User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
After 2006 Recommendation, More Autism Diagnoses Made at Earlier Age
BALTIMORE – The American Academy of Pediatrics’ 2006 recommendation to screen all children for autism spectrum disorder at age 18 months appears to have resulted in a substantially earlier age of diagnosis among children seen in at least one U.S. center.
Among children diagnosed with autism spectrum disorder (ASD) and referred to the Children’s Evaluation and Rehabilitation Center of Montefiore Medical Center in the Bronx, N.Y., the average age of initial ASD diagnosis fell from 45 months among 295 diagnosed children born in 2003 or 2004 to 31 months among 217 diagnosed children born during or after 2005, Dr. Maria D. Valicenti-McDermott said at the annual meeting of the Pediatric Academic Societies.
Expressed another way, the percentage of children first diagnosed with ASD at age 4 years or older fell from 67% of children born during 2003 and 2004 to 26% of those born during or after 2005, said Dr. Valicenti-McDermott, a developmental pediatrician at Montefiore.
Although the review did not examine the outcomes of those children, she said that earlier age at diagnosis has been proven in previously reported studies to make a “big difference” for prognosis.
“The earlier you start treatment, the better the outcomes,” Dr. Valicenti-McDermott said in an interview. “More and more literature shows that the age of diagnosis of ASD is very important.”
Interventions that seem to make a difference when begun earlier include applied behavioral analysis and intensive speech and language therapy. A recent study by Dr. Valicenti-McDermott and her associates at Montefiore documented that those early interventions reversed the ASD diagnosis in at least some children, although she noted that many of these children continue to have problems, such as academic difficulties. She also acknowledged that some of this “reversal” may result from “instability” of the ASD diagnosis when made at a relatively early age.
The findings she reported came from a review of all children diagnosed with ASD and seen at Montefiore during 2003-2012. The analysis also showed that the earlier age of diagnosis after 2006 occurred across racial and ethnic groups, with similar reductions seen among Hispanic, African American, and white children.
In a multivariate analysis, the odds ratio for a first diagnosis of ASD at age 4 years or older was fourfold greater among children born during 2003 or 2004, compared with those born during 2005 or after.
Dr. Valicenti-McDermott conceded it was impossible to fully credit the 2006 screening recommendation from the American Academy of Pediatrics for that shift, based on her observational study. Another possible factor was increased awareness among parents about ASD over the time frame studied. In addition, community physicians also may have helped drive earlier diagnosis.
BALTIMORE – The American Academy of Pediatrics’ 2006 recommendation to screen all children for autism spectrum disorder at age 18 months appears to have resulted in a substantially earlier age of diagnosis among children seen in at least one U.S. center.
Among children diagnosed with autism spectrum disorder (ASD) and referred to the Children’s Evaluation and Rehabilitation Center of Montefiore Medical Center in the Bronx, N.Y., the average age of initial ASD diagnosis fell from 45 months among 295 diagnosed children born in 2003 or 2004 to 31 months among 217 diagnosed children born during or after 2005, Dr. Maria D. Valicenti-McDermott said at the annual meeting of the Pediatric Academic Societies.
Expressed another way, the percentage of children first diagnosed with ASD at age 4 years or older fell from 67% of children born during 2003 and 2004 to 26% of those born during or after 2005, said Dr. Valicenti-McDermott, a developmental pediatrician at Montefiore.
Although the review did not examine the outcomes of those children, she said that earlier age at diagnosis has been proven in previously reported studies to make a “big difference” for prognosis.
“The earlier you start treatment, the better the outcomes,” Dr. Valicenti-McDermott said in an interview. “More and more literature shows that the age of diagnosis of ASD is very important.”
Interventions that seem to make a difference when begun earlier include applied behavioral analysis and intensive speech and language therapy. A recent study by Dr. Valicenti-McDermott and her associates at Montefiore documented that those early interventions reversed the ASD diagnosis in at least some children, although she noted that many of these children continue to have problems, such as academic difficulties. She also acknowledged that some of this “reversal” may result from “instability” of the ASD diagnosis when made at a relatively early age.
The findings she reported came from a review of all children diagnosed with ASD and seen at Montefiore during 2003-2012. The analysis also showed that the earlier age of diagnosis after 2006 occurred across racial and ethnic groups, with similar reductions seen among Hispanic, African American, and white children.
In a multivariate analysis, the odds ratio for a first diagnosis of ASD at age 4 years or older was fourfold greater among children born during 2003 or 2004, compared with those born during 2005 or after.
Dr. Valicenti-McDermott conceded it was impossible to fully credit the 2006 screening recommendation from the American Academy of Pediatrics for that shift, based on her observational study. Another possible factor was increased awareness among parents about ASD over the time frame studied. In addition, community physicians also may have helped drive earlier diagnosis.
BALTIMORE – The American Academy of Pediatrics’ 2006 recommendation to screen all children for autism spectrum disorder at age 18 months appears to have resulted in a substantially earlier age of diagnosis among children seen in at least one U.S. center.
Among children diagnosed with autism spectrum disorder (ASD) and referred to the Children’s Evaluation and Rehabilitation Center of Montefiore Medical Center in the Bronx, N.Y., the average age of initial ASD diagnosis fell from 45 months among 295 diagnosed children born in 2003 or 2004 to 31 months among 217 diagnosed children born during or after 2005, Dr. Maria D. Valicenti-McDermott said at the annual meeting of the Pediatric Academic Societies.
Expressed another way, the percentage of children first diagnosed with ASD at age 4 years or older fell from 67% of children born during 2003 and 2004 to 26% of those born during or after 2005, said Dr. Valicenti-McDermott, a developmental pediatrician at Montefiore.
Although the review did not examine the outcomes of those children, she said that earlier age at diagnosis has been proven in previously reported studies to make a “big difference” for prognosis.
“The earlier you start treatment, the better the outcomes,” Dr. Valicenti-McDermott said in an interview. “More and more literature shows that the age of diagnosis of ASD is very important.”
Interventions that seem to make a difference when begun earlier include applied behavioral analysis and intensive speech and language therapy. A recent study by Dr. Valicenti-McDermott and her associates at Montefiore documented that those early interventions reversed the ASD diagnosis in at least some children, although she noted that many of these children continue to have problems, such as academic difficulties. She also acknowledged that some of this “reversal” may result from “instability” of the ASD diagnosis when made at a relatively early age.
The findings she reported came from a review of all children diagnosed with ASD and seen at Montefiore during 2003-2012. The analysis also showed that the earlier age of diagnosis after 2006 occurred across racial and ethnic groups, with similar reductions seen among Hispanic, African American, and white children.
In a multivariate analysis, the odds ratio for a first diagnosis of ASD at age 4 years or older was fourfold greater among children born during 2003 or 2004, compared with those born during 2005 or after.
Dr. Valicenti-McDermott conceded it was impossible to fully credit the 2006 screening recommendation from the American Academy of Pediatrics for that shift, based on her observational study. Another possible factor was increased awareness among parents about ASD over the time frame studied. In addition, community physicians also may have helped drive earlier diagnosis.
AT THE PAS ANNUAL MEETING
After 2006 recommendation, more autism diagnoses made at earlier age
BALTIMORE – The American Academy of Pediatrics’ 2006 recommendation to screen all children for autism spectrum disorder at age 18 months appears to have resulted in a substantially earlier age of diagnosis among children seen in at least one U.S. center.
Among children diagnosed with autism spectrum disorder (ASD) and referred to the Children’s Evaluation and Rehabilitation Center of Montefiore Medical Center in the Bronx, N.Y., the average age of initial ASD diagnosis fell from 45 months among 295 diagnosed children born in 2003 or 2004 to 31 months among 217 diagnosed children born during or after 2005, Dr. Maria D. Valicenti-McDermott said at the annual meeting of the Pediatric Academic Societies.
Expressed another way, the percentage of children first diagnosed with ASD at age 4 years or older fell from 67% of children born during 2003 and 2004 to 26% of those born during or after 2005, said Dr. Valicenti-McDermott, a developmental pediatrician at Montefiore.
Although the review did not examine the outcomes of those children, she said that earlier age at diagnosis has been proven in previously reported studies to make a “big difference” for prognosis.
“The earlier you start treatment, the better the outcomes,” Dr. Valicenti-McDermott said in an interview. “More and more literature shows that the age of diagnosis of ASD is very important.”
Interventions that seem to make a difference when begun earlier include applied behavioral analysis and intensive speech and language therapy. A recent study by Dr. Valicenti-McDermott and her associates at Montefiore documented that those early interventions reversed the ASD diagnosis in at least some children, although she noted that many of these children continue to have problems, such as academic difficulties. She also acknowledged that some of this “reversal” may result from “instability” of the ASD diagnosis when made at a relatively early age.
The findings she reported came from a review of all children diagnosed with ASD and seen at Montefiore during 2003-2012. The analysis also showed that the earlier age of diagnosis after 2006 occurred across racial and ethnic groups, with similar reductions seen among Hispanic, African American, and white children.
In a multivariate analysis, the odds ratio for a first diagnosis of ASD at age 4 years or older was fourfold greater among children born during 2003 or 2004, compared with those born during 2005 or after.
Dr. Valicenti-McDermott conceded it was impossible to fully credit the 2006 screening recommendation from the American Academy of Pediatrics for that shift, based on her observational study. Another possible factor was increased awareness among parents about ASD over the time frame studied. In addition, community physicians also may have helped drive earlier diagnosis.
On Twitter @mitchelzoler
BALTIMORE – The American Academy of Pediatrics’ 2006 recommendation to screen all children for autism spectrum disorder at age 18 months appears to have resulted in a substantially earlier age of diagnosis among children seen in at least one U.S. center.
Among children diagnosed with autism spectrum disorder (ASD) and referred to the Children’s Evaluation and Rehabilitation Center of Montefiore Medical Center in the Bronx, N.Y., the average age of initial ASD diagnosis fell from 45 months among 295 diagnosed children born in 2003 or 2004 to 31 months among 217 diagnosed children born during or after 2005, Dr. Maria D. Valicenti-McDermott said at the annual meeting of the Pediatric Academic Societies.
Expressed another way, the percentage of children first diagnosed with ASD at age 4 years or older fell from 67% of children born during 2003 and 2004 to 26% of those born during or after 2005, said Dr. Valicenti-McDermott, a developmental pediatrician at Montefiore.
Although the review did not examine the outcomes of those children, she said that earlier age at diagnosis has been proven in previously reported studies to make a “big difference” for prognosis.
“The earlier you start treatment, the better the outcomes,” Dr. Valicenti-McDermott said in an interview. “More and more literature shows that the age of diagnosis of ASD is very important.”
Interventions that seem to make a difference when begun earlier include applied behavioral analysis and intensive speech and language therapy. A recent study by Dr. Valicenti-McDermott and her associates at Montefiore documented that those early interventions reversed the ASD diagnosis in at least some children, although she noted that many of these children continue to have problems, such as academic difficulties. She also acknowledged that some of this “reversal” may result from “instability” of the ASD diagnosis when made at a relatively early age.
The findings she reported came from a review of all children diagnosed with ASD and seen at Montefiore during 2003-2012. The analysis also showed that the earlier age of diagnosis after 2006 occurred across racial and ethnic groups, with similar reductions seen among Hispanic, African American, and white children.
In a multivariate analysis, the odds ratio for a first diagnosis of ASD at age 4 years or older was fourfold greater among children born during 2003 or 2004, compared with those born during 2005 or after.
Dr. Valicenti-McDermott conceded it was impossible to fully credit the 2006 screening recommendation from the American Academy of Pediatrics for that shift, based on her observational study. Another possible factor was increased awareness among parents about ASD over the time frame studied. In addition, community physicians also may have helped drive earlier diagnosis.
On Twitter @mitchelzoler
BALTIMORE – The American Academy of Pediatrics’ 2006 recommendation to screen all children for autism spectrum disorder at age 18 months appears to have resulted in a substantially earlier age of diagnosis among children seen in at least one U.S. center.
Among children diagnosed with autism spectrum disorder (ASD) and referred to the Children’s Evaluation and Rehabilitation Center of Montefiore Medical Center in the Bronx, N.Y., the average age of initial ASD diagnosis fell from 45 months among 295 diagnosed children born in 2003 or 2004 to 31 months among 217 diagnosed children born during or after 2005, Dr. Maria D. Valicenti-McDermott said at the annual meeting of the Pediatric Academic Societies.
Expressed another way, the percentage of children first diagnosed with ASD at age 4 years or older fell from 67% of children born during 2003 and 2004 to 26% of those born during or after 2005, said Dr. Valicenti-McDermott, a developmental pediatrician at Montefiore.
Although the review did not examine the outcomes of those children, she said that earlier age at diagnosis has been proven in previously reported studies to make a “big difference” for prognosis.
“The earlier you start treatment, the better the outcomes,” Dr. Valicenti-McDermott said in an interview. “More and more literature shows that the age of diagnosis of ASD is very important.”
Interventions that seem to make a difference when begun earlier include applied behavioral analysis and intensive speech and language therapy. A recent study by Dr. Valicenti-McDermott and her associates at Montefiore documented that those early interventions reversed the ASD diagnosis in at least some children, although she noted that many of these children continue to have problems, such as academic difficulties. She also acknowledged that some of this “reversal” may result from “instability” of the ASD diagnosis when made at a relatively early age.
The findings she reported came from a review of all children diagnosed with ASD and seen at Montefiore during 2003-2012. The analysis also showed that the earlier age of diagnosis after 2006 occurred across racial and ethnic groups, with similar reductions seen among Hispanic, African American, and white children.
In a multivariate analysis, the odds ratio for a first diagnosis of ASD at age 4 years or older was fourfold greater among children born during 2003 or 2004, compared with those born during 2005 or after.
Dr. Valicenti-McDermott conceded it was impossible to fully credit the 2006 screening recommendation from the American Academy of Pediatrics for that shift, based on her observational study. Another possible factor was increased awareness among parents about ASD over the time frame studied. In addition, community physicians also may have helped drive earlier diagnosis.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Diagnosis of autism spectrum disorder occurred significantly earlier for children born in 2005 or later, compared with children born in prior years, suggesting an impact from the 2006 U.S. recommendation for universal screening at age 18 months.
Major finding: Age at autism diagnosis fell from 45 months in children born in 2003 or 2004 to 31 months in those born later.
Data source: Review of 512 children diagnosed with autism spectrum disorder at one U.S. center during 2003-2012.
Disclosures: Dr. Valicenti-McDermott had no disclosures.
Family’s Psychosocial Problems Complicate Pediatric Obesity
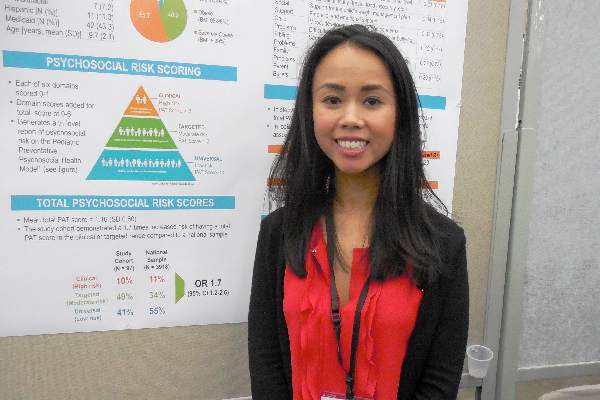
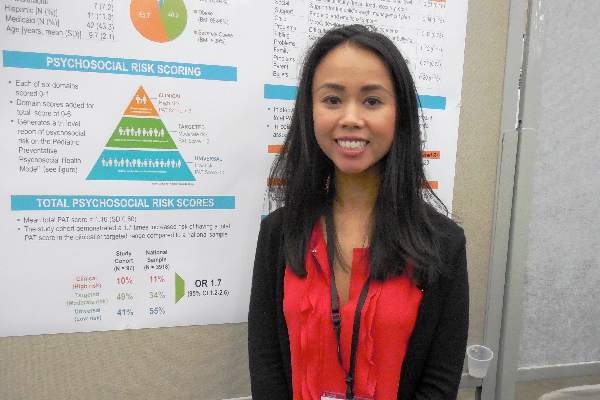
BALTIMORE – Childhood obesity can result from more than just poor diet, not enough exercise, and too much screen time; it also often occurs in families with parents who have a significantly increased prevalence of psychosocial problems, judging from findings from a pilot, single-center study involving 97 parents who brought their child to a tertiary-care pediatric obesity center.
This preliminary finding “supports the need for universal psychosocial screening in this population, with particular attention to families whose children have comorbid behavioral health problems,” Dr. Thao-Ly T. Phan said while presenting a poster at the annual meeting of the Pediatric Academic Societies.
“You might think that when a child is brought to an obesity clinic, you just need to ask what foods the child eats, how often the child exercises and how much television they watch, but we also need to ask about problems in the families and address those problems,” said Dr. Phan, a pediatrician and weight management specialist at the Alfred I. duPont Hospital for Children in Wilmington, Del.
