User login
Gene variations tied to drug-related hearing loss

Photo by Peter Barta
New research has revealed inherited genetic variations associated with rapid hearing loss in young cancer patients who receive cisplatin.
The drug is used to treat a range of cancers and is known to pose a risk of severe hearing loss, but the risk factors involved are not completely understood.
Now, researchers have found that variations in the gene ACYP2 are associated with an increased risk of cisplatin-related hearing loss.
Jun J. Yang, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported this discovery in Nature Genetics.
The researchers checked the DNA of 238 young patients with brain tumors for more than 1.7 million common genetic variations. The team found that variations in ACYP2 were associated with as much as a 4-fold greater risk of cisplatin-related hearing loss.
The screening is among the first to survey the genetic landscape for clues to help explain why the risk of cisplatin-related hearing loss varies so widely among patients.
“This is an important first step in being able to pinpoint patients who are at higher risk of developing cisplatin toxicity and to learn how to better manage that risk,” said study author Clinton Stewart, PharmD, also of St Jude.
The researchers confirmed the association between the high-risk ACYP2 variants and cisplatin-related hearing loss in a separate group of 68 brain tumor patients. The association was independent of other risk factors for cisplatin-related hearing loss, including patient age and receipt of radiation therapy.
Twenty-four of the 306 patients in this study had at least one copy of the high-risk ACYP2 variant. All 24 patients had measurable hearing loss that occurred as early as weeks after beginning cisplatin therapy.
Overall, however, the ACYP2 variant explained a relatively small proportion of hearing damage. Just 12.4% of the 194 patients in this study with cisplatin-related hearing loss carried the ACYP2 variant.
“This suggests that other genes also contribute to the risk of hearing loss and are yet to be identified,” Dr Yang said. “Further research is needed to understand how the ACYP2 variations modify the risk . . . of cisplatin toxicity.”
Such studies could potentially lead to new medications to protect high-risk patients from cisplatin-related toxicity or help identify candidates for intensive monitoring of their hearing, Dr Stewart said. Early intervention could then be offered if problems are identified.
This study included patients enrolled in 1 of 3 trials designed by St Jude investigators for newly diagnosed pediatric brain tumors. The protocols involved similar treatment, including surgery to remove as much of the tumor as possible, followed by radiation, which was modified based on patient age and other risk factors.
The patients were scheduled to receive 4 rounds of cisplatin therapy. Patients’ hearing was tested before treatment began, after radiation therapy, after each round of chemotherapy, and then at regular standardized intervals. Analysis of the resulting data led to identification of ACYP2 and other variants.
“Our primary goal is to cure children with brain tumors, but we also have a duty to help patients survive with a high quality of life,” said Giles Robinson, MD, also of St Jude.
“Hearing loss can have a significant impact on a child’s quality of life, language development, and academic performance. There is no easy fix, but the more we know about the risk factors, the better we will understand how to use cisplatin.” ![]()

Photo by Peter Barta
New research has revealed inherited genetic variations associated with rapid hearing loss in young cancer patients who receive cisplatin.
The drug is used to treat a range of cancers and is known to pose a risk of severe hearing loss, but the risk factors involved are not completely understood.
Now, researchers have found that variations in the gene ACYP2 are associated with an increased risk of cisplatin-related hearing loss.
Jun J. Yang, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported this discovery in Nature Genetics.
The researchers checked the DNA of 238 young patients with brain tumors for more than 1.7 million common genetic variations. The team found that variations in ACYP2 were associated with as much as a 4-fold greater risk of cisplatin-related hearing loss.
The screening is among the first to survey the genetic landscape for clues to help explain why the risk of cisplatin-related hearing loss varies so widely among patients.
“This is an important first step in being able to pinpoint patients who are at higher risk of developing cisplatin toxicity and to learn how to better manage that risk,” said study author Clinton Stewart, PharmD, also of St Jude.
The researchers confirmed the association between the high-risk ACYP2 variants and cisplatin-related hearing loss in a separate group of 68 brain tumor patients. The association was independent of other risk factors for cisplatin-related hearing loss, including patient age and receipt of radiation therapy.
Twenty-four of the 306 patients in this study had at least one copy of the high-risk ACYP2 variant. All 24 patients had measurable hearing loss that occurred as early as weeks after beginning cisplatin therapy.
Overall, however, the ACYP2 variant explained a relatively small proportion of hearing damage. Just 12.4% of the 194 patients in this study with cisplatin-related hearing loss carried the ACYP2 variant.
“This suggests that other genes also contribute to the risk of hearing loss and are yet to be identified,” Dr Yang said. “Further research is needed to understand how the ACYP2 variations modify the risk . . . of cisplatin toxicity.”
Such studies could potentially lead to new medications to protect high-risk patients from cisplatin-related toxicity or help identify candidates for intensive monitoring of their hearing, Dr Stewart said. Early intervention could then be offered if problems are identified.
This study included patients enrolled in 1 of 3 trials designed by St Jude investigators for newly diagnosed pediatric brain tumors. The protocols involved similar treatment, including surgery to remove as much of the tumor as possible, followed by radiation, which was modified based on patient age and other risk factors.
The patients were scheduled to receive 4 rounds of cisplatin therapy. Patients’ hearing was tested before treatment began, after radiation therapy, after each round of chemotherapy, and then at regular standardized intervals. Analysis of the resulting data led to identification of ACYP2 and other variants.
“Our primary goal is to cure children with brain tumors, but we also have a duty to help patients survive with a high quality of life,” said Giles Robinson, MD, also of St Jude.
“Hearing loss can have a significant impact on a child’s quality of life, language development, and academic performance. There is no easy fix, but the more we know about the risk factors, the better we will understand how to use cisplatin.” ![]()

Photo by Peter Barta
New research has revealed inherited genetic variations associated with rapid hearing loss in young cancer patients who receive cisplatin.
The drug is used to treat a range of cancers and is known to pose a risk of severe hearing loss, but the risk factors involved are not completely understood.
Now, researchers have found that variations in the gene ACYP2 are associated with an increased risk of cisplatin-related hearing loss.
Jun J. Yang, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported this discovery in Nature Genetics.
The researchers checked the DNA of 238 young patients with brain tumors for more than 1.7 million common genetic variations. The team found that variations in ACYP2 were associated with as much as a 4-fold greater risk of cisplatin-related hearing loss.
The screening is among the first to survey the genetic landscape for clues to help explain why the risk of cisplatin-related hearing loss varies so widely among patients.
“This is an important first step in being able to pinpoint patients who are at higher risk of developing cisplatin toxicity and to learn how to better manage that risk,” said study author Clinton Stewart, PharmD, also of St Jude.
The researchers confirmed the association between the high-risk ACYP2 variants and cisplatin-related hearing loss in a separate group of 68 brain tumor patients. The association was independent of other risk factors for cisplatin-related hearing loss, including patient age and receipt of radiation therapy.
Twenty-four of the 306 patients in this study had at least one copy of the high-risk ACYP2 variant. All 24 patients had measurable hearing loss that occurred as early as weeks after beginning cisplatin therapy.
Overall, however, the ACYP2 variant explained a relatively small proportion of hearing damage. Just 12.4% of the 194 patients in this study with cisplatin-related hearing loss carried the ACYP2 variant.
“This suggests that other genes also contribute to the risk of hearing loss and are yet to be identified,” Dr Yang said. “Further research is needed to understand how the ACYP2 variations modify the risk . . . of cisplatin toxicity.”
Such studies could potentially lead to new medications to protect high-risk patients from cisplatin-related toxicity or help identify candidates for intensive monitoring of their hearing, Dr Stewart said. Early intervention could then be offered if problems are identified.
This study included patients enrolled in 1 of 3 trials designed by St Jude investigators for newly diagnosed pediatric brain tumors. The protocols involved similar treatment, including surgery to remove as much of the tumor as possible, followed by radiation, which was modified based on patient age and other risk factors.
The patients were scheduled to receive 4 rounds of cisplatin therapy. Patients’ hearing was tested before treatment began, after radiation therapy, after each round of chemotherapy, and then at regular standardized intervals. Analysis of the resulting data led to identification of ACYP2 and other variants.
“Our primary goal is to cure children with brain tumors, but we also have a duty to help patients survive with a high quality of life,” said Giles Robinson, MD, also of St Jude.
“Hearing loss can have a significant impact on a child’s quality of life, language development, and academic performance. There is no easy fix, but the more we know about the risk factors, the better we will understand how to use cisplatin.” ![]()
Signs may predict death in cancer patients

Researchers have identified 8 highly specific physical and cognitive signs that seem to be associated with imminent death in cancer patients.
The findings, published in Cancer, could offer clinicians the ability to better communicate with patients and their families.
The research might also help guide the medical team and caregivers when it comes to complex decision making, such as discontinuing tests and therapy, plans for hospital discharge, and hospice referral.
Previous studies in end-of-life care have focused on physicians prognosticating better. However, research on how to tell if a patient has entered the final days of life has been minimal, according to David Hui, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“In the past, studies trying to understand the signs associated with impending death were conducted in people who were recognized as dying, so there’s a potential bias built into this model,” Dr Hui said.
“With our study, we observed a list of signs in patients from the time they were admitted to the palliative care unit. They were observed systematically, twice a day, without knowing if the patient would die or be discharged.”
Dr Hui and his colleagues observed 357 cancer patients, 57% of whom ultimately died. The researchers observed 52 physical and cognitive signs—identified by Dr Hui and his colleagues in previous research—twice a day from the patient’s admission to discharge or death.
Of those 52 signs, the 8 most highly associated with impending death within 3 days were:
- Nonreactive pupils
- Decreased response to verbal stimuli
- Decreased response to visual stimuli
- Inability to close eyelids
- Drooping of the nasolabial fold
- Neck hyperextension
- Grunting of vocal cords
- Upper gastrointestinal bleeding.
“When cancer patients reach the last days of life, this is an extremely emotional time for families; their stress levels cannot be understated,” Dr Hui said.
“Knowing when death is imminent would provide more information so caregivers can plan appropriately. For clinicians, having this information could help reassure families that we are providing the best care possible.”
Dr Hui stressed that this research is not yet practice-changing, but is an important step in understanding these 8 signs and their relation to impending death. In addition, the findings are only representative of imminent cancer death and should not be generalized to other causes of death.
Follow-up studies in different settings are planned. Dr Hui and his colleagues plan to look at the reliability of the identified signs, as well as evaluate this research in other countries and in the hospice setting. ![]()

