User login
DNA delivery vehicles may circumvent drug resistance in AML

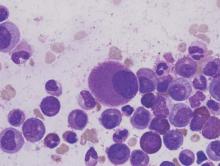
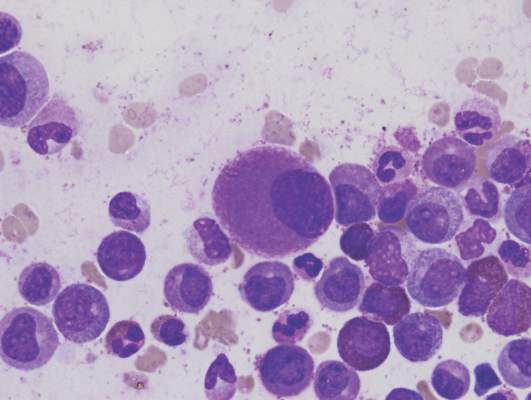
Image courtesy of PNAS
DNA origami nanostructures may be used to overcome drug resistance in acute myeloid leukemia (AML), according to preclinical research published in the journal Small.
Researchers found they could create these nanostructures in 10 minutes and load them with the anthracycline daunorubicin.
When the team introduced the structures to daunorubicin-resistant AML cells, the drug delivery vehicles entered the cells via endocytosis.
This allowed the drug to bypass defenses in the cell membrane that are effective against the free drug.
Once the nanostructures broke down, daunorubicin flooded the cells and killed them off.
Other research groups have used this delivery technique to overcome drug resistance in solid tumors, but this is the first time researchers have shown the same technique works on drug-resistant leukemia cells.
To create the DNA origami nanostructures, the researchers used the genome of a common bacteriophage and synthetic strands that were designed to fold up the bacteriophage DNA.
Although the folded-up shape performs a function, the DNA itself does not, explained Patrick Halley, a graduate student at The Ohio State University in Columbus.
“[T]he DNA capsule doesn’t do anything except hold a shape,” Halley said. “It’s just a static, rigid structure that carries things. It doesn’t encode any proteins or do anything else that we normally think of DNA as doing.”
The researchers tested the DNA origami nanostructures in AML cell lines that had developed resistance to daunorubicin. When molecules of daunorubicin enter these cells, the cells recognize the drug molecules and eject them through openings in the cell wall.
“Cancer cells have novel ways of resisting drugs, like these ‘pumps,’ and the exciting part of packaging the drug this way is that we can circumvent those defenses so that the drug accumulates in the cancer cell and causes it to die,” said John Byrd, MD, of The Ohio State University.
“Potentially, we can also tailor these structures to make them deliver drugs selectively to cancer cells and not to other parts of the body where they can cause side effects.”
In tests, the resistant AML cells effectively absorbed molecules of daunorubicin when they were hidden inside the rod-shaped nanostructures.
The researchers tracked the nanostructures inside the cells using fluorescent tags. Each structure measures about 15 nanometers wide and 100 nanometers long, and each has 4 hollow, open-ended interior compartments.
Study author Christopher Lucas, PhD, of The Ohio State University, said the design of the nanostructures maximizes the surface area available to carry the drug.
“The way daunorubicin works is it tucks into the cancer cell’s DNA and prevents it from replicating,” Dr Lucas said. “So we designed a capsule structure that would have lots of accessible DNA base-pairs for it to tuck into. When the capsule breaks down, the drug molecules are freed to flood the cell.”
The researchers said they designed the nanostructures to be strong and stable so they wouldn’t fully disintegrate and release the bulk of the drug until it was too late for the cells to eject them.
And that’s what the team observed with a fluorescence microscope. The cells drew the nanostructures into the organelles that would normally digest them (if they were food).
When the nanostructures broke down, the drug flooded the cells and caused them to disintegrate. Most cells died within the first 15 hours after consuming the nanostructures.
“DNA origami nanostructures have a lot of potential for drug delivery, not just for making effective drug delivery vehicles, but enabling new ways to study drug delivery,” said Carlos Castro, PhD, of The Ohio State University.
“For instance, we can vary the shape or mechanical stiffness of a structure very precisely and see how that affects entry into cells.”
Dr Castro said he hopes to create a streamlined and economically viable process for building DNA origami nanostructures as part of a modular drug delivery system.
Dr Byrd said the technique should work on most any form of drug-resistant cancer if further research shows it can be translated to animal models. ![]()

Image courtesy of PNAS
DNA origami nanostructures may be used to overcome drug resistance in acute myeloid leukemia (AML), according to preclinical research published in the journal Small.
Researchers found they could create these nanostructures in 10 minutes and load them with the anthracycline daunorubicin.
When the team introduced the structures to daunorubicin-resistant AML cells, the drug delivery vehicles entered the cells via endocytosis.
This allowed the drug to bypass defenses in the cell membrane that are effective against the free drug.
Once the nanostructures broke down, daunorubicin flooded the cells and killed them off.
Other research groups have used this delivery technique to overcome drug resistance in solid tumors, but this is the first time researchers have shown the same technique works on drug-resistant leukemia cells.
To create the DNA origami nanostructures, the researchers used the genome of a common bacteriophage and synthetic strands that were designed to fold up the bacteriophage DNA.
Although the folded-up shape performs a function, the DNA itself does not, explained Patrick Halley, a graduate student at The Ohio State University in Columbus.
“[T]he DNA capsule doesn’t do anything except hold a shape,” Halley said. “It’s just a static, rigid structure that carries things. It doesn’t encode any proteins or do anything else that we normally think of DNA as doing.”
The researchers tested the DNA origami nanostructures in AML cell lines that had developed resistance to daunorubicin. When molecules of daunorubicin enter these cells, the cells recognize the drug molecules and eject them through openings in the cell wall.
“Cancer cells have novel ways of resisting drugs, like these ‘pumps,’ and the exciting part of packaging the drug this way is that we can circumvent those defenses so that the drug accumulates in the cancer cell and causes it to die,” said John Byrd, MD, of The Ohio State University.
“Potentially, we can also tailor these structures to make them deliver drugs selectively to cancer cells and not to other parts of the body where they can cause side effects.”
In tests, the resistant AML cells effectively absorbed molecules of daunorubicin when they were hidden inside the rod-shaped nanostructures.
The researchers tracked the nanostructures inside the cells using fluorescent tags. Each structure measures about 15 nanometers wide and 100 nanometers long, and each has 4 hollow, open-ended interior compartments.
Study author Christopher Lucas, PhD, of The Ohio State University, said the design of the nanostructures maximizes the surface area available to carry the drug.
“The way daunorubicin works is it tucks into the cancer cell’s DNA and prevents it from replicating,” Dr Lucas said. “So we designed a capsule structure that would have lots of accessible DNA base-pairs for it to tuck into. When the capsule breaks down, the drug molecules are freed to flood the cell.”
The researchers said they designed the nanostructures to be strong and stable so they wouldn’t fully disintegrate and release the bulk of the drug until it was too late for the cells to eject them.
And that’s what the team observed with a fluorescence microscope. The cells drew the nanostructures into the organelles that would normally digest them (if they were food).
When the nanostructures broke down, the drug flooded the cells and caused them to disintegrate. Most cells died within the first 15 hours after consuming the nanostructures.
“DNA origami nanostructures have a lot of potential for drug delivery, not just for making effective drug delivery vehicles, but enabling new ways to study drug delivery,” said Carlos Castro, PhD, of The Ohio State University.
“For instance, we can vary the shape or mechanical stiffness of a structure very precisely and see how that affects entry into cells.”
Dr Castro said he hopes to create a streamlined and economically viable process for building DNA origami nanostructures as part of a modular drug delivery system.
Dr Byrd said the technique should work on most any form of drug-resistant cancer if further research shows it can be translated to animal models. ![]()

