC, while two participants had “stark alterations” in their microbiome.
“Such CMC sensitivity was not associated with overt signs of intestinal inflammation but nonetheless might mark proneness to chronic inflammation, compelling us to better understand mechanisms that mediate CMC sensitivity,” the investigators wrote.
To learn more, Dr. Daniel and colleagues conducted the present study, which involved a series of analyses and experiments.
They first compared inflammatory bowel disease-associated mutations and basal gene expression between CMC-sensitive and CMC-insensitive individuals from their previous trial. Neither were associated with CMC sensitivity, they found.
Evaluating microbiota was a more fruitful approach. Microbiome multivariable association with linear models analysis revealed 11 amplicon sequence variants (ASVs) that differed between groups.
“This algorithm did not detect differences between randomly selected subjects, arguing that ASVs that are associated with CMC sensitivity were not false discoveries but rather had marked, and perhaps contributed to, CMC sensitivity status,” the investigators wrote.
Next, they transplanted pre-CMC fecal samples from 2 CMC-sensitive and 2 CMC-insensitive individuals into germ-free, colitis-prone, interleukin 10-/- mice. Exposing these mice to CMC led to distinct changes in microbiota that was not clearly associated with the sensitivity status of the donor. However, mice that received transplants from CMC-sensitive individuals demonstrated increased microbiota-derived proinflammatory markers, increased microbiota encroachment, and “stark” intestinal inflammation after CMC consumption, suggesting that these responses were somehow mediated by the microbiome.
“These [results] indicate a role for basal microbiotas in influencing CMC impact on this cardinal feature of intestinal inflammation and suspected driver of chronic diseases,” the investigators wrote.
“Our findings suggest that the microbiota participate in the extent to which an individual harbors proneness to CMC-induced inflammatory diseases,” they added. “Accordingly, CMC consumption may be one trigger of chronic inflammation in genetically prone individuals colonized with a given microbial ecosystem.”
Research on a larger number of participants appears needed to substantiate their observations and determine the exact microbiota contributor(s) driving CMC sensitivity, the researchers concluded.
The investigators disclosed no conflicts of interest. Funding support came from a starting grant from the European Research Council under the European Union’s Horizon 2020 research and innovation program, a Chaire d’Excellence from IdEx Université de Paris, an award from the Fondation de l’Avenir, ANR grants EMULBIONT and DREAM, and the national program Microbiote from INSERM (B.C.). Supported also came from National Institutes of Health grants, the Penn Center for Nutritional Science and Medicine, and the Max Planck Society.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
AI Shows Potential for Detecting Mucosal Healing in Ulcerative Colitis
Artificial intelligence (AI) systems show high potential for detecting mucosal healing in ulcerative colitis with optimal diagnostic performance, according to a new systematic review and meta-analysis.
AI algorithms replicated expert opinion with high sensitivity and specificity when evaluating images and videos. At the same time, moderate-high heterogeneity of the data was found, the authors noted.
“Artificial intelligence software is expected to potentially solve the longstanding issue of low-to-moderate interobserver agreement when human endoscopists are required to indicate mucosal healing or different grades of inflammation in ulcerative colitis,” Alessandro Rimondi, lead author and clinical fellow at the Royal Free Hospital and University College London Institute for Liver and Digestive Health, London, England, told this news organization.
“However, high levels of heterogeneity have been found, potentially linked to how differently the AI software was trained and how many cases it has been tested on,” he said. “This partially limits the quality of the body of evidence.”
The study was published online in Digestive and Liver Disease.
Evaluating AI Detection
In clinical practice, assessing mucosal healing in inflammatory bowel disease (IBD) is critical for evaluating a patient’s response to therapy and guiding strategies for treatment, surgery, and endoscopic surveillance. In an era of precision medicine, assessment of mucosal healing should be precise, readily available in an endoscopic report, and highly reproducible, which requires high accuracy and agreement in endoscopic diagnosis, the authors noted.
AI systems — particularly deep learning algorithms based on convolutional neural network architecture — may allow endoscopists to establish an objective and real-time diagnosis of mucosal healing and improve the average quality standards at primary and tertiary care centers, the authors wrote. Research on AI in IBD has looked at potential implications for endoscopy and clinical management, which opens new areas to explore.
Dr. Rimondi and colleagues conducted a systematic review of studies up to December 2022 that involved an AI-based system used to estimate any degree of endoscopic inflammation in IBD, whether ulcerative colitis or Crohn’s disease. After that, they conducted a diagnostic test accuracy meta-analysis restricted to the field in which more than five studies providing diagnostic performance — mucosal healing in ulcerative colitis based on luminal imaging — were available.
The researchers identified 12 studies with luminal imaging in patients with ulcerative colitis. Four evaluated the performance of AI systems on videos, six focused on fixed images, and two looked at both.
Overall, the AI systems achieved a satisfactory performance in evaluating mucosal healing in ulcerative colitis. When evaluating fixed images, the algorithms achieved a sensitivity of 0.91 and specificity of 0.89, with a diagnostic odds ratio (DOR) of 92.42, summary receiver operating characteristic curve (SROC) of 0.957, and area under the curve (AUC) of 0.957. When evaluating videos, the algorithms achieved 0.86 sensitivity, 0.91 specificity, 70.86 DOR, 0.941 SROC, and 0.941 AUC.
“It is exciting to see artificial intelligence expand and be effective for conditions beyond colon polyps,” Seth Gross, MD, professor of medicine and clinical chief of gastroenterology and hepatology at NYU Langone Health, New York, told this news organization.
Dr. Gross, who wasn’t involved with this study, has researched AI applications in endoscopy and colonoscopy. He and colleagues have found that machine learning software can improve lesion and polyp detection, serving as a “second set of eyes” for practitioners.
“Mucosal healing interpretation can be variable amongst providers,” he said. “AI has the potential to help standardize the assessment of mucosal healing in patients with ulcerative colitis.”
Improving AI Training
The authors found moderate-high levels of heterogeneity among the studies, which limited the quality of the evidence. Only 2 of the 12 studies used an external dataset to validate the AI systems, and 1 evaluated the AI system on a mixed database. However, seven used an internal validation dataset separate from the training dataset.
It is crucial to find a shared consensus on training for AI models, with a shared definition of mucosal healing and cutoff thresholds based on recent guidelines, Dr. Rimondi and colleagues noted. Training data ideally should be on the basis of a broad and shared database containing images and videos with high interobserver agreement on the degree of inflammation, they added.
“We probably need a consensus or guidelines that identify the standards for training and testing newly developed software, stating the bare minimum number of images or videos for the training and testing sections,” Dr. Rimondi said.
In addition, due to interobserver misalignment, an expert-validated database could help serve the purpose of a gold standard, he added.
“In my opinion, artificial intelligence tends to better perform when it is required to evaluate a dichotomic outcome (such as polyp detection, which is a yes or no task) than when it is required to replicate more difficult tasks (such as polyp characterization or judging a degree of inflammation), which have a continuous range of expression,” Dr. Rimondi said.
The authors declared no financial support for this study. Dr. Rimondi and Dr. Gross reported no financial disclosures.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) systems show high potential for detecting mucosal healing in ulcerative colitis with optimal diagnostic performance, according to a new systematic review and meta-analysis.
AI algorithms replicated expert opinion with high sensitivity and specificity when evaluating images and videos. At the same time, moderate-high heterogeneity of the data was found, the authors noted.
“Artificial intelligence software is expected to potentially solve the longstanding issue of low-to-moderate interobserver agreement when human endoscopists are required to indicate mucosal healing or different grades of inflammation in ulcerative colitis,” Alessandro Rimondi, lead author and clinical fellow at the Royal Free Hospital and University College London Institute for Liver and Digestive Health, London, England, told this news organization.
“However, high levels of heterogeneity have been found, potentially linked to how differently the AI software was trained and how many cases it has been tested on,” he said. “This partially limits the quality of the body of evidence.”
The study was published online in Digestive and Liver Disease.
Evaluating AI Detection
In clinical practice, assessing mucosal healing in inflammatory bowel disease (IBD) is critical for evaluating a patient’s response to therapy and guiding strategies for treatment, surgery, and endoscopic surveillance. In an era of precision medicine, assessment of mucosal healing should be precise, readily available in an endoscopic report, and highly reproducible, which requires high accuracy and agreement in endoscopic diagnosis, the authors noted.
AI systems — particularly deep learning algorithms based on convolutional neural network architecture — may allow endoscopists to establish an objective and real-time diagnosis of mucosal healing and improve the average quality standards at primary and tertiary care centers, the authors wrote. Research on AI in IBD has looked at potential implications for endoscopy and clinical management, which opens new areas to explore.
Dr. Rimondi and colleagues conducted a systematic review of studies up to December 2022 that involved an AI-based system used to estimate any degree of endoscopic inflammation in IBD, whether ulcerative colitis or Crohn’s disease. After that, they conducted a diagnostic test accuracy meta-analysis restricted to the field in which more than five studies providing diagnostic performance — mucosal healing in ulcerative colitis based on luminal imaging — were available.
The researchers identified 12 studies with luminal imaging in patients with ulcerative colitis. Four evaluated the performance of AI systems on videos, six focused on fixed images, and two looked at both.
Overall, the AI systems achieved a satisfactory performance in evaluating mucosal healing in ulcerative colitis. When evaluating fixed images, the algorithms achieved a sensitivity of 0.91 and specificity of 0.89, with a diagnostic odds ratio (DOR) of 92.42, summary receiver operating characteristic curve (SROC) of 0.957, and area under the curve (AUC) of 0.957. When evaluating videos, the algorithms achieved 0.86 sensitivity, 0.91 specificity, 70.86 DOR, 0.941 SROC, and 0.941 AUC.
“It is exciting to see artificial intelligence expand and be effective for conditions beyond colon polyps,” Seth Gross, MD, professor of medicine and clinical chief of gastroenterology and hepatology at NYU Langone Health, New York, told this news organization.
Dr. Gross, who wasn’t involved with this study, has researched AI applications in endoscopy and colonoscopy. He and colleagues have found that machine learning software can improve lesion and polyp detection, serving as a “second set of eyes” for practitioners.
“Mucosal healing interpretation can be variable amongst providers,” he said. “AI has the potential to help standardize the assessment of mucosal healing in patients with ulcerative colitis.”
Improving AI Training
The authors found moderate-high levels of heterogeneity among the studies, which limited the quality of the evidence. Only 2 of the 12 studies used an external dataset to validate the AI systems, and 1 evaluated the AI system on a mixed database. However, seven used an internal validation dataset separate from the training dataset.
It is crucial to find a shared consensus on training for AI models, with a shared definition of mucosal healing and cutoff thresholds based on recent guidelines, Dr. Rimondi and colleagues noted. Training data ideally should be on the basis of a broad and shared database containing images and videos with high interobserver agreement on the degree of inflammation, they added.
“We probably need a consensus or guidelines that identify the standards for training and testing newly developed software, stating the bare minimum number of images or videos for the training and testing sections,” Dr. Rimondi said.
In addition, due to interobserver misalignment, an expert-validated database could help serve the purpose of a gold standard, he added.
“In my opinion, artificial intelligence tends to better perform when it is required to evaluate a dichotomic outcome (such as polyp detection, which is a yes or no task) than when it is required to replicate more difficult tasks (such as polyp characterization or judging a degree of inflammation), which have a continuous range of expression,” Dr. Rimondi said.
The authors declared no financial support for this study. Dr. Rimondi and Dr. Gross reported no financial disclosures.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) systems show high potential for detecting mucosal healing in ulcerative colitis with optimal diagnostic performance, according to a new systematic review and meta-analysis.
AI algorithms replicated expert opinion with high sensitivity and specificity when evaluating images and videos. At the same time, moderate-high heterogeneity of the data was found, the authors noted.
“Artificial intelligence software is expected to potentially solve the longstanding issue of low-to-moderate interobserver agreement when human endoscopists are required to indicate mucosal healing or different grades of inflammation in ulcerative colitis,” Alessandro Rimondi, lead author and clinical fellow at the Royal Free Hospital and University College London Institute for Liver and Digestive Health, London, England, told this news organization.
“However, high levels of heterogeneity have been found, potentially linked to how differently the AI software was trained and how many cases it has been tested on,” he said. “This partially limits the quality of the body of evidence.”
The study was published online in Digestive and Liver Disease.
Evaluating AI Detection
In clinical practice, assessing mucosal healing in inflammatory bowel disease (IBD) is critical for evaluating a patient’s response to therapy and guiding strategies for treatment, surgery, and endoscopic surveillance. In an era of precision medicine, assessment of mucosal healing should be precise, readily available in an endoscopic report, and highly reproducible, which requires high accuracy and agreement in endoscopic diagnosis, the authors noted.
AI systems — particularly deep learning algorithms based on convolutional neural network architecture — may allow endoscopists to establish an objective and real-time diagnosis of mucosal healing and improve the average quality standards at primary and tertiary care centers, the authors wrote. Research on AI in IBD has looked at potential implications for endoscopy and clinical management, which opens new areas to explore.
Dr. Rimondi and colleagues conducted a systematic review of studies up to December 2022 that involved an AI-based system used to estimate any degree of endoscopic inflammation in IBD, whether ulcerative colitis or Crohn’s disease. After that, they conducted a diagnostic test accuracy meta-analysis restricted to the field in which more than five studies providing diagnostic performance — mucosal healing in ulcerative colitis based on luminal imaging — were available.
The researchers identified 12 studies with luminal imaging in patients with ulcerative colitis. Four evaluated the performance of AI systems on videos, six focused on fixed images, and two looked at both.
Overall, the AI systems achieved a satisfactory performance in evaluating mucosal healing in ulcerative colitis. When evaluating fixed images, the algorithms achieved a sensitivity of 0.91 and specificity of 0.89, with a diagnostic odds ratio (DOR) of 92.42, summary receiver operating characteristic curve (SROC) of 0.957, and area under the curve (AUC) of 0.957. When evaluating videos, the algorithms achieved 0.86 sensitivity, 0.91 specificity, 70.86 DOR, 0.941 SROC, and 0.941 AUC.
“It is exciting to see artificial intelligence expand and be effective for conditions beyond colon polyps,” Seth Gross, MD, professor of medicine and clinical chief of gastroenterology and hepatology at NYU Langone Health, New York, told this news organization.
Dr. Gross, who wasn’t involved with this study, has researched AI applications in endoscopy and colonoscopy. He and colleagues have found that machine learning software can improve lesion and polyp detection, serving as a “second set of eyes” for practitioners.
“Mucosal healing interpretation can be variable amongst providers,” he said. “AI has the potential to help standardize the assessment of mucosal healing in patients with ulcerative colitis.”
Improving AI Training
The authors found moderate-high levels of heterogeneity among the studies, which limited the quality of the evidence. Only 2 of the 12 studies used an external dataset to validate the AI systems, and 1 evaluated the AI system on a mixed database. However, seven used an internal validation dataset separate from the training dataset.
It is crucial to find a shared consensus on training for AI models, with a shared definition of mucosal healing and cutoff thresholds based on recent guidelines, Dr. Rimondi and colleagues noted. Training data ideally should be on the basis of a broad and shared database containing images and videos with high interobserver agreement on the degree of inflammation, they added.
“We probably need a consensus or guidelines that identify the standards for training and testing newly developed software, stating the bare minimum number of images or videos for the training and testing sections,” Dr. Rimondi said.
In addition, due to interobserver misalignment, an expert-validated database could help serve the purpose of a gold standard, he added.
“In my opinion, artificial intelligence tends to better perform when it is required to evaluate a dichotomic outcome (such as polyp detection, which is a yes or no task) than when it is required to replicate more difficult tasks (such as polyp characterization or judging a degree of inflammation), which have a continuous range of expression,” Dr. Rimondi said.
The authors declared no financial support for this study. Dr. Rimondi and Dr. Gross reported no financial disclosures.
A version of this article appeared on Medscape.com.
FROM DIGESTIVE AND LIVER DISEASE
Who Is Helped by AI Use During Colonoscopy?
Artificial intelligence (AI) holds the promise of identifying premalignant and advanced malignant lesions during colonoscopy that might otherwise be missed.
Is it living up to that promise?
It seems that depends on where, how, and by whom it’s being implemented.
Clinical Trials vs the Real World
The majority of randomized clinical trials of AI use conducted worldwide “clearly show an increase in the adenoma detection rate (ADR) during colonoscopy,” Prateek Sharma, MD, a gastroenterologist at The University of Kansas Cancer Center, Kansas City, told this news. “But the real-world results have been quite varied; some show improvement, and others don’t.”
Dr. Sharma is coauthor of a recent pooled analysis of nine randomized controlled trials on the impact of AI on colonoscopy surveillance after polyp removal. It found that AI use increased the proportion of patients requiring intensive surveillance by approximately 35% in the United States and 20% in Europe (absolute increases of 2.9% and 1.3%, respectively).
“While this may contribute to improved cancer prevention, it significantly adds patient burden and healthcare costs,” the authors concluded.
A recent retrospective analysis of staggered implementation of a computer-aided detection (CADe) system at a single academic center in Chicago found that for screening and surveillance colonoscopy combined, endoscopists using CADe identified more adenomas and serrated polyps — but only endoscopists who used CADe regularly (“majority” users).
A systematic review and meta-analysis of 21 randomized controlled trials comparing CADe with standard colonoscopy found increased detection of adenomas, but not of advanced adenomas, as well as higher rates of unnecessary removal of non-neoplastic polyps.
Adding to the mix, a multicenter randomized controlled trial of patients with a positive fecal immunochemical test found that AI use was not associated with better detection of advanced neoplasias. Lead author Carolina Mangas Sanjuán, MD, PhD, Hospital General Universitario Dr. Balmis, Alicante, Spain, told this news organization the results were “surprising,” given previous studies showing benefit.
Similarly, a pragmatic implementation trial conducted by Stanford, California, researchers showed no significant effect of CADe on ADR, adenomas per colonoscopy, or any other detection metric. Furthermore, CADe had no effect on procedure times or non-neoplastic detection rates.
The authors cautioned against viewing their study as an “outlier,” however, and pointed to an Israeli study comparing adenoma and polyp detection rates 6 months before and after the introduction of AI-aided colonoscopy. Those authors reported no performance improvement with the AI device and concluded that it was not useful in routine practice.
A ‘Mishmash’ of Methods
“It’s not clear why some studies are positive, and some are negative,” Dr. Sharma acknowledged.
Study design is a factor, particularly in real-world studies, he said. Some researchers use the before/after approach, as in the Israeli study; others compare use in different rooms — that is, one with a CADe device and one without. Like the Chicago analysis, findings from such studies probably depend on whether the colonoscopists with the CADe device in the room actually use it.
Other real-world studies look at detection by time, Dr. Sharma said.
For example, a study of 1780 colonoscopies in China found that AI systems showed higher assistance ability among colonoscopies performed later in the day, when adenoma detection rates typically declined, perhaps owing to fatigue.
These authors suggest that AI may have the potential to maintain high quality and homogeneity of colonoscopies and improve endoscopist performance in large screening programs and centers with high workloads.
“There’s a mishmash of different kinds of real-world studies coming in, and it’s very difficult to figure it all out,” Dr. Sharma said. “We just have to look at these devices as innovations and embrace them and work with them to see how it fits it in our practice.”