Researchers have identified 8 highly specific physical and cognitive signs that seem to be associated with imminent death in cancer patients.
The findings, published in Cancer, could offer clinicians the ability to better communicate with patients and their families.
The research might also help guide the medical team and caregivers when it comes to complex decision making, such as discontinuing tests and therapy, plans for hospital discharge, and hospice referral.
Previous studies in end-of-life care have focused on physicians prognosticating better. However, research on how to tell if a patient has entered the final days of life has been minimal, according to David Hui, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“In the past, studies trying to understand the signs associated with impending death were conducted in people who were recognized as dying, so there’s a potential bias built into this model,” Dr Hui said.
“With our study, we observed a list of signs in patients from the time they were admitted to the palliative care unit. They were observed systematically, twice a day, without knowing if the patient would die or be discharged.”
Dr Hui and his colleagues observed 357 cancer patients, 57% of whom ultimately died. The researchers observed 52 physical and cognitive signs—identified by Dr Hui and his colleagues in previous research—twice a day from the patient’s admission to discharge or death.
Of those 52 signs, the 8 most highly associated with impending death within 3 days were:
- Nonreactive pupils
- Decreased response to verbal stimuli
- Decreased response to visual stimuli
- Inability to close eyelids
- Drooping of the nasolabial fold
- Neck hyperextension
- Grunting of vocal cords
- Upper gastrointestinal bleeding.
“When cancer patients reach the last days of life, this is an extremely emotional time for families; their stress levels cannot be understated,” Dr Hui said.
“Knowing when death is imminent would provide more information so caregivers can plan appropriately. For clinicians, having this information could help reassure families that we are providing the best care possible.”
Dr Hui stressed that this research is not yet practice-changing, but is an important step in understanding these 8 signs and their relation to impending death. In addition, the findings are only representative of imminent cancer death and should not be generalized to other causes of death.
Follow-up studies in different settings are planned. Dr Hui and his colleagues plan to look at the reliability of the identified signs, as well as evaluate this research in other countries and in the hospice setting. ![]()