Image courtesy of PNAS
DNA origami nanostructures may be used to overcome drug resistance in acute myeloid leukemia (AML), according to preclinical research published in the journal Small.
Researchers found they could create these nanostructures in 10 minutes and load them with the anthracycline daunorubicin.
When the team introduced the structures to daunorubicin-resistant AML cells, the drug delivery vehicles entered the cells via endocytosis.
This allowed the drug to bypass defenses in the cell membrane that are effective against the free drug.
Once the nanostructures broke down, daunorubicin flooded the cells and killed them off.
Other research groups have used this delivery technique to overcome drug resistance in solid tumors, but this is the first time researchers have shown the same technique works on drug-resistant leukemia cells.
To create the DNA origami nanostructures, the researchers used the genome of a common bacteriophage and synthetic strands that were designed to fold up the bacteriophage DNA.
Although the folded-up shape performs a function, the DNA itself does not, explained Patrick Halley, a graduate student at The Ohio State University in Columbus.
“[T]he DNA capsule doesn’t do anything except hold a shape,” Halley said. “It’s just a static, rigid structure that carries things. It doesn’t encode any proteins or do anything else that we normally think of DNA as doing.”
The researchers tested the DNA origami nanostructures in AML cell lines that had developed resistance to daunorubicin. When molecules of daunorubicin enter these cells, the cells recognize the drug molecules and eject them through openings in the cell wall.
“Cancer cells have novel ways of resisting drugs, like these ‘pumps,’ and the exciting part of packaging the drug this way is that we can circumvent those defenses so that the drug accumulates in the cancer cell and causes it to die,” said John Byrd, MD, of The Ohio State University.
“Potentially, we can also tailor these structures to make them deliver drugs selectively to cancer cells and not to other parts of the body where they can cause side effects.”
In tests, the resistant AML cells effectively absorbed molecules of daunorubicin when they were hidden inside the rod-shaped nanostructures.
The researchers tracked the nanostructures inside the cells using fluorescent tags. Each structure measures about 15 nanometers wide and 100 nanometers long, and each has 4 hollow, open-ended interior compartments.
Study author Christopher Lucas, PhD, of The Ohio State University, said the design of the nanostructures maximizes the surface area available to carry the drug.
“The way daunorubicin works is it tucks into the cancer cell’s DNA and prevents it from replicating,” Dr Lucas said. “So we designed a capsule structure that would have lots of accessible DNA base-pairs for it to tuck into. When the capsule breaks down, the drug molecules are freed to flood the cell.”
The researchers said they designed the nanostructures to be strong and stable so they wouldn’t fully disintegrate and release the bulk of the drug until it was too late for the cells to eject them.
And that’s what the team observed with a fluorescence microscope. The cells drew the nanostructures into the organelles that would normally digest them (if they were food).
When the nanostructures broke down, the drug flooded the cells and caused them to disintegrate. Most cells died within the first 15 hours after consuming the nanostructures.
“DNA origami nanostructures have a lot of potential for drug delivery, not just for making effective drug delivery vehicles, but enabling new ways to study drug delivery,” said Carlos Castro, PhD, of The Ohio State University.
“For instance, we can vary the shape or mechanical stiffness of a structure very precisely and see how that affects entry into cells.”
Dr Castro said he hopes to create a streamlined and economically viable process for building DNA origami nanostructures as part of a modular drug delivery system.
Dr Byrd said the technique should work on most any form of drug-resistant cancer if further research shows it can be translated to animal models. ![]()
AAs have lower rate of most blood cancers than NHWs

receiving treatment
Photo by Rhoda Baer
A new report suggests African Americans (AAs) have significantly lower rates of most hematologic malignancies than non-Hispanic white (NHW) individuals in the US.
AAs of both sexes had significantly lower rates of leukemia, Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL) than NHWs, but the rate of myeloma was significantly higher among AAs.
The death rates for these malignancies followed the same patterns, with the exception of HL. There was no significant difference in HL mortality between AAs and NHWs of either sex.
These findings can be found in the report, “Cancer Statistics for African Americans, 2016,” appearing in CA: A Cancer Journal for Clinicians.
To compile this report, the researchers used data from the Surveillance, Epidemiology, and End Results program and the Centers for Disease Control and Prevention’s National Program of Cancer Registries.
Incidence
For part of the report, the researchers compared the incidence of cancers between AAs and NHWs (divided by gender) for the period from 2008 to 2012.
Among females, the incidence of leukemia was 8.6 per 100,000 in AAs and 10.7 per 100,000 in NHWs (P<0.05). Among males, the incidence was 13.2 per 100,000 in AAs and 17.7 per 100,000 in NHWs (P<0.05).
The incidence of HL in females was 2.4 per 100,000 in AAs and 2.7 per 100,000 in NHWs (P<0.05). The incidence of HL in males was 3.2 per 100,000 in AAs and 3.4 per 100,000 in NHWs (P<0.05).
The incidence of NHL in females was 12.0 per 100,000 in AAs and 16.6 per 100,000 in NHWs (P<0.05). The incidence of NHL in males was 17.2 per 100,000 in AAs and 24.1 per 100,000 in NHWs (P<0.05).
The incidence of myeloma in females was 11.1 per 100,000 in AAs and 4.3 per 100,000 in NHWs (P<0.05). The incidence of myeloma in males was 14.8 per 100,000 in AAs and 7.0 per 100,000 in NHWs (P<0.05).
Mortality
The researchers also compared cancer mortality between AAs and NHWs (divided by gender) for the period from 2008 to 2012.
The death rate for female leukemia patients was 4.8 per 100,000 in AAs and 5.4 per 100,000 in NHWs (P<0.05). The death rate for male leukemia patients was 8.1 per 100,000 in AAs and 9.9 per 100,000 in NHWs (P<0.05).
The death rate for female HL patients was 0.3 per 100,000 for both AAs and NHWs. The death rate for male HL patients was 0.4 per 100,000 for AAs and 0.5 per 100,000 in NHWs (not significant).
The death rate for female NHL patients was 3.6 per 100,000 in AAs and 5.0 per 100,000 in NHWs (P<0.05). The death rate for male NHL patients was 5.9 per 100,000 in AAs and 8.3 per 100,000 in NHWs (P<0.05).
The death rate for female myeloma patients was 5.4 per 100,000 in AAs and 2.4 per 100,000 in NHWs (P<0.05). The death rate for male myeloma patients was 7.8 per 100,000 in AAs and 4.0 per 100,000 in NHWs (P<0.05).
The researchers noted that the reasons for the higher rates of myeloma and myeloma death among AAs are, at present, unknown. ![]()

receiving treatment
Photo by Rhoda Baer
A new report suggests African Americans (AAs) have significantly lower rates of most hematologic malignancies than non-Hispanic white (NHW) individuals in the US.
AAs of both sexes had significantly lower rates of leukemia, Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL) than NHWs, but the rate of myeloma was significantly higher among AAs.
The death rates for these malignancies followed the same patterns, with the exception of HL. There was no significant difference in HL mortality between AAs and NHWs of either sex.
These findings can be found in the report, “Cancer Statistics for African Americans, 2016,” appearing in CA: A Cancer Journal for Clinicians.
To compile this report, the researchers used data from the Surveillance, Epidemiology, and End Results program and the Centers for Disease Control and Prevention’s National Program of Cancer Registries.
Incidence
For part of the report, the researchers compared the incidence of cancers between AAs and NHWs (divided by gender) for the period from 2008 to 2012.
Among females, the incidence of leukemia was 8.6 per 100,000 in AAs and 10.7 per 100,000 in NHWs (P<0.05). Among males, the incidence was 13.2 per 100,000 in AAs and 17.7 per 100,000 in NHWs (P<0.05).
The incidence of HL in females was 2.4 per 100,000 in AAs and 2.7 per 100,000 in NHWs (P<0.05). The incidence of HL in males was 3.2 per 100,000 in AAs and 3.4 per 100,000 in NHWs (P<0.05).
The incidence of NHL in females was 12.0 per 100,000 in AAs and 16.6 per 100,000 in NHWs (P<0.05). The incidence of NHL in males was 17.2 per 100,000 in AAs and 24.1 per 100,000 in NHWs (P<0.05).
The incidence of myeloma in females was 11.1 per 100,000 in AAs and 4.3 per 100,000 in NHWs (P<0.05). The incidence of myeloma in males was 14.8 per 100,000 in AAs and 7.0 per 100,000 in NHWs (P<0.05).
Mortality
The researchers also compared cancer mortality between AAs and NHWs (divided by gender) for the period from 2008 to 2012.
The death rate for female leukemia patients was 4.8 per 100,000 in AAs and 5.4 per 100,000 in NHWs (P<0.05). The death rate for male leukemia patients was 8.1 per 100,000 in AAs and 9.9 per 100,000 in NHWs (P<0.05).
The death rate for female HL patients was 0.3 per 100,000 for both AAs and NHWs. The death rate for male HL patients was 0.4 per 100,000 for AAs and 0.5 per 100,000 in NHWs (not significant).
The death rate for female NHL patients was 3.6 per 100,000 in AAs and 5.0 per 100,000 in NHWs (P<0.05). The death rate for male NHL patients was 5.9 per 100,000 in AAs and 8.3 per 100,000 in NHWs (P<0.05).
The death rate for female myeloma patients was 5.4 per 100,000 in AAs and 2.4 per 100,000 in NHWs (P<0.05). The death rate for male myeloma patients was 7.8 per 100,000 in AAs and 4.0 per 100,000 in NHWs (P<0.05).
The researchers noted that the reasons for the higher rates of myeloma and myeloma death among AAs are, at present, unknown. ![]()

