User login
Targeting enzymes to treat leukemias

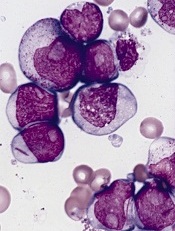
Credit: Volker Brinkmann
Enzymes linked to diabetes and obesity appear to play key roles in arthritis and leukemia, according to research published in Cell Metabolism.
Working with mice, researchers discovered that the same enzymes involved in turning carbohydrates into the building blocks of fats also influence the health of neutrophils.
“The link between these enzymes and neutrophils was a big surprise,” said study author Irfan J. Lodhi, PhD, of the Washington University School of Medicine in St. Louis.
“We had never thought about treating rheumatoid arthritis or leukemia by targeting enzymes that produce fatty acids, but this work supports that line of thinking.”
In the study, mice that couldn’t make enzymes needed to produce a certain type of fat abruptly lost weight and developed extremely low white blood cell counts, with very few neutrophils. Without this fat, called an ether lipid, neutrophils died.
That discovery could lead to the targeting of ether lipids as a way to reduce the number of neutrophils in inflammatory diseases and leukemias. The researchers believe limiting, rather than eliminating, ether lipids may be the best approach because neutrophils are important infection fighters.
“This may be a pathway to limit inflammation,” said study author Clay F. Semenkovich, MD, also of the Washington University School of Medicine.
“If we could reduce the activity of these enzymes without eliminating them entirely, it could lower the levels of ether lipids and potentially help patients with leukemia and inflammatory diseases such as arthritis.”
Dr Semenkovich said the enzymes specifically target neutrophils without affecting other immune cells, “so ether lipids appear to be a very precise target.”
The researchers also learned that inactivating the enzymes didn’t harm the precursors of neutrophils; only mature neutrophils were killed.
That could mean strategies to limit the production of ether lipids might lower neutrophil levels only temporarily so that when treatment stops, a patient’s neutrophil count would gradually rise, allowing the immune system to return to normal. ![]()

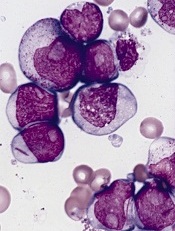
Credit: Volker Brinkmann
Enzymes linked to diabetes and obesity appear to play key roles in arthritis and leukemia, according to research published in Cell Metabolism.
Working with mice, researchers discovered that the same enzymes involved in turning carbohydrates into the building blocks of fats also influence the health of neutrophils.
“The link between these enzymes and neutrophils was a big surprise,” said study author Irfan J. Lodhi, PhD, of the Washington University School of Medicine in St. Louis.
“We had never thought about treating rheumatoid arthritis or leukemia by targeting enzymes that produce fatty acids, but this work supports that line of thinking.”
In the study, mice that couldn’t make enzymes needed to produce a certain type of fat abruptly lost weight and developed extremely low white blood cell counts, with very few neutrophils. Without this fat, called an ether lipid, neutrophils died.
That discovery could lead to the targeting of ether lipids as a way to reduce the number of neutrophils in inflammatory diseases and leukemias. The researchers believe limiting, rather than eliminating, ether lipids may be the best approach because neutrophils are important infection fighters.
“This may be a pathway to limit inflammation,” said study author Clay F. Semenkovich, MD, also of the Washington University School of Medicine.
“If we could reduce the activity of these enzymes without eliminating them entirely, it could lower the levels of ether lipids and potentially help patients with leukemia and inflammatory diseases such as arthritis.”
Dr Semenkovich said the enzymes specifically target neutrophils without affecting other immune cells, “so ether lipids appear to be a very precise target.”
The researchers also learned that inactivating the enzymes didn’t harm the precursors of neutrophils; only mature neutrophils were killed.
That could mean strategies to limit the production of ether lipids might lower neutrophil levels only temporarily so that when treatment stops, a patient’s neutrophil count would gradually rise, allowing the immune system to return to normal. ![]()

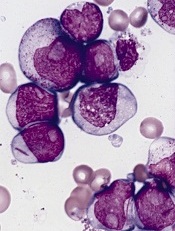
Credit: Volker Brinkmann
Enzymes linked to diabetes and obesity appear to play key roles in arthritis and leukemia, according to research published in Cell Metabolism.
Working with mice, researchers discovered that the same enzymes involved in turning carbohydrates into the building blocks of fats also influence the health of neutrophils.
“The link between these enzymes and neutrophils was a big surprise,” said study author Irfan J. Lodhi, PhD, of the Washington University School of Medicine in St. Louis.
“We had never thought about treating rheumatoid arthritis or leukemia by targeting enzymes that produce fatty acids, but this work supports that line of thinking.”
In the study, mice that couldn’t make enzymes needed to produce a certain type of fat abruptly lost weight and developed extremely low white blood cell counts, with very few neutrophils. Without this fat, called an ether lipid, neutrophils died.
That discovery could lead to the targeting of ether lipids as a way to reduce the number of neutrophils in inflammatory diseases and leukemias. The researchers believe limiting, rather than eliminating, ether lipids may be the best approach because neutrophils are important infection fighters.
“This may be a pathway to limit inflammation,” said study author Clay F. Semenkovich, MD, also of the Washington University School of Medicine.
“If we could reduce the activity of these enzymes without eliminating them entirely, it could lower the levels of ether lipids and potentially help patients with leukemia and inflammatory diseases such as arthritis.”
Dr Semenkovich said the enzymes specifically target neutrophils without affecting other immune cells, “so ether lipids appear to be a very precise target.”
The researchers also learned that inactivating the enzymes didn’t harm the precursors of neutrophils; only mature neutrophils were killed.
That could mean strategies to limit the production of ether lipids might lower neutrophil levels only temporarily so that when treatment stops, a patient’s neutrophil count would gradually rise, allowing the immune system to return to normal. ![]()
Maintenance prolongs PFS, not OS, in relapsed CLL