Researchers have identified 8 highly specific physical and cognitive signs that seem to be associated with imminent death in cancer patients.
The findings, published in Cancer, could offer clinicians the ability to better communicate with patients and their families.
The research might also help guide the medical team and caregivers when it comes to complex decision making, such as discontinuing tests and therapy, plans for hospital discharge, and hospice referral.
Previous studies in end-of-life care have focused on physicians prognosticating better. However, research on how to tell if a patient has entered the final days of life has been minimal, according to David Hui, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“In the past, studies trying to understand the signs associated with impending death were conducted in people who were recognized as dying, so there’s a potential bias built into this model,” Dr Hui said.
“With our study, we observed a list of signs in patients from the time they were admitted to the palliative care unit. They were observed systematically, twice a day, without knowing if the patient would die or be discharged.”
Dr Hui and his colleagues observed 357 cancer patients, 57% of whom ultimately died. The researchers observed 52 physical and cognitive signs—identified by Dr Hui and his colleagues in previous research—twice a day from the patient’s admission to discharge or death.
Of those 52 signs, the 8 most highly associated with impending death within 3 days were:
- Nonreactive pupils
- Decreased response to verbal stimuli
- Decreased response to visual stimuli
- Inability to close eyelids
- Drooping of the nasolabial fold
- Neck hyperextension
- Grunting of vocal cords
- Upper gastrointestinal bleeding.
“When cancer patients reach the last days of life, this is an extremely emotional time for families; their stress levels cannot be understated,” Dr Hui said.
“Knowing when death is imminent would provide more information so caregivers can plan appropriately. For clinicians, having this information could help reassure families that we are providing the best care possible.”
Dr Hui stressed that this research is not yet practice-changing, but is an important step in understanding these 8 signs and their relation to impending death. In addition, the findings are only representative of imminent cancer death and should not be generalized to other causes of death.
Follow-up studies in different settings are planned. Dr Hui and his colleagues plan to look at the reliability of the identified signs, as well as evaluate this research in other countries and in the hospice setting. ![]()
Ro-CHOP: Toxicity increases with efficacy
SAN FRANCISCO—Adding romidepsin to CHOP can enhance the regimen’s efficacy against peripheral T-cell lymphoma (PTCL), but the combination can also induce severe toxicity, results of a phase 1b/2 study have shown.
In patients with previously untreated PTCL, romidepsin plus CHOP elicited an overall response rate of about 69%.
But all patients experienced adverse events, a median of 49 per patient. In addition, rates of hematologic toxicities were high, and 3 patients experienced acute cardiac toxicity.
Bertrand Coiffier, MD, PhD, of CHU Lyon Sud in Pierre Benite, France, presented these findings at the 7th Annual T-cell Lymphoma Forum. Dr Coiffier and other researchers involved in this study receive funds from Celgene, the company developing romidepsin.
“CHOP is widely accepted,” Dr Coiffier noted. “It’s the most-used regimen for peripheral T-cell lymphoma, but it’s not the best one, and we certainly have regimens that do produce more [complete responses] and longer responses.”
He said researchers decided to test romidepsin in combination with CHOP because studies have suggested that romidepsin has very good efficacy in relapsed/refractory peripheral T-cell lymphoma, and the toxicities associated with romidepsin and CHOP alone have been managable.
So the researchers tested the combination in 37 patients with untreated PTCL, most of whom were male (n=20). The median age was 57, and 37.8% were older than 60. About 95% of patients had stage III/IV disease, and about 89% had an ECOG performance status less than 2.
Most patients had angioimmunoblastic T-cell lymphoma (n=17), followed by PTCL not otherwise specified (n=13), ALK- anaplastic large-cell lymphoma (n=3), enteropathy-associated T-cell lymphoma (n=1), hepatosplenic T-cell lymphoma (n=1), primary cutaneous CD4+ small/medium T-cell lymphoma (n=1), and “other” (n=1).
Early DLTs
The researchers used a standard “3+3” dose-escalation scheme, starting with a romidepsin dose of 10 mg/m2 given on days 1 and 8.
In the first 2 cycles, there were 3 dose-limiting toxicities (DLTs)—1 case of grade 3 syncope, 1 case of grade 3 general status alteration, and 1 case of grade 3 hematologic toxicity (neutropenia and thrombocytopenia) lasting longer than 7 days.
“So we looked at the definition of the criteria for DLT, and we thought that, this time, they were too severe,” Dr Coiffier said. “After a lot of discussion between all the investigators, we decided to modify the criteria for DLT regarding neutropenia or thrombocytopenia and to allow a little more toxicity before saying it’s a DLT.”
A DLT was initially defined as grade 3/4 non-hematologic toxicity, grade 3 hematologic toxicity lasting more than 7 days, or grade 4 hematologic toxicity lasting more than 3 days. The researchers modified the criteria so that hematologic toxicities would not be considered DLTs if they lasted less than 10 days for grade 3 or less than 7 days for grade 4.
When the team decreased the romidepsin dose to 8 mg/m2, they did not observe any DLTs according to the new criteria. The same was true when they raised the dose back up to 10 mg/m2.
There were, however, DLTs when the dose was increased to 12 mg/m2. In cohort 5, there was a case of grade 3 cardiac failure, and in cohort 6, there were 2 cases of grade 3 nausea.
Nevertheless, 12 mg/m2 became the phase 2 dose. In all, 25 patients received romidepsin at that dose.
Safety data
Twenty-six of 37 patients completed the 8 planned cycles of treatment. Five patients discontinued treatment due to progression and 6 due to toxicity (5 due to thrombocytopenia).
“One hundred percent of patients experienced at least one adverse event, but most of them were grade 1 or 2 [84%] and occurred during the first 2 cycles [38%],” Dr Coiffier said. “There were no deaths related to adverse events.”
Severe toxicities occurred during the expansion phase. There was a case of severe peripheral sensory neuropathy that led to treatment discontinuation, and there were 3 cases of acute cardiac toxicity. They all occurred after the first cycle, and none were fatal.
The rate of hematologic toxicity was high. Neutropenia occurred in all patients, thrombocytopenia in 94%, and anemia in 89%.
Grade 3/4 adverse events included neutropenia (85%), thrombocytopenia (35%), febrile neutropenia (19%), general status deterioration (13%), nausea/vomiting (10%), anemia (8%), hypophosphatemia (8%), fatigue (5%), mucositis (5%), decreased appetite (5%), hypocalcemia (3%), hyponatremia (3%), hypokalemia (3%), hypomagnesemia (3%), dysgeusia (3%), and peripheral sensory neuropathy (3%).
Response, survival, and next steps
About 51% of patients (18/35) achieved a complete response, and 17% (n=6) had a partial response. Twenty-six percent of patients (n=9) progressed.
The median follow-up was 30 months. The estimated 1-year progression-free survival was 57%, and the estimated 1-year overall survival was 82%.
“The [overall survival] curve is certainly much better than you would expect with just standard CHOP,” Dr Coiffier noted.
He added that this research has progressed to a phase 3 study comparing romidepsin and CHOP in combination to CHOP alone. There are 7 countries participating (France, Belgium, South Korea, Spain, Italy, Germany, and Portugal), and 100 patients have been enrolled thus far. ![]()
SAN FRANCISCO—Adding romidepsin to CHOP can enhance the regimen’s efficacy against peripheral T-cell lymphoma (PTCL), but the combination can also induce severe toxicity, results of a phase 1b/2 study have shown.
In patients with previously untreated PTCL, romidepsin plus CHOP elicited an overall response rate of about 69%.
But all patients experienced adverse events, a median of 49 per patient. In addition, rates of hematologic toxicities were high, and 3 patients experienced acute cardiac toxicity.
Bertrand Coiffier, MD, PhD, of CHU Lyon Sud in Pierre Benite, France, presented these findings at the 7th Annual T-cell Lymphoma Forum. Dr Coiffier and other researchers involved in this study receive funds from Celgene, the company developing romidepsin.
“CHOP is widely accepted,” Dr Coiffier noted. “It’s the most-used regimen for peripheral T-cell lymphoma, but it’s not the best one, and we certainly have regimens that do produce more [complete responses] and longer responses.”
He said researchers decided to test romidepsin in combination with CHOP because studies have suggested that romidepsin has very good efficacy in relapsed/refractory peripheral T-cell lymphoma, and the toxicities associated with romidepsin and CHOP alone have been managable.
So the researchers tested the combination in 37 patients with untreated PTCL, most of whom were male (n=20). The median age was 57, and 37.8% were older than 60. About 95% of patients had stage III/IV disease, and about 89% had an ECOG performance status less than 2.
Most patients had angioimmunoblastic T-cell lymphoma (n=17), followed by PTCL not otherwise specified (n=13), ALK- anaplastic large-cell lymphoma (n=3), enteropathy-associated T-cell lymphoma (n=1), hepatosplenic T-cell lymphoma (n=1), primary cutaneous CD4+ small/medium T-cell lymphoma (n=1), and “other” (n=1).
Early DLTs
The researchers used a standard “3+3” dose-escalation scheme, starting with a romidepsin dose of 10 mg/m2 given on days 1 and 8.
In the first 2 cycles, there were 3 dose-limiting toxicities (DLTs)—1 case of grade 3 syncope, 1 case of grade 3 general status alteration, and 1 case of grade 3 hematologic toxicity (neutropenia and thrombocytopenia) lasting longer than 7 days.
“So we looked at the definition of the criteria for DLT, and we thought that, this time, they were too severe,” Dr Coiffier said. “After a lot of discussion between all the investigators, we decided to modify the criteria for DLT regarding neutropenia or thrombocytopenia and to allow a little more toxicity before saying it’s a DLT.”
A DLT was initially defined as grade 3/4 non-hematologic toxicity, grade 3 hematologic toxicity lasting more than 7 days, or grade 4 hematologic toxicity lasting more than 3 days. The researchers modified the criteria so that hematologic toxicities would not be considered DLTs if they lasted less than 10 days for grade 3 or less than 7 days for grade 4.
When the team decreased the romidepsin dose to 8 mg/m2, they did not observe any DLTs according to the new criteria. The same was true when they raised the dose back up to 10 mg/m2.
There were, however, DLTs when the dose was increased to 12 mg/m2. In cohort 5, there was a case of grade 3 cardiac failure, and in cohort 6, there were 2 cases of grade 3 nausea.
Nevertheless, 12 mg/m2 became the phase 2 dose. In all, 25 patients received romidepsin at that dose.
Safety data
Twenty-six of 37 patients completed the 8 planned cycles of treatment. Five patients discontinued treatment due to progression and 6 due to toxicity (5 due to thrombocytopenia).
“One hundred percent of patients experienced at least one adverse event, but most of them were grade 1 or 2 [84%] and occurred during the first 2 cycles [38%],” Dr Coiffier said. “There were no deaths related to adverse events.”
Severe toxicities occurred during the expansion phase. There was a case of severe peripheral sensory neuropathy that led to treatment discontinuation, and there were 3 cases of acute cardiac toxicity. They all occurred after the first cycle, and none were fatal.
The rate of hematologic toxicity was high. Neutropenia occurred in all patients, thrombocytopenia in 94%, and anemia in 89%.
Grade 3/4 adverse events included neutropenia (85%), thrombocytopenia (35%), febrile neutropenia (19%), general status deterioration (13%), nausea/vomiting (10%), anemia (8%), hypophosphatemia (8%), fatigue (5%), mucositis (5%), decreased appetite (5%), hypocalcemia (3%), hyponatremia (3%), hypokalemia (3%), hypomagnesemia (3%), dysgeusia (3%), and peripheral sensory neuropathy (3%).
Response, survival, and next steps
About 51% of patients (18/35) achieved a complete response, and 17% (n=6) had a partial response. Twenty-six percent of patients (n=9) progressed.
The median follow-up was 30 months. The estimated 1-year progression-free survival was 57%, and the estimated 1-year overall survival was 82%.
“The [overall survival] curve is certainly much better than you would expect with just standard CHOP,” Dr Coiffier noted.
He added that this research has progressed to a phase 3 study comparing romidepsin and CHOP in combination to CHOP alone. There are 7 countries participating (France, Belgium, South Korea, Spain, Italy, Germany, and Portugal), and 100 patients have been enrolled thus far. ![]()
SAN FRANCISCO—Adding romidepsin to CHOP can enhance the regimen’s efficacy against peripheral T-cell lymphoma (PTCL), but the combination can also induce severe toxicity, results of a phase 1b/2 study have shown.
In patients with previously untreated PTCL, romidepsin plus CHOP elicited an overall response rate of about 69%.
But all patients experienced adverse events, a median of 49 per patient. In addition, rates of hematologic toxicities were high, and 3 patients experienced acute cardiac toxicity.
Bertrand Coiffier, MD, PhD, of CHU Lyon Sud in Pierre Benite, France, presented these findings at the 7th Annual T-cell Lymphoma Forum. Dr Coiffier and other researchers involved in this study receive funds from Celgene, the company developing romidepsin.
“CHOP is widely accepted,” Dr Coiffier noted. “It’s the most-used regimen for peripheral T-cell lymphoma, but it’s not the best one, and we certainly have regimens that do produce more [complete responses] and longer responses.”
He said researchers decided to test romidepsin in combination with CHOP because studies have suggested that romidepsin has very good efficacy in relapsed/refractory peripheral T-cell lymphoma, and the toxicities associated with romidepsin and CHOP alone have been managable.
So the researchers tested the combination in 37 patients with untreated PTCL, most of whom were male (n=20). The median age was 57, and 37.8% were older than 60. About 95% of patients had stage III/IV disease, and about 89% had an ECOG performance status less than 2.
Most patients had angioimmunoblastic T-cell lymphoma (n=17), followed by PTCL not otherwise specified (n=13), ALK- anaplastic large-cell lymphoma (n=3), enteropathy-associated T-cell lymphoma (n=1), hepatosplenic T-cell lymphoma (n=1), primary cutaneous CD4+ small/medium T-cell lymphoma (n=1), and “other” (n=1).
Early DLTs
The researchers used a standard “3+3” dose-escalation scheme, starting with a romidepsin dose of 10 mg/m2 given on days 1 and 8.
In the first 2 cycles, there were 3 dose-limiting toxicities (DLTs)—1 case of grade 3 syncope, 1 case of grade 3 general status alteration, and 1 case of grade 3 hematologic toxicity (neutropenia and thrombocytopenia) lasting longer than 7 days.
“So we looked at the definition of the criteria for DLT, and we thought that, this time, they were too severe,” Dr Coiffier said. “After a lot of discussion between all the investigators, we decided to modify the criteria for DLT regarding neutropenia or thrombocytopenia and to allow a little more toxicity before saying it’s a DLT.”
A DLT was initially defined as grade 3/4 non-hematologic toxicity, grade 3 hematologic toxicity lasting more than 7 days, or grade 4 hematologic toxicity lasting more than 3 days. The researchers modified the criteria so that hematologic toxicities would not be considered DLTs if they lasted less than 10 days for grade 3 or less than 7 days for grade 4.
When the team decreased the romidepsin dose to 8 mg/m2, they did not observe any DLTs according to the new criteria. The same was true when they raised the dose back up to 10 mg/m2.
There were, however, DLTs when the dose was increased to 12 mg/m2. In cohort 5, there was a case of grade 3 cardiac failure, and in cohort 6, there were 2 cases of grade 3 nausea.
Nevertheless, 12 mg/m2 became the phase 2 dose. In all, 25 patients received romidepsin at that dose.
Safety data
Twenty-six of 37 patients completed the 8 planned cycles of treatment. Five patients discontinued treatment due to progression and 6 due to toxicity (5 due to thrombocytopenia).
“One hundred percent of patients experienced at least one adverse event, but most of them were grade 1 or 2 [84%] and occurred during the first 2 cycles [38%],” Dr Coiffier said. “There were no deaths related to adverse events.”
Severe toxicities occurred during the expansion phase. There was a case of severe peripheral sensory neuropathy that led to treatment discontinuation, and there were 3 cases of acute cardiac toxicity. They all occurred after the first cycle, and none were fatal.
The rate of hematologic toxicity was high. Neutropenia occurred in all patients, thrombocytopenia in 94%, and anemia in 89%.
Grade 3/4 adverse events included neutropenia (85%), thrombocytopenia (35%), febrile neutropenia (19%), general status deterioration (13%), nausea/vomiting (10%), anemia (8%), hypophosphatemia (8%), fatigue (5%), mucositis (5%), decreased appetite (5%), hypocalcemia (3%), hyponatremia (3%), hypokalemia (3%), hypomagnesemia (3%), dysgeusia (3%), and peripheral sensory neuropathy (3%).
Response, survival, and next steps
About 51% of patients (18/35) achieved a complete response, and 17% (n=6) had a partial response. Twenty-six percent of patients (n=9) progressed.
The median follow-up was 30 months. The estimated 1-year progression-free survival was 57%, and the estimated 1-year overall survival was 82%.
“The [overall survival] curve is certainly much better than you would expect with just standard CHOP,” Dr Coiffier noted.
He added that this research has progressed to a phase 3 study comparing romidepsin and CHOP in combination to CHOP alone. There are 7 countries participating (France, Belgium, South Korea, Spain, Italy, Germany, and Portugal), and 100 patients have been enrolled thus far. ![]()
Mogamulizumab in PTCL: Europe vs Japan
SAN FRANCISCO—Two phase 2 studies testing mogamulizumab in peripheral T-cell lymphomas (PTCLs) suggest that higher response rates don’t necessarily translate to an improvement in progression-free survival (PFS).
The anti-CCR4 antibody produced a higher overall response rate (ORR) in a Japanese study than in a European study—34% and 11%, respectively.
However, median PFS times were similar—about 2 months in both studies.
This similarity is all the more interesting because the studies enrolled different types of patients and followed different dosing schedules, according to Pier Luigi Zinzani, MD, PhD, of the University of Bologna in Italy.
Dr Zinzani discussed details of the European experience testing mogamulizumab in PTCL, comparing it to the Japanese experience, in a presentation at the 7th Annual T-cell Lymphoma Forum.
Kensei Tobinai, MD, PhD, of the National Cancer Center Hospital in Tokyo, Japan, also reviewed the Japanese experience (TCLF 2013, JCO 2014) during the meeting’s keynote address and presented data from an ancillary analysis of this study (which is unpublished).
All of the research was sponsored by Kyowa Hakko Kirin Co., Ltd., the company developing mogamulizumab.
The Japanese experience
The Japanese study included 29 patients with PTCL and 8 with cutaneous T-cell lymphoma (CTCL). All patients had relapsed after their last chemotherapy regimen, and none had received an allogeneic stem cell transplant (allo-SCT). The PTCL patients had a median age of 67, and 69% were male.
All patients received mogamulizumab at 1.0 mg/kg/day weekly for 8 weeks. The ORR was 35%—34% for PTCL patients and 38% for CTCL patients.
Among PTCL patients, there were 5 complete responses (CRs) and 5 partial responses (PRs). Nine patients had stable disease (SD), and 10 progressed.
Of the 16 patients with PTCL-not otherwise specified (PTCL-NOS), 1 had a CR, 2 had a PR, 6 had SD, and 7 progressed. Of the 12 patients with angioimmunoblastic T-cell lymphoma (AITL), 3 had a CR, 3 had a PR, 3 had SD, and 3 progressed. The only patient with ALK- anaplastic large-cell lymphoma (ALCL) had an unconfirmed CR.
The ancillary analysis showed that tumor shrinkage of the target lesions occurred in 72% (21/29) of patients with PTCL. The patients’ median duration of response was 6.4 months, and the median time to response was 1.9 months.
Overall, the median PFS was 3.0 months—2.0 months in patients with PTCL and 3.4 months in patients with CTCL.
Common adverse events (for both PTCL and CTCL patients) included lymphopenia (81%), skin disorders (51%), leukopenia (43%), neutropenia (38%), thrombocytopenia (38%), pyrexia (30%), acute infusion reactions (24%), and anemia (14%).
Dr Tobinai noted that these results are not as favorable as those observed when patients with adult T-cell leukemia-lymphoma receive mogamulizumab.
“But compared to the efficacy rate of other approved agents—pralatrexate and romidepsin—this antibody has promising efficacy,” he said.
In fact, the results of this study prompted the December approval of mogamulizumab to treat PTCL and CTCL patients in Japan.
The European experience
The European study differed from the Japanese study in a few ways, Dr Zinzani pointed out. The European study only enrolled patients with PTCL. And it included patients with relapsed (49%) or refractory (51%) disease, whereas the Japanese study only included relapsed patients.
Furthermore, the Japanese study did not include any patients with an ECOG performance status of 2, while the European study did (39%). And the dosing schedule differed between the 2 studies.
In the European study, patients received mogamulizumab at 1 mg/kg once weekly for 4 weeks and then once every 2 weeks until they progressed or developed unacceptable toxicity.
There were 38 patients in the safety analysis. They had a median age of 58.5 years, and 61% were male.
Thirty-five of these patients were included in the efficacy analysis. They had a median of 2 prior treatments (range, 1-8), and 17 patients (49%) had responded to their last therapy.
The patients had PTCL-NOS (43%, 15/35), AITL (34%, 12), transformed mycosis fungoides (9%, 3), ALK- ALCL (11%, 4), and ALK+ ALCL (3%, 1).
The ORR was 11% (n=4), and 46% of patients (n=16) had SD or better. Two patients with PTCL-NOS responded, as did 2 with AITL.
Six patients with PTCL-NOS had SD, as did 3 with AITL, 1 with transformed mycosis fungoides, and 2 with ALK- ALCL.
The median duration of response (including SD) was 2.9 months. And the median PFS was 2.1 months. Two patients (1 with ALK- ALCL and 1 with PTCL-NOS) went on to allo-SCT.
The most frequent adverse events (occurring in at least 10% of patients) were drug eruption (n=12), pyrexia (n=9), pruritus (n=7), diarrhea (n=7), cough (n=6), vomiting (n=6), thrombocytopenia (n=6), hypotension (n=4), headache (n=4), peripheral edema (n=4), asthenia (n=4), nausea (n=4), anemia (n=4), and neutropenia (n=4).
“For the European experience, there were some differences from the Japanese experience,” Dr Zinzani said in closing. “It was worse in terms of overall response rate—only 11%—but roughly 50% of patients attained at least stable disease. And there was an acceptable safety profile in these really heavily pretreated, relapsed/refractory PTCL patients.” ![]()
SAN FRANCISCO—Two phase 2 studies testing mogamulizumab in peripheral T-cell lymphomas (PTCLs) suggest that higher response rates don’t necessarily translate to an improvement in progression-free survival (PFS).
The anti-CCR4 antibody produced a higher overall response rate (ORR) in a Japanese study than in a European study—34% and 11%, respectively.
However, median PFS times were similar—about 2 months in both studies.
This similarity is all the more interesting because the studies enrolled different types of patients and followed different dosing schedules, according to Pier Luigi Zinzani, MD, PhD, of the University of Bologna in Italy.
Dr Zinzani discussed details of the European experience testing mogamulizumab in PTCL, comparing it to the Japanese experience, in a presentation at the 7th Annual T-cell Lymphoma Forum.
Kensei Tobinai, MD, PhD, of the National Cancer Center Hospital in Tokyo, Japan, also reviewed the Japanese experience (TCLF 2013, JCO 2014) during the meeting’s keynote address and presented data from an ancillary analysis of this study (which is unpublished).
All of the research was sponsored by Kyowa Hakko Kirin Co., Ltd., the company developing mogamulizumab.
The Japanese experience
The Japanese study included 29 patients with PTCL and 8 with cutaneous T-cell lymphoma (CTCL). All patients had relapsed after their last chemotherapy regimen, and none had received an allogeneic stem cell transplant (allo-SCT). The PTCL patients had a median age of 67, and 69% were male.
All patients received mogamulizumab at 1.0 mg/kg/day weekly for 8 weeks. The ORR was 35%—34% for PTCL patients and 38% for CTCL patients.
Among PTCL patients, there were 5 complete responses (CRs) and 5 partial responses (PRs). Nine patients had stable disease (SD), and 10 progressed.
Of the 16 patients with PTCL-not otherwise specified (PTCL-NOS), 1 had a CR, 2 had a PR, 6 had SD, and 7 progressed. Of the 12 patients with angioimmunoblastic T-cell lymphoma (AITL), 3 had a CR, 3 had a PR, 3 had SD, and 3 progressed. The only patient with ALK- anaplastic large-cell lymphoma (ALCL) had an unconfirmed CR.
The ancillary analysis showed that tumor shrinkage of the target lesions occurred in 72% (21/29) of patients with PTCL. The patients’ median duration of response was 6.4 months, and the median time to response was 1.9 months.
Overall, the median PFS was 3.0 months—2.0 months in patients with PTCL and 3.4 months in patients with CTCL.
Common adverse events (for both PTCL and CTCL patients) included lymphopenia (81%), skin disorders (51%), leukopenia (43%), neutropenia (38%), thrombocytopenia (38%), pyrexia (30%), acute infusion reactions (24%), and anemia (14%).
Dr Tobinai noted that these results are not as favorable as those observed when patients with adult T-cell leukemia-lymphoma receive mogamulizumab.
“But compared to the efficacy rate of other approved agents—pralatrexate and romidepsin—this antibody has promising efficacy,” he said.
In fact, the results of this study prompted the December approval of mogamulizumab to treat PTCL and CTCL patients in Japan.
The European experience
The European study differed from the Japanese study in a few ways, Dr Zinzani pointed out. The European study only enrolled patients with PTCL. And it included patients with relapsed (49%) or refractory (51%) disease, whereas the Japanese study only included relapsed patients.
Furthermore, the Japanese study did not include any patients with an ECOG performance status of 2, while the European study did (39%). And the dosing schedule differed between the 2 studies.
In the European study, patients received mogamulizumab at 1 mg/kg once weekly for 4 weeks and then once every 2 weeks until they progressed or developed unacceptable toxicity.
There were 38 patients in the safety analysis. They had a median age of 58.5 years, and 61% were male.
Thirty-five of these patients were included in the efficacy analysis. They had a median of 2 prior treatments (range, 1-8), and 17 patients (49%) had responded to their last therapy.
The patients had PTCL-NOS (43%, 15/35), AITL (34%, 12), transformed mycosis fungoides (9%, 3), ALK- ALCL (11%, 4), and ALK+ ALCL (3%, 1).
The ORR was 11% (n=4), and 46% of patients (n=16) had SD or better. Two patients with PTCL-NOS responded, as did 2 with AITL.
Six patients with PTCL-NOS had SD, as did 3 with AITL, 1 with transformed mycosis fungoides, and 2 with ALK- ALCL.
The median duration of response (including SD) was 2.9 months. And the median PFS was 2.1 months. Two patients (1 with ALK- ALCL and 1 with PTCL-NOS) went on to allo-SCT.
The most frequent adverse events (occurring in at least 10% of patients) were drug eruption (n=12), pyrexia (n=9), pruritus (n=7), diarrhea (n=7), cough (n=6), vomiting (n=6), thrombocytopenia (n=6), hypotension (n=4), headache (n=4), peripheral edema (n=4), asthenia (n=4), nausea (n=4), anemia (n=4), and neutropenia (n=4).
“For the European experience, there were some differences from the Japanese experience,” Dr Zinzani said in closing. “It was worse in terms of overall response rate—only 11%—but roughly 50% of patients attained at least stable disease. And there was an acceptable safety profile in these really heavily pretreated, relapsed/refractory PTCL patients.” ![]()
SAN FRANCISCO—Two phase 2 studies testing mogamulizumab in peripheral T-cell lymphomas (PTCLs) suggest that higher response rates don’t necessarily translate to an improvement in progression-free survival (PFS).
The anti-CCR4 antibody produced a higher overall response rate (ORR) in a Japanese study than in a European study—34% and 11%, respectively.
However, median PFS times were similar—about 2 months in both studies.
This similarity is all the more interesting because the studies enrolled different types of patients and followed different dosing schedules, according to Pier Luigi Zinzani, MD, PhD, of the University of Bologna in Italy.
Dr Zinzani discussed details of the European experience testing mogamulizumab in PTCL, comparing it to the Japanese experience, in a presentation at the 7th Annual T-cell Lymphoma Forum.
Kensei Tobinai, MD, PhD, of the National Cancer Center Hospital in Tokyo, Japan, also reviewed the Japanese experience (TCLF 2013, JCO 2014) during the meeting’s keynote address and presented data from an ancillary analysis of this study (which is unpublished).
All of the research was sponsored by Kyowa Hakko Kirin Co., Ltd., the company developing mogamulizumab.
The Japanese experience
The Japanese study included 29 patients with PTCL and 8 with cutaneous T-cell lymphoma (CTCL). All patients had relapsed after their last chemotherapy regimen, and none had received an allogeneic stem cell transplant (allo-SCT). The PTCL patients had a median age of 67, and 69% were male.
All patients received mogamulizumab at 1.0 mg/kg/day weekly for 8 weeks. The ORR was 35%—34% for PTCL patients and 38% for CTCL patients.
Among PTCL patients, there were 5 complete responses (CRs) and 5 partial responses (PRs). Nine patients had stable disease (SD), and 10 progressed.
Of the 16 patients with PTCL-not otherwise specified (PTCL-NOS), 1 had a CR, 2 had a PR, 6 had SD, and 7 progressed. Of the 12 patients with angioimmunoblastic T-cell lymphoma (AITL), 3 had a CR, 3 had a PR, 3 had SD, and 3 progressed. The only patient with ALK- anaplastic large-cell lymphoma (ALCL) had an unconfirmed CR.
The ancillary analysis showed that tumor shrinkage of the target lesions occurred in 72% (21/29) of patients with PTCL. The patients’ median duration of response was 6.4 months, and the median time to response was 1.9 months.
Overall, the median PFS was 3.0 months—2.0 months in patients with PTCL and 3.4 months in patients with CTCL.
Common adverse events (for both PTCL and CTCL patients) included lymphopenia (81%), skin disorders (51%), leukopenia (43%), neutropenia (38%), thrombocytopenia (38%), pyrexia (30%), acute infusion reactions (24%), and anemia (14%).
Dr Tobinai noted that these results are not as favorable as those observed when patients with adult T-cell leukemia-lymphoma receive mogamulizumab.
“But compared to the efficacy rate of other approved agents—pralatrexate and romidepsin—this antibody has promising efficacy,” he said.
In fact, the results of this study prompted the December approval of mogamulizumab to treat PTCL and CTCL patients in Japan.
The European experience
The European study differed from the Japanese study in a few ways, Dr Zinzani pointed out. The European study only enrolled patients with PTCL. And it included patients with relapsed (49%) or refractory (51%) disease, whereas the Japanese study only included relapsed patients.
Furthermore, the Japanese study did not include any patients with an ECOG performance status of 2, while the European study did (39%). And the dosing schedule differed between the 2 studies.
In the European study, patients received mogamulizumab at 1 mg/kg once weekly for 4 weeks and then once every 2 weeks until they progressed or developed unacceptable toxicity.
There were 38 patients in the safety analysis. They had a median age of 58.5 years, and 61% were male.
Thirty-five of these patients were included in the efficacy analysis. They had a median of 2 prior treatments (range, 1-8), and 17 patients (49%) had responded to their last therapy.
The patients had PTCL-NOS (43%, 15/35), AITL (34%, 12), transformed mycosis fungoides (9%, 3), ALK- ALCL (11%, 4), and ALK+ ALCL (3%, 1).
The ORR was 11% (n=4), and 46% of patients (n=16) had SD or better. Two patients with PTCL-NOS responded, as did 2 with AITL.
Six patients with PTCL-NOS had SD, as did 3 with AITL, 1 with transformed mycosis fungoides, and 2 with ALK- ALCL.
The median duration of response (including SD) was 2.9 months. And the median PFS was 2.1 months. Two patients (1 with ALK- ALCL and 1 with PTCL-NOS) went on to allo-SCT.
The most frequent adverse events (occurring in at least 10% of patients) were drug eruption (n=12), pyrexia (n=9), pruritus (n=7), diarrhea (n=7), cough (n=6), vomiting (n=6), thrombocytopenia (n=6), hypotension (n=4), headache (n=4), peripheral edema (n=4), asthenia (n=4), nausea (n=4), anemia (n=4), and neutropenia (n=4).
“For the European experience, there were some differences from the Japanese experience,” Dr Zinzani said in closing. “It was worse in terms of overall response rate—only 11%—but roughly 50% of patients attained at least stable disease. And there was an acceptable safety profile in these really heavily pretreated, relapsed/refractory PTCL patients.” ![]()
Though costly, blood cancer drugs appear cost-effective