receiving treatment
Photo by Rhoda Baer
A new report suggests African Americans (AAs) have significantly lower rates of most hematologic malignancies than non-Hispanic white (NHW) individuals in the US.
AAs of both sexes had significantly lower rates of leukemia, Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL) than NHWs, but the rate of myeloma was significantly higher among AAs.
The death rates for these malignancies followed the same patterns, with the exception of HL. There was no significant difference in HL mortality between AAs and NHWs of either sex.
These findings can be found in the report, “Cancer Statistics for African Americans, 2016,” appearing in CA: A Cancer Journal for Clinicians.
To compile this report, the researchers used data from the Surveillance, Epidemiology, and End Results program and the Centers for Disease Control and Prevention’s National Program of Cancer Registries.
Incidence
For part of the report, the researchers compared the incidence of cancers between AAs and NHWs (divided by gender) for the period from 2008 to 2012.
Among females, the incidence of leukemia was 8.6 per 100,000 in AAs and 10.7 per 100,000 in NHWs (P<0.05). Among males, the incidence was 13.2 per 100,000 in AAs and 17.7 per 100,000 in NHWs (P<0.05).
The incidence of HL in females was 2.4 per 100,000 in AAs and 2.7 per 100,000 in NHWs (P<0.05). The incidence of HL in males was 3.2 per 100,000 in AAs and 3.4 per 100,000 in NHWs (P<0.05).
The incidence of NHL in females was 12.0 per 100,000 in AAs and 16.6 per 100,000 in NHWs (P<0.05). The incidence of NHL in males was 17.2 per 100,000 in AAs and 24.1 per 100,000 in NHWs (P<0.05).
The incidence of myeloma in females was 11.1 per 100,000 in AAs and 4.3 per 100,000 in NHWs (P<0.05). The incidence of myeloma in males was 14.8 per 100,000 in AAs and 7.0 per 100,000 in NHWs (P<0.05).
Mortality
The researchers also compared cancer mortality between AAs and NHWs (divided by gender) for the period from 2008 to 2012.
The death rate for female leukemia patients was 4.8 per 100,000 in AAs and 5.4 per 100,000 in NHWs (P<0.05). The death rate for male leukemia patients was 8.1 per 100,000 in AAs and 9.9 per 100,000 in NHWs (P<0.05).
The death rate for female HL patients was 0.3 per 100,000 for both AAs and NHWs. The death rate for male HL patients was 0.4 per 100,000 for AAs and 0.5 per 100,000 in NHWs (not significant).
The death rate for female NHL patients was 3.6 per 100,000 in AAs and 5.0 per 100,000 in NHWs (P<0.05). The death rate for male NHL patients was 5.9 per 100,000 in AAs and 8.3 per 100,000 in NHWs (P<0.05).
The death rate for female myeloma patients was 5.4 per 100,000 in AAs and 2.4 per 100,000 in NHWs (P<0.05). The death rate for male myeloma patients was 7.8 per 100,000 in AAs and 4.0 per 100,000 in NHWs (P<0.05).
The researchers noted that the reasons for the higher rates of myeloma and myeloma death among AAs are, at present, unknown. ![]()
Team identifies potential target for T-ALL therapy

New research suggests T-cell acute lymphoblastic leukemia (T-ALL) cells use the tricarboxylic acid (TCA) cycle to support their growth and survival.
Investigators say the findings could aid the development of therapeutics that can kill T-ALL cells by targeting an enzyme that exists in the TCA cycle—dihydrolipoamide S-succinyltransferase (DLST).
The team described this research in the journal Leukemia.
“Researchers have wrongly assumed that cancer cells do not use the TCA cycle to support their growth,” said study author Hui Feng, MD, PhD, of Boston University Medical Center in Massachusetts.
“Our new findings provide solid evidence that these cancer cells depend on the TCA cycle for their survival. Additionally, we demonstrated the importance of DLST in T-cell leukemia development and have identified a targetable enzyme for T-cell leukemia treatment.”
For this study, the investigators set out to examine the mechanisms underlying MYC-mediated tumorigenesis in T-ALL.
They used a zebrafish model of MYC-induced T-ALL to screen for genes that contribute to disease onset. The results suggested the TCA-cycle enzyme DLST is an important contributor to T-ALL development.
And experiments showed that heterozygous inactivation of DLST significantly delayed disease onset in the zebrafish, apparently without affecting the development of the fish.
Further analysis revealed that inhibiting the activity of DLST could effectively kill human T-ALL cells. Specifically, RNAi knockdown of DLST decreased cell viability and induced apoptosis in human T-ALL cell
lines.
The investigators found that knockdown of DLST disrupted the TCA cycle in the human T-ALL cells. But adding succinate, the downstream TCA-cycle intermediate, to the cells rescued defects in cell viability caused by DLST knockdown.
The investigators said the therapeutic benefit of DLST inhibition may extend to cancers other than T-ALL as well. ![]()

New research suggests T-cell acute lymphoblastic leukemia (T-ALL) cells use the tricarboxylic acid (TCA) cycle to support their growth and survival.
Investigators say the findings could aid the development of therapeutics that can kill T-ALL cells by targeting an enzyme that exists in the TCA cycle—dihydrolipoamide S-succinyltransferase (DLST).
The team described this research in the journal Leukemia.
“Researchers have wrongly assumed that cancer cells do not use the TCA cycle to support their growth,” said study author Hui Feng, MD, PhD, of Boston University Medical Center in Massachusetts.
“Our new findings provide solid evidence that these cancer cells depend on the TCA cycle for their survival. Additionally, we demonstrated the importance of DLST in T-cell leukemia development and have identified a targetable enzyme for T-cell leukemia treatment.”
For this study, the investigators set out to examine the mechanisms underlying MYC-mediated tumorigenesis in T-ALL.
They used a zebrafish model of MYC-induced T-ALL to screen for genes that contribute to disease onset. The results suggested the TCA-cycle enzyme DLST is an important contributor to T-ALL development.
And experiments showed that heterozygous inactivation of DLST significantly delayed disease onset in the zebrafish, apparently without affecting the development of the fish.
Further analysis revealed that inhibiting the activity of DLST could effectively kill human T-ALL cells. Specifically, RNAi knockdown of DLST decreased cell viability and induced apoptosis in human T-ALL cell
lines.
The investigators found that knockdown of DLST disrupted the TCA cycle in the human T-ALL cells. But adding succinate, the downstream TCA-cycle intermediate, to the cells rescued defects in cell viability caused by DLST knockdown.
The investigators said the therapeutic benefit of DLST inhibition may extend to cancers other than T-ALL as well. ![]()

New research suggests T-cell acute lymphoblastic leukemia (T-ALL) cells use the tricarboxylic acid (TCA) cycle to support their growth and survival.
Investigators say the findings could aid the development of therapeutics that can kill T-ALL cells by targeting an enzyme that exists in the TCA cycle—dihydrolipoamide S-succinyltransferase (DLST).
The team described this research in the journal Leukemia.
“Researchers have wrongly assumed that cancer cells do not use the TCA cycle to support their growth,” said study author Hui Feng, MD, PhD, of Boston University Medical Center in Massachusetts.
“Our new findings provide solid evidence that these cancer cells depend on the TCA cycle for their survival. Additionally, we demonstrated the importance of DLST in T-cell leukemia development and have identified a targetable enzyme for T-cell leukemia treatment.”
For this study, the investigators set out to examine the mechanisms underlying MYC-mediated tumorigenesis in T-ALL.
They used a zebrafish model of MYC-induced T-ALL to screen for genes that contribute to disease onset. The results suggested the TCA-cycle enzyme DLST is an important contributor to T-ALL development.
And experiments showed that heterozygous inactivation of DLST significantly delayed disease onset in the zebrafish, apparently without affecting the development of the fish.
Further analysis revealed that inhibiting the activity of DLST could effectively kill human T-ALL cells. Specifically, RNAi knockdown of DLST decreased cell viability and induced apoptosis in human T-ALL cell
lines.
The investigators found that knockdown of DLST disrupted the TCA cycle in the human T-ALL cells. But adding succinate, the downstream TCA-cycle intermediate, to the cells rescued defects in cell viability caused by DLST knockdown.
The investigators said the therapeutic benefit of DLST inhibition may extend to cancers other than T-ALL as well. ![]()
Orphan designation recommended for BTK inhibitor

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) is recommending orphan designation for the second-generation BTK inhibitor acalabrutinib (ACP-196) for 3 indications.
The COMP is recommending the drug receive orphan designation as a treatment for chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), mantle cell lymphoma, and Waldenström’s macroglobulinemia.
The COMP adopts an opinion on orphan drug designation, and that opinion is submitted to the European Commission (EC) for endorsement.
To be granted orphan designation by the EC, a medicine must be intended for the treatment, prevention, or diagnosis of a disease that is life-threatening and has a prevalence of up to 5 in 10,000 in the European Union. Additionally, the medicine must aim to provide significant benefit to those affected by the condition.
Orphan designation provides companies with development and market exclusivity incentives for designated compounds and medicines.
About acalabrutinib
Acalabrutinib is under development by AstraZeneca and Acerta Pharma BV. The drug is currently being evaluated in trials of patients with CLL/SLL, mantle cell lymphoma, Waldentröm’s macroglobulinemia, and a range of other hematologic malignancies and solid tumor cancers.
Data from a phase 1/2 trial of acalabrutinib in CLL were presented at the 2015 ASH Annual Meeting and simultaneously published in NEJM.
The researchers reported on 61 patients with relapsed CLL who had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients were still receiving treatment.
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time. ![]()

