User login
Two immunologists receive Nobel Prize in medicine
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
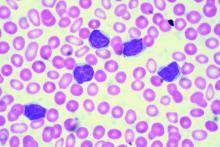
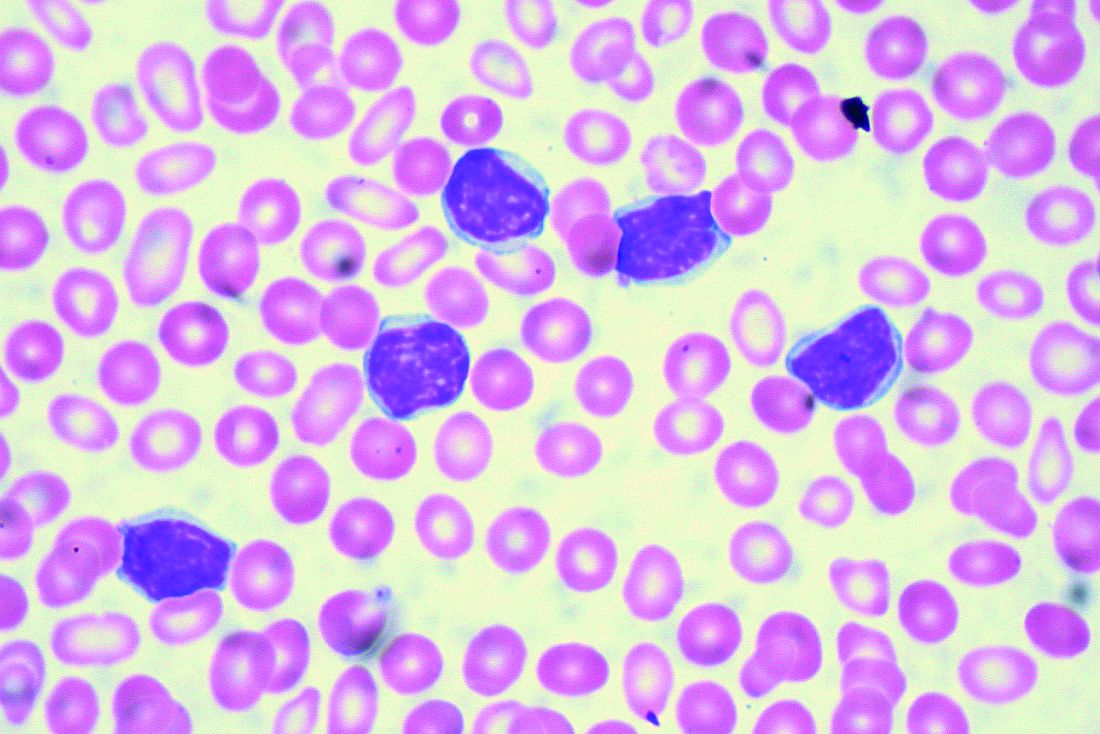
Brentuximab improves survival in older HL patients
Older patients with untreated Hodgkin lymphoma (HL) can achieve significantly improved survival by adding brentuximab vedotin to their treatment before and after standard chemotherapy, a recent study found.
In patients with low comorbidity scores, responses were even more robust, reported lead author Andrew M. Evens, DO, of the Rutgers Cancer Institute of New Jersey, and colleagues.
“Causes of poor outcomes for older patients with HL are not fully understood but have been attributed to a combination of factors, including presence of comorbidities, poorer performance status, disease and biological differences, inability to tolerate chemotherapy at the full dose, and increased treatment-related toxicities,” the authors wrote in the Journal of Clinical Oncology.
The primary goal of the study was to improve outcomes for untreated, older patients, a group that’s historically been a difficult-to-treat patient population.
The phase 2 trial included 48 HL patients with a median age of 69 (range, 60 – 88).
All patients underwent geriatric assessment for comorbidities and loss of activities of daily living.
Treatment consisted of two doses of brentuximab followed by six cycles of doxorubicin, vinblastine, and dacarbazine (AVD), then four more doses of brentuximab (consolidation doses).
The primary endpoint was complete remission at completion of AVD.
Secondary outcomes included overall response rate, 2-year progression-free survival, 2-year overall survival, and safety.
Just over half the patients (52%) completed all cycles of therapy, and almost three quarters (73%) received at least one consolidation dose of brentuximab.
Among the first 23 evaluable patients, both the complete remission rate and overall response rate were 96%. Intention-to-treat survival rates for all 48 patients were 84% for 2-year progression-free survival and 93% for 2-year overall survival.
Historical 2-year progression-free survival rates in similar older patients is poor, at 50%, so the progression-free survival rate of 84% in this study represents a significant improvement.
Of note, patients with fewer comorbidities and without loss of instrumental activities of daily living showed more robust responses.
Patients with Cumulative Illness Rating Scale for Geriatrics (CIRS-G) comorbidity scores of less than 10 had a 2-year progression-free survival rate of 100% versus 45% for those with higher scores.