Photo by Bill Branson
A new analysis indicates that certain high-cost therapies for hematologic malignancies provide reasonable value for money spent.
Most cost-effectiveness ratios were lower than thresholds commonly used to establish cost-effectiveness in the US—$50,000 or $100,000 per quality-adjusted life year (QALY) gained.
The median cost-effectiveness ratio was highest for chronic myeloid leukemia (CML), at $55,000/QALY, and lowest for non-Hodgkin lymphoma (NHL), at $21,500/QALY.
Researchers presented these data in Blood.
“Given the increased discussion about the high cost of these treatments, we were somewhat surprised to discover that their cost-effectiveness ratios were lower than expected,” said study author Peter J. Neumann, ScD, of Tufts Medical Center in Boston.
“Our analysis had a small sample size and included both industry- and non-industry-funded studies. In addition, cost-effectiveness ratios may have changed over time as associated costs or benefits have changed. However, the study underscores that debates in healthcare should consider the value of breakthrough drugs and not just costs.”
With that issue in mind, Dr Neumann and his colleagues had conducted a systematic review of studies published between 1996 and 2012 that examined the cost utility of agents for hematologic malignancies. The cost utility of a drug was depicted as a ratio of a drug’s total cost per patient QALY gained.
The researchers identified 29 studies, 22 of which were industry-funded. Nine studies were conducted from a US perspective, 6 from the UK, 3 from Norway, 3 from Sweden, 2 from France, 1 from Canada, 1 from Finland, and 4 from “other” countries.
The team grouped studies according to malignancy—CML, chronic lymphocytic leukemia (CLL), NHL, and multiple myeloma (MM)—as well as by treatment—α interferon, alemtuzumab, bendamustine, bortezomib, dasatinib, imatinib, lenalidomide, rituximab alone or in combination, and thalidomide.
The studies reported 44 cost-effectiveness ratios, most concerning interventions for NHL (41%) or CML (30%). Most ratios pertained to rituximab (43%), α interferon (18%), or imatinib (16%), and the most common intervention-disease combination was rituximab (alone or in combination) for NHL (36%).
The median cost-effectiveness ratios fluctuated over time, rising from $35,000/QALY (1996-2002) to $52,000/QALY (2003-2006), then falling to $22,000/QALY (2007-2012).
The median cost-effectiveness ratio reported by industry-funded studies was lower ($26,000/QALY) than for non-industry-funded studies ($33,000/QALY).
Four cost-effectiveness ratios, 1 from an industry-funded study, exceeded $100,000/QALY. This included 2 studies of bortezomib in MM, 1 of α interferon in CML, and 1 of imatinib in CML.
The researchers said these results suggest that many new treatments for hematologic malignancies may confer reasonable value for money spent. The distribution of cost-effectiveness ratios is comparable to those for cancers overall and for other healthcare fields, they said.
This study was funded by internal resources at the Center for the Evaluation of Value and Risk in Health. The center receives funding from federal, private foundation, and pharmaceutical industry sources. ![]()