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) is recommending orphan designation for the second-generation BTK inhibitor acalabrutinib (ACP-196) for 3 indications.
The COMP is recommending the drug receive orphan designation as a treatment for chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), mantle cell lymphoma, and Waldenström’s macroglobulinemia.
The COMP adopts an opinion on orphan drug designation, and that opinion is submitted to the European Commission (EC) for endorsement.
To be granted orphan designation by the EC, a medicine must be intended for the treatment, prevention, or diagnosis of a disease that is life-threatening and has a prevalence of up to 5 in 10,000 in the European Union. Additionally, the medicine must aim to provide significant benefit to those affected by the condition.
Orphan designation provides companies with development and market exclusivity incentives for designated compounds and medicines.
About acalabrutinib
Acalabrutinib is under development by AstraZeneca and Acerta Pharma BV. The drug is currently being evaluated in trials of patients with CLL/SLL, mantle cell lymphoma, Waldentröm’s macroglobulinemia, and a range of other hematologic malignancies and solid tumor cancers.
Data from a phase 1/2 trial of acalabrutinib in CLL were presented at the 2015 ASH Annual Meeting and simultaneously published in NEJM.
The researchers reported on 61 patients with relapsed CLL who had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients were still receiving treatment.
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time. ![]()

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) is recommending orphan designation for the second-generation BTK inhibitor acalabrutinib (ACP-196) for 3 indications.
The COMP is recommending the drug receive orphan designation as a treatment for chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), mantle cell lymphoma, and Waldenström’s macroglobulinemia.
The COMP adopts an opinion on orphan drug designation, and that opinion is submitted to the European Commission (EC) for endorsement.
To be granted orphan designation by the EC, a medicine must be intended for the treatment, prevention, or diagnosis of a disease that is life-threatening and has a prevalence of up to 5 in 10,000 in the European Union. Additionally, the medicine must aim to provide significant benefit to those affected by the condition.
Orphan designation provides companies with development and market exclusivity incentives for designated compounds and medicines.
About acalabrutinib
Acalabrutinib is under development by AstraZeneca and Acerta Pharma BV. The drug is currently being evaluated in trials of patients with CLL/SLL, mantle cell lymphoma, Waldentröm’s macroglobulinemia, and a range of other hematologic malignancies and solid tumor cancers.
Data from a phase 1/2 trial of acalabrutinib in CLL were presented at the 2015 ASH Annual Meeting and simultaneously published in NEJM.
The researchers reported on 61 patients with relapsed CLL who had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients were still receiving treatment.
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time. ![]()
Poverty tied to early relapse in kids with ALL

Photo by Logan Tuttle
A new study suggests children with acute lymphoblastic leukemia (ALL) are more likely to suffer early relapse if they live in high-poverty areas.
All of the children studied received the same treatment, and the rates of relapse were similar regardless of poverty level.
But early relapse was more common among children from poorer areas. These children also had a lower rate of 5-year overall survival, but the difference was not significant.
Kira Bona, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and her colleagues reported these results in Pediatric Blood & Cancer.
The team examined outcomes for 575 children, ages 1 to 18, with newly diagnosed ALL who were treated on Dana-Farber Cancer Institute ALL Consortium Protocols at 7 major academic medical centers in the US between 2000 and 2010.
Using US Census Bureau criteria, the investigators defined high-poverty areas as zip codes where 20% or more of residents have incomes below the federal poverty level. For a family of 4, this translates to an annual income of $24,250 or less.
Dr Bona and her colleagues found the overall rates of relapse were similar between children from low-poverty areas and those from high-poverty areas.
However, the timing of relapse differed significantly. Ninety-two percent of children from high-poverty areas who relapsed suffered early relapse (less than 36 months after first achieving complete remission), while 48% of the other children who relapsed did so early (P=0.008).
The 5-year overall survival was 85% for children from high-poverty areas and 92% for children from low-poverty areas. This difference is statistically significant when considered on its own (P=0.02) but not when the analysis is adjusted for other factors (P=0.07).
Still, the investigators said this suggests a possible disparity in survival.
“These children are getting the same best possible care at well-resourced institutions from highly trained clinicians, and we’re still seeing disparities,” Dr Bona said. “In trying to improve cure rates, we, as a field, have focused almost exclusively on biology. If we want to move forward, we also have to look at social determinants.”
Next steps
Dr Bona and her colleagues are undertaking further research designed to delve deeper into the relationship between socioeconomic status and outcomes and to allow for the development of poverty-targeted interventions.
As part of a prospective trial for children with ALL, the researchers will investigate associations between disease outcomes and the socioeconomic status of patients’ families, using a targetable measure of socioeconomic status called material hardship (food, housing, and/or energy insecurity).
The researchers will also investigate possible mechanisms underlying the relationship between socioeconomic status and early relapse, including adherence to oral chemotherapy and delays or dose reductions in chemotherapy due to a child’s underlying health.
In another study, investigators will conduct in-depth interviews with patients’ families, probing their knowledge and experience to pinpoint factors that might explain the disparity in outcomes and identify factors that can be targeted with interventions.
“Doing these next 2 studies is incredibly important,” Dr Bona said. “This study told us that simply providing the current best treatment regimen is not good enough if our goal is to cure every child with cancer.”
“At the same time that we develop new drugs and new treatment protocols, we need to address social determinants of health. Findings from these next studies will help us develop specific interventions to address disparities in outcomes. That’s an amazing opportunity.” ![]()

Photo by Logan Tuttle
A new study suggests children with acute lymphoblastic leukemia (ALL) are more likely to suffer early relapse if they live in high-poverty areas.
All of the children studied received the same treatment, and the rates of relapse were similar regardless of poverty level.
But early relapse was more common among children from poorer areas. These children also had a lower rate of 5-year overall survival, but the difference was not significant.
Kira Bona, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and her colleagues reported these results in Pediatric Blood & Cancer.
The team examined outcomes for 575 children, ages 1 to 18, with newly diagnosed ALL who were treated on Dana-Farber Cancer Institute ALL Consortium Protocols at 7 major academic medical centers in the US between 2000 and 2010.
Using US Census Bureau criteria, the investigators defined high-poverty areas as zip codes where 20% or more of residents have incomes below the federal poverty level. For a family of 4, this translates to an annual income of $24,250 or less.
Dr Bona and her colleagues found the overall rates of relapse were similar between children from low-poverty areas and those from high-poverty areas.
However, the timing of relapse differed significantly. Ninety-two percent of children from high-poverty areas who relapsed suffered early relapse (less than 36 months after first achieving complete remission), while 48% of the other children who relapsed did so early (P=0.008).
The 5-year overall survival was 85% for children from high-poverty areas and 92% for children from low-poverty areas. This difference is statistically significant when considered on its own (P=0.02) but not when the analysis is adjusted for other factors (P=0.07).
Still, the investigators said this suggests a possible disparity in survival.
“These children are getting the same best possible care at well-resourced institutions from highly trained clinicians, and we’re still seeing disparities,” Dr Bona said. “In trying to improve cure rates, we, as a field, have focused almost exclusively on biology. If we want to move forward, we also have to look at social determinants.”
Next steps
Dr Bona and her colleagues are undertaking further research designed to delve deeper into the relationship between socioeconomic status and outcomes and to allow for the development of poverty-targeted interventions.
As part of a prospective trial for children with ALL, the researchers will investigate associations between disease outcomes and the socioeconomic status of patients’ families, using a targetable measure of socioeconomic status called material hardship (food, housing, and/or energy insecurity).
The researchers will also investigate possible mechanisms underlying the relationship between socioeconomic status and early relapse, including adherence to oral chemotherapy and delays or dose reductions in chemotherapy due to a child’s underlying health.
In another study, investigators will conduct in-depth interviews with patients’ families, probing their knowledge and experience to pinpoint factors that might explain the disparity in outcomes and identify factors that can be targeted with interventions.
“Doing these next 2 studies is incredibly important,” Dr Bona said. “This study told us that simply providing the current best treatment regimen is not good enough if our goal is to cure every child with cancer.”
“At the same time that we develop new drugs and new treatment protocols, we need to address social determinants of health. Findings from these next studies will help us develop specific interventions to address disparities in outcomes. That’s an amazing opportunity.” ![]()