Similarly, patients without loss of instrumental activities achieved a progression-free survival rate of 94% versus 25% for those who had lost some instrumental activities.
Grade 3 or 4 adverse events occurred in 42% of patients, with neutropenia being the most common (44%).
“This study represents among the best-reported outcomes to date for untreated older patients with HL,” the investigators concluded.
Seattle Genetics supported the investigator-initiated trial.
Older patients with untreated Hodgkin lymphoma (HL) can achieve significantly improved survival by adding brentuximab vedotin to their treatment before and after standard chemotherapy, a recent study found.
In patients with low comorbidity scores, responses were even more robust, reported lead author Andrew M. Evens, DO, of the Rutgers Cancer Institute of New Jersey, and colleagues.
“Causes of poor outcomes for older patients with HL are not fully understood but have been attributed to a combination of factors, including presence of comorbidities, poorer performance status, disease and biological differences, inability to tolerate chemotherapy at the full dose, and increased treatment-related toxicities,” the authors wrote in the Journal of Clinical Oncology.
The primary goal of the study was to improve outcomes for untreated, older patients, a group that’s historically been a difficult-to-treat patient population.
The phase 2 trial included 48 HL patients with a median age of 69 (range, 60 – 88).
All patients underwent geriatric assessment for comorbidities and loss of activities of daily living.
Treatment consisted of two doses of brentuximab followed by six cycles of doxorubicin, vinblastine, and dacarbazine (AVD), then four more doses of brentuximab (consolidation doses).
The primary endpoint was complete remission at completion of AVD.
Secondary outcomes included overall response rate, 2-year progression-free survival, 2-year overall survival, and safety.
Just over half the patients (52%) completed all cycles of therapy, and almost three quarters (73%) received at least one consolidation dose of brentuximab.
Among the first 23 evaluable patients, both the complete remission rate and overall response rate were 96%. Intention-to-treat survival rates for all 48 patients were 84% for 2-year progression-free survival and 93% for 2-year overall survival.
Historical 2-year progression-free survival rates in similar older patients is poor, at 50%, so the progression-free survival rate of 84% in this study represents a significant improvement.
Of note, patients with fewer comorbidities and without loss of instrumental activities of daily living showed more robust responses.
Patients with Cumulative Illness Rating Scale for Geriatrics (CIRS-G) comorbidity scores of less than 10 had a 2-year progression-free survival rate of 100% versus 45% for those with higher scores.
Similarly, patients without loss of instrumental activities achieved a progression-free survival rate of 94% versus 25% for those who had lost some instrumental activities.
Grade 3 or 4 adverse events occurred in 42% of patients, with neutropenia being the most common (44%).
“This study represents among the best-reported outcomes to date for untreated older patients with HL,” the investigators concluded.
Seattle Genetics supported the investigator-initiated trial.
Older patients with untreated Hodgkin lymphoma (HL) can achieve significantly improved survival by adding brentuximab vedotin to their treatment before and after standard chemotherapy, a recent study found.
In patients with low comorbidity scores, responses were even more robust, reported lead author Andrew M. Evens, DO, of the Rutgers Cancer Institute of New Jersey, and colleagues.
“Causes of poor outcomes for older patients with HL are not fully understood but have been attributed to a combination of factors, including presence of comorbidities, poorer performance status, disease and biological differences, inability to tolerate chemotherapy at the full dose, and increased treatment-related toxicities,” the authors wrote in the Journal of Clinical Oncology.
The primary goal of the study was to improve outcomes for untreated, older patients, a group that’s historically been a difficult-to-treat patient population.
The phase 2 trial included 48 HL patients with a median age of 69 (range, 60 – 88).
All patients underwent geriatric assessment for comorbidities and loss of activities of daily living.
Treatment consisted of two doses of brentuximab followed by six cycles of doxorubicin, vinblastine, and dacarbazine (AVD), then four more doses of brentuximab (consolidation doses).
The primary endpoint was complete remission at completion of AVD.
Secondary outcomes included overall response rate, 2-year progression-free survival, 2-year overall survival, and safety.
Just over half the patients (52%) completed all cycles of therapy, and almost three quarters (73%) received at least one consolidation dose of brentuximab.
Among the first 23 evaluable patients, both the complete remission rate and overall response rate were 96%. Intention-to-treat survival rates for all 48 patients were 84% for 2-year progression-free survival and 93% for 2-year overall survival.
Historical 2-year progression-free survival rates in similar older patients is poor, at 50%, so the progression-free survival rate of 84% in this study represents a significant improvement.
Of note, patients with fewer comorbidities and without loss of instrumental activities of daily living showed more robust responses.
Patients with Cumulative Illness Rating Scale for Geriatrics (CIRS-G) comorbidity scores of less than 10 had a 2-year progression-free survival rate of 100% versus 45% for those with higher scores.
Similarly, patients without loss of instrumental activities achieved a progression-free survival rate of 94% versus 25% for those who had lost some instrumental activities.