Photo by Bill Branson
A new analysis indicates that certain high-cost therapies for hematologic malignancies provide reasonable value for money spent.
Most cost-effectiveness ratios were lower than thresholds commonly used to establish cost-effectiveness in the US—$50,000 or $100,000 per quality-adjusted life year (QALY) gained.
The median cost-effectiveness ratio was highest for chronic myeloid leukemia (CML), at $55,000/QALY, and lowest for non-Hodgkin lymphoma (NHL), at $21,500/QALY.
Researchers presented these data in Blood.
“Given the increased discussion about the high cost of these treatments, we were somewhat surprised to discover that their cost-effectiveness ratios were lower than expected,” said study author Peter J. Neumann, ScD, of Tufts Medical Center in Boston.
“Our analysis had a small sample size and included both industry- and non-industry-funded studies. In addition, cost-effectiveness ratios may have changed over time as associated costs or benefits have changed. However, the study underscores that debates in healthcare should consider the value of breakthrough drugs and not just costs.”
With that issue in mind, Dr Neumann and his colleagues had conducted a systematic review of studies published between 1996 and 2012 that examined the cost utility of agents for hematologic malignancies. The cost utility of a drug was depicted as a ratio of a drug’s total cost per patient QALY gained.
The researchers identified 29 studies, 22 of which were industry-funded. Nine studies were conducted from a US perspective, 6 from the UK, 3 from Norway, 3 from Sweden, 2 from France, 1 from Canada, 1 from Finland, and 4 from “other” countries.
The team grouped studies according to malignancy—CML, chronic lymphocytic leukemia (CLL), NHL, and multiple myeloma (MM)—as well as by treatment—α interferon, alemtuzumab, bendamustine, bortezomib, dasatinib, imatinib, lenalidomide, rituximab alone or in combination, and thalidomide.
The studies reported 44 cost-effectiveness ratios, most concerning interventions for NHL (41%) or CML (30%). Most ratios pertained to rituximab (43%), α interferon (18%), or imatinib (16%), and the most common intervention-disease combination was rituximab (alone or in combination) for NHL (36%).
The median cost-effectiveness ratios fluctuated over time, rising from $35,000/QALY (1996-2002) to $52,000/QALY (2003-2006), then falling to $22,000/QALY (2007-2012).
The median cost-effectiveness ratio reported by industry-funded studies was lower ($26,000/QALY) than for non-industry-funded studies ($33,000/QALY).
Four cost-effectiveness ratios, 1 from an industry-funded study, exceeded $100,000/QALY. This included 2 studies of bortezomib in MM, 1 of α interferon in CML, and 1 of imatinib in CML.
The researchers said these results suggest that many new treatments for hematologic malignancies may confer reasonable value for money spent. The distribution of cost-effectiveness ratios is comparable to those for cancers overall and for other healthcare fields, they said.
This study was funded by internal resources at the Center for the Evaluation of Value and Risk in Health. The center receives funding from federal, private foundation, and pharmaceutical industry sources. ![]()

Photo by Bill Branson
A new analysis indicates that certain high-cost therapies for hematologic malignancies provide reasonable value for money spent.
Most cost-effectiveness ratios were lower than thresholds commonly used to establish cost-effectiveness in the US—$50,000 or $100,000 per quality-adjusted life year (QALY) gained.
The median cost-effectiveness ratio was highest for chronic myeloid leukemia (CML), at $55,000/QALY, and lowest for non-Hodgkin lymphoma (NHL), at $21,500/QALY.
Researchers presented these data in Blood.
“Given the increased discussion about the high cost of these treatments, we were somewhat surprised to discover that their cost-effectiveness ratios were lower than expected,” said study author Peter J. Neumann, ScD, of Tufts Medical Center in Boston.
“Our analysis had a small sample size and included both industry- and non-industry-funded studies. In addition, cost-effectiveness ratios may have changed over time as associated costs or benefits have changed. However, the study underscores that debates in healthcare should consider the value of breakthrough drugs and not just costs.”
With that issue in mind, Dr Neumann and his colleagues had conducted a systematic review of studies published between 1996 and 2012 that examined the cost utility of agents for hematologic malignancies. The cost utility of a drug was depicted as a ratio of a drug’s total cost per patient QALY gained.
The researchers identified 29 studies, 22 of which were industry-funded. Nine studies were conducted from a US perspective, 6 from the UK, 3 from Norway, 3 from Sweden, 2 from France, 1 from Canada, 1 from Finland, and 4 from “other” countries.
The team grouped studies according to malignancy—CML, chronic lymphocytic leukemia (CLL), NHL, and multiple myeloma (MM)—as well as by treatment—α interferon, alemtuzumab, bendamustine, bortezomib, dasatinib, imatinib, lenalidomide, rituximab alone or in combination, and thalidomide.
The studies reported 44 cost-effectiveness ratios, most concerning interventions for NHL (41%) or CML (30%). Most ratios pertained to rituximab (43%), α interferon (18%), or imatinib (16%), and the most common intervention-disease combination was rituximab (alone or in combination) for NHL (36%).
The median cost-effectiveness ratios fluctuated over time, rising from $35,000/QALY (1996-2002) to $52,000/QALY (2003-2006), then falling to $22,000/QALY (2007-2012).
The median cost-effectiveness ratio reported by industry-funded studies was lower ($26,000/QALY) than for non-industry-funded studies ($33,000/QALY).
Four cost-effectiveness ratios, 1 from an industry-funded study, exceeded $100,000/QALY. This included 2 studies of bortezomib in MM, 1 of α interferon in CML, and 1 of imatinib in CML.
The researchers said these results suggest that many new treatments for hematologic malignancies may confer reasonable value for money spent. The distribution of cost-effectiveness ratios is comparable to those for cancers overall and for other healthcare fields, they said.
This study was funded by internal resources at the Center for the Evaluation of Value and Risk in Health. The center receives funding from federal, private foundation, and pharmaceutical industry sources. ![]()
EC approves bortezomib for MCL

Photo courtesy of Millennium
The European Commission (EC) has approved bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) in whom hematopoietic stem cell transplant (HSCT) is considered unsuitable.
Now, bortezomib can be marketed for this indication in all 28 countries of the European Union (EU).
Bortezomib is already approved in the EU to treat multiple myeloma (MM), either as monotherapy or in combination with other agents.
The EC’s approval of bortezomib in MCL is based on data from a phase 3 study known as LYM-3002.
This randomized trial included 487 patients with newly diagnosed MCL who were ineligible, or not considered, for HSCT. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AEs) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
About bortezomib
Bortezomib works by reversibly interrupting the normal working of cell proteasomes, inducing cancerous cells to stop growing and die.
In addition to the new MCL indication, the drug is approved in the EU to treat various stages of MM. It’s approved in combination with melphalan and prednisone to treat previously untreated adults with MM who are unsuitable for high-dose chemotherapy with HSCT.
Bortezomib is also approved in combination with dexamethasone, or with dexamethasone plus thalidomide, to treat previously untreated MM patients set to receive high-dose chemotherapy followed by HSCT.
And the drug is approved as monotherapy or in combination with pegylated liposomal doxorubicin or dexamethasone to treat adults with MM whose disease has progressed after at least one other treatment and who have already had, or cannot undergo, HSCT.
Bortezomib is approved in more than 90 countries and has been used to treat more than 550,000 patients worldwide.
The product is co-developed by Millennium, the Takeda Oncology Company, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, and Janssen Pharmaceutical Companies.
Millennium is responsible for commercialization in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world. Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote the drug in Japan. ![]()