Photo by Logan Tuttle
A new study suggests children with acute lymphoblastic leukemia (ALL) are more likely to suffer early relapse if they live in high-poverty areas.
All of the children studied received the same treatment, and the rates of relapse were similar regardless of poverty level.
But early relapse was more common among children from poorer areas. These children also had a lower rate of 5-year overall survival, but the difference was not significant.
Kira Bona, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and her colleagues reported these results in Pediatric Blood & Cancer.
The team examined outcomes for 575 children, ages 1 to 18, with newly diagnosed ALL who were treated on Dana-Farber Cancer Institute ALL Consortium Protocols at 7 major academic medical centers in the US between 2000 and 2010.
Using US Census Bureau criteria, the investigators defined high-poverty areas as zip codes where 20% or more of residents have incomes below the federal poverty level. For a family of 4, this translates to an annual income of $24,250 or less.
Dr Bona and her colleagues found the overall rates of relapse were similar between children from low-poverty areas and those from high-poverty areas.
However, the timing of relapse differed significantly. Ninety-two percent of children from high-poverty areas who relapsed suffered early relapse (less than 36 months after first achieving complete remission), while 48% of the other children who relapsed did so early (P=0.008).
The 5-year overall survival was 85% for children from high-poverty areas and 92% for children from low-poverty areas. This difference is statistically significant when considered on its own (P=0.02) but not when the analysis is adjusted for other factors (P=0.07).
Still, the investigators said this suggests a possible disparity in survival.
“These children are getting the same best possible care at well-resourced institutions from highly trained clinicians, and we’re still seeing disparities,” Dr Bona said. “In trying to improve cure rates, we, as a field, have focused almost exclusively on biology. If we want to move forward, we also have to look at social determinants.”
Next steps
Dr Bona and her colleagues are undertaking further research designed to delve deeper into the relationship between socioeconomic status and outcomes and to allow for the development of poverty-targeted interventions.
As part of a prospective trial for children with ALL, the researchers will investigate associations between disease outcomes and the socioeconomic status of patients’ families, using a targetable measure of socioeconomic status called material hardship (food, housing, and/or energy insecurity).
The researchers will also investigate possible mechanisms underlying the relationship between socioeconomic status and early relapse, including adherence to oral chemotherapy and delays or dose reductions in chemotherapy due to a child’s underlying health.
In another study, investigators will conduct in-depth interviews with patients’ families, probing their knowledge and experience to pinpoint factors that might explain the disparity in outcomes and identify factors that can be targeted with interventions.
“Doing these next 2 studies is incredibly important,” Dr Bona said. “This study told us that simply providing the current best treatment regimen is not good enough if our goal is to cure every child with cancer.”
“At the same time that we develop new drugs and new treatment protocols, we need to address social determinants of health. Findings from these next studies will help us develop specific interventions to address disparities in outcomes. That’s an amazing opportunity.” ![]()
How an anticancer drug fights lymphoid malignancies

Photo by Cameron Wells,
Walter and Eliza Hall
Institute of Medical Research
Research published in Cell Reports helps explain how the anticancer agent Nutlin3a fights lymphoma and other hematologic malignancies.
Nutlin3a is known to activate the tumor suppressor p53, but it hasn’t been clear exactly which p53 target genes are essential for the drug’s therapeutic activity.
The new research revealed that PUMA-mediated apoptosis—not p21-mediated cell-cycle arrest or senescence—is responsible for Nutlin3a’s therapeutic activity in lymphoid malignancies.
“By understanding how nutlins are killing cancer cells, we can begin to formulate their best possible use, including choosing the best partner drugs to combine the nutlins with,” said study author Andreas Strasser, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia.
With this study, Dr Strasser and his colleagues first found that Nutlin3a activates p53 target gene expression and causes cell-cycle arrest and apoptosis in non-transformed mouse lymphoid cells in vitro.
The team then showed that Nutlin3a-mediated killing of these cells requires PUMA but not p21. In vivo, loss of PUMA protected non-transformed mouse lymphoid cells against Nutlin3a-induced killing. Loss of p21 did not provide the same protection.
Next, the researchers found that malignant Eµ-Myc lymphoma cells were much more sensitive to Nutlin3a than were non-transformed lymphoid cells. In vitro experiments with Eµ-Myc lymphoma cells showed that Nutlin3a promotes p53 accumulation and downstream effector pathway activation.
As in previous experiments, PUMA (not p21) proved critical for Nutlin3a-induced killing of Eµ-Myc lymphoma cells in vitro. And loss of PUMA (but not p21) impaired the regression of Eµ-Myc lymphomas induced by Nutlin3a in vivo.
Finally, the researchers found that PUMA contributed to Nutlin3a-induced apoptosis in myeloid leukemia, multiple myeloma, and Burkitt lymphoma cell lines.
The team noted that, because PUMA, a pro-apoptotic BH3-only protein, is critical for the therapeutic impact of Nutlin3a, it may be possible to boost the drug’s efficacy by combining it with BH3 mimetic drugs such as navitoclax or venetoclax. ![]()

Photo by Cameron Wells,
Walter and Eliza Hall
Institute of Medical Research
Research published in Cell Reports helps explain how the anticancer agent Nutlin3a fights lymphoma and other hematologic malignancies.
Nutlin3a is known to activate the tumor suppressor p53, but it hasn’t been clear exactly which p53 target genes are essential for the drug’s therapeutic activity.
The new research revealed that PUMA-mediated apoptosis—not p21-mediated cell-cycle arrest or senescence—is responsible for Nutlin3a’s therapeutic activity in lymphoid malignancies.
“By understanding how nutlins are killing cancer cells, we can begin to formulate their best possible use, including choosing the best partner drugs to combine the nutlins with,” said study author Andreas Strasser, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia.
With this study, Dr Strasser and his colleagues first found that Nutlin3a activates p53 target gene expression and causes cell-cycle arrest and apoptosis in non-transformed mouse lymphoid cells in vitro.
The team then showed that Nutlin3a-mediated killing of these cells requires PUMA but not p21. In vivo, loss of PUMA protected non-transformed mouse lymphoid cells against Nutlin3a-induced killing. Loss of p21 did not provide the same protection.
Next, the researchers found that malignant Eµ-Myc lymphoma cells were much more sensitive to Nutlin3a than were non-transformed lymphoid cells. In vitro experiments with Eµ-Myc lymphoma cells showed that Nutlin3a promotes p53 accumulation and downstream effector pathway activation.
As in previous experiments, PUMA (not p21) proved critical for Nutlin3a-induced killing of Eµ-Myc lymphoma cells in vitro. And loss of PUMA (but not p21) impaired the regression of Eµ-Myc lymphomas induced by Nutlin3a in vivo.
Finally, the researchers found that PUMA contributed to Nutlin3a-induced apoptosis in myeloid leukemia, multiple myeloma, and Burkitt lymphoma cell lines.
The team noted that, because PUMA, a pro-apoptotic BH3-only protein, is critical for the therapeutic impact of Nutlin3a, it may be possible to boost the drug’s efficacy by combining it with BH3 mimetic drugs such as navitoclax or venetoclax. ![]()

Photo by Cameron Wells,
Walter and Eliza Hall
Institute of Medical Research
Research published in Cell Reports helps explain how the anticancer agent Nutlin3a fights lymphoma and other hematologic malignancies.
Nutlin3a is known to activate the tumor suppressor p53, but it hasn’t been clear exactly which p53 target genes are essential for the drug’s therapeutic activity.
The new research revealed that PUMA-mediated apoptosis—not p21-mediated cell-cycle arrest or senescence—is responsible for Nutlin3a’s therapeutic activity in lymphoid malignancies.
“By understanding how nutlins are killing cancer cells, we can begin to formulate their best possible use, including choosing the best partner drugs to combine the nutlins with,” said study author Andreas Strasser, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia.
With this study, Dr Strasser and his colleagues first found that Nutlin3a activates p53 target gene expression and causes cell-cycle arrest and apoptosis in non-transformed mouse lymphoid cells in vitro.
The team then showed that Nutlin3a-mediated killing of these cells requires PUMA but not p21. In vivo, loss of PUMA protected non-transformed mouse lymphoid cells against Nutlin3a-induced killing. Loss of p21 did not provide the same protection.
Next, the researchers found that malignant Eµ-Myc lymphoma cells were much more sensitive to Nutlin3a than were non-transformed lymphoid cells. In vitro experiments with Eµ-Myc lymphoma cells showed that Nutlin3a promotes p53 accumulation and downstream effector pathway activation.
As in previous experiments, PUMA (not p21) proved critical for Nutlin3a-induced killing of Eµ-Myc lymphoma cells in vitro. And loss of PUMA (but not p21) impaired the regression of Eµ-Myc lymphomas induced by Nutlin3a in vivo.
Finally, the researchers found that PUMA contributed to Nutlin3a-induced apoptosis in myeloid leukemia, multiple myeloma, and Burkitt lymphoma cell lines.
The team noted that, because PUMA, a pro-apoptotic BH3-only protein, is critical for the therapeutic impact of Nutlin3a, it may be possible to boost the drug’s efficacy by combining it with BH3 mimetic drugs such as navitoclax or venetoclax. ![]()
Factors appear to confer poor survival in AML