Grade 3 or 4 adverse events occurred in 42% of patients, with neutropenia being the most common (44%).
“This study represents among the best-reported outcomes to date for untreated older patients with HL,” the investigators concluded.
Seattle Genetics supported the investigator-initiated trial.
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
FDA authorizes ClonoSEQ to detect MRD in ALL, myeloma
, the U.S. Food and Drug Administration announced. Marketing authorization of the ClonoSEQ assay was granted to Adaptive Biotechnologies.
The ClonoSEQ assay is an in vitro diagnostic test that uses multiplex polymerase chain reaction and next-generation sequencing to identify and quantify certain gene sequences in DNA extracted from the bone marrow from patients with ALL or multiple myeloma. This is a single-site assay collected by the patient’s provider and sent to Adaptive Biotechnologies for evaluation.
The ClonoSEQ assay is capable of detecting minimal residual disease at levels below 1 in 1 million cells. Currently, providers test for MRD using flow cytometry assays or polymerase chain reaction–based assays. Those methods are usually capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
“Determining whether a patient has residual cancer cells remaining after treatment provides information on how well a patient has responded to therapy and how long remission may last. Having a highly sensitive test available to measure minimal residual disease in ALL or multiple myeloma patients can help providers manage their patients’ care,” FDA Commissioner Scott Gottlieb, MD, said in a press release.
Along with this authorization, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the accuracy, reliability, and effectiveness of tests intended to be used as an aid to measure MRD to assess the change in burden of disease during and after treatment. These special controls, when met along with general controls, provide a reasonable assurance of safety and effectiveness for these tests, the agency said in the release. This action also creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through the FDA’s 510(k) process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a previously approved device.
“The FDA is applying novel regulatory approaches to make sure that these rapidly evolving [next-generation sequencing] tests are accurate and reliable. At the same time, we’re seeing more and more laboratory-developed tests seek marketing authorization from the FDA,” he said, adding that the agency has put forward a plan to modernize the regulatory framework for all in vitro clinical tests.
The FDA evaluated data to demonstrate clinical validity from a retrospective analysis of samples obtained from three previously conducted clinical studies including 273 patients with ALL, an ongoing study of 323 patients with multiple myeloma, and a study of 706 patients with multiple myeloma, according to the FDA release.
For patients with ALL, the ClonoSEQ assay was used to assess MRD at various disease burden thresholds to show that the MRD level correlated with event-free survival – the length of time, after treatment, that the patient remains free of certain complications or events. Patients whose ClonoSEQ assay result was MRD negative had longer event-free survival, while patients with higher MRD assay results had lower event-free survival. Similar patterns of results were seen for progression-free and disease-free survival in patients with multiple myeloma.
, the U.S. Food and Drug Administration announced. Marketing authorization of the ClonoSEQ assay was granted to Adaptive Biotechnologies.
The ClonoSEQ assay is an in vitro diagnostic test that uses multiplex polymerase chain reaction and next-generation sequencing to identify and quantify certain gene sequences in DNA extracted from the bone marrow from patients with ALL or multiple myeloma. This is a single-site assay collected by the patient’s provider and sent to Adaptive Biotechnologies for evaluation.
The ClonoSEQ assay is capable of detecting minimal residual disease at levels below 1 in 1 million cells. Currently, providers test for MRD using flow cytometry assays or polymerase chain reaction–based assays. Those methods are usually capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
“Determining whether a patient has residual cancer cells remaining after treatment provides information on how well a patient has responded to therapy and how long remission may last. Having a highly sensitive test available to measure minimal residual disease in ALL or multiple myeloma patients can help providers manage their patients’ care,” FDA Commissioner Scott Gottlieb, MD, said in a press release.
Along with this authorization, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the accuracy, reliability, and effectiveness of tests intended to be used as an aid to measure MRD to assess the change in burden of disease during and after treatment. These special controls, when met along with general controls, provide a reasonable assurance of safety and effectiveness for these tests, the agency said in the release. This action also creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through the FDA’s 510(k) process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a previously approved device.
“The FDA is applying novel regulatory approaches to make sure that these rapidly evolving [next-generation sequencing] tests are accurate and reliable. At the same time, we’re seeing more and more laboratory-developed tests seek marketing authorization from the FDA,” he said, adding that the agency has put forward a plan to modernize the regulatory framework for all in vitro clinical tests.
The FDA evaluated data to demonstrate clinical validity from a retrospective analysis of samples obtained from three previously conducted clinical studies including 273 patients with ALL, an ongoing study of 323 patients with multiple myeloma, and a study of 706 patients with multiple myeloma, according to the FDA release.
For patients with ALL, the ClonoSEQ assay was used to assess MRD at various disease burden thresholds to show that the MRD level correlated with event-free survival – the length of time, after treatment, that the patient remains free of certain complications or events. Patients whose ClonoSEQ assay result was MRD negative had longer event-free survival, while patients with higher MRD assay results had lower event-free survival. Similar patterns of results were seen for progression-free and disease-free survival in patients with multiple myeloma.