Credit: Linda Bartlett
SAN FRANCISCO—Maintenance therapy with the anti-CD20 monoclonal antibody ofatumumab improves progression-free survival (PFS), but not overall survival (OS), in patients with relapsed chronic lymphocytic leukemia (CLL), according to an interim analysis of the PROLONG study.
The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance (P<0.0001).
But there was no significant difference in the median OS, which was not reached in either treatment arm.
Marinus H.J. van Oers, MD, PhD, of the Academisch Medisch Centrum and HOVON in Amsterdam, The Netherlands, reported these results at the 2014 ASH Annual Meeting (abstract 21*). The study was sponsored by GlaxoSmithKline, makers of ofatumumab.
“[A]s of 2014, still we cannot say that we are able to cure CLL,” Dr van Oers noted. “And CLL is characterized by decreasing response duration with subsequent lines of treatment. In this respect, but also a number of other respects, there are similarities in biological behavior between CLL and follicular lymphoma.”
“There is definitely a role—although it’s somewhat debated—for maintenance treatment in follicular lymphoma. Therefore, it is rational to explore safe and effective maintenance treatment in CLL as well.”
To that end, Dr van Oers and his colleagues compared ofatumumab maintenance to observation in patients who were in remission after induction treatment for relapsed CLL. The team enrolled 474 patients who were in complete or partial remission after their 2nd- or 3rd-line treatment for CLL.
Patients were randomized to observation (n=236) or to receive ofatumumab (n=238) at 300 mg, followed 1 week later by 1000 mg every 8 weeks for up to 2 years. Patients on ofatumumab also received premedication with acetaminophen, antihistamine, and glucocorticoid.
The patients were stratified by the number and type of prior therapy, as well as remission status after induction treatment, and baseline characteristics were similar between the two treatment arms.
“The median age was about 65, and about 30% of patients were older than 70 years,” Dr van Oers noted. “[There was] a male preponderance, as you would expect, and the time since diagnosis was somewhere between 5 and 6 years.”
“Most patients were in [partial response], actually 80%, and most patients had received 2 prior regimens, about 70%. As for prior treatments, 80% of patients had received effective immuno-chemotherapy.”
“In both arms, there were only a few patients with unfavorable cytogenetics—11q and 17p deletion. [As for] β2 microglobulin, two-thirds [of patients in both arms] had low levels. And, in both arms, there were almost twice as many IGVH-mutated as unmutated patients.”
Patient outcomes
The median follow-up was 19.1 months. The study’s primary endpoint was PFS, which was defined as the time from randomization to the date of disease progression or death from any cause.
The median PFS was significantly longer in the ofatumumab arm than in the observation arm, at 29.4 months and 15.2 months, respectively (hazard ratio [HR]=0.50; P<0.0001).
Similarly, the time to the start of patients’ next therapy was significantly longer in the ofatumumab arm than in the in observation arm—a median of 38 months and 31.1 months, respectively (HR=0.66, P=0.108).
However, there was no significant difference in OS, which was not reached in either arm (HR=0.85, P=0.4877).
Adverse events (AEs) occurred in 86% of patients in the ofatumumab arm and 72% of patients in the observation arm (P<0.001). Sixty percent of AEs were considered related to ofatumumab. None of the AEs led to study withdrawal.
Grade 3 or higher AEs occurred in 46% of patients in the ofatumumab arm and 28% in the observation arm. They included neutropenia (24% and 10%, respectively; P<0.001), infections (13% and 8%, respectively), thrombocytopenia (2% and 3%, respectively), and infusion-related reactions (1% and 0%, respectively).
There were 5 deaths in the observation arm—1 due to progression and 4 due to causes other than progression, infection, or secondary malignancy. There were 2 deaths in the ofatumumab arm—1 due to infection/sepsis and 1 due to an “other” cause.
“So based on this planned interim analysis, we can conclude that ofatumumab maintenance in relapsed CLL results in a highly significant and clinically meaningful improvement of progression-free survival,” Dr van Oers said in closing.
“It significantly prolongs time to next treatment, it’s well-tolerated, and it’s associated with an adverse event profile which is quite characteristic of anti-CD20 monoclonal antibodies.” ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Linda Bartlett
SAN FRANCISCO—Maintenance therapy with the anti-CD20 monoclonal antibody ofatumumab improves progression-free survival (PFS), but not overall survival (OS), in patients with relapsed chronic lymphocytic leukemia (CLL), according to an interim analysis of the PROLONG study.
The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance (P<0.0001).
But there was no significant difference in the median OS, which was not reached in either treatment arm.
Marinus H.J. van Oers, MD, PhD, of the Academisch Medisch Centrum and HOVON in Amsterdam, The Netherlands, reported these results at the 2014 ASH Annual Meeting (abstract 21*). The study was sponsored by GlaxoSmithKline, makers of ofatumumab.
“[A]s of 2014, still we cannot say that we are able to cure CLL,” Dr van Oers noted. “And CLL is characterized by decreasing response duration with subsequent lines of treatment. In this respect, but also a number of other respects, there are similarities in biological behavior between CLL and follicular lymphoma.”
“There is definitely a role—although it’s somewhat debated—for maintenance treatment in follicular lymphoma. Therefore, it is rational to explore safe and effective maintenance treatment in CLL as well.”
To that end, Dr van Oers and his colleagues compared ofatumumab maintenance to observation in patients who were in remission after induction treatment for relapsed CLL. The team enrolled 474 patients who were in complete or partial remission after their 2nd- or 3rd-line treatment for CLL.
Patients were randomized to observation (n=236) or to receive ofatumumab (n=238) at 300 mg, followed 1 week later by 1000 mg every 8 weeks for up to 2 years. Patients on ofatumumab also received premedication with acetaminophen, antihistamine, and glucocorticoid.
The patients were stratified by the number and type of prior therapy, as well as remission status after induction treatment, and baseline characteristics were similar between the two treatment arms.
“The median age was about 65, and about 30% of patients were older than 70 years,” Dr van Oers noted. “[There was] a male preponderance, as you would expect, and the time since diagnosis was somewhere between 5 and 6 years.”
“Most patients were in [partial response], actually 80%, and most patients had received 2 prior regimens, about 70%. As for prior treatments, 80% of patients had received effective immuno-chemotherapy.”
“In both arms, there were only a few patients with unfavorable cytogenetics—11q and 17p deletion. [As for] β2 microglobulin, two-thirds [of patients in both arms] had low levels. And, in both arms, there were almost twice as many IGVH-mutated as unmutated patients.”
Patient outcomes
The median follow-up was 19.1 months. The study’s primary endpoint was PFS, which was defined as the time from randomization to the date of disease progression or death from any cause.
The median PFS was significantly longer in the ofatumumab arm than in the observation arm, at 29.4 months and 15.2 months, respectively (hazard ratio [HR]=0.50; P<0.0001).
Similarly, the time to the start of patients’ next therapy was significantly longer in the ofatumumab arm than in the in observation arm—a median of 38 months and 31.1 months, respectively (HR=0.66, P=0.108).
However, there was no significant difference in OS, which was not reached in either arm (HR=0.85, P=0.4877).
Adverse events (AEs) occurred in 86% of patients in the ofatumumab arm and 72% of patients in the observation arm (P<0.001). Sixty percent of AEs were considered related to ofatumumab. None of the AEs led to study withdrawal.
Grade 3 or higher AEs occurred in 46% of patients in the ofatumumab arm and 28% in the observation arm. They included neutropenia (24% and 10%, respectively; P<0.001), infections (13% and 8%, respectively), thrombocytopenia (2% and 3%, respectively), and infusion-related reactions (1% and 0%, respectively).
There were 5 deaths in the observation arm—1 due to progression and 4 due to causes other than progression, infection, or secondary malignancy. There were 2 deaths in the ofatumumab arm—1 due to infection/sepsis and 1 due to an “other” cause.
“So based on this planned interim analysis, we can conclude that ofatumumab maintenance in relapsed CLL results in a highly significant and clinically meaningful improvement of progression-free survival,” Dr van Oers said in closing.
“It significantly prolongs time to next treatment, it’s well-tolerated, and it’s associated with an adverse event profile which is quite characteristic of anti-CD20 monoclonal antibodies.” ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Linda Bartlett
SAN FRANCISCO—Maintenance therapy with the anti-CD20 monoclonal antibody ofatumumab improves progression-free survival (PFS), but not overall survival (OS), in patients with relapsed chronic lymphocytic leukemia (CLL), according to an interim analysis of the PROLONG study.
The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance (P<0.0001).
But there was no significant difference in the median OS, which was not reached in either treatment arm.
Marinus H.J. van Oers, MD, PhD, of the Academisch Medisch Centrum and HOVON in Amsterdam, The Netherlands, reported these results at the 2014 ASH Annual Meeting (abstract 21*). The study was sponsored by GlaxoSmithKline, makers of ofatumumab.
“[A]s of 2014, still we cannot say that we are able to cure CLL,” Dr van Oers noted. “And CLL is characterized by decreasing response duration with subsequent lines of treatment. In this respect, but also a number of other respects, there are similarities in biological behavior between CLL and follicular lymphoma.”
“There is definitely a role—although it’s somewhat debated—for maintenance treatment in follicular lymphoma. Therefore, it is rational to explore safe and effective maintenance treatment in CLL as well.”
To that end, Dr van Oers and his colleagues compared ofatumumab maintenance to observation in patients who were in remission after induction treatment for relapsed CLL. The team enrolled 474 patients who were in complete or partial remission after their 2nd- or 3rd-line treatment for CLL.
Patients were randomized to observation (n=236) or to receive ofatumumab (n=238) at 300 mg, followed 1 week later by 1000 mg every 8 weeks for up to 2 years. Patients on ofatumumab also received premedication with acetaminophen, antihistamine, and glucocorticoid.
The patients were stratified by the number and type of prior therapy, as well as remission status after induction treatment, and baseline characteristics were similar between the two treatment arms.
“The median age was about 65, and about 30% of patients were older than 70 years,” Dr van Oers noted. “[There was] a male preponderance, as you would expect, and the time since diagnosis was somewhere between 5 and 6 years.”
“Most patients were in [partial response], actually 80%, and most patients had received 2 prior regimens, about 70%. As for prior treatments, 80% of patients had received effective immuno-chemotherapy.”
“In both arms, there were only a few patients with unfavorable cytogenetics—11q and 17p deletion. [As for] β2 microglobulin, two-thirds [of patients in both arms] had low levels. And, in both arms, there were almost twice as many IGVH-mutated as unmutated patients.”
Patient outcomes
The median follow-up was 19.1 months. The study’s primary endpoint was PFS, which was defined as the time from randomization to the date of disease progression or death from any cause.
The median PFS was significantly longer in the ofatumumab arm than in the observation arm, at 29.4 months and 15.2 months, respectively (hazard ratio [HR]=0.50; P<0.0001).
Similarly, the time to the start of patients’ next therapy was significantly longer in the ofatumumab arm than in the in observation arm—a median of 38 months and 31.1 months, respectively (HR=0.66, P=0.108).
However, there was no significant difference in OS, which was not reached in either arm (HR=0.85, P=0.4877).
Adverse events (AEs) occurred in 86% of patients in the ofatumumab arm and 72% of patients in the observation arm (P<0.001). Sixty percent of AEs were considered related to ofatumumab. None of the AEs led to study withdrawal.
Grade 3 or higher AEs occurred in 46% of patients in the ofatumumab arm and 28% in the observation arm. They included neutropenia (24% and 10%, respectively; P<0.001), infections (13% and 8%, respectively), thrombocytopenia (2% and 3%, respectively), and infusion-related reactions (1% and 0%, respectively).
There were 5 deaths in the observation arm—1 due to progression and 4 due to causes other than progression, infection, or secondary malignancy. There were 2 deaths in the ofatumumab arm—1 due to infection/sepsis and 1 due to an “other” cause.
“So based on this planned interim analysis, we can conclude that ofatumumab maintenance in relapsed CLL results in a highly significant and clinically meaningful improvement of progression-free survival,” Dr van Oers said in closing.
“It significantly prolongs time to next treatment, it’s well-tolerated, and it’s associated with an adverse event profile which is quite characteristic of anti-CD20 monoclonal antibodies.” ![]()
*Information in the abstract differs from that presented at the meeting.
Ibrutinib proves active in high-risk CLL