Perceptions and Expectations
Emerging evidence suggests that endoscopists’ perceptions and expectations may affect assessments of AI’s potential benefits in practice, Dr. Sharma noted.
“Someone might say, ‘I’m a trained physician. Why do I need a machine to help me?’ That can create a situation in which the endoscopist is constantly challenging the device, trying to overrule it or not give it credit.”
Others might perceive that the AI device will definitely help and therefore not look as carefully themselves for adenomas.
A study at The University of Texas MD Anderson Cancer Center in Houston in which activation of the AI system was at the discretion of the endoscopist found that real-time CADe did not improve adenoma detection among endoscopists with high baseline detection rates.
However, despite its availability, AI-assisted colonoscopy was activated in only half of the cases, and multiple concerns were raised by staff and endoscopists in a postprocedural survey. In particular, endoscopists were concerned that the system would result in too many false-positive signals (82.4%), was too distracting (58.8%), and prolonged procedure time (47.1%).
The authors of the Stanford study that found no benefit with CADe in routine practice noted, “Most concerning would be if, inadvertently, CADe use was accompanied by a simultaneous unconscious degradation in the quality of mucosal exposure, possibly due to a false sense of comfort that CADe would ensure a high-quality examination.”
“We’re trying to evaluate some of these interactions between endoscopists and AI devices both pragmatically in practice as well as in clinical trials,” Dr. Sharma said. “Much depends on the context of how you approach and present the devices. We tell physicians that this is an assist device, not something you’re competing against and not something that’s here to replace you. This is something which may make your lives easier, so try it out.”
Are Less Experienced Endoscopists Helped More?
It seems intuitive that less experienced endoscopists would be helped by AI, and indeed, some recent studies confirm this.
A small randomized controlled trial in Japan, presented during the Presidential Plenary at the American Society for Gastrointestinal Endoscopy (ASGE) annual meeting in May 2023, showed that a CADe system was “particularly useful” for beginning endoscopists, who had lower adenoma miss rates with the device vs a white light control device.
Another randomized controlled trial in Japan found that CADe use was associated with an increased overall ADR among endoscopists in training.
But experienced endoscopists probably can benefit as well, noted Jennifer Christie, MD, Division Director, Gastroenterology and Hepatology at the University of Colorado School of Medicine Anschutz Medical Campus in Aurora.
“We know that these AI devices can be useful in training our fellows to detect certain lesions in the colon,” she said. “However, they’re also helpful for many very seasoned practitioners, as an adjunctive tool to help in terms of diagnosis.”
Some studies reflect that dual benefit.
The AID-2 study, designed specifically to look at whether experience had an effect on AI findings during colonoscopy, was conducted among nonexpert endoscopists (lifetime volume of less than 2000 colonoscopies). The researchers, including Dr. Sharma, found that CADe increased the ADR by 22% compared with the control group.
An earlier study, AID-1 , used a similar design but was conducted among experienced endoscopists. In AID-1, the ADR was also significantly higher in the CADe group (54.8%) compared with the control group (40.4%), and adenomas detected per colonoscopy were significantly higher in the CADe group (mean, 1.07) than in the control group (mean, 0.71).
A multivariate post hoc analysis that pooled results from both AID-1 and AID-2 showed that use of CADe and colonoscopy indication, but not the level of examiner experience, were associated with ADR differences. This led the researchers to conclude, “Experience appears to play a minor role as a determining factor for ADR.”
Similarly, a 2023 study from China looked at the mean number of adenomas detected per colonoscopy according to the endoscopist’s experience. All rates were significantly higher in AI-assisted colonoscopies compared with conventional non-AI colonoscopy: overall ADR, 39.9% vs 32.4%; advanced ADR, 6.6% vs 4.9%; ADR of expert endoscopists, 42.3% vs 32.8%; ADR of nonexpert endoscopists, 37.5% vs 32.1%; and adenomas per colonoscopy, 0.59 vs 0.45, respectively.
The authors concluded that “AI-assisted colonoscopy improved overall ADR, advanced ADR, and ADR of both expert and nonexpert attending endoscopists.”
Improving the Algorithms
Experts agree that current and future research will improve the accuracy and quality of AI colonoscopy for all users, leading to new standards and more consistent outcomes in both clinical trials and real-world applications.
Work underway now to improve the algorithms will be an important step in that direction, according to Dr. Christie.
“We need to have enough information to create AI algorithms that allow us to detect early lesions, at least from an imaging standpoint, and we need to improve and increase the sensitivity and the specificity, as well as the predictive value,” she said.
AI can also play a role in health equity, she noted.
“But it’s a double-edged sword, because it depends again on algorithms and machine learning. Perhaps AI can eliminate some of the bias in our clinical decision-making. However, if we don’t train the machine properly with a good, diverse sample of patients and figure out how to integrate some of the social determinants of health that a computer may not otherwise consider, it can create larger disparities and larger biases. AI devices can only be as good and as inclusive as we make them,” Dr. Christie said.
Looking Ahead
Dr. Sharma predicts that “the next slew of studies are going to be on characterization — not just saying there’s an abnormality but distinguishing it further and saying whether the lesion is noncancerous, precancerous, or cancer.”
Other studies will focus on quality improvement of factors, such as withdrawal time and bowel preparation.
In its clinical practice update on AI, the American Gastroenterological Association states, “Eventually, we predict an AI suite of tools for colonoscopy will seem indispensable, as a powerful adjunct to support safe and efficient clinical practice. AI tools that improve colonoscopy quality may become more accepted, and perhaps demanded, by payors, administrators, and possibly even by well-informed patients who want to ensure the highest-quality examination of their colon.”
Dr. Sharma and Dr. Christie disclose no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) holds the promise of identifying premalignant and advanced malignant lesions during colonoscopy that might otherwise be missed.
Is it living up to that promise?
It seems that depends on where, how, and by whom it’s being implemented.
Clinical Trials vs the Real World
The majority of randomized clinical trials of AI use conducted worldwide “clearly show an increase in the adenoma detection rate (ADR) during colonoscopy,” Prateek Sharma, MD, a gastroenterologist at The University of Kansas Cancer Center, Kansas City, told this news. “But the real-world results have been quite varied; some show improvement, and others don’t.”
Dr. Sharma is coauthor of a recent pooled analysis of nine randomized controlled trials on the impact of AI on colonoscopy surveillance after polyp removal. It found that AI use increased the proportion of patients requiring intensive surveillance by approximately 35% in the United States and 20% in Europe (absolute increases of 2.9% and 1.3%, respectively).
“While this may contribute to improved cancer prevention, it significantly adds patient burden and healthcare costs,” the authors concluded.
A recent retrospective analysis of staggered implementation of a computer-aided detection (CADe) system at a single academic center in Chicago found that for screening and surveillance colonoscopy combined, endoscopists using CADe identified more adenomas and serrated polyps — but only endoscopists who used CADe regularly (“majority” users).
A systematic review and meta-analysis of 21 randomized controlled trials comparing CADe with standard colonoscopy found increased detection of adenomas, but not of advanced adenomas, as well as higher rates of unnecessary removal of non-neoplastic polyps.
Adding to the mix, a multicenter randomized controlled trial of patients with a positive fecal immunochemical test found that AI use was not associated with better detection of advanced neoplasias. Lead author Carolina Mangas Sanjuán, MD, PhD, Hospital General Universitario Dr. Balmis, Alicante, Spain, told this news organization the results were “surprising,” given previous studies showing benefit.
Similarly, a pragmatic implementation trial conducted by Stanford, California, researchers showed no significant effect of CADe on ADR, adenomas per colonoscopy, or any other detection metric. Furthermore, CADe had no effect on procedure times or non-neoplastic detection rates.
The authors cautioned against viewing their study as an “outlier,” however, and pointed to an Israeli study comparing adenoma and polyp detection rates 6 months before and after the introduction of AI-aided colonoscopy. Those authors reported no performance improvement with the AI device and concluded that it was not useful in routine practice.
A ‘Mishmash’ of Methods
“It’s not clear why some studies are positive, and some are negative,” Dr. Sharma acknowledged.
Study design is a factor, particularly in real-world studies, he said. Some researchers use the before/after approach, as in the Israeli study; others compare use in different rooms — that is, one with a CADe device and one without. Like the Chicago analysis, findings from such studies probably depend on whether the colonoscopists with the CADe device in the room actually use it.
Other real-world studies look at detection by time, Dr. Sharma said.
For example, a study of 1780 colonoscopies in China found that AI systems showed higher assistance ability among colonoscopies performed later in the day, when adenoma detection rates typically declined, perhaps owing to fatigue.
These authors suggest that AI may have the potential to maintain high quality and homogeneity of colonoscopies and improve endoscopist performance in large screening programs and centers with high workloads.
“There’s a mishmash of different kinds of real-world studies coming in, and it’s very difficult to figure it all out,” Dr. Sharma said. “We just have to look at these devices as innovations and embrace them and work with them to see how it fits it in our practice.”
Perceptions and Expectations
Emerging evidence suggests that endoscopists’ perceptions and expectations may affect assessments of AI’s potential benefits in practice, Dr. Sharma noted.
“Someone might say, ‘I’m a trained physician. Why do I need a machine to help me?’ That can create a situation in which the endoscopist is constantly challenging the device, trying to overrule it or not give it credit.”
Others might perceive that the AI device will definitely help and therefore not look as carefully themselves for adenomas.
A study at The University of Texas MD Anderson Cancer Center in Houston in which activation of the AI system was at the discretion of the endoscopist found that real-time CADe did not improve adenoma detection among endoscopists with high baseline detection rates.
However, despite its availability, AI-assisted colonoscopy was activated in only half of the cases, and multiple concerns were raised by staff and endoscopists in a postprocedural survey. In particular, endoscopists were concerned that the system would result in too many false-positive signals (82.4%), was too distracting (58.8%), and prolonged procedure time (47.1%).
The authors of the Stanford study that found no benefit with CADe in routine practice noted, “Most concerning would be if, inadvertently, CADe use was accompanied by a simultaneous unconscious degradation in the quality of mucosal exposure, possibly due to a false sense of comfort that CADe would ensure a high-quality examination.”
“We’re trying to evaluate some of these interactions between endoscopists and AI devices both pragmatically in practice as well as in clinical trials,” Dr. Sharma said. “Much depends on the context of how you approach and present the devices. We tell physicians that this is an assist device, not something you’re competing against and not something that’s here to replace you. This is something which may make your lives easier, so try it out.”
Are Less Experienced Endoscopists Helped More?
It seems intuitive that less experienced endoscopists would be helped by AI, and indeed, some recent studies confirm this.
A small randomized controlled trial in Japan, presented during the Presidential Plenary at the American Society for Gastrointestinal Endoscopy (ASGE) annual meeting in May 2023, showed that a CADe system was “particularly useful” for beginning endoscopists, who had lower adenoma miss rates with the device vs a white light control device.
Another randomized controlled trial in Japan found that CADe use was associated with an increased overall ADR among endoscopists in training.
But experienced endoscopists probably can benefit as well, noted Jennifer Christie, MD, Division Director, Gastroenterology and Hepatology at the University of Colorado School of Medicine Anschutz Medical Campus in Aurora.
“We know that these AI devices can be useful in training our fellows to detect certain lesions in the colon,” she said. “However, they’re also helpful for many very seasoned practitioners, as an adjunctive tool to help in terms of diagnosis.”
Some studies reflect that dual benefit.
The AID-2 study, designed specifically to look at whether experience had an effect on AI findings during colonoscopy, was conducted among nonexpert endoscopists (lifetime volume of less than 2000 colonoscopies). The researchers, including Dr. Sharma, found that CADe increased the ADR by 22% compared with the control group.
An earlier study, AID-1 , used a similar design but was conducted among experienced endoscopists. In AID-1, the ADR was also significantly higher in the CADe group (54.8%) compared with the control group (40.4%), and adenomas detected per colonoscopy were significantly higher in the CADe group (mean, 1.07) than in the control group (mean, 0.71).
A multivariate post hoc analysis that pooled results from both AID-1 and AID-2 showed that use of CADe and colonoscopy indication, but not the level of examiner experience, were associated with ADR differences. This led the researchers to conclude, “Experience appears to play a minor role as a determining factor for ADR.”
Similarly, a 2023 study from China looked at the mean number of adenomas detected per colonoscopy according to the endoscopist’s experience. All rates were significantly higher in AI-assisted colonoscopies compared with conventional non-AI colonoscopy: overall ADR, 39.9% vs 32.4%; advanced ADR, 6.6% vs 4.9%; ADR of expert endoscopists, 42.3% vs 32.8%; ADR of nonexpert endoscopists, 37.5% vs 32.1%; and adenomas per colonoscopy, 0.59 vs 0.45, respectively.
The authors concluded that “AI-assisted colonoscopy improved overall ADR, advanced ADR, and ADR of both expert and nonexpert attending endoscopists.”
Improving the Algorithms
Experts agree that current and future research will improve the accuracy and quality of AI colonoscopy for all users, leading to new standards and more consistent outcomes in both clinical trials and real-world applications.
Work underway now to improve the algorithms will be an important step in that direction, according to Dr. Christie.
“We need to have enough information to create AI algorithms that allow us to detect early lesions, at least from an imaging standpoint, and we need to improve and increase the sensitivity and the specificity, as well as the predictive value,” she said.
AI can also play a role in health equity, she noted.
“But it’s a double-edged sword, because it depends again on algorithms and machine learning. Perhaps AI can eliminate some of the bias in our clinical decision-making. However, if we don’t train the machine properly with a good, diverse sample of patients and figure out how to integrate some of the social determinants of health that a computer may not otherwise consider, it can create larger disparities and larger biases. AI devices can only be as good and as inclusive as we make them,” Dr. Christie said.
Looking Ahead
Dr. Sharma predicts that “the next slew of studies are going to be on characterization — not just saying there’s an abnormality but distinguishing it further and saying whether the lesion is noncancerous, precancerous, or cancer.”
Other studies will focus on quality improvement of factors, such as withdrawal time and bowel preparation.
In its clinical practice update on AI, the American Gastroenterological Association states, “Eventually, we predict an AI suite of tools for colonoscopy will seem indispensable, as a powerful adjunct to support safe and efficient clinical practice. AI tools that improve colonoscopy quality may become more accepted, and perhaps demanded, by payors, administrators, and possibly even by well-informed patients who want to ensure the highest-quality examination of their colon.”
Dr. Sharma and Dr. Christie disclose no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) holds the promise of identifying premalignant and advanced malignant lesions during colonoscopy that might otherwise be missed.
Is it living up to that promise?
It seems that depends on where, how, and by whom it’s being implemented.
Clinical Trials vs the Real World
The majority of randomized clinical trials of AI use conducted worldwide “clearly show an increase in the adenoma detection rate (ADR) during colonoscopy,” Prateek Sharma, MD, a gastroenterologist at The University of Kansas Cancer Center, Kansas City, told this news. “But the real-world results have been quite varied; some show improvement, and others don’t.”
Dr. Sharma is coauthor of a recent pooled analysis of nine randomized controlled trials on the impact of AI on colonoscopy surveillance after polyp removal. It found that AI use increased the proportion of patients requiring intensive surveillance by approximately 35% in the United States and 20% in Europe (absolute increases of 2.9% and 1.3%, respectively).
“While this may contribute to improved cancer prevention, it significantly adds patient burden and healthcare costs,” the authors concluded.
A recent retrospective analysis of staggered implementation of a computer-aided detection (CADe) system at a single academic center in Chicago found that for screening and surveillance colonoscopy combined, endoscopists using CADe identified more adenomas and serrated polyps — but only endoscopists who used CADe regularly (“majority” users).
A systematic review and meta-analysis of 21 randomized controlled trials comparing CADe with standard colonoscopy found increased detection of adenomas, but not of advanced adenomas, as well as higher rates of unnecessary removal of non-neoplastic polyps.
Adding to the mix, a multicenter randomized controlled trial of patients with a positive fecal immunochemical test found that AI use was not associated with better detection of advanced neoplasias. Lead author Carolina Mangas Sanjuán, MD, PhD, Hospital General Universitario Dr. Balmis, Alicante, Spain, told this news organization the results were “surprising,” given previous studies showing benefit.
Similarly, a pragmatic implementation trial conducted by Stanford, California, researchers showed no significant effect of CADe on ADR, adenomas per colonoscopy, or any other detection metric. Furthermore, CADe had no effect on procedure times or non-neoplastic detection rates.
The authors cautioned against viewing their study as an “outlier,” however, and pointed to an Israeli study comparing adenoma and polyp detection rates 6 months before and after the introduction of AI-aided colonoscopy. Those authors reported no performance improvement with the AI device and concluded that it was not useful in routine practice.
A ‘Mishmash’ of Methods
“It’s not clear why some studies are positive, and some are negative,” Dr. Sharma acknowledged.
Study design is a factor, particularly in real-world studies, he said. Some researchers use the before/after approach, as in the Israeli study; others compare use in different rooms — that is, one with a CADe device and one without. Like the Chicago analysis, findings from such studies probably depend on whether the colonoscopists with the CADe device in the room actually use it.
Other real-world studies look at detection by time, Dr. Sharma said.
For example, a study of 1780 colonoscopies in China found that AI systems showed higher assistance ability among colonoscopies performed later in the day, when adenoma detection rates typically declined, perhaps owing to fatigue.
These authors suggest that AI may have the potential to maintain high quality and homogeneity of colonoscopies and improve endoscopist performance in large screening programs and centers with high workloads.
“There’s a mishmash of different kinds of real-world studies coming in, and it’s very difficult to figure it all out,” Dr. Sharma said. “We just have to look at these devices as innovations and embrace them and work with them to see how it fits it in our practice.”
Perceptions and Expectations
Emerging evidence suggests that endoscopists’ perceptions and expectations may affect assessments of AI’s potential benefits in practice, Dr. Sharma noted.
“Someone might say, ‘I’m a trained physician. Why do I need a machine to help me?’ That can create a situation in which the endoscopist is constantly challenging the device, trying to overrule it or not give it credit.”
Others might perceive that the AI device will definitely help and therefore not look as carefully themselves for adenomas.
A study at The University of Texas MD Anderson Cancer Center in Houston in which activation of the AI system was at the discretion of the endoscopist found that real-time CADe did not improve adenoma detection among endoscopists with high baseline detection rates.
However, despite its availability, AI-assisted colonoscopy was activated in only half of the cases, and multiple concerns were raised by staff and endoscopists in a postprocedural survey. In particular, endoscopists were concerned that the system would result in too many false-positive signals (82.4%), was too distracting (58.8%), and prolonged procedure time (47.1%).
The authors of the Stanford study that found no benefit with CADe in routine practice noted, “Most concerning would be if, inadvertently, CADe use was accompanied by a simultaneous unconscious degradation in the quality of mucosal exposure, possibly due to a false sense of comfort that CADe would ensure a high-quality examination.”
“We’re trying to evaluate some of these interactions between endoscopists and AI devices both pragmatically in practice as well as in clinical trials,” Dr. Sharma said. “Much depends on the context of how you approach and present the devices. We tell physicians that this is an assist device, not something you’re competing against and not something that’s here to replace you. This is something which may make your lives easier, so try it out.”
Are Less Experienced Endoscopists Helped More?