Dr. Phan said although a key next step in this research is to assess how interventions aimed at family psychosocial problems affect a child’s obesity and well-being, her experience so far suggests that the psychosocial setting where a child lives can play a significant role in the etiology and maintenance of obesity.
“We find that families at higher psychosocial risk don’t come back for treatment, and when that happens the children don’t do well. That’s a reason to screen [for such problems] and intervene with psychological and social work support,” she said in an interview.
“A lot of our messages to families focus on things like screen time and eating more fruits and vegetables, but if the family can’t implement that, then we’re missing the boat,” Dr. Phan said.
She and her associates used the Psychosocial Assessment Tool (PAT), a screening tool for parents that takes about 5-10 minutes to complete and that was developed by researchers at the Children’s Hospital of Philadelphia (ACTA Oncologica. 2015 May;54[5]:574-80). The PAT poses a series of questions that deal with a spectrum of potential psychosocial issues including financial status, a child’s problems at school, parents’ mood and substance abuse, and parental views of weight and health issues.
The investigators administered the PAT to 97 parents of children aged 4-12 years old who had their first visit to the tertiary-care pediatric obesity clinic at Alfred I. duPont. The children had body mass index levels that averaged close to the 99th percentile, with 56% of the children classified as severely obese with a BMI at or above the 99th percentile, 40% classified as obese with a BMI in the 95th-98th percentile, and 4% classified as overweight with a BMI at the 85th-94th percentile.
The PAT scores in these 97 parents identified 41% with a low risk for having psychosocial problems, 49% with a moderate risk, and 10% with a higher risk. In contrast, a historical control group of 3,918 representative U.S. parents who took the PAT showed 55% at low risk, 34% at moderate risk, and 11% at high risk, which meant that the parents of the children at the clinic had a statistically significant 70% increased prevalence of being in a high- or moderate-risk group for psychosocial problems, compared with parents in the general U.S. population, Dr. Phan reported.
A stepwise linear regression analysis of the PAT results identified two factors that significantly linked with higher PAT scores in these parents: attention- deficit/hyperactivity disorder in the child, and mood disorder in a parent. Logistic regression analysis further narrowed this down to just the child’s attention-deficit/hyperactivity disorder as the only significant correlate with higher PAT scores. The analysis showed that the severity of obesity had no significant correlation with psychosocial risk scores.
The next steps are to assess more parents of obese children this way, see whether the questions posed in the PAT can be better focused for this setting to make the screening simpler and easier to administer, and determine how interventions aimed at the identified risks improve child outcomes, Dr. Phan said.
Another goal of this research is to raise the profile of family psychosocial problems as an important factor in the development and maintenance of obesity in children, she said. “I think that people who work at pediatric weight management clinics have recognized the role of family psychosocial problems, but it is less recognized by the general pediatric community.”
Dr. Phan had no relevant financial disclosures.
BALTIMORE – Childhood obesity can result from more than just poor diet, not enough exercise, and too much screen time; it also often occurs in families with parents who have a significantly increased prevalence of psychosocial problems, judging from findings from a pilot, single-center study involving 97 parents who brought their child to a tertiary-care pediatric obesity center.
This preliminary finding “supports the need for universal psychosocial screening in this population, with particular attention to families whose children have comorbid behavioral health problems,” Dr. Thao-Ly T. Phan said while presenting a poster at the annual meeting of the Pediatric Academic Societies.
“You might think that when a child is brought to an obesity clinic, you just need to ask what foods the child eats, how often the child exercises and how much television they watch, but we also need to ask about problems in the families and address those problems,” said Dr. Phan, a pediatrician and weight management specialist at the Alfred I. duPont Hospital for Children in Wilmington, Del.
Dr. Phan said although a key next step in this research is to assess how interventions aimed at family psychosocial problems affect a child’s obesity and well-being, her experience so far suggests that the psychosocial setting where a child lives can play a significant role in the etiology and maintenance of obesity.
“We find that families at higher psychosocial risk don’t come back for treatment, and when that happens the children don’t do well. That’s a reason to screen [for such problems] and intervene with psychological and social work support,” she said in an interview.
“A lot of our messages to families focus on things like screen time and eating more fruits and vegetables, but if the family can’t implement that, then we’re missing the boat,” Dr. Phan said.
She and her associates used the Psychosocial Assessment Tool (PAT), a screening tool for parents that takes about 5-10 minutes to complete and that was developed by researchers at the Children’s Hospital of Philadelphia (ACTA Oncologica. 2015 May;54[5]:574-80). The PAT poses a series of questions that deal with a spectrum of potential psychosocial issues including financial status, a child’s problems at school, parents’ mood and substance abuse, and parental views of weight and health issues.
The investigators administered the PAT to 97 parents of children aged 4-12 years old who had their first visit to the tertiary-care pediatric obesity clinic at Alfred I. duPont. The children had body mass index levels that averaged close to the 99th percentile, with 56% of the children classified as severely obese with a BMI at or above the 99th percentile, 40% classified as obese with a BMI in the 95th-98th percentile, and 4% classified as overweight with a BMI at the 85th-94th percentile.
The PAT scores in these 97 parents identified 41% with a low risk for having psychosocial problems, 49% with a moderate risk, and 10% with a higher risk. In contrast, a historical control group of 3,918 representative U.S. parents who took the PAT showed 55% at low risk, 34% at moderate risk, and 11% at high risk, which meant that the parents of the children at the clinic had a statistically significant 70% increased prevalence of being in a high- or moderate-risk group for psychosocial problems, compared with parents in the general U.S. population, Dr. Phan reported.
A stepwise linear regression analysis of the PAT results identified two factors that significantly linked with higher PAT scores in these parents: attention- deficit/hyperactivity disorder in the child, and mood disorder in a parent. Logistic regression analysis further narrowed this down to just the child’s attention-deficit/hyperactivity disorder as the only significant correlate with higher PAT scores. The analysis showed that the severity of obesity had no significant correlation with psychosocial risk scores.
The next steps are to assess more parents of obese children this way, see whether the questions posed in the PAT can be better focused for this setting to make the screening simpler and easier to administer, and determine how interventions aimed at the identified risks improve child outcomes, Dr. Phan said.
Another goal of this research is to raise the profile of family psychosocial problems as an important factor in the development and maintenance of obesity in children, she said. “I think that people who work at pediatric weight management clinics have recognized the role of family psychosocial problems, but it is less recognized by the general pediatric community.”
Dr. Phan had no relevant financial disclosures.
BALTIMORE – Childhood obesity can result from more than just poor diet, not enough exercise, and too much screen time; it also often occurs in families with parents who have a significantly increased prevalence of psychosocial problems, judging from findings from a pilot, single-center study involving 97 parents who brought their child to a tertiary-care pediatric obesity center.
This preliminary finding “supports the need for universal psychosocial screening in this population, with particular attention to families whose children have comorbid behavioral health problems,” Dr. Thao-Ly T. Phan said while presenting a poster at the annual meeting of the Pediatric Academic Societies.
“You might think that when a child is brought to an obesity clinic, you just need to ask what foods the child eats, how often the child exercises and how much television they watch, but we also need to ask about problems in the families and address those problems,” said Dr. Phan, a pediatrician and weight management specialist at the Alfred I. duPont Hospital for Children in Wilmington, Del.
Dr. Phan said although a key next step in this research is to assess how interventions aimed at family psychosocial problems affect a child’s obesity and well-being, her experience so far suggests that the psychosocial setting where a child lives can play a significant role in the etiology and maintenance of obesity.
“We find that families at higher psychosocial risk don’t come back for treatment, and when that happens the children don’t do well. That’s a reason to screen [for such problems] and intervene with psychological and social work support,” she said in an interview.
“A lot of our messages to families focus on things like screen time and eating more fruits and vegetables, but if the family can’t implement that, then we’re missing the boat,” Dr. Phan said.
She and her associates used the Psychosocial Assessment Tool (PAT), a screening tool for parents that takes about 5-10 minutes to complete and that was developed by researchers at the Children’s Hospital of Philadelphia (ACTA Oncologica. 2015 May;54[5]:574-80). The PAT poses a series of questions that deal with a spectrum of potential psychosocial issues including financial status, a child’s problems at school, parents’ mood and substance abuse, and parental views of weight and health issues.
The investigators administered the PAT to 97 parents of children aged 4-12 years old who had their first visit to the tertiary-care pediatric obesity clinic at Alfred I. duPont. The children had body mass index levels that averaged close to the 99th percentile, with 56% of the children classified as severely obese with a BMI at or above the 99th percentile, 40% classified as obese with a BMI in the 95th-98th percentile, and 4% classified as overweight with a BMI at the 85th-94th percentile.
The PAT scores in these 97 parents identified 41% with a low risk for having psychosocial problems, 49% with a moderate risk, and 10% with a higher risk. In contrast, a historical control group of 3,918 representative U.S. parents who took the PAT showed 55% at low risk, 34% at moderate risk, and 11% at high risk, which meant that the parents of the children at the clinic had a statistically significant 70% increased prevalence of being in a high- or moderate-risk group for psychosocial problems, compared with parents in the general U.S. population, Dr. Phan reported.
A stepwise linear regression analysis of the PAT results identified two factors that significantly linked with higher PAT scores in these parents: attention- deficit/hyperactivity disorder in the child, and mood disorder in a parent. Logistic regression analysis further narrowed this down to just the child’s attention-deficit/hyperactivity disorder as the only significant correlate with higher PAT scores. The analysis showed that the severity of obesity had no significant correlation with psychosocial risk scores.
The next steps are to assess more parents of obese children this way, see whether the questions posed in the PAT can be better focused for this setting to make the screening simpler and easier to administer, and determine how interventions aimed at the identified risks improve child outcomes, Dr. Phan said.
Another goal of this research is to raise the profile of family psychosocial problems as an important factor in the development and maintenance of obesity in children, she said. “I think that people who work at pediatric weight management clinics have recognized the role of family psychosocial problems, but it is less recognized by the general pediatric community.”
Dr. Phan had no relevant financial disclosures.
AT THE PAS ANNUAL MEETING
Family’s psychosocial problems complicate pediatric obesity
BALTIMORE – Childhood obesity can result from more than just poor diet, not enough exercise, and too much screen time; it also often occurs in families with parents who have a significantly increased prevalence of psychosocial problems, judging from findings from a pilot, single-center study involving 97 parents who brought their child to a tertiary-care pediatric obesity center.
This preliminary finding “supports the need for universal psychosocial screening in this population, with particular attention to families whose children have comorbid behavioral health problems,” Dr. Thao-Ly T. Phan said while presenting a poster at the annual meeting of the Pediatric Academic Societies.
“You might think that when a child is brought to an obesity clinic, you just need to ask what foods the child eats, how often the child exercises and how much television they watch, but we also need to ask about problems in the families and address those problems,” said Dr. Phan, a pediatrician and weight management specialist at the Alfred I. duPont Hospital for Children in Wilmington, Del.
Dr. Phan said although a key next step in this research is to assess how interventions aimed at family psychosocial problems affect a child’s obesity and well-being, her experience so far suggests that the psychosocial setting where a child lives can play a significant role in the etiology and maintenance of obesity.
“We find that families at higher psychosocial risk don’t come back for treatment, and when that happens the children don’t do well. That’s a reason to screen [for such problems] and intervene with psychological and social work support,” she said in an interview.
“A lot of our messages to families focus on things like screen time and eating more fruits and vegetables, but if the family can’t implement that, then we’re missing the boat,” Dr. Phan said.
She and her associates used the Psychosocial Assessment Tool (PAT), a screening tool for parents that takes about 5-10 minutes to complete and that was developed by researchers at the Children’s Hospital of Philadelphia (ACTA Oncologica. 2015 May;54[5]:574-80). The PAT poses a series of questions that deal with a spectrum of potential psychosocial issues including financial status, a child’s problems at school, parents’ mood and substance abuse, and parental views of weight and health issues.
The investigators administered the PAT to 97 parents of children aged 4-12 years old who had their first visit to the tertiary-care pediatric obesity clinic at Alfred I. duPont. The children had body mass index levels that averaged close to the 99th percentile, with 56% of the children classified as severely obese with a BMI at or above the 99th percentile, 40% classified as obese with a BMI in the 95th-98th percentile, and 4% classified as overweight with a BMI at the 85th-94th percentile.
The PAT scores in these 97 parents identified 41% with a low risk for having psychosocial problems, 49% with a moderate risk, and 10% with a higher risk. In contrast, a historical control group of 3,918 representative U.S. parents who took the PAT showed 55% at low risk, 34% at moderate risk, and 11% at high risk, which meant that the parents of the children at the clinic had a statistically significant 70% increased prevalence of being in a high- or moderate-risk group for psychosocial problems, compared with parents in the general U.S. population, Dr. Phan reported.
A stepwise linear regression analysis of the PAT results identified two factors that significantly linked with higher PAT scores in these parents: attention- deficit/hyperactivity disorder in the child, and mood disorder in a parent. Logistic regression analysis further narrowed this down to just the child’s attention-deficit/hyperactivity disorder as the only significant correlate with higher PAT scores. The analysis showed that the severity of obesity had no significant correlation with psychosocial risk scores.
The next steps are to assess more parents of obese children this way, see whether the questions posed in the PAT can be better focused for this setting to make the screening simpler and easier to administer, and determine how interventions aimed at the identified risks improve child outcomes, Dr. Phan said.
Another goal of this research is to raise the profile of family psychosocial problems as an important factor in the development and maintenance of obesity in children, she said. “I think that people who work at pediatric weight management clinics have recognized the role of family psychosocial problems, but it is less recognized by the general pediatric community.”
Dr. Phan had no relevant financial disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BALTIMORE – Childhood obesity can result from more than just poor diet, not enough exercise, and too much screen time; it also often occurs in families with parents who have a significantly increased prevalence of psychosocial problems, judging from findings from a pilot, single-center study involving 97 parents who brought their child to a tertiary-care pediatric obesity center.
This preliminary finding “supports the need for universal psychosocial screening in this population, with particular attention to families whose children have comorbid behavioral health problems,” Dr. Thao-Ly T. Phan said while presenting a poster at the annual meeting of the Pediatric Academic Societies.
“You might think that when a child is brought to an obesity clinic, you just need to ask what foods the child eats, how often the child exercises and how much television they watch, but we also need to ask about problems in the families and address those problems,” said Dr. Phan, a pediatrician and weight management specialist at the Alfred I. duPont Hospital for Children in Wilmington, Del.
Dr. Phan said although a key next step in this research is to assess how interventions aimed at family psychosocial problems affect a child’s obesity and well-being, her experience so far suggests that the psychosocial setting where a child lives can play a significant role in the etiology and maintenance of obesity.
“We find that families at higher psychosocial risk don’t come back for treatment, and when that happens the children don’t do well. That’s a reason to screen [for such problems] and intervene with psychological and social work support,” she said in an interview.
“A lot of our messages to families focus on things like screen time and eating more fruits and vegetables, but if the family can’t implement that, then we’re missing the boat,” Dr. Phan said.
She and her associates used the Psychosocial Assessment Tool (PAT), a screening tool for parents that takes about 5-10 minutes to complete and that was developed by researchers at the Children’s Hospital of Philadelphia (ACTA Oncologica. 2015 May;54[5]:574-80). The PAT poses a series of questions that deal with a spectrum of potential psychosocial issues including financial status, a child’s problems at school, parents’ mood and substance abuse, and parental views of weight and health issues.
The investigators administered the PAT to 97 parents of children aged 4-12 years old who had their first visit to the tertiary-care pediatric obesity clinic at Alfred I. duPont. The children had body mass index levels that averaged close to the 99th percentile, with 56% of the children classified as severely obese with a BMI at or above the 99th percentile, 40% classified as obese with a BMI in the 95th-98th percentile, and 4% classified as overweight with a BMI at the 85th-94th percentile.
The PAT scores in these 97 parents identified 41% with a low risk for having psychosocial problems, 49% with a moderate risk, and 10% with a higher risk. In contrast, a historical control group of 3,918 representative U.S. parents who took the PAT showed 55% at low risk, 34% at moderate risk, and 11% at high risk, which meant that the parents of the children at the clinic had a statistically significant 70% increased prevalence of being in a high- or moderate-risk group for psychosocial problems, compared with parents in the general U.S. population, Dr. Phan reported.
A stepwise linear regression analysis of the PAT results identified two factors that significantly linked with higher PAT scores in these parents: attention- deficit/hyperactivity disorder in the child, and mood disorder in a parent. Logistic regression analysis further narrowed this down to just the child’s attention-deficit/hyperactivity disorder as the only significant correlate with higher PAT scores. The analysis showed that the severity of obesity had no significant correlation with psychosocial risk scores.
The next steps are to assess more parents of obese children this way, see whether the questions posed in the PAT can be better focused for this setting to make the screening simpler and easier to administer, and determine how interventions aimed at the identified risks improve child outcomes, Dr. Phan said.
Another goal of this research is to raise the profile of family psychosocial problems as an important factor in the development and maintenance of obesity in children, she said. “I think that people who work at pediatric weight management clinics have recognized the role of family psychosocial problems, but it is less recognized by the general pediatric community.”
Dr. Phan had no relevant financial disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
BALTIMORE – Childhood obesity can result from more than just poor diet, not enough exercise, and too much screen time; it also often occurs in families with parents who have a significantly increased prevalence of psychosocial problems, judging from findings from a pilot, single-center study involving 97 parents who brought their child to a tertiary-care pediatric obesity center.
This preliminary finding “supports the need for universal psychosocial screening in this population, with particular attention to families whose children have comorbid behavioral health problems,” Dr. Thao-Ly T. Phan said while presenting a poster at the annual meeting of the Pediatric Academic Societies.
“You might think that when a child is brought to an obesity clinic, you just need to ask what foods the child eats, how often the child exercises and how much television they watch, but we also need to ask about problems in the families and address those problems,” said Dr. Phan, a pediatrician and weight management specialist at the Alfred I. duPont Hospital for Children in Wilmington, Del.
Dr. Phan said although a key next step in this research is to assess how interventions aimed at family psychosocial problems affect a child’s obesity and well-being, her experience so far suggests that the psychosocial setting where a child lives can play a significant role in the etiology and maintenance of obesity.
“We find that families at higher psychosocial risk don’t come back for treatment, and when that happens the children don’t do well. That’s a reason to screen [for such problems] and intervene with psychological and social work support,” she said in an interview.
“A lot of our messages to families focus on things like screen time and eating more fruits and vegetables, but if the family can’t implement that, then we’re missing the boat,” Dr. Phan said.
She and her associates used the Psychosocial Assessment Tool (PAT), a screening tool for parents that takes about 5-10 minutes to complete and that was developed by researchers at the Children’s Hospital of Philadelphia (ACTA Oncologica. 2015 May;54[5]:574-80). The PAT poses a series of questions that deal with a spectrum of potential psychosocial issues including financial status, a child’s problems at school, parents’ mood and substance abuse, and parental views of weight and health issues.
The investigators administered the PAT to 97 parents of children aged 4-12 years old who had their first visit to the tertiary-care pediatric obesity clinic at Alfred I. duPont. The children had body mass index levels that averaged close to the 99th percentile, with 56% of the children classified as severely obese with a BMI at or above the 99th percentile, 40% classified as obese with a BMI in the 95th-98th percentile, and 4% classified as overweight with a BMI at the 85th-94th percentile.
The PAT scores in these 97 parents identified 41% with a low risk for having psychosocial problems, 49% with a moderate risk, and 10% with a higher risk. In contrast, a historical control group of 3,918 representative U.S. parents who took the PAT showed 55% at low risk, 34% at moderate risk, and 11% at high risk, which meant that the parents of the children at the clinic had a statistically significant 70% increased prevalence of being in a high- or moderate-risk group for psychosocial problems, compared with parents in the general U.S. population, Dr. Phan reported.
A stepwise linear regression analysis of the PAT results identified two factors that significantly linked with higher PAT scores in these parents: attention- deficit/hyperactivity disorder in the child, and mood disorder in a parent. Logistic regression analysis further narrowed this down to just the child’s attention-deficit/hyperactivity disorder as the only significant correlate with higher PAT scores. The analysis showed that the severity of obesity had no significant correlation with psychosocial risk scores.
The next steps are to assess more parents of obese children this way, see whether the questions posed in the PAT can be better focused for this setting to make the screening simpler and easier to administer, and determine how interventions aimed at the identified risks improve child outcomes, Dr. Phan said.
Another goal of this research is to raise the profile of family psychosocial problems as an important factor in the development and maintenance of obesity in children, she said. “I think that people who work at pediatric weight management clinics have recognized the role of family psychosocial problems, but it is less recognized by the general pediatric community.”
Dr. Phan had no relevant financial disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Parents of children who came to a tertiary-care pediatric obesity clinic showed a relatively high prevalence of psychosocial problems, suggesting a new intervention target for refractory childhood obesity.
Major finding: Parents of children presenting to a referral obesity clinic had a psychosocial risk score 70% higher than the U.S. average.
Data source: A single-center study of 97 parents of children initially presenting to a tertiary-care pediatric obesity clinic.
Disclosures: Dr. Phan had no relevant financial disclosures.
NSAIDs work best in selected systemic JIA kids
BALTIMORE – Children with systemic juvenile idiopathic arthritis have the best odds for responding to initial treatment with a nonsteroidal anti-inflammatory drug if they are no older than 6 years old, have five or fewer involved joints, and have a serum level of C-reactive protein that is at or below 13 mg/dL, based on a review of 57 children with systemic juvenile idiopathic arthritis treated with these drugs at a single U.S. center during 2000-2014.
“We recommend a trial of NSAID [nonsteroidal anti-inflammatory drug] monotherapy for these patients with systemic juvenile idiopathic arthritis [JIA],” Dr. Anjali S. Sura said at the annual meeting of the Pediatric Academic Societies. A reasonable trial of NSAID monotherapy would last 6 weeks; if patients failed to adequately respond at the end of 6 weeks, it would be reasonable to switch to another of the first-line drugs recommended for children starting treatment for JIA, either a glucocorticoid or the biological agent anakinra (Kineret), said Dr. Sura, a pediatrician at the University of Michigan in Ann Arbor.
Initial treatment with a NSAID is preferred, even though it will probably work in only about a quarter of patients, because it generally has the best safety profile among these three options, Dr. Sura said in an interview. “If we can risk-stratify children with systemic JIA for NSAID therapy” using these three criteria, “then NSAID monotherapy may be more effective,” she explained.
The NSAIDs most commonly used to treat systemic JIA are naproxen or indomethacin, at anti-inflammatory dosages, which for naproxen is 15-20 mg/kg per day, and for indomethacin 3-4 mg/kg per day, she said.
But Dr. Sura also cautioned that the analysis she presented focused on a relatively small and selected group of children with systemic JIA who received initial NSAID monotherapy. The series she and her associates reviewed included 99 patients, of whom 57 received NSAID monotherapy; 35 of these patients were 6 years old or younger.
The researchers compared the 15 NSAID responders (26%), defined as patients who had clinically inactive disease, with the 42 nonresponders and identified the three clinical and demographic characteristics that occurred much more often among responders. The ideal candidates for initial NSAID monotherapy should fulfill all three criteria: age, number of affected joints, and serum level of C-reactive protein, Dr. Sura said in her report.
Dr. Sura noted that a panel of the American College of Rheumatology said that NSAIDs, glucocorticoids, and anakinra were equally good options for initial treatment of JIA in their 2013 update of JIA recommendations (Arthritis Rheum. 2013 Oct;65[10]:2499-512). This 2013 update excepted patients with no actively affected joints, whom the panel said should specifically receive an NSAID, and excepted patients with a high global severity score as rated by their physicians, whom the panel said should receive either a glucocorticoid or anakinra but not NSAID monotherapy. The European League Against Rheumatism has not issued recommendations for managing systemic JIA.
Dr. Sura had no disclosures.
On Twitter @mitchelzoler
BALTIMORE – Children with systemic juvenile idiopathic arthritis have the best odds for responding to initial treatment with a nonsteroidal anti-inflammatory drug if they are no older than 6 years old, have five or fewer involved joints, and have a serum level of C-reactive protein that is at or below 13 mg/dL, based on a review of 57 children with systemic juvenile idiopathic arthritis treated with these drugs at a single U.S. center during 2000-2014.
“We recommend a trial of NSAID [nonsteroidal anti-inflammatory drug] monotherapy for these patients with systemic juvenile idiopathic arthritis [JIA],” Dr. Anjali S. Sura said at the annual meeting of the Pediatric Academic Societies. A reasonable trial of NSAID monotherapy would last 6 weeks; if patients failed to adequately respond at the end of 6 weeks, it would be reasonable to switch to another of the first-line drugs recommended for children starting treatment for JIA, either a glucocorticoid or the biological agent anakinra (Kineret), said Dr. Sura, a pediatrician at the University of Michigan in Ann Arbor.
Initial treatment with a NSAID is preferred, even though it will probably work in only about a quarter of patients, because it generally has the best safety profile among these three options, Dr. Sura said in an interview. “If we can risk-stratify children with systemic JIA for NSAID therapy” using these three criteria, “then NSAID monotherapy may be more effective,” she explained.
The NSAIDs most commonly used to treat systemic JIA are naproxen or indomethacin, at anti-inflammatory dosages, which for naproxen is 15-20 mg/kg per day, and for indomethacin 3-4 mg/kg per day, she said.
But Dr. Sura also cautioned that the analysis she presented focused on a relatively small and selected group of children with systemic JIA who received initial NSAID monotherapy. The series she and her associates reviewed included 99 patients, of whom 57 received NSAID monotherapy; 35 of these patients were 6 years old or younger.
The researchers compared the 15 NSAID responders (26%), defined as patients who had clinically inactive disease, with the 42 nonresponders and identified the three clinical and demographic characteristics that occurred much more often among responders. The ideal candidates for initial NSAID monotherapy should fulfill all three criteria: age, number of affected joints, and serum level of C-reactive protein, Dr. Sura said in her report.
Dr. Sura noted that a panel of the American College of Rheumatology said that NSAIDs, glucocorticoids, and anakinra were equally good options for initial treatment of JIA in their 2013 update of JIA recommendations (Arthritis Rheum. 2013 Oct;65[10]:2499-512). This 2013 update excepted patients with no actively affected joints, whom the panel said should specifically receive an NSAID, and excepted patients with a high global severity score as rated by their physicians, whom the panel said should receive either a glucocorticoid or anakinra but not NSAID monotherapy. The European League Against Rheumatism has not issued recommendations for managing systemic JIA.
Dr. Sura had no disclosures.
On Twitter @mitchelzoler
BALTIMORE – Children with systemic juvenile idiopathic arthritis have the best odds for responding to initial treatment with a nonsteroidal anti-inflammatory drug if they are no older than 6 years old, have five or fewer involved joints, and have a serum level of C-reactive protein that is at or below 13 mg/dL, based on a review of 57 children with systemic juvenile idiopathic arthritis treated with these drugs at a single U.S. center during 2000-2014.
“We recommend a trial of NSAID [nonsteroidal anti-inflammatory drug] monotherapy for these patients with systemic juvenile idiopathic arthritis [JIA],” Dr. Anjali S. Sura said at the annual meeting of the Pediatric Academic Societies. A reasonable trial of NSAID monotherapy would last 6 weeks; if patients failed to adequately respond at the end of 6 weeks, it would be reasonable to switch to another of the first-line drugs recommended for children starting treatment for JIA, either a glucocorticoid or the biological agent anakinra (Kineret), said Dr. Sura, a pediatrician at the University of Michigan in Ann Arbor.
Initial treatment with a NSAID is preferred, even though it will probably work in only about a quarter of patients, because it generally has the best safety profile among these three options, Dr. Sura said in an interview. “If we can risk-stratify children with systemic JIA for NSAID therapy” using these three criteria, “then NSAID monotherapy may be more effective,” she explained.
The NSAIDs most commonly used to treat systemic JIA are naproxen or indomethacin, at anti-inflammatory dosages, which for naproxen is 15-20 mg/kg per day, and for indomethacin 3-4 mg/kg per day, she said.
But Dr. Sura also cautioned that the analysis she presented focused on a relatively small and selected group of children with systemic JIA who received initial NSAID monotherapy. The series she and her associates reviewed included 99 patients, of whom 57 received NSAID monotherapy; 35 of these patients were 6 years old or younger.
The researchers compared the 15 NSAID responders (26%), defined as patients who had clinically inactive disease, with the 42 nonresponders and identified the three clinical and demographic characteristics that occurred much more often among responders. The ideal candidates for initial NSAID monotherapy should fulfill all three criteria: age, number of affected joints, and serum level of C-reactive protein, Dr. Sura said in her report.
Dr. Sura noted that a panel of the American College of Rheumatology said that NSAIDs, glucocorticoids, and anakinra were equally good options for initial treatment of JIA in their 2013 update of JIA recommendations (Arthritis Rheum. 2013 Oct;65[10]:2499-512). This 2013 update excepted patients with no actively affected joints, whom the panel said should specifically receive an NSAID, and excepted patients with a high global severity score as rated by their physicians, whom the panel said should receive either a glucocorticoid or anakinra but not NSAID monotherapy. The European League Against Rheumatism has not issued recommendations for managing systemic JIA.
Dr. Sura had no disclosures.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Three clinical parameters identified the children with systemic juvenile idiopathic arthritis who historically responded best to initial treatment with a nonsteroidal anti-inflammatory drug.
Major finding: Five or fewer involved joints, 6 years old or younger, and C-reactive protein of 13 mg/dL or less identified the best NSAID responders.
Data source: Review of 57 children with systemic juvenile idiopathic arthritis treated initially with NSAID monotherapy at one U.S. center.
Disclosures: Dr. Sura had no disclosures.
Ambulatory blood pressure rules hypertension diagnosis and follow-up
Evidence is becoming overwhelming that ambulatory blood pressure monitoring is the only reliable way to measure blood pressure for both diagnosing hypertension and following patients once they are diagnosed.
Office-based blood pressure measurement is out, be it a one-off reading or a cluster of sequential readings during a single office visit. Ambulatory blood pressure monitoring (ABPM) increasingly is the standard of care.
One recent nail in the coffin of office-based measurement came in a modestly-sized but revealing study reported by Dr. Joyce P. Samuel, a pediatric hypertension specialist at the University of Texas in Houston. She reported her experience directly comparing ambulatory and carefully-done office-based blood pressure measurement in a presentation at the annual meeting of the Pediatric Academic Societies in Baltimore.
Dr. Samuel followed 40 patients age 9-21 years whom she had previously diagnosed with essential hypertension (children with a systolic blood pressure at or above the 95th percentile for sex, age, and height), and repeatedly measured their blood pressures by both ambulatory and office-based readings at 2-week intervals as she searched for the best combination of antihypertensive drugs for each patient. She sent patients home for 24 hours of blood-pressure monitoring with an ambulatory device, and when they returned to her office the next day, she performed an office-based measurement using meticulous technique: Each child was seated and calm, measured on the right arm, with four measurements taken sequentially at about 1 minute intervals with the first reading discarded and the remaining three averaged.
Over the course of several months, she collected 173 paired ambulatory and office-based systolic blood pressure readings from individual patients. Substantial differences between the two forms of measurement were remarkably common. In 20% of the pairs, the ambulatory systolic reading was at least 10 mm Hg higher than the office-based reading, and for some pairs the differences ran as high as 30 mm Hg. In an additional 32% of the paired readings, office-based systolic pressure ran at least 10 mm Hg higher and in some cases as much as 35 mm Hg higher than the ambulatory reading.
Dr. Samuel also analyzed her findings a different way to assess the clinical consequences of these differences based on whether a child’s systolic pressure identified the patient as normotensive, hypertensive, or prehypertensive (a systolic pressure at the 90-94th percentile for the child’s age, sex and height). She found that the diagnoses matched for only 49% of the paired measurements. In 24% of the paired readings, ABPM identified children with hypertension that was not seen with concurrent office-based measurement, cases of masked hypertension. In 17% of the pairs, office-based measurement diagnosed hypertension that was not confirmed by ABPM, cases of white-coat hypertension. The remaining 10% of pairs were mismatched by showing normotensive with one method and prehypertensive with the other method. Dr. Samuel searched for any consistent patterns in these differences and found none. The disparate results with ambulatory and office-based measurements seemed almost random, with no correlation with age, sex, race, the medications patients received, or how many times a patient had already undergone dual blood-pressure monitoring. Individual patients had no meaningful differences between some of their paired measurements but had a meaningful disparity for others.
“We were unable to predict discrepancies,” said Dr. Samuels.
“You can’t get around it, you need ambulatory blood pressure monitoring to make the best diagnosis” of hypertension, she told me. “We need to push to make ambulatory monitoring more available. I am moving toward believing that ambulatory blood pressure monitoring must be routinely done on everyone. This is what the data suggest.”
It’s also where medicine is headed. In 2015, the U.S. Preventative Services Task Force (USPSTF) issued new recommendations for hypertension screening in adults aged 18 years or older, indicating that there was “convincing evidence that ABPM is the best method for diagnosing hypertension,” and the agency further recommended that ABPM is “the reference standard for confirming the diagnosis of hypertension.” Another endorsement of ambulatory blood pressure monitoring came out last year from the International Society for Chronobiology.
Recommendations are not yet as evolved for children. The USPSTF last weighed in on screening kids for hypertension in 2013, and said the evidence as of then was “insufficient” to assess the benefits and harms of screening for hypertension in children and adolescents. That document endorsed careful office-based blood pressure measurement, which highlights how recently expert sentiment has shifted on the issue of measurement. In response to the USPSTF 2013 statement, the American Academy of Pediatrics noted that it continued to back recommendations that are more than a decade old from the National High Blood Pressure Education Program that called for hypertension screening in children starting when they are 3 years old. Neither of these two groups has made any recent statement about the preferred method to measure blood pressure.
On Twitter @mitchelzoler
Evidence is becoming overwhelming that ambulatory blood pressure monitoring is the only reliable way to measure blood pressure for both diagnosing hypertension and following patients once they are diagnosed.
Office-based blood pressure measurement is out, be it a one-off reading or a cluster of sequential readings during a single office visit. Ambulatory blood pressure monitoring (ABPM) increasingly is the standard of care.
One recent nail in the coffin of office-based measurement came in a modestly-sized but revealing study reported by Dr. Joyce P. Samuel, a pediatric hypertension specialist at the University of Texas in Houston. She reported her experience directly comparing ambulatory and carefully-done office-based blood pressure measurement in a presentation at the annual meeting of the Pediatric Academic Societies in Baltimore.
Dr. Samuel followed 40 patients age 9-21 years whom she had previously diagnosed with essential hypertension (children with a systolic blood pressure at or above the 95th percentile for sex, age, and height), and repeatedly measured their blood pressures by both ambulatory and office-based readings at 2-week intervals as she searched for the best combination of antihypertensive drugs for each patient. She sent patients home for 24 hours of blood-pressure monitoring with an ambulatory device, and when they returned to her office the next day, she performed an office-based measurement using meticulous technique: Each child was seated and calm, measured on the right arm, with four measurements taken sequentially at about 1 minute intervals with the first reading discarded and the remaining three averaged.
Over the course of several months, she collected 173 paired ambulatory and office-based systolic blood pressure readings from individual patients. Substantial differences between the two forms of measurement were remarkably common. In 20% of the pairs, the ambulatory systolic reading was at least 10 mm Hg higher than the office-based reading, and for some pairs the differences ran as high as 30 mm Hg. In an additional 32% of the paired readings, office-based systolic pressure ran at least 10 mm Hg higher and in some cases as much as 35 mm Hg higher than the ambulatory reading.
Dr. Samuel also analyzed her findings a different way to assess the clinical consequences of these differences based on whether a child’s systolic pressure identified the patient as normotensive, hypertensive, or prehypertensive (a systolic pressure at the 90-94th percentile for the child’s age, sex and height). She found that the diagnoses matched for only 49% of the paired measurements. In 24% of the paired readings, ABPM identified children with hypertension that was not seen with concurrent office-based measurement, cases of masked hypertension. In 17% of the pairs, office-based measurement diagnosed hypertension that was not confirmed by ABPM, cases of white-coat hypertension. The remaining 10% of pairs were mismatched by showing normotensive with one method and prehypertensive with the other method. Dr. Samuel searched for any consistent patterns in these differences and found none. The disparate results with ambulatory and office-based measurements seemed almost random, with no correlation with age, sex, race, the medications patients received, or how many times a patient had already undergone dual blood-pressure monitoring. Individual patients had no meaningful differences between some of their paired measurements but had a meaningful disparity for others.
“We were unable to predict discrepancies,” said Dr. Samuels.
“You can’t get around it, you need ambulatory blood pressure monitoring to make the best diagnosis” of hypertension, she told me. “We need to push to make ambulatory monitoring more available. I am moving toward believing that ambulatory blood pressure monitoring must be routinely done on everyone. This is what the data suggest.”
It’s also where medicine is headed. In 2015, the U.S. Preventative Services Task Force (USPSTF) issued new recommendations for hypertension screening in adults aged 18 years or older, indicating that there was “convincing evidence that ABPM is the best method for diagnosing hypertension,” and the agency further recommended that ABPM is “the reference standard for confirming the diagnosis of hypertension.” Another endorsement of ambulatory blood pressure monitoring came out last year from the International Society for Chronobiology.
Recommendations are not yet as evolved for children. The USPSTF last weighed in on screening kids for hypertension in 2013, and said the evidence as of then was “insufficient” to assess the benefits and harms of screening for hypertension in children and adolescents. That document endorsed careful office-based blood pressure measurement, which highlights how recently expert sentiment has shifted on the issue of measurement. In response to the USPSTF 2013 statement, the American Academy of Pediatrics noted that it continued to back recommendations that are more than a decade old from the National High Blood Pressure Education Program that called for hypertension screening in children starting when they are 3 years old. Neither of these two groups has made any recent statement about the preferred method to measure blood pressure.
On Twitter @mitchelzoler
Evidence is becoming overwhelming that ambulatory blood pressure monitoring is the only reliable way to measure blood pressure for both diagnosing hypertension and following patients once they are diagnosed.
Office-based blood pressure measurement is out, be it a one-off reading or a cluster of sequential readings during a single office visit. Ambulatory blood pressure monitoring (ABPM) increasingly is the standard of care.
One recent nail in the coffin of office-based measurement came in a modestly-sized but revealing study reported by Dr. Joyce P. Samuel, a pediatric hypertension specialist at the University of Texas in Houston. She reported her experience directly comparing ambulatory and carefully-done office-based blood pressure measurement in a presentation at the annual meeting of the Pediatric Academic Societies in Baltimore.
Dr. Samuel followed 40 patients age 9-21 years whom she had previously diagnosed with essential hypertension (children with a systolic blood pressure at or above the 95th percentile for sex, age, and height), and repeatedly measured their blood pressures by both ambulatory and office-based readings at 2-week intervals as she searched for the best combination of antihypertensive drugs for each patient. She sent patients home for 24 hours of blood-pressure monitoring with an ambulatory device, and when they returned to her office the next day, she performed an office-based measurement using meticulous technique: Each child was seated and calm, measured on the right arm, with four measurements taken sequentially at about 1 minute intervals with the first reading discarded and the remaining three averaged.
Over the course of several months, she collected 173 paired ambulatory and office-based systolic blood pressure readings from individual patients. Substantial differences between the two forms of measurement were remarkably common. In 20% of the pairs, the ambulatory systolic reading was at least 10 mm Hg higher than the office-based reading, and for some pairs the differences ran as high as 30 mm Hg. In an additional 32% of the paired readings, office-based systolic pressure ran at least 10 mm Hg higher and in some cases as much as 35 mm Hg higher than the ambulatory reading.
Dr. Samuel also analyzed her findings a different way to assess the clinical consequences of these differences based on whether a child’s systolic pressure identified the patient as normotensive, hypertensive, or prehypertensive (a systolic pressure at the 90-94th percentile for the child’s age, sex and height). She found that the diagnoses matched for only 49% of the paired measurements. In 24% of the paired readings, ABPM identified children with hypertension that was not seen with concurrent office-based measurement, cases of masked hypertension. In 17% of the pairs, office-based measurement diagnosed hypertension that was not confirmed by ABPM, cases of white-coat hypertension. The remaining 10% of pairs were mismatched by showing normotensive with one method and prehypertensive with the other method. Dr. Samuel searched for any consistent patterns in these differences and found none. The disparate results with ambulatory and office-based measurements seemed almost random, with no correlation with age, sex, race, the medications patients received, or how many times a patient had already undergone dual blood-pressure monitoring. Individual patients had no meaningful differences between some of their paired measurements but had a meaningful disparity for others.
“We were unable to predict discrepancies,” said Dr. Samuels.
“You can’t get around it, you need ambulatory blood pressure monitoring to make the best diagnosis” of hypertension, she told me. “We need to push to make ambulatory monitoring more available. I am moving toward believing that ambulatory blood pressure monitoring must be routinely done on everyone. This is what the data suggest.”
It’s also where medicine is headed. In 2015, the U.S. Preventative Services Task Force (USPSTF) issued new recommendations for hypertension screening in adults aged 18 years or older, indicating that there was “convincing evidence that ABPM is the best method for diagnosing hypertension,” and the agency further recommended that ABPM is “the reference standard for confirming the diagnosis of hypertension.” Another endorsement of ambulatory blood pressure monitoring came out last year from the International Society for Chronobiology.
Recommendations are not yet as evolved for children. The USPSTF last weighed in on screening kids for hypertension in 2013, and said the evidence as of then was “insufficient” to assess the benefits and harms of screening for hypertension in children and adolescents. That document endorsed careful office-based blood pressure measurement, which highlights how recently expert sentiment has shifted on the issue of measurement. In response to the USPSTF 2013 statement, the American Academy of Pediatrics noted that it continued to back recommendations that are more than a decade old from the National High Blood Pressure Education Program that called for hypertension screening in children starting when they are 3 years old. Neither of these two groups has made any recent statement about the preferred method to measure blood pressure.
On Twitter @mitchelzoler
TAVR enters a new risk-scoring era
In the 14 years since the first transcatheter aortic valve replacement in 2002, devices and delivery methods have undergone several generations of improvement, but one facet of the procedure remained largely unchanged: When prospective patients underwent preprocedural assessment to gauge their risk level, the long-standing approach to quantify their disease severity and 30-day mortality risk was to run their clinical and demographic numbers through the risk calculator developed by the Society of Thoracic Surgeons.
Although determining a patient’s Society of Thoracic Surgeons (STS) risk score using a formula based on extensive experience performing surgical aortic valve replacement (SAVR) by open surgery made a lot of sense during an era when the preeminent question was how transcatheter aortic valve replacement (TAVR) compared with SAVR, it also carried the inherent limitation of estimating a patient’s risk when undergoing TAVR based on SAVR’s track record.
That limitation is now gone.
In December 2015, a team of cardiothoracic surgeons and interventional cardiologists assembled by the STS and the American College of Cardiology placed a new risk calculator online to estimate a prospective TAVR patient’s risk for dying in hospital following a TAVR procedure. The panel developed this risk calculator with data from nearly 14,000 U.S. TAVR patients enrolled in the STS/ACC Transcatheter Valve Replacement Registry during November 2011–February 2014 and then validated it with data from another nearly 7,000 U.S. TAVR patients who underwent their procedure during March-October 2014. This created the first mortality-risk calculator for TAVR patients based entirely on experience with such patients (JAMA Cardiology. 2016 Apr;1[1]:46-52).
In May 2016, a second, independent risk calculator will go live, also based exclusively on experience in TAVR patients, that estimates a patient’s risk for either dying or having a worsened or unimproved and poor quality of life during the 6 months following TAVR. This risk calculator, developed by a team led by researchers based at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., used data collected from more than 2,000 TAVR patients enrolled in the PARTNER trial or in the continued-access PARTNER registry (Circulation. 2014 June 24;129[25]:2682-90), and is offered to users by Health Outcomes Sciences, a Kansas City–based company that’s affiliated with Saint Luke’s.
Although use of these two TAVR-specific risk calculators during their early days of availability remains relatively light, TAVR experts see them as marking a new era in the workup of TAVR candidates.
“There is universal agreement that risk models must be developed based on the history of patients who actually received the treatment,” said Dr. Fred H. Edwards, the cardiothoracic surgeon at the University of Florida, Jacksonville, who led the team that developed the transcatheter valve therapy (TVT)-derived in-hospital mortality risk calculator. “Everyone realized that the STS score and the EuroScore [another operative-risk calculator historically used for prospective TAVR patients] were inadequate to extrapolate to TAVR patients.” But development had to wait until an adequately-sized experience with TAVR had accumulated. “We started the process [to develop the TVT risk calculator] when we reached about 10,000 patients” enrolled in the registry, after which it took “close to 2 years” to produce the finished product, Dr. Edwards said in an interview.
The TVT in-hospital mortality predictor gradually goes mainstream
“There is consensus that the new TVT calculator will be more reliable than the STS operative-risk model” for assessing patients being considered for TAVR, but it has not yet gained widespread use “because it is so new,” noted Dr. Edwards.
“It will take a while to incorporate it into routine practice, but I think it will be used quite a bit,” especially for “trickier and harder cases,” commented Dr. George Dangas, a professor of medicine at the Mount Sinai School of Medicine in New York and an interventional cardiologist who performs TAVR.
He also predicted that prospective patients and their families will become frequent users of the TVT in-hospital risk calculator. He sees the new risk tool as a complement to the STS risk score rather than something to replace it.
“Patients find it useful to receive an estimate of their surgical risk, and they’ll want to compare that” with their TAVR risk. “It helps to know both,” Dr. Dangas said in an interview. “Patients will likely compute it themselves.”
He foresees fairly quick integration of the new TVT score into heart team discussions as well. “The STS score will always be part of the discussion, but over time as people grow accustomed to the TVT score they will incorporate it as well. The [TAVR] community has to figure out how to use the two scores in combination.”
“There has been need for a risk calculator specific to TAVR since the patient population has only some overlap with the patients who underwent SAVR in the past,” said Dr. John D. Carroll, professor and director of interventional cardiology at the University of Colorado at Denver, Aurora, and a member of the TVT Registry panel that developed the calculator. “The STS score does not include variables that are frequently found in TAVR patients, such as liver disease, pulmonary hypertension, very-advance age, and frailty.”
A big plus for the new TVT risk calculator is its derivation from thousands of real-world, U.S. patients, Dr. Carroll noted. “It provides a patient-specific risk assessment rather than an assessment based on average patients from TAVR clinical trials.” Dr. Carroll added that since its introduction he has used the TVT risk calculator for some of his own patients being considered for TAVR.
The Saint Luke’s TAVR risk calculator
Although experts foresee an important role for profiling a patient’s predicted gain or loss in quality of life following TAVR as another element in the discussions between heart teams and patients, the risk calculator becoming available in May from Health Outcomes Sciences faces some significant issues, they said.
The Saint Luke’s Mid America team that developed the calculator used as their endpoint for a poor patient outcome 6 months after TAVR the combined rate of either death or two different measures of impaired quality of life: a Kansas City Cardiomyopathy Questionnaire–Overall Summary Scale (KCCQ-OS) score of less than 45 (measured on a scale of 0-100, where higher scores reflect better quality of life and function) or at least a 10-point reduction from baseline in a patient’s KCCQ-OS score.
By predicting a patient’s likelihood of emerging from TAVR with either a low or significantly worsened quality of life and function, this score is a “complement” to the TVT in-hospital mortality score, said Dr. Suzanne V. Arnold, a cardiologist at Saint Luke’s Mid America and one of the lead developers of this risk calculator.
“In-hospital mortality is an assessment of whether a patient will make it through the TAVR procedure. Our model is more about failure to recover after the procedure,” she explained in an interview. She and others also say that the Saint Luke’s calculator is a measure of probable futility when performing TAVR – that is, the likelihood that a patient will either not live long after the procedure or gain enough benefit from it to make performing the TAVR procedure an attractive option.
Dr. Arnold and her associates derived and validated the risk model using data collected from the “high risk” patients enrolled in the initial PARTNER trial and registry, so for the time being it remains primarily applicable to high-risk patients, who have classically been defined as patients with a STS risk score of 8% or greater (patients who have at least an 8% predicted risk of death during the 30 days following SAVR). She and her associates plan to see if they can validate the Saint Luke’s calculator in intermediate risk patients with aortic stenosis (usually defined as patients with a STS risk score of 4%-8%) with data collected in trials that enrolled these patients, such as PARTNER 2. At the ACC’s annual meeting in April in Chicago, Dr. Arnold presented a report in which she and her associates further validated their model using data collected from the high-risk patients enrolled in the CoreValve TAVR trial. This validation confirmed that the model worked “beautifully,” Dr. Arnold said.
The Saint Luke’s risk calculator uses six data entries: whether or not the patient has diabetes, atrial fibrillation, or requires oxygen support at home; whether the patient has no, mild, or moderate-to-severe dementia; the patient’s mean aortic gradient; and the patient’s score on the Kansas City Cardiomyopathy Questionnaire-12 (an abbreviated version of the 23-question KCCQ-OS scale). The result it produces – the likelihood of death or poor quality of life at 6 months – is “another piece of data to help the physician, surgeon, and patient make a decision” on whether to proceed with TAVR, she explained. “I would probably advise that if the predicted risk is high, the patient consider undergoing balloon aortic valvuloplasty” instead of TAVR “to see whether the patient has some recovery before committing to TAVR, but there are no hard and fast rules,” she acknowledged.
Dr. Arnold gave this recent case she had as an example of how running the Saint Luke’s risk calculator helped decision making:
A potential TAVR patient was a man in his 60s with end-stage renal disease, oxygen-dependent lung disease, and poor functional status. Applying the risk calculator to this patient “changed the conversation a surgeon and I had with the patient,” she said. “We let him know that TAVR might not make him feel better and it wouldn’t fix his kidneys or his lungs. Given his [relatively young] age, the patient still wanted to proceed, and we performed balloon aortic valvuloplasty, after which he seemed to do much better. He eventually underwent TAVR and did okay.”
This was a good application of the Saint Luke’s prediction model, Dr. Arnold said. As a consequence of the risk quantification, it provided that “the patient more fully understood the risk of the TAVR procedure” and had a better understanding of his prospects for recovery.
The heart teams at Saint Luke’s Mid America that perform TAVR began running this risk calculator on every high-risk patient evaluated in their valve clinic, about five patients each week, starting in mid-March 2016. The results are displayed in the patient’s chart next to the STS risk score.
By late April 2016, the staff at Health Outcomes Services, the commercial partner to Saint Luke’s that will offer the calculator online to the public, planned to have this risk calculator ready for routine use online by sometime in May. They said the company will make access to it available to any physician, surgeon, or other member of a heart team at no charge.*
Pros and cons of the Saint Luke’s risk calculator
While others applauded the creation of the Saint Luke’s risk calculator and the broader range of outcomes it predicts, they also questioned the generalizability of a risk assessment that is modeled against the selected patients enrolled in the PARTNER trial and registry, and some uncertainty on how to best use this information to inform clinical decision making.
“We certainly need to assess benefit as well as risk,” commented Dr. Edwards. The Kansas City–led group “is solidly on the right track,” and “I hope people will use their model,” he said.
In fact, the TVT Registry panel he heads is currently moving toward producing a similar expansion of their in-hospital mortality risk calculator that takes into account midterm changes in KCCQ status. Dr. Edwards said he hopes this expanded version of the TVT calculator might be ready in another year or two.
“KCCQ data are hard and time-consuming to collect, and clinicians who participate in the TVT Registry do not always do it,” he explained. “It’s an administrative burden” to make a KCCQ assessment both at baseline and at 6 or 12 month follow-up after TAVR.
“We’ve done a lot of education with registry participants to improve KCCQ data collection.” Dr. Edwards said he hopes that within another year this aspect of patient assessment will occur for about 90% of patients enrolled in the TVT Registry.
Dr. Edwards also highlighted the inherent limitations of applying the Saint Luke’s risk-assessment model, developed and validated in patients enrolled in the PARTNER and CoreValve trials and PARTNER registry, an aggregate of roughly 5,000 selected patients, to the more diverse patients seen in routine practice today and entered into the TVT Registry.
“The advantages of the TVT Registry are the huge numbers and the all-comers population,” he said. “You need to ask whether the randomized trial populations are truly representative.”
That’s a concern shared by Dr. Dangas, who also highlighted the challenges of assessing the risk a patient faces from noncardiovascular comorbidities and how that might affect a decision of whether or not to perform TAVR.
“These are elderly patients with many comorbidities. I’m not sure how well the noncardiac comorbidities were captured in the databases” for the PARTNER and CoreValve trials and registry, he said. “I’m not sure the noncardiac comorbidities were as well figured out” in those trials run several years ago as they might be today. “It’s not exactly what TAVR is about in 2016.” Despite his skepticism, Dr. Dangas acknowledged that a scoring formula that reliably captures and follows data collected by the KCCQ “would be useful.”
Another challenge is using a risk assessment tool that takes into account patient “frailty” as a way to judge whether TAVR might be “futile” for a specific patient, Dr. Dangas said.
“It’s a tough discussion to have prospectively with a patient. The question is valid, but how confident can we be prospectively, at the time of TAVR, that the procedure will be futile within a year?” He envisions that with more time and data, researchers will create a reliable risk assessment formula to gauge a patient’s midterm benefit from TAVR, but for now the Saint Luke’s scoring formula probably needs “more refinement,” he said.
“Patients need guidance by an individualized assessment that takes into account not only the risk they face from TAVR but also the benefit – the likelihood that they will not only be alive following TAVR but that they will gain improvement in functionality and in quality of life,” said Dr. Carroll. “This is especially important for patients who have other conditions that might prevent them from fully benefiting from TAVR, such as being on dialysis, having significant lung disease, or other conditions that could limit their ability to become more functional and feel better after TAVR.”
Although Health Outcomes Services is a for-profit company, it plans to make access to the Saint Luke’s risk calculator, which they call the “TAVI [transcatheter aortic valve implantation] Risk Calculator,” free to any health professional who applies for access, with a promised turnaround for access after application of about a day, said Joy Efron, the company’s vice president for commercialization. They do not plan to provide calculator access to patients. According to Ms. Efron, Health Outcomes Services decided to make their calculator available at no charge in the hope of potentially interesting some users in an upgraded, more extensive version of the calculator bundled with related products and features that are available as a package for a monthly subscription fee.
Dr. Edwards, Dr. Dangas, Dr. Carroll, and Dr. Arnold had no relevant disclosures. Saint Luke’s Mid America Heart Institute, where Dr. Arnold works, was an early investor in Health Outcomes Services, the company that is marketing the Saint Luke’s risk calculator.
On Twitter @mitchelzoler
*An earlier version of this article misstated the cost of the Saint Luke's TAVR risk calculator.
In the 14 years since the first transcatheter aortic valve replacement in 2002, devices and delivery methods have undergone several generations of improvement, but one facet of the procedure remained largely unchanged: When prospective patients underwent preprocedural assessment to gauge their risk level, the long-standing approach to quantify their disease severity and 30-day mortality risk was to run their clinical and demographic numbers through the risk calculator developed by the Society of Thoracic Surgeons.
Although determining a patient’s Society of Thoracic Surgeons (STS) risk score using a formula based on extensive experience performing surgical aortic valve replacement (SAVR) by open surgery made a lot of sense during an era when the preeminent question was how transcatheter aortic valve replacement (TAVR) compared with SAVR, it also carried the inherent limitation of estimating a patient’s risk when undergoing TAVR based on SAVR’s track record.
That limitation is now gone.
In December 2015, a team of cardiothoracic surgeons and interventional cardiologists assembled by the STS and the American College of Cardiology placed a new risk calculator online to estimate a prospective TAVR patient’s risk for dying in hospital following a TAVR procedure. The panel developed this risk calculator with data from nearly 14,000 U.S. TAVR patients enrolled in the STS/ACC Transcatheter Valve Replacement Registry during November 2011–February 2014 and then validated it with data from another nearly 7,000 U.S. TAVR patients who underwent their procedure during March-October 2014. This created the first mortality-risk calculator for TAVR patients based entirely on experience with such patients (JAMA Cardiology. 2016 Apr;1[1]:46-52).
In May 2016, a second, independent risk calculator will go live, also based exclusively on experience in TAVR patients, that estimates a patient’s risk for either dying or having a worsened or unimproved and poor quality of life during the 6 months following TAVR. This risk calculator, developed by a team led by researchers based at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., used data collected from more than 2,000 TAVR patients enrolled in the PARTNER trial or in the continued-access PARTNER registry (Circulation. 2014 June 24;129[25]:2682-90), and is offered to users by Health Outcomes Sciences, a Kansas City–based company that’s affiliated with Saint Luke’s.
Although use of these two TAVR-specific risk calculators during their early days of availability remains relatively light, TAVR experts see them as marking a new era in the workup of TAVR candidates.
“There is universal agreement that risk models must be developed based on the history of patients who actually received the treatment,” said Dr. Fred H. Edwards, the cardiothoracic surgeon at the University of Florida, Jacksonville, who led the team that developed the transcatheter valve therapy (TVT)-derived in-hospital mortality risk calculator. “Everyone realized that the STS score and the EuroScore [another operative-risk calculator historically used for prospective TAVR patients] were inadequate to extrapolate to TAVR patients.” But development had to wait until an adequately-sized experience with TAVR had accumulated. “We started the process [to develop the TVT risk calculator] when we reached about 10,000 patients” enrolled in the registry, after which it took “close to 2 years” to produce the finished product, Dr. Edwards said in an interview.
The TVT in-hospital mortality predictor gradually goes mainstream
“There is consensus that the new TVT calculator will be more reliable than the STS operative-risk model” for assessing patients being considered for TAVR, but it has not yet gained widespread use “because it is so new,” noted Dr. Edwards.
“It will take a while to incorporate it into routine practice, but I think it will be used quite a bit,” especially for “trickier and harder cases,” commented Dr. George Dangas, a professor of medicine at the Mount Sinai School of Medicine in New York and an interventional cardiologist who performs TAVR.
He also predicted that prospective patients and their families will become frequent users of the TVT in-hospital risk calculator. He sees the new risk tool as a complement to the STS risk score rather than something to replace it.
“Patients find it useful to receive an estimate of their surgical risk, and they’ll want to compare that” with their TAVR risk. “It helps to know both,” Dr. Dangas said in an interview. “Patients will likely compute it themselves.”
He foresees fairly quick integration of the new TVT score into heart team discussions as well. “The STS score will always be part of the discussion, but over time as people grow accustomed to the TVT score they will incorporate it as well. The [TAVR] community has to figure out how to use the two scores in combination.”
“There has been need for a risk calculator specific to TAVR since the patient population has only some overlap with the patients who underwent SAVR in the past,” said Dr. John D. Carroll, professor and director of interventional cardiology at the University of Colorado at Denver, Aurora, and a member of the TVT Registry panel that developed the calculator. “The STS score does not include variables that are frequently found in TAVR patients, such as liver disease, pulmonary hypertension, very-advance age, and frailty.”
A big plus for the new TVT risk calculator is its derivation from thousands of real-world, U.S. patients, Dr. Carroll noted. “It provides a patient-specific risk assessment rather than an assessment based on average patients from TAVR clinical trials.” Dr. Carroll added that since its introduction he has used the TVT risk calculator for some of his own patients being considered for TAVR.
The Saint Luke’s TAVR risk calculator
Although experts foresee an important role for profiling a patient’s predicted gain or loss in quality of life following TAVR as another element in the discussions between heart teams and patients, the risk calculator becoming available in May from Health Outcomes Sciences faces some significant issues, they said.
The Saint Luke’s Mid America team that developed the calculator used as their endpoint for a poor patient outcome 6 months after TAVR the combined rate of either death or two different measures of impaired quality of life: a Kansas City Cardiomyopathy Questionnaire–Overall Summary Scale (KCCQ-OS) score of less than 45 (measured on a scale of 0-100, where higher scores reflect better quality of life and function) or at least a 10-point reduction from baseline in a patient’s KCCQ-OS score.
By predicting a patient’s likelihood of emerging from TAVR with either a low or significantly worsened quality of life and function, this score is a “complement” to the TVT in-hospital mortality score, said Dr. Suzanne V. Arnold, a cardiologist at Saint Luke’s Mid America and one of the lead developers of this risk calculator.
“In-hospital mortality is an assessment of whether a patient will make it through the TAVR procedure. Our model is more about failure to recover after the procedure,” she explained in an interview. She and others also say that the Saint Luke’s calculator is a measure of probable futility when performing TAVR – that is, the likelihood that a patient will either not live long after the procedure or gain enough benefit from it to make performing the TAVR procedure an attractive option.
Dr. Arnold and her associates derived and validated the risk model using data collected from the “high risk” patients enrolled in the initial PARTNER trial and registry, so for the time being it remains primarily applicable to high-risk patients, who have classically been defined as patients with a STS risk score of 8% or greater (patients who have at least an 8% predicted risk of death during the 30 days following SAVR). She and her associates plan to see if they can validate the Saint Luke’s calculator in intermediate risk patients with aortic stenosis (usually defined as patients with a STS risk score of 4%-8%) with data collected in trials that enrolled these patients, such as PARTNER 2. At the ACC’s annual meeting in April in Chicago, Dr. Arnold presented a report in which she and her associates further validated their model using data collected from the high-risk patients enrolled in the CoreValve TAVR trial. This validation confirmed that the model worked “beautifully,” Dr. Arnold said.
The Saint Luke’s risk calculator uses six data entries: whether or not the patient has diabetes, atrial fibrillation, or requires oxygen support at home; whether the patient has no, mild, or moderate-to-severe dementia; the patient’s mean aortic gradient; and the patient’s score on the Kansas City Cardiomyopathy Questionnaire-12 (an abbreviated version of the 23-question KCCQ-OS scale). The result it produces – the likelihood of death or poor quality of life at 6 months – is “another piece of data to help the physician, surgeon, and patient make a decision” on whether to proceed with TAVR, she explained. “I would probably advise that if the predicted risk is high, the patient consider undergoing balloon aortic valvuloplasty” instead of TAVR “to see whether the patient has some recovery before committing to TAVR, but there are no hard and fast rules,” she acknowledged.
Dr. Arnold gave this recent case she had as an example of how running the Saint Luke’s risk calculator helped decision making:
A potential TAVR patient was a man in his 60s with end-stage renal disease, oxygen-dependent lung disease, and poor functional status. Applying the risk calculator to this patient “changed the conversation a surgeon and I had with the patient,” she said. “We let him know that TAVR might not make him feel better and it wouldn’t fix his kidneys or his lungs. Given his [relatively young] age, the patient still wanted to proceed, and we performed balloon aortic valvuloplasty, after which he seemed to do much better. He eventually underwent TAVR and did okay.”
This was a good application of the Saint Luke’s prediction model, Dr. Arnold said. As a consequence of the risk quantification, it provided that “the patient more fully understood the risk of the TAVR procedure” and had a better understanding of his prospects for recovery.
The heart teams at Saint Luke’s Mid America that perform TAVR began running this risk calculator on every high-risk patient evaluated in their valve clinic, about five patients each week, starting in mid-March 2016. The results are displayed in the patient’s chart next to the STS risk score.
By late April 2016, the staff at Health Outcomes Services, the commercial partner to Saint Luke’s that will offer the calculator online to the public, planned to have this risk calculator ready for routine use online by sometime in May. They said the company will make access to it available to any physician, surgeon, or other member of a heart team at no charge.*
Pros and cons of the Saint Luke’s risk calculator
While others applauded the creation of the Saint Luke’s risk calculator and the broader range of outcomes it predicts, they also questioned the generalizability of a risk assessment that is modeled against the selected patients enrolled in the PARTNER trial and registry, and some uncertainty on how to best use this information to inform clinical decision making.
“We certainly need to assess benefit as well as risk,” commented Dr. Edwards. The Kansas City–led group “is solidly on the right track,” and “I hope people will use their model,” he said.
In fact, the TVT Registry panel he heads is currently moving toward producing a similar expansion of their in-hospital mortality risk calculator that takes into account midterm changes in KCCQ status. Dr. Edwards said he hopes this expanded version of the TVT calculator might be ready in another year or two.
“KCCQ data are hard and time-consuming to collect, and clinicians who participate in the TVT Registry do not always do it,” he explained. “It’s an administrative burden” to make a KCCQ assessment both at baseline and at 6 or 12 month follow-up after TAVR.
“We’ve done a lot of education with registry participants to improve KCCQ data collection.” Dr. Edwards said he hopes that within another year this aspect of patient assessment will occur for about 90% of patients enrolled in the TVT Registry.
Dr. Edwards also highlighted the inherent limitations of applying the Saint Luke’s risk-assessment model, developed and validated in patients enrolled in the PARTNER and CoreValve trials and PARTNER registry, an aggregate of roughly 5,000 selected patients, to the more diverse patients seen in routine practice today and entered into the TVT Registry.
“The advantages of the TVT Registry are the huge numbers and the all-comers population,” he said. “You need to ask whether the randomized trial populations are truly representative.”
That’s a concern shared by Dr. Dangas, who also highlighted the challenges of assessing the risk a patient faces from noncardiovascular comorbidities and how that might affect a decision of whether or not to perform TAVR.
“These are elderly patients with many comorbidities. I’m not sure how well the noncardiac comorbidities were captured in the databases” for the PARTNER and CoreValve trials and registry, he said. “I’m not sure the noncardiac comorbidities were as well figured out” in those trials run several years ago as they might be today. “It’s not exactly what TAVR is about in 2016.” Despite his skepticism, Dr. Dangas acknowledged that a scoring formula that reliably captures and follows data collected by the KCCQ “would be useful.”
Another challenge is using a risk assessment tool that takes into account patient “frailty” as a way to judge whether TAVR might be “futile” for a specific patient, Dr. Dangas said.
“It’s a tough discussion to have prospectively with a patient. The question is valid, but how confident can we be prospectively, at the time of TAVR, that the procedure will be futile within a year?” He envisions that with more time and data, researchers will create a reliable risk assessment formula to gauge a patient’s midterm benefit from TAVR, but for now the Saint Luke’s scoring formula probably needs “more refinement,” he said.
“Patients need guidance by an individualized assessment that takes into account not only the risk they face from TAVR but also the benefit – the likelihood that they will not only be alive following TAVR but that they will gain improvement in functionality and in quality of life,” said Dr. Carroll. “This is especially important for patients who have other conditions that might prevent them from fully benefiting from TAVR, such as being on dialysis, having significant lung disease, or other conditions that could limit their ability to become more functional and feel better after TAVR.”
Although Health Outcomes Services is a for-profit company, it plans to make access to the Saint Luke’s risk calculator, which they call the “TAVI [transcatheter aortic valve implantation] Risk Calculator,” free to any health professional who applies for access, with a promised turnaround for access after application of about a day, said Joy Efron, the company’s vice president for commercialization. They do not plan to provide calculator access to patients. According to Ms. Efron, Health Outcomes Services decided to make their calculator available at no charge in the hope of potentially interesting some users in an upgraded, more extensive version of the calculator bundled with related products and features that are available as a package for a monthly subscription fee.
Dr. Edwards, Dr. Dangas, Dr. Carroll, and Dr. Arnold had no relevant disclosures. Saint Luke’s Mid America Heart Institute, where Dr. Arnold works, was an early investor in Health Outcomes Services, the company that is marketing the Saint Luke’s risk calculator.
On Twitter @mitchelzoler
*An earlier version of this article misstated the cost of the Saint Luke's TAVR risk calculator.
In the 14 years since the first transcatheter aortic valve replacement in 2002, devices and delivery methods have undergone several generations of improvement, but one facet of the procedure remained largely unchanged: When prospective patients underwent preprocedural assessment to gauge their risk level, the long-standing approach to quantify their disease severity and 30-day mortality risk was to run their clinical and demographic numbers through the risk calculator developed by the Society of Thoracic Surgeons.
Although determining a patient’s Society of Thoracic Surgeons (STS) risk score using a formula based on extensive experience performing surgical aortic valve replacement (SAVR) by open surgery made a lot of sense during an era when the preeminent question was how transcatheter aortic valve replacement (TAVR) compared with SAVR, it also carried the inherent limitation of estimating a patient’s risk when undergoing TAVR based on SAVR’s track record.
That limitation is now gone.
In December 2015, a team of cardiothoracic surgeons and interventional cardiologists assembled by the STS and the American College of Cardiology placed a new risk calculator online to estimate a prospective TAVR patient’s risk for dying in hospital following a TAVR procedure. The panel developed this risk calculator with data from nearly 14,000 U.S. TAVR patients enrolled in the STS/ACC Transcatheter Valve Replacement Registry during November 2011–February 2014 and then validated it with data from another nearly 7,000 U.S. TAVR patients who underwent their procedure during March-October 2014. This created the first mortality-risk calculator for TAVR patients based entirely on experience with such patients (JAMA Cardiology. 2016 Apr;1[1]:46-52).
In May 2016, a second, independent risk calculator will go live, also based exclusively on experience in TAVR patients, that estimates a patient’s risk for either dying or having a worsened or unimproved and poor quality of life during the 6 months following TAVR. This risk calculator, developed by a team led by researchers based at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., used data collected from more than 2,000 TAVR patients enrolled in the PARTNER trial or in the continued-access PARTNER registry (Circulation. 2014 June 24;129[25]:2682-90), and is offered to users by Health Outcomes Sciences, a Kansas City–based company that’s affiliated with Saint Luke’s.
Although use of these two TAVR-specific risk calculators during their early days of availability remains relatively light, TAVR experts see them as marking a new era in the workup of TAVR candidates.
“There is universal agreement that risk models must be developed based on the history of patients who actually received the treatment,” said Dr. Fred H. Edwards, the cardiothoracic surgeon at the University of Florida, Jacksonville, who led the team that developed the transcatheter valve therapy (TVT)-derived in-hospital mortality risk calculator. “Everyone realized that the STS score and the EuroScore [another operative-risk calculator historically used for prospective TAVR patients] were inadequate to extrapolate to TAVR patients.” But development had to wait until an adequately-sized experience with TAVR had accumulated. “We started the process [to develop the TVT risk calculator] when we reached about 10,000 patients” enrolled in the registry, after which it took “close to 2 years” to produce the finished product, Dr. Edwards said in an interview.
The TVT in-hospital mortality predictor gradually goes mainstream
“There is consensus that the new TVT calculator will be more reliable than the STS operative-risk model” for assessing patients being considered for TAVR, but it has not yet gained widespread use “because it is so new,” noted Dr. Edwards.
“It will take a while to incorporate it into routine practice, but I think it will be used quite a bit,” especially for “trickier and harder cases,” commented Dr. George Dangas, a professor of medicine at the Mount Sinai School of Medicine in New York and an interventional cardiologist who performs TAVR.
He also predicted that prospective patients and their families will become frequent users of the TVT in-hospital risk calculator. He sees the new risk tool as a complement to the STS risk score rather than something to replace it.
“Patients find it useful to receive an estimate of their surgical risk, and they’ll want to compare that” with their TAVR risk. “It helps to know both,” Dr. Dangas said in an interview. “Patients will likely compute it themselves.”
He foresees fairly quick integration of the new TVT score into heart team discussions as well. “The STS score will always be part of the discussion, but over time as people grow accustomed to the TVT score they will incorporate it as well. The [TAVR] community has to figure out how to use the two scores in combination.”
“There has been need for a risk calculator specific to TAVR since the patient population has only some overlap with the patients who underwent SAVR in the past,” said Dr. John D. Carroll, professor and director of interventional cardiology at the University of Colorado at Denver, Aurora, and a member of the TVT Registry panel that developed the calculator. “The STS score does not include variables that are frequently found in TAVR patients, such as liver disease, pulmonary hypertension, very-advance age, and frailty.”
A big plus for the new TVT risk calculator is its derivation from thousands of real-world, U.S. patients, Dr. Carroll noted. “It provides a patient-specific risk assessment rather than an assessment based on average patients from TAVR clinical trials.” Dr. Carroll added that since its introduction he has used the TVT risk calculator for some of his own patients being considered for TAVR.
The Saint Luke’s TAVR risk calculator
Although experts foresee an important role for profiling a patient’s predicted gain or loss in quality of life following TAVR as another element in the discussions between heart teams and patients, the risk calculator becoming available in May from Health Outcomes Sciences faces some significant issues, they said.
The Saint Luke’s Mid America team that developed the calculator used as their endpoint for a poor patient outcome 6 months after TAVR the combined rate of either death or two different measures of impaired quality of life: a Kansas City Cardiomyopathy Questionnaire–Overall Summary Scale (KCCQ-OS) score of less than 45 (measured on a scale of 0-100, where higher scores reflect better quality of life and function) or at least a 10-point reduction from baseline in a patient’s KCCQ-OS score.
By predicting a patient’s likelihood of emerging from TAVR with either a low or significantly worsened quality of life and function, this score is a “complement” to the TVT in-hospital mortality score, said Dr. Suzanne V. Arnold, a cardiologist at Saint Luke’s Mid America and one of the lead developers of this risk calculator.
“In-hospital mortality is an assessment of whether a patient will make it through the TAVR procedure. Our model is more about failure to recover after the procedure,” she explained in an interview. She and others also say that the Saint Luke’s calculator is a measure of probable futility when performing TAVR – that is, the likelihood that a patient will either not live long after the procedure or gain enough benefit from it to make performing the TAVR procedure an attractive option.
Dr. Arnold and her associates derived and validated the risk model using data collected from the “high risk” patients enrolled in the initial PARTNER trial and registry, so for the time being it remains primarily applicable to high-risk patients, who have classically been defined as patients with a STS risk score of 8% or greater (patients who have at least an 8% predicted risk of death during the 30 days following SAVR). She and her associates plan to see if they can validate the Saint Luke’s calculator in intermediate risk patients with aortic stenosis (usually defined as patients with a STS risk score of 4%-8%) with data collected in trials that enrolled these patients, such as PARTNER 2. At the ACC’s annual meeting in April in Chicago, Dr. Arnold presented a report in which she and her associates further validated their model using data collected from the high-risk patients enrolled in the CoreValve TAVR trial. This validation confirmed that the model worked “beautifully,” Dr. Arnold said.
The Saint Luke’s risk calculator uses six data entries: whether or not the patient has diabetes, atrial fibrillation, or requires oxygen support at home; whether the patient has no, mild, or moderate-to-severe dementia; the patient’s mean aortic gradient; and the patient’s score on the Kansas City Cardiomyopathy Questionnaire-12 (an abbreviated version of the 23-question KCCQ-OS scale). The result it produces – the likelihood of death or poor quality of life at 6 months – is “another piece of data to help the physician, surgeon, and patient make a decision” on whether to proceed with TAVR, she explained. “I would probably advise that if the predicted risk is high, the patient consider undergoing balloon aortic valvuloplasty” instead of TAVR “to see whether the patient has some recovery before committing to TAVR, but there are no hard and fast rules,” she acknowledged.
Dr. Arnold gave this recent case she had as an example of how running the Saint Luke’s risk calculator helped decision making:
A potential TAVR patient was a man in his 60s with end-stage renal disease, oxygen-dependent lung disease, and poor functional status. Applying the risk calculator to this patient “changed the conversation a surgeon and I had with the patient,” she said. “We let him know that TAVR might not make him feel better and it wouldn’t fix his kidneys or his lungs. Given his [relatively young] age, the patient still wanted to proceed, and we performed balloon aortic valvuloplasty, after which he seemed to do much better. He eventually underwent TAVR and did okay.”
This was a good application of the Saint Luke’s prediction model, Dr. Arnold said. As a consequence of the risk quantification, it provided that “the patient more fully understood the risk of the TAVR procedure” and had a better understanding of his prospects for recovery.
The heart teams at Saint Luke’s Mid America that perform TAVR began running this risk calculator on every high-risk patient evaluated in their valve clinic, about five patients each week, starting in mid-March 2016. The results are displayed in the patient’s chart next to the STS risk score.
By late April 2016, the staff at Health Outcomes Services, the commercial partner to Saint Luke’s that will offer the calculator online to the public, planned to have this risk calculator ready for routine use online by sometime in May. They said the company will make access to it available to any physician, surgeon, or other member of a heart team at no charge.*
Pros and cons of the Saint Luke’s risk calculator
While others applauded the creation of the Saint Luke’s risk calculator and the broader range of outcomes it predicts, they also questioned the generalizability of a risk assessment that is modeled against the selected patients enrolled in the PARTNER trial and registry, and some uncertainty on how to best use this information to inform clinical decision making.
“We certainly need to assess benefit as well as risk,” commented Dr. Edwards. The Kansas City–led group “is solidly on the right track,” and “I hope people will use their model,” he said.
In fact, the TVT Registry panel he heads is currently moving toward producing a similar expansion of their in-hospital mortality risk calculator that takes into account midterm changes in KCCQ status. Dr. Edwards said he hopes this expanded version of the TVT calculator might be ready in another year or two.
“KCCQ data are hard and time-consuming to collect, and clinicians who participate in the TVT Registry do not always do it,” he explained. “It’s an administrative burden” to make a KCCQ assessment both at baseline and at 6 or 12 month follow-up after TAVR.
“We’ve done a lot of education with registry participants to improve KCCQ data collection.” Dr. Edwards said he hopes that within another year this aspect of patient assessment will occur for about 90% of patients enrolled in the TVT Registry.
Dr. Edwards also highlighted the inherent limitations of applying the Saint Luke’s risk-assessment model, developed and validated in patients enrolled in the PARTNER and CoreValve trials and PARTNER registry, an aggregate of roughly 5,000 selected patients, to the more diverse patients seen in routine practice today and entered into the TVT Registry.
“The advantages of the TVT Registry are the huge numbers and the all-comers population,” he said. “You need to ask whether the randomized trial populations are truly representative.”
That’s a concern shared by Dr. Dangas, who also highlighted the challenges of assessing the risk a patient faces from noncardiovascular comorbidities and how that might affect a decision of whether or not to perform TAVR.
“These are elderly patients with many comorbidities. I’m not sure how well the noncardiac comorbidities were captured in the databases” for the PARTNER and CoreValve trials and registry, he said. “I’m not sure the noncardiac comorbidities were as well figured out” in those trials run several years ago as they might be today. “It’s not exactly what TAVR is about in 2016.” Despite his skepticism, Dr. Dangas acknowledged that a scoring formula that reliably captures and follows data collected by the KCCQ “would be useful.”
Another challenge is using a risk assessment tool that takes into account patient “frailty” as a way to judge whether TAVR might be “futile” for a specific patient, Dr. Dangas said.
“It’s a tough discussion to have prospectively with a patient. The question is valid, but how confident can we be prospectively, at the time of TAVR, that the procedure will be futile within a year?” He envisions that with more time and data, researchers will create a reliable risk assessment formula to gauge a patient’s midterm benefit from TAVR, but for now the Saint Luke’s scoring formula probably needs “more refinement,” he said.
“Patients need guidance by an individualized assessment that takes into account not only the risk they face from TAVR but also the benefit – the likelihood that they will not only be alive following TAVR but that they will gain improvement in functionality and in quality of life,” said Dr. Carroll. “This is especially important for patients who have other conditions that might prevent them from fully benefiting from TAVR, such as being on dialysis, having significant lung disease, or other conditions that could limit their ability to become more functional and feel better after TAVR.”
Although Health Outcomes Services is a for-profit company, it plans to make access to the Saint Luke’s risk calculator, which they call the “TAVI [transcatheter aortic valve implantation] Risk Calculator,” free to any health professional who applies for access, with a promised turnaround for access after application of about a day, said Joy Efron, the company’s vice president for commercialization. They do not plan to provide calculator access to patients. According to Ms. Efron, Health Outcomes Services decided to make their calculator available at no charge in the hope of potentially interesting some users in an upgraded, more extensive version of the calculator bundled with related products and features that are available as a package for a monthly subscription fee.
Dr. Edwards, Dr. Dangas, Dr. Carroll, and Dr. Arnold had no relevant disclosures. Saint Luke’s Mid America Heart Institute, where Dr. Arnold works, was an early investor in Health Outcomes Services, the company that is marketing the Saint Luke’s risk calculator.
On Twitter @mitchelzoler
*An earlier version of this article misstated the cost of the Saint Luke's TAVR risk calculator.
Target Fortification of Breast Milk Boosts Preemie Growth
BALTIMORE – For a premature infant, breast milk straight from Mom or a donor may not be the ideal meal.
The problem is that breast milk is often unbalanced in its content of protein, fat, and carbohydrates, and for a premature neonate fed by a nasogastric tube, unfortified breast milk can provide too little of one nutrient or too much of another. Conventional fortification of breast milk adds a standardized cocktail of nutrients that doesn’t provide an ideal balance for optimal growth.
Frequent analysis of breast milk’s nutrient content and target fortification to tweak the milk to a more ideal nutrient balance may be a way around this problem, and results from a single-center, randomized trial with 85 premature infants showed that this approach led to significantly better infant weights when measured at 36 weeks postmenstrual age, Dr. Christoph Fusch reported at the annual meeting of the Pediatric Academic Societies.
Target fortification of breast milk resulted in an average weight at 36 weeks postmenstrual age of 2,510 g among 42 infants in the intervention group, compared with an average weight of 2,280 g among 43 control infants who received breast milk that underwent routine fortification with a commercial product – a statistically significant difference for the study’s primary endpoint, said Dr. Fusch, professor of pediatrics at McMaster University and director of the neonatal intensive care unit at McMaster Children’s Hospital, both in Hamilton, Ont.
Baseline weights in the two groups of premature infants, who were born at an average of 27 weeks’ gestation and began the study at an average age of about 30 weeks’ postmenstrual age, were 970 g in the controls and 960 g in the infants who received target fortification.
The benefit from target fortification was even more dramatic in the 50% of infants fed on breast milk with the lowest protein content. In this subgroup, the 21 infants on target fortification weighed an average of 2,540 g at 36 weeks postmenstrual age, compared with an average weight of 2,170 g among 21 control infants.
“If you use standard fortification you never get [the nutrients] right. Too many nutrients will be outside [the ideal range] and those babies have a high risk of not growing,” Dr. Fusch noted in an interview.
One of the key steps in the study was measuring the protein, fat, and carbohydrate content of the breast milk that each infant received 3 days a week and using those data to guide fortification. Assessment of each breast milk specimen takes about 2 minutes, after which a technician adds the required levels of freshly prepared nutrient supplements to produce a final protein content of 3 g/dL, fat at 4.3 g/dL, and carbohydrate at 8.5 g/dL. The researchers set these levels based on an assumed daily intake of 150 mL/kg of fortified breast milk.
Dr. Fusch and his associates plan additional analyses of the data they collected in this study to look at the impact of target fortification on infant length and head circumference, metabolic responses, body composition, and neurodevelopment out to 18 months of age. They also have launched a larger, multicenter study with a similar design at 10 sites in Europe and 8 sites in North America.
The infants who stand to gain the most from target fortification are those fed donor breast milk, an increasingly popular option when breast milk from the infant’s mother is not available, but also a flawed option because this milk is usually low in protein, said Dr. Fusch, who also holds the Jack Sinclair Chair in Neonatology at the university. Target fortification is not an issue for term infants who feed normally because they usually cry to demand more milk when they lack specific nutrients. Premature infants are much more vulnerable when fed by a nasogastric tube because they will become sated simply by milk volume and then stop eating, even when they ingest an unbalanced nutrient supply.
BALTIMORE – For a premature infant, breast milk straight from Mom or a donor may not be the ideal meal.
The problem is that breast milk is often unbalanced in its content of protein, fat, and carbohydrates, and for a premature neonate fed by a nasogastric tube, unfortified breast milk can provide too little of one nutrient or too much of another. Conventional fortification of breast milk adds a standardized cocktail of nutrients that doesn’t provide an ideal balance for optimal growth.
Frequent analysis of breast milk’s nutrient content and target fortification to tweak the milk to a more ideal nutrient balance may be a way around this problem, and results from a single-center, randomized trial with 85 premature infants showed that this approach led to significantly better infant weights when measured at 36 weeks postmenstrual age, Dr. Christoph Fusch reported at the annual meeting of the Pediatric Academic Societies.
Target fortification of breast milk resulted in an average weight at 36 weeks postmenstrual age of 2,510 g among 42 infants in the intervention group, compared with an average weight of 2,280 g among 43 control infants who received breast milk that underwent routine fortification with a commercial product – a statistically significant difference for the study’s primary endpoint, said Dr. Fusch, professor of pediatrics at McMaster University and director of the neonatal intensive care unit at McMaster Children’s Hospital, both in Hamilton, Ont.
Baseline weights in the two groups of premature infants, who were born at an average of 27 weeks’ gestation and began the study at an average age of about 30 weeks’ postmenstrual age, were 970 g in the controls and 960 g in the infants who received target fortification.
The benefit from target fortification was even more dramatic in the 50% of infants fed on breast milk with the lowest protein content. In this subgroup, the 21 infants on target fortification weighed an average of 2,540 g at 36 weeks postmenstrual age, compared with an average weight of 2,170 g among 21 control infants.
“If you use standard fortification you never get [the nutrients] right. Too many nutrients will be outside [the ideal range] and those babies have a high risk of not growing,” Dr. Fusch noted in an interview.
One of the key steps in the study was measuring the protein, fat, and carbohydrate content of the breast milk that each infant received 3 days a week and using those data to guide fortification. Assessment of each breast milk specimen takes about 2 minutes, after which a technician adds the required levels of freshly prepared nutrient supplements to produce a final protein content of 3 g/dL, fat at 4.3 g/dL, and carbohydrate at 8.5 g/dL. The researchers set these levels based on an assumed daily intake of 150 mL/kg of fortified breast milk.
Dr. Fusch and his associates plan additional analyses of the data they collected in this study to look at the impact of target fortification on infant length and head circumference, metabolic responses, body composition, and neurodevelopment out to 18 months of age. They also have launched a larger, multicenter study with a similar design at 10 sites in Europe and 8 sites in North America.
The infants who stand to gain the most from target fortification are those fed donor breast milk, an increasingly popular option when breast milk from the infant’s mother is not available, but also a flawed option because this milk is usually low in protein, said Dr. Fusch, who also holds the Jack Sinclair Chair in Neonatology at the university. Target fortification is not an issue for term infants who feed normally because they usually cry to demand more milk when they lack specific nutrients. Premature infants are much more vulnerable when fed by a nasogastric tube because they will become sated simply by milk volume and then stop eating, even when they ingest an unbalanced nutrient supply.
BALTIMORE – For a premature infant, breast milk straight from Mom or a donor may not be the ideal meal.
The problem is that breast milk is often unbalanced in its content of protein, fat, and carbohydrates, and for a premature neonate fed by a nasogastric tube, unfortified breast milk can provide too little of one nutrient or too much of another. Conventional fortification of breast milk adds a standardized cocktail of nutrients that doesn’t provide an ideal balance for optimal growth.
Frequent analysis of breast milk’s nutrient content and target fortification to tweak the milk to a more ideal nutrient balance may be a way around this problem, and results from a single-center, randomized trial with 85 premature infants showed that this approach led to significantly better infant weights when measured at 36 weeks postmenstrual age, Dr. Christoph Fusch reported at the annual meeting of the Pediatric Academic Societies.
Target fortification of breast milk resulted in an average weight at 36 weeks postmenstrual age of 2,510 g among 42 infants in the intervention group, compared with an average weight of 2,280 g among 43 control infants who received breast milk that underwent routine fortification with a commercial product – a statistically significant difference for the study’s primary endpoint, said Dr. Fusch, professor of pediatrics at McMaster University and director of the neonatal intensive care unit at McMaster Children’s Hospital, both in Hamilton, Ont.
Baseline weights in the two groups of premature infants, who were born at an average of 27 weeks’ gestation and began the study at an average age of about 30 weeks’ postmenstrual age, were 970 g in the controls and 960 g in the infants who received target fortification.
The benefit from target fortification was even more dramatic in the 50% of infants fed on breast milk with the lowest protein content. In this subgroup, the 21 infants on target fortification weighed an average of 2,540 g at 36 weeks postmenstrual age, compared with an average weight of 2,170 g among 21 control infants.
“If you use standard fortification you never get [the nutrients] right. Too many nutrients will be outside [the ideal range] and those babies have a high risk of not growing,” Dr. Fusch noted in an interview.
One of the key steps in the study was measuring the protein, fat, and carbohydrate content of the breast milk that each infant received 3 days a week and using those data to guide fortification. Assessment of each breast milk specimen takes about 2 minutes, after which a technician adds the required levels of freshly prepared nutrient supplements to produce a final protein content of 3 g/dL, fat at 4.3 g/dL, and carbohydrate at 8.5 g/dL. The researchers set these levels based on an assumed daily intake of 150 mL/kg of fortified breast milk.
Dr. Fusch and his associates plan additional analyses of the data they collected in this study to look at the impact of target fortification on infant length and head circumference, metabolic responses, body composition, and neurodevelopment out to 18 months of age. They also have launched a larger, multicenter study with a similar design at 10 sites in Europe and 8 sites in North America.
The infants who stand to gain the most from target fortification are those fed donor breast milk, an increasingly popular option when breast milk from the infant’s mother is not available, but also a flawed option because this milk is usually low in protein, said Dr. Fusch, who also holds the Jack Sinclair Chair in Neonatology at the university. Target fortification is not an issue for term infants who feed normally because they usually cry to demand more milk when they lack specific nutrients. Premature infants are much more vulnerable when fed by a nasogastric tube because they will become sated simply by milk volume and then stop eating, even when they ingest an unbalanced nutrient supply.
AT THE PAS ANNUAL MEETING
Target fortification of breast milk boosts preemie growth
BALTIMORE – For a premature infant, breast milk straight from Mom or a donor may not be the ideal meal.
The problem is that breast milk is often unbalanced in its content of protein, fat, and carbohydrates, and for a premature neonate fed by a nasogastric tube, unfortified breast milk can provide too little of one nutrient or too much of another. Conventional fortification of breast milk adds a standardized cocktail of nutrients that doesn’t provide an ideal balance for optimal growth.
Frequent analysis of breast milk’s nutrient content and target fortification to tweak the milk to a more ideal nutrient balance may be a way around this problem, and results from a single-center, randomized trial with 85 premature infants showed that this approach led to significantly better infant weights when measured at 36 weeks postmenstrual age, Dr. Christoph Fusch reported at the annual meeting of the Pediatric Academic Societies.
Target fortification of breast milk resulted in an average weight at 36 weeks postmenstrual age of 2,510 g among 42 infants in the intervention group, compared with an average weight of 2,280 g among 43 control infants who received breast milk that underwent routine fortification with a commercial product – a statistically significant difference for the study’s primary endpoint, said Dr. Fusch, professor of pediatrics at McMaster University and director of the neonatal intensive care unit at McMaster Children’s Hospital, both in Hamilton, Ont.
Baseline weights in the two groups of premature infants, who were born at an average of 27 weeks’ gestation and began the study at an average age of about 30 weeks’ postmenstrual age, were 970 g in the controls and 960 g in the infants who received target fortification.
The benefit from target fortification was even more dramatic in the 50% of infants fed on breast milk with the lowest protein content. In this subgroup, the 21 infants on target fortification weighed an average of 2,540 g at 36 weeks postmenstrual age, compared with an average weight of 2,170 g among 21 control infants.
“If you use standard fortification you never get [the nutrients] right. Too many nutrients will be outside [the ideal range] and those babies have a high risk of not growing,” Dr. Fusch noted in an interview.
One of the key steps in the study was measuring the protein, fat, and carbohydrate content of the breast milk that each infant received 3 days a week and using those data to guide fortification. Assessment of each breast milk specimen takes about 2 minutes, after which a technician adds the required levels of freshly prepared nutrient supplements to produce a final protein content of 3 g/dL, fat at 4.3 g/dL, and carbohydrate at 8.5 g/dL. The researchers set these levels based on an assumed daily intake of 150 mL/kg of fortified breast milk.
Dr. Fusch and his associates plan additional analyses of the data they collected in this study to look at the impact of target fortification on infant length and head circumference, metabolic responses, body composition, and neurodevelopment out to 18 months of age. They also have launched a larger, multicenter study with a similar design at 10 sites in Europe and 8 sites in North America.
The infants who stand to gain the most from target fortification are those fed donor breast milk, an increasingly popular option when breast milk from the infant’s mother is not available, but also a flawed option because this milk is usually low in protein, said Dr. Fusch, who also holds the Jack Sinclair Chair in Neonatology at the university. Target fortification is not an issue for term infants who feed normally because they usually cry to demand more milk when they lack specific nutrients. Premature infants are much more vulnerable when fed by a nasogastric tube because they will become sated simply by milk volume and then stop eating, even when they ingest an unbalanced nutrient supply.
On Twitter @mitchelzoler
BALTIMORE – For a premature infant, breast milk straight from Mom or a donor may not be the ideal meal.
The problem is that breast milk is often unbalanced in its content of protein, fat, and carbohydrates, and for a premature neonate fed by a nasogastric tube, unfortified breast milk can provide too little of one nutrient or too much of another. Conventional fortification of breast milk adds a standardized cocktail of nutrients that doesn’t provide an ideal balance for optimal growth.
Frequent analysis of breast milk’s nutrient content and target fortification to tweak the milk to a more ideal nutrient balance may be a way around this problem, and results from a single-center, randomized trial with 85 premature infants showed that this approach led to significantly better infant weights when measured at 36 weeks postmenstrual age, Dr. Christoph Fusch reported at the annual meeting of the Pediatric Academic Societies.
Target fortification of breast milk resulted in an average weight at 36 weeks postmenstrual age of 2,510 g among 42 infants in the intervention group, compared with an average weight of 2,280 g among 43 control infants who received breast milk that underwent routine fortification with a commercial product – a statistically significant difference for the study’s primary endpoint, said Dr. Fusch, professor of pediatrics at McMaster University and director of the neonatal intensive care unit at McMaster Children’s Hospital, both in Hamilton, Ont.
Baseline weights in the two groups of premature infants, who were born at an average of 27 weeks’ gestation and began the study at an average age of about 30 weeks’ postmenstrual age, were 970 g in the controls and 960 g in the infants who received target fortification.
The benefit from target fortification was even more dramatic in the 50% of infants fed on breast milk with the lowest protein content. In this subgroup, the 21 infants on target fortification weighed an average of 2,540 g at 36 weeks postmenstrual age, compared with an average weight of 2,170 g among 21 control infants.
“If you use standard fortification you never get [the nutrients] right. Too many nutrients will be outside [the ideal range] and those babies have a high risk of not growing,” Dr. Fusch noted in an interview.
One of the key steps in the study was measuring the protein, fat, and carbohydrate content of the breast milk that each infant received 3 days a week and using those data to guide fortification. Assessment of each breast milk specimen takes about 2 minutes, after which a technician adds the required levels of freshly prepared nutrient supplements to produce a final protein content of 3 g/dL, fat at 4.3 g/dL, and carbohydrate at 8.5 g/dL. The researchers set these levels based on an assumed daily intake of 150 mL/kg of fortified breast milk.
Dr. Fusch and his associates plan additional analyses of the data they collected in this study to look at the impact of target fortification on infant length and head circumference, metabolic responses, body composition, and neurodevelopment out to 18 months of age. They also have launched a larger, multicenter study with a similar design at 10 sites in Europe and 8 sites in North America.
The infants who stand to gain the most from target fortification are those fed donor breast milk, an increasingly popular option when breast milk from the infant’s mother is not available, but also a flawed option because this milk is usually low in protein, said Dr. Fusch, who also holds the Jack Sinclair Chair in Neonatology at the university. Target fortification is not an issue for term infants who feed normally because they usually cry to demand more milk when they lack specific nutrients. Premature infants are much more vulnerable when fed by a nasogastric tube because they will become sated simply by milk volume and then stop eating, even when they ingest an unbalanced nutrient supply.
On Twitter @mitchelzoler
BALTIMORE – For a premature infant, breast milk straight from Mom or a donor may not be the ideal meal.
The problem is that breast milk is often unbalanced in its content of protein, fat, and carbohydrates, and for a premature neonate fed by a nasogastric tube, unfortified breast milk can provide too little of one nutrient or too much of another. Conventional fortification of breast milk adds a standardized cocktail of nutrients that doesn’t provide an ideal balance for optimal growth.
Frequent analysis of breast milk’s nutrient content and target fortification to tweak the milk to a more ideal nutrient balance may be a way around this problem, and results from a single-center, randomized trial with 85 premature infants showed that this approach led to significantly better infant weights when measured at 36 weeks postmenstrual age, Dr. Christoph Fusch reported at the annual meeting of the Pediatric Academic Societies.
Target fortification of breast milk resulted in an average weight at 36 weeks postmenstrual age of 2,510 g among 42 infants in the intervention group, compared with an average weight of 2,280 g among 43 control infants who received breast milk that underwent routine fortification with a commercial product – a statistically significant difference for the study’s primary endpoint, said Dr. Fusch, professor of pediatrics at McMaster University and director of the neonatal intensive care unit at McMaster Children’s Hospital, both in Hamilton, Ont.
Baseline weights in the two groups of premature infants, who were born at an average of 27 weeks’ gestation and began the study at an average age of about 30 weeks’ postmenstrual age, were 970 g in the controls and 960 g in the infants who received target fortification.
The benefit from target fortification was even more dramatic in the 50% of infants fed on breast milk with the lowest protein content. In this subgroup, the 21 infants on target fortification weighed an average of 2,540 g at 36 weeks postmenstrual age, compared with an average weight of 2,170 g among 21 control infants.
“If you use standard fortification you never get [the nutrients] right. Too many nutrients will be outside [the ideal range] and those babies have a high risk of not growing,” Dr. Fusch noted in an interview.
One of the key steps in the study was measuring the protein, fat, and carbohydrate content of the breast milk that each infant received 3 days a week and using those data to guide fortification. Assessment of each breast milk specimen takes about 2 minutes, after which a technician adds the required levels of freshly prepared nutrient supplements to produce a final protein content of 3 g/dL, fat at 4.3 g/dL, and carbohydrate at 8.5 g/dL. The researchers set these levels based on an assumed daily intake of 150 mL/kg of fortified breast milk.
Dr. Fusch and his associates plan additional analyses of the data they collected in this study to look at the impact of target fortification on infant length and head circumference, metabolic responses, body composition, and neurodevelopment out to 18 months of age. They also have launched a larger, multicenter study with a similar design at 10 sites in Europe and 8 sites in North America.
The infants who stand to gain the most from target fortification are those fed donor breast milk, an increasingly popular option when breast milk from the infant’s mother is not available, but also a flawed option because this milk is usually low in protein, said Dr. Fusch, who also holds the Jack Sinclair Chair in Neonatology at the university. Target fortification is not an issue for term infants who feed normally because they usually cry to demand more milk when they lack specific nutrients. Premature infants are much more vulnerable when fed by a nasogastric tube because they will become sated simply by milk volume and then stop eating, even when they ingest an unbalanced nutrient supply.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Premature infants fed breast milk that had undergone target fortification showed significantly better growth to 36 weeks postmenstrual age, compared with control infants fed with conventionally fortified breast milk.
Major finding: Average weight after intervention was 2,510 g in infants fed target-fortified breast milk and 2,280 g in controls.
Data source: Single-center, randomized controlled study with 85 premature infants.
Disclosures: Dr. Fusch had no disclosures.
VIDEO: Preemies on early caffeine not benefited, possibly harmed
BALTIMORE – Early initiation of caffeine treatment in premature neonates on mechanical ventilation did not cut the time to when these babies could successfully wean off the ventilator, according to findings of a single-center, randomized controlled study of 83 children.
The results also showed an “unexpected” trend toward increased mortality among the neonates who received early caffeine treatment, Dr. Cynthia M. Amaro reported at the annual meeting of the Pediatric Academic Societies. This signal of elevated mortality with caffeine treatment prompted the study’s data and safety monitoring board to prematurely stop the trial, limiting enrollment to just 75% of the number originally planned in the study’s design, thereby raising questions about the reliability of the primary-endpoint finding that early caffeine treatment did not result in the benefit of a reduced time to extubation.
Dr. Amaro said that she and her associates ran the study to address what had emerged as a significant area of doubt in routine U.S. practice on how to best use caffeine treatment in this neonatal population following publication of findings from the landmark Caffeine for Apnea of Prematurity (CAP) Trial (N Engl J Med. 2006 May 18;354[20]:2112-21). Results from the CAP Trial had shown in nearly 2,000 randomized, premature infants that treatment with caffeine led to significantly fewer episodes of bronchopulmonary dysplasia as well as quicker time to extubation of mechanical ventilation. Caffeine or other methylxanthines stimulate an infant’s respiratory center to allow faster extubation.
Ever since that publication a decade ago, “clinicians have been using caffeine earlier and more liberally, without really good data to support its early use in mechanically-ventilated preterm babies,” explained Dr. Amaro, a neonatologist at the University of Miami and Holtz Children’s Hospital in Miami.
Based on the new findings from the study she reported, “we are now not routinely initiating caffeine in mechanically ventilated preterm babies and just using caffeine immediately before extubation to treat apnea of prematurity. This returns caffeine treatment to the way it was used in the CAP Trial,” she said. “Further studies are needed before we can say what is best for early treatment of these preterm babies,” Dr. Amaro said in a video interview.
Her report led to a flurry of comments during the question period, with several pediatricians voicing concern about the reliability of results from a study that followed only 83 patients because of its premature termination.
“The data and safety monitoring board’s decision is a big issue,” said Dr. Carl E. Hunt, a pediatrician at the Uniformed Services University of the Health Sciences in Bethesda, Md. “There is a literature that shows results of studies can be very different when they stop early. It’s unfortunate because we don’t have other prospective data, and it may now be hard to do a large randomized, controlled trial” of early caffeine treatment, Dr. Hunt said.
While Dr. Amaro conceded that premature termination limited her study’s size, she also asserted that her analyses confirmed the validity of the finding of no benefit from early caffeine treatment. “We projected to full enrollment, and there still was no difference in the time to first successful extubation,” she said.
Her study enrolled preterm infants during January 2013–December 2015 born at 23-30 weeks’ gestation who required mechanical ventilation during their first 5 days. Randomization assigned 41 infants to receive a 20-mg/kg bolus of caffeine, followed by a maintenance dosage of 5 mg/kg that continued until extubation, while 42 patients received placebo and did not get caffeine until just before attempted extubation. The bolus and maintenance caffeine dosages tested were identical to those used in the CAP Trial.
The researchers defined successful extubation as keeping a child off restart of mechanical ventilation for more than 24 hours. The average gestational age of the enrolled neonates was 26 weeks, their average weight was 700 g, and intubation started an average of 3 hours after delivery.
The study’s primary endpoint, age at first successful extubation, was an average of 24 days among the neonates treated with caffeine and 20 days in those on placebo, Dr. Amaro reported. Mortality occurred at an average of 30 days after delivery in the caffeine recipients and after an average of 10 days in the controls. The incidence of death was 22% in those on early caffeine and 12% among those in the placebo group, an excess of four deaths in the intervention arm that was not statically significant.
A recent review of more than 29,000 matched very-low-birth-weight infants managed in routine practice showed that neonates who received early caffeine had an adjusted mortality risk that was 23% higher than that of matched infants not receiving early caffeine, Dr. Amaro noted (J Pediatrics. 2014 May;164[5]:992-8).
The incidence of bronchopulmonary dysplasia also did not show a statistically significant difference between the two study arms, 46% among those on early caffeine and 53% in the placebo group. Patients on early caffeine also had higher rates of necrotizing enterocolitis, more episodes of necrotizing enterocolitis requiring surgery, and more intraventricular hemorrhages, but none of these differences reached statistical significance.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Clinicians need to be very cautious starting caffeine to treat premature neonates on mechanical ventilation with the goal of reducing the time to extubation. The findings from Dr. Amaro and her associates show that we do not really know whether starting caffeine treatment early is the right thing to do.
Because their study stopped sooner than planned, I don’t believe the number of enrolled patients was large enough to provide clear guidance on when to start treatment with caffeine or another methylxanthine. We still don’t know the answer. In addition, the suggestion of excess mortality with caffeine treatment gives us no reassurance that caffeine is safe in this setting. However, as was clear in the questions and comments from some members of the audience that heard this report, some people continue to believe that early treatment with caffeine of premature infants on mechanical ventilation is appropriate.
As a result of the equivocal results in Dr. Amaro’s study, the best option is probably to go back to using the protocol tested and shown safe and effective in the 2006 report from the Caffeine for Apnea of Prematurity Trial (N Engl J Med. 2006 May 18;354[20]:2112-21). Ideally, researchers will soon run a large, randomized trial that can better address the questions that Dr. Amaro and her associates attempted to answer with their study.
Dr. Clifford W. Bogue is professor of pediatrics at Yale University, New Haven, Conn., and chaired the session where Dr. Amaro presented her report. He had no relevant disclosures. He made these comments in an interview.
Clinicians need to be very cautious starting caffeine to treat premature neonates on mechanical ventilation with the goal of reducing the time to extubation. The findings from Dr. Amaro and her associates show that we do not really know whether starting caffeine treatment early is the right thing to do.
Because their study stopped sooner than planned, I don’t believe the number of enrolled patients was large enough to provide clear guidance on when to start treatment with caffeine or another methylxanthine. We still don’t know the answer. In addition, the suggestion of excess mortality with caffeine treatment gives us no reassurance that caffeine is safe in this setting. However, as was clear in the questions and comments from some members of the audience that heard this report, some people continue to believe that early treatment with caffeine of premature infants on mechanical ventilation is appropriate.
As a result of the equivocal results in Dr. Amaro’s study, the best option is probably to go back to using the protocol tested and shown safe and effective in the 2006 report from the Caffeine for Apnea of Prematurity Trial (N Engl J Med. 2006 May 18;354[20]:2112-21). Ideally, researchers will soon run a large, randomized trial that can better address the questions that Dr. Amaro and her associates attempted to answer with their study.
Dr. Clifford W. Bogue is professor of pediatrics at Yale University, New Haven, Conn., and chaired the session where Dr. Amaro presented her report. He had no relevant disclosures. He made these comments in an interview.
Clinicians need to be very cautious starting caffeine to treat premature neonates on mechanical ventilation with the goal of reducing the time to extubation. The findings from Dr. Amaro and her associates show that we do not really know whether starting caffeine treatment early is the right thing to do.
Because their study stopped sooner than planned, I don’t believe the number of enrolled patients was large enough to provide clear guidance on when to start treatment with caffeine or another methylxanthine. We still don’t know the answer. In addition, the suggestion of excess mortality with caffeine treatment gives us no reassurance that caffeine is safe in this setting. However, as was clear in the questions and comments from some members of the audience that heard this report, some people continue to believe that early treatment with caffeine of premature infants on mechanical ventilation is appropriate.
As a result of the equivocal results in Dr. Amaro’s study, the best option is probably to go back to using the protocol tested and shown safe and effective in the 2006 report from the Caffeine for Apnea of Prematurity Trial (N Engl J Med. 2006 May 18;354[20]:2112-21). Ideally, researchers will soon run a large, randomized trial that can better address the questions that Dr. Amaro and her associates attempted to answer with their study.
Dr. Clifford W. Bogue is professor of pediatrics at Yale University, New Haven, Conn., and chaired the session where Dr. Amaro presented her report. He had no relevant disclosures. He made these comments in an interview.
BALTIMORE – Early initiation of caffeine treatment in premature neonates on mechanical ventilation did not cut the time to when these babies could successfully wean off the ventilator, according to findings of a single-center, randomized controlled study of 83 children.
The results also showed an “unexpected” trend toward increased mortality among the neonates who received early caffeine treatment, Dr. Cynthia M. Amaro reported at the annual meeting of the Pediatric Academic Societies. This signal of elevated mortality with caffeine treatment prompted the study’s data and safety monitoring board to prematurely stop the trial, limiting enrollment to just 75% of the number originally planned in the study’s design, thereby raising questions about the reliability of the primary-endpoint finding that early caffeine treatment did not result in the benefit of a reduced time to extubation.
Dr. Amaro said that she and her associates ran the study to address what had emerged as a significant area of doubt in routine U.S. practice on how to best use caffeine treatment in this neonatal population following publication of findings from the landmark Caffeine for Apnea of Prematurity (CAP) Trial (N Engl J Med. 2006 May 18;354[20]:2112-21). Results from the CAP Trial had shown in nearly 2,000 randomized, premature infants that treatment with caffeine led to significantly fewer episodes of bronchopulmonary dysplasia as well as quicker time to extubation of mechanical ventilation. Caffeine or other methylxanthines stimulate an infant’s respiratory center to allow faster extubation.
Ever since that publication a decade ago, “clinicians have been using caffeine earlier and more liberally, without really good data to support its early use in mechanically-ventilated preterm babies,” explained Dr. Amaro, a neonatologist at the University of Miami and Holtz Children’s Hospital in Miami.
Based on the new findings from the study she reported, “we are now not routinely initiating caffeine in mechanically ventilated preterm babies and just using caffeine immediately before extubation to treat apnea of prematurity. This returns caffeine treatment to the way it was used in the CAP Trial,” she said. “Further studies are needed before we can say what is best for early treatment of these preterm babies,” Dr. Amaro said in a video interview.
Her report led to a flurry of comments during the question period, with several pediatricians voicing concern about the reliability of results from a study that followed only 83 patients because of its premature termination.
“The data and safety monitoring board’s decision is a big issue,” said Dr. Carl E. Hunt, a pediatrician at the Uniformed Services University of the Health Sciences in Bethesda, Md. “There is a literature that shows results of studies can be very different when they stop early. It’s unfortunate because we don’t have other prospective data, and it may now be hard to do a large randomized, controlled trial” of early caffeine treatment, Dr. Hunt said.
While Dr. Amaro conceded that premature termination limited her study’s size, she also asserted that her analyses confirmed the validity of the finding of no benefit from early caffeine treatment. “We projected to full enrollment, and there still was no difference in the time to first successful extubation,” she said.
Her study enrolled preterm infants during January 2013–December 2015 born at 23-30 weeks’ gestation who required mechanical ventilation during their first 5 days. Randomization assigned 41 infants to receive a 20-mg/kg bolus of caffeine, followed by a maintenance dosage of 5 mg/kg that continued until extubation, while 42 patients received placebo and did not get caffeine until just before attempted extubation. The bolus and maintenance caffeine dosages tested were identical to those used in the CAP Trial.
The researchers defined successful extubation as keeping a child off restart of mechanical ventilation for more than 24 hours. The average gestational age of the enrolled neonates was 26 weeks, their average weight was 700 g, and intubation started an average of 3 hours after delivery.
The study’s primary endpoint, age at first successful extubation, was an average of 24 days among the neonates treated with caffeine and 20 days in those on placebo, Dr. Amaro reported. Mortality occurred at an average of 30 days after delivery in the caffeine recipients and after an average of 10 days in the controls. The incidence of death was 22% in those on early caffeine and 12% among those in the placebo group, an excess of four deaths in the intervention arm that was not statically significant.
A recent review of more than 29,000 matched very-low-birth-weight infants managed in routine practice showed that neonates who received early caffeine had an adjusted mortality risk that was 23% higher than that of matched infants not receiving early caffeine, Dr. Amaro noted (J Pediatrics. 2014 May;164[5]:992-8).
The incidence of bronchopulmonary dysplasia also did not show a statistically significant difference between the two study arms, 46% among those on early caffeine and 53% in the placebo group. Patients on early caffeine also had higher rates of necrotizing enterocolitis, more episodes of necrotizing enterocolitis requiring surgery, and more intraventricular hemorrhages, but none of these differences reached statistical significance.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BALTIMORE – Early initiation of caffeine treatment in premature neonates on mechanical ventilation did not cut the time to when these babies could successfully wean off the ventilator, according to findings of a single-center, randomized controlled study of 83 children.
The results also showed an “unexpected” trend toward increased mortality among the neonates who received early caffeine treatment, Dr. Cynthia M. Amaro reported at the annual meeting of the Pediatric Academic Societies. This signal of elevated mortality with caffeine treatment prompted the study’s data and safety monitoring board to prematurely stop the trial, limiting enrollment to just 75% of the number originally planned in the study’s design, thereby raising questions about the reliability of the primary-endpoint finding that early caffeine treatment did not result in the benefit of a reduced time to extubation.
Dr. Amaro said that she and her associates ran the study to address what had emerged as a significant area of doubt in routine U.S. practice on how to best use caffeine treatment in this neonatal population following publication of findings from the landmark Caffeine for Apnea of Prematurity (CAP) Trial (N Engl J Med. 2006 May 18;354[20]:2112-21). Results from the CAP Trial had shown in nearly 2,000 randomized, premature infants that treatment with caffeine led to significantly fewer episodes of bronchopulmonary dysplasia as well as quicker time to extubation of mechanical ventilation. Caffeine or other methylxanthines stimulate an infant’s respiratory center to allow faster extubation.
Ever since that publication a decade ago, “clinicians have been using caffeine earlier and more liberally, without really good data to support its early use in mechanically-ventilated preterm babies,” explained Dr. Amaro, a neonatologist at the University of Miami and Holtz Children’s Hospital in Miami.
Based on the new findings from the study she reported, “we are now not routinely initiating caffeine in mechanically ventilated preterm babies and just using caffeine immediately before extubation to treat apnea of prematurity. This returns caffeine treatment to the way it was used in the CAP Trial,” she said. “Further studies are needed before we can say what is best for early treatment of these preterm babies,” Dr. Amaro said in a video interview.
Her report led to a flurry of comments during the question period, with several pediatricians voicing concern about the reliability of results from a study that followed only 83 patients because of its premature termination.
“The data and safety monitoring board’s decision is a big issue,” said Dr. Carl E. Hunt, a pediatrician at the Uniformed Services University of the Health Sciences in Bethesda, Md. “There is a literature that shows results of studies can be very different when they stop early. It’s unfortunate because we don’t have other prospective data, and it may now be hard to do a large randomized, controlled trial” of early caffeine treatment, Dr. Hunt said.
While Dr. Amaro conceded that premature termination limited her study’s size, she also asserted that her analyses confirmed the validity of the finding of no benefit from early caffeine treatment. “We projected to full enrollment, and there still was no difference in the time to first successful extubation,” she said.
Her study enrolled preterm infants during January 2013–December 2015 born at 23-30 weeks’ gestation who required mechanical ventilation during their first 5 days. Randomization assigned 41 infants to receive a 20-mg/kg bolus of caffeine, followed by a maintenance dosage of 5 mg/kg that continued until extubation, while 42 patients received placebo and did not get caffeine until just before attempted extubation. The bolus and maintenance caffeine dosages tested were identical to those used in the CAP Trial.
The researchers defined successful extubation as keeping a child off restart of mechanical ventilation for more than 24 hours. The average gestational age of the enrolled neonates was 26 weeks, their average weight was 700 g, and intubation started an average of 3 hours after delivery.
The study’s primary endpoint, age at first successful extubation, was an average of 24 days among the neonates treated with caffeine and 20 days in those on placebo, Dr. Amaro reported. Mortality occurred at an average of 30 days after delivery in the caffeine recipients and after an average of 10 days in the controls. The incidence of death was 22% in those on early caffeine and 12% among those in the placebo group, an excess of four deaths in the intervention arm that was not statically significant.
A recent review of more than 29,000 matched very-low-birth-weight infants managed in routine practice showed that neonates who received early caffeine had an adjusted mortality risk that was 23% higher than that of matched infants not receiving early caffeine, Dr. Amaro noted (J Pediatrics. 2014 May;164[5]:992-8).
The incidence of bronchopulmonary dysplasia also did not show a statistically significant difference between the two study arms, 46% among those on early caffeine and 53% in the placebo group. Patients on early caffeine also had higher rates of necrotizing enterocolitis, more episodes of necrotizing enterocolitis requiring surgery, and more intraventricular hemorrhages, but none of these differences reached statistical significance.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Early caffeine treatment of premature neonates on mechanical ventilation did not reduce the time to extubation and produced a trend toward increased mortality.
Major finding: The age of first successful extubation averaged 24 days in infants receiving caffeine and 20 days among controls.
Data source: Single-center, randomized, controlled study of 83 premature neonates.
Disclosures: Dr. Amaro had no disclosures.