Photo courtesy of Millennium
The European Commission (EC) has approved bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) in whom hematopoietic stem cell transplant (HSCT) is considered unsuitable.
Now, bortezomib can be marketed for this indication in all 28 countries of the European Union (EU).
Bortezomib is already approved in the EU to treat multiple myeloma (MM), either as monotherapy or in combination with other agents.
The EC’s approval of bortezomib in MCL is based on data from a phase 3 study known as LYM-3002.
This randomized trial included 487 patients with newly diagnosed MCL who were ineligible, or not considered, for HSCT. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AEs) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
About bortezomib
Bortezomib works by reversibly interrupting the normal working of cell proteasomes, inducing cancerous cells to stop growing and die.
In addition to the new MCL indication, the drug is approved in the EU to treat various stages of MM. It’s approved in combination with melphalan and prednisone to treat previously untreated adults with MM who are unsuitable for high-dose chemotherapy with HSCT.
Bortezomib is also approved in combination with dexamethasone, or with dexamethasone plus thalidomide, to treat previously untreated MM patients set to receive high-dose chemotherapy followed by HSCT.
And the drug is approved as monotherapy or in combination with pegylated liposomal doxorubicin or dexamethasone to treat adults with MM whose disease has progressed after at least one other treatment and who have already had, or cannot undergo, HSCT.
Bortezomib is approved in more than 90 countries and has been used to treat more than 550,000 patients worldwide.
The product is co-developed by Millennium, the Takeda Oncology Company, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, and Janssen Pharmaceutical Companies.
Millennium is responsible for commercialization in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world. Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote the drug in Japan. ![]()

Photo courtesy of Millennium
The European Commission (EC) has approved bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) in whom hematopoietic stem cell transplant (HSCT) is considered unsuitable.
Now, bortezomib can be marketed for this indication in all 28 countries of the European Union (EU).
Bortezomib is already approved in the EU to treat multiple myeloma (MM), either as monotherapy or in combination with other agents.
The EC’s approval of bortezomib in MCL is based on data from a phase 3 study known as LYM-3002.
This randomized trial included 487 patients with newly diagnosed MCL who were ineligible, or not considered, for HSCT. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AEs) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85% of patients, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3% of patients, respectively.
About bortezomib
Bortezomib works by reversibly interrupting the normal working of cell proteasomes, inducing cancerous cells to stop growing and die.
In addition to the new MCL indication, the drug is approved in the EU to treat various stages of MM. It’s approved in combination with melphalan and prednisone to treat previously untreated adults with MM who are unsuitable for high-dose chemotherapy with HSCT.
Bortezomib is also approved in combination with dexamethasone, or with dexamethasone plus thalidomide, to treat previously untreated MM patients set to receive high-dose chemotherapy followed by HSCT.
And the drug is approved as monotherapy or in combination with pegylated liposomal doxorubicin or dexamethasone to treat adults with MM whose disease has progressed after at least one other treatment and who have already had, or cannot undergo, HSCT.
Bortezomib is approved in more than 90 countries and has been used to treat more than 550,000 patients worldwide.
The product is co-developed by Millennium, the Takeda Oncology Company, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, and Janssen Pharmaceutical Companies.
Millennium is responsible for commercialization in the US. Janssen Pharmaceutical Companies are responsible for commercialization in Europe and the rest of the world. Takeda Pharmaceutical Company Limited and Janssen Pharmaceutical K.K. co-promote the drug in Japan. ![]()
Aggressiveness of CLL linked to genetic variability

The genetic variability of chronic lymphocytic leukemia (CLL) appears to predict its aggressiveness, according to a study published in Genome Medicine.
Investigators found evidence suggesting that greater variability in gene expression is associated with more aggressive disease.
The team analyzed gene expression in two cohorts of CLL patients—those with IgVH mutations and a good prognosis and those with unmutated CLL who have more aggressive disease.
The researchers examined 70 mutated and 52 unmutated CLL samples, as well as 20 control samples taken from healthy individuals.
Unmutated, aggressive CLL showed increased gene expression variability across individuals, whereas gene expression variability was lower in less aggressive, mutated CLL.
The investigators validated these observations by comparing them against a second sample group consisting of 24 mutated and 36 unmutated CLL samples.
The results suggested that CLL aggressiveness is specifically determined by a set of 500 genes showing increased expression variability across individuals. The genes are involved in processes such as adaptation to the environment, cell death, tumor growth, and drug resistance.
“Our conclusion is that the coefficient of variation for gene expression in CLL efficiently predicts its aggressiveness,” said study author Alfonso Valencia, PhD, of Centro Nacional de Investigaciones Oncologicas (CNIO) in Madrid, Spain.
“More importantly, if further research confirms these findings, a classifier based on the measurement of gene expression variability could be created to predict the disease subtype of CLL patients.”
The researchers said their next step is to discover the mechanisms responsible for the high levels of expression variability for a given gene across individuals.
Understanding the mechanisms underlying this phenomenon is of crucial relevance for oncology research, the investigators said, as it is linked to tumor heterogeneity, a key feature of cancer progression and drug resistance.
The greater the genetic variability in a tumor, the better it will adapt to its environment, and the more probabilities for this tumor to spread, develop resistance to cancer therapies, and metastasize to distant organs. ![]()

The genetic variability of chronic lymphocytic leukemia (CLL) appears to predict its aggressiveness, according to a study published in Genome Medicine.
Investigators found evidence suggesting that greater variability in gene expression is associated with more aggressive disease.
The team analyzed gene expression in two cohorts of CLL patients—those with IgVH mutations and a good prognosis and those with unmutated CLL who have more aggressive disease.
The researchers examined 70 mutated and 52 unmutated CLL samples, as well as 20 control samples taken from healthy individuals.
Unmutated, aggressive CLL showed increased gene expression variability across individuals, whereas gene expression variability was lower in less aggressive, mutated CLL.
The investigators validated these observations by comparing them against a second sample group consisting of 24 mutated and 36 unmutated CLL samples.
The results suggested that CLL aggressiveness is specifically determined by a set of 500 genes showing increased expression variability across individuals. The genes are involved in processes such as adaptation to the environment, cell death, tumor growth, and drug resistance.
“Our conclusion is that the coefficient of variation for gene expression in CLL efficiently predicts its aggressiveness,” said study author Alfonso Valencia, PhD, of Centro Nacional de Investigaciones Oncologicas (CNIO) in Madrid, Spain.
“More importantly, if further research confirms these findings, a classifier based on the measurement of gene expression variability could be created to predict the disease subtype of CLL patients.”
The researchers said their next step is to discover the mechanisms responsible for the high levels of expression variability for a given gene across individuals.
Understanding the mechanisms underlying this phenomenon is of crucial relevance for oncology research, the investigators said, as it is linked to tumor heterogeneity, a key feature of cancer progression and drug resistance.
The greater the genetic variability in a tumor, the better it will adapt to its environment, and the more probabilities for this tumor to spread, develop resistance to cancer therapies, and metastasize to distant organs. ![]()

The genetic variability of chronic lymphocytic leukemia (CLL) appears to predict its aggressiveness, according to a study published in Genome Medicine.
Investigators found evidence suggesting that greater variability in gene expression is associated with more aggressive disease.
The team analyzed gene expression in two cohorts of CLL patients—those with IgVH mutations and a good prognosis and those with unmutated CLL who have more aggressive disease.
The researchers examined 70 mutated and 52 unmutated CLL samples, as well as 20 control samples taken from healthy individuals.
Unmutated, aggressive CLL showed increased gene expression variability across individuals, whereas gene expression variability was lower in less aggressive, mutated CLL.
The investigators validated these observations by comparing them against a second sample group consisting of 24 mutated and 36 unmutated CLL samples.
The results suggested that CLL aggressiveness is specifically determined by a set of 500 genes showing increased expression variability across individuals. The genes are involved in processes such as adaptation to the environment, cell death, tumor growth, and drug resistance.
“Our conclusion is that the coefficient of variation for gene expression in CLL efficiently predicts its aggressiveness,” said study author Alfonso Valencia, PhD, of Centro Nacional de Investigaciones Oncologicas (CNIO) in Madrid, Spain.
“More importantly, if further research confirms these findings, a classifier based on the measurement of gene expression variability could be created to predict the disease subtype of CLL patients.”
The researchers said their next step is to discover the mechanisms responsible for the high levels of expression variability for a given gene across individuals.
Understanding the mechanisms underlying this phenomenon is of crucial relevance for oncology research, the investigators said, as it is linked to tumor heterogeneity, a key feature of cancer progression and drug resistance.
The greater the genetic variability in a tumor, the better it will adapt to its environment, and the more probabilities for this tumor to spread, develop resistance to cancer therapies, and metastasize to distant organs.
Risk of HBV reactivation ‘underappreciated’

Credit: CDC
Reactivation of the hepatitis B virus (HBV) may be more of a risk than we anticipated, investigators have reported in Hepatology.
Their research indicates that HBV reactivation is associated with the use of chemotherapy, high-dose corticosteroids, biologics targeting tumor necrosis factor-alpha (TNF-α), and agents that aren’t really considered immunosuppressive.
HBV reactivation is also fairly common after organ transplant and hematopoietic stem cell transplant (HSCT).
As reactivation of HBV can be fatal, the study authors suggest routine screening of HBV in all patients prior to the start of these treatments.
The researchers noted that, in September 2013, the US Food and Drug Administration (FDA) issued a Drug Safety Communication in an attempt to decrease the risk of HBV reactivation. The communication advised healthcare professionals to screen patients for HBV prior to the administration of ofatumumab or rituximab.
“[T]his may be just the tip of the iceberg,” said Adrian Di Bisceglie, MD, of Saint Louis University School of Medicine in Missouri.
“Our research suggests that the issue of HBV reactivation may be an underappreciated clinical challenge that extends well beyond the use of just two anti-CD20 medications.”
After a systematic literature review, Dr Di Bisceglie and his colleagues identified 504 studies pertaining to reactivation of HBV.
The investigators reviewed 14 studies in which the antiviral agent lamivudine was used to prevent HBV reactivation in HBsAg-positive patients receiving chemotherapy. Among patients who did not receive lamivudine, HBV reactivation occurred in 32%. Thirteen percent of patients experienced liver failure, and 7% died.
The researchers also looked at patients undergoing HSCT. In one study, 61 patients had resolved HBV infection before HSCT. But 12 of these patients (20%) developed reverse seroconversion (reappearance of HBsAg in a person who was HBsAg-negative, anti-HBc-positive prior to HSCT).
The cumulative probability of reverse seroconversion was 9% a year after HSCT, 21.7% at 2 years, and 42.9% at 4 years.
The investigators also noted that high-dose corticosteroids carry a significant risk of HBV reactivation, both as part of combination treatment for malignancies and when used alone to treat benign conditions.
In addition, the researchers found data showing that HBV reactivation has occurred with antitumor agents that are not thought to be particularly immunosuppressive, such as imatinib and thalidomide. The team said this raises questions about the mechanisms by which drugs are causing HBV reactivation.
The investigators also looked at data from 257 patients with active or recovered HBV infection who received treatment with biological therapies targeting TNF-α.
Forty-two percent of the patients had elevations in serum aminotransferase levels, 39% had reappearance of HBV DNA, 16% had signs and symptoms of liver disease, and 5% died of liver failure.
HBV reactivation was more frequent among patients receiving infliximab than etanercept. It was 7-fold higher among patients who were HBsAg-positive (38%) than those who were HBsAg-negative but anti-HBc-positive (5%).
While it remains unclear how HBV reactivation occurs, experts believe a loss of immune control over viral replication may trigger the process.
“Further study and cooperation between various medical disciplines will help broaden understanding of HBV reactivation,” Dr Di Bisceglie concluded.