, the U.S. Food and Drug Administration announced. Marketing authorization of the ClonoSEQ assay was granted to Adaptive Biotechnologies.
The ClonoSEQ assay is an in vitro diagnostic test that uses multiplex polymerase chain reaction and next-generation sequencing to identify and quantify certain gene sequences in DNA extracted from the bone marrow from patients with ALL or multiple myeloma. This is a single-site assay collected by the patient’s provider and sent to Adaptive Biotechnologies for evaluation.
The ClonoSEQ assay is capable of detecting minimal residual disease at levels below 1 in 1 million cells. Currently, providers test for MRD using flow cytometry assays or polymerase chain reaction–based assays. Those methods are usually capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
“Determining whether a patient has residual cancer cells remaining after treatment provides information on how well a patient has responded to therapy and how long remission may last. Having a highly sensitive test available to measure minimal residual disease in ALL or multiple myeloma patients can help providers manage their patients’ care,” FDA Commissioner Scott Gottlieb, MD, said in a press release.
Along with this authorization, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the accuracy, reliability, and effectiveness of tests intended to be used as an aid to measure MRD to assess the change in burden of disease during and after treatment. These special controls, when met along with general controls, provide a reasonable assurance of safety and effectiveness for these tests, the agency said in the release. This action also creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through the FDA’s 510(k) process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a previously approved device.
“The FDA is applying novel regulatory approaches to make sure that these rapidly evolving [next-generation sequencing] tests are accurate and reliable. At the same time, we’re seeing more and more laboratory-developed tests seek marketing authorization from the FDA,” he said, adding that the agency has put forward a plan to modernize the regulatory framework for all in vitro clinical tests.
The FDA evaluated data to demonstrate clinical validity from a retrospective analysis of samples obtained from three previously conducted clinical studies including 273 patients with ALL, an ongoing study of 323 patients with multiple myeloma, and a study of 706 patients with multiple myeloma, according to the FDA release.
For patients with ALL, the ClonoSEQ assay was used to assess MRD at various disease burden thresholds to show that the MRD level correlated with event-free survival – the length of time, after treatment, that the patient remains free of certain complications or events. Patients whose ClonoSEQ assay result was MRD negative had longer event-free survival, while patients with higher MRD assay results had lower event-free survival. Similar patterns of results were seen for progression-free and disease-free survival in patients with multiple myeloma.
Prognostic factors guide mantle cell treatment decisions
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
REPORTING FROM MHM 2018
CAR T-cell studies dominate ongoing cellular therapy trials
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
EXPERT ANALYSIS FROM THE NCCN HEMATOLOGIC MALIGNANCIES CONGRESS
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration (FDA) has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The FDA had placed the hold in April, and this halted U.S.-based enrollment of new patients in tazemetostat clinical trials.
Now, Epizyme, Inc., the company developing tazemetostat, is in the process of reopening enrollment in all company-sponsored trials in the U.S.
The FDA had placed the partial hold on tazemetostat trials after an adverse event was observed in a pediatric patient on a phase 1 study.
The patient, who had advanced poorly differentiated chordoma, developed secondary T-cell lymphoblastic lymphoma (T-LBL) while taking tazemetostat. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” said Robert Bazemore, president and chief executive officer of Epizyme.
Due to this adverse event and the partial clinical hold, Epizyme began to assess the risk of T-LBL and other secondary malignancies potentially associated with tazemetostat.
The company also assessed the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials.
Epizyme concluded that the benefits of tazemetostat outweigh the risks, and the risk of T-LBL appears confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
Epizyme convened a panel of external scientific and medical experts who reviewed and validated the company’s findings.
“The team at Epizyme has worked diligently in collaboration with external experts and FDA over the past several months, culminating in decisions . . . to lift the partial clinical hold and allow re-opening of enrollment in our clinical trials,” Bazemore said.
He noted that the company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials.
However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies.
Bazemore said the lifting of the partial clinical hold allows Epizyme to turn its full attention to key priorities, including plans to submit a new drug application for tazemetostat in epithelioid sarcoma.
The company also plans to begin preparing for a potential new drug application for tazemetostat in follicular lymphoma.
Tazemetostat is currently under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid tumor malignancies. The drug is also being studied as part of combination therapy for non-small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Now that Epizyme has resolved the U.S. hold on tazemetostat trials, the company is working to resolve partial clinical holds placed in France and Germany to resume trial enrollment in those countries.
The U.S. Food and Drug Administration (FDA) has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The FDA had placed the hold in April, and this halted U.S.-based enrollment of new patients in tazemetostat clinical trials.
Now, Epizyme, Inc., the company developing tazemetostat, is in the process of reopening enrollment in all company-sponsored trials in the U.S.
The FDA had placed the partial hold on tazemetostat trials after an adverse event was observed in a pediatric patient on a phase 1 study.