It seems intuitive that less experienced endoscopists would be helped by AI, and indeed, some recent studies confirm this.
A small randomized controlled trial in Japan, presented during the Presidential Plenary at the American Society for Gastrointestinal Endoscopy (ASGE) annual meeting in May 2023, showed that a CADe system was “particularly useful” for beginning endoscopists, who had lower adenoma miss rates with the device vs a white light control device.
Another randomized controlled trial in Japan found that CADe use was associated with an increased overall ADR among endoscopists in training.
But experienced endoscopists probably can benefit as well, noted Jennifer Christie, MD, Division Director, Gastroenterology and Hepatology at the University of Colorado School of Medicine Anschutz Medical Campus in Aurora.
“We know that these AI devices can be useful in training our fellows to detect certain lesions in the colon,” she said. “However, they’re also helpful for many very seasoned practitioners, as an adjunctive tool to help in terms of diagnosis.”
Some studies reflect that dual benefit.
The AID-2 study, designed specifically to look at whether experience had an effect on AI findings during colonoscopy, was conducted among nonexpert endoscopists (lifetime volume of less than 2000 colonoscopies). The researchers, including Dr. Sharma, found that CADe increased the ADR by 22% compared with the control group.
An earlier study, AID-1 , used a similar design but was conducted among experienced endoscopists. In AID-1, the ADR was also significantly higher in the CADe group (54.8%) compared with the control group (40.4%), and adenomas detected per colonoscopy were significantly higher in the CADe group (mean, 1.07) than in the control group (mean, 0.71).
A multivariate post hoc analysis that pooled results from both AID-1 and AID-2 showed that use of CADe and colonoscopy indication, but not the level of examiner experience, were associated with ADR differences. This led the researchers to conclude, “Experience appears to play a minor role as a determining factor for ADR.”
Similarly, a 2023 study from China looked at the mean number of adenomas detected per colonoscopy according to the endoscopist’s experience. All rates were significantly higher in AI-assisted colonoscopies compared with conventional non-AI colonoscopy: overall ADR, 39.9% vs 32.4%; advanced ADR, 6.6% vs 4.9%; ADR of expert endoscopists, 42.3% vs 32.8%; ADR of nonexpert endoscopists, 37.5% vs 32.1%; and adenomas per colonoscopy, 0.59 vs 0.45, respectively.
The authors concluded that “AI-assisted colonoscopy improved overall ADR, advanced ADR, and ADR of both expert and nonexpert attending endoscopists.”
Improving the Algorithms
Experts agree that current and future research will improve the accuracy and quality of AI colonoscopy for all users, leading to new standards and more consistent outcomes in both clinical trials and real-world applications.
Work underway now to improve the algorithms will be an important step in that direction, according to Dr. Christie.
“We need to have enough information to create AI algorithms that allow us to detect early lesions, at least from an imaging standpoint, and we need to improve and increase the sensitivity and the specificity, as well as the predictive value,” she said.
AI can also play a role in health equity, she noted.
“But it’s a double-edged sword, because it depends again on algorithms and machine learning. Perhaps AI can eliminate some of the bias in our clinical decision-making. However, if we don’t train the machine properly with a good, diverse sample of patients and figure out how to integrate some of the social determinants of health that a computer may not otherwise consider, it can create larger disparities and larger biases. AI devices can only be as good and as inclusive as we make them,” Dr. Christie said.
Looking Ahead
Dr. Sharma predicts that “the next slew of studies are going to be on characterization — not just saying there’s an abnormality but distinguishing it further and saying whether the lesion is noncancerous, precancerous, or cancer.”
Other studies will focus on quality improvement of factors, such as withdrawal time and bowel preparation.
In its clinical practice update on AI, the American Gastroenterological Association states, “Eventually, we predict an AI suite of tools for colonoscopy will seem indispensable, as a powerful adjunct to support safe and efficient clinical practice. AI tools that improve colonoscopy quality may become more accepted, and perhaps demanded, by payors, administrators, and possibly even by well-informed patients who want to ensure the highest-quality examination of their colon.”
Dr. Sharma and Dr. Christie disclose no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Recurrent Bleeding in Small-Intestinal Angiodysplasia Reduced by Thalidomide
, according to results of a new placebo-controlled trial.
At 1 year follow-up, thalidomide doses of 100 mg/day and 50 mg/day outperformed placebo in reducing by at least 50% the number of bleeding episodes, compared with the year prior to treatment, according to the study published online in the New England Journal of Medicine.
SIA, an increasingly recognized cause of repeat obscure gastrointestinal bleeding and iron-deficiency anemia, is a distinct vascular abnormality in the mucosa and submucosa characterized by focal accumulation of ectatic vessels. It is the most common cause of small intestine bleeding, especially among patients older than 50.
There is a high unmet need among patients with SIA for an effective and relatively safe oral medication, given substantial recurrent bleeding risks following endoscopic or surgical procedures, and only observational studies suggest treatment with somatostatin and octreotide, noted senior author Zhizheng Ge, MD, Shanghai Jiao Tong University, Shanghai, China.
SIA is characterized by dilated and tortuous arterial or venous capillaries between thin-walled and immature veins and capillaries without a smooth-muscle layer. Its pathologic process involves chronic hypoxia and vessel sprouting.
Dr. Ge and colleagues postulated that thalidomide’s ability to decrease the expression of proangiogenic factors and angiogenesis would have a long-lasting ameliorating effect on bleeding episodes of angiodysplasia, and thus a continued benefit with respect to bleeding cessation. Their previous small, single-center, open-label, randomized controlled trial of thalidomide for SIA showed a benefit, but it required larger confirmatory trials.
For their current trial, the researchers explored whether a short treatment period, selected to avoid treatment nonadherence, could have a long-term effect. They randomly assigned on a 1:1:1 basis 150 patients with recurrent SIA-related bleeding, defined as at least four episodes during the previous year, to an oral daily dose of 100 mg of thalidomide, 50 mg of thalidomide, or placebo for 4 months.
The patients (median age, 62.2 years; 88% aged 50 years or older) were followed for at least 1 year after treatment. The trial was conducted at 10 sites in China.
The primary endpoint was effective response, defined as a reduction of at least 50% in the number of bleeding episodes in the year following thalidomide treatment, compared with the number in the year before treatment. Bleeding was defined as the presence of overt bleeding or a positive fecal occult blood test.
The percentages of patients with effective response at 1-year follow-up were 68.6% in the 100-mg thalidomide group, 51% in the 50-mg thalidomide group, and 16% in the placebo group.
Among secondary endpoints, the incidence of rebleeding during the 4-month treatment period was 27.5% (14 of 51 patients) in the 100-mg thalidomide group, 42.9% (21 of 49 patients) in the 50-mg thalidomide group, and 90% (45 of 50 patients) in the placebo group. The percentage of patients who received a blood transfusion during the 1-year follow-up period were 17.6% in the 100-mg thalidomide group, 24.5% in the 50-mg thalidomide group, and 62% in the placebo group.
Cessation of bleeding, defined by two consecutive negative fecal occult blood tests on different days, during 1 year of follow-up was observed in 44 patients: 26 (51%) of patients in the 100-mg thalidomide group, 16 (32.7%) in the 50-mg thalidomide group, and 2 (4%) in the placebo group. The authors urge further exploration of the duration of benefit and the efficacy of longer courses of treatment.
Adverse events, all grade 1 or 2, resolved after treatment of symptoms, completion of treatment, or discontinuation of thalidomide or placebo.
Retreatment May Be Necessary
In an accompanying editorial, Loren Laine, MD, chief of the section of digestive diseases, internal medicine, and medical chief, digestive health, Yale School of Medicine, New Haven, Connecticut, affirmed the authors’ conclusions and commended the quality of evidence they provided.
“Their results suggest that thalidomide may be disease-modifying, with efficacy persisting after discontinuation,” wrote Dr. Laine, also a Yale professor of medicine and digestive diseases.
While thalidomide effectively prevented rebleeding for 42 patients during the year after therapy was stopped, suggesting an alteration of angiodysplasias, rebleeding during the subsequent 3-27 months occurred among 20 of those patients, Dr. Laine noted. That finding, “suggests that retreatment will be needed,” although the appropriate duration of treatment before retreatment and the duration of retreatment remain unclear, he added.
The study’s reliance on bleeding episodes that were defined by positive fecal occult blood tests, which may be clinically unimportant, is a weakness in the trial, Dr. Laine wrote.
Despite the study’s positive findings, clinicians may still prefer somatostatin analogues because of their potential for better safety and, with once-monthly injections versus daily thalidomide pills, their likelihood for better adherence, Dr. Laine wrote. “[They] will reserve thalidomide for use in patients who have continued bleeding or side effects with somatostatin analogues,” he added.
Somatostatin is rarely used in the treatment of SIA bleeding in China, where thalidomide is relatively easy to obtain and is being used clinically, Dr. Ge told this news organization in response to Dr. Laine’s editorial. “The clinical application of thalidomide has been taken up in other [Chinese] hospitals that have seen our research,” he added.
Future research may include randomized controlled trials of somatostatin, since Chinese experience with it is so limited, Dr. Ge said. “We would want to compare efficacy, safety, feasibility and cost-effectiveness between somatostatin and thalidomide,” he added.
The study was supported by grants from the National Natural Science Foundation of China and a grant from the Shanghai Municipal Education Commission, Gaofeng Clinical Medicine. The author disclosures can be found with the original article.
, according to results of a new placebo-controlled trial.
At 1 year follow-up, thalidomide doses of 100 mg/day and 50 mg/day outperformed placebo in reducing by at least 50% the number of bleeding episodes, compared with the year prior to treatment, according to the study published online in the New England Journal of Medicine.
SIA, an increasingly recognized cause of repeat obscure gastrointestinal bleeding and iron-deficiency anemia, is a distinct vascular abnormality in the mucosa and submucosa characterized by focal accumulation of ectatic vessels. It is the most common cause of small intestine bleeding, especially among patients older than 50.
There is a high unmet need among patients with SIA for an effective and relatively safe oral medication, given substantial recurrent bleeding risks following endoscopic or surgical procedures, and only observational studies suggest treatment with somatostatin and octreotide, noted senior author Zhizheng Ge, MD, Shanghai Jiao Tong University, Shanghai, China.
SIA is characterized by dilated and tortuous arterial or venous capillaries between thin-walled and immature veins and capillaries without a smooth-muscle layer. Its pathologic process involves chronic hypoxia and vessel sprouting.
Dr. Ge and colleagues postulated that thalidomide’s ability to decrease the expression of proangiogenic factors and angiogenesis would have a long-lasting ameliorating effect on bleeding episodes of angiodysplasia, and thus a continued benefit with respect to bleeding cessation. Their previous small, single-center, open-label, randomized controlled trial of thalidomide for SIA showed a benefit, but it required larger confirmatory trials.
For their current trial, the researchers explored whether a short treatment period, selected to avoid treatment nonadherence, could have a long-term effect. They randomly assigned on a 1:1:1 basis 150 patients with recurrent SIA-related bleeding, defined as at least four episodes during the previous year, to an oral daily dose of 100 mg of thalidomide, 50 mg of thalidomide, or placebo for 4 months.
The patients (median age, 62.2 years; 88% aged 50 years or older) were followed for at least 1 year after treatment. The trial was conducted at 10 sites in China.
The primary endpoint was effective response, defined as a reduction of at least 50% in the number of bleeding episodes in the year following thalidomide treatment, compared with the number in the year before treatment. Bleeding was defined as the presence of overt bleeding or a positive fecal occult blood test.
The percentages of patients with effective response at 1-year follow-up were 68.6% in the 100-mg thalidomide group, 51% in the 50-mg thalidomide group, and 16% in the placebo group.
Among secondary endpoints, the incidence of rebleeding during the 4-month treatment period was 27.5% (14 of 51 patients) in the 100-mg thalidomide group, 42.9% (21 of 49 patients) in the 50-mg thalidomide group, and 90% (45 of 50 patients) in the placebo group. The percentage of patients who received a blood transfusion during the 1-year follow-up period were 17.6% in the 100-mg thalidomide group, 24.5% in the 50-mg thalidomide group, and 62% in the placebo group.
Cessation of bleeding, defined by two consecutive negative fecal occult blood tests on different days, during 1 year of follow-up was observed in 44 patients: 26 (51%) of patients in the 100-mg thalidomide group, 16 (32.7%) in the 50-mg thalidomide group, and 2 (4%) in the placebo group. The authors urge further exploration of the duration of benefit and the efficacy of longer courses of treatment.
Adverse events, all grade 1 or 2, resolved after treatment of symptoms, completion of treatment, or discontinuation of thalidomide or placebo.
Retreatment May Be Necessary
In an accompanying editorial, Loren Laine, MD, chief of the section of digestive diseases, internal medicine, and medical chief, digestive health, Yale School of Medicine, New Haven, Connecticut, affirmed the authors’ conclusions and commended the quality of evidence they provided.
“Their results suggest that thalidomide may be disease-modifying, with efficacy persisting after discontinuation,” wrote Dr. Laine, also a Yale professor of medicine and digestive diseases.
While thalidomide effectively prevented rebleeding for 42 patients during the year after therapy was stopped, suggesting an alteration of angiodysplasias, rebleeding during the subsequent 3-27 months occurred among 20 of those patients, Dr. Laine noted. That finding, “suggests that retreatment will be needed,” although the appropriate duration of treatment before retreatment and the duration of retreatment remain unclear, he added.
The study’s reliance on bleeding episodes that were defined by positive fecal occult blood tests, which may be clinically unimportant, is a weakness in the trial, Dr. Laine wrote.
Despite the study’s positive findings, clinicians may still prefer somatostatin analogues because of their potential for better safety and, with once-monthly injections versus daily thalidomide pills, their likelihood for better adherence, Dr. Laine wrote. “[They] will reserve thalidomide for use in patients who have continued bleeding or side effects with somatostatin analogues,” he added.
Somatostatin is rarely used in the treatment of SIA bleeding in China, where thalidomide is relatively easy to obtain and is being used clinically, Dr. Ge told this news organization in response to Dr. Laine’s editorial. “The clinical application of thalidomide has been taken up in other [Chinese] hospitals that have seen our research,” he added.
Future research may include randomized controlled trials of somatostatin, since Chinese experience with it is so limited, Dr. Ge said. “We would want to compare efficacy, safety, feasibility and cost-effectiveness between somatostatin and thalidomide,” he added.
The study was supported by grants from the National Natural Science Foundation of China and a grant from the Shanghai Municipal Education Commission, Gaofeng Clinical Medicine. The author disclosures can be found with the original article.
, according to results of a new placebo-controlled trial.
At 1 year follow-up, thalidomide doses of 100 mg/day and 50 mg/day outperformed placebo in reducing by at least 50% the number of bleeding episodes, compared with the year prior to treatment, according to the study published online in the New England Journal of Medicine.
SIA, an increasingly recognized cause of repeat obscure gastrointestinal bleeding and iron-deficiency anemia, is a distinct vascular abnormality in the mucosa and submucosa characterized by focal accumulation of ectatic vessels. It is the most common cause of small intestine bleeding, especially among patients older than 50.
There is a high unmet need among patients with SIA for an effective and relatively safe oral medication, given substantial recurrent bleeding risks following endoscopic or surgical procedures, and only observational studies suggest treatment with somatostatin and octreotide, noted senior author Zhizheng Ge, MD, Shanghai Jiao Tong University, Shanghai, China.
SIA is characterized by dilated and tortuous arterial or venous capillaries between thin-walled and immature veins and capillaries without a smooth-muscle layer. Its pathologic process involves chronic hypoxia and vessel sprouting.
Dr. Ge and colleagues postulated that thalidomide’s ability to decrease the expression of proangiogenic factors and angiogenesis would have a long-lasting ameliorating effect on bleeding episodes of angiodysplasia, and thus a continued benefit with respect to bleeding cessation. Their previous small, single-center, open-label, randomized controlled trial of thalidomide for SIA showed a benefit, but it required larger confirmatory trials.
For their current trial, the researchers explored whether a short treatment period, selected to avoid treatment nonadherence, could have a long-term effect. They randomly assigned on a 1:1:1 basis 150 patients with recurrent SIA-related bleeding, defined as at least four episodes during the previous year, to an oral daily dose of 100 mg of thalidomide, 50 mg of thalidomide, or placebo for 4 months.
The patients (median age, 62.2 years; 88% aged 50 years or older) were followed for at least 1 year after treatment. The trial was conducted at 10 sites in China.
The primary endpoint was effective response, defined as a reduction of at least 50% in the number of bleeding episodes in the year following thalidomide treatment, compared with the number in the year before treatment. Bleeding was defined as the presence of overt bleeding or a positive fecal occult blood test.
The percentages of patients with effective response at 1-year follow-up were 68.6% in the 100-mg thalidomide group, 51% in the 50-mg thalidomide group, and 16% in the placebo group.
Among secondary endpoints, the incidence of rebleeding during the 4-month treatment period was 27.5% (14 of 51 patients) in the 100-mg thalidomide group, 42.9% (21 of 49 patients) in the 50-mg thalidomide group, and 90% (45 of 50 patients) in the placebo group. The percentage of patients who received a blood transfusion during the 1-year follow-up period were 17.6% in the 100-mg thalidomide group, 24.5% in the 50-mg thalidomide group, and 62% in the placebo group.
Cessation of bleeding, defined by two consecutive negative fecal occult blood tests on different days, during 1 year of follow-up was observed in 44 patients: 26 (51%) of patients in the 100-mg thalidomide group, 16 (32.7%) in the 50-mg thalidomide group, and 2 (4%) in the placebo group. The authors urge further exploration of the duration of benefit and the efficacy of longer courses of treatment.
Adverse events, all grade 1 or 2, resolved after treatment of symptoms, completion of treatment, or discontinuation of thalidomide or placebo.
Retreatment May Be Necessary
In an accompanying editorial, Loren Laine, MD, chief of the section of digestive diseases, internal medicine, and medical chief, digestive health, Yale School of Medicine, New Haven, Connecticut, affirmed the authors’ conclusions and commended the quality of evidence they provided.
“Their results suggest that thalidomide may be disease-modifying, with efficacy persisting after discontinuation,” wrote Dr. Laine, also a Yale professor of medicine and digestive diseases.
While thalidomide effectively prevented rebleeding for 42 patients during the year after therapy was stopped, suggesting an alteration of angiodysplasias, rebleeding during the subsequent 3-27 months occurred among 20 of those patients, Dr. Laine noted. That finding, “suggests that retreatment will be needed,” although the appropriate duration of treatment before retreatment and the duration of retreatment remain unclear, he added.
The study’s reliance on bleeding episodes that were defined by positive fecal occult blood tests, which may be clinically unimportant, is a weakness in the trial, Dr. Laine wrote.
Despite the study’s positive findings, clinicians may still prefer somatostatin analogues because of their potential for better safety and, with once-monthly injections versus daily thalidomide pills, their likelihood for better adherence, Dr. Laine wrote. “[They] will reserve thalidomide for use in patients who have continued bleeding or side effects with somatostatin analogues,” he added.
Somatostatin is rarely used in the treatment of SIA bleeding in China, where thalidomide is relatively easy to obtain and is being used clinically, Dr. Ge told this news organization in response to Dr. Laine’s editorial. “The clinical application of thalidomide has been taken up in other [Chinese] hospitals that have seen our research,” he added.