Credit: Mary Ann Thompson
Single-agent ibrutinib can elicit a high response rate in patients with high-risk chronic lymphocytic leukemia (CLL), results of a phase 2 trial suggest.
The Bruton’s tyrosine kinase inhibitor prompted a 92% objective response rate in patients who had previously untreated or relapsed/refractory CLL with either 17p deletion (del 17p) or tumor protein 53 (TP53) aberrations.
Researchers reported this and other results of the trial in The Lancet Oncology.
“Ibrutinib treatment results observed in CLL patients with del 17p or TP53 aberrations are very encouraging given that these patients have a high relapse rate after chemotherapy and are in need of tolerable, effective, and durable treatment options,” said study author Mohammed Farooqui, DO, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland.
He and his colleagues studied 51 patients in this trial, 35 with previously untreated CLL and 16 with relapsed or refractory CLL. Forty-seven of the patients (92%) had del 17p, and 4 patients carried the TP53 aberration but did not have del 17p.
The study’s primary endpoint was overall response rate after 24 weeks. Secondary endpoints included safety, overall survival, progression-free survival, best response, and nodal response.
The median follow-up for all patients was 24 months (15 months for the previously untreated cohort). At 24 weeks, 48 patients were evaluable for response, assessed according to the modified IWCLL 2008 criteria.
Response rates
At 24 weeks, 92% (n=44) of the 48 evaluable patients achieved an objective response. Fifty percent of all evaluable patients achieved a partial response (n=24)—55% of previously untreated patients (n=18) and 40% of relapsed/refractory patients (n=6).
As for best response, 10% of all patients achieved a complete response (n=5)—12% of previously untreated patients (n=4) and 7% of relapsed/refractory patients (n=1). And 67% of patients had a partial response (n=32)—70% of previously untreated patients (n=23) and 60% of relapsed/refractory patients (n=9).
After 8 weeks on therapy, ibrutinib was associated with a more than 50% mean reduction in tumor burden in the bone marrow (44%), lymph nodes (70%), and spleen (79%). After 24 weeks of therapy, the rates of tumor burden reduction (> 50%) increased to 83%, 93%, and 95%, respectively.
Survival and safety
The estimated progression-free survival at 24 months for all patients on an intention-to-treat basis was 82%. Forty-two of the 51 patients (82%) continued on ibrutinib treatment without disease progression.
The estimated overall survival at 24 months was 80% for all patients—84% for previously untreated patients and 74% for patients with relapsed or refractory disease.
At the final follow-up, 8 (16%) patients had died—5 (10%) from progressive disease, 2 (4%) from infection, and 1 (2%) patient with a sudden, unexplained death that may have been treatment-related.
The most common adverse events (occurring in more than 30% of all patients) potentially related to ibrutinib were arthralgia (59%), diarrhea (51%), rash (47%), nail ridging (43%), bruising (33%), and muscle spasms (31%).
The most frequent grade 3 or 4 hematologic adverse events were neutropenia (24%), anemia (14%), and thrombocytopenia (10%). The most common nonhematologic grade 3 adverse event was pneumonia, which occurred in 3 patients (6%).
Nine patients (18%) discontinued treatment. The reasons for discontinuation included disease progression in 5 patients (10%) and death for 3 patients (6%).
This research was sponsored by the Intramural Research Program of the National Heart, Lung, and Blood Institute and the National Cancer Institute; Danish Cancer Society; Novo Nordisk Foundation; National Institutes of Health Medical Research Scholars Program; and Pharmacyclics Inc.
Ibrutinib is jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc. ![]()

Credit: Mary Ann Thompson
Single-agent ibrutinib can elicit a high response rate in patients with high-risk chronic lymphocytic leukemia (CLL), results of a phase 2 trial suggest.
The Bruton’s tyrosine kinase inhibitor prompted a 92% objective response rate in patients who had previously untreated or relapsed/refractory CLL with either 17p deletion (del 17p) or tumor protein 53 (TP53) aberrations.
Researchers reported this and other results of the trial in The Lancet Oncology.
“Ibrutinib treatment results observed in CLL patients with del 17p or TP53 aberrations are very encouraging given that these patients have a high relapse rate after chemotherapy and are in need of tolerable, effective, and durable treatment options,” said study author Mohammed Farooqui, DO, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland.
He and his colleagues studied 51 patients in this trial, 35 with previously untreated CLL and 16 with relapsed or refractory CLL. Forty-seven of the patients (92%) had del 17p, and 4 patients carried the TP53 aberration but did not have del 17p.
The study’s primary endpoint was overall response rate after 24 weeks. Secondary endpoints included safety, overall survival, progression-free survival, best response, and nodal response.
The median follow-up for all patients was 24 months (15 months for the previously untreated cohort). At 24 weeks, 48 patients were evaluable for response, assessed according to the modified IWCLL 2008 criteria.
Response rates
At 24 weeks, 92% (n=44) of the 48 evaluable patients achieved an objective response. Fifty percent of all evaluable patients achieved a partial response (n=24)—55% of previously untreated patients (n=18) and 40% of relapsed/refractory patients (n=6).
As for best response, 10% of all patients achieved a complete response (n=5)—12% of previously untreated patients (n=4) and 7% of relapsed/refractory patients (n=1). And 67% of patients had a partial response (n=32)—70% of previously untreated patients (n=23) and 60% of relapsed/refractory patients (n=9).
After 8 weeks on therapy, ibrutinib was associated with a more than 50% mean reduction in tumor burden in the bone marrow (44%), lymph nodes (70%), and spleen (79%). After 24 weeks of therapy, the rates of tumor burden reduction (> 50%) increased to 83%, 93%, and 95%, respectively.
Survival and safety
The estimated progression-free survival at 24 months for all patients on an intention-to-treat basis was 82%. Forty-two of the 51 patients (82%) continued on ibrutinib treatment without disease progression.
The estimated overall survival at 24 months was 80% for all patients—84% for previously untreated patients and 74% for patients with relapsed or refractory disease.
At the final follow-up, 8 (16%) patients had died—5 (10%) from progressive disease, 2 (4%) from infection, and 1 (2%) patient with a sudden, unexplained death that may have been treatment-related.
The most common adverse events (occurring in more than 30% of all patients) potentially related to ibrutinib were arthralgia (59%), diarrhea (51%), rash (47%), nail ridging (43%), bruising (33%), and muscle spasms (31%).
The most frequent grade 3 or 4 hematologic adverse events were neutropenia (24%), anemia (14%), and thrombocytopenia (10%). The most common nonhematologic grade 3 adverse event was pneumonia, which occurred in 3 patients (6%).
Nine patients (18%) discontinued treatment. The reasons for discontinuation included disease progression in 5 patients (10%) and death for 3 patients (6%).
This research was sponsored by the Intramural Research Program of the National Heart, Lung, and Blood Institute and the National Cancer Institute; Danish Cancer Society; Novo Nordisk Foundation; National Institutes of Health Medical Research Scholars Program; and Pharmacyclics Inc.
Ibrutinib is jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc. ![]()