receiving chemotherapy
Photo by Rhoda Baer
A study published in the British Journal of Hematology has revealed factors that appear to affect survival in patients with acute myeloid leukemia (AML).
The research showed that death was more likely among AML patients treated at centers not affiliated with the National Cancer Institute (NCI).
Death was also more likely for black patients, older patients, those without health insurance, and those who lived in poorer neighborhoods.
“Our study reveals that survival inequalities persist among vulnerable patients with acute myeloid leukemia, such as the uninsured, those of black race/ethnicity, and adolescents and young adults,” said study author Renata Abrahão, MD, of Cancer Prevention Institute of California.
“This study can serve as a baseline to compare changes in survival that may result from potential improvements in health insurance coverage following the implementation of the Affordable Care Act.”
Dr Abrahão and her colleagues analyzed 3935 AML patients who were 39 or younger between 1988 and 2011. The team used data from the California Cancer Registry, which participates in the Surveillance, Epidemiology and End Results program of the NCI.
The data revealed an increase over time in the 5-year survival rate, from 32.9% in 1988–1995 to 50% in 2004–2011. However, 58% of the patients (n=2272) died during follow-up. The overall median follow-up was 10 years, and the median time to death was 0.9 years.
A multivariate analysis revealed several subgroups of patients with worse survival.
Older patients had a greater risk of death when compared to patients ages 0 to 9. The hazard ratio (HR) was 1.23 for patients ages 10 to 19, 1.34 for patients ages 20 to 29, and 1.55 for patients ages 30 to 39.
Black patients had an increased risk of death as well. When compared with white patients, the HR was 1.27 for black patients, 1.05 for Hispanic patients, and 0.98 for Asian/Pacific Islanders.
Patients living in the neighborhoods with the lowest socioeconomic status had an HR of 1.14. And patients who received their initial care at a hospital not affiliated with the NCI had an HR of 1.18.
Health insurance information was only available for patients diagnosed from 1996 to 2011. Among these patients, the risk of death was higher among uninsured patients (HR=1.34) than among privately insured patients, but there was no difference between privately and publicly insured patients.
Explaining the findings
The researchers said AML diagnosis in older children, adolescents, and young adults may require more intensive treatment than in young children, which may lead to a higher probability of treatment-related complications. And recent studies have shown the biology of pediatric AML differs from adult AML, which may lead to a favorable prognosis in younger patients.
In addition, older children, adolescents, and young adults are less likely to participate in clinical trials and more likely to receive treatment at hospitals not affiliated with the NCI, when compared to younger children.
The researchers said it is not clear what factors accounted for the inferior survival observed among black patients. The team speculated that genetics may contribute to the difference in chemotherapy response or that black patients had less access to chemotherapy and other treatments such as hematopoietic stem cell transplant.
The association between lower socioeconomic status and death suggests a lack of access to treatment. The same can be said for the association between death and a lack of insurance.
“[T]his study showed that survival after AML remains low among young patients and highlights the need for new therapeutic regimens to treat this disease with various subtypes,” Dr Abrahão said.
“We emphasized the importance of linking population-based data with genetic and clinical information contained in the patients’ medical records in order to better understand the causes of survival inequalities.” ![]()

receiving chemotherapy
Photo by Rhoda Baer
A study published in the British Journal of Hematology has revealed factors that appear to affect survival in patients with acute myeloid leukemia (AML).
The research showed that death was more likely among AML patients treated at centers not affiliated with the National Cancer Institute (NCI).
Death was also more likely for black patients, older patients, those without health insurance, and those who lived in poorer neighborhoods.
“Our study reveals that survival inequalities persist among vulnerable patients with acute myeloid leukemia, such as the uninsured, those of black race/ethnicity, and adolescents and young adults,” said study author Renata Abrahão, MD, of Cancer Prevention Institute of California.
“This study can serve as a baseline to compare changes in survival that may result from potential improvements in health insurance coverage following the implementation of the Affordable Care Act.”
Dr Abrahão and her colleagues analyzed 3935 AML patients who were 39 or younger between 1988 and 2011. The team used data from the California Cancer Registry, which participates in the Surveillance, Epidemiology and End Results program of the NCI.
The data revealed an increase over time in the 5-year survival rate, from 32.9% in 1988–1995 to 50% in 2004–2011. However, 58% of the patients (n=2272) died during follow-up. The overall median follow-up was 10 years, and the median time to death was 0.9 years.
A multivariate analysis revealed several subgroups of patients with worse survival.
Older patients had a greater risk of death when compared to patients ages 0 to 9. The hazard ratio (HR) was 1.23 for patients ages 10 to 19, 1.34 for patients ages 20 to 29, and 1.55 for patients ages 30 to 39.
Black patients had an increased risk of death as well. When compared with white patients, the HR was 1.27 for black patients, 1.05 for Hispanic patients, and 0.98 for Asian/Pacific Islanders.
Patients living in the neighborhoods with the lowest socioeconomic status had an HR of 1.14. And patients who received their initial care at a hospital not affiliated with the NCI had an HR of 1.18.
Health insurance information was only available for patients diagnosed from 1996 to 2011. Among these patients, the risk of death was higher among uninsured patients (HR=1.34) than among privately insured patients, but there was no difference between privately and publicly insured patients.
Explaining the findings
The researchers said AML diagnosis in older children, adolescents, and young adults may require more intensive treatment than in young children, which may lead to a higher probability of treatment-related complications. And recent studies have shown the biology of pediatric AML differs from adult AML, which may lead to a favorable prognosis in younger patients.
In addition, older children, adolescents, and young adults are less likely to participate in clinical trials and more likely to receive treatment at hospitals not affiliated with the NCI, when compared to younger children.
The researchers said it is not clear what factors accounted for the inferior survival observed among black patients. The team speculated that genetics may contribute to the difference in chemotherapy response or that black patients had less access to chemotherapy and other treatments such as hematopoietic stem cell transplant.
The association between lower socioeconomic status and death suggests a lack of access to treatment. The same can be said for the association between death and a lack of insurance.
“[T]his study showed that survival after AML remains low among young patients and highlights the need for new therapeutic regimens to treat this disease with various subtypes,” Dr Abrahão said.
“We emphasized the importance of linking population-based data with genetic and clinical information contained in the patients’ medical records in order to better understand the causes of survival inequalities.” ![]()