Credit: CDC
Reactivation of the hepatitis B virus (HBV) may be more of a risk than we anticipated, investigators have reported in Hepatology.
Their research indicates that HBV reactivation is associated with the use of chemotherapy, high-dose corticosteroids, biologics targeting tumor necrosis factor-alpha (TNF-α), and agents that aren’t really considered immunosuppressive.
HBV reactivation is also fairly common after organ transplant and hematopoietic stem cell transplant (HSCT).
As reactivation of HBV can be fatal, the study authors suggest routine screening of HBV in all patients prior to the start of these treatments.
The researchers noted that, in September 2013, the US Food and Drug Administration (FDA) issued a Drug Safety Communication in an attempt to decrease the risk of HBV reactivation. The communication advised healthcare professionals to screen patients for HBV prior to the administration of ofatumumab or rituximab.
“[T]his may be just the tip of the iceberg,” said Adrian Di Bisceglie, MD, of Saint Louis University School of Medicine in Missouri.
“Our research suggests that the issue of HBV reactivation may be an underappreciated clinical challenge that extends well beyond the use of just two anti-CD20 medications.”
After a systematic literature review, Dr Di Bisceglie and his colleagues identified 504 studies pertaining to reactivation of HBV.
The investigators reviewed 14 studies in which the antiviral agent lamivudine was used to prevent HBV reactivation in HBsAg-positive patients receiving chemotherapy. Among patients who did not receive lamivudine, HBV reactivation occurred in 32%. Thirteen percent of patients experienced liver failure, and 7% died.
The researchers also looked at patients undergoing HSCT. In one study, 61 patients had resolved HBV infection before HSCT. But 12 of these patients (20%) developed reverse seroconversion (reappearance of HBsAg in a person who was HBsAg-negative, anti-HBc-positive prior to HSCT).
The cumulative probability of reverse seroconversion was 9% a year after HSCT, 21.7% at 2 years, and 42.9% at 4 years.
The investigators also noted that high-dose corticosteroids carry a significant risk of HBV reactivation, both as part of combination treatment for malignancies and when used alone to treat benign conditions.
In addition, the researchers found data showing that HBV reactivation has occurred with antitumor agents that are not thought to be particularly immunosuppressive, such as imatinib and thalidomide. The team said this raises questions about the mechanisms by which drugs are causing HBV reactivation.
The investigators also looked at data from 257 patients with active or recovered HBV infection who received treatment with biological therapies targeting TNF-α.
Forty-two percent of the patients had elevations in serum aminotransferase levels, 39% had reappearance of HBV DNA, 16% had signs and symptoms of liver disease, and 5% died of liver failure.
HBV reactivation was more frequent among patients receiving infliximab than etanercept. It was 7-fold higher among patients who were HBsAg-positive (38%) than those who were HBsAg-negative but anti-HBc-positive (5%).
While it remains unclear how HBV reactivation occurs, experts believe a loss of immune control over viral replication may trigger the process.
“Further study and cooperation between various medical disciplines will help broaden understanding of HBV reactivation,” Dr Di Bisceglie concluded.