Credit: Mary Ann Thompson
Single-agent ibrutinib can elicit a high response rate in patients with high-risk chronic lymphocytic leukemia (CLL), results of a phase 2 trial suggest.
The Bruton’s tyrosine kinase inhibitor prompted a 92% objective response rate in patients who had previously untreated or relapsed/refractory CLL with either 17p deletion (del 17p) or tumor protein 53 (TP53) aberrations.
Researchers reported this and other results of the trial in The Lancet Oncology.
“Ibrutinib treatment results observed in CLL patients with del 17p or TP53 aberrations are very encouraging given that these patients have a high relapse rate after chemotherapy and are in need of tolerable, effective, and durable treatment options,” said study author Mohammed Farooqui, DO, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland.
He and his colleagues studied 51 patients in this trial, 35 with previously untreated CLL and 16 with relapsed or refractory CLL. Forty-seven of the patients (92%) had del 17p, and 4 patients carried the TP53 aberration but did not have del 17p.
The study’s primary endpoint was overall response rate after 24 weeks. Secondary endpoints included safety, overall survival, progression-free survival, best response, and nodal response.
The median follow-up for all patients was 24 months (15 months for the previously untreated cohort). At 24 weeks, 48 patients were evaluable for response, assessed according to the modified IWCLL 2008 criteria.
Response rates
At 24 weeks, 92% (n=44) of the 48 evaluable patients achieved an objective response. Fifty percent of all evaluable patients achieved a partial response (n=24)—55% of previously untreated patients (n=18) and 40% of relapsed/refractory patients (n=6).
As for best response, 10% of all patients achieved a complete response (n=5)—12% of previously untreated patients (n=4) and 7% of relapsed/refractory patients (n=1). And 67% of patients had a partial response (n=32)—70% of previously untreated patients (n=23) and 60% of relapsed/refractory patients (n=9).
After 8 weeks on therapy, ibrutinib was associated with a more than 50% mean reduction in tumor burden in the bone marrow (44%), lymph nodes (70%), and spleen (79%). After 24 weeks of therapy, the rates of tumor burden reduction (> 50%) increased to 83%, 93%, and 95%, respectively.
Survival and safety
The estimated progression-free survival at 24 months for all patients on an intention-to-treat basis was 82%. Forty-two of the 51 patients (82%) continued on ibrutinib treatment without disease progression.
The estimated overall survival at 24 months was 80% for all patients—84% for previously untreated patients and 74% for patients with relapsed or refractory disease.
At the final follow-up, 8 (16%) patients had died—5 (10%) from progressive disease, 2 (4%) from infection, and 1 (2%) patient with a sudden, unexplained death that may have been treatment-related.
The most common adverse events (occurring in more than 30% of all patients) potentially related to ibrutinib were arthralgia (59%), diarrhea (51%), rash (47%), nail ridging (43%), bruising (33%), and muscle spasms (31%).
The most frequent grade 3 or 4 hematologic adverse events were neutropenia (24%), anemia (14%), and thrombocytopenia (10%). The most common nonhematologic grade 3 adverse event was pneumonia, which occurred in 3 patients (6%).
Nine patients (18%) discontinued treatment. The reasons for discontinuation included disease progression in 5 patients (10%) and death for 3 patients (6%).
This research was sponsored by the Intramural Research Program of the National Heart, Lung, and Blood Institute and the National Cancer Institute; Danish Cancer Society; Novo Nordisk Foundation; National Institutes of Health Medical Research Scholars Program; and Pharmacyclics Inc.
Ibrutinib is jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc. ![]()
Anti-CD38 antibodies poised to transform myeloma treatment
SAN FRANCISCO – Combining anti-CD38 monoclonal antibodies with standard antimyeloma therapies proved highly active without excessive toxicity in newly diagnosed as well as relapsed or refractory multiple myeloma in a pair of phase Ib studies.
“These anti-CD38 antibodies are the next blockbuster class of agents,” Dr. Thomas Martin III, lead author of one of the studies, said during a press briefing at the annual meeting of the American Society of Hematology. “These are the next agents that are really going to show some benefit for myeloma patients. And the next 5 years are going to be really fun moving them from the refractory setting to the less refractory setting to the frontline setting.”
Three agents are in development that target CD38, a cell surface glycoprotein that is strongly expressed in multiple myeloma. All three – daratumumab, SAR650984, and MOR202 – bind to a different part of the anti-CD39 receptor, but “whether that makes any clinical difference, we certainly don’t know at this point in time,” said Dr. Martin of the University of California, San Francisco.
Immunomodulatory drugs (IMiDs) and proteasome inhibitors (PI) are the current blockbuster agents in myeloma and have advanced overall survival from about 3 years to 7-10 years. But all patients still relapse after IMiD and PI failure, and survival outcomes remain poor at a median of about 9 months for those with advanced relapsed/refractory disease. Further, myeloma has failed to respond like the B-cell lymphomas to anti-CD20 antibodies such as rituximab (Rituxan).
Dr. Martin and his associates launched a phase Ib dose-escalation trial to evaluate SAR650984 in combination with standard doses of lenalidomide (Revlimid) and dexamethasone in adults with relapsed or refractory multiple myeloma failing at least two prior therapies.
SAR650984 was given intravenously on days 1 and 15 of a 28-day cycle at 3 mg/kg to 4 patients (cohort 1), 5 mg/kg to 3 patients (cohort 2), and 10 mg/kg to 6 patients (cohort 3) plus an additional 18 patients in an expansion cohort.
All 31 patients were heavily pretreated, with 94% previously treated with lenalidomide or bortezomib (Velcade), 29% with pomalidomide (Pomalyst), and 48% with carfilzomib (Kyprolis). Many (84%) were considered double refractory, or relapsed and refractory, to their last IMiD therapy, Dr. Martin reported.
Despite this, nearly two-thirds (58%) had a response, including two stringent complete responses, seven very good partial responses, and nine partial responses. The overall response rate (ORR) was 25% in cohort 1, 67% in cohort 2, and 63% at the 10-mg dose level or double what was seen as a single agent, he said. The clinical benefit rates were 50%, 67%, and 67%.
In addition, the ORR was 50% in patients who were IMiD relapsed and refractory and 33% in patients pomalidomide relapsed and refractory, he reported.
At 9 months’ follow-up, median progression-free survival was 6.2 months and had not been reached in patients who received fewer than three lines of prior therapy.
The most common treatment-related adverse events were infusion reactions, fatigue, nausea, upper respiratory tract infection, and diarrhea. Infusion reactions occurred about a third of the time, typically in the first or second cycle, and were mostly mild (grade 1 or 2), Dr. Martin said. Only two patients discontinued treatment because of infusion reactions, one for a serious grade 3 anaphylactic reaction in cycle 1 and the other for a nonserious grade 3 maculopapular rash in cycle 2.
Daratumumab
The second highlighted study looked at the benefit and safety of adding daratumumab to commonly used backbone regimens in patients with newly diagnosed, relapsed, or treatment-resistant myeloma.
Single-agent daratumumab has shown activity in prior studies and received breakthrough therapy designation in May 2013 for patients with multiple myeloma after at least three prior lines of therapy including a proteasome inhibitor and an IMiD or those double refractory to a PI and IMiD.
In the four-arm, open-label study, daratumumab was given at a starting dose of 16 mg/kg in combination with bortezomib-dexamethasone (VD), bortezomib-thalidomide-dexamethasone (VTD), bortezomib-melphalan-prednisone (VMP), and pomalidomide-dexamethasone (POM-D). Treatment was for 18 three-week cycles or until transplantation in the VD and VTD arms, for 9 six-week cycles in the VMP arm, and was given in four-week cycles until disease progression in the POM-D arm.
Newly diagnosed patients were included in the VD and VTD arms irrespective of transplant eligibility, while patients in the VMP arm were newly diagnosed and transplant ineligible. Patients in the POM-D arm were relapsed/refractory to two or more lines of therapy including two consecutive cycles of lenalidomide and bortezomib. In all, 24 patients were evaluable for efficacy.
The ORR in newly diagnosed patients was 100%, including partial responses and very good partial responses, and 50% in the relapsed group, including one complete response, study coauthor Dr. María-Victoria Mateos said at the briefing.
Daratumumab does not appear to have a negative effect on stem cell mobilization, with five patients electively taken off study for autologous stem cell transplantation after cycle 4.
Three of the seven patients in the POM-D arm dropped out (one because of physician decision and two because of disease progression).
The addition of daratumumab to the various backbones was well tolerated in all evaluable patients and did not result in significant additional toxicity, said Dr. Mateos of University Hospital of Salamanca, Spain.
Adverse events possibly or probably related to daratumumab included one grade 3 neutropenia in the VD arm, one grade 3 thrombocytopenia in the VMP arm, and one serious infectious pneumonia in the POM-D arm. There were a few infusion-related reactions, but most were grade 1 or 2 and occurred within the first infusions, she said.
“This is a very new and exciting concept in multiple myeloma, as we are seeing that combining this precision approach with the standard of care is leading to more effective treatment without increased toxicity,” Dr. Philippe Moreau, lead study author, of University Hospital of Nantes, France, said in a statement. “By targeting a simple molecule expressed by the cancer cells, this therapy has the potential to become a potent addition to conventional treatment.”
Dr. Brad S. Kahl, press briefing moderator, of the University of Wisconsin-Madison, was enthusiastic about the potential for anti-CD38 antibodies to transform the treatment of multiple myeloma.
“Obviously it’s very, very early, probably too early to plant a victory flag in the ground,” he said. “Having said that, the early data is very promising and totally justifies all the comments about bringing these drugs forward, aggressively moving them into the front line.”
Phase III studies are ongoing or will be initiated shortly with daratumumab plus VD in relapsed myeloma (MMY3004-CASTOR), with VMP in non–transplant eligible patients (MMY3007-ALCYONE), and with VTD as induction therapy (MMY3006/IFM-HOVON-CASSIOPEIA).
SAN FRANCISCO – Combining anti-CD38 monoclonal antibodies with standard antimyeloma therapies proved highly active without excessive toxicity in newly diagnosed as well as relapsed or refractory multiple myeloma in a pair of phase Ib studies.
“These anti-CD38 antibodies are the next blockbuster class of agents,” Dr. Thomas Martin III, lead author of one of the studies, said during a press briefing at the annual meeting of the American Society of Hematology. “These are the next agents that are really going to show some benefit for myeloma patients. And the next 5 years are going to be really fun moving them from the refractory setting to the less refractory setting to the frontline setting.”
Three agents are in development that target CD38, a cell surface glycoprotein that is strongly expressed in multiple myeloma. All three – daratumumab, SAR650984, and MOR202 – bind to a different part of the anti-CD39 receptor, but “whether that makes any clinical difference, we certainly don’t know at this point in time,” said Dr. Martin of the University of California, San Francisco.
Immunomodulatory drugs (IMiDs) and proteasome inhibitors (PI) are the current blockbuster agents in myeloma and have advanced overall survival from about 3 years to 7-10 years. But all patients still relapse after IMiD and PI failure, and survival outcomes remain poor at a median of about 9 months for those with advanced relapsed/refractory disease. Further, myeloma has failed to respond like the B-cell lymphomas to anti-CD20 antibodies such as rituximab (Rituxan).
Dr. Martin and his associates launched a phase Ib dose-escalation trial to evaluate SAR650984 in combination with standard doses of lenalidomide (Revlimid) and dexamethasone in adults with relapsed or refractory multiple myeloma failing at least two prior therapies.
SAR650984 was given intravenously on days 1 and 15 of a 28-day cycle at 3 mg/kg to 4 patients (cohort 1), 5 mg/kg to 3 patients (cohort 2), and 10 mg/kg to 6 patients (cohort 3) plus an additional 18 patients in an expansion cohort.