Future research may include randomized controlled trials of somatostatin, since Chinese experience with it is so limited, Dr. Ge said. “We would want to compare efficacy, safety, feasibility and cost-effectiveness between somatostatin and thalidomide,” he added.
The study was supported by grants from the National Natural Science Foundation of China and a grant from the Shanghai Municipal Education Commission, Gaofeng Clinical Medicine. The author disclosures can be found with the original article.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Caring for LGBTQ+ Patients with IBD
Cases
Patient 1: 55-year-old cis-male, who identifies as gay, has ulcerative colitis that has been refractory to multiple biologic therapies. His provider recommends a total proctocolectomy with ileal pouch anal anastomosis (TPC with IPAA), but the patient has questions regarding sexual function following surgery. Specifically, he is wondering when, or if, he can resume receptive anal intercourse. How would you counsel him?
Patient 2: 25-year-old, trans-female, status-post vaginoplasty with use of sigmoid colon and with well-controlled ulcerative colitis, presents with vaginal discharge, weight loss, and rectal bleeding. How do you explain what has happened to her? During your discussion, she also asks you why her chart continues to use her “dead name.” How do you respond?
Patient 3: 32-year-old, cis-female, G2P2, who identifies as a lesbian, has active ulcerative colitis. She wants to discuss medical or surgical therapy and future pregnancies. How would you counsel her?
Many gastroenterologists would likely know how to address patient 3’s concerns, but the concerns of patients 1 and 2 often go unaddressed or dismissed. Numerous studies and surveys have been conducted on patients with inflammatory bowel disease (IBD), but the focus of these studies has always been through a heteronormative cisgender lens. The focus of many studies is on fertility or sexual health and function in cisgender, heteronormative individuals.1-3 In the last few years, however, there has been increasing awareness of the health disparities, stigma, and discrimination that sexual and gender minorities (SGM) experience.4-6 For the purposes of this discussion, individuals within the lesbian, gay, bisexual, transgender, queer/questioning, intersex, and asexual (LGBTQIA+) community will be referred to as SGM. We recognize that even this exhaustive listing above does not acknowledge the full spectrum of diversity within the SGM community.
Clinical Care/Competency for SGM with IBD is Lacking
Almost 10% of the US population identifies as some form of SGM, and that number can be higher within the younger generations.4 SGM patients tend to delay or avoid seeking health care due to concern for provider mistreatment or lack of regard for their individual concerns. Additionally, there are several gaps in clinical knowledge about caring for SGM individuals. Little is known regarding the incidence or prevalence of IBD in SGM populations, but it is perceived to be similar to cisgender heterosexual individuals. Furthermore, as Newman et al. highlighted in their systematic review published in May 2023, there is a lack of guidance regarding sexual activity in the setting of IBD in SGM individuals.5 There is also a significant lack of knowledge on the impact of gender-affirming care on the natural history and treatments of IBD in transgender and gender non-conforming (TGNC) individuals. This can impact providers’ comfort and competence in caring for TGNC individuals.
Another important point to make is that the SGM community still faces discrimination due to sexual orientation or gender identity to this day, which impacts the quality and delivery of their care.7 Culturally-competent care should include care that is free from stigma, implicit and explicit biases, and discrimination. In 2011, an Institute of Medicine report documented, among other issues, provider discomfort in delivering care to SGM patients.8 While SGM individuals prefer a provider who acknowledges their sexual orientation and gender identity and treats them with the dignity and respect they deserve, many SGM individuals share valid concerns regarding their safety, which impact their desire to disclose their identity to health care providers.9 This certainly can have an impact on the quality of care they receive, including important health maintenance milestones and cancer screenings.10
An internal survey at our institution of providers (nurses, physician assistants, surgeons, and physicians) found that among 85 responders, 70% have cared for SGM who have undergone TPC with ileal pouch anal anastomosis (IPAA). Of these, 75% did not ask about sexual orientation or practices before pouch formation (though almost all of them agreed it would be important to ask). A total of 55% were comfortable in discussing SGM-related concerns; 53% did not feel comfortable discussing sexual orientation or practices; and in particular when it came to anoreceptive intercourse (ARI), 73% did not feel confident discussing recommendations.11
All of these issues highlight the importance of developing curricula that focus on reducing implicit and explicit biases towards SGM individuals and increasing the competence of providers to take care of SGM individuals in a safe space.
Additionally, it further justifies the need for ethical research that focuses on the needs of SGM individuals to guide evidence-based approaches to care. Given the implicit and explicit heterosexism and transphobia in society and many health care systems, Rainbows in Gastro was formed as an advocacy group for SGM patients, trainees, and staff in gastroenterology and hepatology.4
Research in SGM and IBD is lacking
There are additional needs for research in IBD and how it pertains to the needs of SGM individuals. Figure 1 highlights the lack of PubMed results for the search terms “IBD + LGBT,” “IBD + LGBTQ,” or “IBD + queer.” In contrast, the search terms “IBD + fertility” and “IBD + sexual dysfunction” generate many results. Even a systemic review conducted by Newman et al. of multiple databases in 2022 found only seven articles that demonstrated appropriately performed studies on SGM patients with IBD.5 This highlights the significant dearth of research in the realm of SGM health in IBD.
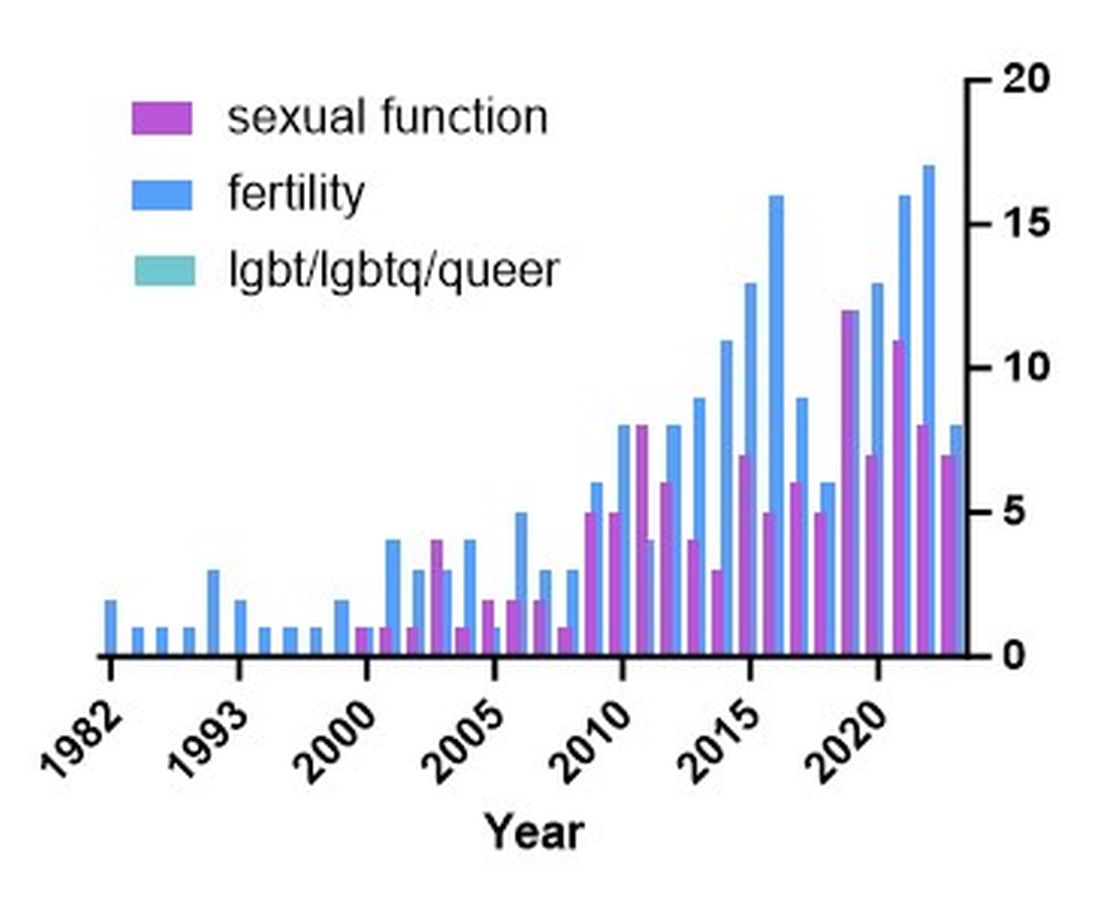
Newman and colleagues have recently published research considerations for SGM individuals. They highlighted the need to include understanding the “unique combination of psychosocial, biomedical, and legal experiences” that results in different needs and outcomes. There were several areas identified, including minority stress, which comes from existence of being SGM, especially as transgender individuals face increasing legal challenges in a variety of settings, not just healthcare.6 In a retrospective chart review investigating social determinants of health in SGM-IBD populations,12 36% of patients reported some level of social isolation, and almost 50% reported some level of stress. A total of 40% of them self-reported some perceived level of risk with respect to employment, and 17% reported depression. Given that this was a chart review and not a strict questionnaire, this study was certainly limited, and we would hypothesize that these numbers are therefore underestimating the true proportion of SGM-IBD patients who deal with employment concerns, social isolation, or psychological distress.
What Next? Back to the Patients
Circling back to our patients from the introduction, how would you counsel each of them? In patient 1’s case, we would inform him that pelvic surgery can increase the risk for sexual dysfunction, such as erectile dysfunction. He additionally would be advised during a staged TPC with IPAA, he may experience issues with body image. However, should he desire to participate in receptive anal intercourse after completion of his surgeries, the general recommendation would be to wait at least 6 months and with proven remission. It should further be noted that these are not formalized recommendations, only highlighting the need for more research and consensus on standards of care for SGM patients. He should finally be told that because he has ulcerative colitis, removal of the colon does not remove the risk for future intestinal involvement such as possible pouchitis.
In patient 2’s case, she is likely experiencing diversion vaginitis related to use of her colon for her neo-vagina. She should undergo colonoscopy and vaginoscopy in addition to standard work-up for her known ulcerative colitis.13 Management should be done in a multidisciplinary approach between the IBD provider, gynecologist, and gender-affirming provider. The electronic medical record should be updated to reflect the patient’s preferred name, pronouns, and gender identity, and her medical records, including automated clinical reports, should be updated accordingly.
As for patient 3, she would be counseled according to well-documented guidelines on pregnancy and IBD, including risks of medications (such as Jak inhibitors or methotrexate) versus the risk of uncontrolled IBD during pregnancy.1
Regardless of a patient’s gender identity or sexual orientation, patient-centered, culturally competent, and sensitive care should be provided. At Mayo Clinic in Rochester, we started one of the first Pride in IBD Clinics, which focuses on the care of SGM individuals with IBD. Our focus is to address the needs of patients who belong to the SGM community in a wholistic approach within a safe space (https://www.youtube.com/watch?v=pYa_zYaCA6M; https://www.mayoclinic.org/departments-centers/inflammatory-bowel-disease-clinic/overview/ovc-20357763). Our process of developing the clinic included training all staff on proper communication and cultural sensitivity for the SGM community.
Furthermore, providing welcoming and affirming signs of inclusivity for SGM individuals at the provider’s office — including but not limited to rainbow progressive flags, gender-neutral bathroom signs, or pronoun pins on provider identification badges (see Figure 2) — are usually appreciated by patients. Ensuring that patient education materials do not assume gender (for example, using the term “parents” rather than “mother and father”) and using gender neutral terms on intake forms is very important. Inclusive communication includes providers introducing themselves by preferred name and pronouns, asking the patients to introduce themselves, and welcoming them to share their pronouns. These simple actions can provide an atmosphere of safety for SGM patients, which would serve to enhance the quality of care we can provide for them.
For Resources and Further Reading: CDC,14 the Fenway Institute’s National LGBTQIA+ Health Education Center,15 and US Department of Health and Human Services.16
Dr. Chiang and Dr. Chedid are both in the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota. Dr. Chedid is also with the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic. Neither of the authors have any relevant conflicts of interest. They are on X, formerly Twitter: @dr_davidchiang , @VictorChedidMD .
CITATIONS
1. Mahadevan U et al. Inflammatory bowel disease in pregnancy clinical care pathway: A report from the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology. 2019;156:1508-24.
2. Pires F et al. A survey on the impact of IBD in sexual health: Into intimacy. Medicine (Baltimore). 2022;101:e32279.
3. Mules TC et al. The impact of disease activity on sexual and erectile dysfunction in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2023;29:1244-54.
4. Duong N et al. Overcoming disparities for sexual and gender minority patients and providers in gastroenterology and hepatology: Introduction to Rainbows in Gastro. Lancet Gastroenterol Hepatol. 2023;8:299-301.
5. Newman KL et al. A systematic review of inflammatory bowel disease epidemiology and health outcomes in sexual and gender minority individuals. Gastroenterology. 2023;164:866-71.
6. Newman KL et al. Research considerations in Digestive and liver disease in transgender and gender-diverse populations. Gastroenterology. 2023;165:523-28 e1.
7. Velez C et al. Digestive health in sexual and gender minority populations. Am J Gastroenterol. 2022;117:865-75.
8. Medicine Io. Washington (DC): The National Academies Press, 2011.
9. Austin EL. Sexual orientation disclosure to health care providers among urban and non-urban southern lesbians. Women Health. 2013;53:41-55.
10. Oladeru OT et al. Breast and cervical cancer screening disparities in transgender people. Am J Clin Oncol. 2022;45:116-21.
11. Vinsard DG et al. Healthcare providers’ perspectives on anoreceptive intercourse in sexual and gender minorities with ileal pouch anal anastomosis. Digestive Disease Week (DDW). Chicago, IL, 2023.
12. Ghusn W et al. Social determinants of health in LGBTQIA+ patients with inflammatory bowel disease. American College of Gastroenterology (ACG). Charlotte, NC, 2022.
13. Grasman ME et al. Neovaginal sparing in a transgender woman with ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14:e73-4.
14. Prevention CfDCa. Lesbian, Gay, Bisexual, and Transgender Health — https://www.cdc.gov/lgbthealth/index.htm.
15. Institute TF. National LGBTQIA+ Health Education Center — https://www.lgbtqiahealtheducation.org/.
16. Services UDoHaH. LGBTQI+ Resources — https://www.hhs.gov/programs/topic-sites/lgbtqi/resources/index.html.
Cases
Patient 1: 55-year-old cis-male, who identifies as gay, has ulcerative colitis that has been refractory to multiple biologic therapies. His provider recommends a total proctocolectomy with ileal pouch anal anastomosis (TPC with IPAA), but the patient has questions regarding sexual function following surgery. Specifically, he is wondering when, or if, he can resume receptive anal intercourse. How would you counsel him?
Patient 2: 25-year-old, trans-female, status-post vaginoplasty with use of sigmoid colon and with well-controlled ulcerative colitis, presents with vaginal discharge, weight loss, and rectal bleeding. How do you explain what has happened to her? During your discussion, she also asks you why her chart continues to use her “dead name.” How do you respond?
Patient 3: 32-year-old, cis-female, G2P2, who identifies as a lesbian, has active ulcerative colitis. She wants to discuss medical or surgical therapy and future pregnancies. How would you counsel her?
Many gastroenterologists would likely know how to address patient 3’s concerns, but the concerns of patients 1 and 2 often go unaddressed or dismissed. Numerous studies and surveys have been conducted on patients with inflammatory bowel disease (IBD), but the focus of these studies has always been through a heteronormative cisgender lens. The focus of many studies is on fertility or sexual health and function in cisgender, heteronormative individuals.1-3 In the last few years, however, there has been increasing awareness of the health disparities, stigma, and discrimination that sexual and gender minorities (SGM) experience.4-6 For the purposes of this discussion, individuals within the lesbian, gay, bisexual, transgender, queer/questioning, intersex, and asexual (LGBTQIA+) community will be referred to as SGM. We recognize that even this exhaustive listing above does not acknowledge the full spectrum of diversity within the SGM community.
Clinical Care/Competency for SGM with IBD is Lacking
Almost 10% of the US population identifies as some form of SGM, and that number can be higher within the younger generations.4 SGM patients tend to delay or avoid seeking health care due to concern for provider mistreatment or lack of regard for their individual concerns. Additionally, there are several gaps in clinical knowledge about caring for SGM individuals. Little is known regarding the incidence or prevalence of IBD in SGM populations, but it is perceived to be similar to cisgender heterosexual individuals. Furthermore, as Newman et al. highlighted in their systematic review published in May 2023, there is a lack of guidance regarding sexual activity in the setting of IBD in SGM individuals.5 There is also a significant lack of knowledge on the impact of gender-affirming care on the natural history and treatments of IBD in transgender and gender non-conforming (TGNC) individuals. This can impact providers’ comfort and competence in caring for TGNC individuals.
Another important point to make is that the SGM community still faces discrimination due to sexual orientation or gender identity to this day, which impacts the quality and delivery of their care.7 Culturally-competent care should include care that is free from stigma, implicit and explicit biases, and discrimination. In 2011, an Institute of Medicine report documented, among other issues, provider discomfort in delivering care to SGM patients.8 While SGM individuals prefer a provider who acknowledges their sexual orientation and gender identity and treats them with the dignity and respect they deserve, many SGM individuals share valid concerns regarding their safety, which impact their desire to disclose their identity to health care providers.9 This certainly can have an impact on the quality of care they receive, including important health maintenance milestones and cancer screenings.10
An internal survey at our institution of providers (nurses, physician assistants, surgeons, and physicians) found that among 85 responders, 70% have cared for SGM who have undergone TPC with ileal pouch anal anastomosis (IPAA). Of these, 75% did not ask about sexual orientation or practices before pouch formation (though almost all of them agreed it would be important to ask). A total of 55% were comfortable in discussing SGM-related concerns; 53% did not feel comfortable discussing sexual orientation or practices; and in particular when it came to anoreceptive intercourse (ARI), 73% did not feel confident discussing recommendations.11
All of these issues highlight the importance of developing curricula that focus on reducing implicit and explicit biases towards SGM individuals and increasing the competence of providers to take care of SGM individuals in a safe space.
Additionally, it further justifies the need for ethical research that focuses on the needs of SGM individuals to guide evidence-based approaches to care. Given the implicit and explicit heterosexism and transphobia in society and many health care systems, Rainbows in Gastro was formed as an advocacy group for SGM patients, trainees, and staff in gastroenterology and hepatology.4
Research in SGM and IBD is lacking
There are additional needs for research in IBD and how it pertains to the needs of SGM individuals. Figure 1 highlights the lack of PubMed results for the search terms “IBD + LGBT,” “IBD + LGBTQ,” or “IBD + queer.” In contrast, the search terms “IBD + fertility” and “IBD + sexual dysfunction” generate many results. Even a systemic review conducted by Newman et al. of multiple databases in 2022 found only seven articles that demonstrated appropriately performed studies on SGM patients with IBD.5 This highlights the significant dearth of research in the realm of SGM health in IBD.