The patient, who had advanced poorly differentiated chordoma, developed secondary T-cell lymphoblastic lymphoma (T-LBL) while taking tazemetostat. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” said Robert Bazemore, president and chief executive officer of Epizyme.
Due to this adverse event and the partial clinical hold, Epizyme began to assess the risk of T-LBL and other secondary malignancies potentially associated with tazemetostat.
The company also assessed the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials.
Epizyme concluded that the benefits of tazemetostat outweigh the risks, and the risk of T-LBL appears confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
Epizyme convened a panel of external scientific and medical experts who reviewed and validated the company’s findings.
“The team at Epizyme has worked diligently in collaboration with external experts and FDA over the past several months, culminating in decisions . . . to lift the partial clinical hold and allow re-opening of enrollment in our clinical trials,” Bazemore said.
He noted that the company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials.
However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies.
Bazemore said the lifting of the partial clinical hold allows Epizyme to turn its full attention to key priorities, including plans to submit a new drug application for tazemetostat in epithelioid sarcoma.
The company also plans to begin preparing for a potential new drug application for tazemetostat in follicular lymphoma.
Tazemetostat is currently under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid tumor malignancies. The drug is also being studied as part of combination therapy for non-small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Now that Epizyme has resolved the U.S. hold on tazemetostat trials, the company is working to resolve partial clinical holds placed in France and Germany to resume trial enrollment in those countries.
The U.S. Food and Drug Administration (FDA) has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The FDA had placed the hold in April, and this halted U.S.-based enrollment of new patients in tazemetostat clinical trials.
Now, Epizyme, Inc., the company developing tazemetostat, is in the process of reopening enrollment in all company-sponsored trials in the U.S.
The FDA had placed the partial hold on tazemetostat trials after an adverse event was observed in a pediatric patient on a phase 1 study.
The patient, who had advanced poorly differentiated chordoma, developed secondary T-cell lymphoblastic lymphoma (T-LBL) while taking tazemetostat. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” said Robert Bazemore, president and chief executive officer of Epizyme.
Due to this adverse event and the partial clinical hold, Epizyme began to assess the risk of T-LBL and other secondary malignancies potentially associated with tazemetostat.
The company also assessed the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials.
Epizyme concluded that the benefits of tazemetostat outweigh the risks, and the risk of T-LBL appears confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
Epizyme convened a panel of external scientific and medical experts who reviewed and validated the company’s findings.
“The team at Epizyme has worked diligently in collaboration with external experts and FDA over the past several months, culminating in decisions . . . to lift the partial clinical hold and allow re-opening of enrollment in our clinical trials,” Bazemore said.
He noted that the company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials.
However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies.
Bazemore said the lifting of the partial clinical hold allows Epizyme to turn its full attention to key priorities, including plans to submit a new drug application for tazemetostat in epithelioid sarcoma.
The company also plans to begin preparing for a potential new drug application for tazemetostat in follicular lymphoma.
Tazemetostat is currently under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid tumor malignancies. The drug is also being studied as part of combination therapy for non-small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Now that Epizyme has resolved the U.S. hold on tazemetostat trials, the company is working to resolve partial clinical holds placed in France and Germany to resume trial enrollment in those countries.
Real-world clues for optimal sequencing of CLL novel agents
NEW YORK – Although optimal sequencing strategies in chronic lymphocytic leukemia are still unclear, real-world data suggest an alternate kinase inhibitor or venetoclax is the best approach for a patient who has received ibrutinib or idelalisib, according to John N. Allan, MD, of Cornell University, New York.
“I think for the most part, there’s enough evidence,” Dr. Allan said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“If you had one to two lines of therapy, it still favors the novel agents rather than the chemotherapy arms in all these studies,” said Dr. Allan, referring to some of the pivotal trials supporting approval of novel agents in chronic lymphocytic leukemia (CLL). “The earlier we get to these drugs, I believe, the better.”
While venetoclax after ibrutinib is supported by multiple studies, “vice versa is unknown, but there’s seemingly no reason to think it wouldn’t work – different mechanisms of actions, different pathways,” Dr. Allan said.
What is clear, he added, is that retreating those patients with chemoimmunotherapy is not optimal.
In support of that, he cited a multicenter retrospective analysis, which is believed to be the largest real-world experience to date of novel agents in CLL looking at post–kinase inhibitor salvage strategies (Ann Oncol. 2017 May 1;28[5]:1050-6).
Using an alternate kinase inhibitor or venetoclax resulted in superior progression-free survival versus chemoimmunotherapy at the time of initial kinase inhibitor failure in that study, which looked at treatment strategies and outcomes for 683 patients.
Ibrutinib appeared to be superior to idelalisib as a first kinase inhibitor, with significantly better progression-free survival in both frontline and relapsed/refractory settings, and in both complex karyotype and del17p patients, according to the report. Additionally, the response rate to venetoclax seemed superior to that of idelalisib in patients who discontinued ibrutinib because of progression or toxicity.