All 31 patients were heavily pretreated, with 94% previously treated with lenalidomide or bortezomib (Velcade), 29% with pomalidomide (Pomalyst), and 48% with carfilzomib (Kyprolis). Many (84%) were considered double refractory, or relapsed and refractory, to their last IMiD therapy, Dr. Martin reported.
Despite this, nearly two-thirds (58%) had a response, including two stringent complete responses, seven very good partial responses, and nine partial responses. The overall response rate (ORR) was 25% in cohort 1, 67% in cohort 2, and 63% at the 10-mg dose level or double what was seen as a single agent, he said. The clinical benefit rates were 50%, 67%, and 67%.
In addition, the ORR was 50% in patients who were IMiD relapsed and refractory and 33% in patients pomalidomide relapsed and refractory, he reported.
At 9 months’ follow-up, median progression-free survival was 6.2 months and had not been reached in patients who received fewer than three lines of prior therapy.
The most common treatment-related adverse events were infusion reactions, fatigue, nausea, upper respiratory tract infection, and diarrhea. Infusion reactions occurred about a third of the time, typically in the first or second cycle, and were mostly mild (grade 1 or 2), Dr. Martin said. Only two patients discontinued treatment because of infusion reactions, one for a serious grade 3 anaphylactic reaction in cycle 1 and the other for a nonserious grade 3 maculopapular rash in cycle 2.
Daratumumab
The second highlighted study looked at the benefit and safety of adding daratumumab to commonly used backbone regimens in patients with newly diagnosed, relapsed, or treatment-resistant myeloma.
Single-agent daratumumab has shown activity in prior studies and received breakthrough therapy designation in May 2013 for patients with multiple myeloma after at least three prior lines of therapy including a proteasome inhibitor and an IMiD or those double refractory to a PI and IMiD.
In the four-arm, open-label study, daratumumab was given at a starting dose of 16 mg/kg in combination with bortezomib-dexamethasone (VD), bortezomib-thalidomide-dexamethasone (VTD), bortezomib-melphalan-prednisone (VMP), and pomalidomide-dexamethasone (POM-D). Treatment was for 18 three-week cycles or until transplantation in the VD and VTD arms, for 9 six-week cycles in the VMP arm, and was given in four-week cycles until disease progression in the POM-D arm.
Newly diagnosed patients were included in the VD and VTD arms irrespective of transplant eligibility, while patients in the VMP arm were newly diagnosed and transplant ineligible. Patients in the POM-D arm were relapsed/refractory to two or more lines of therapy including two consecutive cycles of lenalidomide and bortezomib. In all, 24 patients were evaluable for efficacy.
The ORR in newly diagnosed patients was 100%, including partial responses and very good partial responses, and 50% in the relapsed group, including one complete response, study coauthor Dr. María-Victoria Mateos said at the briefing.
Daratumumab does not appear to have a negative effect on stem cell mobilization, with five patients electively taken off study for autologous stem cell transplantation after cycle 4.
Three of the seven patients in the POM-D arm dropped out (one because of physician decision and two because of disease progression).
The addition of daratumumab to the various backbones was well tolerated in all evaluable patients and did not result in significant additional toxicity, said Dr. Mateos of University Hospital of Salamanca, Spain.
Adverse events possibly or probably related to daratumumab included one grade 3 neutropenia in the VD arm, one grade 3 thrombocytopenia in the VMP arm, and one serious infectious pneumonia in the POM-D arm. There were a few infusion-related reactions, but most were grade 1 or 2 and occurred within the first infusions, she said.
“This is a very new and exciting concept in multiple myeloma, as we are seeing that combining this precision approach with the standard of care is leading to more effective treatment without increased toxicity,” Dr. Philippe Moreau, lead study author, of University Hospital of Nantes, France, said in a statement. “By targeting a simple molecule expressed by the cancer cells, this therapy has the potential to become a potent addition to conventional treatment.”
Dr. Brad S. Kahl, press briefing moderator, of the University of Wisconsin-Madison, was enthusiastic about the potential for anti-CD38 antibodies to transform the treatment of multiple myeloma.
“Obviously it’s very, very early, probably too early to plant a victory flag in the ground,” he said. “Having said that, the early data is very promising and totally justifies all the comments about bringing these drugs forward, aggressively moving them into the front line.”
Phase III studies are ongoing or will be initiated shortly with daratumumab plus VD in relapsed myeloma (MMY3004-CASTOR), with VMP in non–transplant eligible patients (MMY3007-ALCYONE), and with VTD as induction therapy (MMY3006/IFM-HOVON-CASSIOPEIA).
SAN FRANCISCO – Combining anti-CD38 monoclonal antibodies with standard antimyeloma therapies proved highly active without excessive toxicity in newly diagnosed as well as relapsed or refractory multiple myeloma in a pair of phase Ib studies.
“These anti-CD38 antibodies are the next blockbuster class of agents,” Dr. Thomas Martin III, lead author of one of the studies, said during a press briefing at the annual meeting of the American Society of Hematology. “These are the next agents that are really going to show some benefit for myeloma patients. And the next 5 years are going to be really fun moving them from the refractory setting to the less refractory setting to the frontline setting.”
Three agents are in development that target CD38, a cell surface glycoprotein that is strongly expressed in multiple myeloma. All three – daratumumab, SAR650984, and MOR202 – bind to a different part of the anti-CD39 receptor, but “whether that makes any clinical difference, we certainly don’t know at this point in time,” said Dr. Martin of the University of California, San Francisco.
Immunomodulatory drugs (IMiDs) and proteasome inhibitors (PI) are the current blockbuster agents in myeloma and have advanced overall survival from about 3 years to 7-10 years. But all patients still relapse after IMiD and PI failure, and survival outcomes remain poor at a median of about 9 months for those with advanced relapsed/refractory disease. Further, myeloma has failed to respond like the B-cell lymphomas to anti-CD20 antibodies such as rituximab (Rituxan).
Dr. Martin and his associates launched a phase Ib dose-escalation trial to evaluate SAR650984 in combination with standard doses of lenalidomide (Revlimid) and dexamethasone in adults with relapsed or refractory multiple myeloma failing at least two prior therapies.
SAR650984 was given intravenously on days 1 and 15 of a 28-day cycle at 3 mg/kg to 4 patients (cohort 1), 5 mg/kg to 3 patients (cohort 2), and 10 mg/kg to 6 patients (cohort 3) plus an additional 18 patients in an expansion cohort.
All 31 patients were heavily pretreated, with 94% previously treated with lenalidomide or bortezomib (Velcade), 29% with pomalidomide (Pomalyst), and 48% with carfilzomib (Kyprolis). Many (84%) were considered double refractory, or relapsed and refractory, to their last IMiD therapy, Dr. Martin reported.
Despite this, nearly two-thirds (58%) had a response, including two stringent complete responses, seven very good partial responses, and nine partial responses. The overall response rate (ORR) was 25% in cohort 1, 67% in cohort 2, and 63% at the 10-mg dose level or double what was seen as a single agent, he said. The clinical benefit rates were 50%, 67%, and 67%.
In addition, the ORR was 50% in patients who were IMiD relapsed and refractory and 33% in patients pomalidomide relapsed and refractory, he reported.
At 9 months’ follow-up, median progression-free survival was 6.2 months and had not been reached in patients who received fewer than three lines of prior therapy.
The most common treatment-related adverse events were infusion reactions, fatigue, nausea, upper respiratory tract infection, and diarrhea. Infusion reactions occurred about a third of the time, typically in the first or second cycle, and were mostly mild (grade 1 or 2), Dr. Martin said. Only two patients discontinued treatment because of infusion reactions, one for a serious grade 3 anaphylactic reaction in cycle 1 and the other for a nonserious grade 3 maculopapular rash in cycle 2.
Daratumumab
The second highlighted study looked at the benefit and safety of adding daratumumab to commonly used backbone regimens in patients with newly diagnosed, relapsed, or treatment-resistant myeloma.
Single-agent daratumumab has shown activity in prior studies and received breakthrough therapy designation in May 2013 for patients with multiple myeloma after at least three prior lines of therapy including a proteasome inhibitor and an IMiD or those double refractory to a PI and IMiD.
In the four-arm, open-label study, daratumumab was given at a starting dose of 16 mg/kg in combination with bortezomib-dexamethasone (VD), bortezomib-thalidomide-dexamethasone (VTD), bortezomib-melphalan-prednisone (VMP), and pomalidomide-dexamethasone (POM-D). Treatment was for 18 three-week cycles or until transplantation in the VD and VTD arms, for 9 six-week cycles in the VMP arm, and was given in four-week cycles until disease progression in the POM-D arm.
Newly diagnosed patients were included in the VD and VTD arms irrespective of transplant eligibility, while patients in the VMP arm were newly diagnosed and transplant ineligible. Patients in the POM-D arm were relapsed/refractory to two or more lines of therapy including two consecutive cycles of lenalidomide and bortezomib. In all, 24 patients were evaluable for efficacy.
The ORR in newly diagnosed patients was 100%, including partial responses and very good partial responses, and 50% in the relapsed group, including one complete response, study coauthor Dr. María-Victoria Mateos said at the briefing.
Daratumumab does not appear to have a negative effect on stem cell mobilization, with five patients electively taken off study for autologous stem cell transplantation after cycle 4.
Three of the seven patients in the POM-D arm dropped out (one because of physician decision and two because of disease progression).
The addition of daratumumab to the various backbones was well tolerated in all evaluable patients and did not result in significant additional toxicity, said Dr. Mateos of University Hospital of Salamanca, Spain.
Adverse events possibly or probably related to daratumumab included one grade 3 neutropenia in the VD arm, one grade 3 thrombocytopenia in the VMP arm, and one serious infectious pneumonia in the POM-D arm. There were a few infusion-related reactions, but most were grade 1 or 2 and occurred within the first infusions, she said.
“This is a very new and exciting concept in multiple myeloma, as we are seeing that combining this precision approach with the standard of care is leading to more effective treatment without increased toxicity,” Dr. Philippe Moreau, lead study author, of University Hospital of Nantes, France, said in a statement. “By targeting a simple molecule expressed by the cancer cells, this therapy has the potential to become a potent addition to conventional treatment.”
Dr. Brad S. Kahl, press briefing moderator, of the University of Wisconsin-Madison, was enthusiastic about the potential for anti-CD38 antibodies to transform the treatment of multiple myeloma.
“Obviously it’s very, very early, probably too early to plant a victory flag in the ground,” he said. “Having said that, the early data is very promising and totally justifies all the comments about bringing these drugs forward, aggressively moving them into the front line.”
Phase III studies are ongoing or will be initiated shortly with daratumumab plus VD in relapsed myeloma (MMY3004-CASTOR), with VMP in non–transplant eligible patients (MMY3007-ALCYONE), and with VTD as induction therapy (MMY3006/IFM-HOVON-CASSIOPEIA).
AT ASH 2014
Key clinical point: The investigational anti-CD38 antibodies SAR650984 and daratumumab in combination with standard regimens were highly active in untreated and relapsed/refractory multiple myeloma.
Major finding: Overall response rates were 58% in patients treated with SAR650984, and 100% and 50%, respectively, in newly diagnosed and relapsed patients given daratumumab.
Data source: Two phase Ib studies in patients with newly diagnosed or relapsed/refractory multiple myeloma.
Disclosures: Sanofi Oncology sponsored the SAR650984 study. Dr. Martin reported research funding from Sanofi and serving as a speaker for Novartis. Genmab sponsored the daratumumab study. Dr. Mateos and Dr. Moreau reported ties with Janssen. Dr. Kahl reported ties with numerous drug companies.
Certain cancers primarily result from ‘bad luck’
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates. ![]()
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates. ![]()
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates. ![]()
CARs come in different makes and models