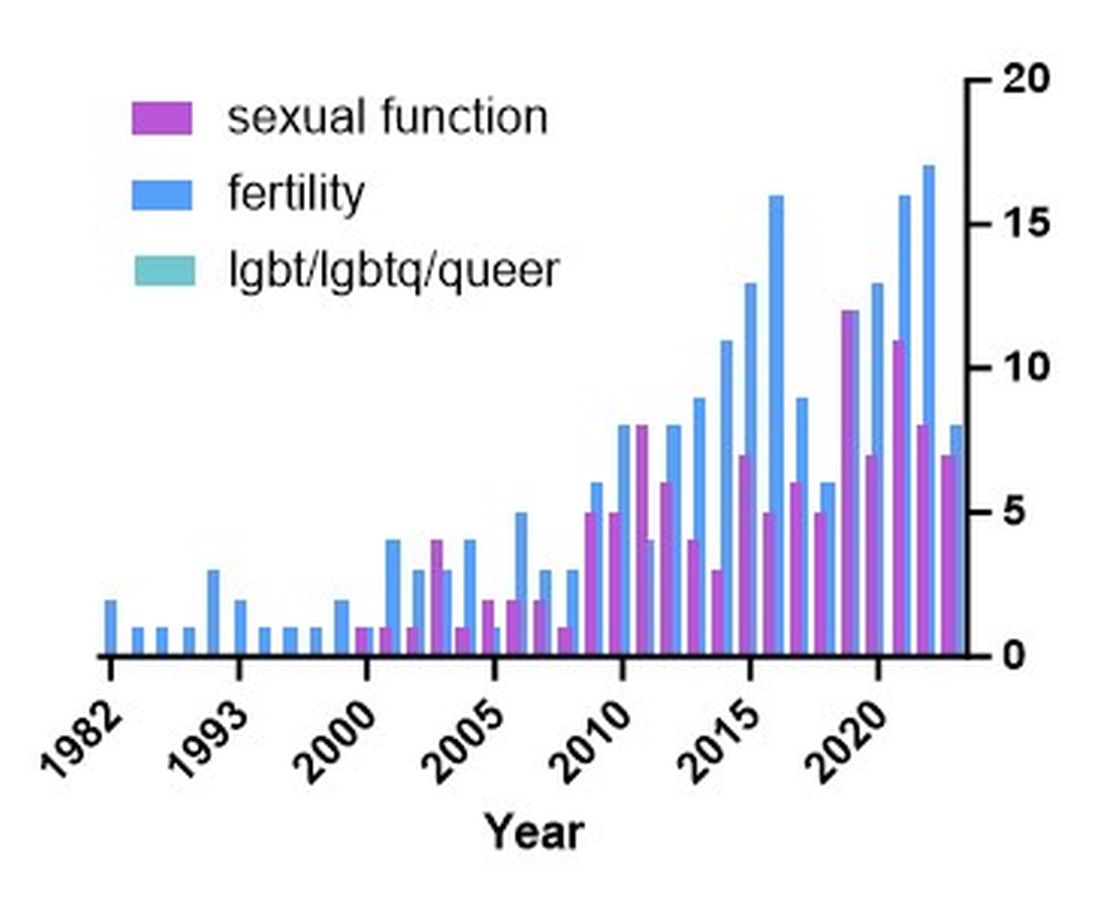
Newman and colleagues have recently published research considerations for SGM individuals. They highlighted the need to include understanding the “unique combination of psychosocial, biomedical, and legal experiences” that results in different needs and outcomes. There were several areas identified, including minority stress, which comes from existence of being SGM, especially as transgender individuals face increasing legal challenges in a variety of settings, not just healthcare.6 In a retrospective chart review investigating social determinants of health in SGM-IBD populations,12 36% of patients reported some level of social isolation, and almost 50% reported some level of stress. A total of 40% of them self-reported some perceived level of risk with respect to employment, and 17% reported depression. Given that this was a chart review and not a strict questionnaire, this study was certainly limited, and we would hypothesize that these numbers are therefore underestimating the true proportion of SGM-IBD patients who deal with employment concerns, social isolation, or psychological distress.
What Next? Back to the Patients
Circling back to our patients from the introduction, how would you counsel each of them? In patient 1’s case, we would inform him that pelvic surgery can increase the risk for sexual dysfunction, such as erectile dysfunction. He additionally would be advised during a staged TPC with IPAA, he may experience issues with body image. However, should he desire to participate in receptive anal intercourse after completion of his surgeries, the general recommendation would be to wait at least 6 months and with proven remission. It should further be noted that these are not formalized recommendations, only highlighting the need for more research and consensus on standards of care for SGM patients. He should finally be told that because he has ulcerative colitis, removal of the colon does not remove the risk for future intestinal involvement such as possible pouchitis.
In patient 2’s case, she is likely experiencing diversion vaginitis related to use of her colon for her neo-vagina. She should undergo colonoscopy and vaginoscopy in addition to standard work-up for her known ulcerative colitis.13 Management should be done in a multidisciplinary approach between the IBD provider, gynecologist, and gender-affirming provider. The electronic medical record should be updated to reflect the patient’s preferred name, pronouns, and gender identity, and her medical records, including automated clinical reports, should be updated accordingly.
As for patient 3, she would be counseled according to well-documented guidelines on pregnancy and IBD, including risks of medications (such as Jak inhibitors or methotrexate) versus the risk of uncontrolled IBD during pregnancy.1
Regardless of a patient’s gender identity or sexual orientation, patient-centered, culturally competent, and sensitive care should be provided. At Mayo Clinic in Rochester, we started one of the first Pride in IBD Clinics, which focuses on the care of SGM individuals with IBD. Our focus is to address the needs of patients who belong to the SGM community in a wholistic approach within a safe space (https://www.youtube.com/watch?v=pYa_zYaCA6M; https://www.mayoclinic.org/departments-centers/inflammatory-bowel-disease-clinic/overview/ovc-20357763). Our process of developing the clinic included training all staff on proper communication and cultural sensitivity for the SGM community.
Furthermore, providing welcoming and affirming signs of inclusivity for SGM individuals at the provider’s office — including but not limited to rainbow progressive flags, gender-neutral bathroom signs, or pronoun pins on provider identification badges (see Figure 2) — are usually appreciated by patients. Ensuring that patient education materials do not assume gender (for example, using the term “parents” rather than “mother and father”) and using gender neutral terms on intake forms is very important. Inclusive communication includes providers introducing themselves by preferred name and pronouns, asking the patients to introduce themselves, and welcoming them to share their pronouns. These simple actions can provide an atmosphere of safety for SGM patients, which would serve to enhance the quality of care we can provide for them.
For Resources and Further Reading: CDC,14 the Fenway Institute’s National LGBTQIA+ Health Education Center,15 and US Department of Health and Human Services.16
Dr. Chiang and Dr. Chedid are both in the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota. Dr. Chedid is also with the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic. Neither of the authors have any relevant conflicts of interest. They are on X, formerly Twitter: @dr_davidchiang , @VictorChedidMD .
CITATIONS
1. Mahadevan U et al. Inflammatory bowel disease in pregnancy clinical care pathway: A report from the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology. 2019;156:1508-24.
2. Pires F et al. A survey on the impact of IBD in sexual health: Into intimacy. Medicine (Baltimore). 2022;101:e32279.
3. Mules TC et al. The impact of disease activity on sexual and erectile dysfunction in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2023;29:1244-54.
4. Duong N et al. Overcoming disparities for sexual and gender minority patients and providers in gastroenterology and hepatology: Introduction to Rainbows in Gastro. Lancet Gastroenterol Hepatol. 2023;8:299-301.
5. Newman KL et al. A systematic review of inflammatory bowel disease epidemiology and health outcomes in sexual and gender minority individuals. Gastroenterology. 2023;164:866-71.
6. Newman KL et al. Research considerations in Digestive and liver disease in transgender and gender-diverse populations. Gastroenterology. 2023;165:523-28 e1.
7. Velez C et al. Digestive health in sexual and gender minority populations. Am J Gastroenterol. 2022;117:865-75.
8. Medicine Io. Washington (DC): The National Academies Press, 2011.
9. Austin EL. Sexual orientation disclosure to health care providers among urban and non-urban southern lesbians. Women Health. 2013;53:41-55.
10. Oladeru OT et al. Breast and cervical cancer screening disparities in transgender people. Am J Clin Oncol. 2022;45:116-21.
11. Vinsard DG et al. Healthcare providers’ perspectives on anoreceptive intercourse in sexual and gender minorities with ileal pouch anal anastomosis. Digestive Disease Week (DDW). Chicago, IL, 2023.
12. Ghusn W et al. Social determinants of health in LGBTQIA+ patients with inflammatory bowel disease. American College of Gastroenterology (ACG). Charlotte, NC, 2022.
13. Grasman ME et al. Neovaginal sparing in a transgender woman with ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14:e73-4.
14. Prevention CfDCa. Lesbian, Gay, Bisexual, and Transgender Health — https://www.cdc.gov/lgbthealth/index.htm.
15. Institute TF. National LGBTQIA+ Health Education Center — https://www.lgbtqiahealtheducation.org/.
16. Services UDoHaH. LGBTQI+ Resources — https://www.hhs.gov/programs/topic-sites/lgbtqi/resources/index.html.
Cases
Patient 1: 55-year-old cis-male, who identifies as gay, has ulcerative colitis that has been refractory to multiple biologic therapies. His provider recommends a total proctocolectomy with ileal pouch anal anastomosis (TPC with IPAA), but the patient has questions regarding sexual function following surgery. Specifically, he is wondering when, or if, he can resume receptive anal intercourse. How would you counsel him?
Patient 2: 25-year-old, trans-female, status-post vaginoplasty with use of sigmoid colon and with well-controlled ulcerative colitis, presents with vaginal discharge, weight loss, and rectal bleeding. How do you explain what has happened to her? During your discussion, she also asks you why her chart continues to use her “dead name.” How do you respond?
Patient 3: 32-year-old, cis-female, G2P2, who identifies as a lesbian, has active ulcerative colitis. She wants to discuss medical or surgical therapy and future pregnancies. How would you counsel her?
Many gastroenterologists would likely know how to address patient 3’s concerns, but the concerns of patients 1 and 2 often go unaddressed or dismissed. Numerous studies and surveys have been conducted on patients with inflammatory bowel disease (IBD), but the focus of these studies has always been through a heteronormative cisgender lens. The focus of many studies is on fertility or sexual health and function in cisgender, heteronormative individuals.1-3 In the last few years, however, there has been increasing awareness of the health disparities, stigma, and discrimination that sexual and gender minorities (SGM) experience.4-6 For the purposes of this discussion, individuals within the lesbian, gay, bisexual, transgender, queer/questioning, intersex, and asexual (LGBTQIA+) community will be referred to as SGM. We recognize that even this exhaustive listing above does not acknowledge the full spectrum of diversity within the SGM community.
Clinical Care/Competency for SGM with IBD is Lacking
Almost 10% of the US population identifies as some form of SGM, and that number can be higher within the younger generations.4 SGM patients tend to delay or avoid seeking health care due to concern for provider mistreatment or lack of regard for their individual concerns. Additionally, there are several gaps in clinical knowledge about caring for SGM individuals. Little is known regarding the incidence or prevalence of IBD in SGM populations, but it is perceived to be similar to cisgender heterosexual individuals. Furthermore, as Newman et al. highlighted in their systematic review published in May 2023, there is a lack of guidance regarding sexual activity in the setting of IBD in SGM individuals.5 There is also a significant lack of knowledge on the impact of gender-affirming care on the natural history and treatments of IBD in transgender and gender non-conforming (TGNC) individuals. This can impact providers’ comfort and competence in caring for TGNC individuals.
Another important point to make is that the SGM community still faces discrimination due to sexual orientation or gender identity to this day, which impacts the quality and delivery of their care.7 Culturally-competent care should include care that is free from stigma, implicit and explicit biases, and discrimination. In 2011, an Institute of Medicine report documented, among other issues, provider discomfort in delivering care to SGM patients.8 While SGM individuals prefer a provider who acknowledges their sexual orientation and gender identity and treats them with the dignity and respect they deserve, many SGM individuals share valid concerns regarding their safety, which impact their desire to disclose their identity to health care providers.9 This certainly can have an impact on the quality of care they receive, including important health maintenance milestones and cancer screenings.10
An internal survey at our institution of providers (nurses, physician assistants, surgeons, and physicians) found that among 85 responders, 70% have cared for SGM who have undergone TPC with ileal pouch anal anastomosis (IPAA). Of these, 75% did not ask about sexual orientation or practices before pouch formation (though almost all of them agreed it would be important to ask). A total of 55% were comfortable in discussing SGM-related concerns; 53% did not feel comfortable discussing sexual orientation or practices; and in particular when it came to anoreceptive intercourse (ARI), 73% did not feel confident discussing recommendations.11
All of these issues highlight the importance of developing curricula that focus on reducing implicit and explicit biases towards SGM individuals and increasing the competence of providers to take care of SGM individuals in a safe space.
Additionally, it further justifies the need for ethical research that focuses on the needs of SGM individuals to guide evidence-based approaches to care. Given the implicit and explicit heterosexism and transphobia in society and many health care systems, Rainbows in Gastro was formed as an advocacy group for SGM patients, trainees, and staff in gastroenterology and hepatology.4
Research in SGM and IBD is lacking
There are additional needs for research in IBD and how it pertains to the needs of SGM individuals. Figure 1 highlights the lack of PubMed results for the search terms “IBD + LGBT,” “IBD + LGBTQ,” or “IBD + queer.” In contrast, the search terms “IBD + fertility” and “IBD + sexual dysfunction” generate many results. Even a systemic review conducted by Newman et al. of multiple databases in 2022 found only seven articles that demonstrated appropriately performed studies on SGM patients with IBD.5 This highlights the significant dearth of research in the realm of SGM health in IBD.
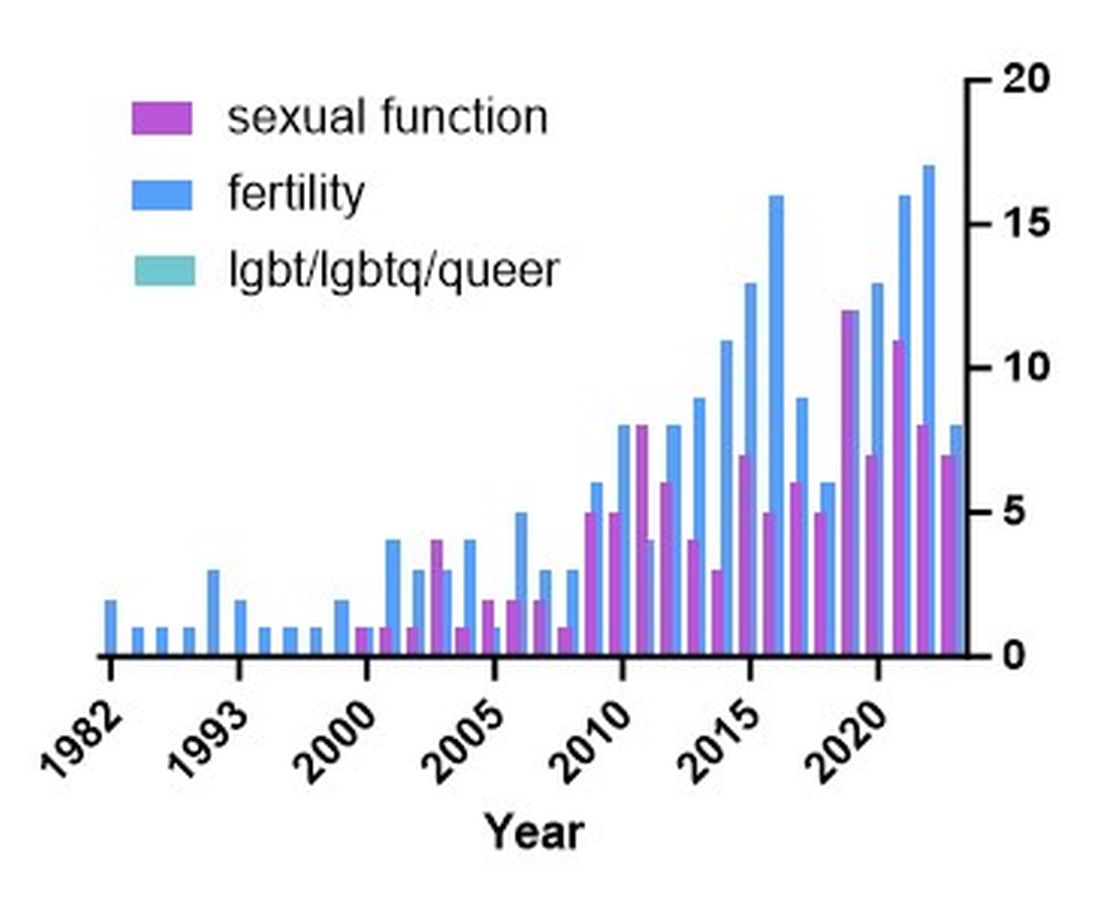
Newman and colleagues have recently published research considerations for SGM individuals. They highlighted the need to include understanding the “unique combination of psychosocial, biomedical, and legal experiences” that results in different needs and outcomes. There were several areas identified, including minority stress, which comes from existence of being SGM, especially as transgender individuals face increasing legal challenges in a variety of settings, not just healthcare.6 In a retrospective chart review investigating social determinants of health in SGM-IBD populations,12 36% of patients reported some level of social isolation, and almost 50% reported some level of stress. A total of 40% of them self-reported some perceived level of risk with respect to employment, and 17% reported depression. Given that this was a chart review and not a strict questionnaire, this study was certainly limited, and we would hypothesize that these numbers are therefore underestimating the true proportion of SGM-IBD patients who deal with employment concerns, social isolation, or psychological distress.
What Next? Back to the Patients
Circling back to our patients from the introduction, how would you counsel each of them? In patient 1’s case, we would inform him that pelvic surgery can increase the risk for sexual dysfunction, such as erectile dysfunction. He additionally would be advised during a staged TPC with IPAA, he may experience issues with body image. However, should he desire to participate in receptive anal intercourse after completion of his surgeries, the general recommendation would be to wait at least 6 months and with proven remission. It should further be noted that these are not formalized recommendations, only highlighting the need for more research and consensus on standards of care for SGM patients. He should finally be told that because he has ulcerative colitis, removal of the colon does not remove the risk for future intestinal involvement such as possible pouchitis.
In patient 2’s case, she is likely experiencing diversion vaginitis related to use of her colon for her neo-vagina. She should undergo colonoscopy and vaginoscopy in addition to standard work-up for her known ulcerative colitis.13 Management should be done in a multidisciplinary approach between the IBD provider, gynecologist, and gender-affirming provider. The electronic medical record should be updated to reflect the patient’s preferred name, pronouns, and gender identity, and her medical records, including automated clinical reports, should be updated accordingly.
As for patient 3, she would be counseled according to well-documented guidelines on pregnancy and IBD, including risks of medications (such as Jak inhibitors or methotrexate) versus the risk of uncontrolled IBD during pregnancy.1
Regardless of a patient’s gender identity or sexual orientation, patient-centered, culturally competent, and sensitive care should be provided. At Mayo Clinic in Rochester, we started one of the first Pride in IBD Clinics, which focuses on the care of SGM individuals with IBD. Our focus is to address the needs of patients who belong to the SGM community in a wholistic approach within a safe space (https://www.youtube.com/watch?v=pYa_zYaCA6M; https://www.mayoclinic.org/departments-centers/inflammatory-bowel-disease-clinic/overview/ovc-20357763). Our process of developing the clinic included training all staff on proper communication and cultural sensitivity for the SGM community.