Credit: CDC
Reactivation of the hepatitis B virus (HBV) may be more of a risk than we anticipated, investigators have reported in Hepatology.
Their research indicates that HBV reactivation is associated with the use of chemotherapy, high-dose corticosteroids, biologics targeting tumor necrosis factor-alpha (TNF-α), and agents that aren’t really considered immunosuppressive.
HBV reactivation is also fairly common after organ transplant and hematopoietic stem cell transplant (HSCT).
As reactivation of HBV can be fatal, the study authors suggest routine screening of HBV in all patients prior to the start of these treatments.
The researchers noted that, in September 2013, the US Food and Drug Administration (FDA) issued a Drug Safety Communication in an attempt to decrease the risk of HBV reactivation. The communication advised healthcare professionals to screen patients for HBV prior to the administration of ofatumumab or rituximab.
“[T]his may be just the tip of the iceberg,” said Adrian Di Bisceglie, MD, of Saint Louis University School of Medicine in Missouri.
“Our research suggests that the issue of HBV reactivation may be an underappreciated clinical challenge that extends well beyond the use of just two anti-CD20 medications.”
After a systematic literature review, Dr Di Bisceglie and his colleagues identified 504 studies pertaining to reactivation of HBV.
The investigators reviewed 14 studies in which the antiviral agent lamivudine was used to prevent HBV reactivation in HBsAg-positive patients receiving chemotherapy. Among patients who did not receive lamivudine, HBV reactivation occurred in 32%. Thirteen percent of patients experienced liver failure, and 7% died.
The researchers also looked at patients undergoing HSCT. In one study, 61 patients had resolved HBV infection before HSCT. But 12 of these patients (20%) developed reverse seroconversion (reappearance of HBsAg in a person who was HBsAg-negative, anti-HBc-positive prior to HSCT).
The cumulative probability of reverse seroconversion was 9% a year after HSCT, 21.7% at 2 years, and 42.9% at 4 years.
The investigators also noted that high-dose corticosteroids carry a significant risk of HBV reactivation, both as part of combination treatment for malignancies and when used alone to treat benign conditions.
In addition, the researchers found data showing that HBV reactivation has occurred with antitumor agents that are not thought to be particularly immunosuppressive, such as imatinib and thalidomide. The team said this raises questions about the mechanisms by which drugs are causing HBV reactivation.
The investigators also looked at data from 257 patients with active or recovered HBV infection who received treatment with biological therapies targeting TNF-α.
Forty-two percent of the patients had elevations in serum aminotransferase levels, 39% had reappearance of HBV DNA, 16% had signs and symptoms of liver disease, and 5% died of liver failure.
HBV reactivation was more frequent among patients receiving infliximab than etanercept. It was 7-fold higher among patients who were HBsAg-positive (38%) than those who were HBsAg-negative but anti-HBc-positive (5%).
While it remains unclear how HBV reactivation occurs, experts believe a loss of immune control over viral replication may trigger the process.
“Further study and cooperation between various medical disciplines will help broaden understanding of HBV reactivation,” Dr Di Bisceglie concluded.
Vaccine gets orphan designation for ATLL
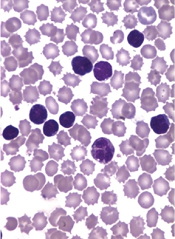
The European Medicines Agency (EMA) has granted orphan drug designation for a therapeutic vaccine candidate known as THV02 to treat adult T-cell leukemia/lymphoma (ATLL).
THV02 is an experimental treatment composed of 2 lentiviral vectors to be used in a prime/boost regimen in ATLL patients infected by the HTLV-1 virus.
Both investigational drugs encode the same antigens, derived from 4 proteins of the HTLV-1 virus.
THV02 is intended to induce an immune response against HTLV antigens born by ATLL with the aim of enabling the patients’ immune system to fight leukemic cells.
Preclinical evaluation has suggested that THV02 is safe, and the vaccine has presented an “unprecedented” immunogenicity profile in several models, according to THERAVECTYS, the company developing THV02.
“Preclinical immunogenicity results obtained to date are very promising, and we are really excited by the prospect of bringing a safe and better-tolerated alternative to patients who are desperately in need of a treatment,” said Déborah Revaud, the senior scientist in charge of developing THV02.
The EMA grants orphan designation to drugs in development intended for the treatment, prevention, or diagnosis of life-threatening or chronically debilitating diseases occurring in fewer than 5 in 10,000 people.
The designation allows sponsors to benefit from an accelerated development process, financial incentives, and a 10-year period of market exclusivity once the drug is on the market.
“We are extremely pleased that the European Medicines Agency has granted an orphan drug status to our vaccine candidate against ATLL,” said Emmanuelle Sabbah-Petrover, PhD, head of regulatory affairs at THERAVECTYS.
“We expect to recruit our first patients towards the end of Q3 2015 in Europe and advance further developments in the US and in Japan in 2016.”
Should THV02 demonstrate a convincing safety and efficacy profile during its development against ATLL, THERAVECTYS said it will consider developing the vaccine for HTLV-related infections as treatment and possibly as prophylaxis.
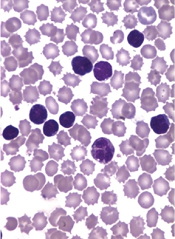
The European Medicines Agency (EMA) has granted orphan drug designation for a therapeutic vaccine candidate known as THV02 to treat adult T-cell leukemia/lymphoma (ATLL).
THV02 is an experimental treatment composed of 2 lentiviral vectors to be used in a prime/boost regimen in ATLL patients infected by the HTLV-1 virus.
Both investigational drugs encode the same antigens, derived from 4 proteins of the HTLV-1 virus.
THV02 is intended to induce an immune response against HTLV antigens born by ATLL with the aim of enabling the patients’ immune system to fight leukemic cells.
Preclinical evaluation has suggested that THV02 is safe, and the vaccine has presented an “unprecedented” immunogenicity profile in several models, according to THERAVECTYS, the company developing THV02.
“Preclinical immunogenicity results obtained to date are very promising, and we are really excited by the prospect of bringing a safe and better-tolerated alternative to patients who are desperately in need of a treatment,” said Déborah Revaud, the senior scientist in charge of developing THV02.
The EMA grants orphan designation to drugs in development intended for the treatment, prevention, or diagnosis of life-threatening or chronically debilitating diseases occurring in fewer than 5 in 10,000 people.
The designation allows sponsors to benefit from an accelerated development process, financial incentives, and a 10-year period of market exclusivity once the drug is on the market.
“We are extremely pleased that the European Medicines Agency has granted an orphan drug status to our vaccine candidate against ATLL,” said Emmanuelle Sabbah-Petrover, PhD, head of regulatory affairs at THERAVECTYS.
“We expect to recruit our first patients towards the end of Q3 2015 in Europe and advance further developments in the US and in Japan in 2016.”
Should THV02 demonstrate a convincing safety and efficacy profile during its development against ATLL, THERAVECTYS said it will consider developing the vaccine for HTLV-related infections as treatment and possibly as prophylaxis.
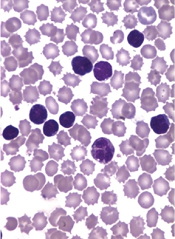
The European Medicines Agency (EMA) has granted orphan drug designation for a therapeutic vaccine candidate known as THV02 to treat adult T-cell leukemia/lymphoma (ATLL).
THV02 is an experimental treatment composed of 2 lentiviral vectors to be used in a prime/boost regimen in ATLL patients infected by the HTLV-1 virus.
Both investigational drugs encode the same antigens, derived from 4 proteins of the HTLV-1 virus.
THV02 is intended to induce an immune response against HTLV antigens born by ATLL with the aim of enabling the patients’ immune system to fight leukemic cells.
Preclinical evaluation has suggested that THV02 is safe, and the vaccine has presented an “unprecedented” immunogenicity profile in several models, according to THERAVECTYS, the company developing THV02.
“Preclinical immunogenicity results obtained to date are very promising, and we are really excited by the prospect of bringing a safe and better-tolerated alternative to patients who are desperately in need of a treatment,” said Déborah Revaud, the senior scientist in charge of developing THV02.
The EMA grants orphan designation to drugs in development intended for the treatment, prevention, or diagnosis of life-threatening or chronically debilitating diseases occurring in fewer than 5 in 10,000 people.
The designation allows sponsors to benefit from an accelerated development process, financial incentives, and a 10-year period of market exclusivity once the drug is on the market.
“We are extremely pleased that the European Medicines Agency has granted an orphan drug status to our vaccine candidate against ATLL,” said Emmanuelle Sabbah-Petrover, PhD, head of regulatory affairs at THERAVECTYS.
“We expect to recruit our first patients towards the end of Q3 2015 in Europe and advance further developments in the US and in Japan in 2016.”
Should THV02 demonstrate a convincing safety and efficacy profile during its development against ATLL, THERAVECTYS said it will consider developing the vaccine for HTLV-related infections as treatment and possibly as prophylaxis.
MicroRNA may be therapeutic target for ALK- ALCL
SAN FRANCISCO—MicroRNA-155 (miR-155) can act as an oncogenic driver in ALK− anaplastic large-cell lymphoma (ALCL) and may therefore be a therapeutic target for the disease, according to a presentation at the 7th Annual T-cell Lymphoma Forum.
Analyzing patient samples and cell lines, researchers discovered that miR-155 is highly expressed in ALK− ALCL but is nearly absent in ALK+ ALCL.
They also found evidence suggesting that miR-155 drives tumor growth in mouse models of ALK− ALCL.
Philipp Staber, MD, PhD, of the Medical University of Vienna in Austria, presented these findings at the meeting.
Dr Staber and his colleagues previously found (Merkel et al, PNAS 2010) that miR-155 was highly expressed in ALK− ALCL. So they decided to take a closer look at the phenomenon.
They assessed miR-155 expression in samples from patients with ALK+ or ALK− ALCL, as well as 6 ALCL cell lines.
miR-155 expression was significantly higher in the ALK− patient samples than in the ALK+ samples (P<0.001). And it was significantly higher (P<0.001) in the ALK− cell lines (DL-40, Mac1, and Mac2a) than in the ALK+ cell lines (K299, SR789, and SUP-M2).
Dr Staber and his colleagues then overexpressed miR-155 in ALK+ ALCL cell lines (K299 and SR789). And they observed a decrease in known target genes of miR-155—C/EBPβ, SOCS1, and SHIP1.
The researchers also observed an inverse correlation between miR-155 host gene promoter methylation and miR-155 expression in an ALCL+ cell line, which suggested that ALK activity has no direct effect on miR-155 levels.
The team treated the K299 cell line with the ALK inhibitor crizotinib at 100 nM, 200 nM, and 400 nM doses and found that miR-155 did not increase at any dose. Dr Staber noted, however, that the researchers were only able to treat cells for a maximum of 24 hours.
The group then discovered that anti-miR-155 mimics could reduce tumor growth in mouse models of ALK- ALCL. Mice were injected with Mac1 or Mac2a cells transfected with anti-miR-155, control RNA, or pre-miR-155 oligos.
In both Mac1 and Mac2 models, tumors were substantially smaller in the anti-mir-155 mice than in the pre-miR-155 mice (P=0.038 and P=0.006, respectively). But tumor growth was not significantly reduced compared to controls.
“Immunohistochemistry in these tumors shows quite a clear picture,” Dr Staber said. “The C/EBPβ target gene is overexpressed when using anti-miR-155, and [expression is decreased] with overexpression of miR-155. And the same is true for SOCS1. STAT3 signaling is increased through overexpression of miR-155.”
The researchers observed the same effect in ALK− ALCL patient samples.
Using ALK+ cell lines (K299 and SR789), the team went on to show that miR-155 suppresses IL-8 expression and induces IL-22 expression, a finding they verified in mice.
“IL-8 is a direct target of C/EBPβ, and C/EBPβ, as shown before, is a target of miR-155, so this makes sense,” Dr Staber said. “On the other hand, IL-22 is a strong inducer of STAT3 signaling, which is strongly induced when we increase miR-155 expression.”
Dr Staber and his colleagues concluded that these findings, when taken together, suggest that miR-155 could be a therapeutic target for ALK− ALCL.
SAN FRANCISCO—MicroRNA-155 (miR-155) can act as an oncogenic driver in ALK− anaplastic large-cell lymphoma (ALCL) and may therefore be a therapeutic target for the disease, according to a presentation at the 7th Annual T-cell Lymphoma Forum.
Analyzing patient samples and cell lines, researchers discovered that miR-155 is highly expressed in ALK− ALCL but is nearly absent in ALK+ ALCL.
They also found evidence suggesting that miR-155 drives tumor growth in mouse models of ALK− ALCL.
Philipp Staber, MD, PhD, of the Medical University of Vienna in Austria, presented these findings at the meeting.
Dr Staber and his colleagues previously found (Merkel et al, PNAS 2010) that miR-155 was highly expressed in ALK− ALCL. So they decided to take a closer look at the phenomenon.
They assessed miR-155 expression in samples from patients with ALK+ or ALK− ALCL, as well as 6 ALCL cell lines.
miR-155 expression was significantly higher in the ALK− patient samples than in the ALK+ samples (P<0.001). And it was significantly higher (P<0.001) in the ALK− cell lines (DL-40, Mac1, and Mac2a) than in the ALK+ cell lines (K299, SR789, and SUP-M2).
Dr Staber and his colleagues then overexpressed miR-155 in ALK+ ALCL cell lines (K299 and SR789). And they observed a decrease in known target genes of miR-155—C/EBPβ, SOCS1, and SHIP1.
The researchers also observed an inverse correlation between miR-155 host gene promoter methylation and miR-155 expression in an ALCL+ cell line, which suggested that ALK activity has no direct effect on miR-155 levels.
The team treated the K299 cell line with the ALK inhibitor crizotinib at 100 nM, 200 nM, and 400 nM doses and found that miR-155 did not increase at any dose. Dr Staber noted, however, that the researchers were only able to treat cells for a maximum of 24 hours.
The group then discovered that anti-miR-155 mimics could reduce tumor growth in mouse models of ALK- ALCL. Mice were injected with Mac1 or Mac2a cells transfected with anti-miR-155, control RNA, or pre-miR-155 oligos.
In both Mac1 and Mac2 models, tumors were substantially smaller in the anti-mir-155 mice than in the pre-miR-155 mice (P=0.038 and P=0.006, respectively). But tumor growth was not significantly reduced compared to controls.
“Immunohistochemistry in these tumors shows quite a clear picture,” Dr Staber said. “The C/EBPβ target gene is overexpressed when using anti-miR-155, and [expression is decreased] with overexpression of miR-155. And the same is true for SOCS1. STAT3 signaling is increased through overexpression of miR-155.”
The researchers observed the same effect in ALK− ALCL patient samples.
Using ALK+ cell lines (K299 and SR789), the team went on to show that miR-155 suppresses IL-8 expression and induces IL-22 expression, a finding they verified in mice.
“IL-8 is a direct target of C/EBPβ, and C/EBPβ, as shown before, is a target of miR-155, so this makes sense,” Dr Staber said. “On the other hand, IL-22 is a strong inducer of STAT3 signaling, which is strongly induced when we increase miR-155 expression.”
Dr Staber and his colleagues concluded that these findings, when taken together, suggest that miR-155 could be a therapeutic target for ALK− ALCL.
SAN FRANCISCO—MicroRNA-155 (miR-155) can act as an oncogenic driver in ALK− anaplastic large-cell lymphoma (ALCL) and may therefore be a therapeutic target for the disease, according to a presentation at the 7th Annual T-cell Lymphoma Forum.
Analyzing patient samples and cell lines, researchers discovered that miR-155 is highly expressed in ALK− ALCL but is nearly absent in ALK+ ALCL.
They also found evidence suggesting that miR-155 drives tumor growth in mouse models of ALK− ALCL.
Philipp Staber, MD, PhD, of the Medical University of Vienna in Austria, presented these findings at the meeting.
Dr Staber and his colleagues previously found (Merkel et al, PNAS 2010) that miR-155 was highly expressed in ALK− ALCL. So they decided to take a closer look at the phenomenon.
They assessed miR-155 expression in samples from patients with ALK+ or ALK− ALCL, as well as 6 ALCL cell lines.
miR-155 expression was significantly higher in the ALK− patient samples than in the ALK+ samples (P<0.001). And it was significantly higher (P<0.001) in the ALK− cell lines (DL-40, Mac1, and Mac2a) than in the ALK+ cell lines (K299, SR789, and SUP-M2).
Dr Staber and his colleagues then overexpressed miR-155 in ALK+ ALCL cell lines (K299 and SR789). And they observed a decrease in known target genes of miR-155—C/EBPβ, SOCS1, and SHIP1.
The researchers also observed an inverse correlation between miR-155 host gene promoter methylation and miR-155 expression in an ALCL+ cell line, which suggested that ALK activity has no direct effect on miR-155 levels.
The team treated the K299 cell line with the ALK inhibitor crizotinib at 100 nM, 200 nM, and 400 nM doses and found that miR-155 did not increase at any dose. Dr Staber noted, however, that the researchers were only able to treat cells for a maximum of 24 hours.
The group then discovered that anti-miR-155 mimics could reduce tumor growth in mouse models of ALK- ALCL. Mice were injected with Mac1 or Mac2a cells transfected with anti-miR-155, control RNA, or pre-miR-155 oligos.
In both Mac1 and Mac2 models, tumors were substantially smaller in the anti-mir-155 mice than in the pre-miR-155 mice (P=0.038 and P=0.006, respectively). But tumor growth was not significantly reduced compared to controls.
“Immunohistochemistry in these tumors shows quite a clear picture,” Dr Staber said. “The C/EBPβ target gene is overexpressed when using anti-miR-155, and [expression is decreased] with overexpression of miR-155. And the same is true for SOCS1. STAT3 signaling is increased through overexpression of miR-155.”
The researchers observed the same effect in ALK− ALCL patient samples.
Using ALK+ cell lines (K299 and SR789), the team went on to show that miR-155 suppresses IL-8 expression and induces IL-22 expression, a finding they verified in mice.
“IL-8 is a direct target of C/EBPβ, and C/EBPβ, as shown before, is a target of miR-155, so this makes sense,” Dr Staber said. “On the other hand, IL-22 is a strong inducer of STAT3 signaling, which is strongly induced when we increase miR-155 expression.”
Dr Staber and his colleagues concluded that these findings, when taken together, suggest that miR-155 could be a therapeutic target for ALK− ALCL.