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics. ![]()

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics. ![]()

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics. ![]()
CAR is feasible in majority of ALL patients, team says

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant. ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant. ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant. ![]()
*Information in the abstract differs from that presented at the meeting.
CAR produces durable responses in B-cell ALL

Credit: Charles Haymond
SAN FRANCISCO—JCAR015, a chimeric antigen receptor (CAR) T-cell therapy, can produce durable responses in patients with B-cell acute lymphoblastic leukemia (ALL) who do not undergo subsequent hematopoietic stem cell transplant (HSCT), new research suggests.
JCAR015 consists of autologous T cells genetically modified to express 19-28z chimeric antigen receptor (19-28z CAR) targeting CD19.
Jae H. Park, MD, of Memorial Sloan Kettering Cancer Center in New York, presented data on JCAR015 at the 2014 ASH Annual Meeting (abstract 382).* The study is sponsored by Memorial Sloan Kettering, but funding has also been provided by Juno Therapeutics, the company developing JCAR015.
JCAR015 was tested at a dose of 1 - 3 x 106 CAR cells/kg in 33 adults with relapsed/refractory B-cell ALL. Twenty-eight patients were evaluable for toxicity, 27 for response, and 5 patients were too early in their treatment to evaluate at the time of data cutoff.
Twenty-one patients were male, and the median age was 55 (range, 23 to 74).
Thirteen patients (46%) had minimal disease (<5% blasts) immediately prior to T-cell infusion, and 15 patients (54%) had morphologic disease of 5% to 100% blasts (median 63%).
Eighteen patients (64%) had received 2 prior lines of therapy, and 5 (18%) each had 3 or more prior lines.
Eight patients (29%) underwent prior allogeneic HSCT, 9 patients (32%) were Philadelphia chromosome positive (Ph+), and 3 (11%) had the T315I mutation.
The overall complete response (CR) rate was 89%, and the minimal residual disease-negative CR rate was 88%. The median time to CR was 22.5 days (range, 9 to 33).
The investigators performed a subgroup analysis and found that 100% of the 13 patients with minimal disease before therapy achieved a CR, compared to 79% of patients with morphologic disease.
Eighty-six percent (6/7) of patients who had a prior HSCT and 90% (18/20) without a prior HSCT achieved a CR. Eighty-nine percent (8/9) of Ph+ patients achieved a CR, and 89% (16/18) of Philadelphia-negative patients (89%) achieved a CR.
At a median follow-up of 6 months (range, 1 to 38 months), 12 patients remained disease-free, including 7 patients who had more than a year of follow-up. Seven patients are disease-free without a subsequent HSCT.
Nine patients relapsed during a follow-up of 3 to 8 months, and 10 patients proceeded to HSCT. Two relapses occurred after HSCT, one in a patient who had CD19-negative blasts, and 7 relapses occurred without HSCT.
The overall survival rate at 6 months was 57%, and the median survival was 8.5 months.
For those patients who had a transplant after CAR therapy, the median survival was 10.8 months, and the survival rate at 6 months was 68%.
Dr Park pointed out that maximum T-cell expansion occurred between days 7 and 14 and correlated with the occurrence of cytokine release syndrome (CRS). The T cells persisted for 1 to 3 months following infusion.
The main adverse events were those associated with CRS and neurologic changes. Severe CRS requiring vasopressors or mechanical ventilation occurred in 5 patients (18%) overall and in 5 patients (33%) with morphologic disease before therapy. Severe CRS did not occur in any patient with minimal disease before therapy.
Grade 3 or 4 neurotoxicity occurred in 7 patients (25%) overall, in 6 patients (40%) with morphologic disease, and in 1 with minimal disease (8%) before therapy.
The investigators observed no graft-vs-host disease exacerbation, and CRS was managed with an IL-6R inhibitor, steroids, or both.
Dr Park noted that the neurologic symptoms are reversible and can occur independently of CRS.
He also pointed out that CR rates were similar regardless of different disease risk factors, and that durable responses have been achieved in patients who did not have a subsequent HSCT. ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Charles Haymond
SAN FRANCISCO—JCAR015, a chimeric antigen receptor (CAR) T-cell therapy, can produce durable responses in patients with B-cell acute lymphoblastic leukemia (ALL) who do not undergo subsequent hematopoietic stem cell transplant (HSCT), new research suggests.
JCAR015 consists of autologous T cells genetically modified to express 19-28z chimeric antigen receptor (19-28z CAR) targeting CD19.
Jae H. Park, MD, of Memorial Sloan Kettering Cancer Center in New York, presented data on JCAR015 at the 2014 ASH Annual Meeting (abstract 382).* The study is sponsored by Memorial Sloan Kettering, but funding has also been provided by Juno Therapeutics, the company developing JCAR015.
JCAR015 was tested at a dose of 1 - 3 x 106 CAR cells/kg in 33 adults with relapsed/refractory B-cell ALL. Twenty-eight patients were evaluable for toxicity, 27 for response, and 5 patients were too early in their treatment to evaluate at the time of data cutoff.
Twenty-one patients were male, and the median age was 55 (range, 23 to 74).
Thirteen patients (46%) had minimal disease (<5% blasts) immediately prior to T-cell infusion, and 15 patients (54%) had morphologic disease of 5% to 100% blasts (median 63%).
Eighteen patients (64%) had received 2 prior lines of therapy, and 5 (18%) each had 3 or more prior lines.
Eight patients (29%) underwent prior allogeneic HSCT, 9 patients (32%) were Philadelphia chromosome positive (Ph+), and 3 (11%) had the T315I mutation.
The overall complete response (CR) rate was 89%, and the minimal residual disease-negative CR rate was 88%. The median time to CR was 22.5 days (range, 9 to 33).
The investigators performed a subgroup analysis and found that 100% of the 13 patients with minimal disease before therapy achieved a CR, compared to 79% of patients with morphologic disease.
Eighty-six percent (6/7) of patients who had a prior HSCT and 90% (18/20) without a prior HSCT achieved a CR. Eighty-nine percent (8/9) of Ph+ patients achieved a CR, and 89% (16/18) of Philadelphia-negative patients (89%) achieved a CR.
At a median follow-up of 6 months (range, 1 to 38 months), 12 patients remained disease-free, including 7 patients who had more than a year of follow-up. Seven patients are disease-free without a subsequent HSCT.
Nine patients relapsed during a follow-up of 3 to 8 months, and 10 patients proceeded to HSCT. Two relapses occurred after HSCT, one in a patient who had CD19-negative blasts, and 7 relapses occurred without HSCT.
The overall survival rate at 6 months was 57%, and the median survival was 8.5 months.
For those patients who had a transplant after CAR therapy, the median survival was 10.8 months, and the survival rate at 6 months was 68%.
Dr Park pointed out that maximum T-cell expansion occurred between days 7 and 14 and correlated with the occurrence of cytokine release syndrome (CRS). The T cells persisted for 1 to 3 months following infusion.
The main adverse events were those associated with CRS and neurologic changes. Severe CRS requiring vasopressors or mechanical ventilation occurred in 5 patients (18%) overall and in 5 patients (33%) with morphologic disease before therapy. Severe CRS did not occur in any patient with minimal disease before therapy.
Grade 3 or 4 neurotoxicity occurred in 7 patients (25%) overall, in 6 patients (40%) with morphologic disease, and in 1 with minimal disease (8%) before therapy.
The investigators observed no graft-vs-host disease exacerbation, and CRS was managed with an IL-6R inhibitor, steroids, or both.
Dr Park noted that the neurologic symptoms are reversible and can occur independently of CRS.
He also pointed out that CR rates were similar regardless of different disease risk factors, and that durable responses have been achieved in patients who did not have a subsequent HSCT. ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Charles Haymond
SAN FRANCISCO—JCAR015, a chimeric antigen receptor (CAR) T-cell therapy, can produce durable responses in patients with B-cell acute lymphoblastic leukemia (ALL) who do not undergo subsequent hematopoietic stem cell transplant (HSCT), new research suggests.
JCAR015 consists of autologous T cells genetically modified to express 19-28z chimeric antigen receptor (19-28z CAR) targeting CD19.
Jae H. Park, MD, of Memorial Sloan Kettering Cancer Center in New York, presented data on JCAR015 at the 2014 ASH Annual Meeting (abstract 382).* The study is sponsored by Memorial Sloan Kettering, but funding has also been provided by Juno Therapeutics, the company developing JCAR015.
JCAR015 was tested at a dose of 1 - 3 x 106 CAR cells/kg in 33 adults with relapsed/refractory B-cell ALL. Twenty-eight patients were evaluable for toxicity, 27 for response, and 5 patients were too early in their treatment to evaluate at the time of data cutoff.
Twenty-one patients were male, and the median age was 55 (range, 23 to 74).
Thirteen patients (46%) had minimal disease (<5% blasts) immediately prior to T-cell infusion, and 15 patients (54%) had morphologic disease of 5% to 100% blasts (median 63%).
Eighteen patients (64%) had received 2 prior lines of therapy, and 5 (18%) each had 3 or more prior lines.
Eight patients (29%) underwent prior allogeneic HSCT, 9 patients (32%) were Philadelphia chromosome positive (Ph+), and 3 (11%) had the T315I mutation.
The overall complete response (CR) rate was 89%, and the minimal residual disease-negative CR rate was 88%. The median time to CR was 22.5 days (range, 9 to 33).
The investigators performed a subgroup analysis and found that 100% of the 13 patients with minimal disease before therapy achieved a CR, compared to 79% of patients with morphologic disease.
Eighty-six percent (6/7) of patients who had a prior HSCT and 90% (18/20) without a prior HSCT achieved a CR. Eighty-nine percent (8/9) of Ph+ patients achieved a CR, and 89% (16/18) of Philadelphia-negative patients (89%) achieved a CR.
At a median follow-up of 6 months (range, 1 to 38 months), 12 patients remained disease-free, including 7 patients who had more than a year of follow-up. Seven patients are disease-free without a subsequent HSCT.
Nine patients relapsed during a follow-up of 3 to 8 months, and 10 patients proceeded to HSCT. Two relapses occurred after HSCT, one in a patient who had CD19-negative blasts, and 7 relapses occurred without HSCT.
The overall survival rate at 6 months was 57%, and the median survival was 8.5 months.
For those patients who had a transplant after CAR therapy, the median survival was 10.8 months, and the survival rate at 6 months was 68%.
Dr Park pointed out that maximum T-cell expansion occurred between days 7 and 14 and correlated with the occurrence of cytokine release syndrome (CRS). The T cells persisted for 1 to 3 months following infusion.
The main adverse events were those associated with CRS and neurologic changes. Severe CRS requiring vasopressors or mechanical ventilation occurred in 5 patients (18%) overall and in 5 patients (33%) with morphologic disease before therapy. Severe CRS did not occur in any patient with minimal disease before therapy.
Grade 3 or 4 neurotoxicity occurred in 7 patients (25%) overall, in 6 patients (40%) with morphologic disease, and in 1 with minimal disease (8%) before therapy.
The investigators observed no graft-vs-host disease exacerbation, and CRS was managed with an IL-6R inhibitor, steroids, or both.
Dr Park noted that the neurologic symptoms are reversible and can occur independently of CRS.
He also pointed out that CR rates were similar regardless of different disease risk factors, and that durable responses have been achieved in patients who did not have a subsequent HSCT.
*Information in the abstract differs from that presented at the meeting.
New data added to obinutuzumab label