Furthermore, providing welcoming and affirming signs of inclusivity for SGM individuals at the provider’s office — including but not limited to rainbow progressive flags, gender-neutral bathroom signs, or pronoun pins on provider identification badges (see Figure 2) — are usually appreciated by patients. Ensuring that patient education materials do not assume gender (for example, using the term “parents” rather than “mother and father”) and using gender neutral terms on intake forms is very important. Inclusive communication includes providers introducing themselves by preferred name and pronouns, asking the patients to introduce themselves, and welcoming them to share their pronouns. These simple actions can provide an atmosphere of safety for SGM patients, which would serve to enhance the quality of care we can provide for them.
For Resources and Further Reading: CDC,14 the Fenway Institute’s National LGBTQIA+ Health Education Center,15 and US Department of Health and Human Services.16
Dr. Chiang and Dr. Chedid are both in the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota. Dr. Chedid is also with the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Mayo Clinic. Neither of the authors have any relevant conflicts of interest. They are on X, formerly Twitter: @dr_davidchiang , @VictorChedidMD .
CITATIONS
1. Mahadevan U et al. Inflammatory bowel disease in pregnancy clinical care pathway: A report from the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology. 2019;156:1508-24.
2. Pires F et al. A survey on the impact of IBD in sexual health: Into intimacy. Medicine (Baltimore). 2022;101:e32279.
3. Mules TC et al. The impact of disease activity on sexual and erectile dysfunction in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2023;29:1244-54.
4. Duong N et al. Overcoming disparities for sexual and gender minority patients and providers in gastroenterology and hepatology: Introduction to Rainbows in Gastro. Lancet Gastroenterol Hepatol. 2023;8:299-301.
5. Newman KL et al. A systematic review of inflammatory bowel disease epidemiology and health outcomes in sexual and gender minority individuals. Gastroenterology. 2023;164:866-71.
6. Newman KL et al. Research considerations in Digestive and liver disease in transgender and gender-diverse populations. Gastroenterology. 2023;165:523-28 e1.
7. Velez C et al. Digestive health in sexual and gender minority populations. Am J Gastroenterol. 2022;117:865-75.
8. Medicine Io. Washington (DC): The National Academies Press, 2011.
9. Austin EL. Sexual orientation disclosure to health care providers among urban and non-urban southern lesbians. Women Health. 2013;53:41-55.
10. Oladeru OT et al. Breast and cervical cancer screening disparities in transgender people. Am J Clin Oncol. 2022;45:116-21.
11. Vinsard DG et al. Healthcare providers’ perspectives on anoreceptive intercourse in sexual and gender minorities with ileal pouch anal anastomosis. Digestive Disease Week (DDW). Chicago, IL, 2023.
12. Ghusn W et al. Social determinants of health in LGBTQIA+ patients with inflammatory bowel disease. American College of Gastroenterology (ACG). Charlotte, NC, 2022.
13. Grasman ME et al. Neovaginal sparing in a transgender woman with ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14:e73-4.
14. Prevention CfDCa. Lesbian, Gay, Bisexual, and Transgender Health — https://www.cdc.gov/lgbthealth/index.htm.
15. Institute TF. National LGBTQIA+ Health Education Center — https://www.lgbtqiahealtheducation.org/.
16. Services UDoHaH. LGBTQI+ Resources — https://www.hhs.gov/programs/topic-sites/lgbtqi/resources/index.html.
Real-world evidence: Early ileocecal resection outperforms anti-TNF therapy for Crohn’s disease
These findings add weight to previously reported data from the LIR!C trial, suggesting that ileocecal resection should be considered a first-line treatment option for CD, reported principal investigator Kristine H. Allin, MD, PhD, of Aalborg University, Copenhagen.
“The LIR!C randomized clinical trial has demonstrated comparable quality of life with ileocecal resection and infliximab as a first-line treatment for limited, nonstricturing ileocecal CD at 1 year of follow-up, and improved outcomes with ileocecal resection on retrospective analysis of long-term follow-up data,” the investigators wrote in Gastroenterology. “However, in the real world, the long-term impact of early ileocecal resection for CD, compared with medical therapy, remains largely unexplored.”
To gather these real-world data, the investigators turned to the Danish National Patient Registry and the Danish National Prescription Registry, which included 1,279 individuals diagnosed with CD between 2003 and 2018 who received anti-TNF therapy or underwent ileocecal resection within 1 year of diagnosis. Within this group, slightly less than half underwent ileocecal resection (45.4%) while the remainder (54.6%) received anti-TNF therapy.
The primary outcome was a composite of one or more events: perianal CD, CD-related surgery, systemic corticosteroid exposure, and CD-related hospitalization. Secondary analyses evaluated the relative risks of these same four events as independent entities.
Multifactor-adjusted Cox proportional hazards regression analysis revealed that patients who underwent ileocecal resection had a 33% lower risk of the composite outcome compared with those who received anti-TNF therapy (adjusted hazard ratio [aHR], 0.67; 95% CI, 0.54-0.83).
In the secondary analyses, which examined risks for each component of the composite outcome, the surgery group had a significantly lower risk of CD-related surgery (aHR, 0.56; 95% CI, 0.39-0.80) and corticosteroid exposure (aHR, 0.71; 95% CI, 0.54-0.92), but not perianal CD or CD-related hospitalization.
After 5 years, half of the patients (49.7%) who underwent ileocecal resection were not receiving any treatment for CD. At the same timepoint, a slightly lower percentage of this group (46.3%) had started immunomodulator therapy, while 16.8% started anti-TNF therapy. Just 1.8% of these patients required a second intestinal resection.
“To our knowledge, these are the first real-world data in a population-based cohort with long-term follow-up of early ileocecal resection compared with anti-TNF therapy for newly diagnosed ileal and ileocecal CD,” the investigators wrote. “These data suggest that ileocecal resection may have a role as first-line therapy in Crohn’s disease management and challenge the current paradigm of reserving surgery for complicated Crohn’s disease refractory or intolerant to medications.”
Corresponding author Manasi Agrawal, MD, of Icahn School of Medicine at Mount Sinai, New York, suggested that “validation of our findings in external cohorts [is needed], and understanding of factors associated with improved outcomes following ileocecal resection.”
For clinicians and patients choosing between first-line anti-TNF therapy versus ileocecal resection using currently available evidence, Dr. Agrawal suggested that a variety of factors need to be considered, including disease location, extent of terminal ileum involved, presence of complications such as stricture, fistula, comorbid conditions, access to biologics, financial considerations, and patient preferences.
Benjamin Cohen, MD, staff physician and co-section head and clinical director for inflammatory bowel diseases in the department of gastroenterology, hepatology, and nutrition at Cleveland Clinic, called this “an important study” because it offers the first real-world evidence to support the findings from the LIR!C trial.
Dr. Cohen agreed with Dr. Agrawal that more work is needed to determine which patients benefit most from early ileocecal resection, although he suggested that known risk factors for worse outcomes — such as early age at diagnosis, penetrating features of disease, or perianal disease — may increase strength of surgical candidacy.
Still, based on the “fairly strong” body of data now available, he suggested that all patients should be educated about first-line ileocecal resection, as it is “reasonable” approach.
“It’s always important to present surgery as a treatment option,” Dr. Cohen said in an interview. “We don’t want to think of surgery as a last resort, or a failure, because that really colors it in a negative light, and then that ultimately impacts patients’ quality of life, and their perception of outcomes.”
The study was supported by the Danish National Research Foundation. The investigators disclosed no conflicts of interest. Dr. Cohen disclosed consulting and speaking honoraria from AbbVie.
These findings add weight to previously reported data from the LIR!C trial, suggesting that ileocecal resection should be considered a first-line treatment option for CD, reported principal investigator Kristine H. Allin, MD, PhD, of Aalborg University, Copenhagen.
“The LIR!C randomized clinical trial has demonstrated comparable quality of life with ileocecal resection and infliximab as a first-line treatment for limited, nonstricturing ileocecal CD at 1 year of follow-up, and improved outcomes with ileocecal resection on retrospective analysis of long-term follow-up data,” the investigators wrote in Gastroenterology. “However, in the real world, the long-term impact of early ileocecal resection for CD, compared with medical therapy, remains largely unexplored.”
To gather these real-world data, the investigators turned to the Danish National Patient Registry and the Danish National Prescription Registry, which included 1,279 individuals diagnosed with CD between 2003 and 2018 who received anti-TNF therapy or underwent ileocecal resection within 1 year of diagnosis. Within this group, slightly less than half underwent ileocecal resection (45.4%) while the remainder (54.6%) received anti-TNF therapy.
The primary outcome was a composite of one or more events: perianal CD, CD-related surgery, systemic corticosteroid exposure, and CD-related hospitalization. Secondary analyses evaluated the relative risks of these same four events as independent entities.
Multifactor-adjusted Cox proportional hazards regression analysis revealed that patients who underwent ileocecal resection had a 33% lower risk of the composite outcome compared with those who received anti-TNF therapy (adjusted hazard ratio [aHR], 0.67; 95% CI, 0.54-0.83).
In the secondary analyses, which examined risks for each component of the composite outcome, the surgery group had a significantly lower risk of CD-related surgery (aHR, 0.56; 95% CI, 0.39-0.80) and corticosteroid exposure (aHR, 0.71; 95% CI, 0.54-0.92), but not perianal CD or CD-related hospitalization.
After 5 years, half of the patients (49.7%) who underwent ileocecal resection were not receiving any treatment for CD. At the same timepoint, a slightly lower percentage of this group (46.3%) had started immunomodulator therapy, while 16.8% started anti-TNF therapy. Just 1.8% of these patients required a second intestinal resection.
“To our knowledge, these are the first real-world data in a population-based cohort with long-term follow-up of early ileocecal resection compared with anti-TNF therapy for newly diagnosed ileal and ileocecal CD,” the investigators wrote. “These data suggest that ileocecal resection may have a role as first-line therapy in Crohn’s disease management and challenge the current paradigm of reserving surgery for complicated Crohn’s disease refractory or intolerant to medications.”
Corresponding author Manasi Agrawal, MD, of Icahn School of Medicine at Mount Sinai, New York, suggested that “validation of our findings in external cohorts [is needed], and understanding of factors associated with improved outcomes following ileocecal resection.”
For clinicians and patients choosing between first-line anti-TNF therapy versus ileocecal resection using currently available evidence, Dr. Agrawal suggested that a variety of factors need to be considered, including disease location, extent of terminal ileum involved, presence of complications such as stricture, fistula, comorbid conditions, access to biologics, financial considerations, and patient preferences.
Benjamin Cohen, MD, staff physician and co-section head and clinical director for inflammatory bowel diseases in the department of gastroenterology, hepatology, and nutrition at Cleveland Clinic, called this “an important study” because it offers the first real-world evidence to support the findings from the LIR!C trial.
Dr. Cohen agreed with Dr. Agrawal that more work is needed to determine which patients benefit most from early ileocecal resection, although he suggested that known risk factors for worse outcomes — such as early age at diagnosis, penetrating features of disease, or perianal disease — may increase strength of surgical candidacy.
Still, based on the “fairly strong” body of data now available, he suggested that all patients should be educated about first-line ileocecal resection, as it is “reasonable” approach.
“It’s always important to present surgery as a treatment option,” Dr. Cohen said in an interview. “We don’t want to think of surgery as a last resort, or a failure, because that really colors it in a negative light, and then that ultimately impacts patients’ quality of life, and their perception of outcomes.”
The study was supported by the Danish National Research Foundation. The investigators disclosed no conflicts of interest. Dr. Cohen disclosed consulting and speaking honoraria from AbbVie.
These findings add weight to previously reported data from the LIR!C trial, suggesting that ileocecal resection should be considered a first-line treatment option for CD, reported principal investigator Kristine H. Allin, MD, PhD, of Aalborg University, Copenhagen.
“The LIR!C randomized clinical trial has demonstrated comparable quality of life with ileocecal resection and infliximab as a first-line treatment for limited, nonstricturing ileocecal CD at 1 year of follow-up, and improved outcomes with ileocecal resection on retrospective analysis of long-term follow-up data,” the investigators wrote in Gastroenterology. “However, in the real world, the long-term impact of early ileocecal resection for CD, compared with medical therapy, remains largely unexplored.”
To gather these real-world data, the investigators turned to the Danish National Patient Registry and the Danish National Prescription Registry, which included 1,279 individuals diagnosed with CD between 2003 and 2018 who received anti-TNF therapy or underwent ileocecal resection within 1 year of diagnosis. Within this group, slightly less than half underwent ileocecal resection (45.4%) while the remainder (54.6%) received anti-TNF therapy.
The primary outcome was a composite of one or more events: perianal CD, CD-related surgery, systemic corticosteroid exposure, and CD-related hospitalization. Secondary analyses evaluated the relative risks of these same four events as independent entities.
Multifactor-adjusted Cox proportional hazards regression analysis revealed that patients who underwent ileocecal resection had a 33% lower risk of the composite outcome compared with those who received anti-TNF therapy (adjusted hazard ratio [aHR], 0.67; 95% CI, 0.54-0.83).
In the secondary analyses, which examined risks for each component of the composite outcome, the surgery group had a significantly lower risk of CD-related surgery (aHR, 0.56; 95% CI, 0.39-0.80) and corticosteroid exposure (aHR, 0.71; 95% CI, 0.54-0.92), but not perianal CD or CD-related hospitalization.
After 5 years, half of the patients (49.7%) who underwent ileocecal resection were not receiving any treatment for CD. At the same timepoint, a slightly lower percentage of this group (46.3%) had started immunomodulator therapy, while 16.8% started anti-TNF therapy. Just 1.8% of these patients required a second intestinal resection.
“To our knowledge, these are the first real-world data in a population-based cohort with long-term follow-up of early ileocecal resection compared with anti-TNF therapy for newly diagnosed ileal and ileocecal CD,” the investigators wrote. “These data suggest that ileocecal resection may have a role as first-line therapy in Crohn’s disease management and challenge the current paradigm of reserving surgery for complicated Crohn’s disease refractory or intolerant to medications.”
Corresponding author Manasi Agrawal, MD, of Icahn School of Medicine at Mount Sinai, New York, suggested that “validation of our findings in external cohorts [is needed], and understanding of factors associated with improved outcomes following ileocecal resection.”
For clinicians and patients choosing between first-line anti-TNF therapy versus ileocecal resection using currently available evidence, Dr. Agrawal suggested that a variety of factors need to be considered, including disease location, extent of terminal ileum involved, presence of complications such as stricture, fistula, comorbid conditions, access to biologics, financial considerations, and patient preferences.
Benjamin Cohen, MD, staff physician and co-section head and clinical director for inflammatory bowel diseases in the department of gastroenterology, hepatology, and nutrition at Cleveland Clinic, called this “an important study” because it offers the first real-world evidence to support the findings from the LIR!C trial.
Dr. Cohen agreed with Dr. Agrawal that more work is needed to determine which patients benefit most from early ileocecal resection, although he suggested that known risk factors for worse outcomes — such as early age at diagnosis, penetrating features of disease, or perianal disease — may increase strength of surgical candidacy.
Still, based on the “fairly strong” body of data now available, he suggested that all patients should be educated about first-line ileocecal resection, as it is “reasonable” approach.
“It’s always important to present surgery as a treatment option,” Dr. Cohen said in an interview. “We don’t want to think of surgery as a last resort, or a failure, because that really colors it in a negative light, and then that ultimately impacts patients’ quality of life, and their perception of outcomes.”
The study was supported by the Danish National Research Foundation. The investigators disclosed no conflicts of interest. Dr. Cohen disclosed consulting and speaking honoraria from AbbVie.
FROM GASTROENTEROLOGY
AGA clinical practice guideline affirms role of biomarkers in Crohn’s disease management
, offering the most specific evidence-based recommendations yet for the use of fecal calprotectin (FCP) and serum C-reactive protein (CRP) in assessing disease activity.
Repeated monitoring with endoscopy allows for an objective assessment of inflammation and mucosal healing compared with symptoms alone. However, relying solely on endoscopy to guide management is an approach “limited by cost and resource utilization, invasiveness, and reduced patient acceptability,” wrote guideline authors on behalf of the AGA Clinical Guidelines Committee. The guideline was published online Nov. 17 in Gastroenterology.
“Use of biomarkers is no longer considered experimental and should be an integral part of IBD care and monitoring,” said Ashwin Ananthakrishnan, MBBS, MPH, a gastroenterologist with Massachusetts General Hospital in Boston and first author of the guideline. “We need further studies to define their optimal longitudinal use, but at a given time point, there is now abundant evidence that biomarkers provide significant incremental benefit over symptoms alone in assessing a patient’s status.”
Using evidence from randomized controlled trials and observational studies, and applying it to common clinical scenarios, there are conditional recommendations on the use of biomarkers in patients with established, diagnosed disease who were asymptomatic, symptomatic, or in surgically induced remission. Those recommendations, laid out in a detailed Clinical Decision Support Tool, include the following:
For asymptomatic patients: Check CRP and FCP every 6-12 months. Patients with normal levels, and who have endoscopically confirmed remission within the last 3 years without any subsequent change in symptoms or treatment, need not undergo endoscopy and can be followed with biomarker and clinical checks alone. If CRP or FCP are elevated (defined as CRP ≥ 5 mg/L, FCP ≥ 150 mcg/g), consider repeating biomarkers and/or performing endoscopic assessment of disease activity before adjusting treatment.
For mildly symptomatic patients: Role of biomarker testing may be limited and endoscopic or radiologic assessment may be required to assess active inflammation given the higher rate of false positive and false negative results with biomarkers in this population.
For patients with more severe symptoms: Elevated CRP or FCP can be used to guide treatment adjustment without endoscopic confirmation in certain situations. Normal levels may be false negative and should be confirmed by endoscopic assessment of disease activity.
For patients in surgically induced remission with a low likelihood of recurrence: FCP levels below 50 mcg/g can be used in lieu of routine endoscopic assessment within the first year after surgery. Higher FCP levels should prompt endoscopic assessment.
For patients in surgically induced remission with a high risk of recurrence: Do not rely on biomarkers. Perform endoscopic assessment.
All recommendations were deemed of low to moderate certainty based on results from randomized clinical trials and observational studies that utilized these biomarkers in patients with Crohn’s disease. Citing a dearth of quality evidence, the guideline authors determined they could not make recommendations on the use of a third proprietary biomarker — the endoscopic healing index (EHI).
Recent AGA Clinical Practice Guidelines on the role of biomarkers in ulcerative colitis, published in March, also support a strong role for fecal and blood biomarkers, determining when these can be used to avoid unneeded endoscopic assessments. However, in patients with Crohn’s disease, symptoms correlate less well with endoscopic activity.
As a result, “biomarker performance was acceptable only in asymptomatic individuals who had recently confirmed endoscopic remission; in those without recent endoscopic assessment, test performance was suboptimal.” In addition, the weaker correlation between symptoms and endoscopic activity in Crohn’s “reduced the utility of biomarker measurement to infer disease activity in those with mild symptoms.”