receiving chemotherapy
Photo by Rhoda Baer
A study published in the British Journal of Hematology has revealed factors that appear to affect survival in patients with acute myeloid leukemia (AML).
The research showed that death was more likely among AML patients treated at centers not affiliated with the National Cancer Institute (NCI).
Death was also more likely for black patients, older patients, those without health insurance, and those who lived in poorer neighborhoods.
“Our study reveals that survival inequalities persist among vulnerable patients with acute myeloid leukemia, such as the uninsured, those of black race/ethnicity, and adolescents and young adults,” said study author Renata Abrahão, MD, of Cancer Prevention Institute of California.
“This study can serve as a baseline to compare changes in survival that may result from potential improvements in health insurance coverage following the implementation of the Affordable Care Act.”
Dr Abrahão and her colleagues analyzed 3935 AML patients who were 39 or younger between 1988 and 2011. The team used data from the California Cancer Registry, which participates in the Surveillance, Epidemiology and End Results program of the NCI.
The data revealed an increase over time in the 5-year survival rate, from 32.9% in 1988–1995 to 50% in 2004–2011. However, 58% of the patients (n=2272) died during follow-up. The overall median follow-up was 10 years, and the median time to death was 0.9 years.
A multivariate analysis revealed several subgroups of patients with worse survival.
Older patients had a greater risk of death when compared to patients ages 0 to 9. The hazard ratio (HR) was 1.23 for patients ages 10 to 19, 1.34 for patients ages 20 to 29, and 1.55 for patients ages 30 to 39.
Black patients had an increased risk of death as well. When compared with white patients, the HR was 1.27 for black patients, 1.05 for Hispanic patients, and 0.98 for Asian/Pacific Islanders.
Patients living in the neighborhoods with the lowest socioeconomic status had an HR of 1.14. And patients who received their initial care at a hospital not affiliated with the NCI had an HR of 1.18.
Health insurance information was only available for patients diagnosed from 1996 to 2011. Among these patients, the risk of death was higher among uninsured patients (HR=1.34) than among privately insured patients, but there was no difference between privately and publicly insured patients.
Explaining the findings
The researchers said AML diagnosis in older children, adolescents, and young adults may require more intensive treatment than in young children, which may lead to a higher probability of treatment-related complications. And recent studies have shown the biology of pediatric AML differs from adult AML, which may lead to a favorable prognosis in younger patients.
In addition, older children, adolescents, and young adults are less likely to participate in clinical trials and more likely to receive treatment at hospitals not affiliated with the NCI, when compared to younger children.
The researchers said it is not clear what factors accounted for the inferior survival observed among black patients. The team speculated that genetics may contribute to the difference in chemotherapy response or that black patients had less access to chemotherapy and other treatments such as hematopoietic stem cell transplant.
The association between lower socioeconomic status and death suggests a lack of access to treatment. The same can be said for the association between death and a lack of insurance.
“[T]his study showed that survival after AML remains low among young patients and highlights the need for new therapeutic regimens to treat this disease with various subtypes,” Dr Abrahão said.
“We emphasized the importance of linking population-based data with genetic and clinical information contained in the patients’ medical records in order to better understand the causes of survival inequalities.”
An extremely indolent T-cell leukemia: an 18-year follow-up
T-cell prolymphocytic leukemia (T-PLL) is a rare malignancy that comprises about 2% of all mature lymphoid neoplasms. Patients usually present with prominent peripheral blood lymphocytosis, splenomegaly, hepatomegaly, lymphadenopathy, B symptoms, and occasionally with skin lesions.1 The disease follows an aggressive clinical course with rapid progression and typically has a median survival of less than 1 year. In some cases, the disease is indolent for a period of time before becoming aggressive.2 In 2002, 7 years after initial diagnosis in 1995, the case discussed herein was reported as a rare, indolent form of T-PLL.3 We now present 11 additional years of follow-up of this case, during which time the patient remained asymptomatic with respect to his lymphoid neoplasm.
Click on the PDF icon at the top of this introduction to read the full article.
T-cell prolymphocytic leukemia (T-PLL) is a rare malignancy that comprises about 2% of all mature lymphoid neoplasms. Patients usually present with prominent peripheral blood lymphocytosis, splenomegaly, hepatomegaly, lymphadenopathy, B symptoms, and occasionally with skin lesions.1 The disease follows an aggressive clinical course with rapid progression and typically has a median survival of less than 1 year. In some cases, the disease is indolent for a period of time before becoming aggressive.2 In 2002, 7 years after initial diagnosis in 1995, the case discussed herein was reported as a rare, indolent form of T-PLL.3 We now present 11 additional years of follow-up of this case, during which time the patient remained asymptomatic with respect to his lymphoid neoplasm.
Click on the PDF icon at the top of this introduction to read the full article.
T-cell prolymphocytic leukemia (T-PLL) is a rare malignancy that comprises about 2% of all mature lymphoid neoplasms. Patients usually present with prominent peripheral blood lymphocytosis, splenomegaly, hepatomegaly, lymphadenopathy, B symptoms, and occasionally with skin lesions.1 The disease follows an aggressive clinical course with rapid progression and typically has a median survival of less than 1 year. In some cases, the disease is indolent for a period of time before becoming aggressive.2 In 2002, 7 years after initial diagnosis in 1995, the case discussed herein was reported as a rare, indolent form of T-PLL.3 We now present 11 additional years of follow-up of this case, during which time the patient remained asymptomatic with respect to his lymphoid neoplasm.
Click on the PDF icon at the top of this introduction to read the full article.
Prognostic value of complete remission with superior platelet counts in acute myeloid leukemia
Background Complete remission (CR) in acute myeloid leukemia (AML) is defined as having ≤5% leukemic blast cells in the bone marrow and return of normal hematopoiesis after the first induction cycle. There is a subset of patients, however, who achieve reduction of leukemic blast cells with a subnormal platelet count, designated as CR with incomplete platelet recovery (platelet count, ≤100,000/mcL; normal, 150,000-450,000/mcL), which is associated with inferior outcomes when compared with CR. Furthermore, there is another subset of patients with CR but superior platelet counts (≥400,000/mcL) whose prognostic significance is unclear.
Objective To establish whether CR with superior platelet counts is associated with better outcomes and can be used as a separate entity for prognostication.
Methods A retrospective chart review of 104 cases of AML was conducted. The highest platelet count during days 25-35 from initiation of induction chemotherapy (designated as day 30 platelet count) was documented. A multivariate analysis for other factors such as age, sex, risk categories, day 14+ plasma cell count (average plasma cell percentage at days 14-21), infections, allogeneic bone marrow transplant, and remission status was done.
Results Day 30 platelet count was found to be an independent predictor of survival in AML. On the multivariate analysis, the subgroup with superior platelet counts (≥400,000/mcL) was found to be associated with better outcomes.
Limitations Results need to be validated in a larger cohort.
Conclusions CR with superior platelet recovery (≥400,000/mcL) is a unique subcategory in itself and has prognostic significance. This may help better assess response to chemotherapeutic agents and aid in further decision-making regarding treatment.
Click on the PDF icon at the top of this introduction to read the full article.
Background Complete remission (CR) in acute myeloid leukemia (AML) is defined as having ≤5% leukemic blast cells in the bone marrow and return of normal hematopoiesis after the first induction cycle. There is a subset of patients, however, who achieve reduction of leukemic blast cells with a subnormal platelet count, designated as CR with incomplete platelet recovery (platelet count, ≤100,000/mcL; normal, 150,000-450,000/mcL), which is associated with inferior outcomes when compared with CR. Furthermore, there is another subset of patients with CR but superior platelet counts (≥400,000/mcL) whose prognostic significance is unclear.
Objective To establish whether CR with superior platelet counts is associated with better outcomes and can be used as a separate entity for prognostication.
Methods A retrospective chart review of 104 cases of AML was conducted. The highest platelet count during days 25-35 from initiation of induction chemotherapy (designated as day 30 platelet count) was documented. A multivariate analysis for other factors such as age, sex, risk categories, day 14+ plasma cell count (average plasma cell percentage at days 14-21), infections, allogeneic bone marrow transplant, and remission status was done.
Results Day 30 platelet count was found to be an independent predictor of survival in AML. On the multivariate analysis, the subgroup with superior platelet counts (≥400,000/mcL) was found to be associated with better outcomes.
Limitations Results need to be validated in a larger cohort.
Conclusions CR with superior platelet recovery (≥400,000/mcL) is a unique subcategory in itself and has prognostic significance. This may help better assess response to chemotherapeutic agents and aid in further decision-making regarding treatment.
Click on the PDF icon at the top of this introduction to read the full article.
Background Complete remission (CR) in acute myeloid leukemia (AML) is defined as having ≤5% leukemic blast cells in the bone marrow and return of normal hematopoiesis after the first induction cycle. There is a subset of patients, however, who achieve reduction of leukemic blast cells with a subnormal platelet count, designated as CR with incomplete platelet recovery (platelet count, ≤100,000/mcL; normal, 150,000-450,000/mcL), which is associated with inferior outcomes when compared with CR. Furthermore, there is another subset of patients with CR but superior platelet counts (≥400,000/mcL) whose prognostic significance is unclear.
Objective To establish whether CR with superior platelet counts is associated with better outcomes and can be used as a separate entity for prognostication.
Methods A retrospective chart review of 104 cases of AML was conducted. The highest platelet count during days 25-35 from initiation of induction chemotherapy (designated as day 30 platelet count) was documented. A multivariate analysis for other factors such as age, sex, risk categories, day 14+ plasma cell count (average plasma cell percentage at days 14-21), infections, allogeneic bone marrow transplant, and remission status was done.
Results Day 30 platelet count was found to be an independent predictor of survival in AML. On the multivariate analysis, the subgroup with superior platelet counts (≥400,000/mcL) was found to be associated with better outcomes.
Limitations Results need to be validated in a larger cohort.
Conclusions CR with superior platelet recovery (≥400,000/mcL) is a unique subcategory in itself and has prognostic significance. This may help better assess response to chemotherapeutic agents and aid in further decision-making regarding treatment.
Click on the PDF icon at the top of this introduction to read the full article.
Ponatinib effective in chronic phase CML regardless of baseline mutation status
In heavily pretreated patients with chronic phase chronic myeloid leukemia (CP-CML), response to the tyrosine kinase inhibitor ponatinib did not depend on baseline mutation status, and no single or compound mutation was a major driver of primary or secondary resistance to ponatinib, according to researchers.
Irrespective of baseline mutation status, responses to ponatinib were durable. As determined by next-generation sequencing (NGS), patients with zero, one, or two or more BCR-ABL1 mutations had rates of 50%-61% for major cytogenetic response (MCyR) by 1 year and 29%-45% for major molecular response (MMR) at any time. The rates were similar to those observed with mutation status determined by Sanger sequencing. Rates of sustained response at 2 years for MCyR and MMR were 87% and 65%, respectively (Blood. 2016 Feb 11. doi: 10.1182/blood-2015-08-660977).
Sanger sequencing typically is used to identify BCR-ABL1 mutations associated with tyrosine kinase inhibitor (TKI) resistance, but the method fails to detect low-level mutations that occur in less than 10%-20% of cells. Researchers used NGS to determine the impact of low-level mutations, as well as compound mutations, on the efficacy of the third generation TKI ponatinib.
Ponatinib is the most potent BCR-ABL1 TKI but is associated with considerable cardiovascular toxicity.
“The role of NGS in this setting may be to identify patients with (low level) T315I who are unlikely to derive lasting benefit from second-generation TKIs, but have a high likelihood of achieving durable cytogenetic and molecular responses to ponatinib, an important factor for balancing risks and benefits of salvage therapy selection,” wrote Dr. Michael W. Deininger, Chief of Hematology at the Huntsman Cancer Institute at the University of Utah, Salt Lake City, and his colleagues.
Patients with low-level mutations had similar response rates to those with no mutations: MCyR by one year and MMR at any time were 43% and 31%, respectively, compared with 50% and 29%. Response rates were higher in patients with compound mutations (64% and 52%) or one or more mutation (57% and 64%). The researchers speculated that the lower response rates in patients with low level or no mutations may reflect resistance mechanisms independent of BCR-ABL1.
Analysis of postbaseline samples from 127 patients (24 of whom had discontinued ponatinib for at least 1 month) determined the impact of acquired resistance. At a median follow-up of 30.1 months, emergence of previously undetected single and compound mutants during ponatinib therapy was observed in 8 patients.
The study analyzed patients from the PACE trial who had CP-CML with resistance or intolerance to dasatinib or nilotinib, or with a T315I mutation, and who were treated with ponatinib. All 267 patients had baseline mutation status determined by Sanger sequencing, with 161 mutations detected in 131 patients. NGS identified these and 105 additional mutations. Consistent with greater sensitivity of NGS, the proportion of patients with no baseline mutations by 39% by NGS vs. 51% by Sanger sequencing, and the proportion with multiple mutations was 23% vs. 10%.
The study was funded by ARIAD Pharmaceuticals. Dr. Deininger reported financial ties to ARIAD, Bristol Myers-Squibb, Novartis, Celgene, Genzyme, Gilead, Incyte, and Pfizer. Several of his coauthors reported ties to industry.
In heavily pretreated patients with chronic phase chronic myeloid leukemia (CP-CML), response to the tyrosine kinase inhibitor ponatinib did not depend on baseline mutation status, and no single or compound mutation was a major driver of primary or secondary resistance to ponatinib, according to researchers.
Irrespective of baseline mutation status, responses to ponatinib were durable. As determined by next-generation sequencing (NGS), patients with zero, one, or two or more BCR-ABL1 mutations had rates of 50%-61% for major cytogenetic response (MCyR) by 1 year and 29%-45% for major molecular response (MMR) at any time. The rates were similar to those observed with mutation status determined by Sanger sequencing. Rates of sustained response at 2 years for MCyR and MMR were 87% and 65%, respectively (Blood. 2016 Feb 11. doi: 10.1182/blood-2015-08-660977).
Sanger sequencing typically is used to identify BCR-ABL1 mutations associated with tyrosine kinase inhibitor (TKI) resistance, but the method fails to detect low-level mutations that occur in less than 10%-20% of cells. Researchers used NGS to determine the impact of low-level mutations, as well as compound mutations, on the efficacy of the third generation TKI ponatinib.
Ponatinib is the most potent BCR-ABL1 TKI but is associated with considerable cardiovascular toxicity.
“The role of NGS in this setting may be to identify patients with (low level) T315I who are unlikely to derive lasting benefit from second-generation TKIs, but have a high likelihood of achieving durable cytogenetic and molecular responses to ponatinib, an important factor for balancing risks and benefits of salvage therapy selection,” wrote Dr. Michael W. Deininger, Chief of Hematology at the Huntsman Cancer Institute at the University of Utah, Salt Lake City, and his colleagues.
Patients with low-level mutations had similar response rates to those with no mutations: MCyR by one year and MMR at any time were 43% and 31%, respectively, compared with 50% and 29%. Response rates were higher in patients with compound mutations (64% and 52%) or one or more mutation (57% and 64%). The researchers speculated that the lower response rates in patients with low level or no mutations may reflect resistance mechanisms independent of BCR-ABL1.
Analysis of postbaseline samples from 127 patients (24 of whom had discontinued ponatinib for at least 1 month) determined the impact of acquired resistance. At a median follow-up of 30.1 months, emergence of previously undetected single and compound mutants during ponatinib therapy was observed in 8 patients.
The study analyzed patients from the PACE trial who had CP-CML with resistance or intolerance to dasatinib or nilotinib, or with a T315I mutation, and who were treated with ponatinib. All 267 patients had baseline mutation status determined by Sanger sequencing, with 161 mutations detected in 131 patients. NGS identified these and 105 additional mutations. Consistent with greater sensitivity of NGS, the proportion of patients with no baseline mutations by 39% by NGS vs. 51% by Sanger sequencing, and the proportion with multiple mutations was 23% vs. 10%.
The study was funded by ARIAD Pharmaceuticals. Dr. Deininger reported financial ties to ARIAD, Bristol Myers-Squibb, Novartis, Celgene, Genzyme, Gilead, Incyte, and Pfizer. Several of his coauthors reported ties to industry.
In heavily pretreated patients with chronic phase chronic myeloid leukemia (CP-CML), response to the tyrosine kinase inhibitor ponatinib did not depend on baseline mutation status, and no single or compound mutation was a major driver of primary or secondary resistance to ponatinib, according to researchers.
Irrespective of baseline mutation status, responses to ponatinib were durable. As determined by next-generation sequencing (NGS), patients with zero, one, or two or more BCR-ABL1 mutations had rates of 50%-61% for major cytogenetic response (MCyR) by 1 year and 29%-45% for major molecular response (MMR) at any time. The rates were similar to those observed with mutation status determined by Sanger sequencing. Rates of sustained response at 2 years for MCyR and MMR were 87% and 65%, respectively (Blood. 2016 Feb 11. doi: 10.1182/blood-2015-08-660977).
Sanger sequencing typically is used to identify BCR-ABL1 mutations associated with tyrosine kinase inhibitor (TKI) resistance, but the method fails to detect low-level mutations that occur in less than 10%-20% of cells. Researchers used NGS to determine the impact of low-level mutations, as well as compound mutations, on the efficacy of the third generation TKI ponatinib.
Ponatinib is the most potent BCR-ABL1 TKI but is associated with considerable cardiovascular toxicity.
“The role of NGS in this setting may be to identify patients with (low level) T315I who are unlikely to derive lasting benefit from second-generation TKIs, but have a high likelihood of achieving durable cytogenetic and molecular responses to ponatinib, an important factor for balancing risks and benefits of salvage therapy selection,” wrote Dr. Michael W. Deininger, Chief of Hematology at the Huntsman Cancer Institute at the University of Utah, Salt Lake City, and his colleagues.
Patients with low-level mutations had similar response rates to those with no mutations: MCyR by one year and MMR at any time were 43% and 31%, respectively, compared with 50% and 29%. Response rates were higher in patients with compound mutations (64% and 52%) or one or more mutation (57% and 64%). The researchers speculated that the lower response rates in patients with low level or no mutations may reflect resistance mechanisms independent of BCR-ABL1.
Analysis of postbaseline samples from 127 patients (24 of whom had discontinued ponatinib for at least 1 month) determined the impact of acquired resistance. At a median follow-up of 30.1 months, emergence of previously undetected single and compound mutants during ponatinib therapy was observed in 8 patients.
The study analyzed patients from the PACE trial who had CP-CML with resistance or intolerance to dasatinib or nilotinib, or with a T315I mutation, and who were treated with ponatinib. All 267 patients had baseline mutation status determined by Sanger sequencing, with 161 mutations detected in 131 patients. NGS identified these and 105 additional mutations. Consistent with greater sensitivity of NGS, the proportion of patients with no baseline mutations by 39% by NGS vs. 51% by Sanger sequencing, and the proportion with multiple mutations was 23% vs. 10%.
The study was funded by ARIAD Pharmaceuticals. Dr. Deininger reported financial ties to ARIAD, Bristol Myers-Squibb, Novartis, Celgene, Genzyme, Gilead, Incyte, and Pfizer. Several of his coauthors reported ties to industry.
FROM BLOOD
Key clinical point: Baseline mutation status had little impact on ponatinib response, and no single or compound mutation was a major driver of primary or secondary resistance to ponatinib in patients with chronic phase chronic myeloid leukemia (CP-CML).
Major finding: In patients with zero, one, or two or more BCR-ABL1 mutations at baseline by next-generation sequencing were 50%-61% for major cytogenetic response (MCyR) by 1 year and 29%-45% for major molecular response (MMR) at any time; rates of sustained response at 2 years for MCyR and MMR were 87% and 65%, respectively.
Data source: From the PACE trial, 267 patients with CP-CML with resistance or intolerance to dasatinib or nilotinib, or with a T315I mutation, were treated with ponatinib.
Disclosures: The study was funded by ARIAD Pharmaceuticals. Dr. Deininger reported financial ties to ARIAD, Bristol Myers-Squibb, Novartis, Celgene, Genzyme, Gilead, Incyte, and Pfizer. Several of his coauthors reported ties to industry.