Credit: Bill Branson
The US Food and Drug Administration (FDA) has approved a supplemental biologics license application for obinutuzumab (Gazyva) in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia (CLL).
The approval adds to the drug’s label data from stage 2 of the CLL11 study, which showed that obinutuzumab plus chlorambucil offers significant clinical improvements when compared head-to-head with rituximab plus chlorambucil.
This includes progression-free survival (PFS), complete response (CR), and minimal residual disease (MRD) data from stage 2 of the study. In addition, overall survival data was added from stage 1, in which researchers compared obinutuzumab plus chlorambucil to chlorambucil alone.
The label now reflects that obinutuzumab plus chlorambucil improved PFS compared to rituximab plus chlorambucil. The median PFS was 26.7 months and 14.9 months, respectively (hazard ratio=0.42, P<0.0001).
Additionally, obinutuzumab plus chlorambucil nearly tripled the CR rate when compared to rituximab plus chlorambucil. The CR rates were 26.1% and 8.8%, respectively.
Of the patients who achieved a CR with or without complete recovery from abnormal blood cell counts, 19% (18/94) of patients in the obinutuzumab arm and 6% (2/34) in the rituximab arm were MRD negative in the bone marrow.
Forty-one percent (39/94) of patients in the obinutuzumab arm and 12% (4/34) in the rituximab arm were MRD-negative in the peripheral blood.
At nearly 2 years, the rate of death was 9% (22/238) for patients who received obinutuzumab plus chlorambucil and 20% (24/118) for those who received chlorambucil alone (hazard ratio=0.41). The median overall survival has not yet been reached.
About obinutuzumab
Obinutuzumab is an engineered monoclonal antibody designed to attach to CD20 on B cells. The drug attacks targeted cells both directly and together with the body’s immune system.
The prescribing information for obinutuzumab includes warnings that the drug can cause serious or life-threatening side effects. These include hepatitis B reactivation, progressive multifocal leukoencephalopathy, infusion reactions, tumor lysis syndrome, infections, and neutropenia.
The most common side effects of the drug are infusion reactions, neutropenia, thrombocytopenia, anemia, fever, cough, nausea, and diarrhea.
Obinutuzumab was FDA-approved for use in combination with chlorambucil to treat previously untreated CLL in November 2013. The drug (which is known as Gazyvaro in Europe) was approved by the European Commission for the same indication in July 2014.
Obinutuzumab was discovered by Roche Glycart AG, an independent research unit of Roche. In the US, the drug is part of a collaboration between Genentech and Biogen Idec.

Credit: Bill Branson
The US Food and Drug Administration (FDA) has approved a supplemental biologics license application for obinutuzumab (Gazyva) in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia (CLL).
The approval adds to the drug’s label data from stage 2 of the CLL11 study, which showed that obinutuzumab plus chlorambucil offers significant clinical improvements when compared head-to-head with rituximab plus chlorambucil.
This includes progression-free survival (PFS), complete response (CR), and minimal residual disease (MRD) data from stage 2 of the study. In addition, overall survival data was added from stage 1, in which researchers compared obinutuzumab plus chlorambucil to chlorambucil alone.
The label now reflects that obinutuzumab plus chlorambucil improved PFS compared to rituximab plus chlorambucil. The median PFS was 26.7 months and 14.9 months, respectively (hazard ratio=0.42, P<0.0001).
Additionally, obinutuzumab plus chlorambucil nearly tripled the CR rate when compared to rituximab plus chlorambucil. The CR rates were 26.1% and 8.8%, respectively.
Of the patients who achieved a CR with or without complete recovery from abnormal blood cell counts, 19% (18/94) of patients in the obinutuzumab arm and 6% (2/34) in the rituximab arm were MRD negative in the bone marrow.
Forty-one percent (39/94) of patients in the obinutuzumab arm and 12% (4/34) in the rituximab arm were MRD-negative in the peripheral blood.
At nearly 2 years, the rate of death was 9% (22/238) for patients who received obinutuzumab plus chlorambucil and 20% (24/118) for those who received chlorambucil alone (hazard ratio=0.41). The median overall survival has not yet been reached.
About obinutuzumab
Obinutuzumab is an engineered monoclonal antibody designed to attach to CD20 on B cells. The drug attacks targeted cells both directly and together with the body’s immune system.
The prescribing information for obinutuzumab includes warnings that the drug can cause serious or life-threatening side effects. These include hepatitis B reactivation, progressive multifocal leukoencephalopathy, infusion reactions, tumor lysis syndrome, infections, and neutropenia.
The most common side effects of the drug are infusion reactions, neutropenia, thrombocytopenia, anemia, fever, cough, nausea, and diarrhea.
Obinutuzumab was FDA-approved for use in combination with chlorambucil to treat previously untreated CLL in November 2013. The drug (which is known as Gazyvaro in Europe) was approved by the European Commission for the same indication in July 2014.
Obinutuzumab was discovered by Roche Glycart AG, an independent research unit of Roche. In the US, the drug is part of a collaboration between Genentech and Biogen Idec.

Credit: Bill Branson
The US Food and Drug Administration (FDA) has approved a supplemental biologics license application for obinutuzumab (Gazyva) in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia (CLL).
The approval adds to the drug’s label data from stage 2 of the CLL11 study, which showed that obinutuzumab plus chlorambucil offers significant clinical improvements when compared head-to-head with rituximab plus chlorambucil.
This includes progression-free survival (PFS), complete response (CR), and minimal residual disease (MRD) data from stage 2 of the study. In addition, overall survival data was added from stage 1, in which researchers compared obinutuzumab plus chlorambucil to chlorambucil alone.
The label now reflects that obinutuzumab plus chlorambucil improved PFS compared to rituximab plus chlorambucil. The median PFS was 26.7 months and 14.9 months, respectively (hazard ratio=0.42, P<0.0001).
Additionally, obinutuzumab plus chlorambucil nearly tripled the CR rate when compared to rituximab plus chlorambucil. The CR rates were 26.1% and 8.8%, respectively.
Of the patients who achieved a CR with or without complete recovery from abnormal blood cell counts, 19% (18/94) of patients in the obinutuzumab arm and 6% (2/34) in the rituximab arm were MRD negative in the bone marrow.
Forty-one percent (39/94) of patients in the obinutuzumab arm and 12% (4/34) in the rituximab arm were MRD-negative in the peripheral blood.
At nearly 2 years, the rate of death was 9% (22/238) for patients who received obinutuzumab plus chlorambucil and 20% (24/118) for those who received chlorambucil alone (hazard ratio=0.41). The median overall survival has not yet been reached.
About obinutuzumab
Obinutuzumab is an engineered monoclonal antibody designed to attach to CD20 on B cells. The drug attacks targeted cells both directly and together with the body’s immune system.
The prescribing information for obinutuzumab includes warnings that the drug can cause serious or life-threatening side effects. These include hepatitis B reactivation, progressive multifocal leukoencephalopathy, infusion reactions, tumor lysis syndrome, infections, and neutropenia.
The most common side effects of the drug are infusion reactions, neutropenia, thrombocytopenia, anemia, fever, cough, nausea, and diarrhea.
Obinutuzumab was FDA-approved for use in combination with chlorambucil to treat previously untreated CLL in November 2013. The drug (which is known as Gazyvaro in Europe) was approved by the European Commission for the same indication in July 2014.
Obinutuzumab was discovered by Roche Glycart AG, an independent research unit of Roche. In the US, the drug is part of a collaboration between Genentech and Biogen Idec.
Study shows higher risk of MDS, leukemia after breast cancer