The guidelines were fully funded by the AGA Institute. The authors disclosed a number of potential conflicts of interest, including receiving research grants, as well as consulting and speaking fees, from pharmaceutical companies.
, offering the most specific evidence-based recommendations yet for the use of fecal calprotectin (FCP) and serum C-reactive protein (CRP) in assessing disease activity.
Repeated monitoring with endoscopy allows for an objective assessment of inflammation and mucosal healing compared with symptoms alone. However, relying solely on endoscopy to guide management is an approach “limited by cost and resource utilization, invasiveness, and reduced patient acceptability,” wrote guideline authors on behalf of the AGA Clinical Guidelines Committee. The guideline was published online Nov. 17 in Gastroenterology.
“Use of biomarkers is no longer considered experimental and should be an integral part of IBD care and monitoring,” said Ashwin Ananthakrishnan, MBBS, MPH, a gastroenterologist with Massachusetts General Hospital in Boston and first author of the guideline. “We need further studies to define their optimal longitudinal use, but at a given time point, there is now abundant evidence that biomarkers provide significant incremental benefit over symptoms alone in assessing a patient’s status.”
Using evidence from randomized controlled trials and observational studies, and applying it to common clinical scenarios, there are conditional recommendations on the use of biomarkers in patients with established, diagnosed disease who were asymptomatic, symptomatic, or in surgically induced remission. Those recommendations, laid out in a detailed Clinical Decision Support Tool, include the following:
For asymptomatic patients: Check CRP and FCP every 6-12 months. Patients with normal levels, and who have endoscopically confirmed remission within the last 3 years without any subsequent change in symptoms or treatment, need not undergo endoscopy and can be followed with biomarker and clinical checks alone. If CRP or FCP are elevated (defined as CRP ≥ 5 mg/L, FCP ≥ 150 mcg/g), consider repeating biomarkers and/or performing endoscopic assessment of disease activity before adjusting treatment.
For mildly symptomatic patients: Role of biomarker testing may be limited and endoscopic or radiologic assessment may be required to assess active inflammation given the higher rate of false positive and false negative results with biomarkers in this population.
For patients with more severe symptoms: Elevated CRP or FCP can be used to guide treatment adjustment without endoscopic confirmation in certain situations. Normal levels may be false negative and should be confirmed by endoscopic assessment of disease activity.
For patients in surgically induced remission with a low likelihood of recurrence: FCP levels below 50 mcg/g can be used in lieu of routine endoscopic assessment within the first year after surgery. Higher FCP levels should prompt endoscopic assessment.
For patients in surgically induced remission with a high risk of recurrence: Do not rely on biomarkers. Perform endoscopic assessment.
All recommendations were deemed of low to moderate certainty based on results from randomized clinical trials and observational studies that utilized these biomarkers in patients with Crohn’s disease. Citing a dearth of quality evidence, the guideline authors determined they could not make recommendations on the use of a third proprietary biomarker — the endoscopic healing index (EHI).
Recent AGA Clinical Practice Guidelines on the role of biomarkers in ulcerative colitis, published in March, also support a strong role for fecal and blood biomarkers, determining when these can be used to avoid unneeded endoscopic assessments. However, in patients with Crohn’s disease, symptoms correlate less well with endoscopic activity.
As a result, “biomarker performance was acceptable only in asymptomatic individuals who had recently confirmed endoscopic remission; in those without recent endoscopic assessment, test performance was suboptimal.” In addition, the weaker correlation between symptoms and endoscopic activity in Crohn’s “reduced the utility of biomarker measurement to infer disease activity in those with mild symptoms.”
The guidelines were fully funded by the AGA Institute. The authors disclosed a number of potential conflicts of interest, including receiving research grants, as well as consulting and speaking fees, from pharmaceutical companies.
, offering the most specific evidence-based recommendations yet for the use of fecal calprotectin (FCP) and serum C-reactive protein (CRP) in assessing disease activity.
Repeated monitoring with endoscopy allows for an objective assessment of inflammation and mucosal healing compared with symptoms alone. However, relying solely on endoscopy to guide management is an approach “limited by cost and resource utilization, invasiveness, and reduced patient acceptability,” wrote guideline authors on behalf of the AGA Clinical Guidelines Committee. The guideline was published online Nov. 17 in Gastroenterology.
“Use of biomarkers is no longer considered experimental and should be an integral part of IBD care and monitoring,” said Ashwin Ananthakrishnan, MBBS, MPH, a gastroenterologist with Massachusetts General Hospital in Boston and first author of the guideline. “We need further studies to define their optimal longitudinal use, but at a given time point, there is now abundant evidence that biomarkers provide significant incremental benefit over symptoms alone in assessing a patient’s status.”
Using evidence from randomized controlled trials and observational studies, and applying it to common clinical scenarios, there are conditional recommendations on the use of biomarkers in patients with established, diagnosed disease who were asymptomatic, symptomatic, or in surgically induced remission. Those recommendations, laid out in a detailed Clinical Decision Support Tool, include the following:
For asymptomatic patients: Check CRP and FCP every 6-12 months. Patients with normal levels, and who have endoscopically confirmed remission within the last 3 years without any subsequent change in symptoms or treatment, need not undergo endoscopy and can be followed with biomarker and clinical checks alone. If CRP or FCP are elevated (defined as CRP ≥ 5 mg/L, FCP ≥ 150 mcg/g), consider repeating biomarkers and/or performing endoscopic assessment of disease activity before adjusting treatment.
For mildly symptomatic patients: Role of biomarker testing may be limited and endoscopic or radiologic assessment may be required to assess active inflammation given the higher rate of false positive and false negative results with biomarkers in this population.
For patients with more severe symptoms: Elevated CRP or FCP can be used to guide treatment adjustment without endoscopic confirmation in certain situations. Normal levels may be false negative and should be confirmed by endoscopic assessment of disease activity.
For patients in surgically induced remission with a low likelihood of recurrence: FCP levels below 50 mcg/g can be used in lieu of routine endoscopic assessment within the first year after surgery. Higher FCP levels should prompt endoscopic assessment.
For patients in surgically induced remission with a high risk of recurrence: Do not rely on biomarkers. Perform endoscopic assessment.
All recommendations were deemed of low to moderate certainty based on results from randomized clinical trials and observational studies that utilized these biomarkers in patients with Crohn’s disease. Citing a dearth of quality evidence, the guideline authors determined they could not make recommendations on the use of a third proprietary biomarker — the endoscopic healing index (EHI).
Recent AGA Clinical Practice Guidelines on the role of biomarkers in ulcerative colitis, published in March, also support a strong role for fecal and blood biomarkers, determining when these can be used to avoid unneeded endoscopic assessments. However, in patients with Crohn’s disease, symptoms correlate less well with endoscopic activity.
As a result, “biomarker performance was acceptable only in asymptomatic individuals who had recently confirmed endoscopic remission; in those without recent endoscopic assessment, test performance was suboptimal.” In addition, the weaker correlation between symptoms and endoscopic activity in Crohn’s “reduced the utility of biomarker measurement to infer disease activity in those with mild symptoms.”
The guidelines were fully funded by the AGA Institute. The authors disclosed a number of potential conflicts of interest, including receiving research grants, as well as consulting and speaking fees, from pharmaceutical companies.
FROM GASTROENTEROLOGY
Acyclcarnitines could drive IBD via dysbiosis
These findings improve our understanding of IBD pathogenesis and disease course, and could prove valuable in biomarker research, reported lead author Gary D. Wu, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
In health, carnitine and acylcarnitines aid in fatty acid transport, the investigators wrote in September in Cellular and Molecular Gastroenterology and Hepatology. Acylcarnitines are also involved in metabolic signaling, and in the absence of sufficient short-chain fatty acids may serve as an alternative energy source for the intestinal epithelium.
“Recently, we and others have shown that fecal acylcarnitines are increased in patients with IBD, especially during dysbiosis,” they noted. “However, the mechanism(s) responsible for the increase of fecal acylcarnitines in IBD and their biological function have not been elucidated.”
The present study aimed to address this knowledge gap by characterizing both carnitine and acylcarnitines in pediatric IBD.
First, the investigators confirmed that both carnitine and acylcarnitines were elevated in fecal samples from pediatric patients with IBD.
Next, they analyzed fecal samples from subjects in the Food and Resulting Microbiota and Metabolome (FARMM) study, which compared microbiota recovery after gut purge and antibiotics among participants eating an omnivorous diet, a vegan diet, or an exclusive enteral nutrition (EEN) diet lacking in fiber. After the antibiotics, levels of fecal carnitine and acylcarnitines increased significantly in all groups, suggesting that microbiota were consuming these molecules.
To clarify the relationship between inflammation and levels of carnitine and acylcarnitines in the absence of microbiota, Dr. Wu and colleagues employed a germ-free mouse model with dextran sodium sulfate (DSS)–induced colitis. Levels of both molecule types were significantly increased in bile and plasma of mice with colitis versus those that were not exposed to DSS.
“Because the gut microbiota consumes both carnitine and acylcarnitines, these results are consistent with the notion that the increase of these metabolites in the feces of patients with IBD is driven by increased biliary delivery of acylcarnitines to the lumen combined with the reduced number and function of mitochondria in the colonic epithelium as previously reported,” the investigators wrote.
Further experiments with plated cultures and mice revealed that various bacterial species consumed carnitine and acylcarnitines in distinct patterns. Enterobacteriaceae demonstrated a notable proclivity for consumption in vitro and within the murine gut.
“As a high-dimensional analytic feature, the pattern of fecal acylcarnitines, perhaps together with bacterial taxonomy, may have utility as a biomarker for the presence or prognosis of IBD,” Dr. Wu and colleagues concluded. “In addition, based on currently available information about the impact of carnitine on the biology of Enterobacteriaceae, acylcarnitines also may have an important functional effect on the biology of the gut microbiota that is relevant to the pathogenesis or course of disease in patients with IBD.”
The study was supported by the Crohn’s and Colitis Foundation, the PennCHOP Microbiome Program, the Penn Center for Nutritional Science and Medicine, and others. The investigators disclosed no conflicts of interest.
The description of noninvasive biomarkers for inflammatory bowel disease (IBD) is key to better characterizing the disease pathogenesis. In this new publication, Lemons et al. describe deleterious effects of gut luminal carnitine and acylcarnitine in pediatric IBD patients, showing that these metabolites can serve as energy substrates to the microbiota, especially Enterobacteriaceae, promoting the growth of pathobionts and contributing to the persistence of dysbiosis which, in turn, may foster the course of IBD. In fact, acylcarnitine had been highlighted as a potential new target for IBD during dysbiosis by a previous multi-omics study of the gut microbiome. Moreover, Dr. Gary Wu’s team has shown that the intestinal epithelium can uptake and use acylcarnitine as an alternative source for energy production. However, epithelial mitochondrial dysfunction triggered by inflammation reduces the capacity of colonocytes to consume long-chain fatty acids, thus enhancing the fecal levels of acylcarnitine as described in IBD patients.
The description of noninvasive biomarkers for inflammatory bowel disease (IBD) is key to better characterizing the disease pathogenesis. In this new publication, Lemons et al. describe deleterious effects of gut luminal carnitine and acylcarnitine in pediatric IBD patients, showing that these metabolites can serve as energy substrates to the microbiota, especially Enterobacteriaceae, promoting the growth of pathobionts and contributing to the persistence of dysbiosis which, in turn, may foster the course of IBD. In fact, acylcarnitine had been highlighted as a potential new target for IBD during dysbiosis by a previous multi-omics study of the gut microbiome. Moreover, Dr. Gary Wu’s team has shown that the intestinal epithelium can uptake and use acylcarnitine as an alternative source for energy production. However, epithelial mitochondrial dysfunction triggered by inflammation reduces the capacity of colonocytes to consume long-chain fatty acids, thus enhancing the fecal levels of acylcarnitine as described in IBD patients.
The description of noninvasive biomarkers for inflammatory bowel disease (IBD) is key to better characterizing the disease pathogenesis. In this new publication, Lemons et al. describe deleterious effects of gut luminal carnitine and acylcarnitine in pediatric IBD patients, showing that these metabolites can serve as energy substrates to the microbiota, especially Enterobacteriaceae, promoting the growth of pathobionts and contributing to the persistence of dysbiosis which, in turn, may foster the course of IBD. In fact, acylcarnitine had been highlighted as a potential new target for IBD during dysbiosis by a previous multi-omics study of the gut microbiome. Moreover, Dr. Gary Wu’s team has shown that the intestinal epithelium can uptake and use acylcarnitine as an alternative source for energy production. However, epithelial mitochondrial dysfunction triggered by inflammation reduces the capacity of colonocytes to consume long-chain fatty acids, thus enhancing the fecal levels of acylcarnitine as described in IBD patients.
These findings improve our understanding of IBD pathogenesis and disease course, and could prove valuable in biomarker research, reported lead author Gary D. Wu, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
In health, carnitine and acylcarnitines aid in fatty acid transport, the investigators wrote in September in Cellular and Molecular Gastroenterology and Hepatology. Acylcarnitines are also involved in metabolic signaling, and in the absence of sufficient short-chain fatty acids may serve as an alternative energy source for the intestinal epithelium.
“Recently, we and others have shown that fecal acylcarnitines are increased in patients with IBD, especially during dysbiosis,” they noted. “However, the mechanism(s) responsible for the increase of fecal acylcarnitines in IBD and their biological function have not been elucidated.”
The present study aimed to address this knowledge gap by characterizing both carnitine and acylcarnitines in pediatric IBD.
First, the investigators confirmed that both carnitine and acylcarnitines were elevated in fecal samples from pediatric patients with IBD.
Next, they analyzed fecal samples from subjects in the Food and Resulting Microbiota and Metabolome (FARMM) study, which compared microbiota recovery after gut purge and antibiotics among participants eating an omnivorous diet, a vegan diet, or an exclusive enteral nutrition (EEN) diet lacking in fiber. After the antibiotics, levels of fecal carnitine and acylcarnitines increased significantly in all groups, suggesting that microbiota were consuming these molecules.
To clarify the relationship between inflammation and levels of carnitine and acylcarnitines in the absence of microbiota, Dr. Wu and colleagues employed a germ-free mouse model with dextran sodium sulfate (DSS)–induced colitis. Levels of both molecule types were significantly increased in bile and plasma of mice with colitis versus those that were not exposed to DSS.
“Because the gut microbiota consumes both carnitine and acylcarnitines, these results are consistent with the notion that the increase of these metabolites in the feces of patients with IBD is driven by increased biliary delivery of acylcarnitines to the lumen combined with the reduced number and function of mitochondria in the colonic epithelium as previously reported,” the investigators wrote.
Further experiments with plated cultures and mice revealed that various bacterial species consumed carnitine and acylcarnitines in distinct patterns. Enterobacteriaceae demonstrated a notable proclivity for consumption in vitro and within the murine gut.
“As a high-dimensional analytic feature, the pattern of fecal acylcarnitines, perhaps together with bacterial taxonomy, may have utility as a biomarker for the presence or prognosis of IBD,” Dr. Wu and colleagues concluded. “In addition, based on currently available information about the impact of carnitine on the biology of Enterobacteriaceae, acylcarnitines also may have an important functional effect on the biology of the gut microbiota that is relevant to the pathogenesis or course of disease in patients with IBD.”
The study was supported by the Crohn’s and Colitis Foundation, the PennCHOP Microbiome Program, the Penn Center for Nutritional Science and Medicine, and others. The investigators disclosed no conflicts of interest.
These findings improve our understanding of IBD pathogenesis and disease course, and could prove valuable in biomarker research, reported lead author Gary D. Wu, MD, of the University of Pennsylvania, Philadelphia, and colleagues.
In health, carnitine and acylcarnitines aid in fatty acid transport, the investigators wrote in September in Cellular and Molecular Gastroenterology and Hepatology. Acylcarnitines are also involved in metabolic signaling, and in the absence of sufficient short-chain fatty acids may serve as an alternative energy source for the intestinal epithelium.
“Recently, we and others have shown that fecal acylcarnitines are increased in patients with IBD, especially during dysbiosis,” they noted. “However, the mechanism(s) responsible for the increase of fecal acylcarnitines in IBD and their biological function have not been elucidated.”
The present study aimed to address this knowledge gap by characterizing both carnitine and acylcarnitines in pediatric IBD.
First, the investigators confirmed that both carnitine and acylcarnitines were elevated in fecal samples from pediatric patients with IBD.
Next, they analyzed fecal samples from subjects in the Food and Resulting Microbiota and Metabolome (FARMM) study, which compared microbiota recovery after gut purge and antibiotics among participants eating an omnivorous diet, a vegan diet, or an exclusive enteral nutrition (EEN) diet lacking in fiber. After the antibiotics, levels of fecal carnitine and acylcarnitines increased significantly in all groups, suggesting that microbiota were consuming these molecules.
To clarify the relationship between inflammation and levels of carnitine and acylcarnitines in the absence of microbiota, Dr. Wu and colleagues employed a germ-free mouse model with dextran sodium sulfate (DSS)–induced colitis. Levels of both molecule types were significantly increased in bile and plasma of mice with colitis versus those that were not exposed to DSS.
“Because the gut microbiota consumes both carnitine and acylcarnitines, these results are consistent with the notion that the increase of these metabolites in the feces of patients with IBD is driven by increased biliary delivery of acylcarnitines to the lumen combined with the reduced number and function of mitochondria in the colonic epithelium as previously reported,” the investigators wrote.
Further experiments with plated cultures and mice revealed that various bacterial species consumed carnitine and acylcarnitines in distinct patterns. Enterobacteriaceae demonstrated a notable proclivity for consumption in vitro and within the murine gut.
“As a high-dimensional analytic feature, the pattern of fecal acylcarnitines, perhaps together with bacterial taxonomy, may have utility as a biomarker for the presence or prognosis of IBD,” Dr. Wu and colleagues concluded. “In addition, based on currently available information about the impact of carnitine on the biology of Enterobacteriaceae, acylcarnitines also may have an important functional effect on the biology of the gut microbiota that is relevant to the pathogenesis or course of disease in patients with IBD.”
The study was supported by the Crohn’s and Colitis Foundation, the PennCHOP Microbiome Program, the Penn Center for Nutritional Science and Medicine, and others. The investigators disclosed no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Low-dose aspirin provokes no flares in patients with IBD during pregnancy
, shows new research presented in October at the American College of Gastroenterology (ACG) Annual Scientific Meeting.
Low-dose aspirin is recommended for pregnant women who are at risk of hypertensive disorders, such as eclampsia, preeclampsia, and gestational diabetes, said Uma Mahadevan, MD, AGAF, a gastroenterologist and director of the University of California, San Francisco Colitis and Crohn’s Disease Center, who presented the research at the meeting. Regular nonsteroidal anti-inflammatory drug use has been associated with increased disease activity in patients with inflammatory bowel disease (IBD), but the impact of low-dose aspirin on IBD during pregnancy has not been well studied, she said.
The study, which was conducted between January 2013 and December 2022 at a single clinic, included 325 women (mean age 34 years) with IBD who had at least one pregnancy. Of these, 53% had ulcerative colitis and 47% had Crohn’s disease. The primary outcome was IBD flare during pregnancy or within 6 months postpartum. Flares were defined as an IBD-related hospitalization and/or surgery, new initiation of IBD therapy, elevated level of fecal calprotectin greater than 150 micrograms per milligram, or new active endoscopic disease.