All of that supports the need for trials to test various sequencing strategies and establish clear treatment algorithms, according to Dr. Allan. “Optimal sequencing is unknown, but real-world data gives us some idea.”
For relapsed/refractory patients, ibrutinib, idelalisib, and venetoclax all have lengthened responses, improved survival, and are approved by the Food and Drug Administration, he added, noting that the toxicity profiles vary and must be understood when dosing and prescribing these agents.
More novel treatments are on the way. On Sept. 24, just days after Dr. Allan’s NCCN presentation, the FDA granted approval to duvelisib for adults with relapsed or refractory CLL or small lymphocytic lymphoma following two or more previous lines of therapy.
Dr. Allan reported financial disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis Pharmaceuticals, and Verastem Oncology.
NEW YORK – Although optimal sequencing strategies in chronic lymphocytic leukemia are still unclear, real-world data suggest an alternate kinase inhibitor or venetoclax is the best approach for a patient who has received ibrutinib or idelalisib, according to John N. Allan, MD, of Cornell University, New York.
“I think for the most part, there’s enough evidence,” Dr. Allan said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“If you had one to two lines of therapy, it still favors the novel agents rather than the chemotherapy arms in all these studies,” said Dr. Allan, referring to some of the pivotal trials supporting approval of novel agents in chronic lymphocytic leukemia (CLL). “The earlier we get to these drugs, I believe, the better.”
While venetoclax after ibrutinib is supported by multiple studies, “vice versa is unknown, but there’s seemingly no reason to think it wouldn’t work – different mechanisms of actions, different pathways,” Dr. Allan said.
What is clear, he added, is that retreating those patients with chemoimmunotherapy is not optimal.
In support of that, he cited a multicenter retrospective analysis, which is believed to be the largest real-world experience to date of novel agents in CLL looking at post–kinase inhibitor salvage strategies (Ann Oncol. 2017 May 1;28[5]:1050-6).
Using an alternate kinase inhibitor or venetoclax resulted in superior progression-free survival versus chemoimmunotherapy at the time of initial kinase inhibitor failure in that study, which looked at treatment strategies and outcomes for 683 patients.
Ibrutinib appeared to be superior to idelalisib as a first kinase inhibitor, with significantly better progression-free survival in both frontline and relapsed/refractory settings, and in both complex karyotype and del17p patients, according to the report. Additionally, the response rate to venetoclax seemed superior to that of idelalisib in patients who discontinued ibrutinib because of progression or toxicity.
All of that supports the need for trials to test various sequencing strategies and establish clear treatment algorithms, according to Dr. Allan. “Optimal sequencing is unknown, but real-world data gives us some idea.”
For relapsed/refractory patients, ibrutinib, idelalisib, and venetoclax all have lengthened responses, improved survival, and are approved by the Food and Drug Administration, he added, noting that the toxicity profiles vary and must be understood when dosing and prescribing these agents.
More novel treatments are on the way. On Sept. 24, just days after Dr. Allan’s NCCN presentation, the FDA granted approval to duvelisib for adults with relapsed or refractory CLL or small lymphocytic lymphoma following two or more previous lines of therapy.
Dr. Allan reported financial disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis Pharmaceuticals, and Verastem Oncology.
NEW YORK – Although optimal sequencing strategies in chronic lymphocytic leukemia are still unclear, real-world data suggest an alternate kinase inhibitor or venetoclax is the best approach for a patient who has received ibrutinib or idelalisib, according to John N. Allan, MD, of Cornell University, New York.
“I think for the most part, there’s enough evidence,” Dr. Allan said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“If you had one to two lines of therapy, it still favors the novel agents rather than the chemotherapy arms in all these studies,” said Dr. Allan, referring to some of the pivotal trials supporting approval of novel agents in chronic lymphocytic leukemia (CLL). “The earlier we get to these drugs, I believe, the better.”
While venetoclax after ibrutinib is supported by multiple studies, “vice versa is unknown, but there’s seemingly no reason to think it wouldn’t work – different mechanisms of actions, different pathways,” Dr. Allan said.
What is clear, he added, is that retreating those patients with chemoimmunotherapy is not optimal.
In support of that, he cited a multicenter retrospective analysis, which is believed to be the largest real-world experience to date of novel agents in CLL looking at post–kinase inhibitor salvage strategies (Ann Oncol. 2017 May 1;28[5]:1050-6).
Using an alternate kinase inhibitor or venetoclax resulted in superior progression-free survival versus chemoimmunotherapy at the time of initial kinase inhibitor failure in that study, which looked at treatment strategies and outcomes for 683 patients.
Ibrutinib appeared to be superior to idelalisib as a first kinase inhibitor, with significantly better progression-free survival in both frontline and relapsed/refractory settings, and in both complex karyotype and del17p patients, according to the report. Additionally, the response rate to venetoclax seemed superior to that of idelalisib in patients who discontinued ibrutinib because of progression or toxicity.
All of that supports the need for trials to test various sequencing strategies and establish clear treatment algorithms, according to Dr. Allan. “Optimal sequencing is unknown, but real-world data gives us some idea.”
For relapsed/refractory patients, ibrutinib, idelalisib, and venetoclax all have lengthened responses, improved survival, and are approved by the Food and Drug Administration, he added, noting that the toxicity profiles vary and must be understood when dosing and prescribing these agents.
More novel treatments are on the way. On Sept. 24, just days after Dr. Allan’s NCCN presentation, the FDA granted approval to duvelisib for adults with relapsed or refractory CLL or small lymphocytic lymphoma following two or more previous lines of therapy.
Dr. Allan reported financial disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis Pharmaceuticals, and Verastem Oncology.
EXPERT ANALYSIS FROM NCCN HEMATOLOGIC MALIGNANCIES CONGRESS
CAR T may have curative potential in Hodgkin lymphoma
NEW YORK – Although the data set is small and not yet mature, chimeric antigen receptor (CAR) T-cell therapy appears to be a promising approach for Hodgkin lymphoma, according to Philippe Armand, MD, PhD, of Dana-Farber/Brigham and Women’s Cancer Center and the Massachusetts General Hospital Cancer Center in Boston.
While based on a handful of patients, the data do suggest this approach may play a role by targeting CD30 or Epstein Barr virus (EBV), Dr. Armand said at the NCCN Annual Congress: Hematologic Malignancies.
“Most importantly perhaps, like its experience outside of Hodgkin lymphoma, it may really have curative potential, based on the long [complete response] rates that have been already exhibited,” he said.
Much of the published clinical experience to date is with CD30-directed CAR Ts, Dr. Armand said, noting that in Hodgkin lymphoma, results so far show promise for this particular approach.
In a recent phase 1 dose escalation study, nine patients with relapsed/refractory Hodgkin lymphoma or anaplastic large-cell lymphoma (ALCL) received infusions of autologous T cells modified to express CD30-specific CAR T cells encoding the CD28 costimulatory domain, with no conditioning regimen.
Out of seven relapsed Hodgkin lymphoma patients, one had a complete response (CR) lasting beyond 2.5 years following a second infusion. Another patient had a CR persisting almost 2 years, and three patients had transient stable disease. One of the two ALCL patients had a CR lasting 9 months after a fourth infusion.
No toxicities attributable to the therapy were seen, according to the investigators.
The CD30 CAR T cells are being evaluated with a conditioning regimen in the phase 1 RELY-30 trial. Preliminary results presented at the 2018 European Society for Blood and Marrow Transplantation meeting in Lisbon showed better expansion of CAR T cells and responses in three out of five patients, including two CRs, according to Dr. Armand.
A CD30-directed CAR T-cell therapy with a 4-1BB costimulatory domain has also been tested in a small group of Hodgkin patients with a response rate of 35% – including some CRs – with an apparent lower response rate in patients with extranodal involvement. Dr. Armand noted that those findings need to be validated in additional studies.
Among non CD-30 targeted products, a CD19 CAR-T approach has been tried in Hodgkin lymphoma, though preliminary results suggest only transient activity, according to the presenter.
One interesting approach has been the targeting of EBV, he added. Recently reported results showed that two doses of T cells with specificity for EBV-derived tumor antigens induced clinical responses in patients with EBV-positive Hodgkin lymphoma.
The cells were engineered to express dominant-negative TGF-beta receptor type 2, according to the report. “We know that TGF-beta provides a strong immunosuppressant signal in the tumor microenvironment,” Dr. Armand said, noting that some of the responses in the seven evaluable patients lasted 4 years or more.
Dr. Armand reported financial disclosures related to Adaptive Biotechnologies/Sequenta, Affimed, Bristol-Myers Squibb, Merck, and Roche.
NEW YORK – Although the data set is small and not yet mature, chimeric antigen receptor (CAR) T-cell therapy appears to be a promising approach for Hodgkin lymphoma, according to Philippe Armand, MD, PhD, of Dana-Farber/Brigham and Women’s Cancer Center and the Massachusetts General Hospital Cancer Center in Boston.
While based on a handful of patients, the data do suggest this approach may play a role by targeting CD30 or Epstein Barr virus (EBV), Dr. Armand said at the NCCN Annual Congress: Hematologic Malignancies.
“Most importantly perhaps, like its experience outside of Hodgkin lymphoma, it may really have curative potential, based on the long [complete response] rates that have been already exhibited,” he said.
Much of the published clinical experience to date is with CD30-directed CAR Ts, Dr. Armand said, noting that in Hodgkin lymphoma, results so far show promise for this particular approach.
In a recent phase 1 dose escalation study, nine patients with relapsed/refractory Hodgkin lymphoma or anaplastic large-cell lymphoma (ALCL) received infusions of autologous T cells modified to express CD30-specific CAR T cells encoding the CD28 costimulatory domain, with no conditioning regimen.
Out of seven relapsed Hodgkin lymphoma patients, one had a complete response (CR) lasting beyond 2.5 years following a second infusion. Another patient had a CR persisting almost 2 years, and three patients had transient stable disease. One of the two ALCL patients had a CR lasting 9 months after a fourth infusion.
No toxicities attributable to the therapy were seen, according to the investigators.
The CD30 CAR T cells are being evaluated with a conditioning regimen in the phase 1 RELY-30 trial. Preliminary results presented at the 2018 European Society for Blood and Marrow Transplantation meeting in Lisbon showed better expansion of CAR T cells and responses in three out of five patients, including two CRs, according to Dr. Armand.
A CD30-directed CAR T-cell therapy with a 4-1BB costimulatory domain has also been tested in a small group of Hodgkin patients with a response rate of 35% – including some CRs – with an apparent lower response rate in patients with extranodal involvement. Dr. Armand noted that those findings need to be validated in additional studies.
Among non CD-30 targeted products, a CD19 CAR-T approach has been tried in Hodgkin lymphoma, though preliminary results suggest only transient activity, according to the presenter.
One interesting approach has been the targeting of EBV, he added. Recently reported results showed that two doses of T cells with specificity for EBV-derived tumor antigens induced clinical responses in patients with EBV-positive Hodgkin lymphoma.
The cells were engineered to express dominant-negative TGF-beta receptor type 2, according to the report. “We know that TGF-beta provides a strong immunosuppressant signal in the tumor microenvironment,” Dr. Armand said, noting that some of the responses in the seven evaluable patients lasted 4 years or more.
Dr. Armand reported financial disclosures related to Adaptive Biotechnologies/Sequenta, Affimed, Bristol-Myers Squibb, Merck, and Roche.
NEW YORK – Although the data set is small and not yet mature, chimeric antigen receptor (CAR) T-cell therapy appears to be a promising approach for Hodgkin lymphoma, according to Philippe Armand, MD, PhD, of Dana-Farber/Brigham and Women’s Cancer Center and the Massachusetts General Hospital Cancer Center in Boston.
While based on a handful of patients, the data do suggest this approach may play a role by targeting CD30 or Epstein Barr virus (EBV), Dr. Armand said at the NCCN Annual Congress: Hematologic Malignancies.
“Most importantly perhaps, like its experience outside of Hodgkin lymphoma, it may really have curative potential, based on the long [complete response] rates that have been already exhibited,” he said.
Much of the published clinical experience to date is with CD30-directed CAR Ts, Dr. Armand said, noting that in Hodgkin lymphoma, results so far show promise for this particular approach.
In a recent phase 1 dose escalation study, nine patients with relapsed/refractory Hodgkin lymphoma or anaplastic large-cell lymphoma (ALCL) received infusions of autologous T cells modified to express CD30-specific CAR T cells encoding the CD28 costimulatory domain, with no conditioning regimen.
Out of seven relapsed Hodgkin lymphoma patients, one had a complete response (CR) lasting beyond 2.5 years following a second infusion. Another patient had a CR persisting almost 2 years, and three patients had transient stable disease. One of the two ALCL patients had a CR lasting 9 months after a fourth infusion.
No toxicities attributable to the therapy were seen, according to the investigators.
The CD30 CAR T cells are being evaluated with a conditioning regimen in the phase 1 RELY-30 trial. Preliminary results presented at the 2018 European Society for Blood and Marrow Transplantation meeting in Lisbon showed better expansion of CAR T cells and responses in three out of five patients, including two CRs, according to Dr. Armand.
A CD30-directed CAR T-cell therapy with a 4-1BB costimulatory domain has also been tested in a small group of Hodgkin patients with a response rate of 35% – including some CRs – with an apparent lower response rate in patients with extranodal involvement. Dr. Armand noted that those findings need to be validated in additional studies.
Among non CD-30 targeted products, a CD19 CAR-T approach has been tried in Hodgkin lymphoma, though preliminary results suggest only transient activity, according to the presenter.
One interesting approach has been the targeting of EBV, he added. Recently reported results showed that two doses of T cells with specificity for EBV-derived tumor antigens induced clinical responses in patients with EBV-positive Hodgkin lymphoma.
The cells were engineered to express dominant-negative TGF-beta receptor type 2, according to the report. “We know that TGF-beta provides a strong immunosuppressant signal in the tumor microenvironment,” Dr. Armand said, noting that some of the responses in the seven evaluable patients lasted 4 years or more.
Dr. Armand reported financial disclosures related to Adaptive Biotechnologies/Sequenta, Affimed, Bristol-Myers Squibb, Merck, and Roche.
EXPERT ANALYSIS FROM NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES
Outpatient lenalidomide/rituximab yields long-term MCL remission
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
FROM BLOOD
Key clinical point:
Major finding: After 64-months of median follow-up, 21 of 33 patients with initial responses remained in remission.
Study details: Five-year follow-up of a phase 2 single arm trial of lenalidomide/rituximab induction and maintenance in 38 patients with mantle cell lymphoma.
Disclosures: The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
Source: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.