chemotherapy
Credit: Rhoda Baer
The risk of developing myelodysplastic syndromes (MDS) or leukemias after treatment for early stage breast cancer is higher than previously reported, according to a study published in the Journal of Clinical Oncology.
Data from earlier studies showed that about 0.25% of breast cancer patients develop MDS or leukemia as a late effect of chemotherapy, said Judith Karp, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
But Dr Karp and her colleagues found the 10-year incidence of MDS and leukemia among breast cancer patients to be about 0.5%.
“[T]he cumulative risk over a decade is now shown to be twice as high as we thought it was, and that risk doesn’t seem to slow down 5 years after treatment,” Dr Karp said. “Most medical oncologists have come to think that the risk is early and short-lived. So this was a little bit of a wake-up call that we are not seeing any plateau of that risk, and it is higher.”
Dr Karp and her colleagues reviewed data on 20,063 breast cancer patients treated at 8 US cancer centers between 1998 and 2007 whose cancer recurrence and secondary cancer rates were recorded in a database kept by the National Comprehensive Cancer Network.
At a median follow-up of 5.1 years, 50 patients had developed a marrow neoplasm, including acute myeloid leukemia (n=24), MDS/acute myeloid leukemia (n=15), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=5), chronic myeloid leukemia (n=3), or acute lymphoblastic leukemia (n=3).
The risk of developing MDS/leukemia was about 7 times higher for patients who underwent surgery and received chemotherapy, compared to patients who did not receive chemotherapy. For patients who underwent surgery and received both chemotherapy and radiation, the risk was about 8 times higher.
The MDS/leukemia rates per 1000 person-years were 0.16 for surgery, 0.43 for surgery plus radiation, 0.46 for surgery plus chemotherapy, and 0.54 for all 3 modalities.
The cumulative incidence of MDS/leukemia doubled between years 5 and 10, rising from 0.24% to 0.48%. And only 9% of patients were alive at 10 years.
Antonio Wolff, MD, of the Johns Hopkins University School of Medicine, said this study could help early stage breast cancer patients and their physicians think more carefully about the use of preventive or adjuvant chemotherapy, especially when patients have a low risk of cancer recurrence.
“Our study provides useful information for physicians and patients to consider a potential downside of preventive or adjuvant chemotherapy in patients with very low risk of breast cancer recurrence,” he said.
“It could be a false and dangerous security blanket to some patients by exposing them to a small risk of serious late effects with little or no real benefit from the treatment.”
The researchers included a hypothetical case to put the risks of early stage breast cancer and its treatment in perspective. They described a 60-year-old woman in average health who was diagnosed with stage 1 breast cancer that was rapidly growing and estrogen receptor-positive.
The patient had an estimated 12.3% risk of dying of breast cancer after 10 years. She could improve her 10-year survival rate by 1.8% with 4 cycles of chemotherapy, but she would also increase her risk of MDS/leukemia over that same time by 0.5%.
Dr Wolff noted that it’s unclear whether the increased risk of MDS/leukemia after postsurgical chemotherapy applies to patients with other kinds of solid tumors, as the drug regimens used in breast cancer differ from those used for other cancers. ![]()

chemotherapy
Credit: Rhoda Baer
The risk of developing myelodysplastic syndromes (MDS) or leukemias after treatment for early stage breast cancer is higher than previously reported, according to a study published in the Journal of Clinical Oncology.
Data from earlier studies showed that about 0.25% of breast cancer patients develop MDS or leukemia as a late effect of chemotherapy, said Judith Karp, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
But Dr Karp and her colleagues found the 10-year incidence of MDS and leukemia among breast cancer patients to be about 0.5%.
“[T]he cumulative risk over a decade is now shown to be twice as high as we thought it was, and that risk doesn’t seem to slow down 5 years after treatment,” Dr Karp said. “Most medical oncologists have come to think that the risk is early and short-lived. So this was a little bit of a wake-up call that we are not seeing any plateau of that risk, and it is higher.”
Dr Karp and her colleagues reviewed data on 20,063 breast cancer patients treated at 8 US cancer centers between 1998 and 2007 whose cancer recurrence and secondary cancer rates were recorded in a database kept by the National Comprehensive Cancer Network.
At a median follow-up of 5.1 years, 50 patients had developed a marrow neoplasm, including acute myeloid leukemia (n=24), MDS/acute myeloid leukemia (n=15), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=5), chronic myeloid leukemia (n=3), or acute lymphoblastic leukemia (n=3).
The risk of developing MDS/leukemia was about 7 times higher for patients who underwent surgery and received chemotherapy, compared to patients who did not receive chemotherapy. For patients who underwent surgery and received both chemotherapy and radiation, the risk was about 8 times higher.
The MDS/leukemia rates per 1000 person-years were 0.16 for surgery, 0.43 for surgery plus radiation, 0.46 for surgery plus chemotherapy, and 0.54 for all 3 modalities.
The cumulative incidence of MDS/leukemia doubled between years 5 and 10, rising from 0.24% to 0.48%. And only 9% of patients were alive at 10 years.
Antonio Wolff, MD, of the Johns Hopkins University School of Medicine, said this study could help early stage breast cancer patients and their physicians think more carefully about the use of preventive or adjuvant chemotherapy, especially when patients have a low risk of cancer recurrence.
“Our study provides useful information for physicians and patients to consider a potential downside of preventive or adjuvant chemotherapy in patients with very low risk of breast cancer recurrence,” he said.
“It could be a false and dangerous security blanket to some patients by exposing them to a small risk of serious late effects with little or no real benefit from the treatment.”
The researchers included a hypothetical case to put the risks of early stage breast cancer and its treatment in perspective. They described a 60-year-old woman in average health who was diagnosed with stage 1 breast cancer that was rapidly growing and estrogen receptor-positive.
The patient had an estimated 12.3% risk of dying of breast cancer after 10 years. She could improve her 10-year survival rate by 1.8% with 4 cycles of chemotherapy, but she would also increase her risk of MDS/leukemia over that same time by 0.5%.
Dr Wolff noted that it’s unclear whether the increased risk of MDS/leukemia after postsurgical chemotherapy applies to patients with other kinds of solid tumors, as the drug regimens used in breast cancer differ from those used for other cancers. ![]()

chemotherapy
Credit: Rhoda Baer
The risk of developing myelodysplastic syndromes (MDS) or leukemias after treatment for early stage breast cancer is higher than previously reported, according to a study published in the Journal of Clinical Oncology.
Data from earlier studies showed that about 0.25% of breast cancer patients develop MDS or leukemia as a late effect of chemotherapy, said Judith Karp, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
But Dr Karp and her colleagues found the 10-year incidence of MDS and leukemia among breast cancer patients to be about 0.5%.
“[T]he cumulative risk over a decade is now shown to be twice as high as we thought it was, and that risk doesn’t seem to slow down 5 years after treatment,” Dr Karp said. “Most medical oncologists have come to think that the risk is early and short-lived. So this was a little bit of a wake-up call that we are not seeing any plateau of that risk, and it is higher.”
Dr Karp and her colleagues reviewed data on 20,063 breast cancer patients treated at 8 US cancer centers between 1998 and 2007 whose cancer recurrence and secondary cancer rates were recorded in a database kept by the National Comprehensive Cancer Network.
At a median follow-up of 5.1 years, 50 patients had developed a marrow neoplasm, including acute myeloid leukemia (n=24), MDS/acute myeloid leukemia (n=15), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=5), chronic myeloid leukemia (n=3), or acute lymphoblastic leukemia (n=3).
The risk of developing MDS/leukemia was about 7 times higher for patients who underwent surgery and received chemotherapy, compared to patients who did not receive chemotherapy. For patients who underwent surgery and received both chemotherapy and radiation, the risk was about 8 times higher.
The MDS/leukemia rates per 1000 person-years were 0.16 for surgery, 0.43 for surgery plus radiation, 0.46 for surgery plus chemotherapy, and 0.54 for all 3 modalities.
The cumulative incidence of MDS/leukemia doubled between years 5 and 10, rising from 0.24% to 0.48%. And only 9% of patients were alive at 10 years.
Antonio Wolff, MD, of the Johns Hopkins University School of Medicine, said this study could help early stage breast cancer patients and their physicians think more carefully about the use of preventive or adjuvant chemotherapy, especially when patients have a low risk of cancer recurrence.
“Our study provides useful information for physicians and patients to consider a potential downside of preventive or adjuvant chemotherapy in patients with very low risk of breast cancer recurrence,” he said.
“It could be a false and dangerous security blanket to some patients by exposing them to a small risk of serious late effects with little or no real benefit from the treatment.”
The researchers included a hypothetical case to put the risks of early stage breast cancer and its treatment in perspective. They described a 60-year-old woman in average health who was diagnosed with stage 1 breast cancer that was rapidly growing and estrogen receptor-positive.
The patient had an estimated 12.3% risk of dying of breast cancer after 10 years. She could improve her 10-year survival rate by 1.8% with 4 cycles of chemotherapy, but she would also increase her risk of MDS/leukemia over that same time by 0.5%.
Dr Wolff noted that it’s unclear whether the increased risk of MDS/leukemia after postsurgical chemotherapy applies to patients with other kinds of solid tumors, as the drug regimens used in breast cancer differ from those used for other cancers. ![]()