A total of 95 patients (29%) used low-dose aspirin during pregnancy; 59 took 81 mg and 36 took 162 mg. The cumulative flare rate was similar between patients who took low-dose aspirin and those who did not (24% vs. 26%, P = .83). However, patients who took low-dose aspirin were significantly more likely than were those who did not to experience preterm birth, younger gestational age at delivery, and cesarean delivery (22.1% vs. 6.1%, 38 weeks vs. 39 weeks, 51% vs. 27%, respectively, P < .01 for all).
Overall rates of hypertensive disorders of pregnancy were similar between the low-dose aspirin and non–low-dose aspirin groups (22% vs. 19%, respectively, P = .59), but individuals on low-dose aspirin were more likely to experience preeclampsia than were those not on low-dose aspirin (11.6% vs 4.3%, P = .03).
The study findings support the benefits of aspirin for pregnant women at increased risk for these conditions. “Pregnant patients with IBD should be offered low-dose aspirin without concern for increased risk of flares,” Dr. Mahadevan said.
“This is a very practical study with high relevance in our everyday management of IBD patients,” Shannon Chang, MD, a specialist in IBD with NYU Langone Health, said in an interview. “Having this study helps us understand the risk of increased IBD activity in the setting of aspirin use during pregnancy.”
Dr. Chang was not surprised by the findings. “Since the [ACOG] guidelines changed several years ago, there have been more and more patients with IBD who have taken aspirin during their pregnancies and the results of this study seem to match what we see in clinical practice,” she said. “This study will help us counsel our patients on the safety of aspirin use during pregnancy, and the findings will also be useful for discussions with our obstetrics colleagues who may seek guidance on the safety of aspirin [use] in our pregnant IBD patients.”
The study received no outside funding. Dr. Mahadevan disclosed relationships with AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Janssen, Pfizer, Prometheus Biosciences, Protagonist Therapeutics, Rani Therapeutics, Roivant, and Takeda. Dr. Chang disclosed serving as a consultant for Pfizer, AbbVie, and BMS.
, shows new research presented in October at the American College of Gastroenterology (ACG) Annual Scientific Meeting.
Low-dose aspirin is recommended for pregnant women who are at risk of hypertensive disorders, such as eclampsia, preeclampsia, and gestational diabetes, said Uma Mahadevan, MD, AGAF, a gastroenterologist and director of the University of California, San Francisco Colitis and Crohn’s Disease Center, who presented the research at the meeting. Regular nonsteroidal anti-inflammatory drug use has been associated with increased disease activity in patients with inflammatory bowel disease (IBD), but the impact of low-dose aspirin on IBD during pregnancy has not been well studied, she said.
The study, which was conducted between January 2013 and December 2022 at a single clinic, included 325 women (mean age 34 years) with IBD who had at least one pregnancy. Of these, 53% had ulcerative colitis and 47% had Crohn’s disease. The primary outcome was IBD flare during pregnancy or within 6 months postpartum. Flares were defined as an IBD-related hospitalization and/or surgery, new initiation of IBD therapy, elevated level of fecal calprotectin greater than 150 micrograms per milligram, or new active endoscopic disease.
A total of 95 patients (29%) used low-dose aspirin during pregnancy; 59 took 81 mg and 36 took 162 mg. The cumulative flare rate was similar between patients who took low-dose aspirin and those who did not (24% vs. 26%, P = .83). However, patients who took low-dose aspirin were significantly more likely than were those who did not to experience preterm birth, younger gestational age at delivery, and cesarean delivery (22.1% vs. 6.1%, 38 weeks vs. 39 weeks, 51% vs. 27%, respectively, P < .01 for all).
Overall rates of hypertensive disorders of pregnancy were similar between the low-dose aspirin and non–low-dose aspirin groups (22% vs. 19%, respectively, P = .59), but individuals on low-dose aspirin were more likely to experience preeclampsia than were those not on low-dose aspirin (11.6% vs 4.3%, P = .03).
The study findings support the benefits of aspirin for pregnant women at increased risk for these conditions. “Pregnant patients with IBD should be offered low-dose aspirin without concern for increased risk of flares,” Dr. Mahadevan said.
“This is a very practical study with high relevance in our everyday management of IBD patients,” Shannon Chang, MD, a specialist in IBD with NYU Langone Health, said in an interview. “Having this study helps us understand the risk of increased IBD activity in the setting of aspirin use during pregnancy.”
Dr. Chang was not surprised by the findings. “Since the [ACOG] guidelines changed several years ago, there have been more and more patients with IBD who have taken aspirin during their pregnancies and the results of this study seem to match what we see in clinical practice,” she said. “This study will help us counsel our patients on the safety of aspirin use during pregnancy, and the findings will also be useful for discussions with our obstetrics colleagues who may seek guidance on the safety of aspirin [use] in our pregnant IBD patients.”
The study received no outside funding. Dr. Mahadevan disclosed relationships with AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Janssen, Pfizer, Prometheus Biosciences, Protagonist Therapeutics, Rani Therapeutics, Roivant, and Takeda. Dr. Chang disclosed serving as a consultant for Pfizer, AbbVie, and BMS.
, shows new research presented in October at the American College of Gastroenterology (ACG) Annual Scientific Meeting.
Low-dose aspirin is recommended for pregnant women who are at risk of hypertensive disorders, such as eclampsia, preeclampsia, and gestational diabetes, said Uma Mahadevan, MD, AGAF, a gastroenterologist and director of the University of California, San Francisco Colitis and Crohn’s Disease Center, who presented the research at the meeting. Regular nonsteroidal anti-inflammatory drug use has been associated with increased disease activity in patients with inflammatory bowel disease (IBD), but the impact of low-dose aspirin on IBD during pregnancy has not been well studied, she said.
The study, which was conducted between January 2013 and December 2022 at a single clinic, included 325 women (mean age 34 years) with IBD who had at least one pregnancy. Of these, 53% had ulcerative colitis and 47% had Crohn’s disease. The primary outcome was IBD flare during pregnancy or within 6 months postpartum. Flares were defined as an IBD-related hospitalization and/or surgery, new initiation of IBD therapy, elevated level of fecal calprotectin greater than 150 micrograms per milligram, or new active endoscopic disease.
A total of 95 patients (29%) used low-dose aspirin during pregnancy; 59 took 81 mg and 36 took 162 mg. The cumulative flare rate was similar between patients who took low-dose aspirin and those who did not (24% vs. 26%, P = .83). However, patients who took low-dose aspirin were significantly more likely than were those who did not to experience preterm birth, younger gestational age at delivery, and cesarean delivery (22.1% vs. 6.1%, 38 weeks vs. 39 weeks, 51% vs. 27%, respectively, P < .01 for all).
Overall rates of hypertensive disorders of pregnancy were similar between the low-dose aspirin and non–low-dose aspirin groups (22% vs. 19%, respectively, P = .59), but individuals on low-dose aspirin were more likely to experience preeclampsia than were those not on low-dose aspirin (11.6% vs 4.3%, P = .03).
The study findings support the benefits of aspirin for pregnant women at increased risk for these conditions. “Pregnant patients with IBD should be offered low-dose aspirin without concern for increased risk of flares,” Dr. Mahadevan said.
“This is a very practical study with high relevance in our everyday management of IBD patients,” Shannon Chang, MD, a specialist in IBD with NYU Langone Health, said in an interview. “Having this study helps us understand the risk of increased IBD activity in the setting of aspirin use during pregnancy.”
Dr. Chang was not surprised by the findings. “Since the [ACOG] guidelines changed several years ago, there have been more and more patients with IBD who have taken aspirin during their pregnancies and the results of this study seem to match what we see in clinical practice,” she said. “This study will help us counsel our patients on the safety of aspirin use during pregnancy, and the findings will also be useful for discussions with our obstetrics colleagues who may seek guidance on the safety of aspirin [use] in our pregnant IBD patients.”
The study received no outside funding. Dr. Mahadevan disclosed relationships with AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Janssen, Pfizer, Prometheus Biosciences, Protagonist Therapeutics, Rani Therapeutics, Roivant, and Takeda. Dr. Chang disclosed serving as a consultant for Pfizer, AbbVie, and BMS.
FROM ACG 2023
Study: CBD provides symptom relief and improvements in gastroparesis
in a phase 2 randomized double-blinded, placebo-controlled study recently published in Clinical Gastroenterology and Hepatology.
There is “significant unmet medical need in gastroparesis,” and compared with cannabis, which has been used to relieve nausea and pain in patients with the condition, CBD has limited psychic effects with the added potential to reduce gut sensation and inflammation, wrote Ting Zheng, MD, and colleagues at Mayo Clinic in Rochester, Minn.
The researchers assessed the symptoms of 44 patients (21 randomized to receive CBD and 23 to receive placebo) – each of whom had nonsurgical gastroparesis with documented delayed gastric emptying of solids (GES) by scintigraphy for at least 3 months – with the American Neurogastroenterology and Motility Society’s Gastroparesis Cardinal Symptom Index (GCSI) Daily Diary.
They measured GES at baseline, and at 4 weeks, they measured GES again as well as fasting and postprandial gastric volumes and satiation using a validated Ensure drink test. (Patients ingested Ensure [Abbott Laboratories] at a rate of 30 mL/min and recorded their sensations every 5 minutes.) The two treatment arms were compared via 2-way analysis of covariance that included body mass index and, when applicable, baseline measurements.
Patients in the CBD group received twice-daily oral Epidiolex (Jazz Pharmaceuticals, Dublin), which is Food and Drug Administration–approved for the treatment of seizures associated with two rare forms of epilepsy and with another rare genetic disease in patients 1 year of age and older.
The researchers documented significant improvements in the CBD group in total GCSI score (P = .0008) and in scores measuring the inability to finish a normal-sized meal (P = .029), number of vomiting episodes/24 hours (P = .006), and overall perceived severity of symptoms (P = .034).
CBD treatment was also associated with greater tolerated volume of Ensure – “without increases in scores for nausea, fullness, bloating, and pain” – and, in another component of the GCSI, there was “a borderline reduction in upper abdominal pain,” Dr. Zheng and coauthors wrote.
There was a significant slowing of GES in the CBD group, however, and no significant differences were seen at 4 weeks in the fasting or accommodation gastric volumes between the two treatment groups. That beneficial effects of CBD were seen despite slowing of GES “raises the question of the contribution of the delayed GE of solids to development of symptoms in patients with gastroparesis, which is supported by some but not all meta-analyses on this topic,” they noted.
Patients had a mean age of 44 and most were female. Of the 44 patients, 32 had idiopathic gastroparesis, 6 had type 1 diabetes, and 6 had type 2 diabetes. Four patients in the study did not tolerate the FDA-recommended full-dose escalation of CBD to 20 mg/kg per day, but completed the study on the highest tolerated dose.
Adverse effects (fatigue, headache, nausea) were distributed equally between the two groups, but diarrhea was more common in the CBD group. Diarrhea was the most common adverse event in a recently published analysis of 892 pediatric patients receiving Epidiolex over an estimated 1,755.7 patient-years of CBD exposure, the researchers noted.
CBD is a cannabinoid receptor 2 inverse agonist with central nervous system effects, but it also affects visceral or somatic sensation peripherally, the authors noted. The beneficial effects of CBD in gastroparesis are “presumed to reflect effects on sensory mechanisms or anti-inflammatory effects mediated via CBR2 (cannabinoid receptor type 2) reversing the hypersensitivity and intrinsic inflammatory pathogenesis recorded in idiopathic and diabetic gastroparesis,” Dr. Zheng and colleagues wrote. CBD may also, in a mechanism unrelated to CB receptors, inhibit smooth muscle contractile activity, they said.
Larger randomized controlled trials of longer-term administration of CBD in both idiopathic and diabetic gastroparesis are warranted, the investigators said.
The researchers disclosed no conflicts. The study was supported by a grant from the National Institutes of Health.
in a phase 2 randomized double-blinded, placebo-controlled study recently published in Clinical Gastroenterology and Hepatology.
There is “significant unmet medical need in gastroparesis,” and compared with cannabis, which has been used to relieve nausea and pain in patients with the condition, CBD has limited psychic effects with the added potential to reduce gut sensation and inflammation, wrote Ting Zheng, MD, and colleagues at Mayo Clinic in Rochester, Minn.
The researchers assessed the symptoms of 44 patients (21 randomized to receive CBD and 23 to receive placebo) – each of whom had nonsurgical gastroparesis with documented delayed gastric emptying of solids (GES) by scintigraphy for at least 3 months – with the American Neurogastroenterology and Motility Society’s Gastroparesis Cardinal Symptom Index (GCSI) Daily Diary.
They measured GES at baseline, and at 4 weeks, they measured GES again as well as fasting and postprandial gastric volumes and satiation using a validated Ensure drink test. (Patients ingested Ensure [Abbott Laboratories] at a rate of 30 mL/min and recorded their sensations every 5 minutes.) The two treatment arms were compared via 2-way analysis of covariance that included body mass index and, when applicable, baseline measurements.
Patients in the CBD group received twice-daily oral Epidiolex (Jazz Pharmaceuticals, Dublin), which is Food and Drug Administration–approved for the treatment of seizures associated with two rare forms of epilepsy and with another rare genetic disease in patients 1 year of age and older.
The researchers documented significant improvements in the CBD group in total GCSI score (P = .0008) and in scores measuring the inability to finish a normal-sized meal (P = .029), number of vomiting episodes/24 hours (P = .006), and overall perceived severity of symptoms (P = .034).
CBD treatment was also associated with greater tolerated volume of Ensure – “without increases in scores for nausea, fullness, bloating, and pain” – and, in another component of the GCSI, there was “a borderline reduction in upper abdominal pain,” Dr. Zheng and coauthors wrote.
There was a significant slowing of GES in the CBD group, however, and no significant differences were seen at 4 weeks in the fasting or accommodation gastric volumes between the two treatment groups. That beneficial effects of CBD were seen despite slowing of GES “raises the question of the contribution of the delayed GE of solids to development of symptoms in patients with gastroparesis, which is supported by some but not all meta-analyses on this topic,” they noted.
Patients had a mean age of 44 and most were female. Of the 44 patients, 32 had idiopathic gastroparesis, 6 had type 1 diabetes, and 6 had type 2 diabetes. Four patients in the study did not tolerate the FDA-recommended full-dose escalation of CBD to 20 mg/kg per day, but completed the study on the highest tolerated dose.
Adverse effects (fatigue, headache, nausea) were distributed equally between the two groups, but diarrhea was more common in the CBD group. Diarrhea was the most common adverse event in a recently published analysis of 892 pediatric patients receiving Epidiolex over an estimated 1,755.7 patient-years of CBD exposure, the researchers noted.
CBD is a cannabinoid receptor 2 inverse agonist with central nervous system effects, but it also affects visceral or somatic sensation peripherally, the authors noted. The beneficial effects of CBD in gastroparesis are “presumed to reflect effects on sensory mechanisms or anti-inflammatory effects mediated via CBR2 (cannabinoid receptor type 2) reversing the hypersensitivity and intrinsic inflammatory pathogenesis recorded in idiopathic and diabetic gastroparesis,” Dr. Zheng and colleagues wrote. CBD may also, in a mechanism unrelated to CB receptors, inhibit smooth muscle contractile activity, they said.
Larger randomized controlled trials of longer-term administration of CBD in both idiopathic and diabetic gastroparesis are warranted, the investigators said.
The researchers disclosed no conflicts. The study was supported by a grant from the National Institutes of Health.
in a phase 2 randomized double-blinded, placebo-controlled study recently published in Clinical Gastroenterology and Hepatology.
There is “significant unmet medical need in gastroparesis,” and compared with cannabis, which has been used to relieve nausea and pain in patients with the condition, CBD has limited psychic effects with the added potential to reduce gut sensation and inflammation, wrote Ting Zheng, MD, and colleagues at Mayo Clinic in Rochester, Minn.
The researchers assessed the symptoms of 44 patients (21 randomized to receive CBD and 23 to receive placebo) – each of whom had nonsurgical gastroparesis with documented delayed gastric emptying of solids (GES) by scintigraphy for at least 3 months – with the American Neurogastroenterology and Motility Society’s Gastroparesis Cardinal Symptom Index (GCSI) Daily Diary.
They measured GES at baseline, and at 4 weeks, they measured GES again as well as fasting and postprandial gastric volumes and satiation using a validated Ensure drink test. (Patients ingested Ensure [Abbott Laboratories] at a rate of 30 mL/min and recorded their sensations every 5 minutes.) The two treatment arms were compared via 2-way analysis of covariance that included body mass index and, when applicable, baseline measurements.
Patients in the CBD group received twice-daily oral Epidiolex (Jazz Pharmaceuticals, Dublin), which is Food and Drug Administration–approved for the treatment of seizures associated with two rare forms of epilepsy and with another rare genetic disease in patients 1 year of age and older.
The researchers documented significant improvements in the CBD group in total GCSI score (P = .0008) and in scores measuring the inability to finish a normal-sized meal (P = .029), number of vomiting episodes/24 hours (P = .006), and overall perceived severity of symptoms (P = .034).
CBD treatment was also associated with greater tolerated volume of Ensure – “without increases in scores for nausea, fullness, bloating, and pain” – and, in another component of the GCSI, there was “a borderline reduction in upper abdominal pain,” Dr. Zheng and coauthors wrote.
There was a significant slowing of GES in the CBD group, however, and no significant differences were seen at 4 weeks in the fasting or accommodation gastric volumes between the two treatment groups. That beneficial effects of CBD were seen despite slowing of GES “raises the question of the contribution of the delayed GE of solids to development of symptoms in patients with gastroparesis, which is supported by some but not all meta-analyses on this topic,” they noted.
Patients had a mean age of 44 and most were female. Of the 44 patients, 32 had idiopathic gastroparesis, 6 had type 1 diabetes, and 6 had type 2 diabetes. Four patients in the study did not tolerate the FDA-recommended full-dose escalation of CBD to 20 mg/kg per day, but completed the study on the highest tolerated dose.
Adverse effects (fatigue, headache, nausea) were distributed equally between the two groups, but diarrhea was more common in the CBD group. Diarrhea was the most common adverse event in a recently published analysis of 892 pediatric patients receiving Epidiolex over an estimated 1,755.7 patient-years of CBD exposure, the researchers noted.
CBD is a cannabinoid receptor 2 inverse agonist with central nervous system effects, but it also affects visceral or somatic sensation peripherally, the authors noted. The beneficial effects of CBD in gastroparesis are “presumed to reflect effects on sensory mechanisms or anti-inflammatory effects mediated via CBR2 (cannabinoid receptor type 2) reversing the hypersensitivity and intrinsic inflammatory pathogenesis recorded in idiopathic and diabetic gastroparesis,” Dr. Zheng and colleagues wrote. CBD may also, in a mechanism unrelated to CB receptors, inhibit smooth muscle contractile activity, they said.
Larger randomized controlled trials of longer-term administration of CBD in both idiopathic and diabetic gastroparesis are warranted, the investigators said.
The researchers disclosed no conflicts. The study was supported by a grant from the National Institutes of Health.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY










